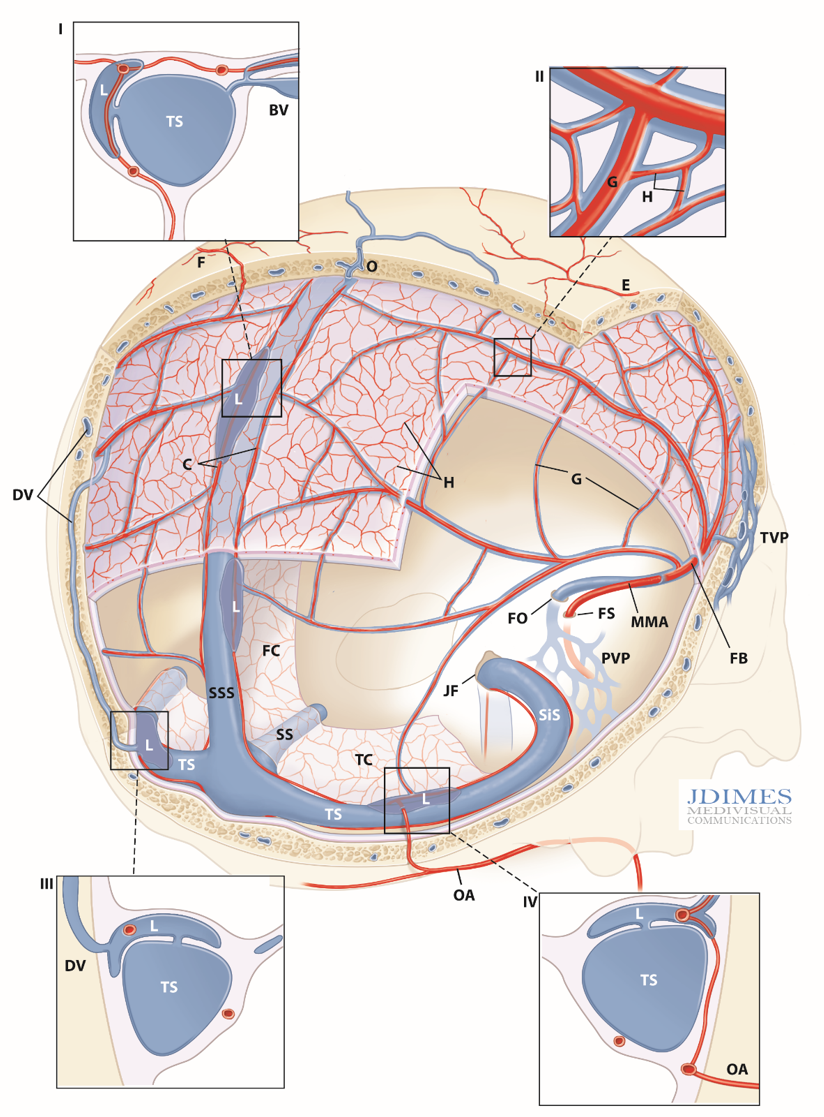
Schematic of intrinsic dural venous system and its drainage — artwork of Jonathan Dimes of JDIMES MEDIVISUAL. I-IV: detail inserts; BV – Bridging Vein (cortical); C – arterial network in sinus walls; DV – Diploic Vein, parietosquamosal region; E – cutaneous artery; F – superficial artery participating in dural supply; FB – Frontal Branch, MMA; FC – Falx Cerebri; FO – Foramen Ovale, FS – Foramen Spinosum; G – primary arterial anastomotic network of the outer layer (100-300 um diameter), H – secondary arterial anastomotic network of the outer layer (50-90 um diameter); JF – Jugular Foramen; L- venous lakes / pouches in walls of major sinuses; MMA– Middle Meningeal Artery; PVP – Pterygopalatine Venous Plexus; SiS – Sigmoid Sinus; SS – Straight Sinus; SSS – Superior Sagittal Sinus; TC – Tentorium Cerebelli; TVP – Temporalis Venous Plexus
DURAL VENOUS SYSTEM
This is totally new. No one has published on intrinsic dural venous system in vivo visualization as of 2021. There are very view ex-vivo studies (see bibliography below).
As we (Eytan Raz, Erez Nossek, Kittipong Srivatanakul, Melanie Walker, Osman Mir, and Peter Kim Nelson) worked on the intrinsic dural arteries project (neuroangio page here, JNIS article here) we got interested in angiographic visualization of dural veins. This led to the first in vivo publication of this type of imaging in JNIS in March 2021. Below is an in-depth review of dural venous drainage, as we know it now.
What do we know? Padget’s famous work on venous development is true genius. No work in our neurovascular literature has withstood the test of time as well. She just had it. I am copying and pasting some of her plates here, with full credit, because they are just the best. Many people tried to ape them (including this author), with acknowledgement or not, but always with worse results than the original.

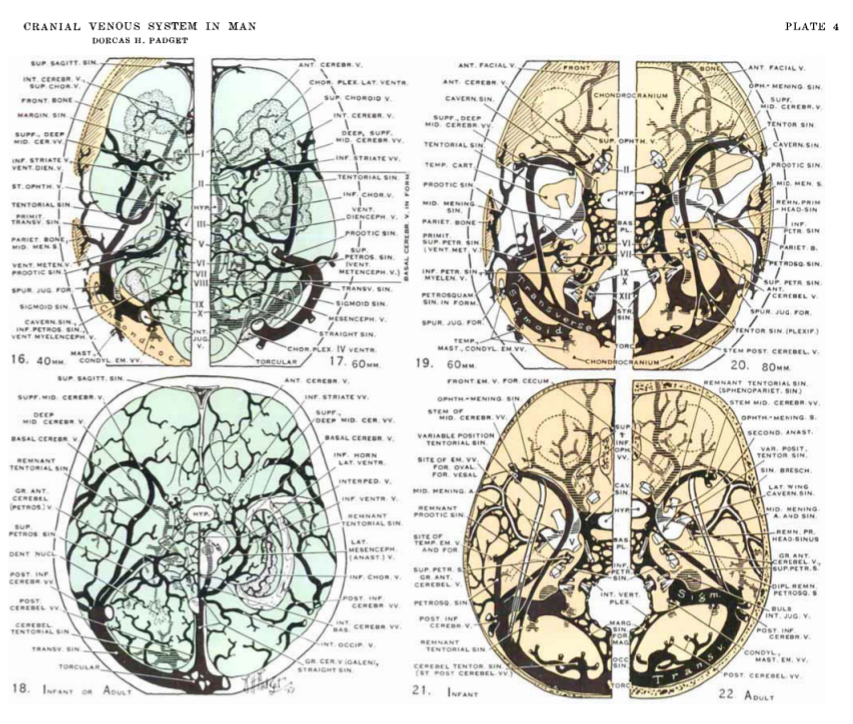
The above plates are complex, requiring real time investment to understand. In plate 4, yellow figures refer to dural venous sinuses mostly. In our discussion, the relevant structures are those draining the dura and skull — the “Remnant Tentorial Sinus”, the “Middle meningeal sinus” — more commonly mis-referred to as middle meningeal vein which is the main tram-tracking vein along the MMA, and finally the “petrosquamosal sinus” — which we will see a lot of down lower.
You can see our own “Cerebral Venous Embryology” page for some more info — but remember — Padget is Padget is the best.
Apart from Padget, we got a few ex-vivo studies that mostly focus on dural arteries, but some also cover veins. It’s not much info. The important points are how the outer layer network arteries are paralleled by veins — the tram-tracking appearance is well known. They are actually sinuses, not veins — going back to Paget’s. The other point is presence of dense venous plexi / lakes / pouches adjacent to the big venous sinuses (SSS, sigmoid, etc). These are probably very important in angioarchitecture and pathophysiology of dural fistulas. The third point is ex-vivo evidence of intrinsic and presumably physiologic dural arteriovenous shunts — precapillary level connections between outer layer dural arteries and veins. This has not been confirmed in vivo yet.
In vivo studies of dural venous system
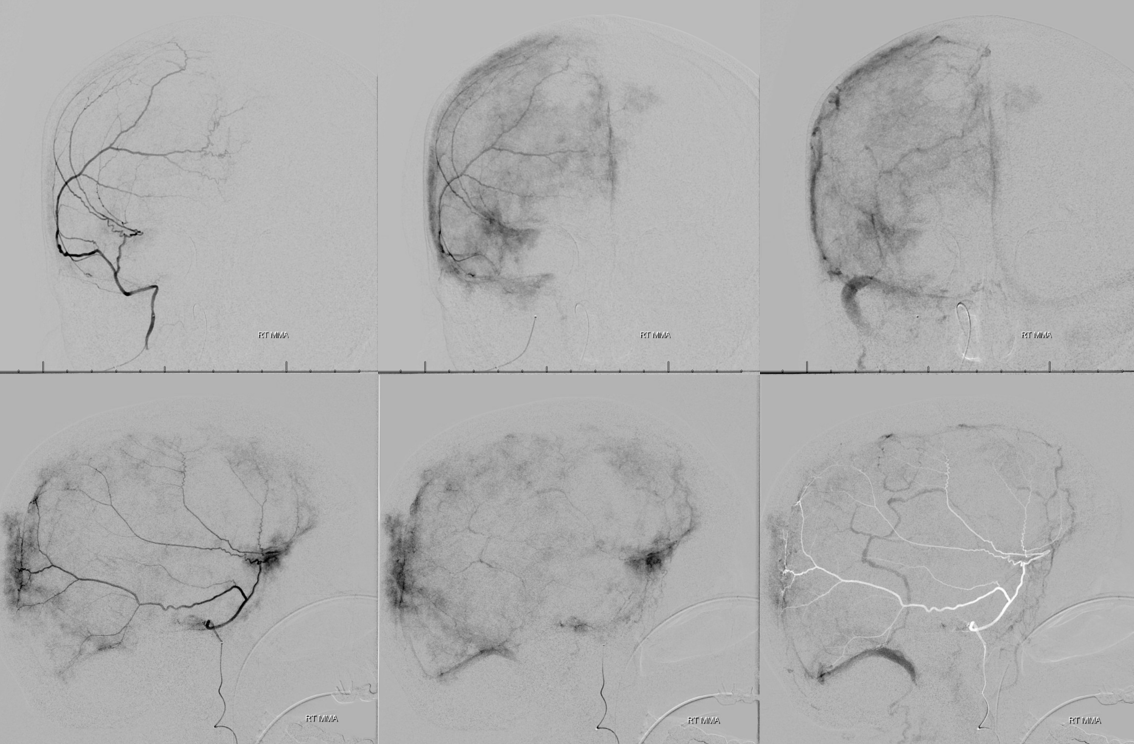
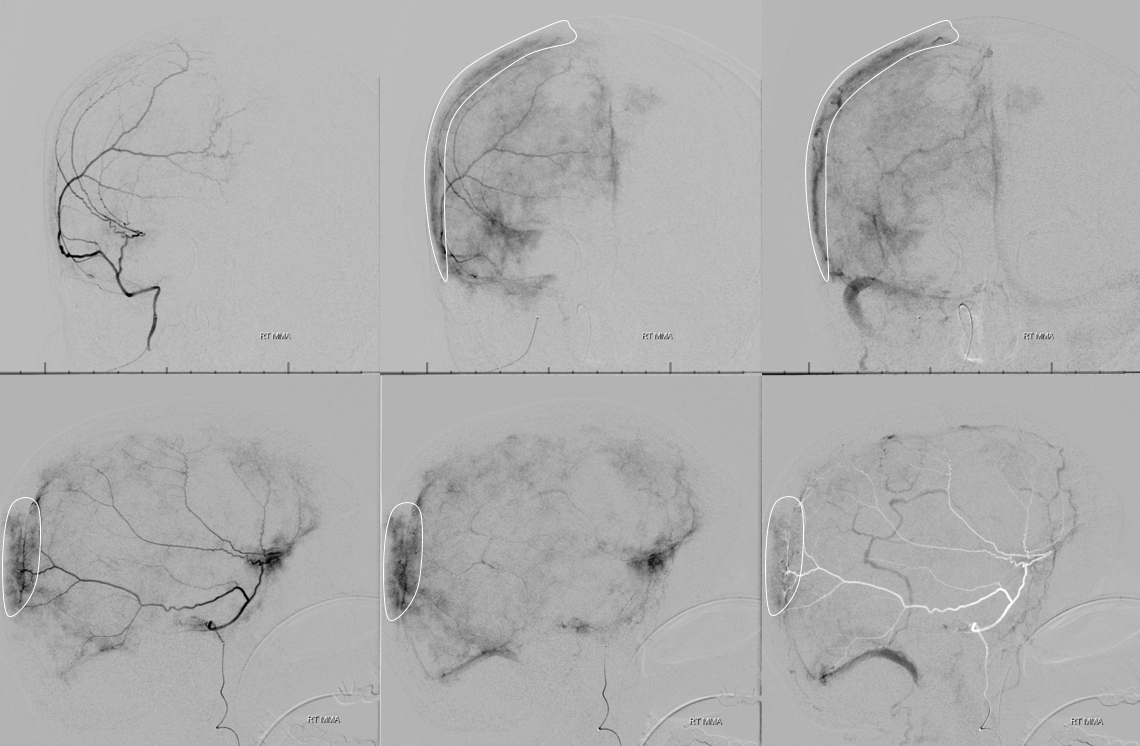
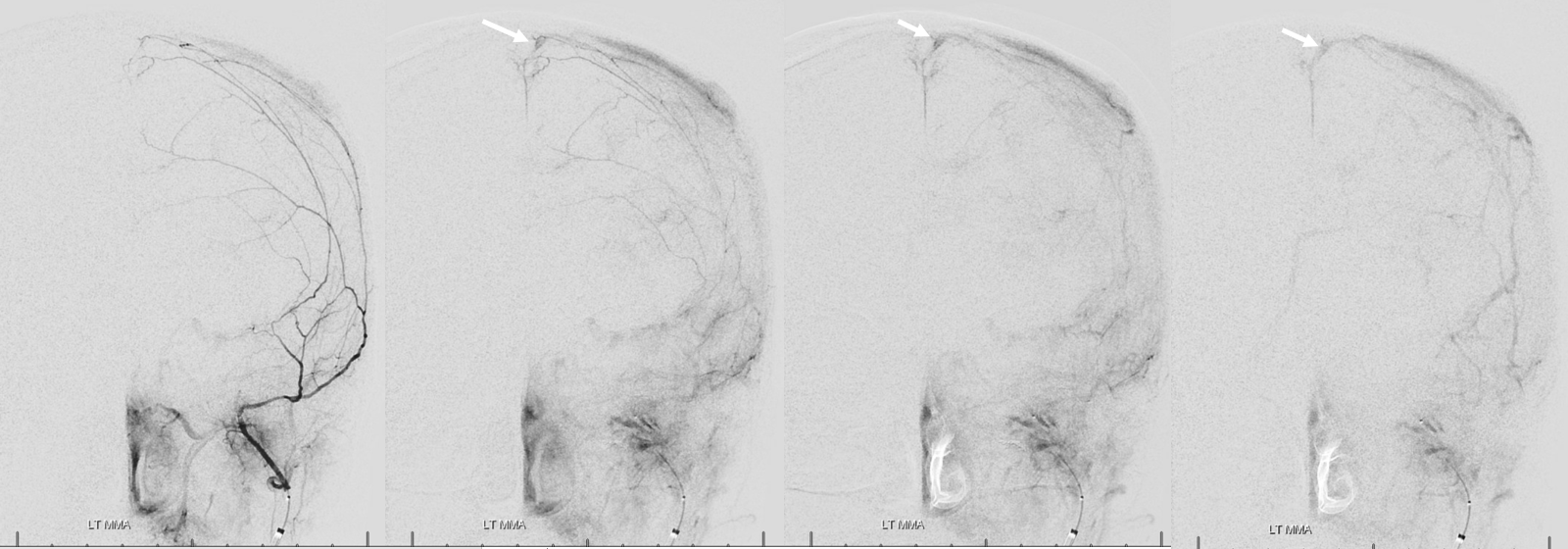
How do we visualize dural veins? Easy — patience. Just keep that pedal pressed down longer and they will appear. The technique is simple. An 021 microcatheter goes into the proximal MMA. Inject with 100% contrast to fill the MMA well at something like 0.3-0.5 ml/sec for about 5-10 seconds. Wait for veins. Set the DSA rate at 0.5 fps instead of the usual 2 or 3 pfs to minimize radiation. Of course, if your subject is awake and moving its not going to come out well. Needs GA. For rotational and DYNA CT, set delay at whatever delay veins appear on the DSA. For example, if arteries appear on frame 2 and veins on frame 11 of a 0.5 fps DSA, the delay should be 18 seconds. Now, if you inject contrast during the “mask” phase of Siemens spin, then you can get a triple-phase image like we will show below.
Now to the anatomy.
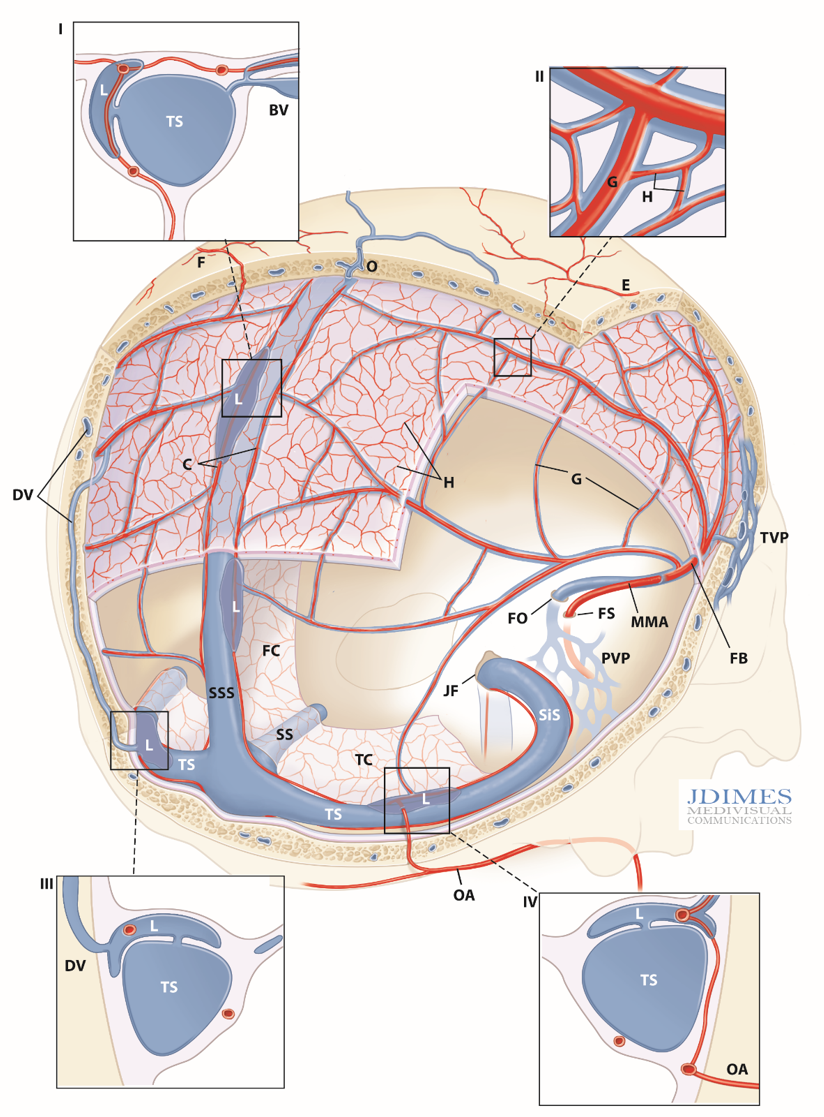
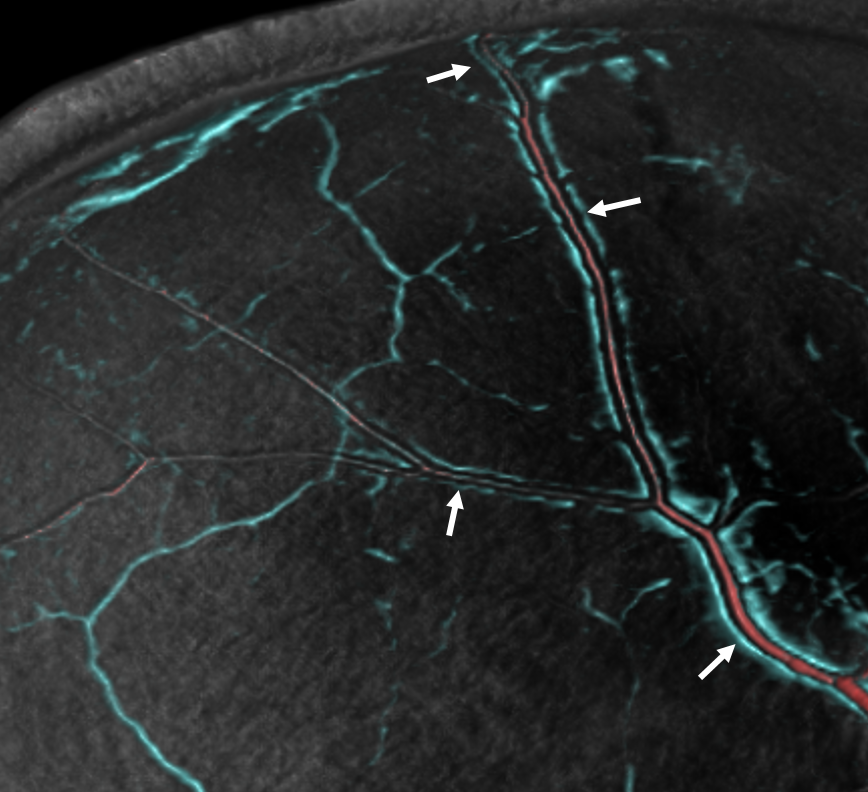
The outer layer arterial network (G, H) is paralleled by veins — those tram-tracking venous sinuses — they are actually sinuses. They are often well seen on DSA. This is the principal intrinsic dural venous system — veins / venous sinuses parallelling the arteries.
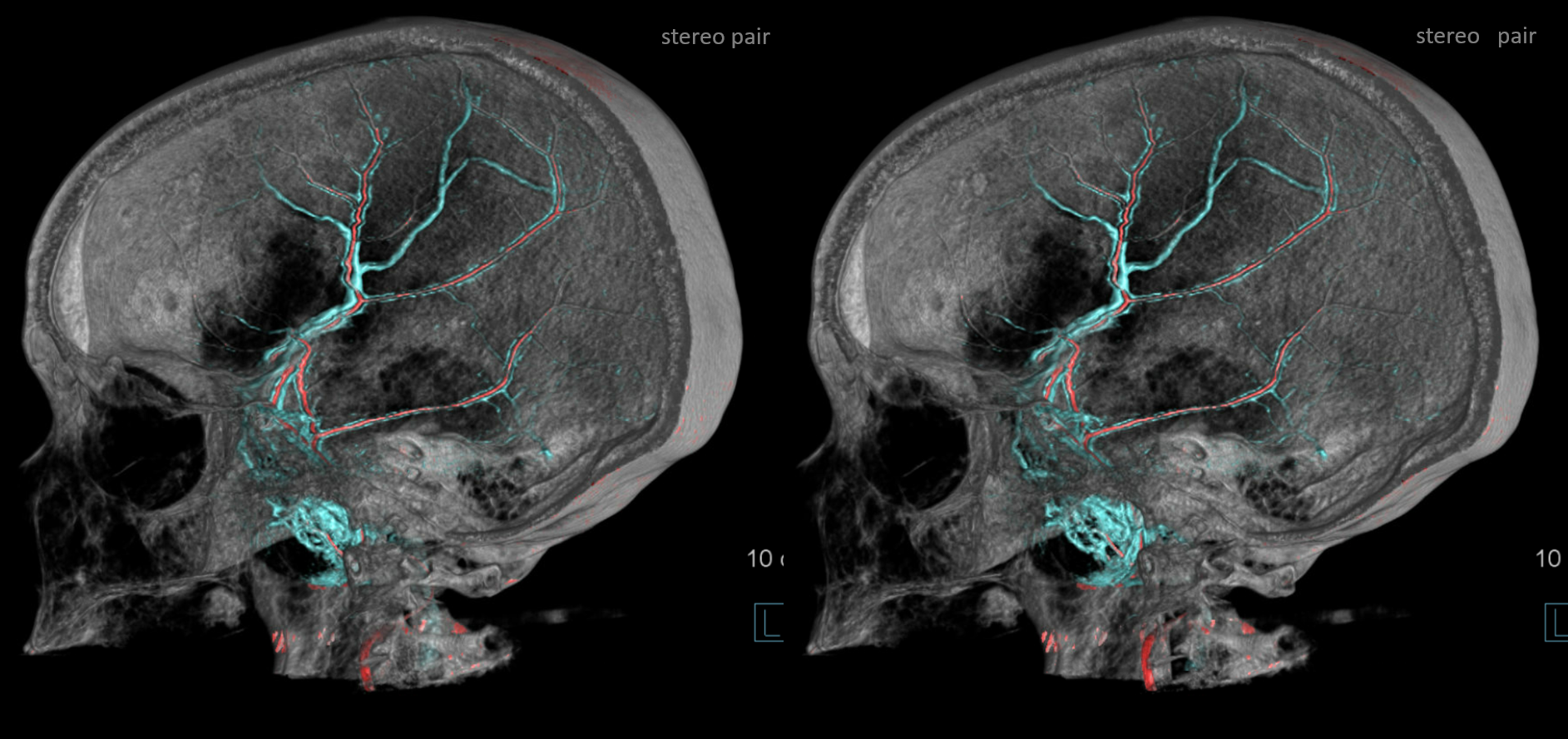
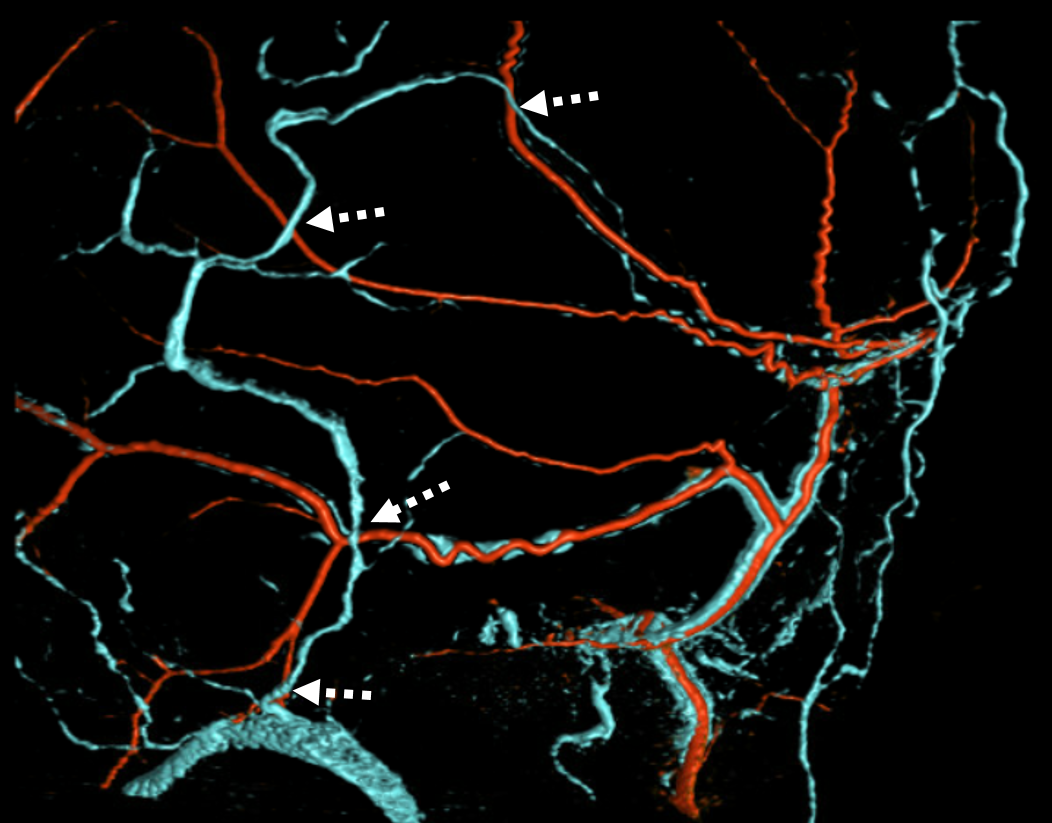
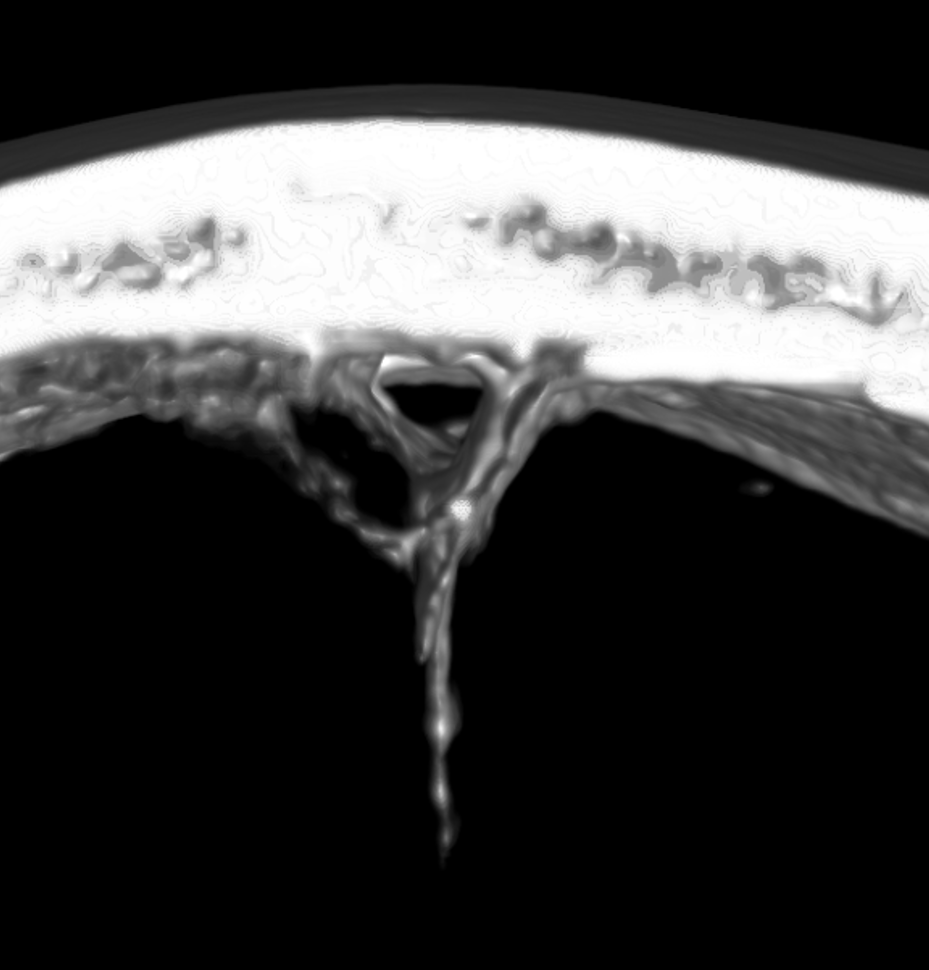
Beautiful example of dual volume rendered images of middle meningeal sinus along the MMA — notice some venous twigs coming at you — they are draining the skull!
GIF — note how the veins do not circumferentially surround the arteries

Anaglyph of same — color is changed to fit the anaglyph glasses better… nothing is perfect
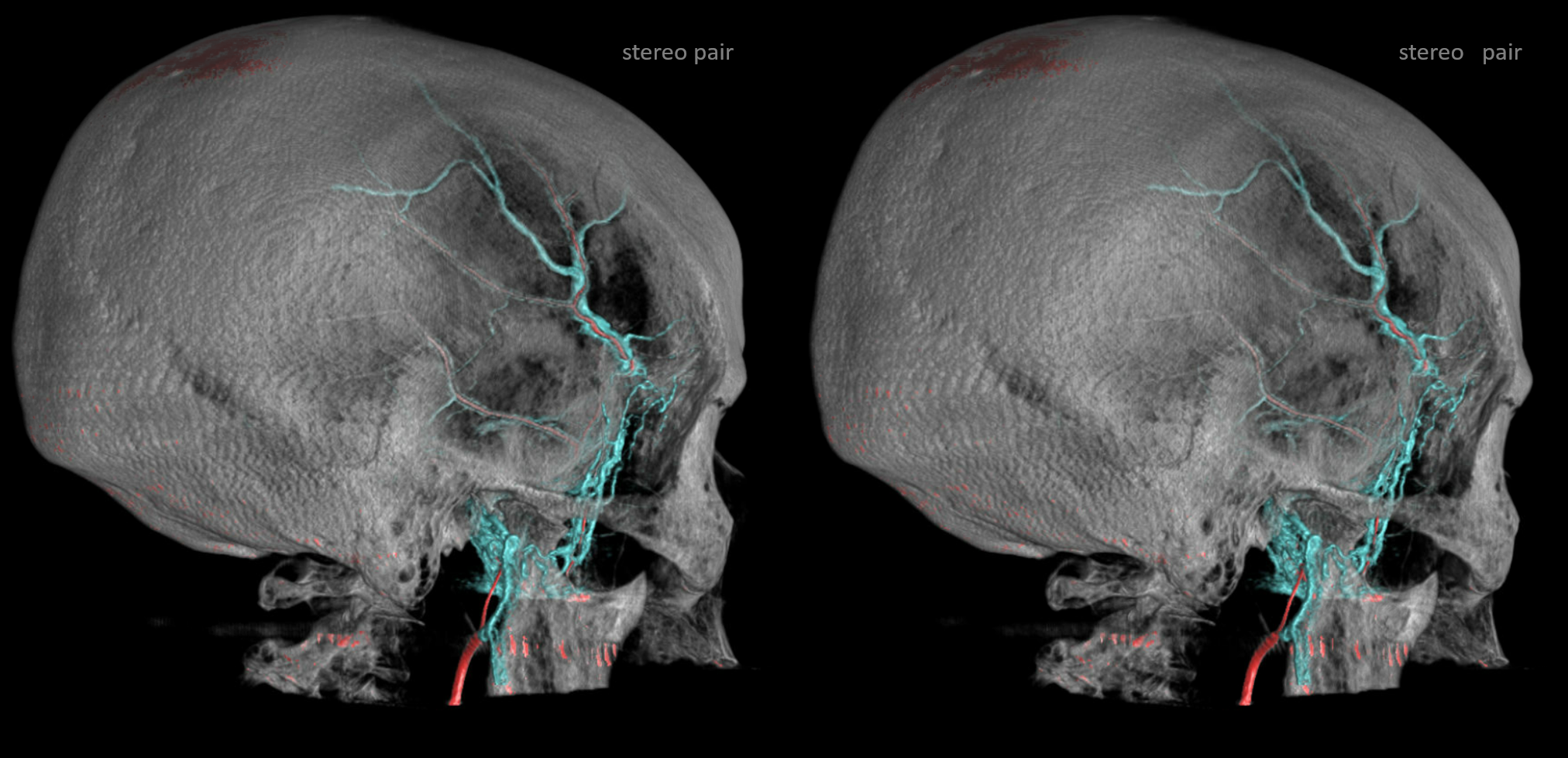
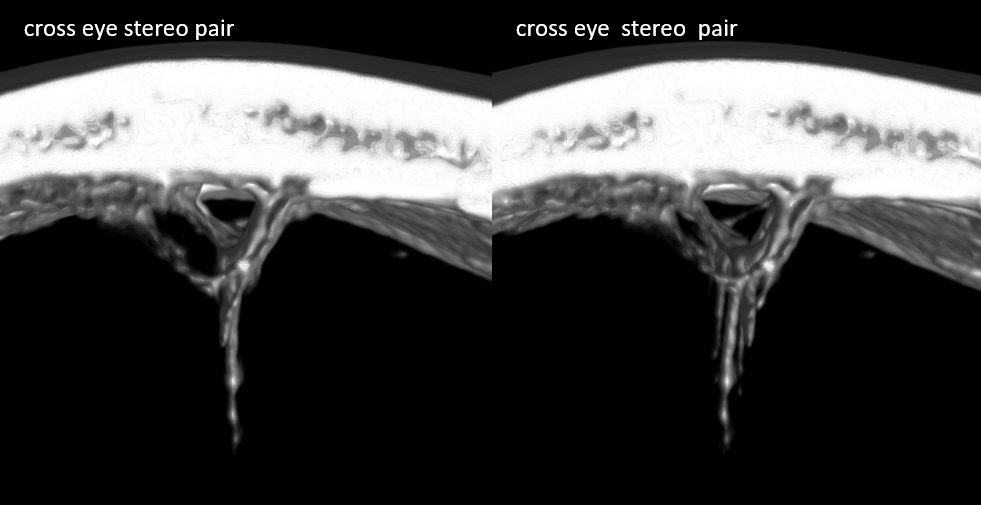
Although the tram-tracking veins are best seen where they are largest — along the main MMA trunk, they extend way deeper into the primary and secondary networks of the outer dural arterial layer (see dural arterial system for more info). Below are some examples of same tram-track a bit more distally
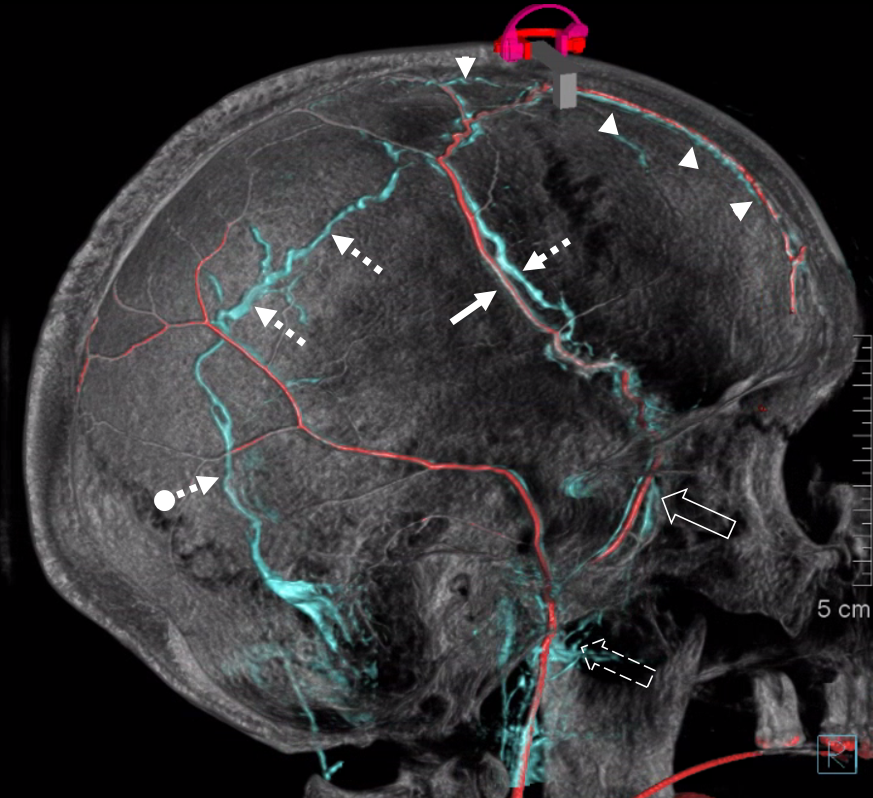
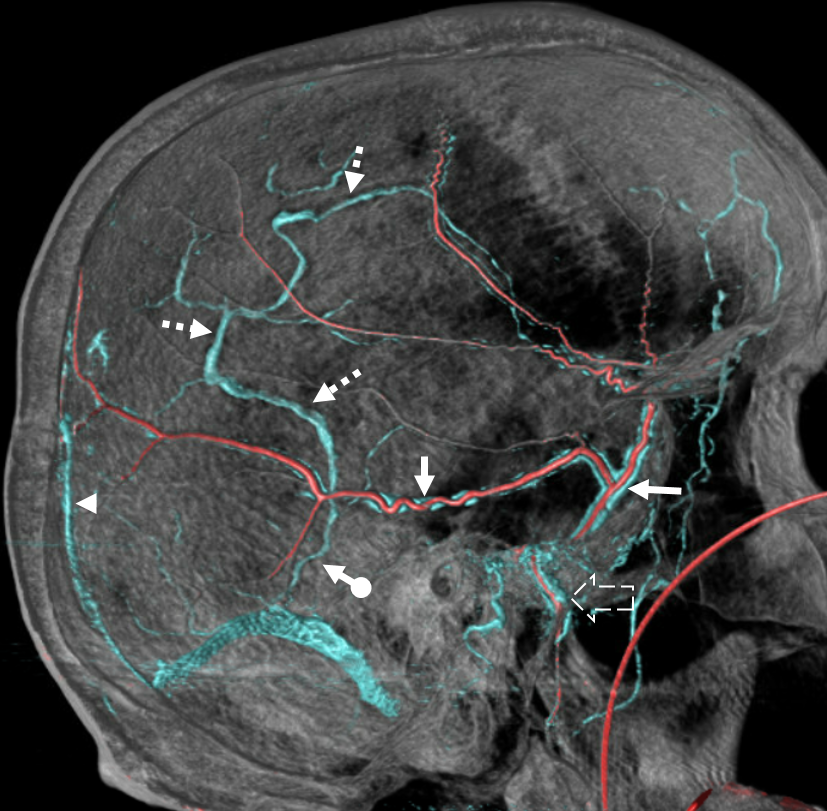
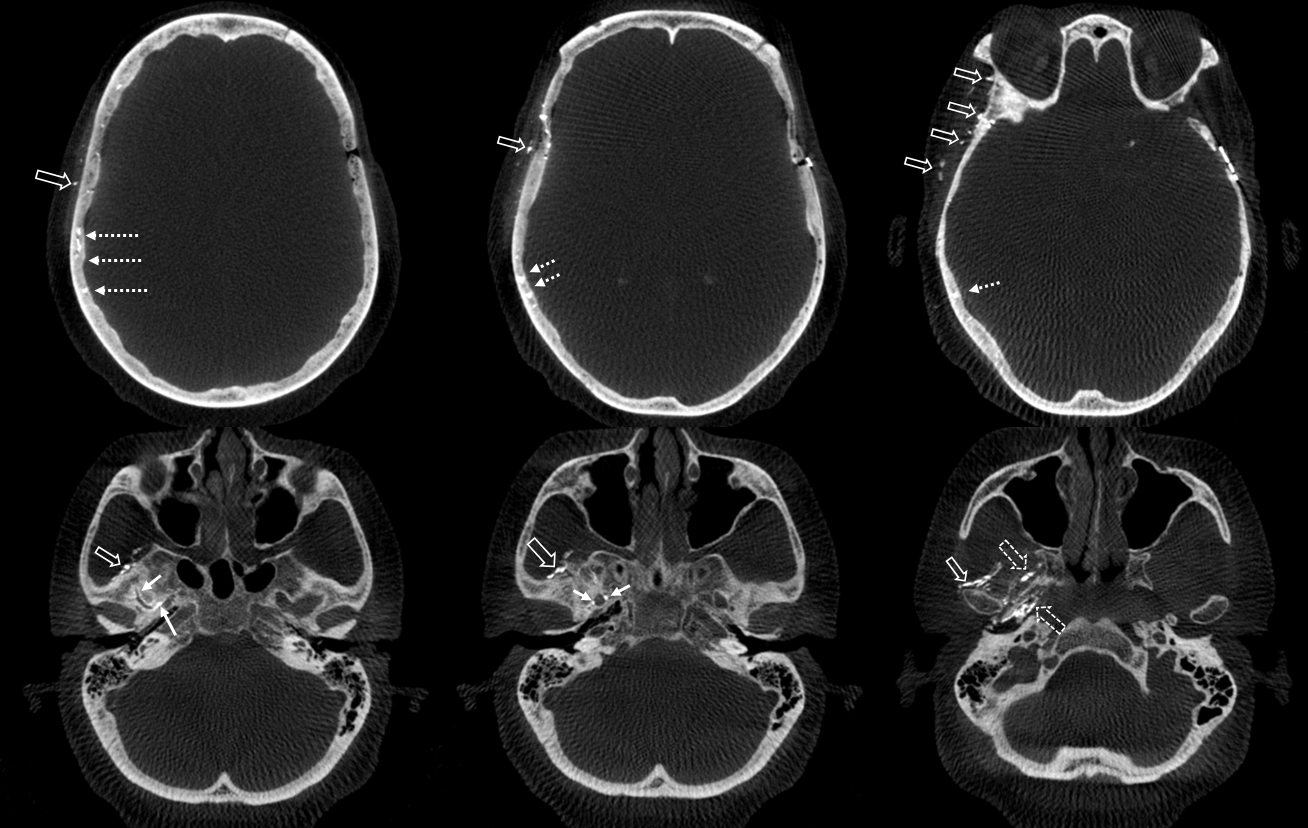
Some more advanced imaging can come in way of DYNA CT — this one is done by subtracting a pre-contrast DYNA from a post-contrast one — its tricky but can usually generate reasonable pictures. It is expected that this will improve with more technological progress. The arteries are marked with arrows, veins with arrowheads.
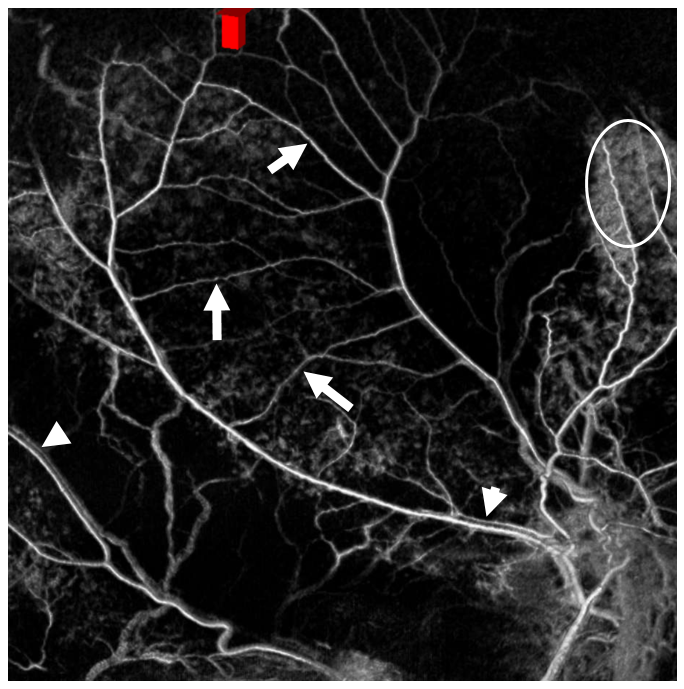
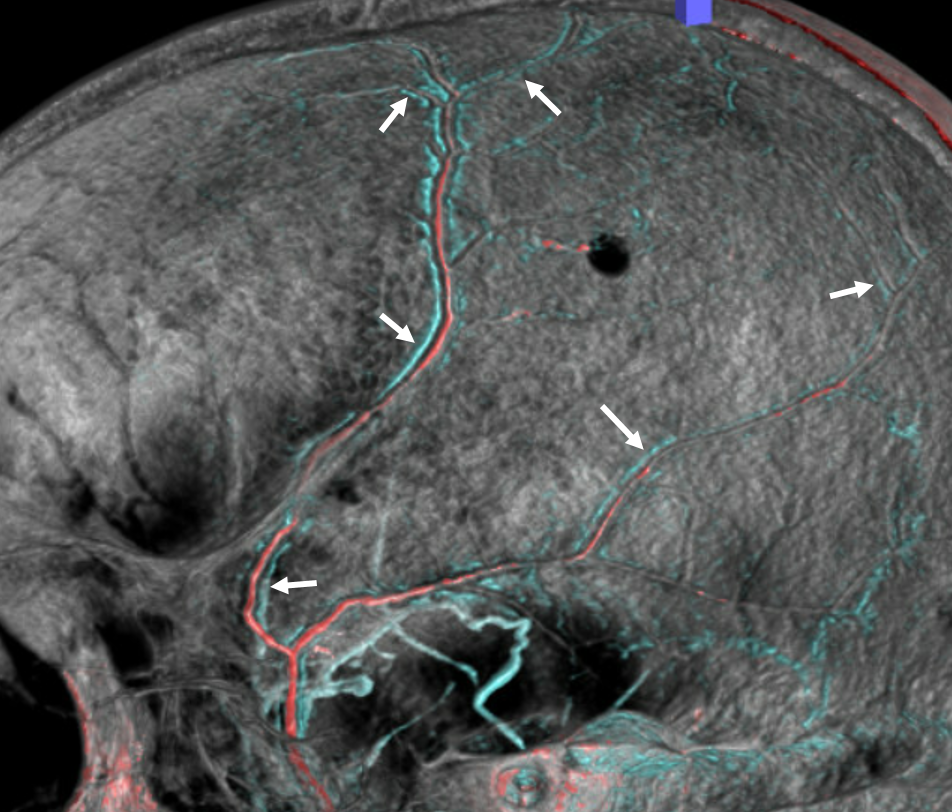
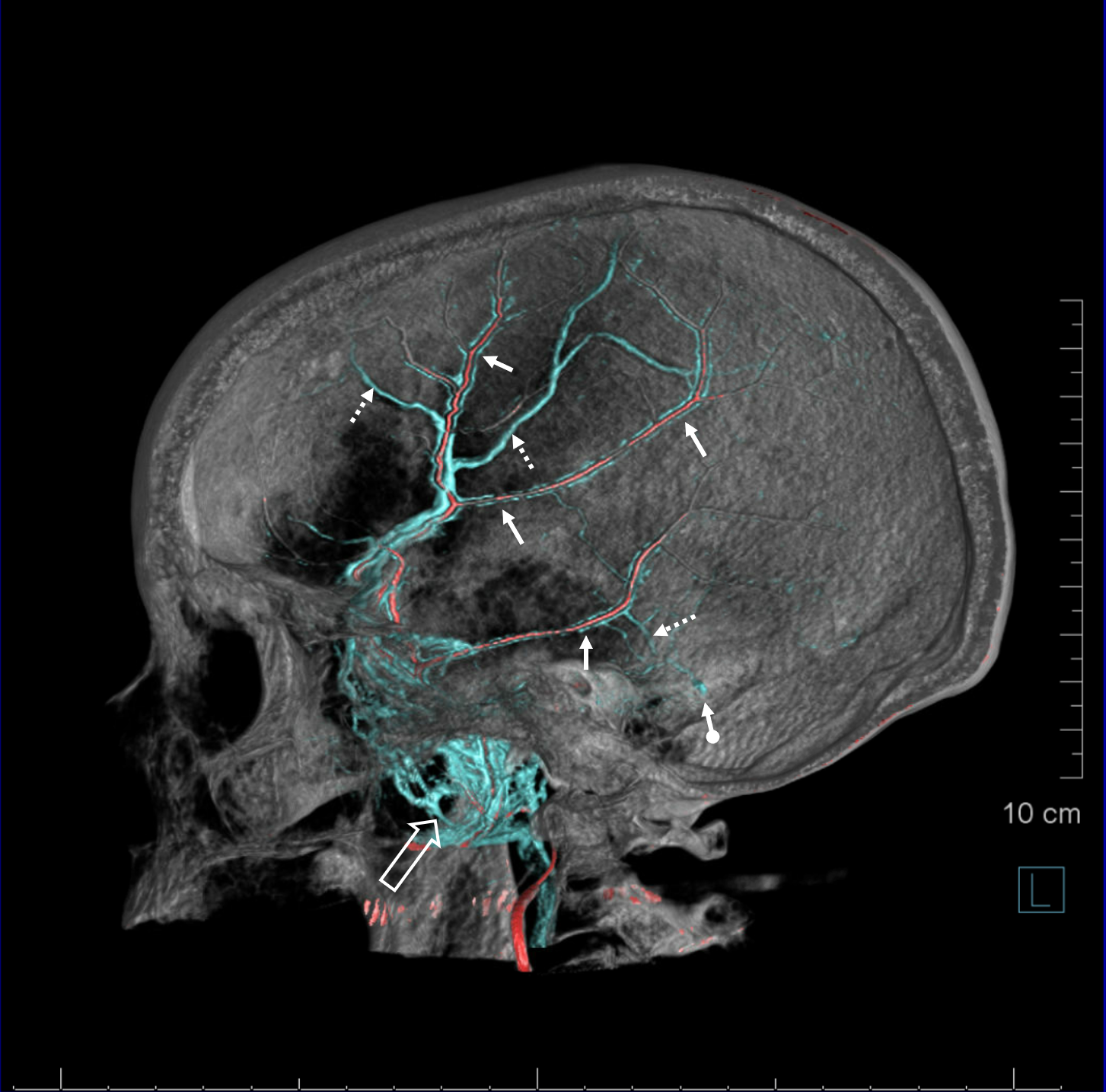
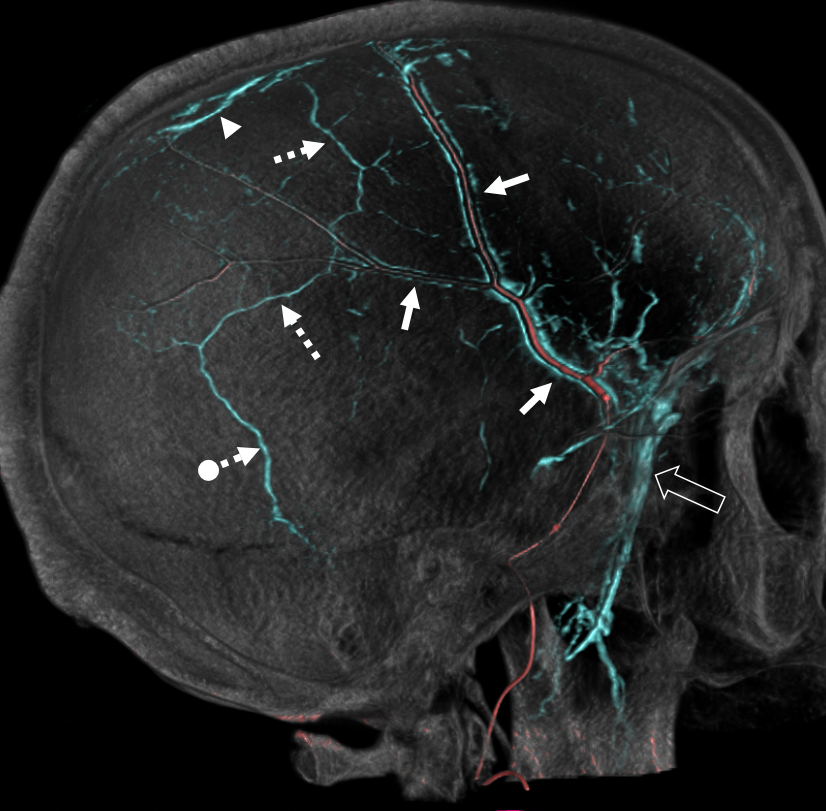
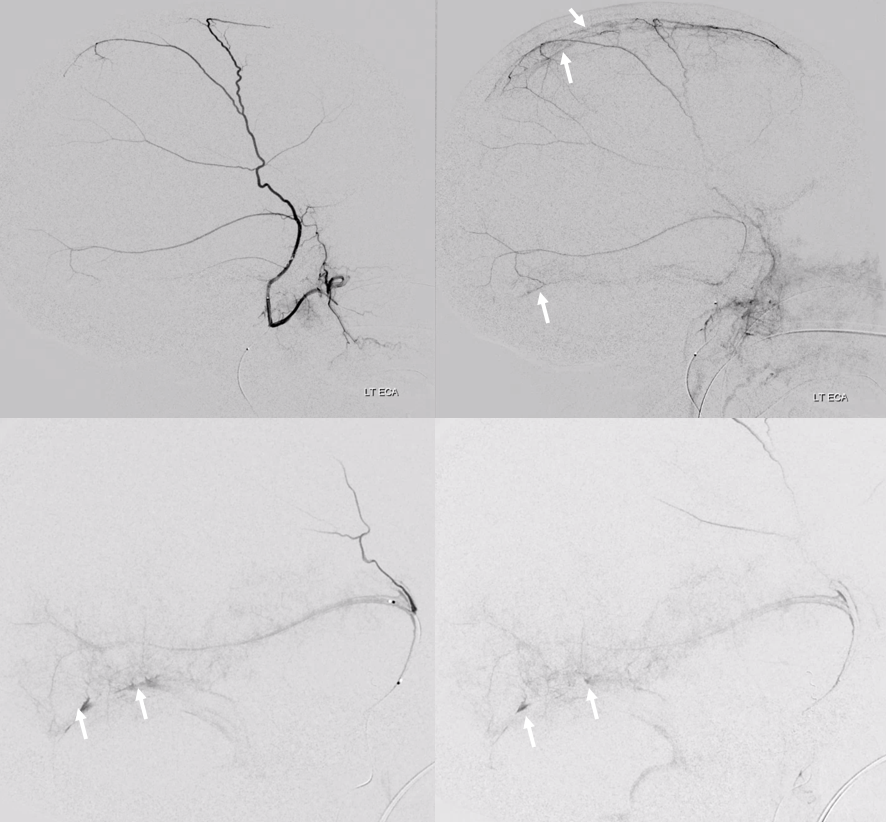
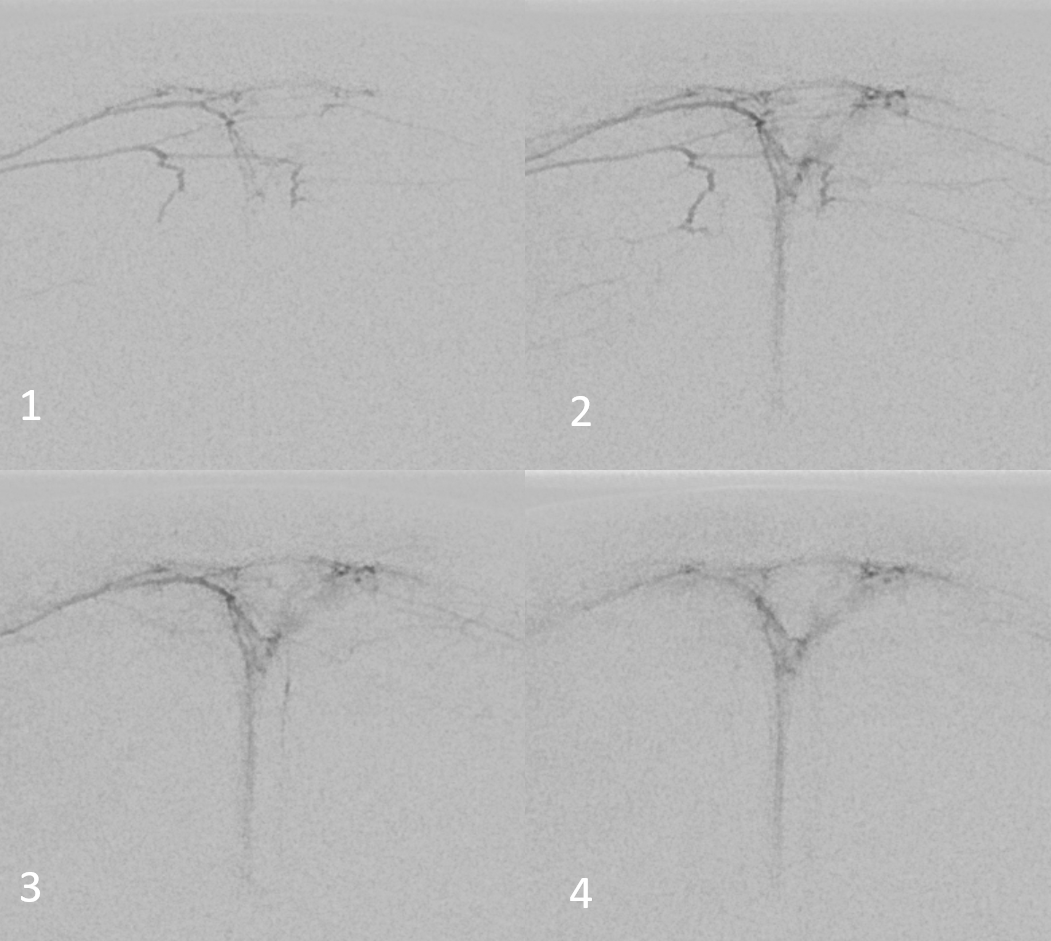
Good old DSA of arterial and venous phases is below, showing both tram-tracking dural sinuses (arrows) and diploic veins (dashed arrows) coalescing around proximal MMA, draining into temporalis and pterygopalatine (open arrow) venous plexi. Also note a small venous pouch in the usual sigmoid location (ball arrow — also visible in arterial phase image on upper left). Finally, frontal views show drainage along the sphenoid ridge (arrowhead) — this is Padget’s “remnant tentorial sinus” — or the true “sphenoparietal” sinus for anatomy purists — that is always confused with the adult version draining the sylvian veins.
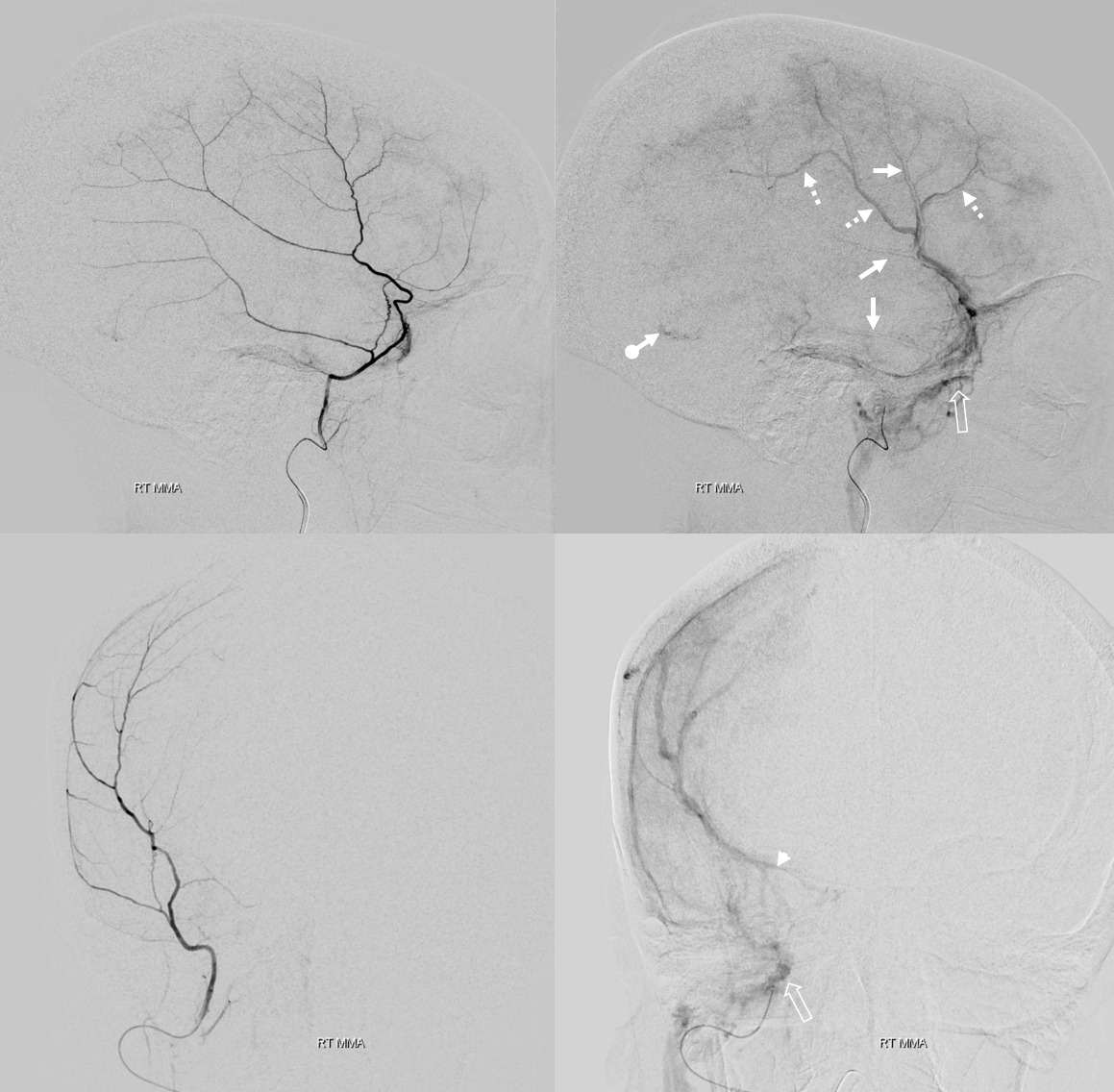
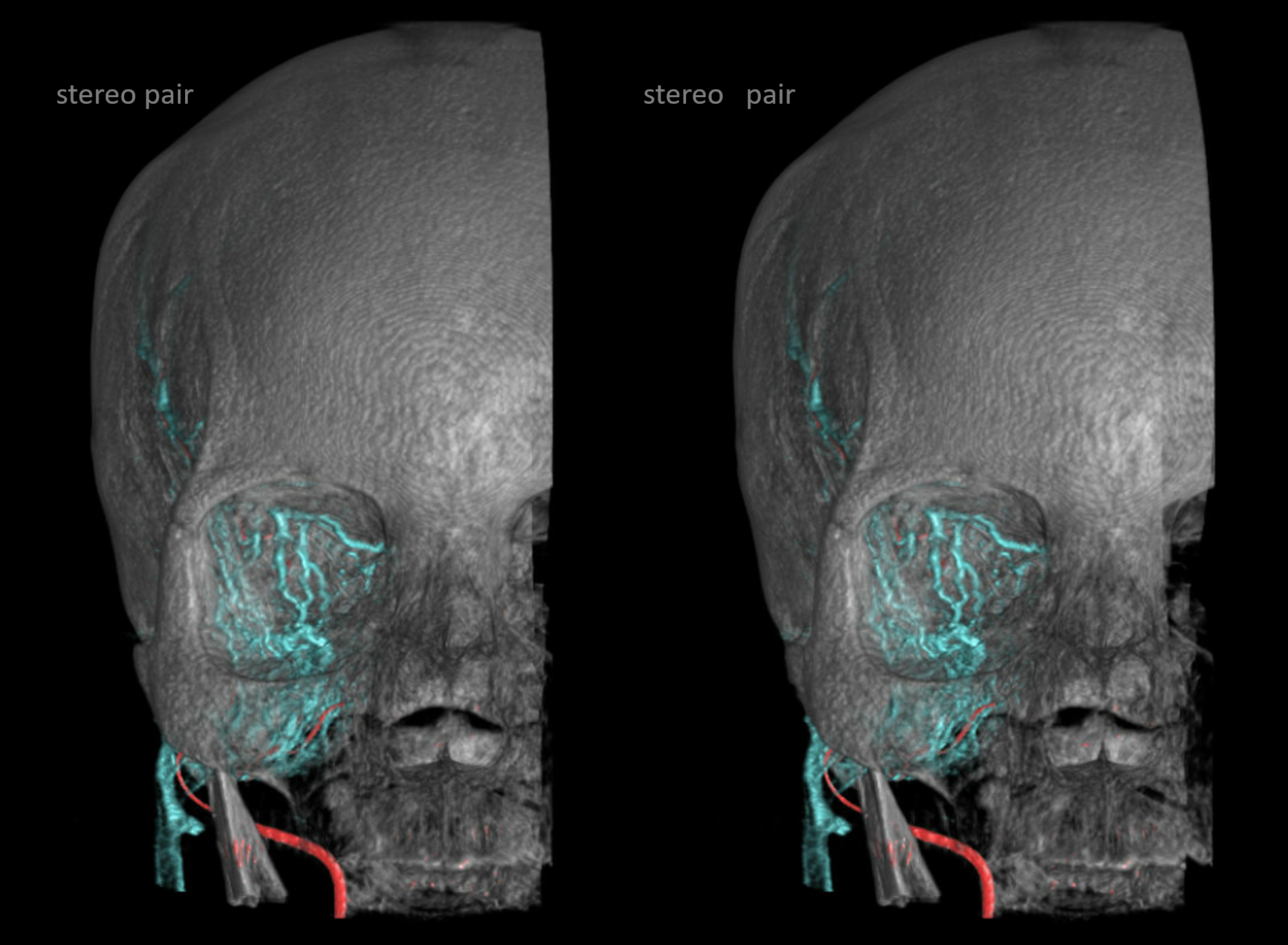
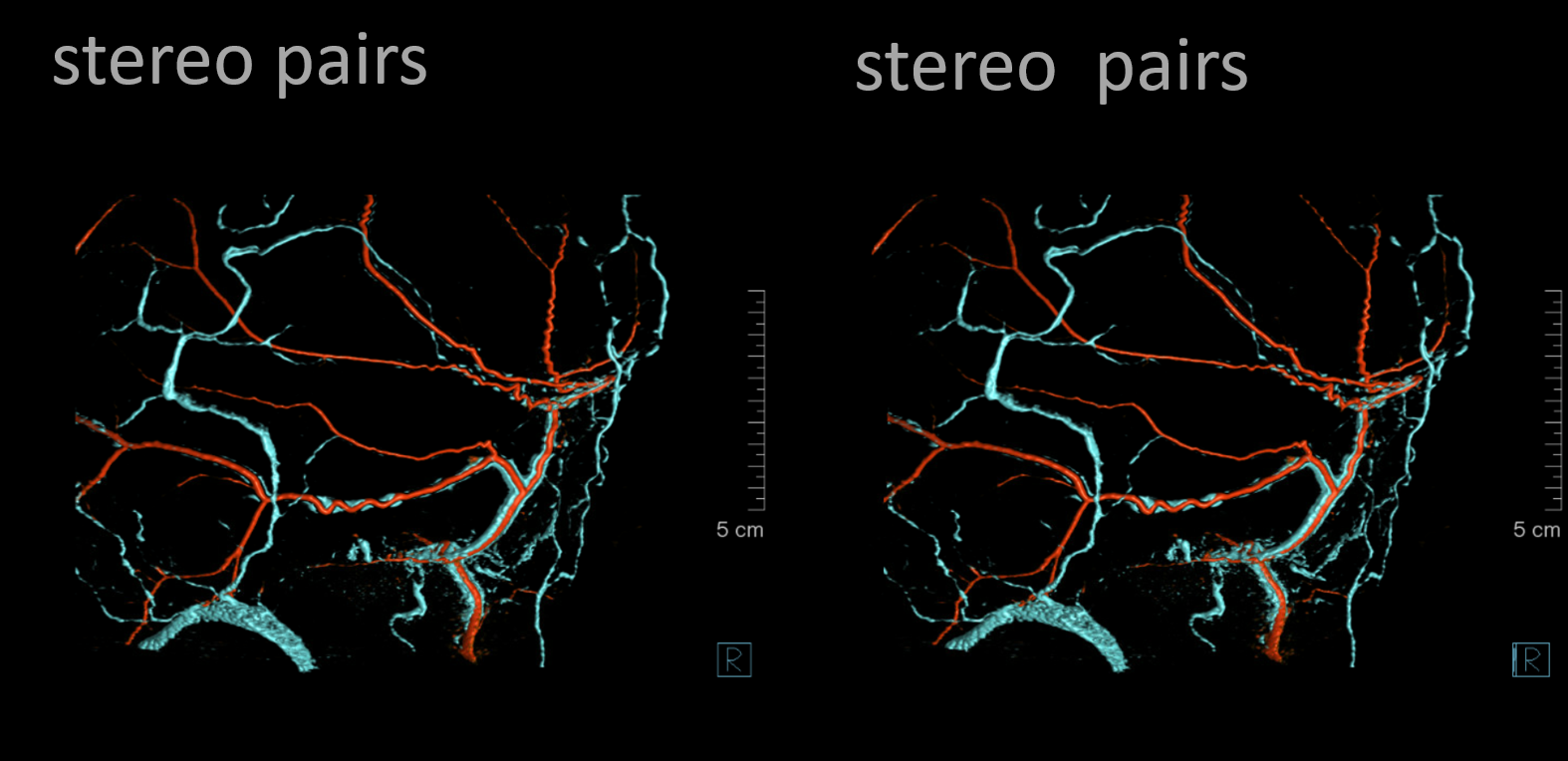
Triple phase image of same patient — same arrows. It is also tricky sometimes to differentiate diploic veins from dural veins — stereo helps because you can see depth in that. Also helps to have arteries in the same picture — a big vein not adjacent to major artery is likely to be diploic.
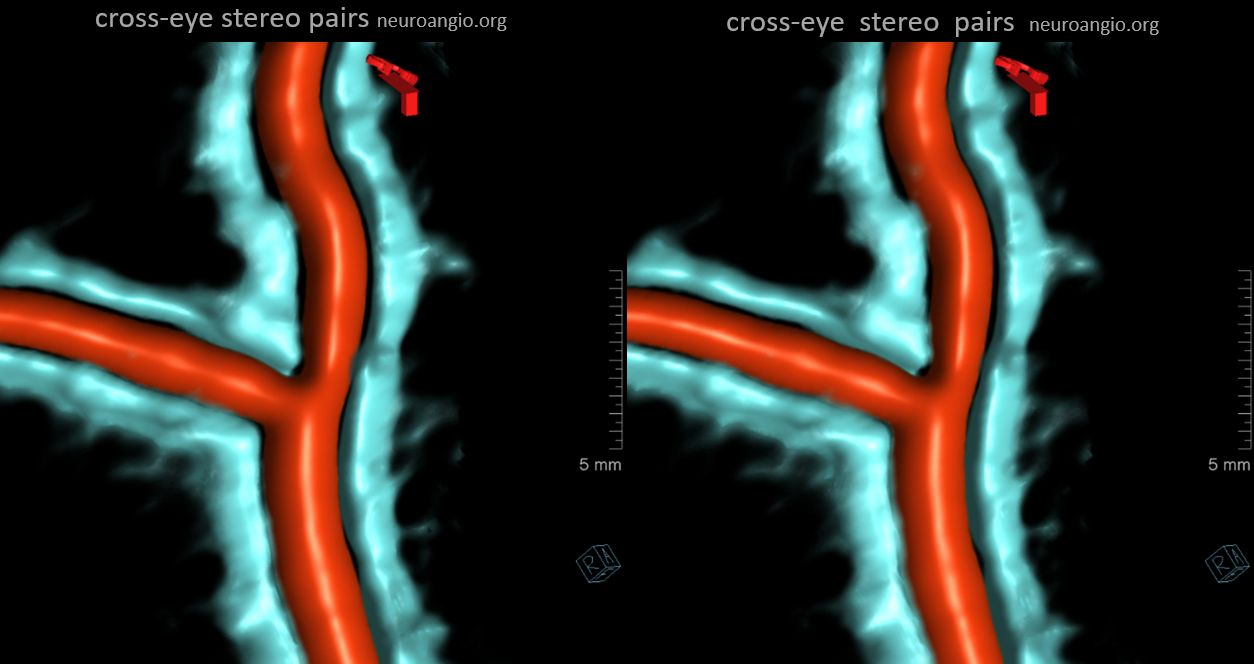
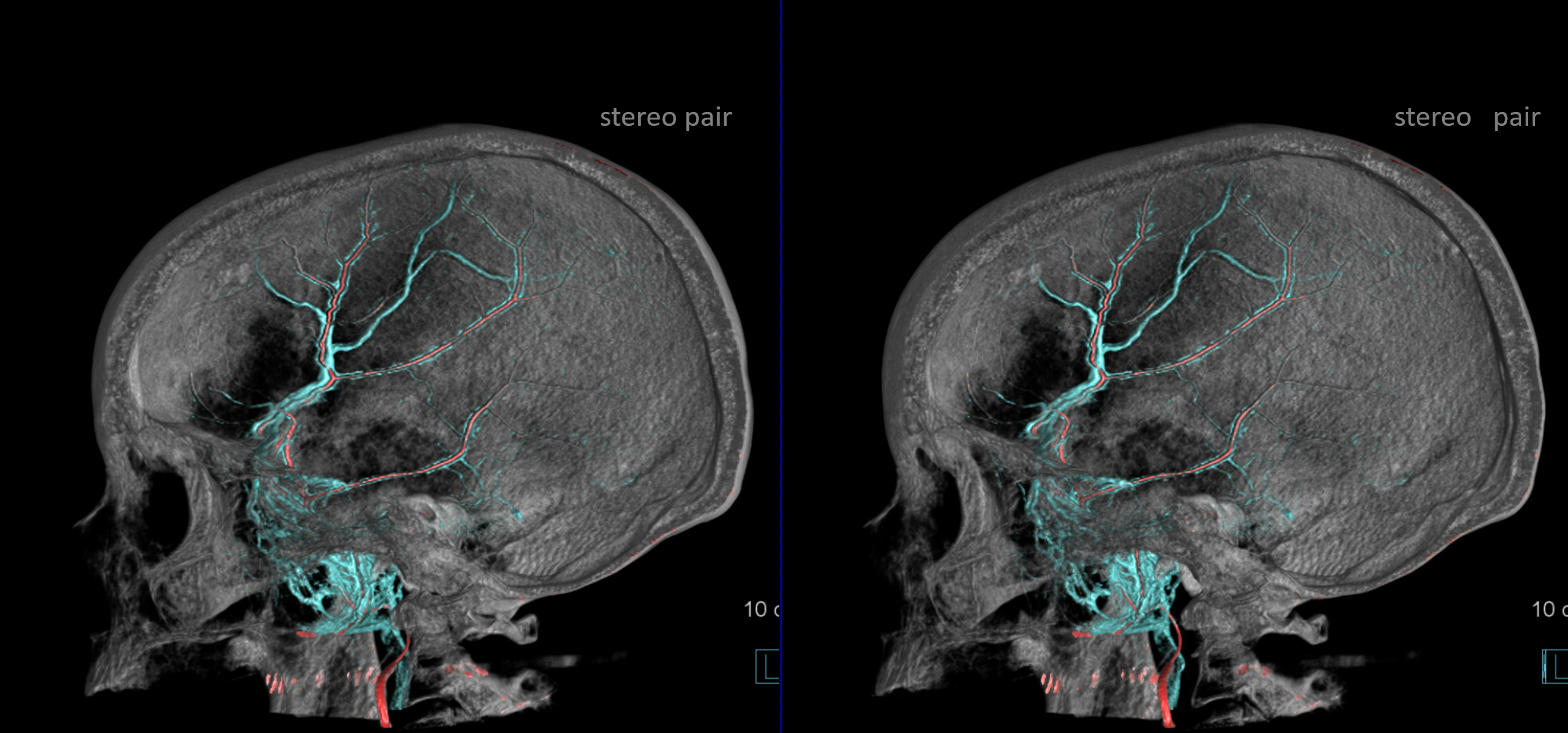
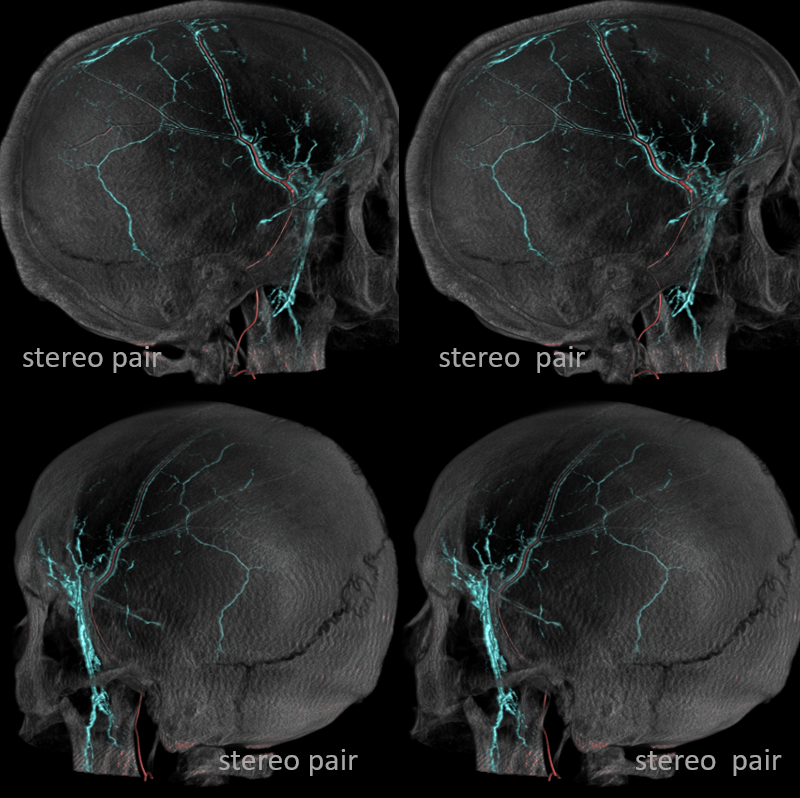
The cross-eye stereos!
So, like in any venous system, veins being like rivers, they collect into ever larger venous channels. At some point these veins have to leave the dura. There are three main ways for this to happen.
Three main dural venous outflow pathways
One is via those tram-tracking sinuses going down to skull base along major meningeal arteries, and existing via skull base foramina — usually not spinosum but ovale, into the pterygopalatine venous plexus. Often, instead of doing that, the tram-tracking sinus finds a hole in the skull — an emissary vein — and drains into the temporalis venous plexus instead.
Second way for blood to leave dura is into those venous plexi adjacent to venous sinuses, and then into sinuses themselves. Especially over sigmoid sinus.
Third way is via diploic veins of the skull. This is a problem because its hard to tell dural drainage into those veins vs. the skull itself. A lot of it is skull drainage and not dural for sure. But some is definitely dural. The biggest diploic channel of this kind is one that runs vertically, over parietal bone, down to squamous. Usually empties into sigmoid sinus. It is probably a remnant of Padget’s primitive parietosquamosal sinus (see above).
Below are examples — dural veins are solid arrows, diploic veins are dashed arrows, the main petrosquamosal diploic channel is a dashed ball arrow, the venous plexus adjacent to sinuses is arrowhead, temporalis venous plexus is open arrow, and pterygopalatine venous plexus is dashed open arrow.
Movies can be very nice — stop them and scroll thru individual images
Stereos can help a lot with depth perception — especially when differentiating diploic from dural from extracranial plexus veins. Notice in bottom set the temporalis veins superficial to the skull
Another way is to get rid of skull completely — it requires two separate rotational datasets — arterial and venous — and co-registration. It can show arteries better, at expense of not having skull. Co-registering 3 datasets would solve this problem, if desired.
One other way to differentiate between diploic and dural veins is the old radiology trick — points of crossing are likely to be in different planes. Here multiple diploic veins (dashed arrows) are crossing arteries.
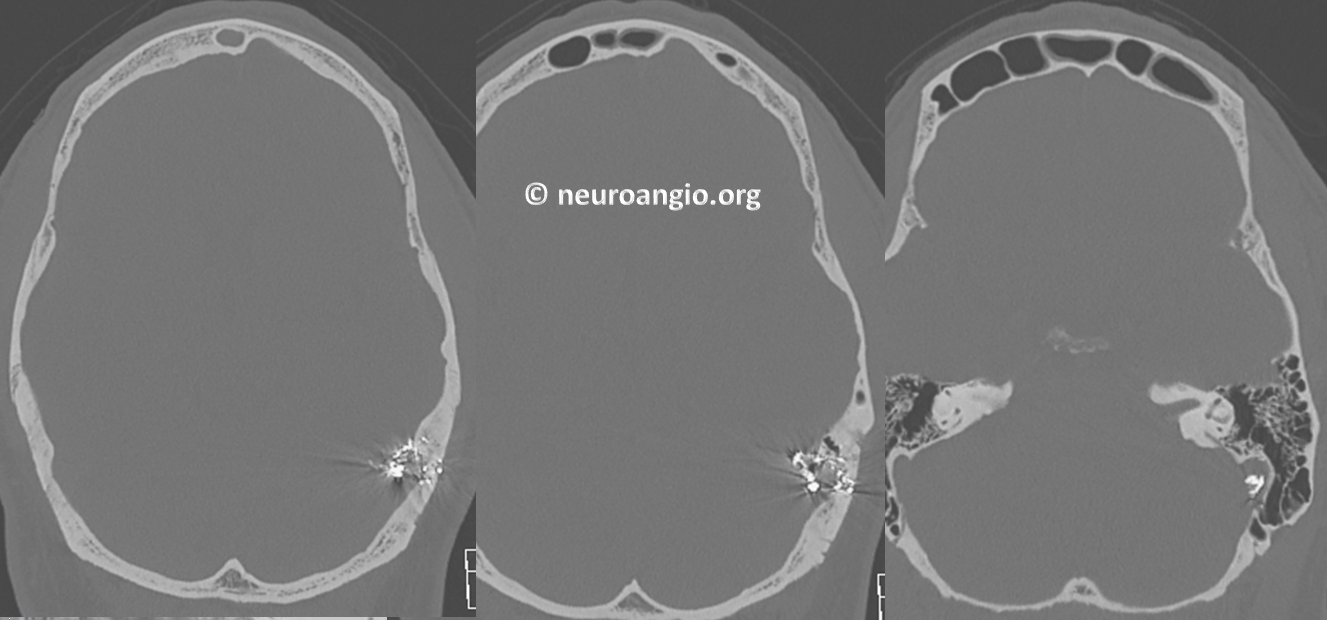
Behind all these colored images are the raw data — and raw data rules when you really need to know what’s going on — super easy to differentiate diploic from extracranial veins of course. The dural veins are hard to see actually because they are small and plastered against the inner table. Notice how nicely you can see veins in foramen ovale (bottom middle image) and the main middle meningeal sinus just above it (bottom right image)
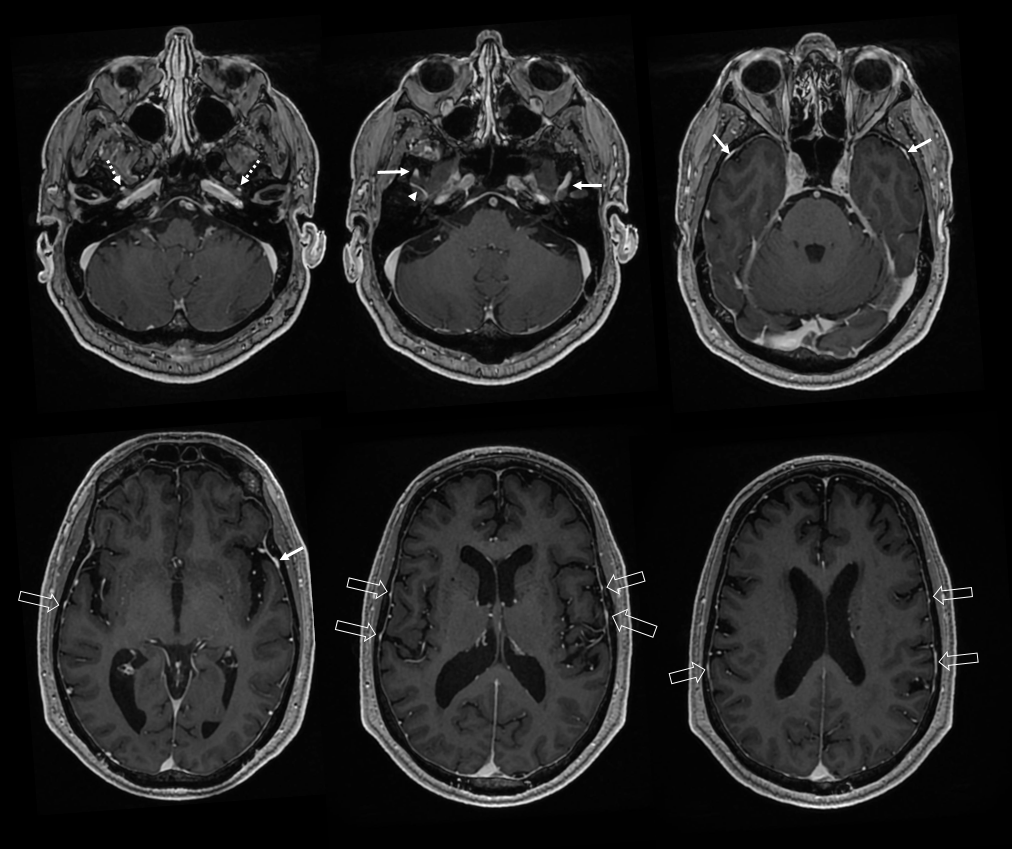
MRI visualization of dural venous drainage
Another way to see it — and really rarely paid attention to. Look at those veins
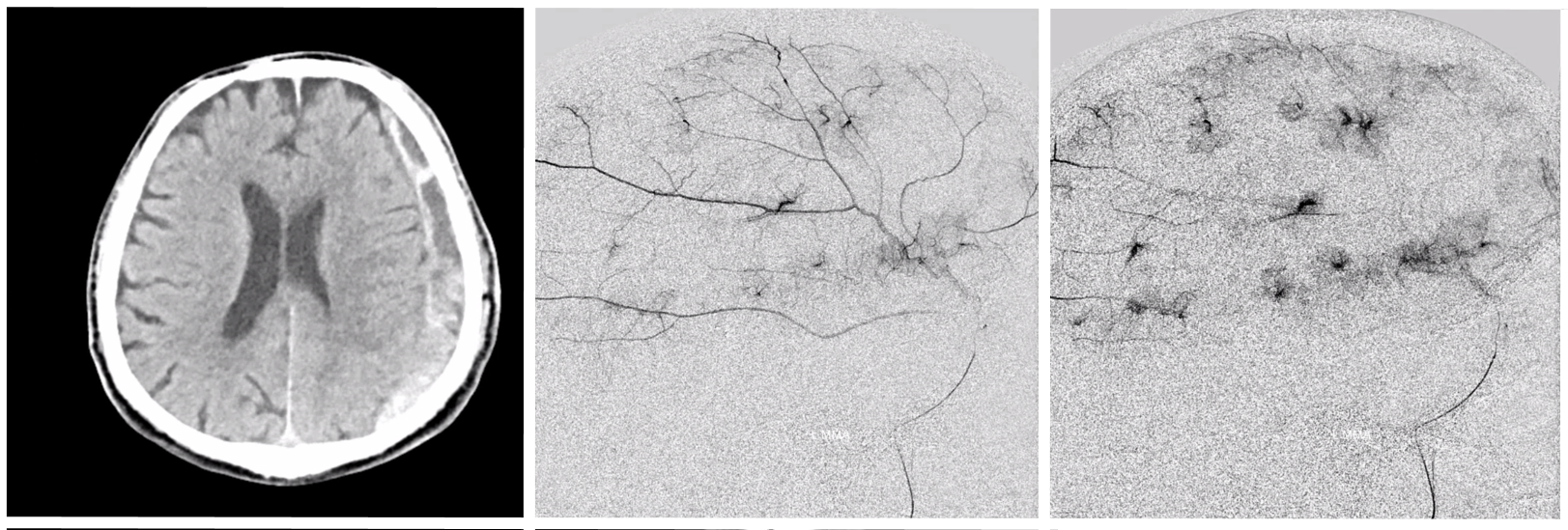
Differentiating skull from dura enhancement and venous drainage
This is not easy. What arteries feed the skull? Meningeal ones mostly — with some contribution from superficial vessels such as occipital and STA. So, how do we tell dura and skull apart? The diploic veins drain both skull and dura, but a lot of it is skull. Arterial supply to skull can be seen as a blush on tangential DSA views. It can be a lot sometimes, and many people confuse skull enhancement for dural membrane enhancement related to subdurals. The image below shows tons of enhancement, but this patient has no subdural — its all skull.
The tangential areas are outlined below
In contrast, the patient below has dural leakage from active SDH extravasation — a much more specific findings than the more common “cotton wool” that can be either skull or dura
Venous pouches / lakes / plexi adjacent to venous sinuses
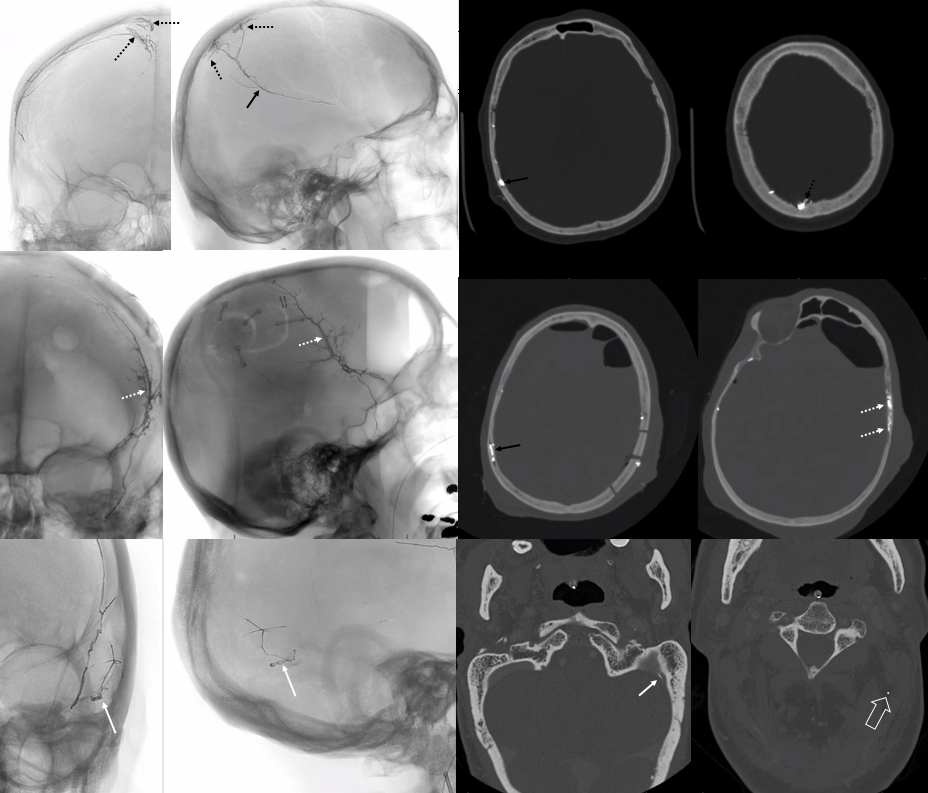
These are quite consistently seen in the sigmoid region — likely a very important fact in regard to dural fistula pathophysiology. The existence of arteries in walls of sinuses we have showcased a lot — see intrinsic dural arteries page and MMA pages for example. The venous pouches look like pockets of contrast adjacent to sinus walls. DSA examples

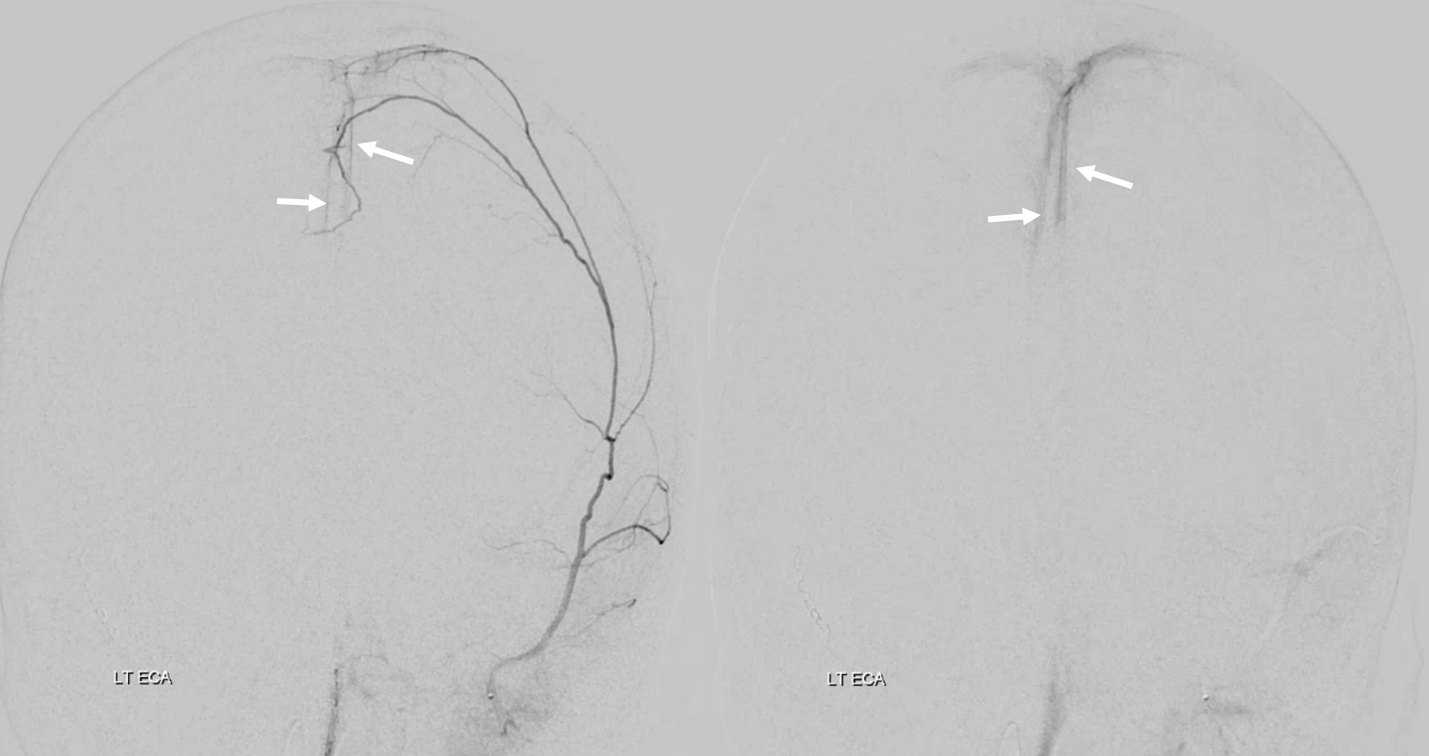
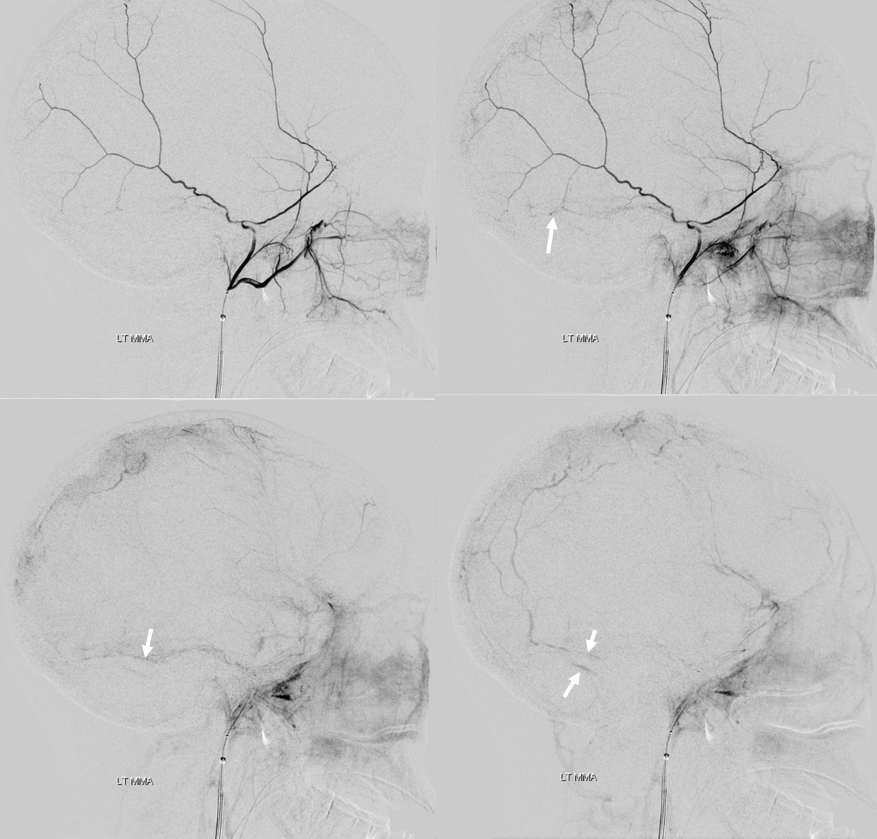
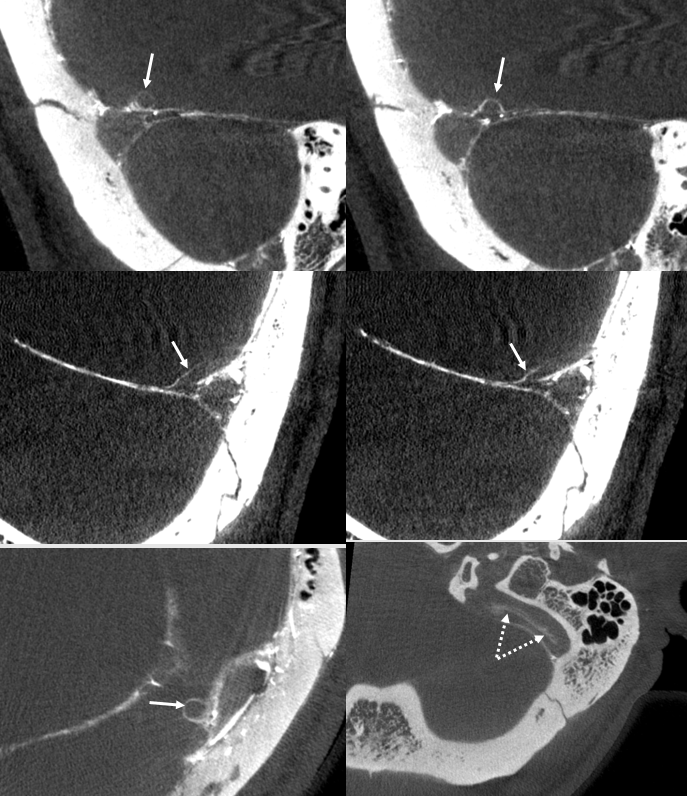
The pouches are much better seen on DYNA — check out three patients with same pouch on DSA and DYNA
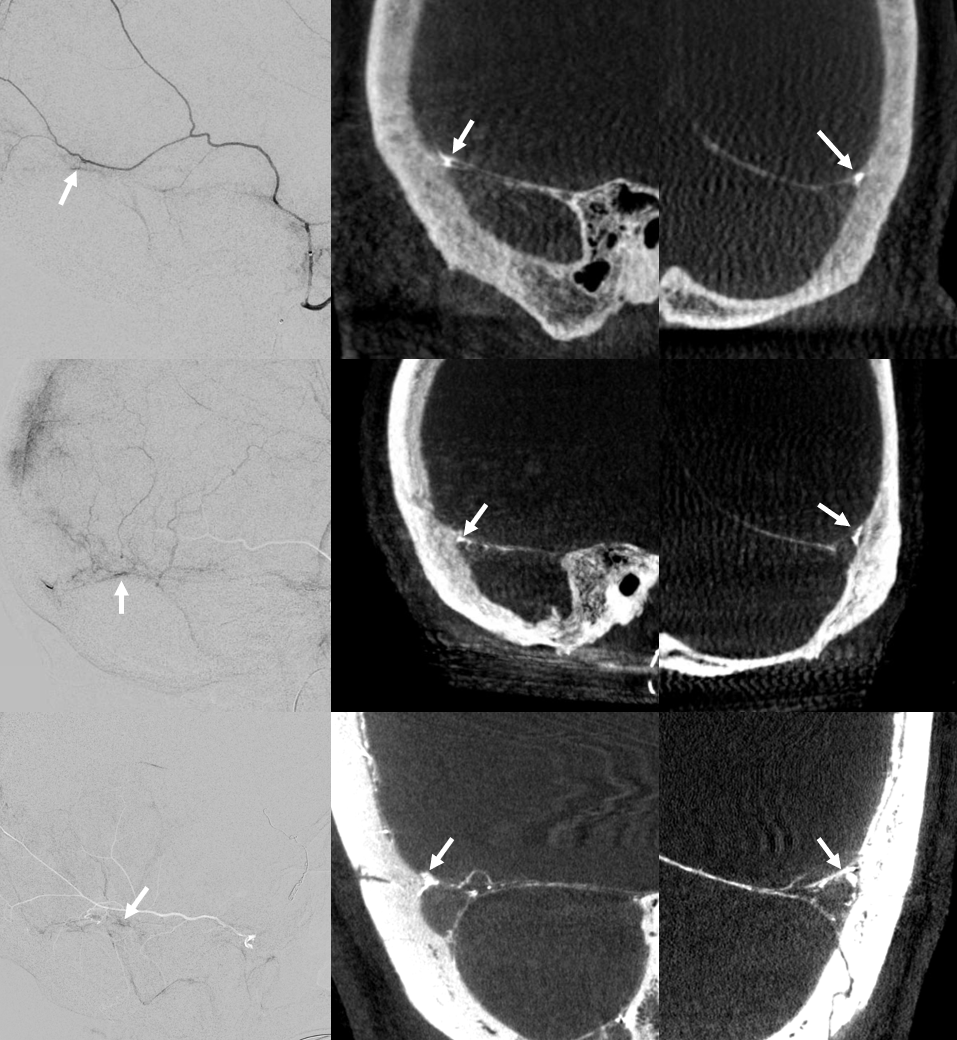
The same patient as lower set of images above — arrows in images below point to a dural venous channel — an MMA injection will not opacify the wall of a tentorial vein. There is slipstreaming of contrast from venous pouches into the sigmoid sinus (dashed arrow)
Below is a nice volume rendered demonstration of vasculature in wall of the superior sagittal sinus. Its a mixed injection — some are arteries, but most are veins i believe.
Movie
Angios to show arterial and venous phases
Again, these venous pouches are intimately related to their arterial venous sinus wall counterparts — see intrinsic dural arteries page and MMA pages for example, and the top drawing where they are illustrated.
Liquid embolic visualization of dural venous system
Not infrequently, Onyx or less often nBCA will extravasate during MMA embolization into the adjacent venous system. There should be no confusion about this — these are iatrogenic vessel ruptures. Of course, they are self-sealing and almost never of clinical significance. And, they help highlight the venous system — a bonus for us. Below are some examples.
This one is all-inclusive — every drainage pathway is represented — a thin tail of onyx extends via the condylar veins into the posterior cervical venous plexus (open arrow). No big deal.
Another one — serial images to show how it happens — from the sigmoid sinus wall artery (two lower right images) to the venous pouch in wall of the sinus (two lower left images)
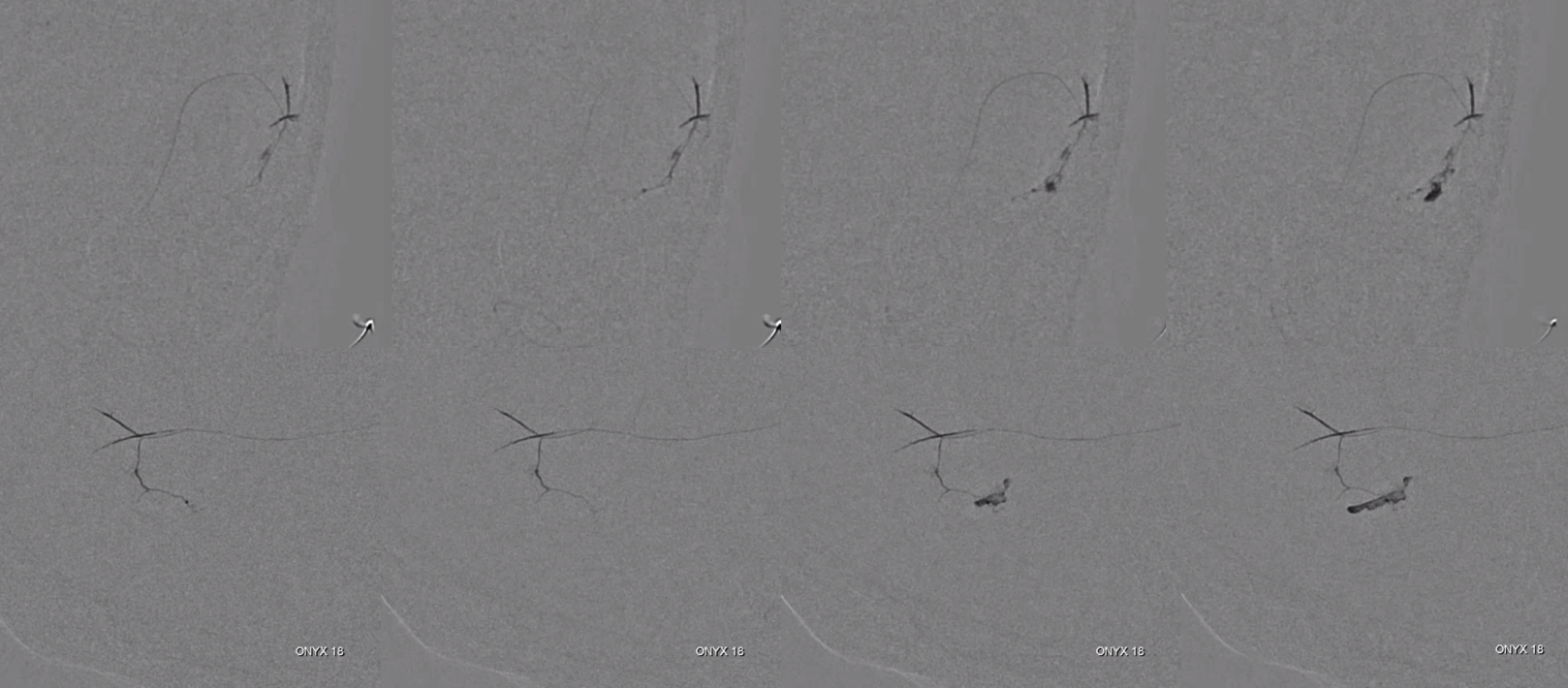
This is onyx in petrosquamosal sinus, with a tail in sigmoid
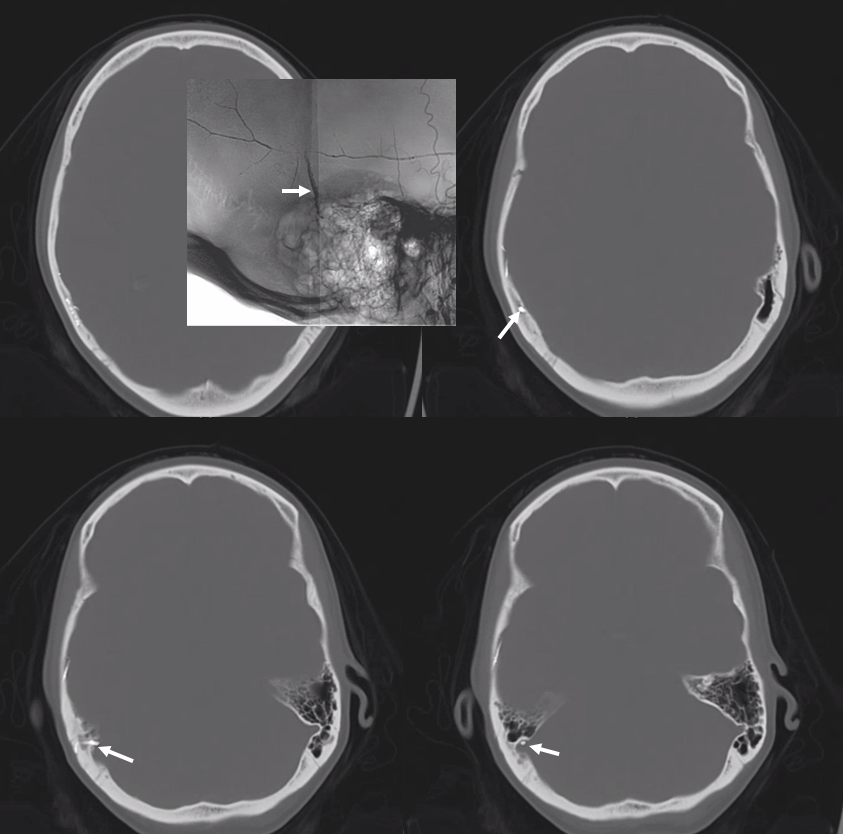
Dural Fistula Significance
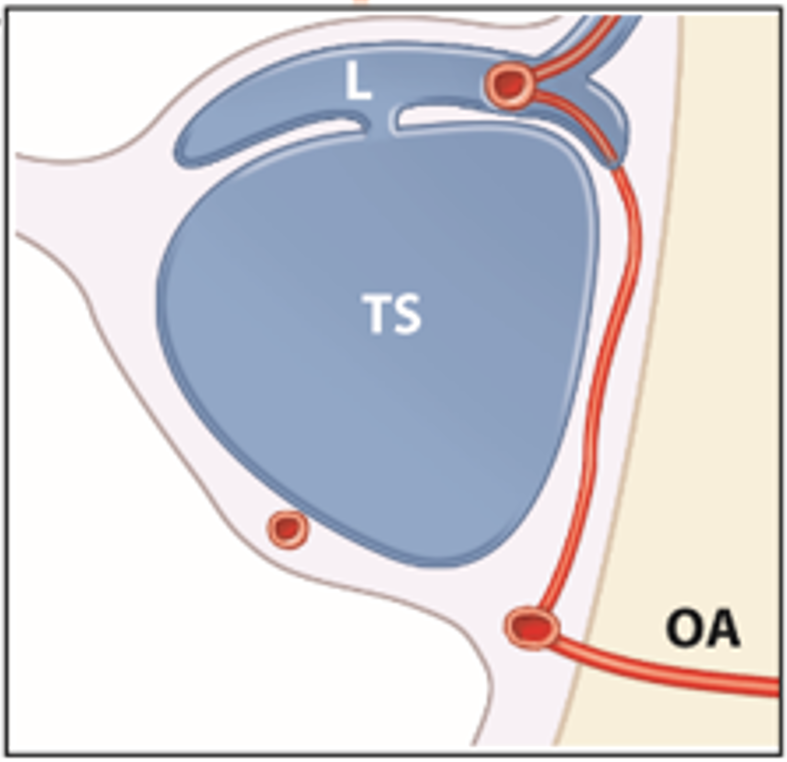
By this point, the connection between these sinus wall venous pouches and dural fistulas is hard to miss. The prevailing idea is that the site of fistula is in the wall of the sinus, with myriad arteries converging into one or several common venous pouches in sinus walls. This is how most simple dural fistulas look like. This is what also allows for superselective treatment by occluding the pouch only, and preserving the sinus proper. We have multiple examples of these superselective treatments (see “Case Library” section).
We have previously written in AJNR that these channels in walls of the sinuses may be common collector arteries rather than venous pouches. This is an example of acknowledging that this is not entirely true. Neither is this completely false. There are, we believe, common collector arteries in sinus walls — the sinus wall arteries we have so frequently emphasized. The fistula point is between these sinus wall arteries and sinus wall venous pouches, which then empty into the sinus proper. Thus closing these pouches works well. It is not always possible, especially with higher grade fistulas, where sinus has been distorted. But, in simple ones, it often is.
Below are some examples from our fistula collection of this kind of common pouch occlusion — the “magic bullet” approach
Balloon is in sigmoid sinus. microcatheter and wire are in the sigmoid sinus venous pouch that is the common collector of the fistula
Fistulogram
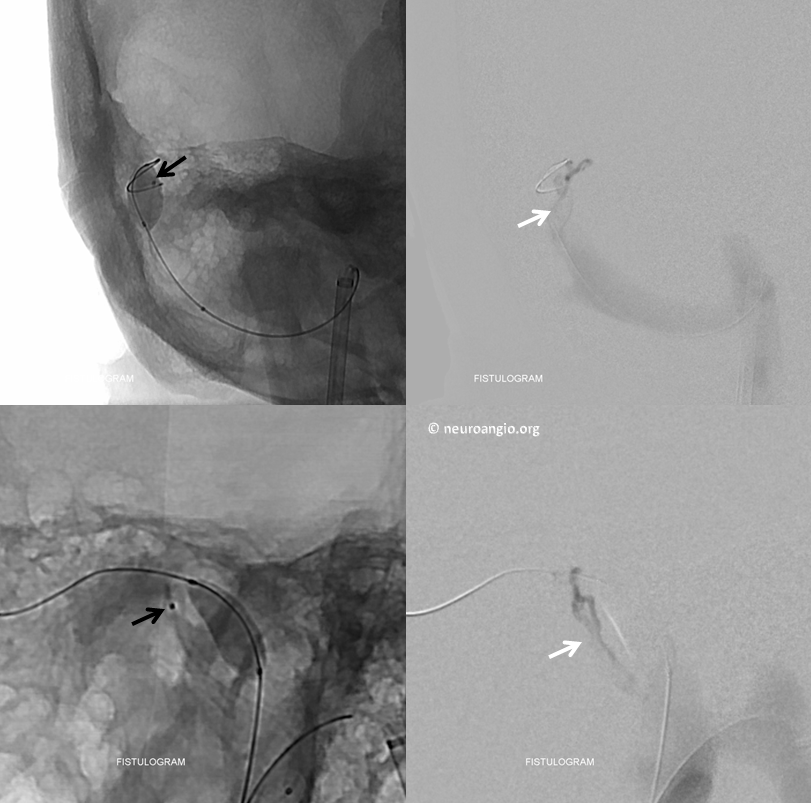
A small coil pack — yes coil works in superselective embo — and fistula is closed
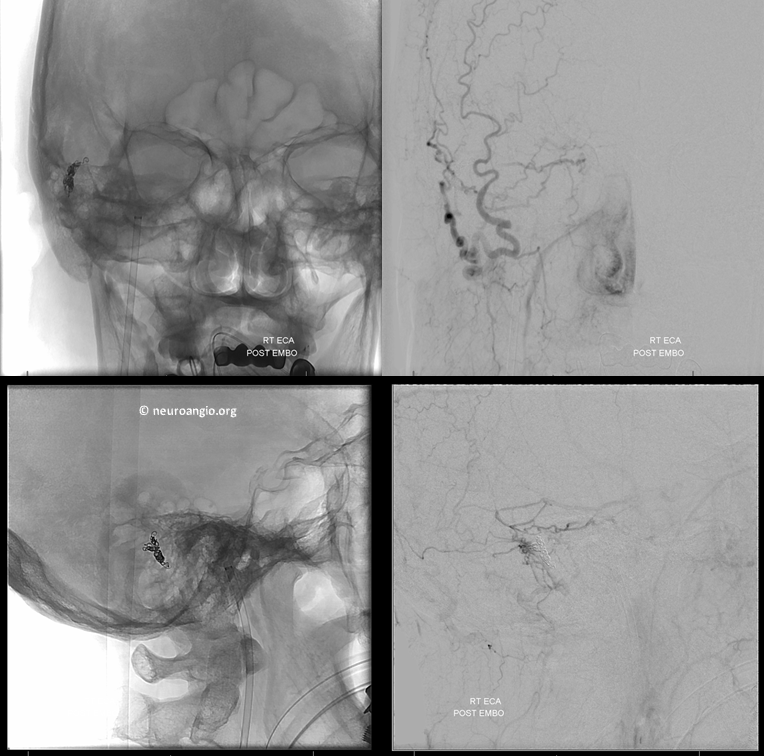
Venous pouch is shown by arrow
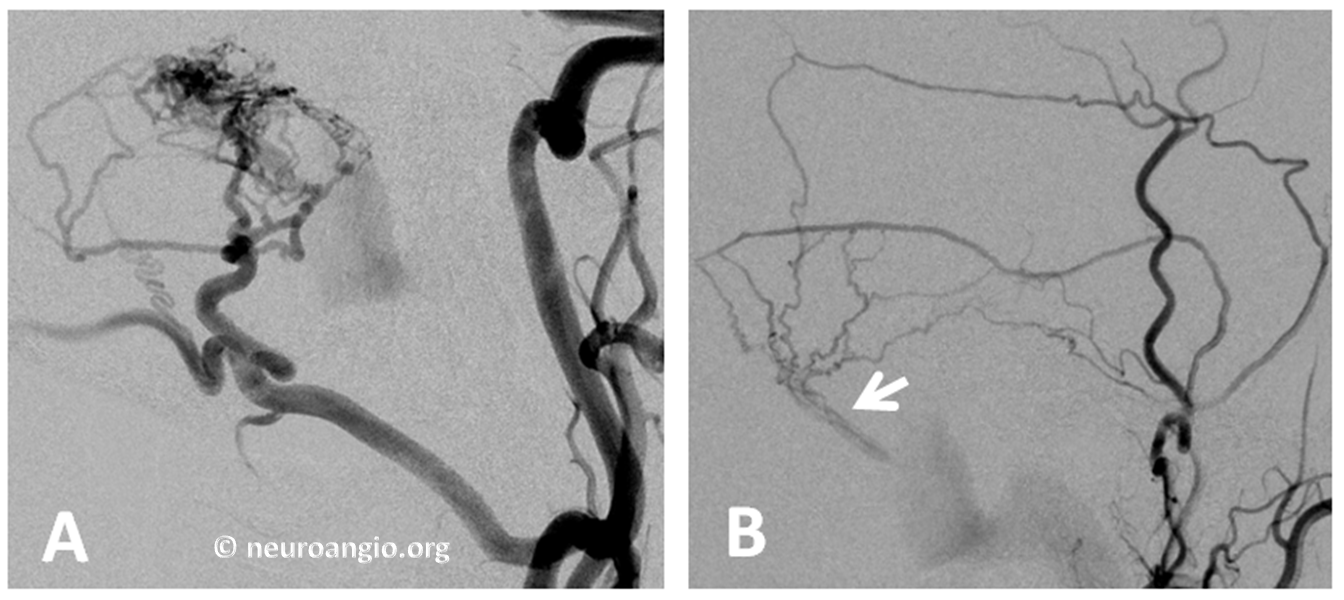
Beautiful retrograde fistulogram — the injection is through the 5F vert stuck in the venous channel, retrogradely showing all the arterial tributaries simultaneously. Awesome!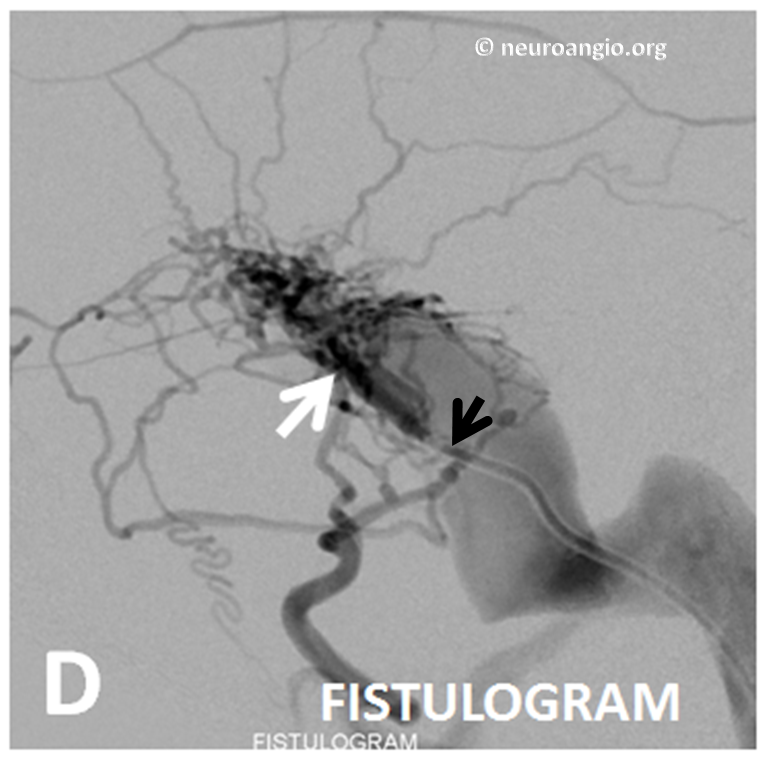
A little bit of Onyx is all it takes

Post
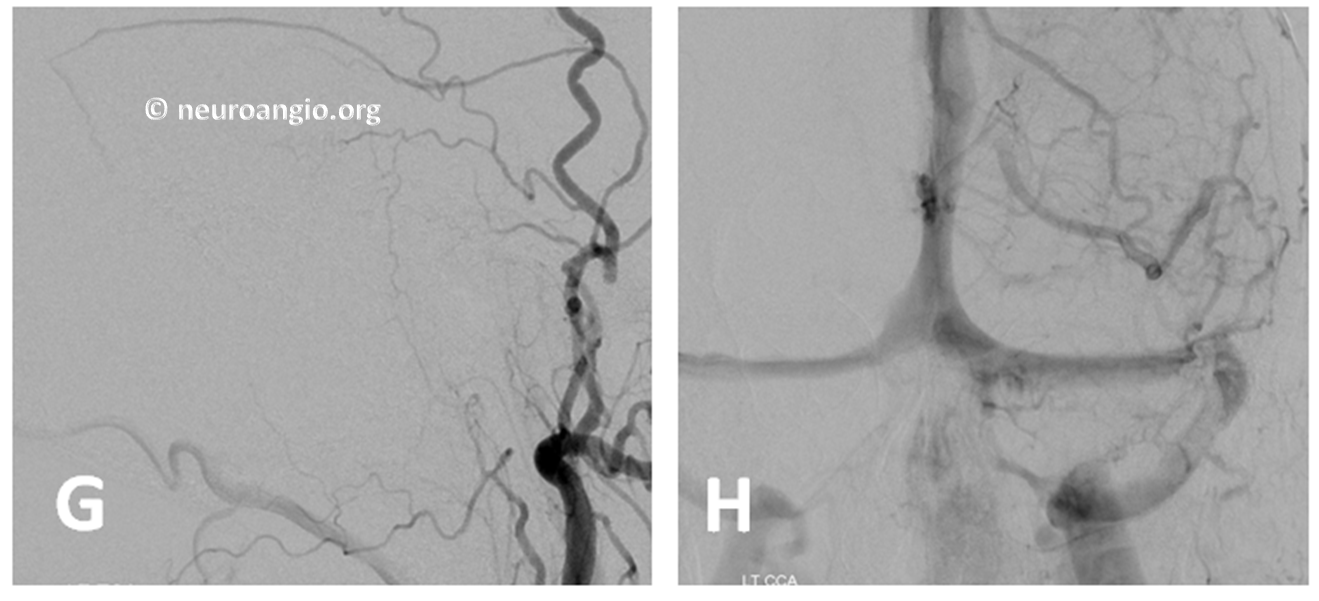
DYNA CT post shows onyx in sinus wall
Other cases are on “Case Library” page
Case Library
Subdural Hematoma Embolization — in development
So, questions / comments — write to neuroangio@neuroangio.org
Bibliography
