Case Courtesy Dr. Eytan Raz. Achilles heel illustration concept courtesy Dr. Melanie Walker
The idea of “shunted pouches” — that careful analysis of dural fistulas suggests angioarchitecture to be myriad of arteries converging on one or several openings into a venous pouch in wall of sinus — suggests possibility of superselective embolization with closure of this pouch alone, while preserving rest of sinus. This works very well in low-grade dural fistulas of sigmoid sinus, where the pouch is usually found in wall of the sinus, allowing it to be closed while preserving sinus proper. Numerous examples of this are shown on our Case Library Page, and the anatomical background of these pouches is demonstrated in our Intrinsic Dural Arteries and Intrinsic Dural Veins pages.
Existence of pouches in the cavernous sinus has been illustrated by Kiyosue et al, Goetz Benndorf and others – see Kiyosue’s image below

However, in practice, unlike sigmoid pouches, these are more difficult to both identify and close superselectively. One major caution in trying to do so is “painting yourself into corner” — failure to completely shut down the fistula while loosing access. This is particularly true for the most common posterior cavernous sinus pouch where access is via the inferior petrosal sinus. If access is lost, other transvenous routes might not exist. The direct puncture transorbital route is an excellent alternative in our experience, despite its extreme appearance. Transarterial routes can also be reasonable, however very serious experience and anatomical familiarity are required.
Below is an example of successful superselective cavernous sinus fistula embolization, illustrating practical details of technique.
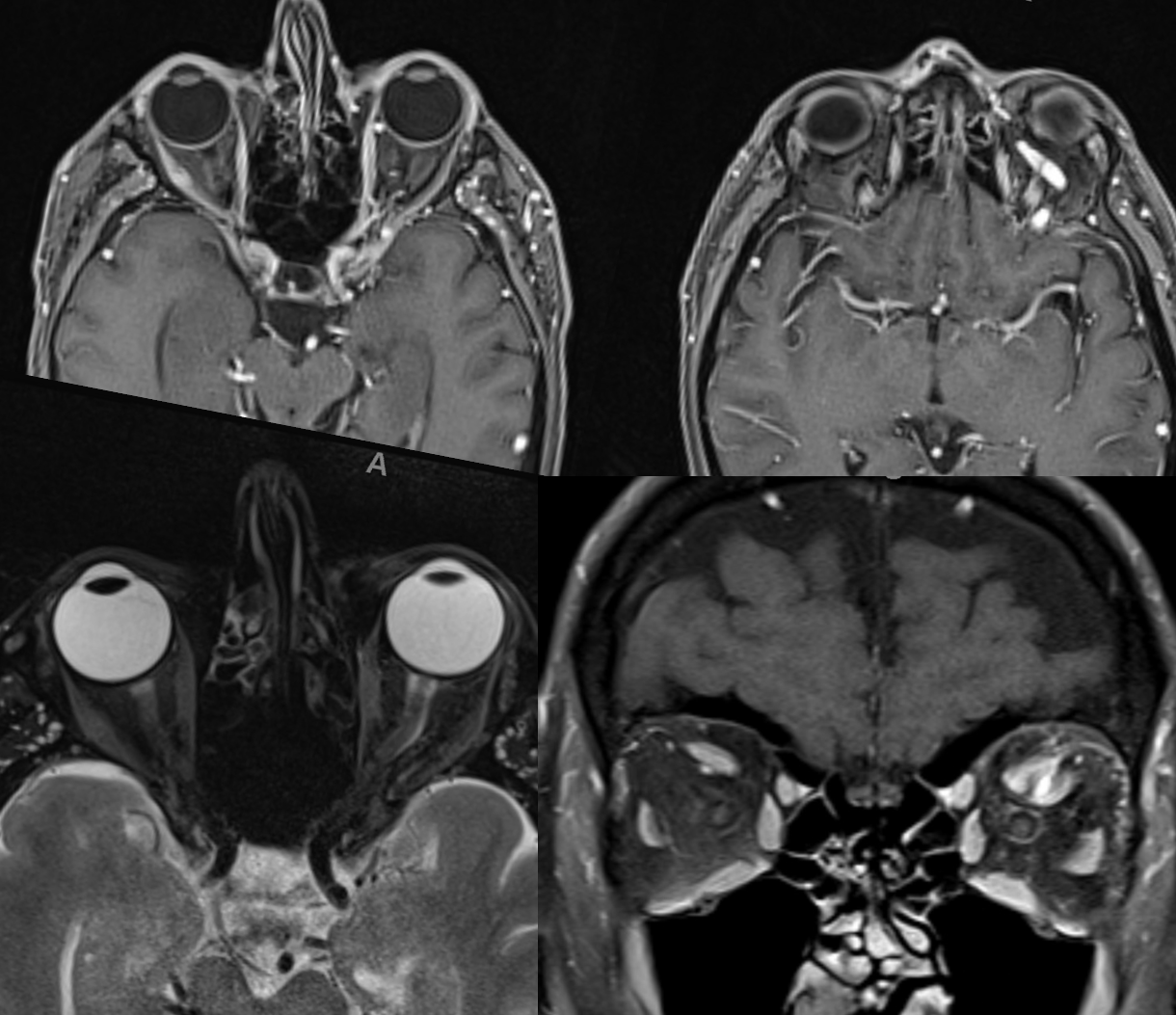
Presentation is typical: left proptosis, chemosis, ophthalmoplegia, early vision loss (color desaturation). Notice swollen left optic nerve, in images below
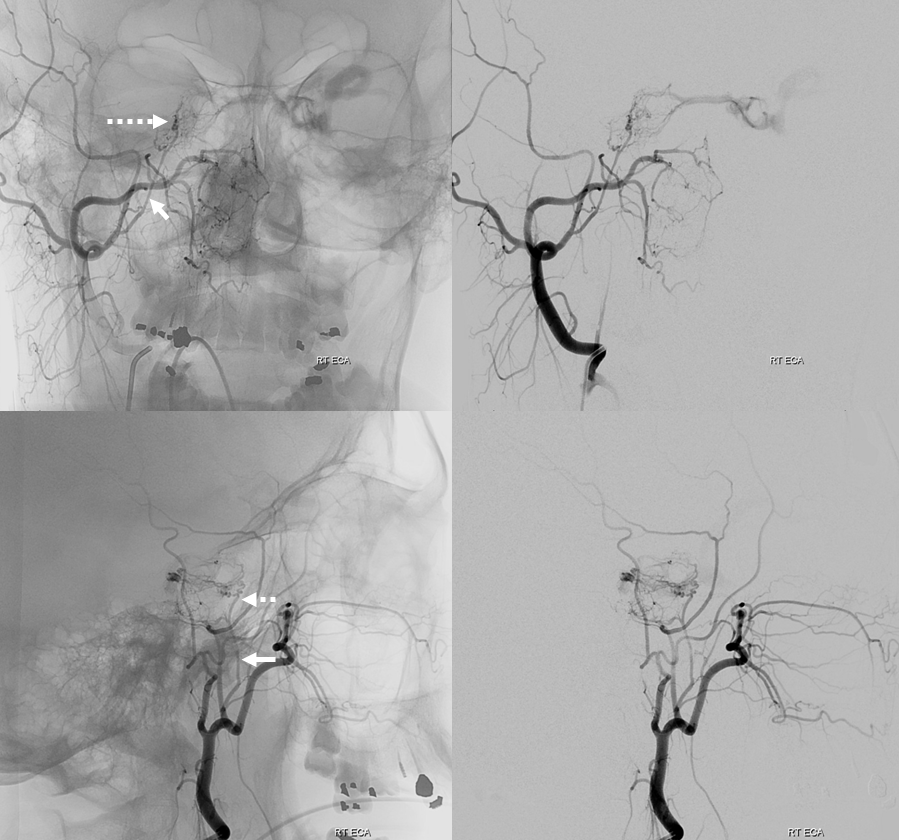
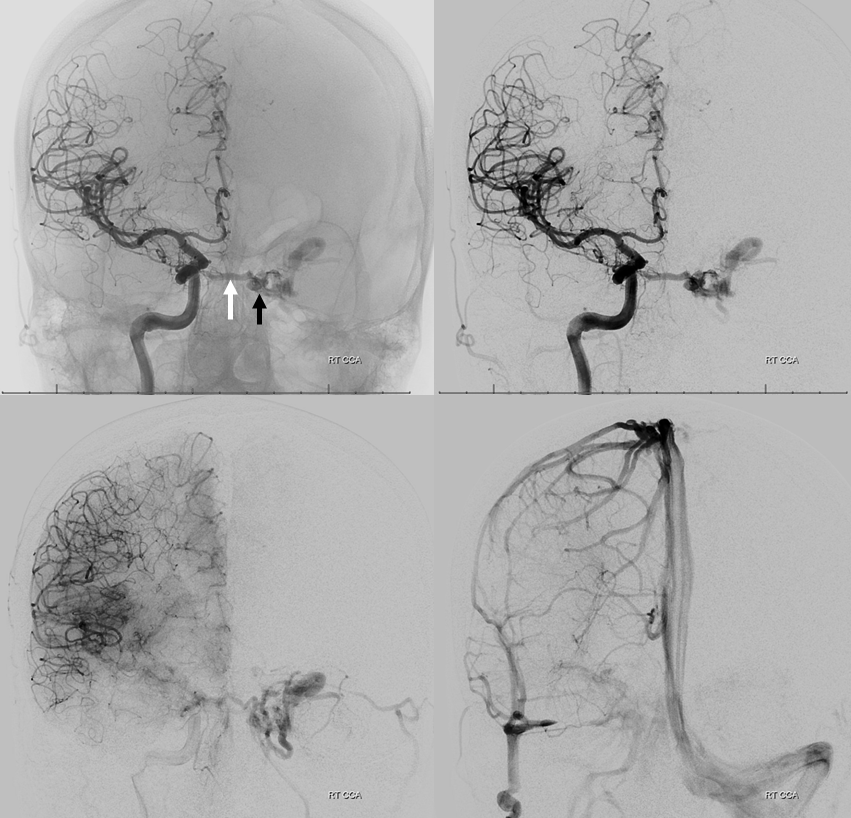
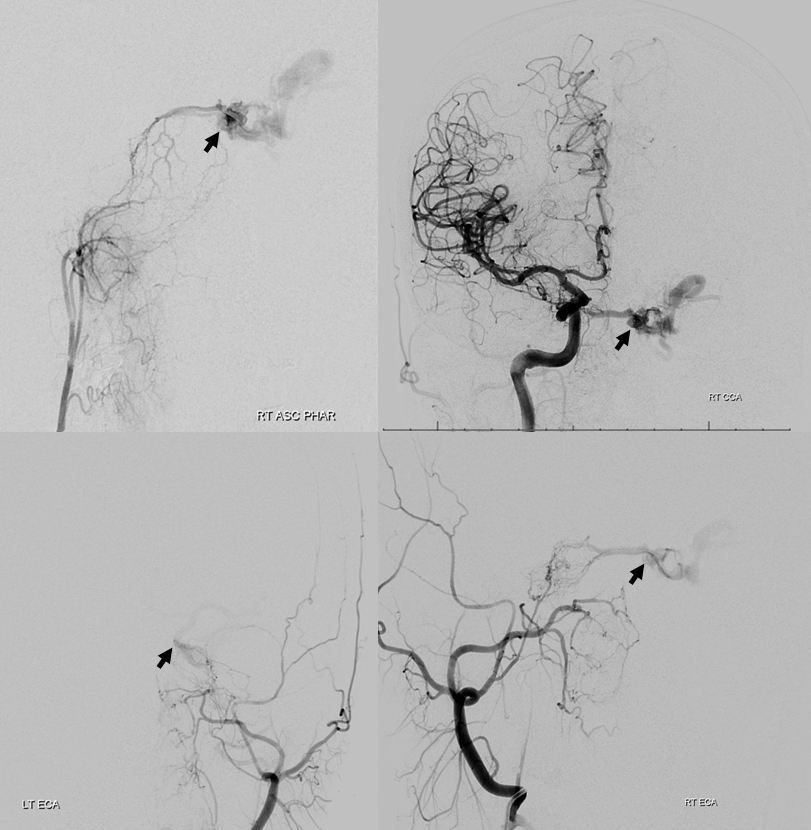
Right ascending pharyngeal injection. Where is fistula? Is it on right side, draining via intercavernous sinus (white arrow) to the left posterior cavernous sinus (black arrow)? Or is the fistula site where black arrow is? Does that mean the structure shown by white arrow is an artery? Or is it a vein “sucking” blood toward the fistula? Are there multiple shunts?
Venous drainage is mainly into the superior ophthalmic vein (SOV) — as expected based on symptoms. Look also at the stump of the inferior ophthalmic vein in the lateral view — not labeled — that’s a perfect target for transorbital approach, if needed.
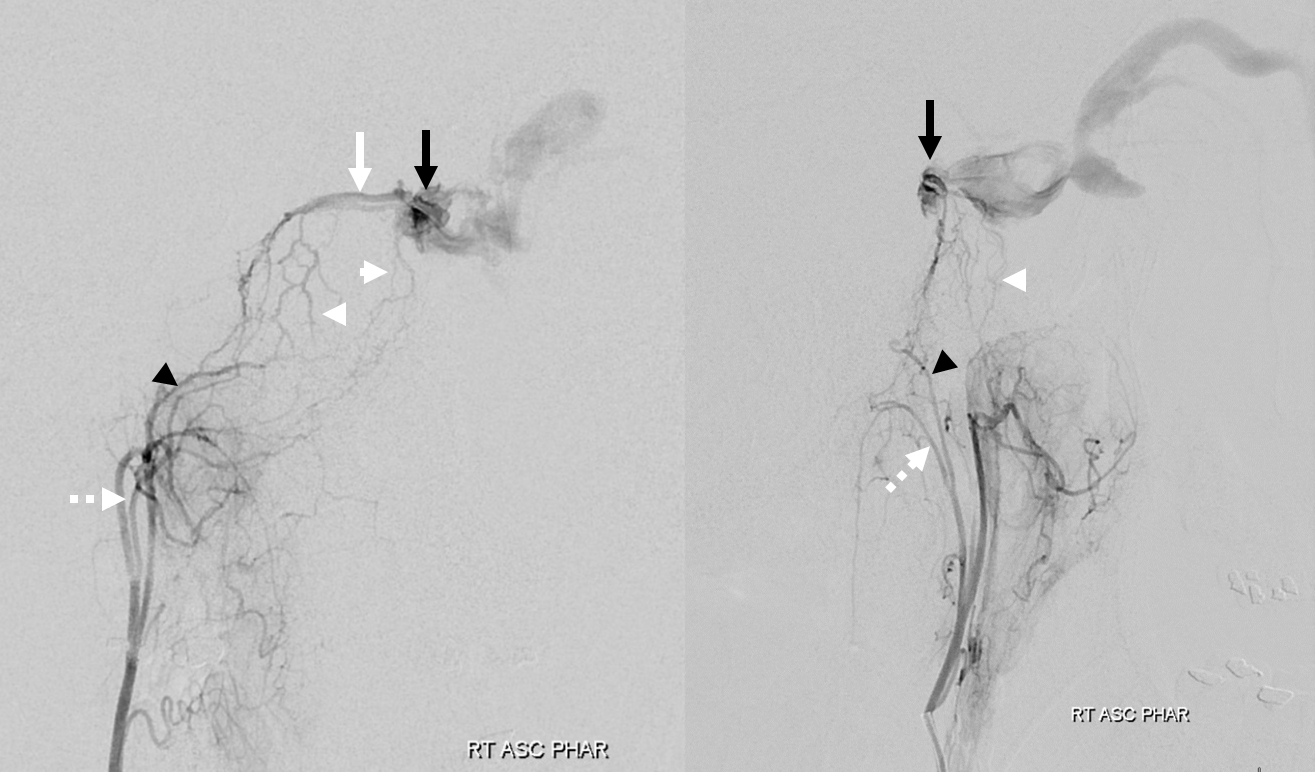
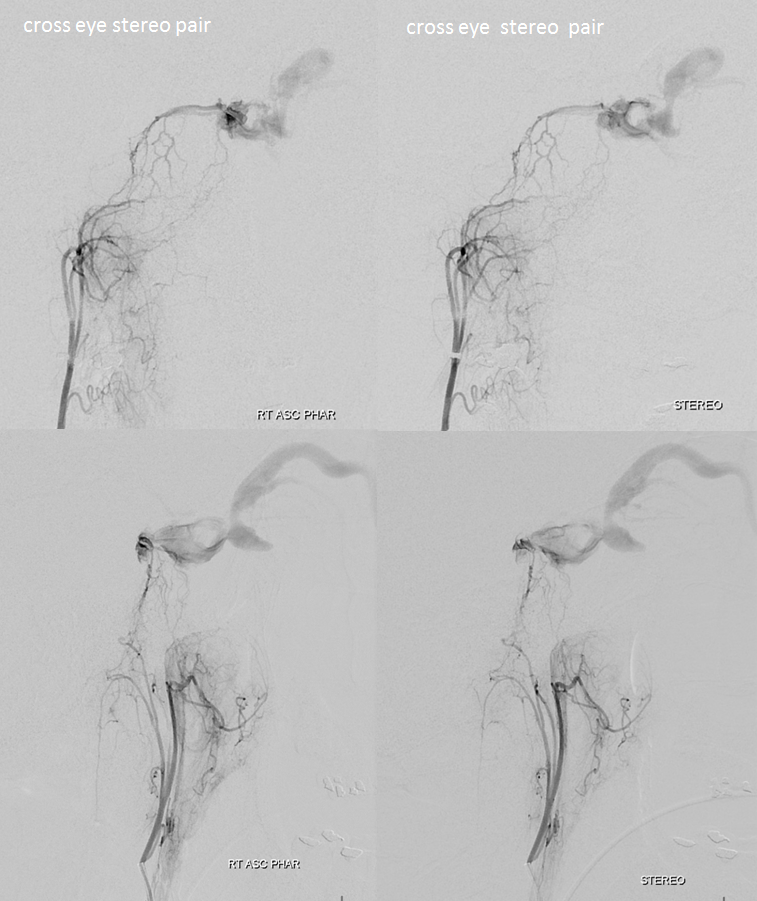
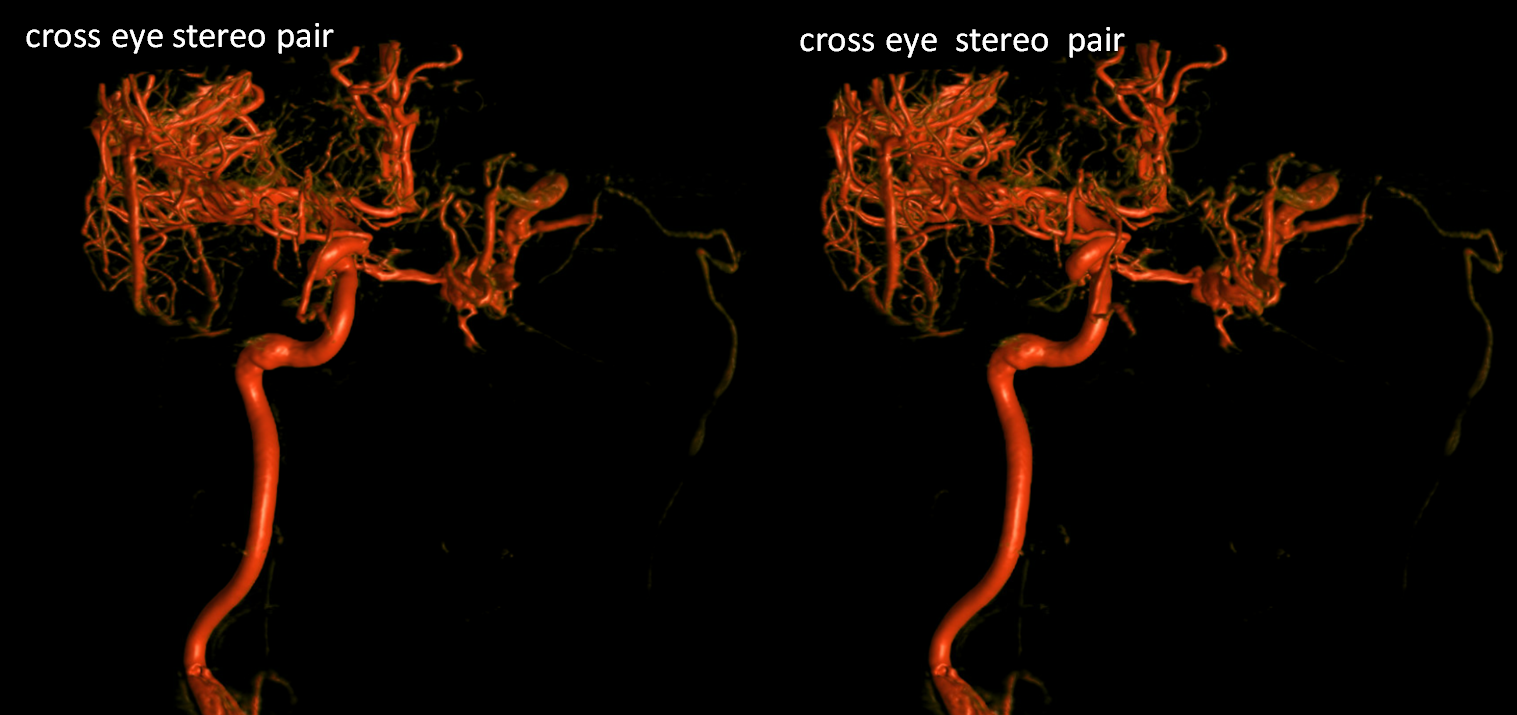
Stereo views
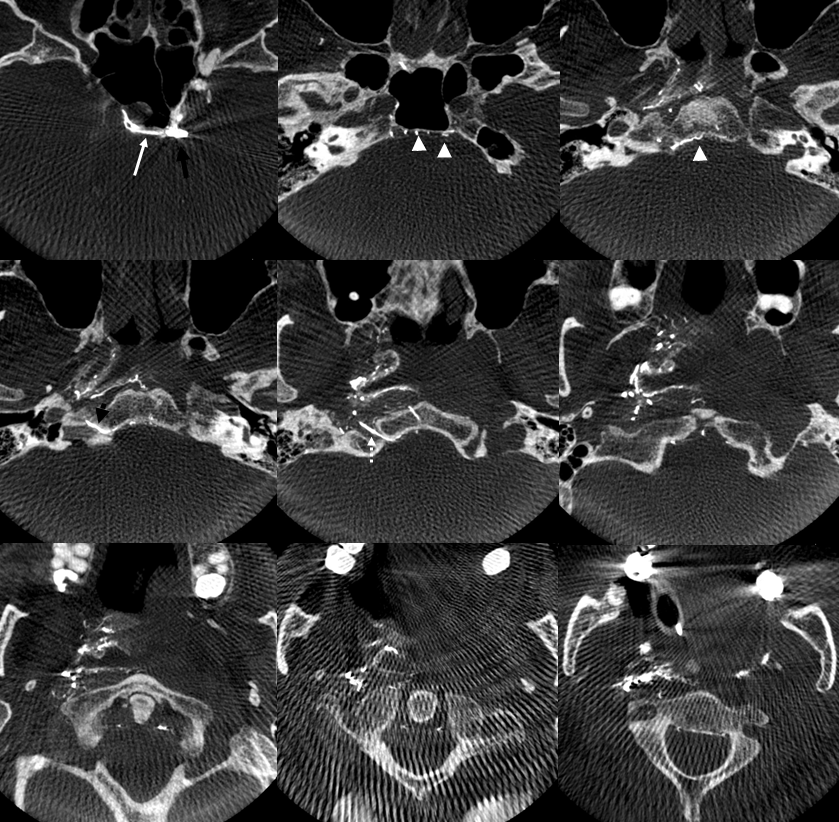
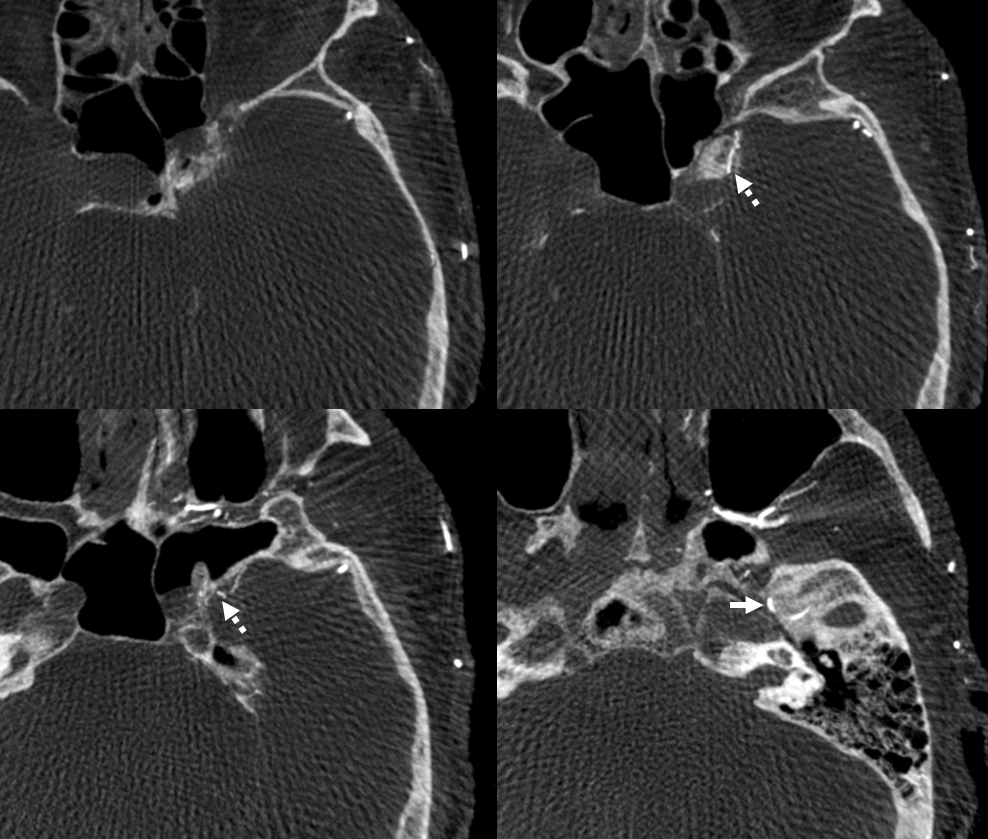
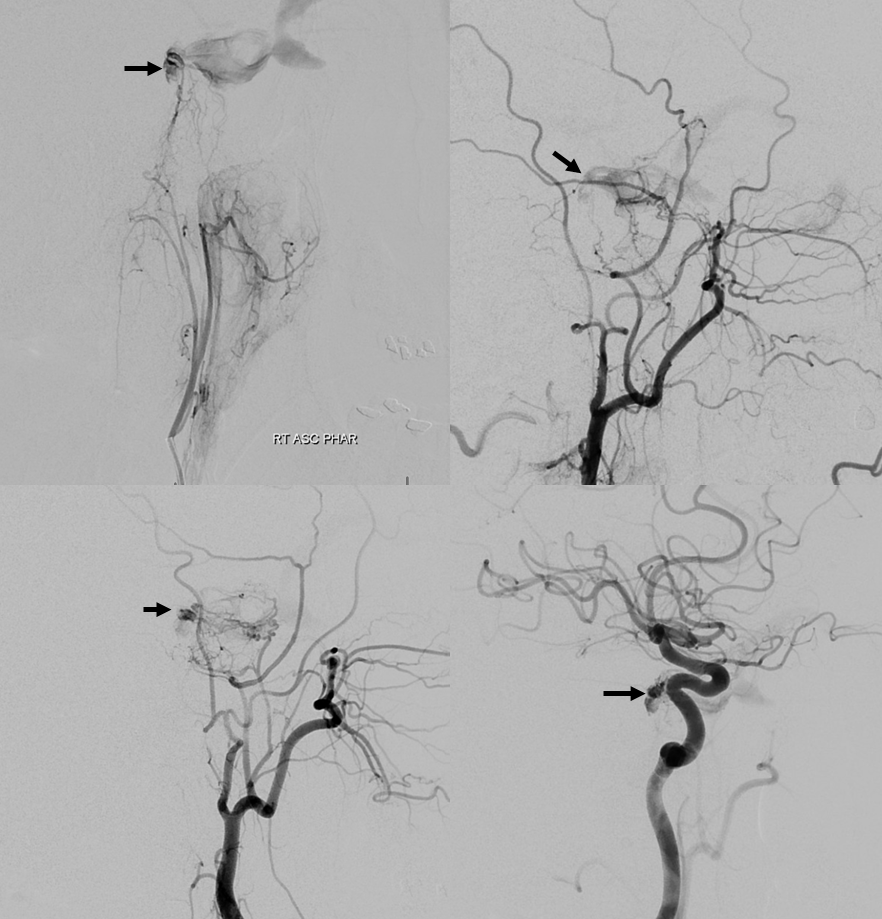
DYNA CTs — same arrows. Notice that there is a very large transosseous branch (black arrowhead in all images) present. It is a relatively good transarterial embo route — of course a myriad arterial-arterial dangerous anastomoses remain. This transosseous should not be misinterpreted as either jugular or hypoglossal branch in DSA images. The hypoglossal branch (dashed white arrow) gives classic connections to the odontoid arcade
Right ECA injection — the main supplier to fistula is the accessory meningeal artery (white arrow), with its cavernous branches (dashed arrow) coming up via the cavernous / Meckel cave region to reach the same point as the ascending pharyngeal artery. Still the same question — is the fistula on right or left side? Are there multiple fistulas?
DYNAs — nicely showing cavernous branches of the accessory meningeal. These are NOT good routes for transarterial embo
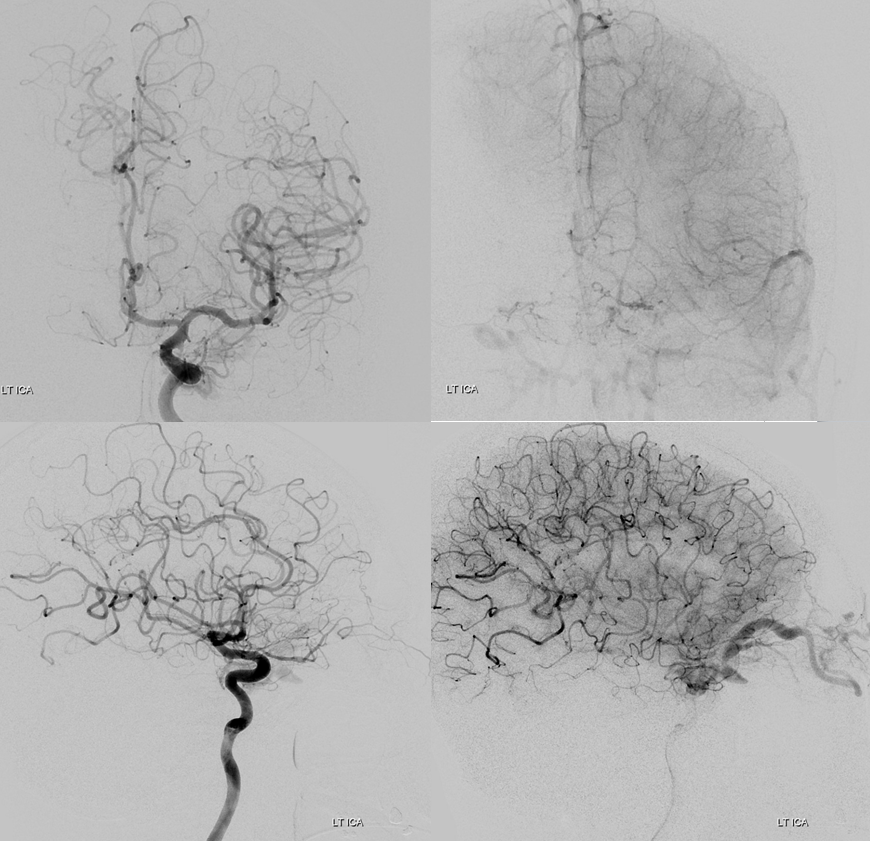
Left ICA — very little supply to the fistula. Notice that SOV outflow is not efficient — there is no ready visualization of angular veins for example. This is part of the reason the patient is so symptomatic.
Left ECA — mostly accessory meningeal supply via cavernous branches, with minor contribution from artery of foramen rotundum (arrowhead)
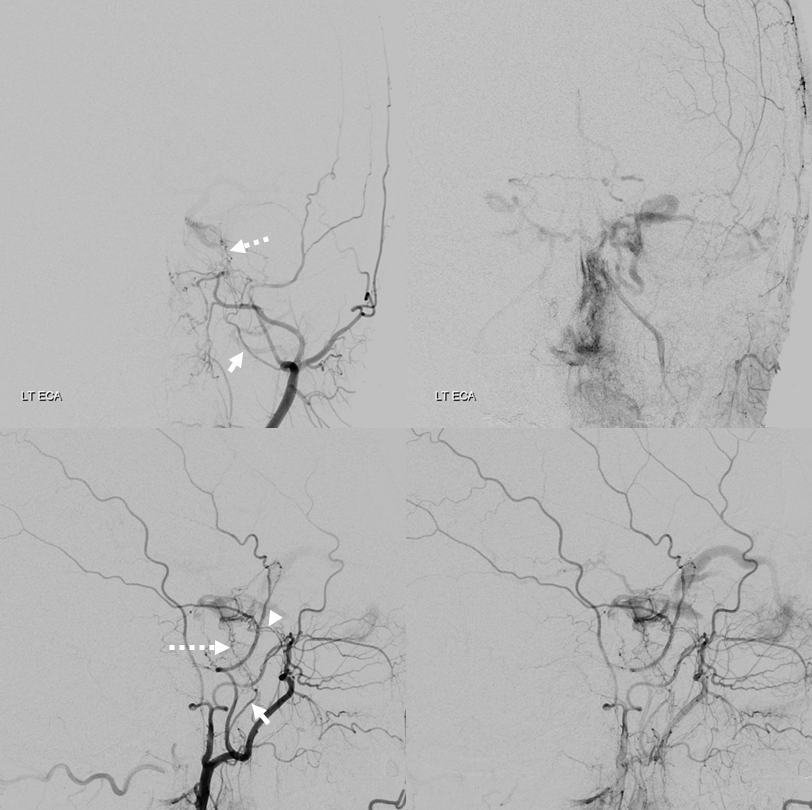
DYNA
Finally, right ICA injection. Contribution is via MHT. Again note lack of efficient SOV outflow
VRs
So, what do we think? Summary of supply, frontal views.
Lateral views
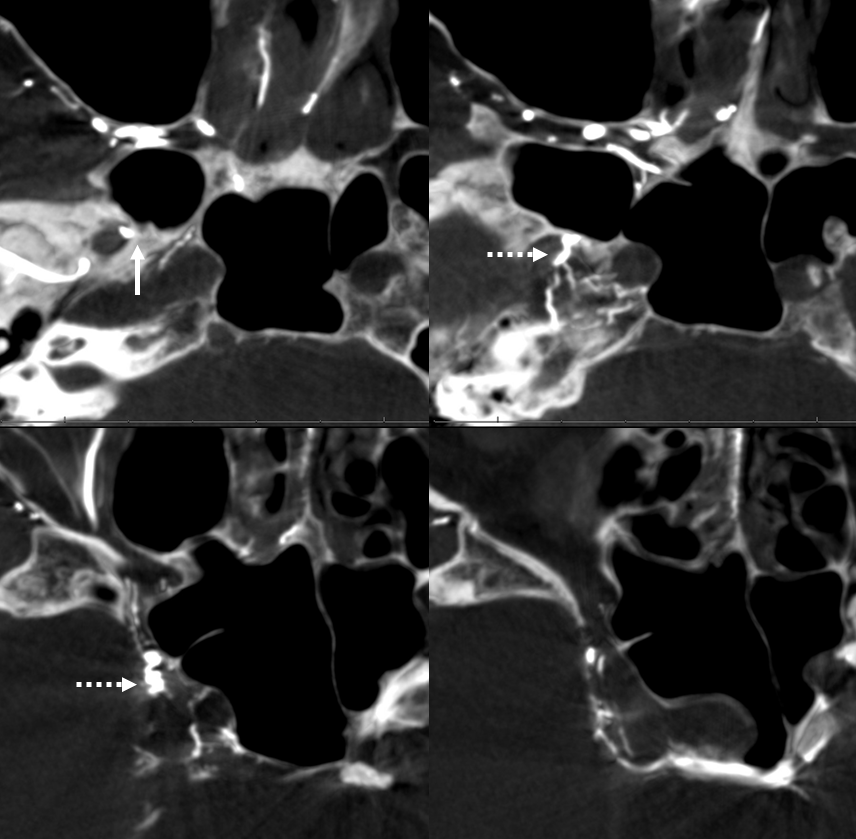
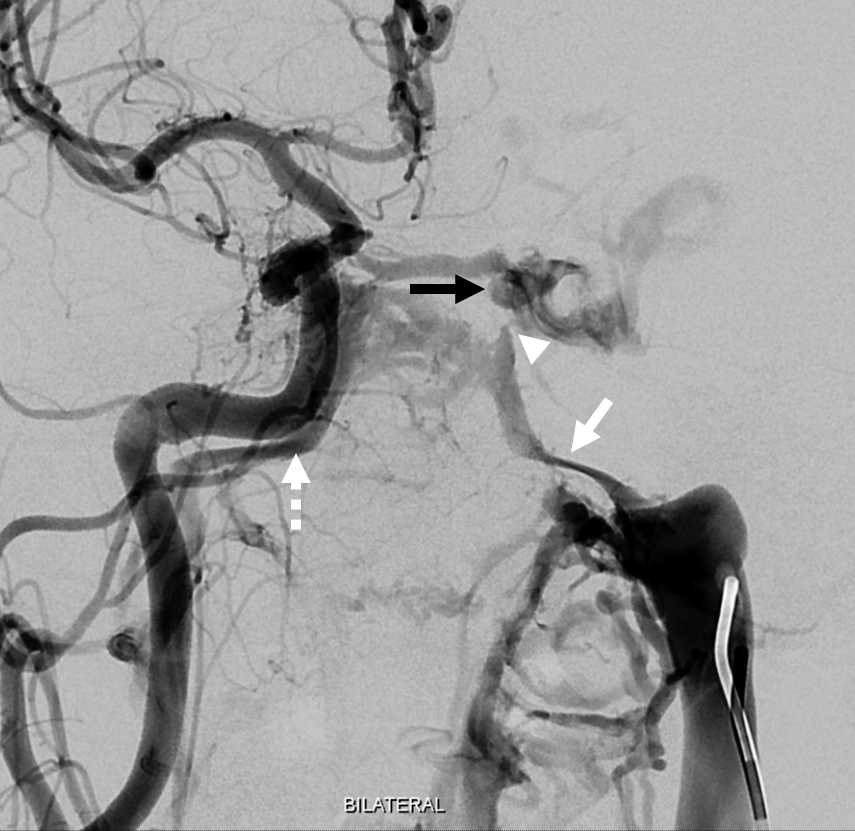
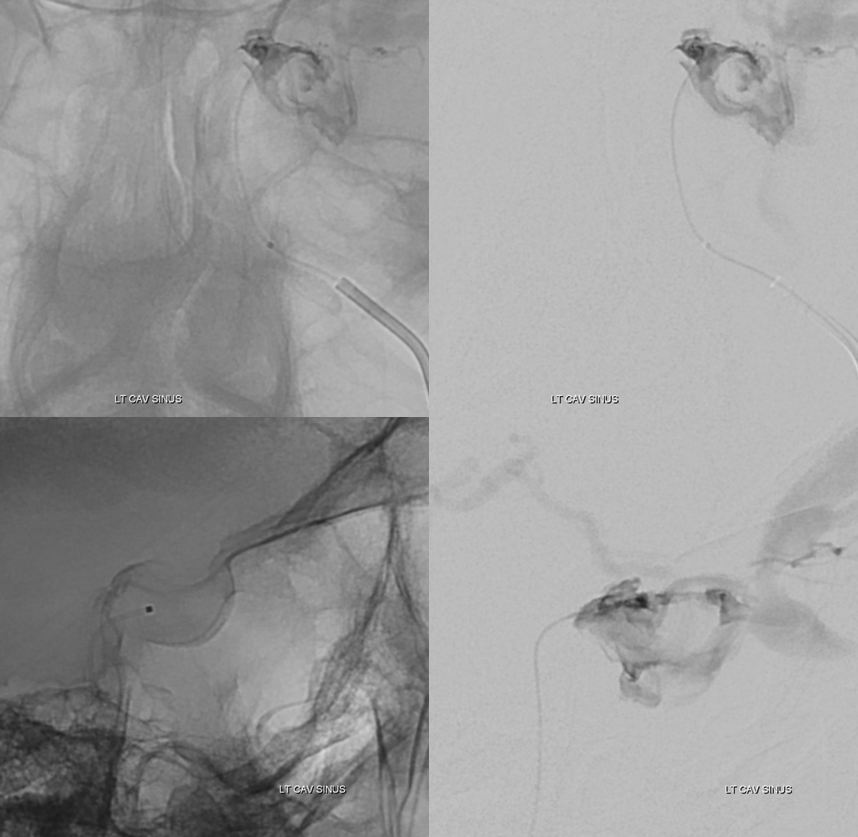
Treatment — a 5F vert is in the left IJ (right IJ is absent btw). The left inferior petrosal sinus (white arrow) and right (dashed arrow) are opacified via the venous left IJ injection. A simultaneous inject of right CCA shows the fistula, with a possible small connection between the fistula region and the left IPS (arrowhead)
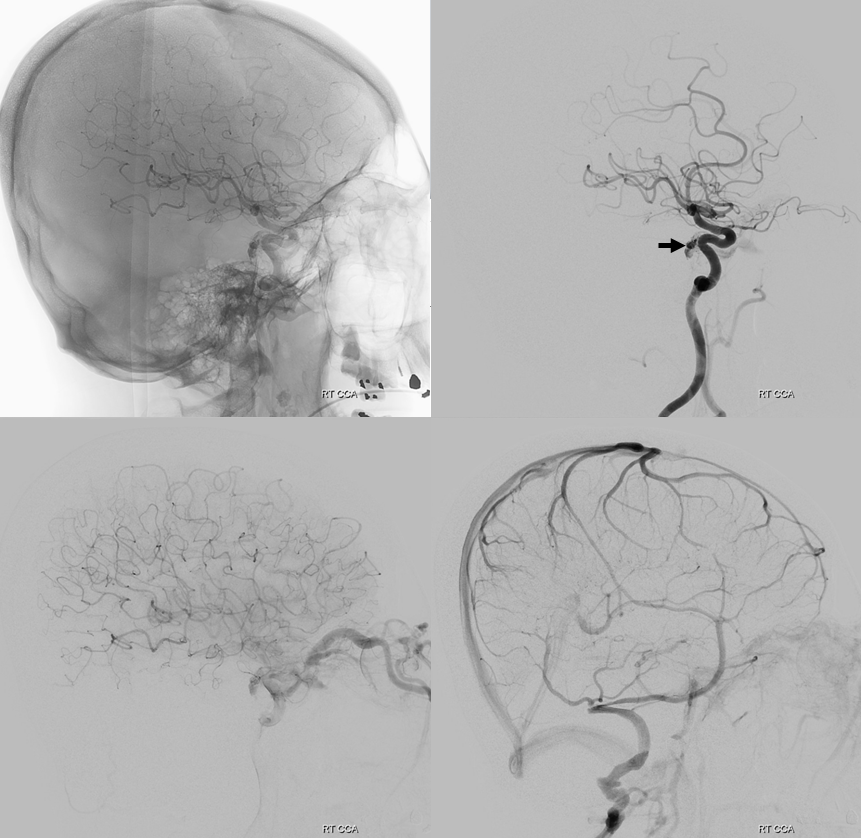
After some manipulation, an SL-10 can be brought up into the general vicinity of the fistula

Injection through the SL-10 shows the same structures we saw from arterial side. We are close — but not there yet. Coiling here is a mistake — we are not in the fistula pouch – just proximal to it (a bit below in lateral views). Coiling here will be a mistake — we will coil off our only decent transvenous access without closing the fistula. A glue or onyx shot is possible, but we want to be more sure.

Some more work with a bit of luck — and we are in the horizontal posteromedial cavernous sinus.

Now, we can do one of two things — either take catheter to origin of SOV and coil off the entire sinus from there — the classic route. Effective but inelegant, and costs a fortune in detachable coils — which is a problem for much of the world. We didn’t feel we could bring a larger catheter inside the sinus to use pushable or longer detachable coils. We were correct in that assumption, as we soon found out.
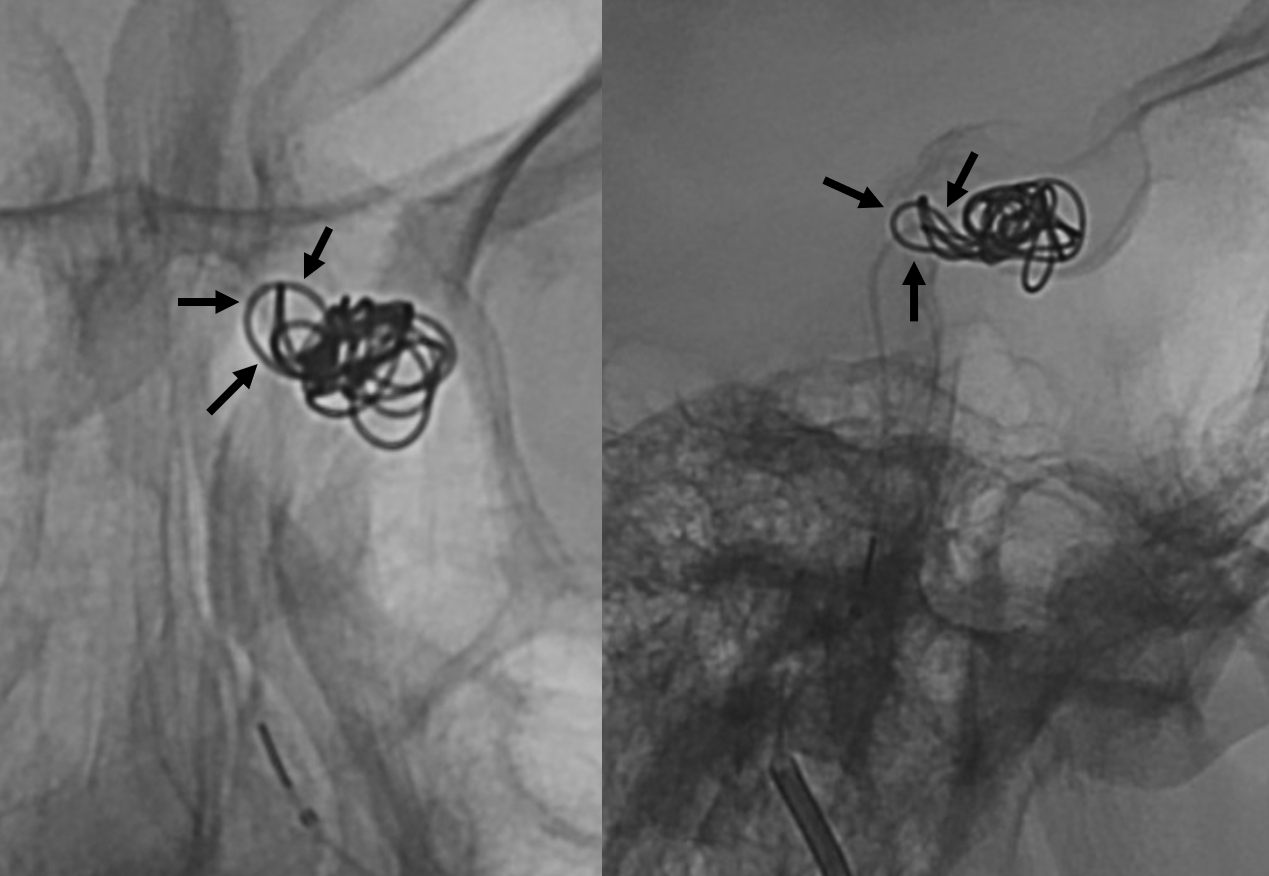
The other option is to use our anatomical understanding — knowing that the fistula is limited to the left posteromedial cavernous sinus (black arrows in all of above images — and image below), we can see if coils can be placed more selectively. So we did, placing a single 6×20 Target 3D XL. Even here, the majority of coil is not “superselective” — three loops however went into the fistula pouch (black arrows). We could not catheterize the pouch from our position, and used the other loops to help push those 3 into the pocket. Took a few repositioning tries to do it.
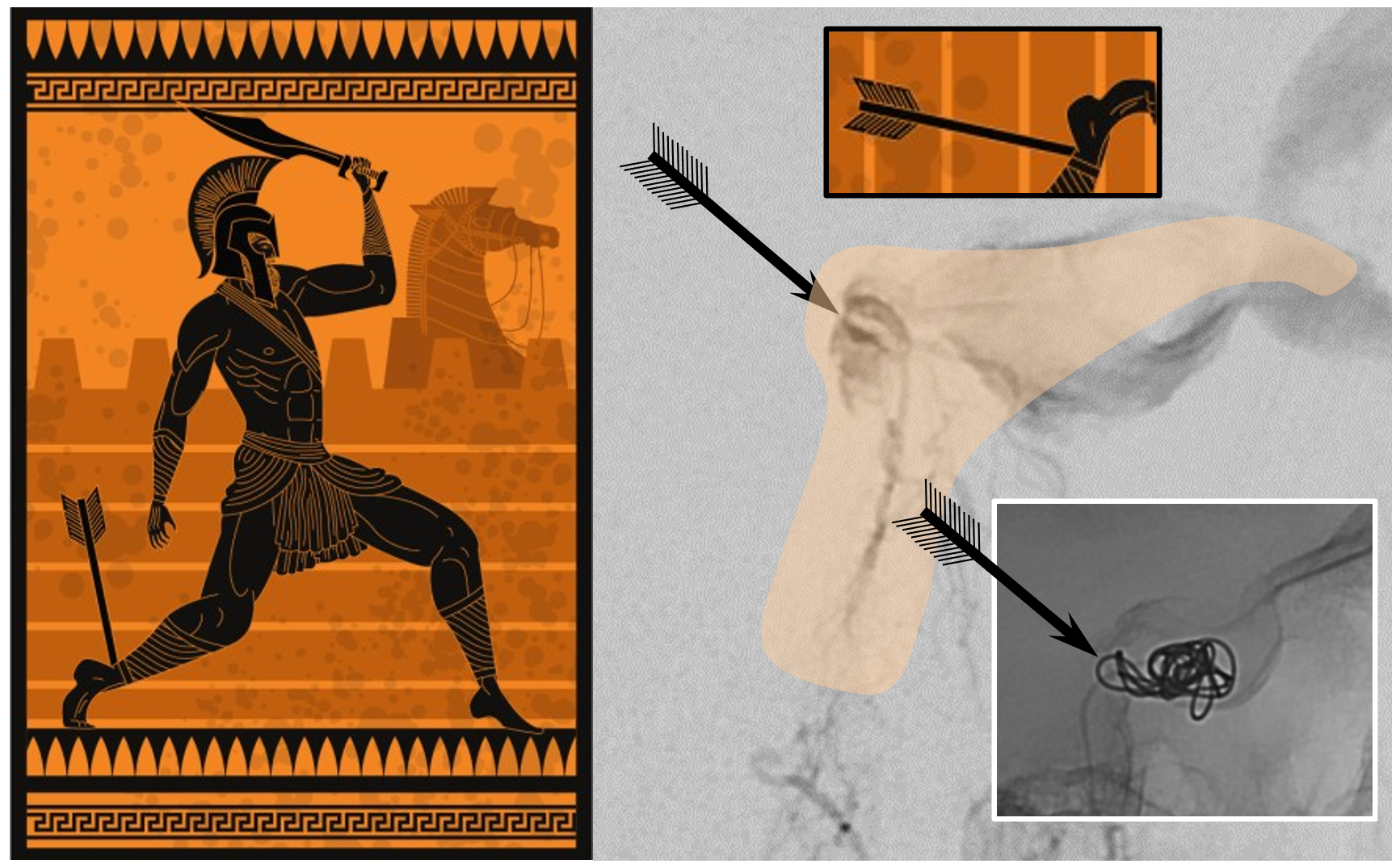
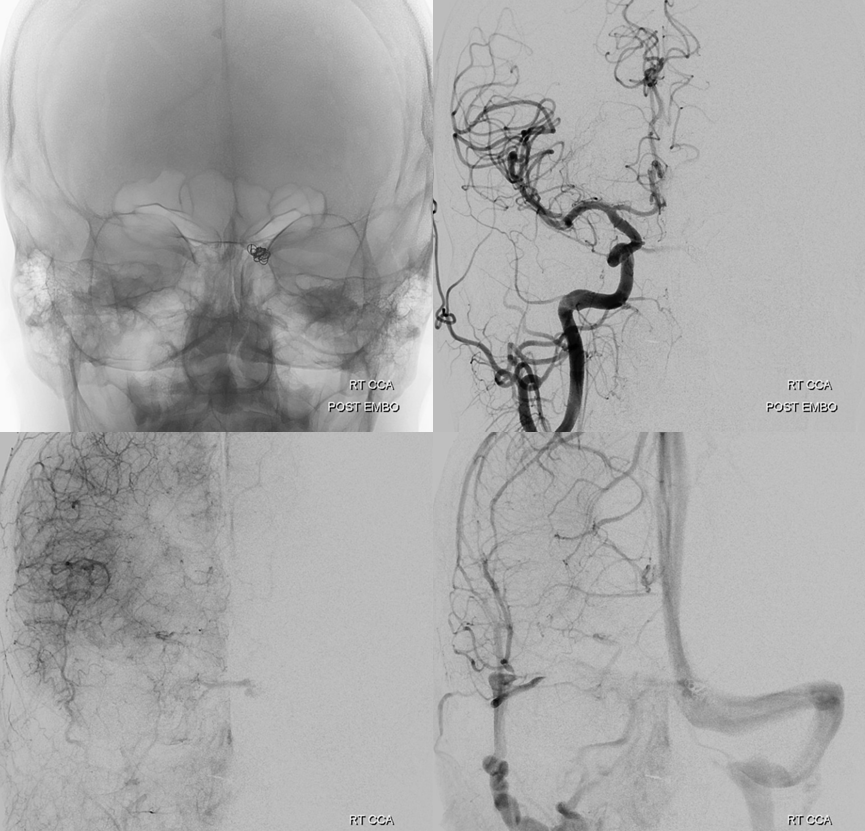
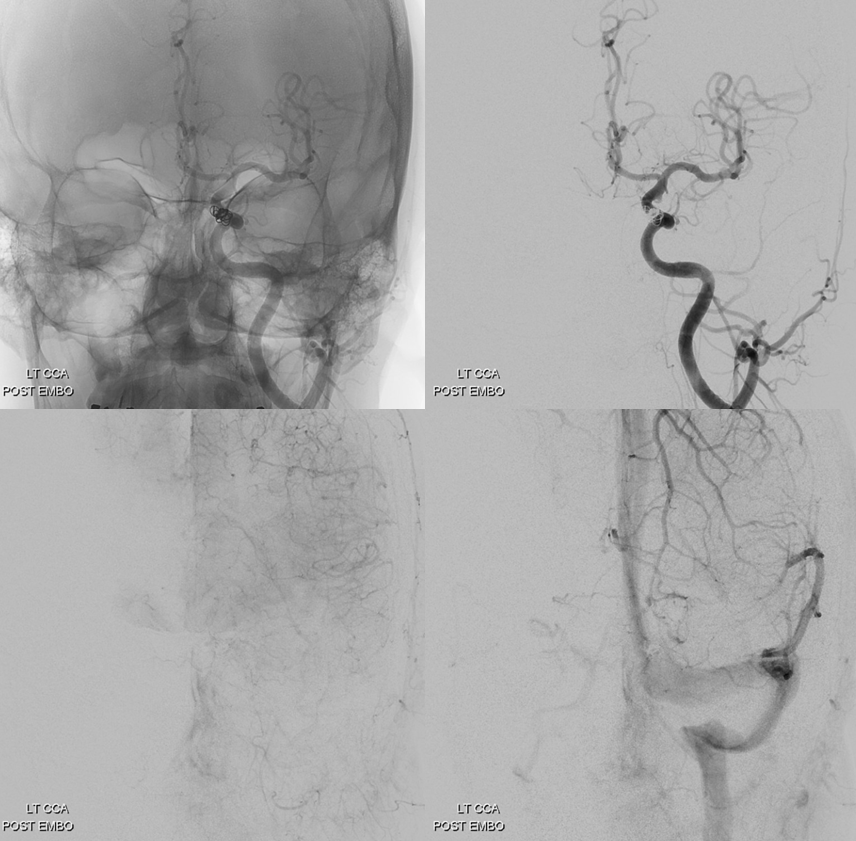
The immediate post was not encouraging. However, here we use something that is rarely utilized in transvenous fistula coiling business — time. Fistulas are very vulnerable to targeted attack from venous side. This is their Achilles heel. Put one coil where you think the heel is, wait a bit, and see. After 15 min, the fistula is gone — the only “one and done” that makes any sense.
We tried to put in one more coil — for good measure. However, it was an ultra-soft type, and we lost catheter position and could not get back in over this flimsy coil. The fistulas stayed closed.
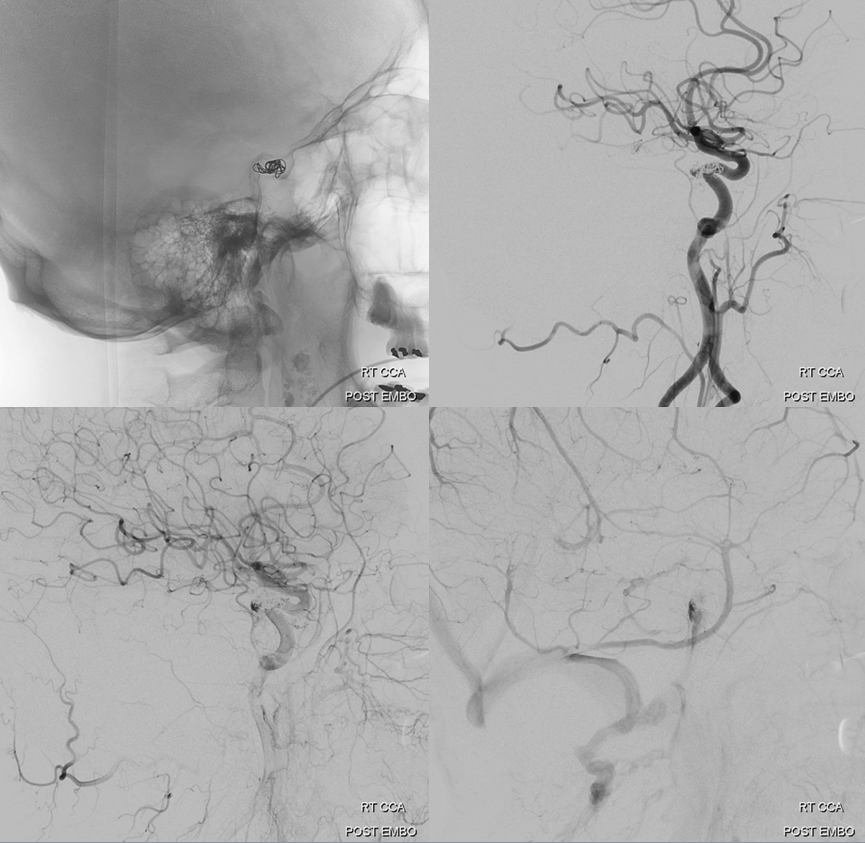
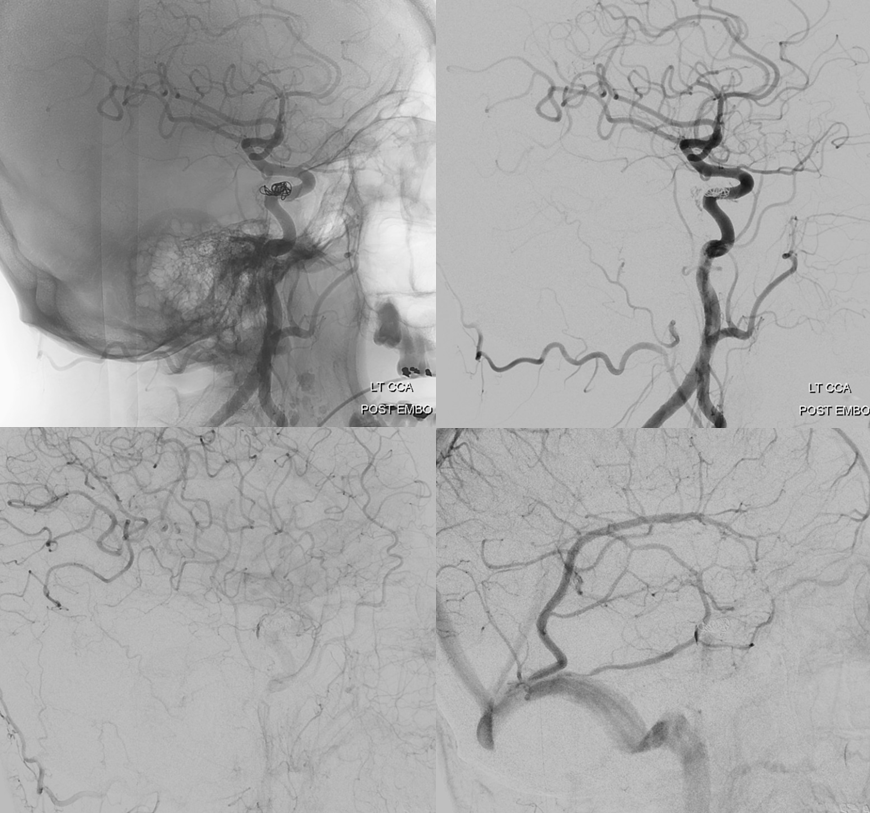
Is it worth trying to go superselective instead of going the sledgehammer route and coiling off the whole sinus? The sinus will thrombose anyway, at least for short term. Later on, though, who knows — perhaps it will become a useful drainage route again. Or the fistula will come back? We will see — so far we have not seen one return once closed completely via the superselective venous route.
Conclusions: Anatomical understanding is essential in knowing where fistula is. It is not complicated. Find one area where everything goes. All tributaries are arteries — there is no “suction” or any other magical concept. Its simple flow from higher pressure arteries to lower pressure vein, that’s all. Once you know where problem is, the venous pouch is the Achilles heel.
