Superficial Cortical Venous Network
An extensive network of interconnected veins, highly variable in size, route, and drainage pathway, subserve venous egress of the cerebral convexity. These veins typically drain the cortex and some underlying deep white matter. Most of hemispheric white matter drains into the deep veins (such as longitudinal caudate veins and lateral atrial veins, and then into the internal cerebral vein). Some of the more constantly noted channels have names. The extent of anastomotic connections between these veins determines the depth of system “reserve” should some portion of the network become dysfunctional. For example, a surgeon can divide a temporal cortical vein in presence of anastomoses to the frontal or parietal network. A large isolated drainage channel cannot be sacficed without substantial risk of a venous infarction. The same goes for deep venous thrombosis, having some bearing on presence and extent of hemorrhagic infarction depending on level of collateral support.
Various names exist for the anastomotic veins of the convexity, however even when no functionally competent anastomosis exists the veins usually keep their names. The vein of Trolard is a large posterior frontal vein (usually in the post-central sulcus) draining into the superior sagittal sinus. The Rolando is a named vein, running by definition in the Rolandic sulcus, anterior to Trolard. Trolard, by the way, is just a name for a big parietal vein — superior, inferior parietal, whatever. The Labbe is the largest vein draining the temporal convexity towards the transverse or sigmoid sinus. The superficial sylvian vein collects tributaries from the region of the operculum and adjacent cortex and has a variable pattern of drainage. Variability is the rule. All sorts of percentages of dominance are found in venerable texts. The bottom line is that anything from a balanced network of interconnected Trolard, Labbe, and Sylvian veins to essentially separate drainage, to dominance of one channel at expense of others is illustrated below. The key is to understand which way venous blood is leaving the brain, and what constraints this may impose on a potential surgical approach or endovascular embolization.
Below are some illustrations of variable superficial drainage patterns.
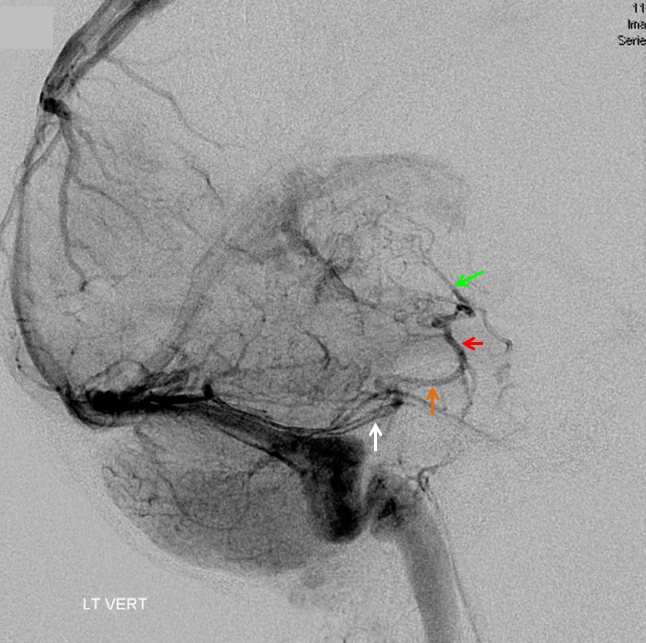
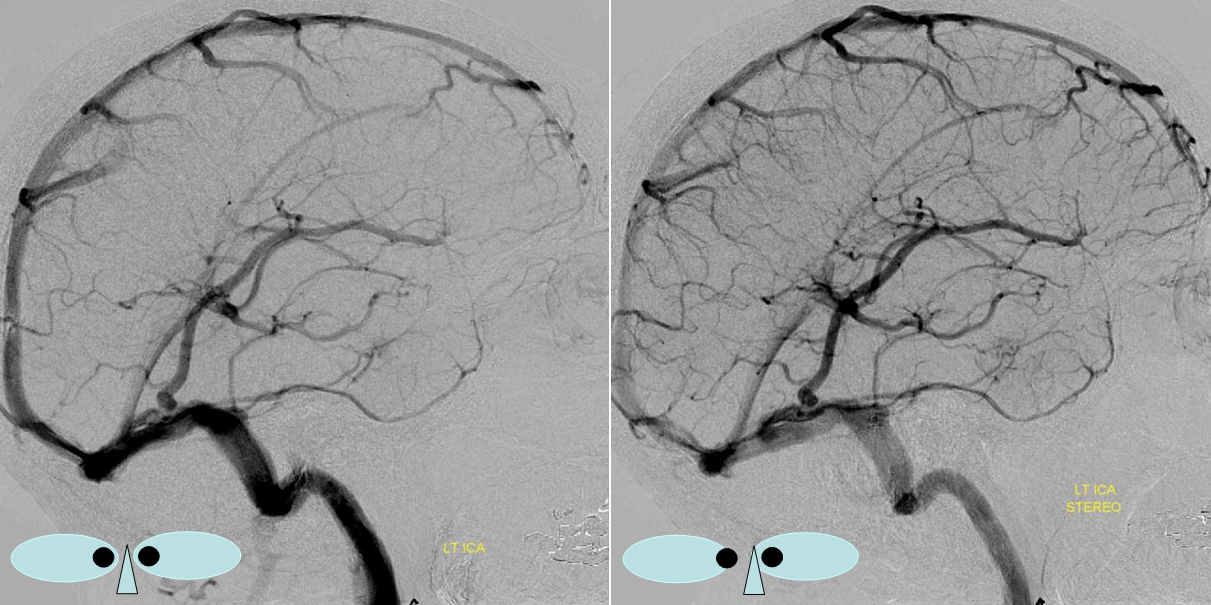
Balanced pattern. The Trolard, Labbe, and Sylvian veins are interconnected in the region of the posterior Sylvian fissure. Any one of these veins can be sacrificed with very low risk of venous infarction. Also notice a sigmoid emissary vein (unmarked).
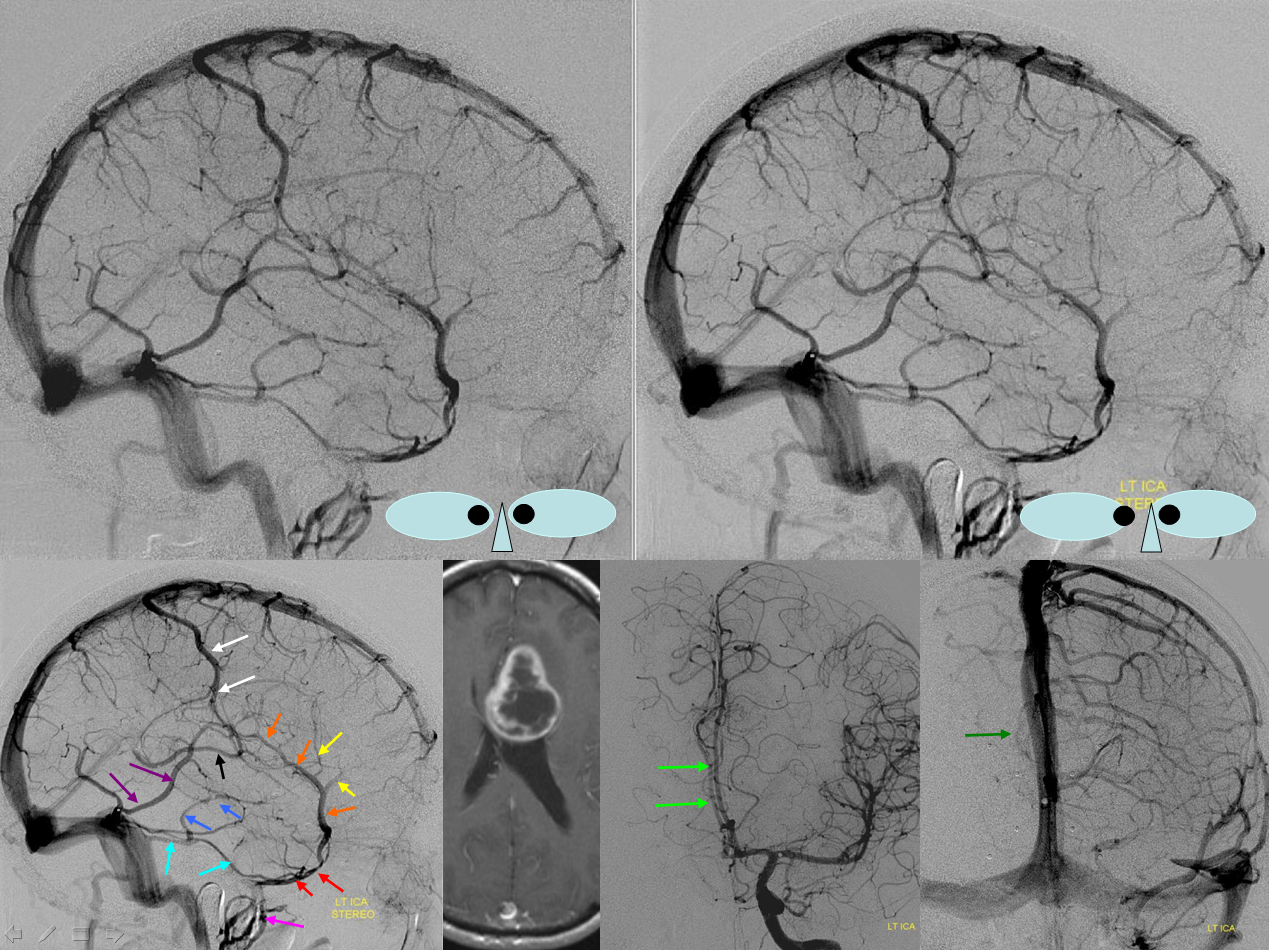
White=Trolard. Orange=Superficial Sylvian Vein draining into sphenoparietal sinus (red) and into the pterygopalatine venous plexus (pink). Purple=Labbe. Notice variant drainage of the basal vein (blue) into the superior petrosal sinus (light blue). Midline shift is evident on AP views (green)
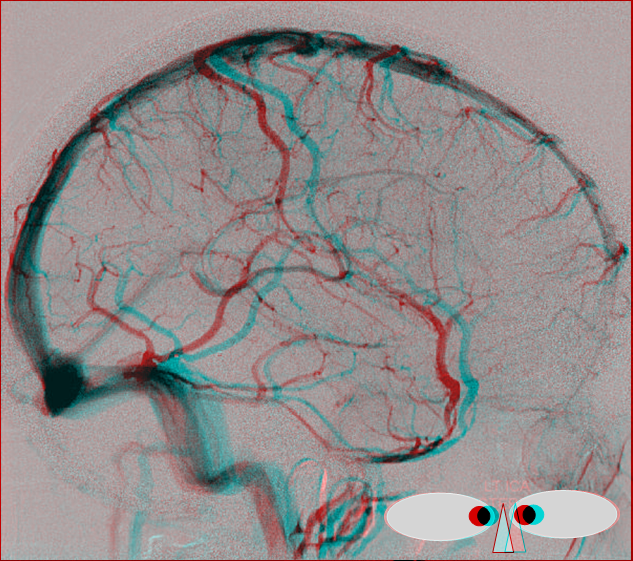
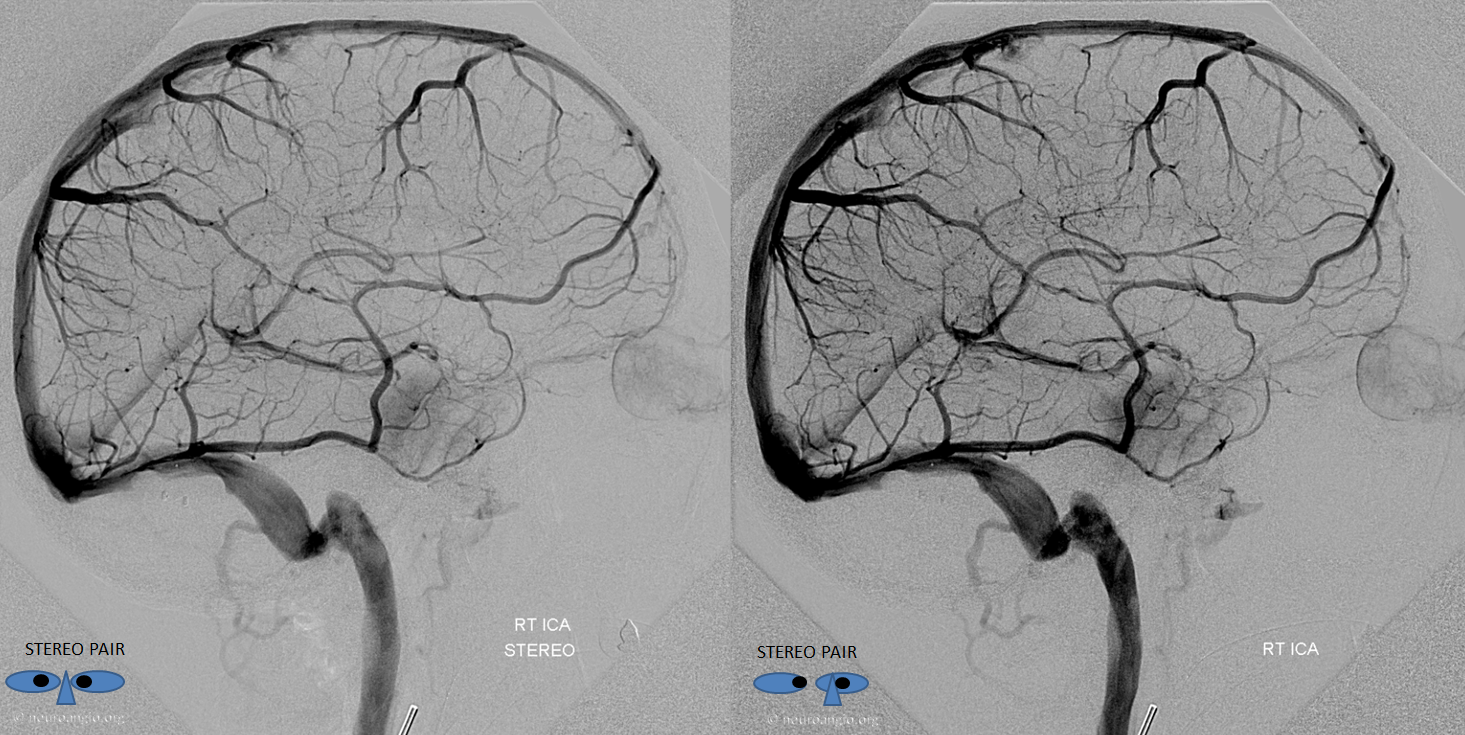
Anaglyph Stereo Below
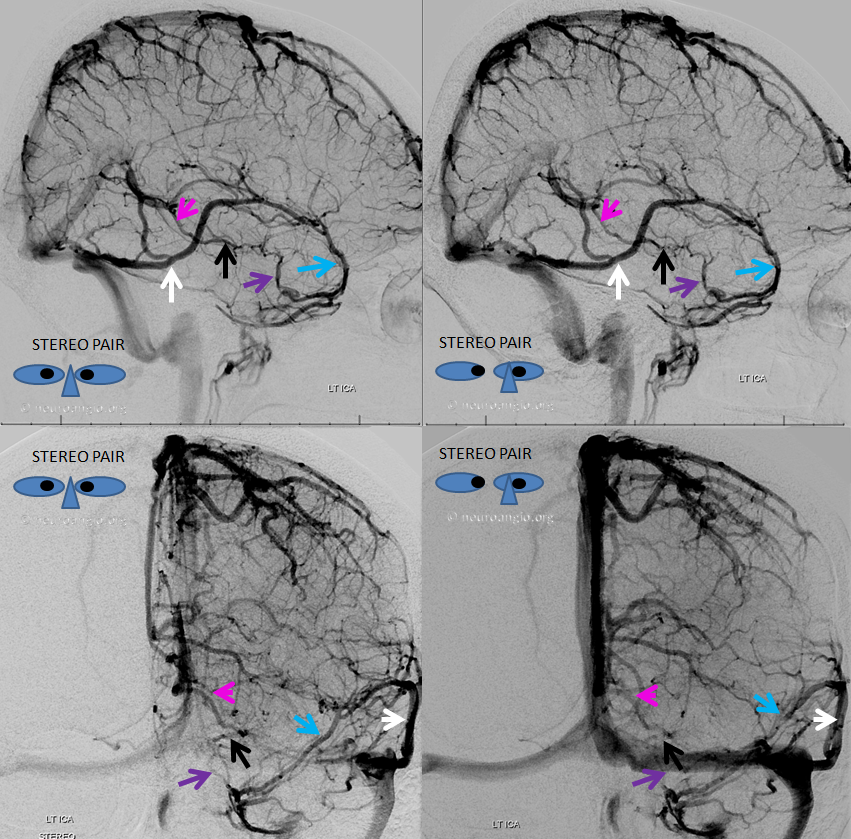
Another illustration of the balanced pattern with a somewhat more dominant Trolard.
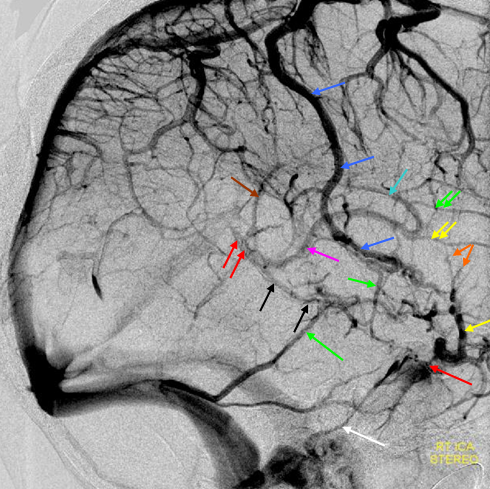
Trolard=dark blue. Labbe=green. Superficial Sylvian vein/ sphenoparietal sinus=yellow. Notice that Trolard-Labbe anastomosis is much lower over temporal convexity than in the previous figure. Cavernous sinus=red. Basal vein=black. Galen=red. Internal Cerebral vein=pink. Thalamostriate vein=light blue. Anterior caudate vein=double green.
Perfectly balanced pattern
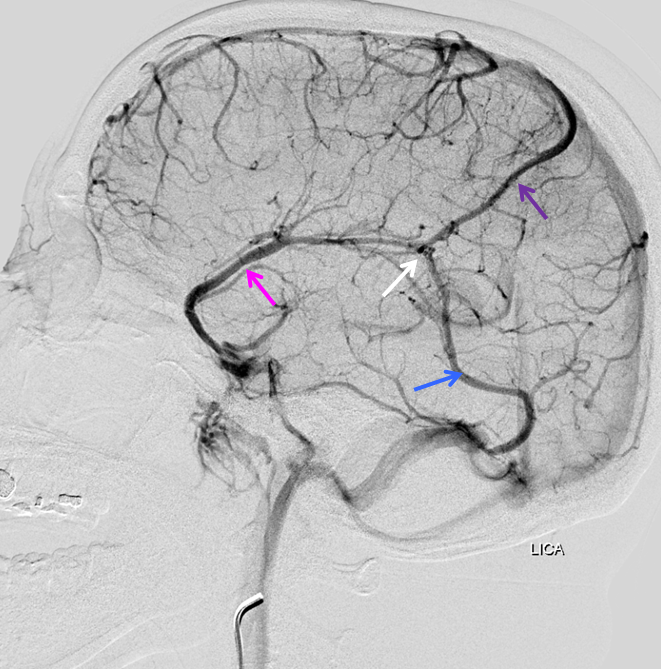
Equal sized Trolard (purple), Labbe (blue), and Superficial Sylvian (pink) veins, all connected to each other (white arrow).
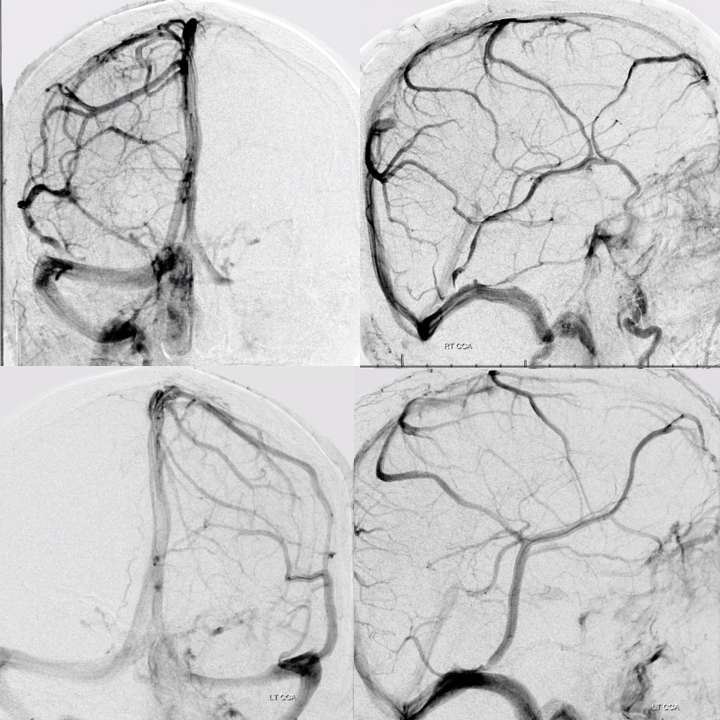
Another example of highly collateralized surface cortical veins, bilaterally in this case
Another example of collateral connections between the Labbe (white) and Superficial Sylvian (blue) veins. Also notice full extent of the basal vein (purple, black, pink arrows) from the cavernous sinus to the Galen.
Here is an example of an anastomosis between the Labbe and a frontal vein, draining into the proximal superior sagittal sinus (no labels)
Dominant Labbe Pattern. As you can seen, the Labbe is draining a huge swath of the cortex, capturing Sylvian territory with a hypoplastic sphenoparietal sinus. Many frontoparietal cortical veins empty into the Superior Sagittal Sinus without connection to the Labbe. This is the kind of Labbe you cannot sacrifice. Also, lack of anastomoses imposes a relative inflexibility to the system with relatively little “reserve” should one of these channels close. Various books report that a dominant Labbe is more common on the left (dominant temporal lobe), whereas the trolard is on the right. That is certainly true, except when its not.
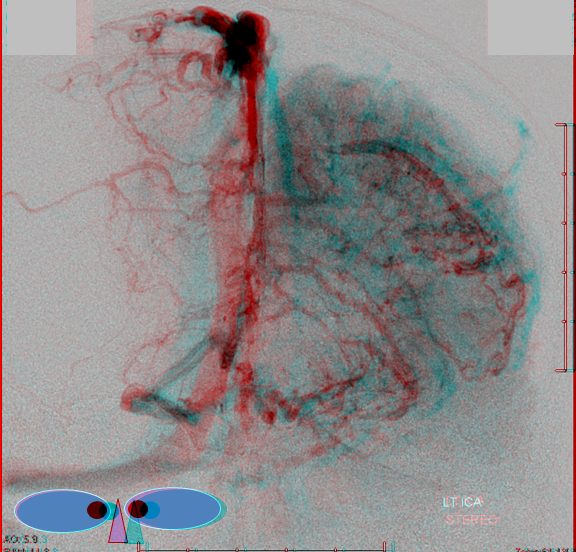
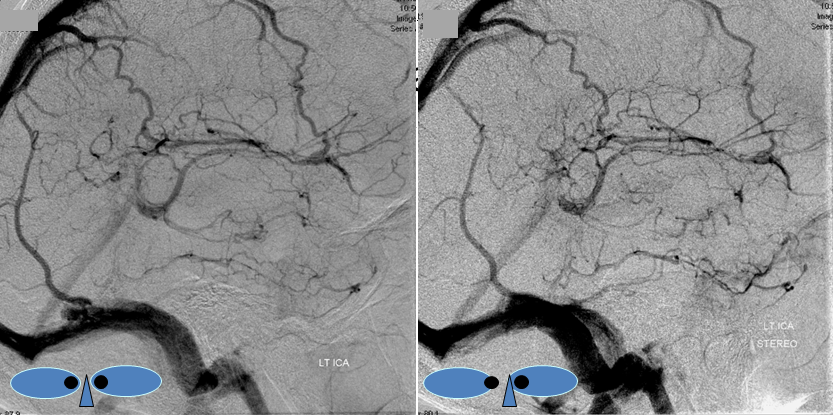
Anaglyph
Labbe=dark blue. Inferior temporal vein=beige. Inferior sagittal sinus=light blue. Straight sinus=black. Basal vein=red. Internal Cerebral Vein=green. Notice dominance of drainage to the sigmoid sinus system with no visualization of the sphenoparietal sinus or cavernous sinus. The basal vein drains exclusively posterior. This patient would be very unlikely to tolerate sigmoid sinus or straight sinus thrombosis.
Another Dominant Labbe pattern on the left. Labbe capturing sylvian vein territory.
Sylivan veins=purple. Labbe=whte. Basal vein=pink. Deep middle cerebral vein=light blue.
Stenosis at Cortical Vein and Sinus Confluence
There is often seen a narrowing in the caliber of a cortical vein when it enters a sinus — either when passing through the dura, or because cortical veins, especially large ones, sometimes have a variable-length dural segment right before entry into the named sinus. Various explanations for this have been advanced, such as narrowing acting as a valve to limit drastic changes in cortical venous pressure during sudden and potentially harmful sinus pressure elevations, such as during Valsalva, standing on ones head in the gymnastics class, etc. Here is an example of such narrowing (pink arrows) in a dominant labbe. The important point is that this narrowing is non-pathologic. Pay attention to these and you will see many more. Also note a well-developed anterior cerebral vein (red, more below)
Pseudo-Labbe Dominance. Giant vein, not Labbe but temporo-occipital vein collecting sylvian and large swaths of convexity territory in a patient with underdeveloped cavernous and petrosal sinuses. Notice how this drainage affects the transverse sinus, which is hypoplastic proximal to the temporo-occipital vein.
Light Blue=sylvian network. Dark blue = temporooccipital vein. Orange = Labbe. White=left transverse sinus. Green= right transverse sinus. Purple=inferior sagittal sinus. Pink=dural sinus channel separate from the straight sinus. Red=Galen. Black = straight sinus.
Although veins like to travel in sulci and fissures, particularly the sylvian fissure, it need not always be the case. The Labbe is probably the most common vein which disregards the fissure, as seen below. This is of course important to the surgeons who may need to preserve such a vein during splitting of the Sylvian fissure

The Labbe term is fairly loose — the idea is of an inferior anastomotic vein. Its classic insertion is at the transverse/sigmoid junction. However variation is rule again. Below is an example of Labbe-like vein, however it joins a short dural venous channel quite posteriorly before emptying into the mid-transverse sinus. Note good connections with mid- and posterior frontal veins that join the SSS
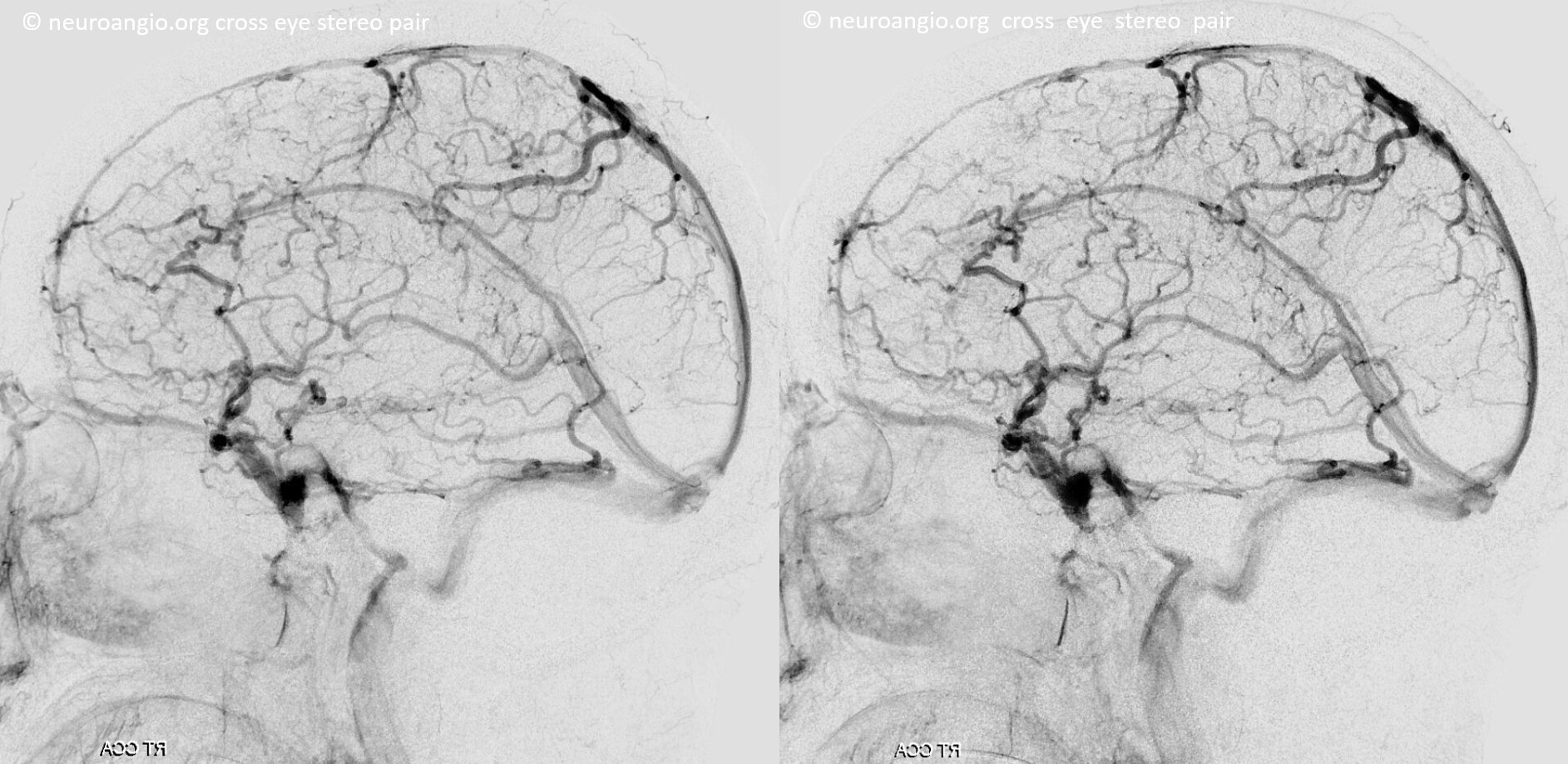
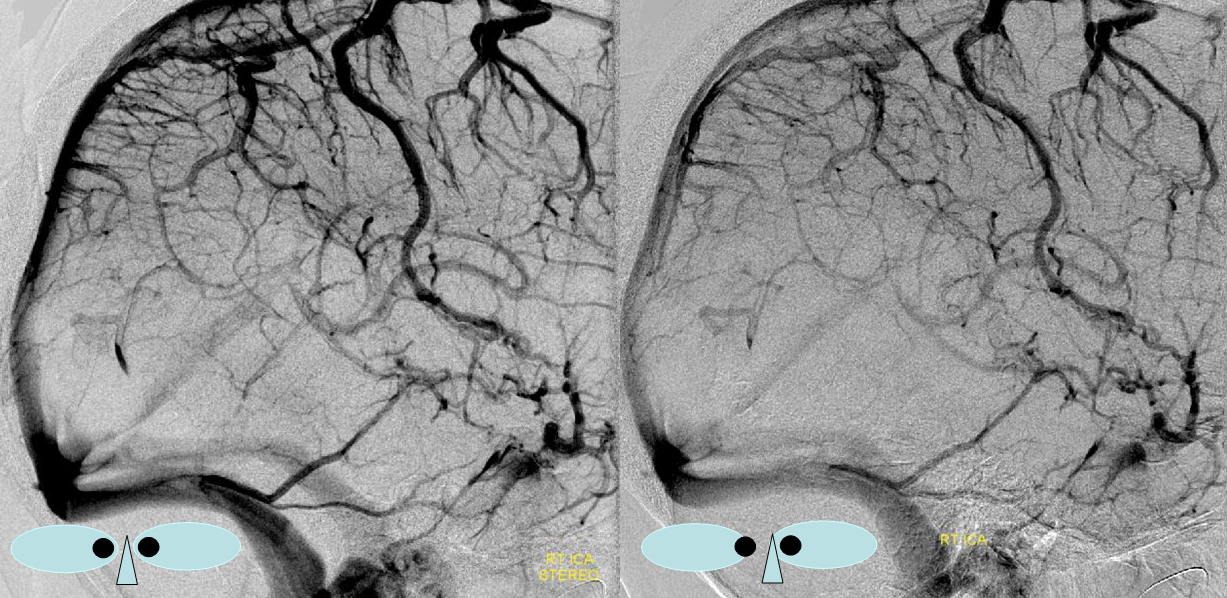
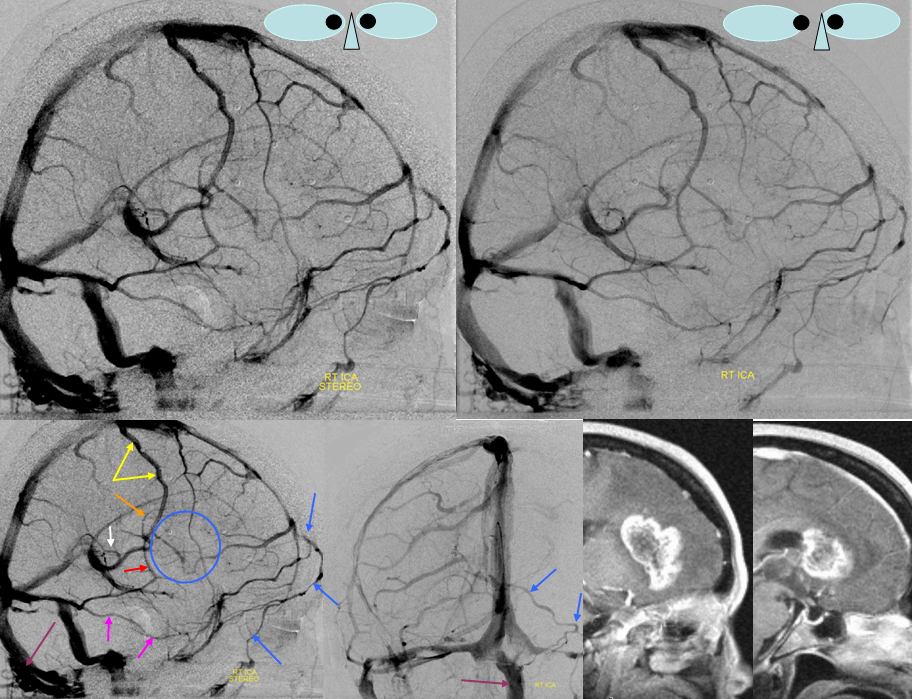
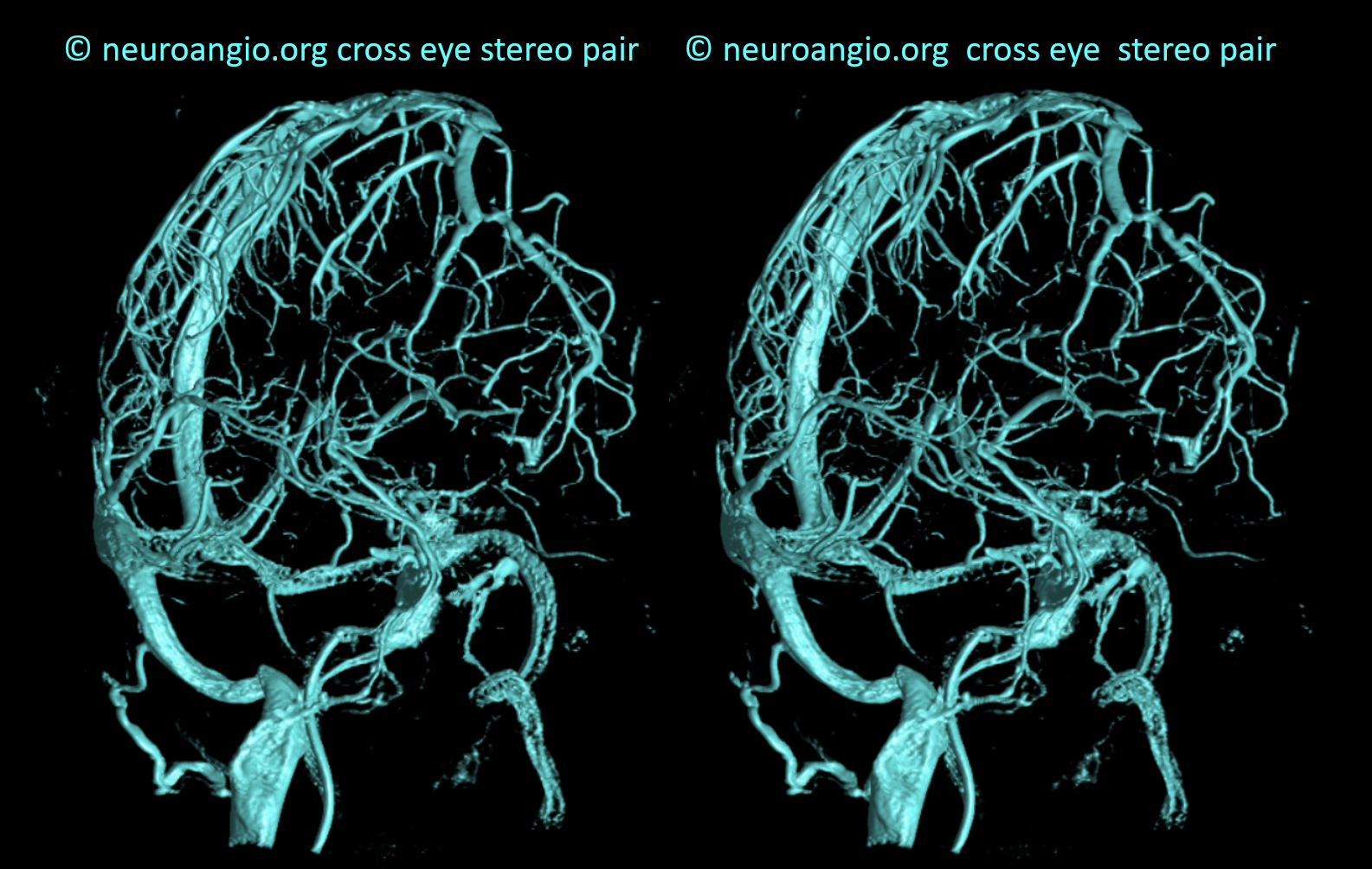
Dominant Rolando
The vein of Rolando (the giant one in the center of the image pair) is situated, appropriately in the Rolandic region, anterior to the Trolard. This extreme example of Rolando dominance of the entire hemisphere convexity illustrates the extent to which a single vein can occasionally assume control of the lateral surface territory. This pattern of very limited flexibility carries relatively very high risk of venous infarction should any misfortune (DVT, iatrogenic injury, etc) befall the dominant vein. On a personal note, I think that these extremes are more likely to be associated with additional vascular abnormalties or variants. This patient has a cavernous angioma with an associated DVA in the posterior right temporal lobe (not shown)
Dominant Superficial Sylvian Veins
The superficial sylvian veins outline the sylvian fissure, coursing inferiorly to mark the anterior aspect of the temporal lobe, and typically draining either into the cavernous sinus, paracavernous sinus (or cavernous sinus lateral compartment, if you wish), or the superior petrosal sinus. Here is an example of markedly dominant superficial sylvian veins (blue), in this case emptying into the cavernous sinus (white)
As is often the case, when Sylvian veins are dominant, several venous channels run in parallel to converge on the sinus, as is well-illustrated above. This arrangement is not commonly seen elsewhere — one might expect these veins to form a common trunk. It also brings up the somewhat obscure but embryologically important discussion regarding the existence of the “sphenoparietal” sinus. There are no less than 4 separate veins here so at least some are draining into the cavernous sinus directly — perhaps all of them. See “Cavernous Sinus” page for more on this exciting topic.
Here is a stereo image of the above. Isn’t stereo cool?
Anaglyph stereos
Dominant Superficial Sylvian Vein Pattern
The Superficial Sylvian vein is dominant, draining into a large superior petrosal sinus via the inferior temporal vein. The cavernous sinus drainage pathway is hypoplastic.
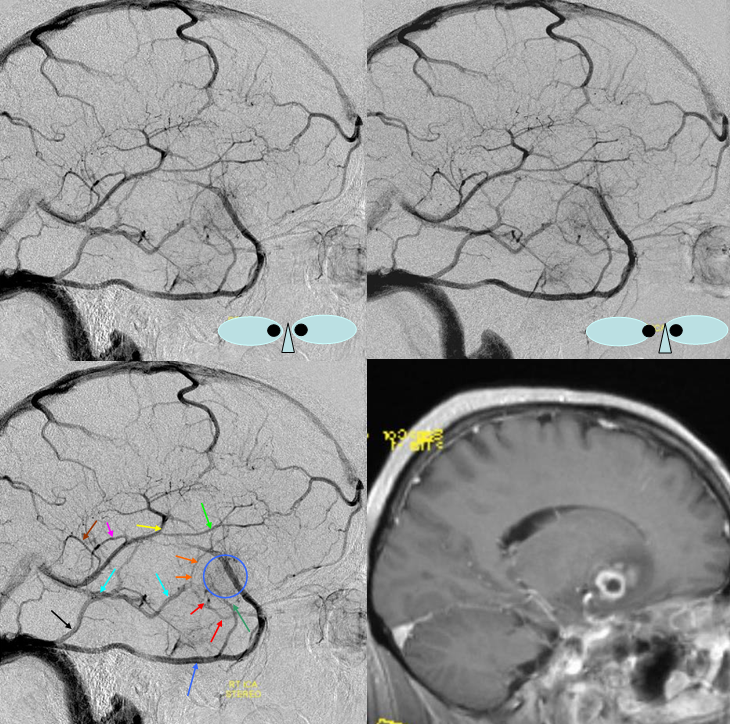
Blue Circle=tumor blush. The superficial sylivan vein is prominent within the circle and extends over the temporal lobe towards the superior petrosal sinus (dark blue arrow). Labbe=black. No trolard is seen, various superior cortical veins drain into the SSS. Basal vein=light blue, dominant posterior drainage. Very nice demonstration of the deep venous system tributaries. Anterior Septal vein=bright green, capturing territory of hypoplastic anterior cerebral vein. The inferior sagittal sinus is absent. Thalamostriate vein with large longitudinal caudate vein=yellow. Direct lateral vein=pink. Posterior caudate/splenial veins=brown.
Discontinuous pattern with cavernous sinus drainage of the Sylvian vein. Unlike the above example, the Sylvian vein drains into the sphenoparietal sinus and subsequently into the cavernous sinus, as is usual. A giant recurrent paraophthalmic segment aneurysm is partially filled with coils.
Sylvian Tributaries over frontotemporal operculum=Dark blue. Sylvian vein/sphenoparietal sinus=light blue. Cavernous sinus=purple. Inferior petrosal sinus=orange. Ovale drainage of the cavernous sinus=white. Pterygopalatine fossa veins=red. Labbe=pink. Thalamostriate=yellow. ICV=black.
Sylvian Drainage into Diploic Veins
Probably the most variable kind of drainage of the surface cortical veins belong to the sylvian ones. They can go many places. Cavernous, laterocavernous, superior petrosal, paracavernous sinuses are all possibilities. Here angio shows lots of pterygopalatine fossa veins. Why? The superficial sylvian veins drain via diploic / emissary veins into the temporalis and pterygopalatine venous plexi. The deep sylvian veins drain into the cavernous sinus, which also empties into the pterygopalatine plexus via the IPS.
Best seen on movie of venous phase flat panel axial MIPS — pause and scroll thru individual images
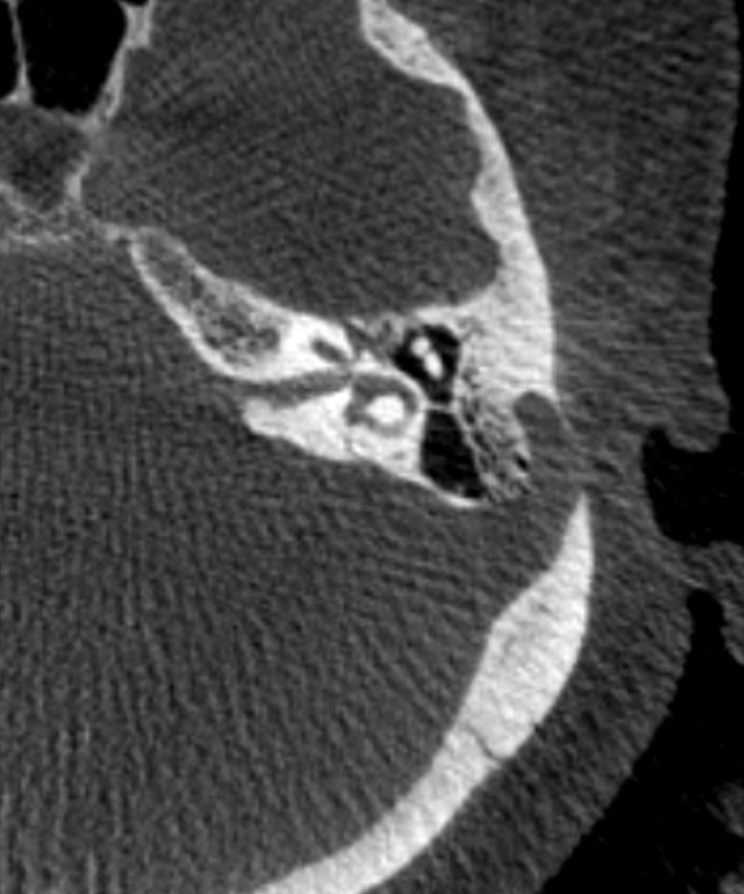
Bone windows — not very impressive are they? Certainly nothing that would be identified preoperatively
Check out venous phase reconstruction VR images
AND — look at that giant sigmoid sinus diverticulum — of course, it is a post-stenotic diverticulum, like most of them are. See Pulsatile Tinnitus page for more info. The diverticulum is well seen in images above also. There was no pulsatile tinnitus in this case.
Paracavernous Sinus — also more broadly can be considered as another dural venous channel. Sylvian veins join sinus channel which runs straight down to the middle fossa base — usually into Ovale. On the right — there is also some drainage into the cavernous sinus. On the left is all into the “paracavernous” one.
MRI — volumetric post — see if you can identify the same structures here.
Dominant sylvian vein egress sacrifice
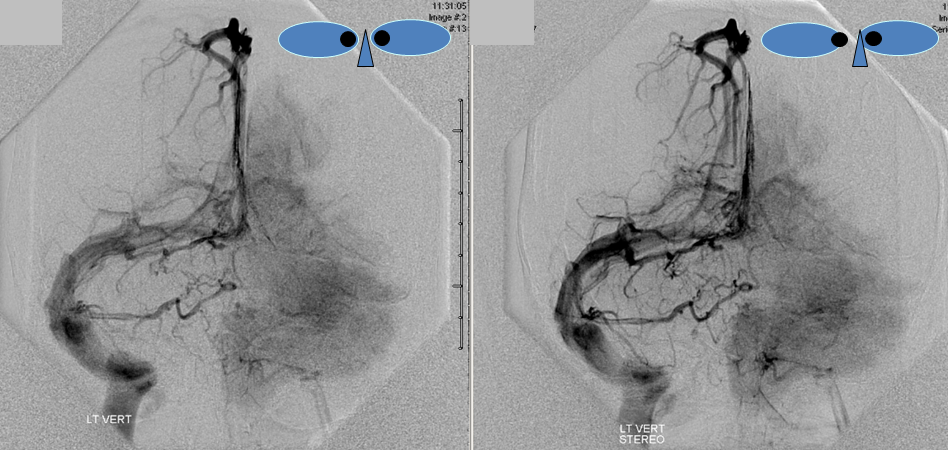
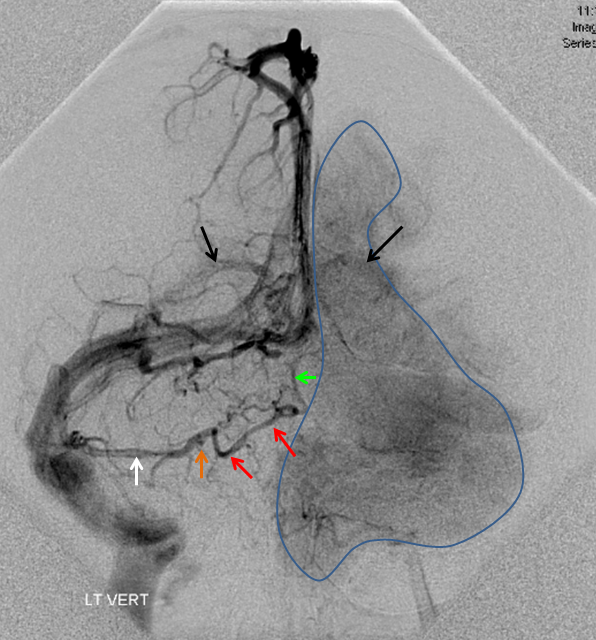
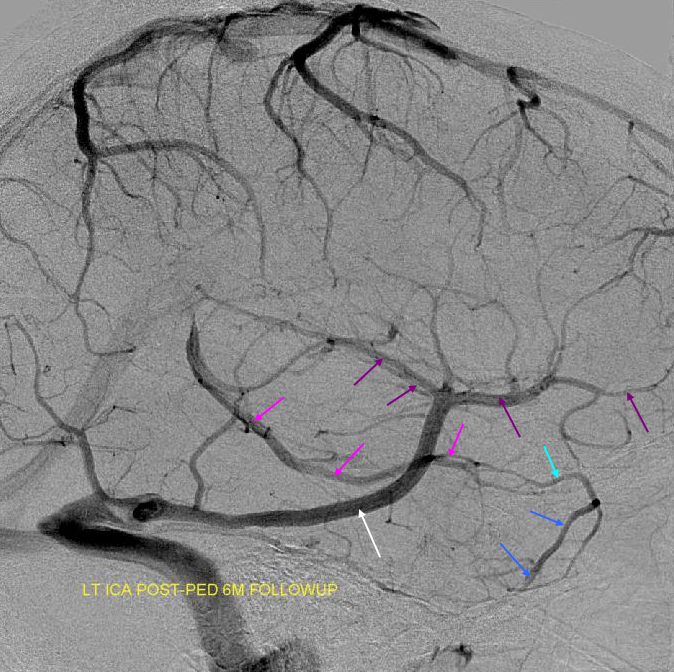
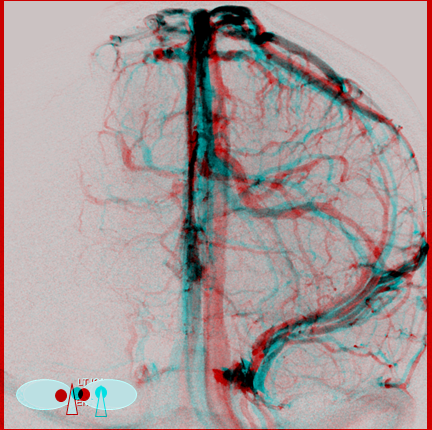
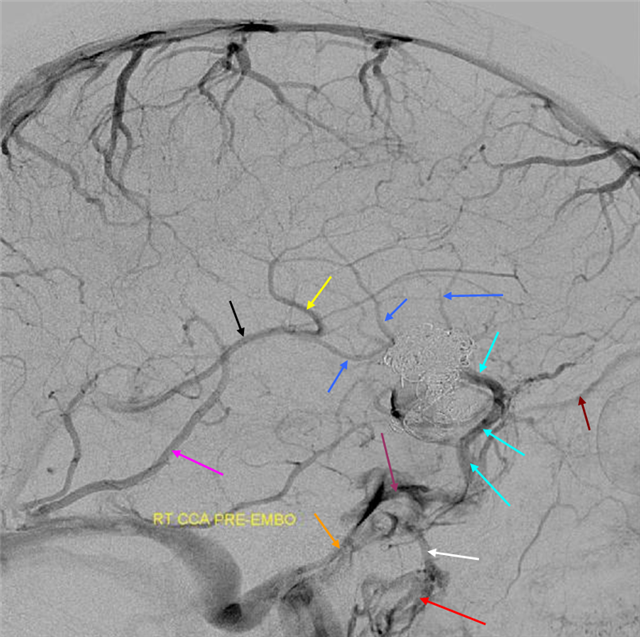
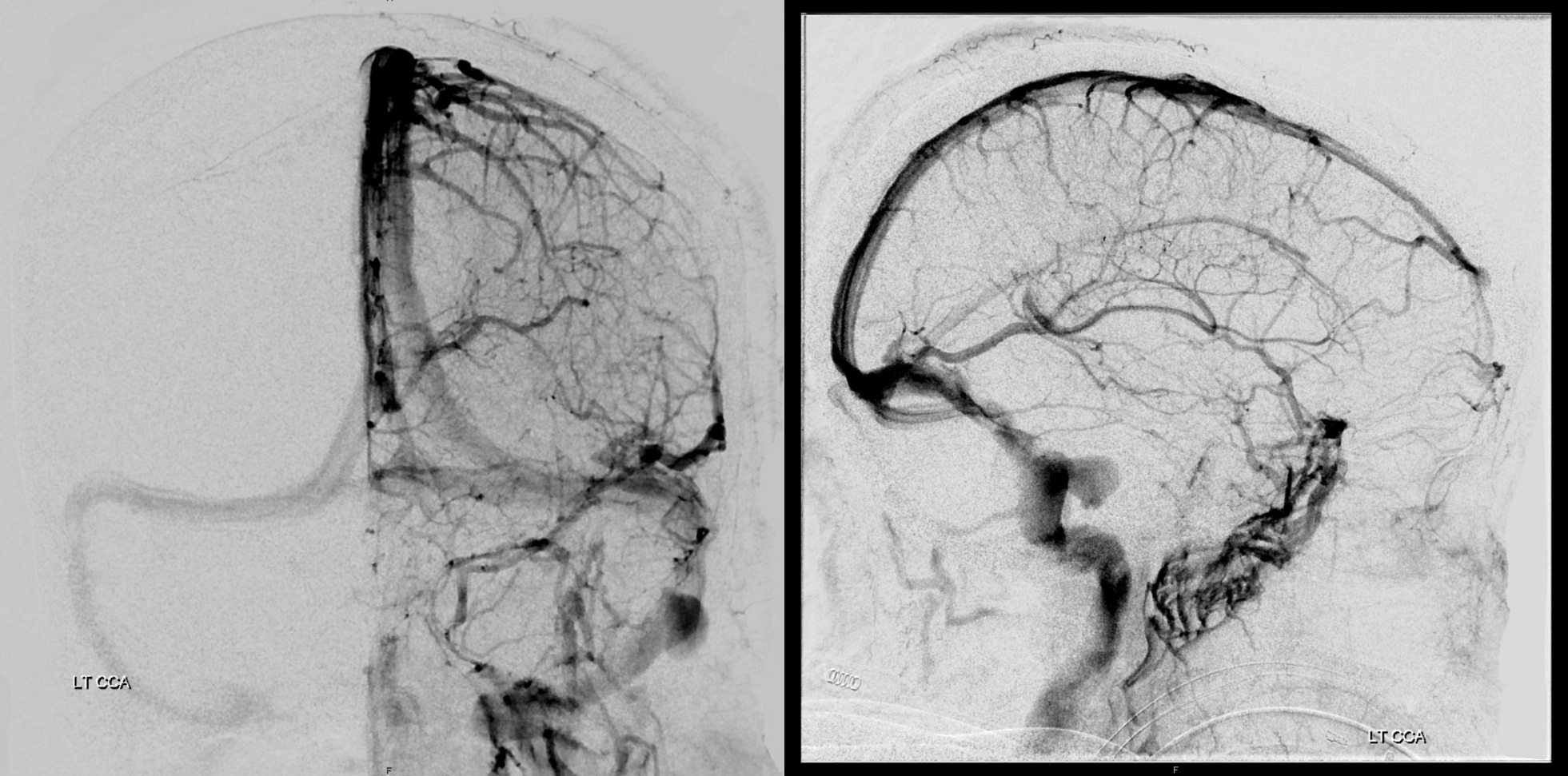
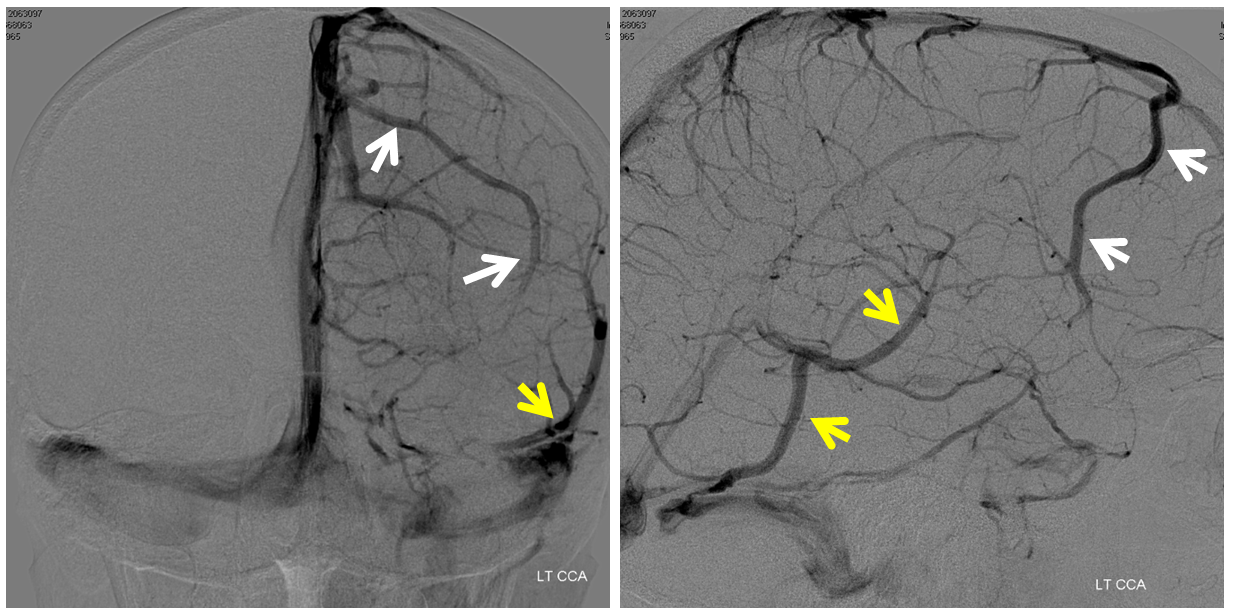
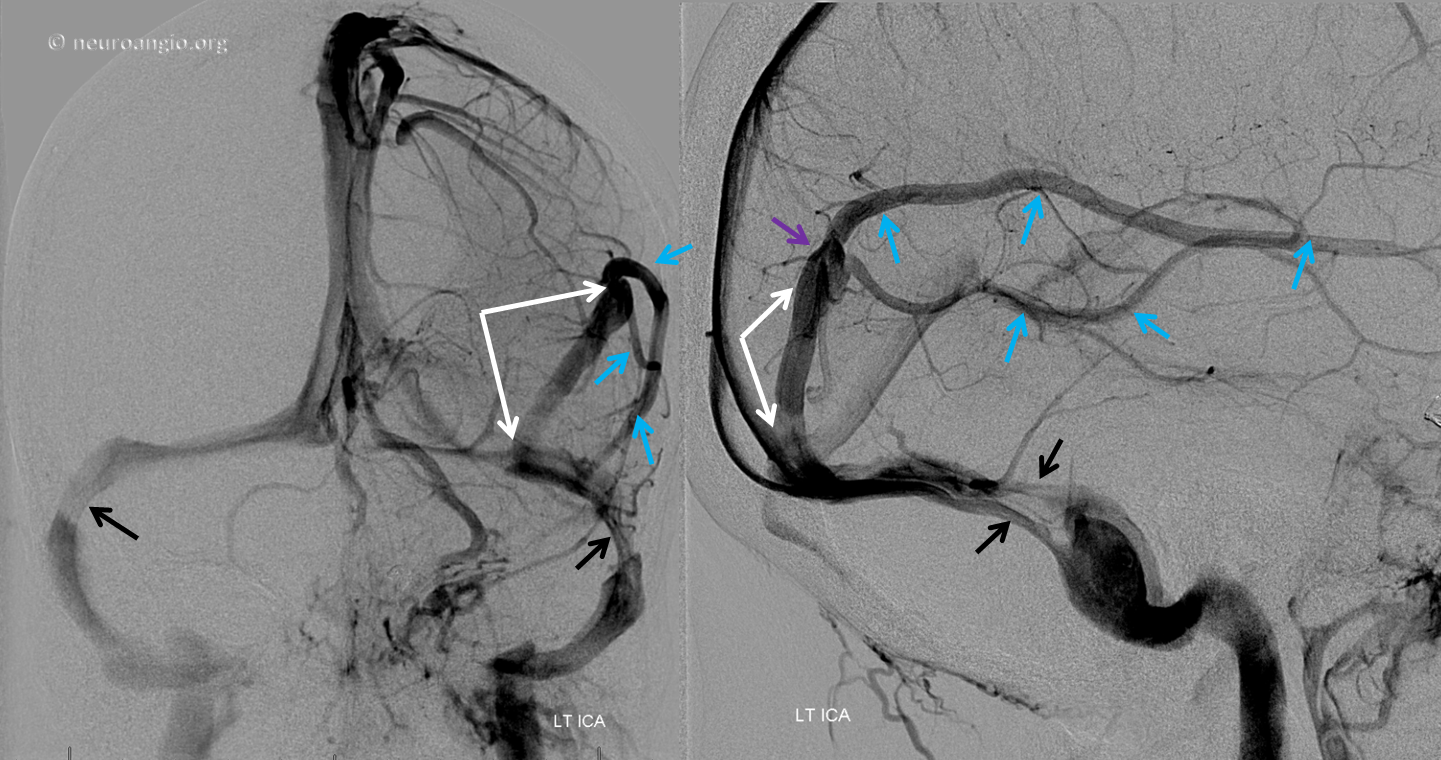
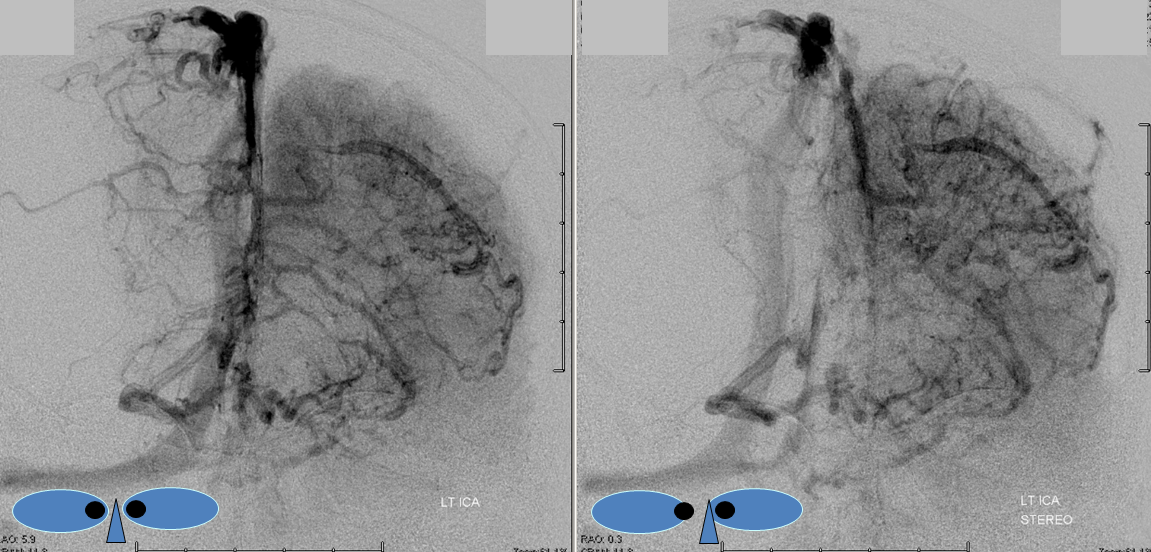
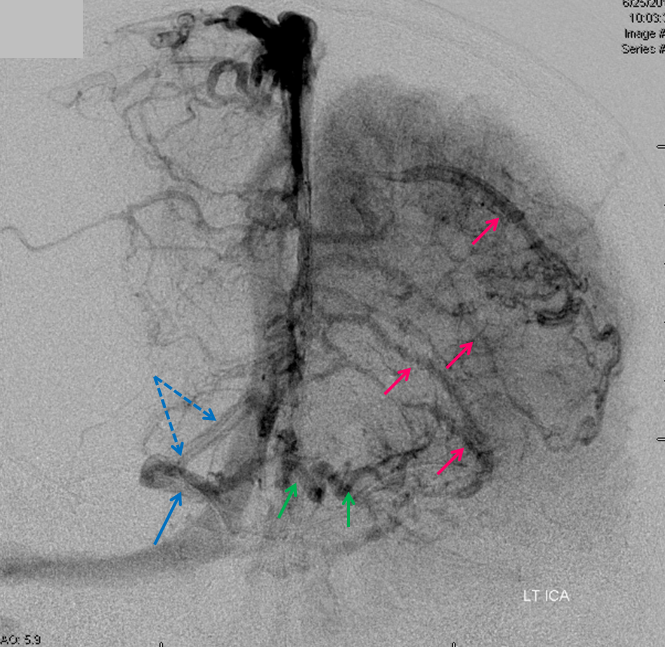
In this patient with a large right temporal lobe hematoma from a surface/pial AVM rupture, the Sylvian vein constitutes primary drainage of the temporal lobe and operculum via the sphenoparietal sinus into the cavernous sinus. No effective Labbe or Trolard type collateral to the sylvian region exists. (LEFT) The AVM was embolized and resected. The sphenoparietal sinus was sacrificed during surgery. Postoperative angiogram (RIGHT) demonstrates marked congestion of the surface hemispheric veins which via multiple small collateral pathways are straining to drain the Sylvian vein territory into the superior sagittal sinus. There was no hemorrhage.
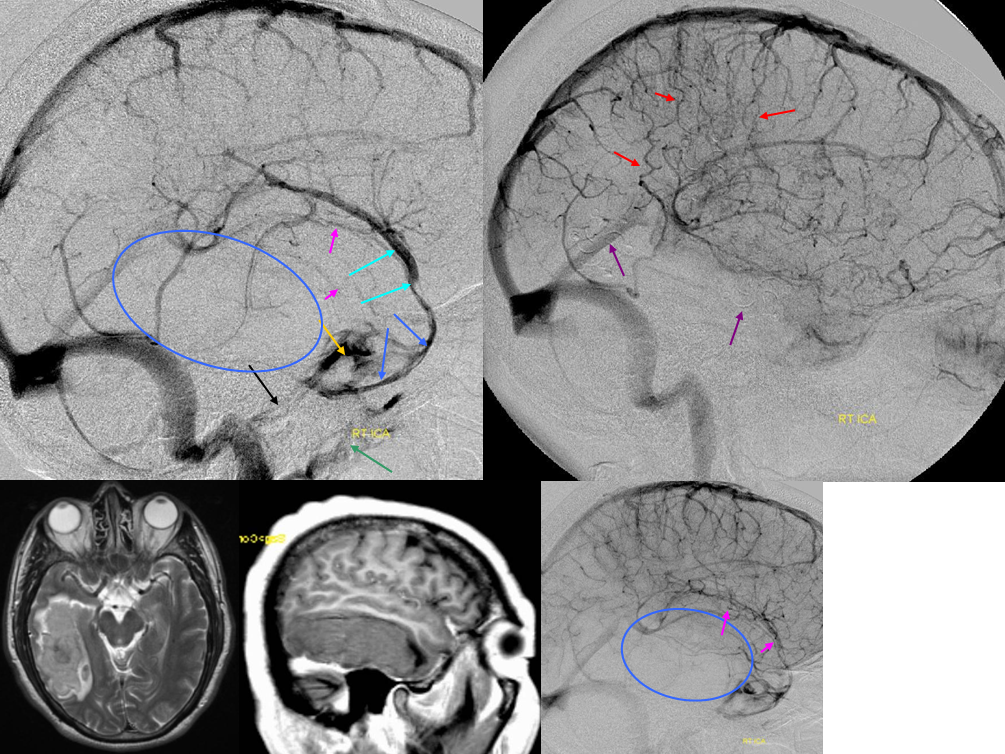
Superficial sylvian vein = light blue. Sphenoparietal sinus = dark blue. Cavernous sinus = orange. Inferior petrosal sinus = black. Pterygopalatine venous plexus = green. Mass = blue oval. Mass effect on Sylvian veins=pink. Congested small veins = red.
Sylvian-Labbe Collateral Pattern s/p sigmoid sinus occlusion:
MRI showing a meningioma filling up the right sigmoid sinus. Angio confirms sinus occlusion. The Labbe is rerouted into the sylvian network, which due to hypoplasia of the cavernous sinus outflow drains into a very capacious basal vein.
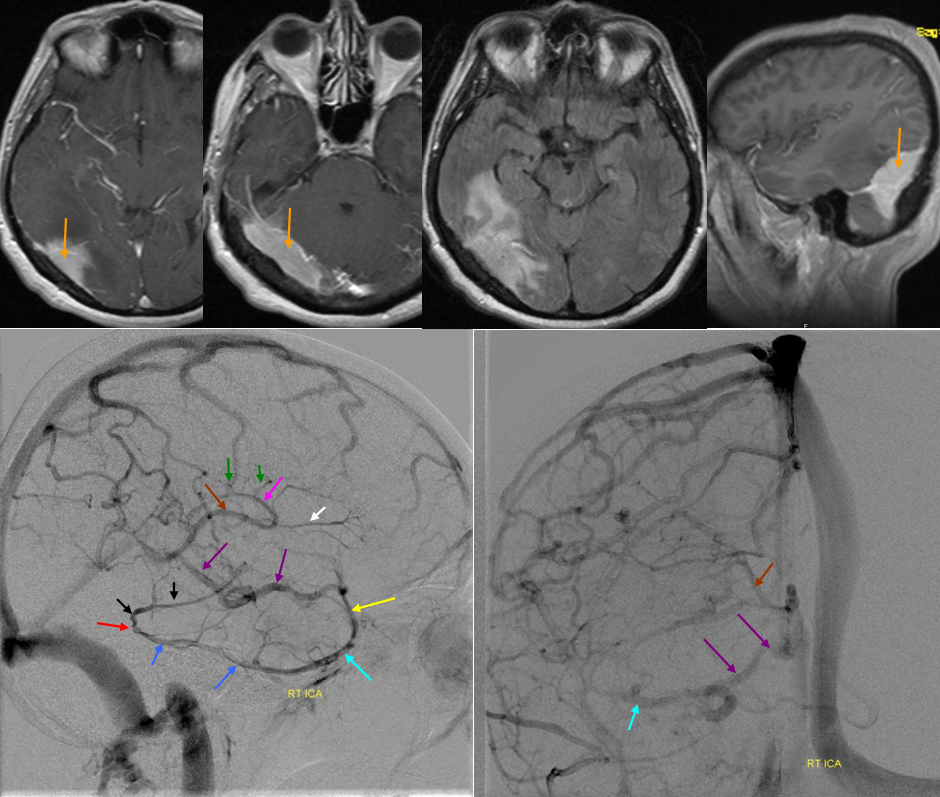
Red=occluded Labbe Segment. Dark Blue=labbe; Light blue=superficial sylvian vein; black=inferior parietal vein; yellow=deep sylvian vein; purple=basal vein; white=anterior septal vein; pink=thalamostriate vein; green=longitudinal caudate tributaries of the thalamostriate vein; brown=internal cerebral vein; orange=meningioma occluding right transverse/sigmoid sinus
Dominant Trolard Pattern. The Trolard is dominant with anastomosis to a smaller Labbe. This Trolard can probably be sacrificed. Notice also a somewhat strange pattern of inferior frontal venous drainange coming over the anterior portion of the SSS to empty contralaterally.
Trolard=yellow. Notice mass effect from tumoral edema/infiltration on the inferior portion of the Trolard (red). Mass effect on the thalamostriate vein (orange). Frontal vein with anomalous drainage = dark blue. Superior petrosal sinus=pink. Notice a very large occipital sinus also=purple.
Dominant Rolando with connection to the deep middle cerebral vein. Numerous anastomoses between “superficial” and “deep” system make this classification somewhat misleading. Its important to keep this in mind. Here, a large Trolard (red) is continuous inferiorly with the deep middle cerebral vein (the most inferior red arrow) draining into the cavernous sinus.
Rolando=red. Deep Middle Cerebral vein=black. Cavernous sinus=white. Anastomotic vein between SSS and ISS=yellow. Basal Vein=pink. Superior Petrosal sinus=Dark blue. Inferior petrosal sinus=light blue. Tumor blush=blue circle
Anterior Frontal Veins — beware the first 1/3rd of the superior sagittal sinus
There is an old rule in neurosurgery, which says that taking (occluding) the first /anterior third of the superior sagittal sinus is generally a safe thing to do. That is certainly true, and the reason for this is that veins are, again, like rivers — the river is as large as the sum total of its tributaries. Because the early anterior tributaries which form the SSS are generally small and few in number, the SSS itself is small anteriorely, and taking it will be fine because the tributary veins will find another way to drain. The important part is to remember the exceptions to the rule, which is basically when there is a large, dominant frontal vein present. This vein is easiest to see on an angiogram, like this one (blue arrows), although trained eyes can pick up the same on an MR or CT with contrast study.
One does have to be careful with TOF MRV images — I think they have lots of problems in general, and in this case this large vein is barely visible — the purple arrow points to the SOV vein and is a fakeout.
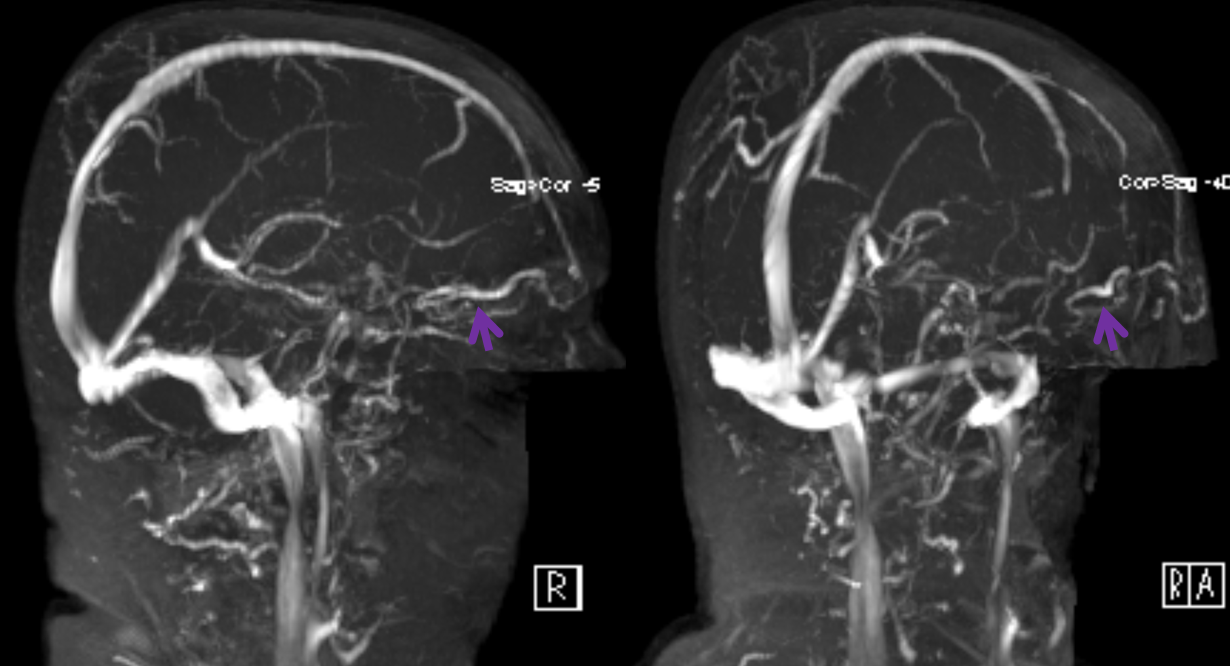
On the next TOF MRV image, obtained on a TrioTim 3T magnet, the vein is seen much better than on the Skyra study
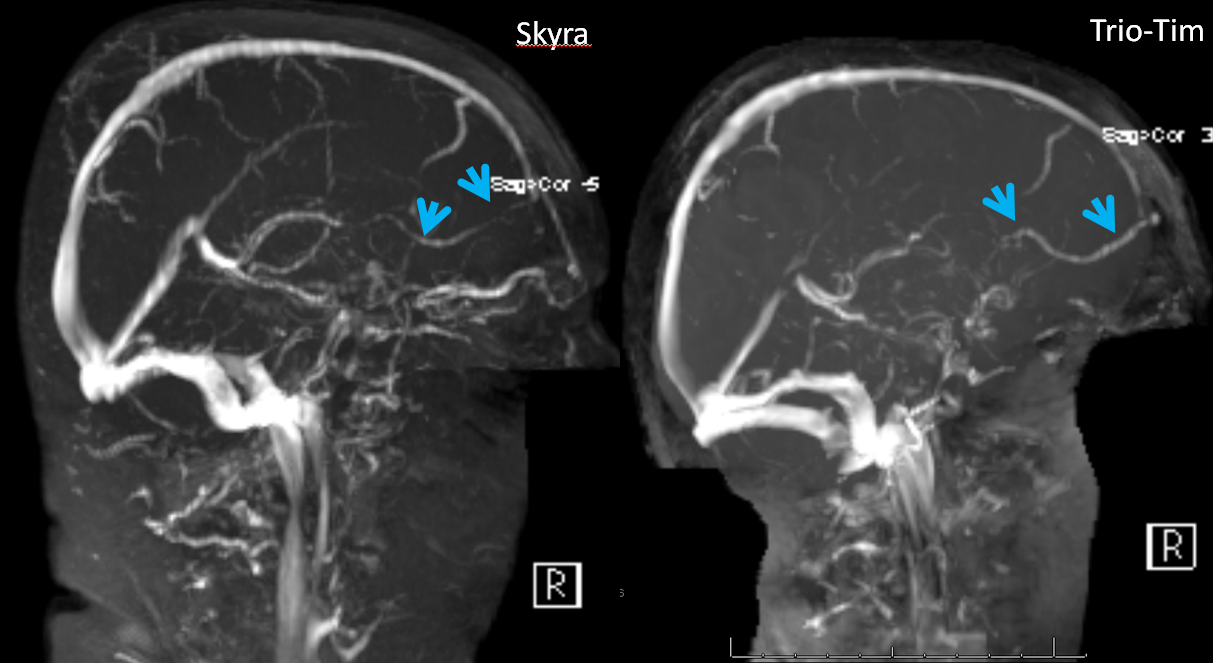
I find it is much better to look at veins on a post-contrast T1 study (of course, one has to be careful about precontrast T1 hyperintensity, etc. However, with good proficiency, postcontrast T1 is better than TOF MRV in most cases). This is what it looks like
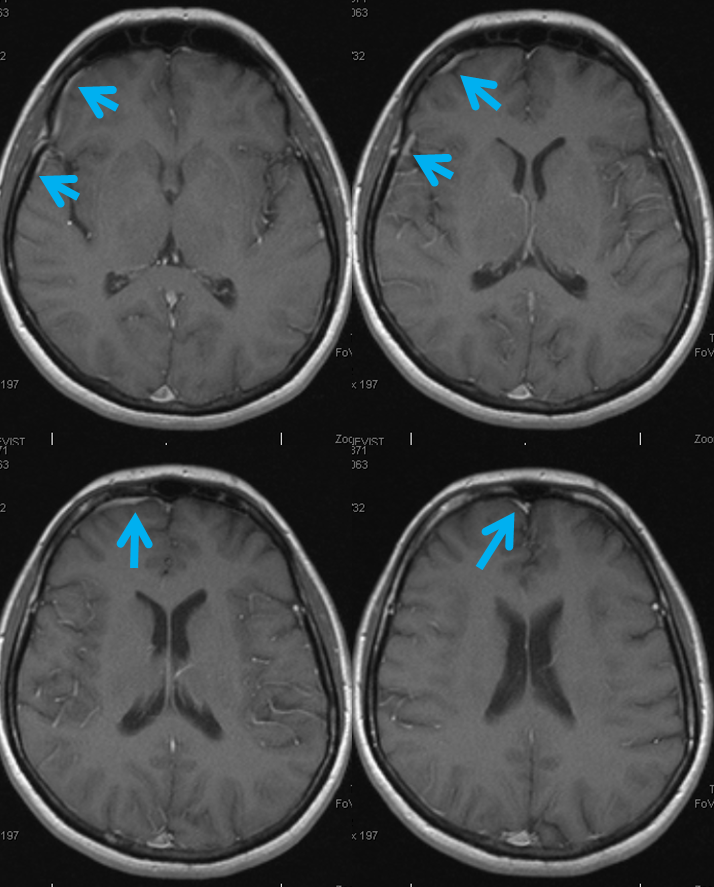
As often the case, there is a dominance of anterior frontal veins on the left also, however joining the SSS a bit more posteriorly (white arrows). A large Labbe (yellow) is also present.
MRI tracing same veins on the left side
Frontal Parasagittal Vein — Another Surgical Pitfall
Sometimes, frontal lobe drainage collects into a peculiar cortical vein that runs in parallel with the SSS for quite a while, before finally giving up and joining it somewhere, like so (black arrows):

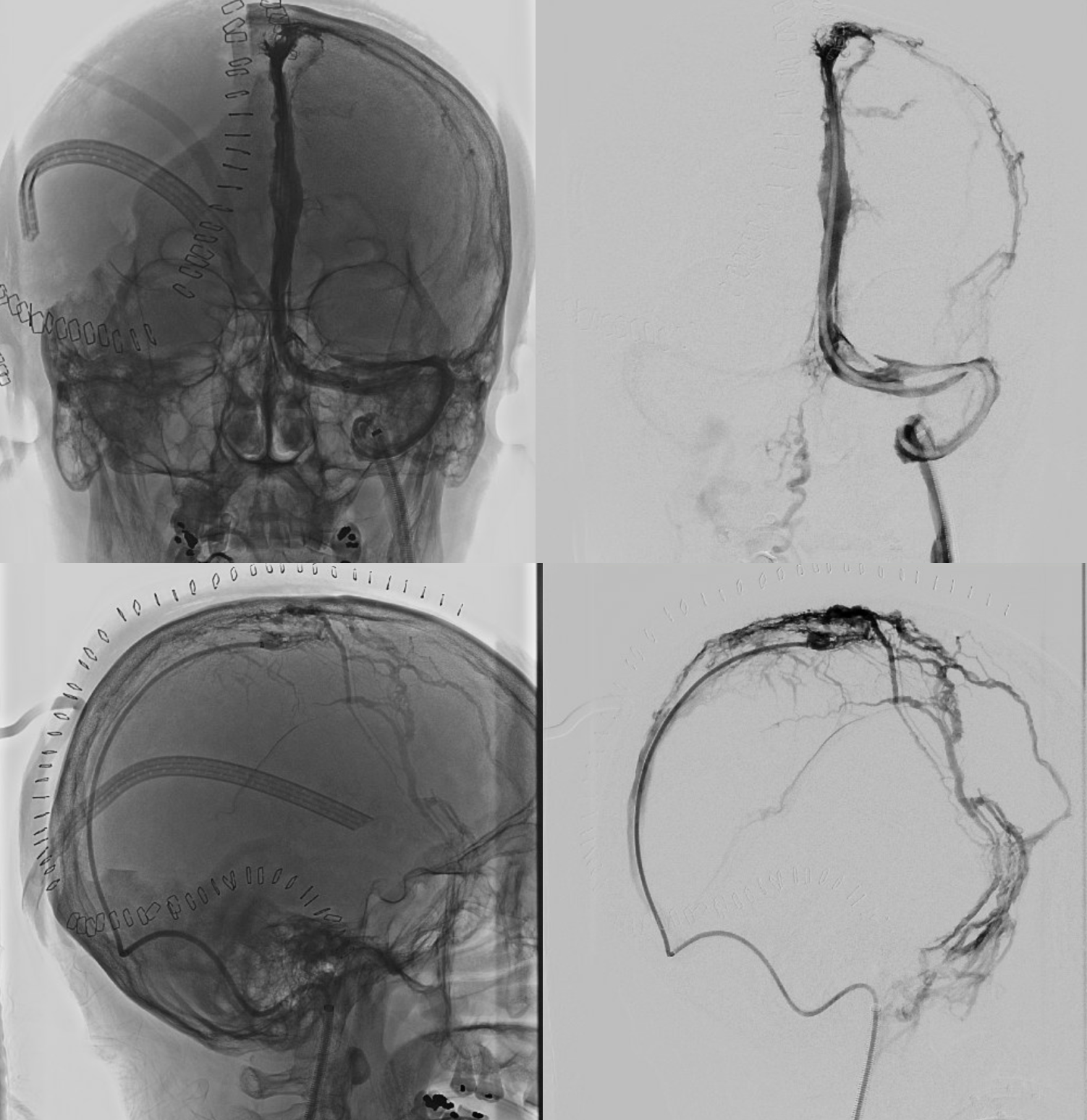
It is also important to be careful with this surgically. This patient presents with a large hemorrhage from a small AVM
Angio shows a particularly large frontal parasagittal vein — it has nothing to do with the AVM, but will be near the ultimate surgical approach
Post-embo and resection via anterior right parasagittal approach — there is impressive frontal congestion, best seen in lateral views. Dural incision and dissection were made with the vein fully in mind, but it closed anyway — possibly from reflecting the dura or retraction.
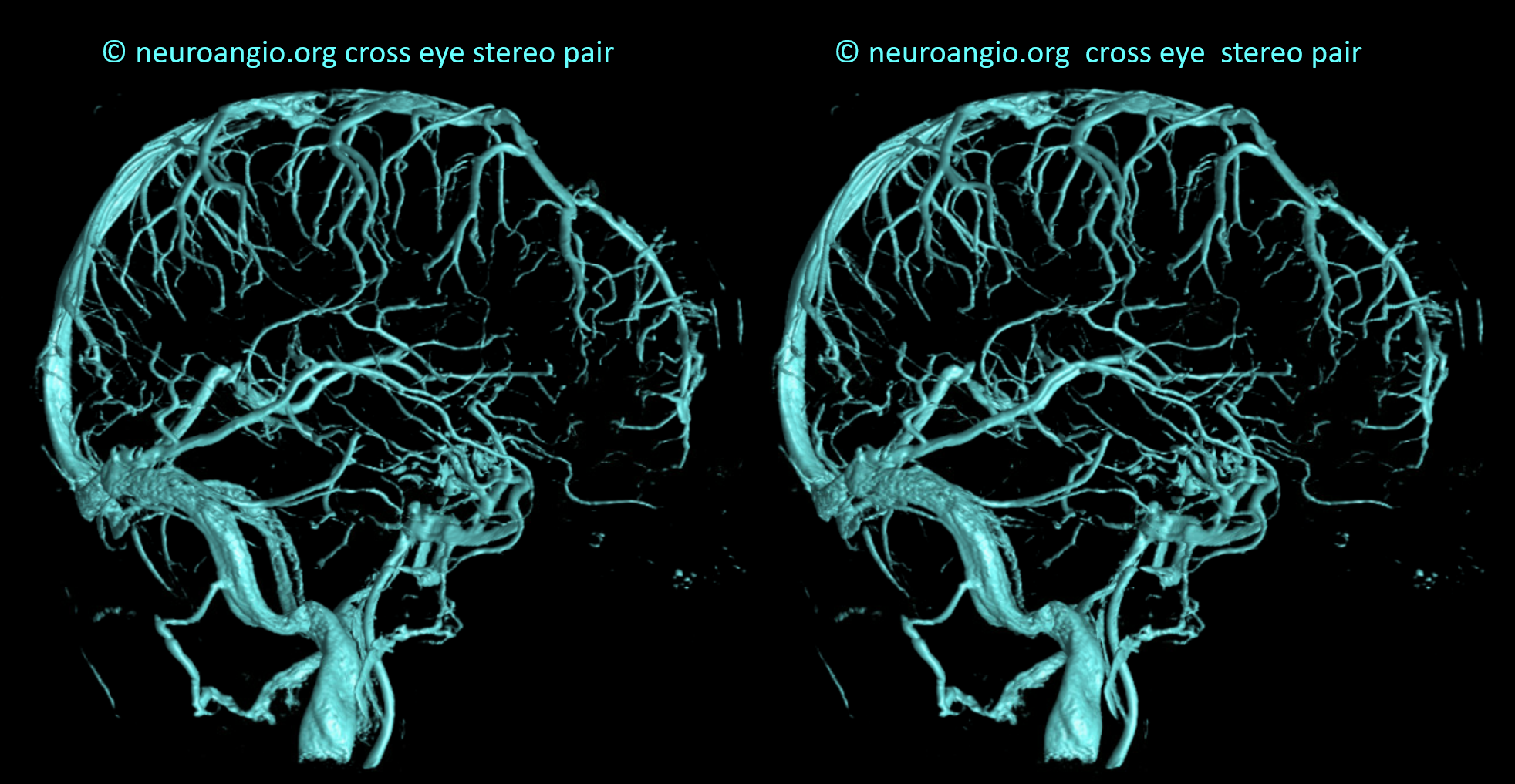
Stereos
Venous volume rendered stereos
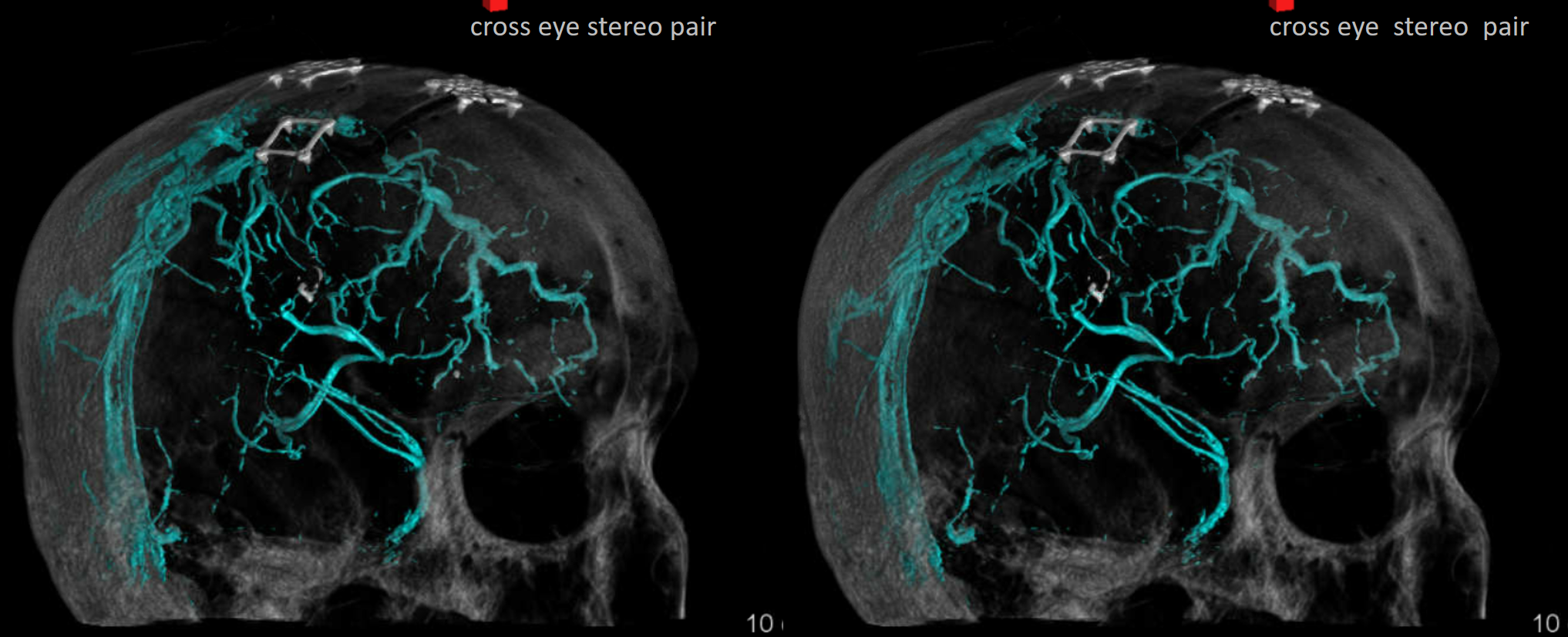
What we don’t understand well is why an angiographically tremendously congested lobe like this remains normal on follow up CT (2 days post surgery), with no infarct or edema, while in other cases venous occlusion is disastrous. Better very lucky than very good here…
Anterior Cerebral Vein
Just like there exists a middle cerebral vein next to the middle cerebral artery, so does the anterior cerebral vein often accompany the anterior cerebral artery. It is not a vein of major importance, other than by association with its embryologically ancient and proud arterial neighbor. The anterior cerebral vein (red arrows) is well seen on these images, which also show a well-developed middle cerebral vein (white) running in the depths of the sylvian fissure and then, over the (almost) temporal pole (green), under the temporal lobe (blue), and into the superior petrosal sinus (purple). The lenticulostriate deep vein (yellow) empties into the caverous sinus (black). A giant Labbe with a typical stenosis (pink) at its confluence with the sinus is also here.
Stereo of the lateral view, which shows everything much better
Frontal view with arrows — because of the ACOM, which allowed for opacification of the right anterior cerebral territory, portions of the right anterior cerebral vein (red) are also seen
Stereo pair below
Understanding Venous Drainage — the deep-superficial venous balance
The balance/spectrum approach to anatomy is key. Brain venous systems can be divided into superficial and deep. Deep is subependymal, draining into the Internal Cerebral Vein. Basal vein is controversial — its part of both maybe — but really it is superficial. Surgically, it sure is deep. But, seeing how it runs on surface of the brain (bottom surface, but surface as any other), it is superficial.
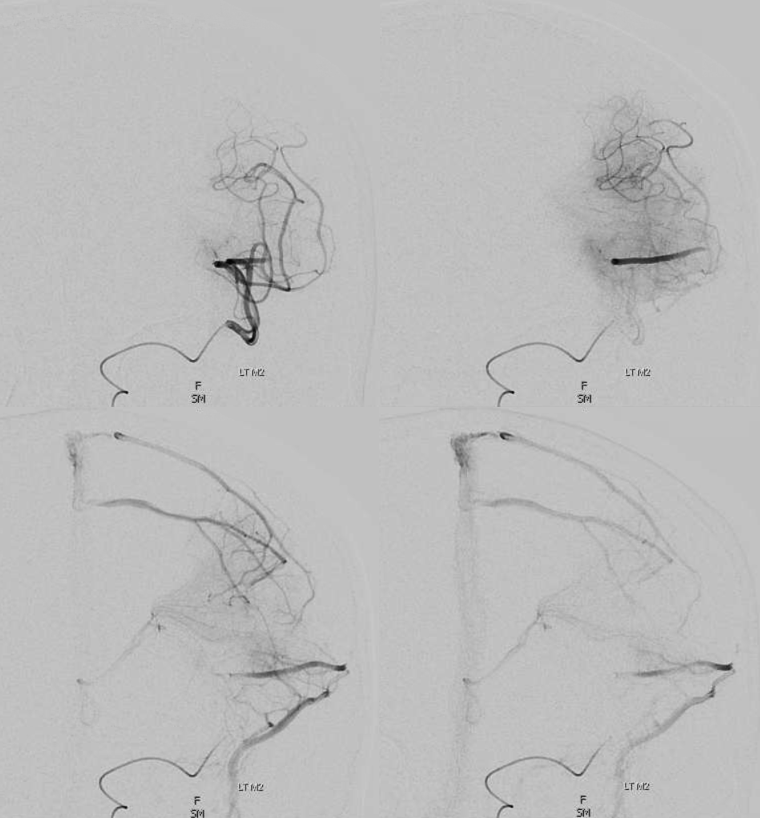
The two systems are connected by transmedullary veins running though white matter. They are key in understanding DVAs. There is balance here also — sometimes, the balance is towards drainage into the superficial veins, sometimes into deep ones. See deep venous system for more info. Here, for example, an M2/3 injection, well beyond the lenticulostriate vessels, and thus theoretically only draining into superficial venous system, actually drains into both. This is important in understanding how apparently superficial AVMs can have deep venous drainage. This image was acquired in preparation for distal thrombectomy — see full case here
Dural Sinuses — much more on this important topic on the Venous Sinuses Page and dedicated Dural Venous Channels Page
Although the majority of superficial veins empty directly into the major named venous sinuses (Superior Sagittal, transverse, straight [see Dural Venous Sinuses page]), the occasional exception whereby the vein joins an unnamed dural venous sinus channel first, reminds us of some relevant embryology and keeps the informed surgeon on his/her toes. During early development, venous channels preferentially form at the confluence of dural sheets (such as falx and upper dura for the superior sagittal sinus, or the tentorium and lateral dura for the transverse sinus). However, short dural channels outside of these confluences are more often present than most people realize. These can be recognized with a trained eye as being somewhat broader along the dural surface and flatter in a tangential plane to the dural sheet within which they are located. Longer ones are progressively less common, but still can be seen with regularity. Below is an example of a parieto-occipital dural sinus (white) which collects a somewhat peculiar duo of surface veins (light blue). The transition from cortical vein to dural sinus is marked by the purple arrow. It is typical to see dural sinuses associated with larger, more dominant surface veins, probably because dural sinus is not a favored embryologic structure, and in order for it to persist the flow demand must be somewhat high. Notice also bilateral transverse/sigmoid sinus stenoses in this patient with pulsatile tinnitus and intracranial hypertension.
Stereo views of the same arrangement, several years later.
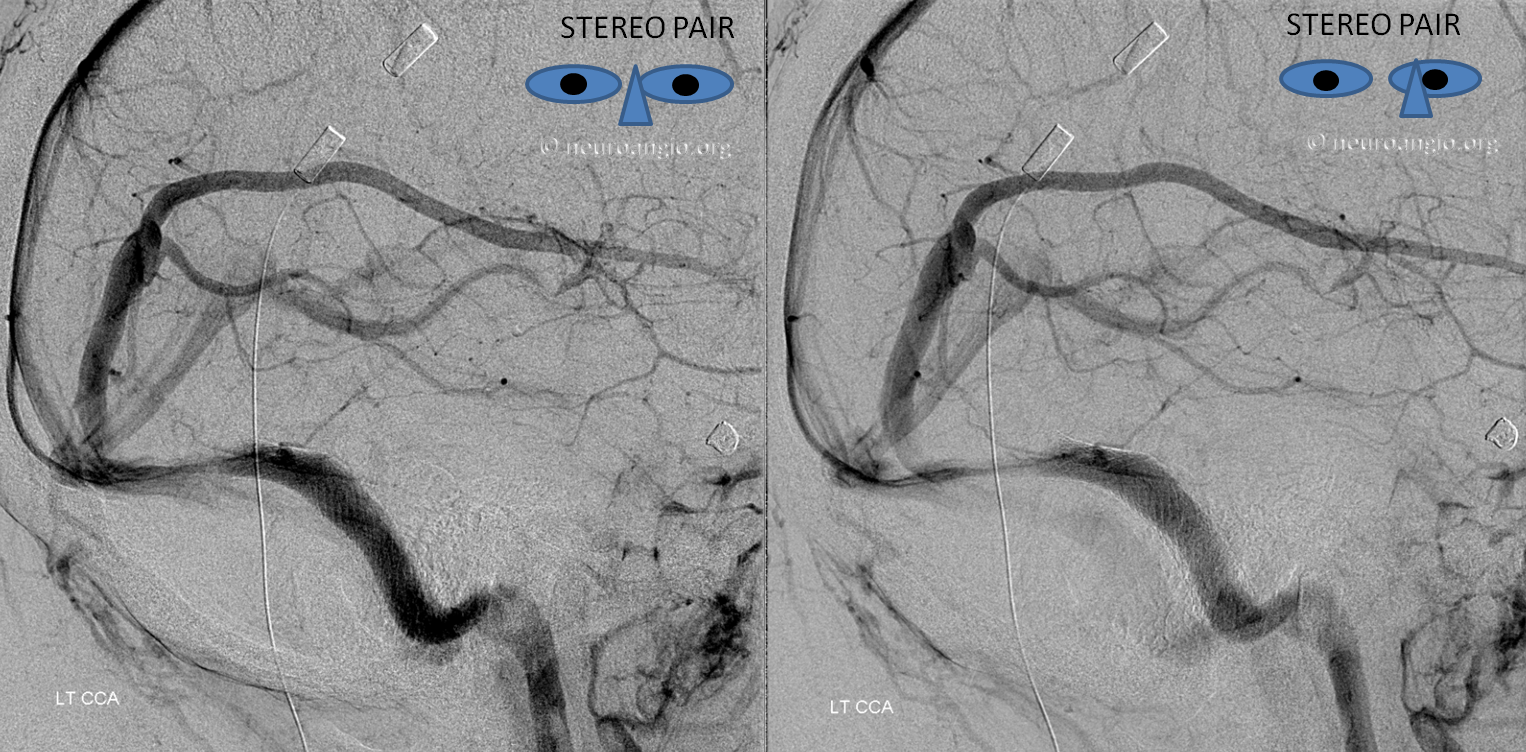
A stent (yellow) has been placed into the dominant sigmoid sinus. While pulsatile tinnitus was cured, the headaches which initially improved then recurred, and a shunt was eventually placed (purple, white). Notice recurrence of narrowing (black) just distal to the stent, as is typical in such failed stent cases.
Dural Sinuses are everywhere — much more common, again, than is taught. Here are a few examples, unmarked, some in ANAGLYPH stereo. Below, dominant Trolard drains into a dural sinus in the Falx cerebri (ANAGLYPH stereo)
Here is one of the very anterior falx, receiving a few anterior frontal convexity veins (STEREO ANAGLYPH)
Finally, here, the dural channel is in the lateral wall of the left cavernous sinus, receiving the deep Sylvian vein.

Same image in ANAGLYPH STEREO
Lateral view of same case shows the typical flattened appearance of the dural sinus when viewed from the side, also in ANAGLYPH
Flat Panel Imaging — what’s possible — volumetric views of venous system
Check this out — pause movies to scroll. See what you’ve learned
Another example
Stereo Imaging — See Stereo Page for more info
Anaglyph Stereos — view with red-blue anaglyph glasses
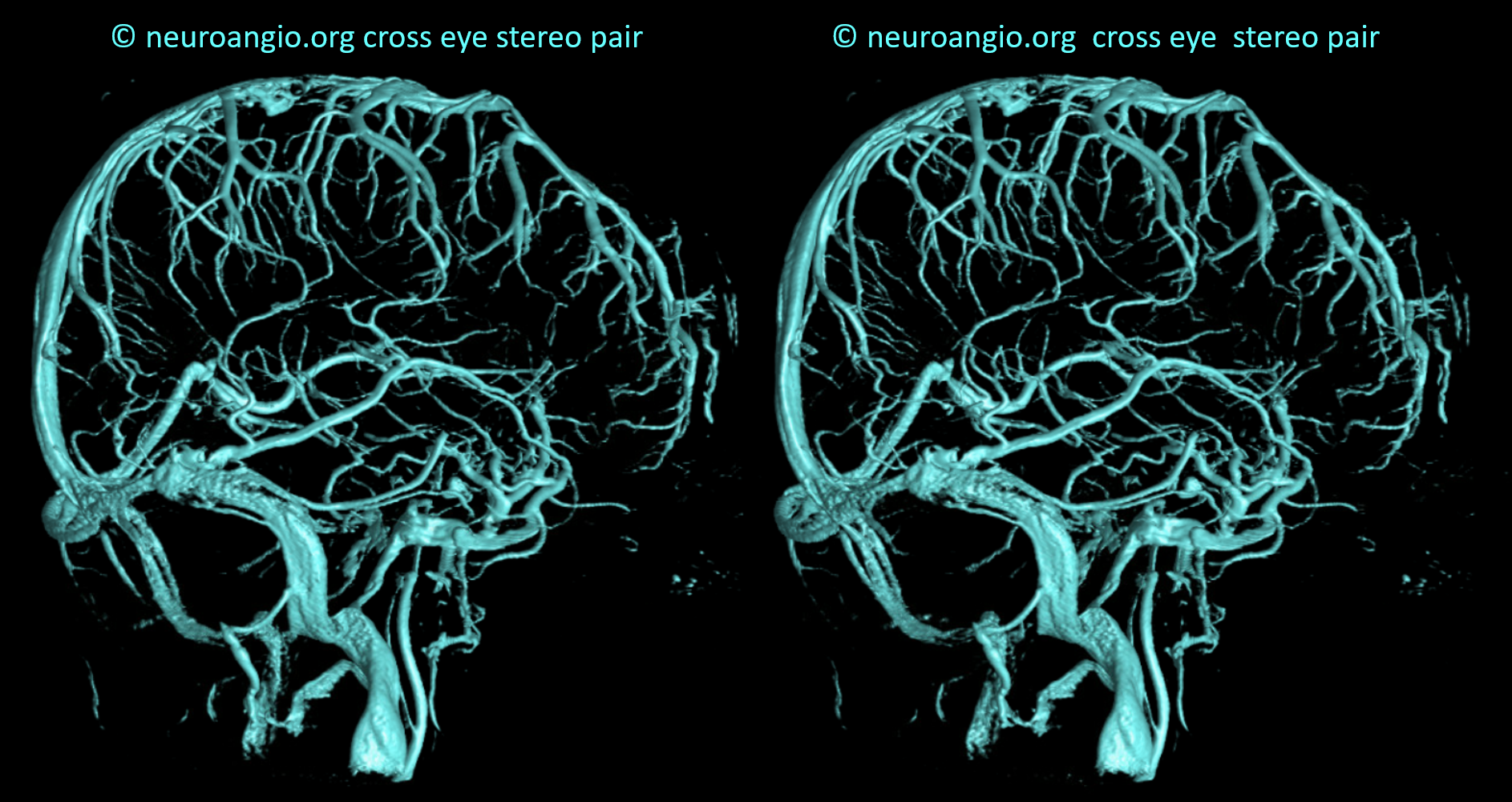
Cross-eye stereos
Advanced venous imaging
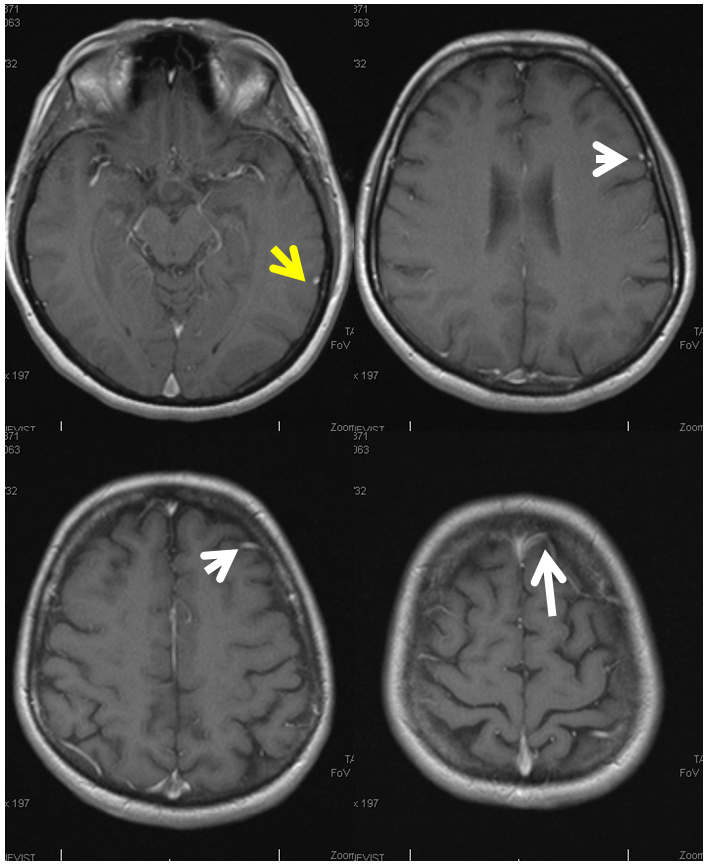
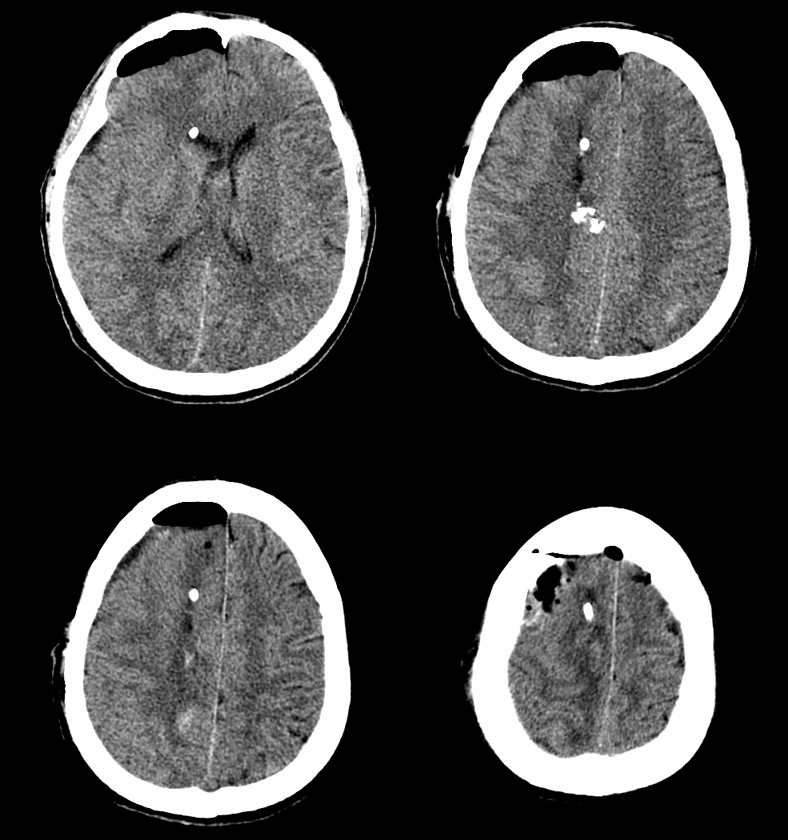
Sometimes, its good to get an angio when you are at a loss about something that might be vascular — bleeding, for example. Here is a young man with spontaneous left temporal lobe hemorrhage. MRI shows no evidence of AVM, aneurysm, or any other problem. In our book, this needs an angio
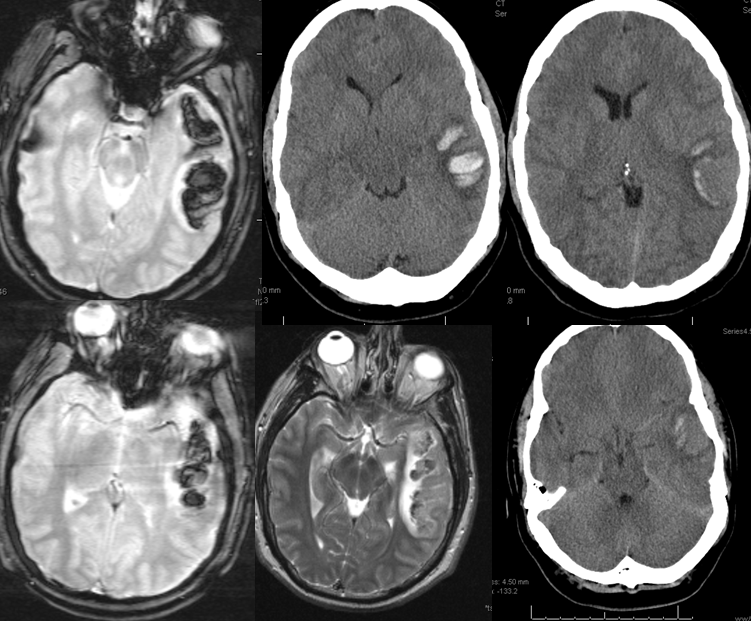
MRI (hemoflash and T2, and CT images of left temporal hemorrhage). Note to radiologists — please don’t ask to see the whole study — there is nothing suspicious there, believe me.

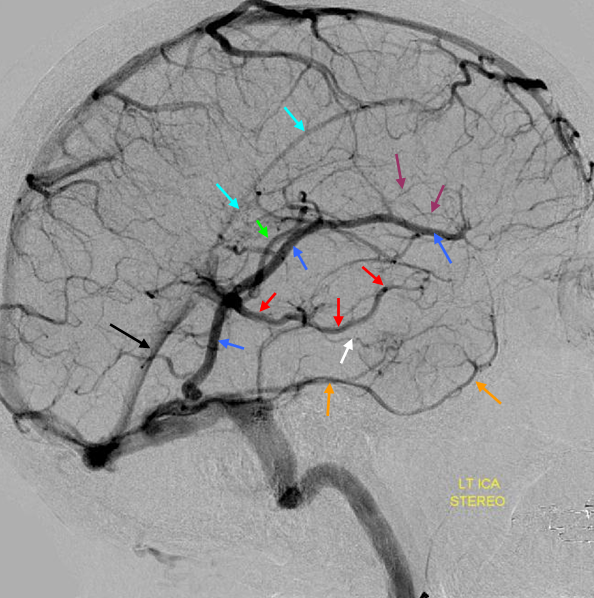
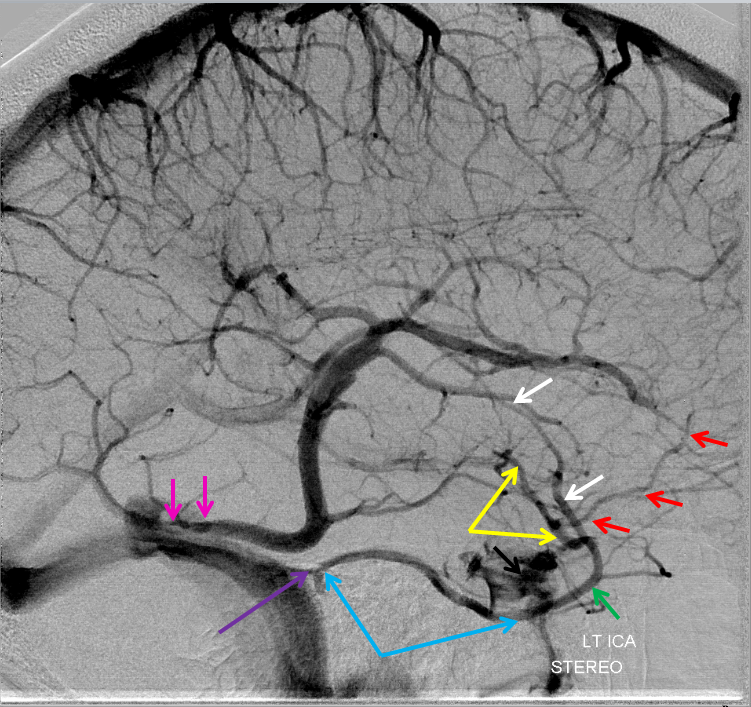
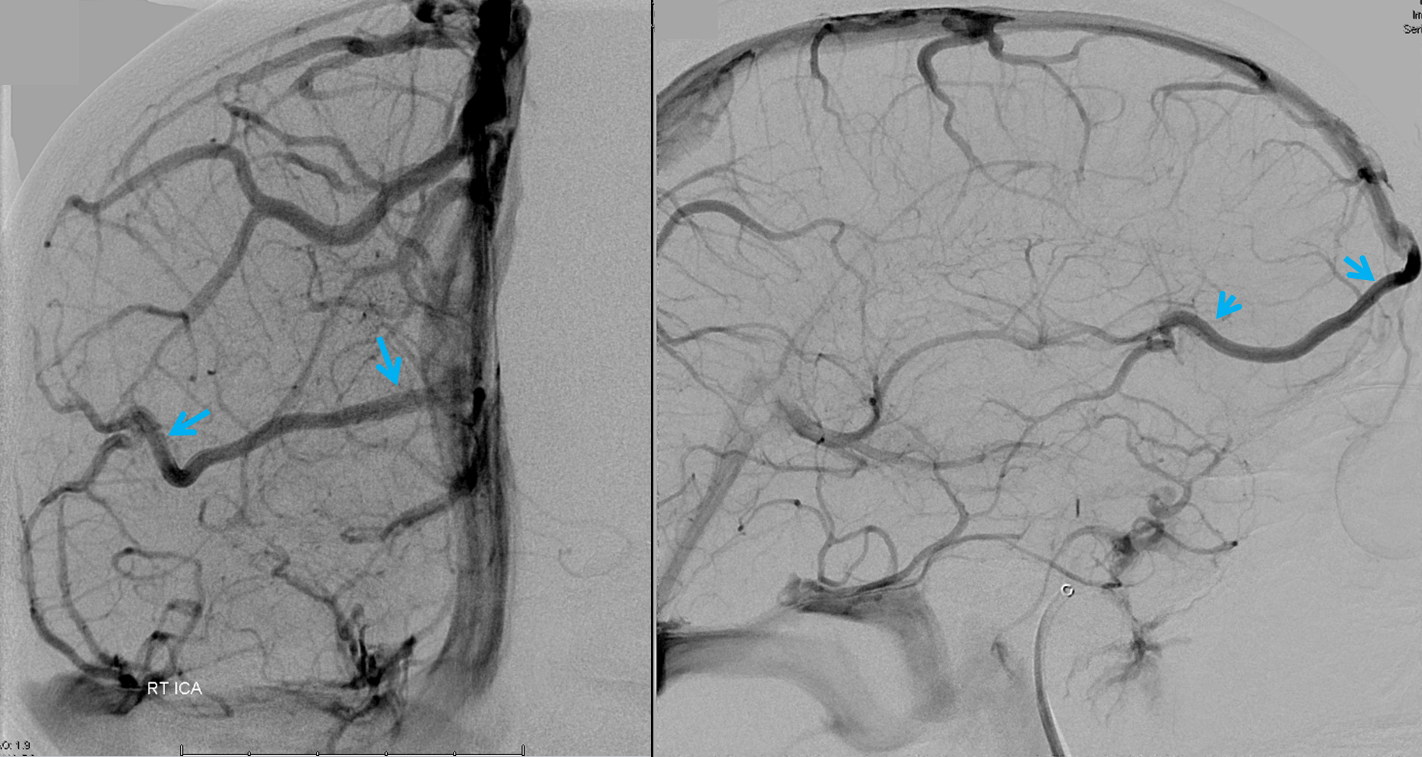
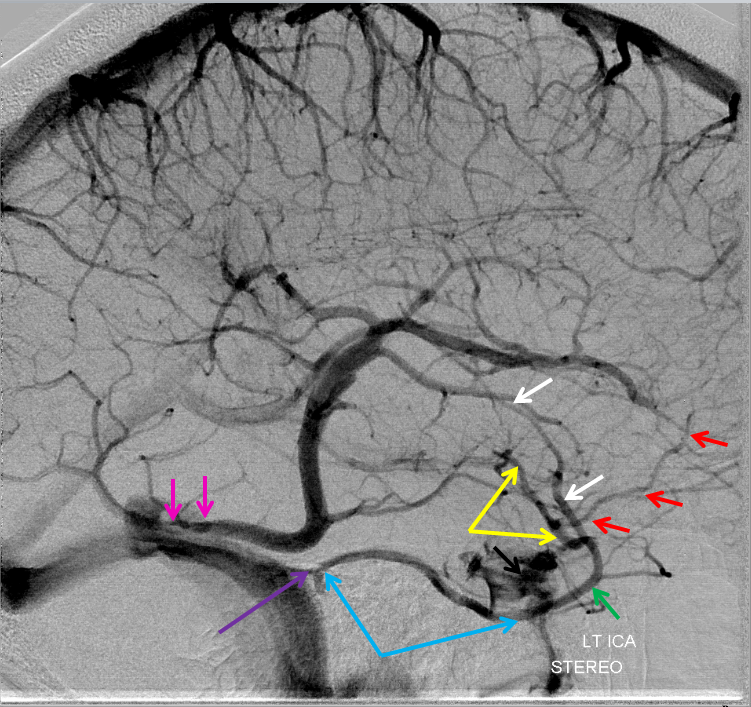
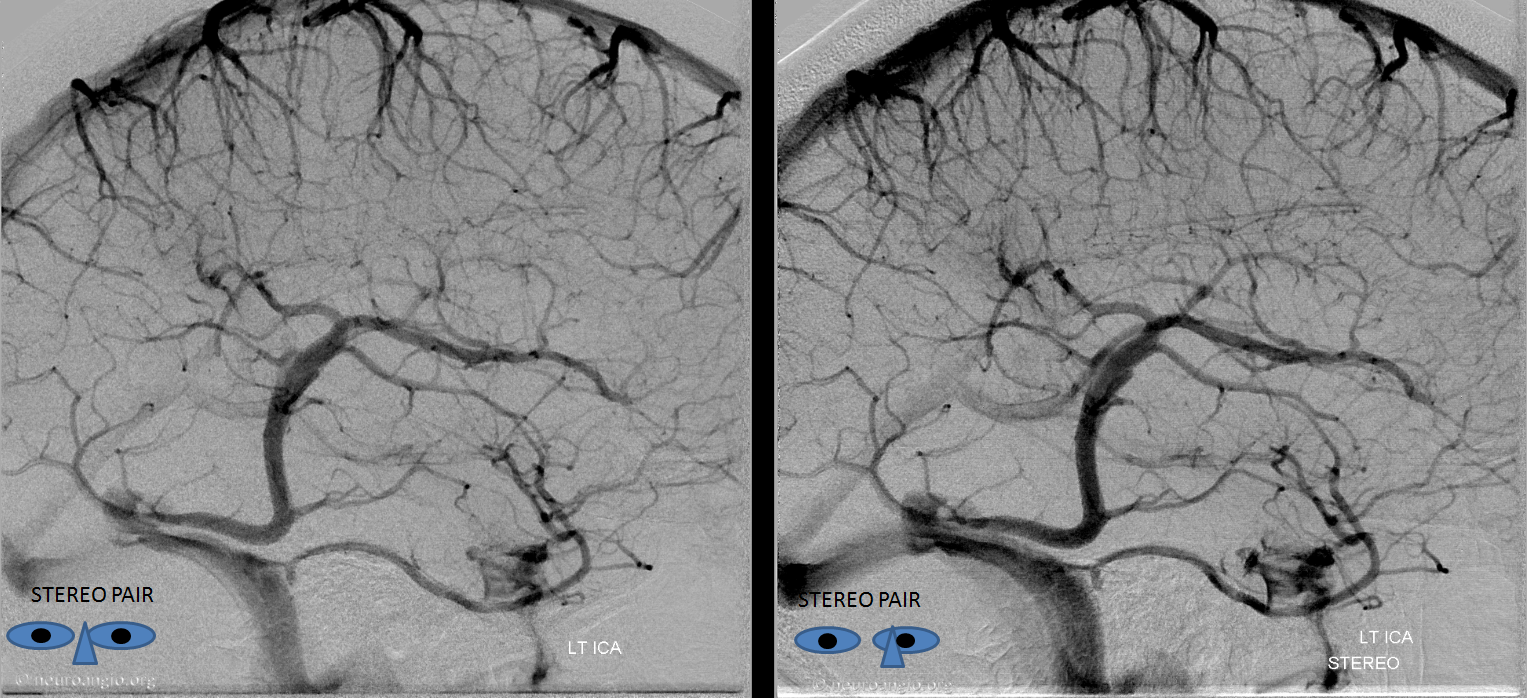
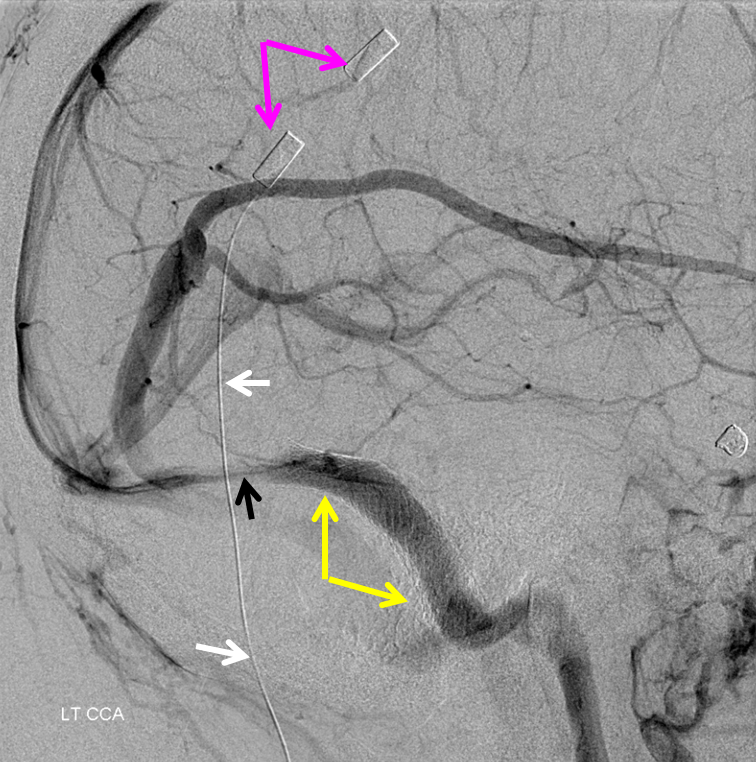
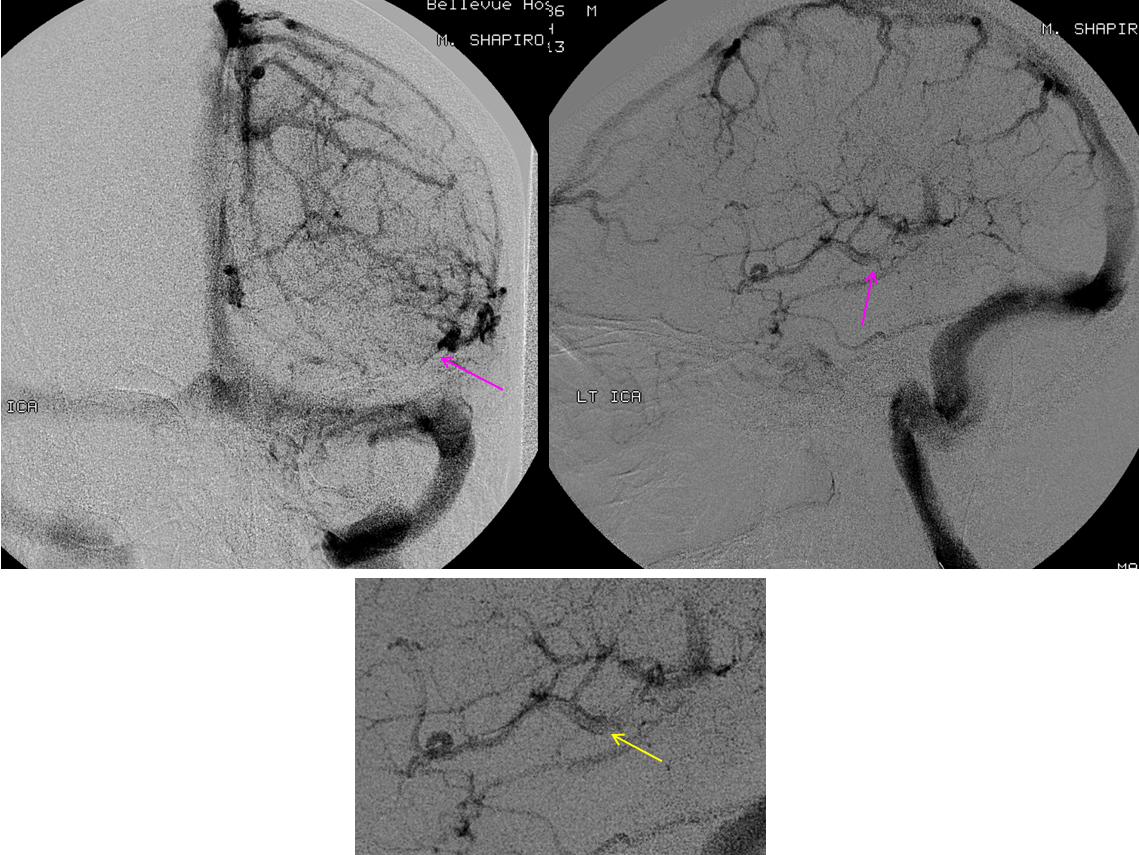
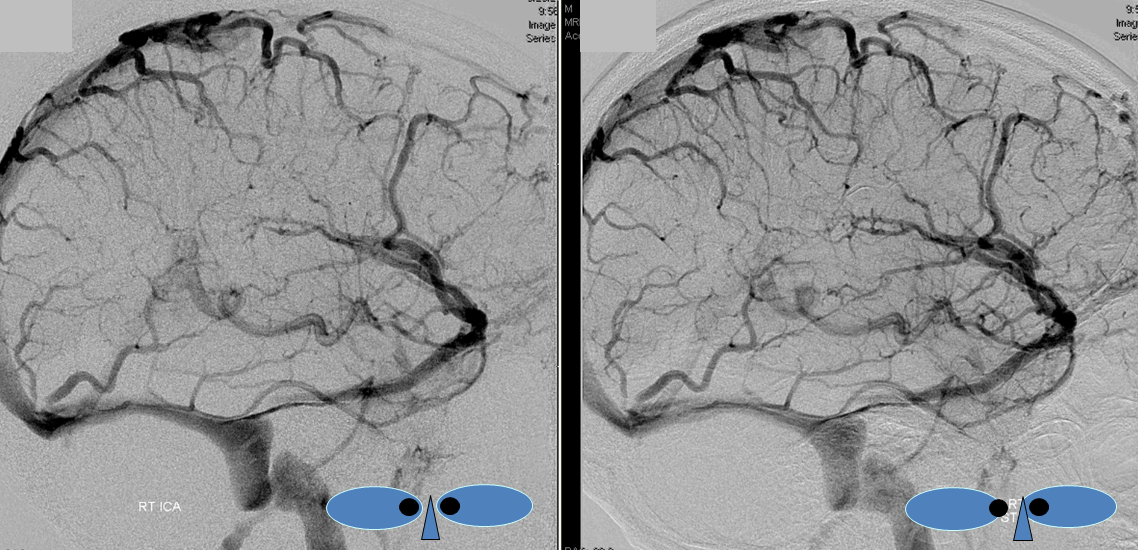
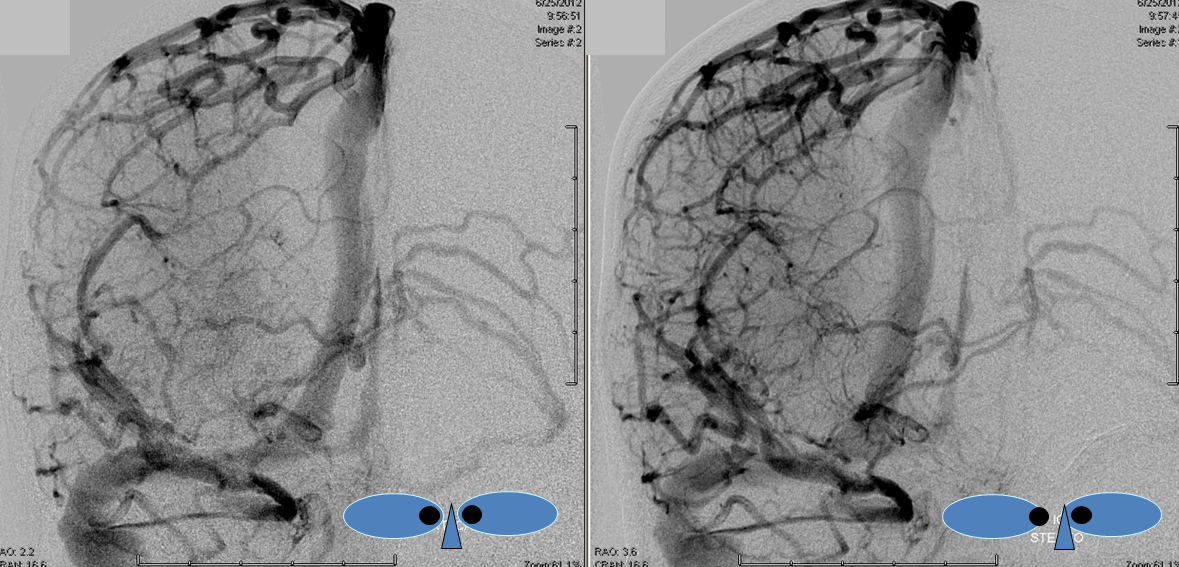
Angio of the same patient — what is the diagnosis?
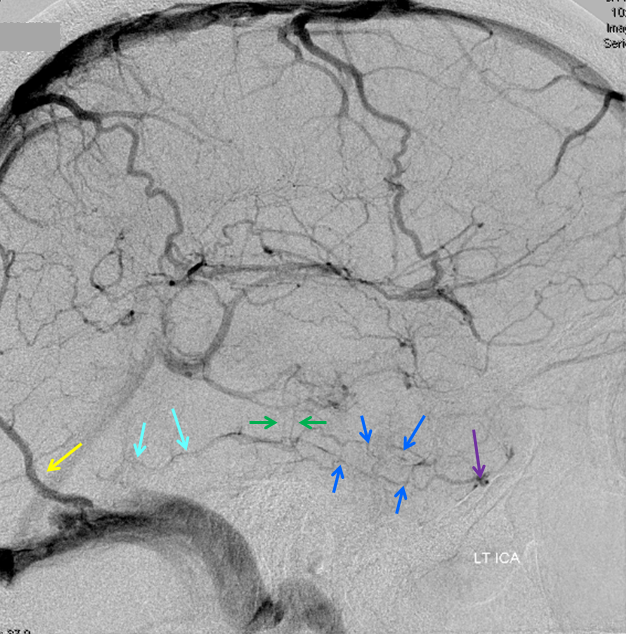
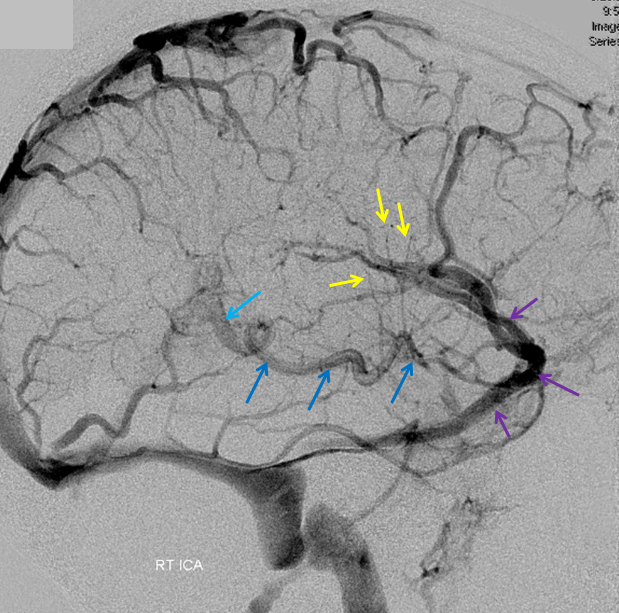
Cerebral venous thrombosis. Isolated thrombosis of the inferior temporal vein/vein of Labbe. Notice irregular and thinned appearance of inferior temporal gyrus vein (dark blue arrows), compared with the larger caliber of the same vein anteriorly (purple) and posteriorly (light blue), which is the vein of Labbe. Other signs are:1) There are no normal veins seen draining the temporal convexity — this cannot possibly be normal. Deep sylvian veins and striate veins are there (unlabeled, see venous system for clarification) If you do enough angio, you will recognize that this appearance is very abnormal. Every other lobe has juicy veins, for example 2) There is evidence of temporal lobe congestion, which is somewhat subtle, but present — in the inferior and superior temporal regions. The middle “layer” of the temporal lobe is hypovascular — corresponding to location of the clot — its a hyperemia-clot-hyperemia sandwich.
As usual, cerebral venous thrombosis can be an elusive diagnosis — especially if the sinuses are not involved. But it certainly happens, and certainly more often than is known about.
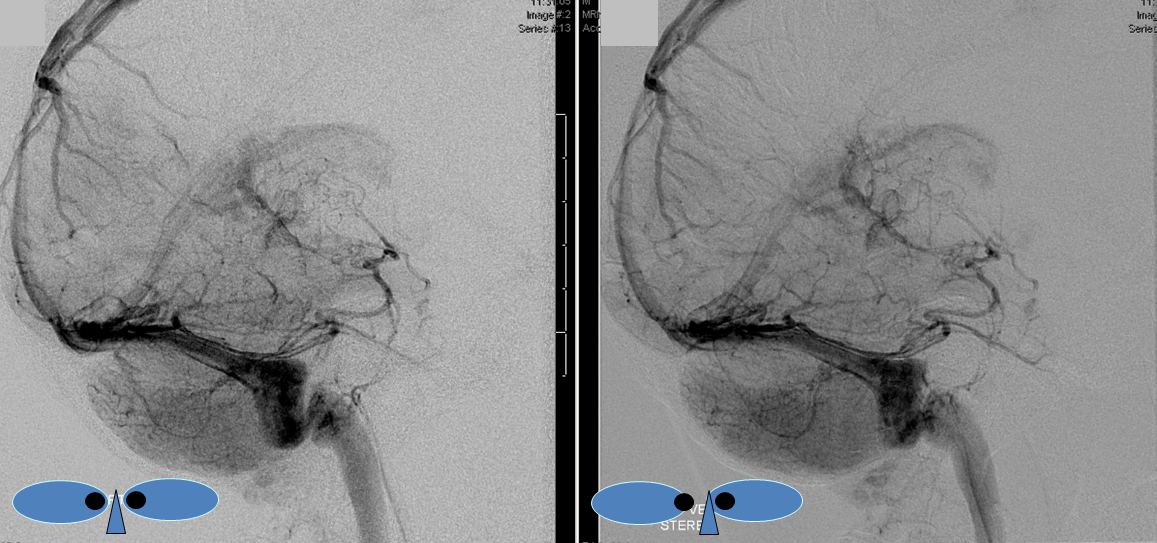
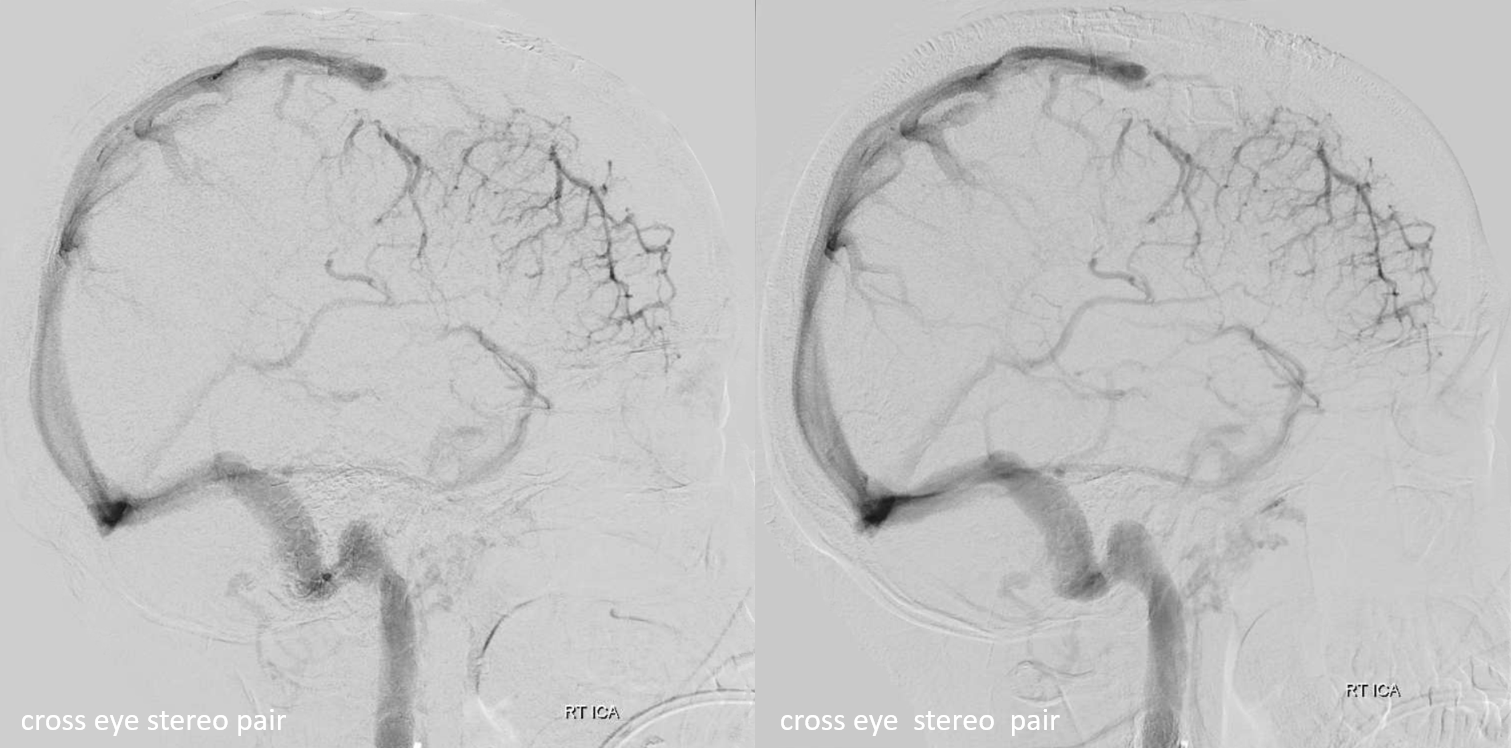
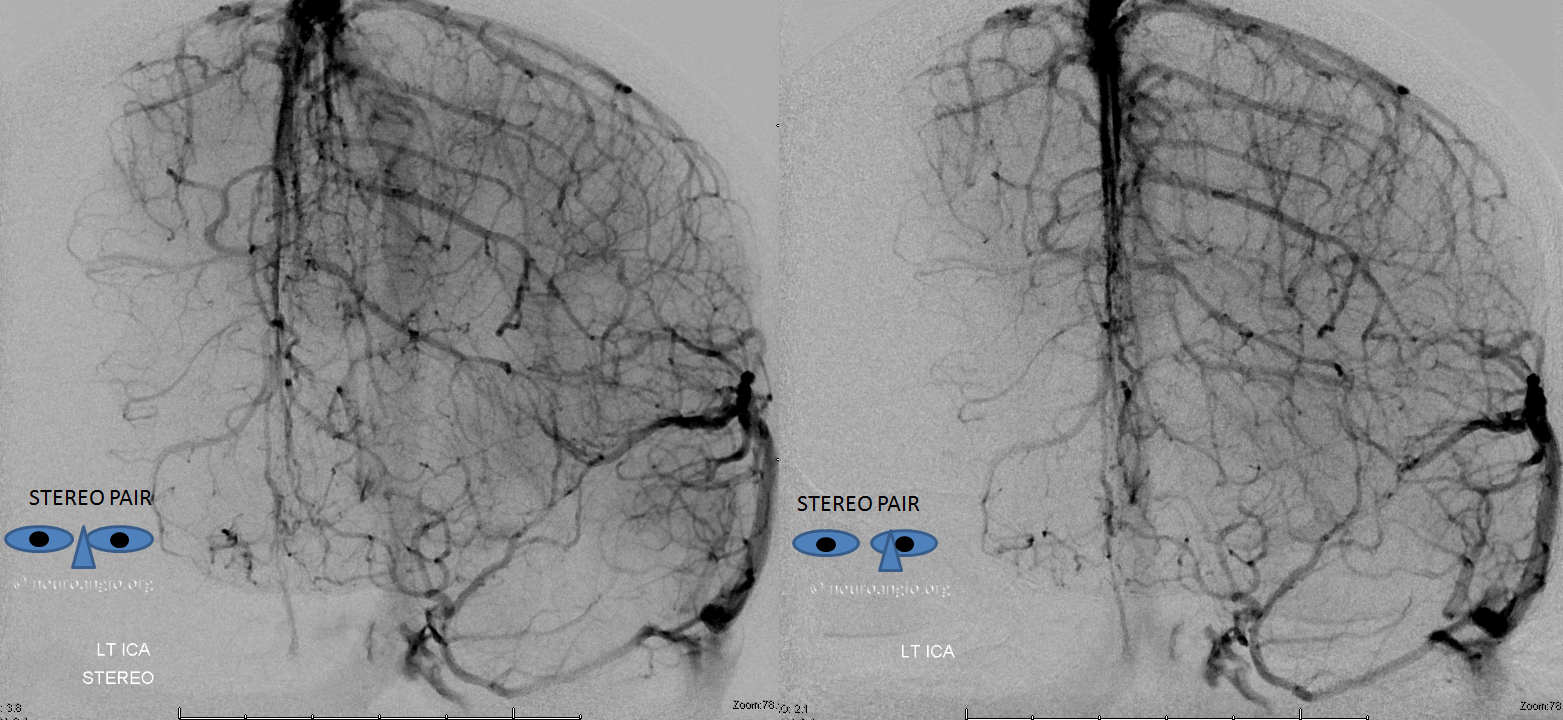
stereo pair of the same patient, can’t resist having one. Notice hyperemia adjacent to congested inferior temporal lobe vein, and clot-related lucency above it.
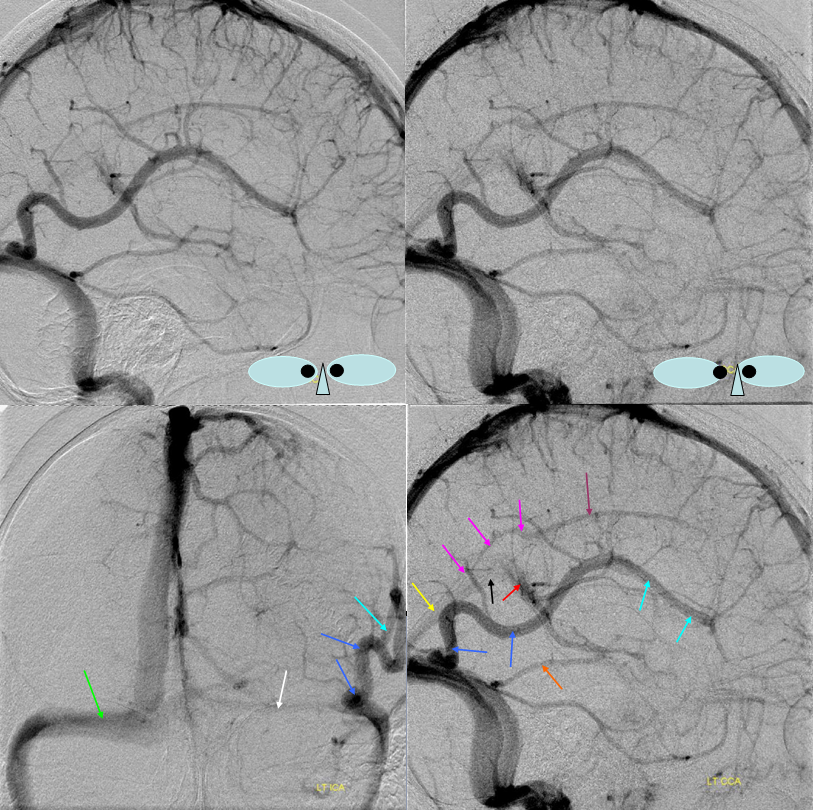
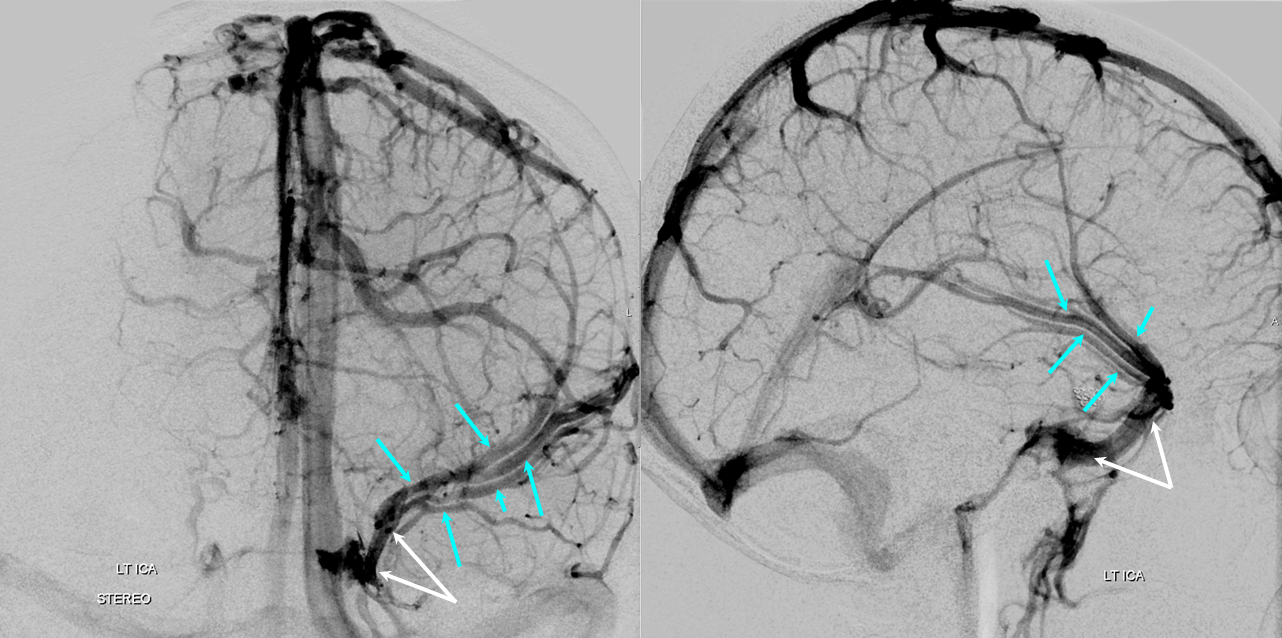
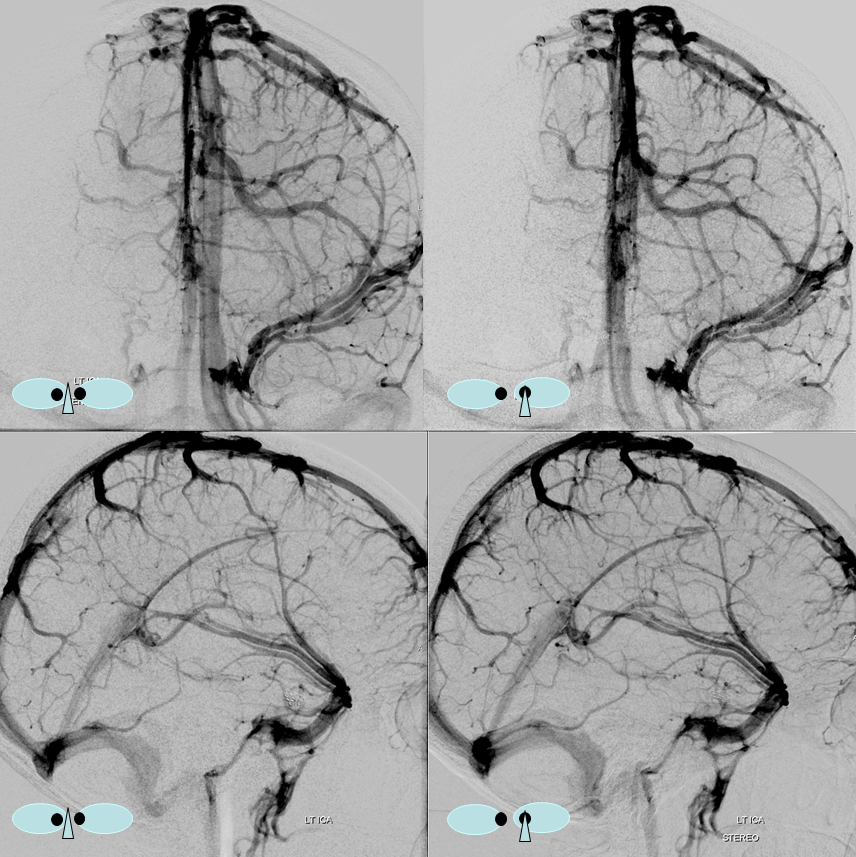
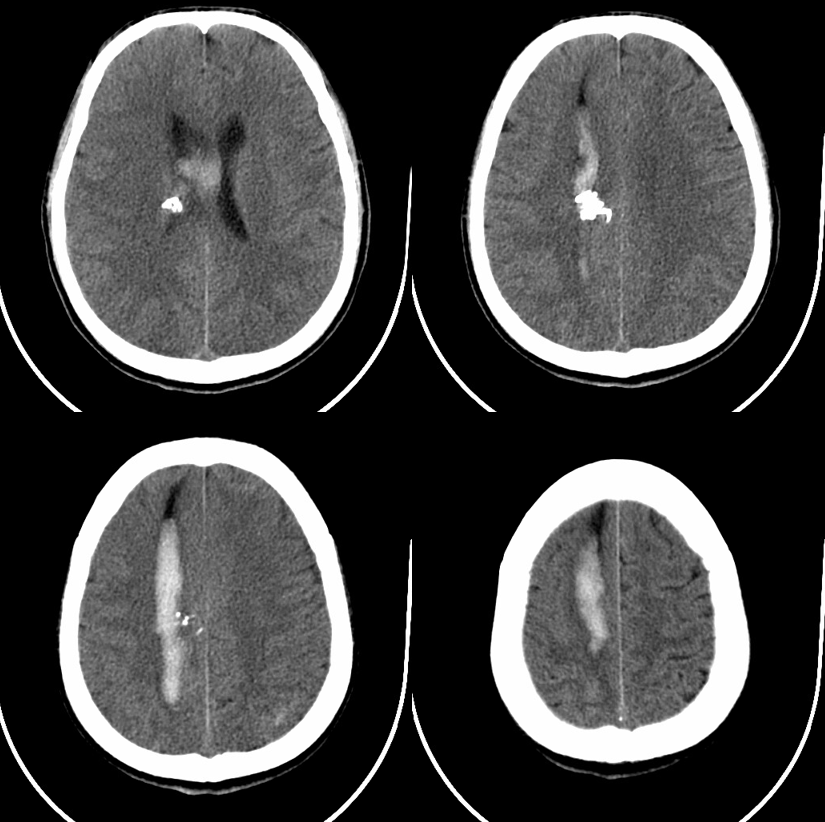
Venous Thrombosis Case 2
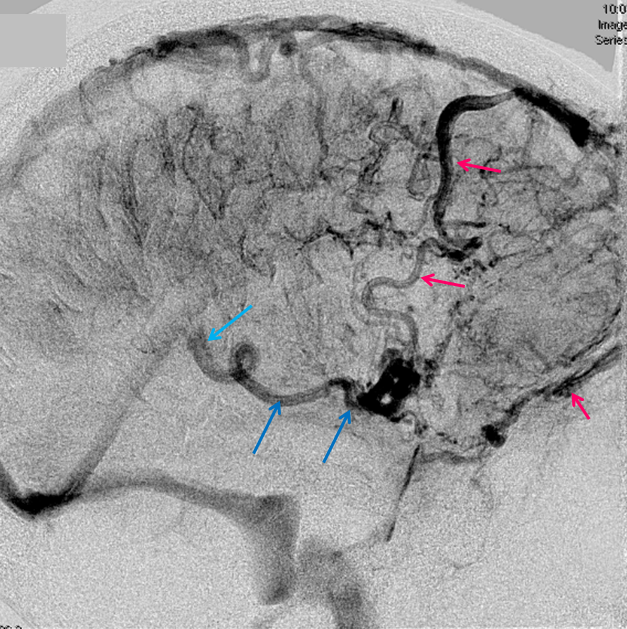
This patient with Sickle Cell Disease presented with headache. CT identified subarachnoid hemorrhage over the convexity (red arrows). The subtle hyperdensity adjacent to the left inner table was not appreciated initially (pink arrows).
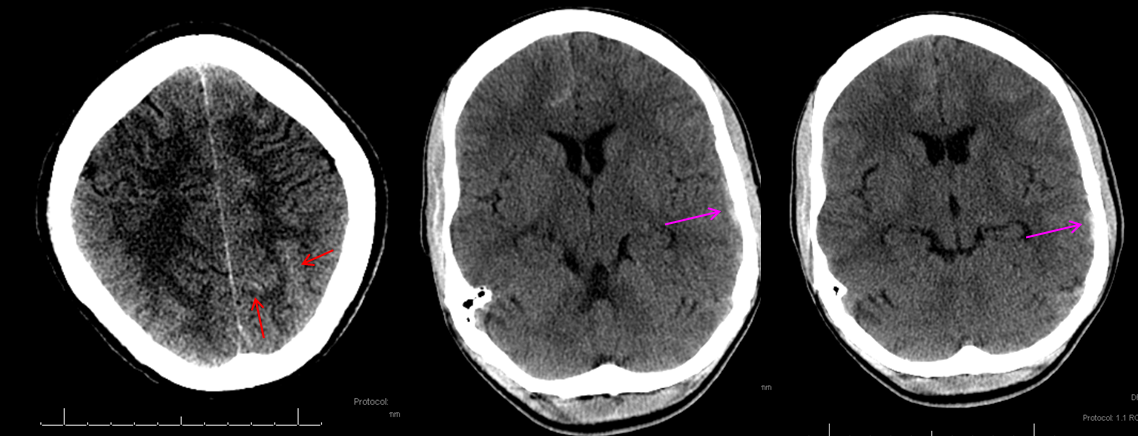
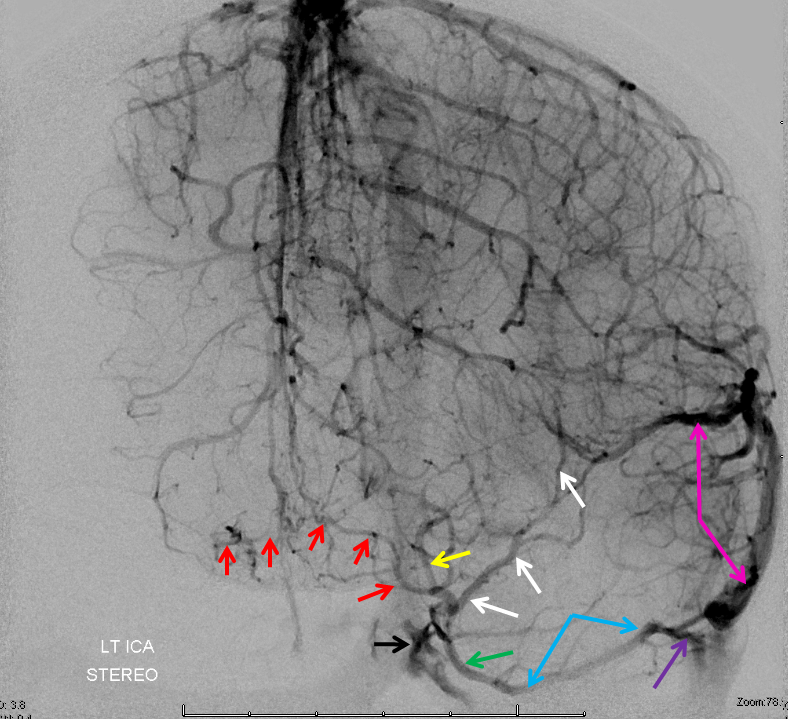
The patient was referred directly for angiography to look for the cause of subarachnoid hemorrhage. Frontal and lateral projection digital subtraction angiographic views of the left ICA injection, in venous phase, demonstrate abrupt cutoff (pink arrows) of the vein of Labbe. “Tram-track” sign of filling defect in the vein is acually seen on the lateral image (yellow arrow). The venous sinuses are fully patent.
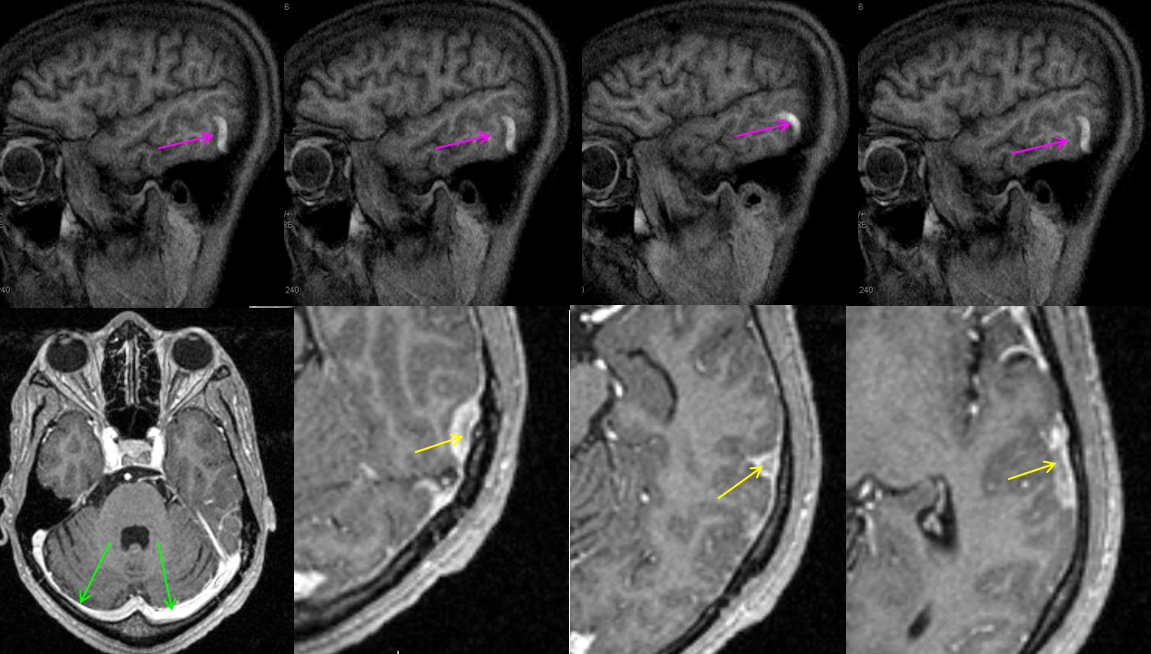
Subsequently obtained contrast MRI demonstrates nicely the hyperintense thrombus on sagittal T1-weighted imaging, and the intraluminal thrombus is seen on post-contrast T1-weighted images (yellow arrows). Again, the sinuses are patent (green arrows). Patients with sickle cell disease are, of course, at major risk for sickling, leading to both arterial and venous thrombosis.
Venous Sinus Thrombosis
As you saw above, understanding why some patients do well with venous sinus thrombosis while others don’t is mostly a matter of anatomy. Occluded sinuses are not the main problem — occluded cortical veins are. It is about venous collaterals. If a sinus receiving a cortical veins is blocked, the extent of severity of venous congestion is determined by presence or absence of alternative outflow sources for the blocked vein. If there is an alternative, not much happens. if there is not, the result is venous infarct.
The best alternative is often the Cavernous Sinus, since it represents a completely different venous system. With Sigmoid or Transverse sinus thrombosis, if the torcular is spared, the SSS is another effective route. You get the idea. Convexity veins can be interconnected or not. The more interconnected they are, the better off the situation will be. See “Superficial Venous System” Page for more info.
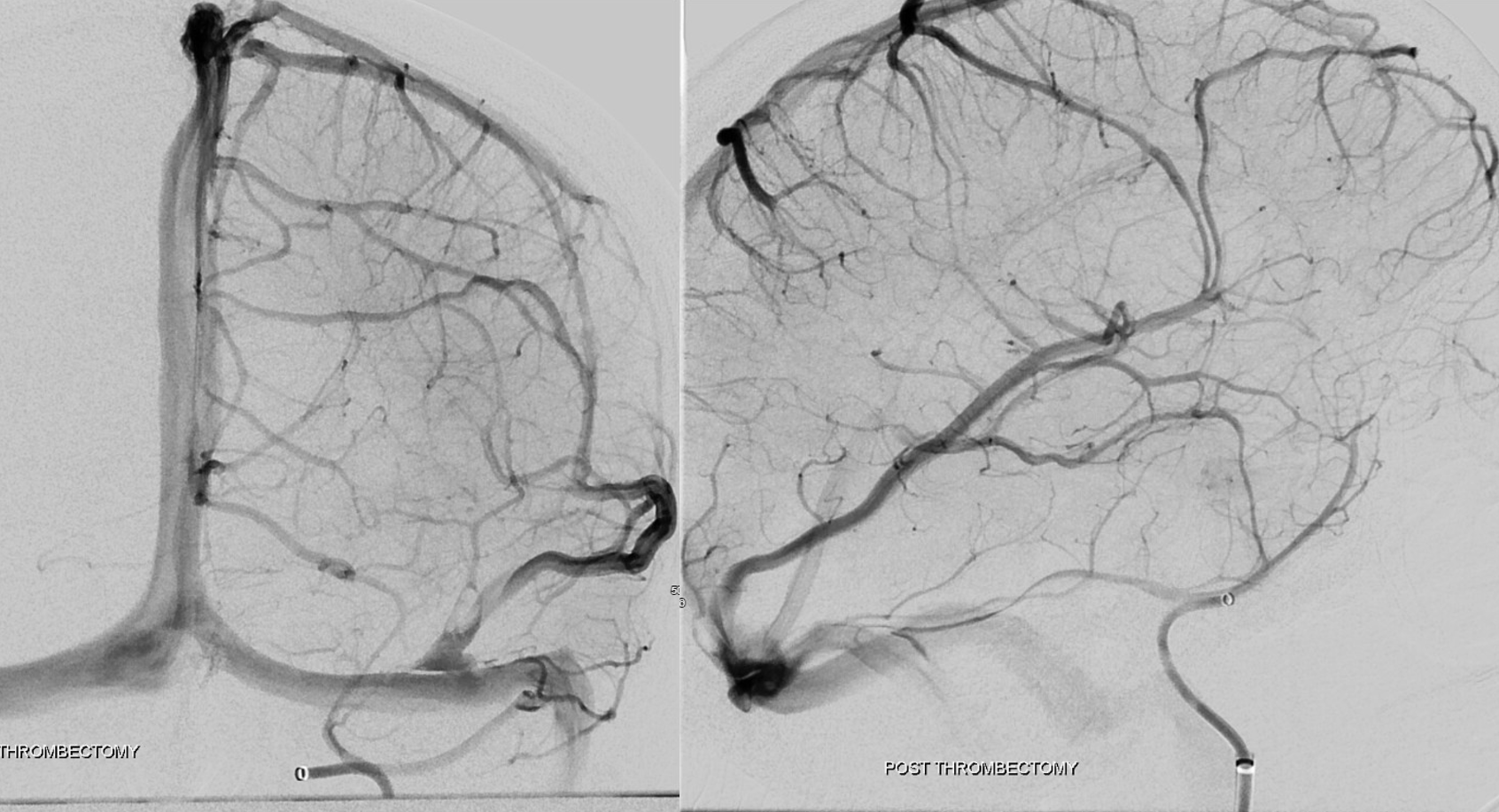
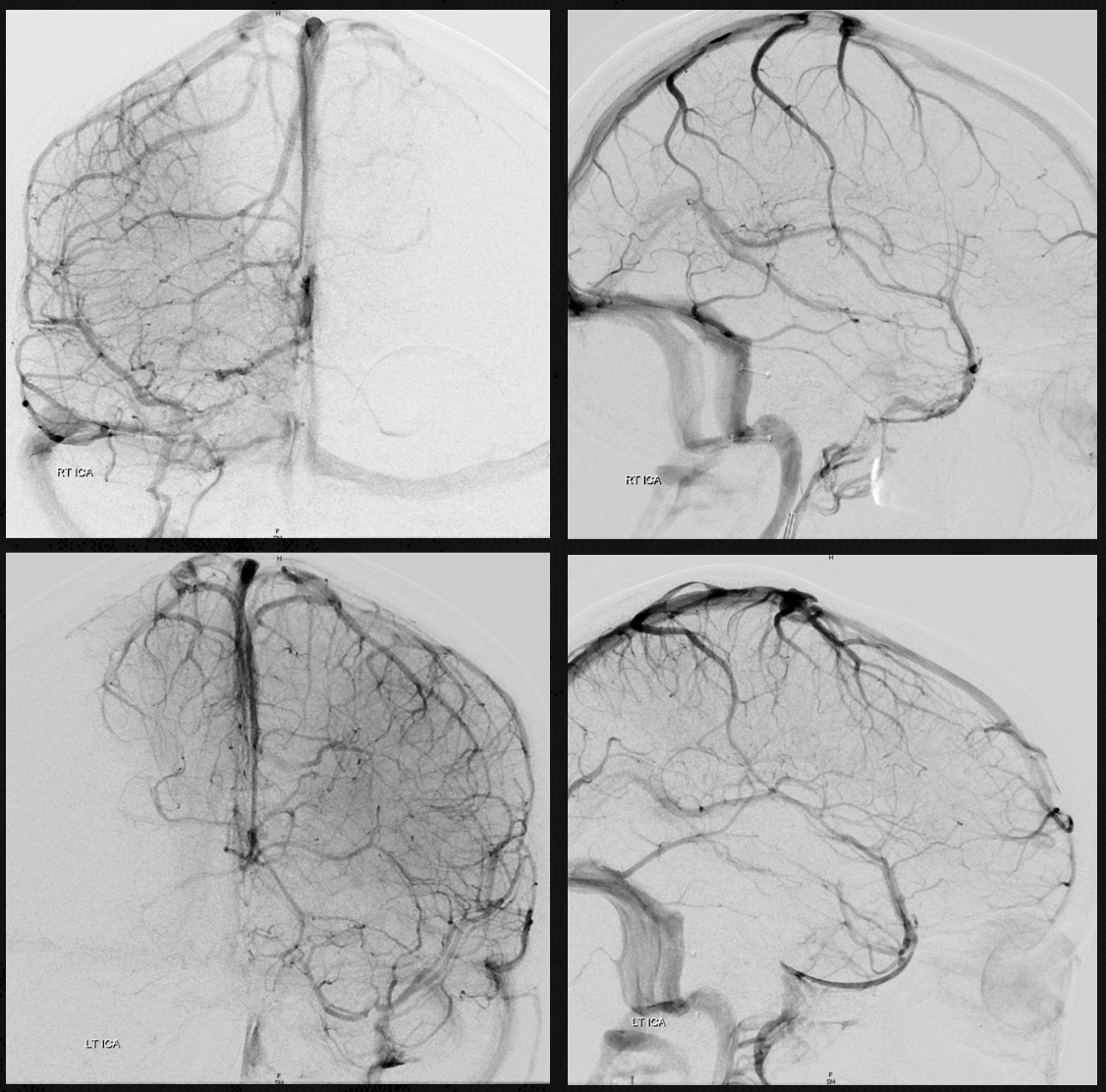
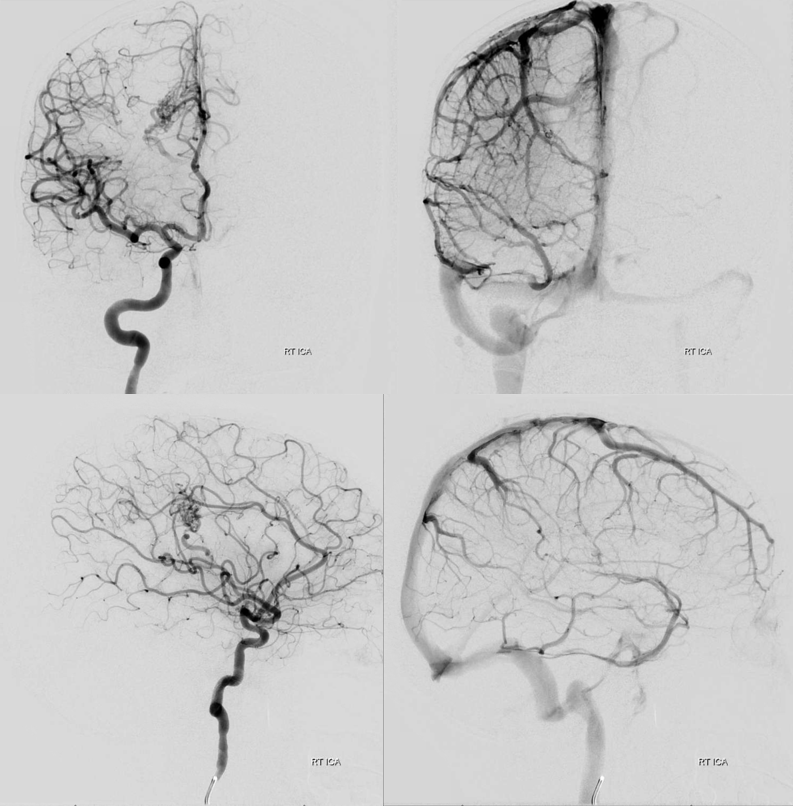
Below is a case of severe venous sinus thrombosis and secondary parenchymal venous infarcts
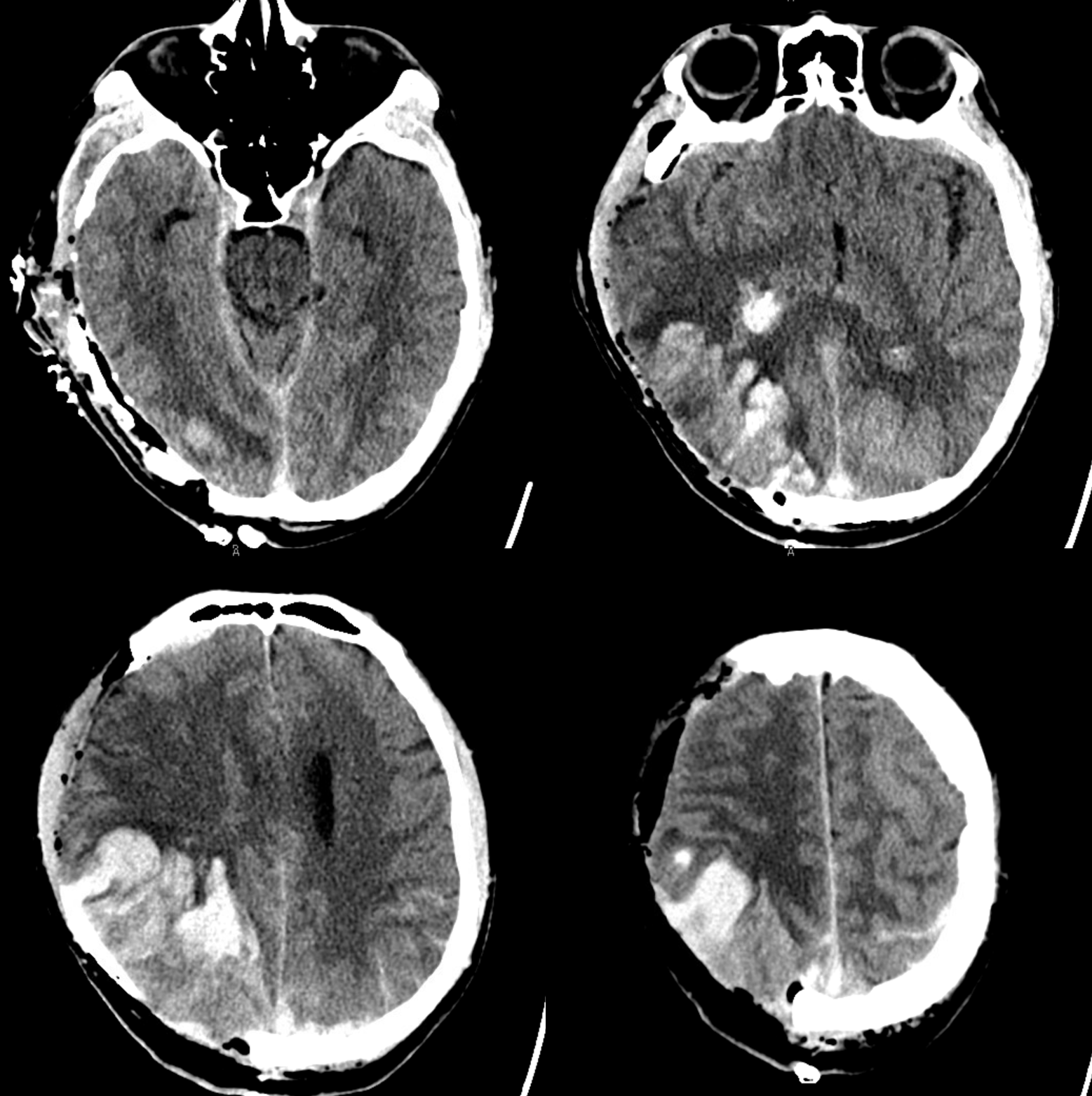
The explanation for the above tragic pattern is below. On the right, sigmoid and transverse sinuses are patent. However, the Labbe is hypoplastic, and majority of outflow used to go to the Trolard, into the now occluded SSS. There is no other effective way to go — the trolard tries to decompress via a left diploic vein, and convexity tries to access the deep venous system (which normally should not be well-seen in setting of hypoplastic right A1 segment). The left situation is much better, as well-developed superficial sylvian veins drain into the patent Cavernous Sinus. Thus, despite thrombosis of the left transverse and sigmoid sinuses, the left hemisphere is doing better, while the right one, which has patent transverse and sigmoid sinuses, is devastated.
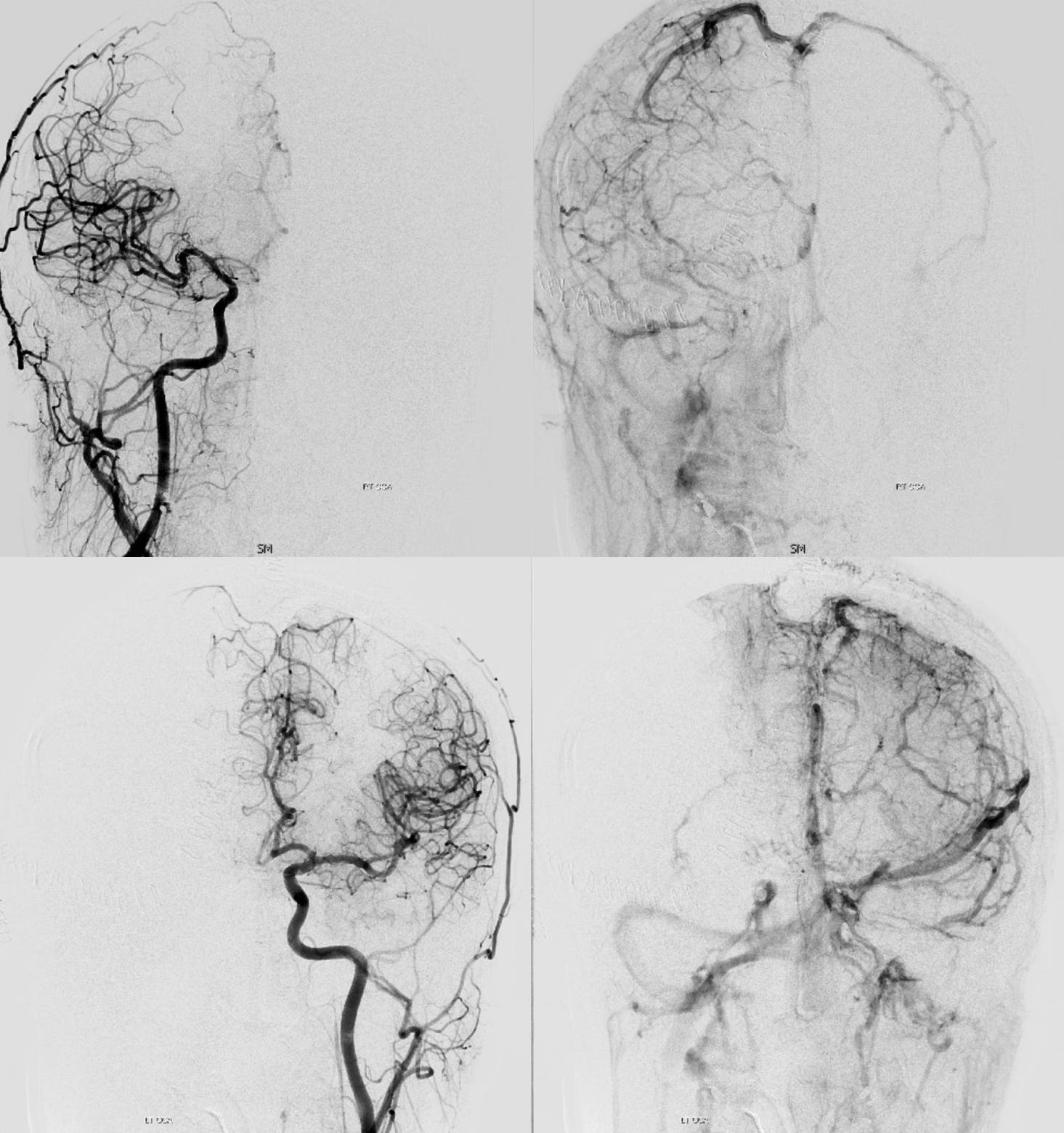
Post venous thrombectomy — with limited results. Note presence of same left diploic vein as seen in right ICA injection, and connection between the distal superior sagittal sinus and the deep venous system via the inferior sagittal sinus.
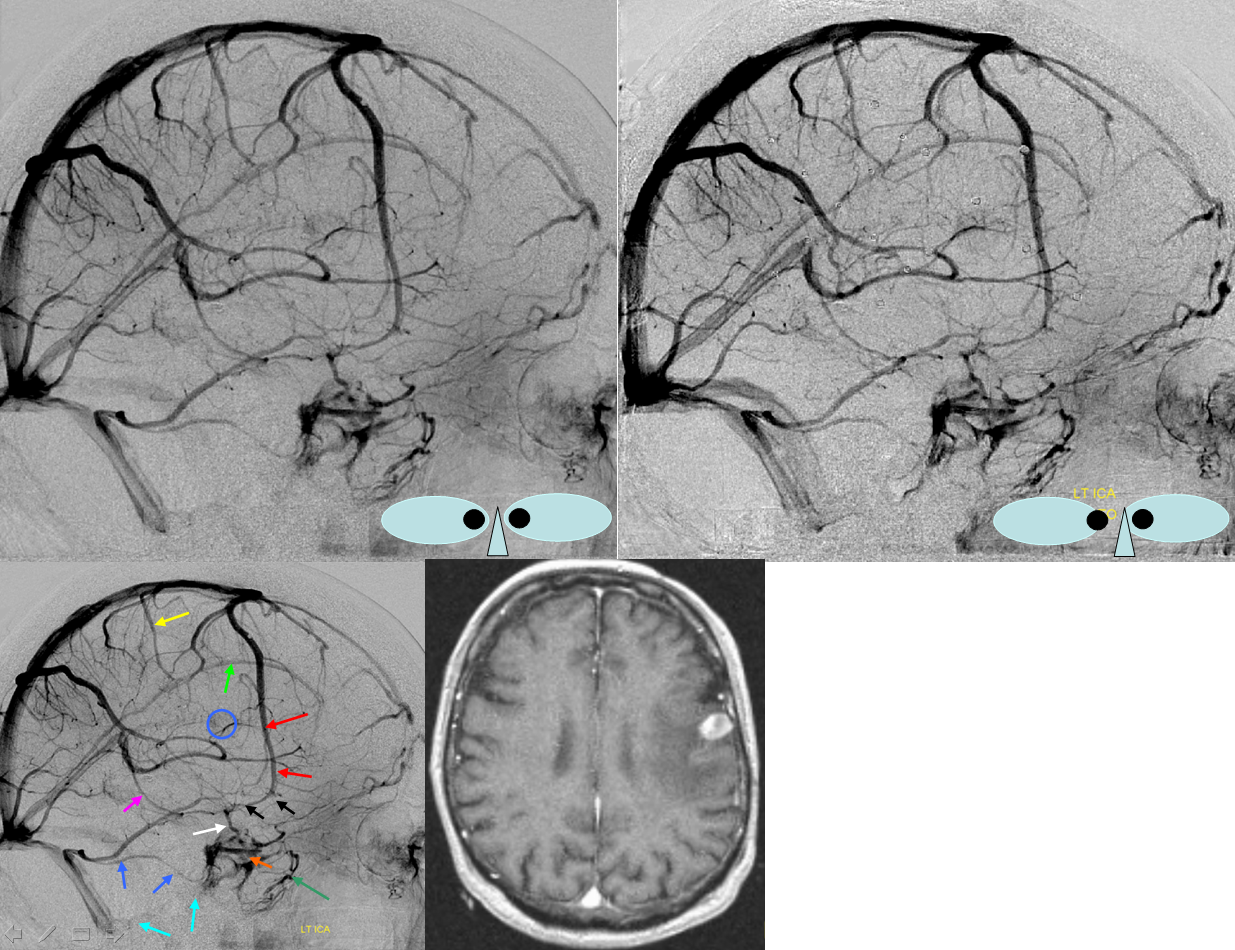
Sturge-Weber Syndrome, a.k.a. Encephalotrigeminal Angiomatosis
SWS is part of a family of neurocutaneous disorders, characterized by abnormalities of ecto- and endoderm. The cutaneous part is a port wine stain (in CN V distribution). The brain part is described below. About 1/3 of patients only have the skin part, 1/3 have only brain, and 1/3 both — no rocket science here. The cause is unknown. There are many sources of excellent information on the Web, but I am afraid that most individuals do not appreciate the underlying vascular issues of SWS in the brain, which is illustrated angiographically below.
Cerebral manifestations of SWS appear to stem from abnormal development of the venous system — particularly surface veins. The hallmark of venous imaging is absence of superficial veins (including basal vein, which is only deep as far as the surgeon is concerned, being in fact a superficial vein on the undersurface). As a result, venous drainage is impaired, with secondary tremendous venous congestion. The congestion leads to engorgement of countless small veins throughout the parenchyma, and particularly on the gyral surface. This produces the characteristic gyral enhancement seen on MRI, and venous congestion that is better appreciated angiographically. The characteristic gyral calcifications probably result from chronic venous congestion.
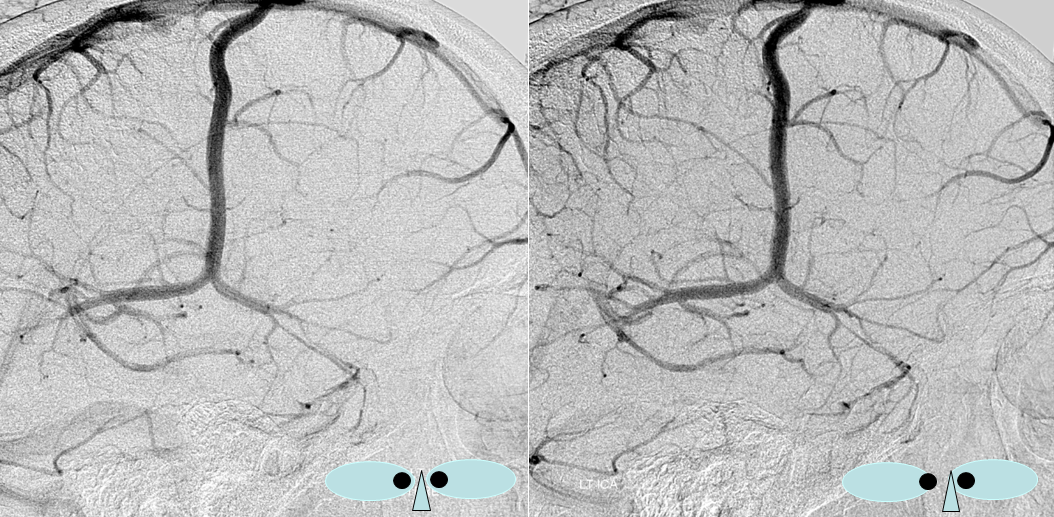
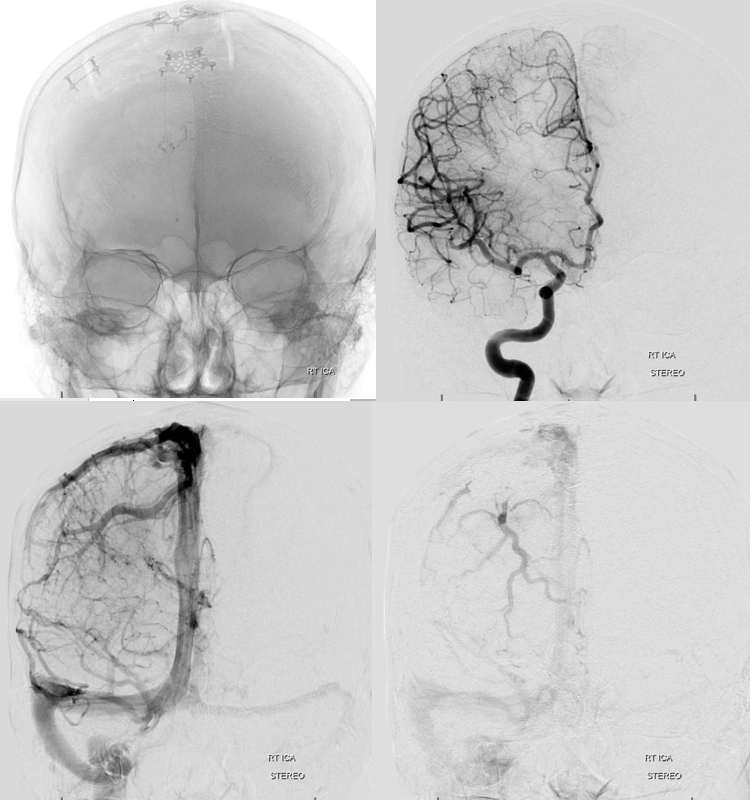
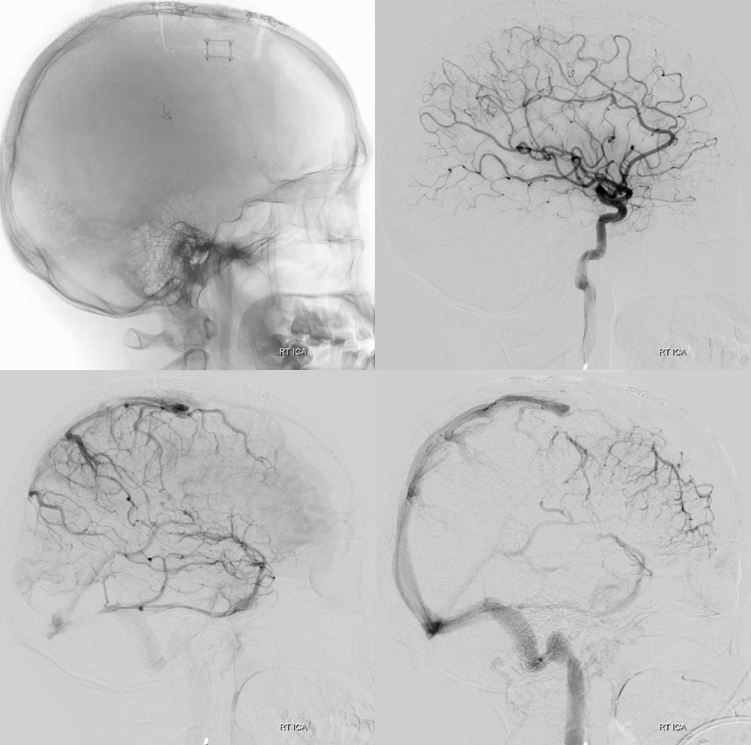
This is a young patient with intractable seizures.
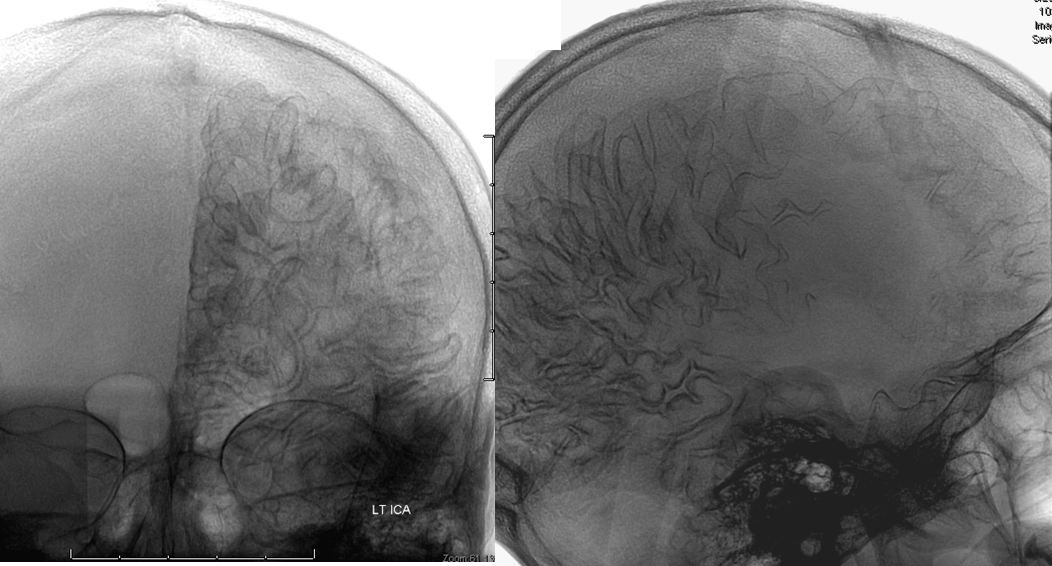
x-ray views of the skull, showing extensive gyral calcifications on background of cerebral atrophy.
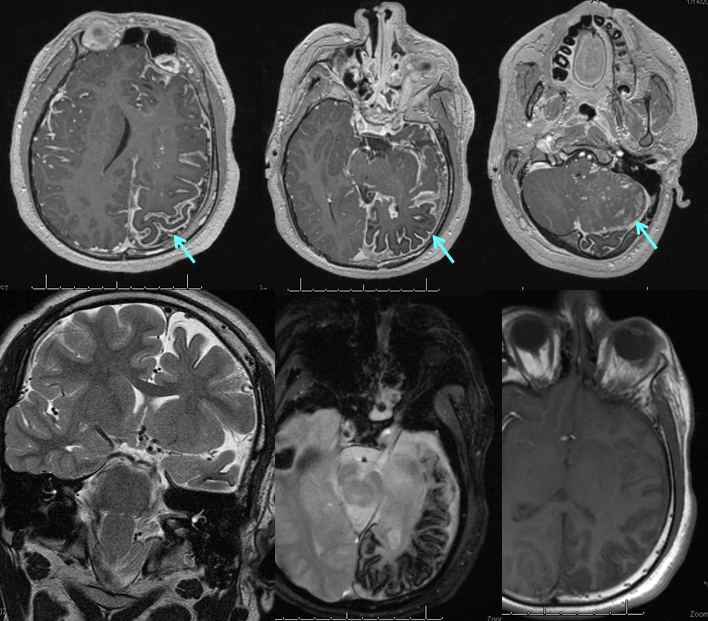
Various MRI sequences highlighting atrophy, calcifications, and gyral pattern of enhancement (top row). Notice absence of left basal vein, and most surface convexity veins.
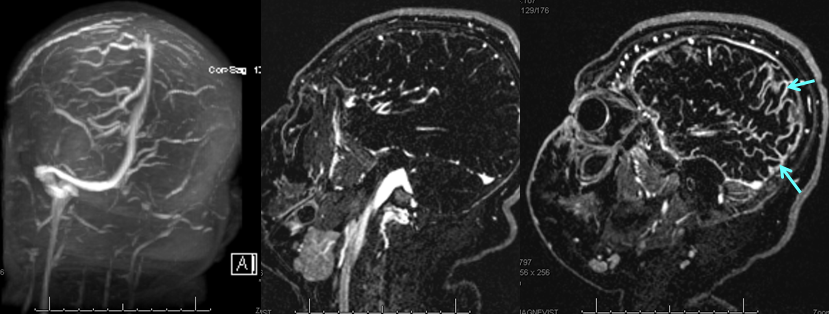
TOF and venovibe images; almost normal venous pattern on the right, and gyral enhancement (arrows) as well as transosseous venous channels on the left.
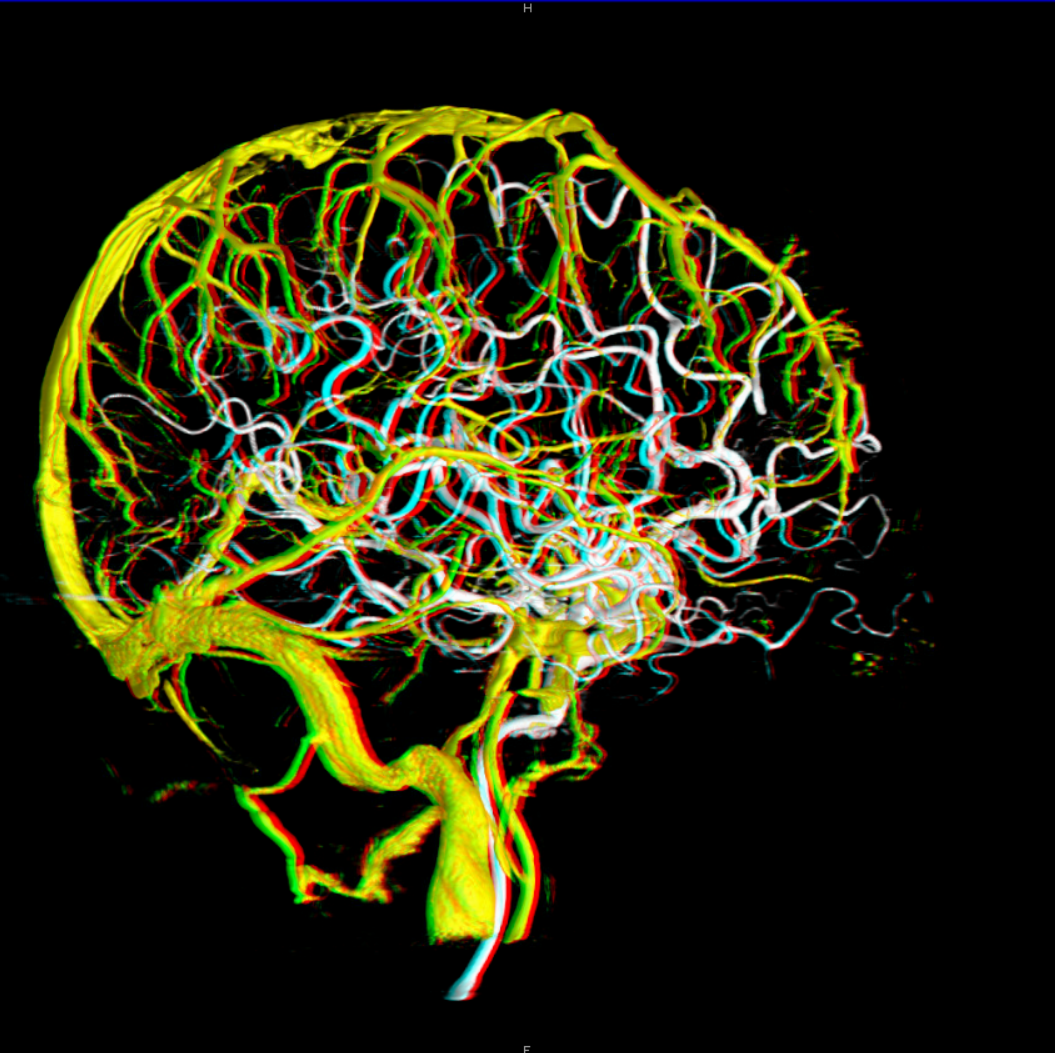
Stereoscopic views (top) and labeled image (bottom) of quasi-normal right ICA injection; convexity surface veins are present. A tremendous, tortuous basal vein (blue arrows) is working overtime. Some of its lenticulostriate tributaries, pathologically enlarged (why?) are labeled yellow. The convexity drainage is dominated by superficial sylvian veins (purple). What vein is missing?

Anaglyph Stereo
 Anaglyph Stereo
Anaglyph Stereo