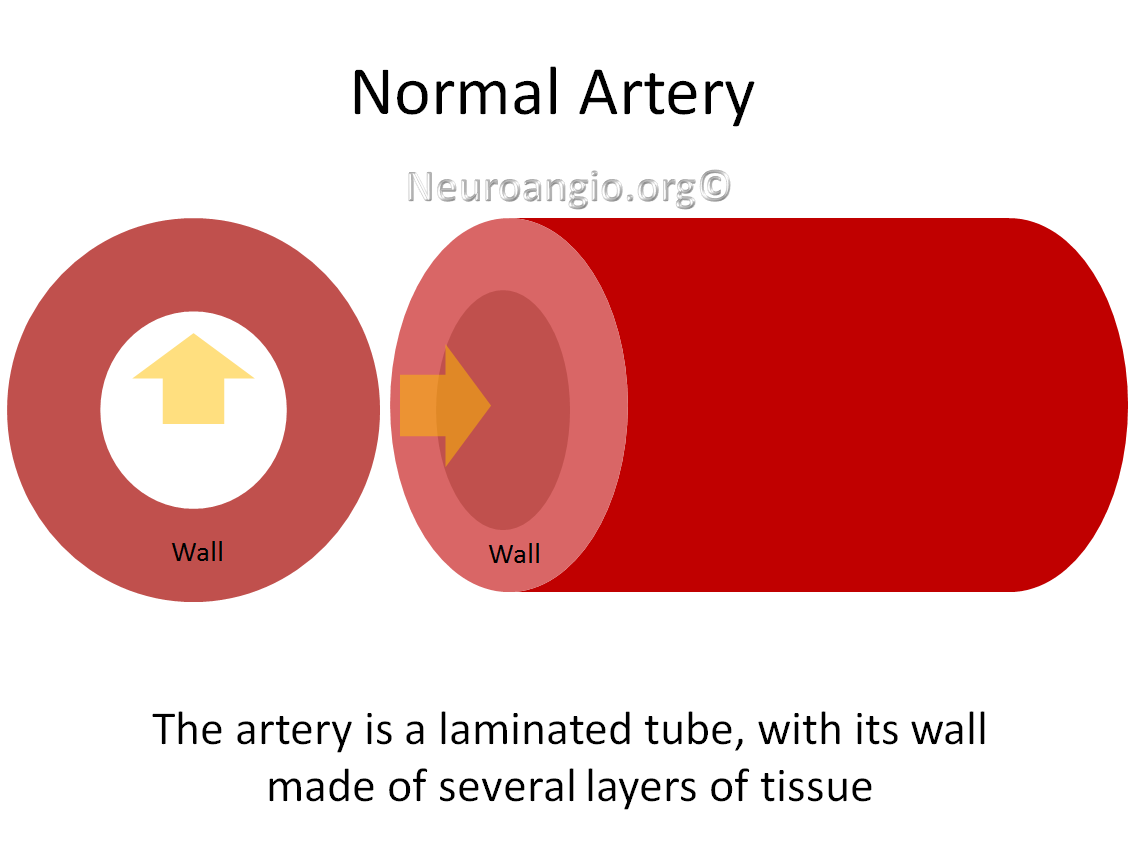
Arterial dissection is a tear of the inside of the artery. Arteries are like laminated tubes, their walls composed of many tissue layers, such as muscle, connective tissue, etc. The inside of the artery is covered with a thin layer of cells called “intima” — it is like a skin for the inside of the artery. The outside is covered with a tough layer called “adventicia”. The middle is made up of muscle, elastic, and other tissues. The yellow arrow represents flow of blood.
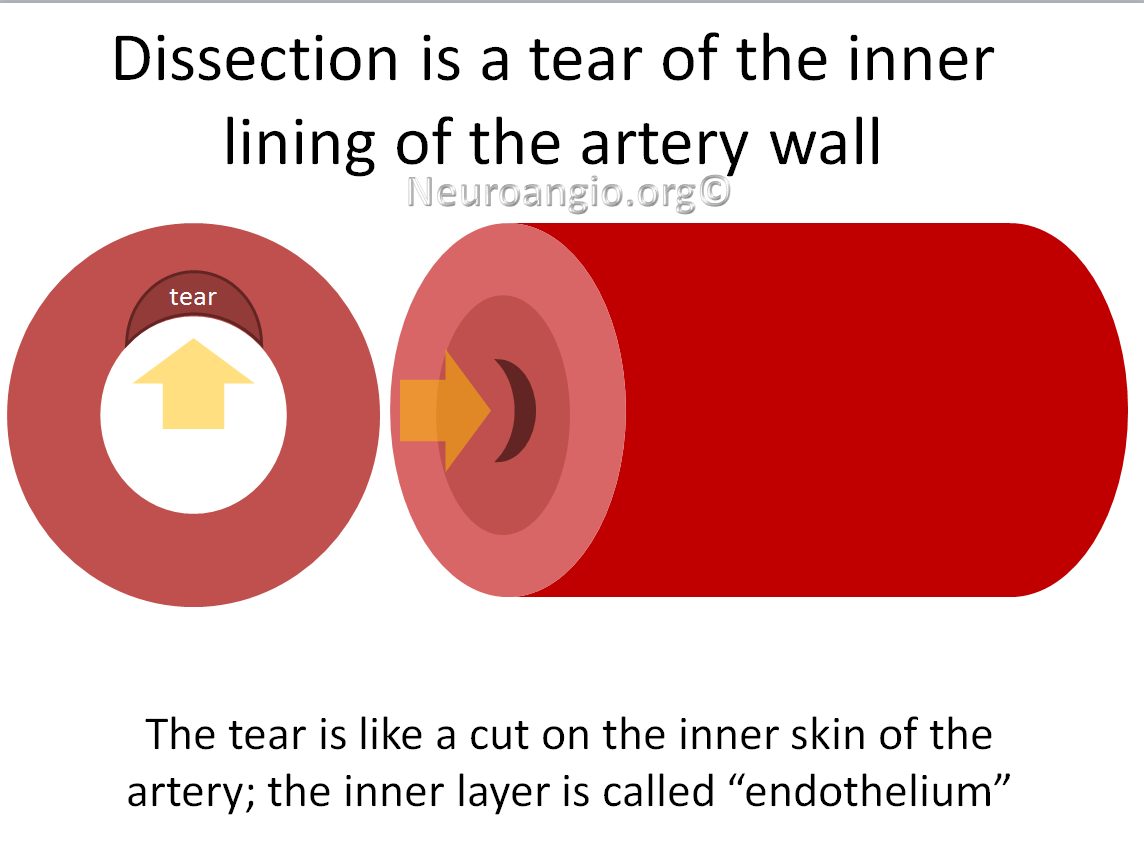
A dissection happens when, for some reason, the inside of the artery — the “intima” is torn. You can think of it as a skin cut, only on the inside.
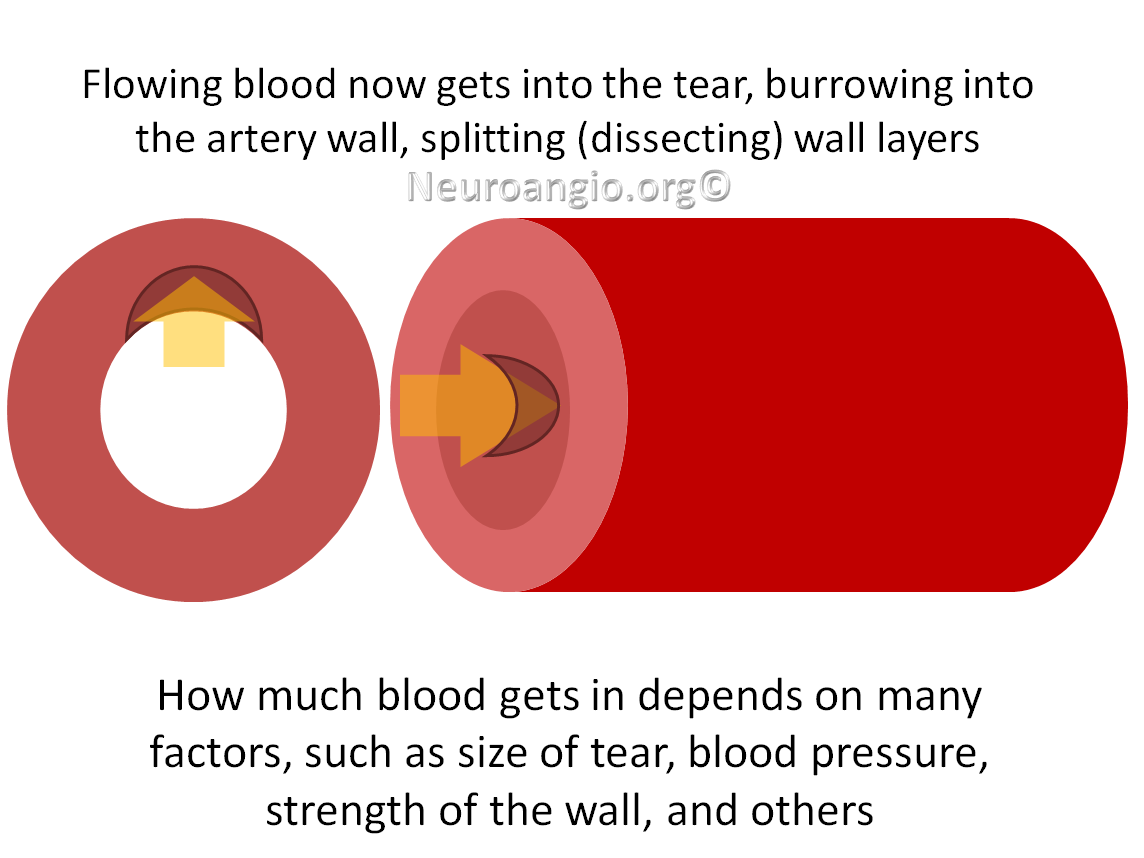
Because the artery is filled with fast-moving blood under arterial pressure, blood can find its way into the tear. It then starts to “dissect” or split the layers of the artery wall, accumulating inside the wall.
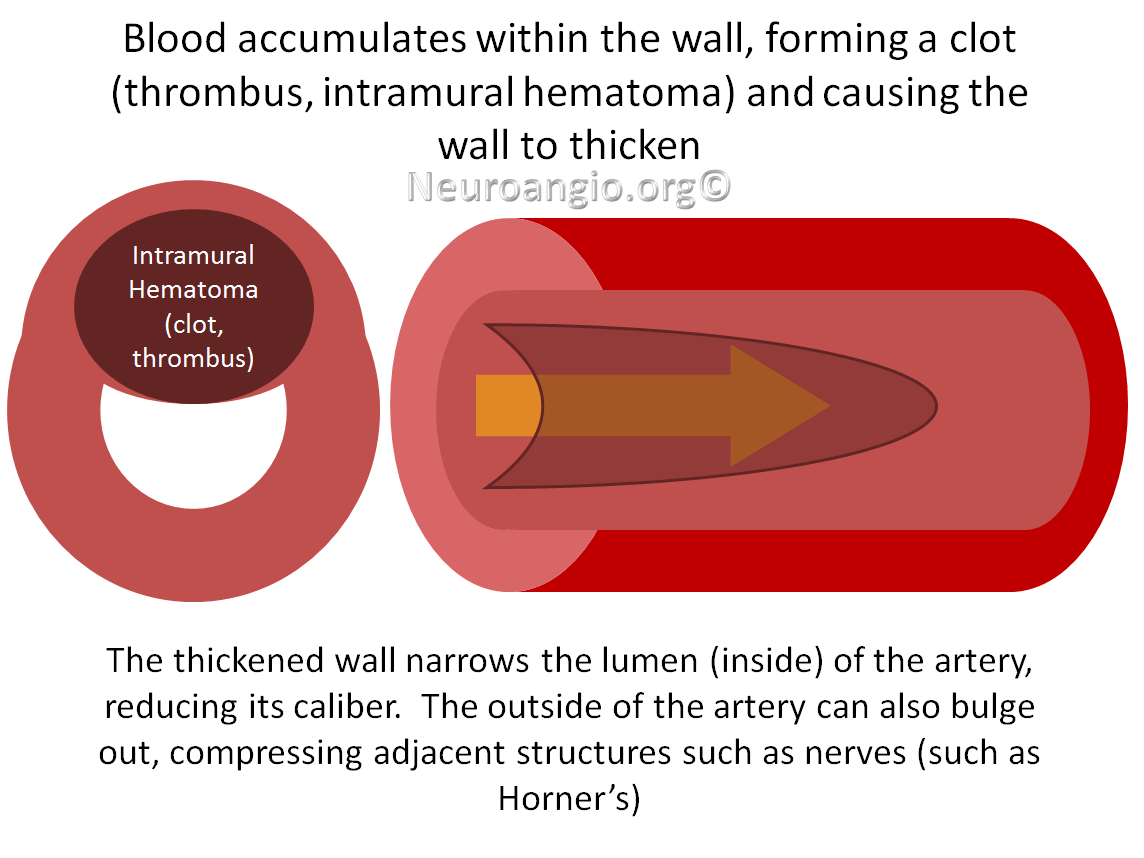
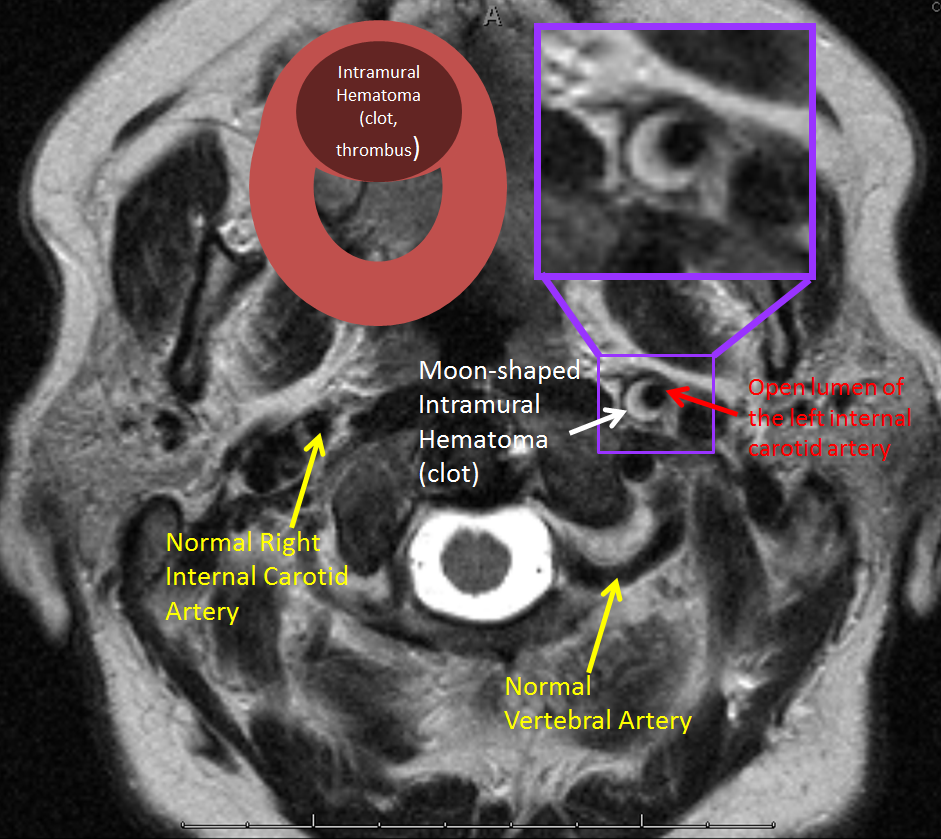
Blood inside the wall usually clots, or thromboses. As a result, the wall becomes filled with blood. This may expand the wall, which will in turn narrow the inner channel or “lumen” or the inside channel of the artery. This can limit how much blood flows through the injured segment.
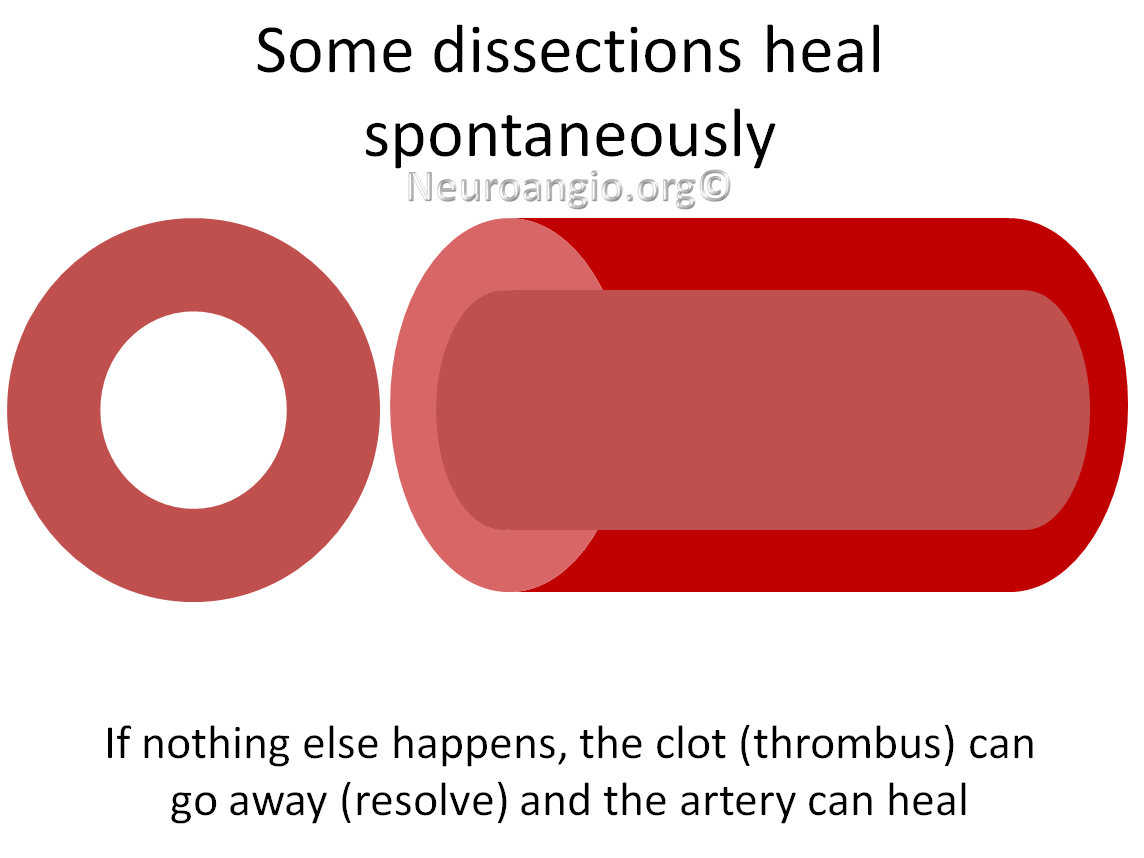
Some dissections will heal spontaneously. This is what happens most of the time.
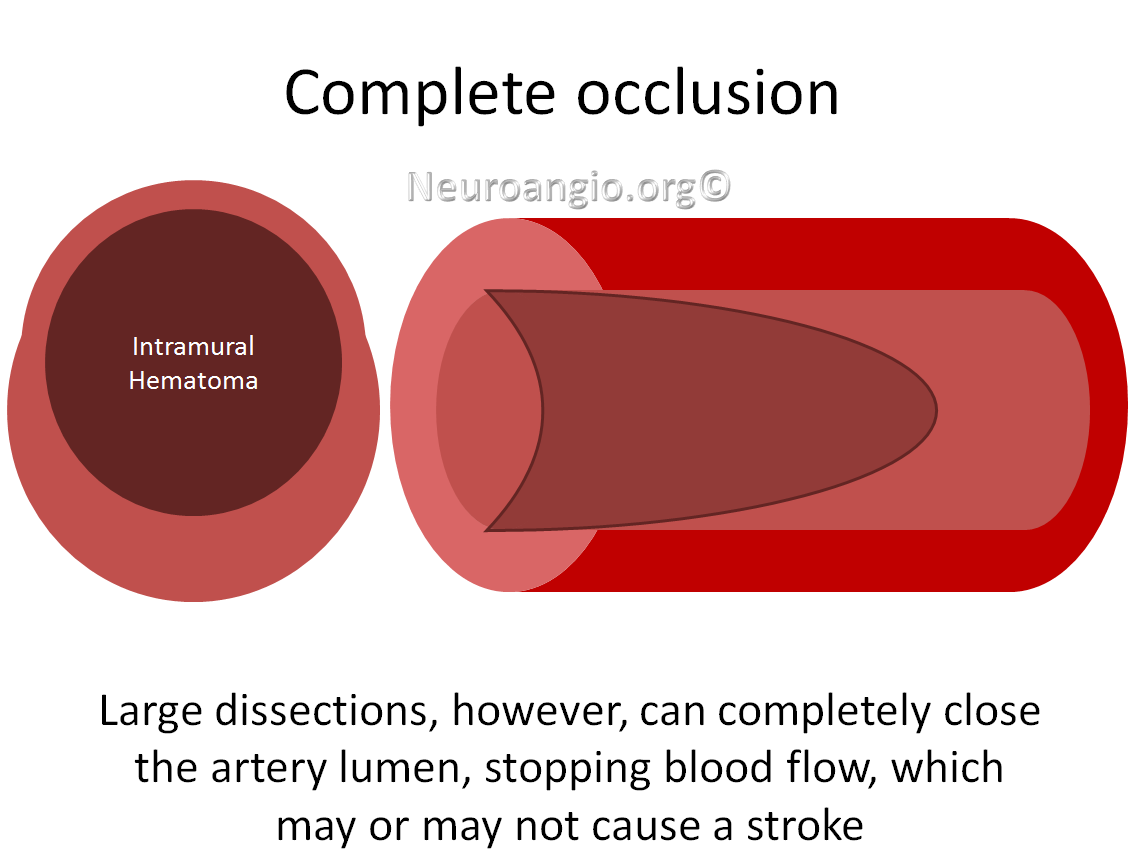
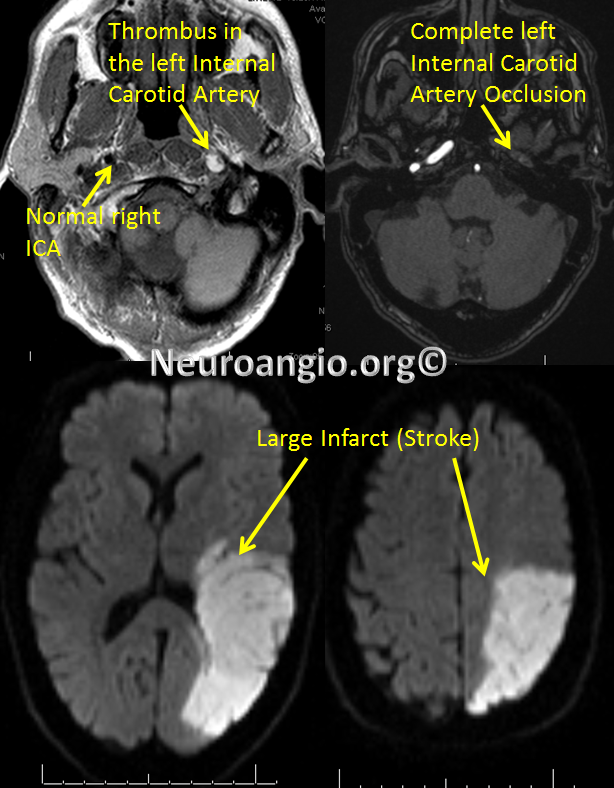
Large dissections, however, can completely close the artery, stopping downstream blood flow. Unless blood can get around the closed segment through other arteries and continue supplying the brain, a stroke will happen.
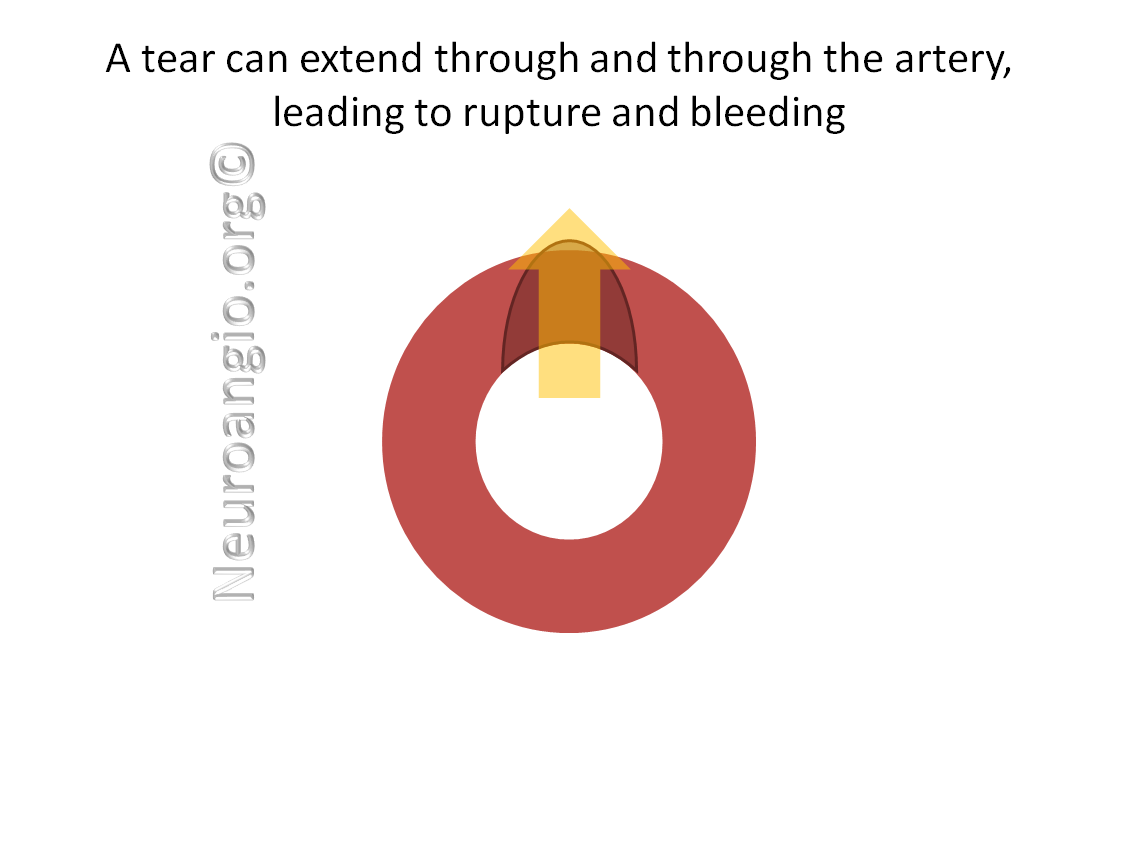
Some dissections can tear through the artery wall completely, leading to a through-and-through tear, or rupture. This is called a dissecting hemorrhage, or ruptured dissection. If the dissection is inside the skull, bleeding will take place around and into the brain (subarachnoid hemorrhage) or sometimes into a venous sinus (lake) surrounding the artery, leading to what’s called an arteriovenous fistula. Carotid-cavernous fistula is one example)
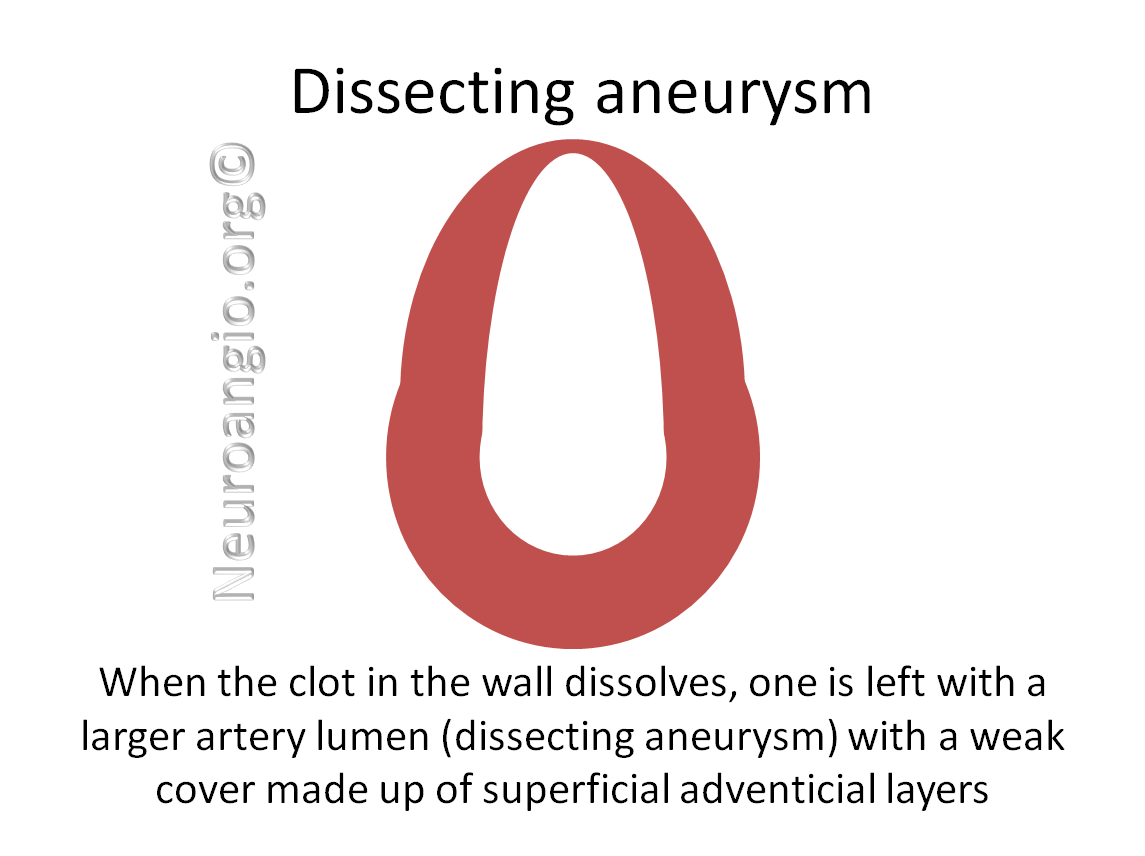
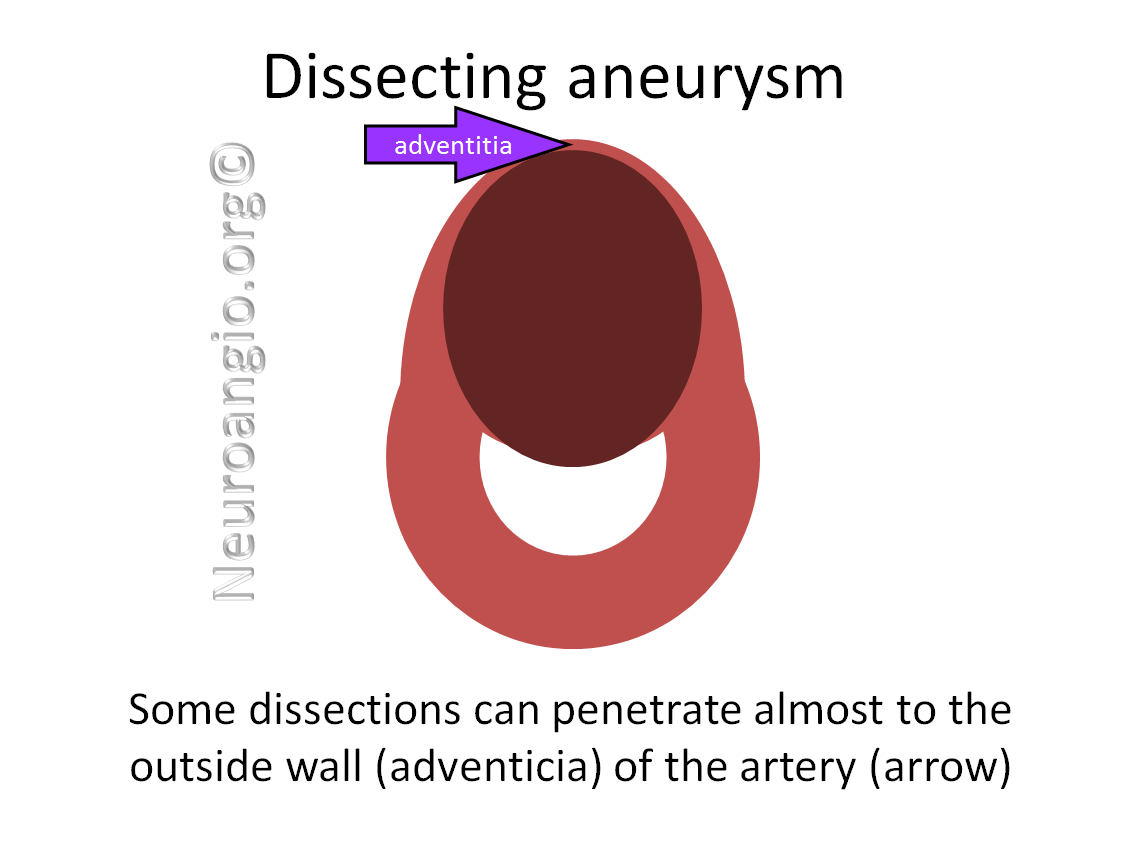
At other times, dissections nearly completely penetrate the wall, and only the tougher outer part of the artery, the adventicia, holds the blood inside and prevents rupture.
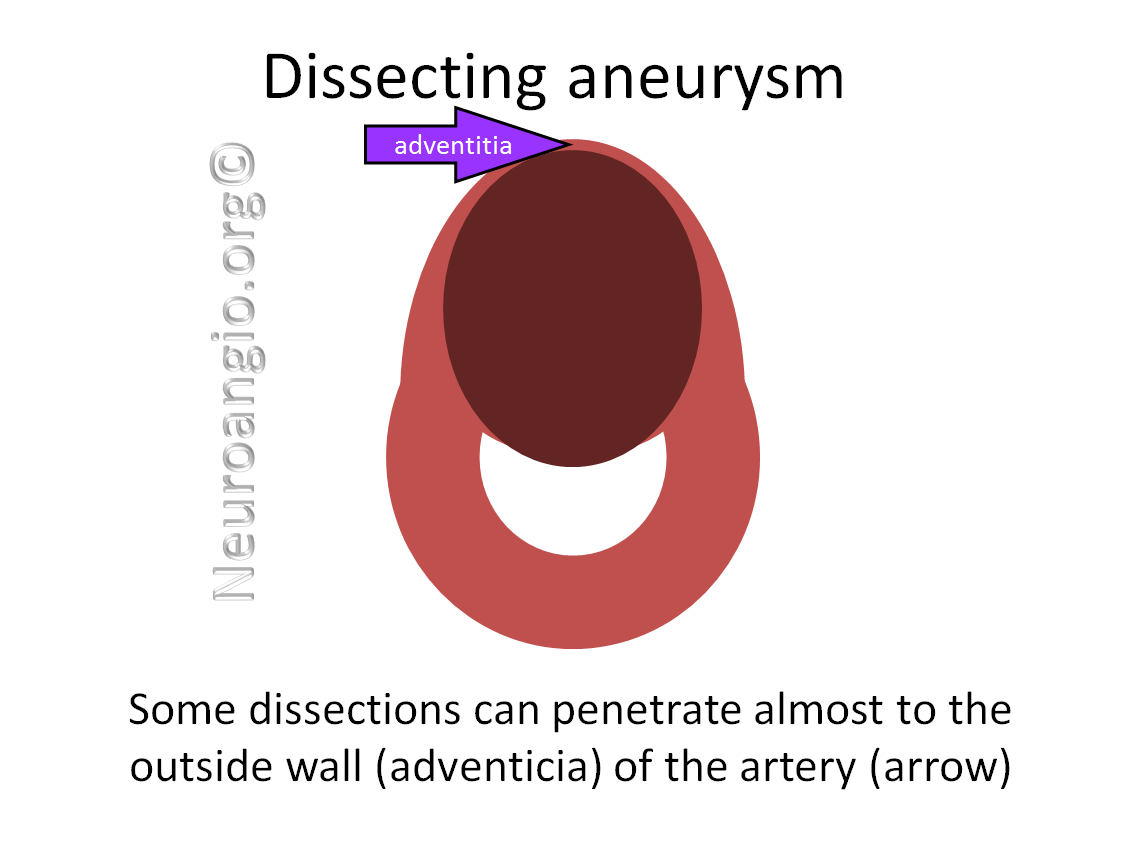
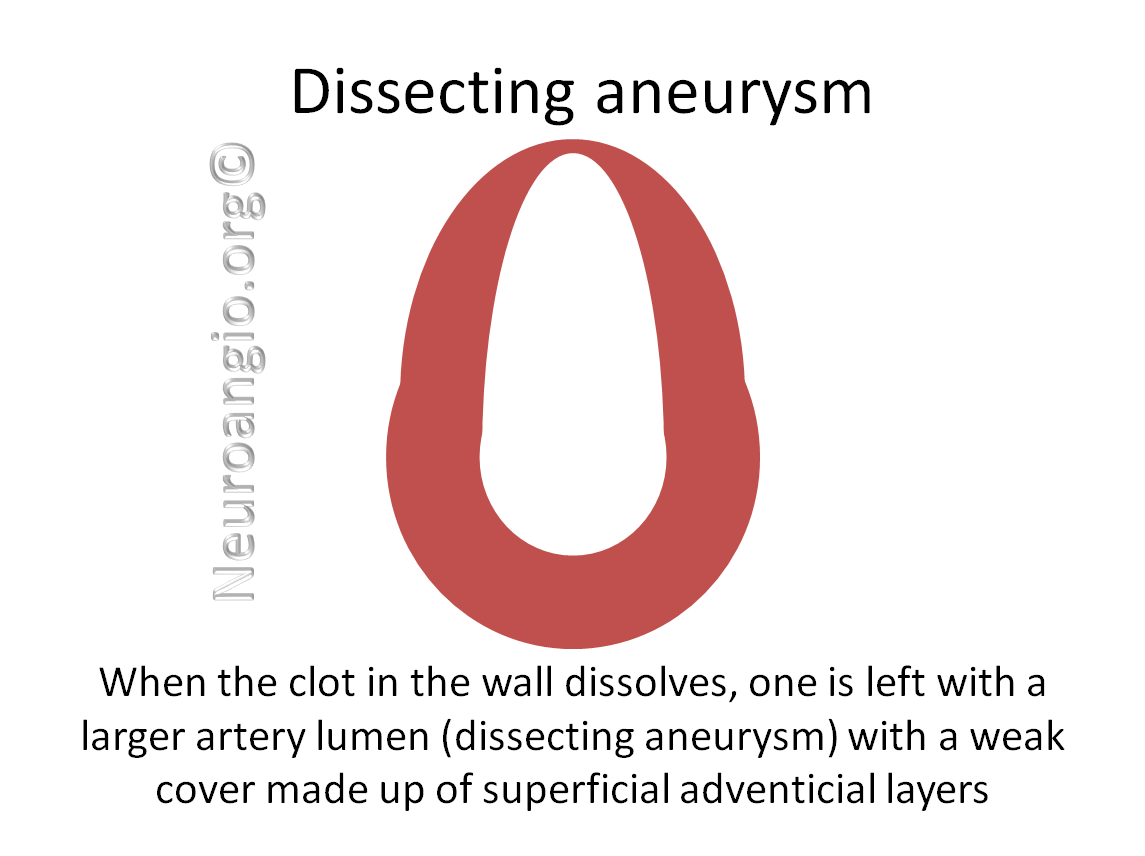
Usually, this situation leads to development of a “Dissecting aneurysm”, which is a kind of “fusiform” or global aneurysmal enlargement of the artery that takes place as the clot dissolves.
Some of these aneurysms go on to rupture later, just like a ruptured dissection does when it first happens.
Other aneurysms do not rupture but grow under arterial pressure, becoming ever larger. Some of these will rupture, while others will get large enough to compress nearby organs, causing symptoms.
At other times the large lumen of the aneurysm becomes partially filled with clot, just like clot (thrombus) can form in the left atrium of patients with enlarged atria and atrial fibrillation. This clot can then break off and travel downstream (embolize), causing a stroke
Here are some of the usual questions about dissections:
Why do dissections happen?
Dissections have many causes. In some people, the arteries are weak because of inflammation, a condition called “vasculitis”. Many different vasculidities exist. In others, the artery is weak because of some kind of genetic defect which makes part of the artery wall weak. There are many of these also — perhaps the most famous one is called Ehlers-Danlos. Usually, these genetic defects also affect organs and tissues other than blood vessels. A condition called Fibromuscular Dysplasia (FMD), which usually affects the media of the vessel wall, can also lead to dissection, though this is uncommon.
Sometimes, dissections happen because of injury — the artery can be torn by twisting or compression, for example during chiropractic manipulations, neck cracking or twisting, choking, various accidents, etc. Millions of people undergo chiropractic manipulations of the neck, yet dissections are rare. Whether or not its the type of manipulation, the patient’s arterial structure, or both contribute to the problem is often unclear.
Dissections can also happen in setting of atherosclerotic disease, smoking, hypertension, and other causes of possible arterial injury.
Finally, in many instances the cause for the dissection remains unclear. These are the so-called “spontaneous” or “idiopathic” dissections. Whether they are some kind of random event, or caused by conditions we do not yet understand, is unclear. While dissections often occur in particular places, such as at points where the artery is subjected to greater movement stress (just below the skull, for example), spontaneous dissections can occur in less typical places.
How do dissections present? What do patients with dissection feel?
The most common symptom is pain — neck pain in case of cervical carotid or vertebral dissections. Unfortunately, there are so many other causes of neck pain that pain itself is not a specific symptom. Other, more telling symptoms or signs, include subtle differences in vision (one pupil smaller than another, or eyelid drooping), but these can also happen for other reasons. Yet another cause is “Pulsatile Tinnitus” — when a person hears their own blood flow — a whooshing sound in the ear, usually on the side of the dissection. There are also many other causes of pulsatile tinnitus. Finally, some patients with dissection develop a stroke (see below). Ultimately, some kind of imaging (CT, MR, or angiogram) is needed to diagnose a dissection.
How dissections cause trouble?
This can happen in several ways. As seen from images above, dissections can cause the inside (lumen) of the artery to narrow or close completely. This will reduce blood flow into the part of the brain supplied by the artery. Unless other arteries can make up for the decreased flow by resupplying the brain through a different (collateral) route, a stroke will result.
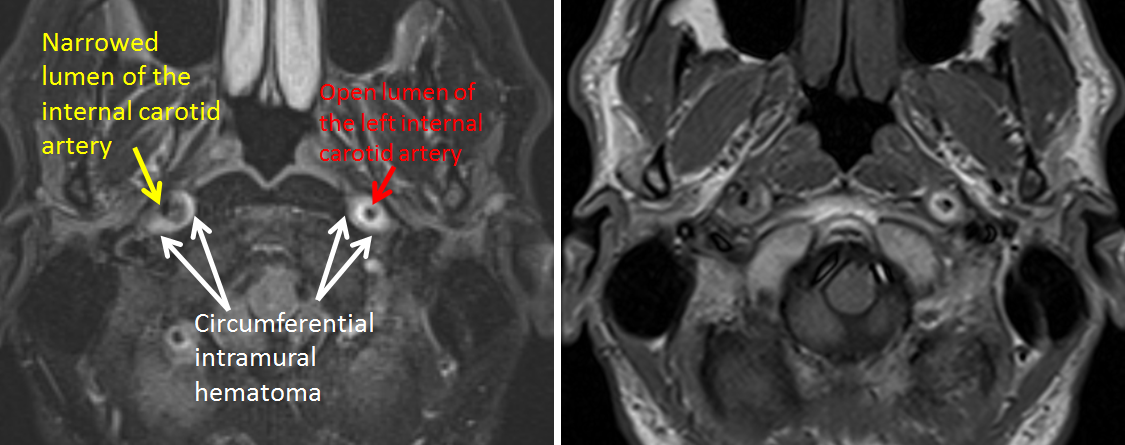
Here is a CTA of a patient with both left and right internal carotid artery dissections, showing how the dissection can narrow the lumen. The white contrast in the artery helps outline the lumen and show the problem. Patients with connective tissue disorders often have multiple dissections. Sometimes, however, even multiple dissections are not found to have a cause we know of.
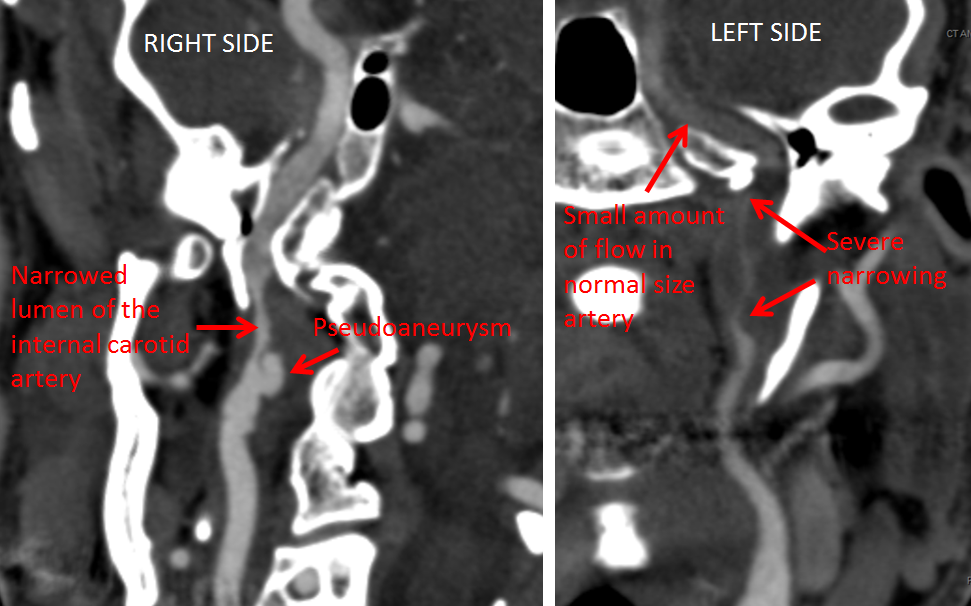
MRI of the same patient, showing the dissections in cross-section. The lumen is now black (black blood imaging) and the white hematoma in the vessel wall is better seen than on the CTA, where it is pretty much invisible.
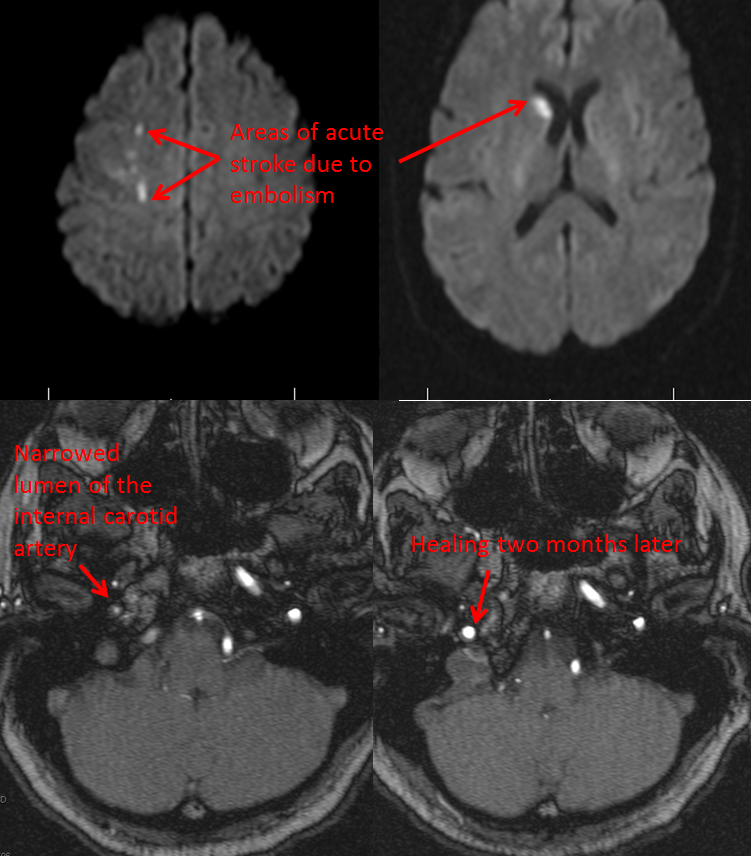
Many dissections heal spontaneously (by themselves). Because dissections are tears in the artery wall, clots which form in the wall also extend to the inside of the vessel, and either totally close it or dislodge and travel up into the brain. These are called “emboli” and are a cause of dissection-related embolic stroke. To miminize the chance of this happening, the patients are often advised to take antiplatelet medications such as aspirin or anticoagulation medications such as coumadin, to reduce the risk of embolism. Over time, most dissections heal and the artery returns to near-normal shape, often slightly irregular, as a kind of inside scar. Here is the same patient, a few weeks later. The dissections have healed, with a slight vessel irregularity.
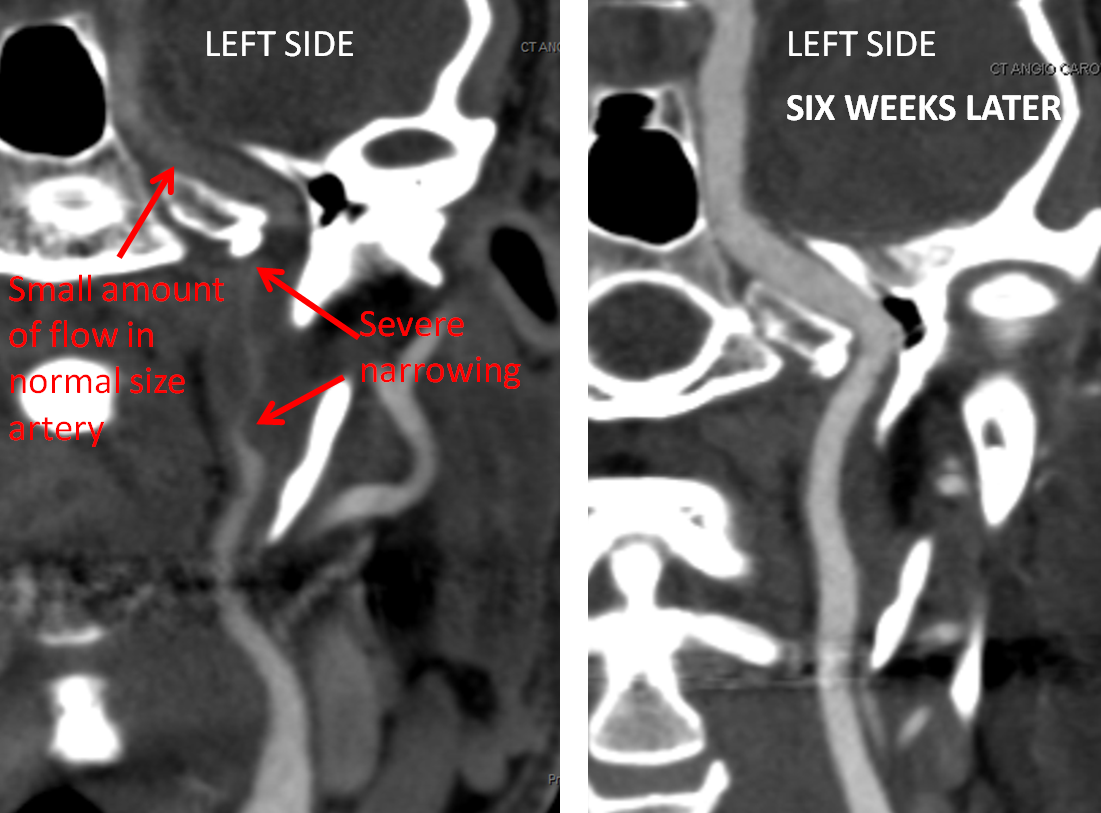
On the right side, even the pseudoaneurysm has healed, though the vessel continues to look somewhat irregular: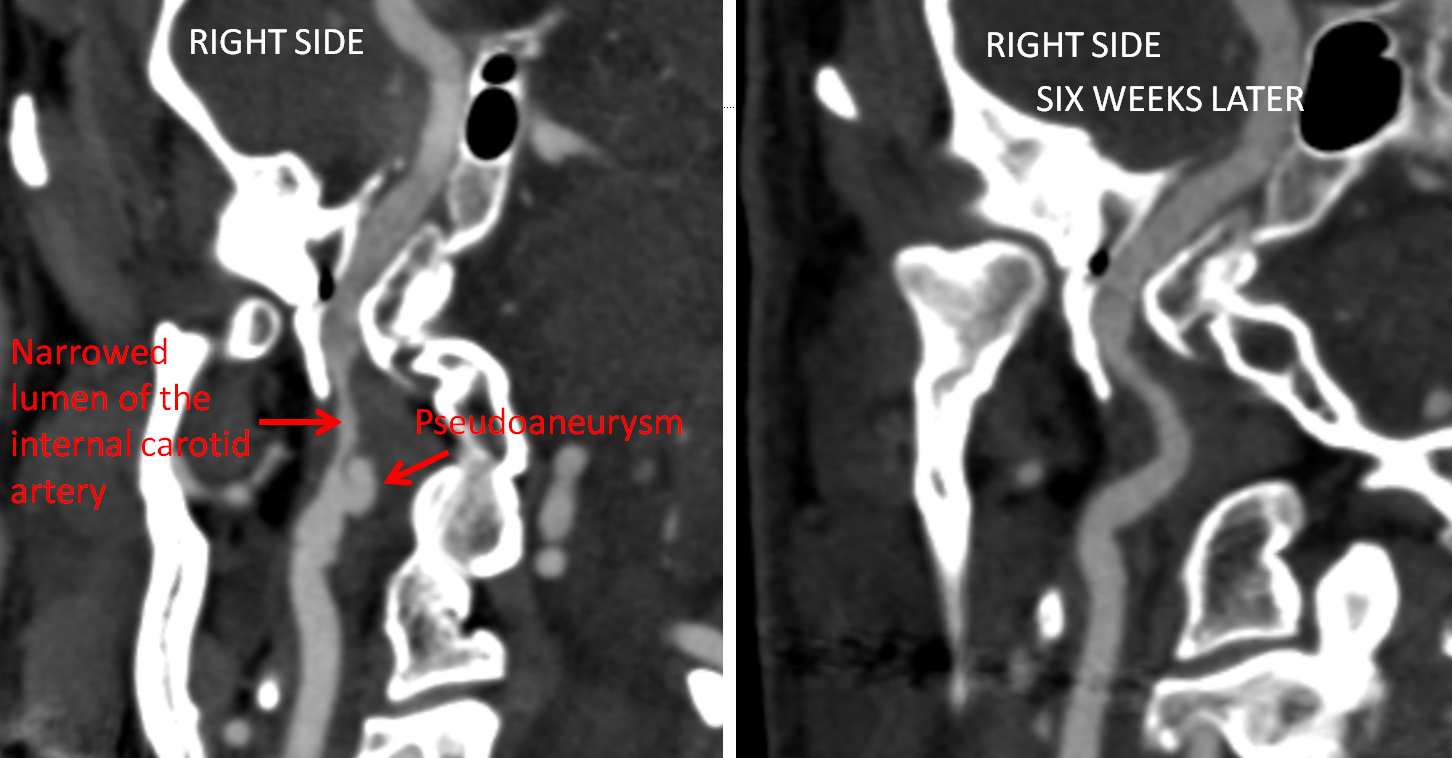
Nerve Palsy (Horner’s Syndrome)
The hematoma inside the vessel can not only compress and narrow the lumen, but expand the size of the vessel itself, as can be seen in the following example, where the dissected left carotid artery is substantially thicker than the right:
The sympathetic nerves to the eye run on the outside of the carotid artery in the neck, encircling it like vines around a tree trunk. These nerves are too small to see on the MRI. The expansion of the carotid artery due to the dissection stretches are damages these delicate nerves, which function to constrict the pupil (make it smaller). When they stp working the pupil gets larger. Thus, a combination of neck pain and and acute Horner’s syndrome (enlargement of the pupil) is strongly suspicious of carotid dissection as a cause. Usually, the nerve will recover and pupil return to normal size, but not always.
Very rarely, patients can develop other cranial nerve palsies as a result of dissection expanding the wall of the vessel and compressing adjacent nerves. It is a very unusual occurrence (most lower cranial nerve palsies do not develop as a result of dissection). An example of dissection causing cranial nerve palsy is shown here.
Stroke
Dissections cause stroke in two ways. First is when clot which forms in the vessel near the tear breaks off and floats (embolises) into the brain, closing off brain vessels. This is called “embolic stroke”. In this patient, several areas of acute stroke (bright areas on a “diffusion” MRI sequence) are seen in association with a right internal carotid artery dissection. Notice that there is still flow in the carotid artery — this is not a complete occlusion. A short time later, the artery has healed. This is a relatively minor stroke, from which the patient is likely to make a full recovery.
The second way in which dissections can cause stroke is when the dissected artery closes completely, cutting off blood flow to the brain. This is an example of complete internal carotid artery occlusion, with poor “collaterals”, meaning no effective way to resupply the brain served by the occluded artery by other “detour” routes. The consequence is a large stroke, demonstrating that while dissections often do very well, that is not unfortunately the case every time. Case courtesy of Dr. Eytan Raz.
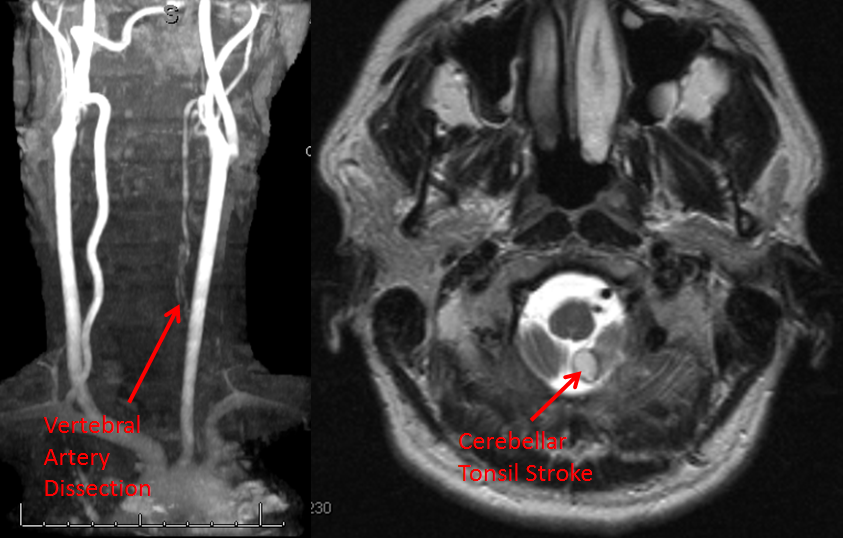
Vertebral arteries supply the back part of the brain, including the brainstem, which is vital to life. The vertebral artery travels in the neck inside special holes (foramina) within the bones of the neck. It is therefore vulnerable to injury when bones are pushed out of alignment or injured. This can happen as a result of accidents, forceful neck manipulation such as chiropractic adjustements, etc. Here is an example of vertebral artery dissection resulting in a stroke of the cerebellum.
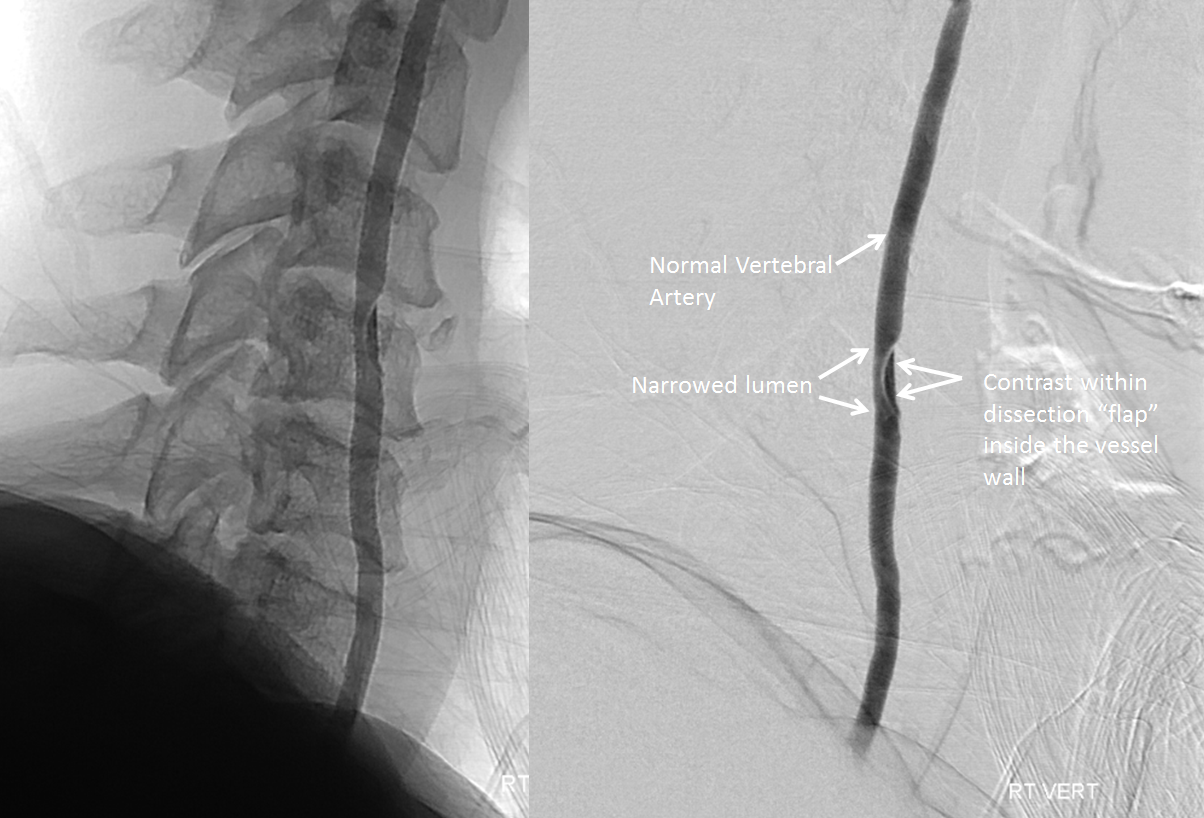
Dissections can sometimes take place as a complication of catheter angiography. For whatever reason, the inside of the artery is injured during catheterization, initiating the dissection. The risk of dissection during angiography in a high-experience institution is very low, but it is not zero. Here is an example of a dissection I created (inadvertently of course) during an angiogram. Recognition of the dissection allows one to initiate necessary steps to minimize any possible damage; this patient did very well.
Dissection as a result of pre-existing vascular disease
Although many dissections are apparently spontaneous, taking place in a segment of an artery with no known pre-existing disease, this is not always the case. For example, dissections can happen on a background of a cholesterol plaque within the artery wall. The scenario is like this — the patient develops atherosclerosis (cholesterol plaque) in an artery (carotid artery in the neck, coronary artery in the heart, etc). The tissue covering the plaque (cap) ruptures, leading to blood penetration into the plaque (penetrating ulcer). The blood dissects through the plaque (and possibly into normal artery), leading to vessel narrowing and stroke or heart attack. In this way, plaques which do not narrow the artery much or at all can suddenly become a nidus for severe narrowing as a result of the dissection. Although this happens in a minority of cases only, at least in the carotid artery, it shows the importance of considering medical and sometimes surgical treatment of all atherosclerotic lesions.
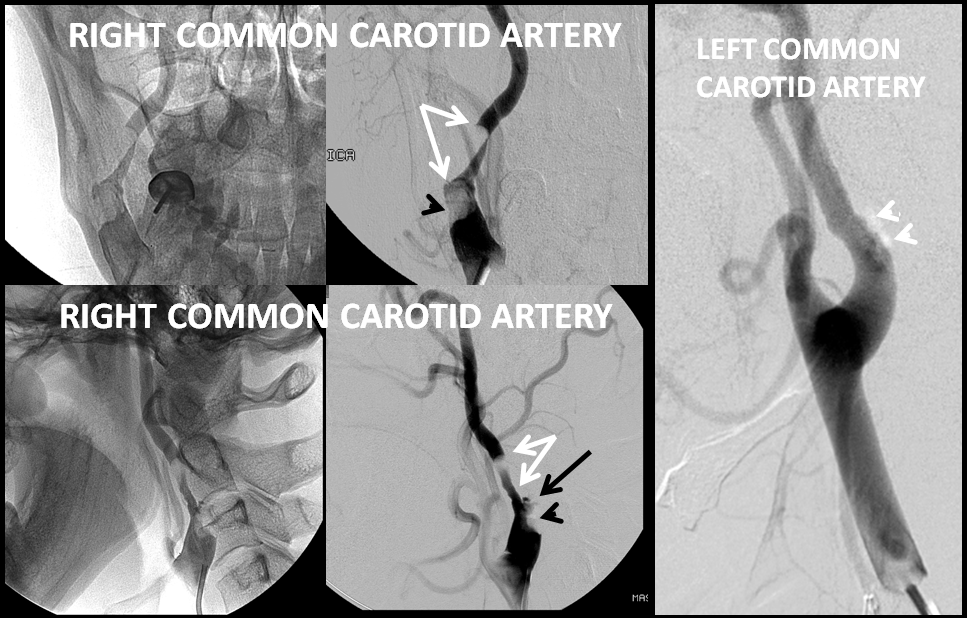
Here is an example of a dissection (white arrows) nearly completely occluding the right internal carotid artery. The dissection is caused by a penetrating ulcer (black arrow) into a pre-existing carotid bifurcation atherosclerotic plaque, a typical location for such cholesterol deposits. A large amount of thrombus (clot) is present underneath the dissection (black arrowhead). Notice “mirror image” atherosclerotic plaque involving the left internal carotid artery (white arrowheads), which causes almost no narrowing of the vessel, just like the right side before it gave rise to the dissection.
Pseudoaneurysm / dissecting aneurysm formation
Dissections can result in formation of a “pseudoaneurysm” An aneurysm is a weakness in the wall of the artery which causes the artery to bulge out — either focally (saccular aneurysm) or circumferentially (fusiform aneurysm). The distinction is actually very artificial, but the naming persists. A pseudoaneurysm is a kind of aneurysm where part of the aneurysm wall is defective, whereas a “regular” aneurysm is supposed to be one where all wall layers are intact. In fact, in neither kind are all layers intact by definition, so again the distinction is rather historical, but historical inaccuracies are hard to correct… So you may see both aneurysm and pseudoaneurysm listed…
In any case, when dissections weaken enough of the vessel wall, the remainder can bulge out, forming a dissecting (pseudo)aneurysm, like so:
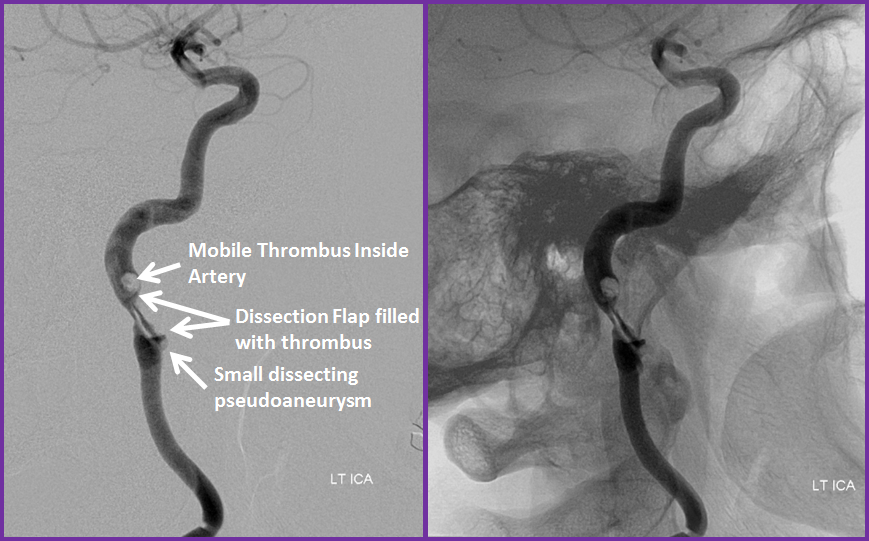
Here is an example of how one evolves. In this angiographic image obtained a few days after a dissection (patient came in with a small stroke), one can actually see thrombus (clot) filling the artery just beyond the dissected segment. The clot loosely adheres to the artery, and is at risk for breaking off. The patient is put on Coumadin, and the clot slowly dissolves. Notice a small pseudoaneurysm present at this time:
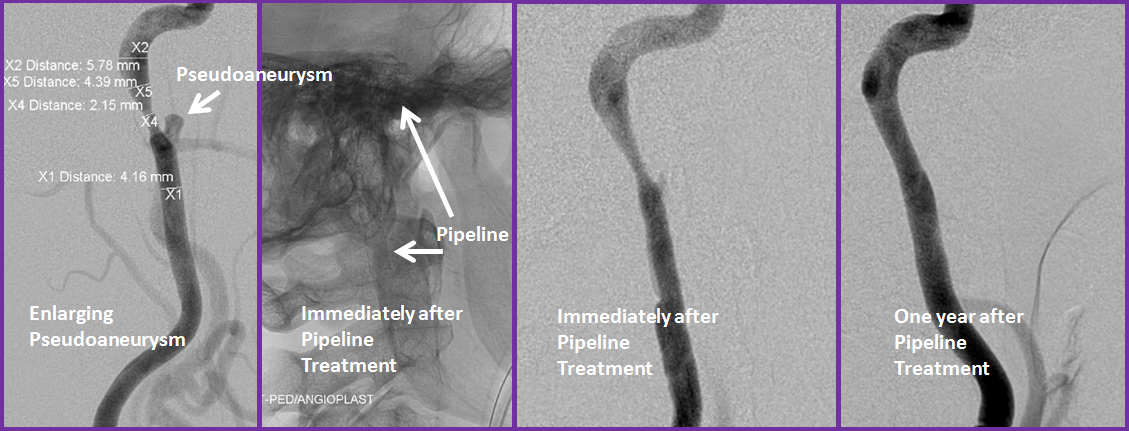
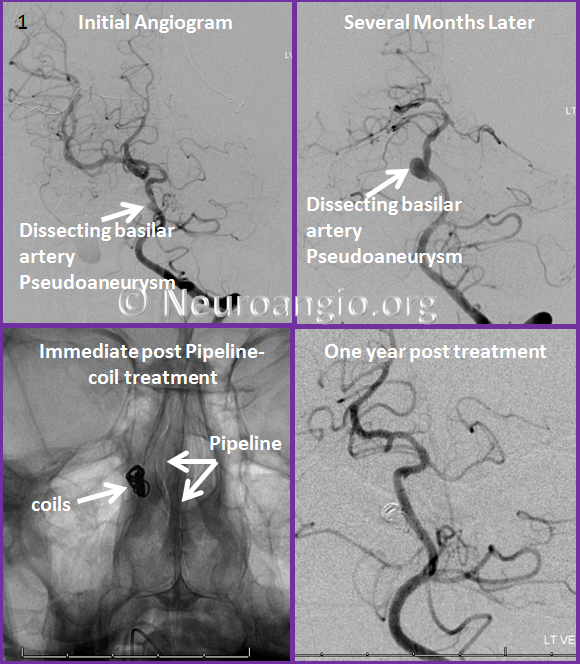
Several months later, the thrombus has dissolved, however the pseudoaneurysm has grown (leftmost image). This was treated by placement of a Pipeline Embolization Device. developed at my institution by my senior mentor Dr. Peter Kim Nelson. One year later, not only has the pseudoaneurysm healed, but the narrowing of the artery has resolved as well.
Here is an example of another dissecting pseudoaneurysm, also involving the internal carotid artery
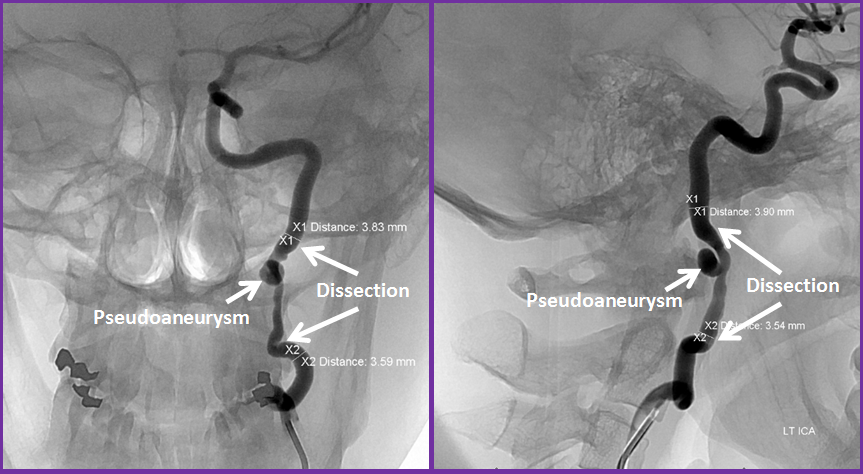
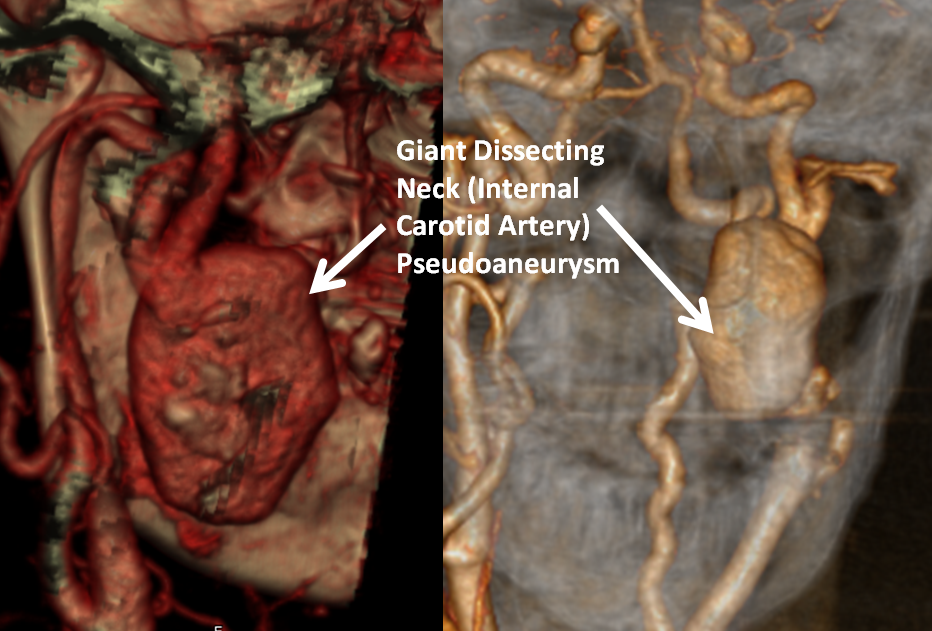
While many times these neck pseudoaneurysms are “observed” by repeat imaging without treatment, sometimes this generally sound approach turns out to not be such a good idea, as in this patient who developed a massive pseudoaneurysm in the neck which started to press on the swallowing organs.
We also usually follow small neck pseudoaneurysms and treat only when they show growth or cause other problems. This is very different from intracranial dissecting aneurysms, as discussed below.
Intracranial Dissection
Most dissections involve the internal carotid or vertebral arteries in the neck. Although potentially dangerous, as you can see from the above, most actually heal quite well with some medications to prevent stroke. Dissections which involve the inside of the skull — either by extension from the neck, or forming there primarily — can be extremely hazardous. Arteries inside the skull are generally weaker than in the neck, and dissections there have a greater chance of rupture, resulting in either subarachnoid hemorrhage (SAH), a fistula, such as carotid-cavernous fistula, or a brain pseudoaneurysm formation (see Patient Information Cerebral Aneurysm and ICA and its aneurysms pages). These aneurysms can be very difficult to treat because of the weakness of the wall that defines them and their often sensitive location. For example, this patient was noted to have a “small” aneurysm, which only a few months later has substantially enlarged — a dissecting basilar artery aneurysm, which was fortunately treated before rupture by a combination of Pipeline and coil devices.
Here is an example of an intracranial dissection involving an artery called the Middle Cerebral Artery. This middle-aged man reported one episode of right-sided weakness, which quickly resolved. He was started on an aspirin for a presumed transient ischemic attack (TIA); he did not take the aspirin, and one week later experienced transient speech difficulty, which resolved quickly as well. This time a real workup was done. CT Angiogram shows “filling defect” inside the left middle cerebral artery — filling defect is something inside the artery that shouldn’t be there. Its a subtle, but in this case critical finding:
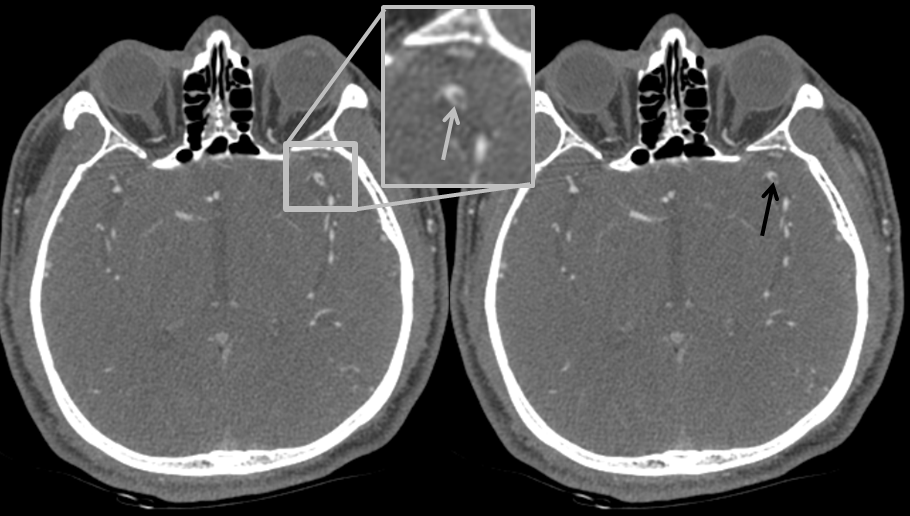
The usual thing to say is that this is clot (thrombus) sitting inside the artery (intraluminal thrombus). However, an astute radiologist, Dr. Adam J. Davis, suspects that this may be a dissection based on its morphology. He suggests an angiogram, which has far higher spatial resolution than than current CT scan — meaning it can see thing in greater detail. Even the venerable, almost 20-year old Bellevue hospital analog biplane we still run there, as of 2015, has that capability.
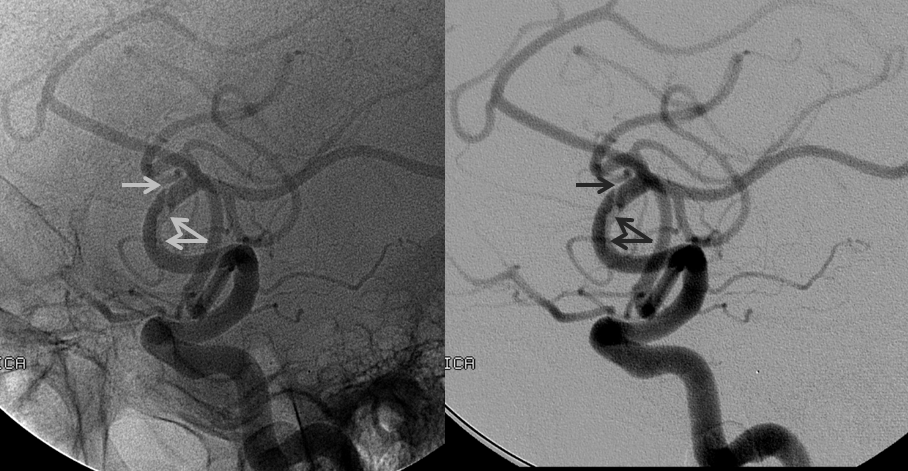
The angio shows a curvilinear dissection flap within the vessel, with about 40% narrowing of the lumen. The two important factors are the degree of vessel narrowing — 40% in this case can be managed with medications and does not require mechanical re-opening — and absence of a pseudoaneurysm (see above). In our institution, any pseudoaneurysmal development is an indication for repair (stenting). In this case, the patient was placed on antiplatelet medications, with close imaging follow up to monitor healing.
Here is a more obvious dissection involving the intracranial middle cerebral artery (red arrow = false lumen, blue arrow = severely narrowed residual true lumen), possibly related to underlying plaque, although there are no other areas of atherosclerosis

Questions/comments: contact me through the “Contact Us” page; to schedule a consultation one can also call the office at 212-263-6008
