Cerebral Venous Sinuses

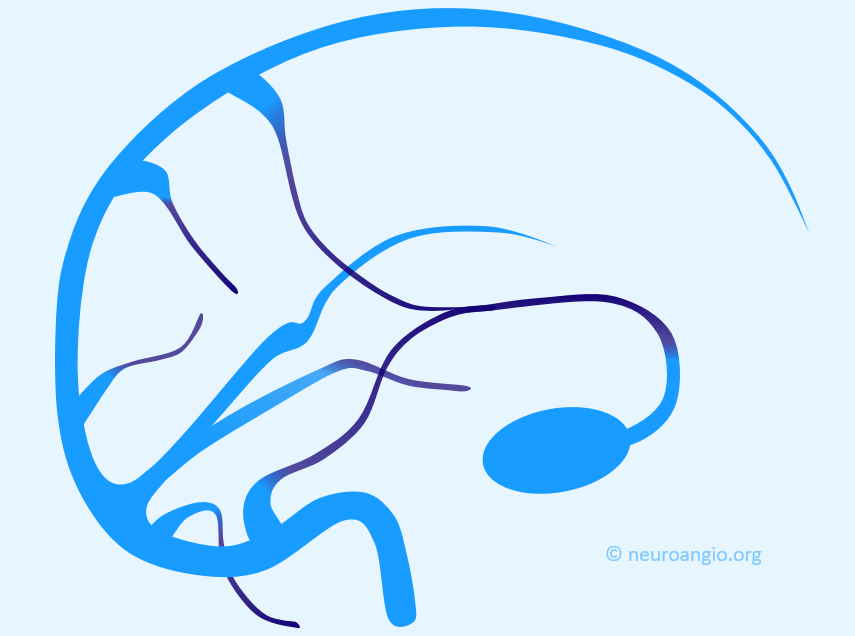
The most important feature regarding venous sinuses, and veins in general, is to keep in mind that veins are like rivers. The size of any vein or sinus is determined by the sum total of the tributaries it gathers, much like a river is exactly as large as the total volume of streams which feed it. Nearly all variations in venous size can be explained by this simple and powerful analogy.
The other point, no less important, is that the entire dura is a “tabula rasa’ for venous flow. Apart from the usual sinuses we will discuss, this page illustrates a tremendously rich spectrum of dural venous channels. The more one thinks of the dura not reading the book on where the classic sinuses should be, the easier comprehension of variants becomes and the better the complete venous picture is understood.
The main sinuses are well known. The superior sagittal sinus is nearly always present but can be variable in its anterior extent; its hypoplasia may be associated with dominance of the cavernous sinus draining the frontal lobes, prominence of normally small inferior sagittal sinus or large emissary veins — remember the rivers analogy. Often the SSS divides before reaching the torcula, an anatomical variant of no clinical significance but sometimes leading to unnecessary imaging to “conclusively” rule out an imaginary thrombus. The frequent variations at the torcular region bear witness to its late embryologic formation from the primordial venous plexus, substantially after the anterior and middle sinus have been formed.
The inferior sagittal sinus is smaller and inconstant. It usually collects tributaries from corpus callosum and cingulate gyrus regions, and drains into the straight sinus.
The transverse sinuses are often asymmetric, the left being more often hypoplastic than the right (pulsations of the right atrium are thought to be responsible for larger capacity of the right jugular system) The jugular foramen on smaller side is correspondingly small as well, helping distinguish developmental hypoplasia from acquired thrombosis.
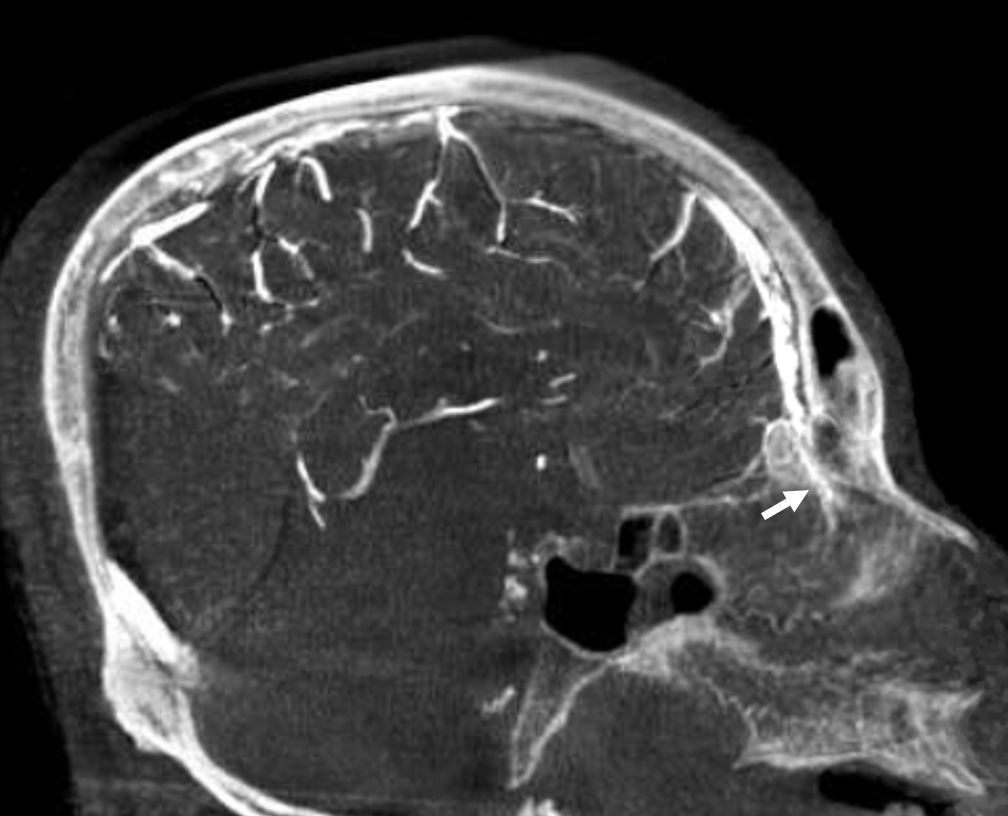
The sigmoid sinuses are not always of the same caliber as the transverse ones, especially when a large vein of Labbe empties into the proximal sigmoid sinus to enlarge it substantially as compared with its transverse tributary. Extensive emissary veins (mastoid, occipital, condylar) often drain in part and occasionally in toto the transverse-sigmoid sinus complex, and the corresponding jugulars may be hypoplastic. Isolated findings of this nature are rarely due to consequences of pathologic shunting, and looking on bone windows for emissary channels can confirm this as a non-pathologic anatomical disposition.
The cavernous sinus collects extensive drainage and sports multiple egress routes. It has multiple compartments and may in fact be regarded, at least functionally, as a collection of separate entities. Not seeing it on an ICA injection does not mean its not there — only one compartment is hypoplastic. Embryologically, although the cavernous sinus is a very early structure, in its earliest form it does not seem to participate in the drainage of the brain — rather collecting tributaries of the future orbital/ophthalmic veins, facial and sphenopalatine systems. Even in the newborn, the connections between sylvian and basal venous systems and cavernous sinus are usually rudimentary– maturation of these connections is one mechanism which allows for stabilization of venous drainage in infants affected by high flow shunts such as some Vein of Galen Malformations, according to Lasjaunias. The developmentally late capture of the cavernous sinus by Sylvian and basal veins explains the marked variability in the extent of such capture in adults, while the ophthalmic vein to cavernous sinus connection is essentially constant.
The sphenoparietal sinus runs along the ridge of sphenoid lesser wing and collects tributaries of the Sylvian veins to empty into the cavernous sinus. Embryologically, a sinus by that name does exist, collecting the venous drainage of the very thin cortical mantle (future superficial sylvian veins), and directing it from the sphenoid area towards the sigmoid sinus, underneath the temporal lobe. This sinus usually disappears in the adult, except for some very rare instances. The very proximal portion of it appears to persist and connect to the cavernous sinus, however it is not clear whether this is in fact the case and if, instead, another channel does not run along the sphenoid ridge. Some believe this sinus in fact does not exist, and Sylvian veins drain directly into the cavernous sinus (See Cavernous Sinus page)
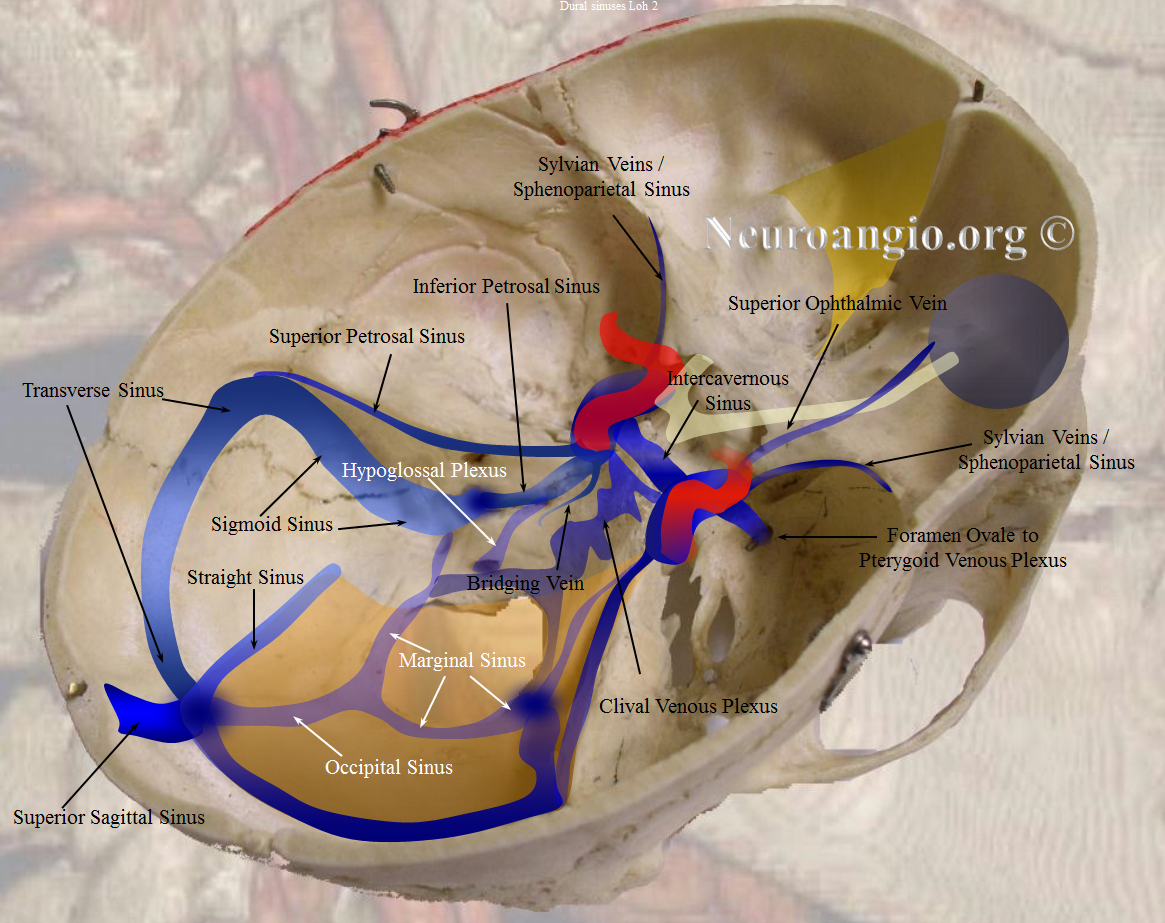
The superior petrosal sinus runs along the petrous ridge from cavernous to the sigmoid sinus. Inferior petrosal sinus runs down the petrous pyramid towards the jugular foramen or, more precisely, towards the very distal extra-cranial jugular vein.
An inconstant, in the adult, and more likely present than absent in the child, occipital sinus drains inferior from the torcula towards the marginal sinus which loosely surrounds the foramen magnum, to exit through it into suboccipital veins, perivertebral venous plexus, or around magnum to the jugular foramen.
Some sinuses are present less commonly than others: the more uncommon ones are labeled in white. The superior and inferior sagittal sinuses are not shown to full extent for clarity. Note how the sphenoparietal sinus runs along the edge of the lesser sphenoid wing, and superior petrosal sinus follows the petrous ridge. Most people have quite asymmetric sinuses.
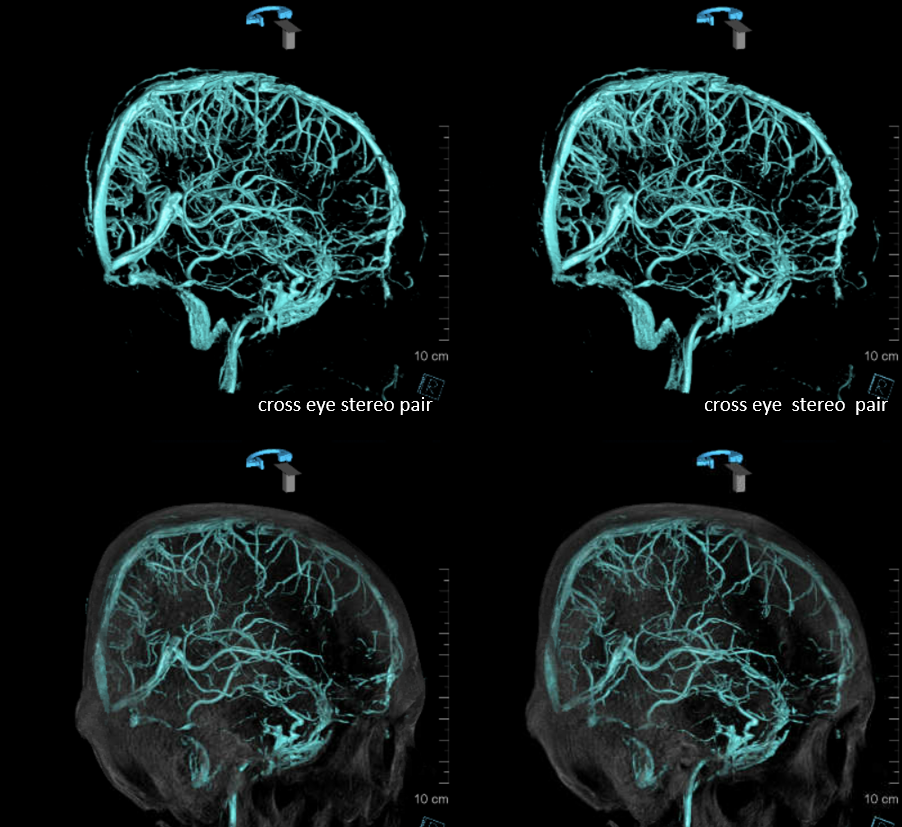
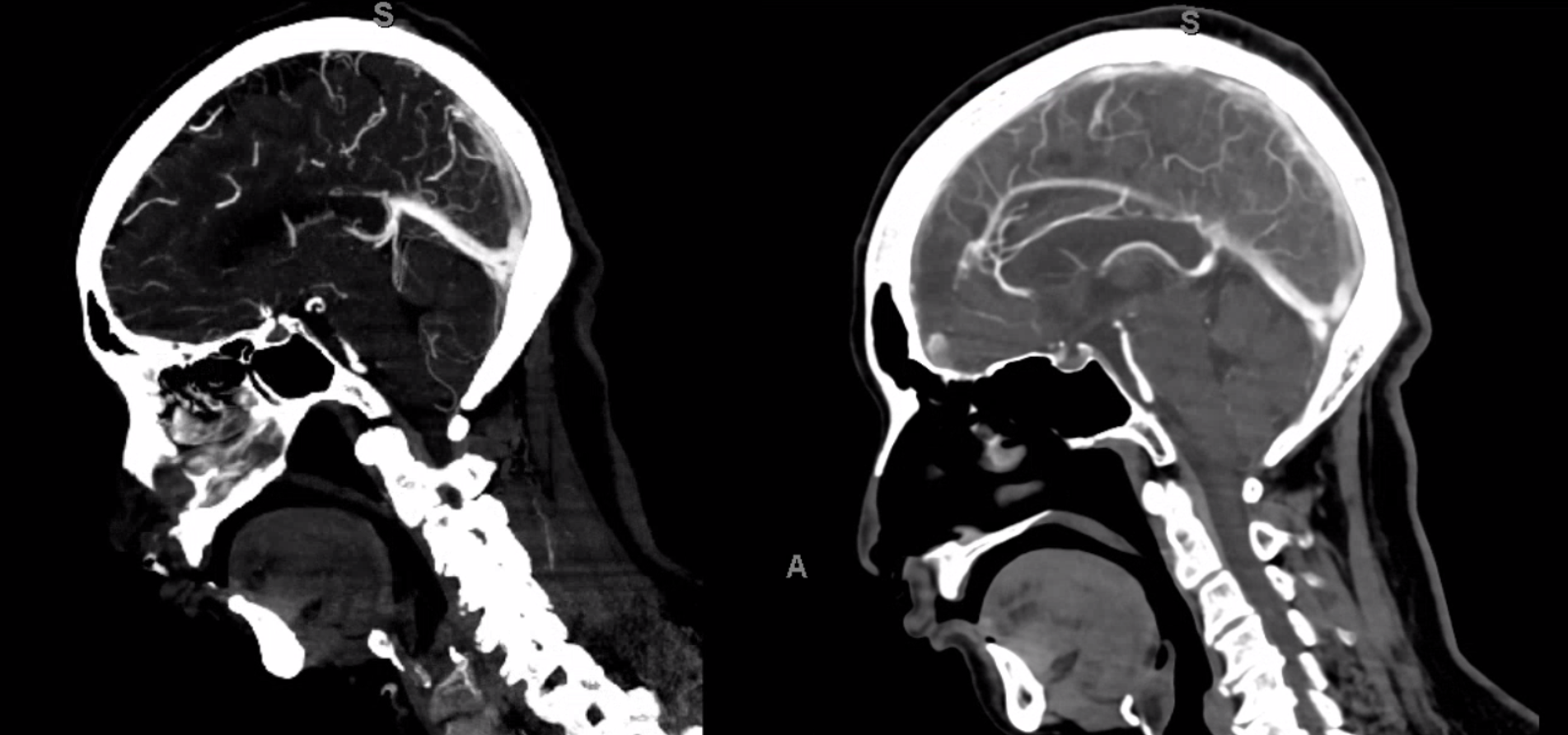
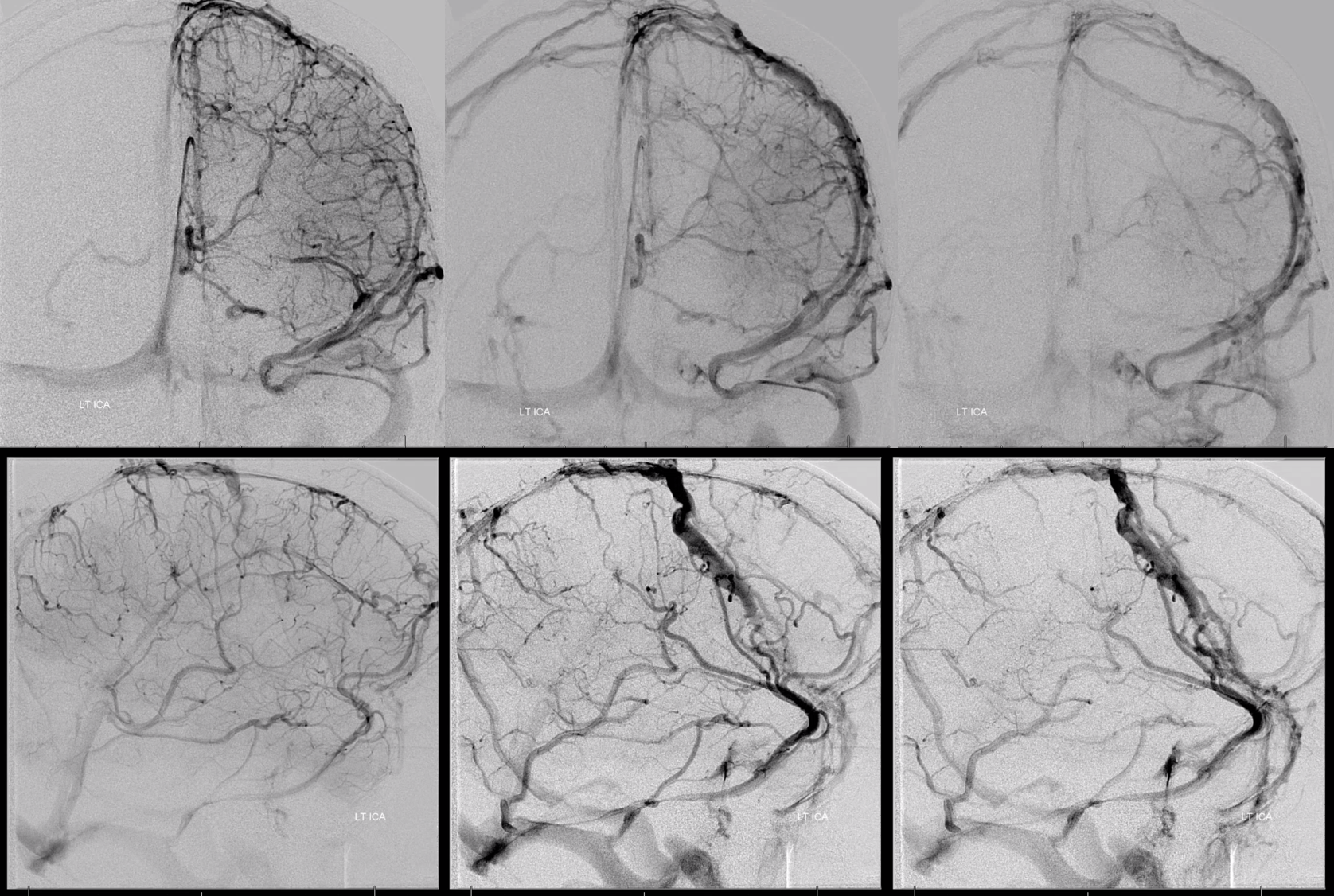
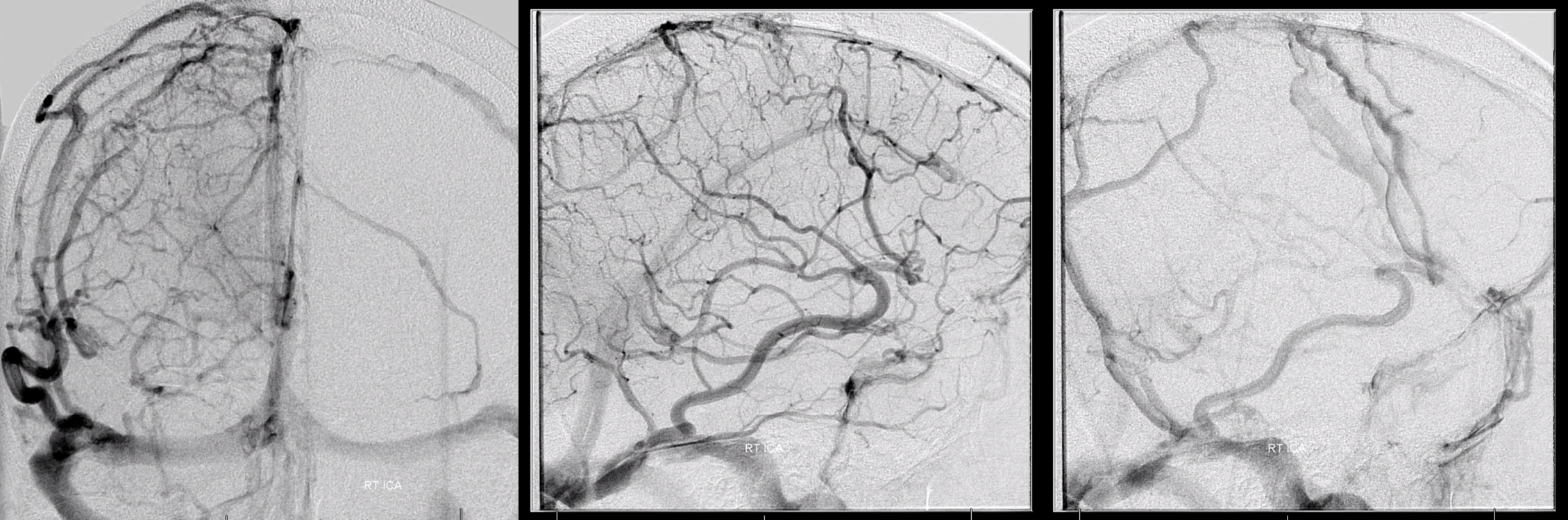
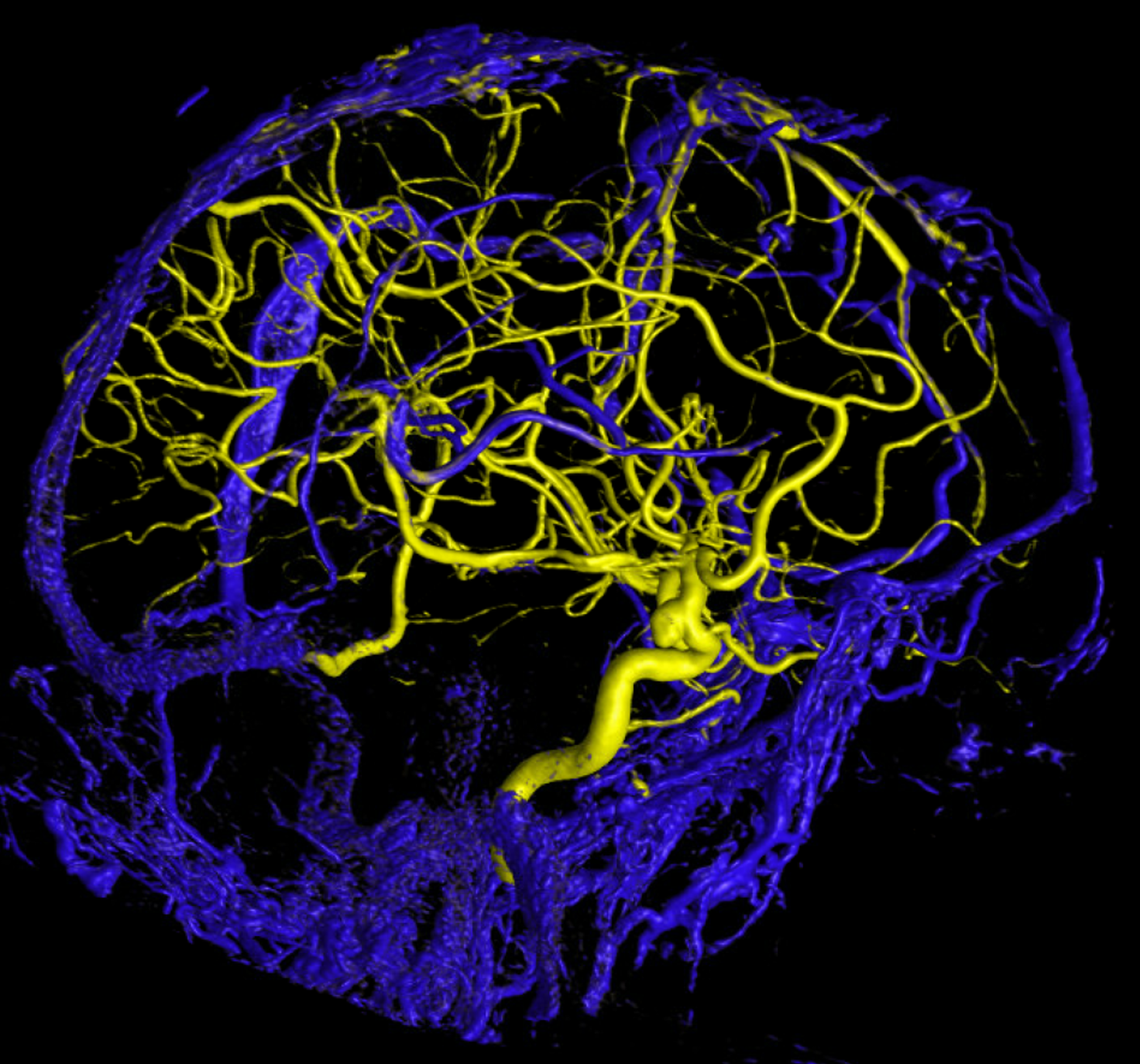
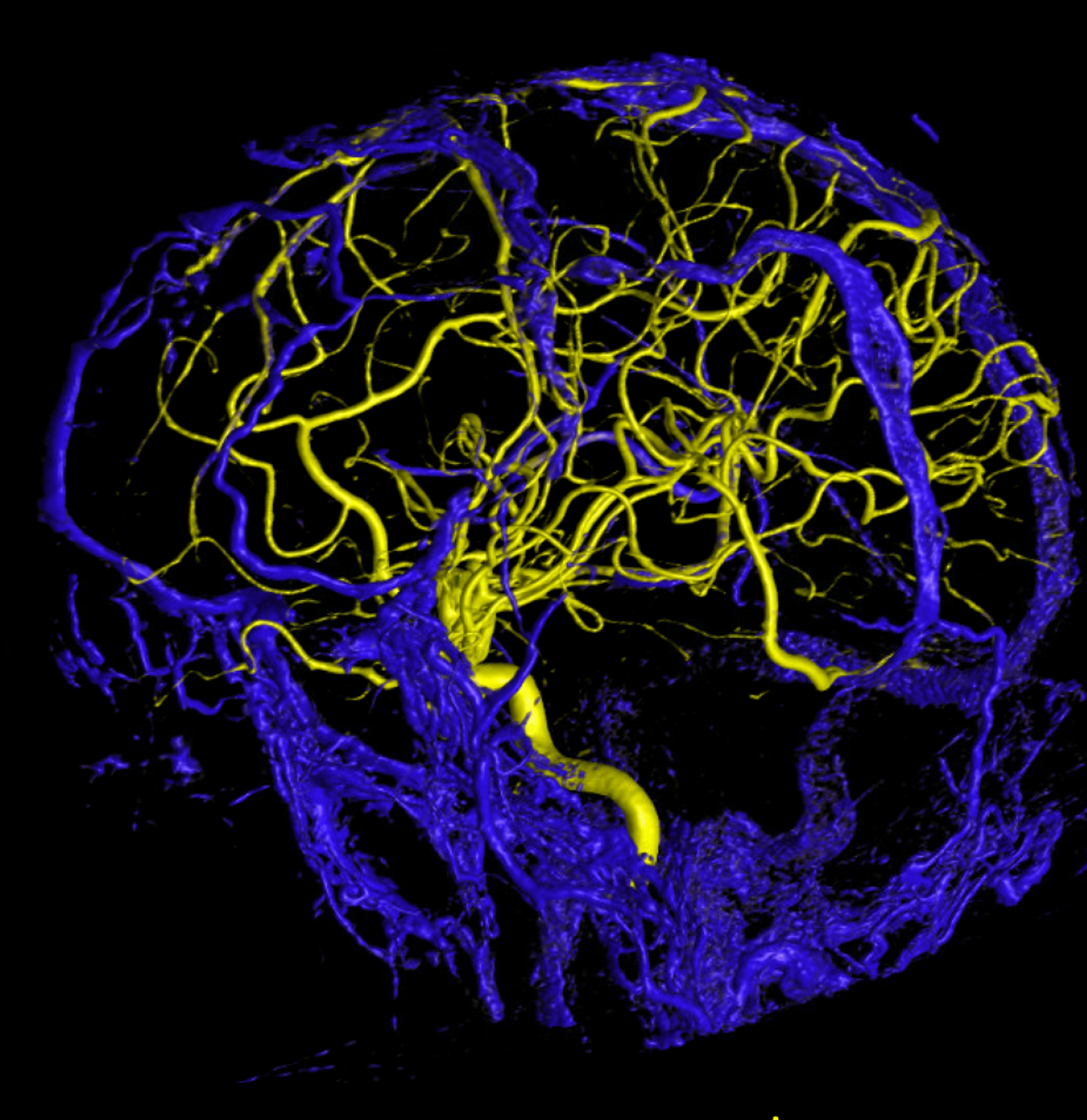
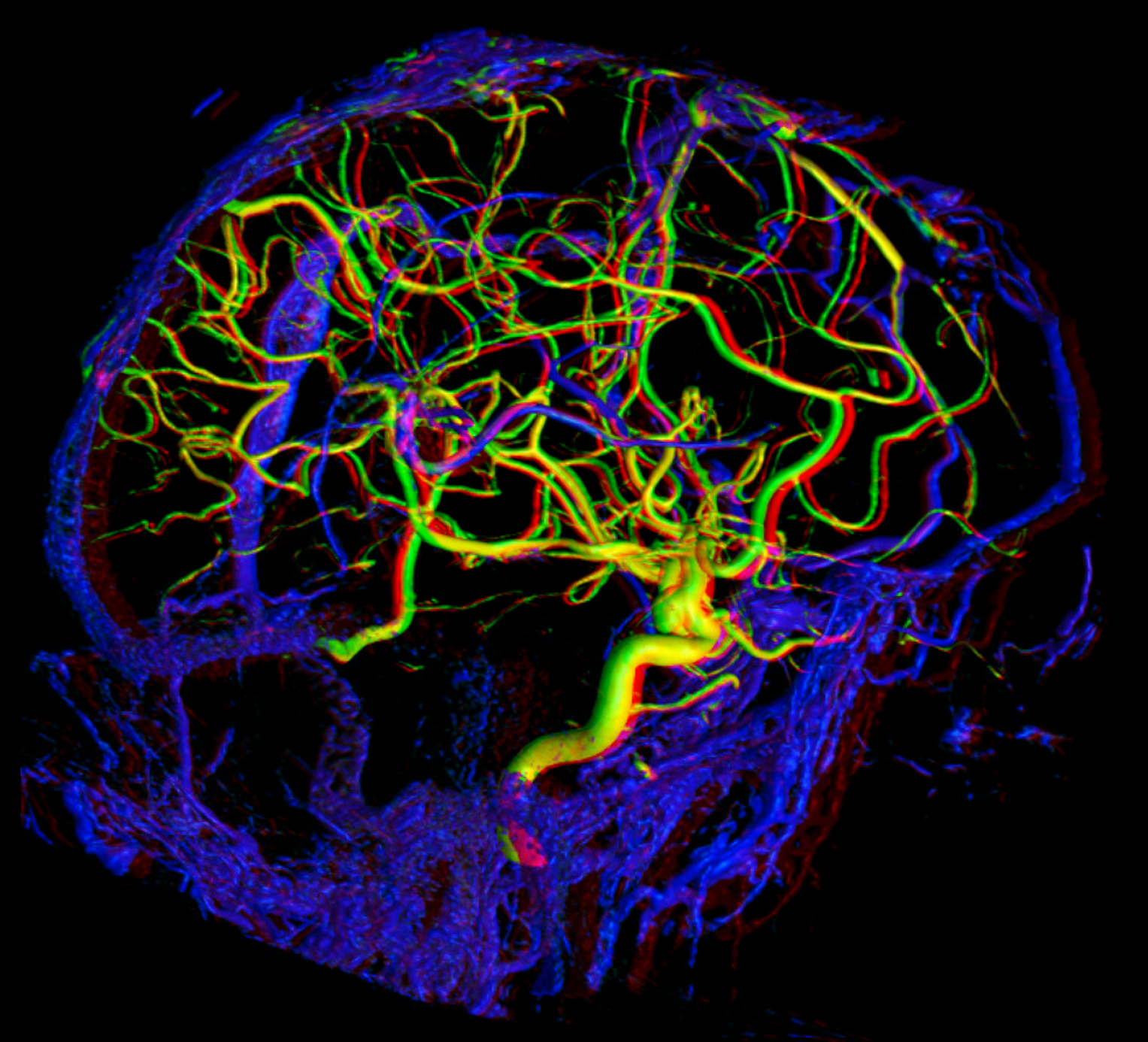
Below are some volumetric images, before we dive in
Pause movies to scroll thru individual frames
Superior Sagittal Sinus
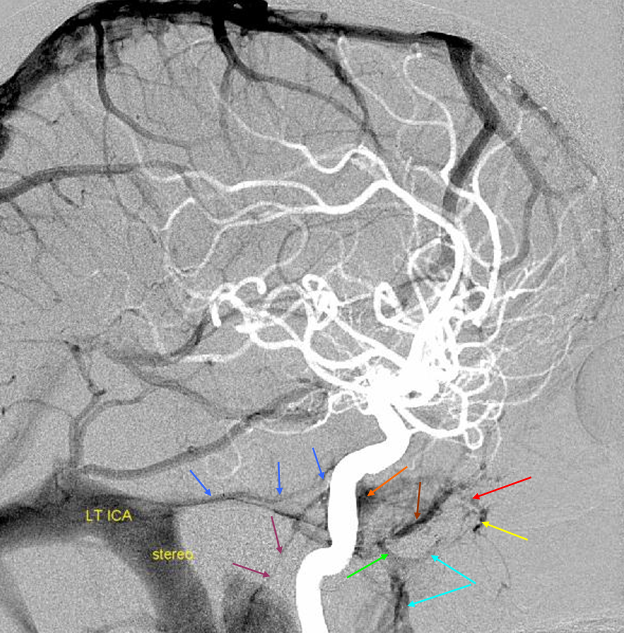
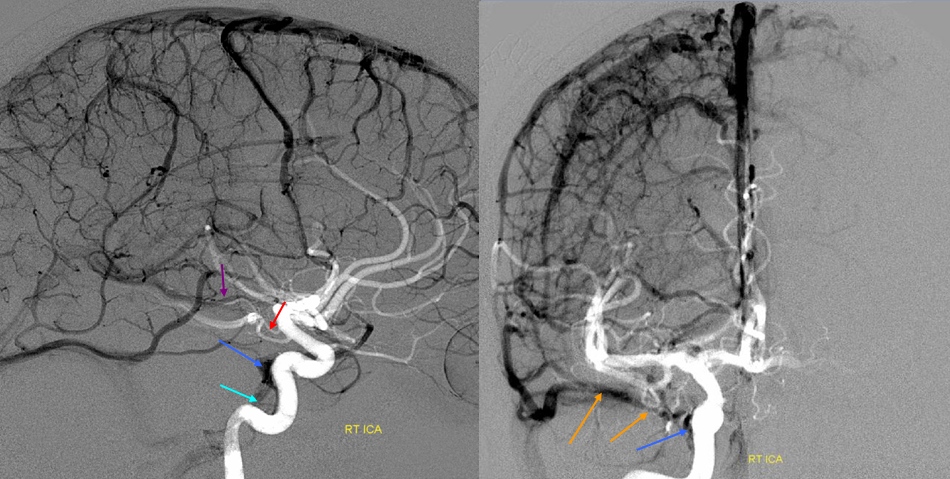
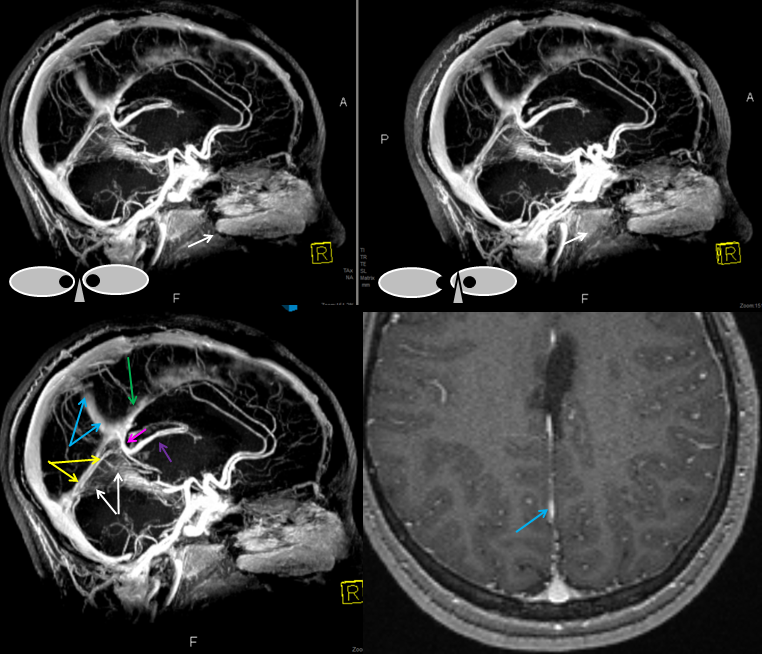
The superior sagittal sinus is a more variable structure than is generally assumed from straight-as-an-arrow diagrams. Although traditionally a single channel spanning the midline and terminating at the torcula, in practice you are likely to see additional dural channels, particularly in the posterior portion of the sinus, usually connecting with the transverse sinus system somewhat off midline. Often the sinus is deviated to the side, again over the occipital region. This is most noticeable on angio or stacked MIP images, as midline deviations when viewed sequentially on cross-sectional imaging are not as impressive. There is no particular clinical significance to this. But, it goes to show, as we emphasize in many places, that any part of dura can be a sinus. It does not have to be exactly where the falx joins. It does become important in surgical planning occasionally, and may play a role in evolution of sinus thrombosis cases (there are reports of “recanalization” of falcine sinus and other dural sinuses in patients with sagittal sinus thrombosis. Ultimately, these additional channels underline the evolution of dural sinuses, which are formed by coalescence of multiple channels, some of which can persist. In the patient below, the posterior portion of the SSS is particularly grotesque, with additional left (yellow) and right (pink) dural channels. The “true” SSS is in purple. The torcula is orange. Notice also a vein (green) which may appear like a dural sinus channel. However, it is only visualized from the left injection and is therefore unlikely to be a sinus.
Superior sagittal sinus angulation: It is extremely common to see the SSS angulated with respect to midline. Here, a small midline dural channel (blue) leads to the torcula proper (pink), while the “main” SSS (red) is deviated to the right. Which is the true torcula here is a matter of semantics; the important point is to recognize the arrangement.

Another example of superior sagittal sinus angulation / off midline location
Another example — on angio and MRI — a volumetric post-contrast T1 is super great for venous visualization.
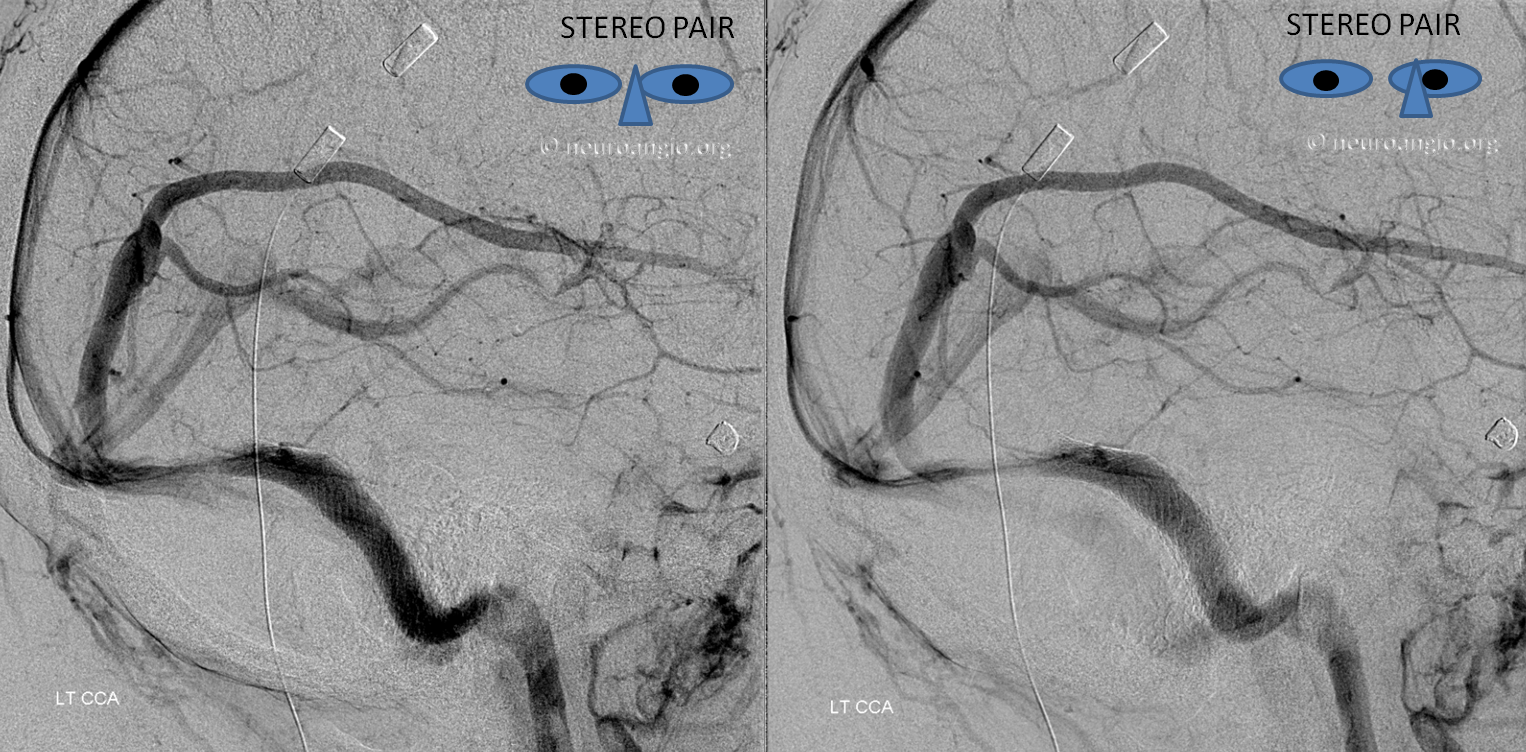
Fenestration of the proximal right transverse sinus, in stereo
Hypoplasia of the anterior aspect of the SSS with frontal convexity veins running along the parasagittal plane to empty into the more posterior part of the SSS. No special significance except that there is a surgical dictum which allows sacrifice of the anterior / distal third of the sinus without too much care about venous infarction. It is a stupid dictum that has led to a number of preventable infarcts in cases where the anterior sagittal sinus is essential. When a large frontal vein draining into the anterior part of SSS, the SSS cannot be sacrificed with impunity (see below)
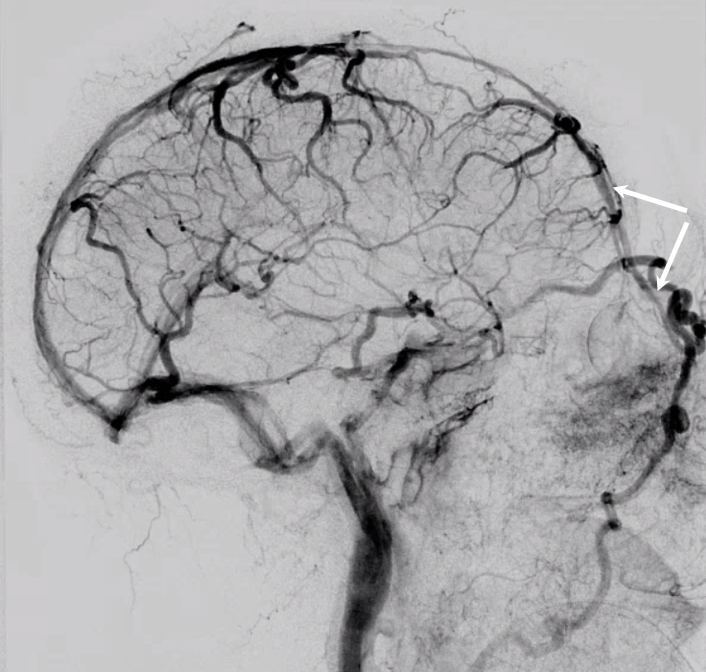
DANGEROUS VARIANT — Functional anterior portion of superior sagittal sinus — a dangerous variant
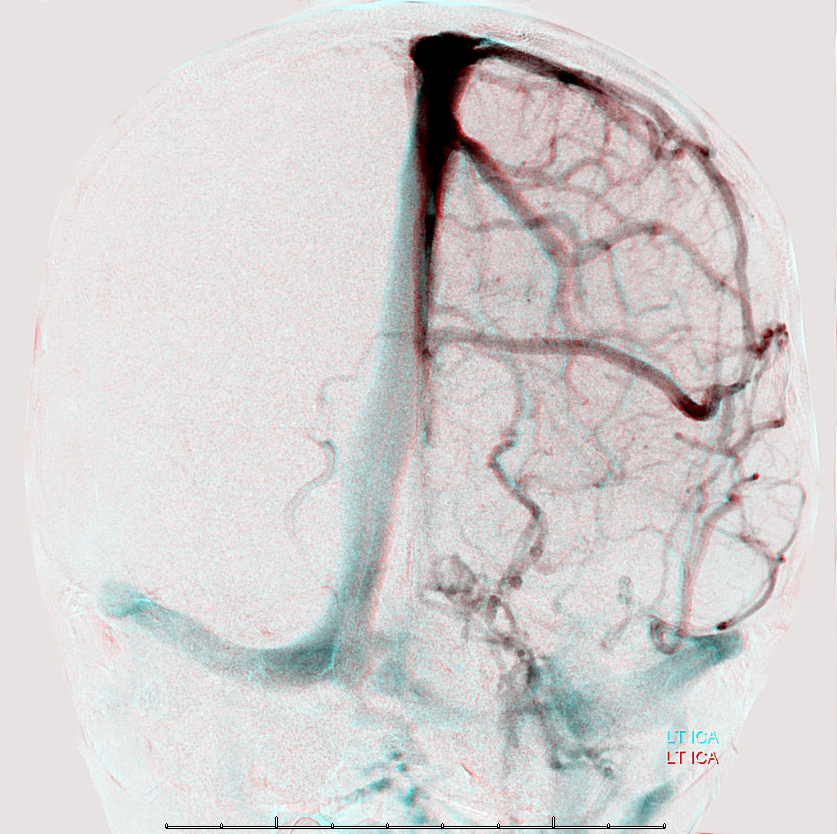
The general neurosurgical fact that the anterior third of the superior sagittal sinus can be safely sacrificed is true almost all the time. When it is not, consequences can be catastrophic. Normally, few veins drain into the anterior 3rd of the SSS, and these usually have collaterals. However, occasionally a large frontal or sylvian vein happens to drain anteriorly. Taking this sinus means risking a venous infarct. Here is an extreme example of dominant inferior left frontal vein draining into the anterior third of the frontal sinus, on MRI. Case courtesy Dr. Howard Riina
Angio is much easier to appreciate. It is well to learn how to spot these veins on MR or CT, as most patients don’t get presurgical angiography for nonvascular lesion

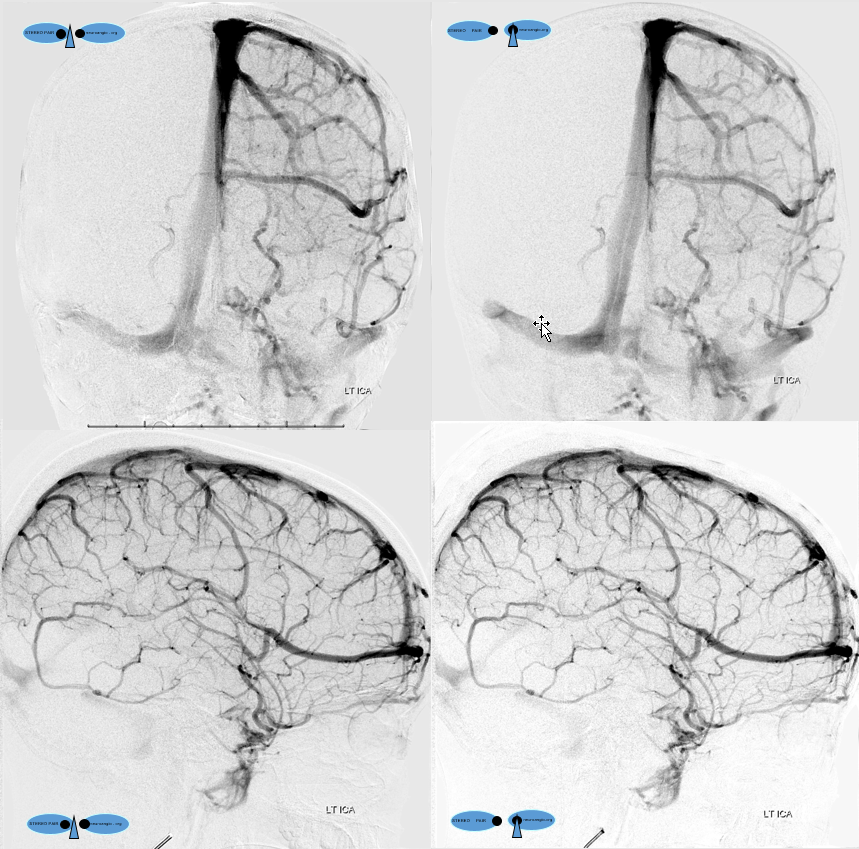
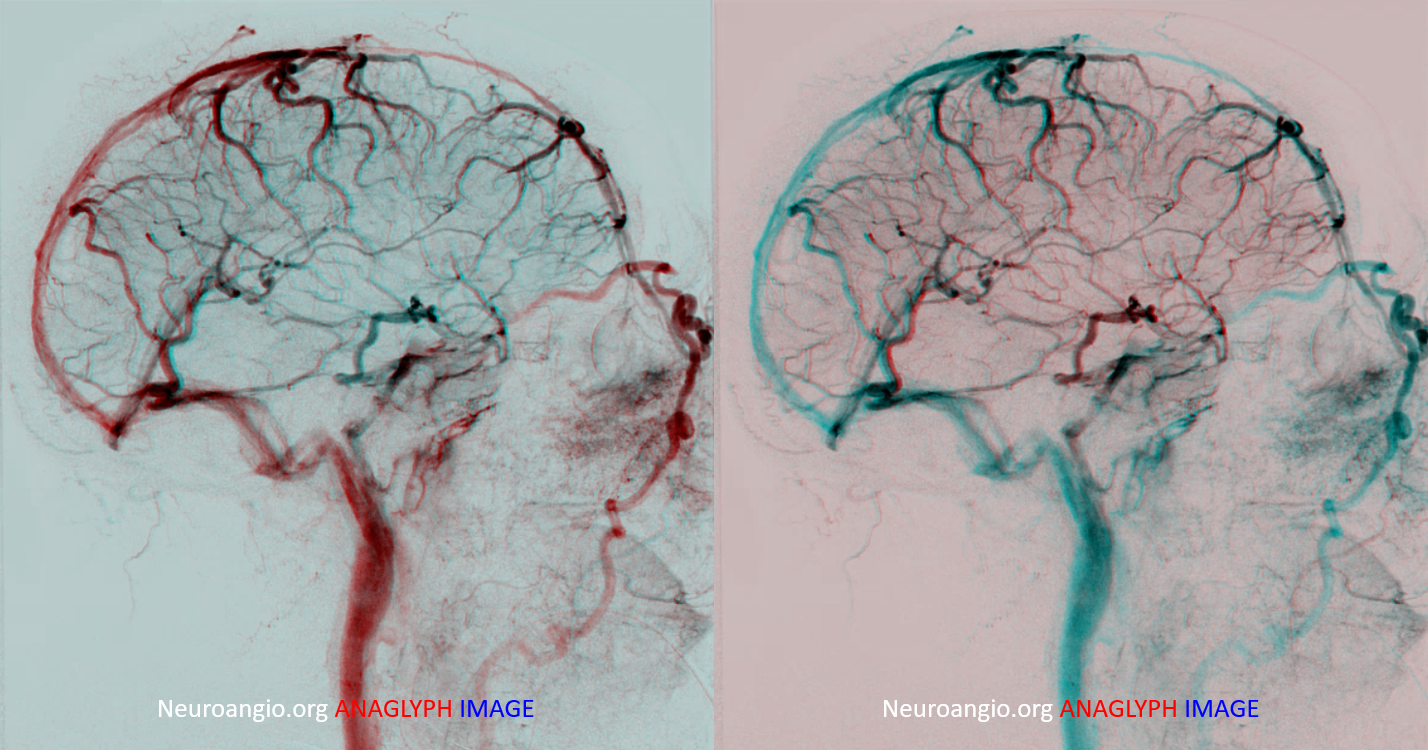
Anaglyph stereo
See Diploic Veins for more information
SSS Hypoplasia — the point we make not often enough is balance — in venous drainage for example. Small size of some vein is usually not pathology — just a spectrum and something else will be larger to compensate. SSS is not exception. It can be developmentally small — not because of some disease, and compensation — diploic , emissary veins, shift to Labbe or cavernous sinus — will take care of it. One needs to see the big picture. Examples below
Foramen Cecum Vein and SSS hypoplasia
Case courtesy Eytan Raz, MD Ph.D.
Vein of Foramen Cecum — a rare variant of embryonic significance but i must say not too much functional significance usually. Foramen cecum transiently contains a dural tail connecting anterior cranial fossa to nasal skin during development. The foramen usually fills with cartilage or bone, but when it is patent it can contain a vein. In this patient with hypoplasia of the superior sagittal sinus there is remarkable reorganization of venous drainage, favoring cavernous sinuses, the superior ophthalmic vein, and likely also responsible for relative prominence of foramen cecum vein
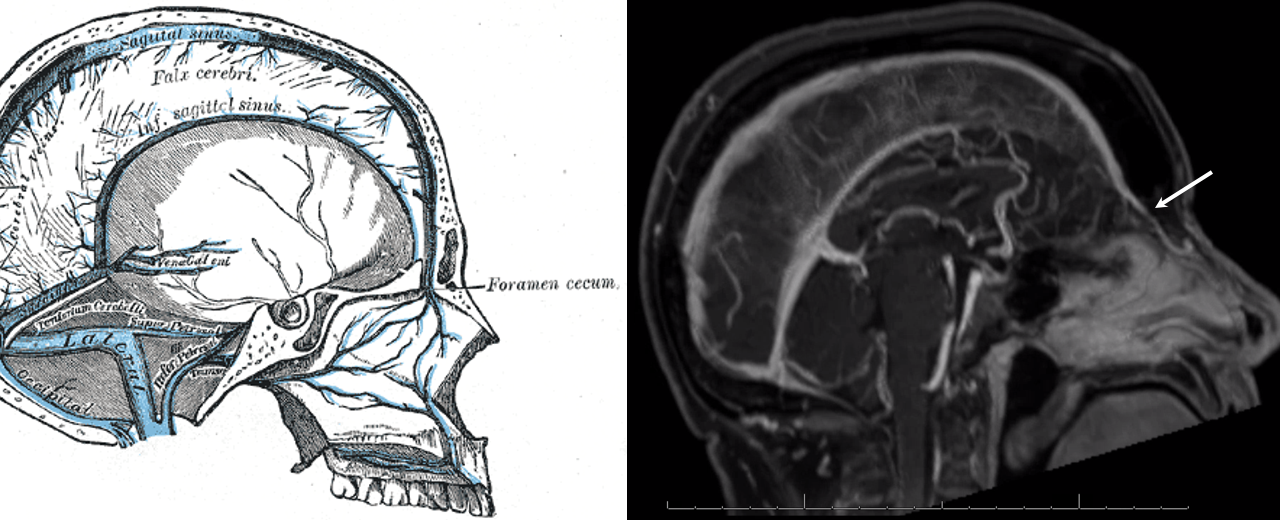
Anaglyphs
Left side
Another foramen Cecum — just to show they are not so exceptionally rare
Movie –stop and scroll thru individual frames
GIF
Stereos
Yet another example — from the top of page movie
Another example of SSS hypoplasia over frontal lobes, this time with compensatory drainage into the inferior sagittal sinus — case courtesy Dr. Eytan Raz
Another example of SSS hypoplasia — this time with diploic venous compensation
Diploic and emissary veins are best seen in late venous phase
Right side
SSS Hypoplasia Again — to show this is not so exceptional
Anaglyph
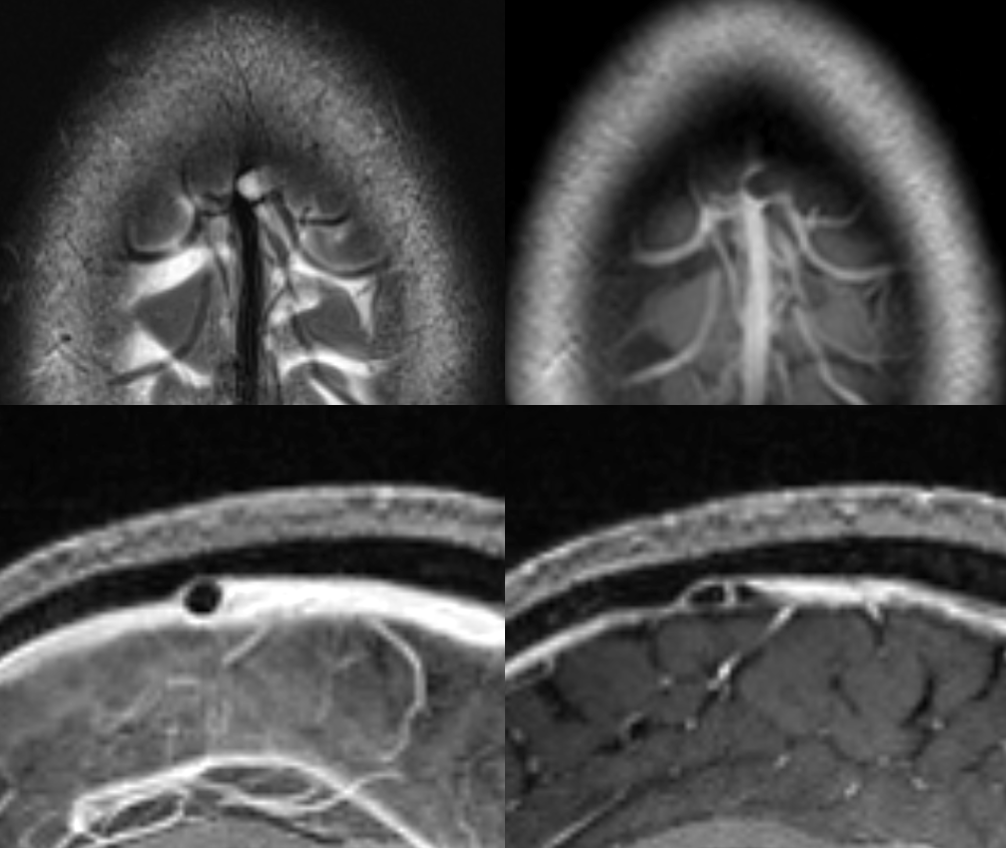
DEEP-SUPERFICIAL DRAINAGE BALANCE
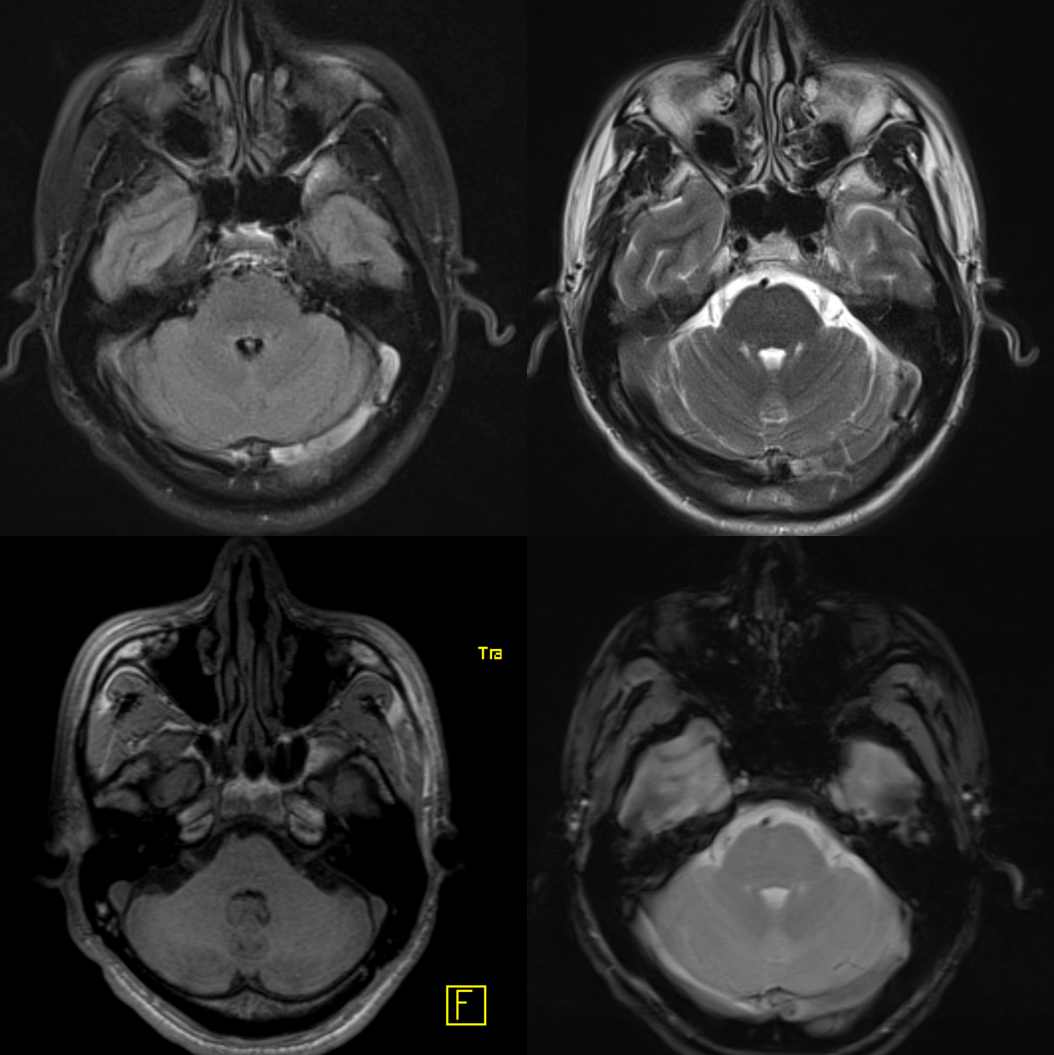
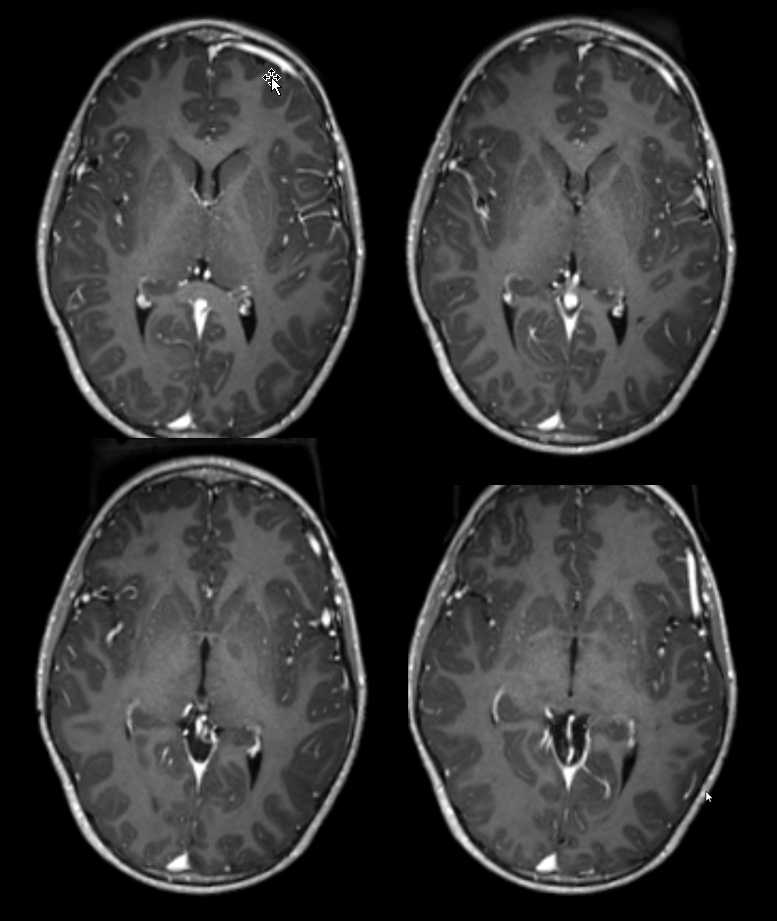
Another compensation for hypoplasia of the SSS is shift of superficial drainage into the deep venous system via the medullary veins draining into the internal cerebral veins. Courtesy Dr. Gopi Nayak. There is hypoplasia of the Superior Sagittal Sinus.
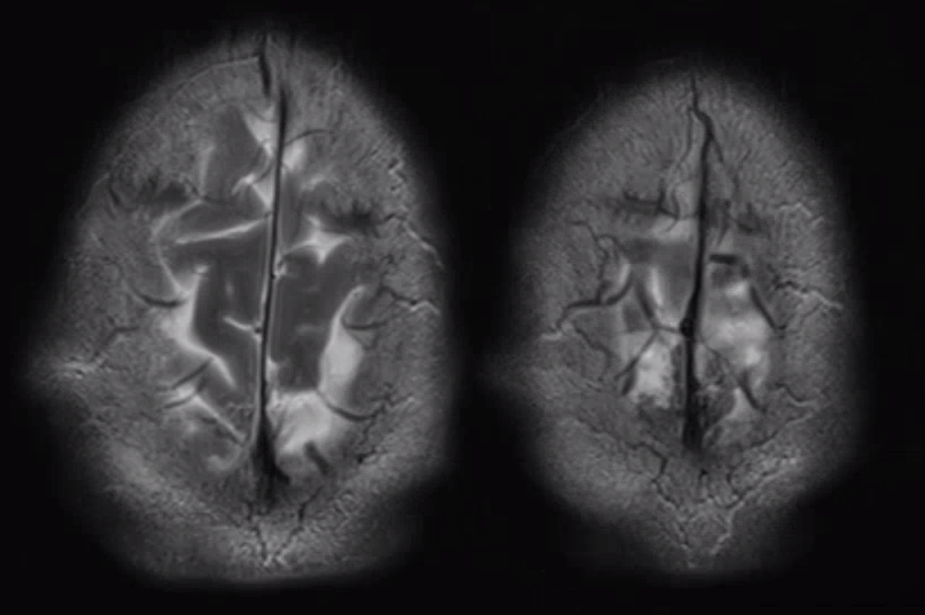
As one way of compensation for this superficial venous system deficiency, there is more venous drainage routed to the deep system. Amazing images of deep medullary/transverse venous prominence — completely nonpathologic, simply reflecting a shift of drainage equilibrium towards the deep venous system
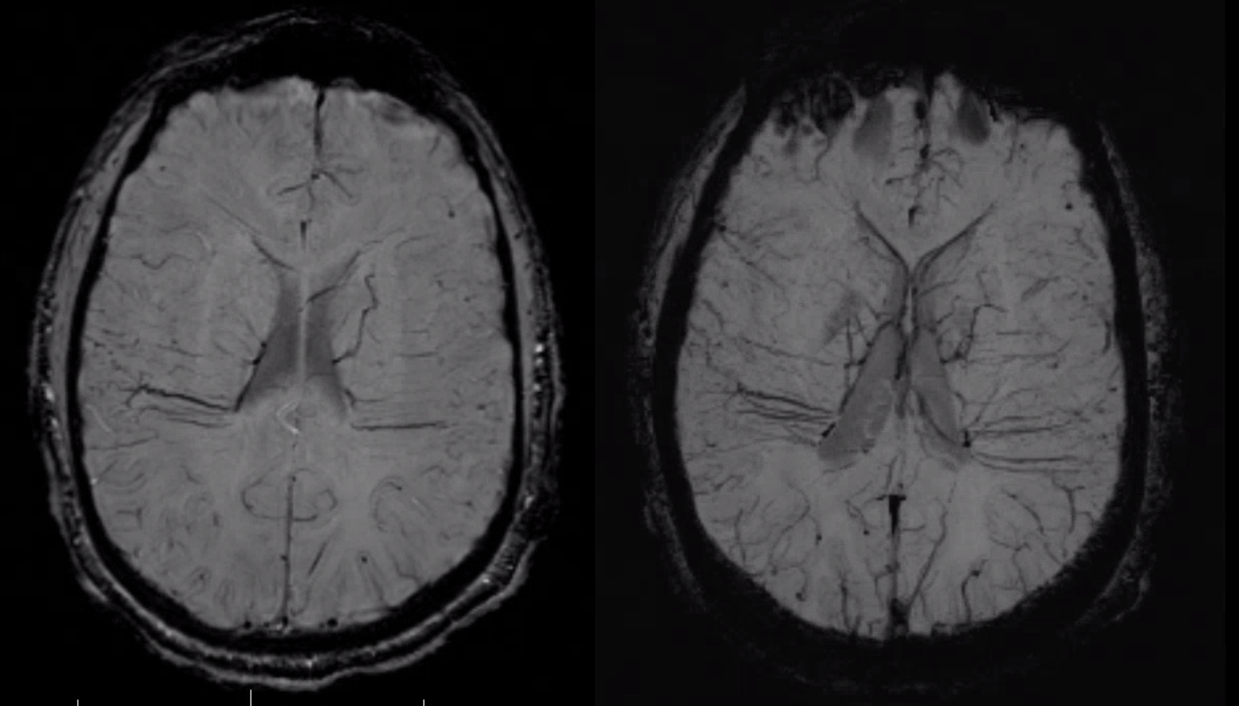
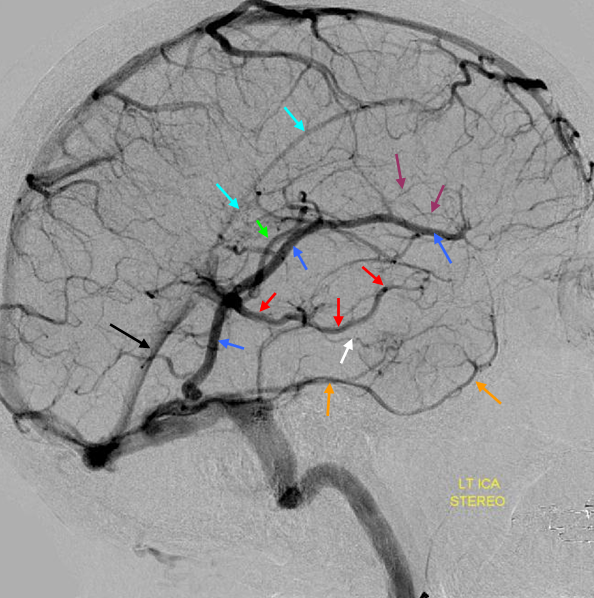
Some arrows. Open white arrows — septal veins on the medial aspect of frontal horn. Thick white arrows — longitudinal caudate venous arcade. Black arrow — direct lateral vein, prominent because of hypoplasia of the posterior segment of the left longitudinal caudate vein. Thin white arrows are transverse/ medullary veins
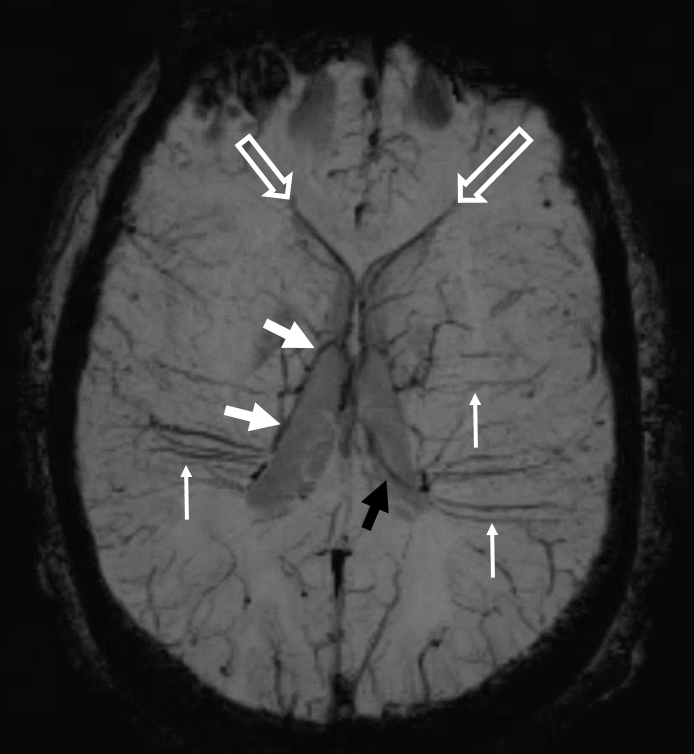
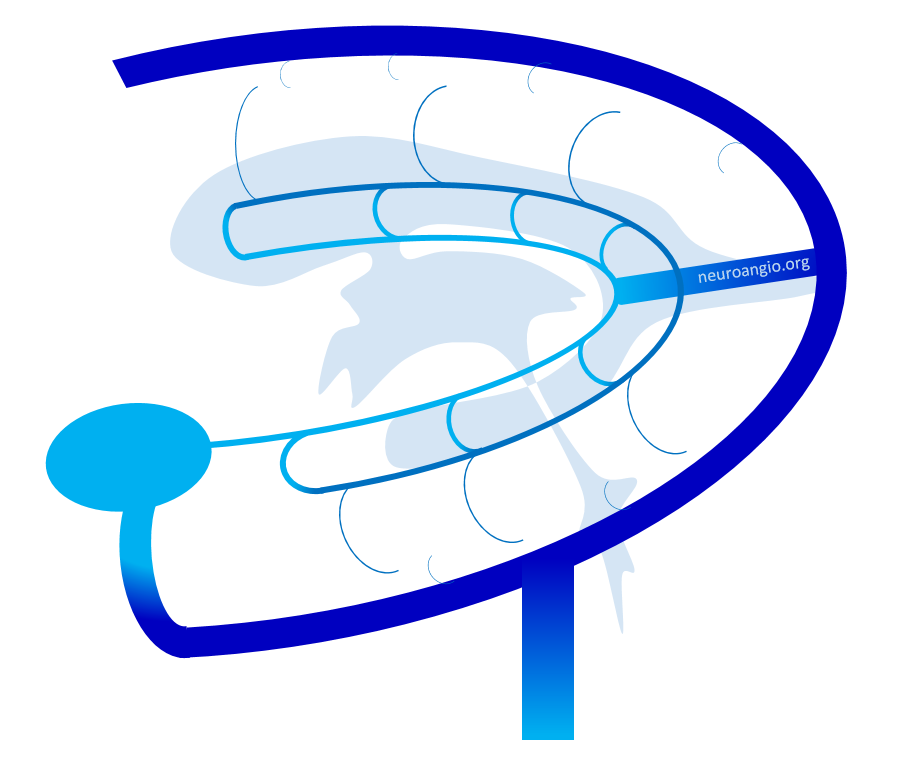
Here is a diagrammatic way of showing the same thing
Convexity Vein Hypoplasia — Prominent ISS
Its not clear what is the chicken or egg — is the SSS hypoplastic because draining vein connections did not develop? Or because of some dural issue? I favor the former. What about this case?

Fenestrations and compartments
See Cavernous Sinus Page for examples of anatomically and functionally relevant fenestrations. Other sinuses, such as sigmoid and superior sagittal, occasionally demonstrate fenestrations, usually of purely incidental nature. However, exceptions define rules. This patient with a sigmoid sinus fenestration, for example, presented with left-sided pulsatile tinnitus which could be suppressed by left jugular compression. Notice that the tinnitus is on the side of nondominant sinus, further supporting the idea that it is fenestration-related

MIP image of the same
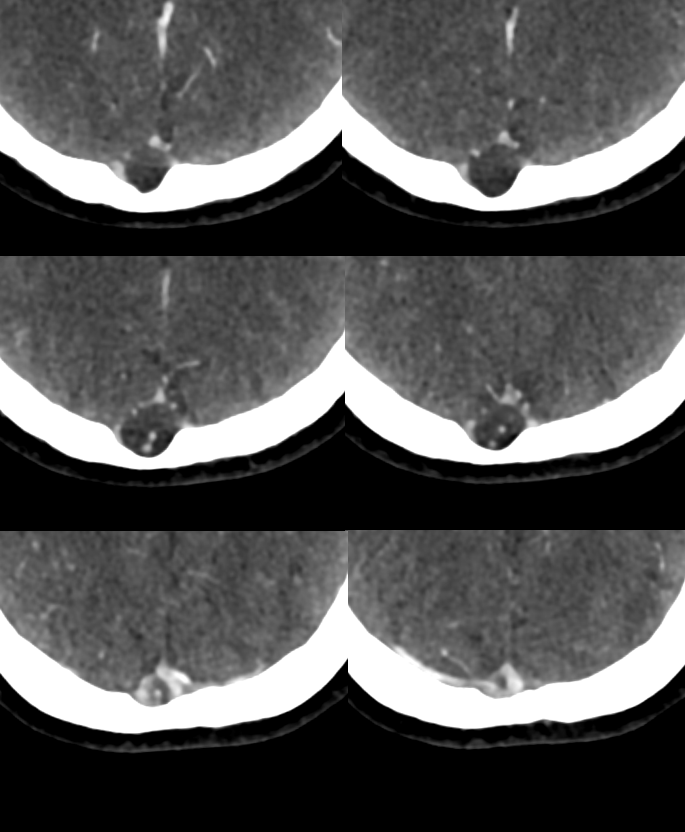
Inferior Petrosal Sinus MRI — some cross-sectional imaging to help identify sinus outflow pathways; inferior petrosal sinus extends along the lateral aspect of the dorsum sella towards the jugular foramen.
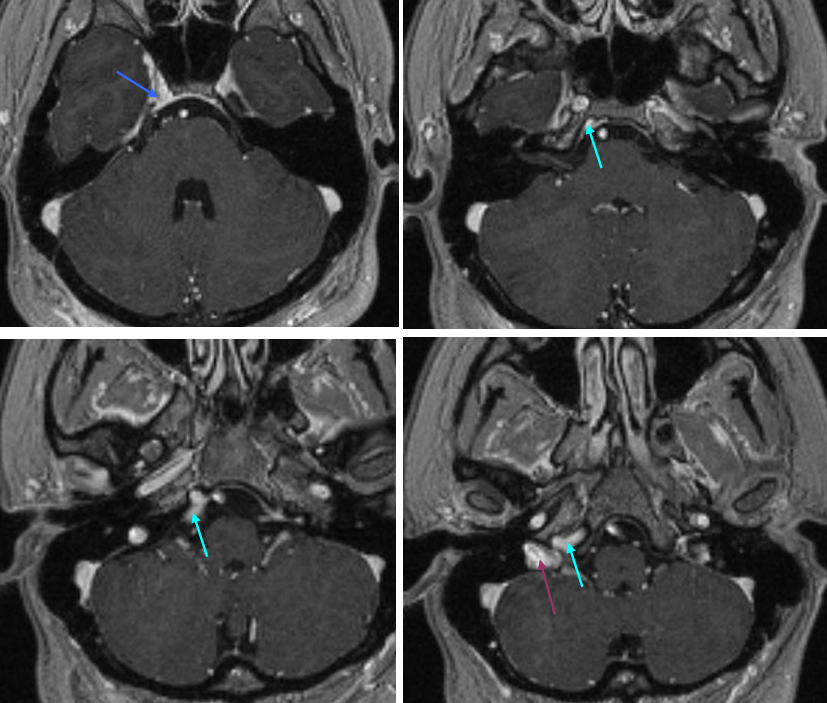
Cavernous Sinus=blue; inferior petrosal sinus=light blue; sigmoid sinus=purple
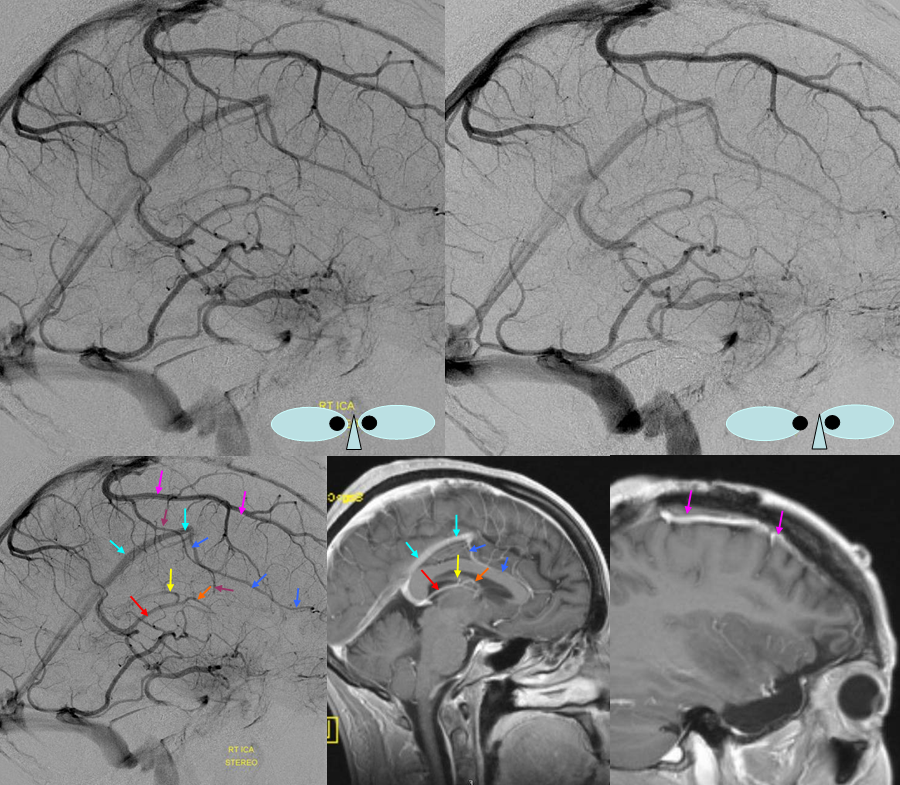
The inferior sagittal sinus is highly variable in extent of development and course. This one (light blue) has an unusual craniocaudal orientation. Notice complete lack of cavernous sinus capture by the sylvian veins, which drain instead towards the sigmoid region.
Labbe=dark blue. Inferior temporal vein=beige. Inferior sagittal sinus=light blue. Straight sinus=black. Basal vein=red. Internal Cerebral Vein=green. Notice dominance of drainage to the sigmoid sinus system with no visualization of the sphenoparietal sinus or cavernous sinus. The basal vein drains exclusively posterior. This patient would be very unlikely to tolerate sigmoid sinus or straight sinus thrombosis.
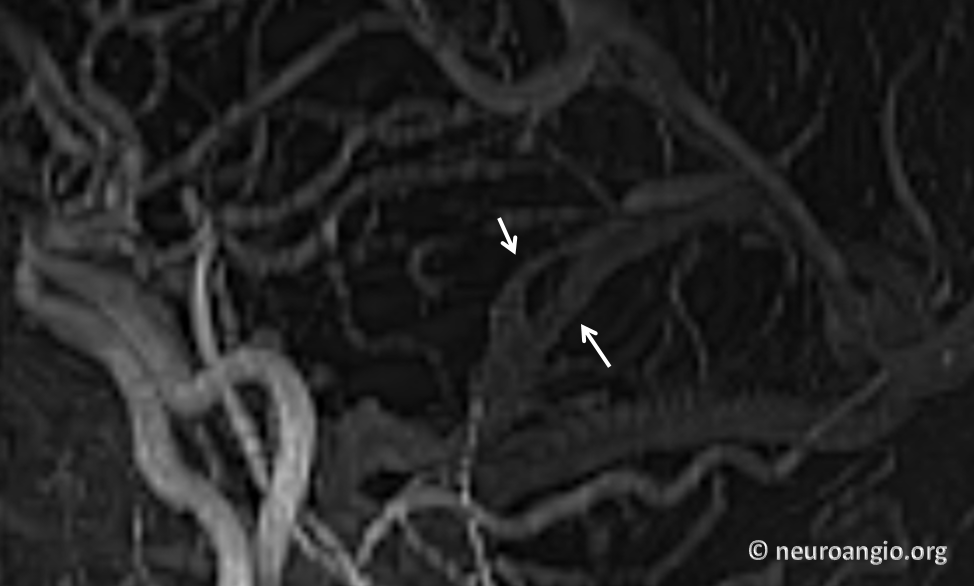
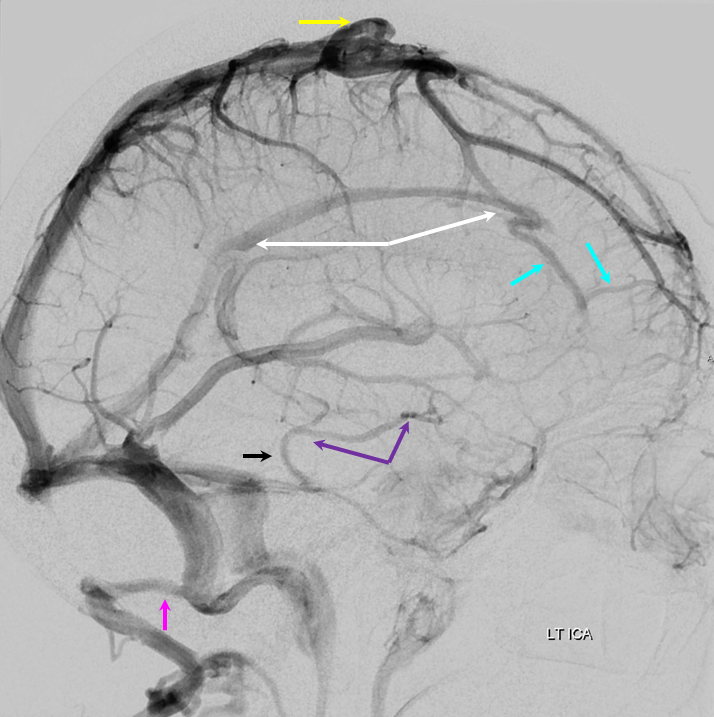
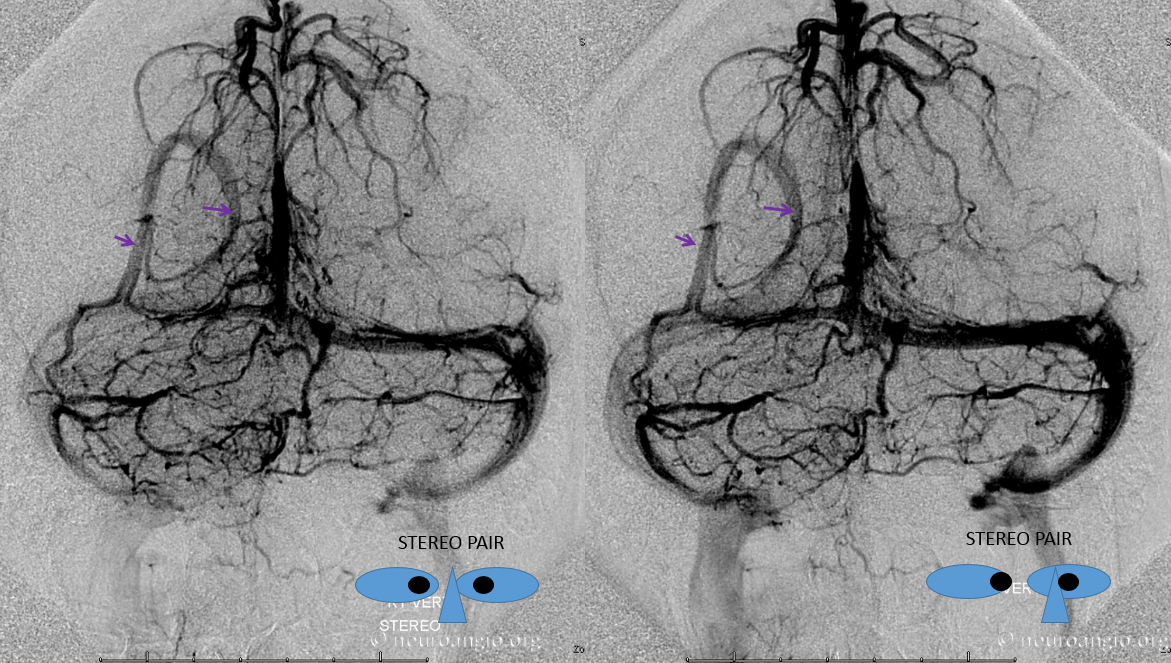
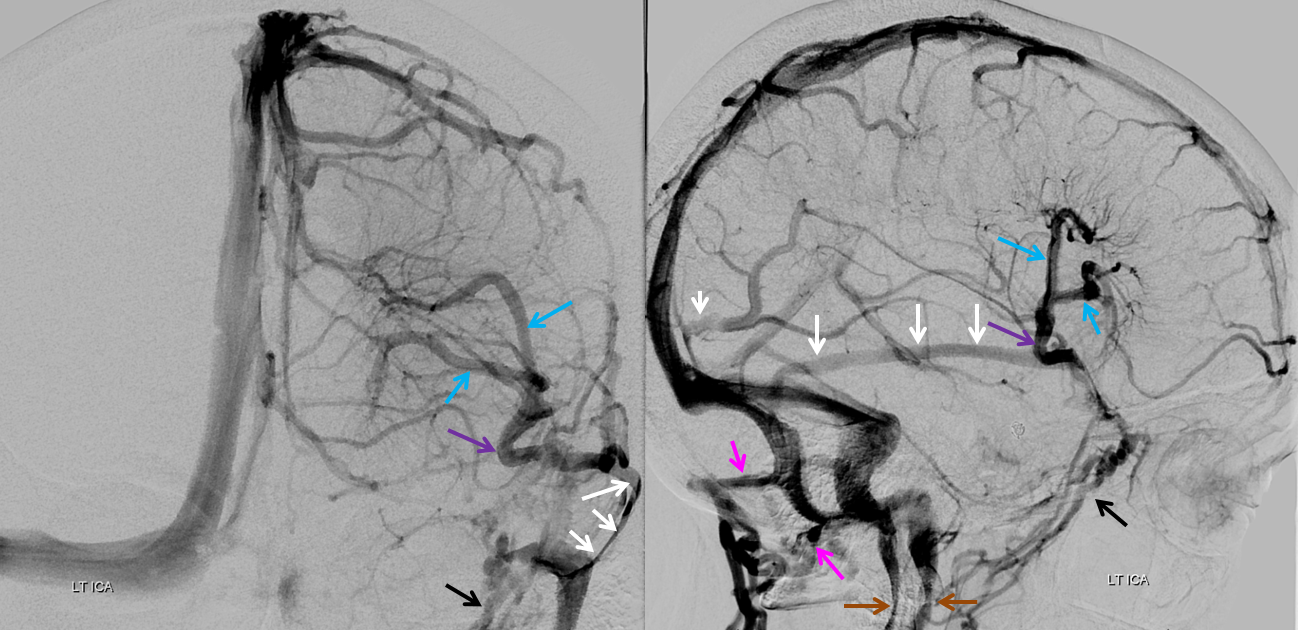
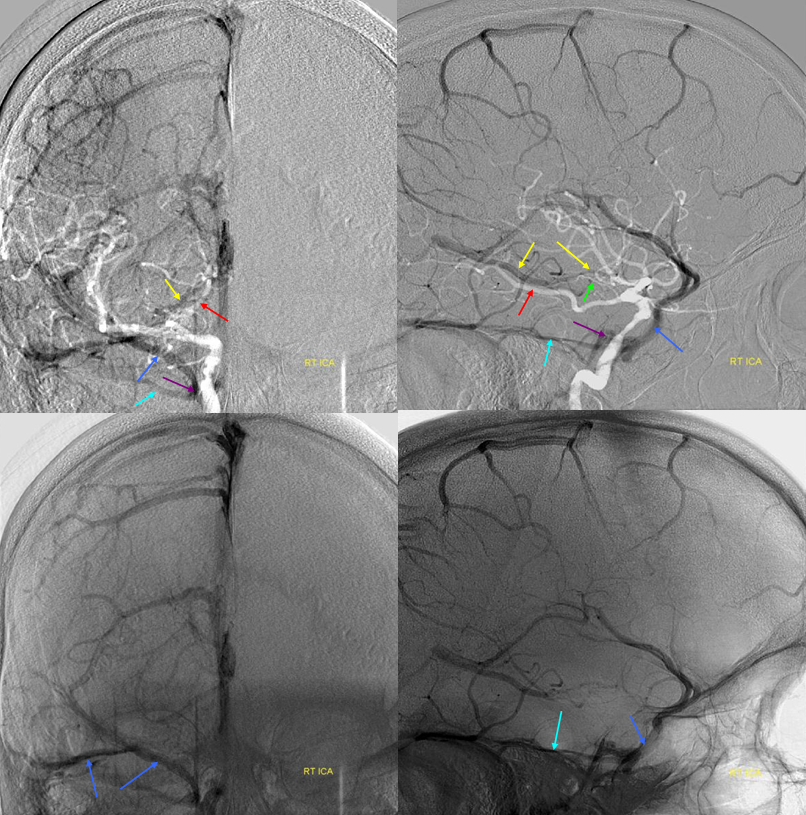
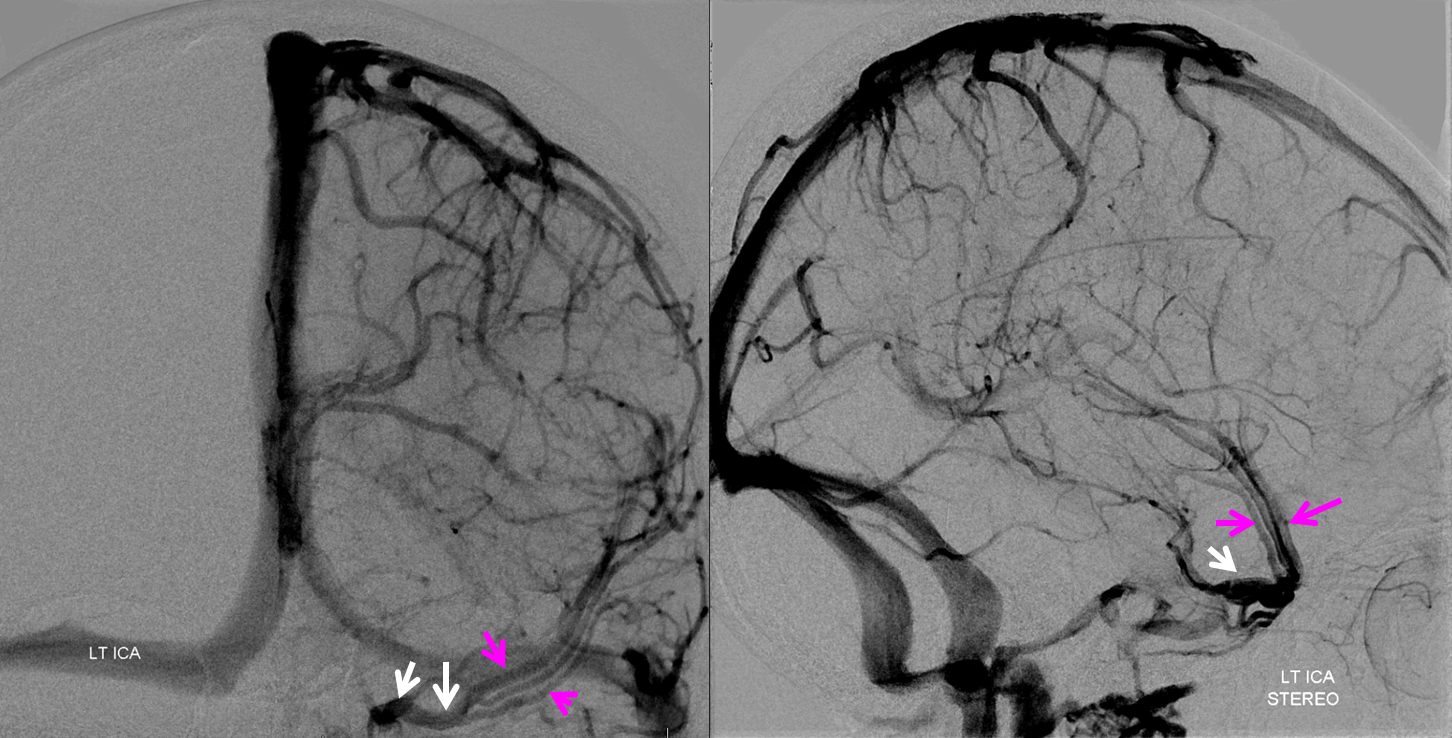
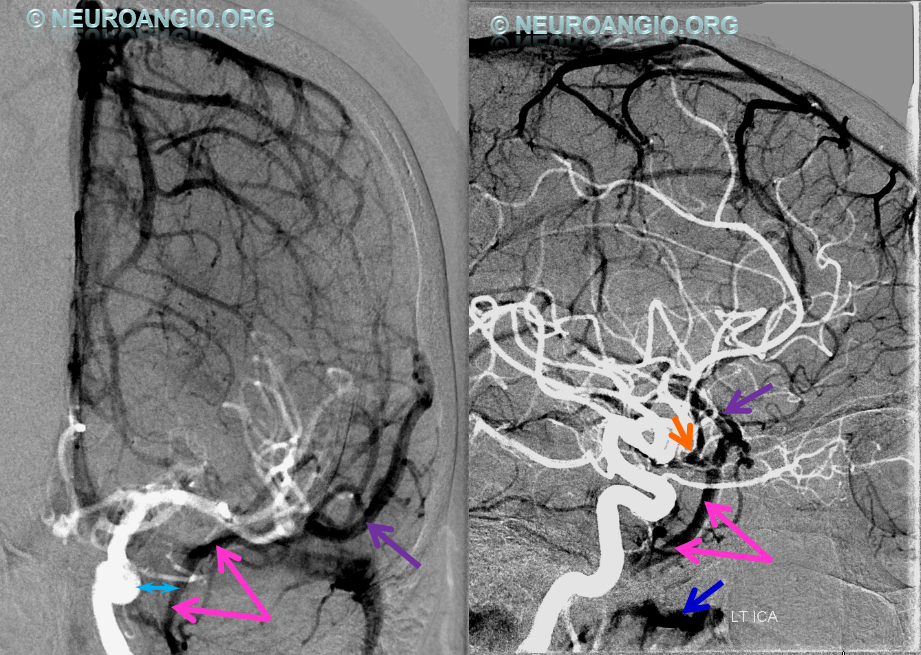
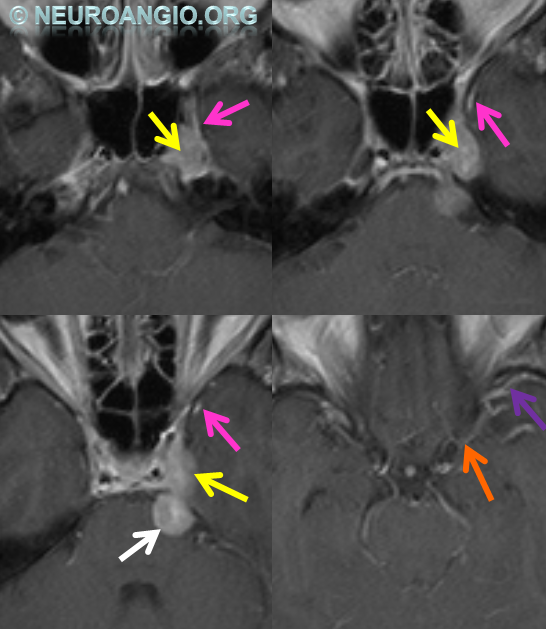
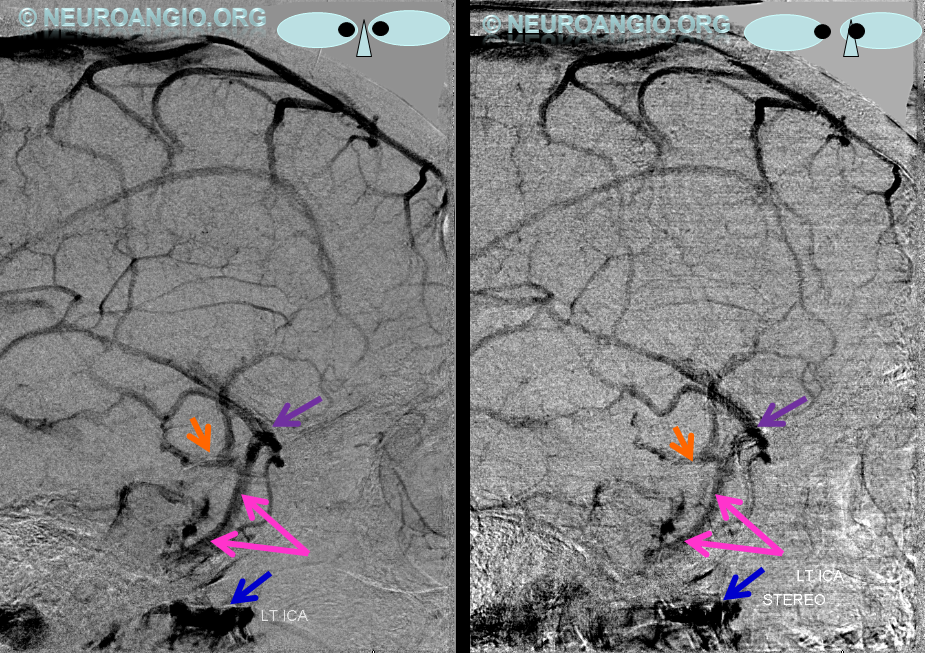
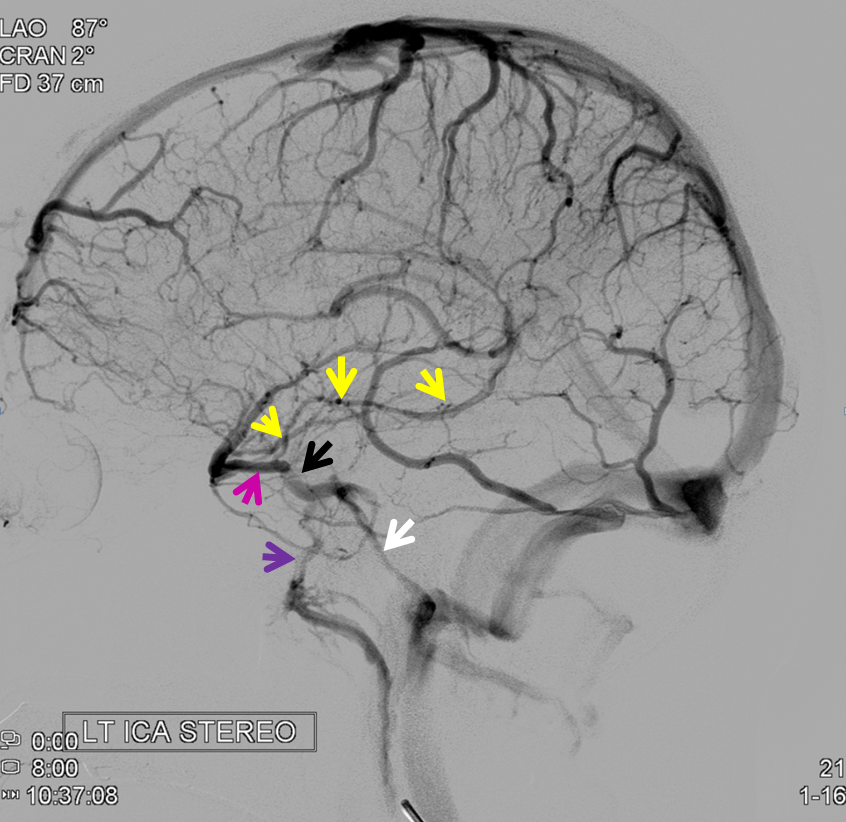
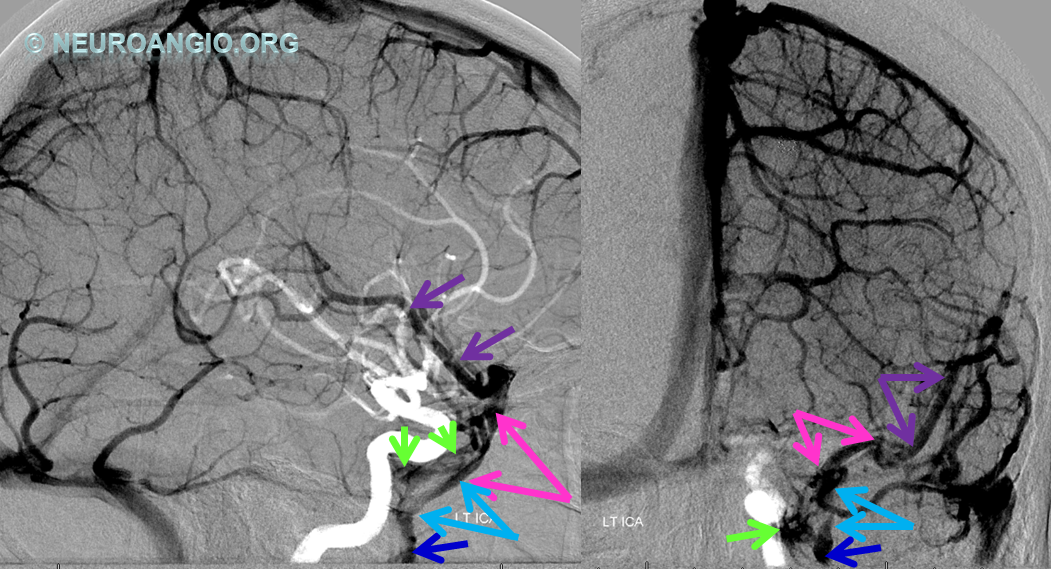
Below is an example of as large an inferior sagittal sinus (white) as one is likely to ever see under non-pathologic circumstances. Why is this sinus so large? Again, the answer is that veins are like rivers — the inferior sagittal sinus happens to be receiving a completely benign, nonpathologic mesial anterior frontal vein (blue arrows). However, the increased inflow into the Galen system has likely resulted in alternate drainage of the basal vein (purple) into the superior petrosal sinus via the lateral mesencephalic vein (black) — see deep venous system and veins of posterior fossa pages for more info. Also notice a large emissary vein (pink)
Stereo of the same
Another example in Anaglyph Stereo
In this patient the inferior sagittal sinus did not develop. Corpus callosum and adjacent territory which may be expected to drain into the inferior sagittal sinus is instead collected by secondarily prominent caudate veins emptying into the thalamostriate and internal cerebral veins. Notice also a well-developed superior petrosal sinus receiving the superficial sylvian system.
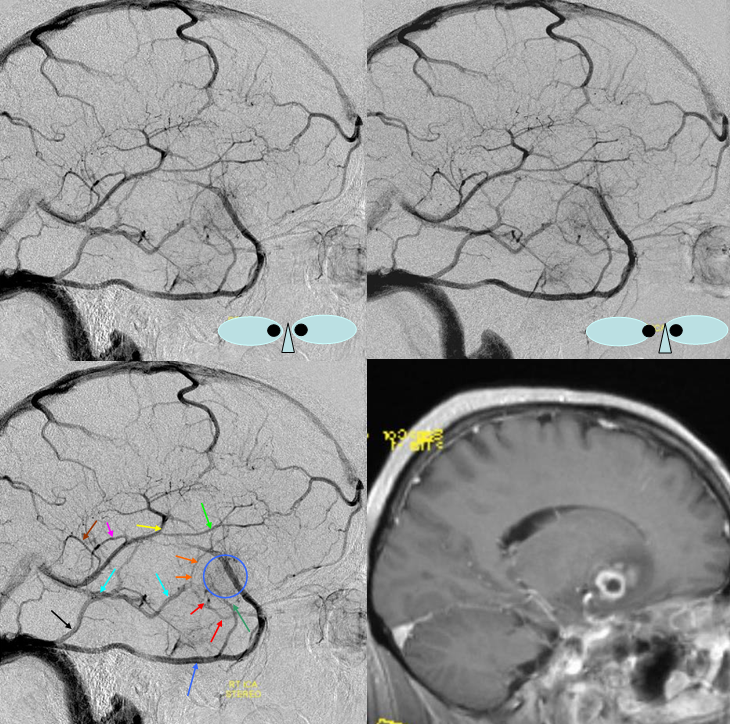
Blue Circle=tumor blush. The superficial Sylvian vein is prominent within the circle and extends over the temporal lobe towards the superior petrosal sinus (dark blue arrow). Labbe=black. No Trolard is seen, various superior cortical veins drain into the SSS. Basal vein=light blue, dominant posterior drainage. Very nice demonstration of the deep venous system tributaries. Anterior Septal vein=bright green, capturing territory of hypoplastic anterior cerebral vein. The inferior sagittal sinus is absent. Thalamostriate vein with large longitudinal caudate vein=yellow. Direct lateral vein=pink. Posterior caudate/splenial veins=brown. A prominent Pericallosal Vein empties into a large inferior sagittal sinus. Also note hypoplasia of the superior sagittal sinus proximal to a large superior frontal convexity tributary.
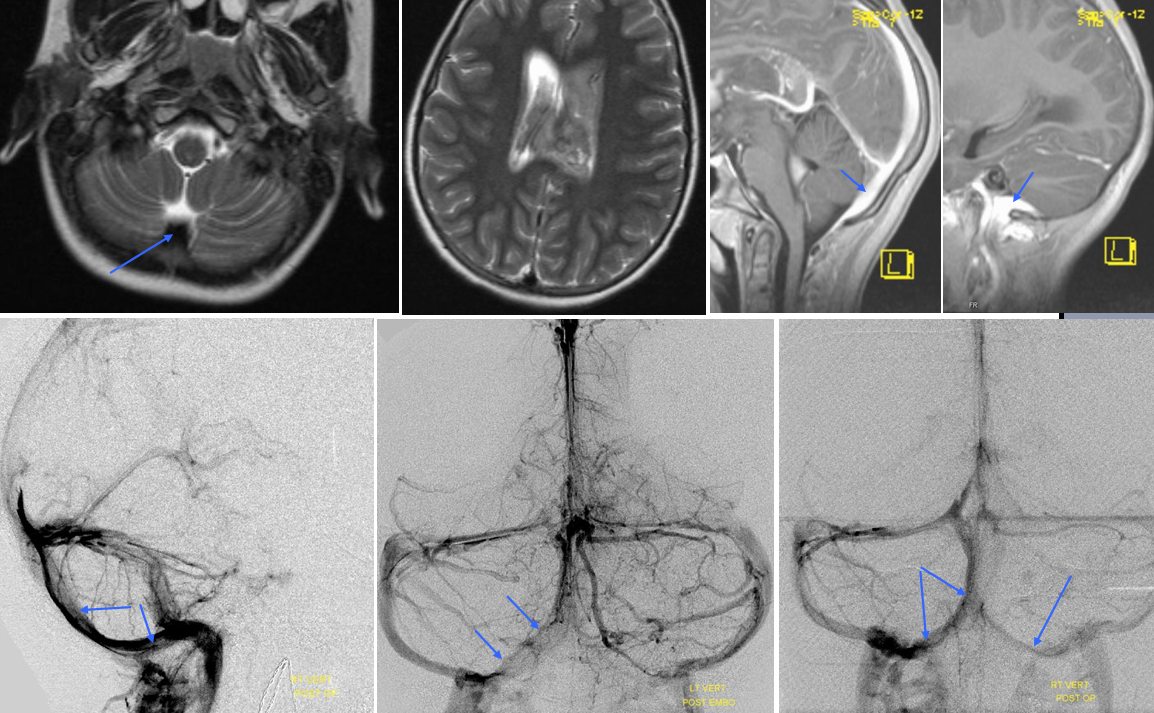
Occipital Sinus — The sinus connecting torcular to the marginal sinus (sinus which abuts, partially or completely surrounds the foramen magnum) is called the occipital sinus, after the bone it is associated with. It is a relatively common find in neonates, and a rare one in adults, again demonstrating that the venous system continues to mature after birth. It is of little clinical significance but of important surgical significance in approaches to the posterior fossa.
Dark blue=percallosal vein. Light blue=inferior sagittal sinus. Pink=frontal convexity vein. Orange=anterior septal vein. Yellow=thalamostriate vein. Red=Internal cerebral vein. Occipital sinus (blue arrows on the sagittal and MRI axial projections), draining into the marginal sinus (dark blue arrows on the AP projections.) The occipital sinus is more commonly seen in children.
Dural / Tentorial Sinuses
it is somewhat a misnomer, as all sinuses are dural. Naturally, major dural sinuses have unique names like the superior sagittal, transverse or sigmoid sinus. There is certainly a developmental propensity for these to form in most people — Dorcas Padget felt that sinuses form at intersection of dural covers due to the resistance of the channel to pressure-related collapse. However, not infrequently we observe existence of other dural venous channels, unnamed, draining this or that group of veins. Eventually these sinuses will join a more well-established sinus. The extra sinuses go under a broad term of “dural sinus” — the best thing to do, as always, is to simply describe what exists — for example “left parietal dural sinus draining into the superior sagittal sinus”.
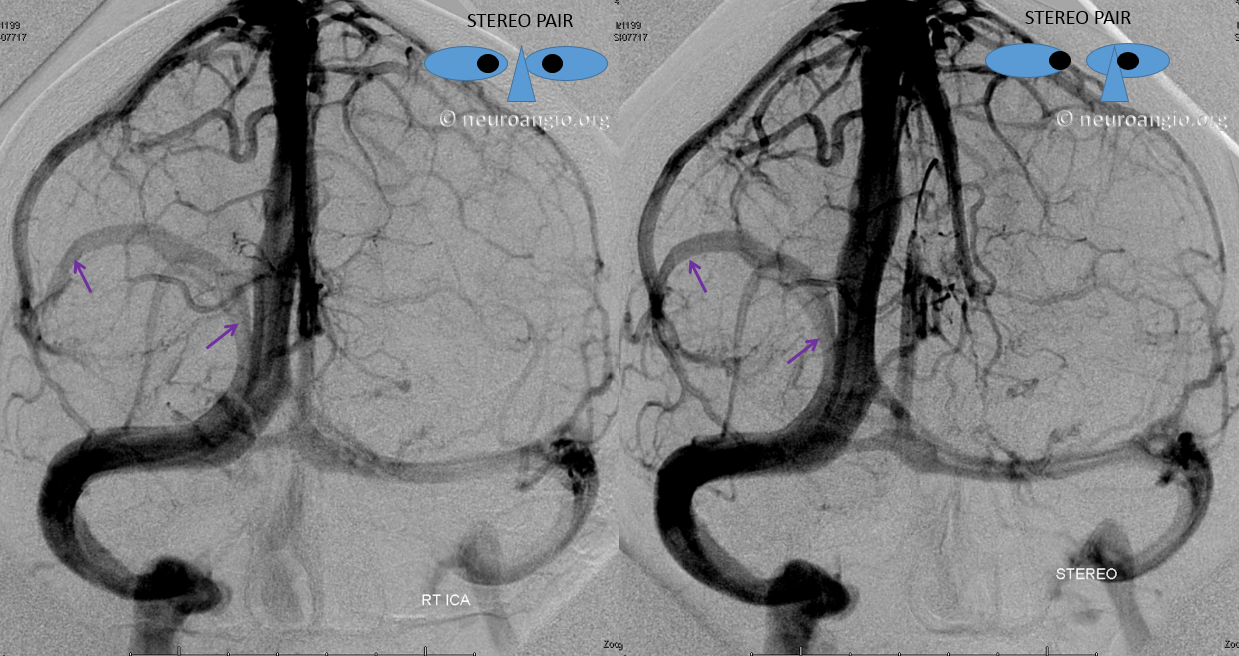
Here is an example of a right parieto-occipital sinus (purple arrows, stereo pair) which collects regional supratentorial and infratentorial veins, emptying into the transverse sinus. Again, this is really only of importance to a surgeon or interventionalist of a procedure in the area is being contemplated.
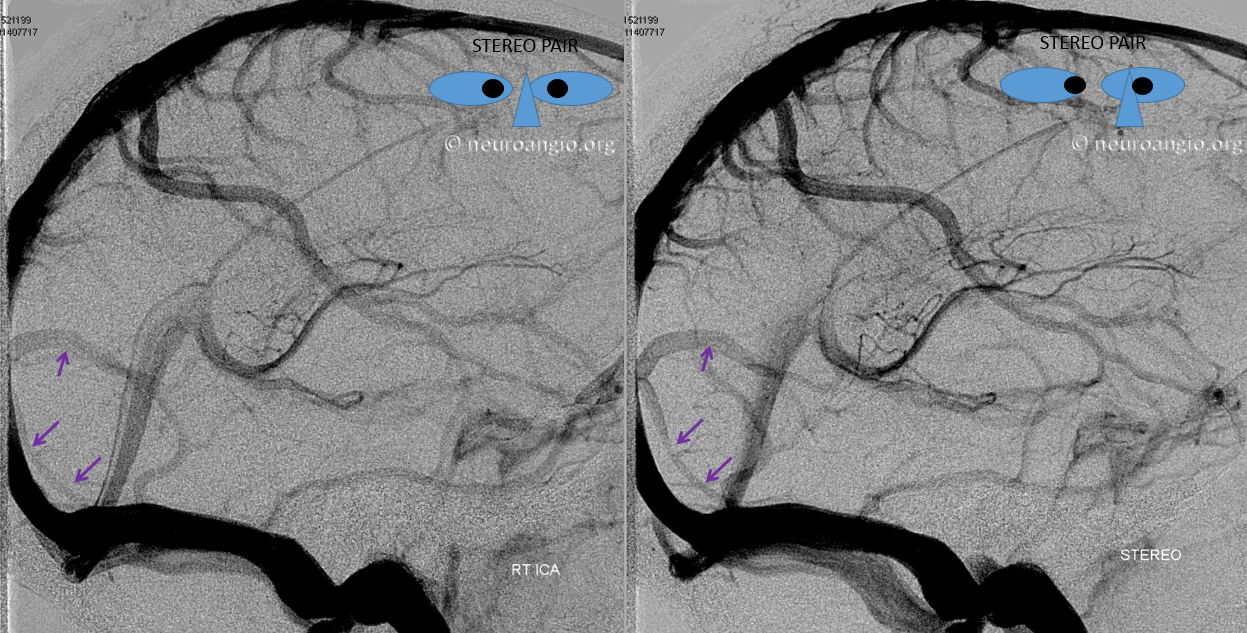
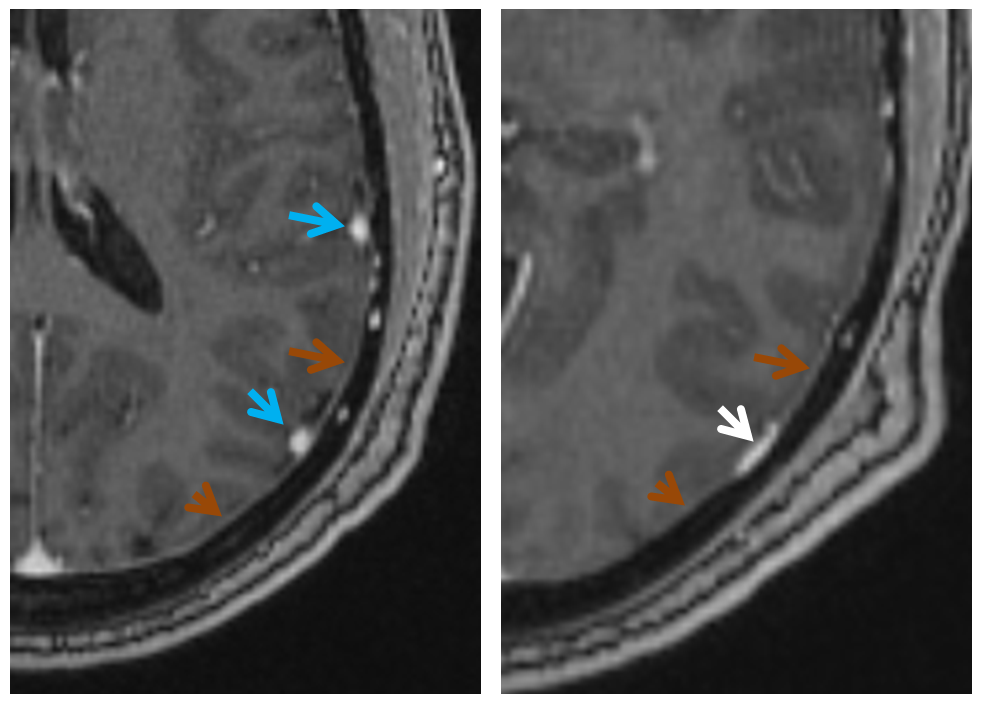
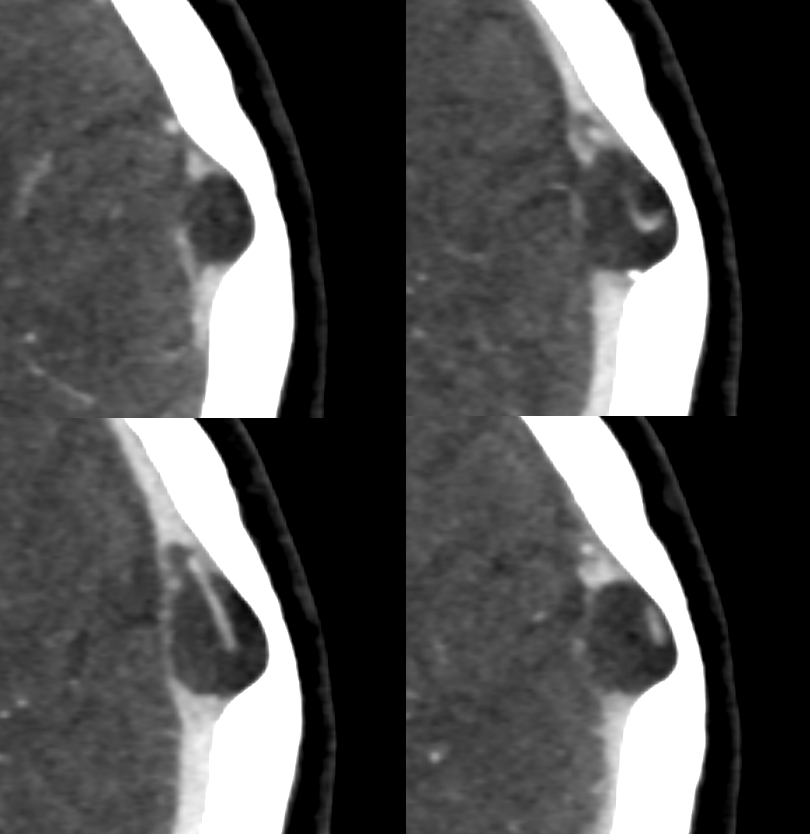
Below is an example of a parieto-occipital dural sinus (white) which collects a somewhat peculiar duo of surface veins (light blue). The transition from cortical vein to dural sinus is marked by the purple arrow. It is typical to see dural sinuses associated with larger, more dominant surface veins, probably because dural sinus is not a favored embryologic structure, and in order for it to persist the flow demand must be somewhat high. Notice also bilateral transverse/sigmoid sinus stenoses in this patient with pulsatile tinnitus and intracranial hypertension.
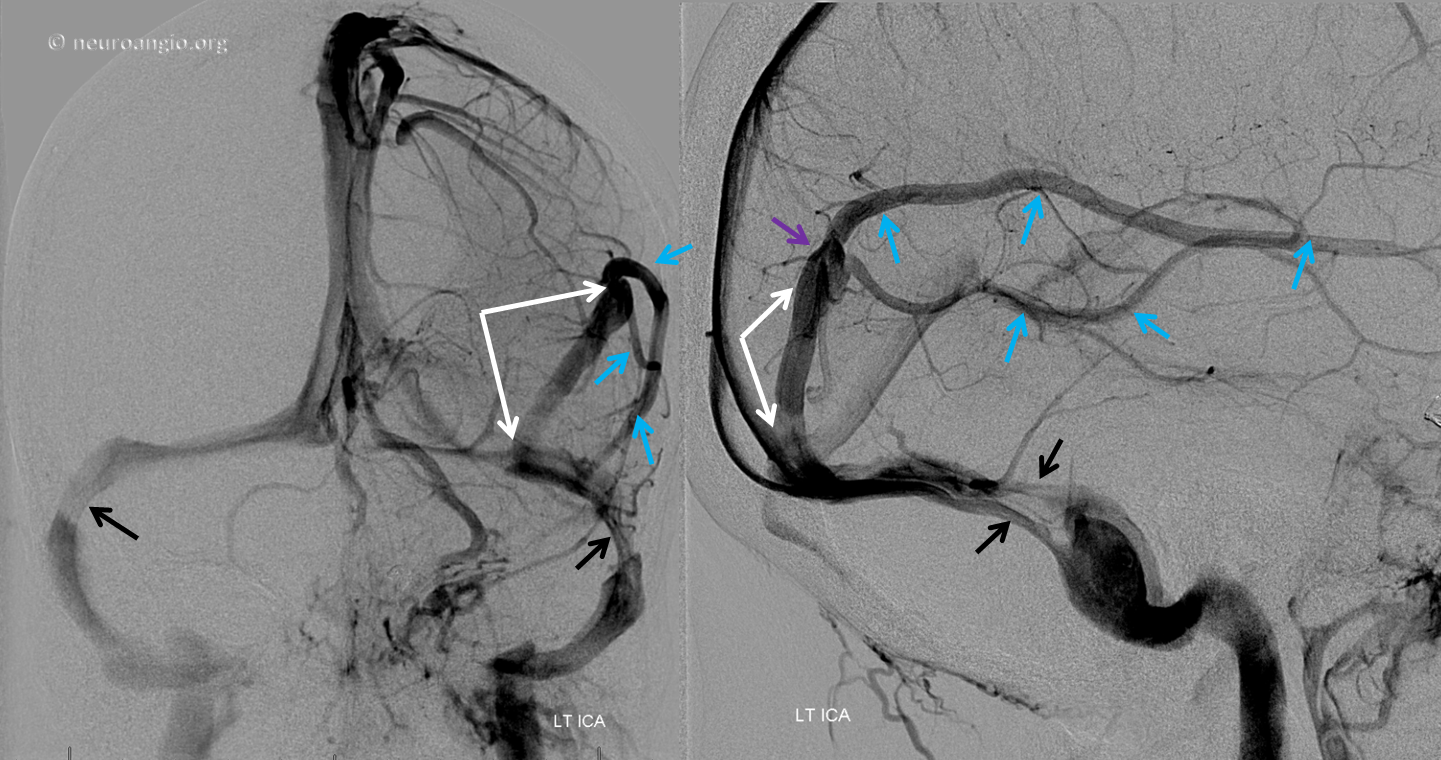
MRI of the same patient shows the characteristic rounded appearance of the cortical vein (light blue arrows), located just medial / deep to the dura (brown arrows), as distinct from the flattened, oval look of the dural sinus (white arrow). The post-contrast high-resolution T1-weighted images are the best way to look for dural sinuses like this one on non-invasive imaging
Stereo views of the same arrangement, several years later.
Cinematic Rendering — a very cool visualization algorithm — courtesy Dr. Matthew Young
A stent (yellow) has been placed into the dominant sigmoid sinus. While pulsatile tinnitus was cured, the headaches which initially improved then recurred, and a shunt was eventually placed (purple, white). Notice recurrence of narrowing (black) just distal to the stent, as is typical in such failed stent cases.
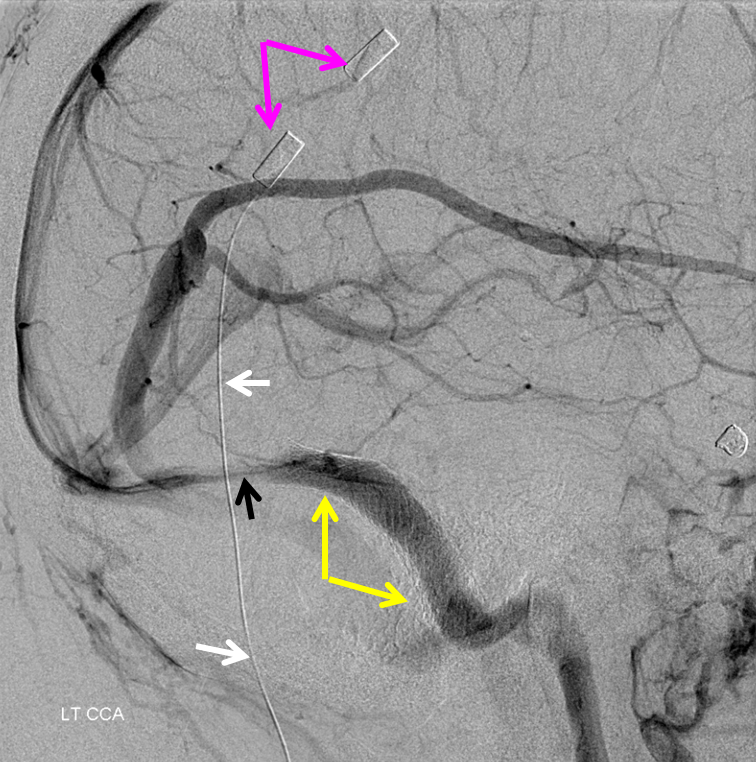
Below is a remarkable example of a long temporal dural sinus associated with a left frontal operculum Developmental Venous Anomaly. Cases like this one support the idea that pretty much any location in the dura can serve for a sinus. Preferentially, dural sinuses are located at confluence of dural sheaths, such as falx and convexity, or convexity and tentorium. However, increased flow can help maintain a dural sinus elsewhere, for example within convexity dura, as shown in above examples. Usually these kinds of dural sinuses are recipients of large cortical veins. In the case below, the sinus (white arrows) extends over the temporal dura, collecting a large DVA (blue, purple) of the frontal operculum. Notice the flattened appearance of the sinus (inferior two white arrows, frontal view), well-shown in the frontal view. This look is classic for a sinus, which is oval and flattened in the medial to lateral dimension as it courses through the dura. Also present is a smaller occipital dural sinus (white arrowhead). Notice also stenoses of the jugular veins (brown) at the C1 lateral mass, and compensatory prominence of the emissary veins (pink)
Same in stereo
Native stereo views
Anaglyph stereo
Dural Venous Lakes
Again, any part of dura can form a venous channel, just like we saw immediately above. This frequently happens at the vertex, where Trolard/Rolando veins join the superior sagittal sinus. What happens? These veins, very often, probably more often than not, first drain into a dural “venous lake” just lateral and superior to the sinus (remember that the sinus is usually slightly below the upper edge of dura). For Trolard/Rolandic group veins, this can be seen as a flattened part of the vein just lateral and above the sinus. For medial / interhemispheric veins, this shows up as a flattened channel in the falx cerebri just inferior to the SSS.
Here is an angiographic example — flattened appearance of dural components of vertex convexity veins (black arrows), rising above the SSS
Anaglyph
Arachnoid Granulations
Pretty much always present in the transverse/sigmoid sinus region. Can be large, small, dispersed, or grouped. When grouped, can be cause of “intrinsic” sinus stenosis. Can be giant — and asymptomatic, such as this one.
Coronal views — inset is a sagittal view.
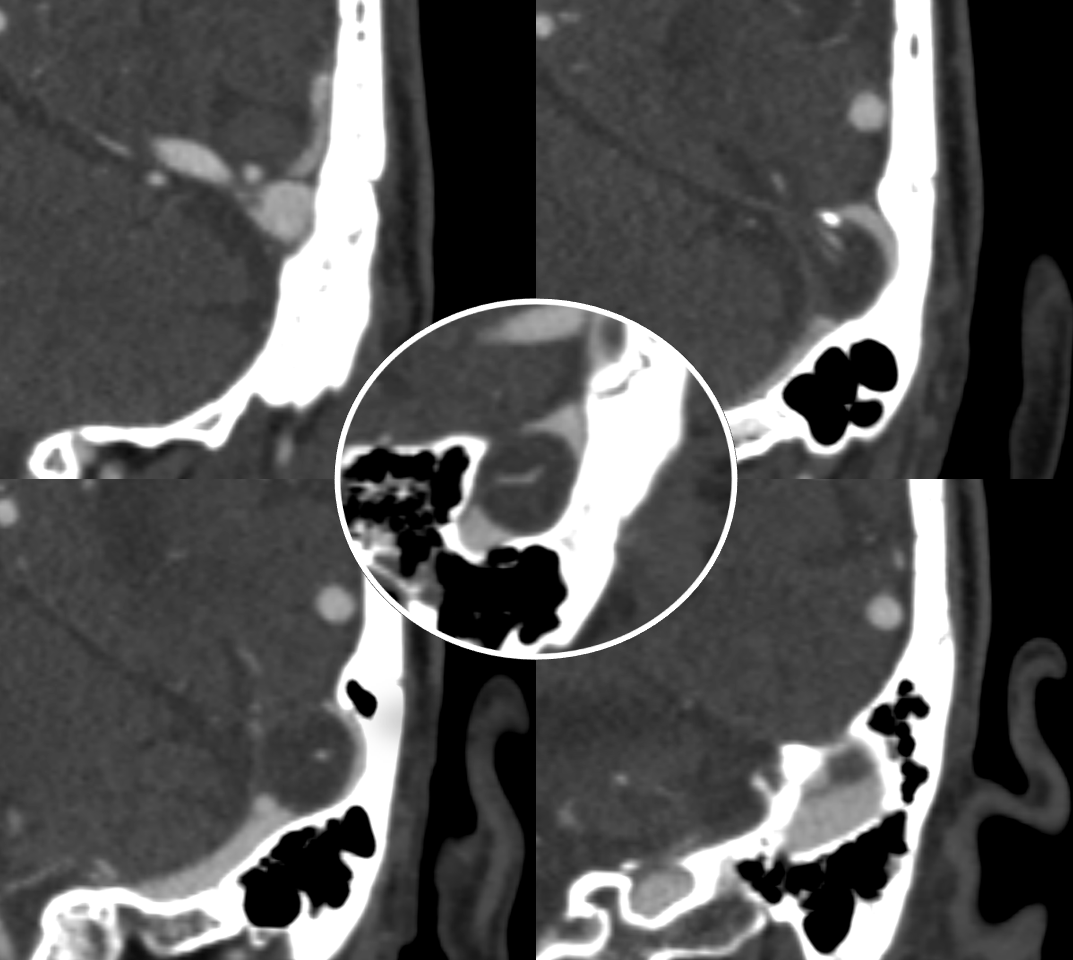
Smaller granulation causing venous pulsatile tinnitus — abolished by jugular compression (intrinsic stenosis — granulation narrowing the sinus)

A larger one in the SSS
Giant SSS — headaches
A bunch of giant ones in different patients
CT Venogram — vein emptying around one
CISS Sequence — larger ones have veins inside them. Asymptomatic
Cavernous Sinus — see also dedicated Cavernous Sinus page
Cavernous sinus is a metaphysical entity. It is a collection of anatomically and functionally separate venous compartment which, altogether, constitute the single venous space we have come to regard as a distinct anatomical structure. It is critical for the neurointerventionalist to understand this, because his or her treatments will be, of necessity, targeting these varied and complex compartments. This is a distinctly different view than the classical question of whether or not the sinus as a whole is involved in a disease process.
Embryologically, although the cavernous sinus is a very early structure, in its earliest form it does not participate in any way in the drainage of the brain — rather collecting tributaries of the future orbital/ophthalmic veins, facial and sphenopalatine systems. Even in the newborn, the connections between sylvian and basal venous systems and cavernous sinus are usually nonexistent — maturation of these connections is one mechanism which allows for stabilization of venous drainage in infants affected by high flow shunts such as some Vein of Galen Malformations. The developmentally late capture of the cavernous sinus by Sylvian and basal veins explains the marked variability in the extent of such capture in adults, while the ophthalmic vein to cavernous sinus connection is essentially constant.
The classical view holds:
Major Tributaries:
1) Basal vein of Rosenthal — typically flows toward CC, but easily reverses flow in cases of fistula, etc.2) Ophthalmic vein — again typically flow is into the sinus, but can easily reverse itself3) Sphenoparietal sinus — also reverses easily. Drains sylvian venous network into the sinus.
Major Egress:
1) Superior Petrosal Sinus
2) Inferior Petrosal Sinus
3) Foramen Rotundum, Foramen Ovale, and other skull base foramina to the pterygoid venous plexus
4) Contralateral Cavernous sinus thru transcavernous channels
5) Clival venous plexus down to foramen magnum region, and from there into jugular veins or marginal sinus. A neat way of projecting arterial phase as a mask for venous phase to demonstrate carotid artery relationship to the cavernous sinus. Many tributaries and egress routes of the cavernous sinus are visible.
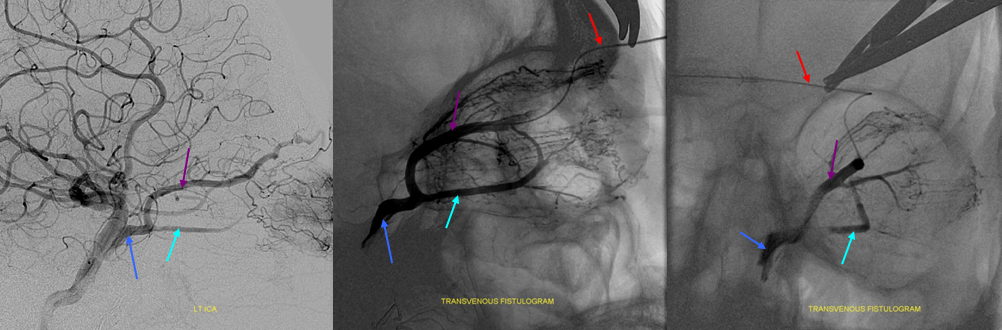
 Stereo of the same
Stereo of the same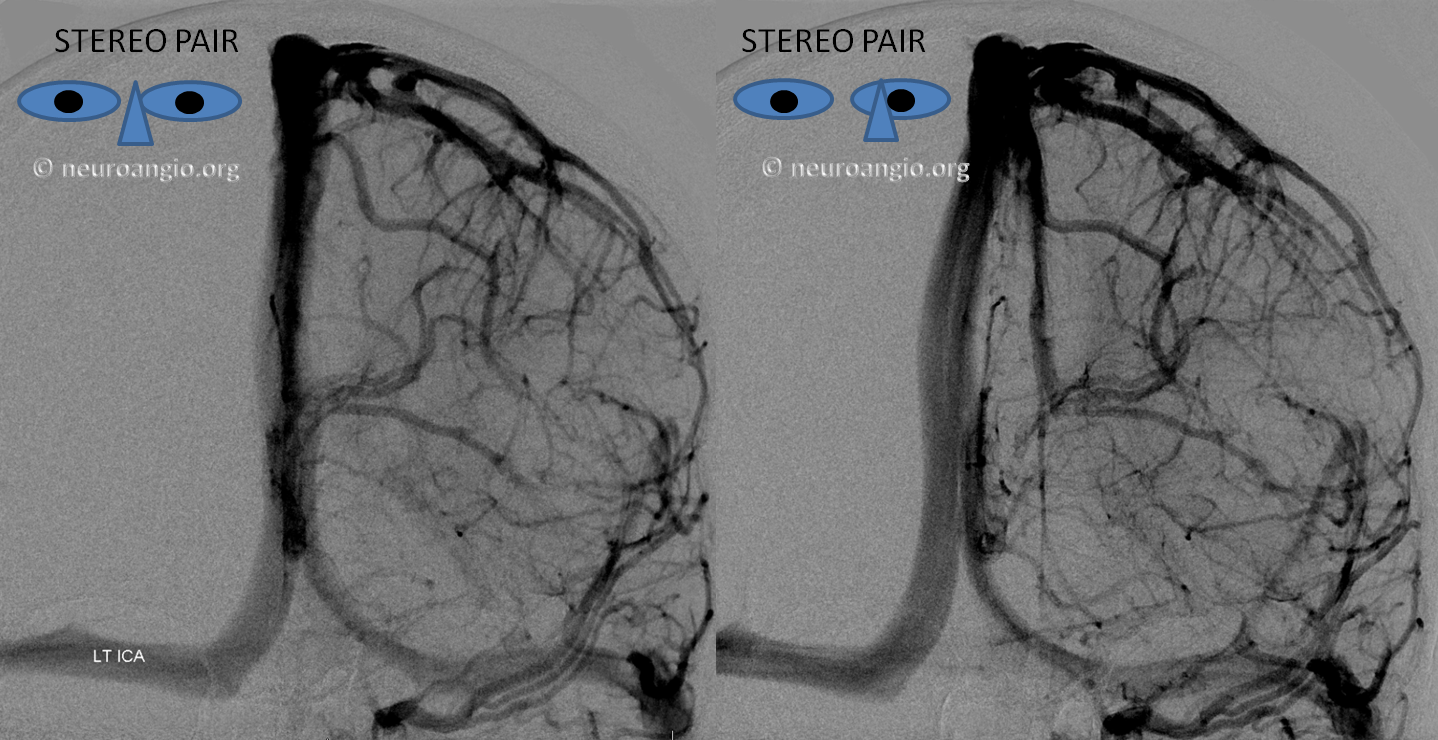
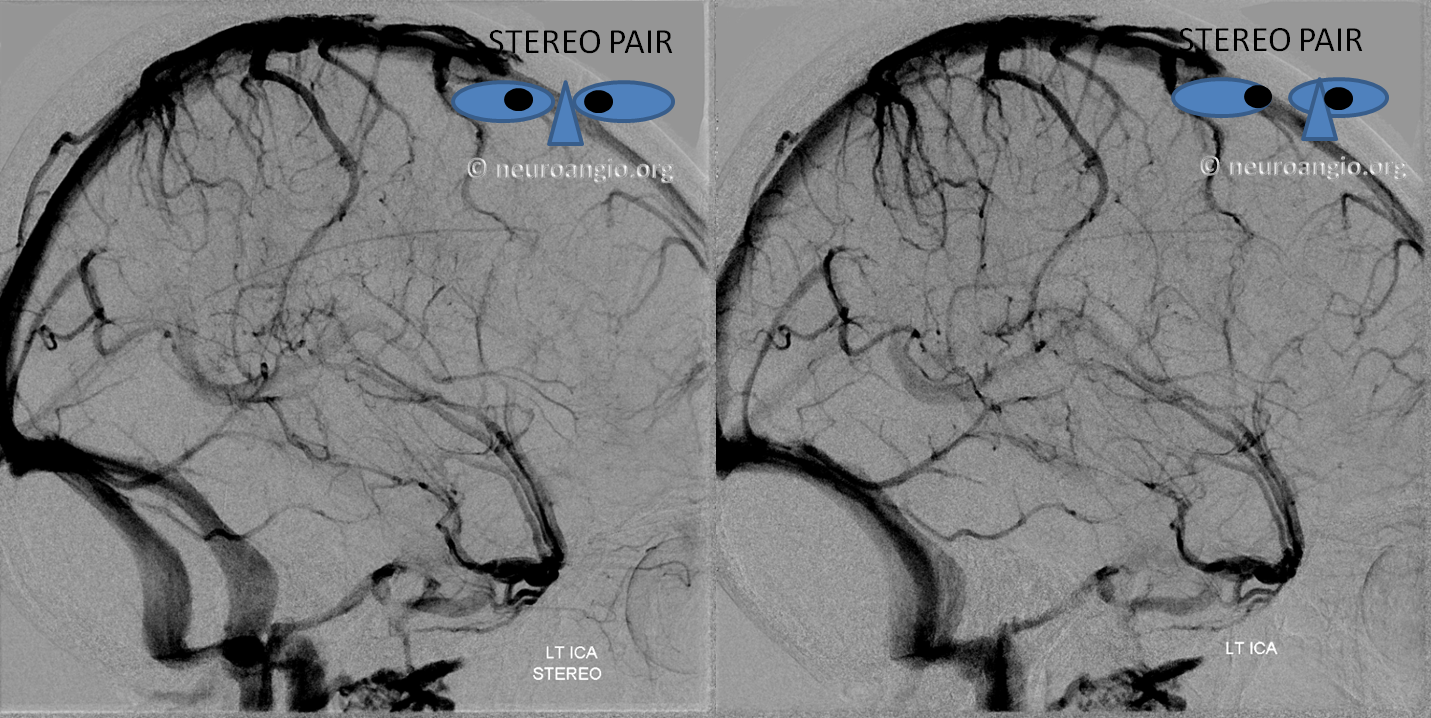
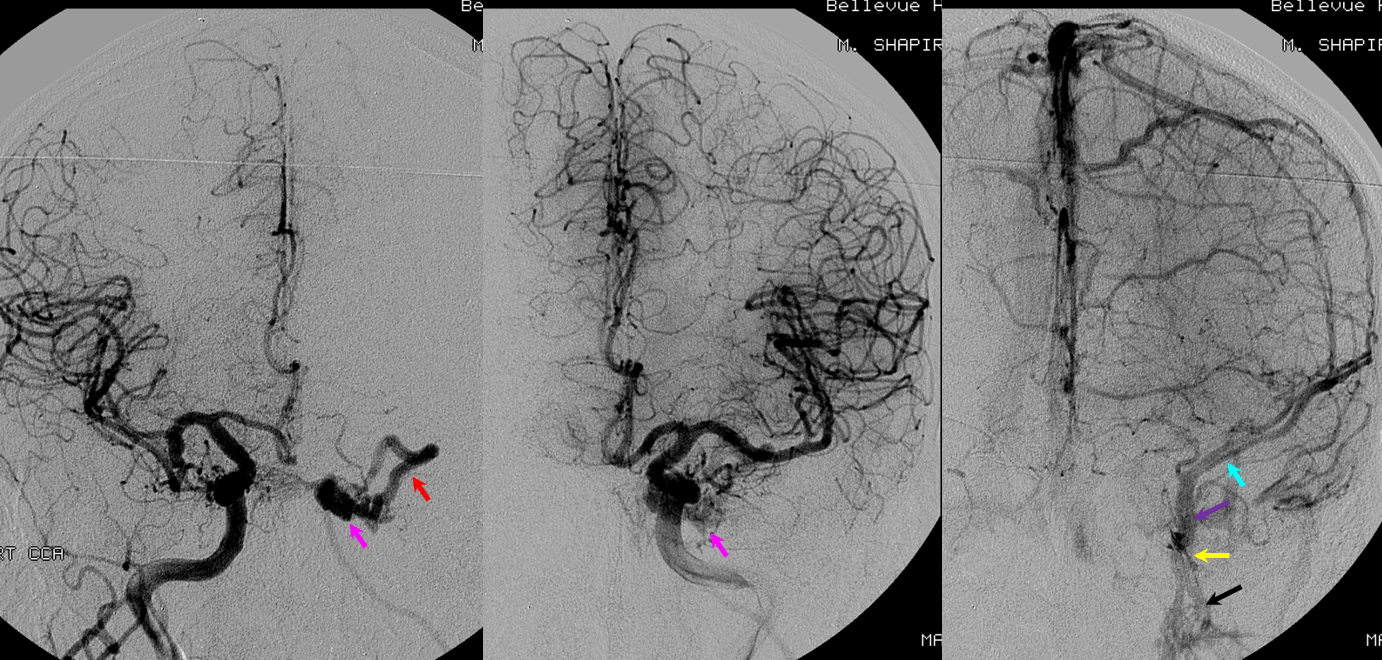
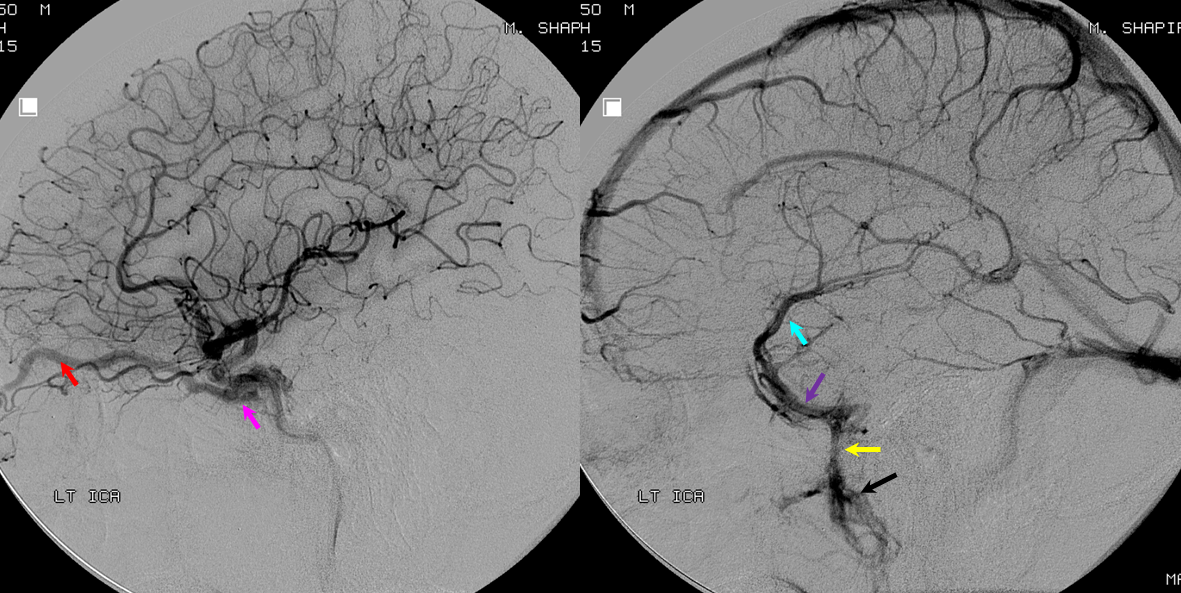
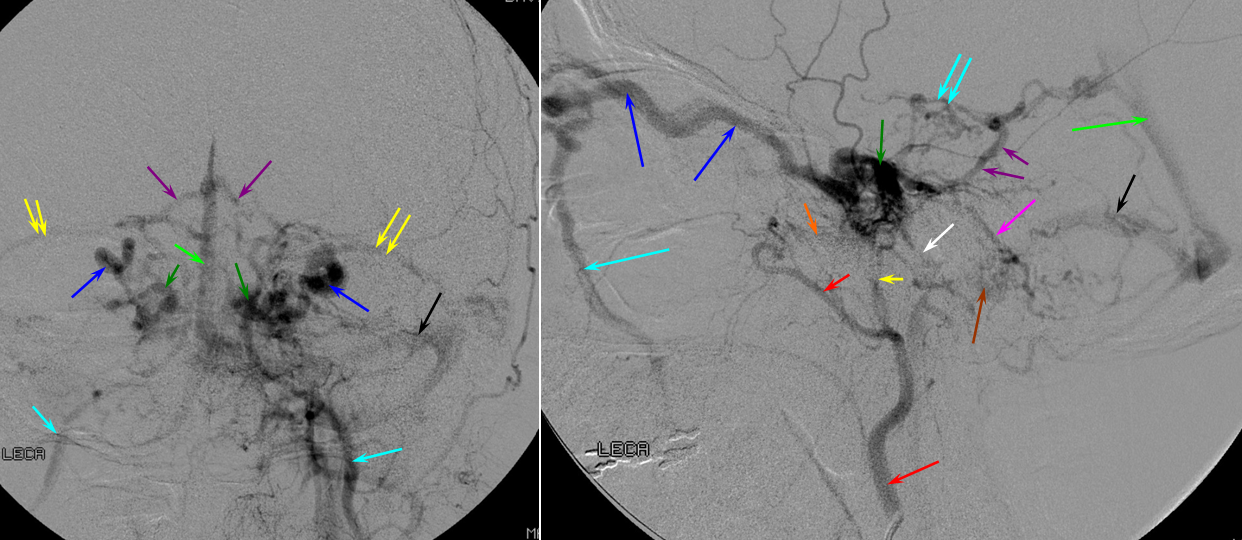
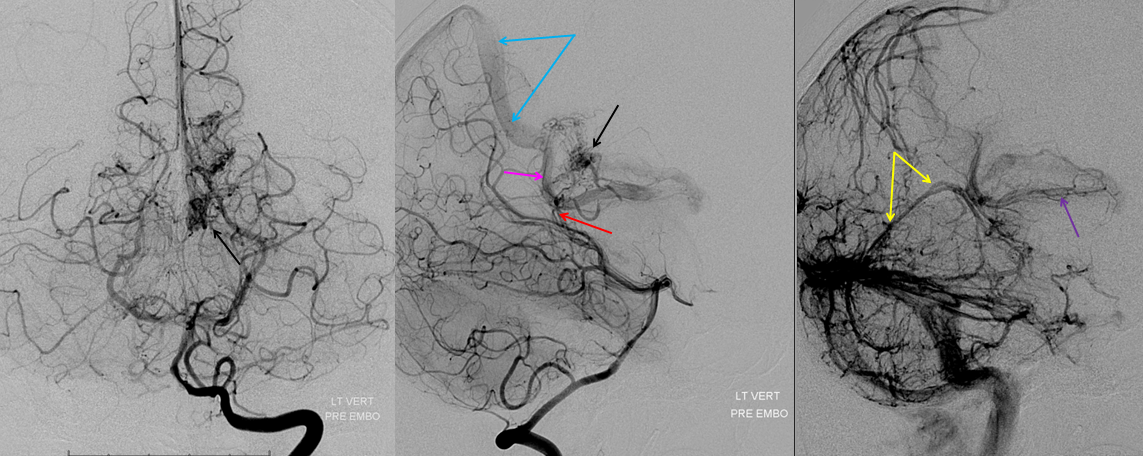
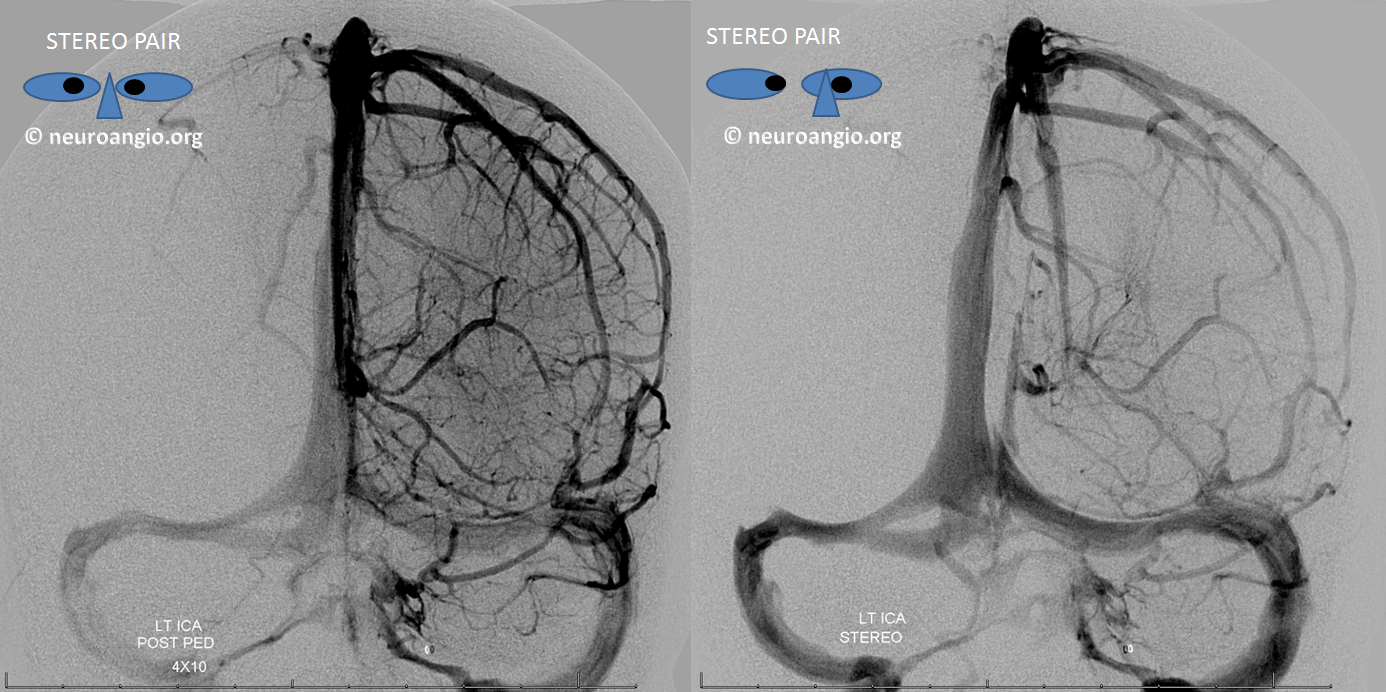
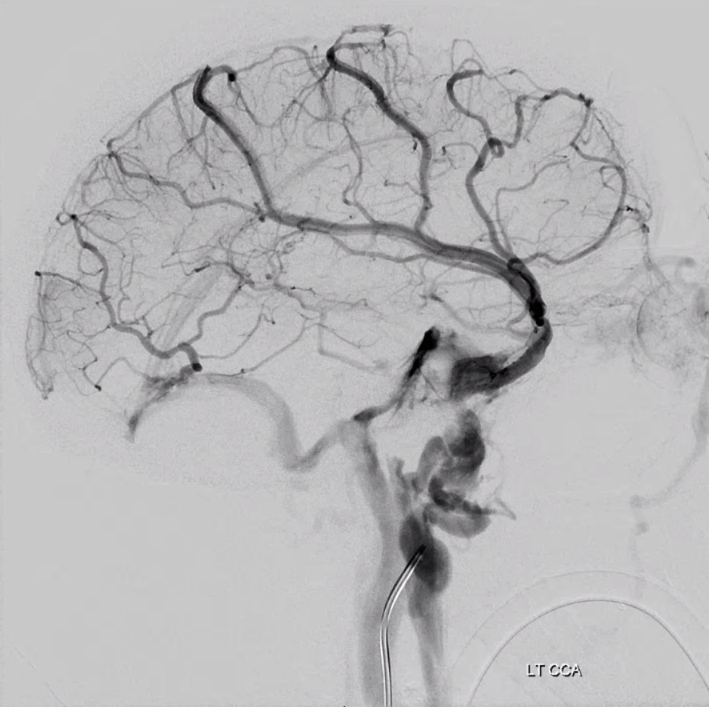
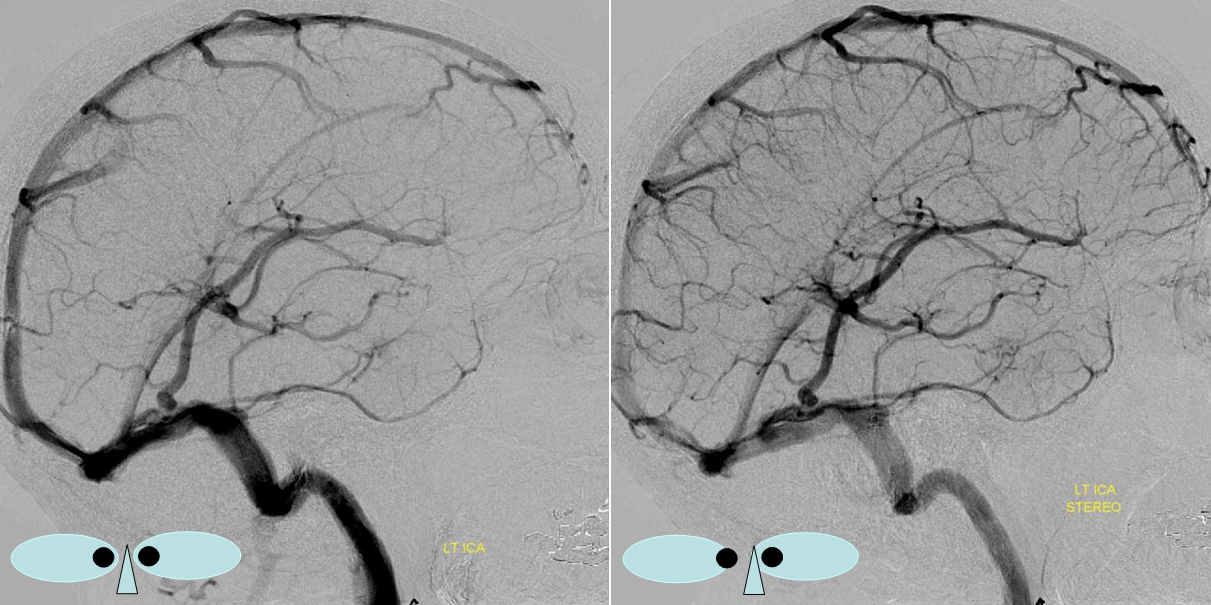
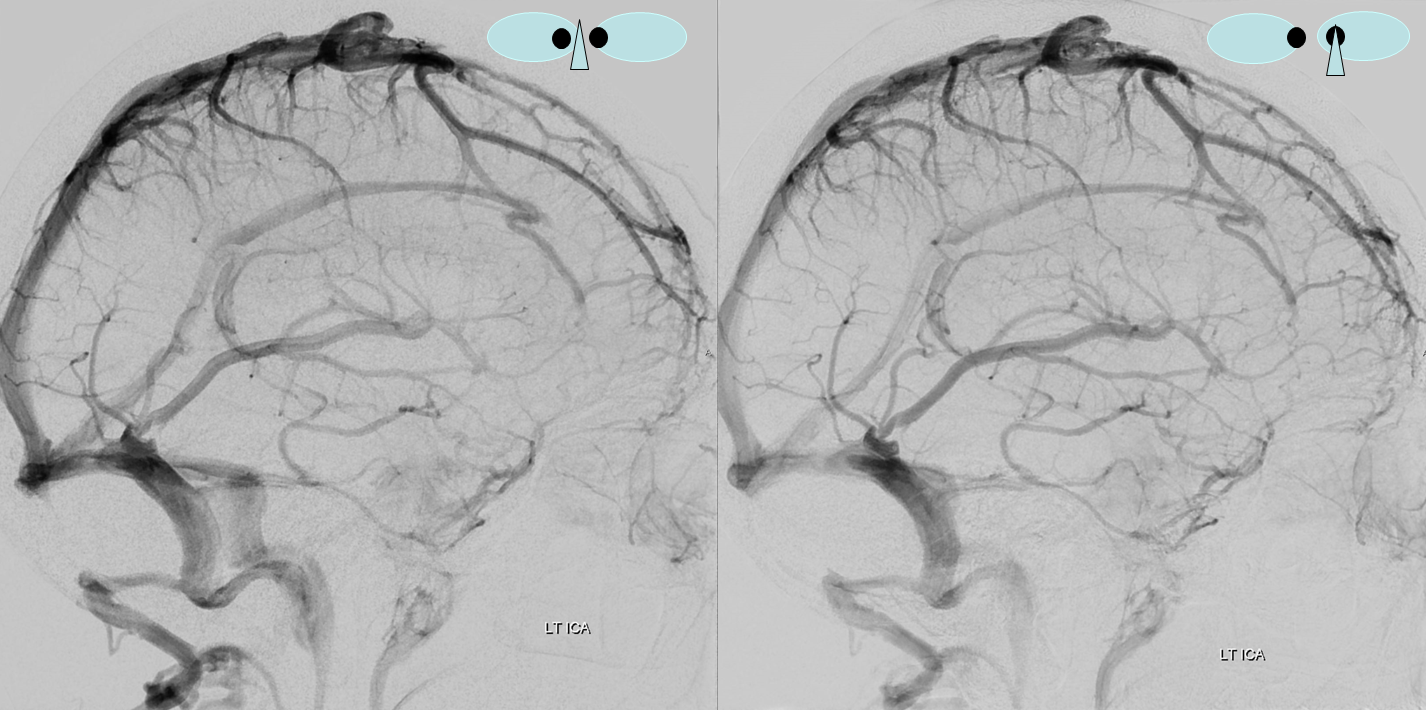
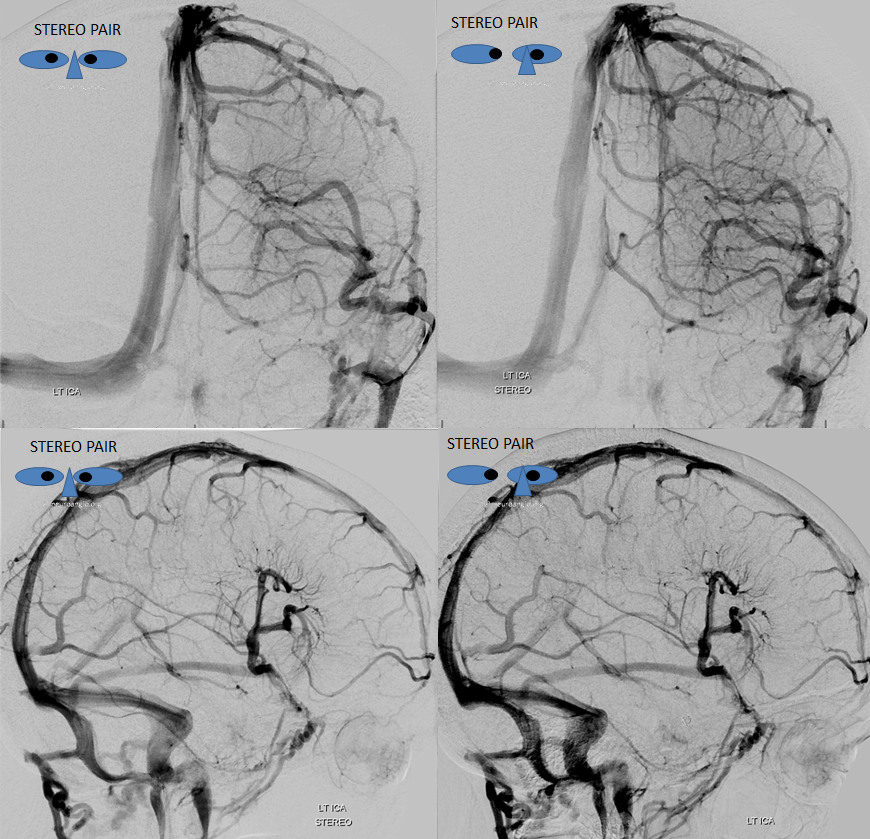
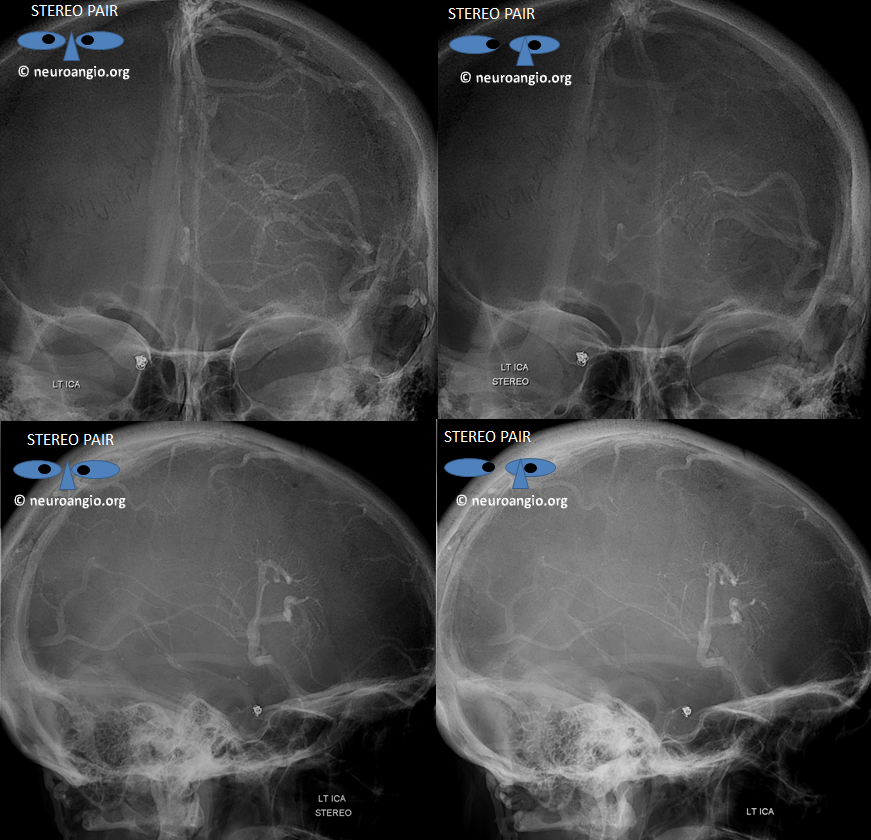
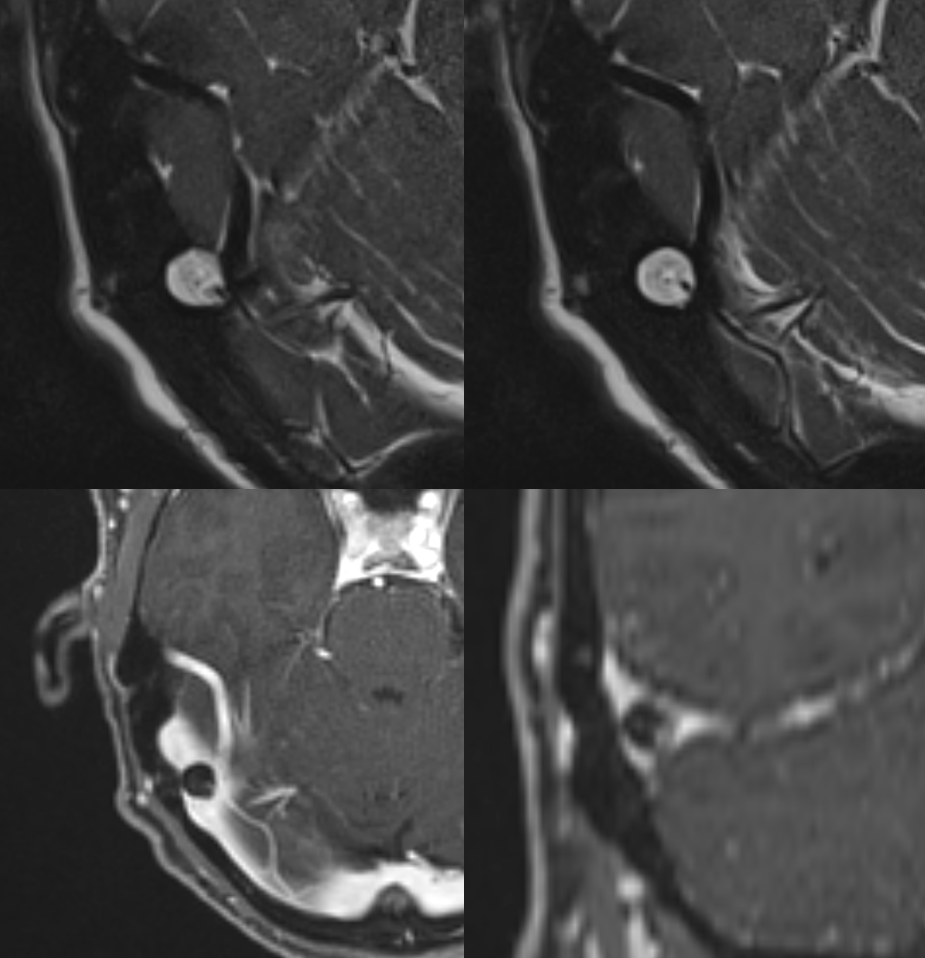
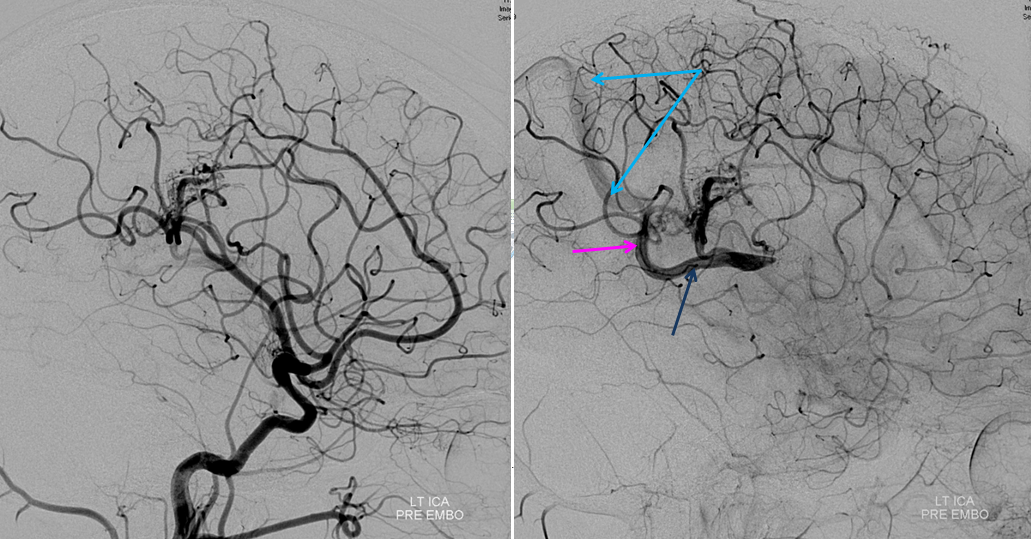 Following embolization, resection, recurrence (as frequently the case with childhood AVMs) and gamma-knife, things look good. Stereo, of course.
Following embolization, resection, recurrence (as frequently the case with childhood AVMs) and gamma-knife, things look good. Stereo, of course.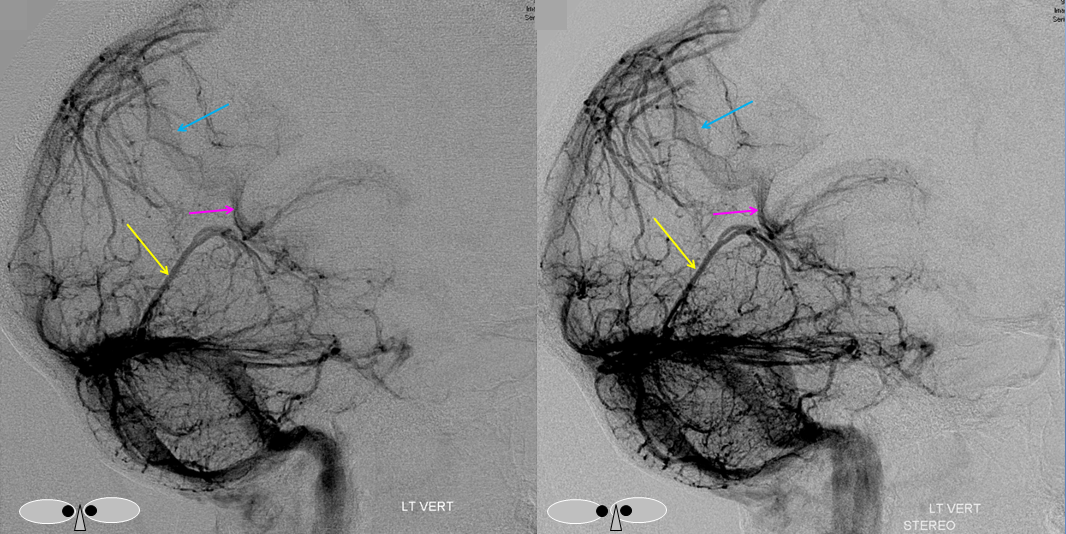
 Emissary Veins
Emissary Veins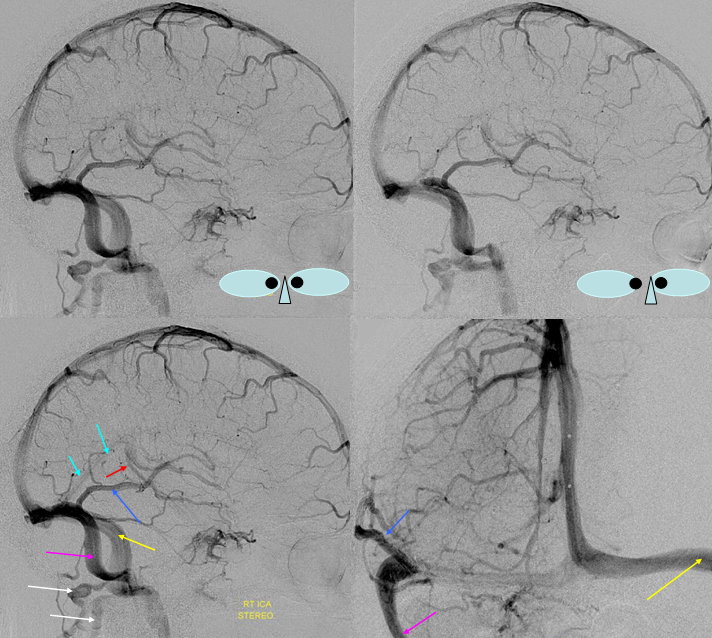 These can sometimes be very prominent, especially when there is associated absence or compression of the jugular vein (this structure can be frequently compressed between the C1 lateral mass and the styloid process). They can become quite efficient. More interesting, perhaps, are the less frequently appreciated but sometimes quite important emissary veins located elsewhere, for example over the frontoparietal convexities. Dry skull specimens sometimes sport a few seemingly random holes on the top, which are emissary foramina for these veins, typically connected to the superior sagittal sinus. The single emissary vein below (white) traverses the skull, marked by its fainter appearane due to skull density. Once part of the scalp, it splits into the ipsilateral (light blue) and contralateral (purple) channels which ultimately empty into the ipsilateral (dark blue) and contralateral (pink) pterygopalatine fossae venous plexuses. The emissary vein can be appreciated without the stereo capability by its course anterior to the sagittal sinus. Since the sagittal sinus is a midline structure, anything anterior to it on a standard lateral projection has to be either intra-osseous or trans-osseous.
These can sometimes be very prominent, especially when there is associated absence or compression of the jugular vein (this structure can be frequently compressed between the C1 lateral mass and the styloid process). They can become quite efficient. More interesting, perhaps, are the less frequently appreciated but sometimes quite important emissary veins located elsewhere, for example over the frontoparietal convexities. Dry skull specimens sometimes sport a few seemingly random holes on the top, which are emissary foramina for these veins, typically connected to the superior sagittal sinus. The single emissary vein below (white) traverses the skull, marked by its fainter appearane due to skull density. Once part of the scalp, it splits into the ipsilateral (light blue) and contralateral (purple) channels which ultimately empty into the ipsilateral (dark blue) and contralateral (pink) pterygopalatine fossae venous plexuses. The emissary vein can be appreciated without the stereo capability by its course anterior to the sagittal sinus. Since the sagittal sinus is a midline structure, anything anterior to it on a standard lateral projection has to be either intra-osseous or trans-osseous.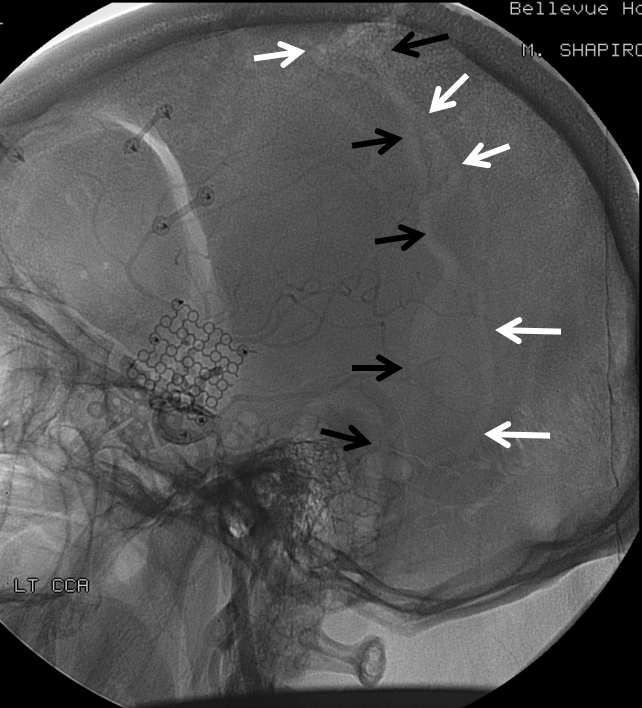
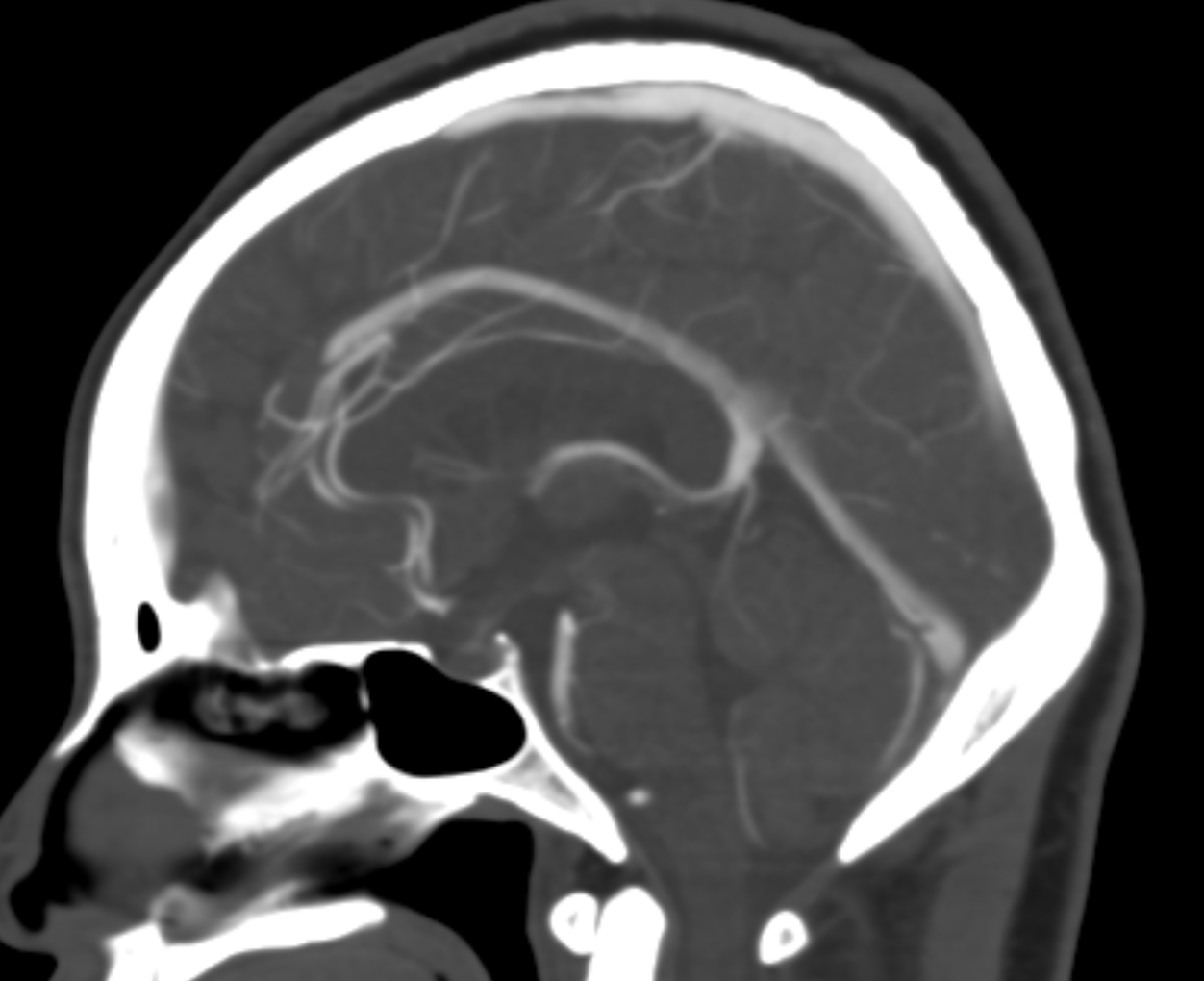
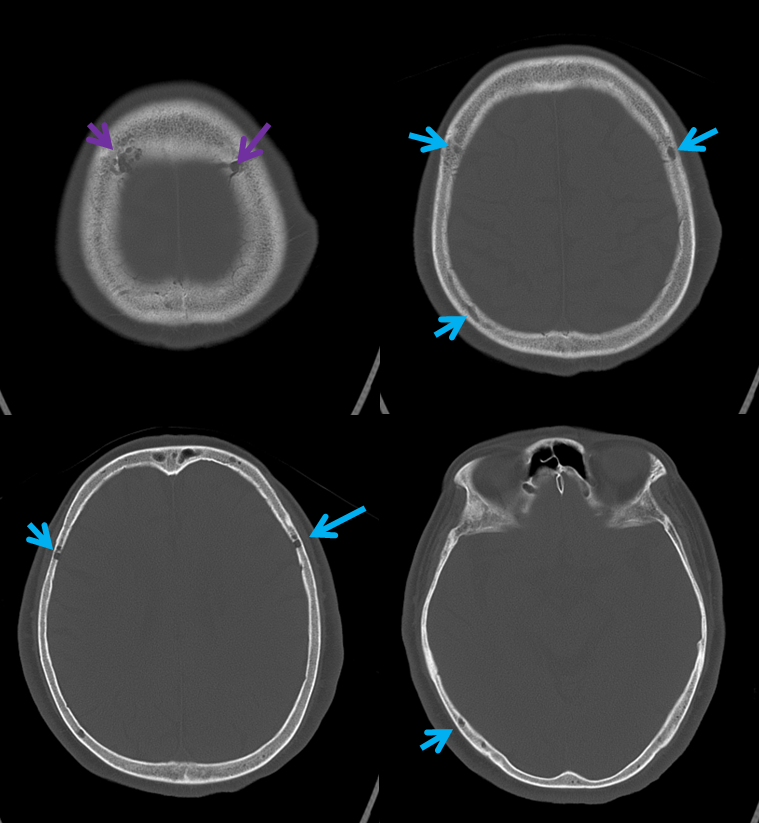 A poorly timed, venous phase CTA shows small caliber of sagital sinus
A poorly timed, venous phase CTA shows small caliber of sagital sinus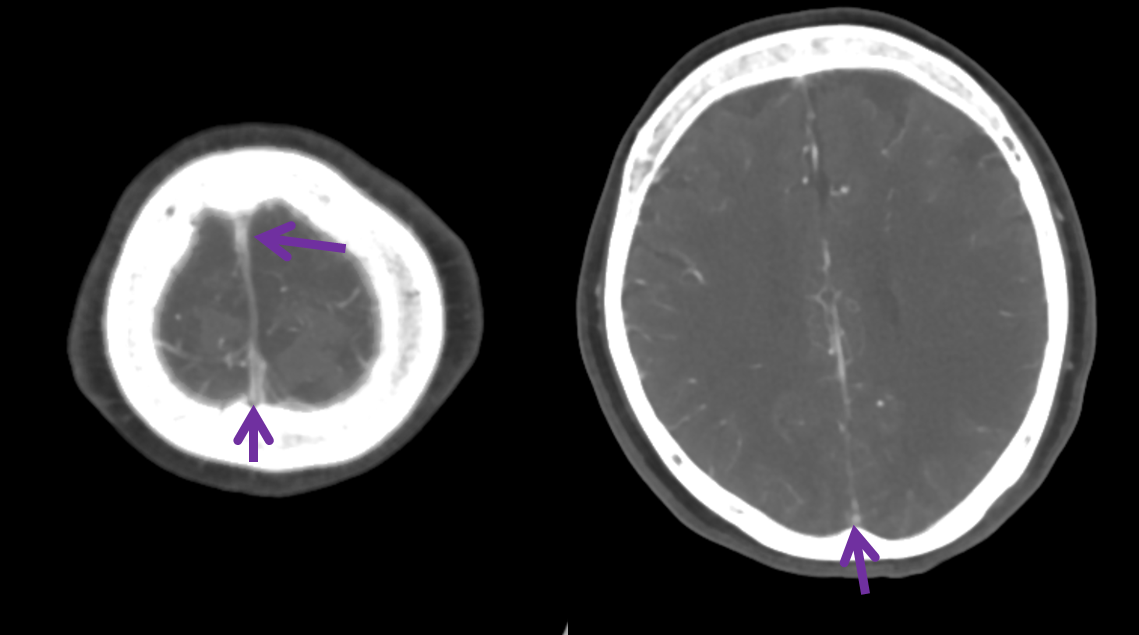
The best alternative is often the Cavernous Sinus, since it represents a completely different venous system. With Sigmoid or Transverse sinus thrombosis, if the torcular is spared, the SSS is another effective route. You get the idea. Convexity veins can be interconnected or not. The more interconnected they are, the better off the situation will be. See “Superficial Venous System” Page for more info.
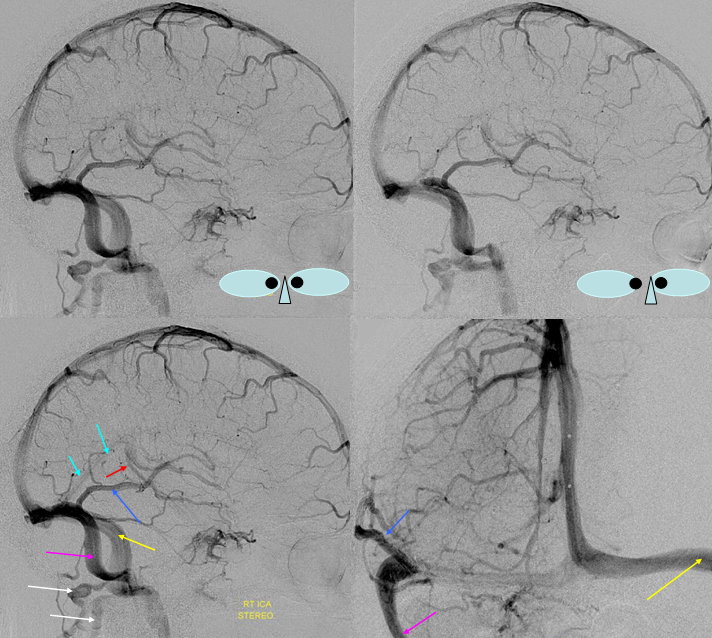
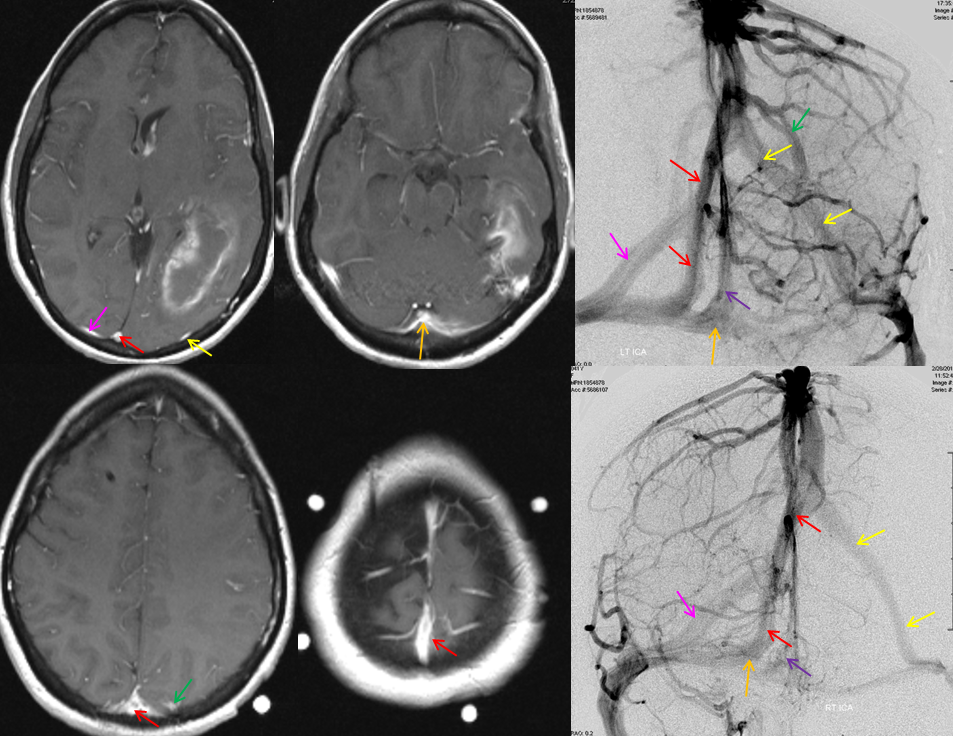
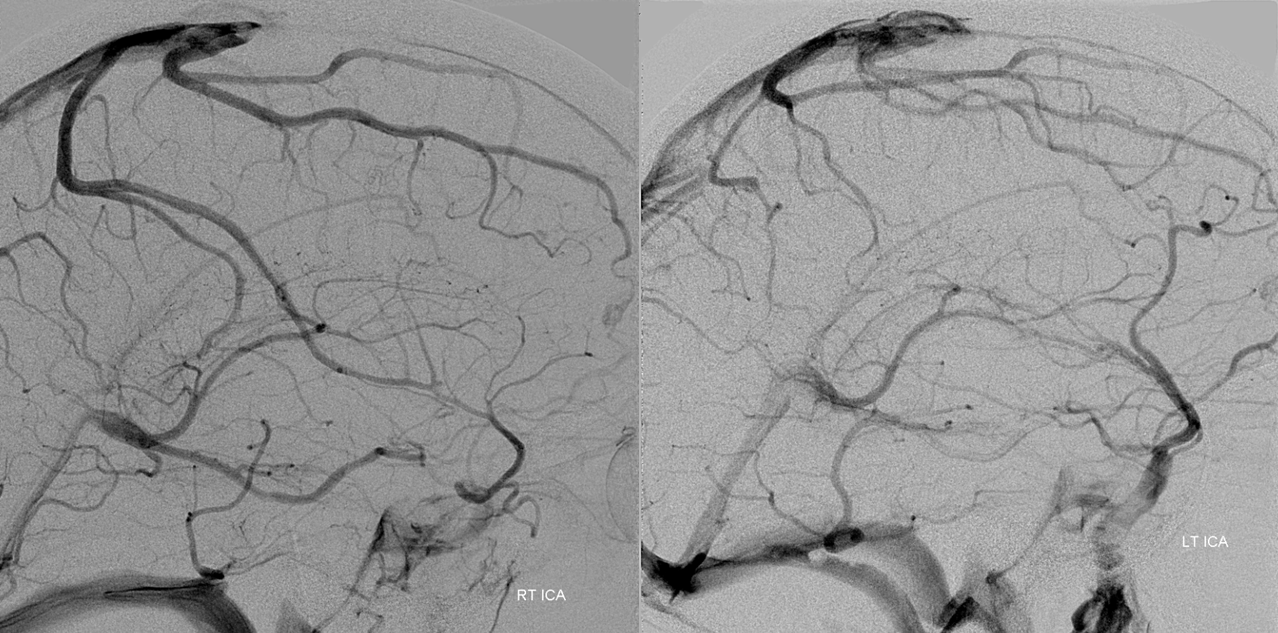
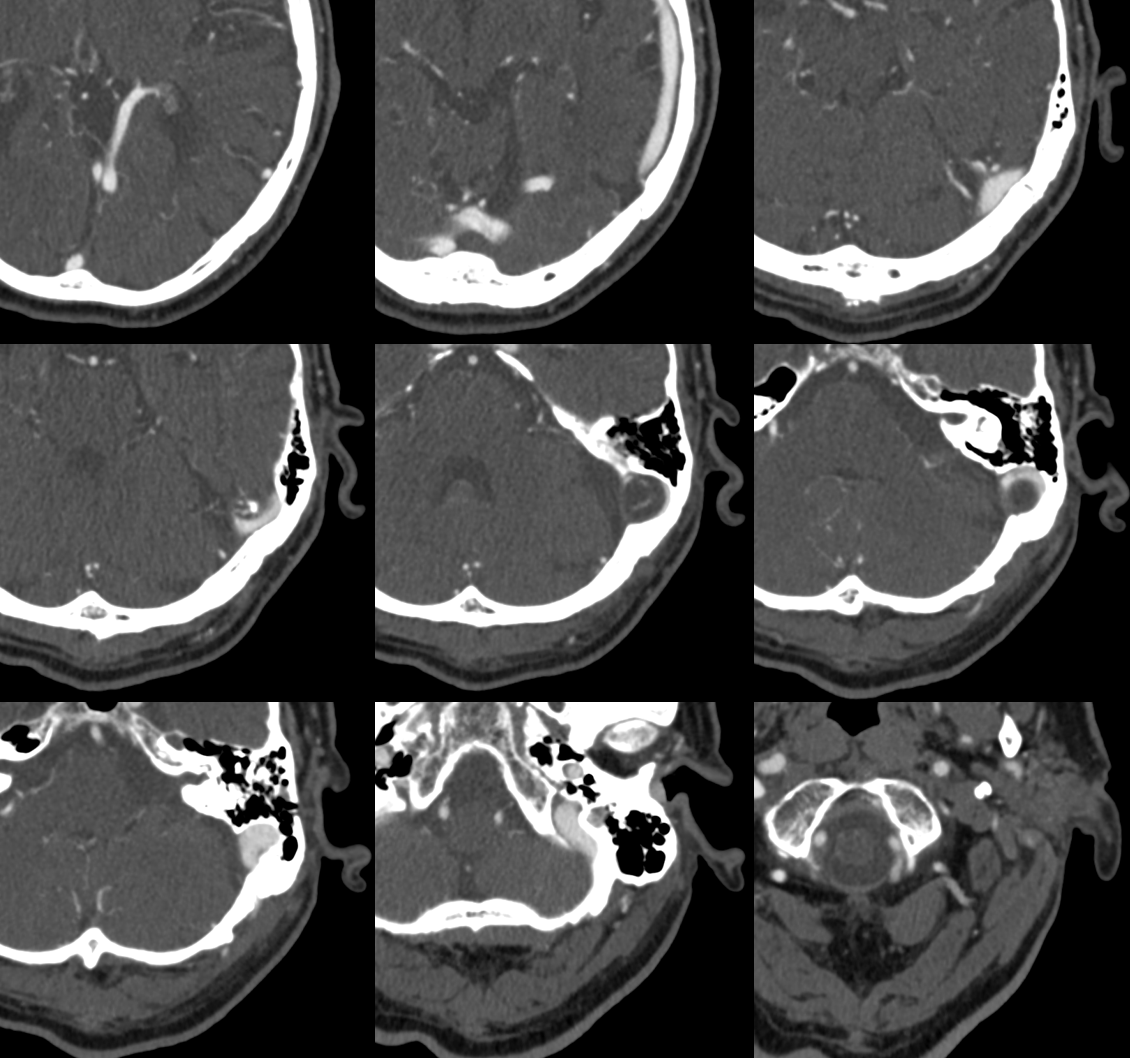
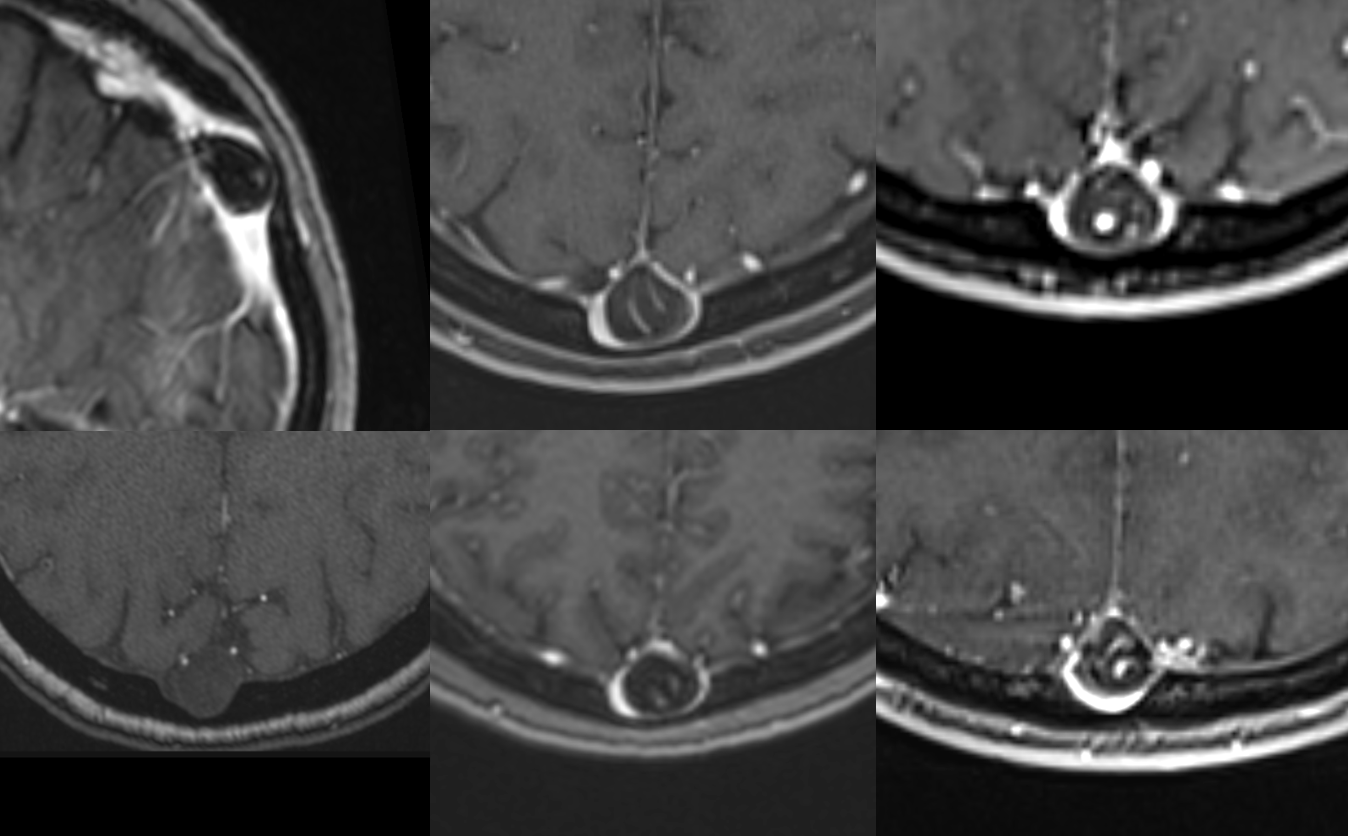
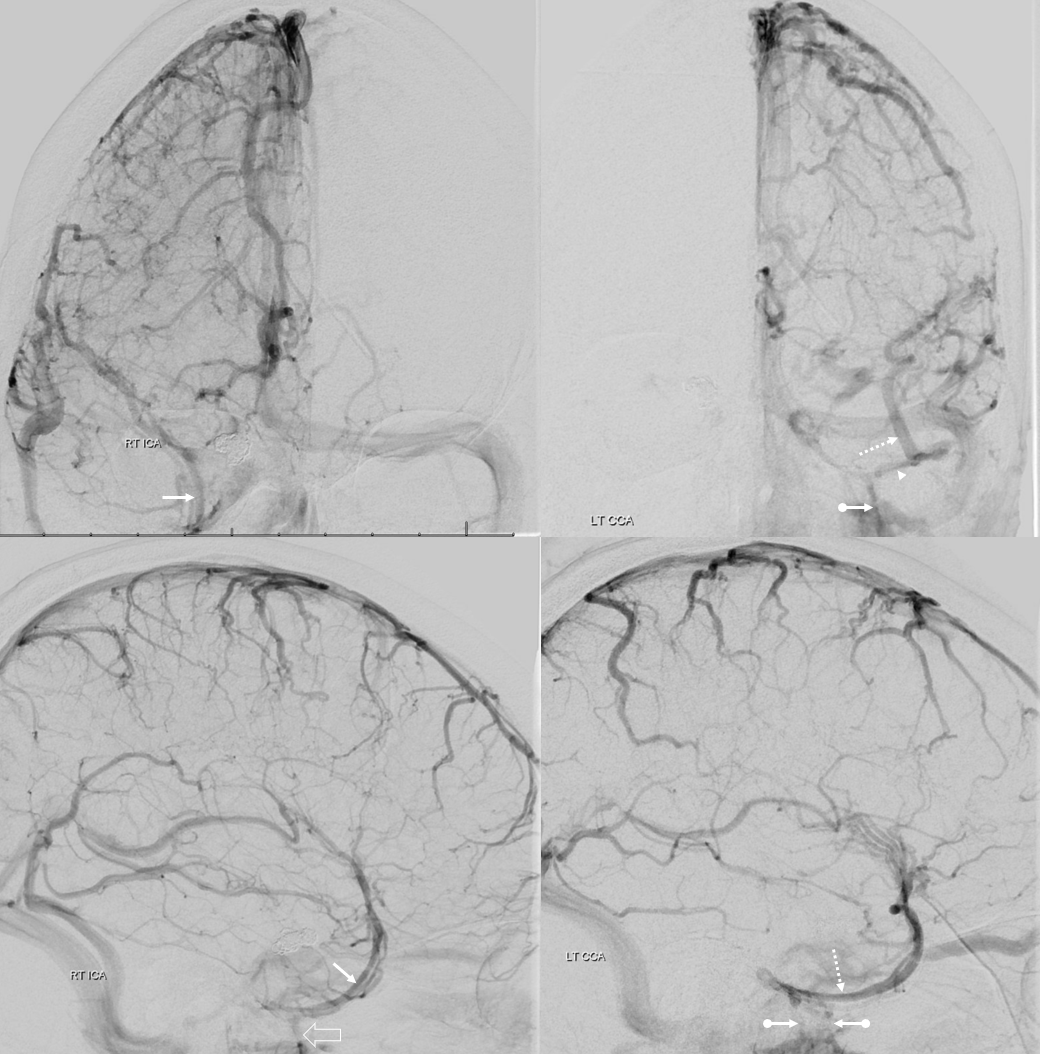
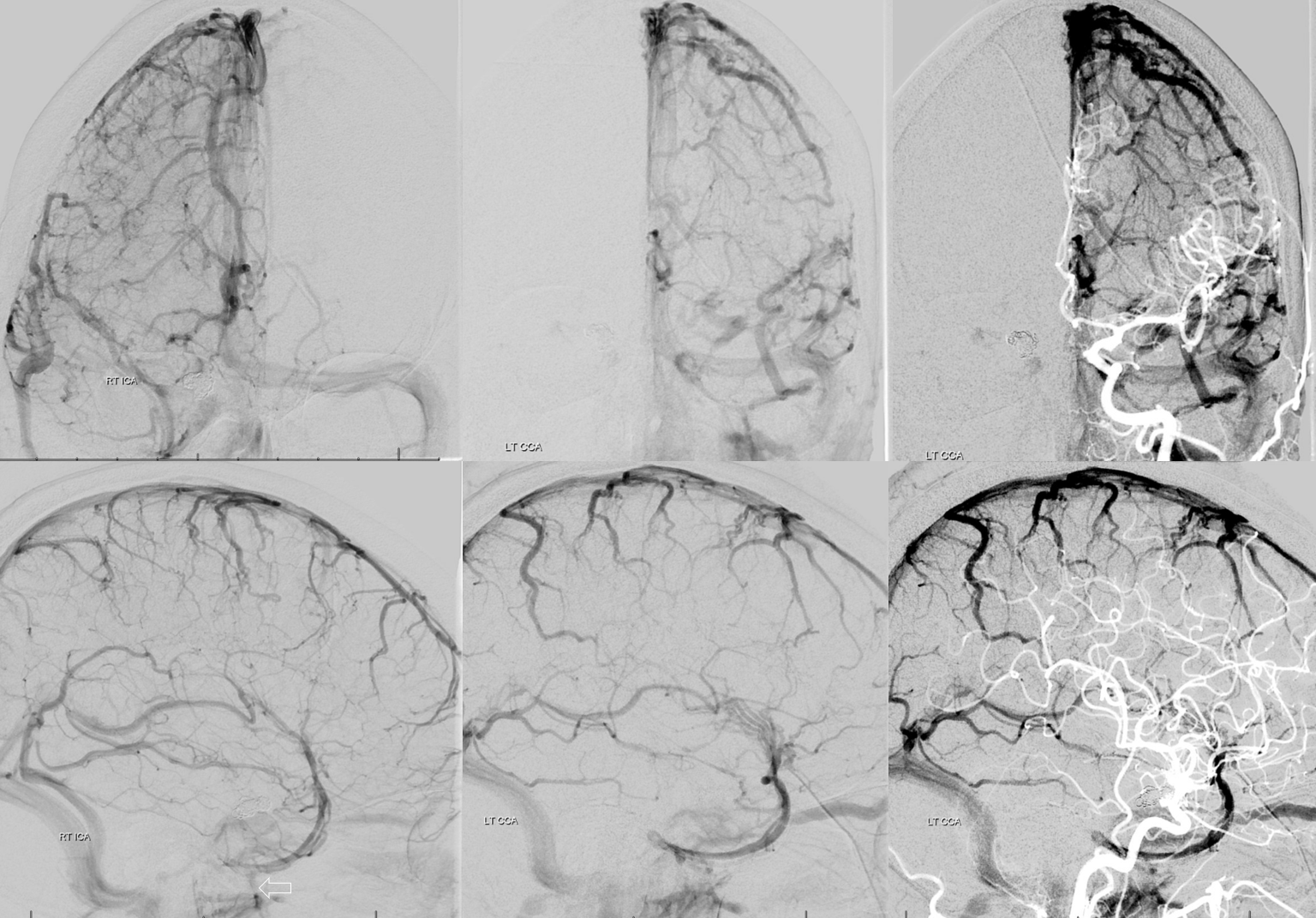
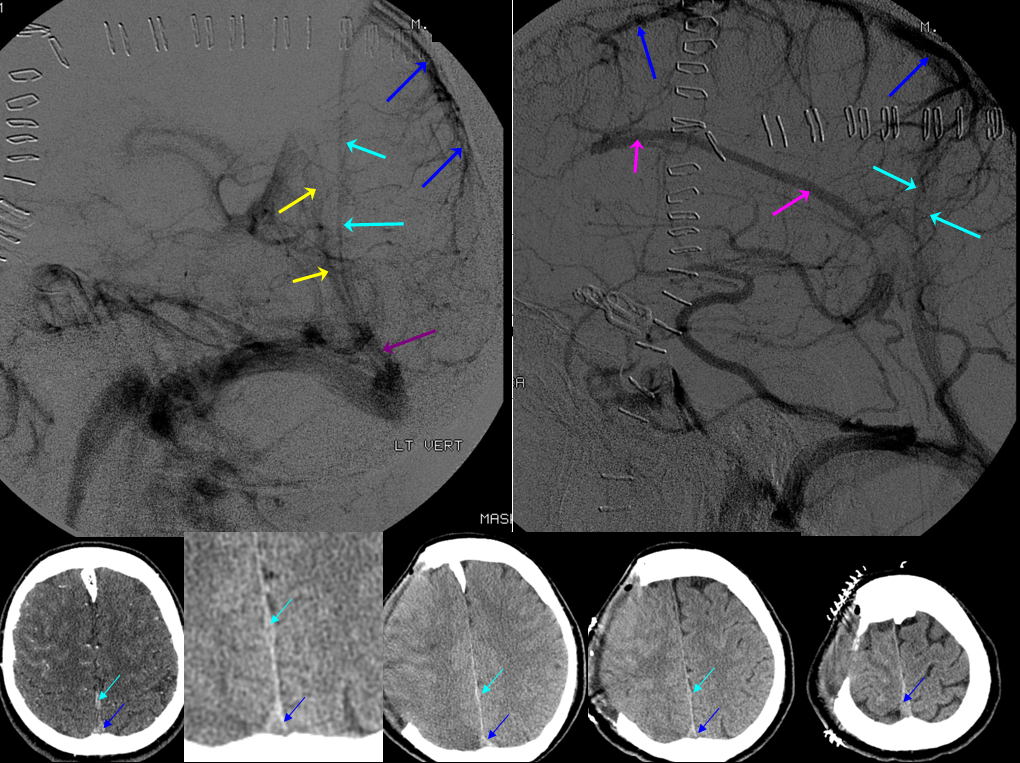
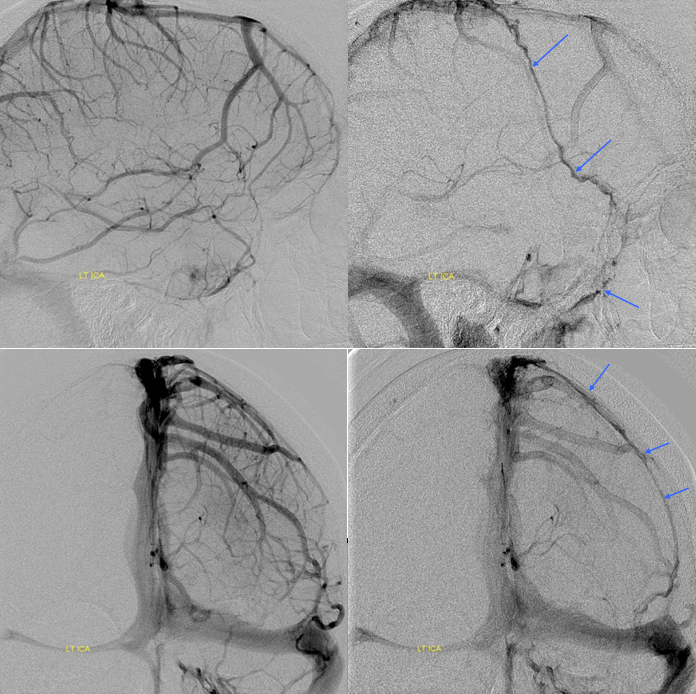
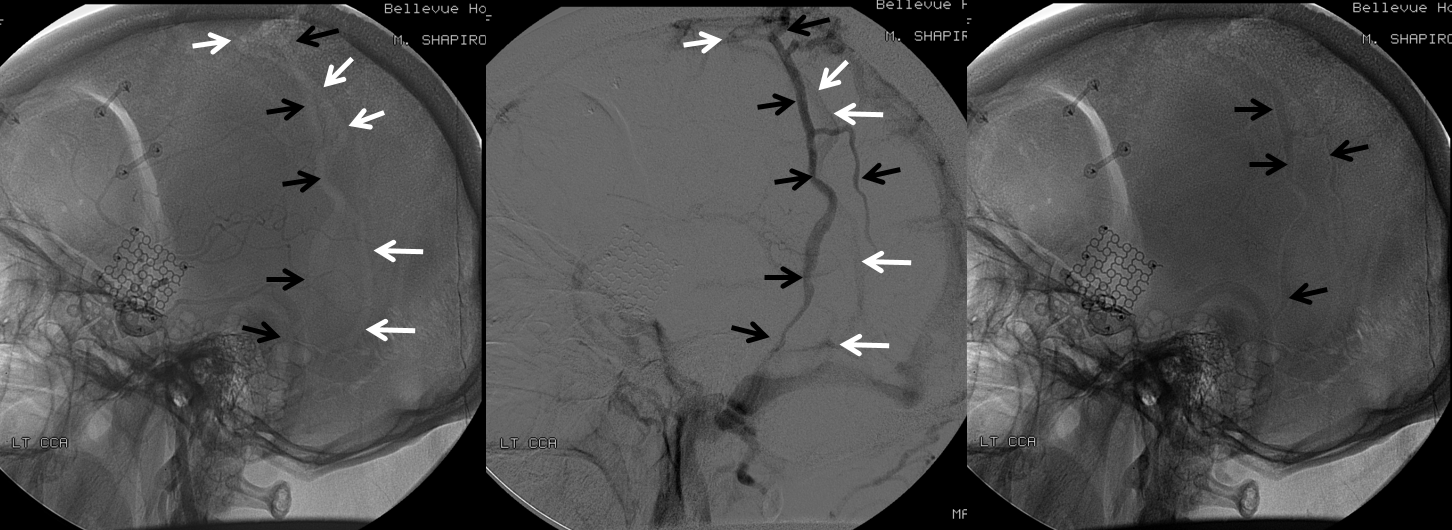
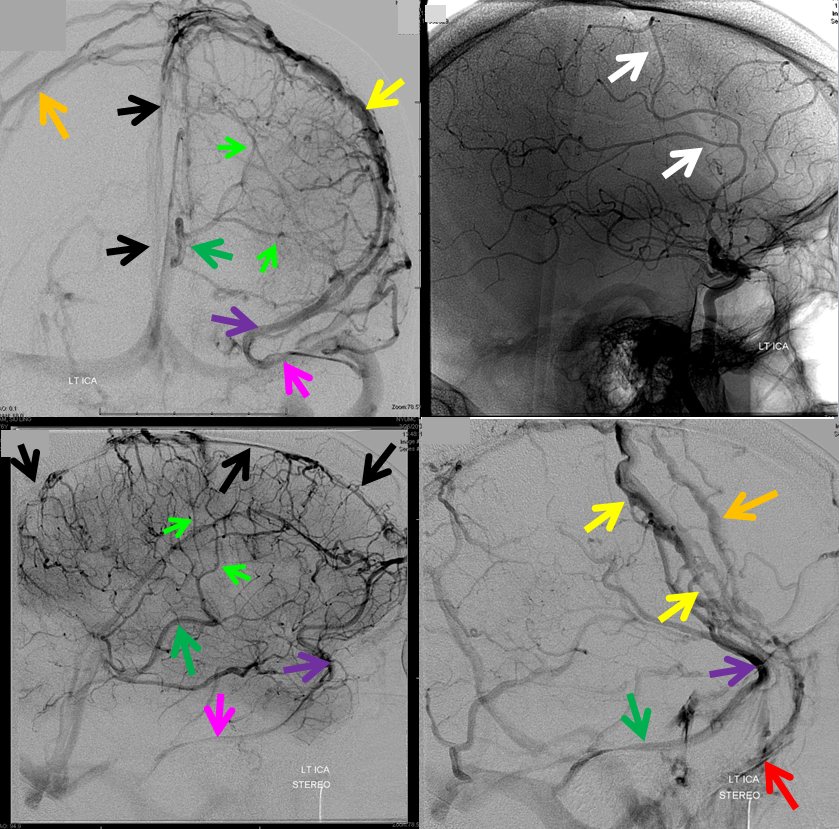
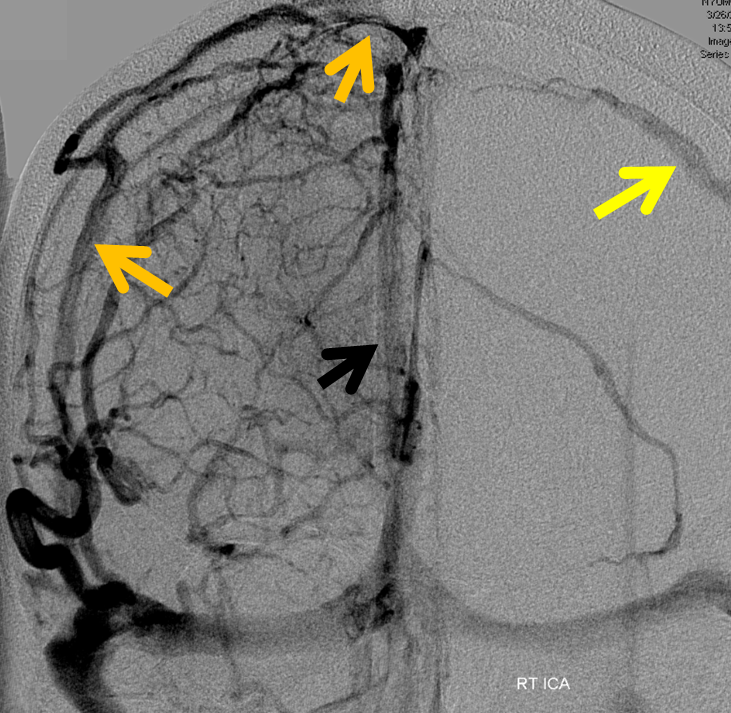
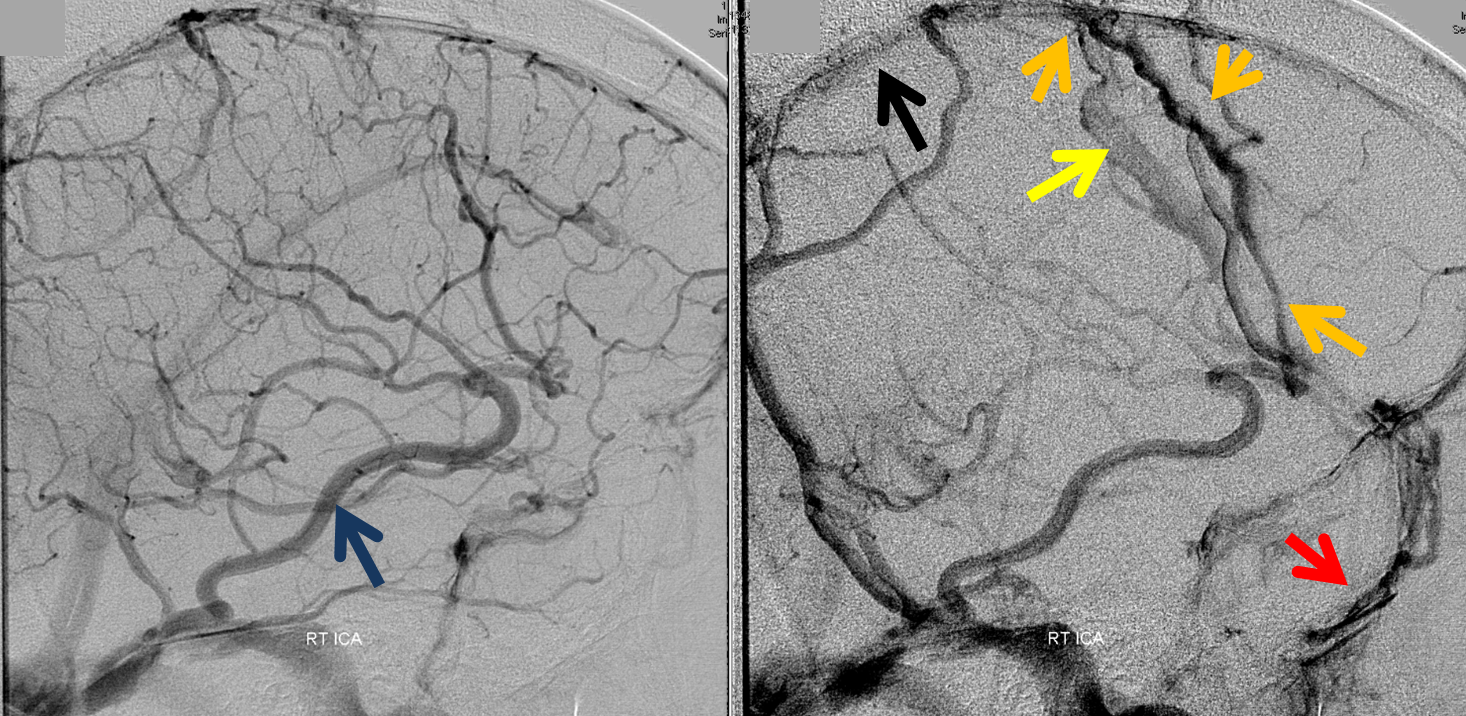
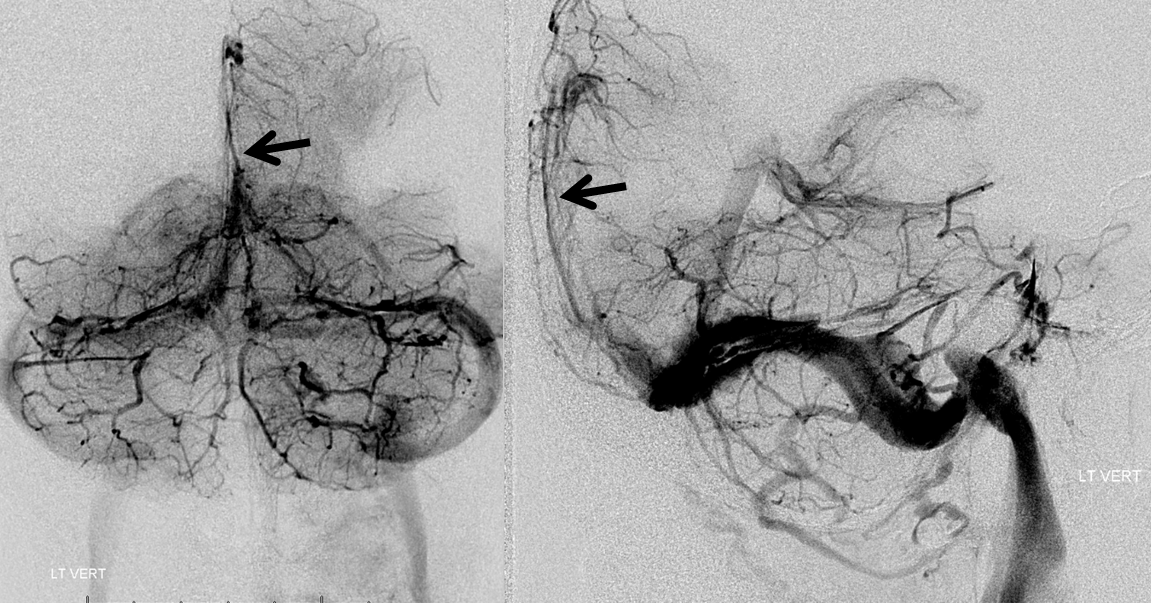
Below is a case of severe venous sinus thrombosis and secondary parenchymal venous infarcts
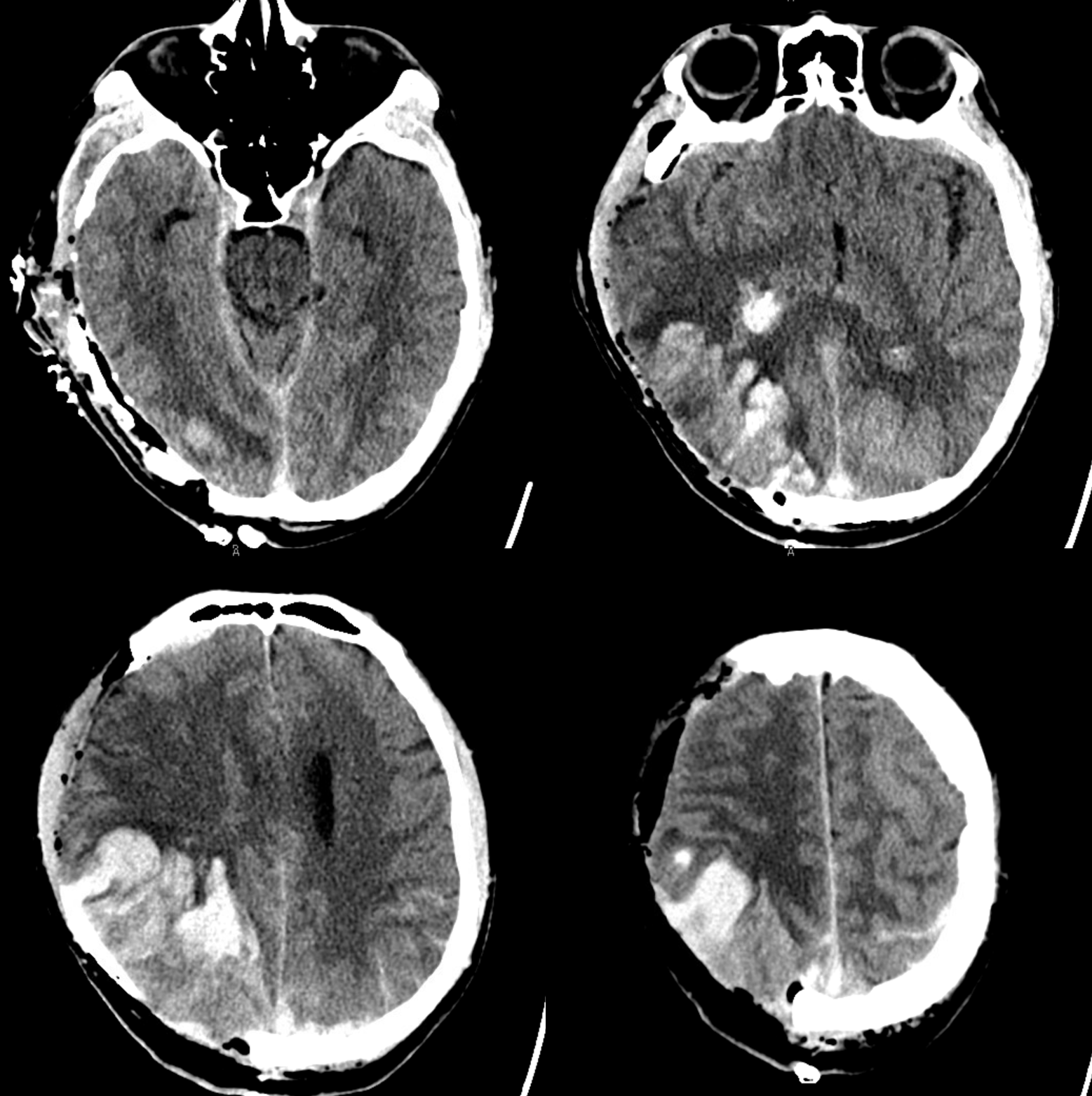
The explanation for the above tragic pattern is below. On the right, sigmoid and transverse sinuses are patent. However, the Labbe is hypoplastic, and majority of outflow used to go to the Trolard, into the now occluded SSS. There is no other effective way to go — the trolard tries to decompress via a left diploic vein, and convexity tries to access the deep venous system (which normally should not be well-seen in setting of hypoplastic right A1 segment). The left situation is much better, as well-developed superficial sylvian veins drain into the patent Cavernous Sinus. Thus, despite thrombosis of the left transverse and sigmoid sinuses, the left hemisphere is doing better, while the right one, which has patent transverse and sigmoid sinuses, is devastated.
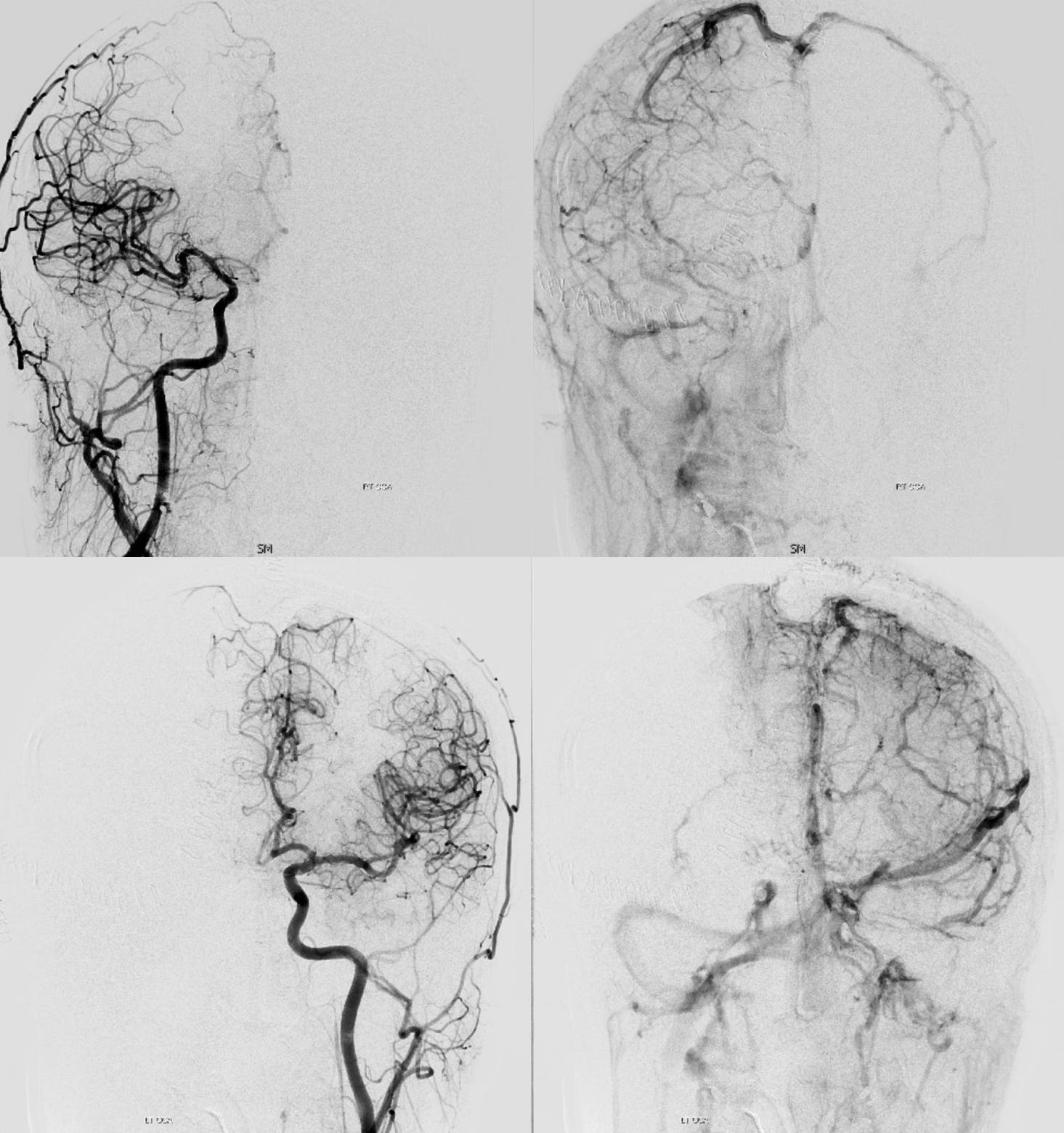
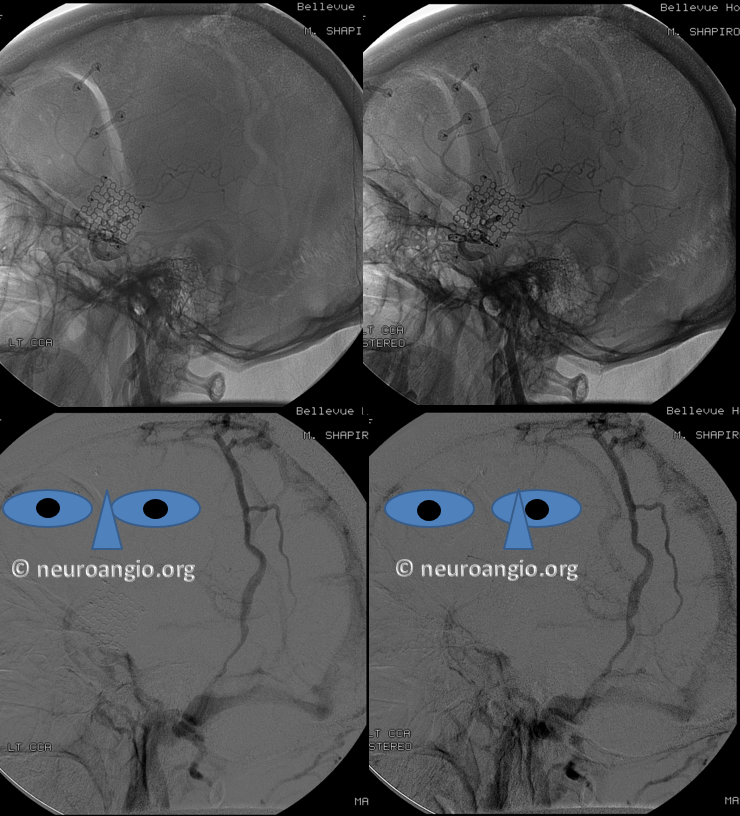
Post venous thrombectomy — with limited results. Note presence of same left diploic vein as seen in right ICA injection, and connection between the distal superior sagittal sinus and the deep venous system via the inferior sagittal sinus.
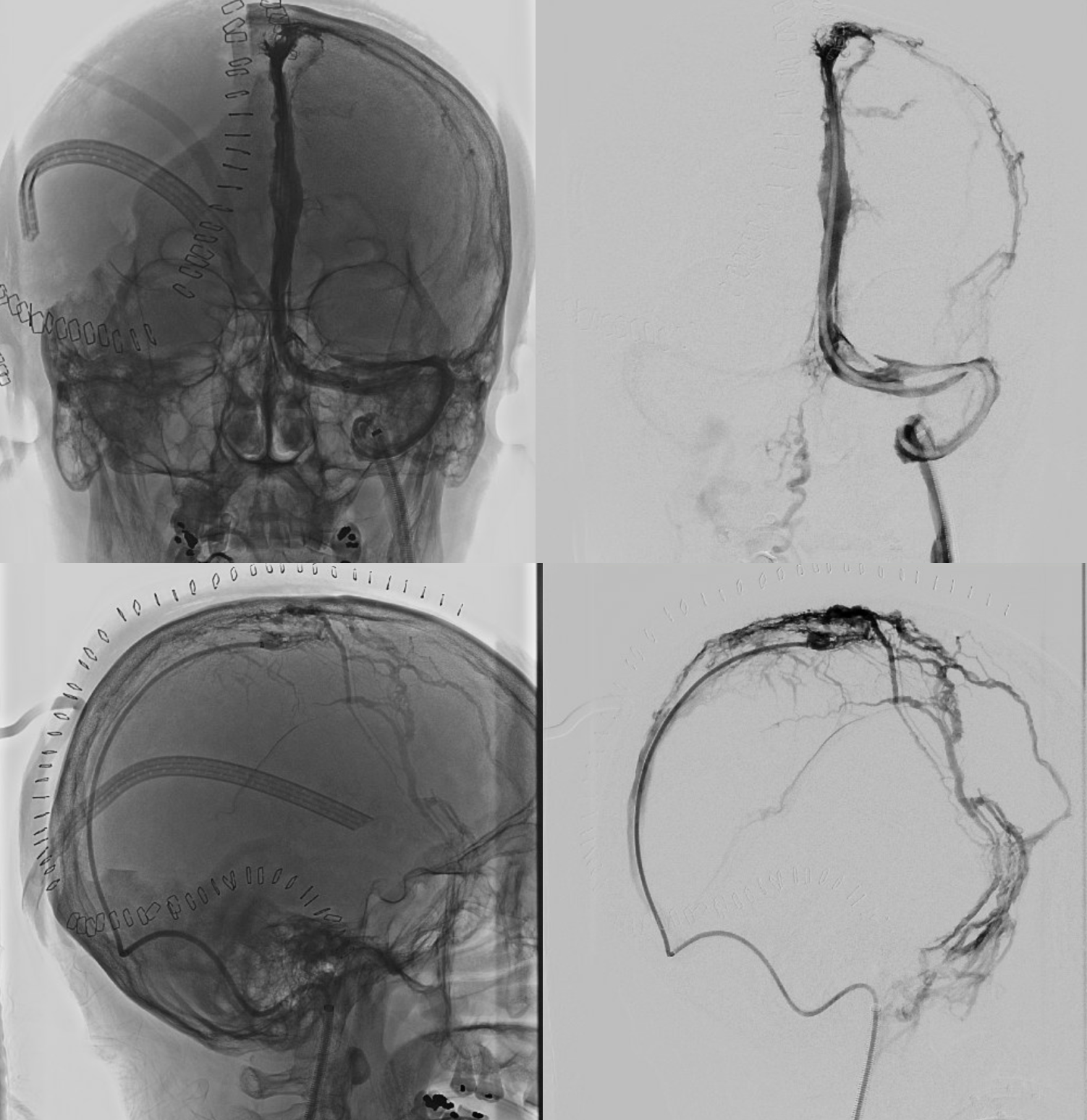
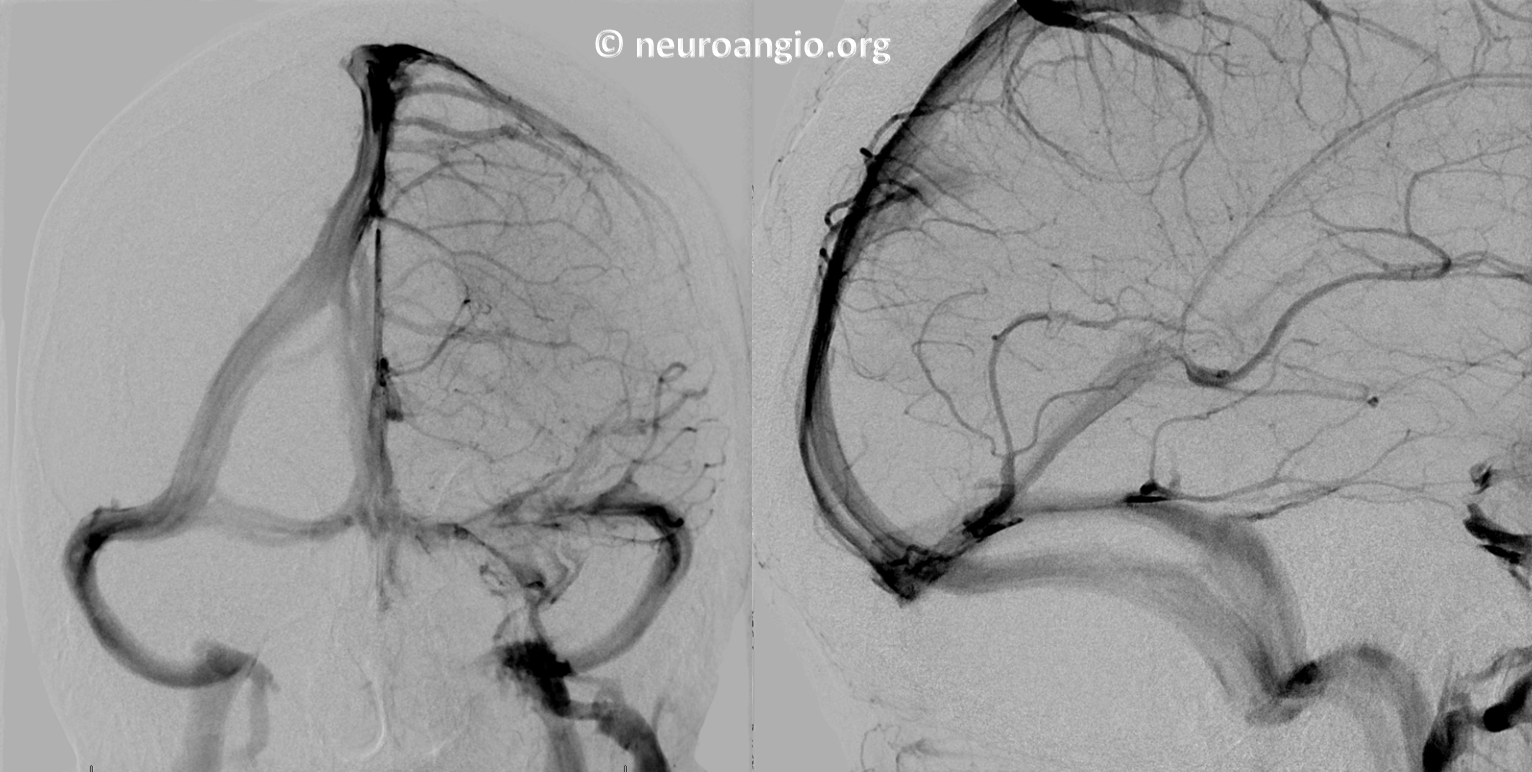
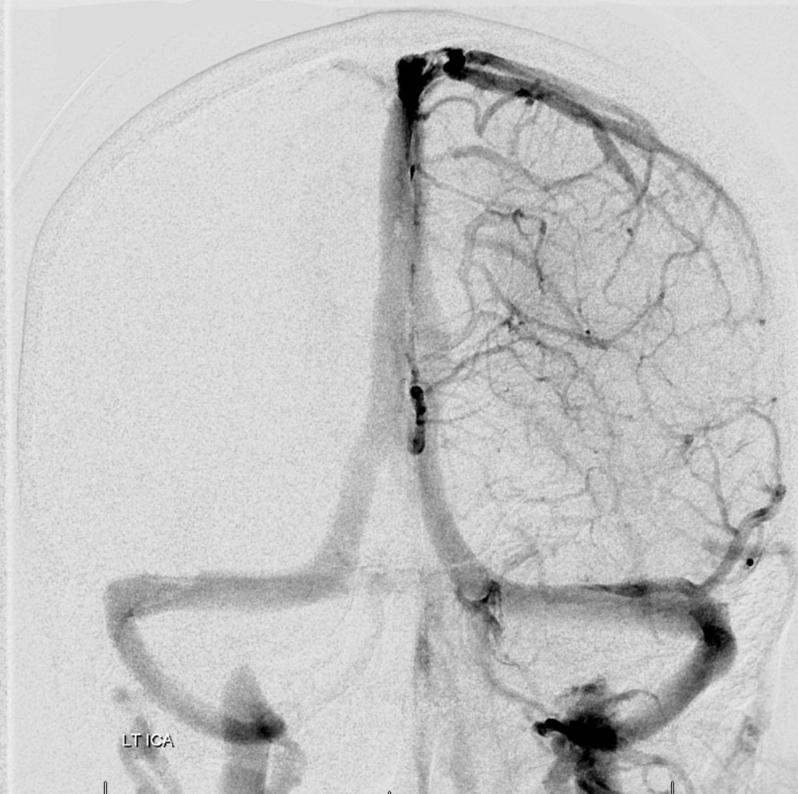
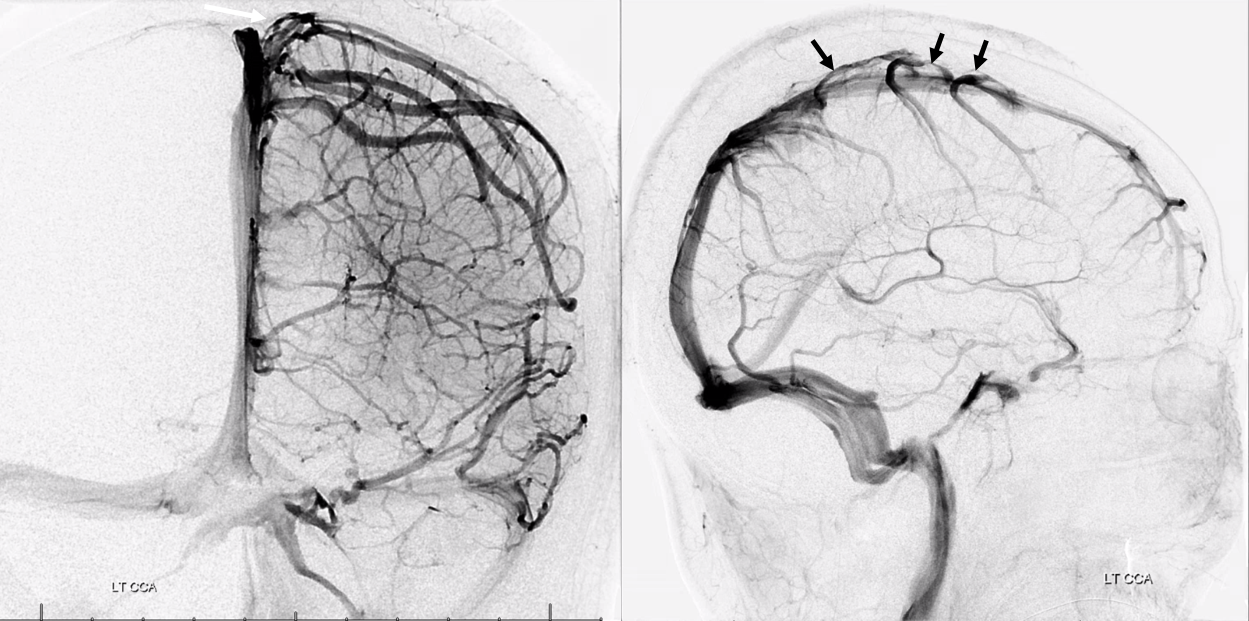
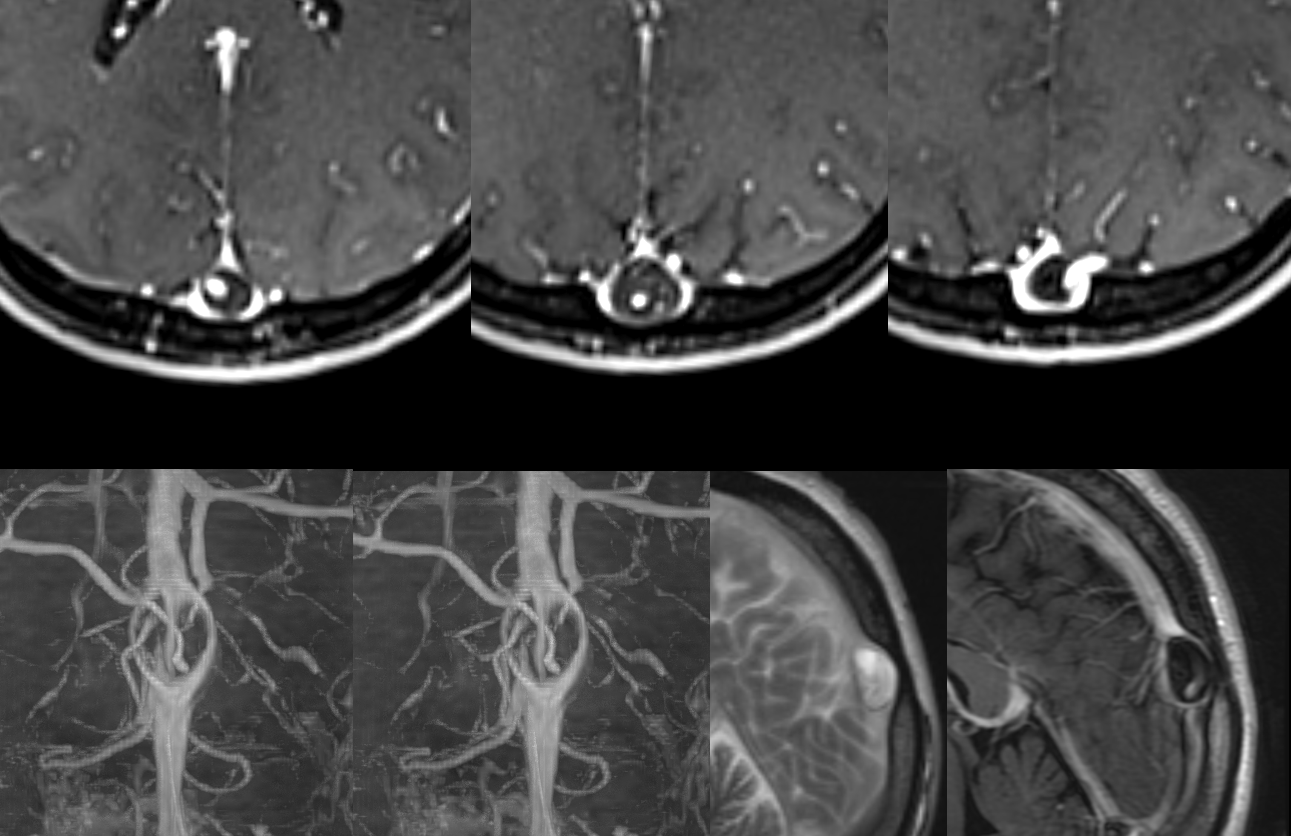
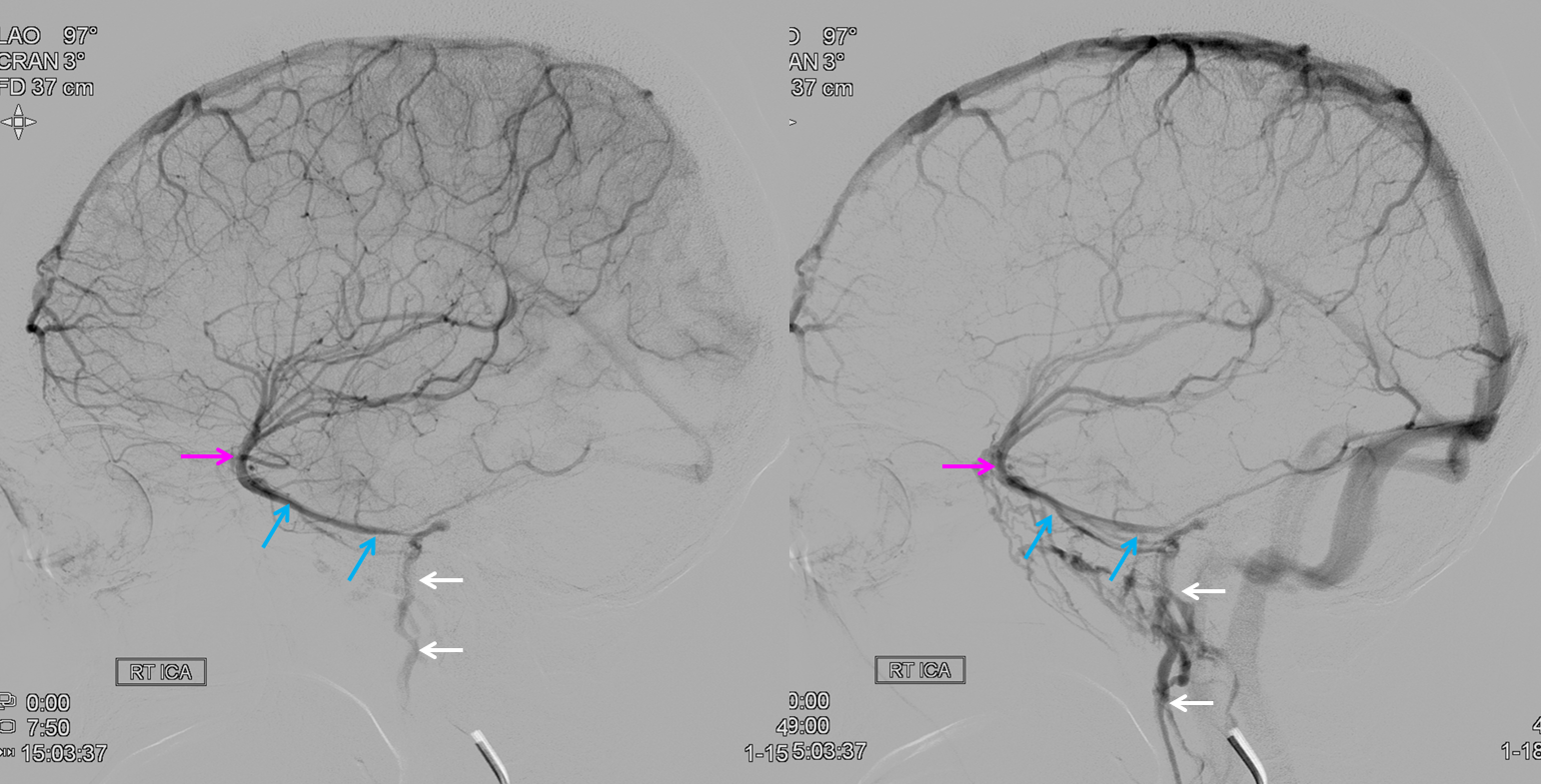
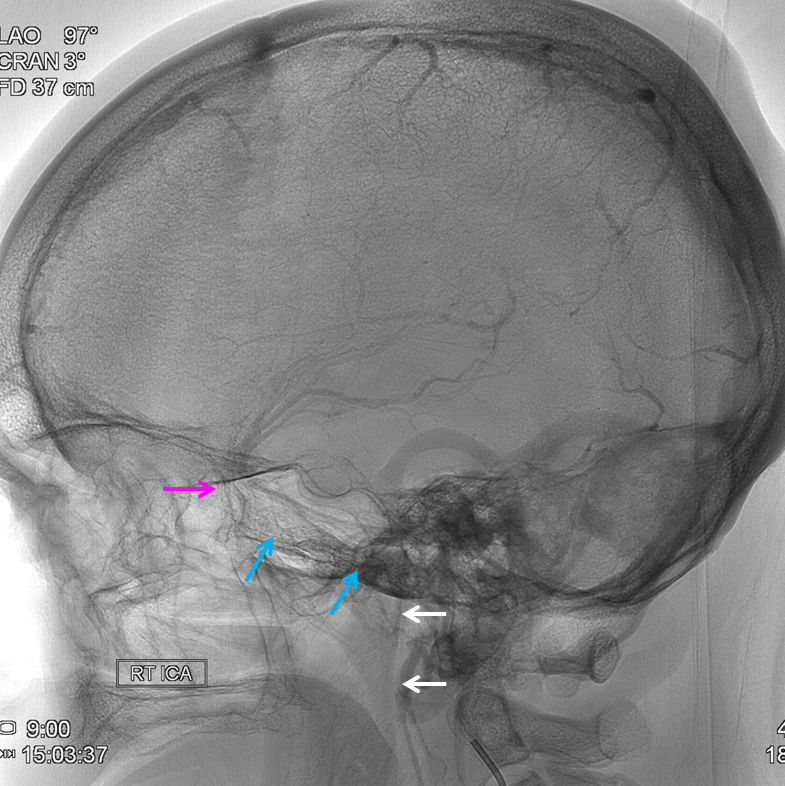
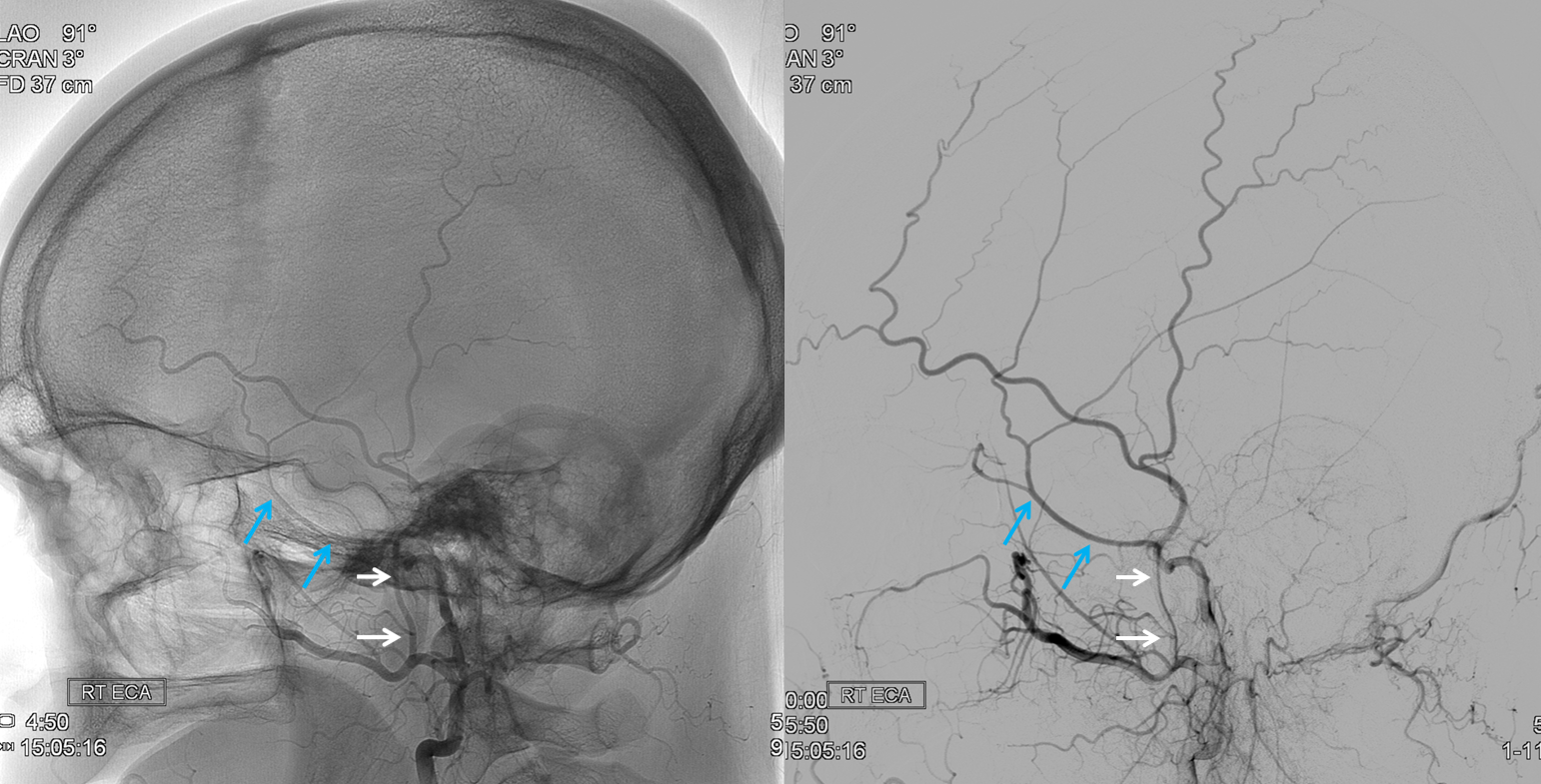
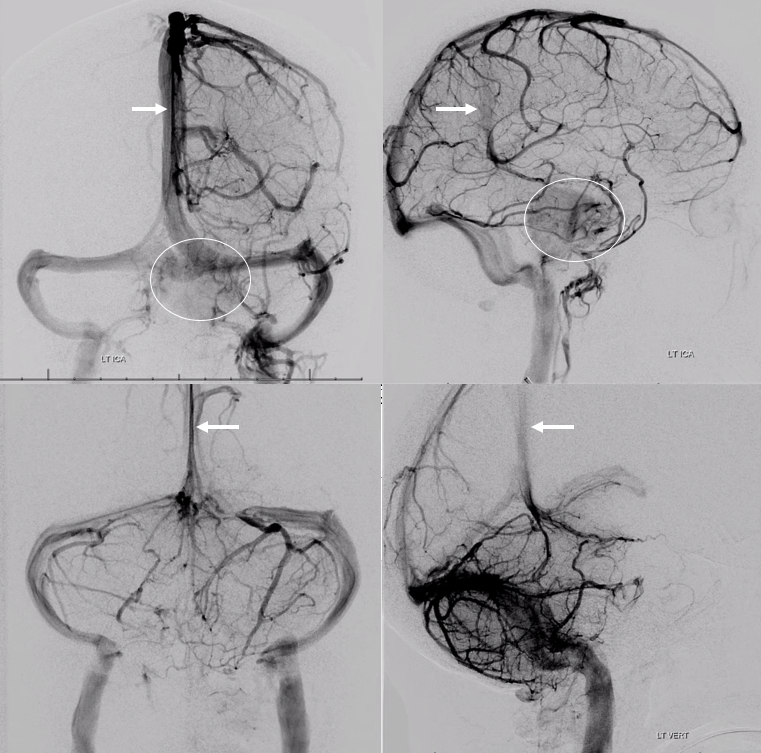
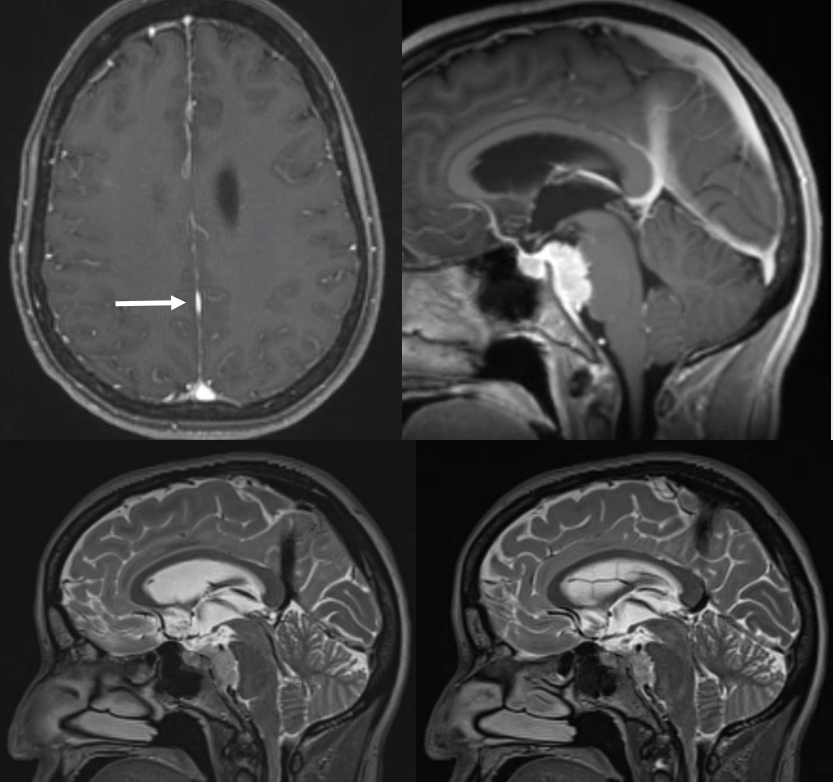
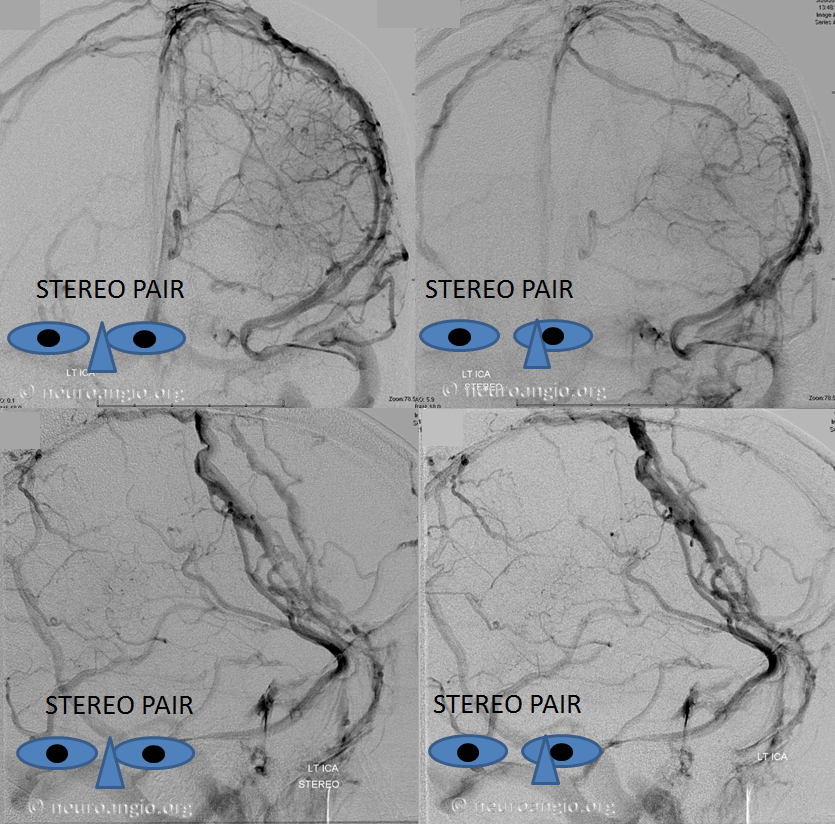
Sagittal Sinus Thrombosis — collaterals.
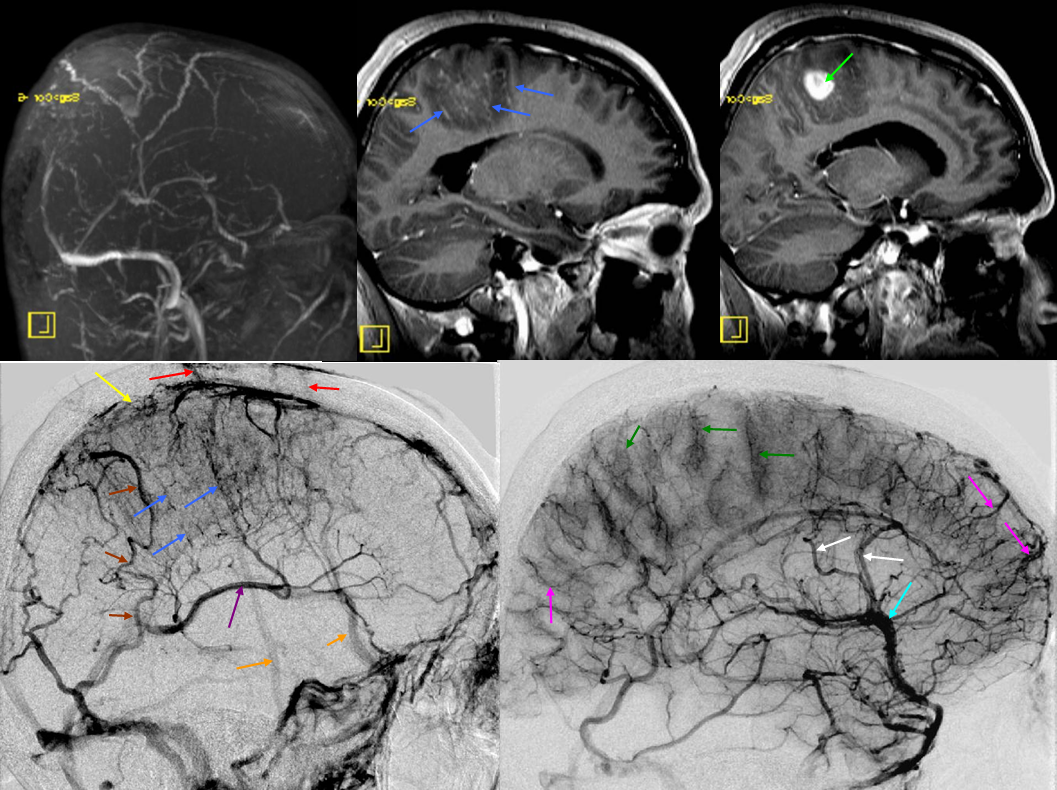
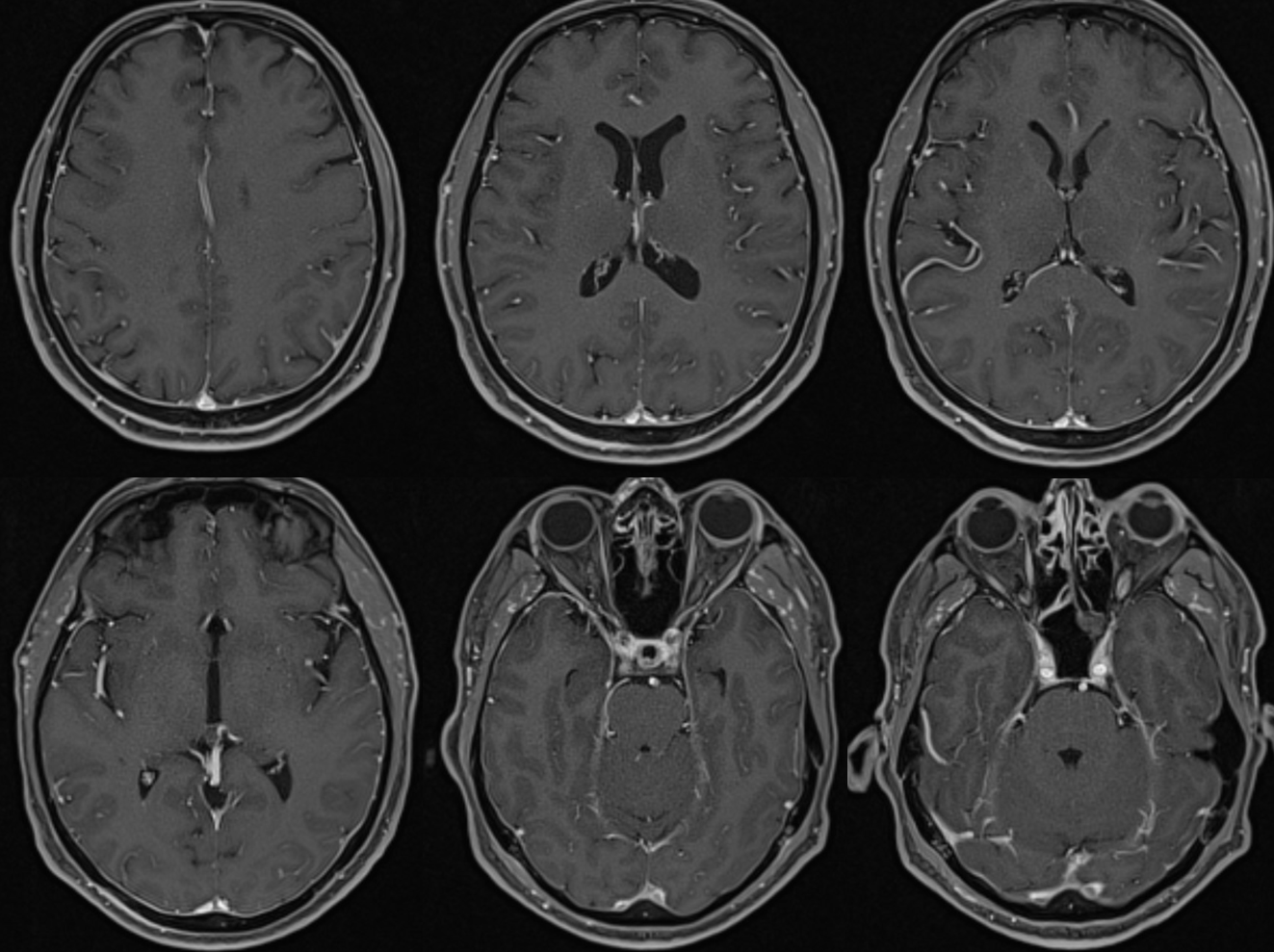
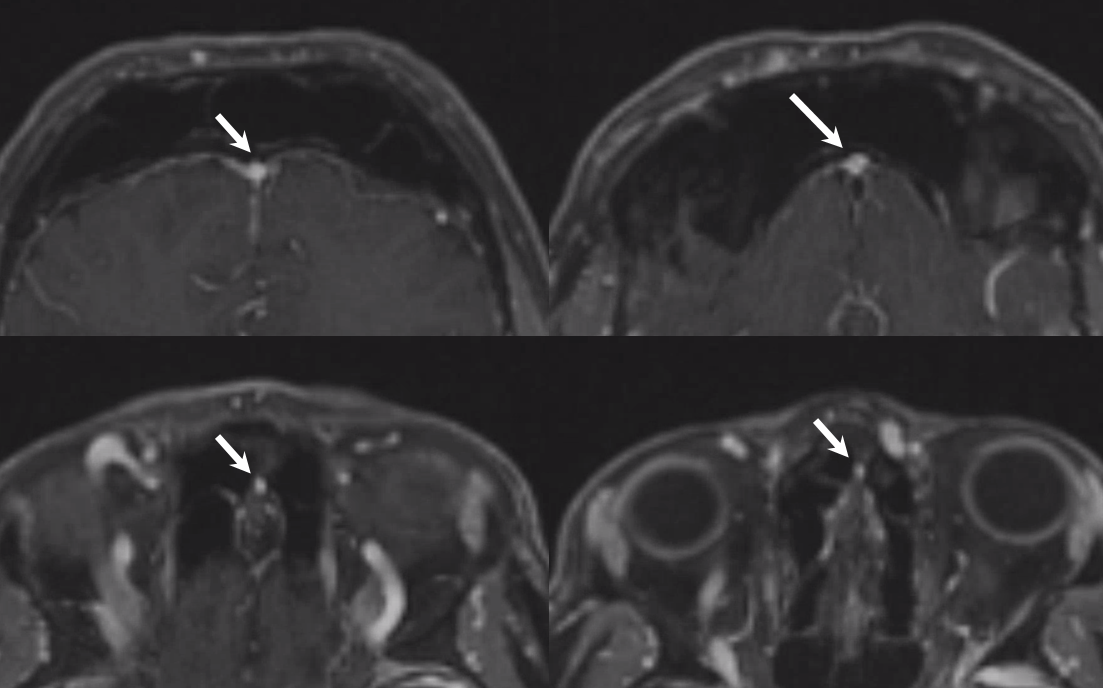
All of the above anatomic knowledge can become very useful in evaluation of venous thrombosis. Numerous collateral pathways develop in this setting attempting to compensate for the loss. The most dramatic cases usually involve the largest channel — the superior sagittal sinus. In this case, a man presented with what initially was thought to be vasculitis-related brain hemorrhage. Subsequent workup led to an angiogram, where sagittal sinus thrombosis with extensive trans-cerebral and trans-osseous emissary vein collateral channels was seen. In retrospect, these findings were present on the patient’s earlier contrast MRI. “Venovibe” or other contrast-enhanced MR venograms can very sensitive, particularly when interpreted with the appropriate index of suspicion. Noncontrast 2-D time of flight MRV I consider to be next to useless as a problem-solving technique. Any thin-slice postcontrast T1 study is vastly superior.