With Eleanor Kim and Irina Belinsky
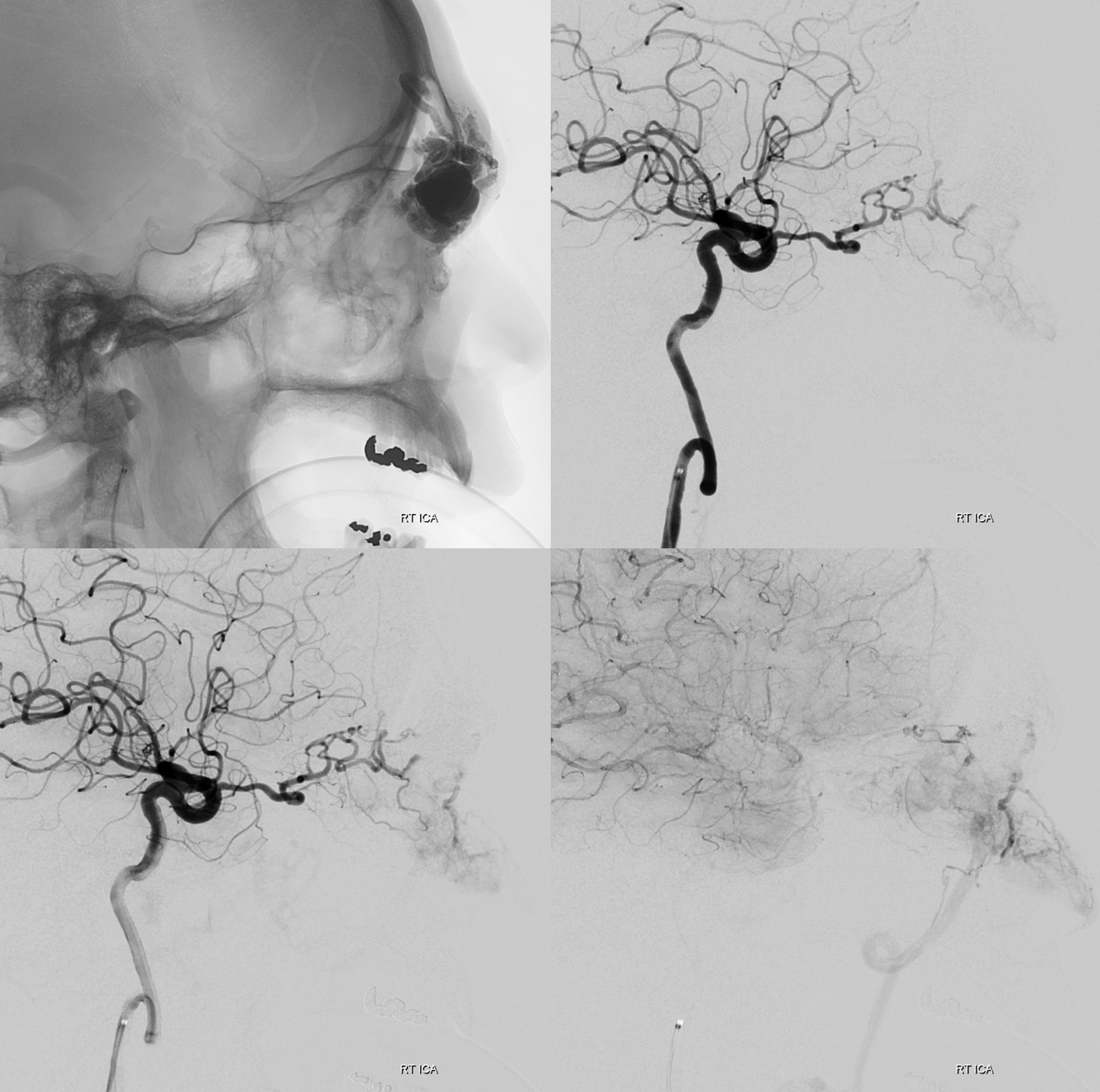
Direct puncture can be a fantastic option not just for low flow but for high flow lesions also. This patient presents for preoperative embolization of orbital AVM
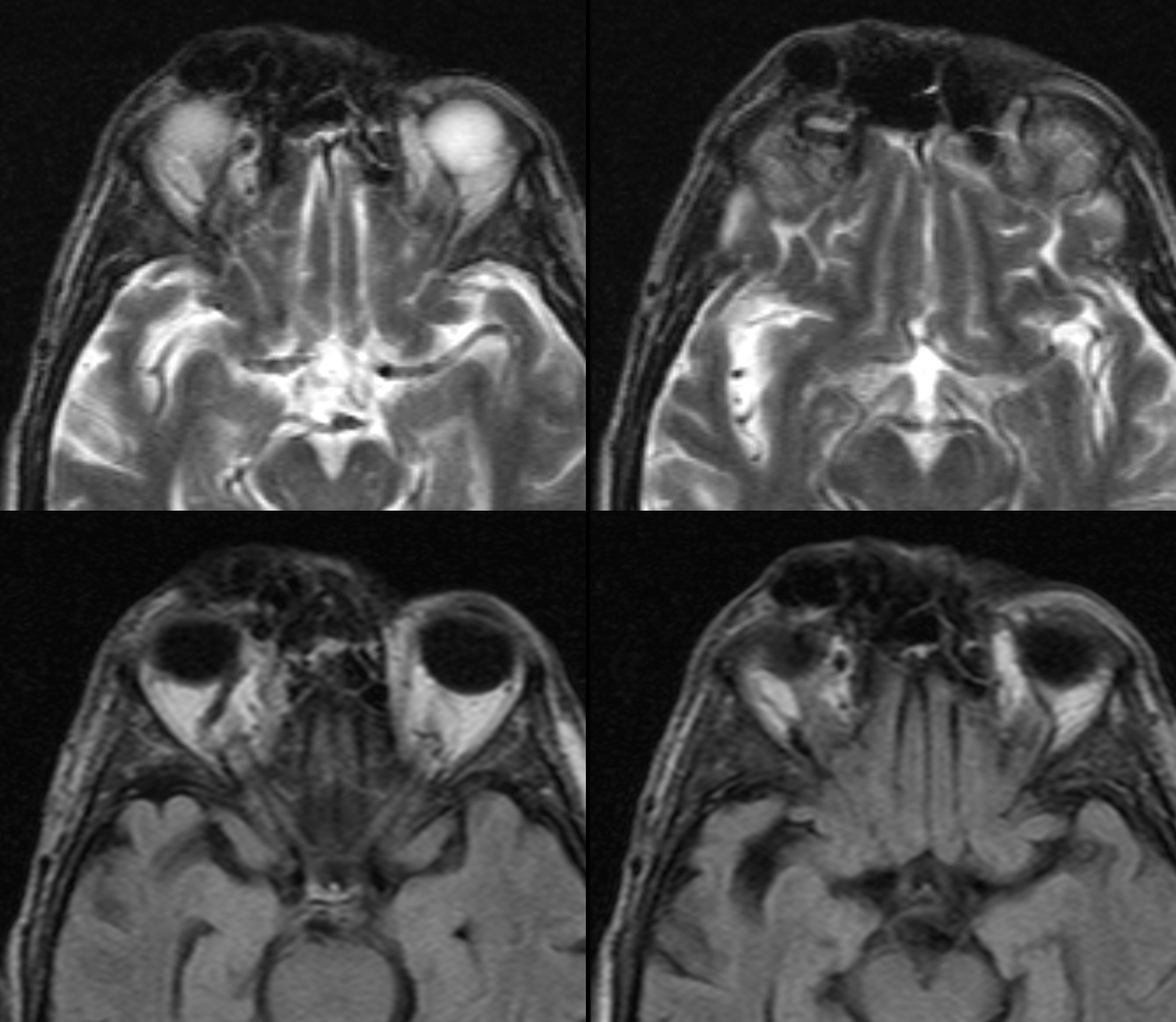
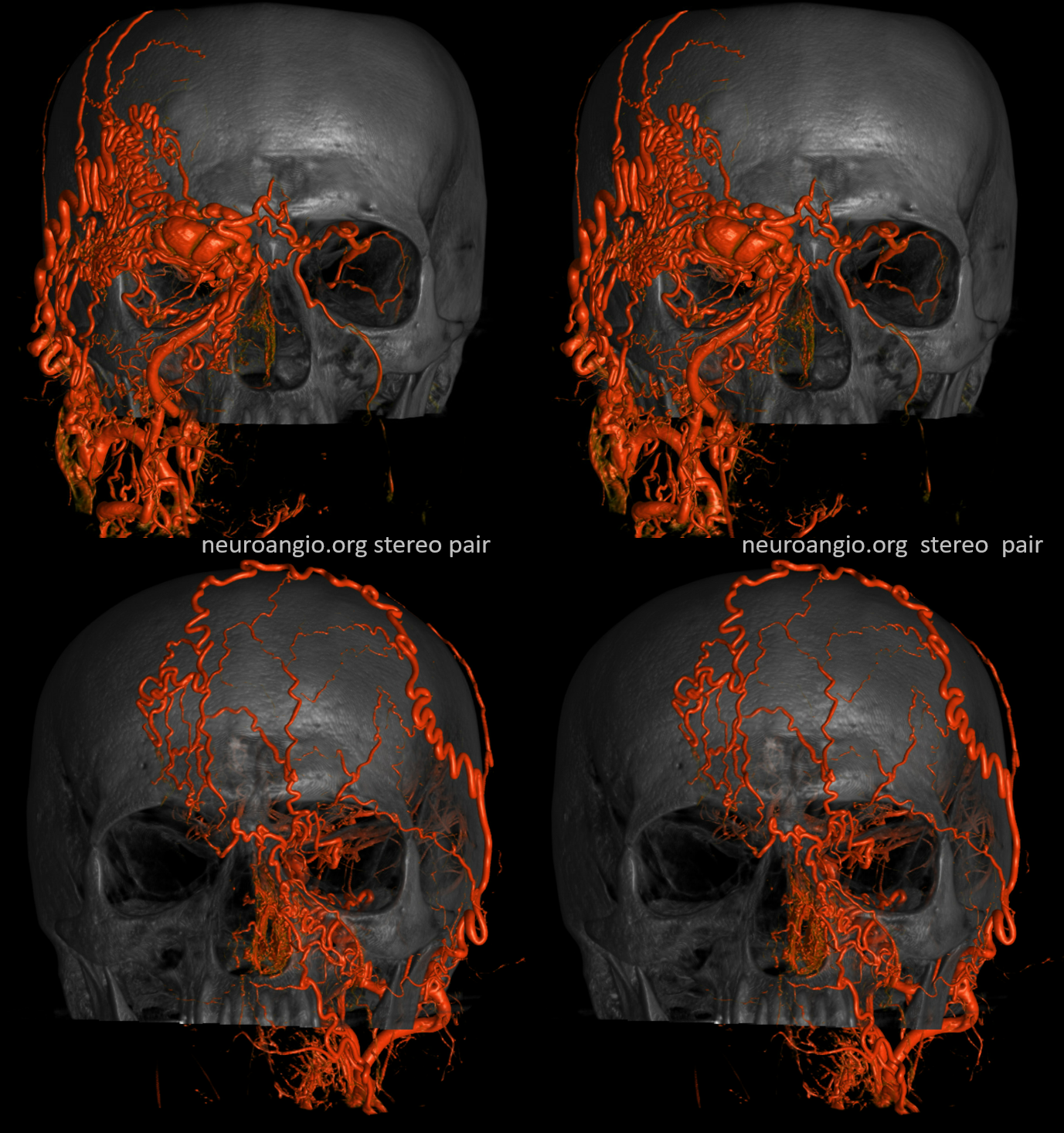
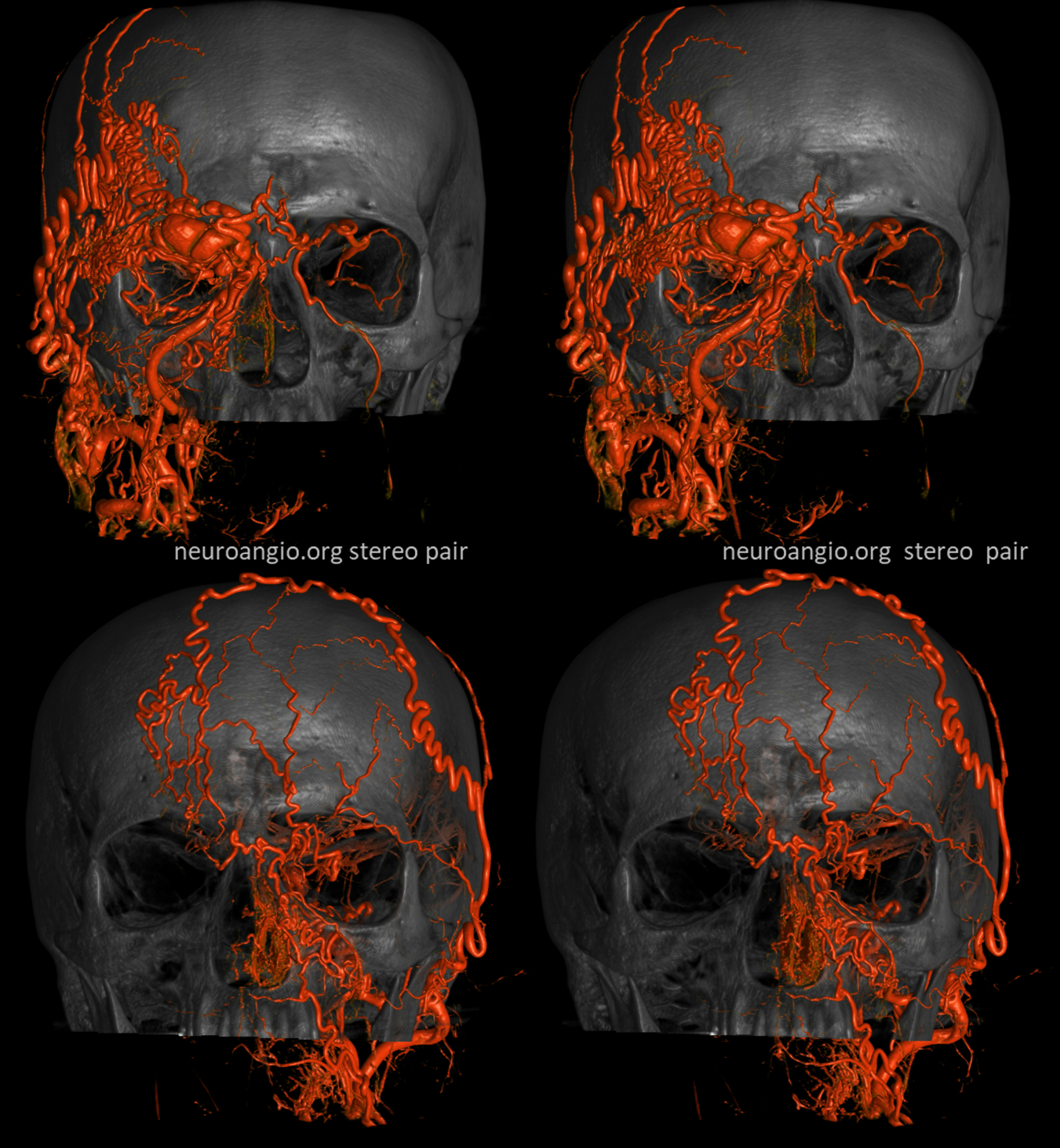
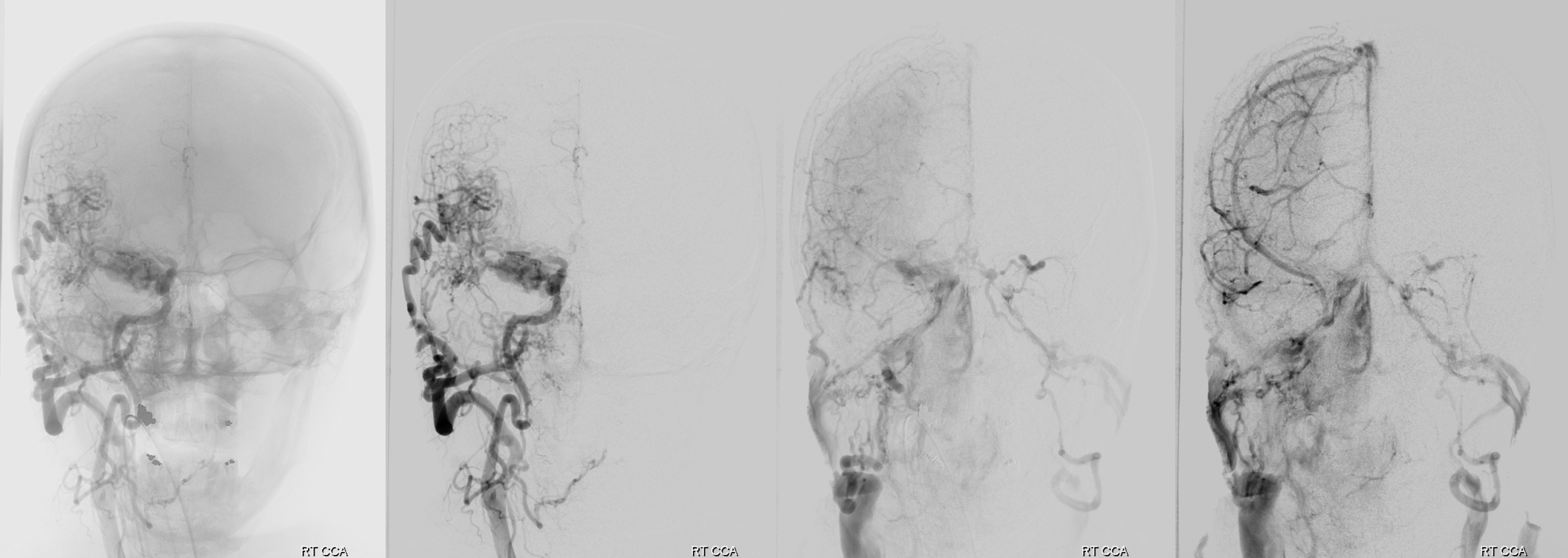
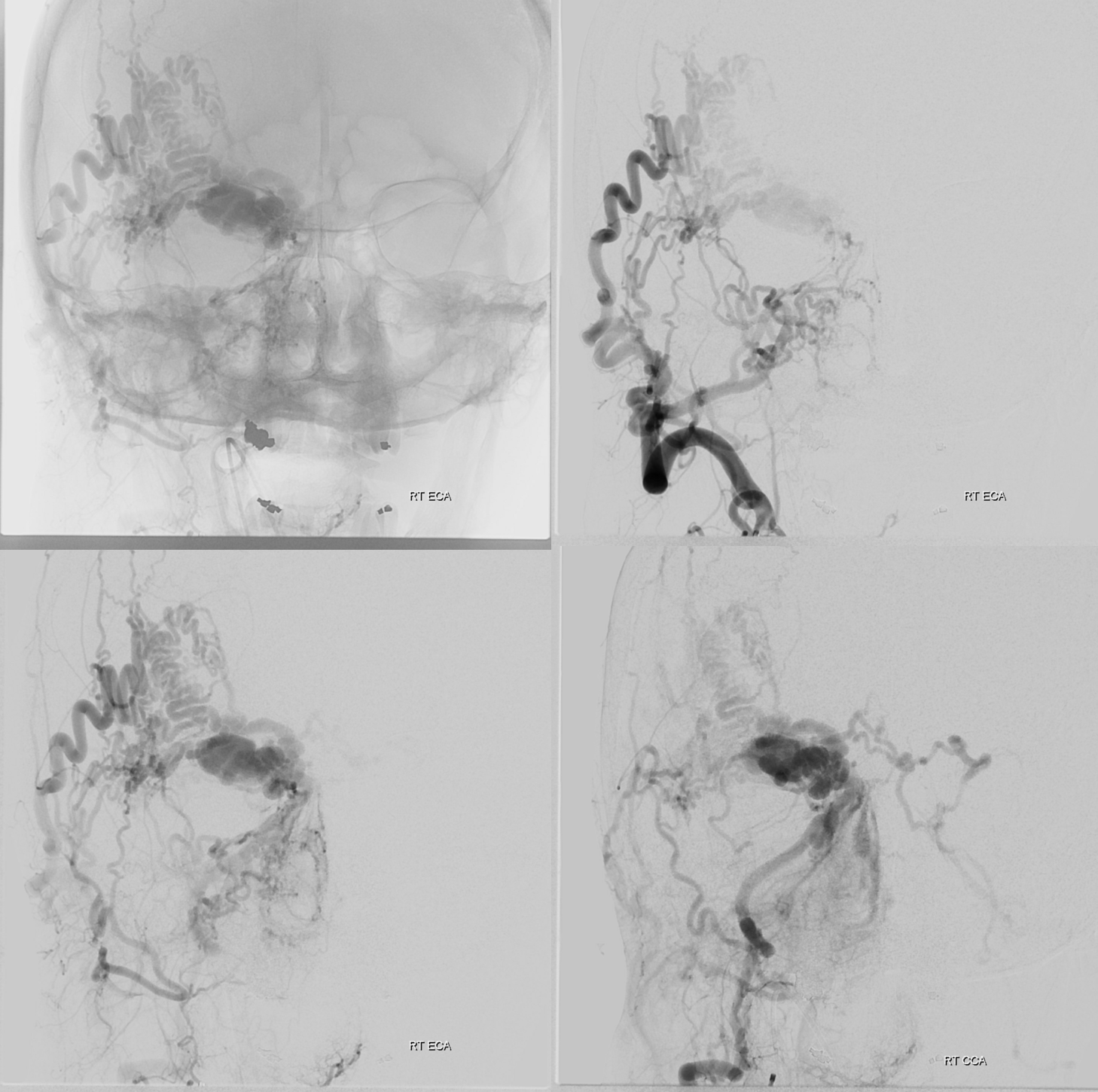
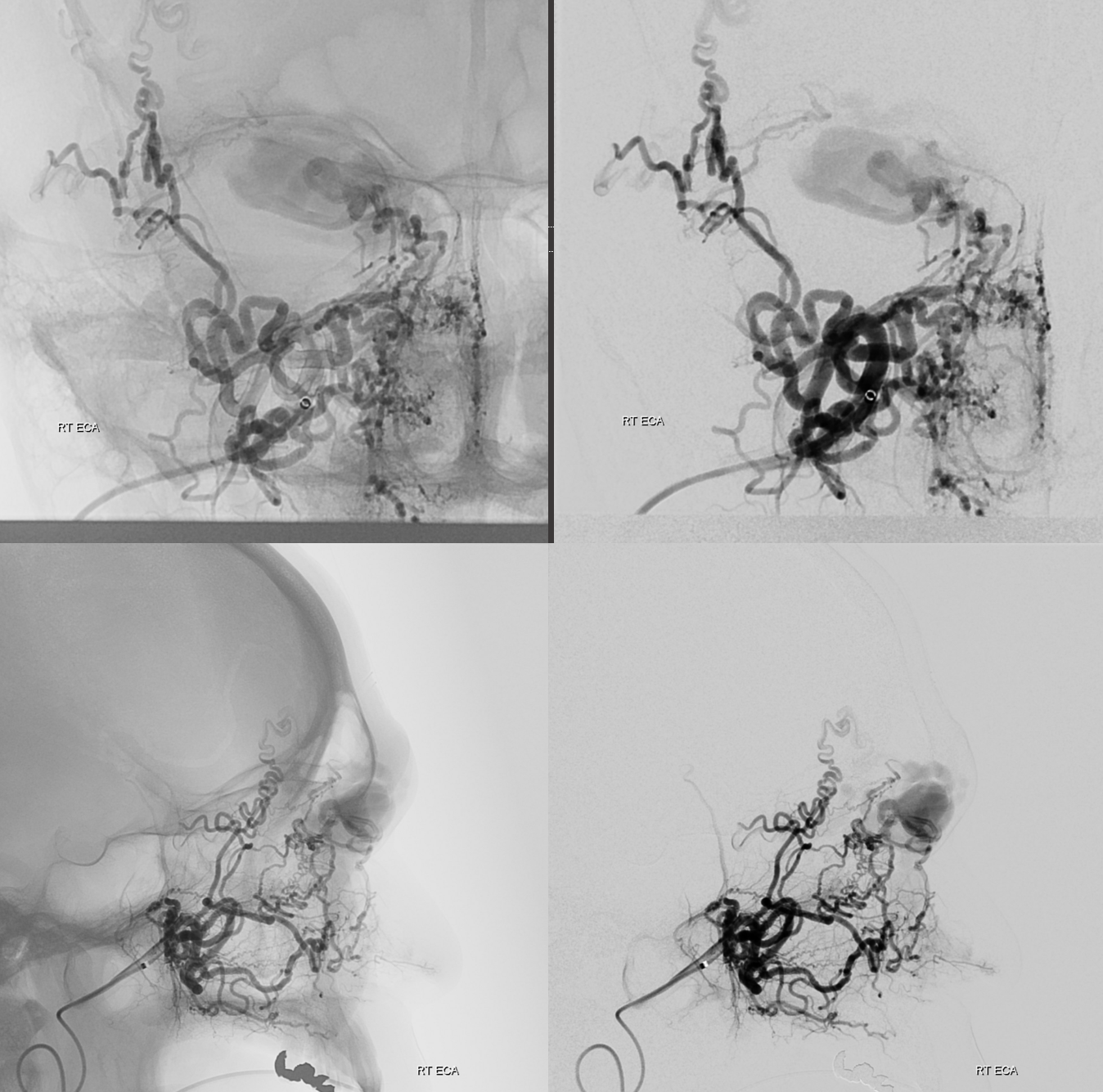
So, what can we conclude? An experienced operator would be impressed by lack of direct arterial supply to the AVM. There are a myriad of small vessels with perhaps most direct one coming from the ophthalmic. The usual reason for this is prior surgery or embolization. There is no embolic material seen. Indeed this person had 2 prior surgical excision attemps.
Which leads us to realize that all transarterial routes are really bad. As are venous ones too
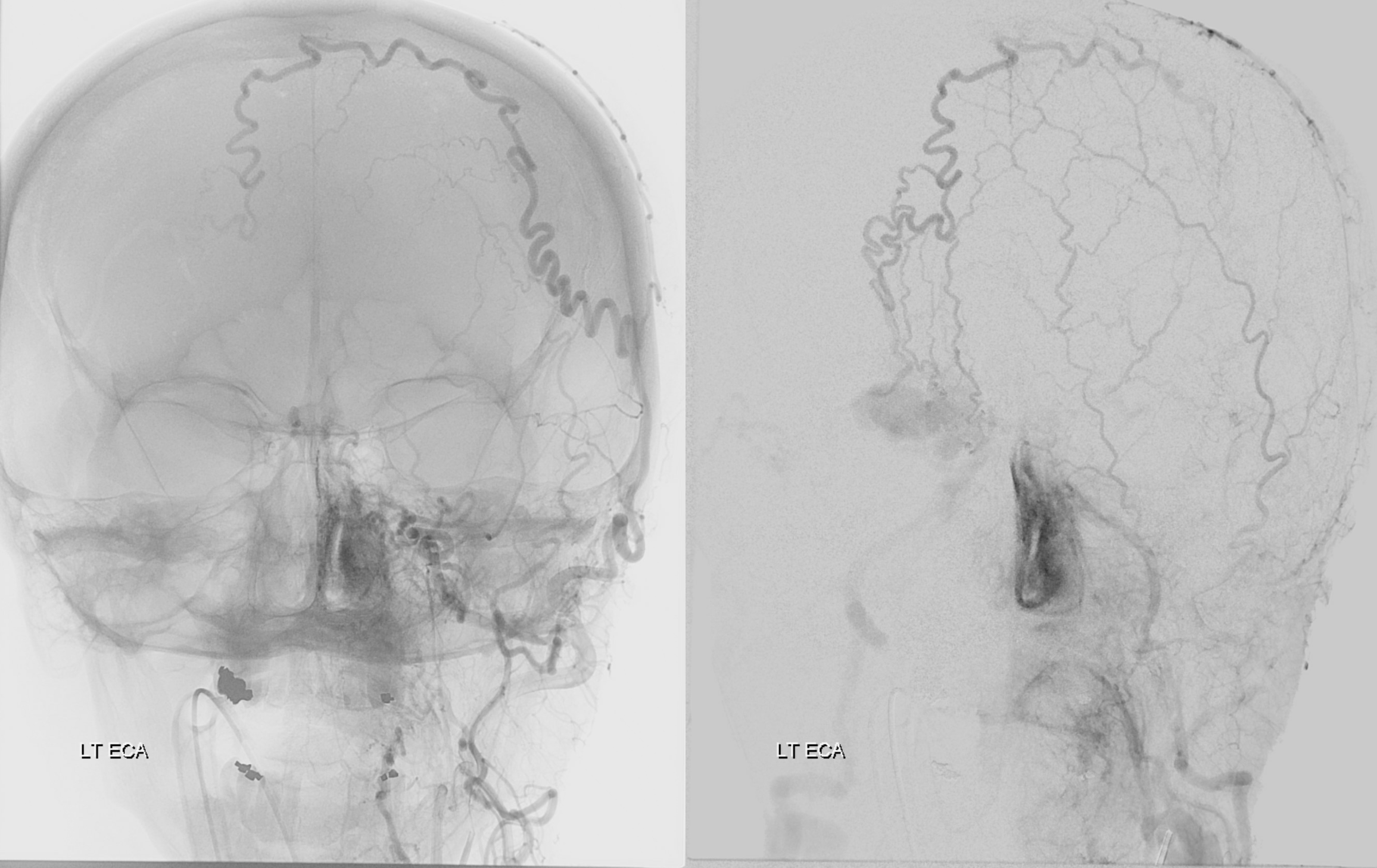
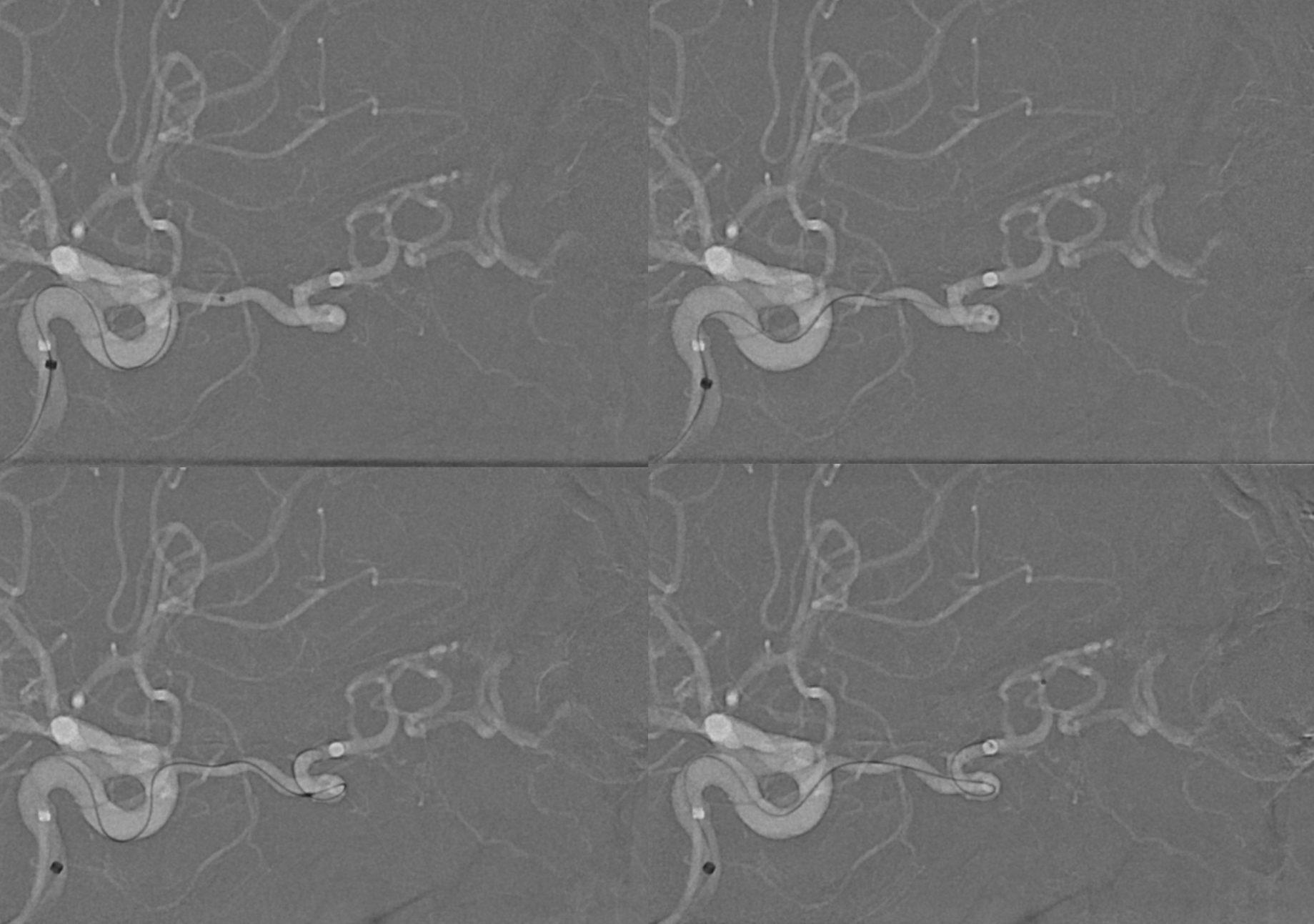
What to do? Direct stick embo. Its surprisingly effective and often quite straightforward. Here, the spot is marked on a roadmap image, and a 21 gauge butterfly needle inserted into the venous pouch.
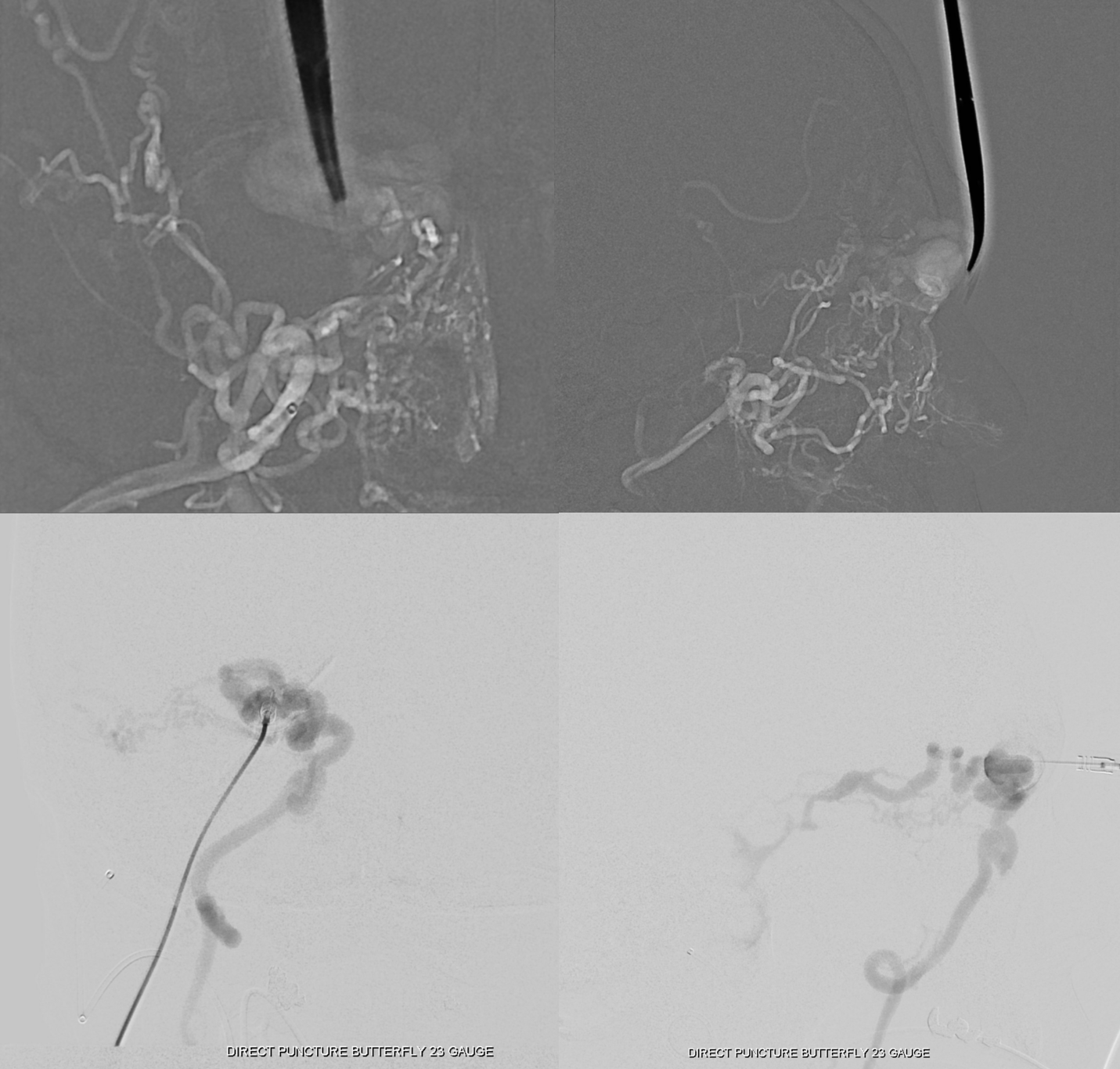
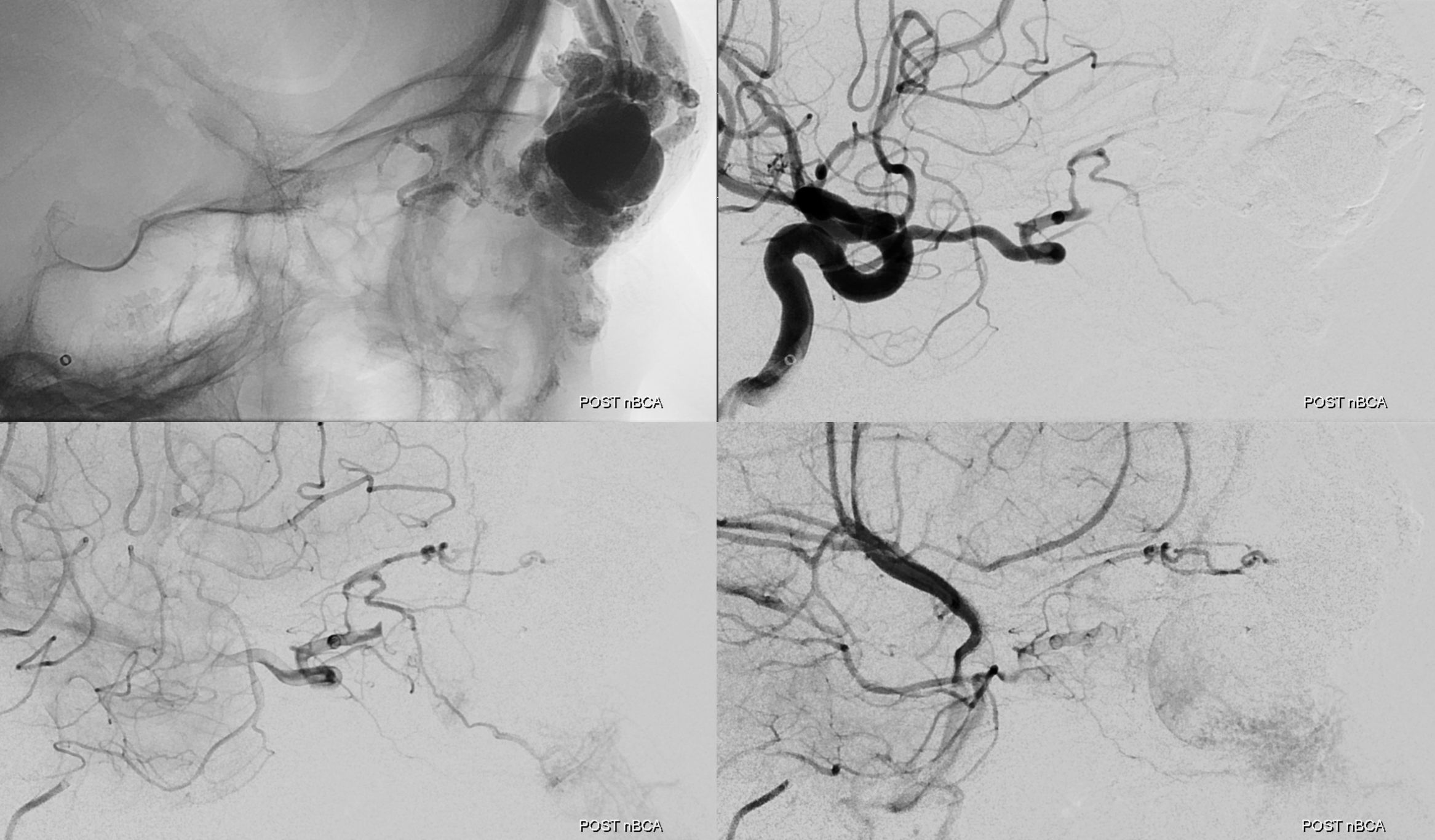
Next comes embo. We prefer nBCA for this. In does not sparkle like Onyx does during resection. It does not discolor the skin. It is a more thrombogenic agent. And it is faster.
We made the nBCA:Lipidol dilution 1:2. Really 1:1 is probably better, as not as much of it flies through the shunt. However, it will take 2x the amount of nBCA, and in the end they are both safe and effective. Movies of injection below. Note that much of the embolic material flies through the shunt, and is trapped in the cavernous sinuses or elsewhere. This is a typical feature of nBCA embolization and is not an issue, unless there is a large right to left shunt present or some extreme pulmonary insufficiency.
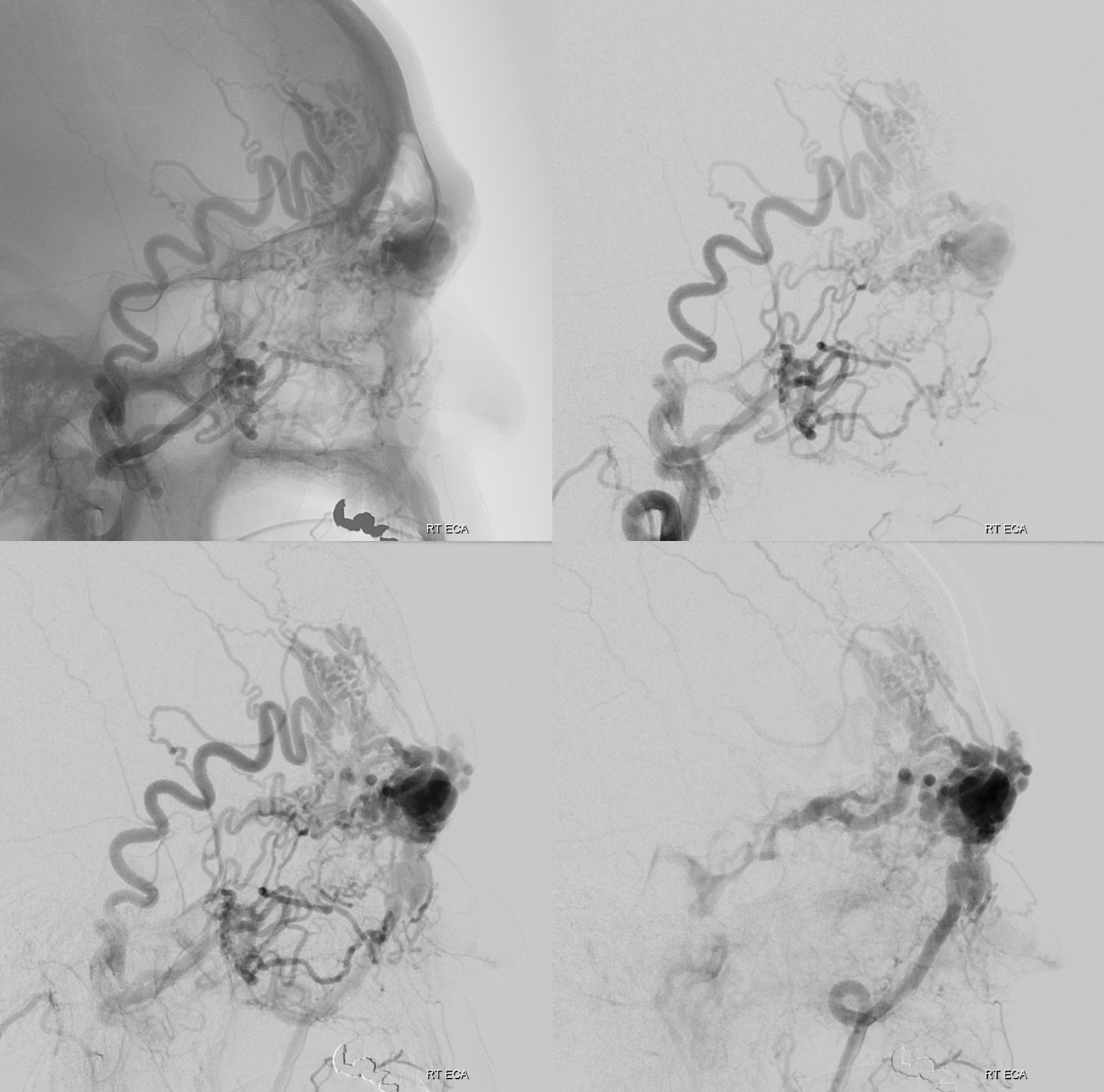
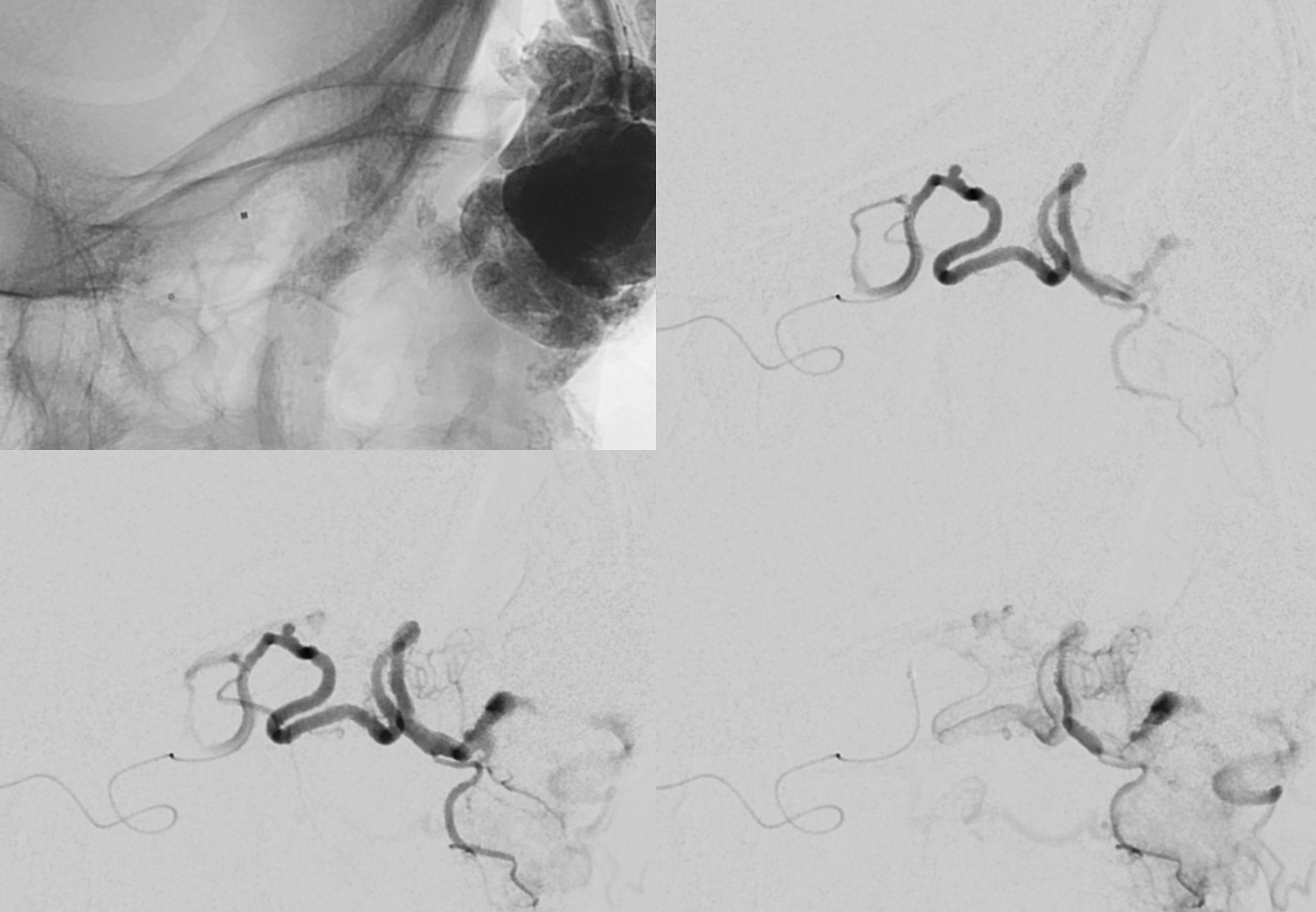
Took about 6 mls of nBCA:Lipidol mix. Post is beautiful
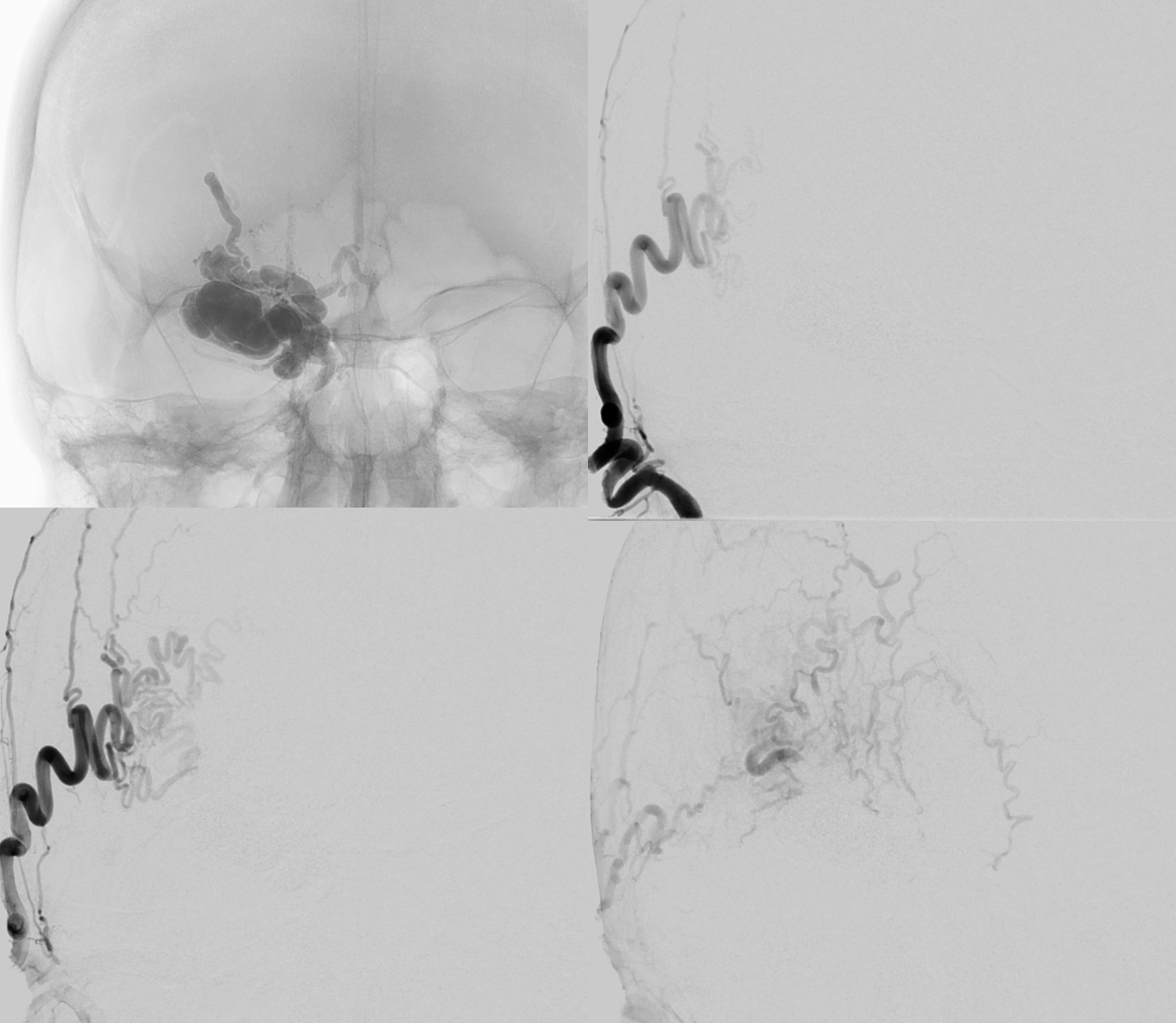
There is a suggestion of something still supplying the “nidus” in the back of the AVM via the ophthalmic artery
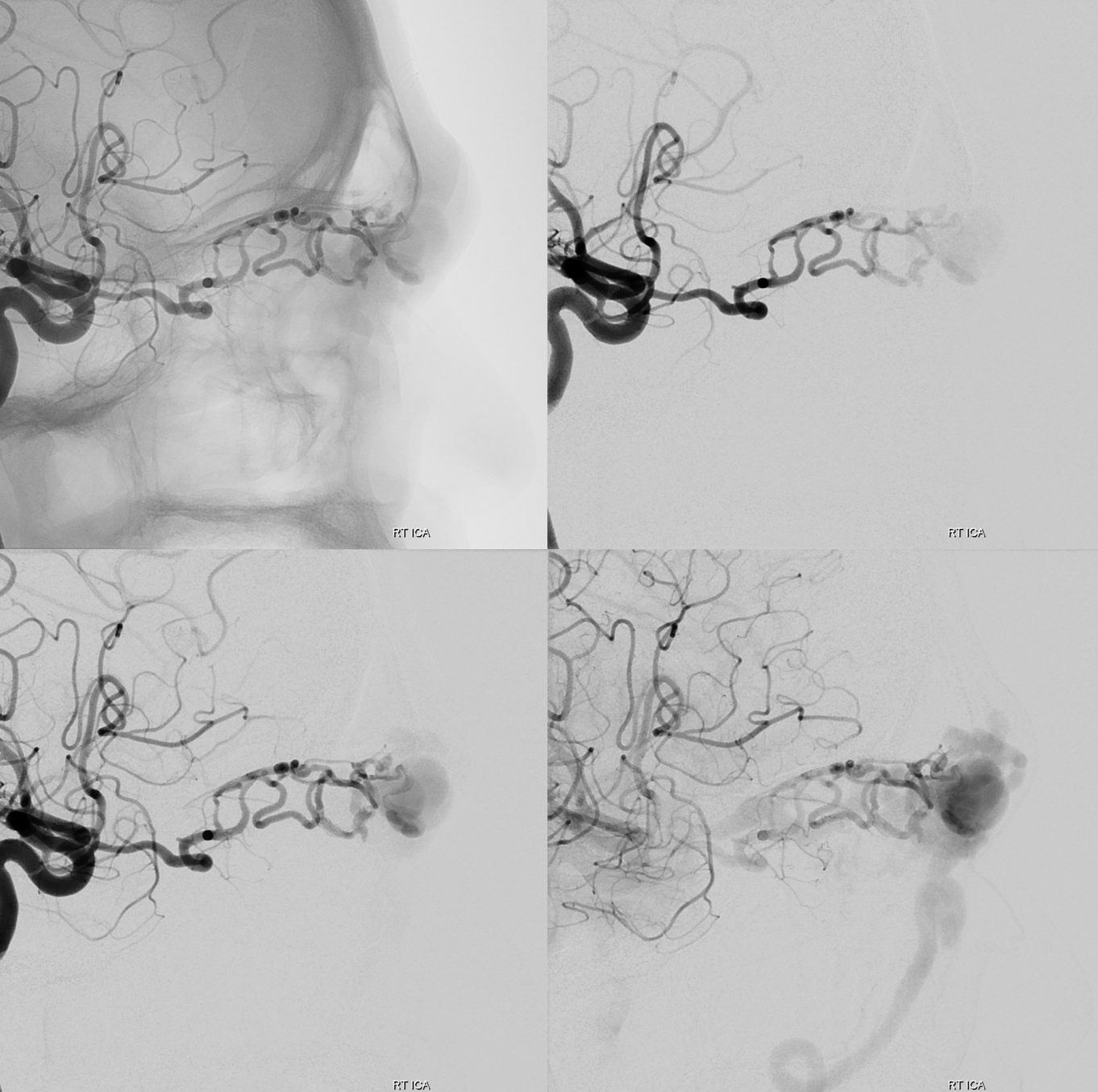
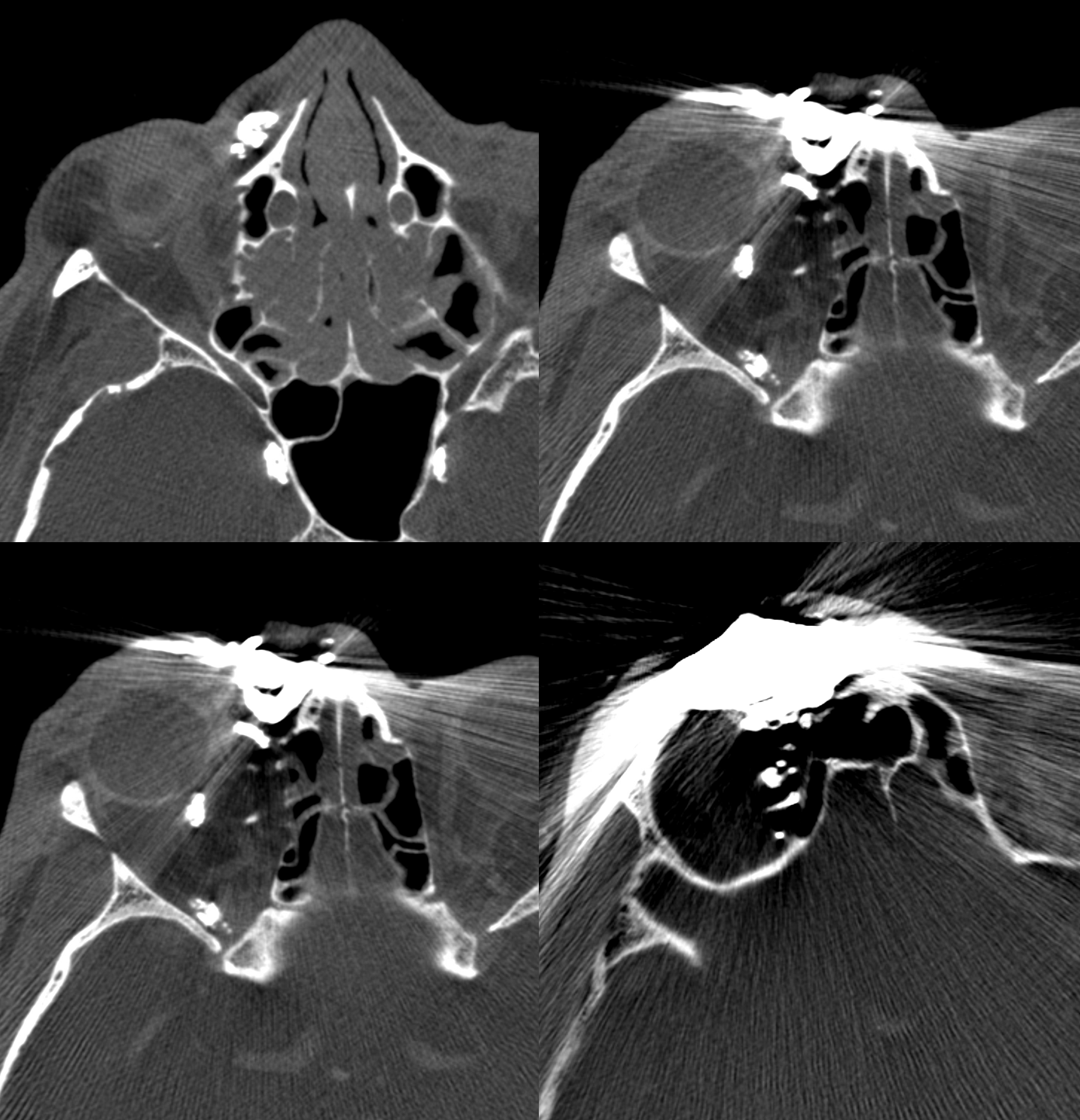
Do we have to go for it? Maybe not. But, if there is a problem, this what’s going to bleed at the bottom of the surgical field. The supply is quite distal. Approach is Magic 1.5F and .08 hybrid
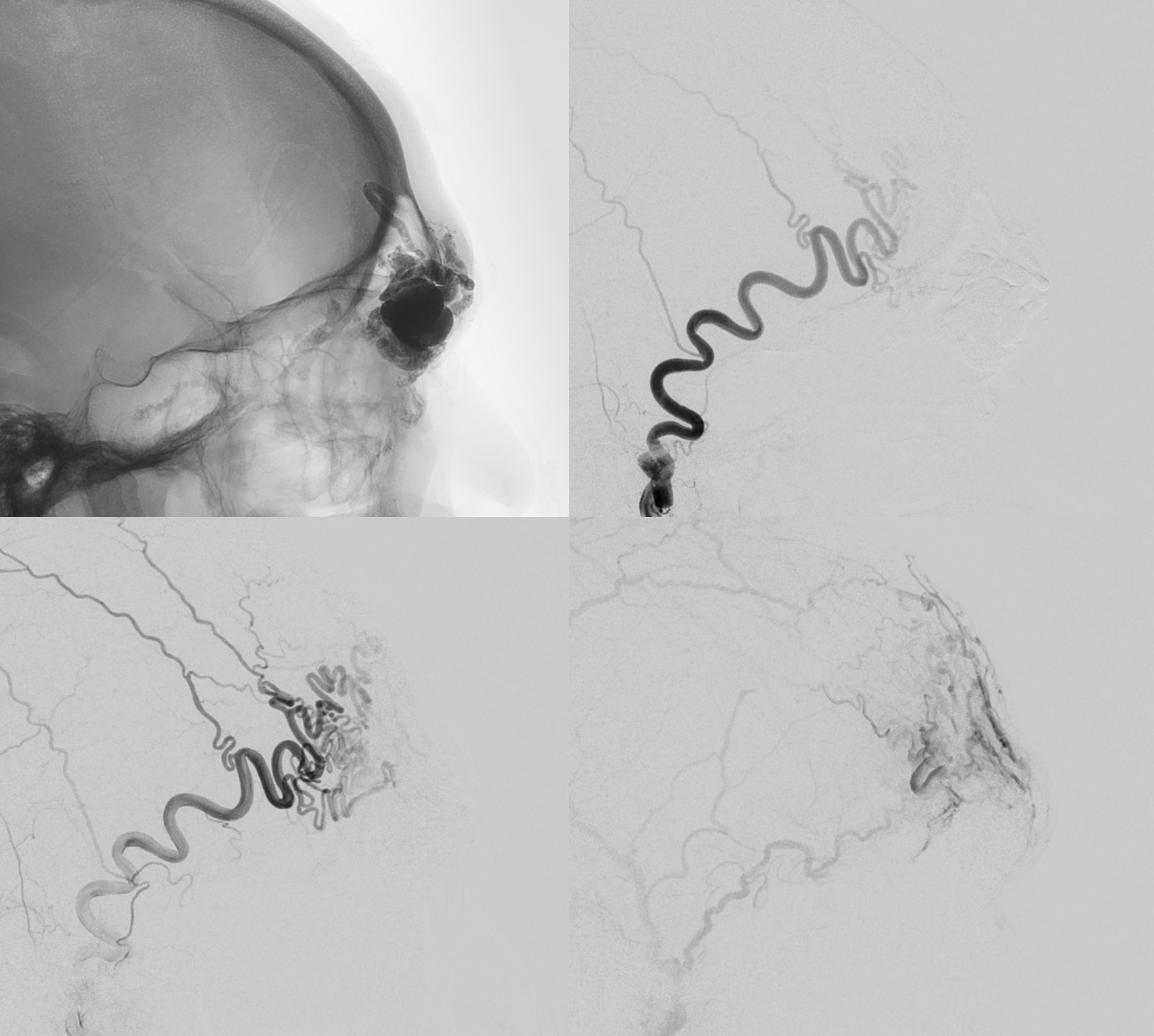
This is as far as we got with the 1.5. A 1.2 would have been better in retrospect, but both are equally safe in terms of the central retinal origin
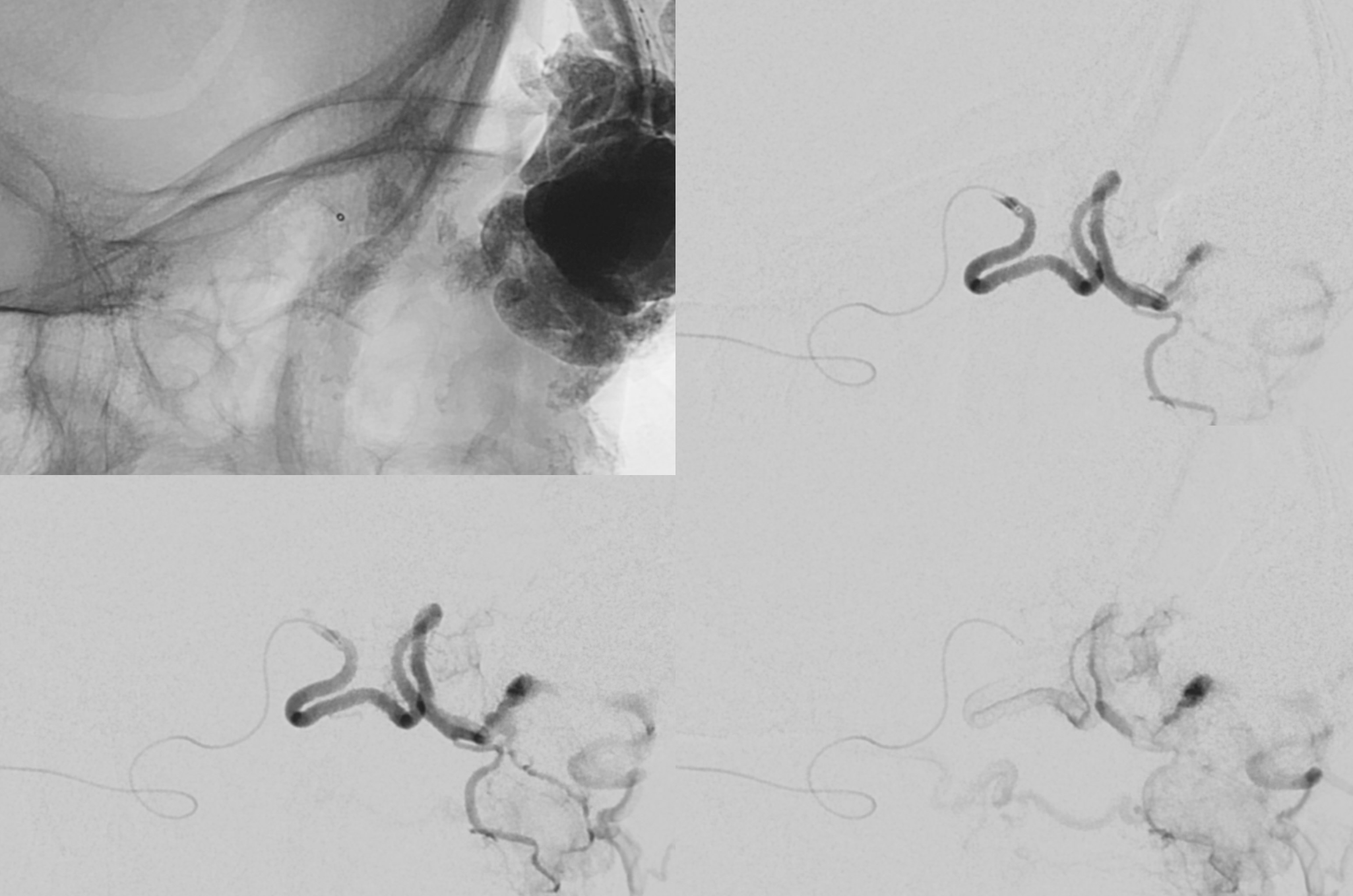
Unfortunately the glue shot was not recorded. The cast is seen in the orbit.
Next day, this comes out as a dry lump of glue




