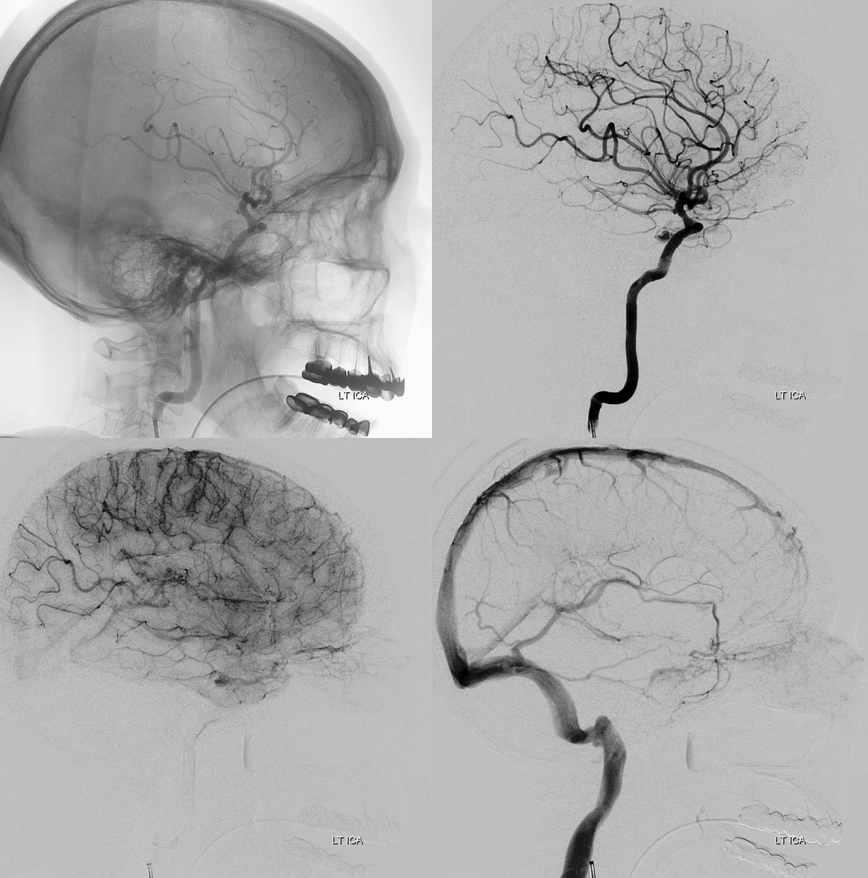
With Eytan Raz. We have several cases illustrated here. This one presents with classic proptosis / chemosis lasting several months, followed by rapid visual acuity decline. Typical CTA appearance
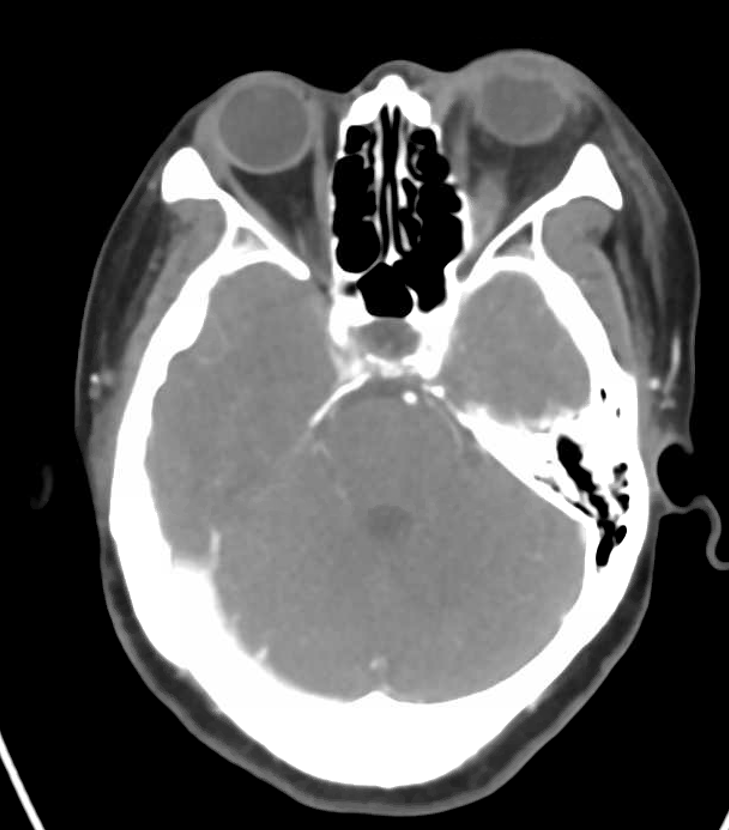
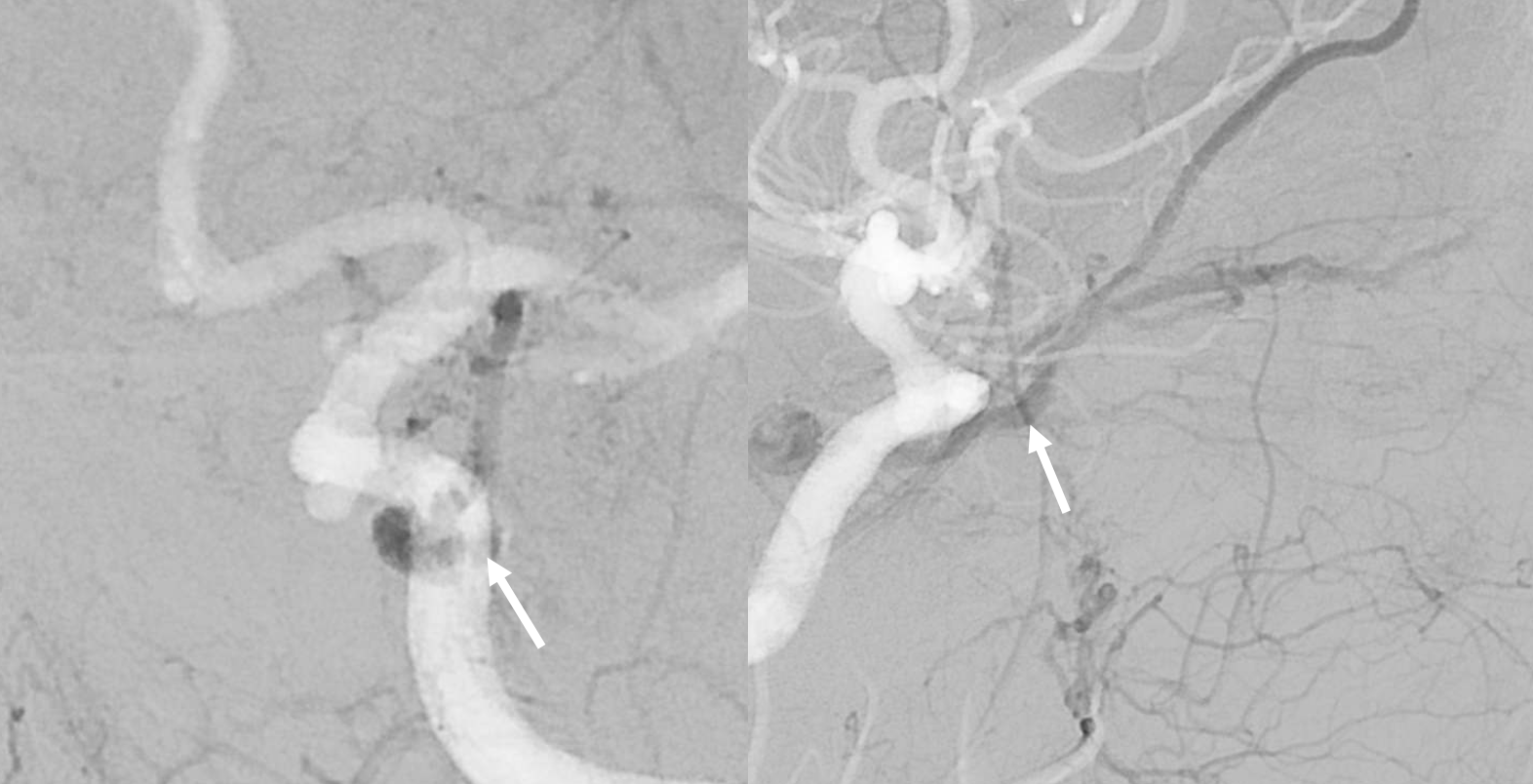
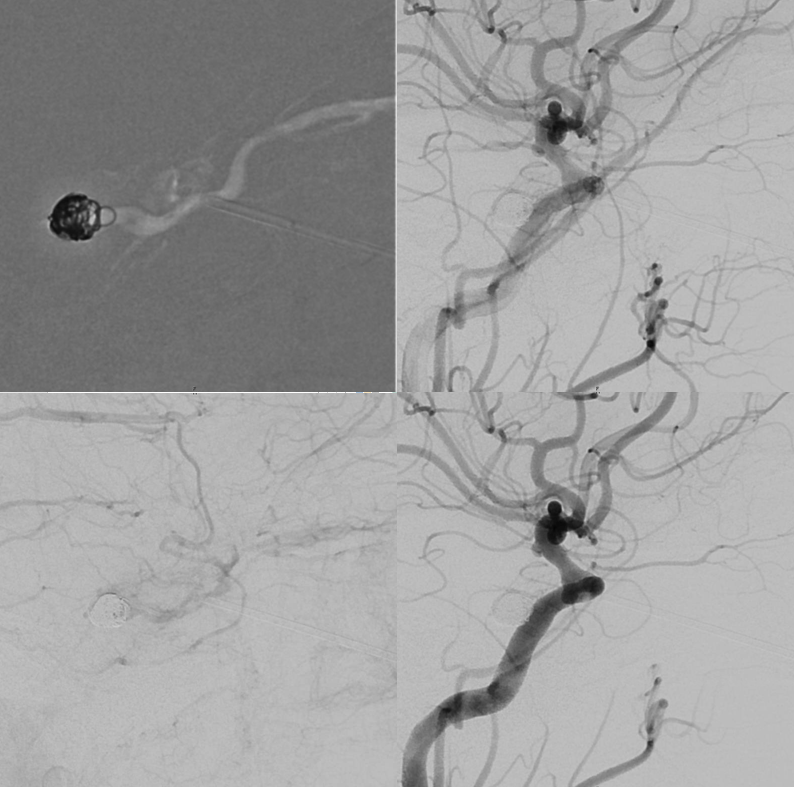
Angiogram shows a key finding — which we always emphasize. Fistula is a venous congestion problem. As such, the symptoms are more directly related to lack of venous outflow than fistula size. One can have a huge high flow cavernous sinus fistula and decent vision — if there is outflow. Or, there can be a small fistula — such as here — and 20/200 vision — because the superior ophthalmic outflow is occluded.
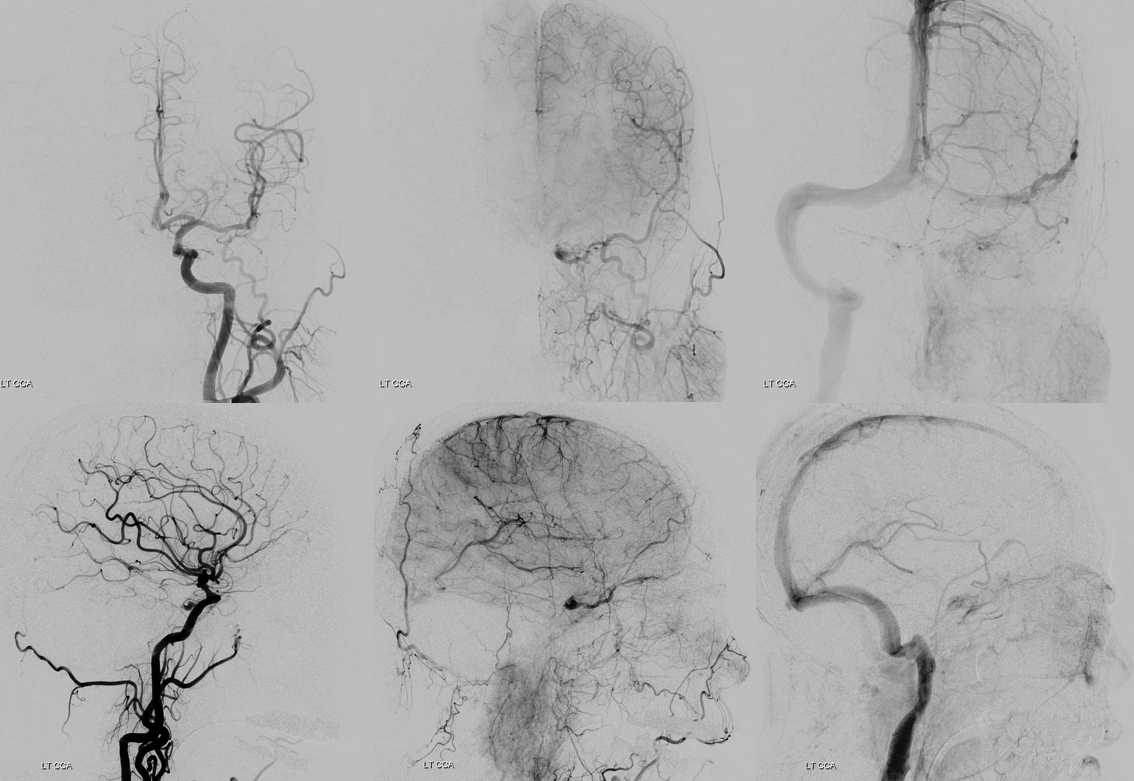
External supply is from where?
Internal supply is from where?
Small fistula with no outflow means big symptoms
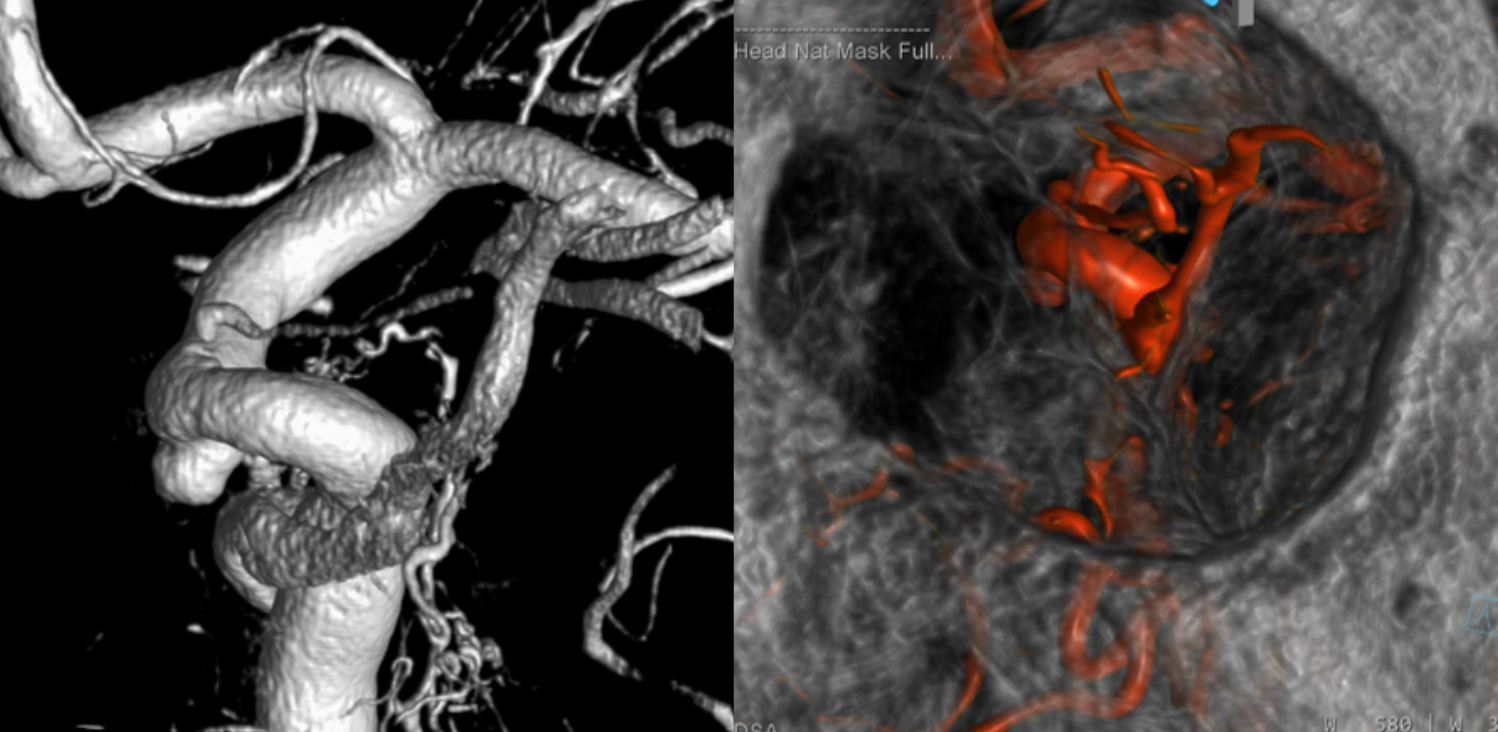
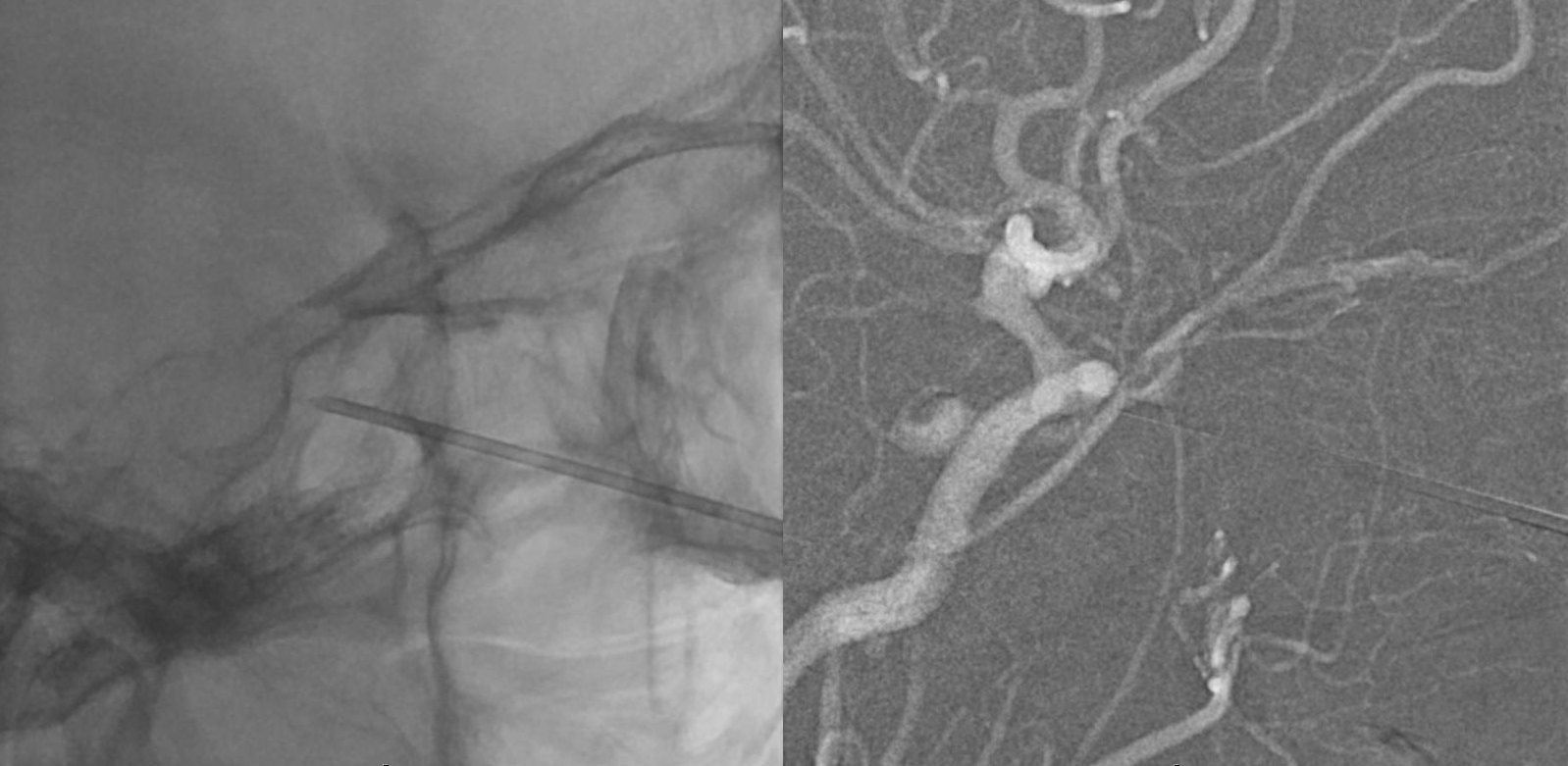
MIP axial DYNA video — stop and scroll thru slices
The dilemma here is that there is no obvious transvenous route. The IPS is not visualized. It might be usable still — see case here for example.
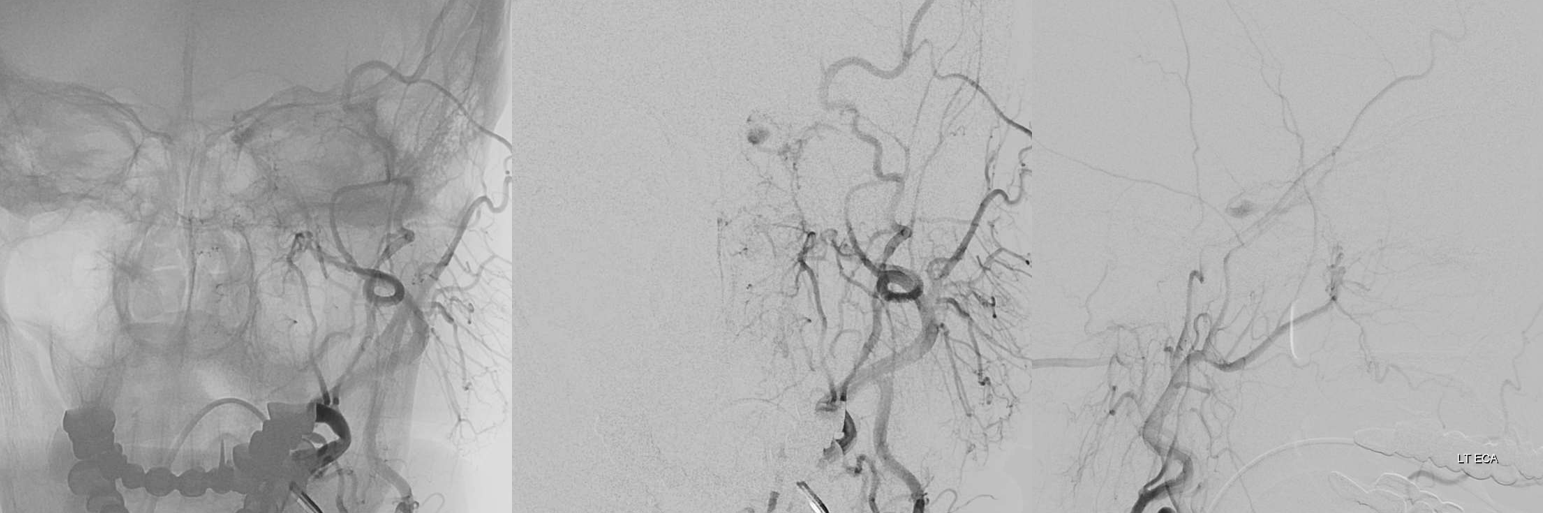
We tried and could not get through. Now what? Transorbital access is an excellent option here. The anterior portion of the cavernous sinus — at its junction with the SOV and IOV — is patent. This junction point — just deep to the upper medial aspect of the inferior orbital fissure – is the target.
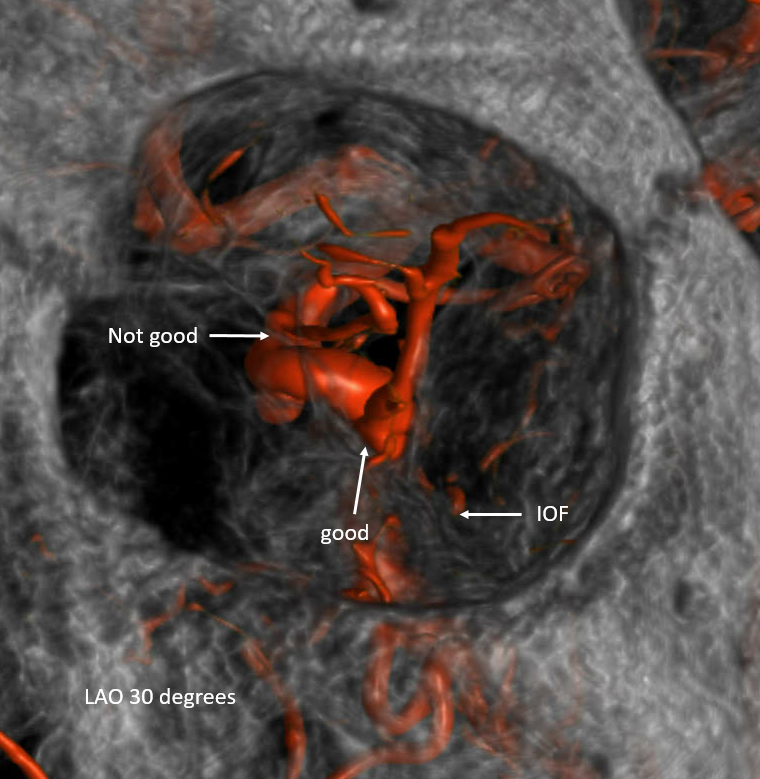
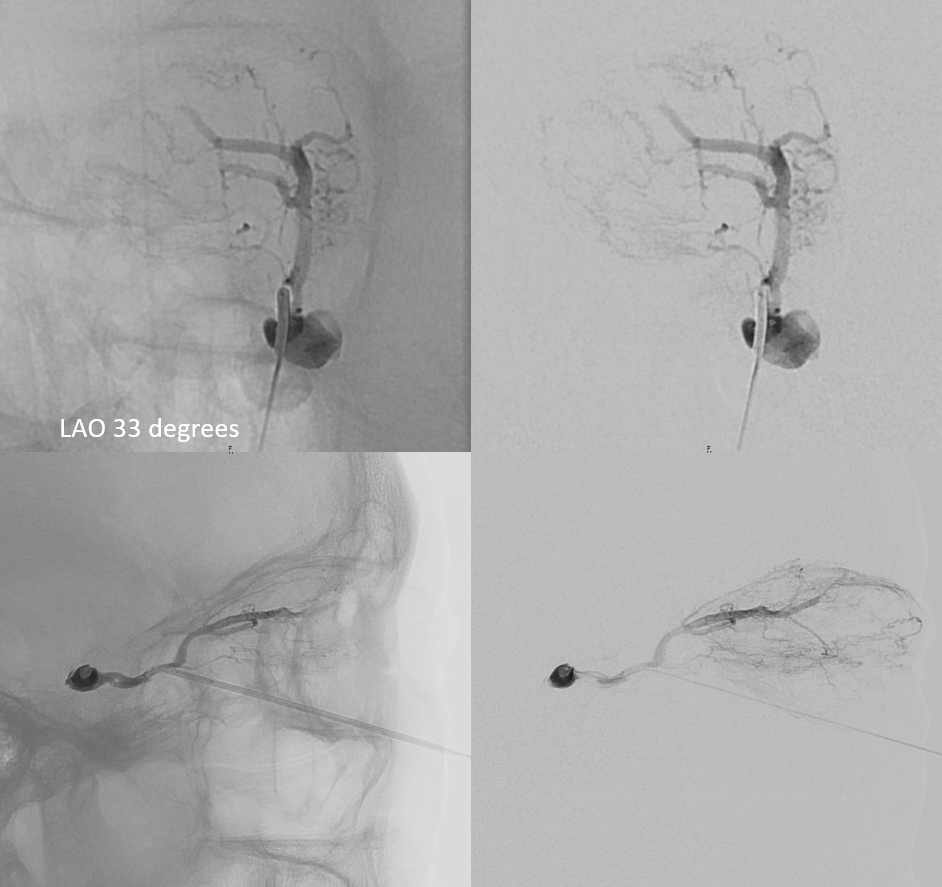
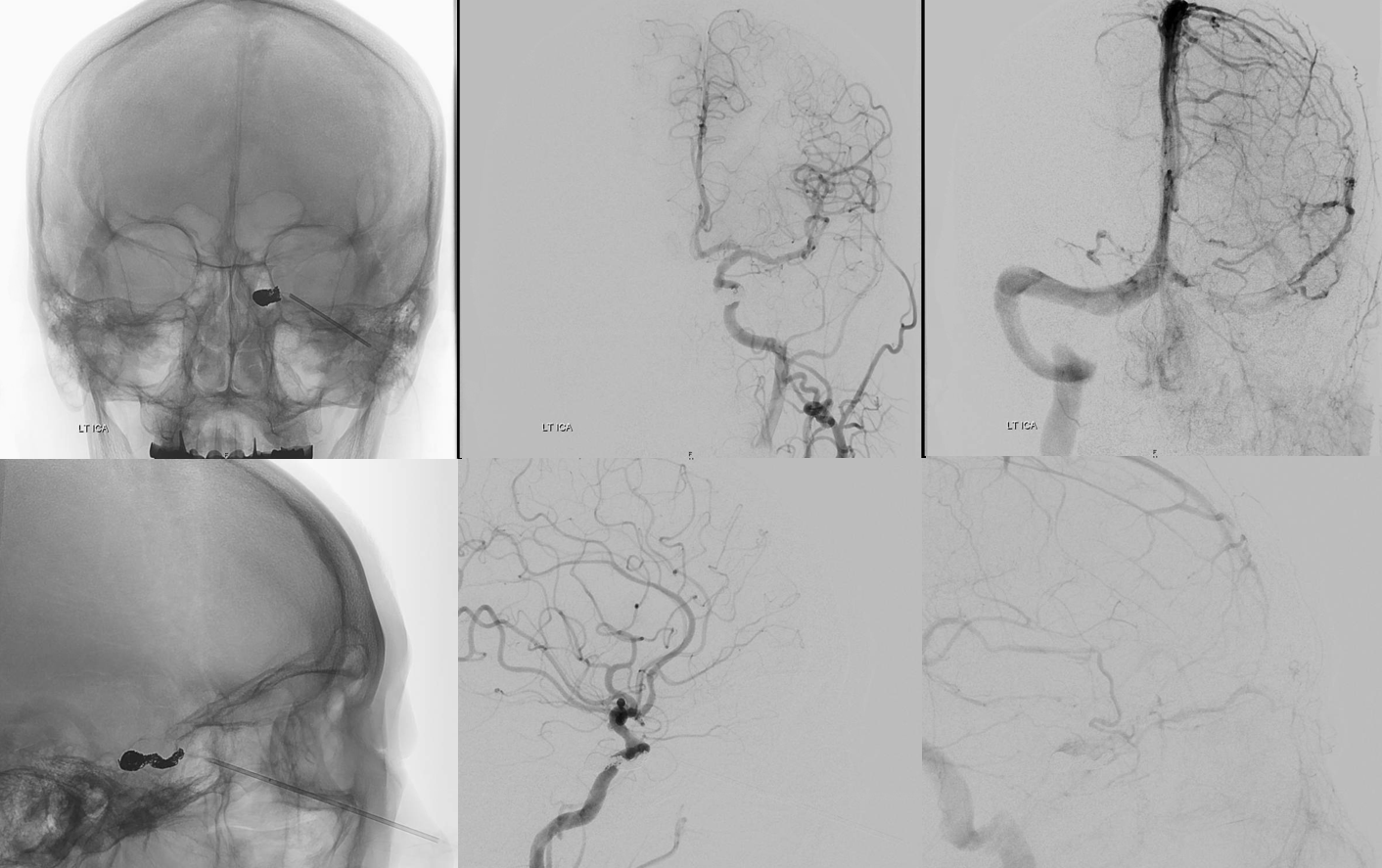
Technique has been described in several publications, including our video. We use angiographic roadmap guidance — not “needle guidance”. The camera is positioned about 30 degrees into ipsilateral oblique (LAO here). This is looking down the orbit directly. Easier to follow the inferior orbital fissure and stay away from the optic canal and ophthalmic artery. See below. The needle is walked along the inferolateral aspect of the orbit (5 o’clock here) — pointing bevel down to walk along bone — until target is reached. Brisk bleeding means its in a good place. We use an 18 gauge femoral access or 3.5 inch spinal needle. In our experience it is better than using micropuncture and trying to exchange needle for micropuncture dilator over a wire — there is risk of losing access — which is very bad, since it means bleeding already hyper-pressurized orbit. The ophthalmologists need to know you are up to this and be ready for a canthotomy.
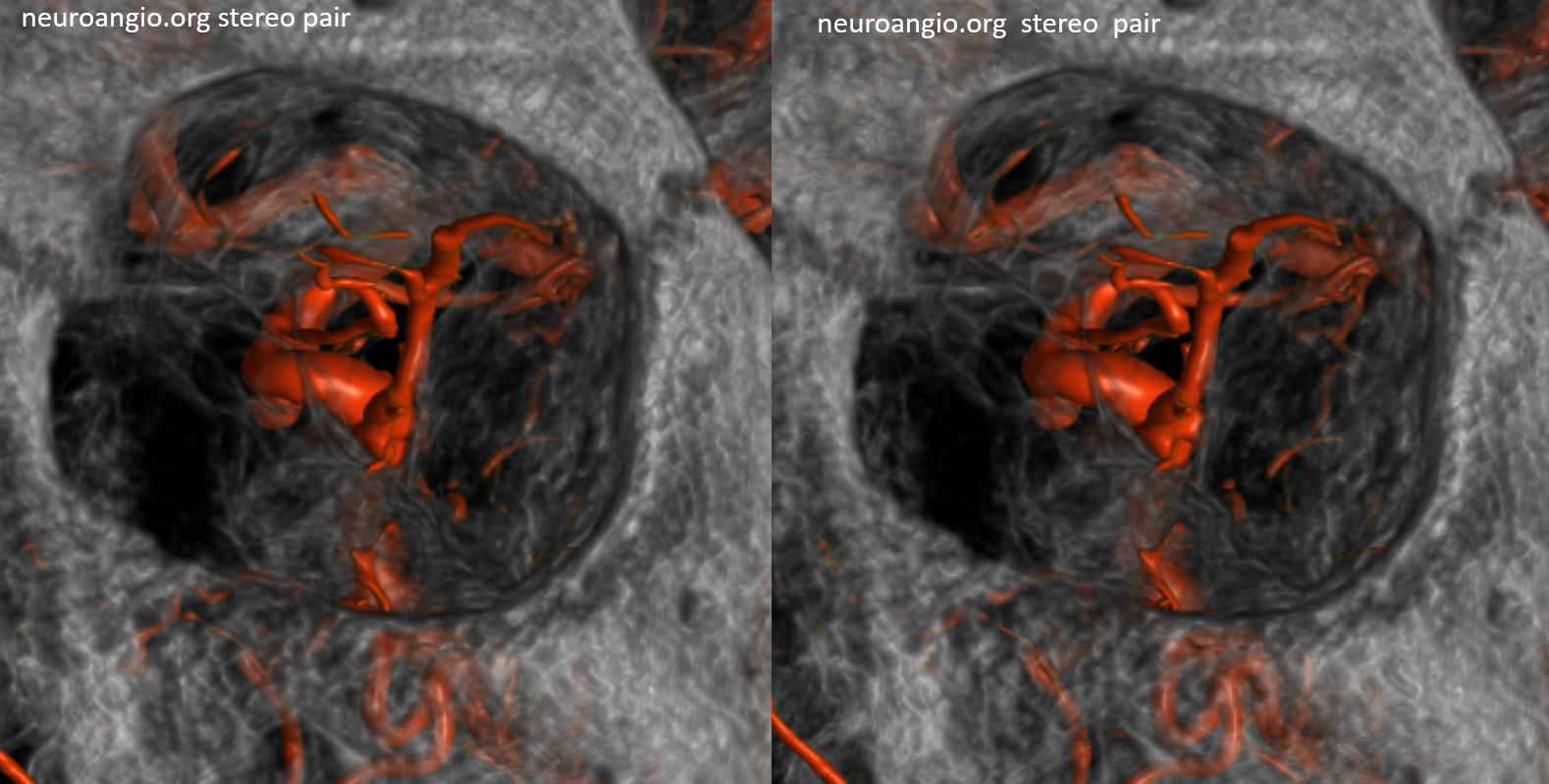
Stereos
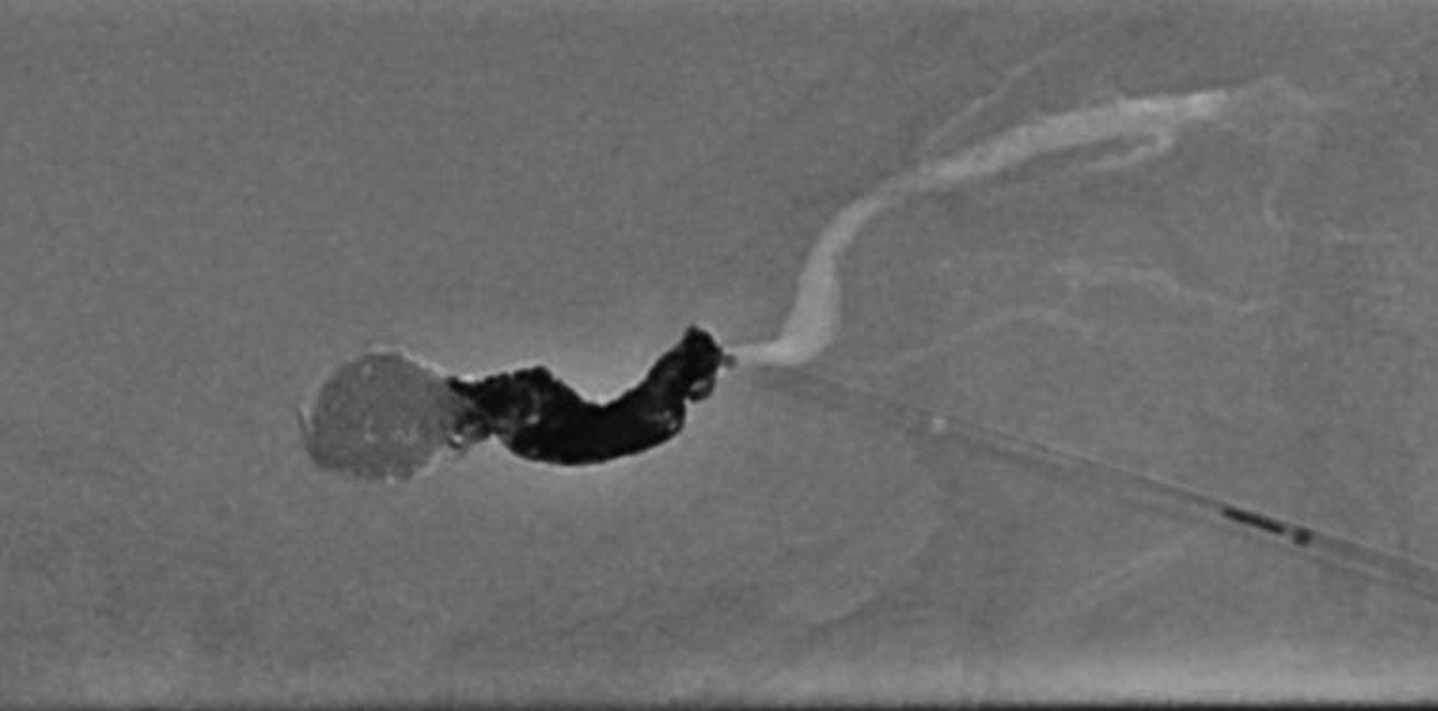
Double Contrast roadmap — the target is arrows
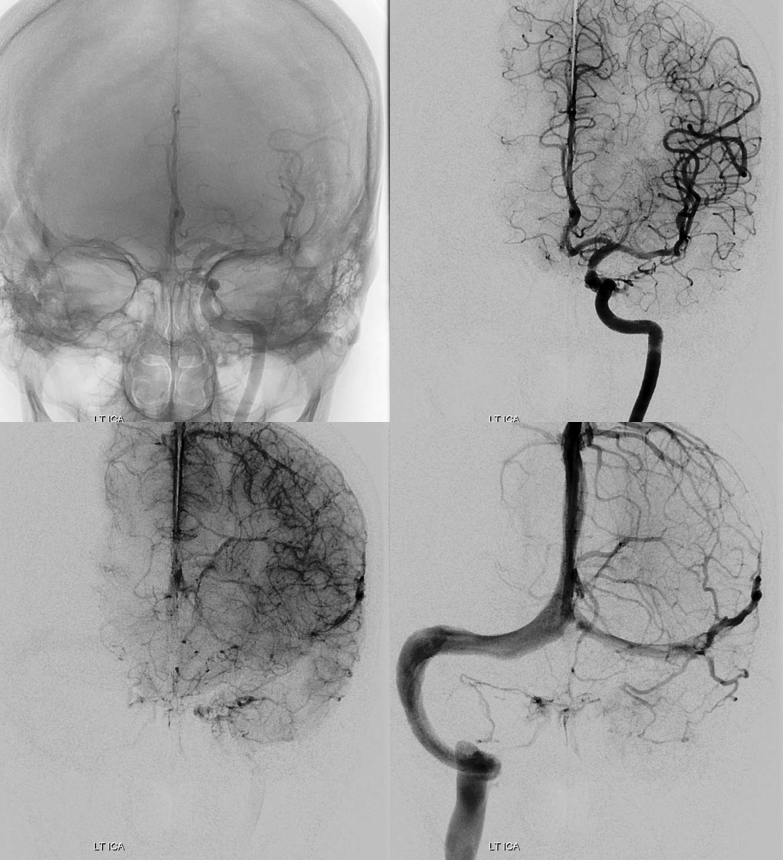
Amazing picture — notice venous congestion of the optic nerve and central retinal vein!
Once needle is in — brisk bleeding — consider advancing another half mm or so — to make sure you are not partially in and partially out (like a myelogram epidural issue) — and bleeding into orbit. Then insert microcatheter / wire and hope it gets into the sinus. It does. Important to get to right place and not paint yourself out of it.
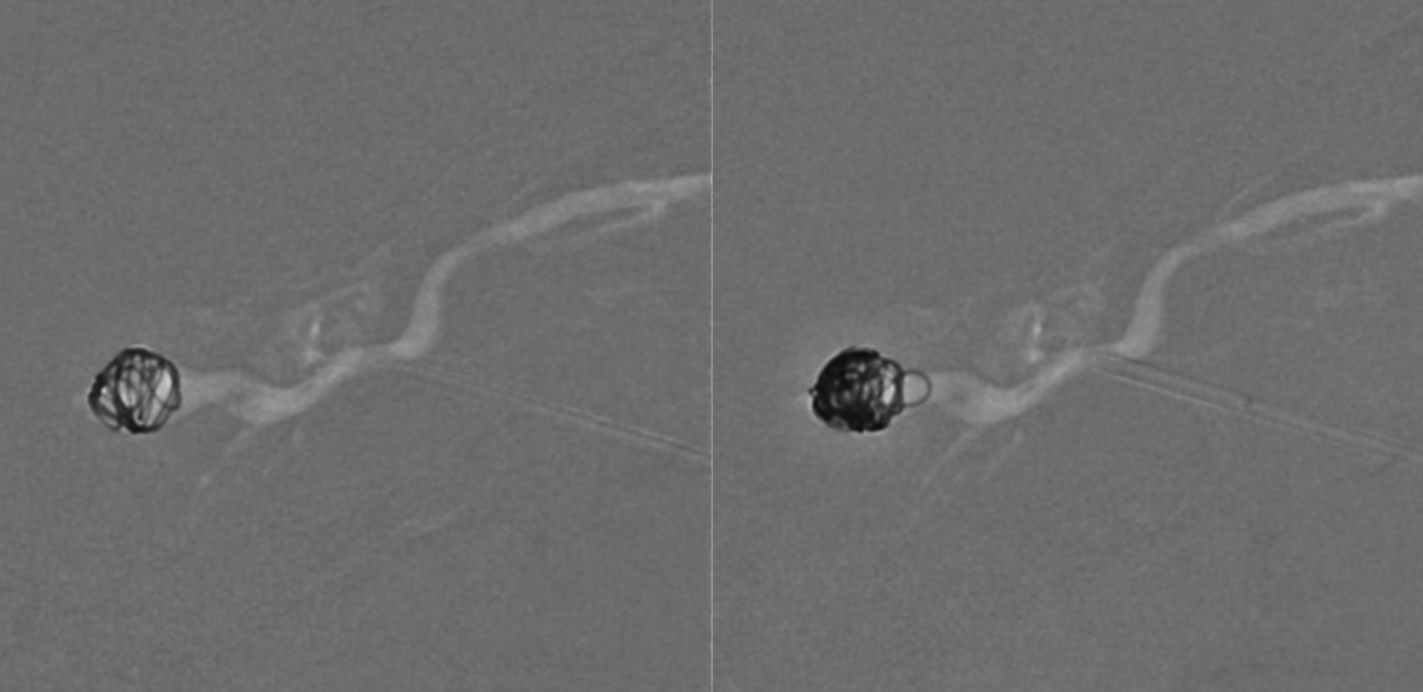
No more fistula
Although a few coils do take care of it — we love superselective embolization — see here — this is one time we don’t like to be too cute. Its best to seal the needle entry point with coils or whatever else.
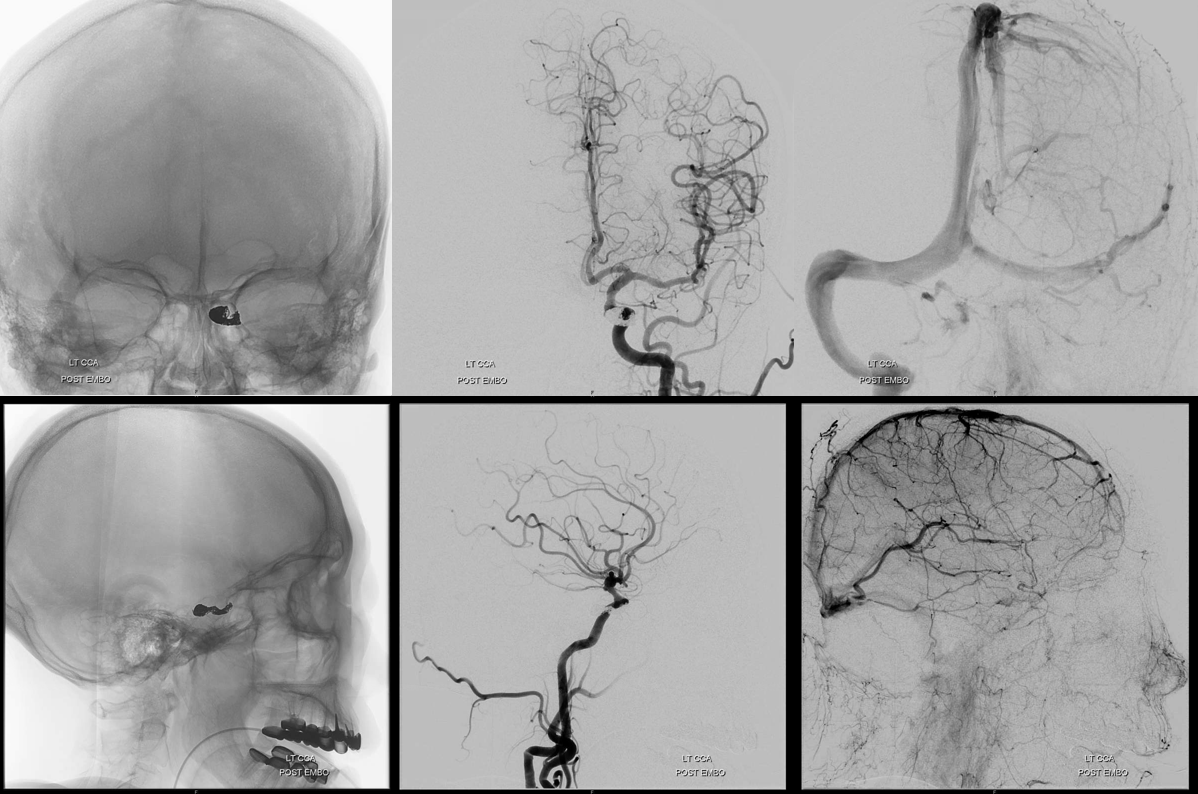
Ultimately this patient made a 20/40 recovery. But, she had a canthotomy in the ER prior to our embo and another canthotomy (one might argue that a full first one would have been enough) right after embo. Although usually one is not necessary, doing this without ophthalmology knowledge is a mistake, especially if you need them after.
See another case of transorbital direct access here
