The utility of preoperative embolization depends on several factors, such as tumor size, location, and vascularity. Large and vascular tumors in relatively accessible locations such as cerebral convexity may still not be as important to embolize preoperatively as smaller and perhaps less vascular tumors in more eloquent locations, such as petroclinoid region or foramen magnum.
The efficacy of embolization is simply a function of how well the tumor can be devascularized at the capillary level. To that end, small particles in my opinion have the greatest efficacy for transarterial embolizations. Liquid embolics do not penetrate as well, since they tend to harden in larger caliber vessels. To achieve maximum particle deposition it is helpful to have a limited number of feeding pedicles. Convexity tumors with one or a few related middle meningeal artery feeders are the easiest, but also least important embolization targets. Skull base lesions, such as petroclinoid or sphenoid ridge types, tend to have multiple feeders. Even if most of these are controlled, the remaining ones will tend to maintain perfusion of the bulk of tumor, albeit at lower efficiency — nevertheless the embo is not going to be that dry.
The foramen magnum lesion is one location where it is possible to achieve a really efficient embolization, because the potential dural sources of supply are limited (similar to convexity masses). The typical source is the odontoid arcade. The direct supply comes from bilateral vertebral arteries, and indirect one from the ascending pharyngeal arteries — 4 pedicles in total. If no leptomeningeal vessels are involved, chances are are quite good that controlling the limited number of feeders will lead to a good result.
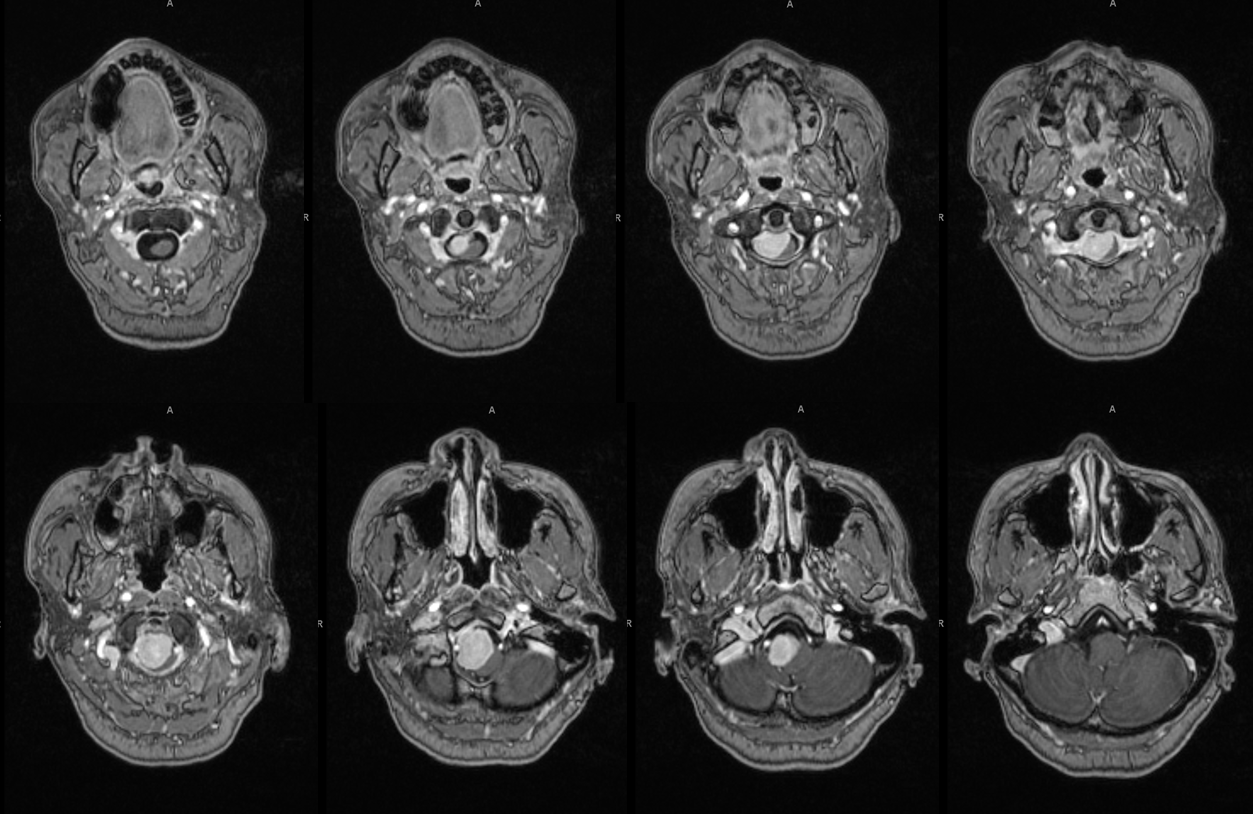
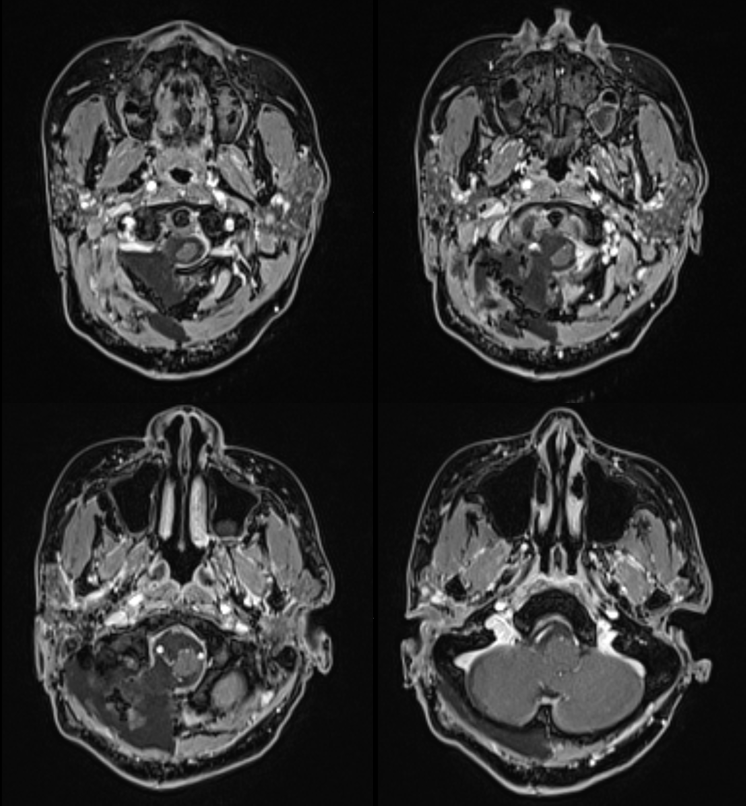
This quite vascular meningioma of the foramen magnum came to light as a result of swallowing difficulties. MRI shows an extra-axial lesion nearly completely filling the foramen magnum
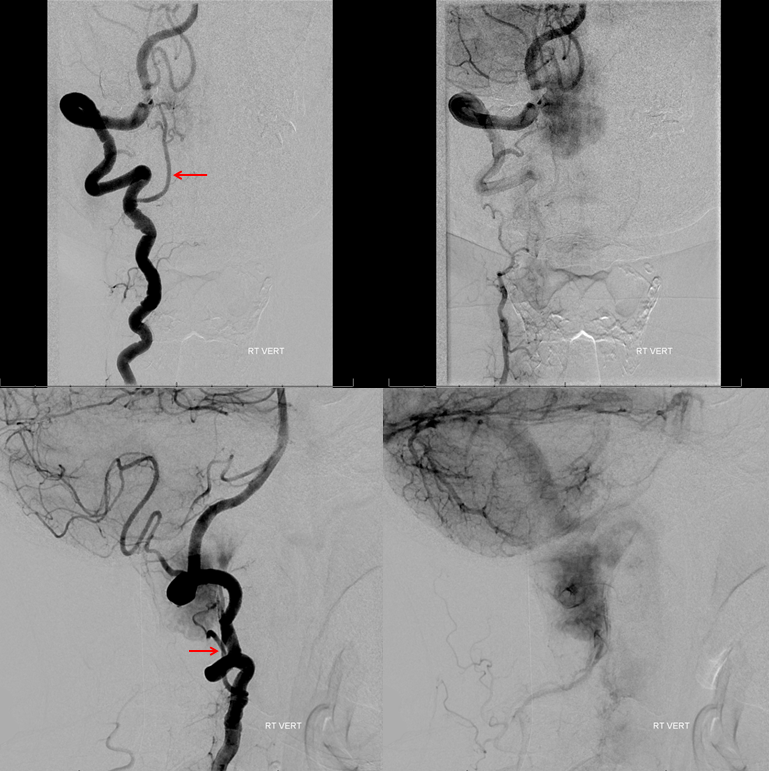
Tortuous nature of left vertebral artery with odontoid arcade source of meningioma supply

Arterial and venous phase demonstrating persistent meningioma blush in venous phase. Odontoid arcade is labeled with red arrow
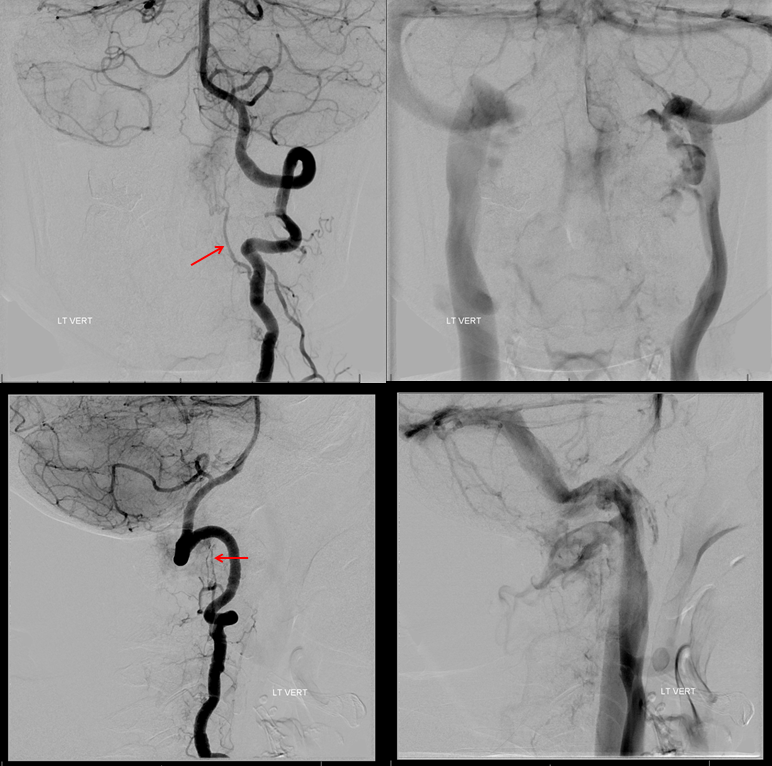
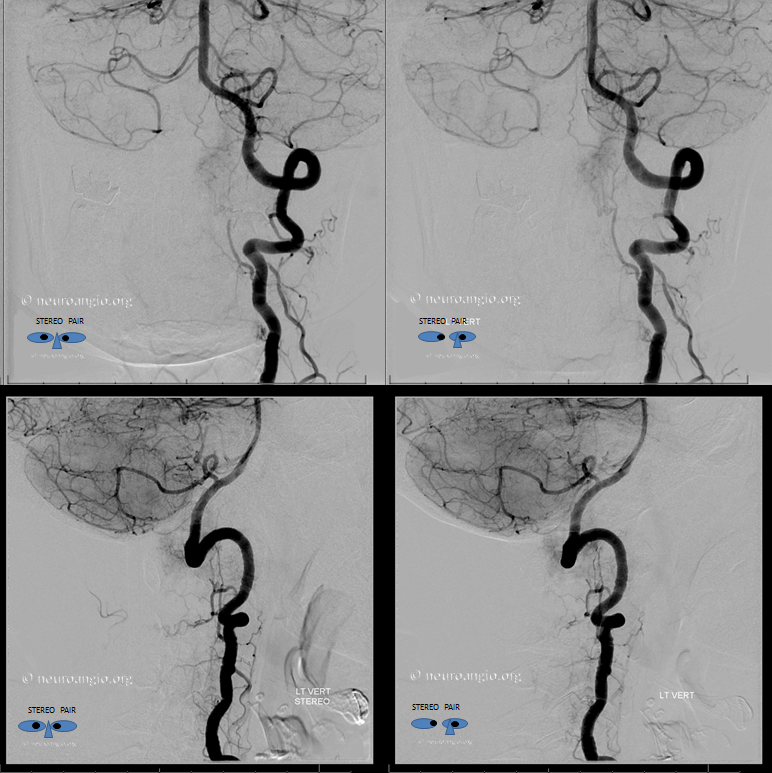
Stereo views
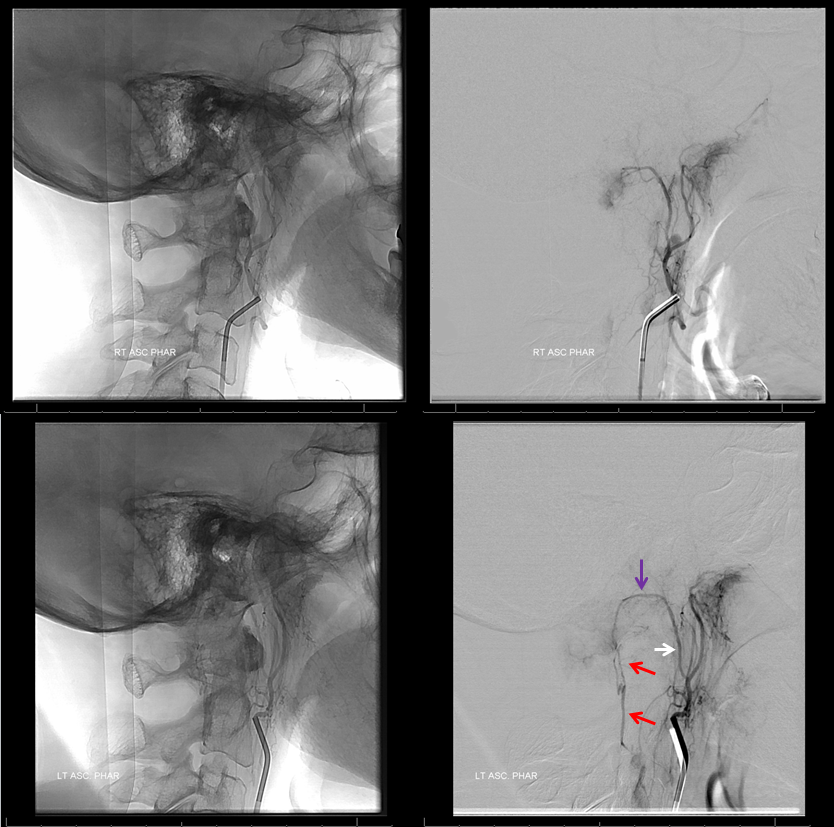
Right (top) and left (bottom) lateral views of ascending pharyngeal artery injections. Notice opacification of the odontoid arcade segment (red) previously seen via the left vertebral injection (same red arrow above), supplied via the neuromeningeal trunk (white arrow)
Right vert injection, with red arrow pointing to the right aspect of odontoid arcade. Intense, homogeneous, and persistent tumor blush, typical of meningioma.
In summary, the supply to the tumor arises exclusively from the odontoid arcade, which is primarily supplied via the vertebral injections and secondarily via the ascending pharyngeal artery. Each pedicle is now catheterized and small particles injected. The more distal the catheter position, especially in the neuromeningeal trunk, the less the chance of cranial nerve injury. Nevertheless, primary embolization should be performed from vertebral approach.
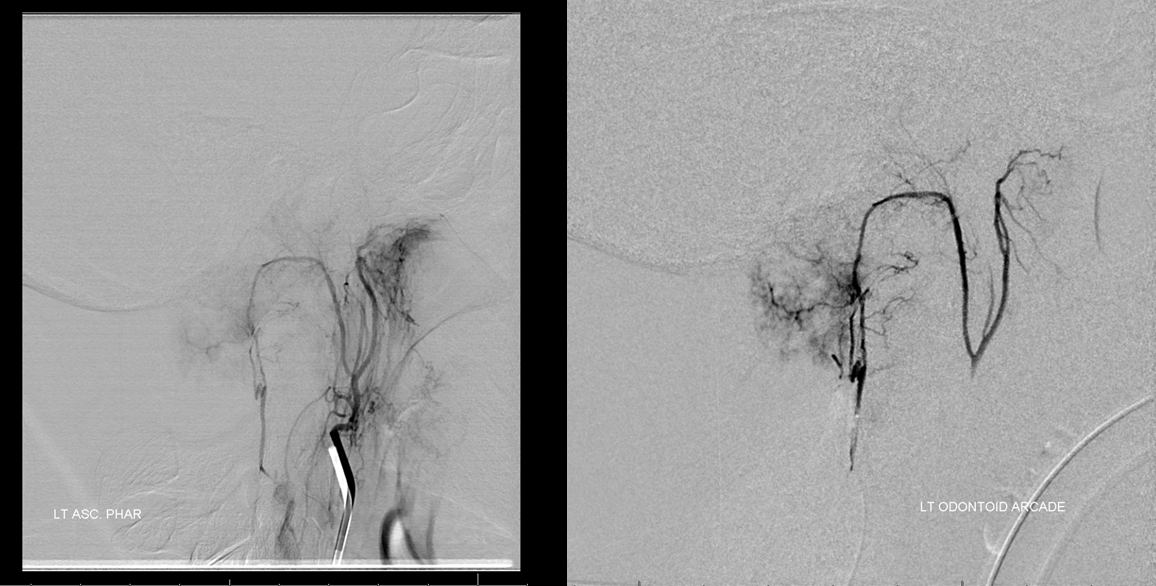
Injection of the left odontoid arcade perfectly visualizes the neuromeningeal and pharyngeal trunks of the ascending pharyngeal artery. Catheterization is followed by particle embo and closure of the odontoid arcade with coils

Side by side views of vertebral and ascending pharyngeal injections to show the point
Continued embolization– ascending pharyngeal artery — notice distal location of the catheter, which minimizes the risk of cranial neuropathy as the odontoid arcade itself is accessed. Small particle embolization follows. The left odontoid arcade coils are visible post embo there.

The bulk of supply comes from the right ondotoid arcade. Classic spokewheel appearance of meningioma
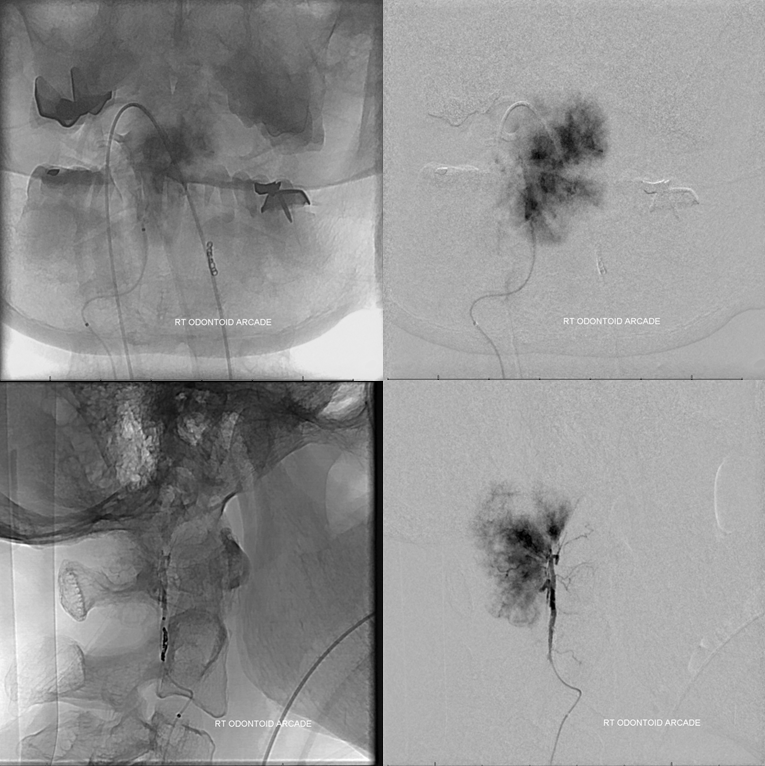
Post right odontoid arcade embo

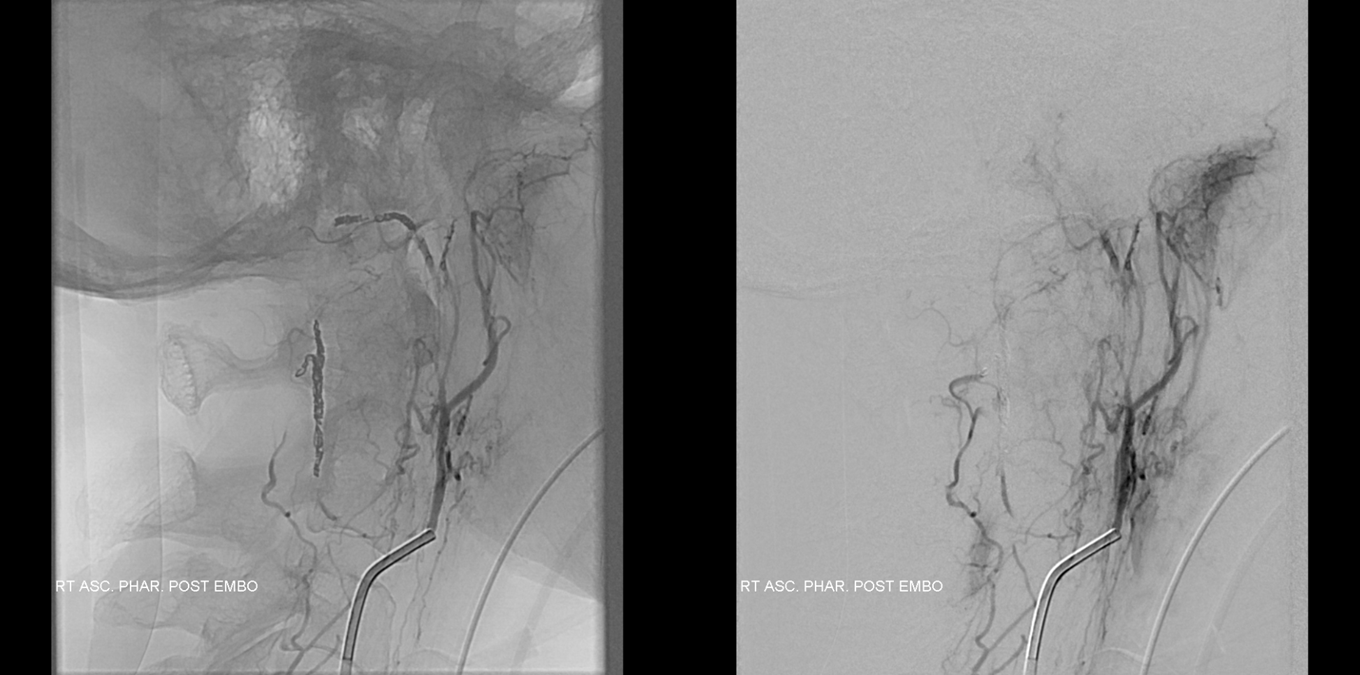
Right ascending pharyngeal is the last pedicle to be embolized — again note residual blush despite the immediately preceeding particle and coil embolization of the same region from below. This shows the importance of controlling all pedicles supplying the tumor, if possible

A distal microcatheterization, followed by particle embo. Even for a 4-pedicle lesion such as this one tumor embo is meticulous work
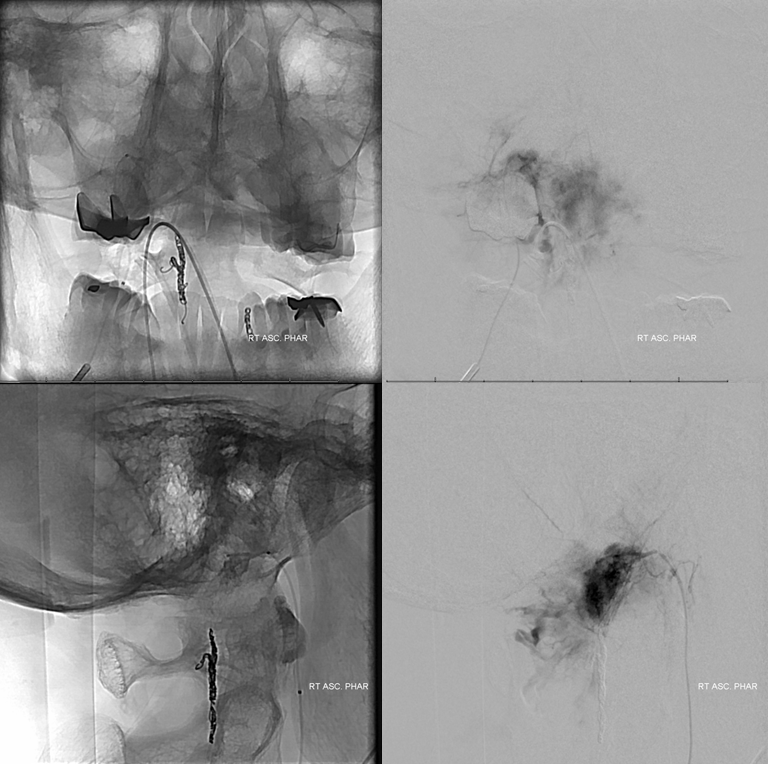
Final post- embo picture. Coils are seen in the neuromeningeal trunk on the right. The tumor is completely devascularized
Postop MRI
Back to Techniques Preoperative Tumor Embolization
