Making this diagnosis remains extremely challenging. We rely on morphology and location to make it pretty much anywhere in the body. What if location is nonspecific, and morphology is hard to tell because vessels are small? It is a problem with important clinical implications, as treatment of dissection is often different from other causes
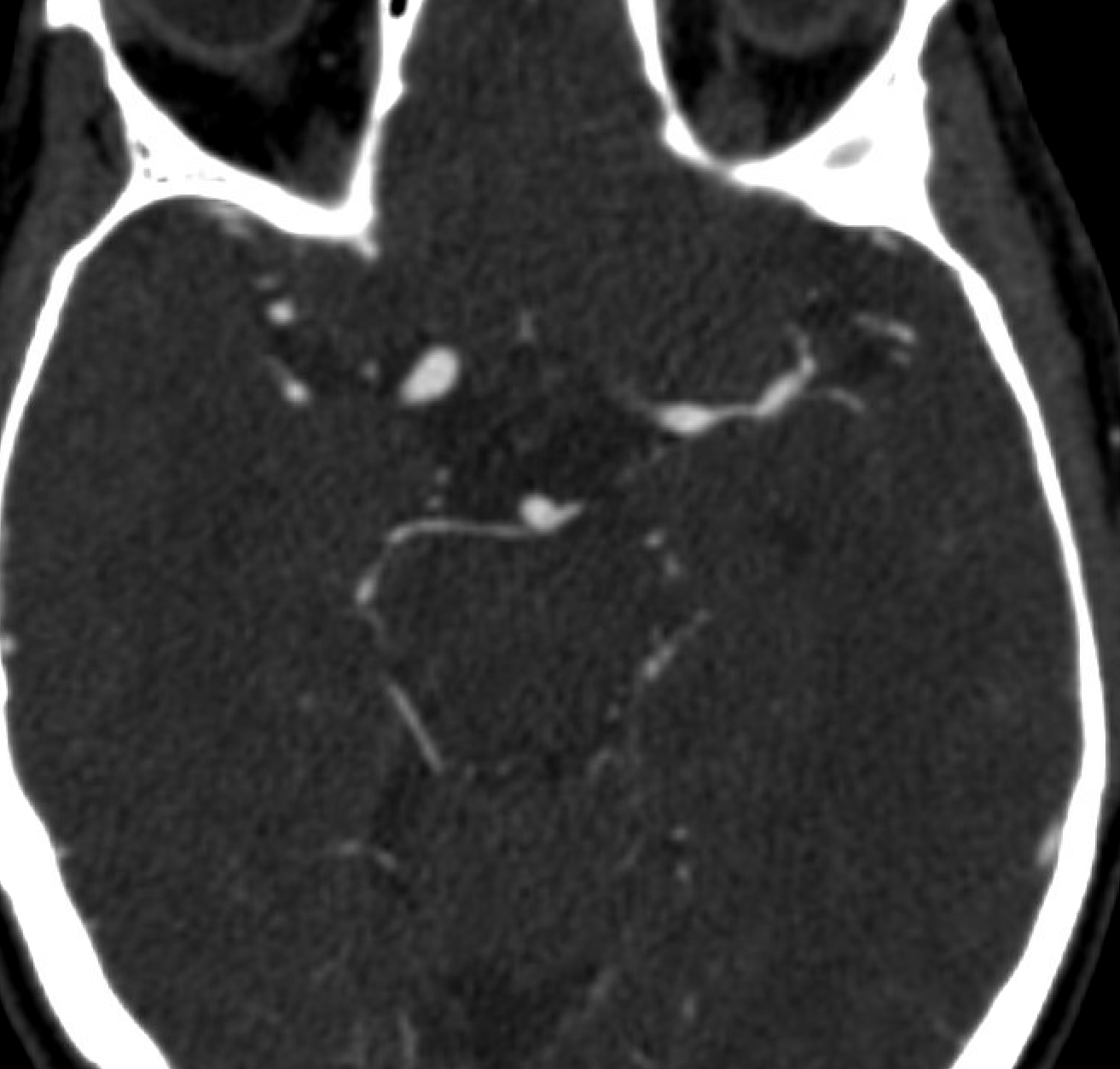
Patient presents with mild aphasia. There are no risk factors for atherosclerosis. CT is normal.
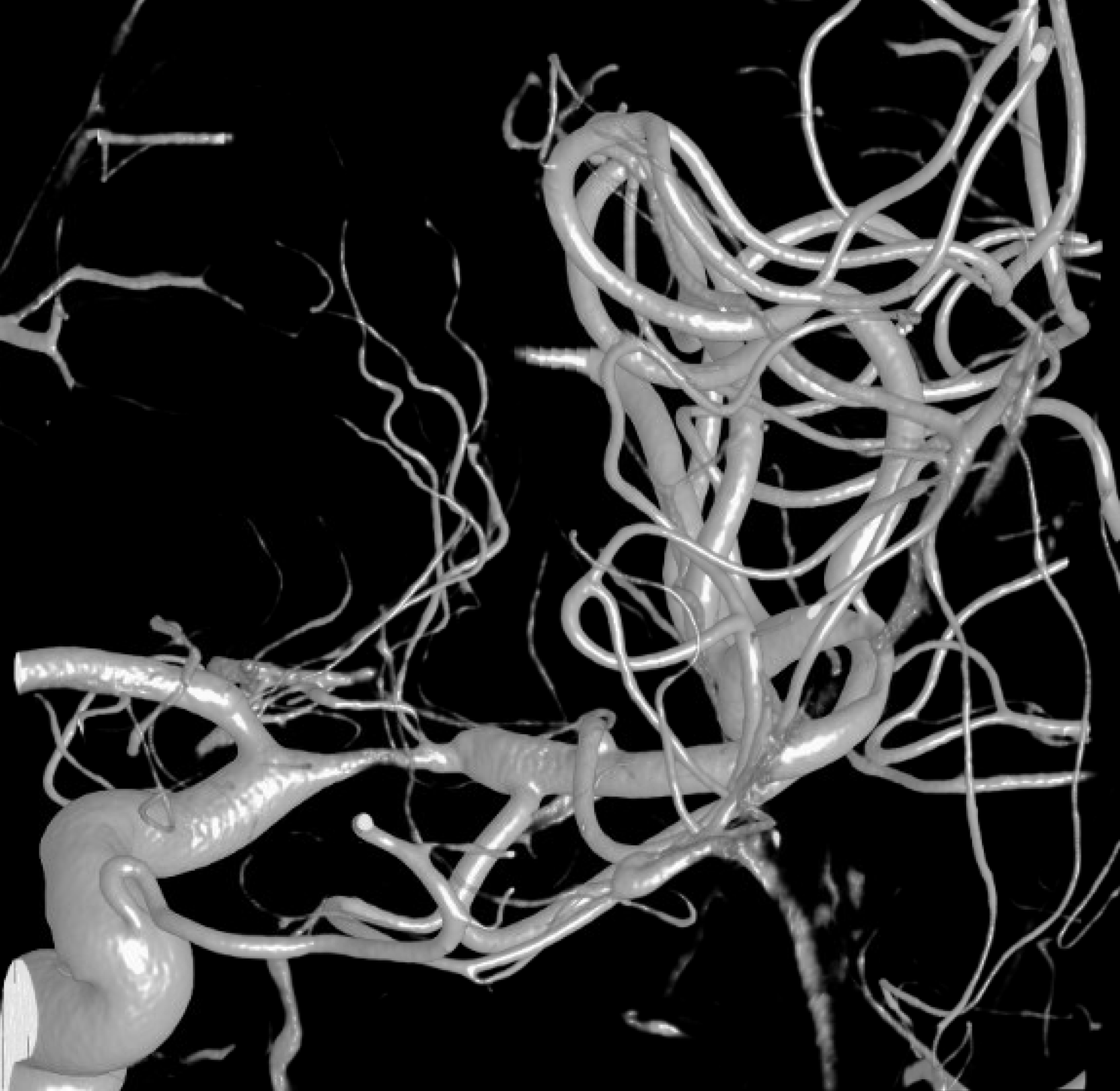
CTA — typical intracranial athero location
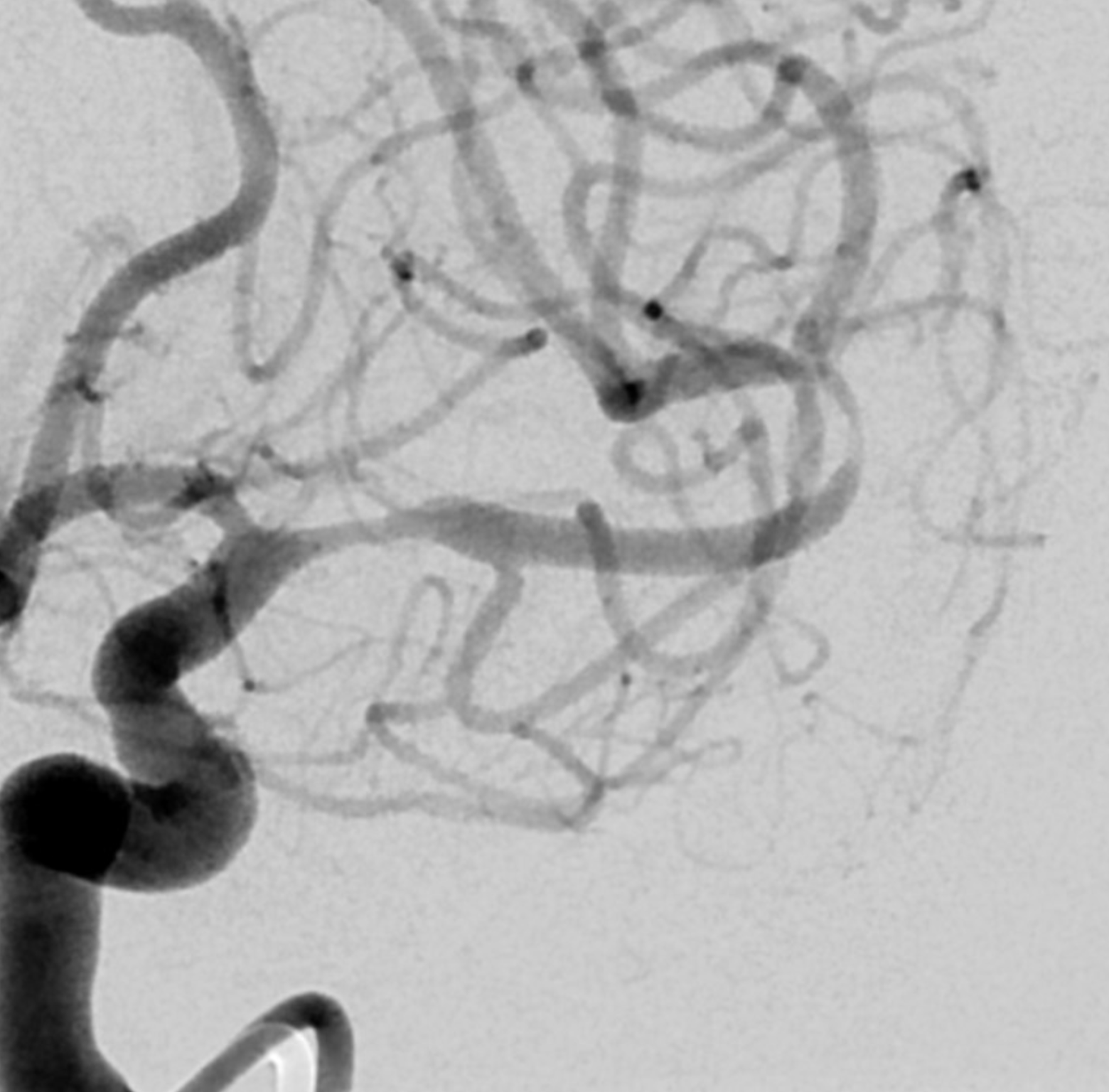
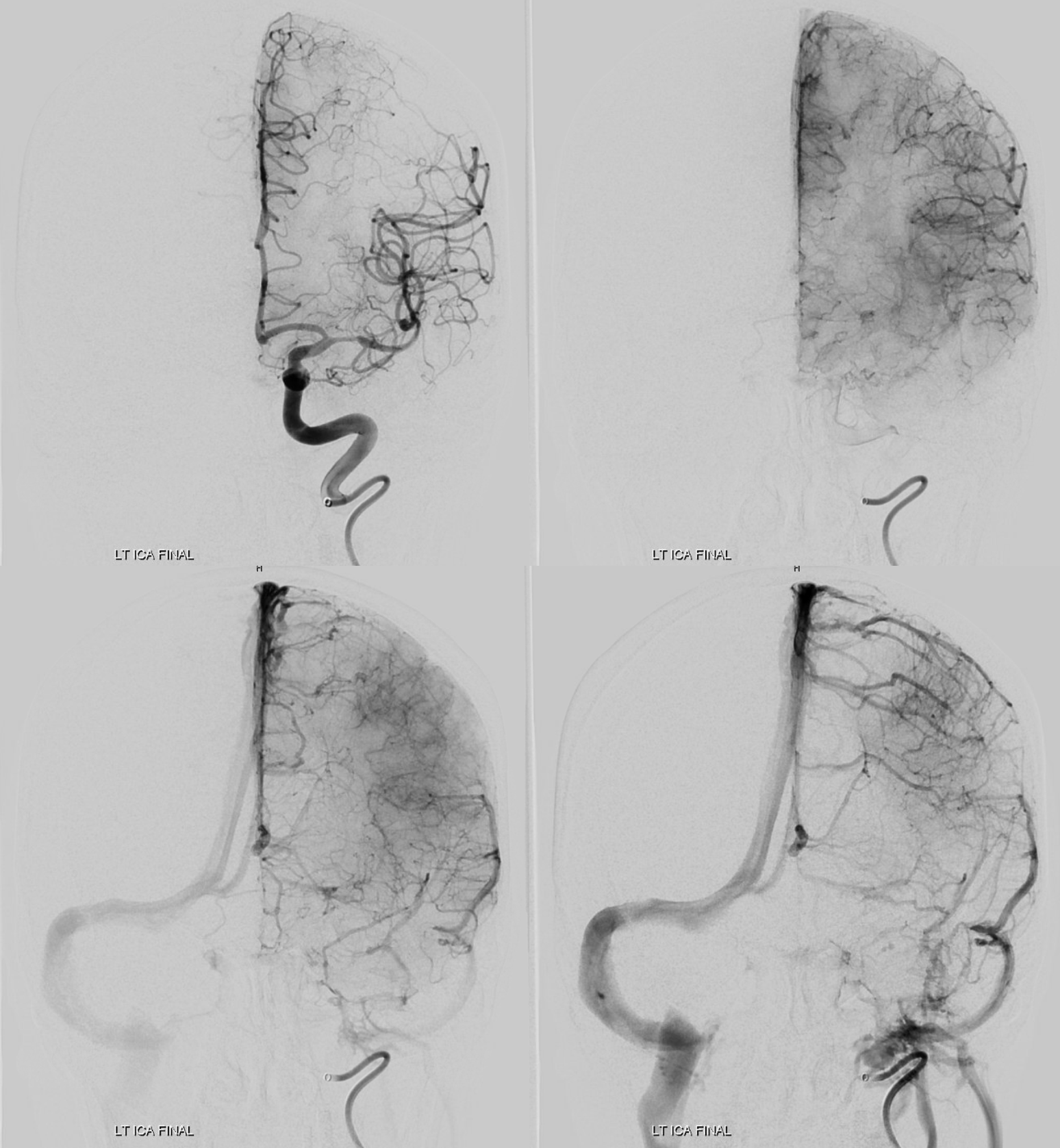
Angio
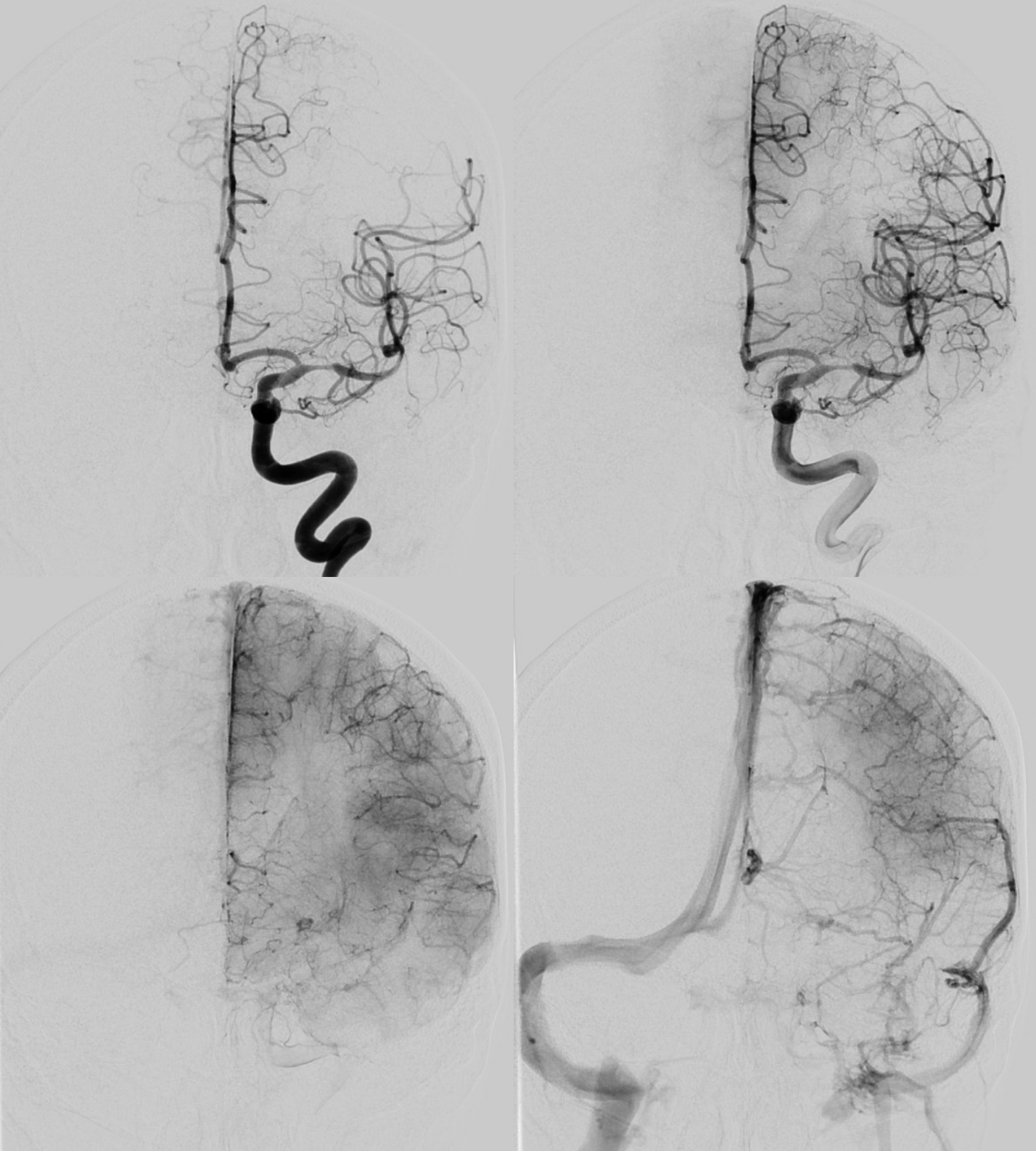
Do you see that there are two lesions? The more distal one was missed on CTA — example of “satisfaction of search” error
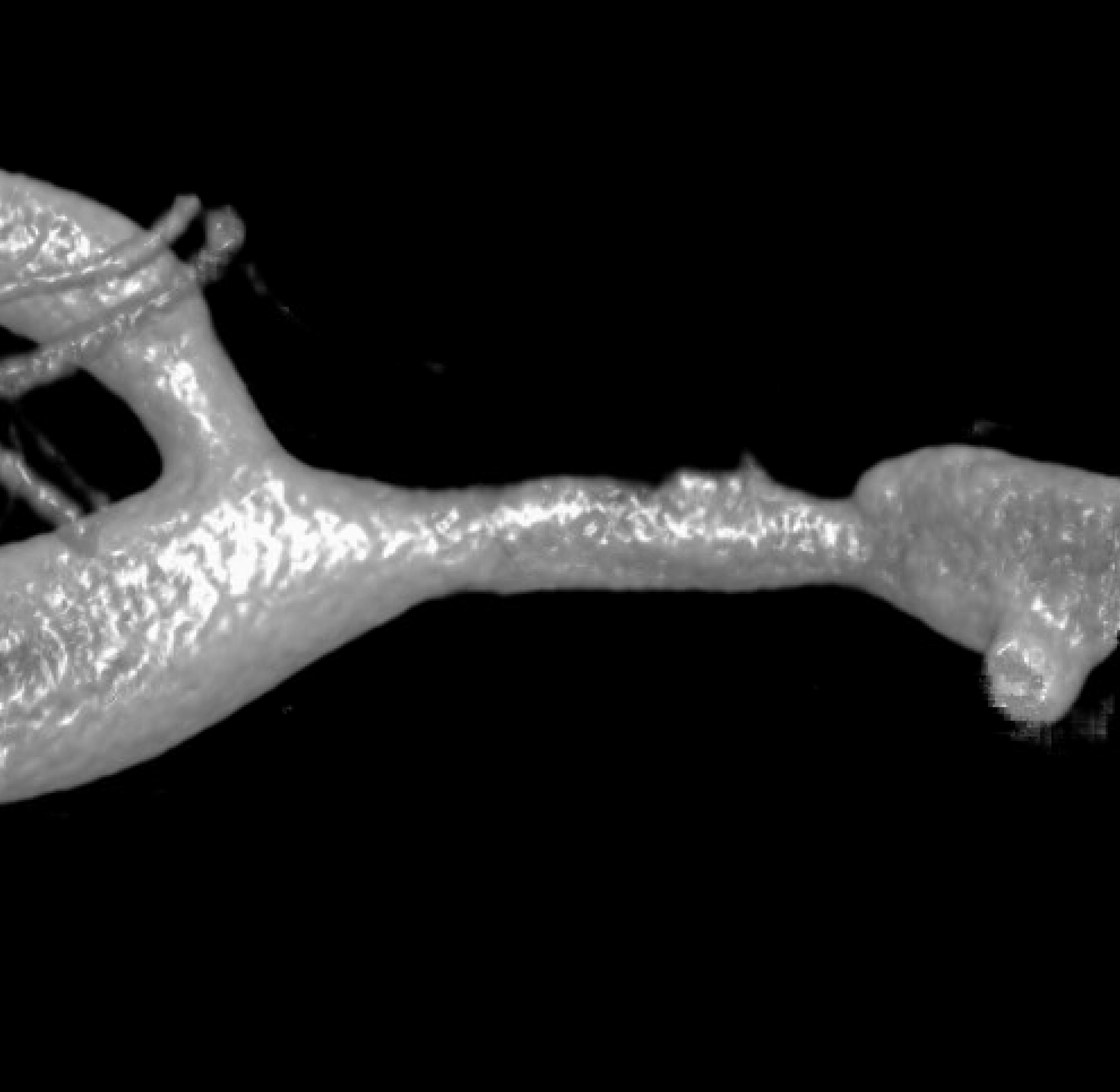
Magnified view — Proximal M1 still looks like athero. Distal M1 (its a long M1 segment, they don’t read the rules – see MCA page — is a smooth type of narrowing — its one possible clue, very nonspecific still
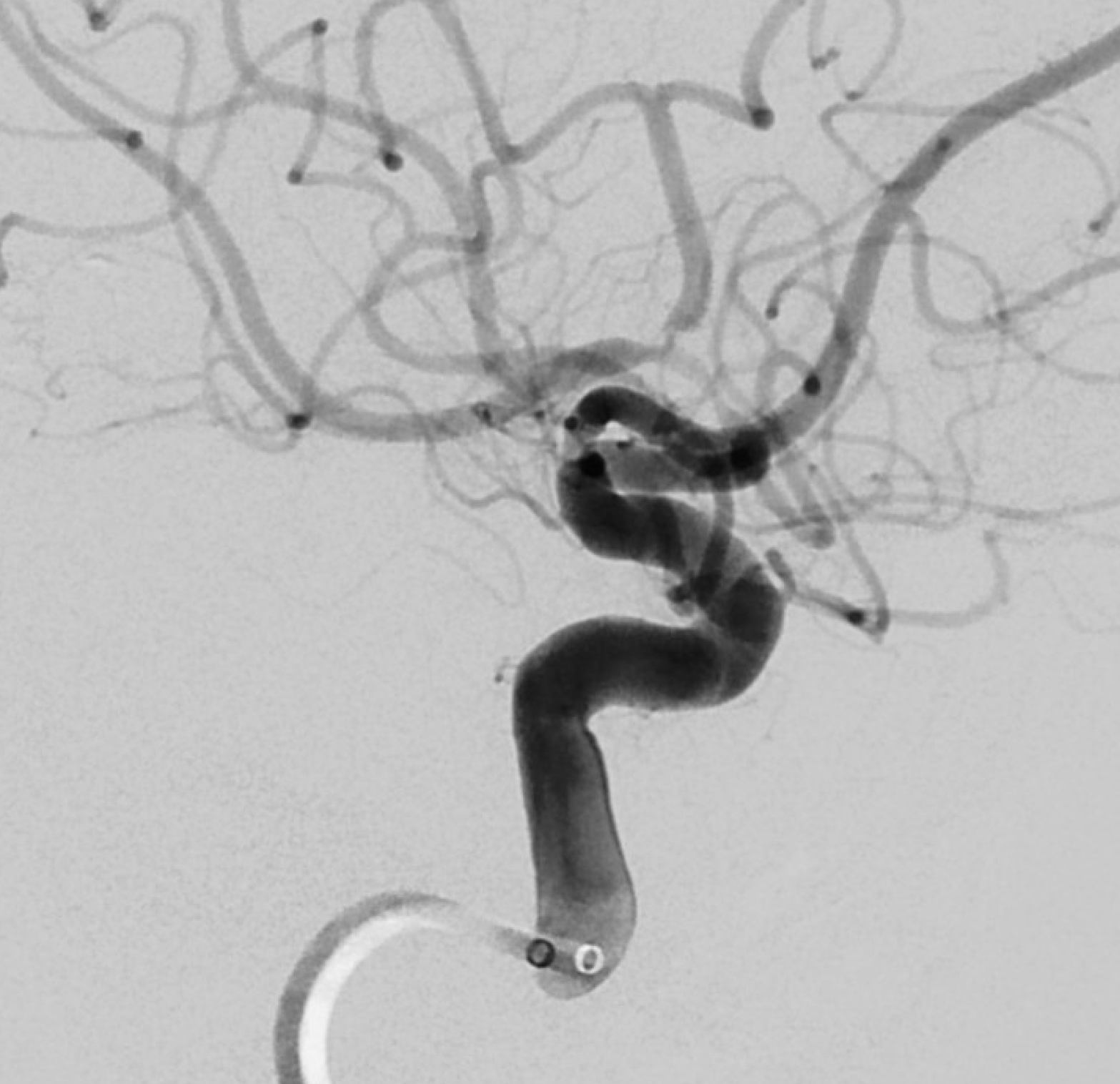
Lateral oblique — the distal M1 stenosis extends into the superior and inferior divisions. The superior division is the worst — and corresponds to the aphasia. Notice the somewhat peculiar morphology of the proximal aspect — still very nonspecific
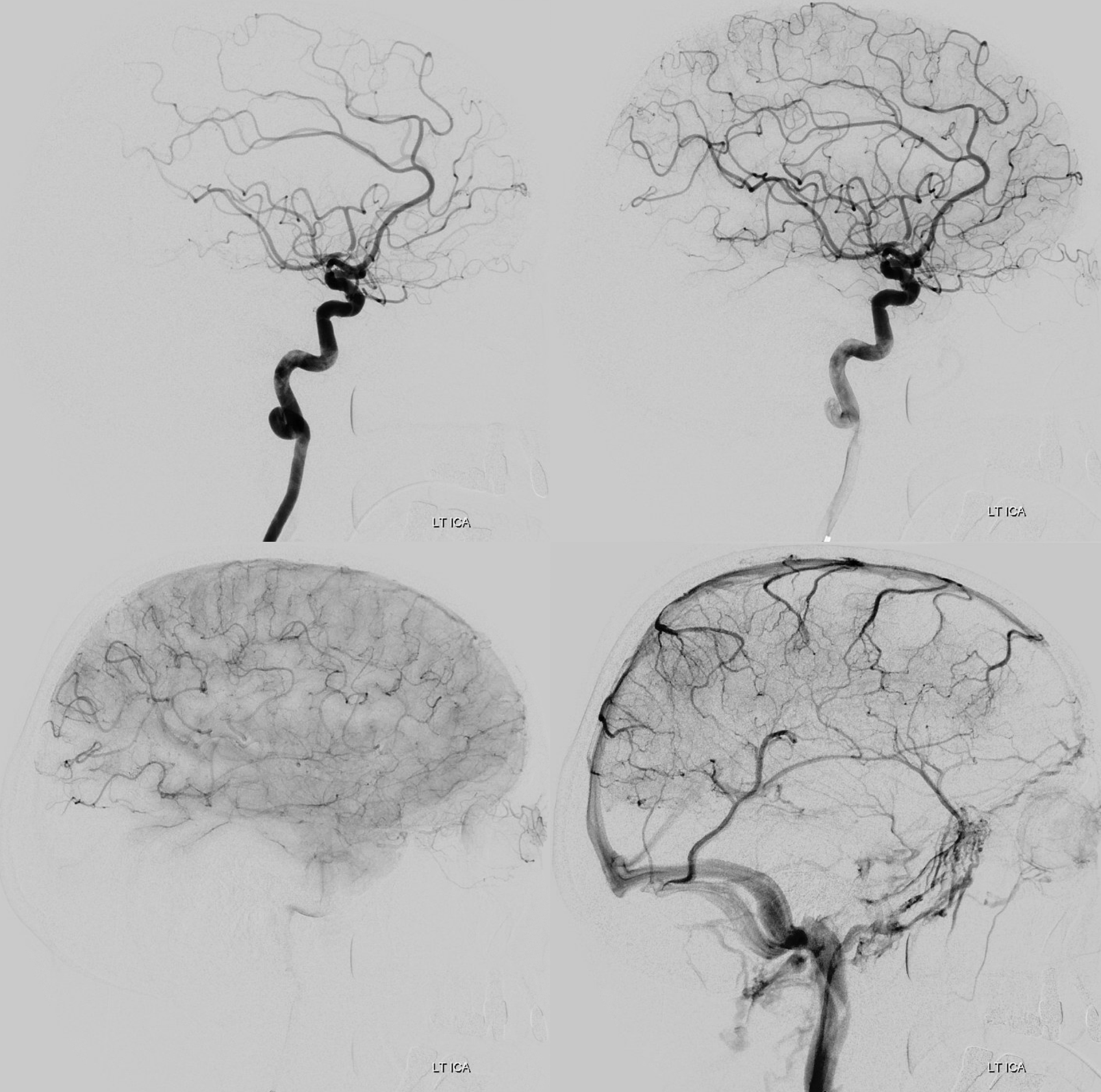
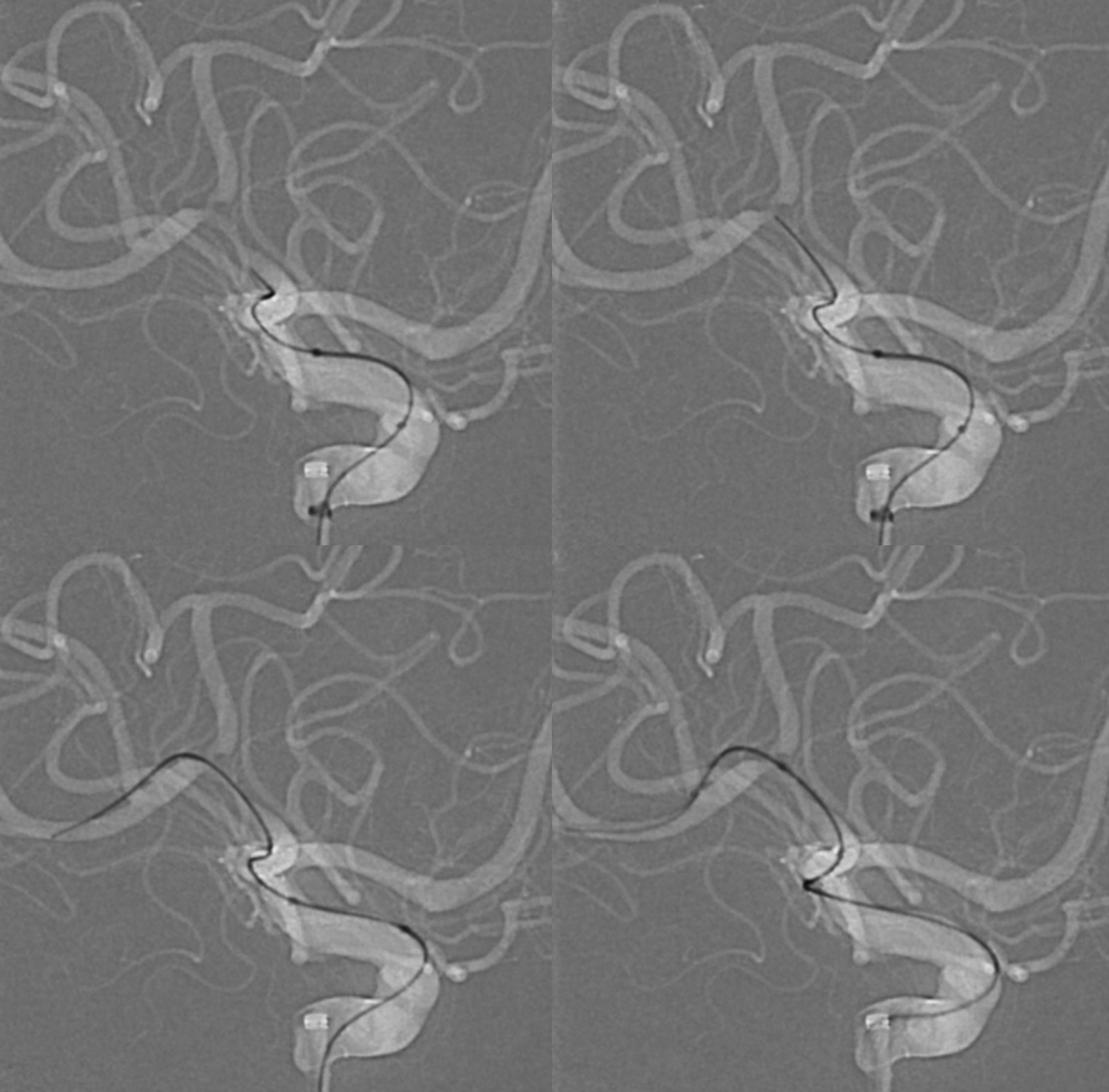
A very gentle catheterization with an Aristotle 014 soft. The microcatheter is a Wedge — we use it for very gentle angioplasty. Here the wedge part does not even cross the lesion
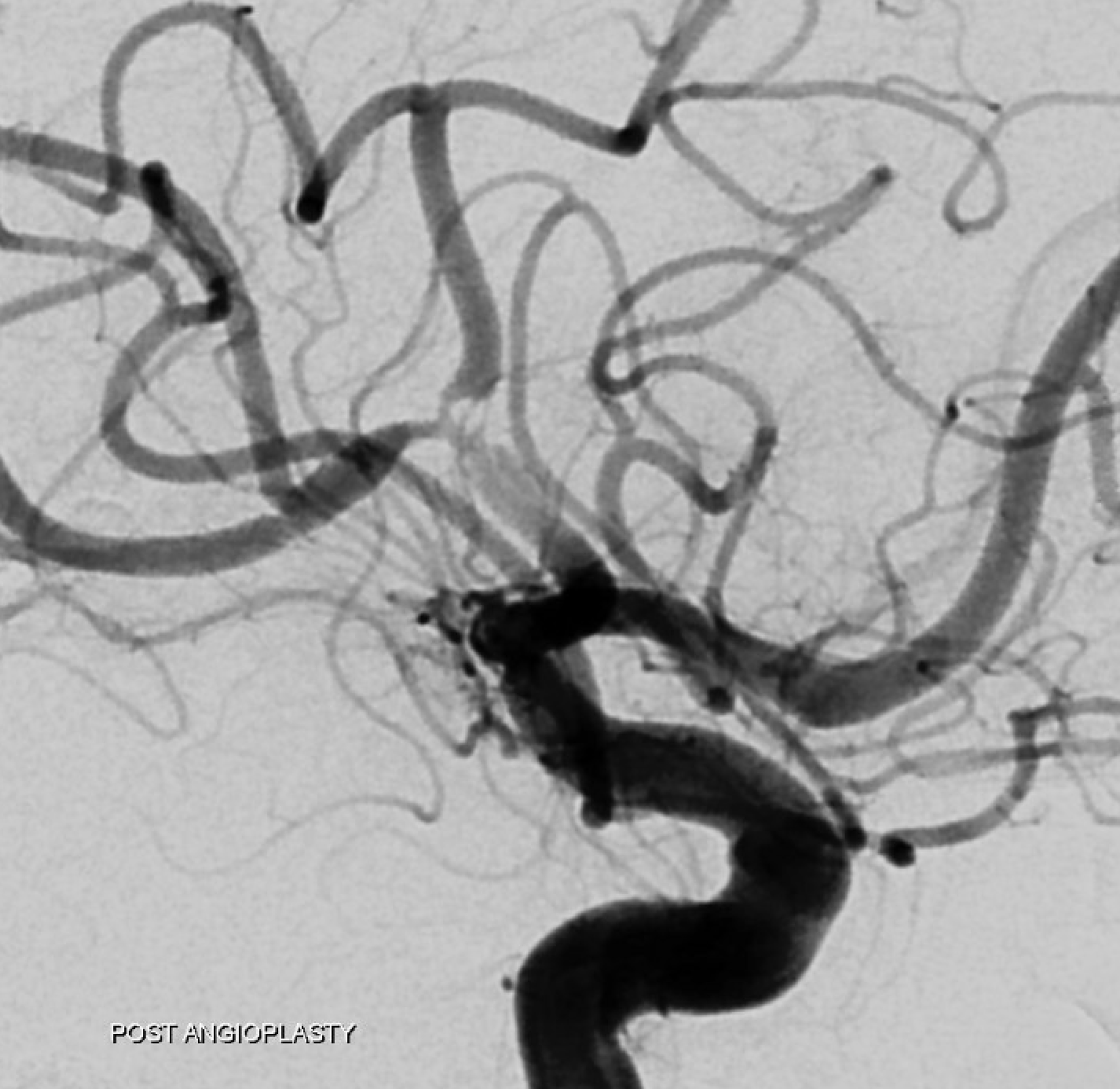
Post angioplasty — see it now? There is a clear dissection flap in distal M1. It is not new but unmasked by the catheterization. These are indeed very treacherous lesions.
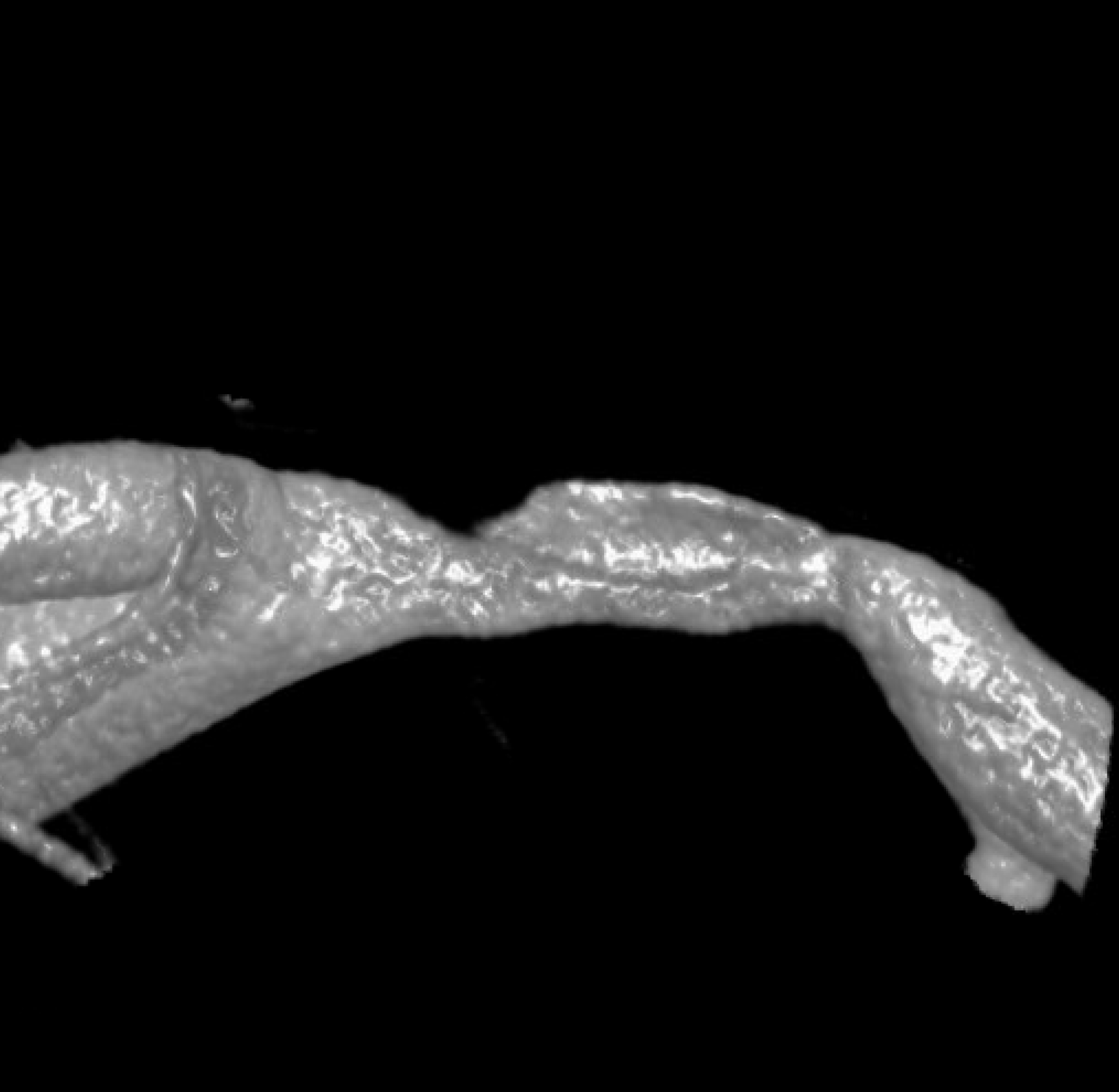
Now lets look at the proximal M1. Here is a global Cone Beam DYNA CT — adds nothing

A more detailed reconstruction — still no added value
Even more detailed reconstruction, frontal view — much better resolution but still nothing to add diagnostically
Now, look at the back of this reconstruction — that’s different! See the spiral groove? That’s the clue. This is not looking like athero anymore. The dissection was hiding on the back wall of the M1 segment.
Movie — convinced now?
MIP
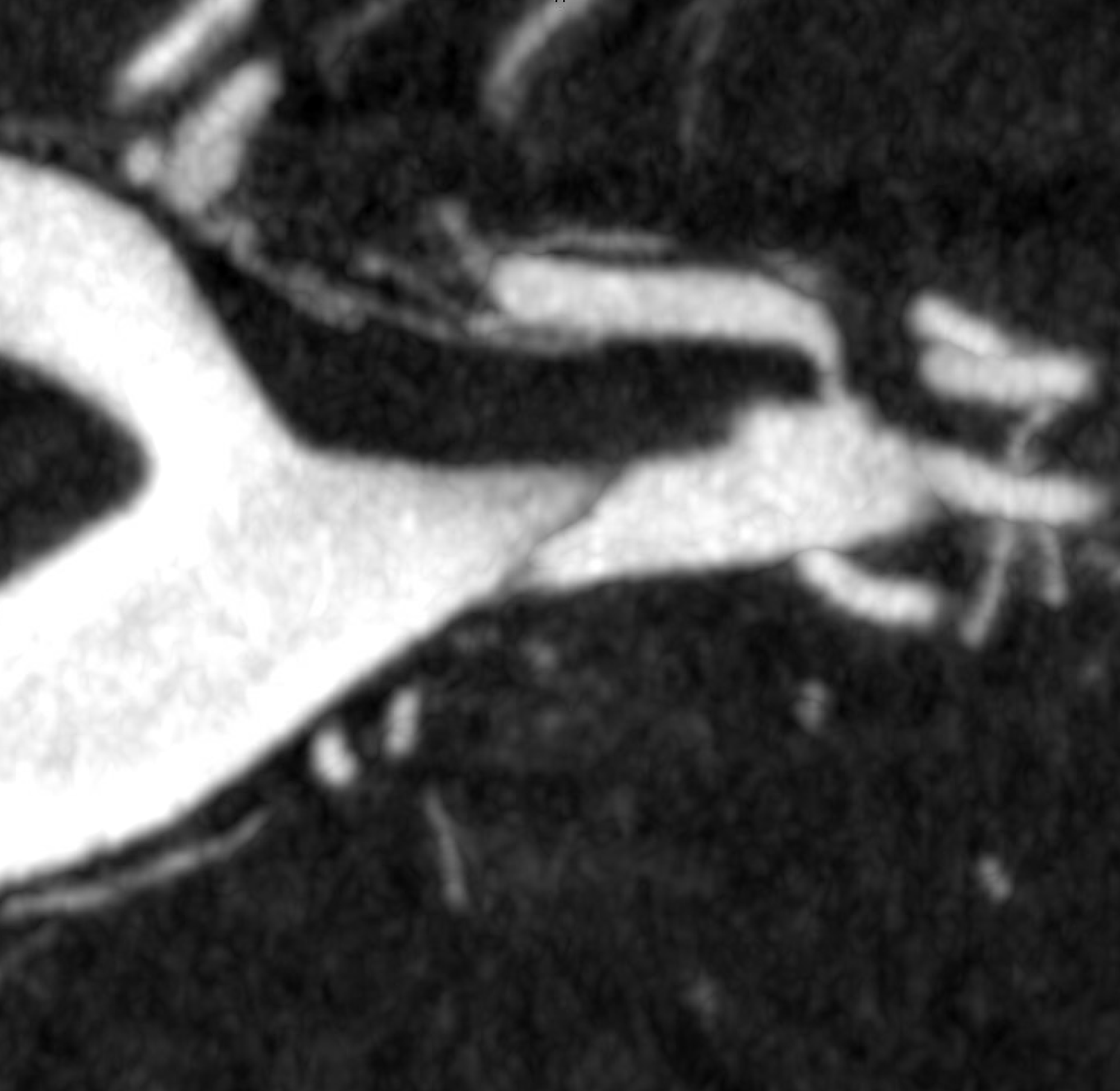
Coronal MIPs
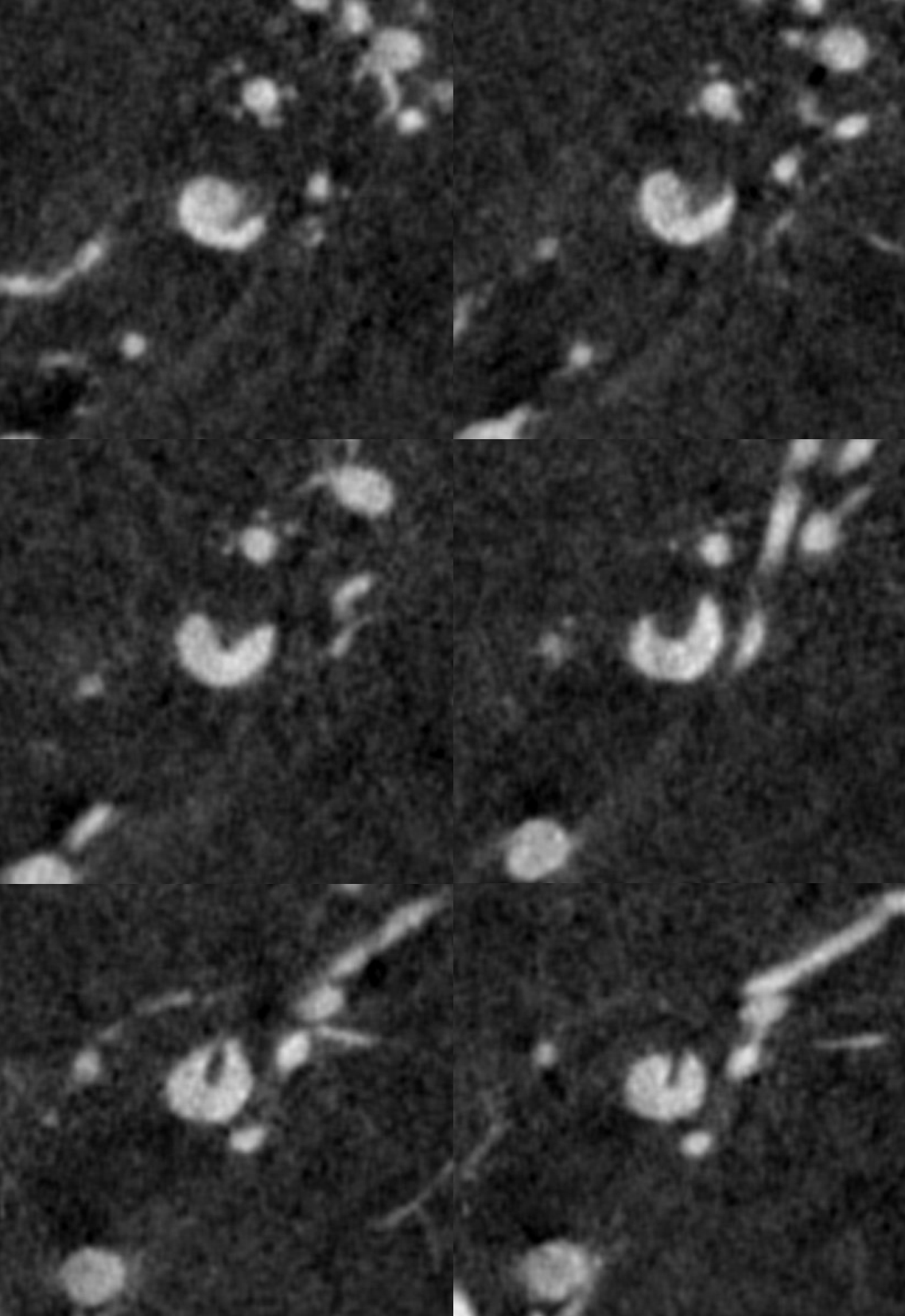
Movie coronal MIPS
Movie of distal M1 dissection before plasty
After plasty
Final post. These are extremely treacherous lesions. It is very easy to make them worse by extending the dissection. Contrary to what some believe, knowing which lumen one is in — true or false — is often very hard. Being in false lumen for distal dissections is very bad.
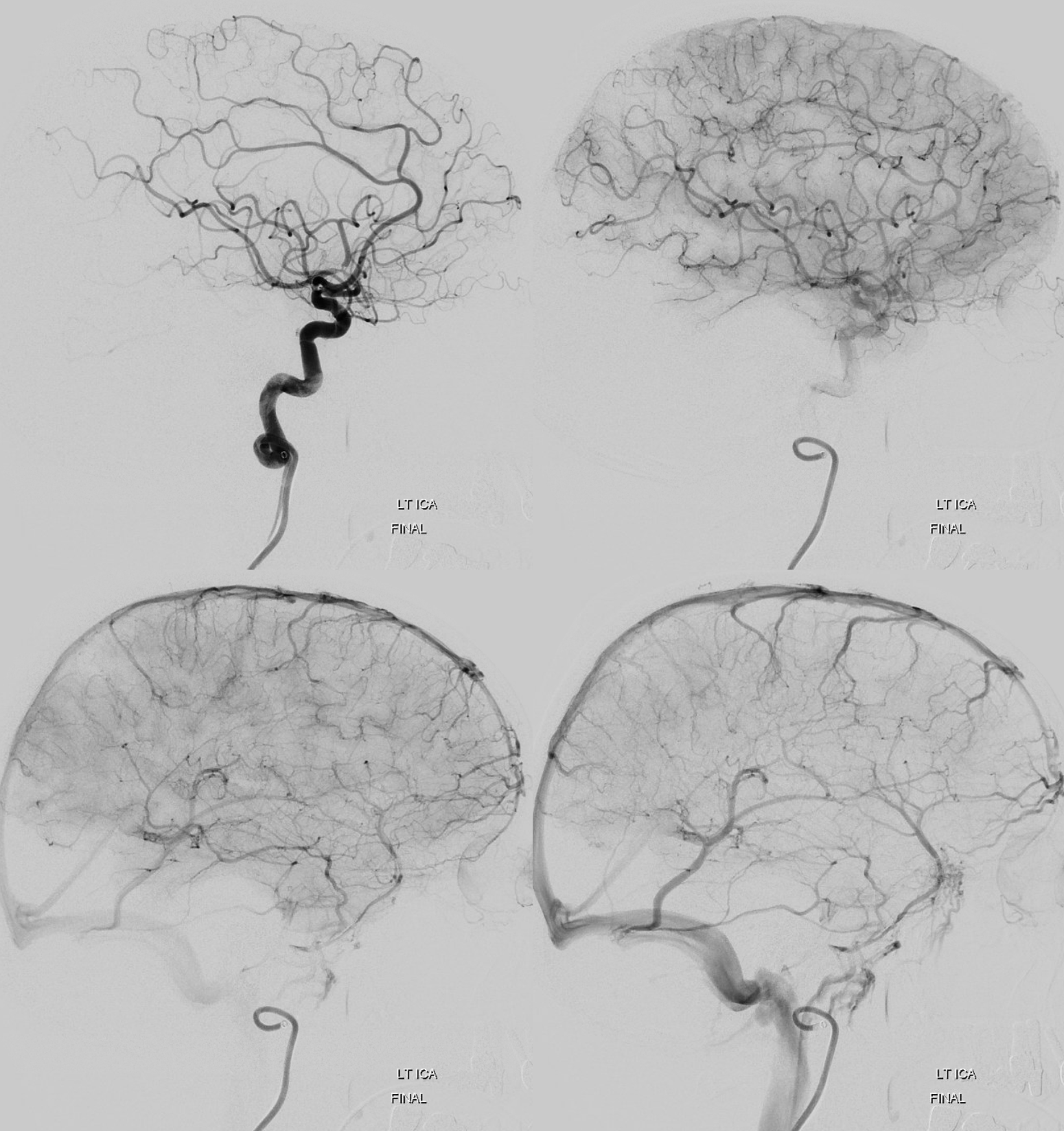
The moral is that we have significant challenges in diagnosing intracranial dissection. In many cases the final diagnosis remains uncertain. Many are not convinced, and these are under-recognized. Here the diagnosis is certain, aided by lack of risk factors for intracranial atherosclerosis. The best diagnostic strategy today is high end Cone Beam CT to uncover the fine detail morphology. This is a very important area for MR vessel wall imaging, however vessel size remains an issue for all techniques.
