With Dr. Nossek
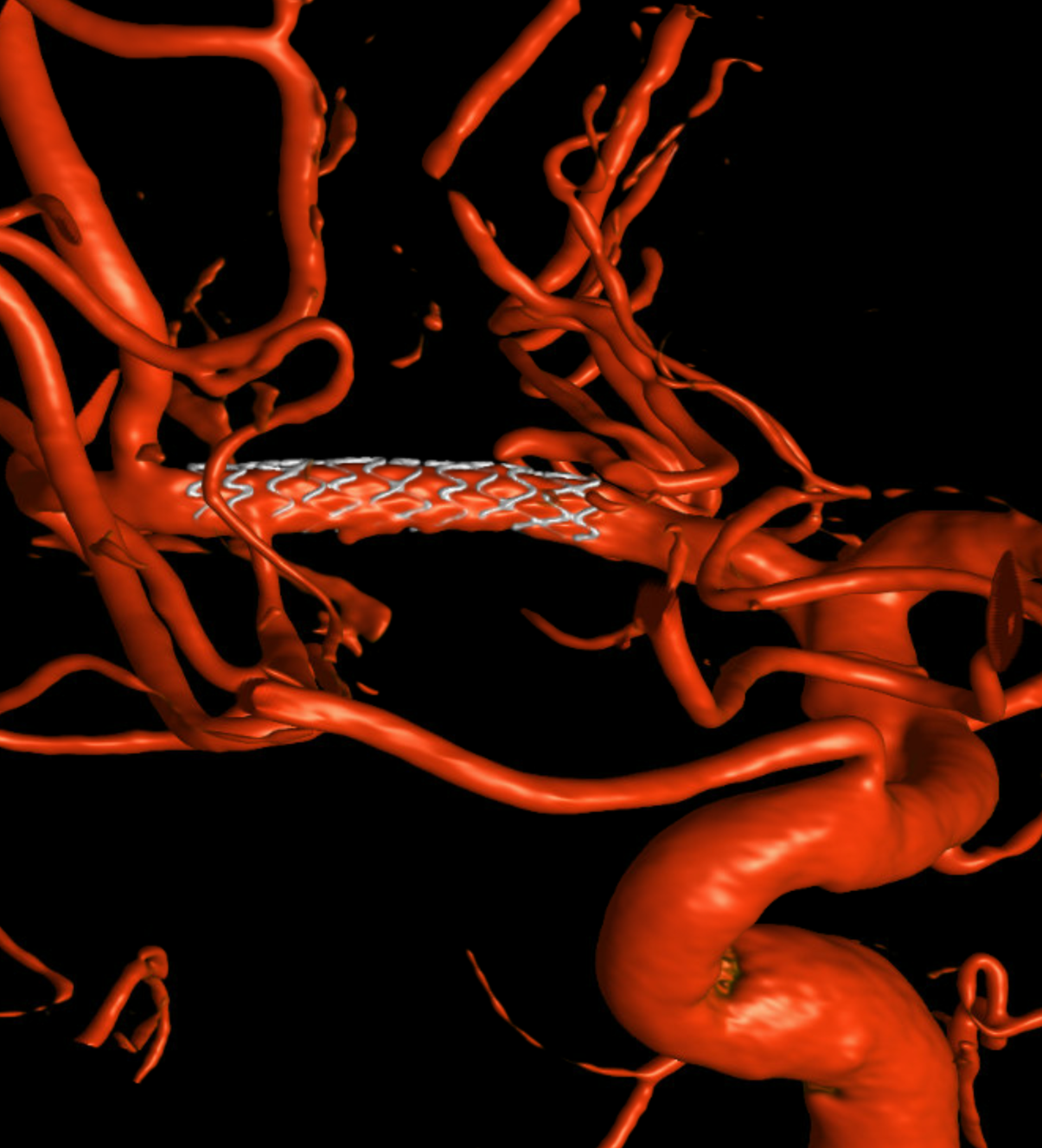
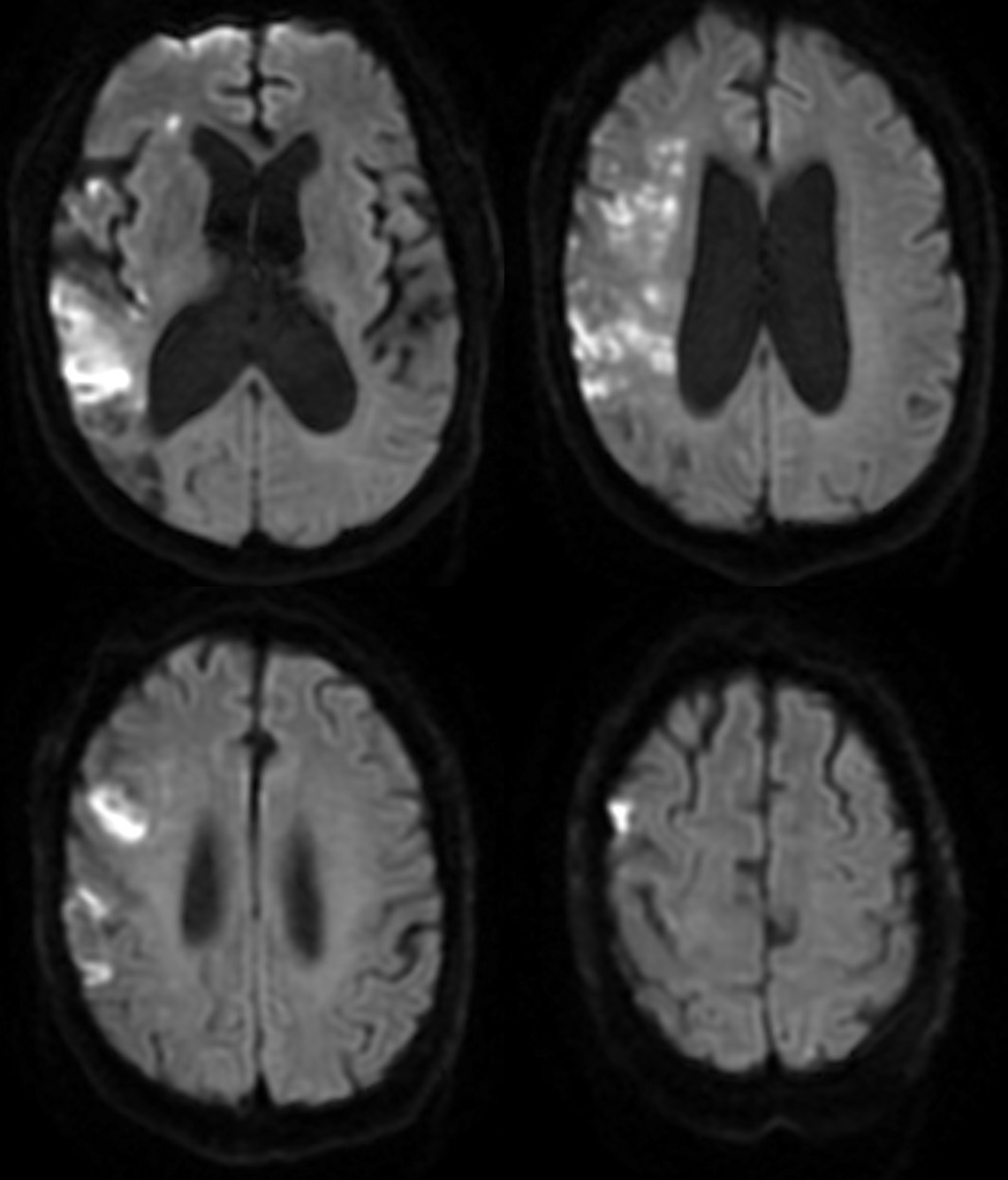
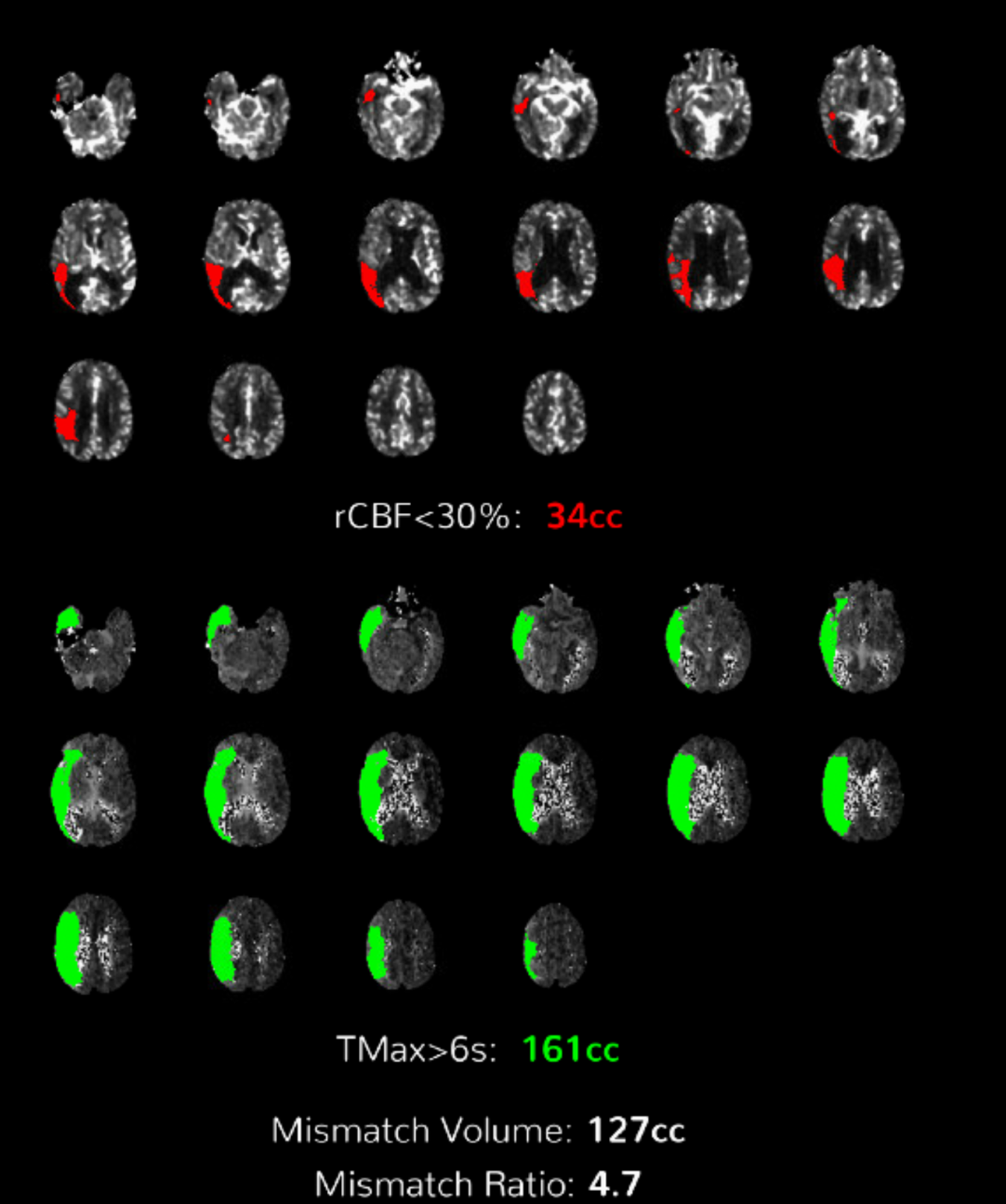
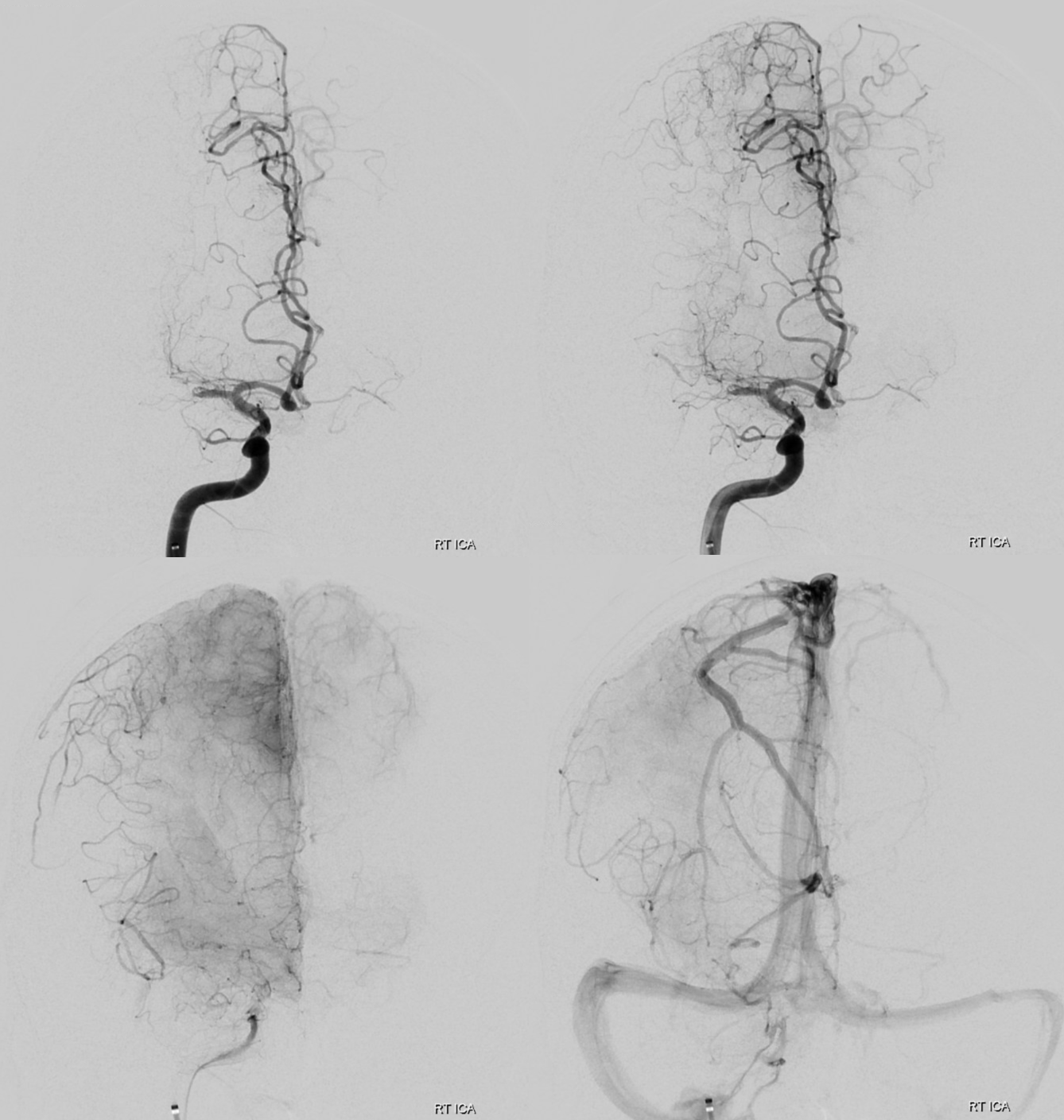
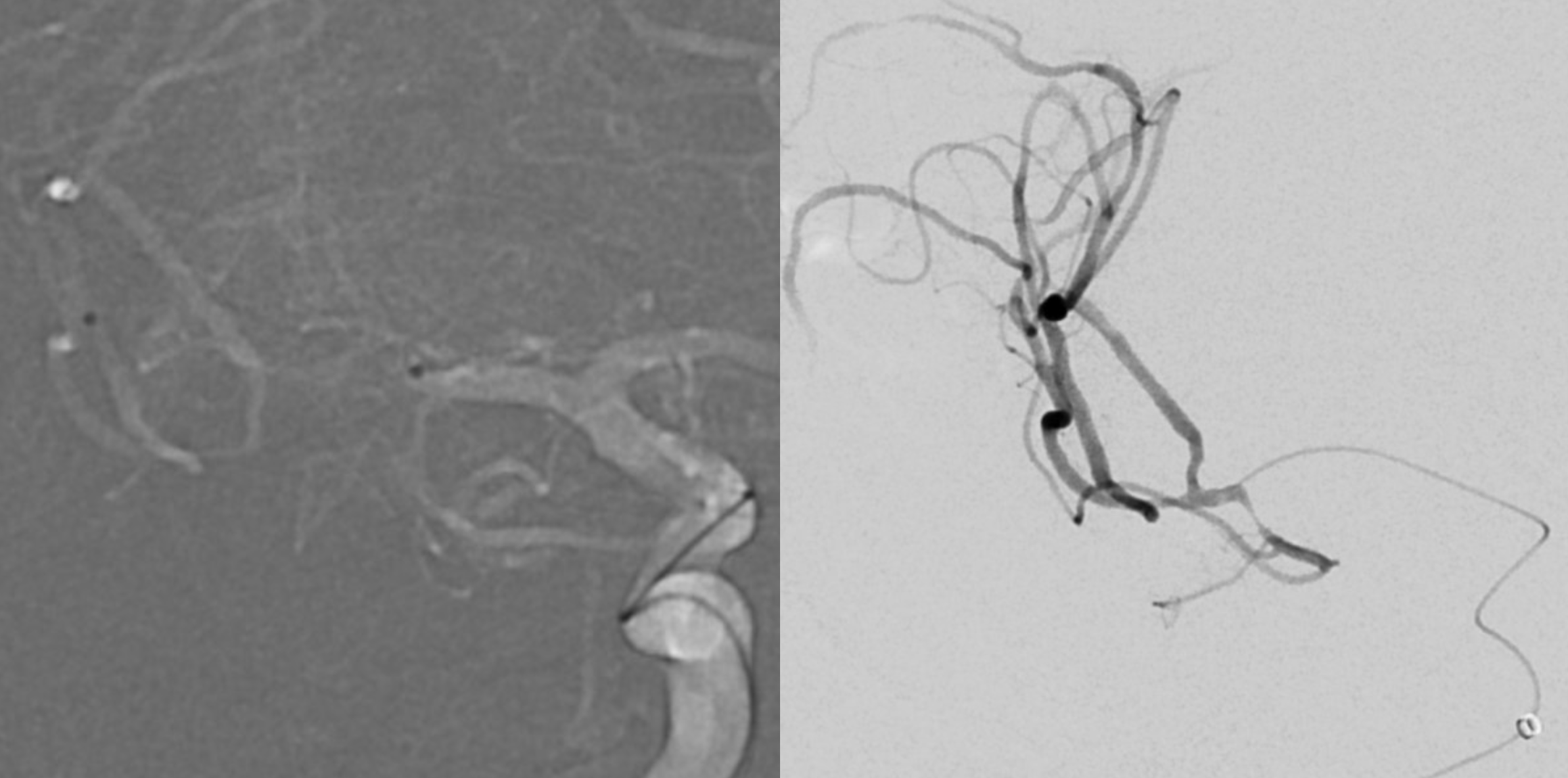
Something advanced and increasingly possible with modern technology — reopening of brain arteries that have been closed for some time. This is very different from hyperacute rush when minutes count in a developing stroke. That is done often now, and usually successfully. Opening something that’s been closed for some time, when scar starts to set in, is quite different. Its both harder and more hazardous. Fortunately, this kind of reopening usually makes sense for still relatively recent occlusions — like several days to several weeks. This MCA was closed for 1 week — and there was stroke when it happened. But there is still plenty of brain that is not getting enough perfusion.
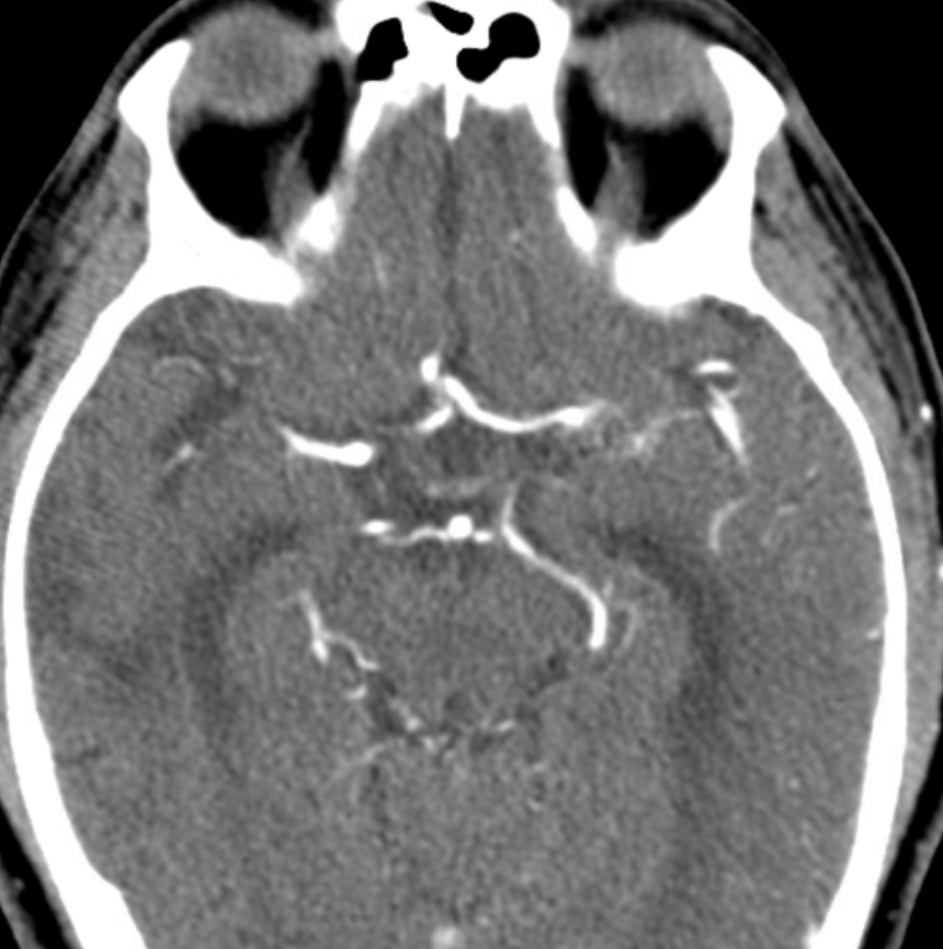
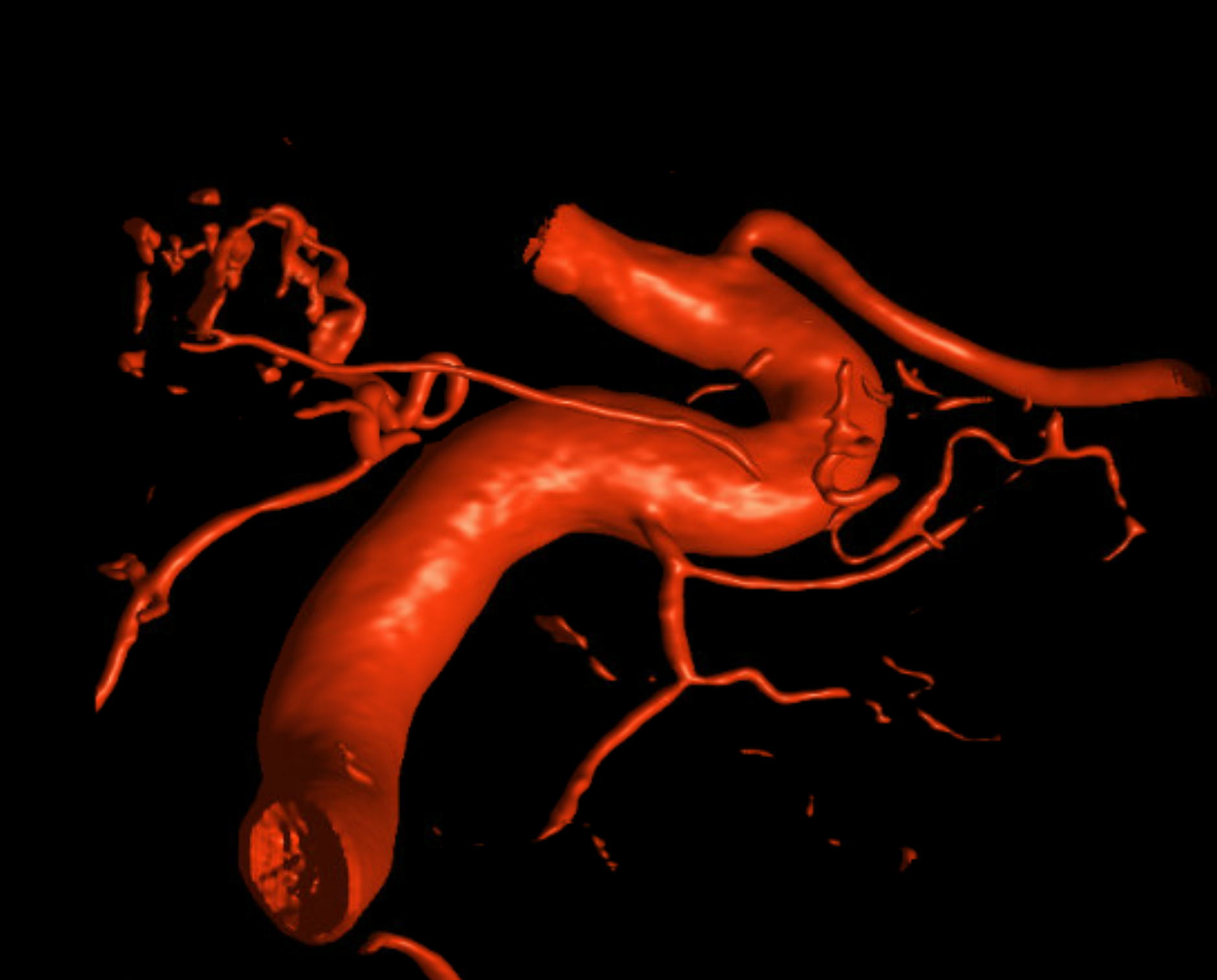
Coexistence of disease in other areas. Be careful…
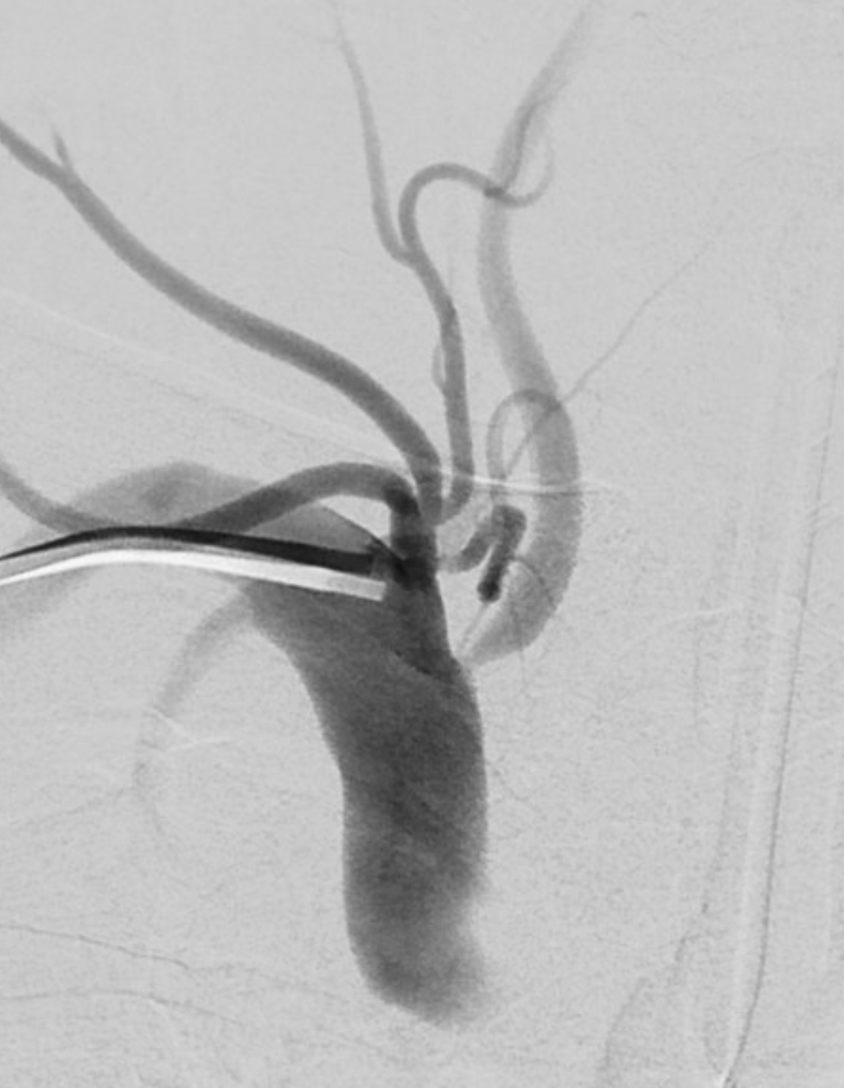
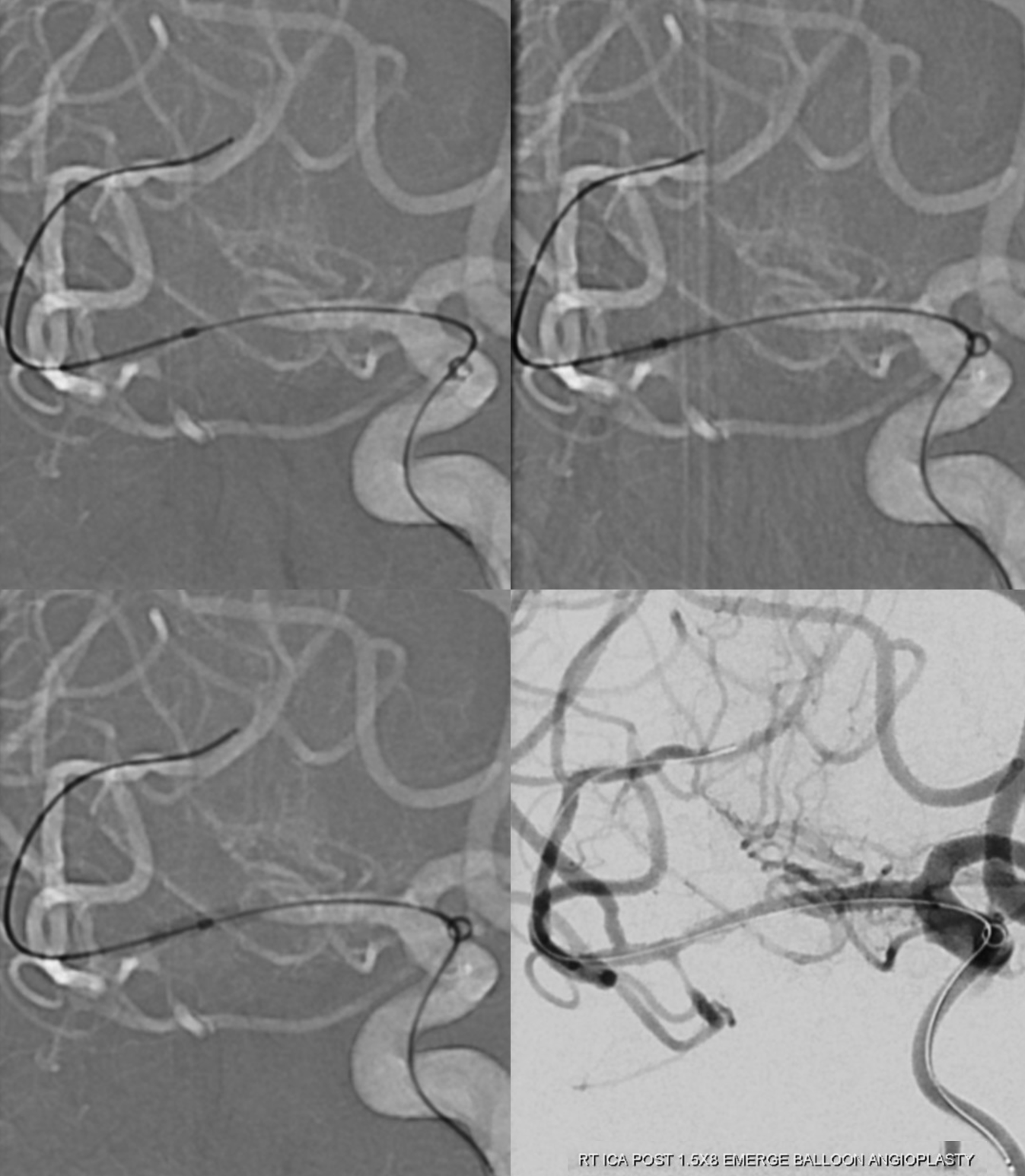
The hardest and most hazardous part is going through occlusion. Here we used an Aristotle 14 soft and Headway Duo 156
Best seen as a movie
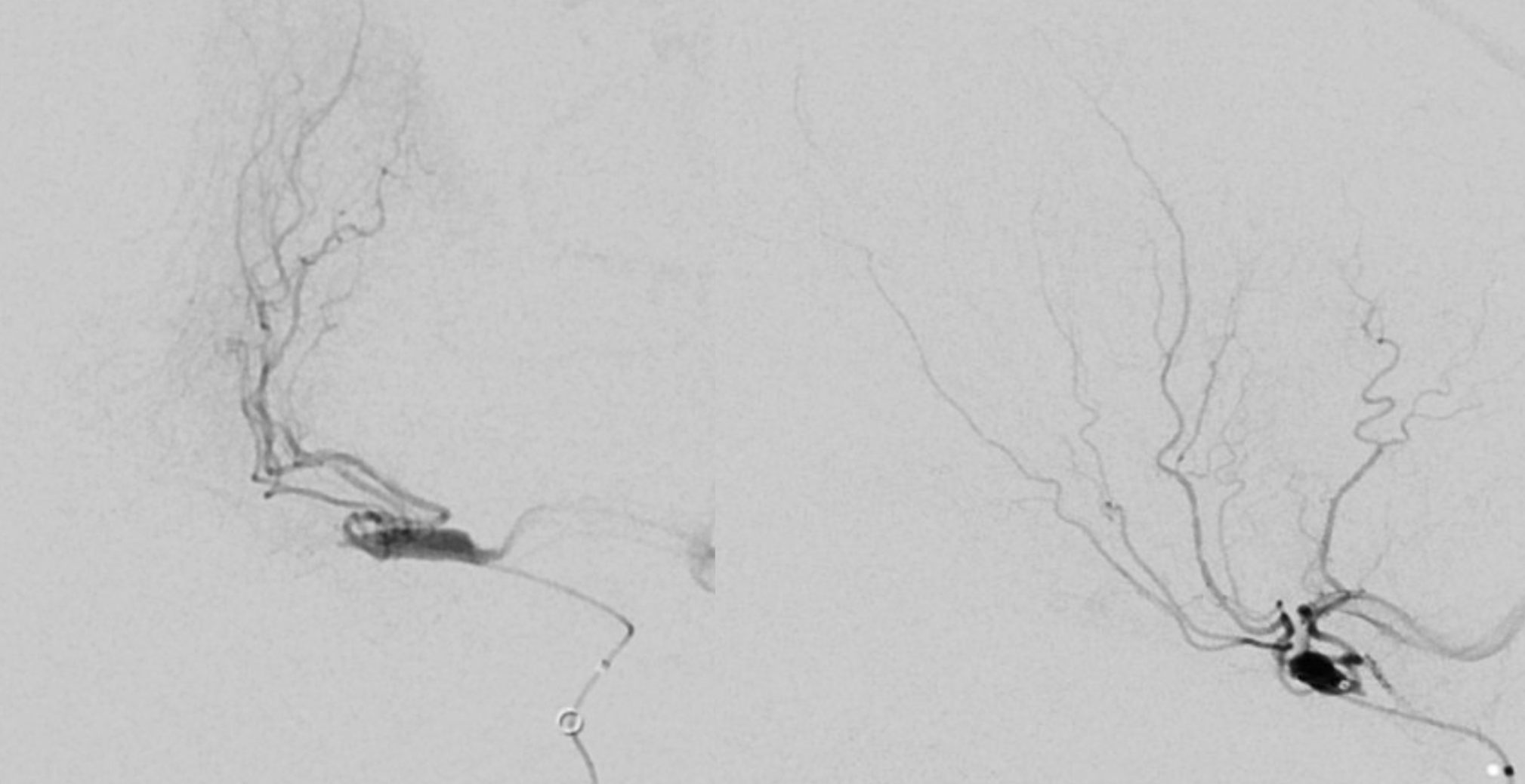
Why put in the Duo? It means some exchanges which can be tricky — because we want to optimally see and size the distal landing zone here, which we don’t see well on CT
Out of abundance of caution, we do a pre-stent angioplasty — make sure we are in right lumen, no perforation, etc. if there is one we can close back the MCA . Looks good though
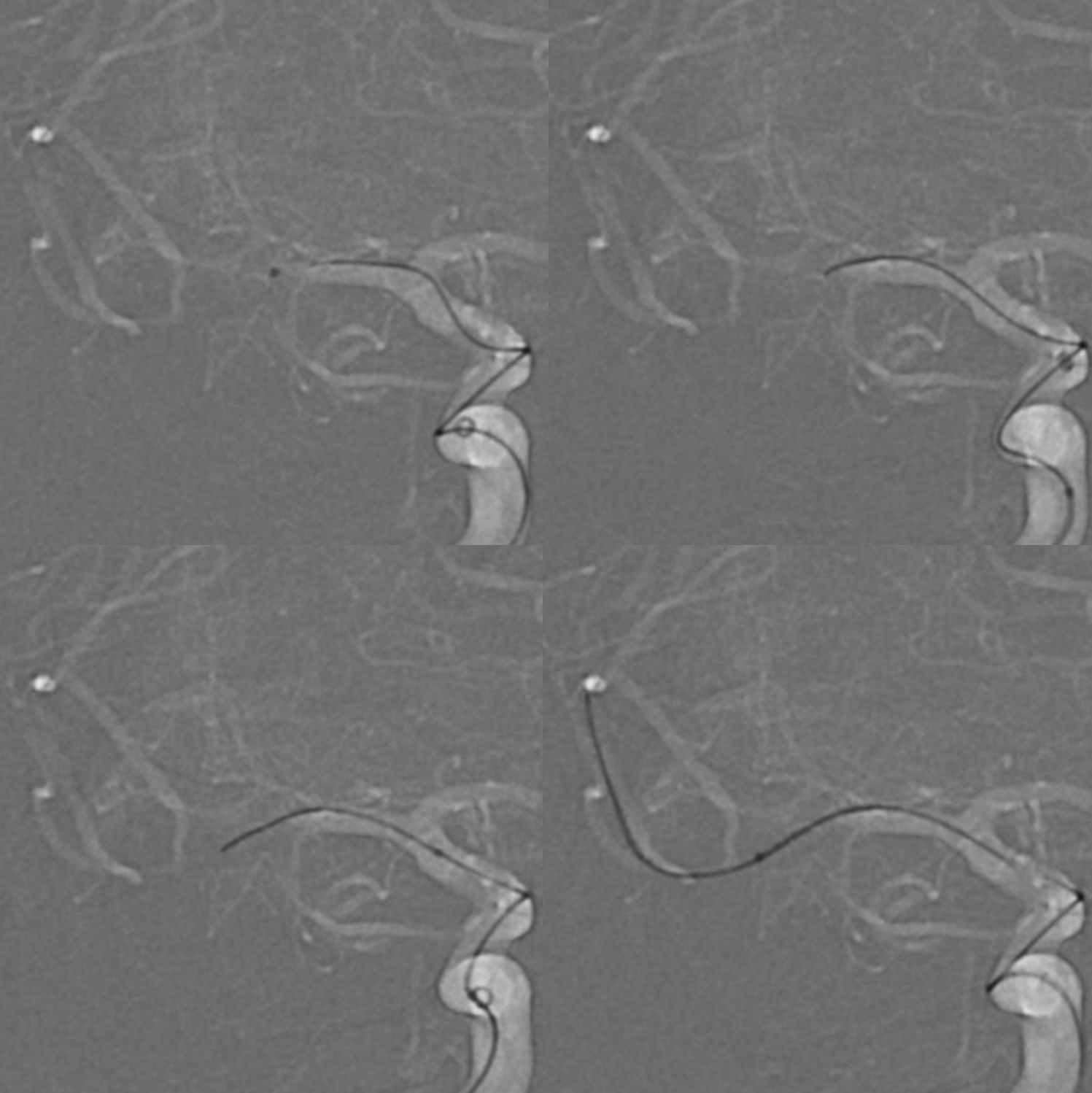
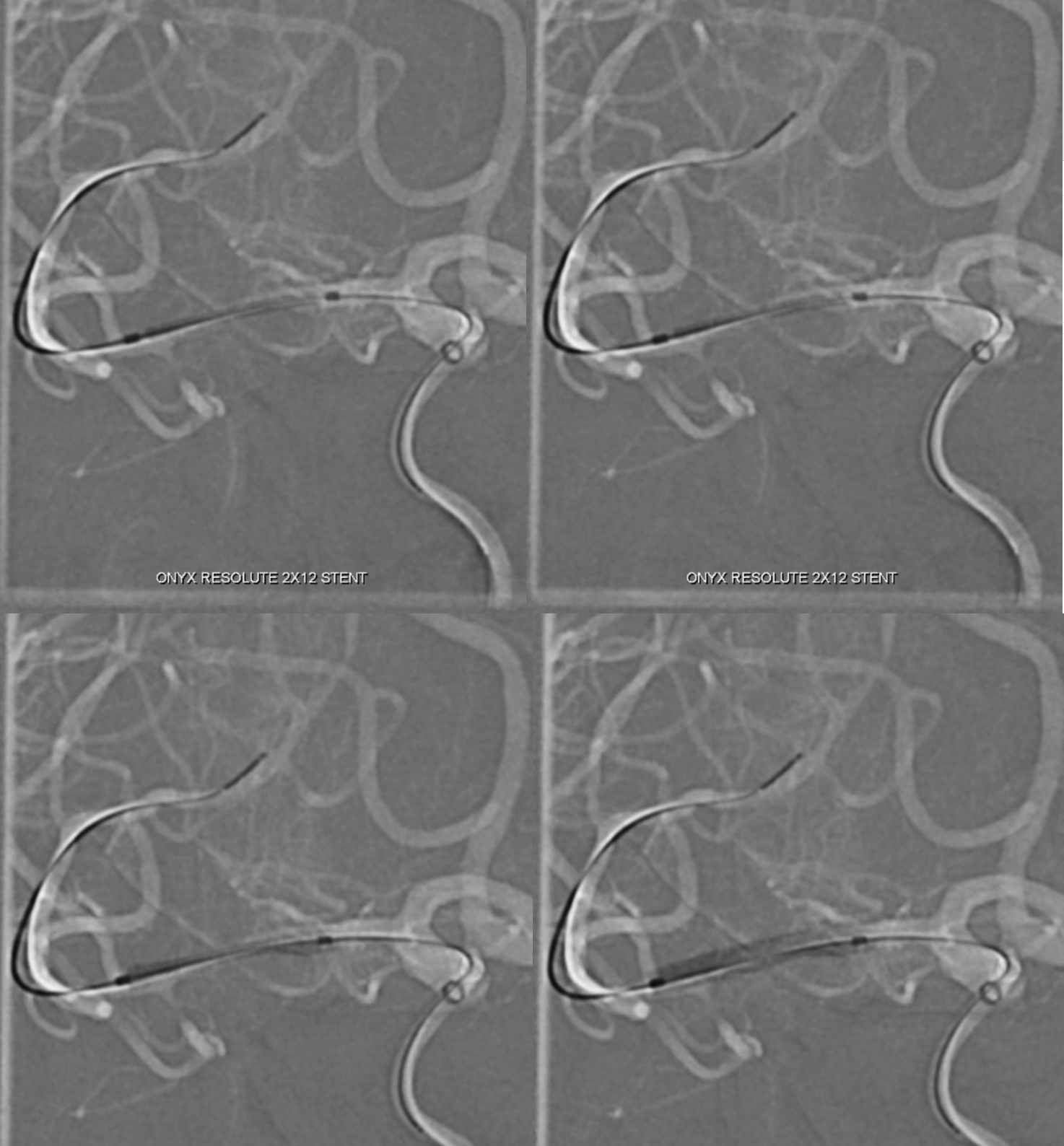
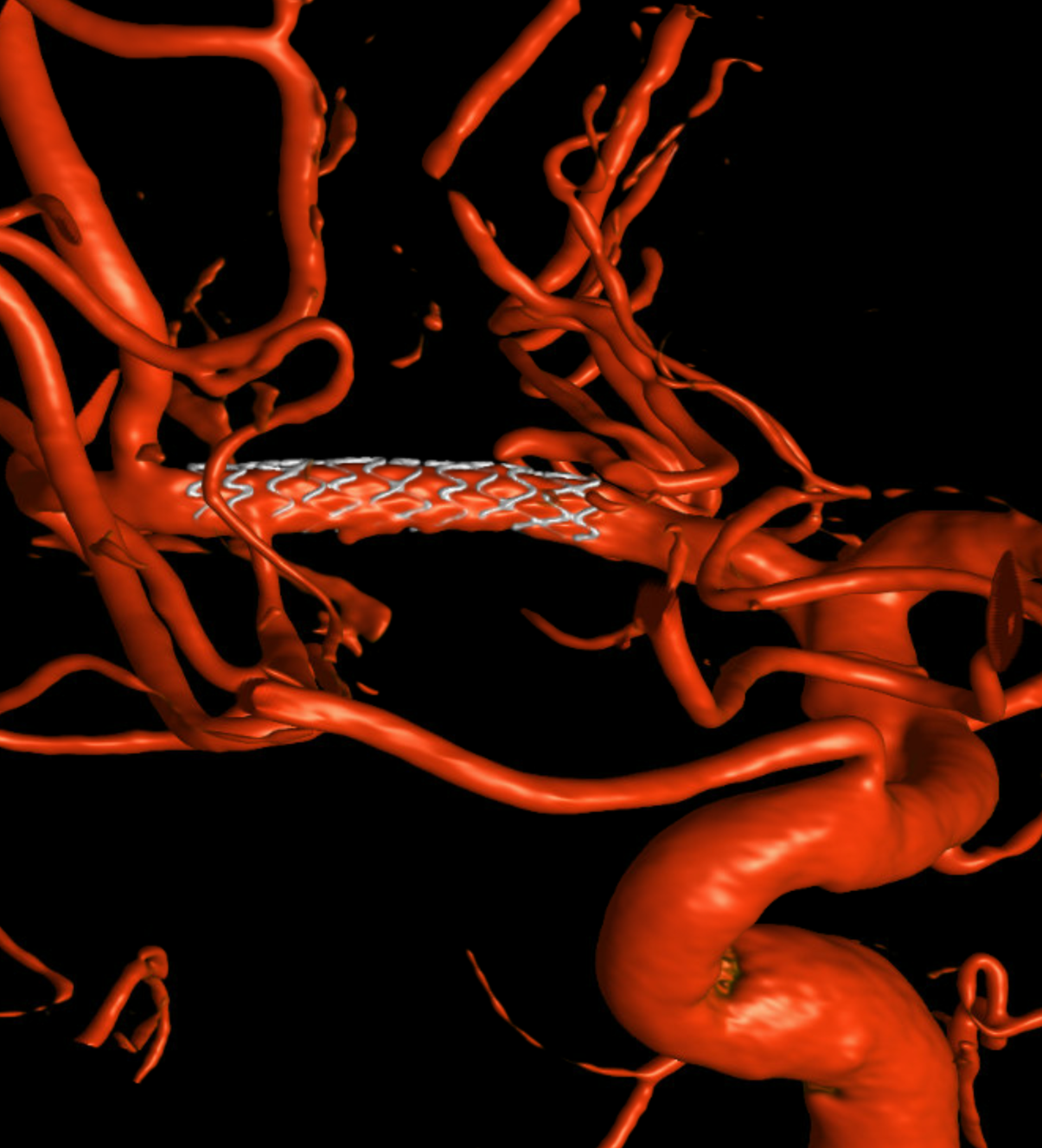
Stent is an off-label coronary balloon-mounted drug-eluting Onyx Resolute. We actually did a DYNA CT to make sure we got the length right and did not measure length on 2-D. There are only 8 and 12 mm options, no 10 mm. Its fine. Smallest diameter is a 2 mm — larger by almost 1 mm than distal M1. Not ideal. However, we know that the M1 was originally something like 2 mm so should be fine
Post — note how the anterior temporal ostium became a bit narrower — a kind of snowplow effect. Its not a critical vessel and had good collaterals — but stayed open anyway.
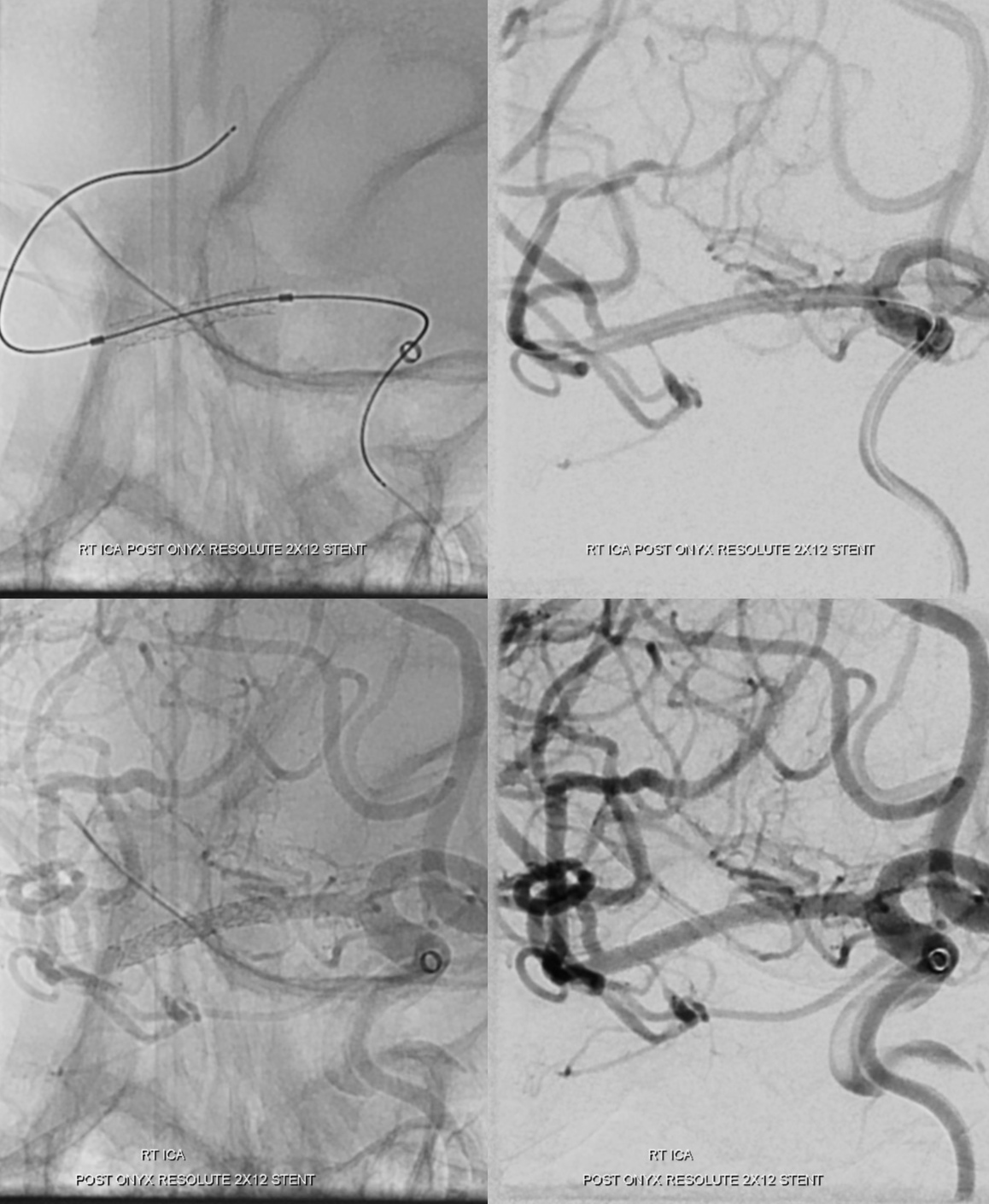
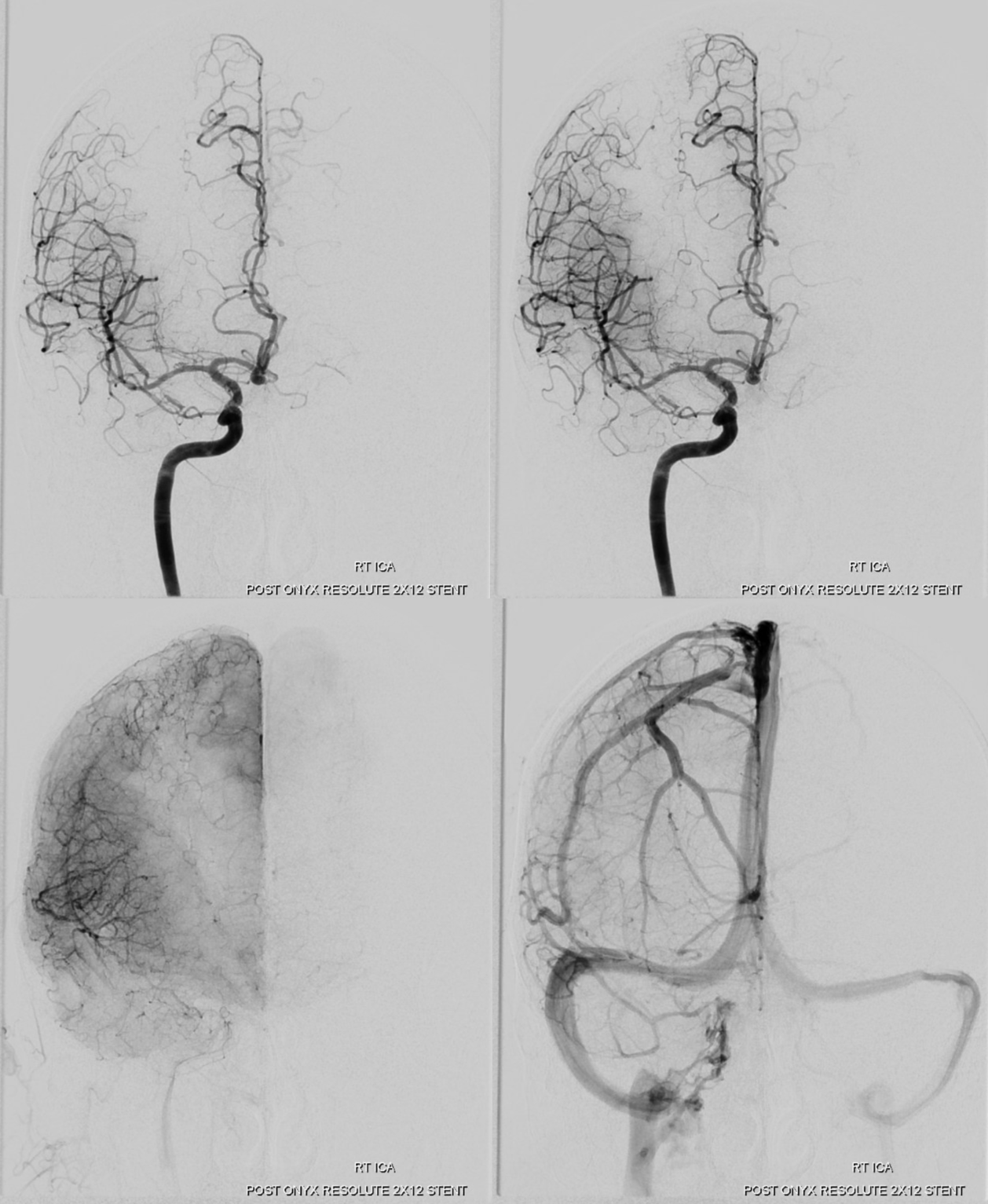
Beautiful lateral venous anatomy. The angular region is supplied by the PCA due to long-term rearrangement of watershed territories.

Some variant ILT anatomy to boot — the marginal tentorial origin is separate from the other three typical branches — anterolateral, rotundum, and meningeal.
This is video of the whole thing
See other stroke case in Case Library
