Case Courtesy Dr. Eytan Raz
An awesome case with lots of super teaching points.
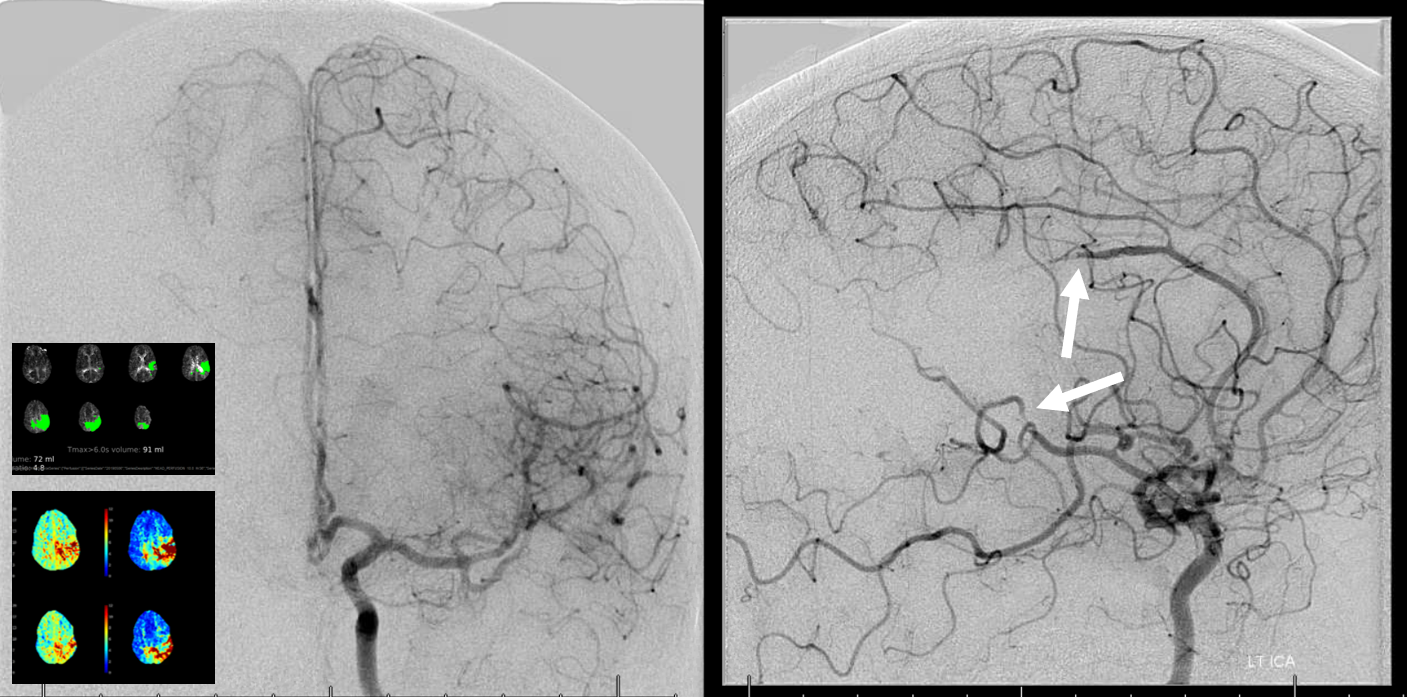
Patient presents with left MCA syndrome (initially)
CT perfusion rapid analysis shows a seemingly strange picture
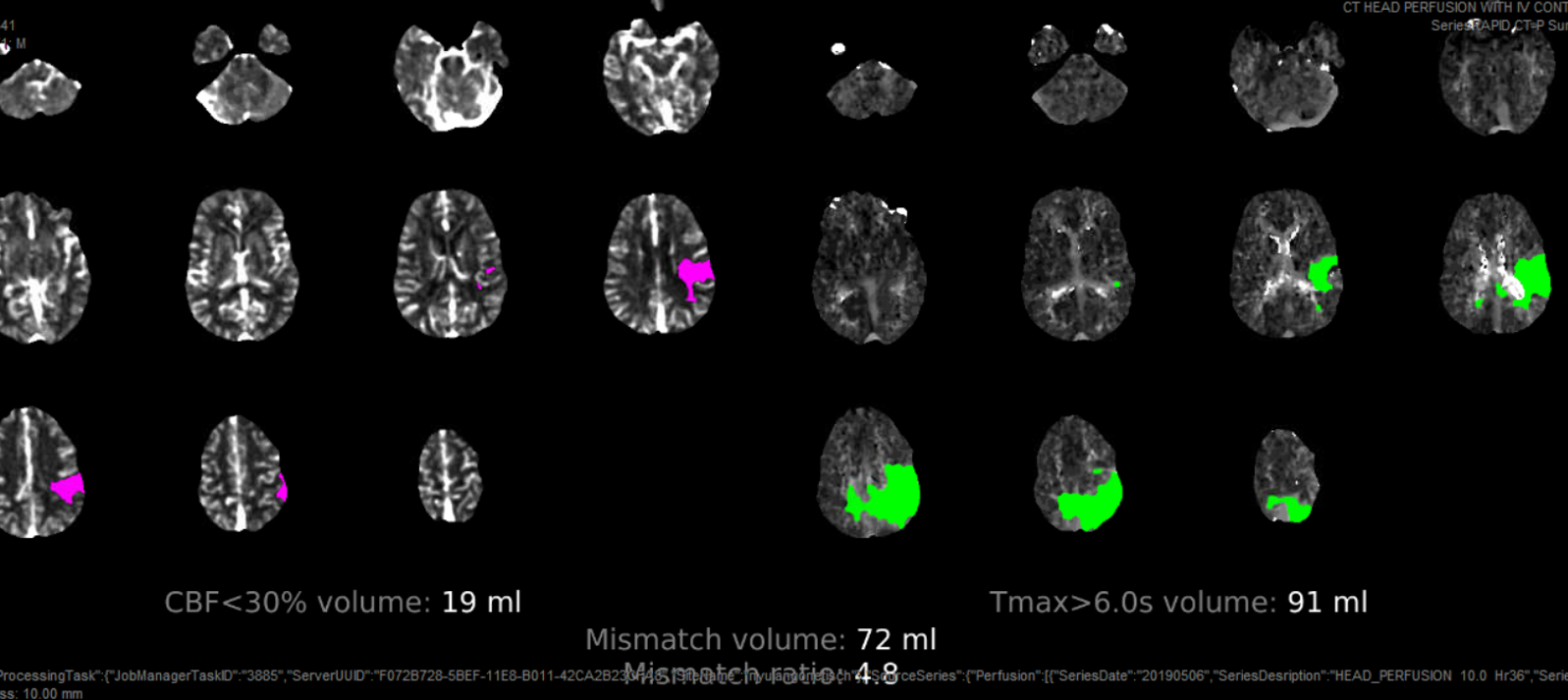
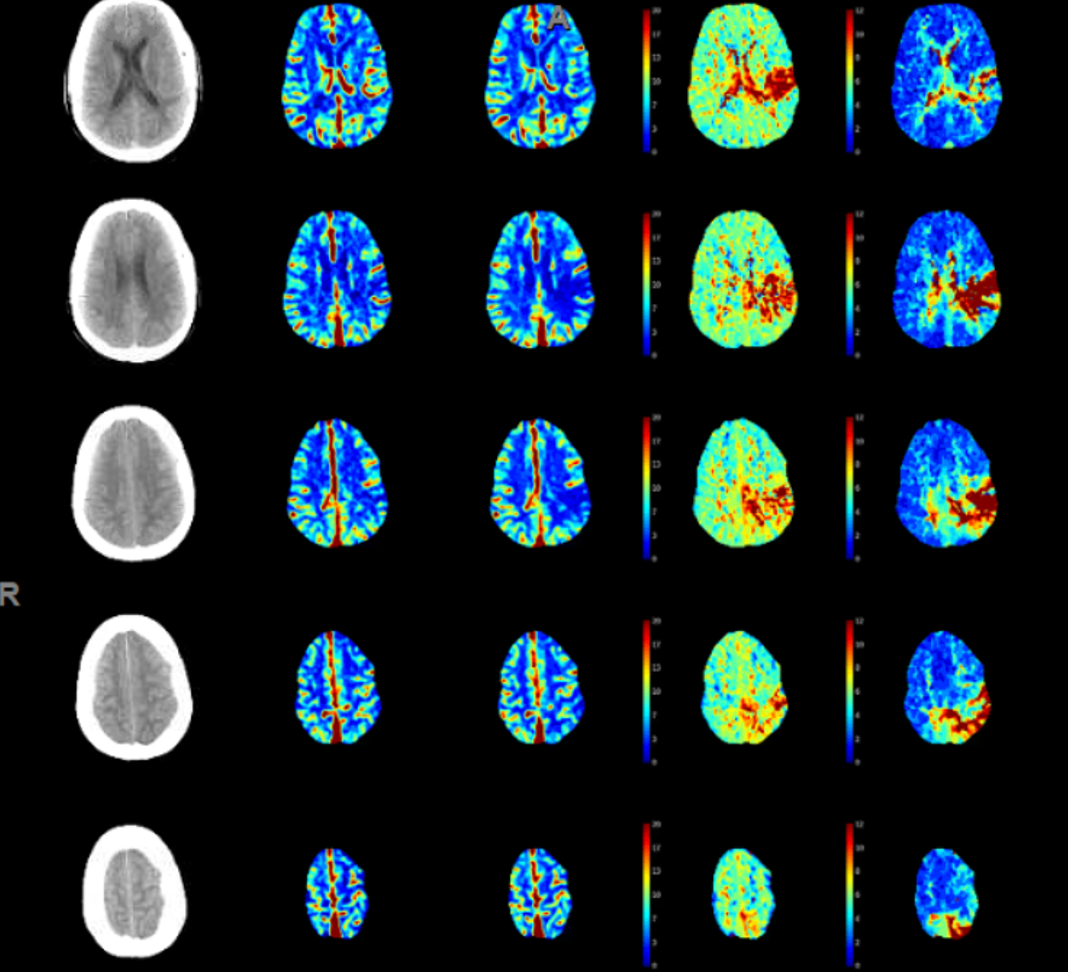
Seems like both MCA and ACA territory involved with some crossover into right mesial frontoparietal area. Do we trust this? Here its important to look at the maps. Maps seem to confirm the situation — there is decreased flow (TMAX is longer) in the same areas. Not much movement seems to be present. The CT images show no infarct changes.
Are there ACA and MCA occlusions? Why is there extension of TMAX to right?
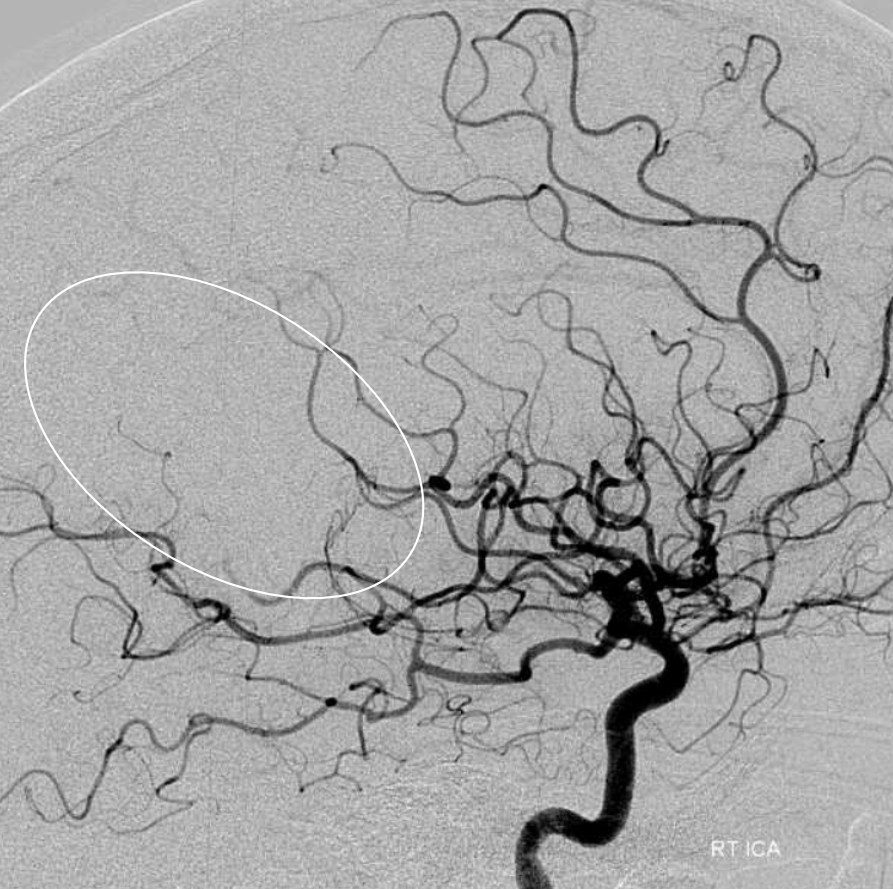
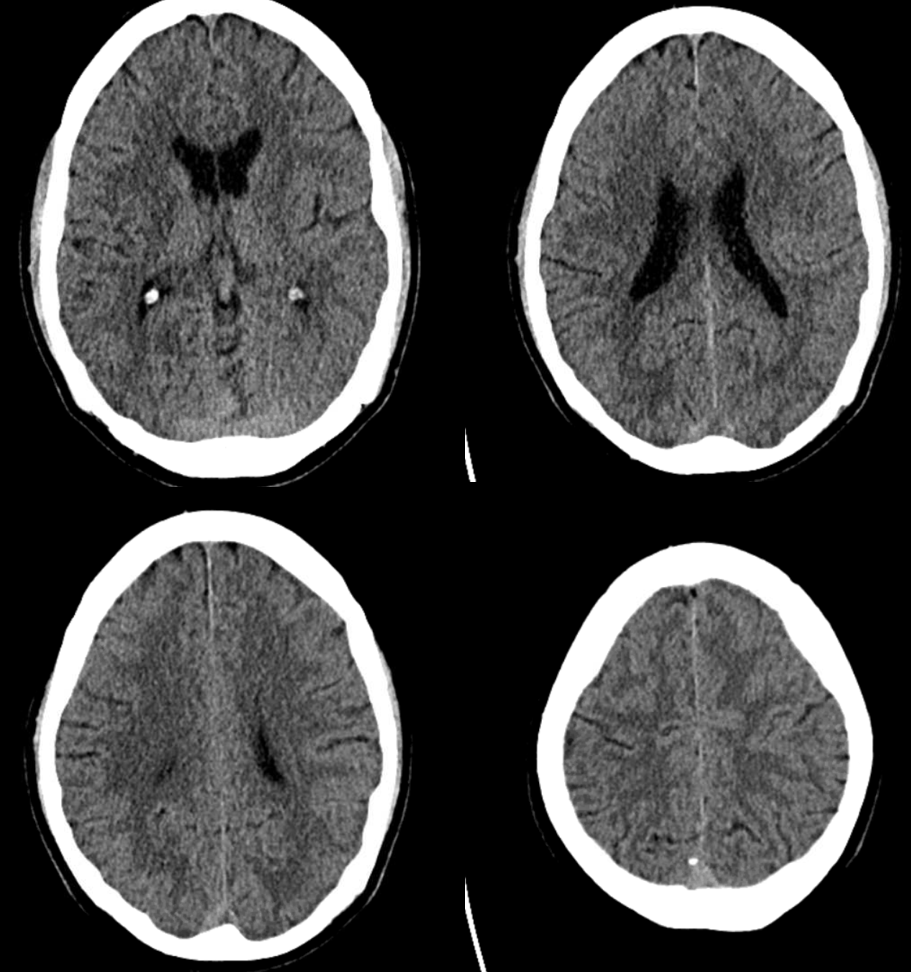
As it happens, 3 months ago the same patient presented with a right MCA embolus (white oval). The same angio also shows the configuration of ACA in this patient, with right A2 supply limited to mesial anterior and mid-frontal territories. The distal pericallosal artery is not seen.
Left ICA injection (again 3 months prior to current stroke presentation) shows what we expect — the pericallosal artery supplies bilateral mesial posterior frontal and parietal hemispheres. This is not uncommon. This configuration as well as the true “azygous” ACA occlusions can lead to bilateral lower extremity weakness mimicking a spine problem, as shown in a companion case here.
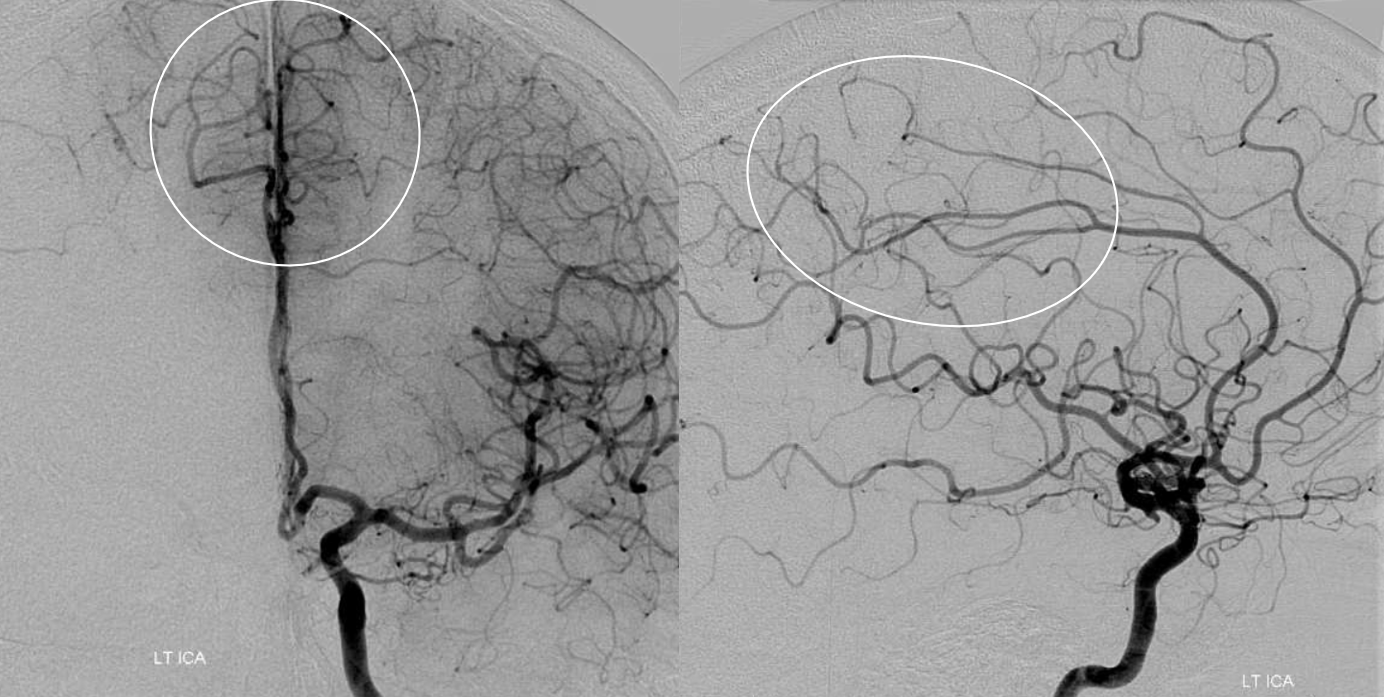
The above analysis shows exactly what to expect. Indeed, there is now a distal ACA (pericallosal) and “medium vessel” left MCA emboli — the angio looks exactly like perfusion. Also important to recognize is that these patients often do poorly, as the leptomeningeal collateral network for either vessel is usually unavailable do occlusion of the other.
Reperfusion — Sofia 5 aspiration of MCA occlusion
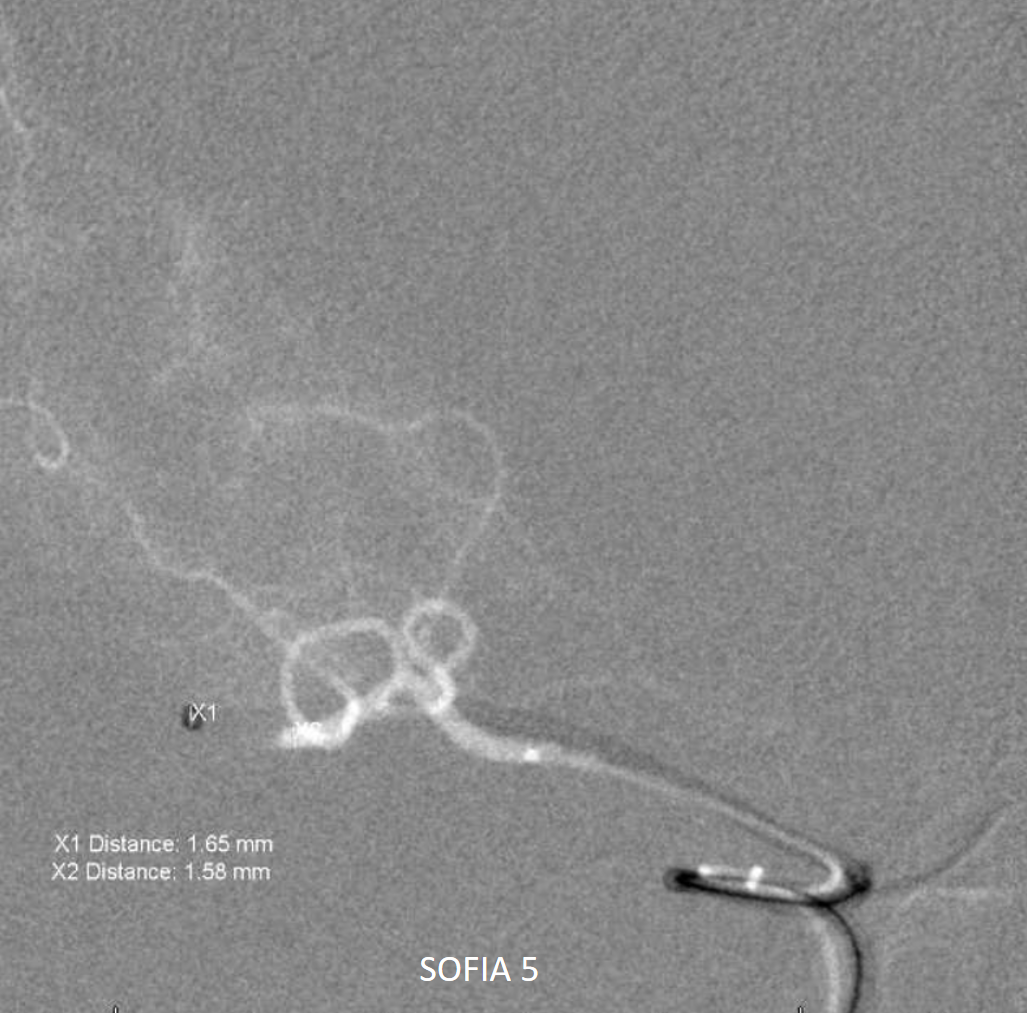
By the time of this recanalization the pericallosal is reopening spontaneously
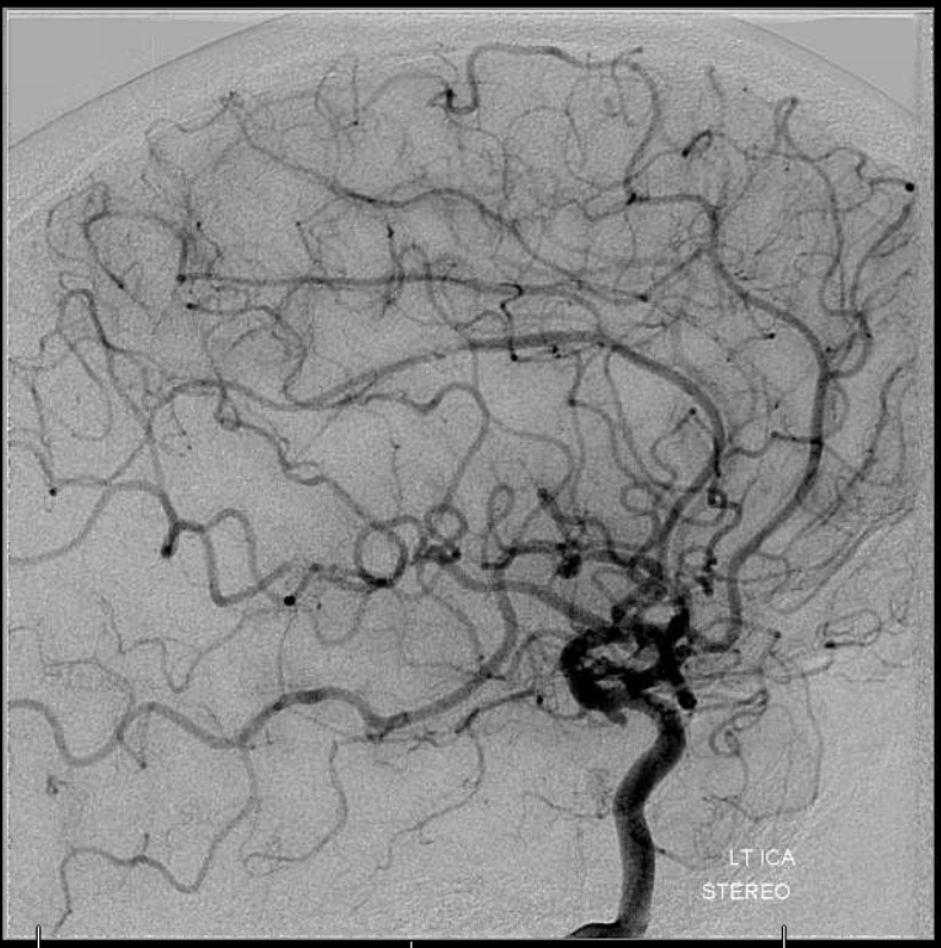
Final post
Takeaway points:
- Use of perfusion as diagnostic tool to understand the site or sites of occlusion and the territories at risk — use of TMAX maps in particular. This use of perfusion is distinct from the “traditional” concept of perfusion as a way to define “core” and “penumbra”. This is not about “core” — its about rapid diagnosis of whether or not an occlusion is present, and what is the territory at risk
- Appreciation of how variations in anatomy guide understanding of acute stroke and treatment decision
Back to Case Library
