Long Night’s Journey Into Day
Case courtesy of Drs. Peter Kim Nelson and Jafar Jafar
The uniquely central location of the falcotentorial junction fistula leads to equally unique vascular arrangements and adaptations. As with the vast majority of dural fistulas, the key concept is a single hole nature of the fistula. Nearly all dural fistulas consist of a single hole or, maybe, a small multi-hole region of AV communication — no matter how “busy” the area may appear. Recognition of this concept allows one to selectively target a small key area where the disease sits, in preference to extensive embolizations which use up large amounts of embolic agents, exposing the patient to more radiation dose and, not infrequently, the hazard of multi-stage procedures.
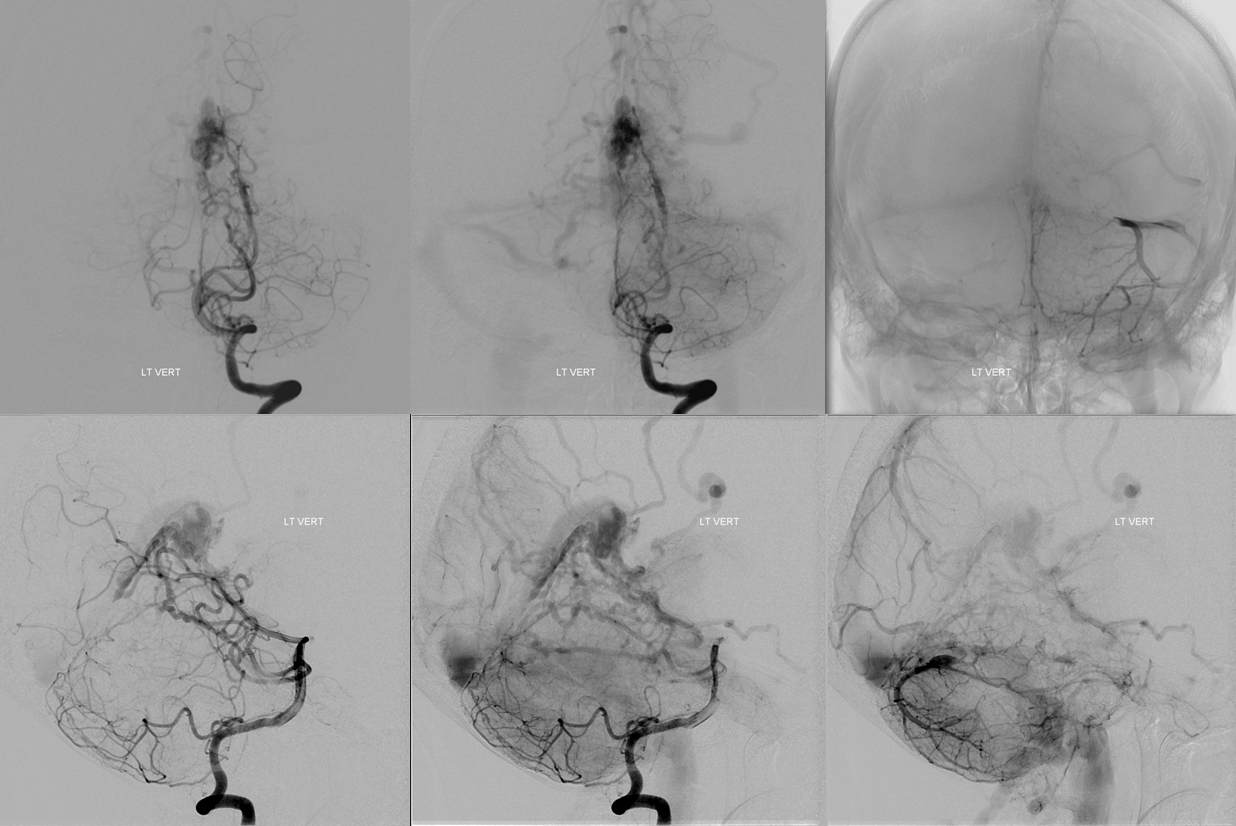
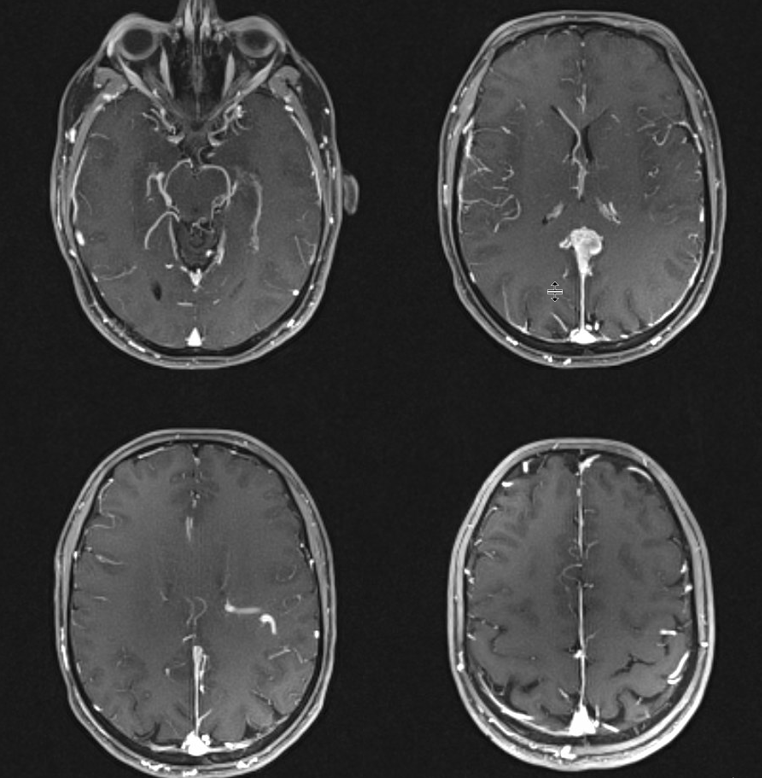
This patient presents with headaches. Notice pulsation-related artifact at the level of the falcotentorial junction (blue arrows) and a markedly enlarged venous structure in the left centrum semi-ovale.
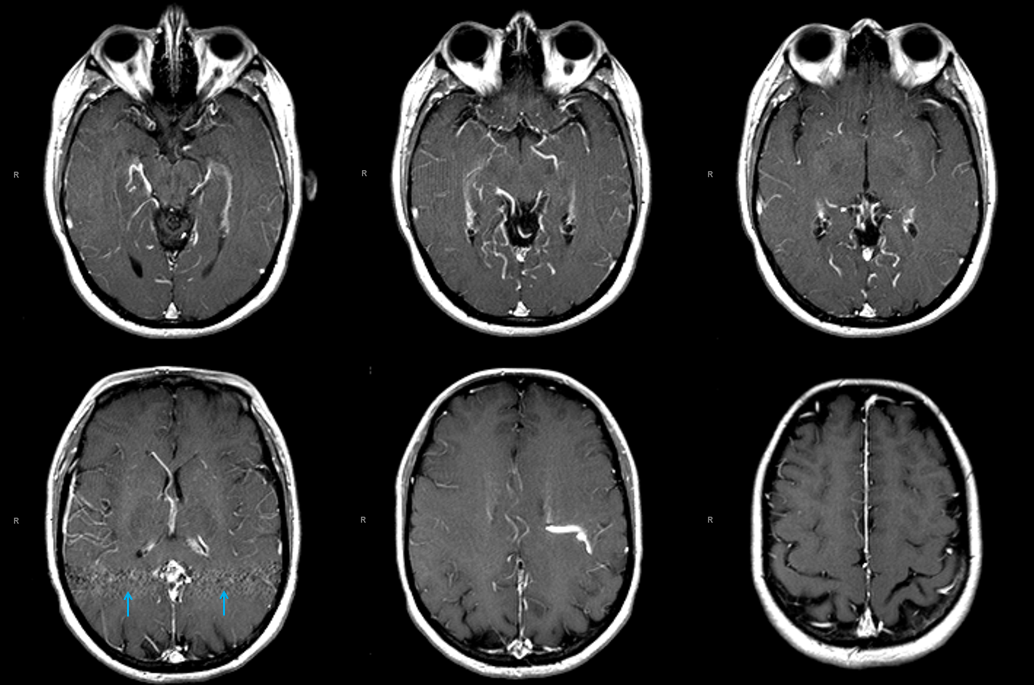
Sagittal MPR reconstructions demonstrating the deep transmedullary vein (white) and a collection of abnormal vessels in the region of the Galen
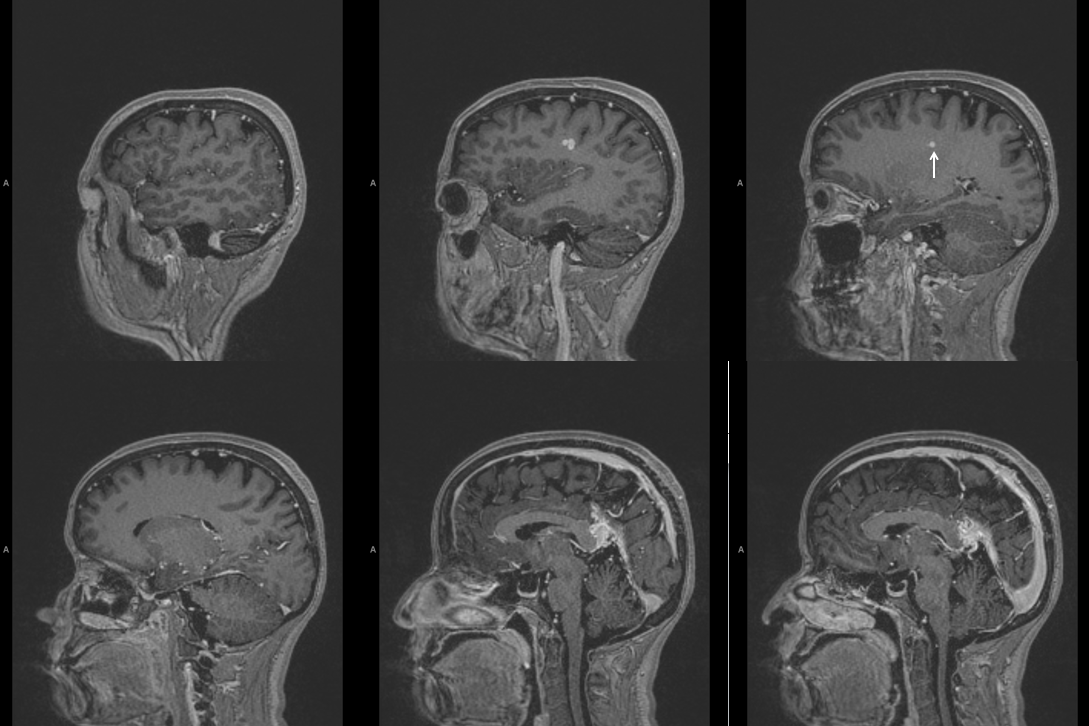
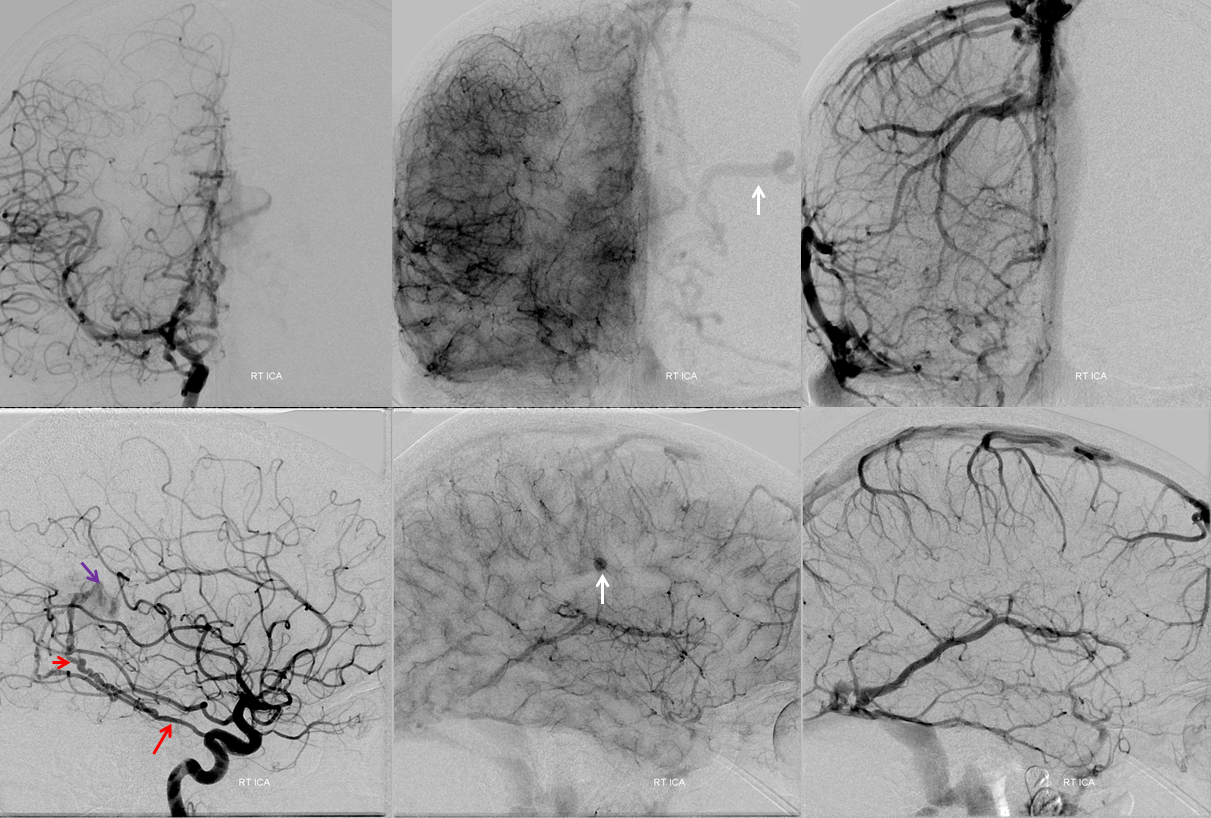
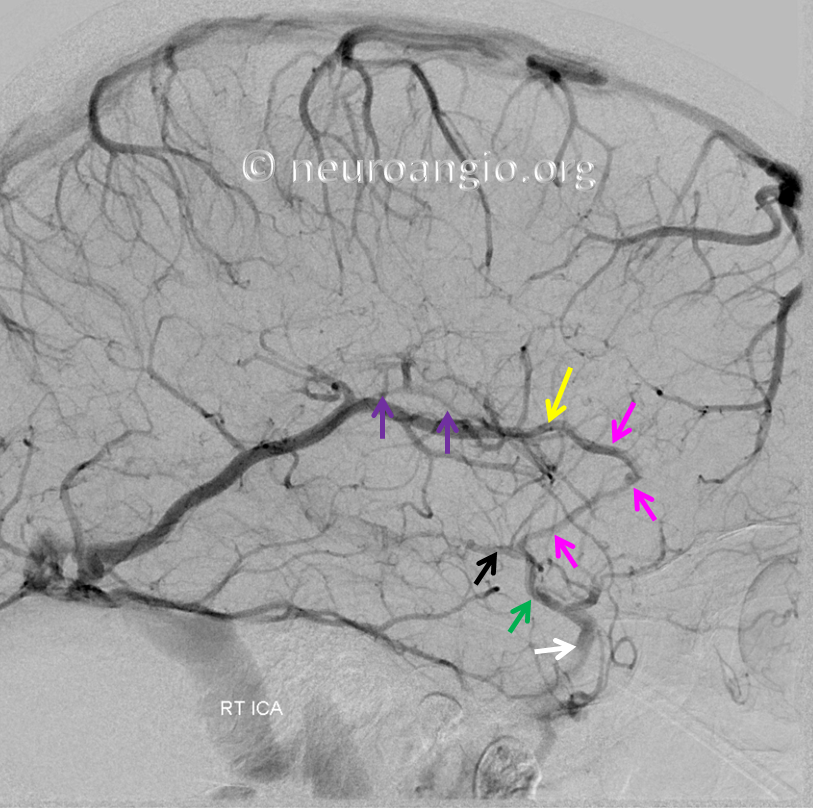
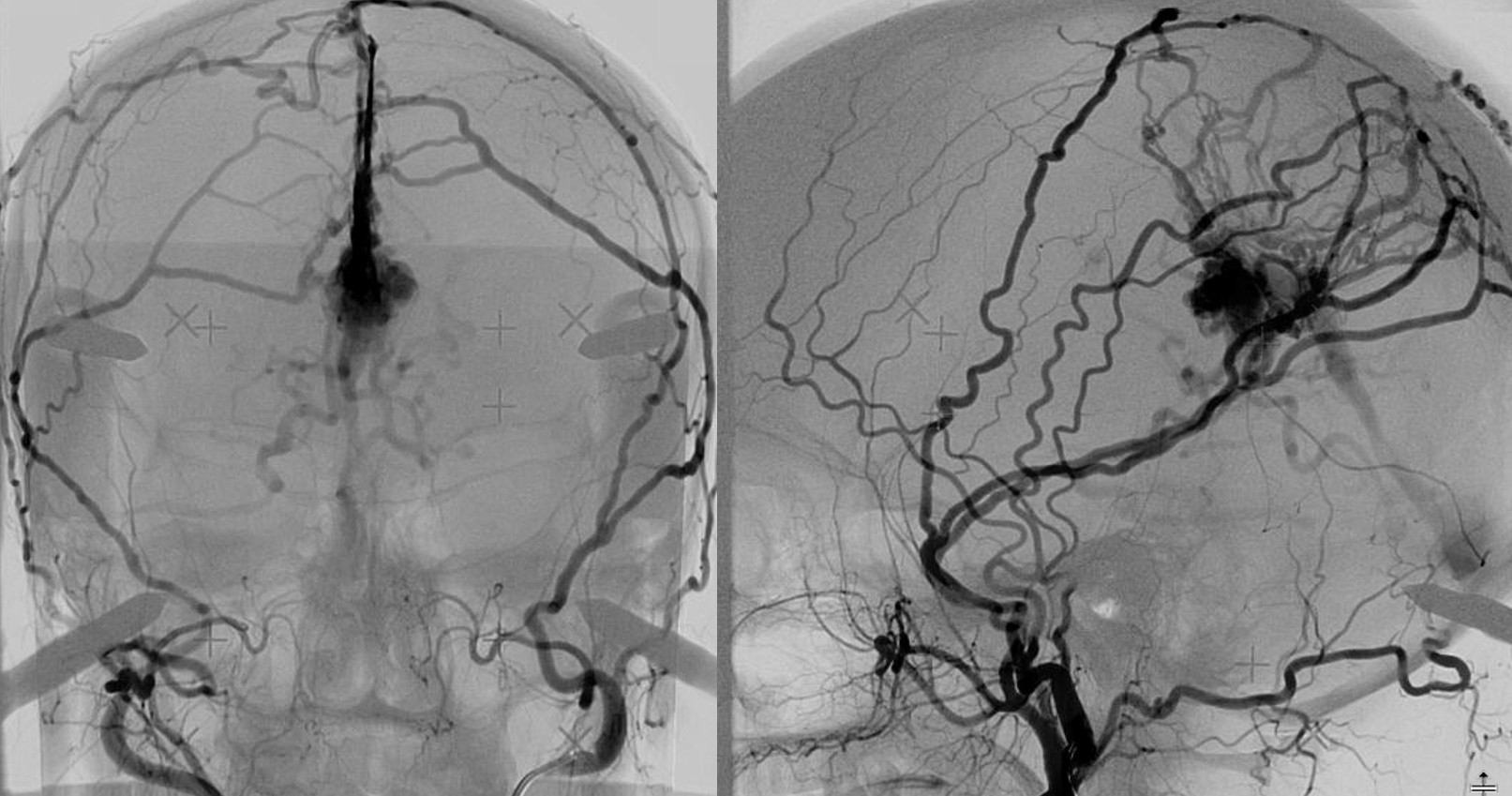
Right ICA injection — the key finding here is not the MHT-derived supply to the fistula (purple) by the artery of the free margin of the tentorium (a.k.a. Bernasconi-Cassinari, red arrows), or the really neat visualization of the left transmedullary vein (white) — the key finding is seen in the venous phase — nonvisualization of the posterior segment of the basal vein, vein of Galen, and straight sinus — thus suggesting that these structures are used exclusively by the fistula (see deep venous system and medullary venous malformation / DVA pages for additional info)
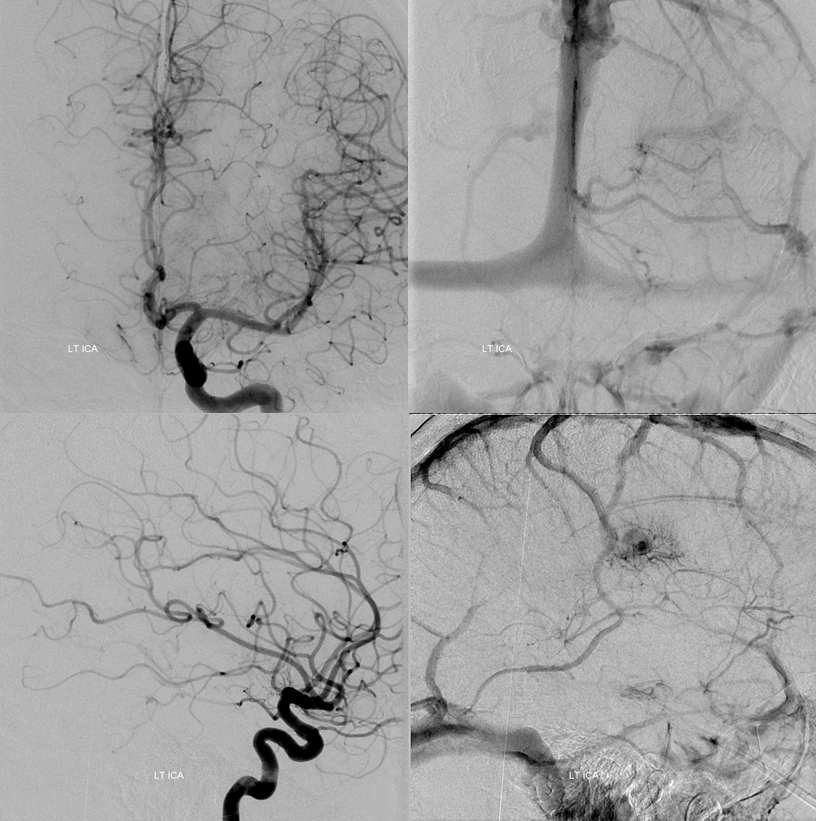
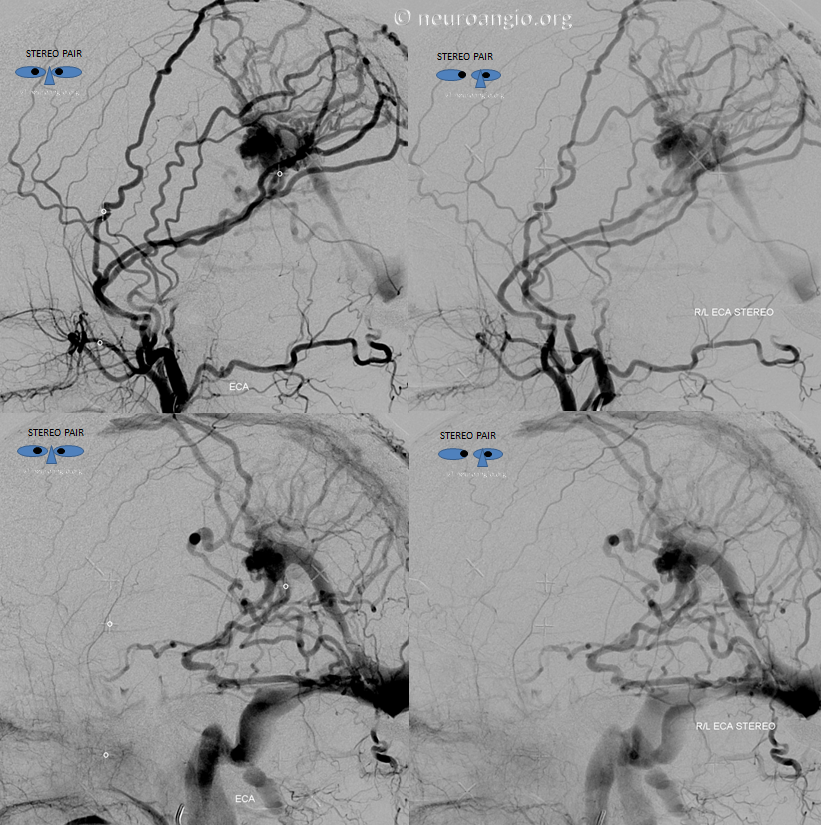
Stereo views of arterial and venous phases. The venous phase shows that the basal vein empties via deep sylvian veins into the cavernous sinus — see Deep Venous System and Cavernous Sinus pages for more info. Essentially, the basal vein often does that anyway.
The remarkable thing here is how the internal cerebral vein is draining — it is difficult to appreciate this without stereoscopic projections, because of the superimposition of the Labbe and Internal Cerebral Veins. Stereo projections, however, show that the internal cerebral vein empties, via the septal vein, into a medial lenticulostriate vein, and then joining the deep sylvian (middle cerebral) veins into the cavernous sinus. Pretty amazing. If you can’t believe it, i suggest learning stereo, if you can, so you might be able to see it better.
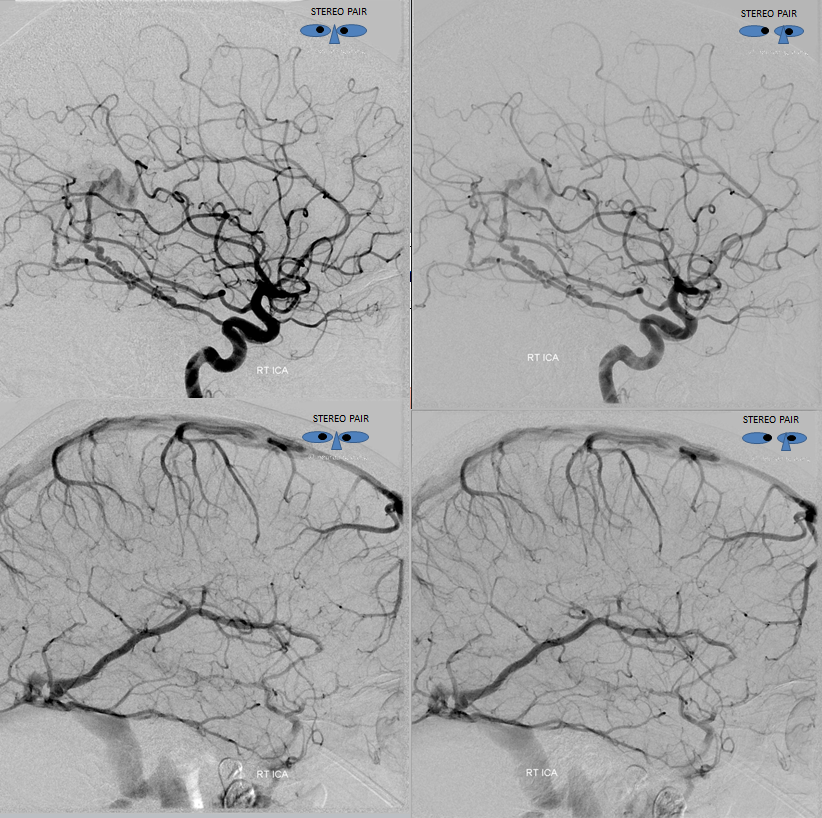
Anaglyph stereo images. Arterial phase is looking from medial to lateral (very useful sometimes for arterial phase). Venous phase is lateral to medial (because it works better for veins generally)
Here is a non-stereo lateral view, showing the above. The thalamostriate vein is purple, the septal vein is yellow, medial lenticulostriate vein is pink, basal vein is black, middle cerebral vein is green, and cavernous sinus is white. Without stereo projections, it is really hard to tell this apart from what looks like superficial sylvian veins connected to the Labbe — however this is a fakeout — trust me on this one. What has happened is that the internal cerebral vein has found an alternative outlet, and is no longer using the Vein of Galen — a remarkable feat of adaptation.
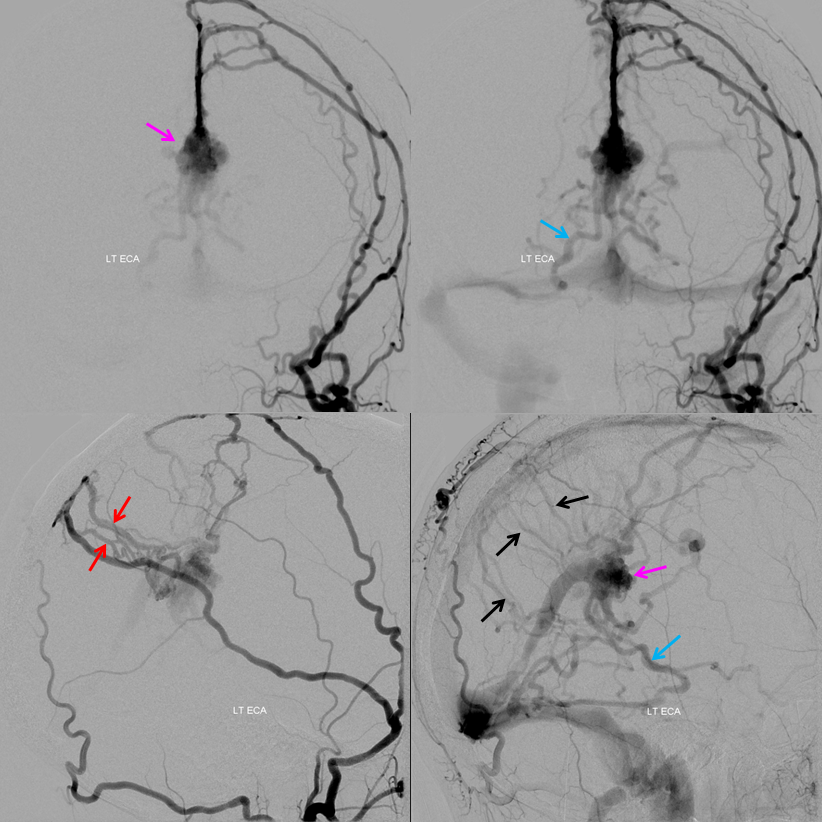
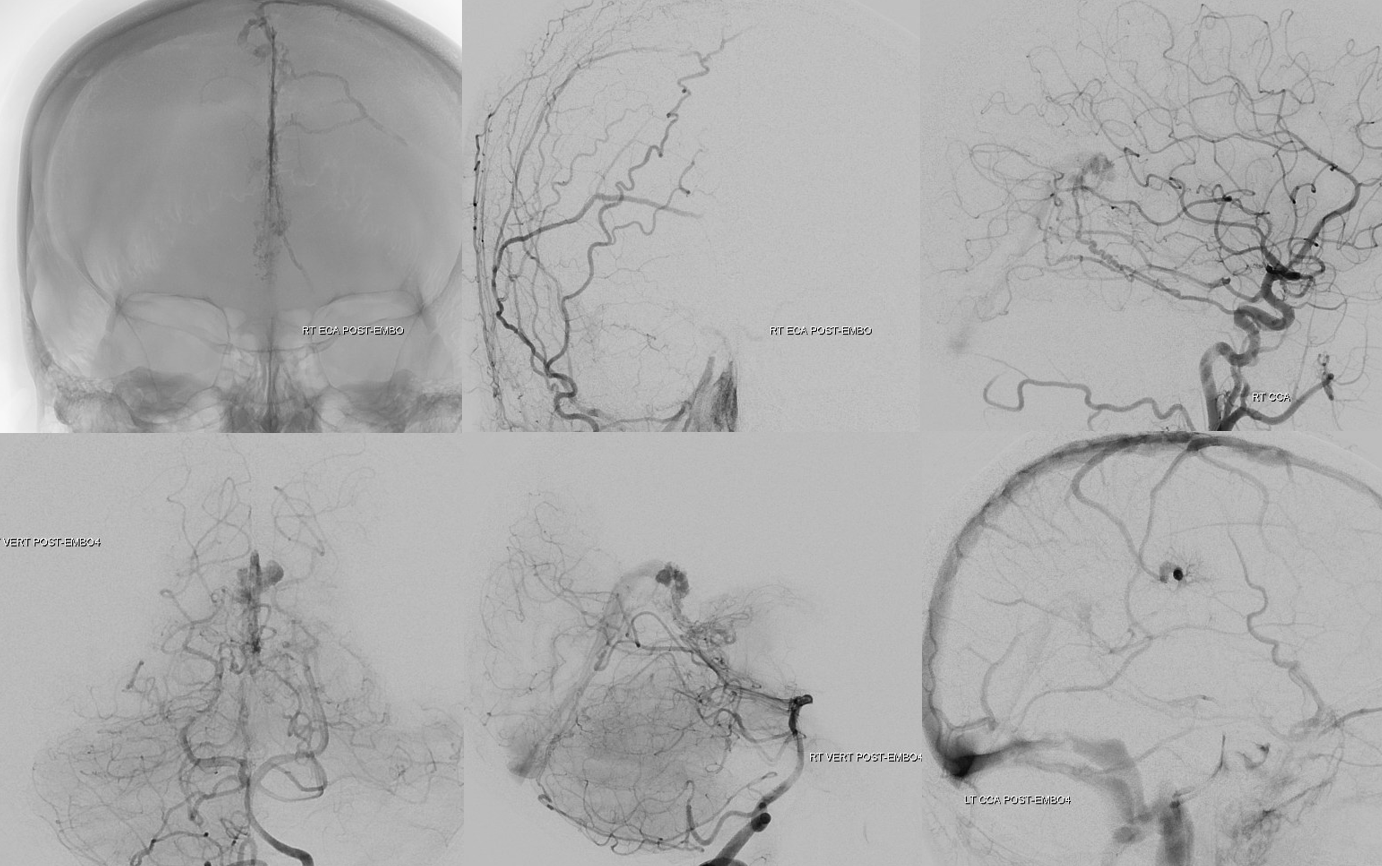
Injection of the right ECA — multiple middle meningeal (orange) feeders into the fistula (purple arrow marks the venous pouch at the site of fistula), via a network of unnamed arteries within the falx cerebri (red arrows). Venous drainage of the fistula proceeds into the straight sinus and via the posterior portion of the basal vein into the right superior petrosal sinus (not labeled). Also notice drainage via the transmedullary vein (white).
It is critical to understand that there is only one fistula — in the region of the Galen, marked by pink arrow. The vessels in the falx (red arrows) are arteries which supply it, not veins.
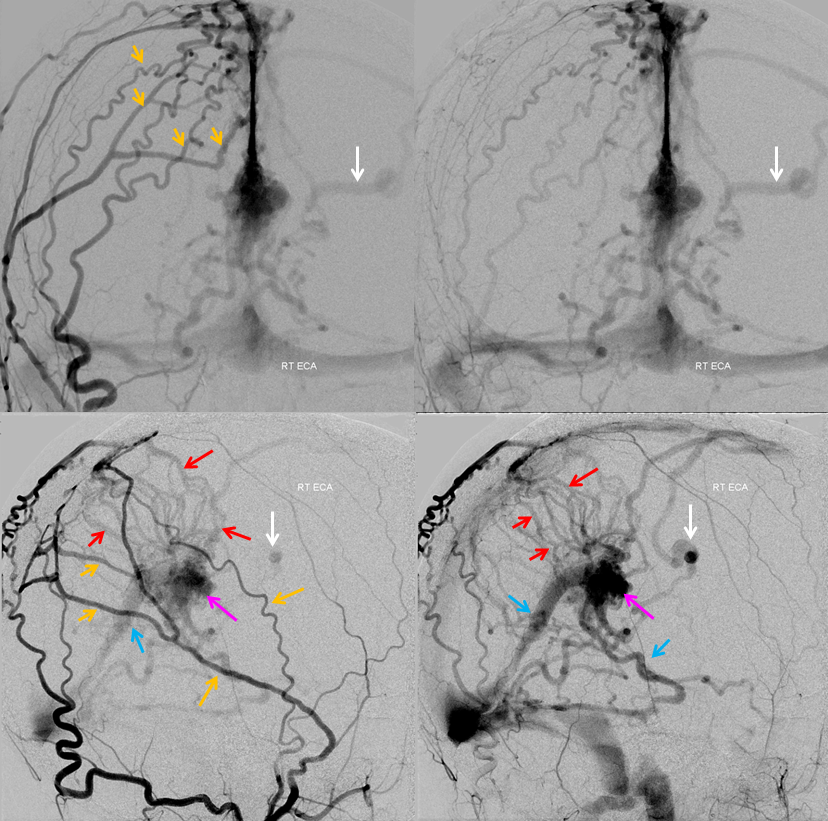
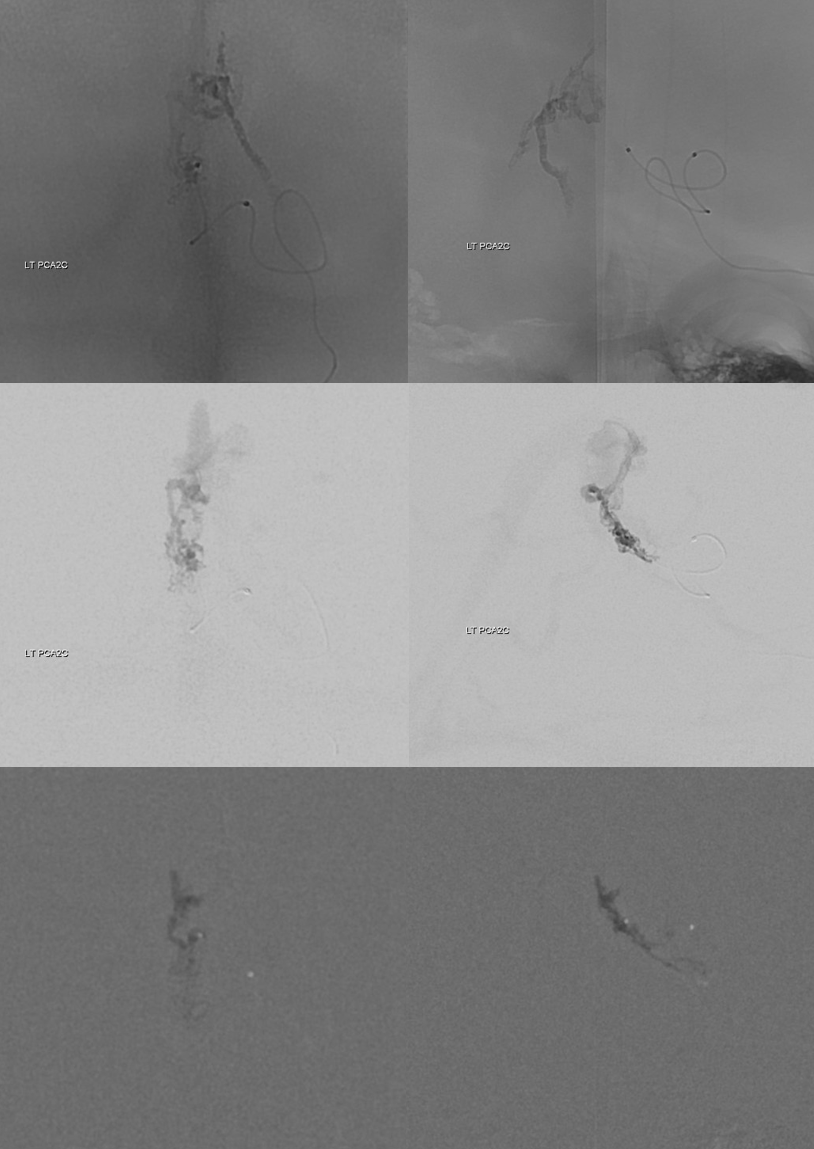
Injection of the right vertebral artery (straight PA view) shows supply via the posterior meningeal artery (red) into the artery of the straight sinus (yellow) — fistula venous pouch is pink again.
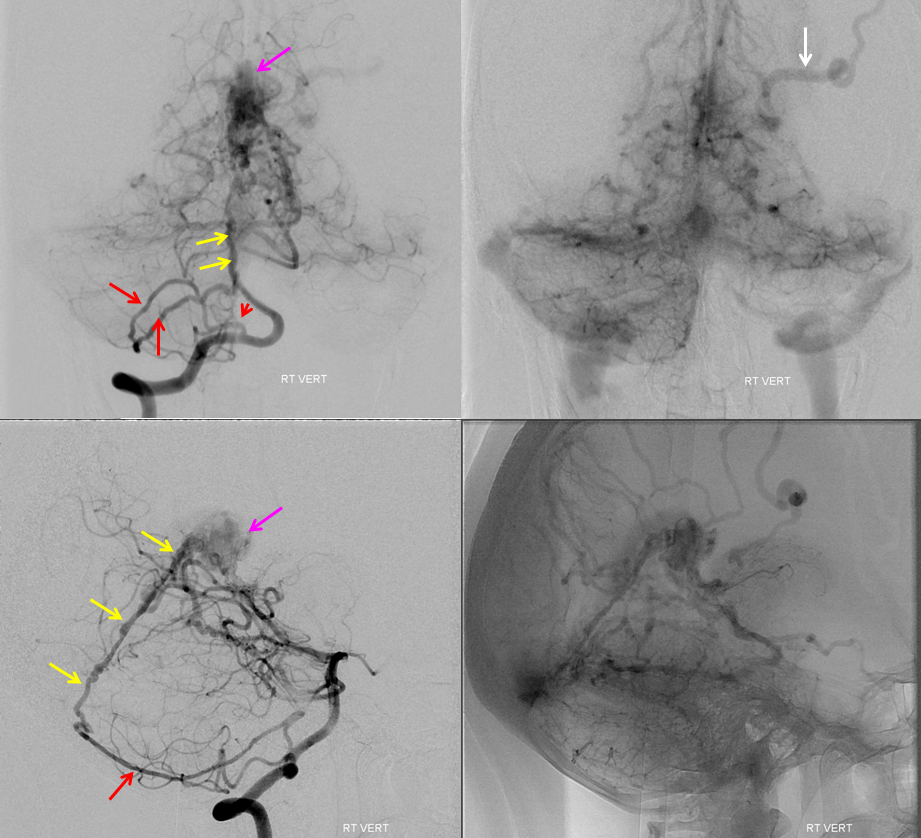
Another right vert injection in a steep Townes projection– to separate the artery of straight sinus from the basilar in frontal view
Left vertebral injection — contributions of the collicular and posterior medial choroidal arteries — better seen than in the above rigtht vert injections
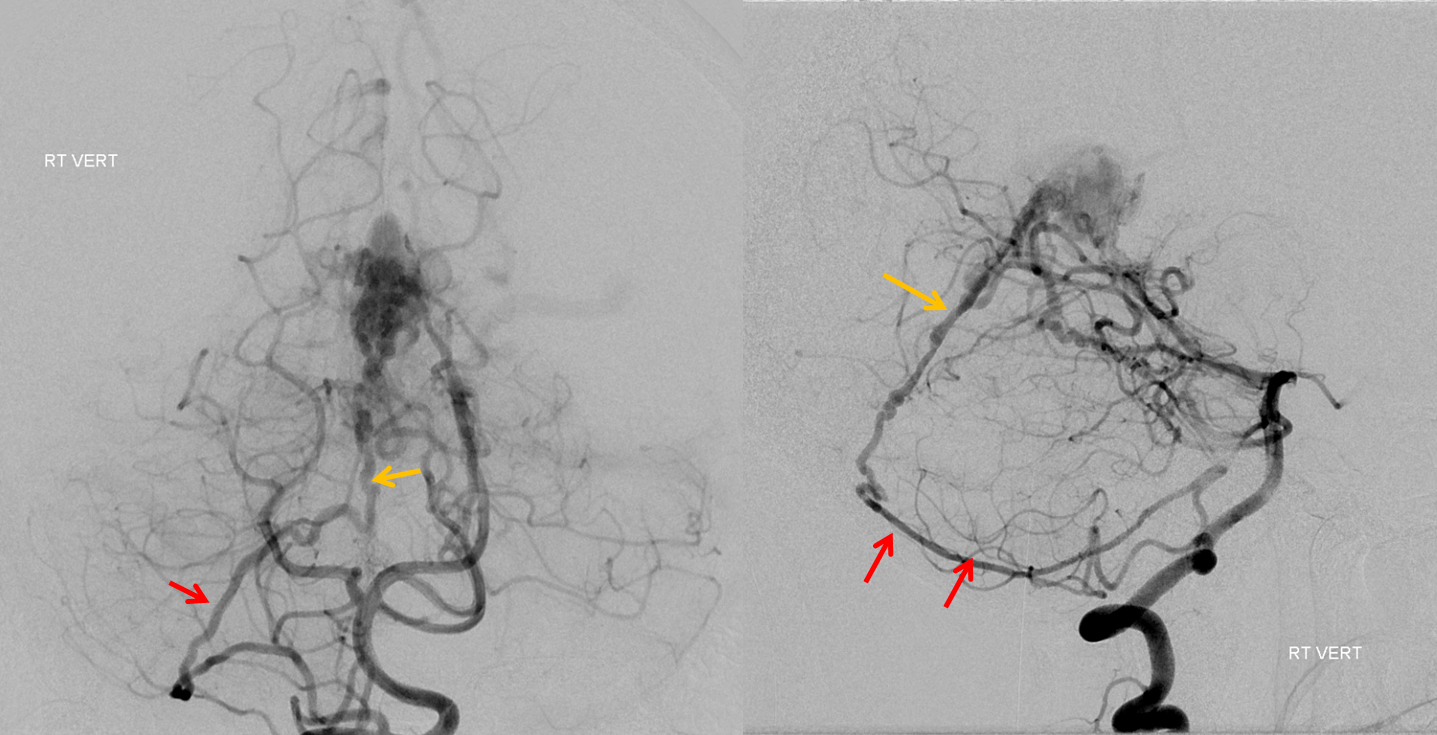
Left external carotid injection — beautiful images. Middle meningeal artery supplies the fistula (pink) via multiple unnamed arterial pedicles within the falx cerebri (red arrows). The same pedicles were seen from the right ECA injections, and show evidence of unopacified inflow by their less concentrated appearance compared with the MMA branches. Venous outflow is conducted into straight sinus, multiple posterior fossa veins, including the posterior portion of the basal vein (blue), and, most importantly, into venous channels within the falx cerebri (black). Notice that these channels are not the same as the arteries which supply the fistula (red). Both veins and arteries are seen running along the falx cerebri. The venous structures likely have the same origin as the falcine sinus — and probably should be called falcine sinuses also.
The super-important left ICA injection. Again, the posterior portion of the basal vein, vein of Galen, and straight sinus are not seen in the venous phase. What is seen are medial lenticulostriate vein and transmedullary vein draining the internal cerebral vein. This is a critical observation, because it shows that the transmedullary vein is used by both fistula and normal brain. Spillage of embolic material into this vein could be catastrophic, leading to left internal cerebral vein territory venous infarction. However, since the Galen and straight sinus are not seen in the brain venous phase on any injection, these normally indispensable structures can in fact be sacrificed — coiling off the venous pouch would take down the fistula without endangering the brain.
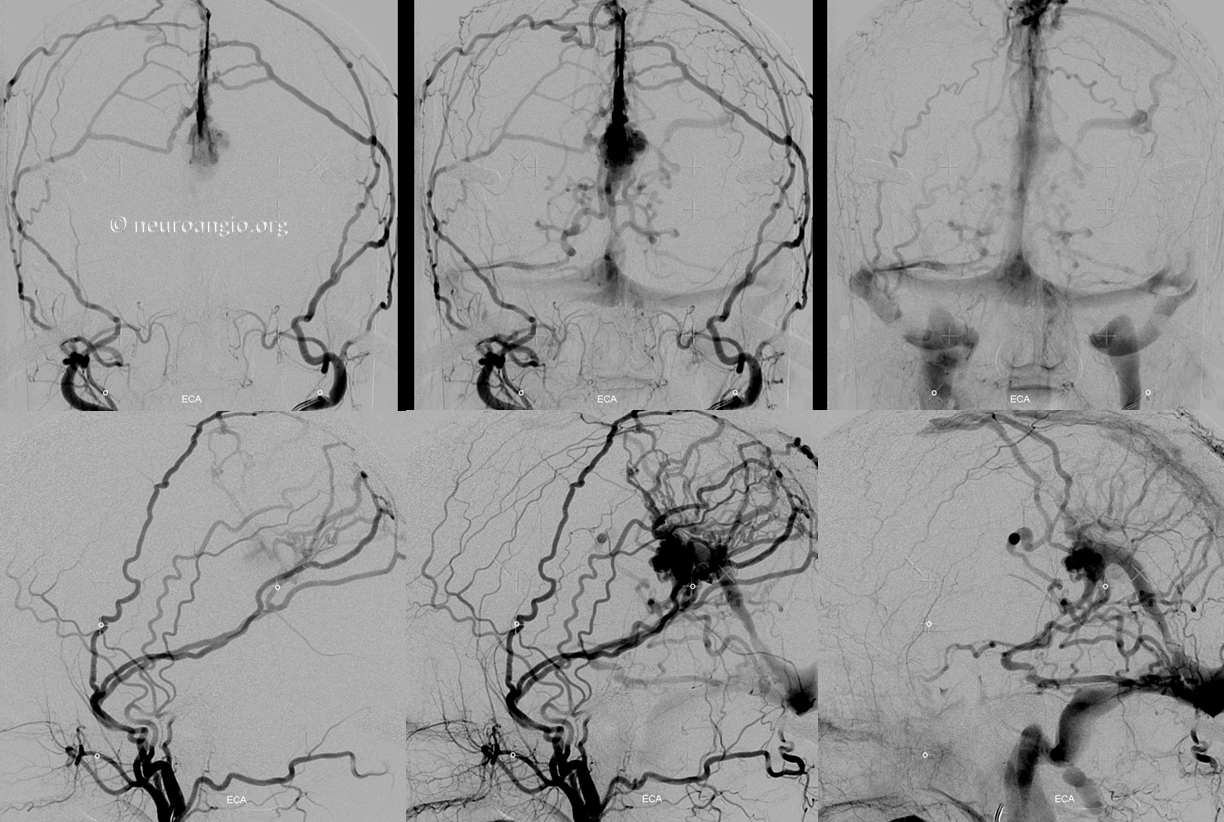
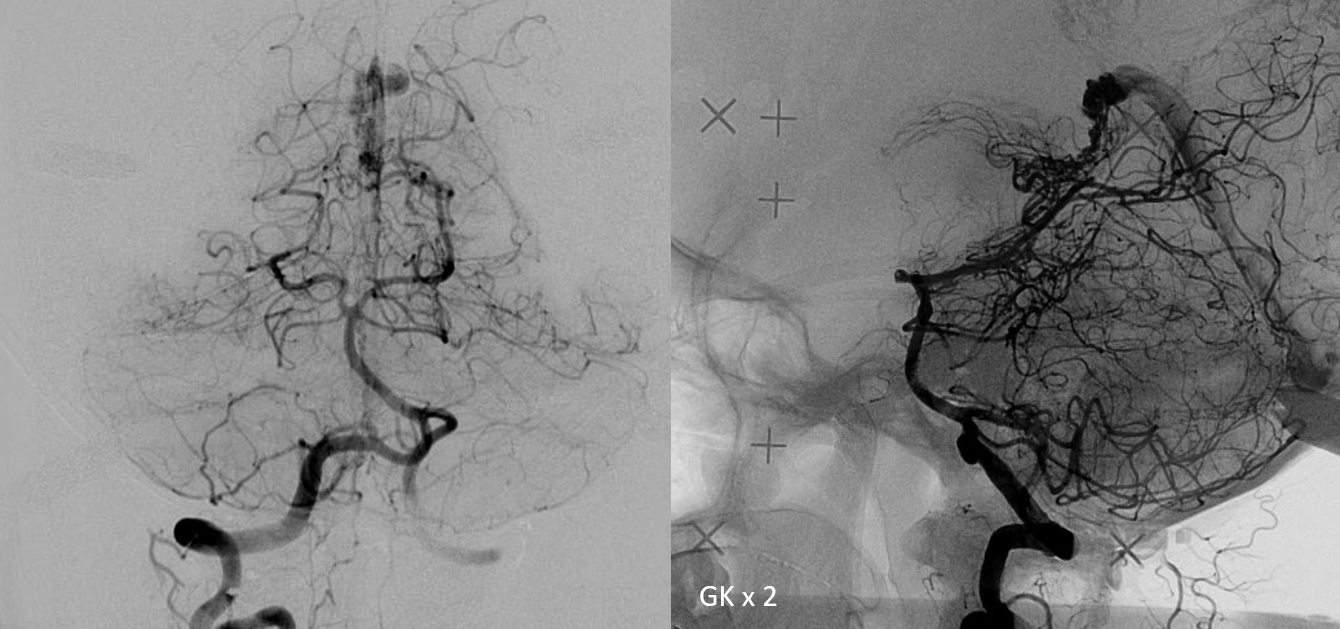
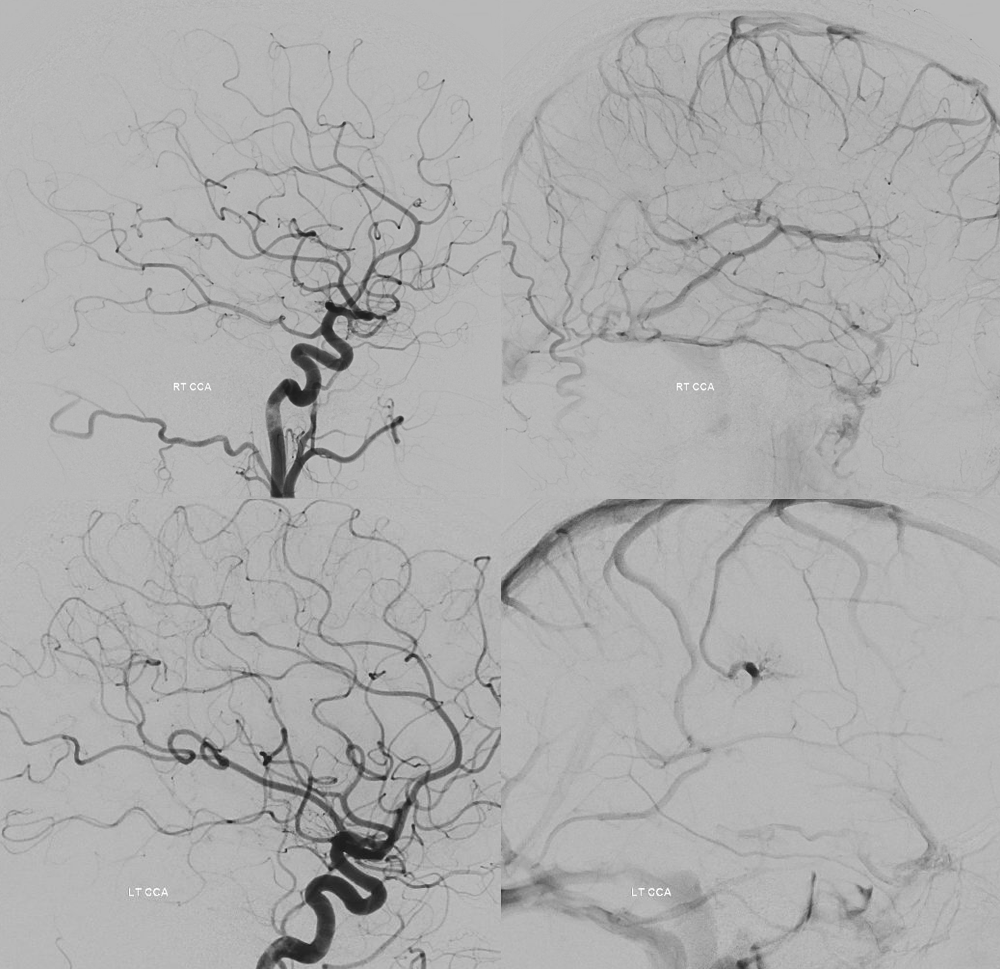
Treatment options include embolization — in this case transvenous coiling of the fistulous venous pouch marked by pink arrows in the images above, or Gamma Knife. In this case, we chose Gamma Knife. Below are bilateral ECA injections, to best demonstrate the target — the round venous pouch.
Cool stereo images of the same, looking from the left side, with the transmedullary vein closer to the viewer in lateral projections
Anaglyph stereos
So, this fistula was radiated
Four years later…

It is a bit less fistulous… really. But — the pretty low efficacy of GK for this kind of fistula is well known.
So, lets go back to the basics… nBCA embolization of the innumerable Davidoff-Schechters…
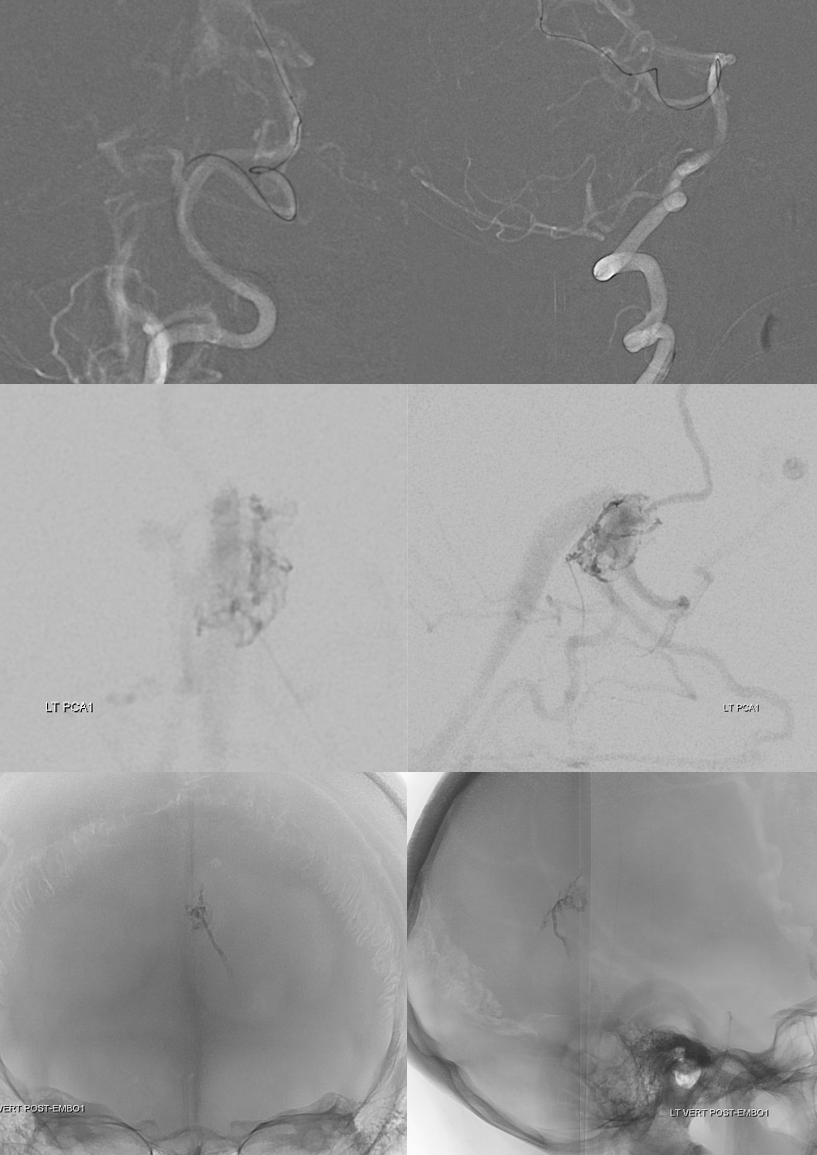
And two more — one from each MMA, wedging (or balloon) in the falx arterial channels


Post embo — pretty decent
Now, second round of radiation — targeting the remaining piodural shunts
“Four more years”….
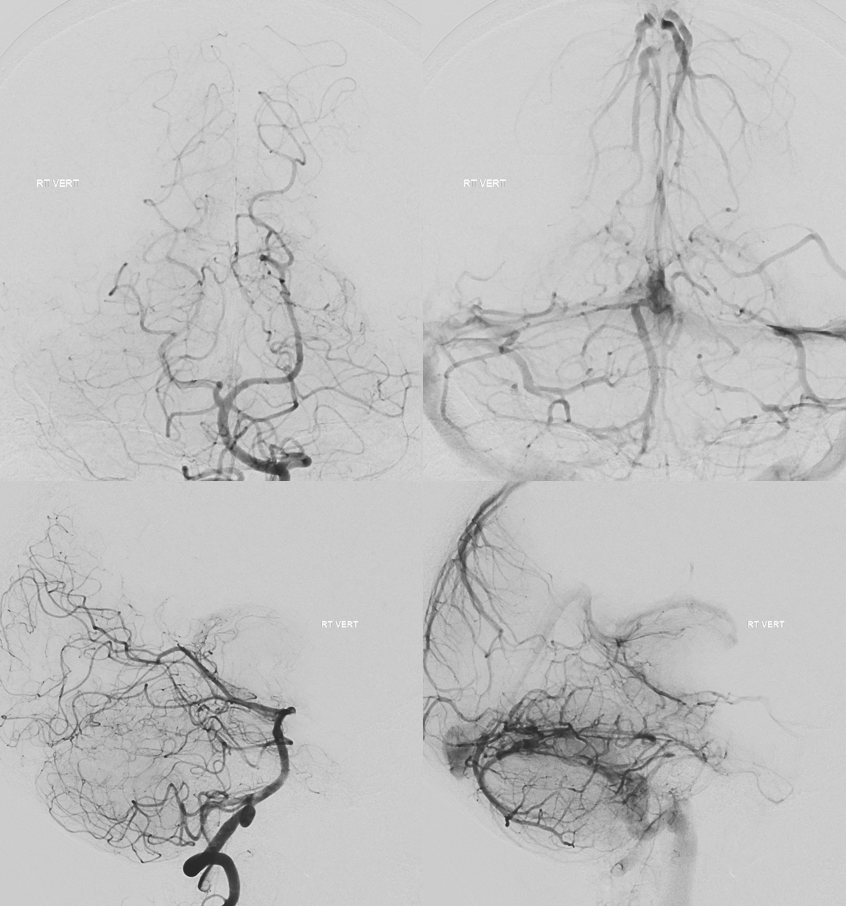
So, about 9 years from diagnosis — was there any upside to waiting? Could the fistula have been cured at the outset by coiling off the Galen? With/without arterial injections?
The downside: waiting, multiple procedures, costs, x-ray dose…
The upside: no complication (despite multiple procedures, each was relatively low risk), cured (can one argue with success?), the galen and straight sinus remain patent, now draining antegradely (right ICV and posterior circulation for example look almost completely normal — as if nothing happened). Left ICV still empties via transmedullary vein, but that would be the case no matter what treatment was done
The alternative: Upfront transvenous embo — upside is cure right away; downside is possibility of (rare but typically catastrophic hemorrage from piodural PCA Davidoff-Schechgter anastomoses); another downside is the patient does not get their Galen back
What would you do if your mother asked you?
