Patient Information Spinal AVM
Overview
An AVM, or arteriovenous malformation, is an abnormal connection between arteries and veins through a disorganized tangle of small curvy vessels called the “nidus”. Normally, blood travels in a predictable route from large to progressively smaller arteries to very small vessels called capillaries, where oxygen and nutrition are delivered and waste picked up, and from there goes on to venules and veins. Occasionally, a short circuit exists when blood bypasses the capillaries (and therefore normal tissue) and goes directly from arteries to veins. One such short circuit is an AVM. Any part of the body can have an AVM (brain AVM are one example). One can also have an AVM which involves the spinal cord. When it only involves the spinal cord, the condition is appropriately called “Spinal AVM”. More complex AVMs, affecting the cord and adjacent bone and soft tissues, are discussed in a separate section under “Spinal Metameric (Juvenile) AVM“
Etiology (reasons why AVMs form)
The reason AVMs form in majority of patients is not clear. Some genetic markers have been studied, but our understanding of why or how they form is quite limited. The AVM itself is almost certainly present at birth, usually in a very small form that is invisible with present-day noninvasive imaging methods, such as MRI. It grows along with the patient, not like cancer, but slower and without possibility of metastatic spread.
Pathophysiology (how AVMs cause problems)
Because the vessels making up the AVM are abnormal in many ways, they are prone to bleeding. Bleeding can come from many places — from the arteries feeding the AVM, the nidus itself, or the venous outflow. AVMs have propensity to develop aneurysms (enlargements and ballooning of the vessel wall) and areas of vessel narrowing or stenosis, both of which can lead to bleeding. The consequences of bleeding depend on location and extent of the bleed. Bleeding is thought to be the most common presentation of a spinal AVM; however, when the diagnosis of the AVM is made, it is usually clear that, in retrospect, some rather nonspecific symptoms were present for some time. These can include back pain, discomfort, slight weakness, and others. The symptoms are typically not severe enough to warrant imaging.
Another way in which AVMs can cause problems is by venous congestion — causing a higher pressure in the veins which drain the AVM. Because these veins were originally meant to drain the spinal cord, and thus communicate with other veins that continue to serve adjacent cord tissue, high pressure in veins around the AVM makes it more difficult for the adjacent spinal cord to drain. This leads to “venous hypertension” — increased pressure in veins. This can lead to dysfunction and eventual death of nerve cells within the cord, with subsequent scarring and permanent deficits.
Other issues can arise depending on the anatomy of the AVM, but they are relatively less important than problems having to do with the spinal cord.
Symptoms
Even large AVMs can have no symptoms (as they are in majority of smaller children), but eventually issues do develop in most patients, usually in their teens or early twenties. Because AVMs can involve any location along the spinal column and produce a host of different problems, the symptoms are extremely variable. Pain, numbness, weakness, loss of bowel/bladder control, incoordination, and impotence are some of the issues. It is very difficult to make a diagnosis of an AVM based on symptoms alone — however most are well seen on MRI or catheter angiography. Many AVMs first come to medical attention by bleeding — this usually presents as acute, severe back pain, followed by weakness, numbness, incontinence; severity ranges from no neurologic dysfunction to complete paralysis, depending on location and extent of bleeding. Bleeding of AVMs located in the cervical spine (neck) usually results in blood spilling over into the head, which can result in severe headaches, neck stiffness, change in consciousness, coma, etc.
Diagnosis
In the “developed” world, diagnosis is almost always established by MRI. Because of their size and very abnormal appearance of adjacent vessels, spinal AVMs are quite easy to visualize on MRI, with or without contrast. Apart from diagnosis, MRI can be invaluable in defining the extent of spinal cord vs. adjacent involvement by the AVM. Continued refinement of MRI technology has made some positive differences in management of spinal AVMs. New methods, particularly time-resolved contrast-based techniques have the potential to obviate the need for catheter spinal angiography in a few select cases.
Another noninvasive method of diagnosis is by CT scan (contrast is very helpful in these cases). CT myelography can also visualize the large vessels surrounding the spinal cord but not the AVM itself, unless it is located on cord surface. CT myelography is performed very rarely, and usually in patients who cannot undergo MRI, for whatever reason.
Spinal Angiography
The next step in evaluation of spinal AVM is catheter spinal angiography. During angiography, a skinny but long catheter is inserted (usually into a large artery in the leg) under x-ray guidance into many vessels giving rise to the AVM and adjacent normal segments, visualizing the arteries and veins during injection of contrast. Spinal angiography gives, by far, the most detailed and dynamic information about the vessels making up the AVM. It is a long procedure which requires the patient to be completely motionless and therefore is almost always done under general anesthesia (completely asleep). Sometimes, angiography may not need to be done (if the diagnosis is already clear and no intervention/treatment is being planned)
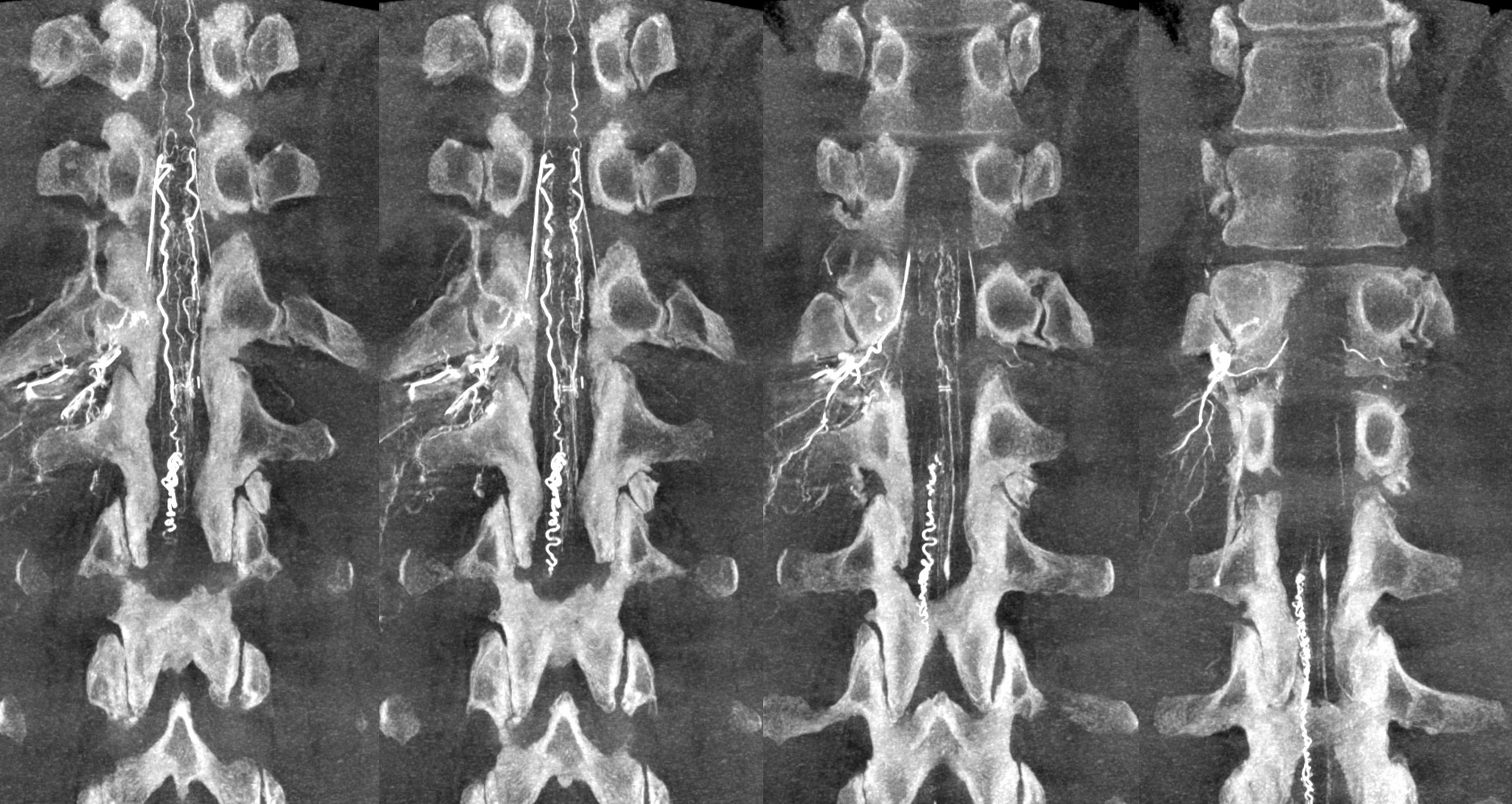
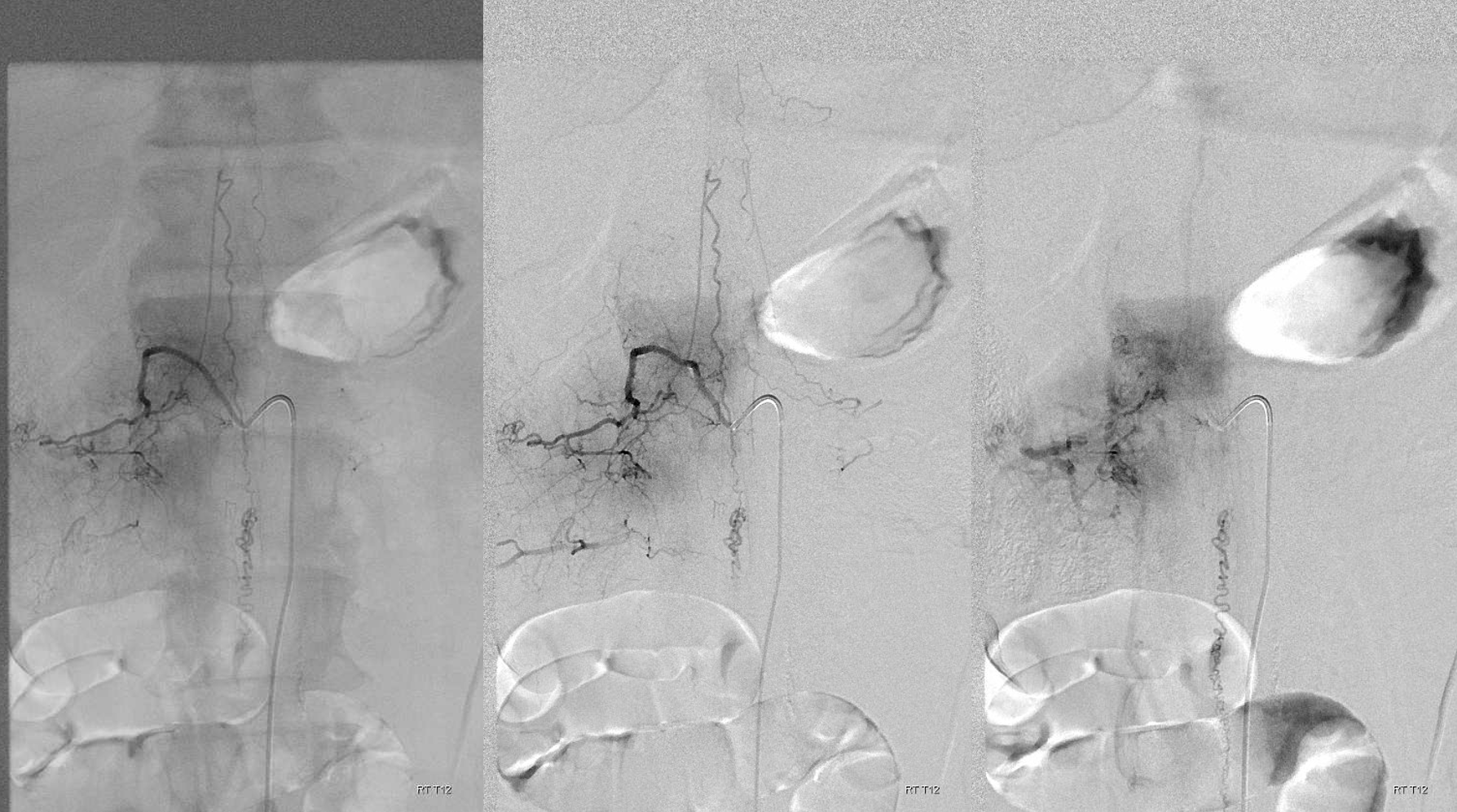
Below are some images of a spinal AVM — full case here.
State of art DYNA images obtained during angiography
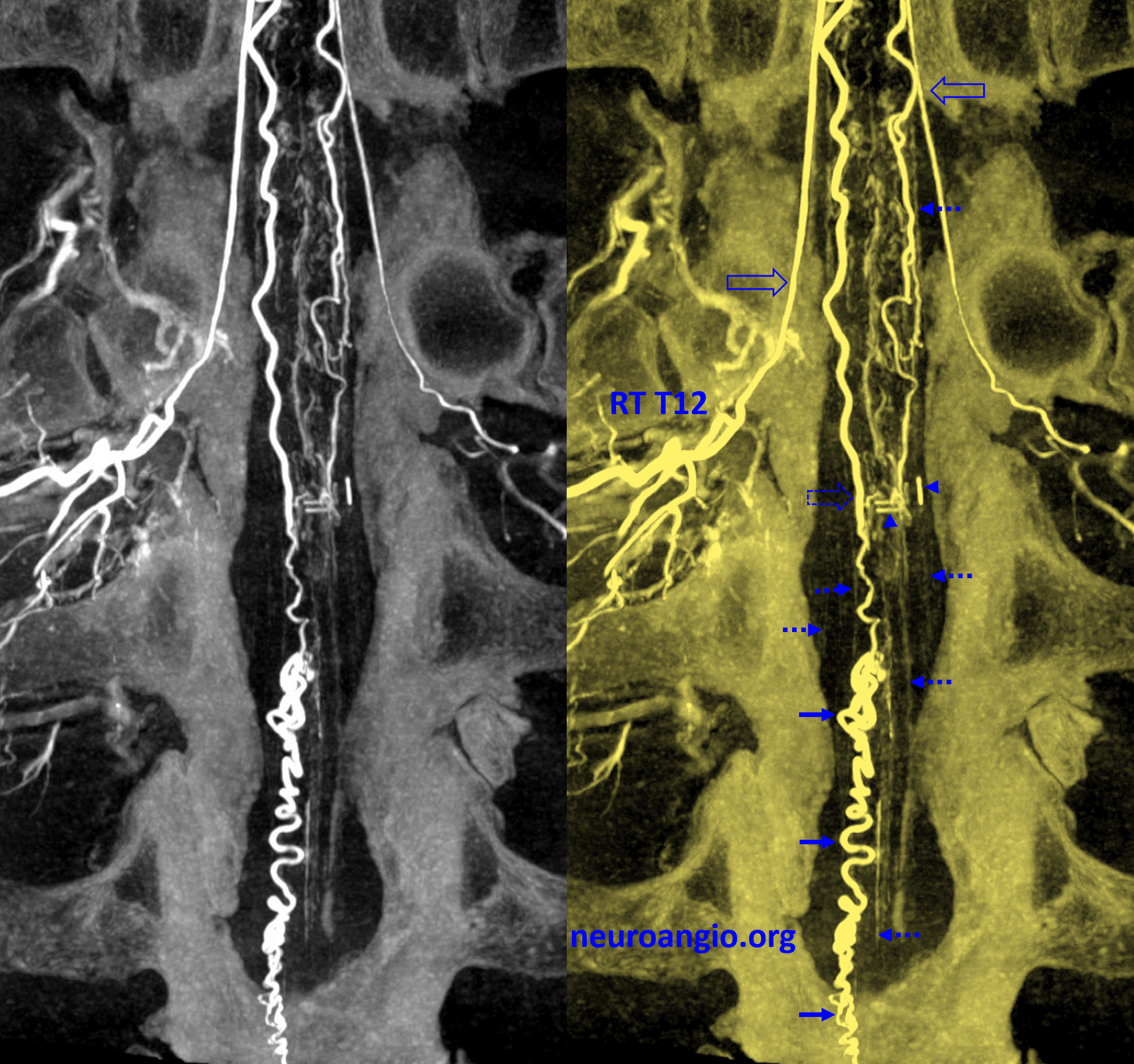
“MIP” reconstructions of DYNA images
Conventional “Digital Subtraction Angiography” of the same case
Additional Testing
Other tests may be necessary depending on the situation, such as urodynamics (a study of how the urinary bladder fills and empties), EMG (electromyography), nerve conduction studies, and evoked potentials (to evaluate possible nerve damage) among others.
Disease Course and Treatment
Overall, medical literature on spinal AVMs is rather pessimistic. Many patients eventually develop significant neurologic dysfunction, meaning weakness, sensory abnormalities, problems with urine/bowel control, pain, etc. It is important to realize, however, that even such formidable lesions as spinal AVMs have a lot of variety — some can run a relatively benign course, and others can be cured. Much depends on the exact location and anatomy of the AVM.
Some spinal AVMs can be cured by surgical excision — AVMs which come to the surface the surface of the cord may not require the surgeon to dissect through functional spinal cord tissue to reach the AVM, are the most favorable types. These operations are nevertheless considered quite risky. The timing of surgery is also crucial. Most surgeons would not operate on an AVM that was discovered incidentally and has not caused the patient any problems. On the other hand, if problems such as bleeding do arise, surgery may be technically more feasible when a blood clot has formed a niche around the AVM. making its removal easier. Unfortunately, many AVMs cannot be surgically cured without a very high chance of paralysis or some other profound neurologic dysfunction.
Neurointerventional catheter-based embolization techniques can play an important role in treatment of spinal AVMs, however the possibility of neurologic damage is relatively high. Everything here depends on understanding the anatomy of the AVM — if it can be proven that important arteries which also supply the spinal cord (such as the anterior spinal artery) do not contribute to AVM supply, there is a possibility that the AVM can be embolized with liquid embolics, such as nBCA or Onyx. Sometimes, even though the AVM cannot be safely embolized, parts of it which are felt to be at especially high risk of causing problems (rupture) can be selectively targeted for embolization (for example, if an aneurysm develops on an artery feeding the AVM, this aneurysm may be selectively embolized)
Gamma Knife and other forms of highly targeted radiation therapy, quite successful in treatment of many brain AVMs, also have more limited role in the spine, because of various technical and anatomical reasons. The exception to this are AVMs located in the high cervical spine (neck) area, where there has been some success with Gamma Knife targeting. This technology continues to improve.
In practice, most spinal AVMs are best managed by a team approach. This is a long-term condition, requiring coordinated care by specialists from neurology, neurosurgery, and diagnostic and neurointerventional radiology. Particularly important is the role of a rehabilitation specialist and a physical/occupation rehabilitation team, which can make a huge difference in functional capacity of the patient. Expert care by specialists in psychiatry and psychology can also be immensely helpful for both patient and loved ones in dealing with the heavy emotional burden and motivating the patient to achieve the best possible functional outcome.
Our role
Our Neurointerventional Radiology group specializes in performance of spinal angiography and transcatheter (endovascular) embolization of spinal vascular malformations. For the patient with spinal AVM, we function to perform spinal angiography to better understand AVM anatomy and therefore select the appropriate treatment modality. We are located at the NYU Langone Medical Center, in New York City. As all centers of excellence, we function as part of a team of neurosurgeons, neurologists, rehabilitation specialists, psychiatrists, and diagnostic radiologists, all of whom have extensive experience with vascular conditions of the spine. Regardless of where you may seek medical advice, we STRONGLY recommend that your evaluation and management be carried out at a major center with extensive experience in treatment of this condition, as details of diagnosis and therapy can be extremely complex. A small number of excellent centers for this condition exist across the US and elsewhere.
Contacting Us
You can contact us by filling out the “Contact Us” form below or calling the office at 1-212-263-6008
