General Information: While a great deal can be said about aneurysms in general, it is truly impossible to make online discussion relevant to the individual patient with his or her particular situation. The only way to meaningfully inform the patient is by direct conversation and review of imaging studies.
The following section provides some information regarding aneurysm diagnosis, evaluation, and treatment-forming a basis for a more in-depth discussion. Also, much excellent information on cerebral aneurysms is available on the web-links are given below
What are cerebral aneurysms and how do they form?
Aneurysms come in all kinds of shapes, sizes, and types:saccular, fusiform, mycotic, vasculitic, large, giant, etc. A more technical page on this site, Internal Carotid Artery and Its Aneurysms, shows no shortage of various aneurysm forms and shapes,and this is just a small fraction of the overall aneurysm mix. Most aneurysms are felt to be “weaknesses” in walls of brain arteries which bulge out over time. The actual mechanisms of aneurysm formation depend on aneurysm type, and, frankly, for most aneurysms the true causes are still unknown. This is not the kind of uncertainty we likeas patients or as physicians, however,such are the facts. Most patients with brain aneurysms have no underlying disorder that we know of. On the other hand, many known disorders are associated with increased risk of forming aneurysms-polycystic kidney disease and sickle cell disease are some of the more common ones. Common conditions which encourage aneurysm growth and increase the likelihood of rupture include hypertension and smoking-the usual suspects.
When do aneurysm form?
Most “saccular” aneurysms-the most common type-are discovered in middle-aged and older adults. This kind is very rare in young adults and extremely rare in children. Why exactly the aneurysm begins to grow, and how fast it does so, are great questions to which we have no answer. When an aneurysm is found “incidentally”, meaning during evaluation of some other problem (by MRI, most typically), the question of “how long has it been there” can usually only be guessed, and depends on the particulars of the patient presentation. There are many other rare types of aneurysms (such as the “mycotic” kind) which form for different reasons and at different times.
Why multiple aneurysms?
About 10-30% of patients, depending on which article you read, have more than one. About 5% will have three or more. In most cases, we don’t know why. Evaluations of such patients for known “connective tissue disorders” or other suspects usually discover nothing of value-which simply means we don’t yet know the reasons or haven’t discovered the underlying disease or genetic abnormality. Genetic studies are beginning to shed light on the issue.
Family History?
The overall prevalence of aneurysms in the North America is between 0.5-2%-perhaps 1 out of 100 middle-aged individuals has one. Most of these patients have no family members with aneurysms that they know of. For those that do have a blood relative with an aneurysm or history of subarachnoid hemorrhage (“SAH” or brain bleeding), screening of first degree relatives with Magnetic Resonance Angiography (MRA). It is important to realize that a normal MRA in a 30 year old is no guarantee and probably should be repeated at 5-10 year intervals until about age 50-60. Patients with polycystic kidney disease and sickle cell disease should be screened regardless of family history, in our opinion.
Aneurysm discovery
With widespread use of MRI and CT technology in North America, most aneurysms are now discovered “incidentally”-an MRI/MRA is done for evaluation of chronic headaches, dizziness, etc., and an aneurysm is found-which has nothing to do with the original complaint. Occasionally, aneurysms grow to be large enough to press on adjacent brain or nerves which produces a “mass effect”-a pupil of the eye getting larger than the other, double vision, etc. Yet another mode of discovery is the “sentinel bleed”-either a small hemorrhage (bleed) or a period of aneurysm growth which produces a new, bad headache. This “sentinel bleed” concept is nebulous but important, because if may be a warning sign of the dreaded aneurysm rupture.
Aneurysm rupture — subarachnoid hemorrhage and other
Unfortunately, most aneurysms produce no symptoms until they are either discovered incidentally or until they rupture. Most aneurysms are located on arteries which surround the brain in a compartment called “subarachnoid space”. Therefore, aneurysm rupture results in bleeding around the brain, the feared “Subarachnoid Hemorrhage”. Not infrequently, bleeding also extending into the brain itself or its internal fluid spaces-called ventricles. The classic symptom of aneurysm rupture is the “worst headache of my life”. It is truly the worst headache ever and there is nothing like it. The headache is caused by sudden rise in intracranial pressure as arterial blood begins to fill the spaces surrounding the brain. The rising intracranial pressure also has the effect of decreasing blood flow to the brain which causes many patients to pass out soon after developing such a headache. Other symptoms include vomiting, lethargy, and weakness.
A special group of aneurysms which are located inside the skull but outside of the sac which surrounds the brain (dural sac) can rupture without the catastrophic consequences of subarachnoid hemorrhage. Many of these aneurysms are located inside a large venous lake at the bottom of the skull called “the cavernous sinus”. Rupture of these “cavernous aneurysms” leads to establishment of a direct communication between the carotid artery (site of aneurysm) and cavernous sinus- a condition called “carotid-cavernous fistula”-usually presenting as a sudden severe pain behind the eye, followed quickly by severe eye swelling and redness-the stuff of horror movies. Nevertheless, this kind of rupture is usually far less dangerous than subarachnoid hemorrhage. Yet other aneurysms can present with bleeding directly into (not around) the brain- mycotic and vasculitic aneurysms being of this kind.
Consequences of aneurysm rupture
The outcome depends on many factors- for example how much bleeding there was, location of aneurysm, age and general health of the patient, and subsequent medical care. Unfortunately, about 15% of patients die before reaching the hospital, and 40% will not survive the first two weeks, despite the best available care. Of the remaining 60%, more than half will be permanently disabled. A minority of perhaps 20% will return to their pre-rupture employment and level of function. These numbers explain why both doctors and patients tend to become quite nervous when facing discovery of an aneurysm. Why such grim statistics? Because the brain is an extremely complex organ, designed for performance in a sheltered environment of the skull, under carefully controlled conditions- and has a very low tolerance for injury. It is simply not built to tolerate lack of blood flow, high surrounding pressure, or irritation produced by bleeding for any extended length of time. Most damage caused by aneurysm rupture is typically sustained in the first minutes of the event. Even flawless subsequent care – and such care is extremely complicated and very often subject to setbacks and additional complications even in the best of centers – can only prevent future bleeding and help mitigate the harmful effects of the initial rupture to give the brain the best chance for ultimate recovery; it cannot reverse whatever damage was already done.
Will the aneurysm rupture?
That is the key question facing a patient with an unruptured aneurysm. We have no crystal ball to predict which one will rupture and when. The best advice we can give is offered because of evidence-based studies which followed patients with different aneurysms for many years without treatment-either because of patient preference or because treatment was felt to be ineffective or too risky. What we learned-and continue learning-from these studies is that the risk of rupture depends on the size and location of the aneurysm as well as possibly additional parameters such as aneurysm shape, possible symptoms, family history, etc. Undoubtedly, there are other factors yet unknown, and many are being investigated. For the time being, we can only speak in terms of probabilities; this is not what either patients or doctors want in the ideal world, but such are the facts. For example, one can say that a 5 mm ophthalmic aneurysm has a rupture rate well below 1% per year whereas the same size aneurysm located on the posterior communicating artery or basilar artery has a rupture risk of perhaps 1-2% per year. One can never say that a given aneurysm will never rupture or will rupture for sure.
What do all these statistics mean?
To make an informed decision, the modern patient needs to appreciate that everything has a certain risk. Living with an aneurysm has risk. Treating aneurysms also has risks. What needs to be decided on individual basis is which makes more sense: treatment or observation. In other words, is the risk of treatment justified by the risk of disease? For example, we may recommend that a small aneurysm in an elderly patient be observed (not treated) if we feel that treatment is more likely to harm the patient than the risk of the aneurysm rupturing over the patient’s projected lifetime. On the other hand, we may advise treating the same size aneurysm in a younger, healthier patient who has a greater life expectancy and therefore a greater cumulative risk of rupture.
Patient perspective
Usually, patients need time to do their research and come to their conclusion about what they wish to do. Much here depends on how different people perceive risk. One person may not wish for any treatment- because all treatments have risks- and would rather take chances and live with the risk of rupture. Other patients come to seek treatment despite the fact that their small aneurysms are unlikely to ever rupture and treatment may well be more hazardous than the disease; they are simply unable to continue living normal lives with the knowledge that there is an aneurysm inside their head- however small the chance of rupture may be. All of these factors form the basis of individual patient-doctor discussions which we hold with patients referred for aneurysm evaluation.
How are aneurysms investigated?
This depends on several factors. Ruptured aneurysms are dealt with in hospital settings with an array of imaging and treatment modalities which include CT, MR, and catheter angiography; treatment options include surgery and catheter-based (endovascular) treatment. Unruptured aneurysms-which are usually discovered by MRI (or CT)- may require more diagnostic imaging before a management decision is made. Our preference is to perform catheter angiography on most patients with unruptured aneurysms which we feel gives us the best information needed to make an informed decision as to what should be done. For more information, you can visit the Introductory Brain Angiography page
Treatment options
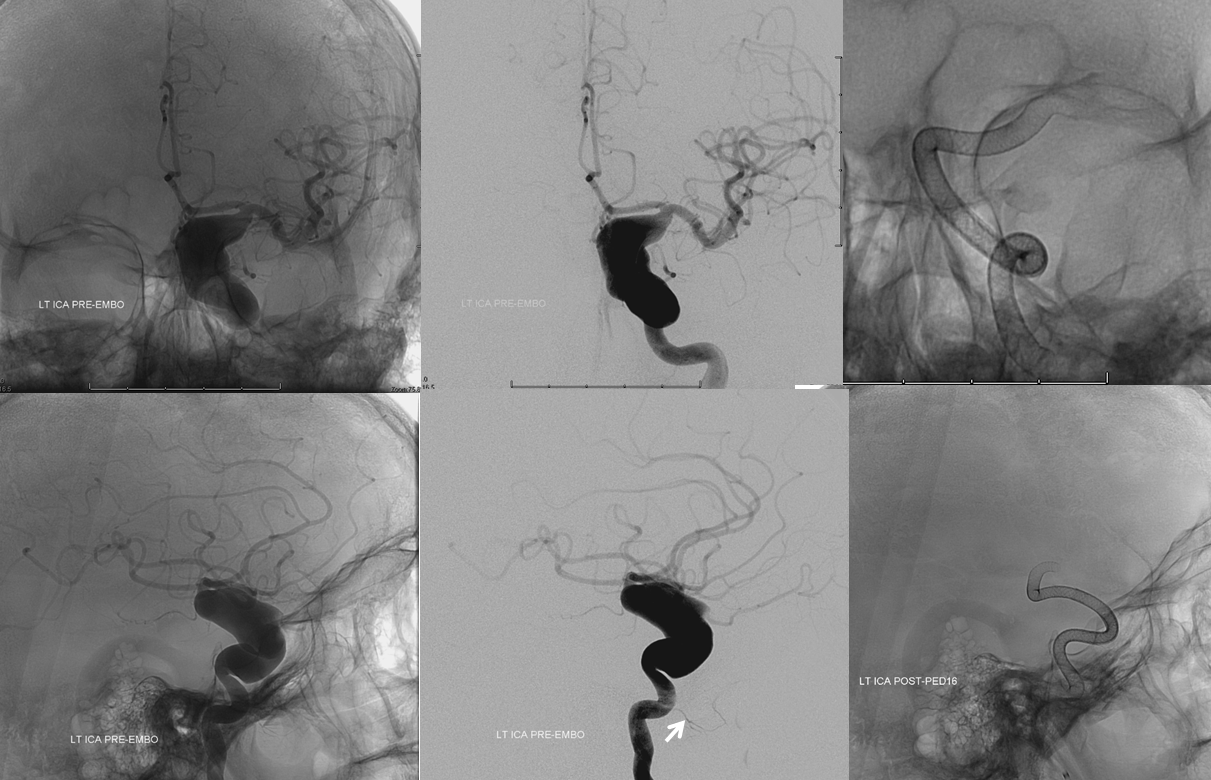
The two main options are endovascular treatment (which is performed through catheters inserted into arteries under x-ray guidance) and open surgery. Which option is right? This depends on many factors: aneurysm location, size, patient condition, patient preference, and local expertise. This decision has to be made on an individual basis. Endovascular (catheter-based) treatments continue to evolve so that more and more aneurysms are now amenable to durable treatment. The main criticism of endovascular methods-which are, overall, beyond any reasonable doubt safer and gentler on the patient than open surgery-is a higher chance of incomplete aneurysm treatment than with surgery. This leads to need for occasional re-treatment and may not fully protect the patient against rupture-the reason for undergoing the procedure in the first place. Improvements in endovascular techniques (including those developed at our institution) maximize the chances of complete endovascular cure. Few patients wish to have their heads opened if a less invasive option is available. On the other hand, we too feel that certain aneurysms should still be safely and effectively treated with open surgery (many middle cerebral, posterior communicating, and anterior choroidal types, for example) even though our particular expertise is in the endovascular arena.
How do I know which treatment is appropriate?
Frankly, you have to trust your doctor to give you their best advice and trust your intuition that you are being treated in a fair way. In Europe, it is becoming increasingly difficult to find surgeons who are capable of operating on aneurysms since the vast majority of aneurysms discovered there are treated by endovascular methods. The very same aneurysms, however, continue to be dealt with predominantly by open surgery in other places- such as Japan or Finland. In North America, some centers are almost exclusively offering surgery, others endovascular, and many do both. As a patient, you should be aware of this important fact- particularly as endovascular methods are considerably more advanced now than in the era of classic “coiling” which began the endovascular revolution 20 years ago. Modern options include Pipeline and other flow diverters, more advanced coils, balloons, stents, and combinations thereof. It is in the best interest of the patient to inquire how many aneurysms the center and particular physician in question treats over a given period of time; this is never a guarantee of good outcome, but all things being equal more experience is better than less experience. Barring rare emergencies which require the group to cover several hospitals simultaneously, our center has at least two faculty physicians “scrub in” on every scheduled aneurysm case. The number of times this approach has proved critical is beyond count.
Whatever treatment is ultimately chosen, it is critical for the patient and family to have trust in the goodwill and ability of the physician: endovascular or open surgeon. The fact is that, despite our best efforts, things sometimes do not go as hoped during treatment-a time when both family and patient may find comfort in knowledge that the physician did his or her best, and unfortunately, none of medicine’s procedures are perfect. In a perfect world, there would perhaps be no aneurysms in the first place.
Treatment of ruptured aneurysms is a different matter; both surgery and endovascular options are also available and, in this setting, it is probably best to do whatever the particular medical center at hand is most experienced in.
Follow-up care
For unruptured aneurysms, recovery typically takes days to weeks depending on treatment modality, procedure success, etc. Endovascular treatments are associated with significantly shorter recovery times, in general. Ruptured aneurysms require prolonged hospitalization in intensive care units and typically protracted recovery in various rehabilitation settings. Most patients continue to be periodically monitored for durability of treatment and possible new aneurysm emergence with various imaging modalities.
What do to?
Having seen many patients through the process of decision-making I see that, ultimately, most patients make decisions based on trust and intuition. Everyone within reach of a computer has access to a bewildering wealth of data- frequently of uncertain quality or relevance to the aneurysm at hand. Ultimately, we absorb information through a prism of our beliefs and attitudes, which assigns to all information its “impact factor” toward our decision-making process. Not infrequently, some seemingly minor fact or viewpoint resonates with a particular patient and crystallizes his or her decision. If you have done your homework, and are still not sure how to proceed, chances are that the answer will come from within rather than from without. To the extent that the patient wishes to make an informed decision, he or she should look inside themselves to see what their true motivations and apprehensions are. This kind of courageous self-reflection usually clears rather than complicates the decision-making process.
Again, while a great deal can be said about aneurysms in general, it is truly impossible to make online discussion relevant to the individual patient with his or her particular situation. The only way to meaningfully inform the patient is by direct conversation and review of imaging studies.
To physicians and patients
While a great deal can be said about aneurysms in general, it is truly impossible to make the discussion relevant to the individual patient, with his or her particular situation. The only way to meaningfully inform the patient is by direct conversation and review of imaging studies. If you are seeking an opinion, referral, have questions, comments, or think our section can be of help to you, use “Contact Us” page for inquiry or appointment. The NYU Neurointerventional team is a world leader in treatment of cerebral aneurysms. Devices which revolutionized the field of interventional neuroradiology-such as the Pipeline Embolization Device and the Neuroform stent- were developed at NYU by its current section head Dr. Peter Kim Nelson. The group continues its tradition of unparalleled care, guiding patients through the diagnosis and management of a wide range of cerebrovascular conditions- including cerebral (brain) aneurysms.
Should you need more information, or if you are a patient wishing to make an appointment, you can write me directly via the “Contact Us” section, or call the office at 1-212-263-6008
Excellent online resources are available on the subject:
Brain Aneurysm Foundation: http://www.bafsupport.org/
PUBMED: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002387/
Wikipedia: http://en.wikipedia.org/wiki/Cerebral_aneurysm and https://en.wikipedia.org/wiki/Brain_aneurysm
American Heart Association: http://www.strokeassociation.org/STROKEORG/AboutStroke/TypesofStroke/What-You-Should-Know-About-Cerebral-Aneurysms_UCM_310103_Article.jsp
SNIS: Society of Neurointerventional Surgery (as a disclaimer, I am a member of this Society): http://www.brainaneurysm.com
An expert local resource for patients with headaches, including sudden onset ones, not all of which are aneurysm-related: http://www.doctorstrizhak.com/Worst_Headache_Cause.php
