Mandibulovidian Artery
The MV artery originates from the petrous portion of the Internal Carotid artery. The artery, typically, consists of two branches — the Mandibular and the Vidian. Either or both branches may be present separately.
Both Mandibular and Vidian branches originate from the ascending petrous portion of the ICA in the foramen lacerum. The Vidian branch courses forward to enter the Vidian canal (together with the greater superficial petrosal nerve) and exits into the pterygopalatine fossa, where it meets the Internal Maxillary Artery. Think of the Vidian is a thin connection between the much larger ICA and IMAX. In fact, the name Vidian artery is applied to both ICA and IMAX origin vessels, creating confusion. The overall idea, again is a spectrum between ICA and IMAX dominance, which can be shifted by disease or intervention.
For the sake of clarity, we will call the branch either Vidian ICA or Vidian IMAX, depending on the vessel of origin. If you see a larger Vidian IMAX, there will likely not be a visible Vidian ICA. Typically, the internal maxillary artery dominates supply of the regional tissues, which explains in part why the “Vidian ICA” artery is rarely seen. The second part is technical — the Vidian canal is a small tube enclosed in dense bone, which does not help visualization. The Vidian ICA artery is on occasion prominent when no pathology is evident (i.e. when IMAX contribution is for some reason minimized) and in this disposition supplies the vidian nerve and various structures in the region of the pterygopalatine fossa, such as portions of the posterior nasopharynx, nasal septum, turbinates, and surrounding musculature. It is however often enlarged in setting of vascular diseases of the nasopharynx and adjacent tissues, notably juvenile nasopharyngeal angiofibroma. Iatrogenic occlusion/sacrifice of the IMAX, such as during treatment of epistaxis, can also lead to Vidian enlargement. Conversely, the Vidian occasionally enlarges after proximal occlusion of the ICA and may be one source of ICA reconstitution from the IMAX, albeit considerably less common or efficient than Ophthlamic or middle meningeal routes. The Ascending Pharyngeal artery (superior division pharyngeal trunk) also collateralizes with the Vidian in the pterygopalatine fossa. The overall idea, again, is balance.
The mandibular branch of the Mandibulovidian artery does NOT enter the Vidian canal. Its course is anterior and inferior, in contrast to the more anterior straight course of the Vidian ICA. Because of its inferior slant, it soon exits the temporal bone to supply the neighboring soft tissues, which includes the pterygoid muscles and portions of the posterior pharyngeal wall, and possibly the mandibular condyle (foramen lacerum is situated slightly posteromedial to the mandibular condyle). Often, however, the mandibular branch projects medially away from the condyle. As in case of the Vidian ICA, the IMAX also has a mandibular branch which goes to the same area around the condyle as the ICA mandibular twig. So the same situation applies — usually the IMAX supply is dominant.
EMBRYOLOGY
For the most extensive discussion of Vidian embryology in modern literature, please consult an excellent article by Dr. Osborn in Radiology. Osborn, A. G. The vidian artery: normal and pathologic anatomy. Radiology 1980 (136) 373-8
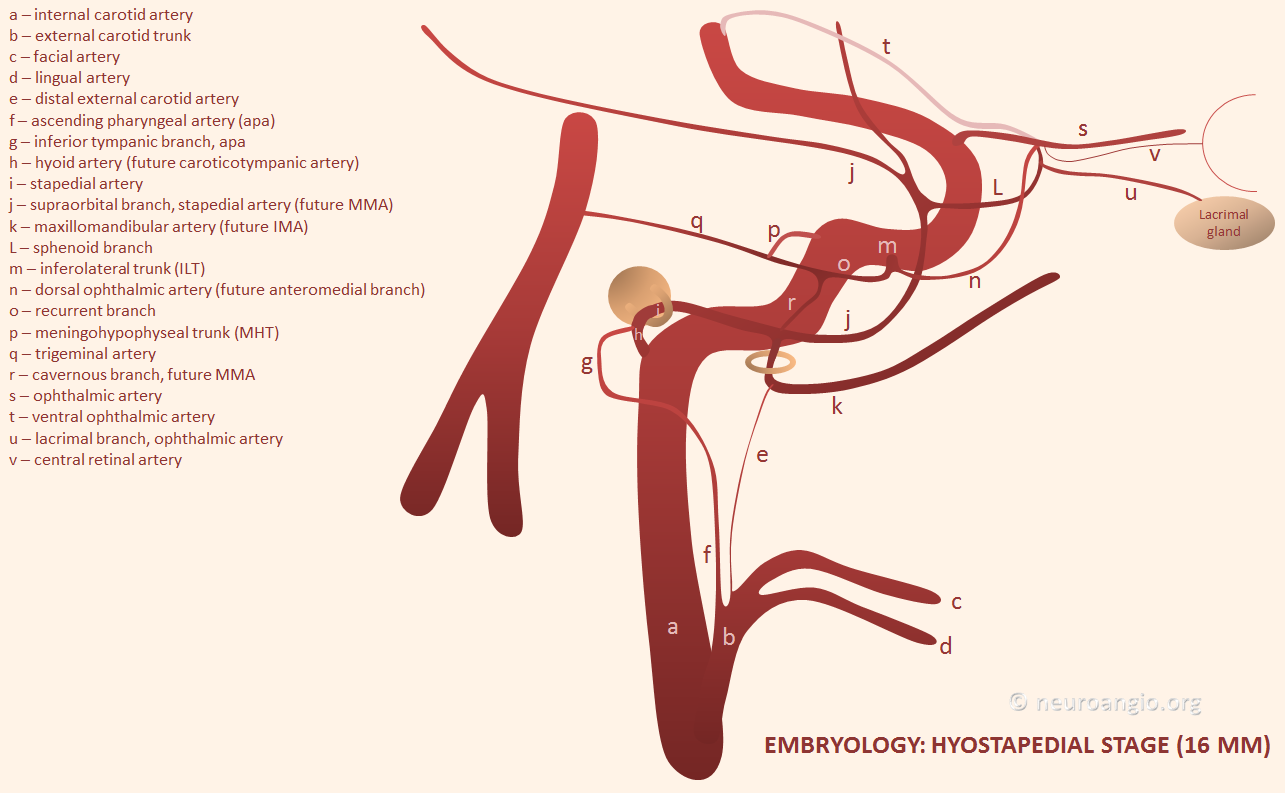
Briefly, the Vidian artery is a “remnant” of the first aortic arch. At 4-5 mm embryonic stage (i.e. very early) the first aortic arch regresses, and the remaining vessel assumes the name of Embryonic (of Fetal) Mandibular artery. The first arch supplied structures related to the pharynx and future facial region. The mandibular artery and its vascular plexus continues this role until its territory is taken over by branches of the primitive hyoid artery (a second arch derivative), which in turn is later annexed by the developing external carotid circulation. A tiny portion of the original embryonic mandibular artery territory may continue to be supplied by the adult version of the Mandibular artery. The Vidian artery develops along with and supplies the Vidian nerve, a sympatheic/parasympathetic derivative of the First Branchial apparatus. The embryologic memory of the MV artery as a first arch derivative explains why, in cases of IMAX hypoplasia or injury/closure, the Mandibulovidian artery supplies portions of the pharynx or nasal cavity.
VIDIAN BRANCH
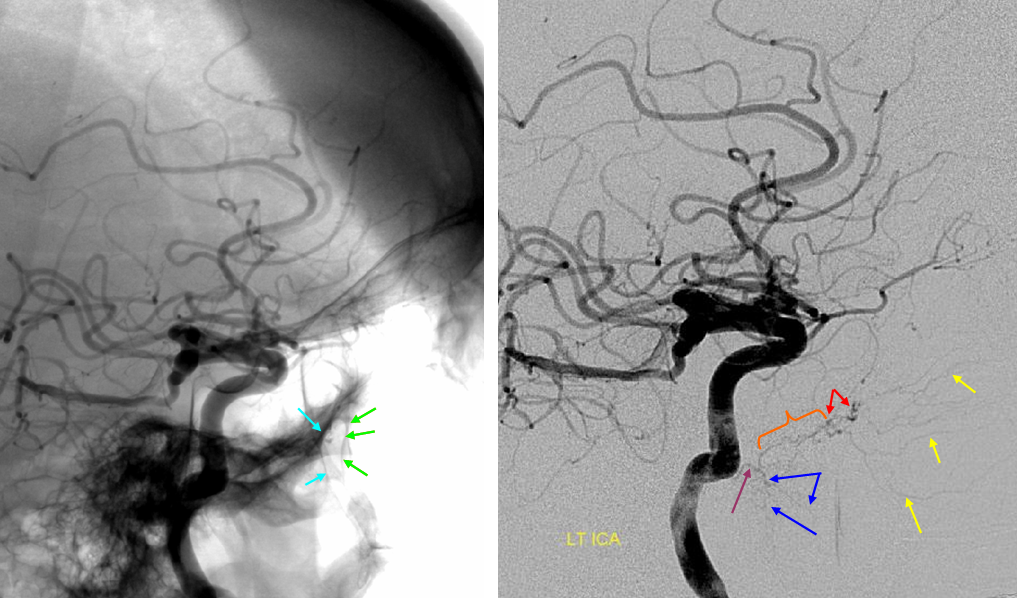
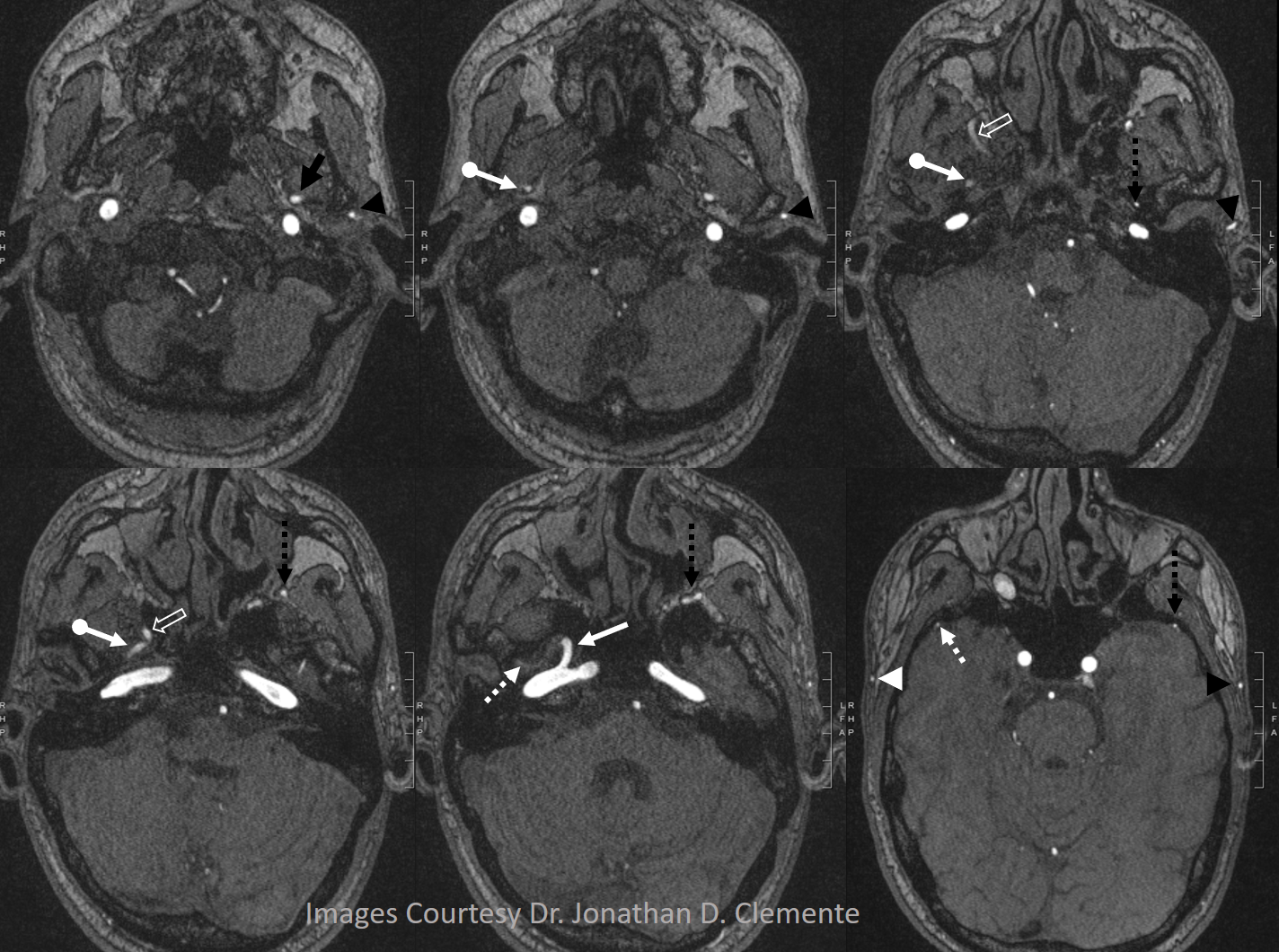
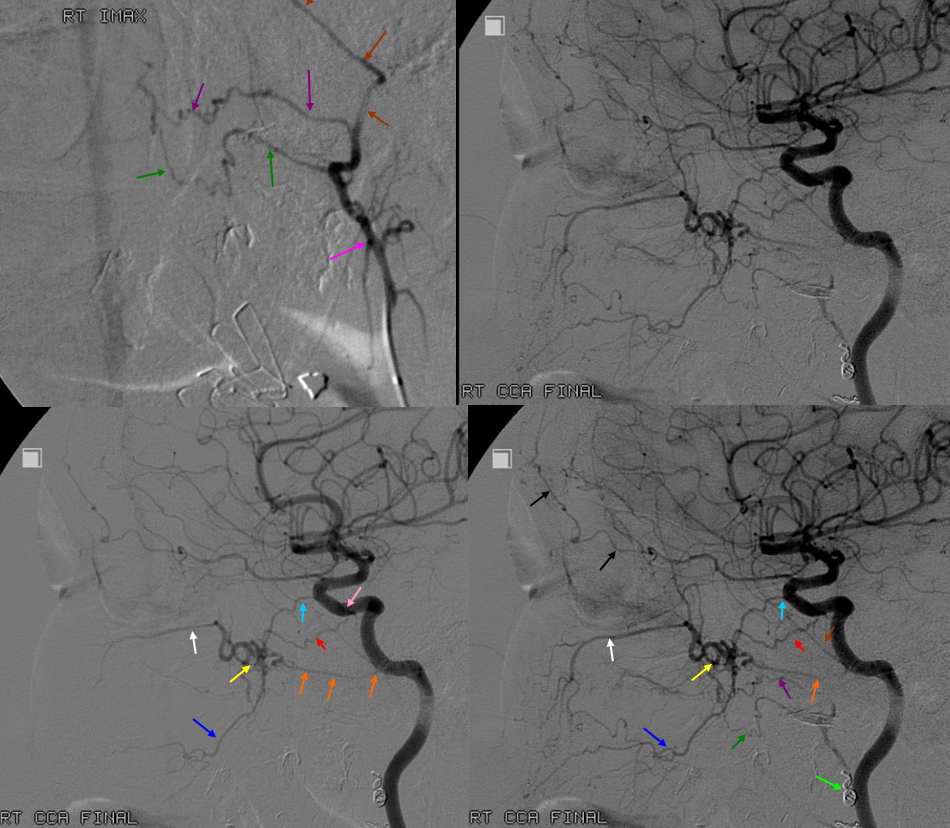
Native and subtraction Lateral (top) and AP (bottom) views of a particularly prominent mandibulovidian artery in absence of pathology. The proximal trunk is labeled in purple. The Vidian artery portion inside the canal is orange and projects above the mandibular portion. The Vidian canal opens into the posterior portion of the pterygopalatine fossa which is a consistent landmark (blue arrows back wall, green arrows front wall). The part in the fossa is marked with red arrows. In this case, the artery supplies extensively the nasal septum (yellow arrows). Typically, the nasal septum is supplied by sphenopalatine artery branches of the IMAX, which in this case is hypoplastic. The mandibular branch is labeled with blue arrows and supplies tissues adjacent to the mandibular condyle.
Vidian IMAX Branch — the more typical origin of the Vidian artery, it projects posterior to the terminal IMAX portion in the pterygopalatine fossa.
The Vidian artery (red) is a small branch projecting posterior to the terminal IMAX. The foramen rotundum branch also projects posterior but would be pointing more rostral towards the cavernous portion of the carotid artery. Notice prominent ethmoidal branches of the ophthlamic artery (purple) and the more typical supply of the nasal septum and turbinates via sphenopalatine branches of the IMAX (yellow)
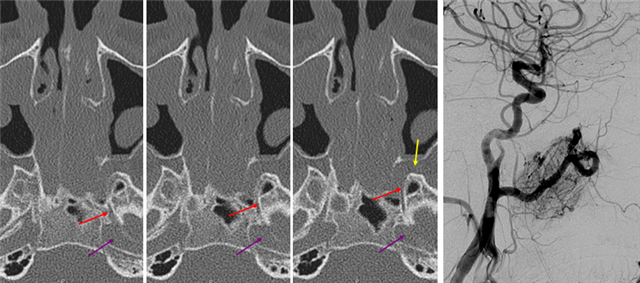
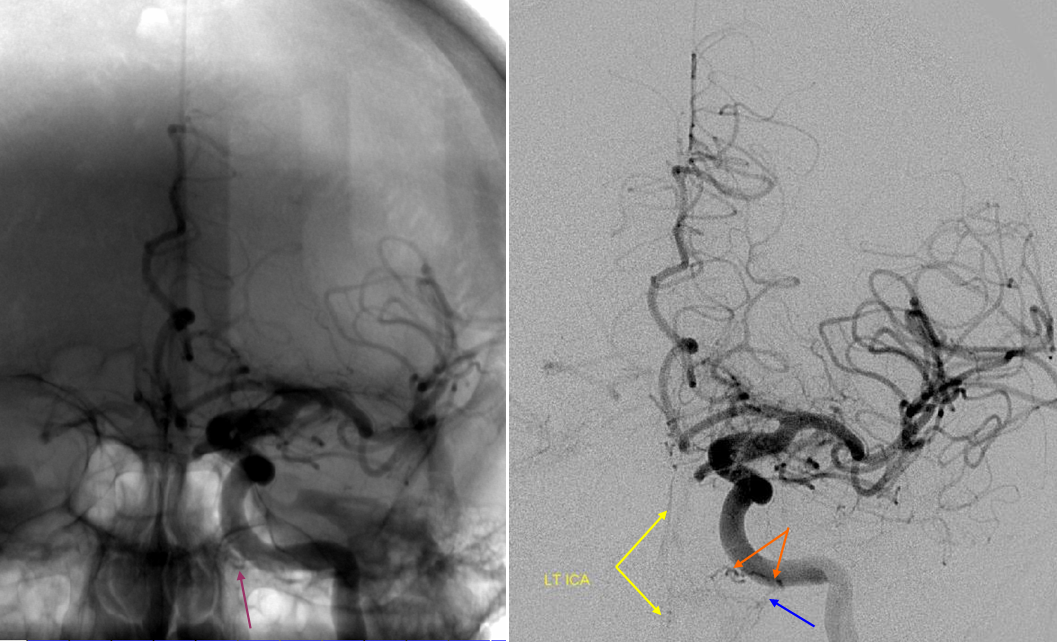
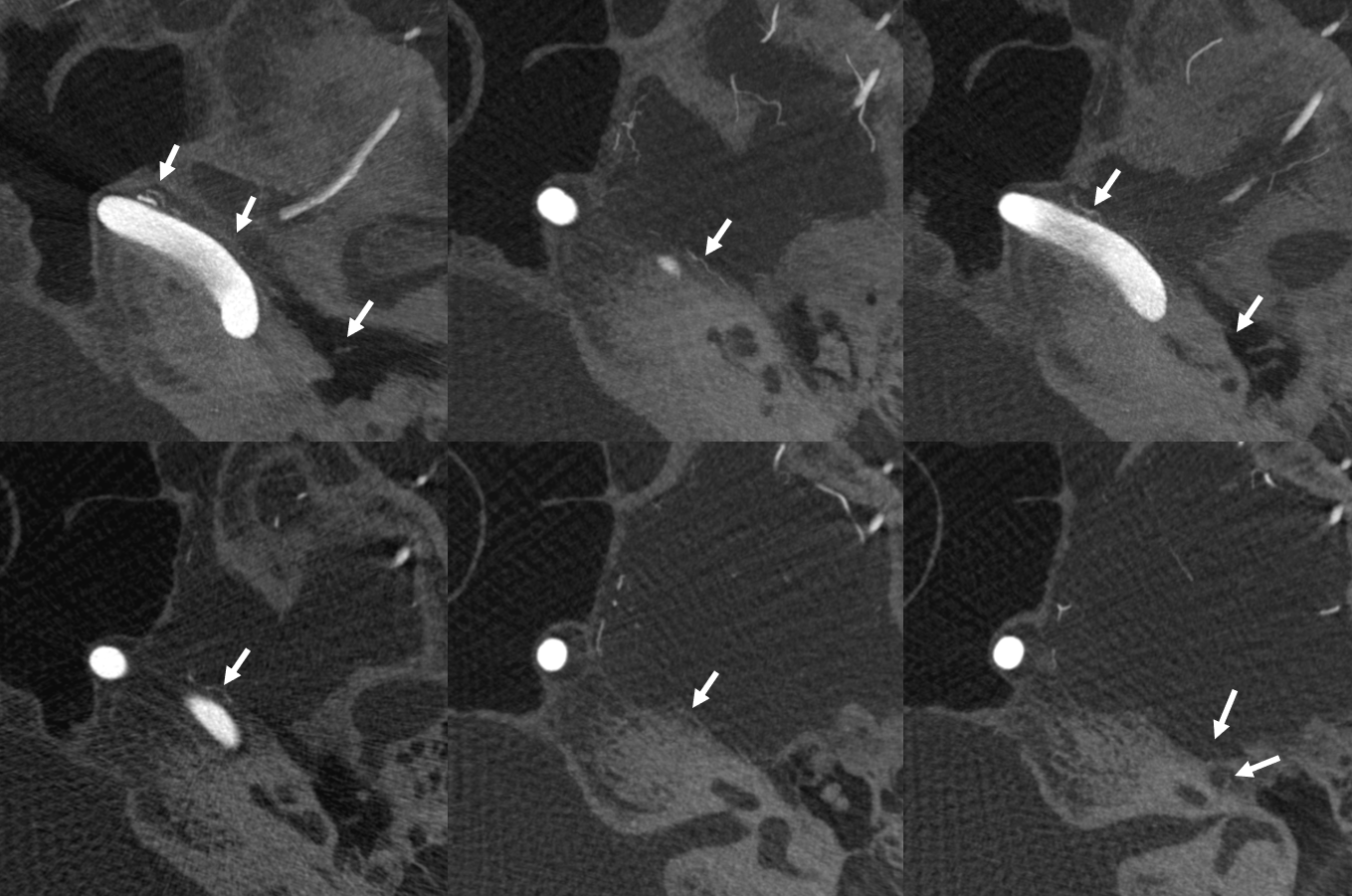
Sequential axial CT images through the Vidian canal (red) connecting the proximal petrous carotid ICA (purple) to the pterygopalatine fossa (yellow). The pterygopalatine fossa on the left is enlarged by a Juvenile Angiofibroma. The vidian artery did not however participate in supply of the lesion, as seen on a pre-operative embolization angiogram (right).
DYNA CT
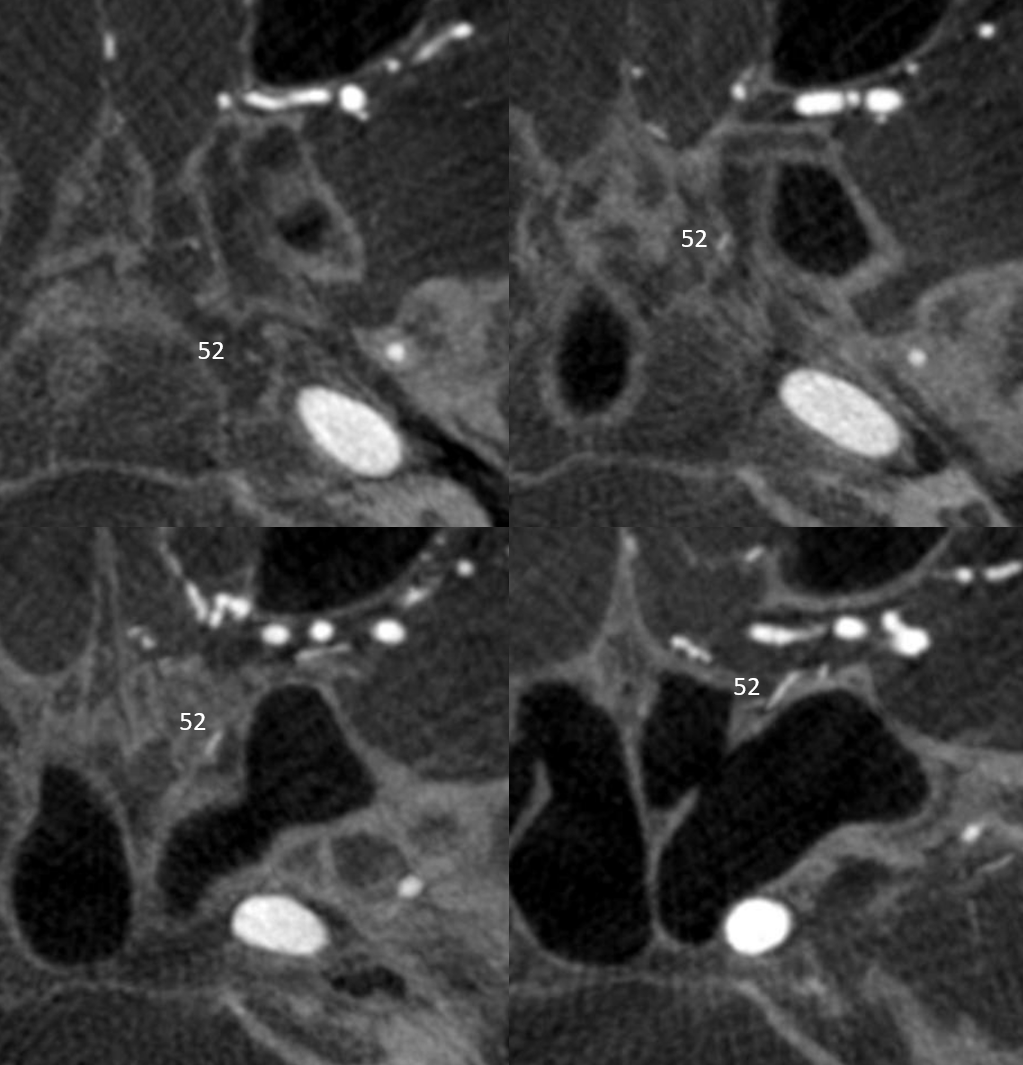
Visualization of this kind of anatomy is greatly aided by flat panel CT such as DYNA CT. Here is an example — vidian artery (52) axial views in vidian canal
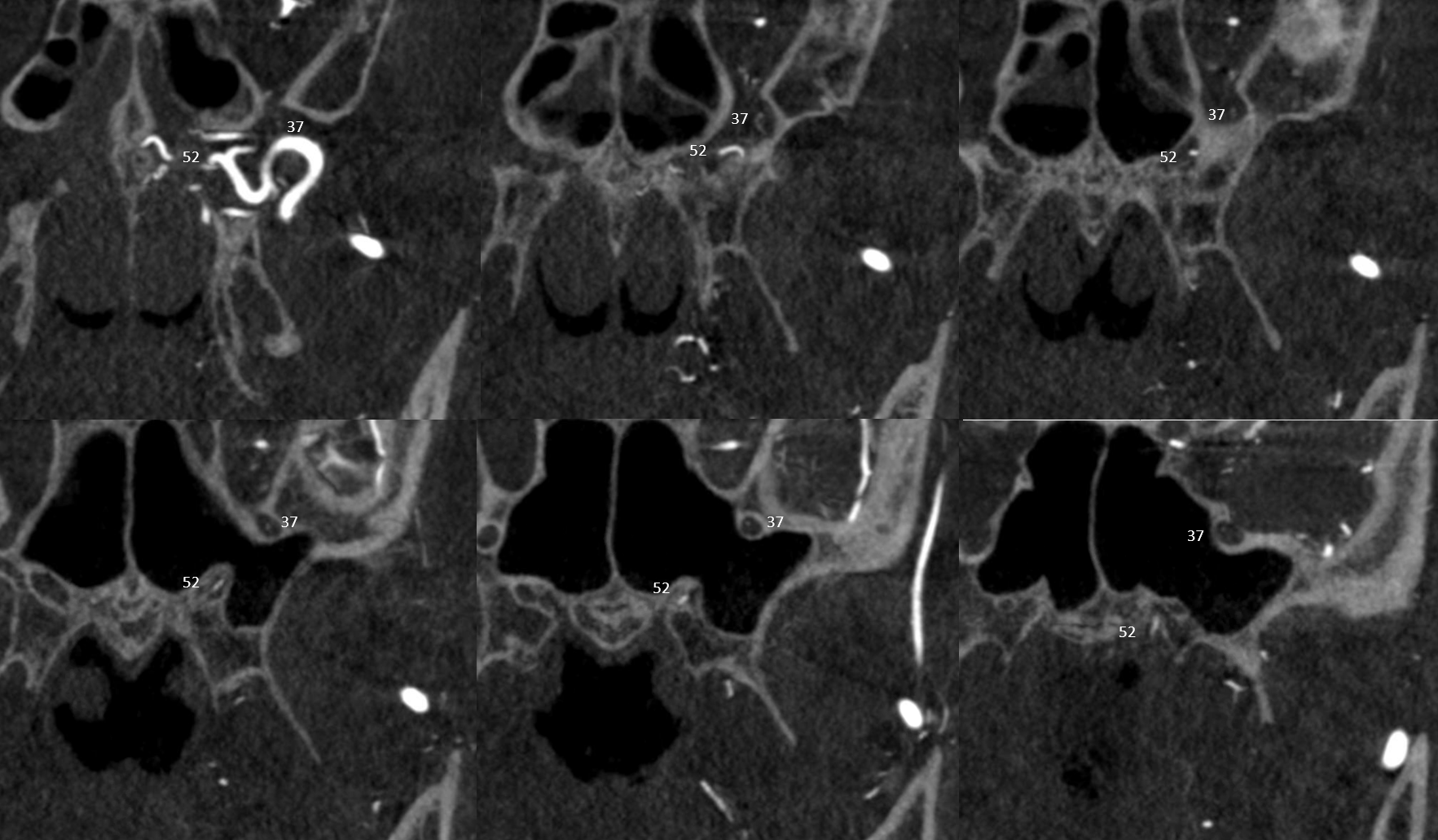
Coronals are better — there is also foramen rotundum artery (37)
Dominant Mandibulovidian artery supplying the posterior nasopharynx — in balance with superior division of the ascending pharyngeal artery pharyngeal trunk, and the extracranial portion of the accessory meningeal artery — tissues around the Eustachian tube opening.

Vidian artery supply of Juvenile Angiofibroma 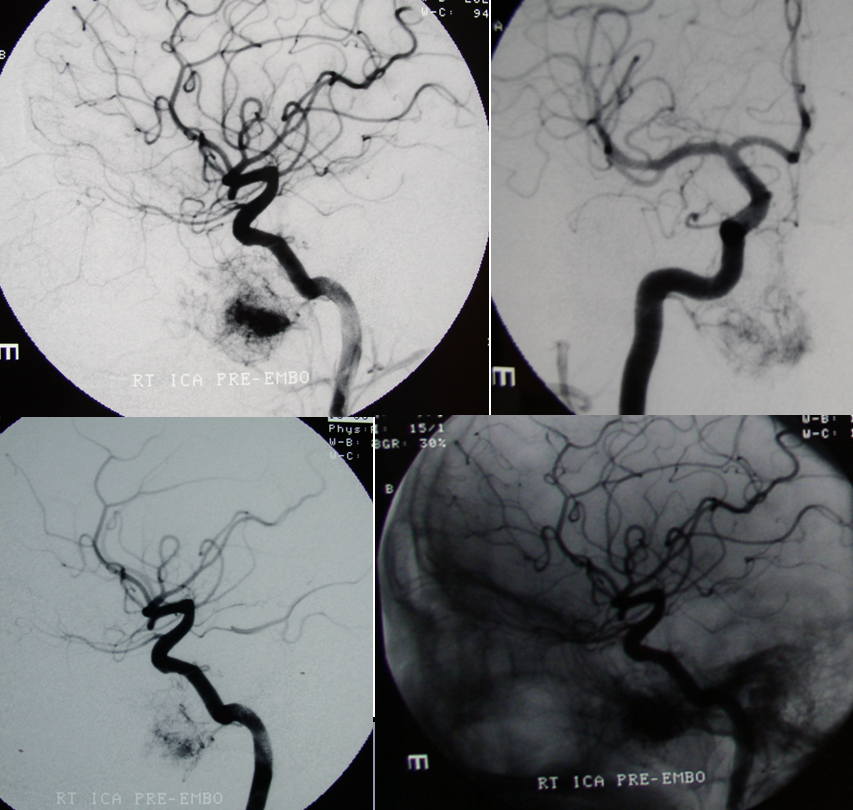
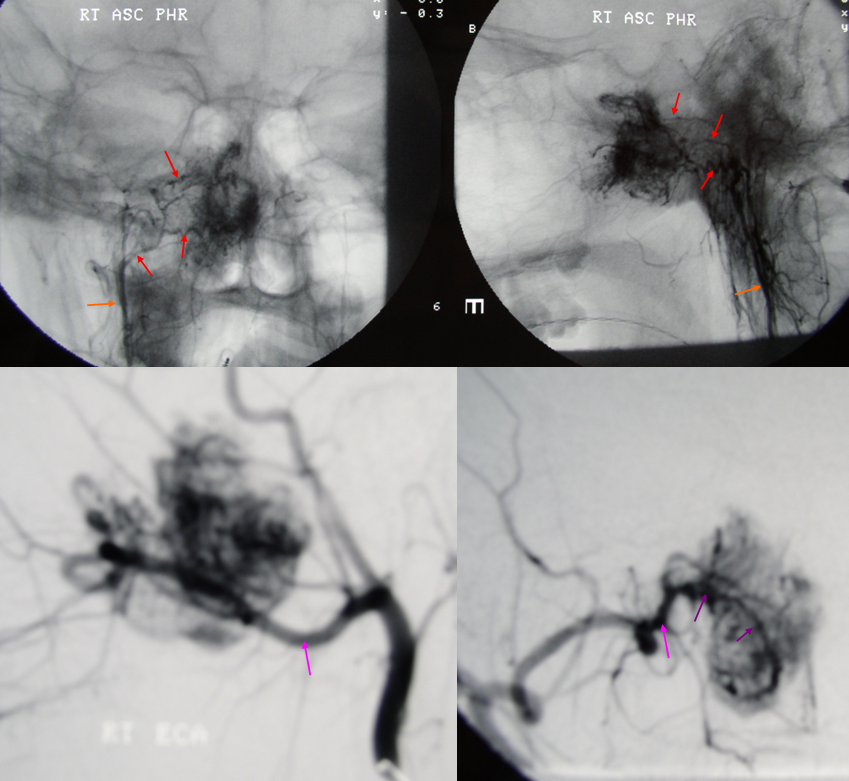
Emergency angiography performed after biopsy of nasopharyngeal mass, a JNA, shows extensive supply from the MV artery. Notice also extensive supply of same tumor via the superior division (red) of the ascending pharyngeal artery (orange) and sphenopalatine branches (purple) of the IMAX (pink)
Another illustration of a prominent Vidian artery (arrowhead) supplying tissues of the nasal cavity and nasopharynx.
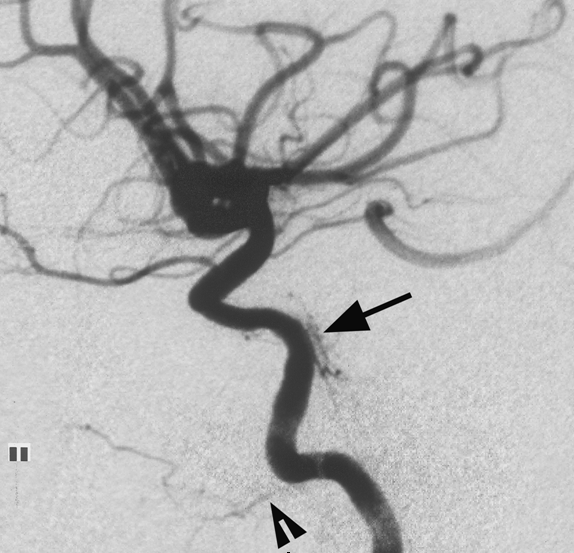
Image courtesy of Dr. Peter Kim Nelson. From: Jason W. Allen, M.D., PH.D., Anthony J. G. Alastra, M.D., and Peter K. Nelson, M.D. Proximal intracranial internal carotid artery branches: prevalence and importance for balloon occlusion test. Journal of Neurosugery 2005; 102(1) 45-52
ICA reconstitution via the Vidian Branch

Ascending Pharyngeal-Vidian Anastomosis
Besides the IMAX, the Ascending Pharyngeal artery, through its superior pharyngeal branch, contributes to supply of the nasopharynx. A demonstration of this relationship is shown here.
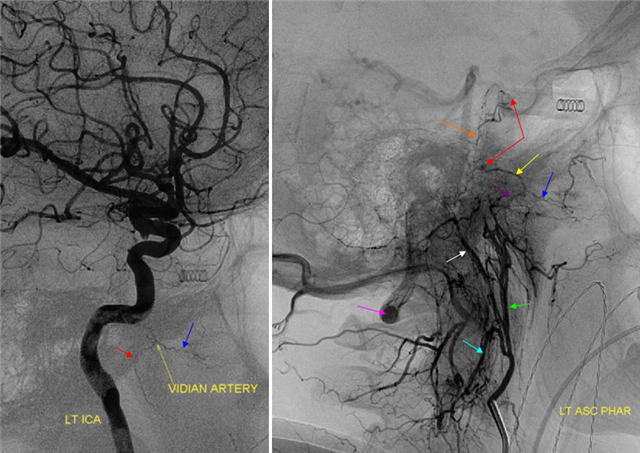
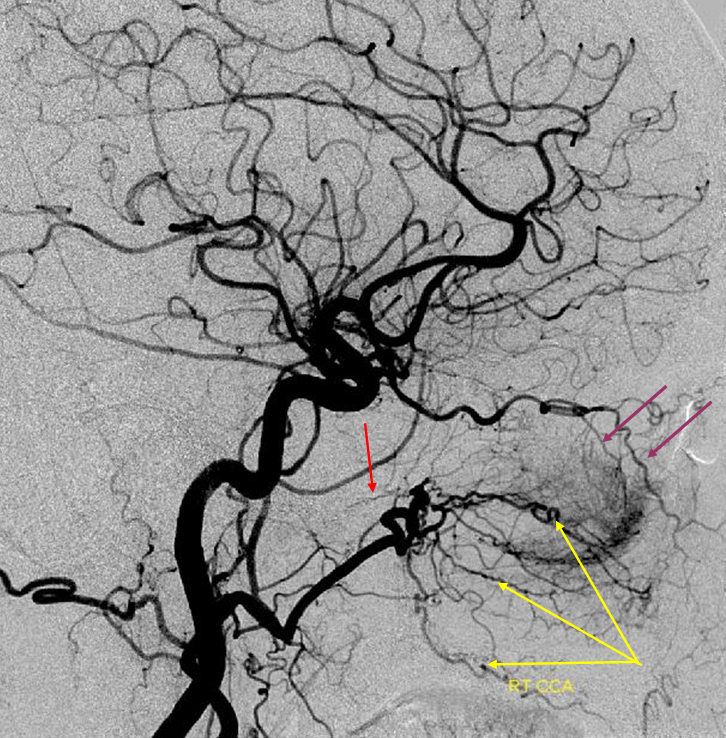
Lateral ICA projection injection (left) demonstrates a Vidian artery. Lateral ascending pharyngeal injection shows a number of very instructive findings. The pharyngeal trunk (green) of the AP, through its superior branch (purple) reconstitutes the vidian artery (yellow) with a faintly seen blush at its point of anastomosis with the ICA (red arrow). Also notice, by way of interest, prominent ascending clival branches (orange) of the hypoglossal division of the neuromeningeal trunk (white) which anastomose with the cavernous ICA at the level of the meningohypophyseal trunk through its inferior clival branches (red arrow, upper). The AP also has a prominent muscular trunk (light blue) which anastomoses prominently with the vertebral artery (purple). See also Ascending Pharyngeal section.
AP injection of the ascending pharyngeal artery of the same case. The Vidian is marked with yellow arrow. Notice also the odontoid arch system, well outlined by the black arrows. This arch arises from the hypoglossal branch (white) of the neuromeningeal trunk.
Ascending pharyngeal to Mandibulovidian Collaterals
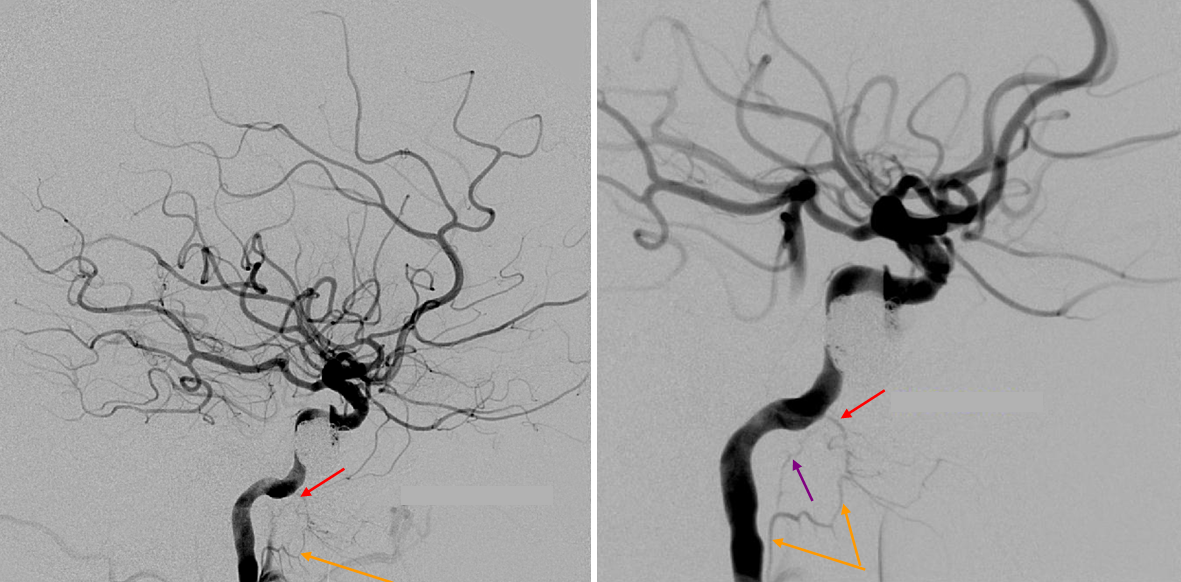
Two lateral views of internal carotid injection demonstrating a mandibulovidian artery (red) collateralizing with superior division of the ascending pharyngeal (orange). The foramen lacerum branch (purple) is also visible.
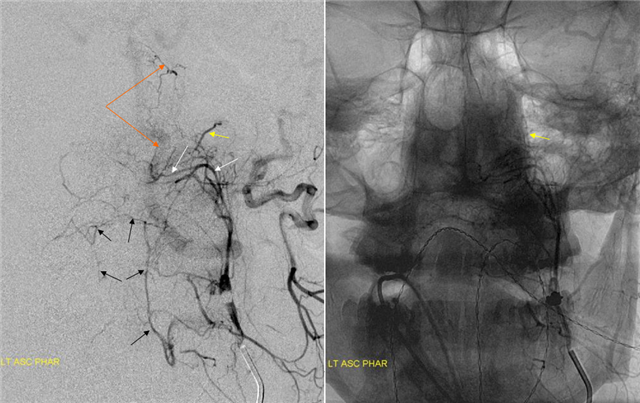
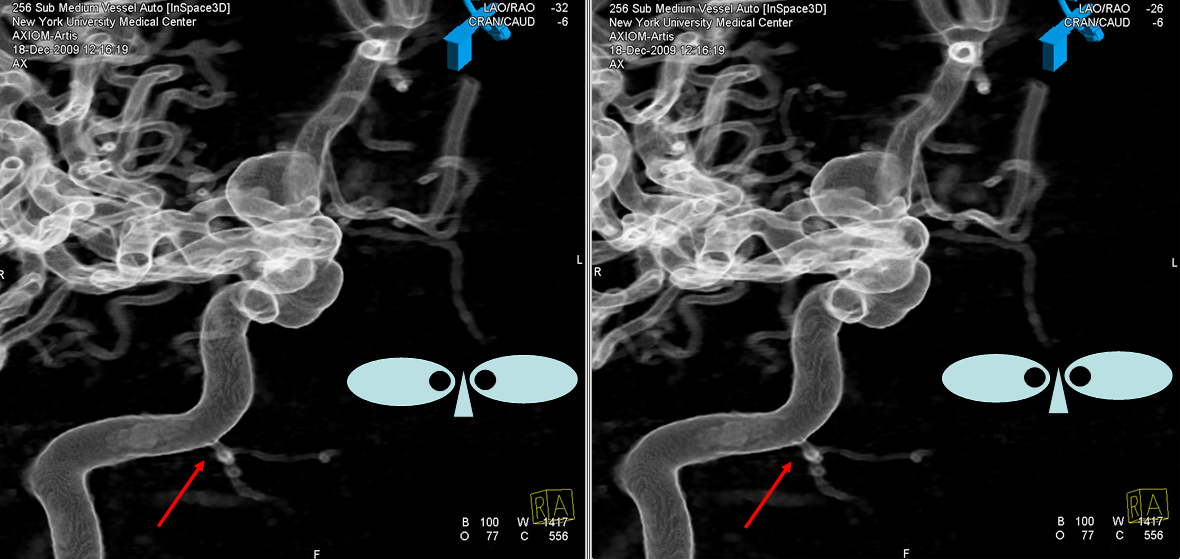
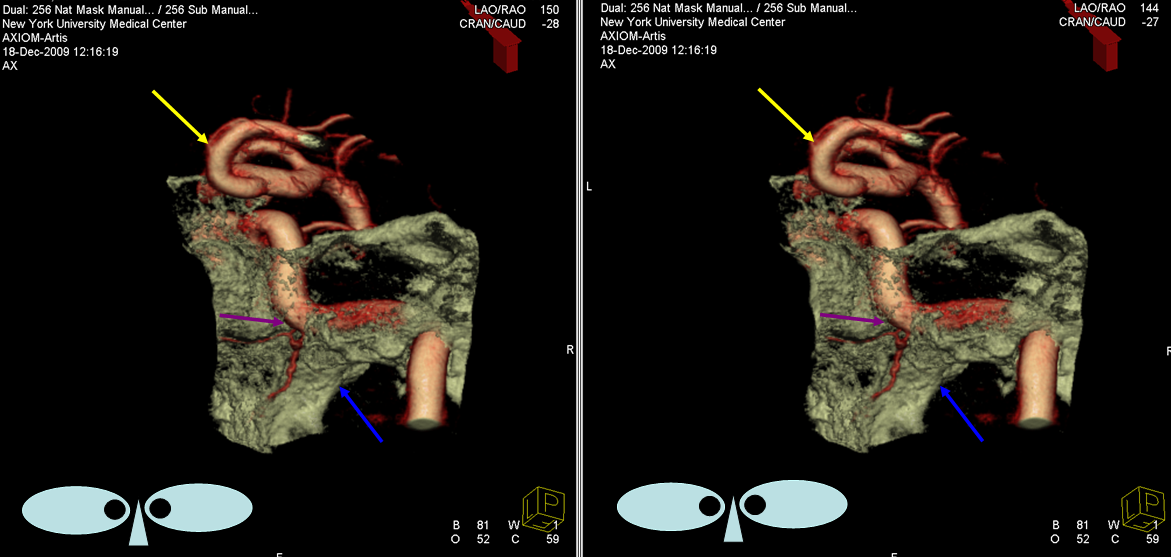
Ascending Pharyngeal-MV collaterals 2: — an even better demonstration of a prominent collateral pathway between the superior division of the AP artery and the MV artery in a patient with intracranial MCA dissection. The flow in the ICA is diminished due to decreased runoff into dissected territory, possibly exagerrating runoff into dural branches — ILT, MHT, and very well seen.
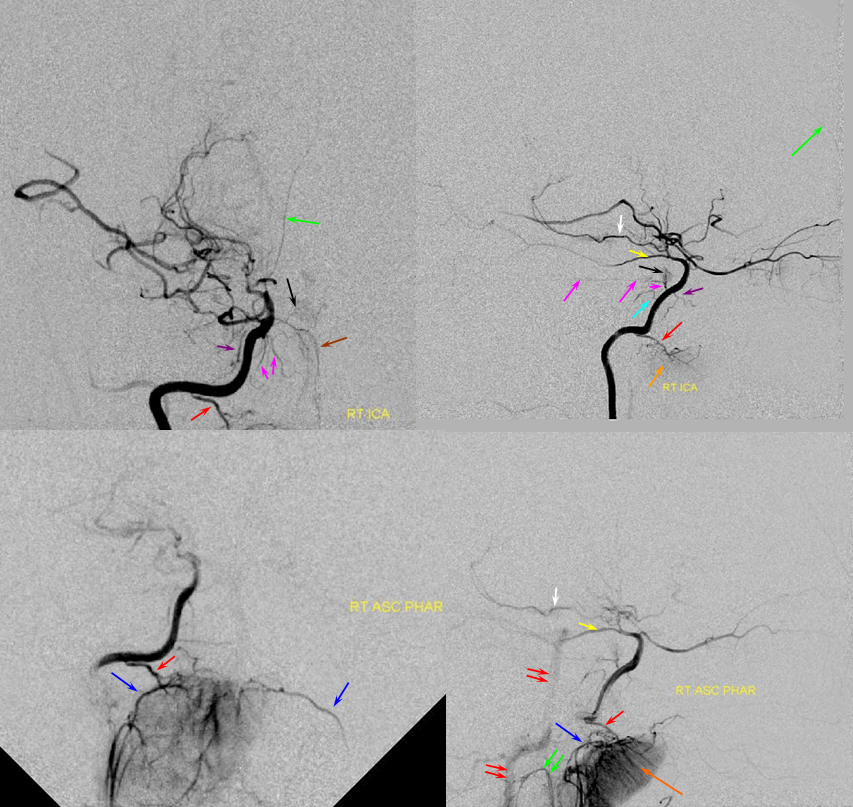
Red=mandibulovidian branch; Orange=mucosal blush of the posterior nasopharynx; dark blue=Ascending Pharyngeal, superior division (contralateral side also visible on the AP ascending pharygeal projection on bottom left); Purple=ILT; Pink=MHT; Black=pituitary blush; Yellow=PCOM; White=anterior choroidal; Green=anterior meningeal (off ophthalmic, origin outside field of view on the lateral ICA projection); Double Green=odontoid arch of the neuromeningeal division of the ascending pharyngeal artery; Double Red=vertebral artery.
Mandibular Branch
A supremely rare variant, supplied by Dr. Jonathan D. Clemente. See Middle Meningeal Artery for much more info on this kind of spectrum. Both MMA and IMAX are supplied by the vidian artery — yes, its not hyostapedial, but is on the spectrum of the same variant. The only case we’ve ever come across. Makes one wonder if the embryology theory is really valid, but here it is.
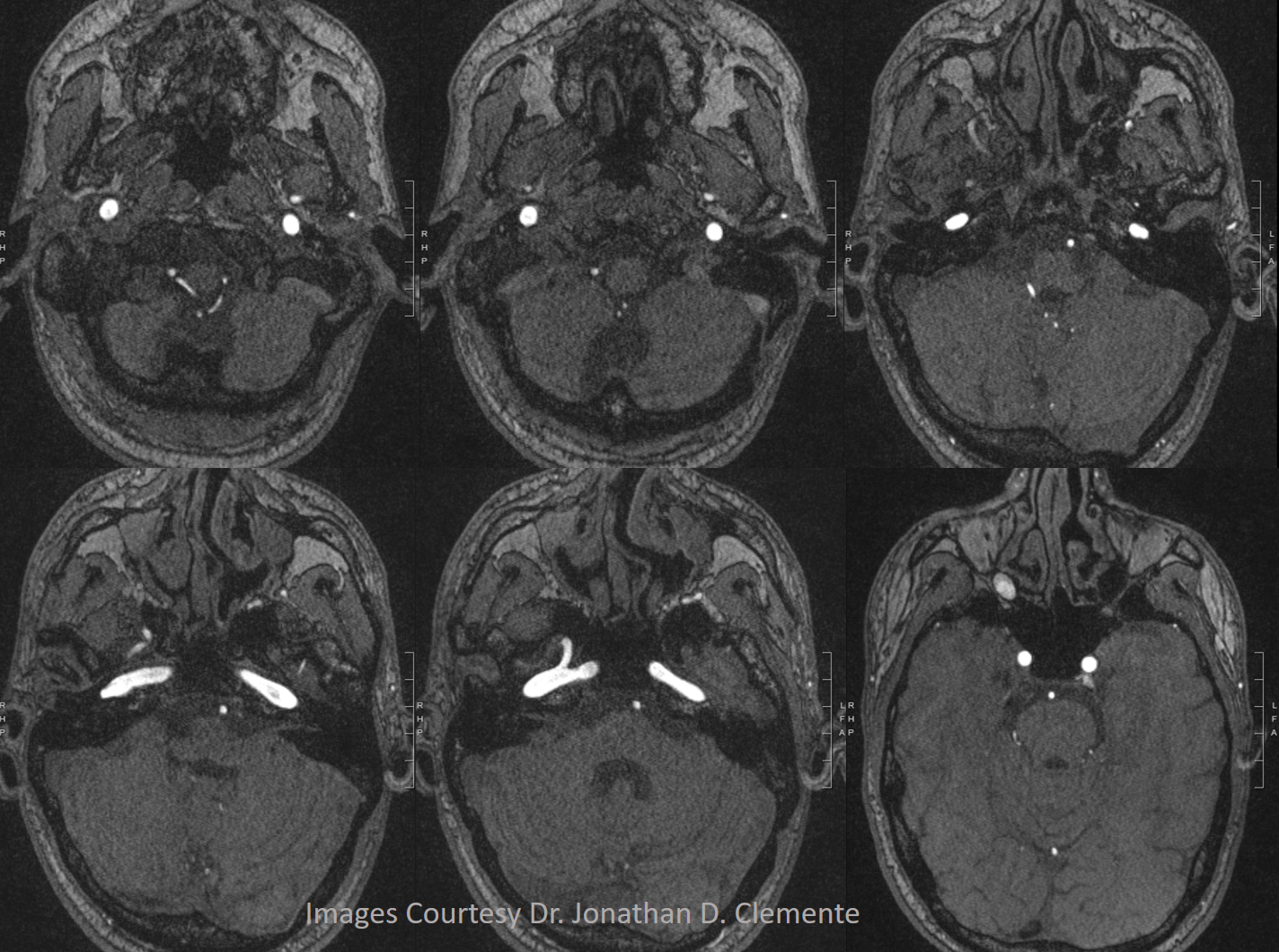
Below is one with arrows. On the normal left side, the IMAX (black arrow), STA (black arrowhead), and MMA (dashed black arrow) are all in usual places. On the right, the vidian artery (white arrow) supplies both proximal (white ball arrow) and distal (open white arrow) IMAX. The IMAX “gives rise” to both MMA (dashed white arrow) and STA (white arrowhead). Not bad, huh!
Volume rendered image of same

Extremely rare — Vidian origin facial nerve / geniculate ganglion supply
Happens…
Movie of same
