Case in conjunction with Dr. Paul Huang, Dr. Steven Russel, and Dr. Omar Tanweer, Bellevue HHC, New York City
Intraoperative Video Courtesy of Dr. Omar Tanweer, NYU
A middle-aged woman presented with progressive quadriparesis. MRI showed typical, if nonspecific, findings of a vividly enhancing intradural mass and a ton of associated edema, up and down the cord:
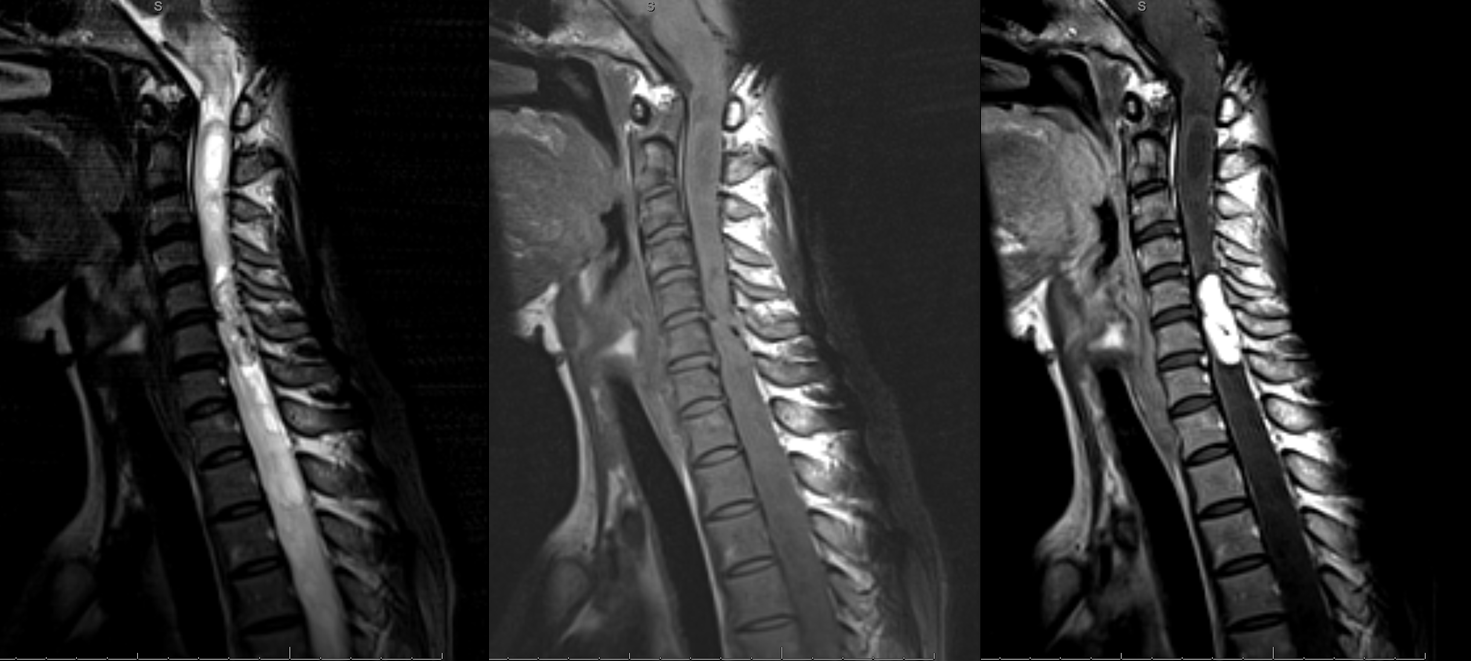
A syrinx at the thoracic level
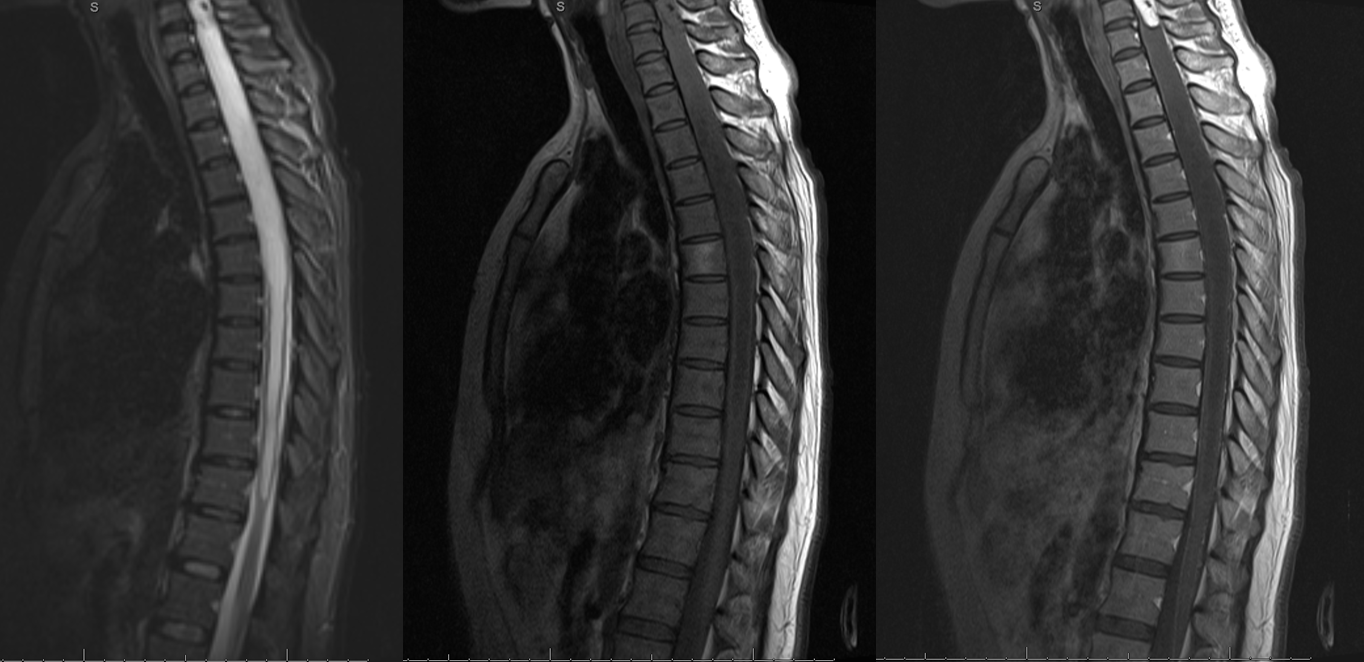
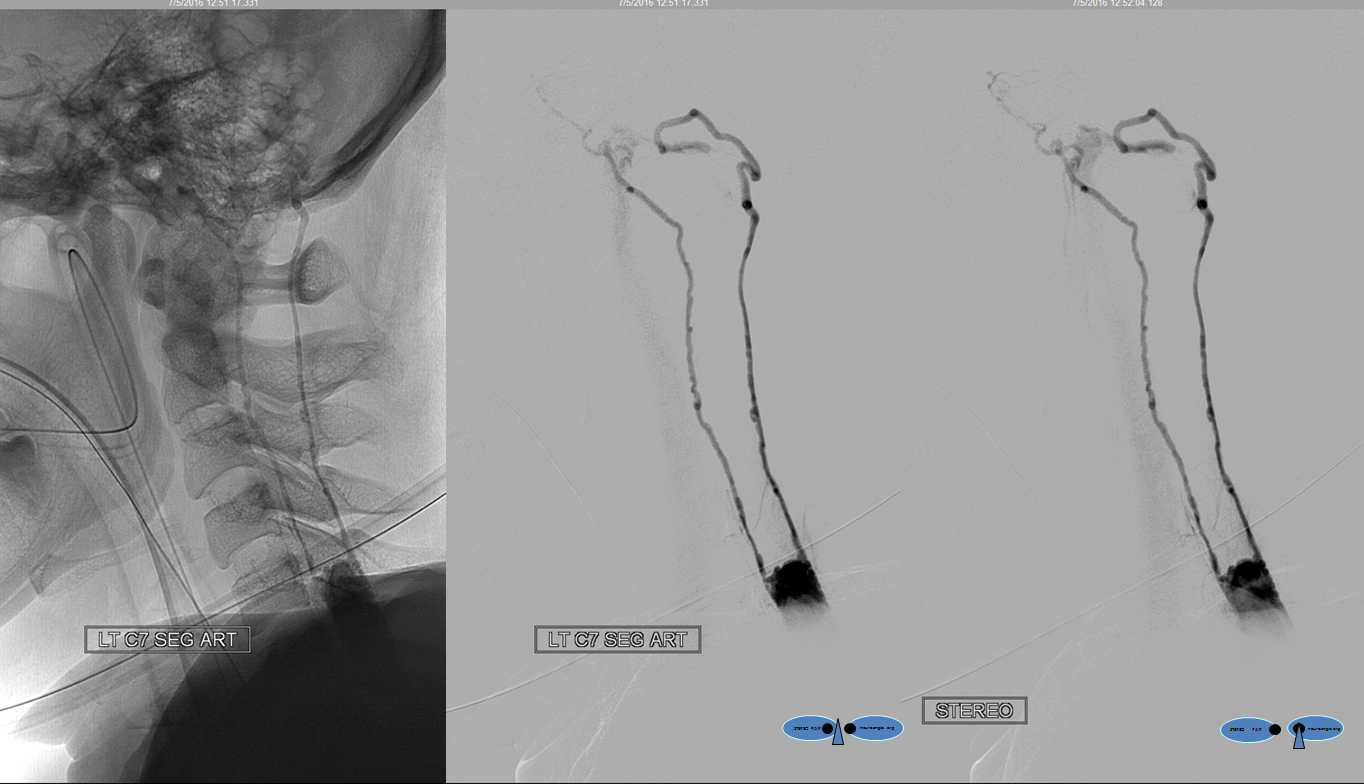
Preop angio shows left deep cervical origin radiculomedullary artery at left T8 level, with no anterior spinal contribution to the mass. Good news.

Here is the juicy pedicle, a standalone left T7 segmental artery, feeding most of this tumor. Notice tremendous vascularity and secondary venous congestion (blue arrows)
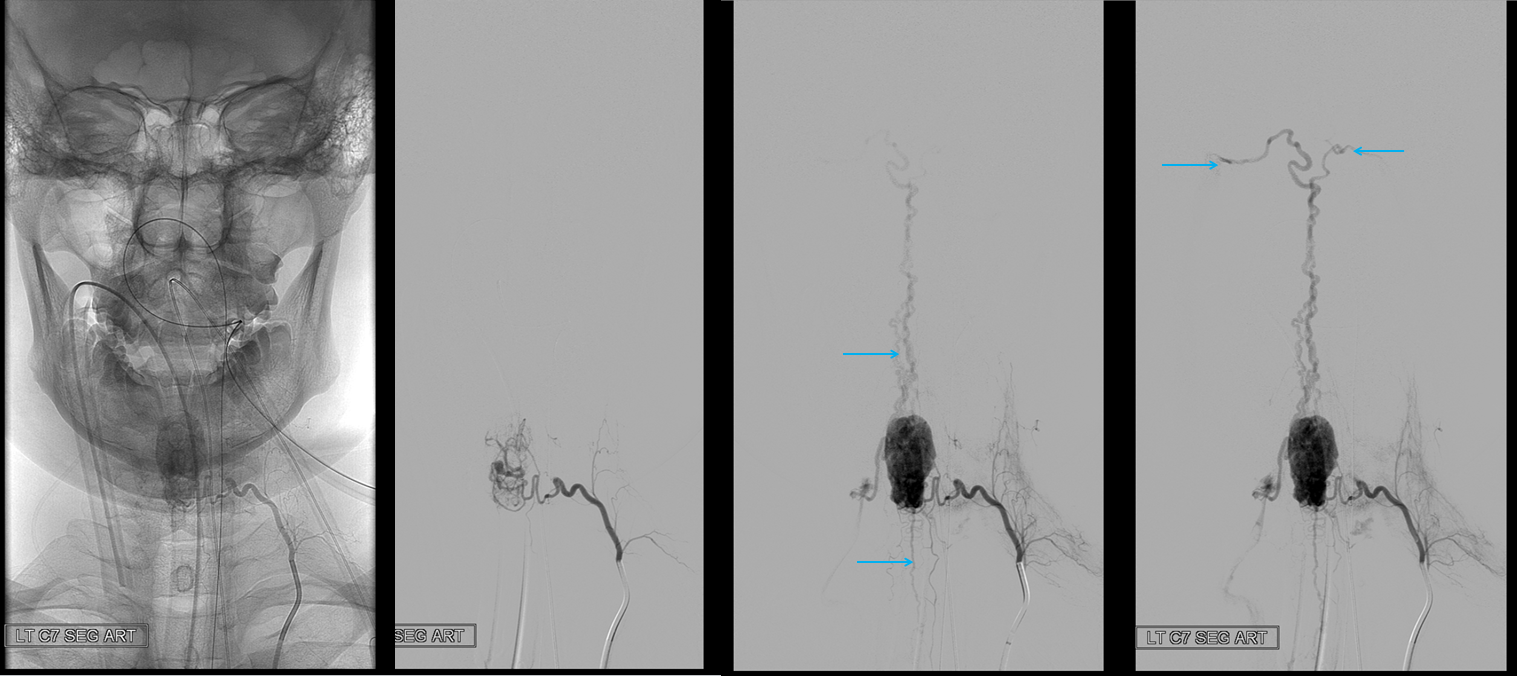
Stereo views, as is traditional; drainage into marginal sinus
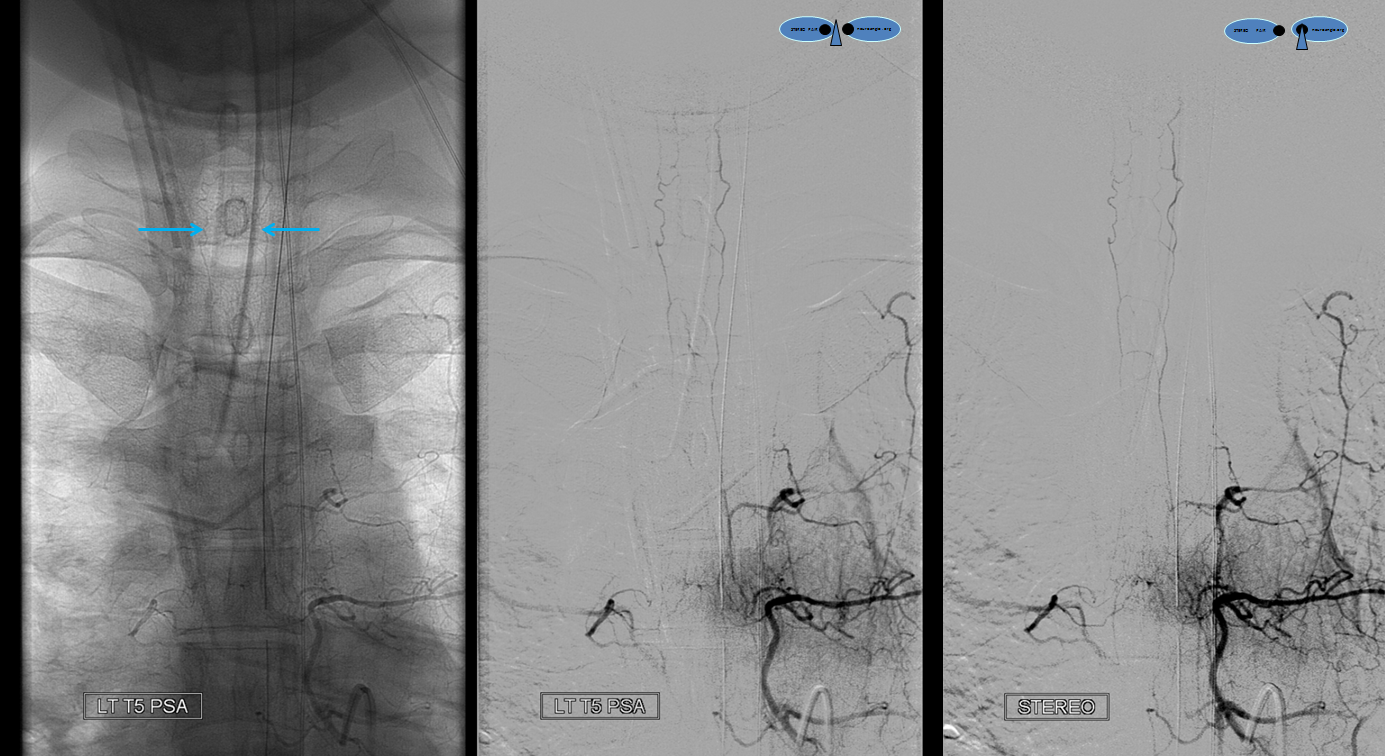
Pretty intense lateral views, stereo again, again drainage into marginal sinus and congestion of the anterior pontomesencephalic vein (top ventral)
Coned down views show an important finding of paired posterior spinal arteries (blue arrows) — normally posterior spinals are barely visible — these are very large.

Why are they so large? Because they are contributing to tumor supply — confirming its intra-axial nature. Physiologically, flow in these vessels is caudocranial into the tumor. In the above imge, the catheter is occlusive and the force of injection reverses flow in these PSAs. How to prove it? Find the primary segmental artery which supplies them — in this case left T5, see below:
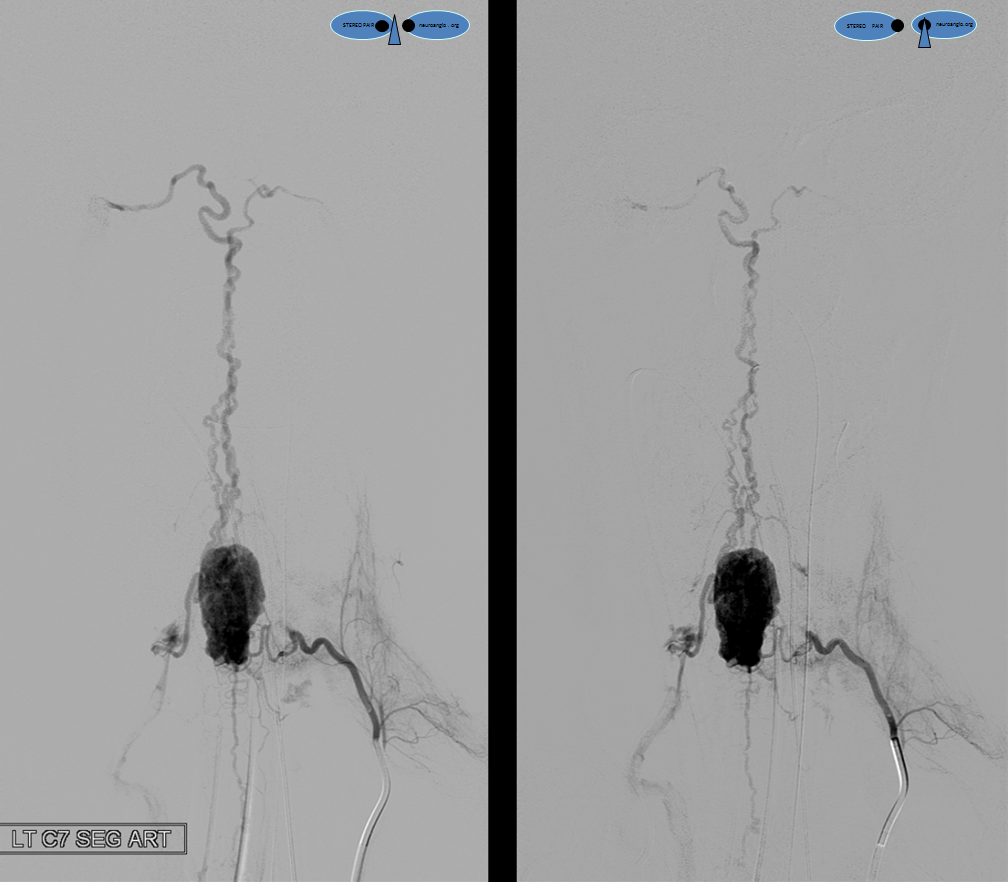
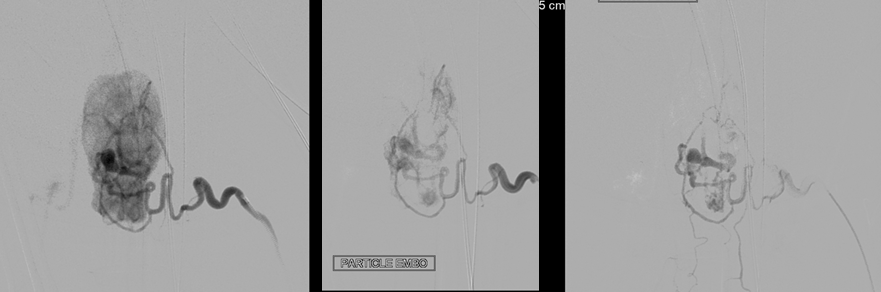
Now what? Because of these hemodynamics, particle embolization from the left C7 position, as long as the embolization catheter is not occlusive, will primarily carry flow and particles into the mass. This can be done as long as the posterior spinals are not visible on embolization runs (leftmost image and center image below). Once enough tumor has been embolized, flow dynamics will shift towards the PSAs (rightmost image below) — at this point the embo is stopped.
Post particle embo. C7 segmental artery is closed with coils. Injection of left deep cervical shows preserved anterior spinal artery (red arrows)

Control injection from left T5 shows preservation of entire posterior spinal axis (blue arrows), which is now opacifying remnants of tumor-related vasculature (white arrows). Notice beautiful vasocorona vessel connecting the two posterior spinal arteries at the inferior margin of the tumor (inferior-most white arrow)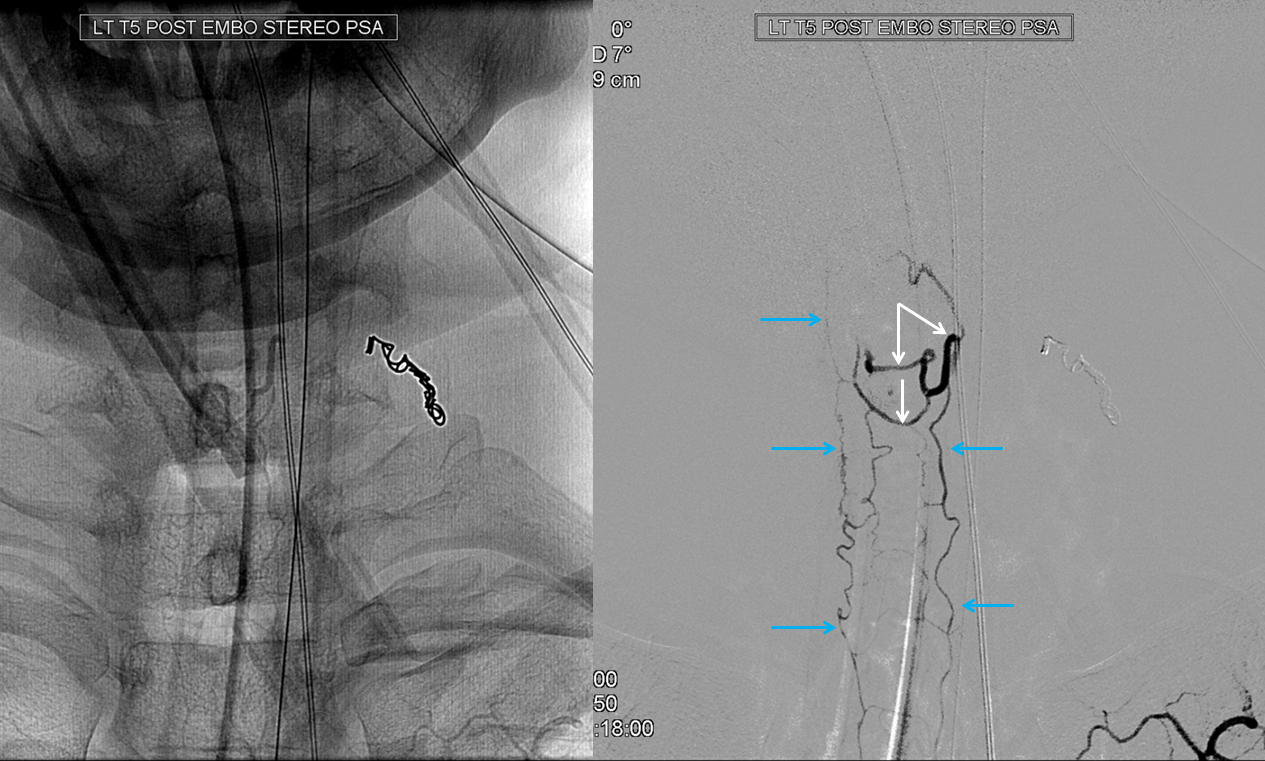
Below is the intraoperative video, courtesy Dr. Omar Tanweer
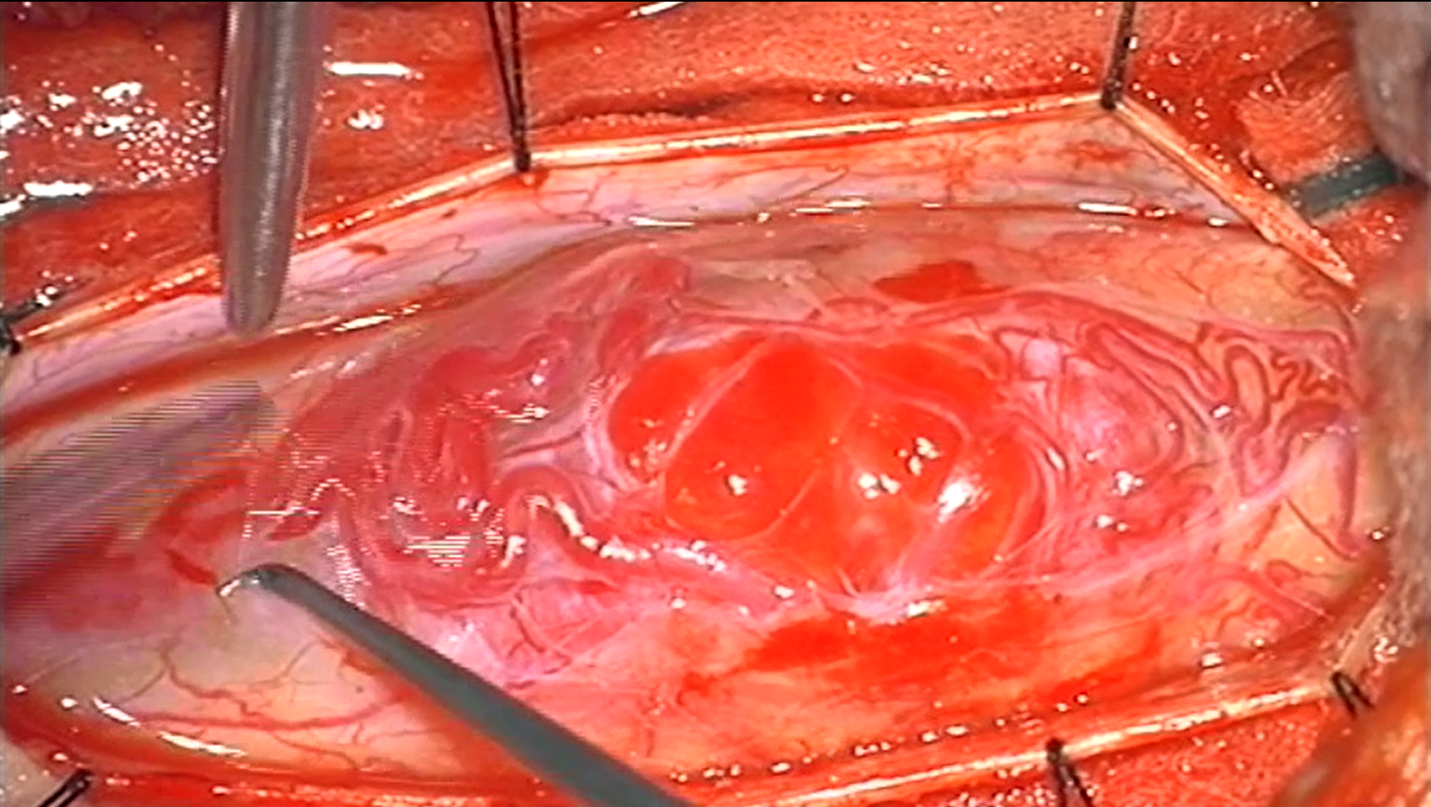
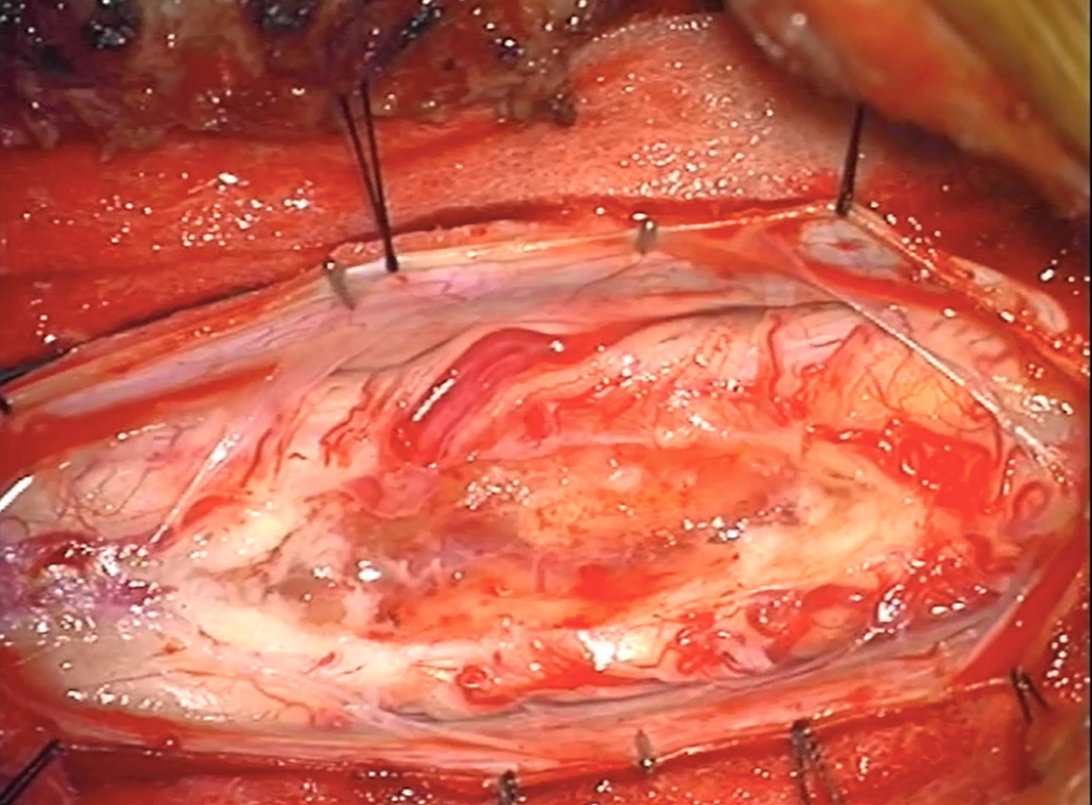
Here are some images, in case video does not play well
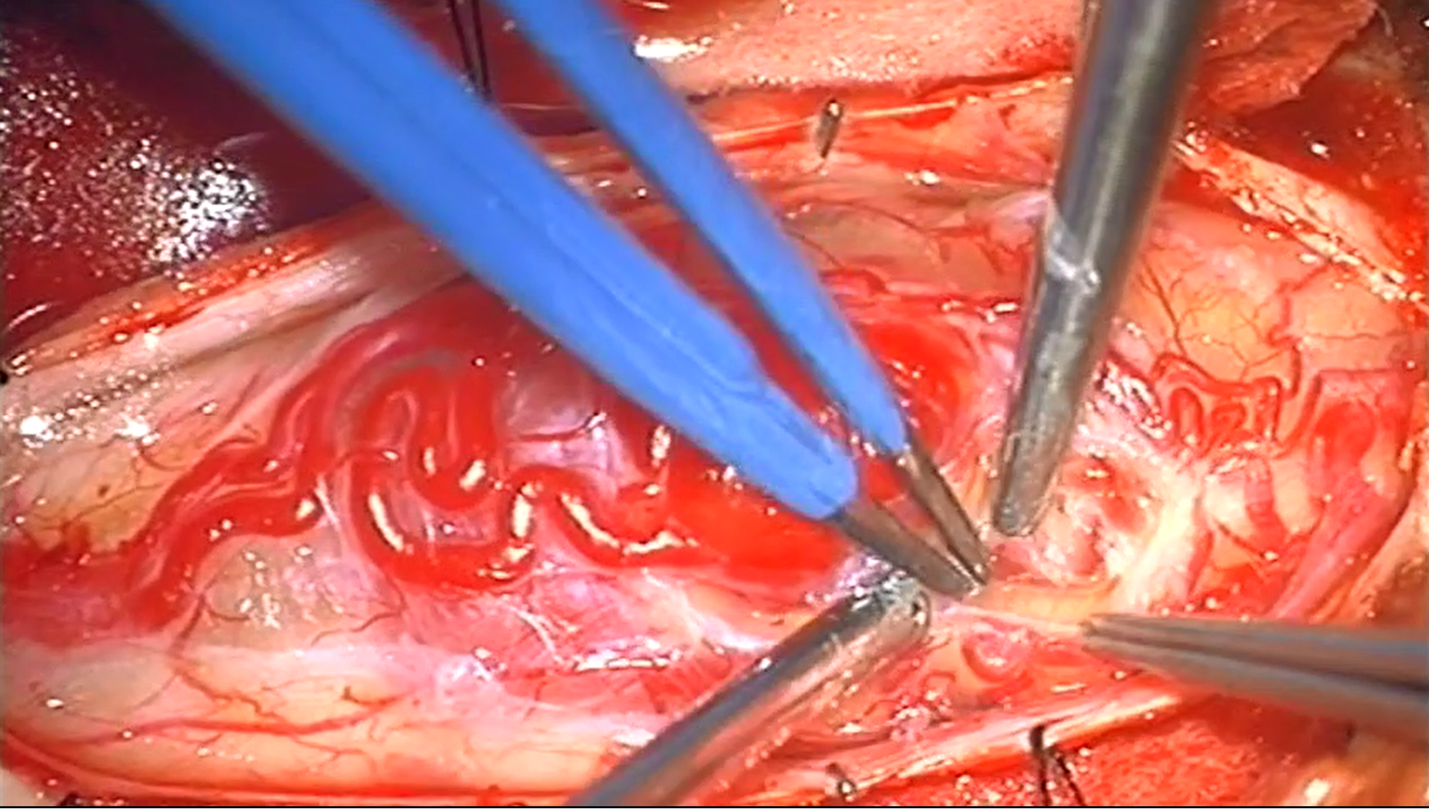
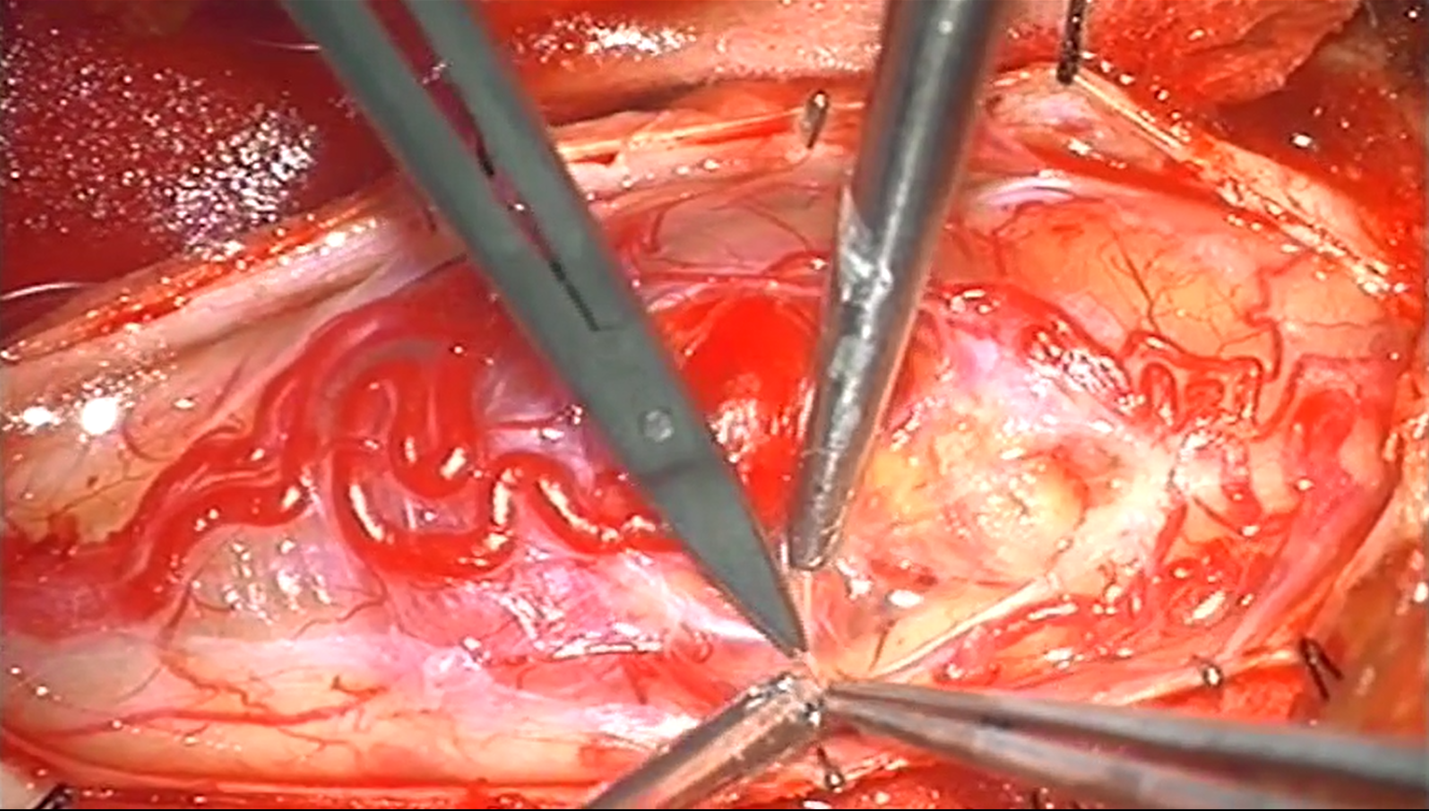
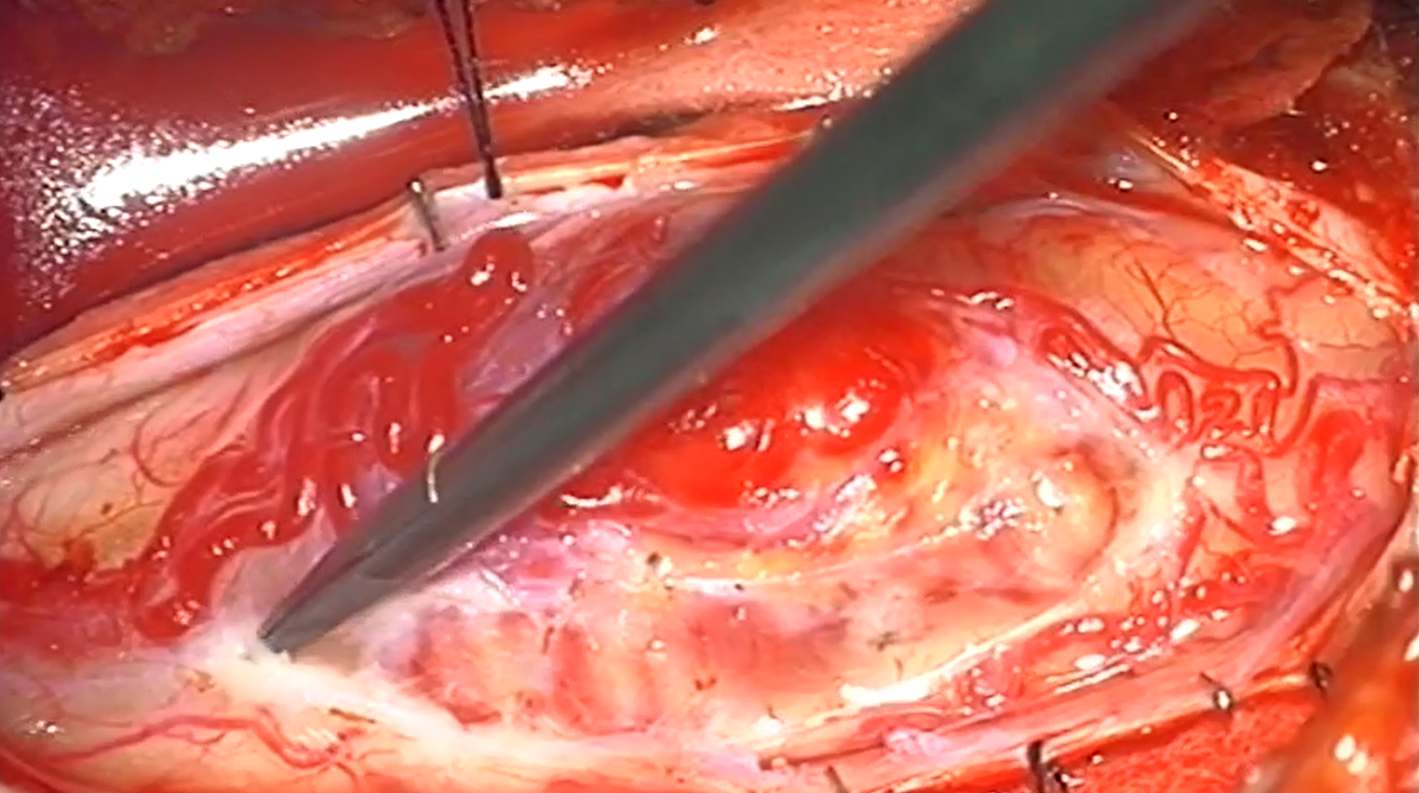
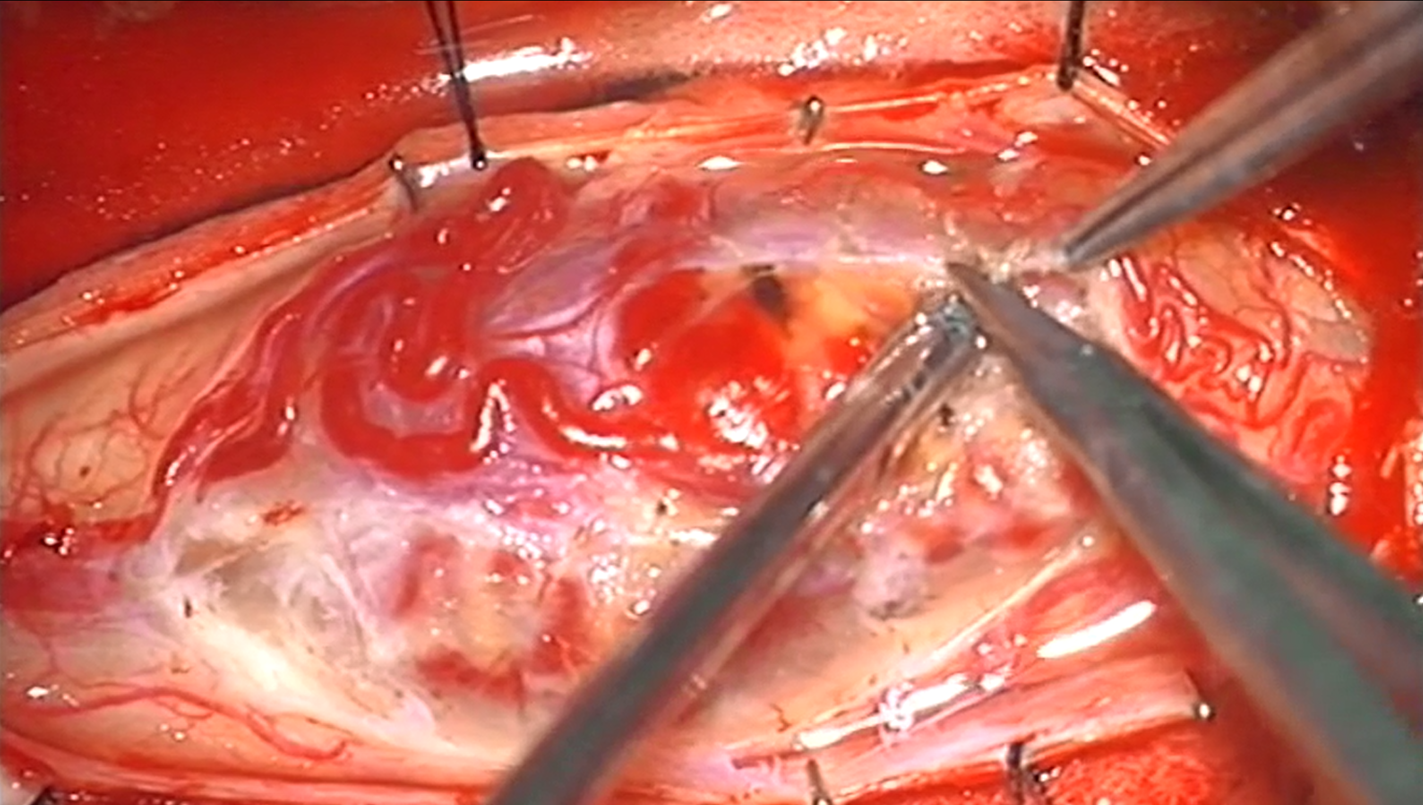
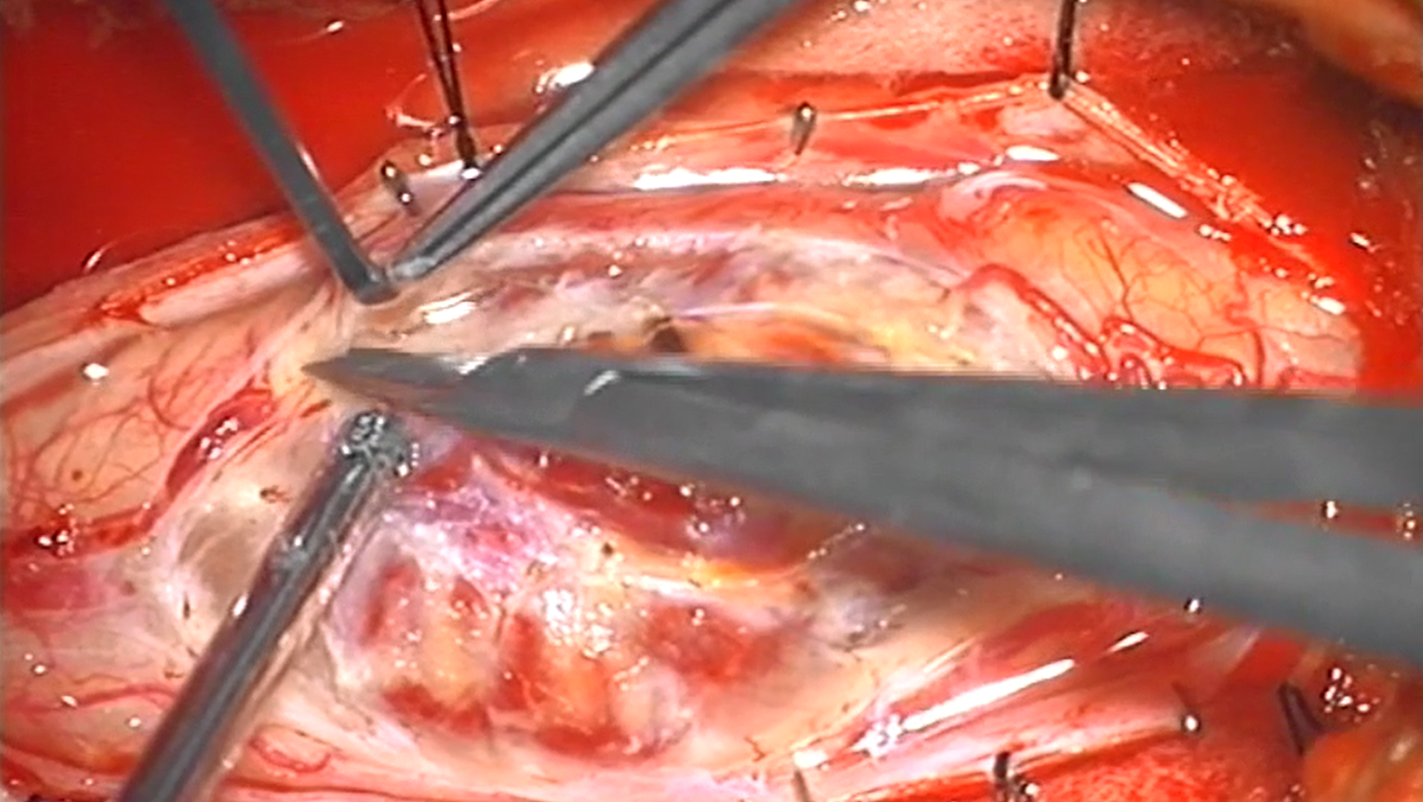
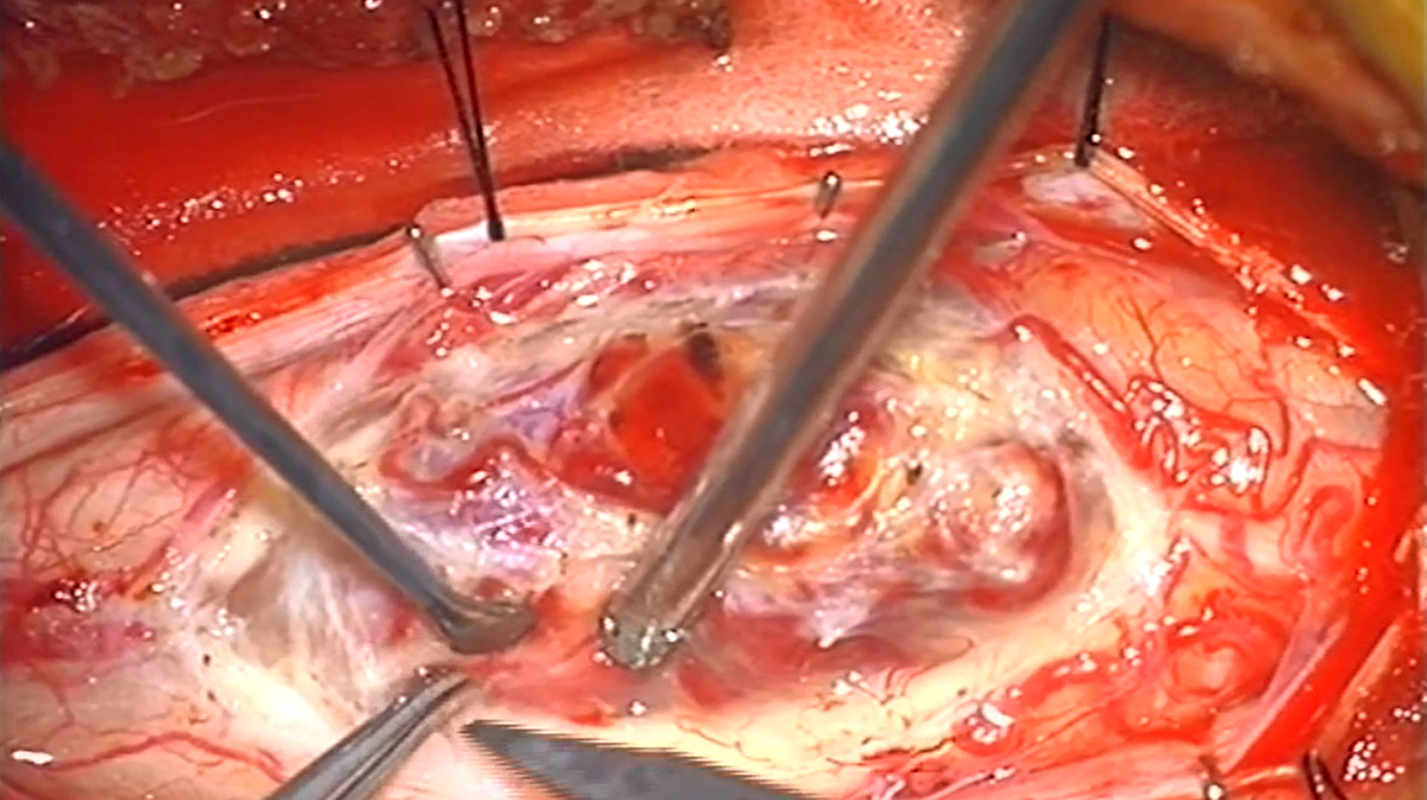
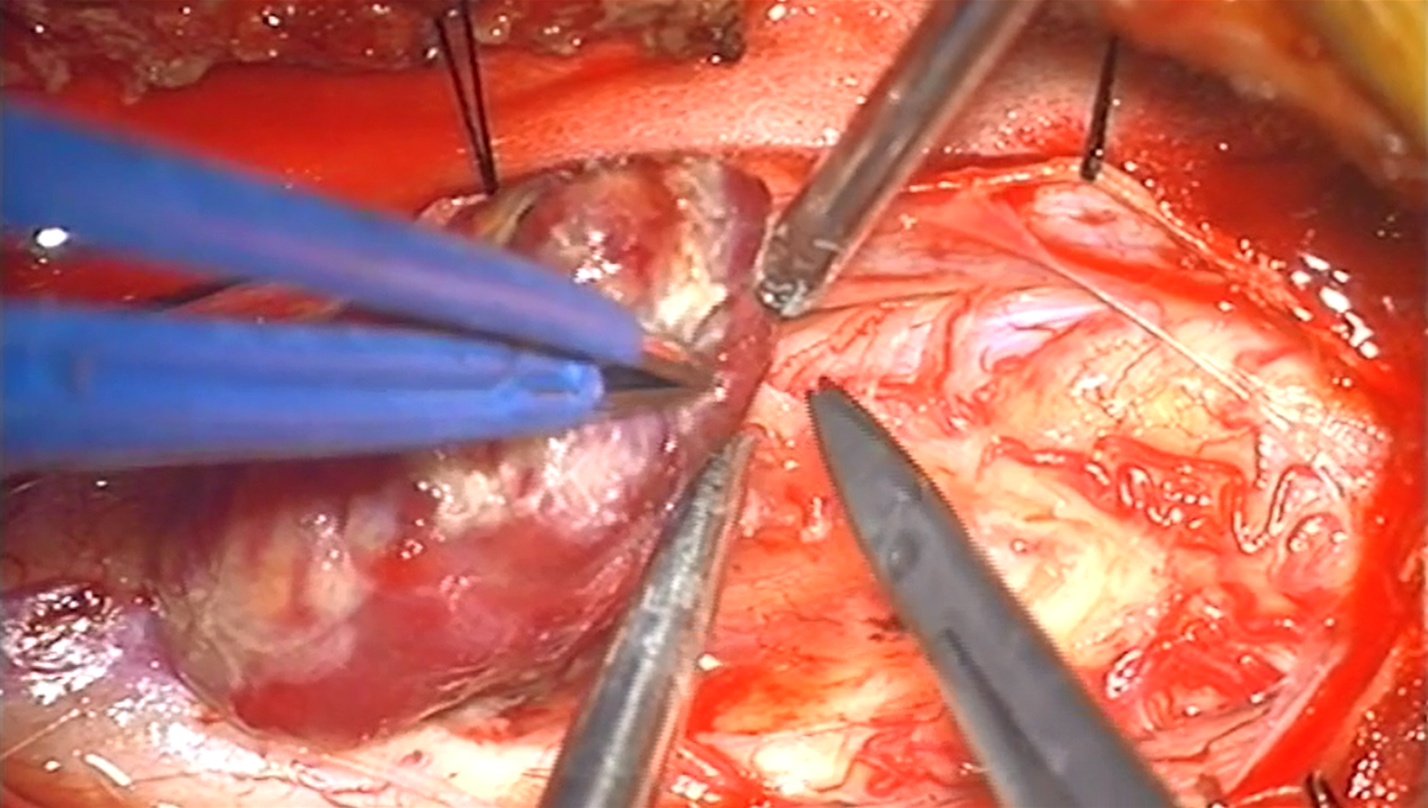
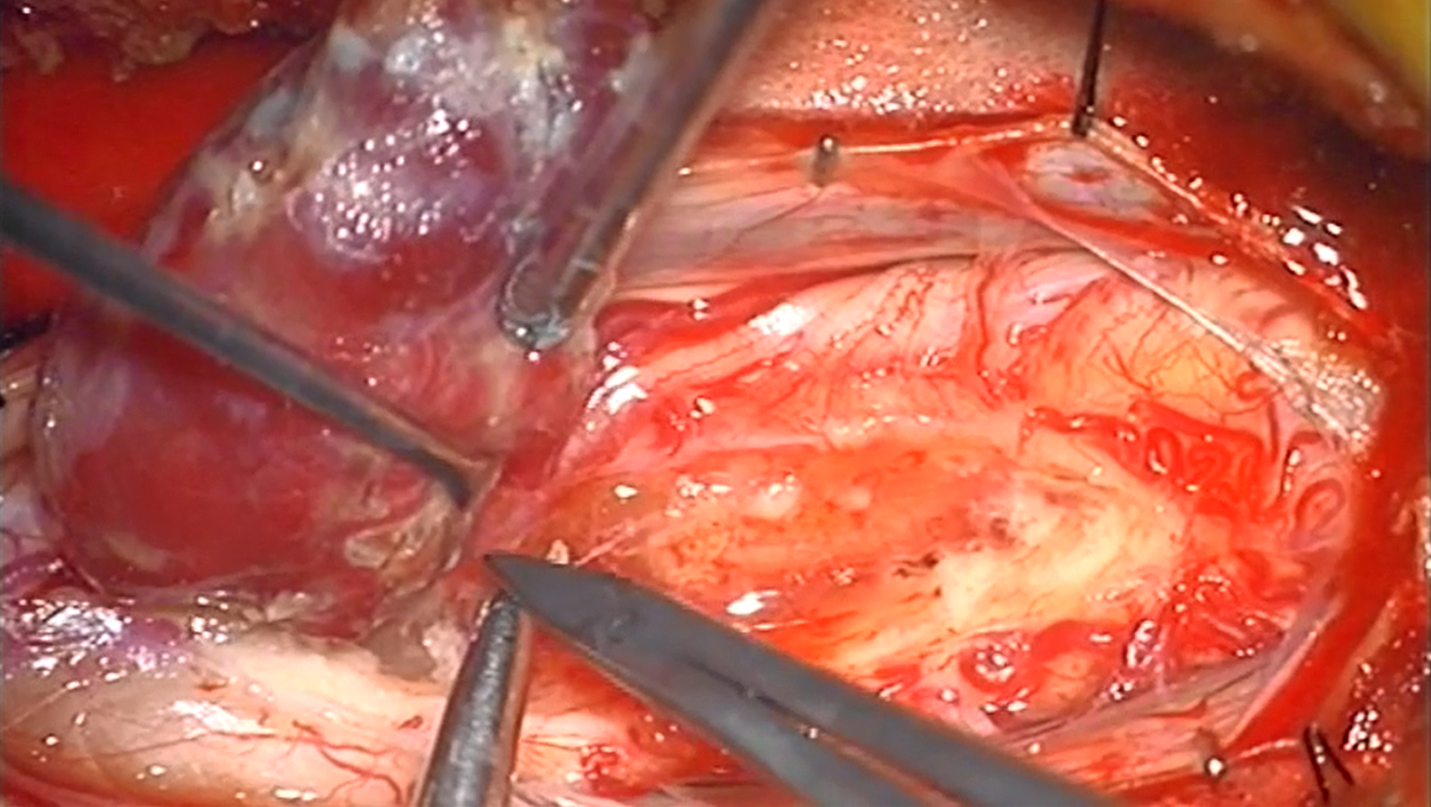
Resection cavity
Immediate postop MRI of gross total resection, associated with excellent clinical result:

No, there will never, from now until the end of Milky Way, be a randomized trial on utility of preoperative spinal cord tumor embolization. However, there was a time, not so long ago, when such embolization came in useful for someone else too — check out this link. So far embo seems to be winning. Pathology is hemangioblastoma.
Further reading
http://www.ajnr.org/content/26/4/936
