Case Courtesy Drs. Jay Morrow and Matthew Nicholas
Terson syndrome (or Terson’s syndrome) — is a not so rare as you might think complication of elevated intracranial pressure in general but subarachnoid hemorrhage in particular. It is characterized by hemorrhage in the eye, usually subhyaloid (between vitreous and retina), but often vitreous. It is thought to be caused by sudden rise in intracranial pressure, of which SAH is a prime example. It is well described in ophthalmology literature but not so well in neurosurgical/neurointerventional one. According to our eye colleagues, up to 13% of SAH patients have it. If so, I feel that majority must be asymptomatic.
Here is a classic case of one. The patient complains of a dark spot in right eye, after extubation following onset of sudden severe headache, subsequent diagnosis of subarachnoid hemorrhage, and coiling of a ruptured dissecting fusiform left intradural vertebral artery aneurysm
Classic CT of subarachnoid hemorrhage and focal hyperdensity in the globe. The hemorrhage is likely subhyaloid, which is in front of the retina. Therefore, the patient sees a dark spot.
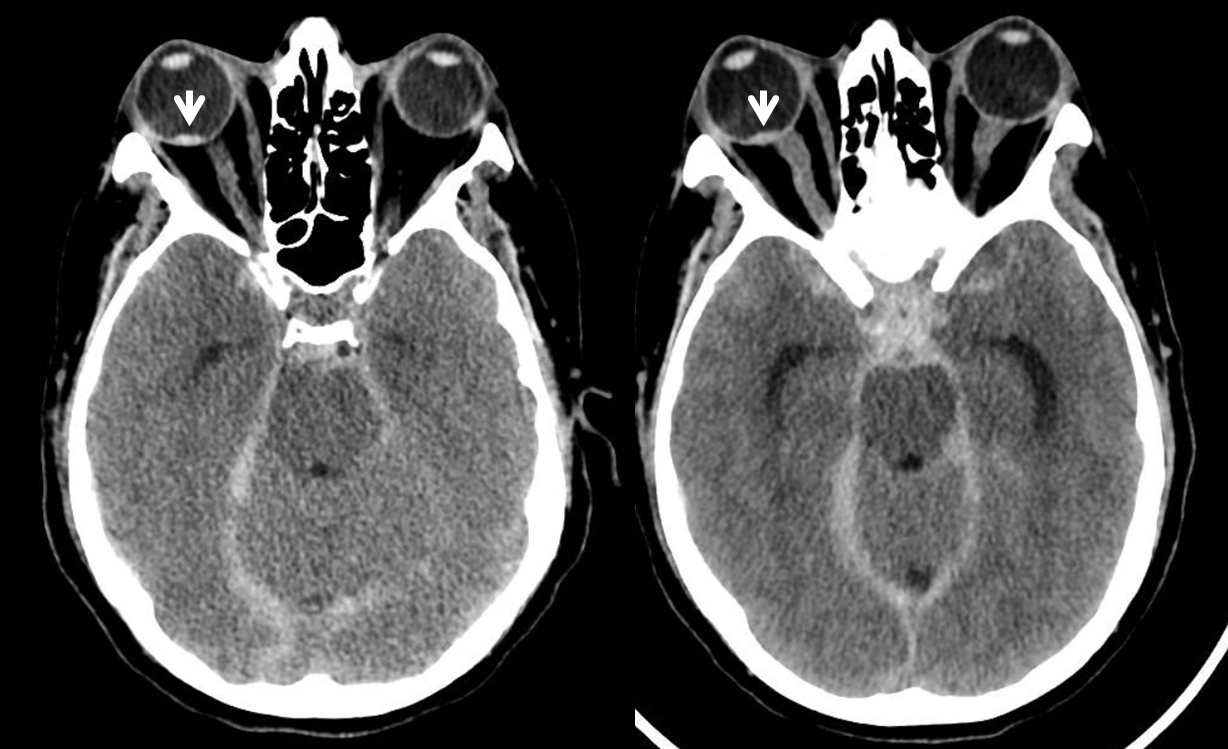
Notice blood tracking in the optic nerve sheath. It is not the same blood as in the eye — that is due to rupture of a small artery or vein in the globe. However blood tacks like this can be seen in Terson’s.

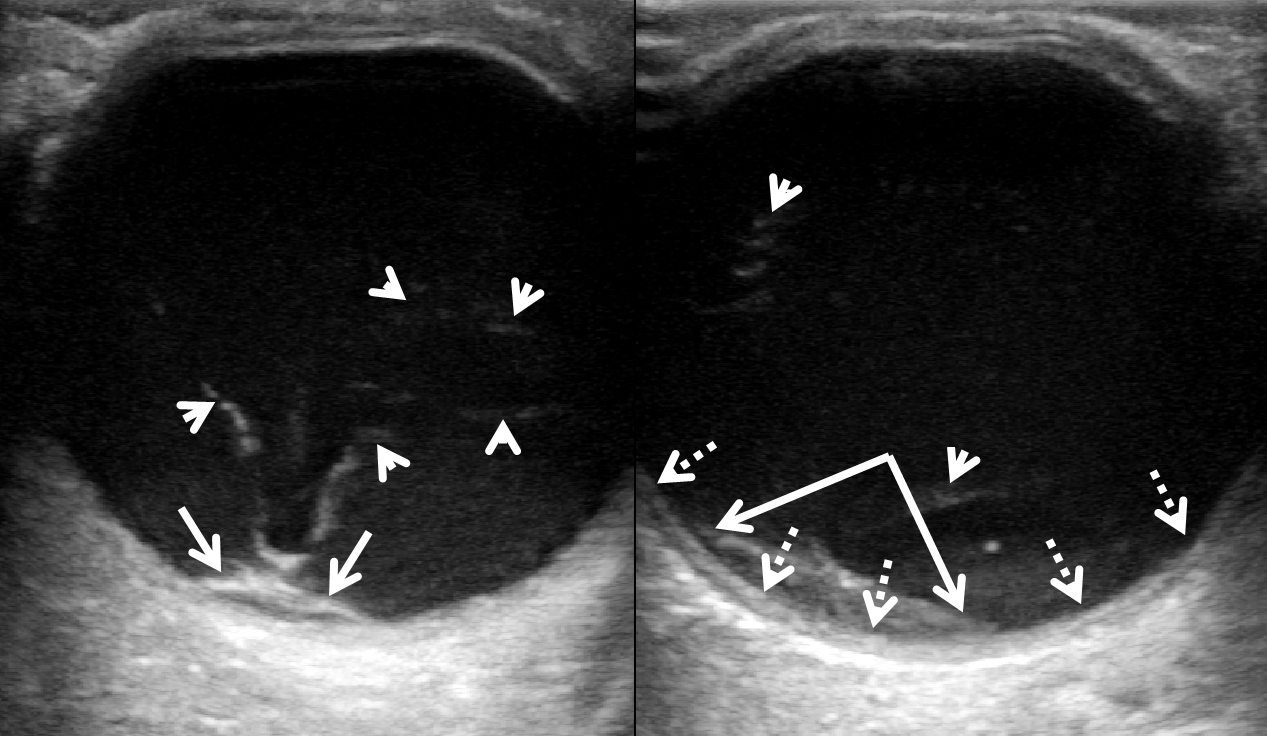
Patient worsens with new extreme blurred vision however sees light and pupillary reflex is preserved. Now we have an ultrasound, which is much better than CT. No special machine is needed, although the ones ophthalmologists have are much better. This was done on a modest portable ultrasound with a standard 13 MHz linear probe. Probe goes over the closed eyelid. Here we better see the normal retina (dashed arrows), subhyaloid hemorrhage (solid arrows) and all kinds of vitreous hemorrhagic debris (arrowheads). The explanation for worsening of vision is extension of previously focal subhyaloid hemorrhage into the vitreous.
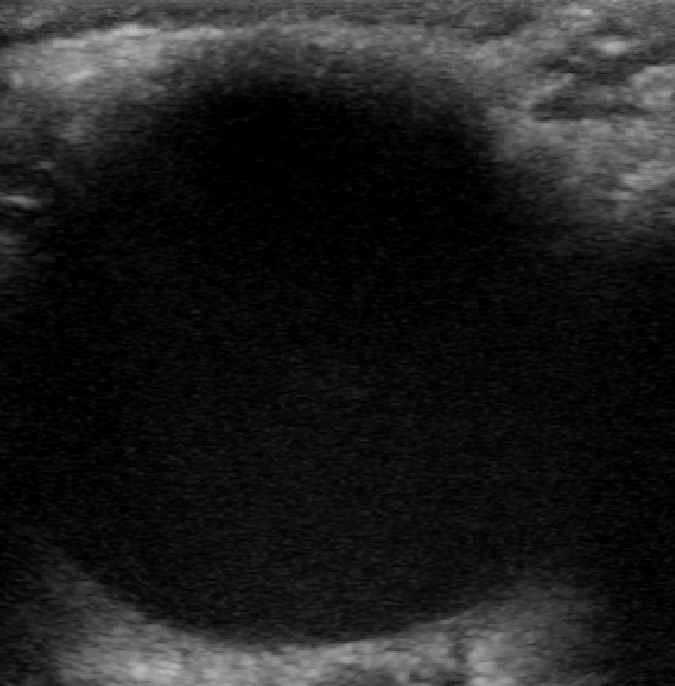
Here is a normal eye, for us non-ophthalmologists
T2 MRI
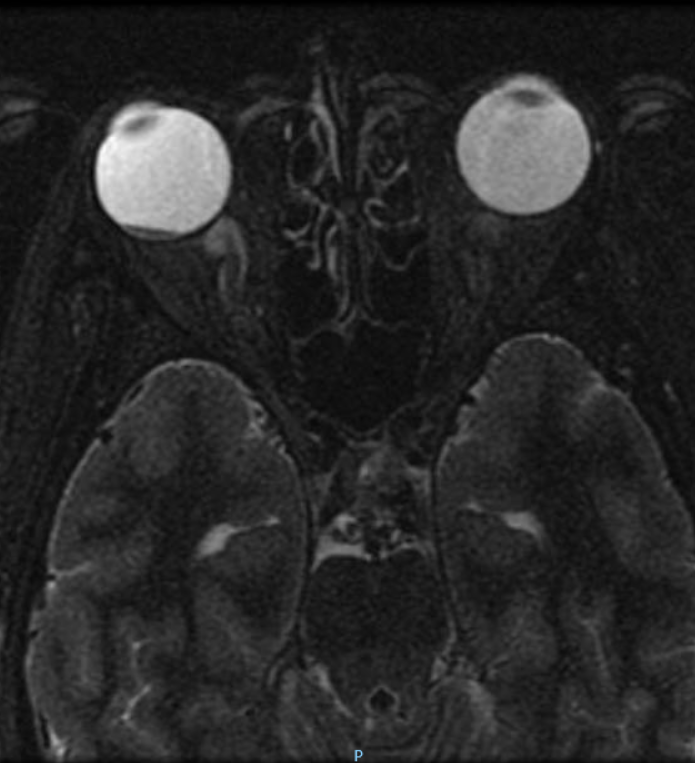
Gradient Echo

The cause is a dissecting vertebral artery aneurysm
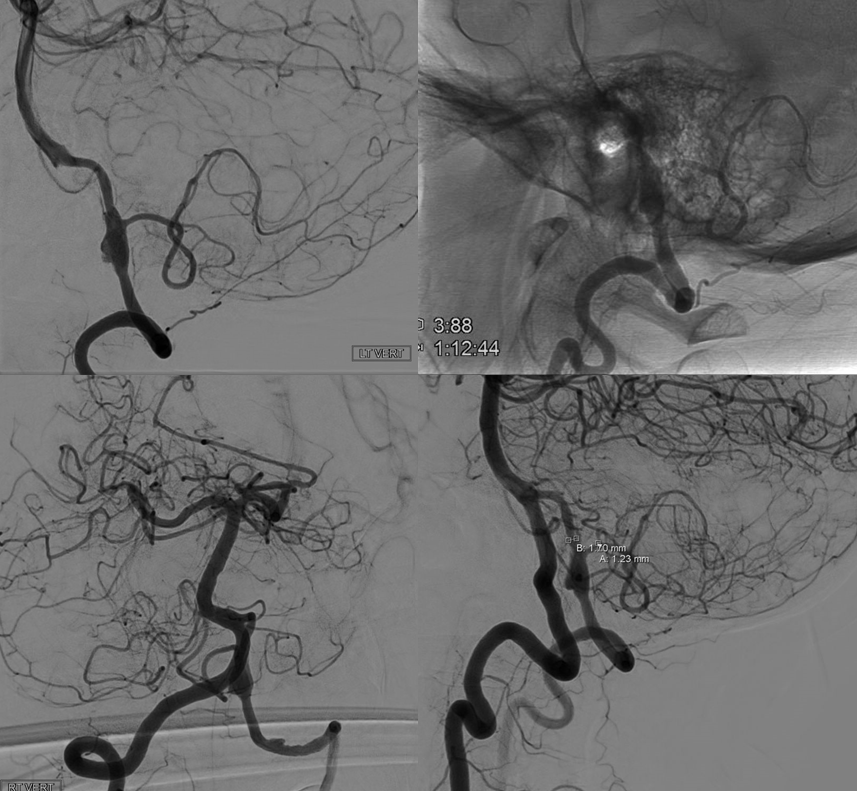
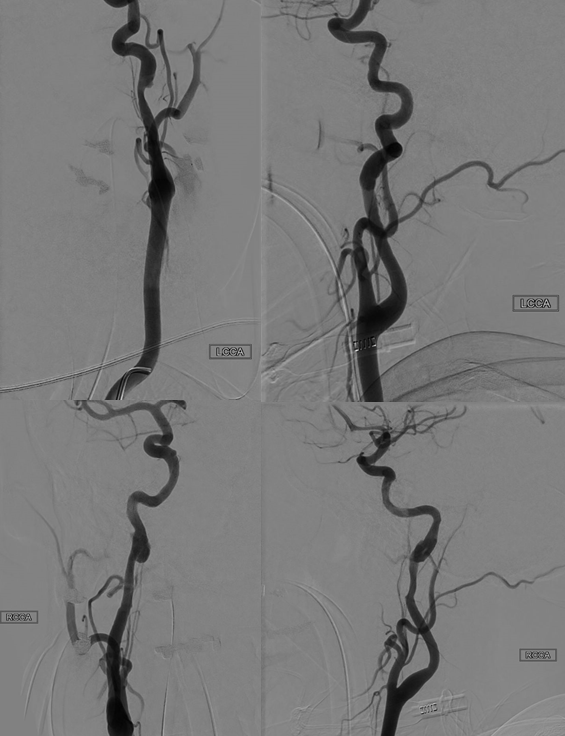
Also of interest are two additional dissections of the upper cervical internal carotids, to showcase the spectrum of dissection consequences. One has a small lumen stenosis, one has a pseudoaneurysm, and another one ruptured intradurally.
Further reading
