While the main determinant of spinal dural fistula embolization efficacy is the ability to close the “foot” of the vein, safety is dictated by avoidance of inadvertently introducing liquid embolic into arteries supplying the spinal cord — anterior or posterior ones. Traditionally, embolization at the same level as anterior spinal artery is not done, and patient is referred to surgery. Increasingly, this is also the pattern for fistulas with adjacent level spinal arteries. Certainly this is safe and surgery, in experienced hands, is highly effective. Nevertheless, it is still surgery, and non-neurologic morbidity (infection, leaks) is there. There is no absolute reason why embolization cannot be done with adjacent level spinal arteries (see case here) or, under exceptional anatomic and clinical circumstances, for same-level fistulas (case here).
Below is an example of embolization with both anterior and posterior spinal arteries arising from contralateral segmental level.
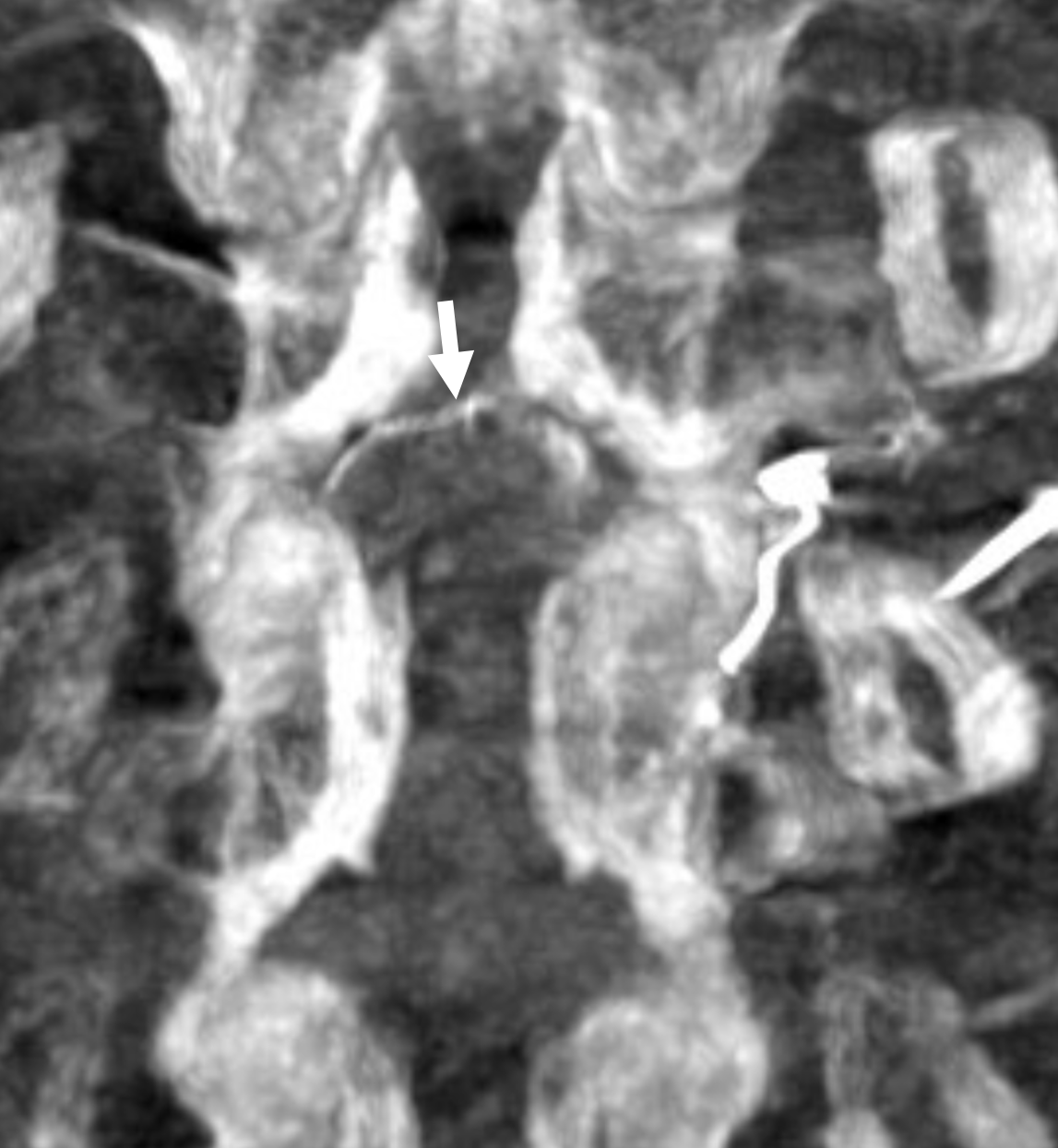
Typical MRI

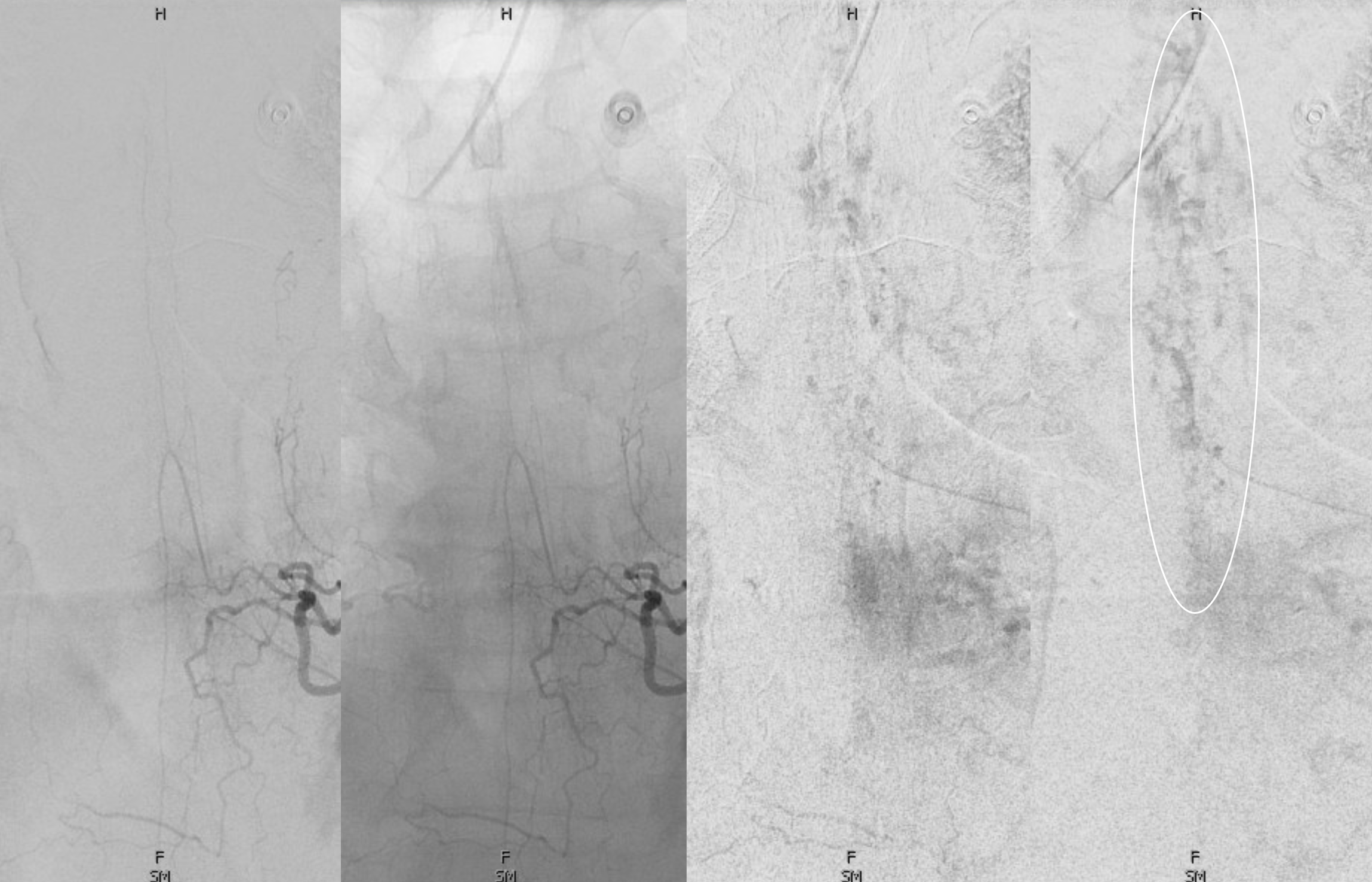
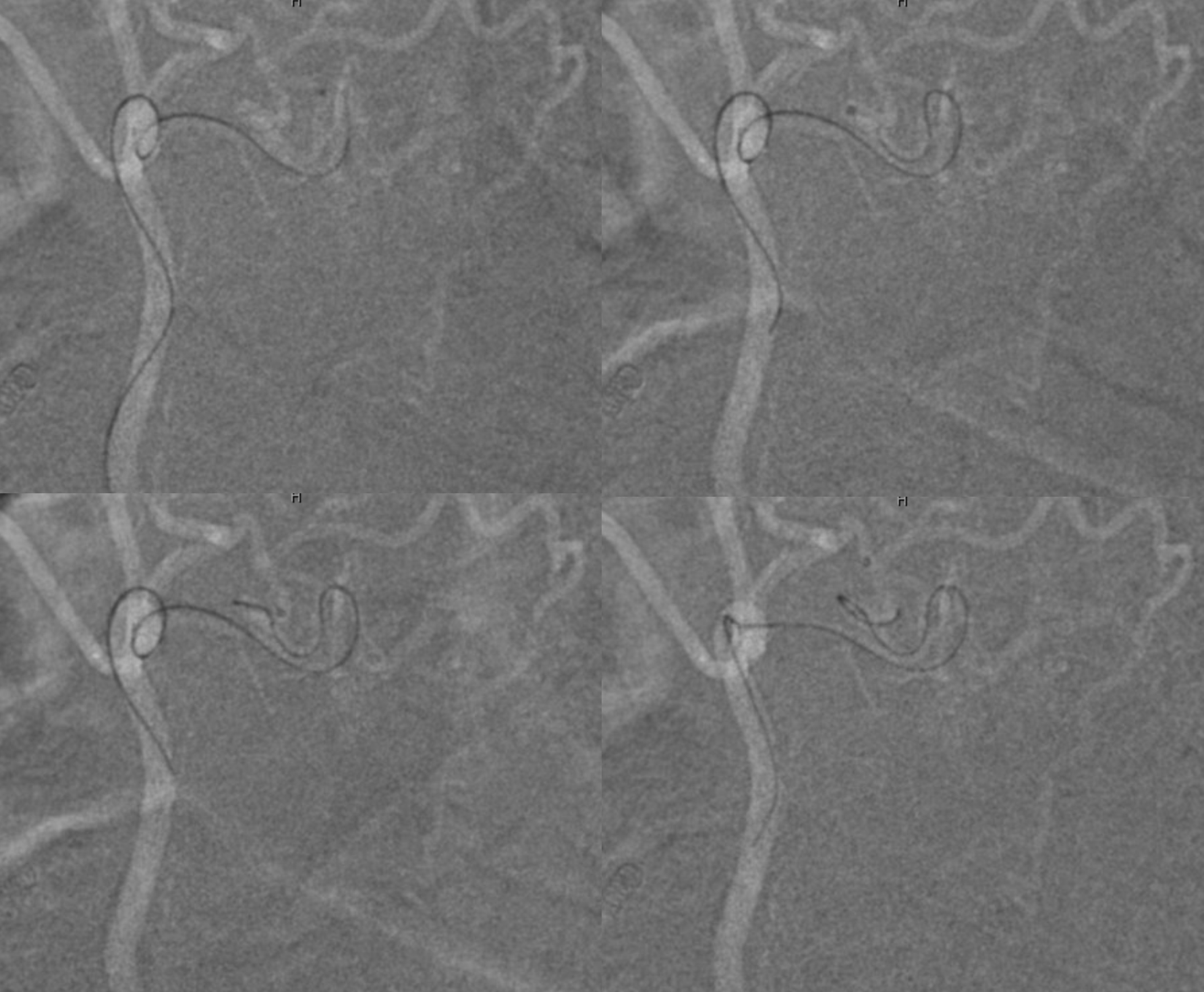
“Radiculomedullopial” artery — supply to both anterior and posterior spinal systems — from left T6. Note lack of cord venous phase — attesting to venous congestion
Fistula is across — at right T6
Magnified views show communication with the right T5 level via lateral dural arcade (arrow)
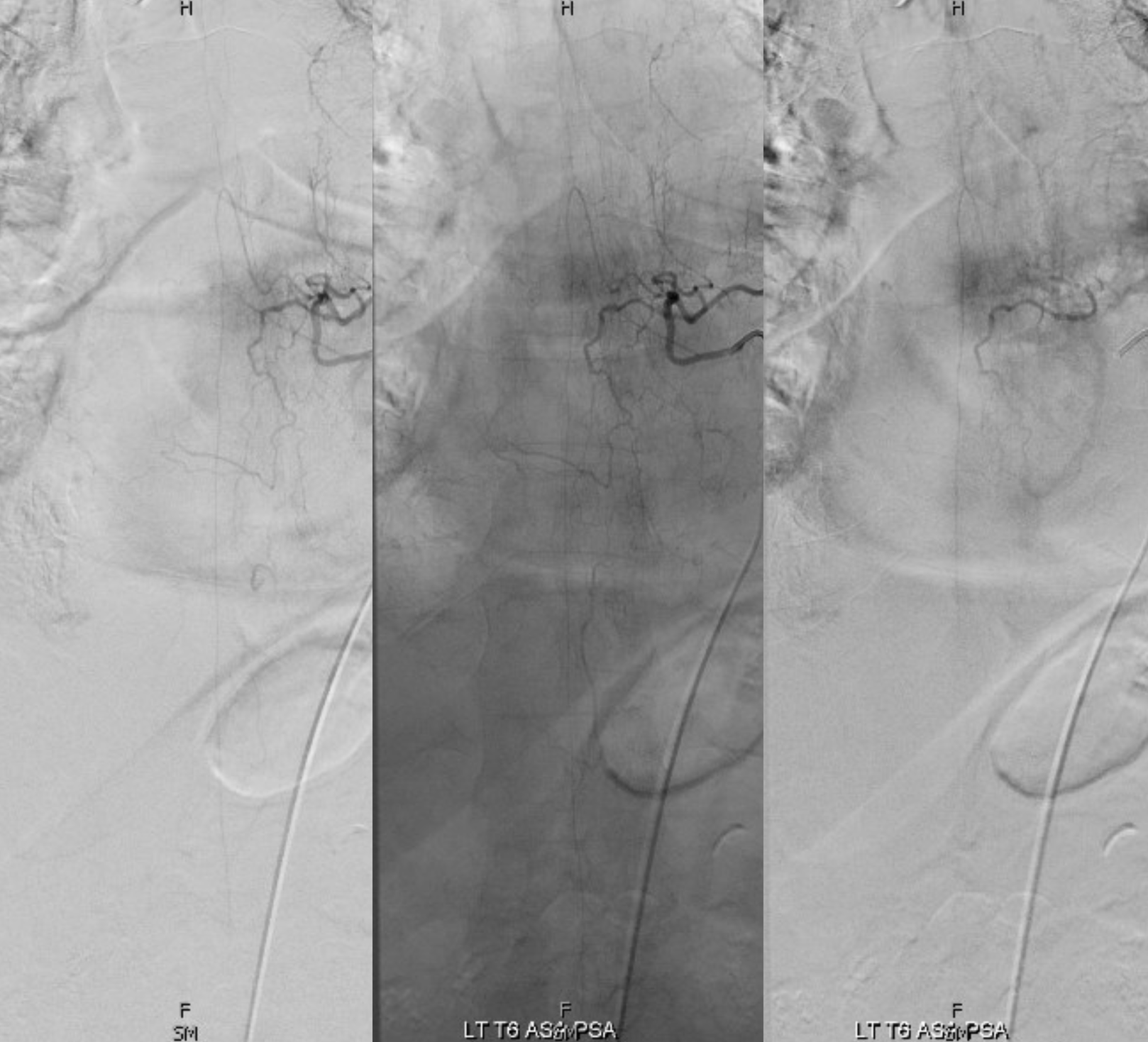
The only other adjacent contributor we can see is from right T4 to a large right posterior spinal artery (they can be quite large in thoracic region)

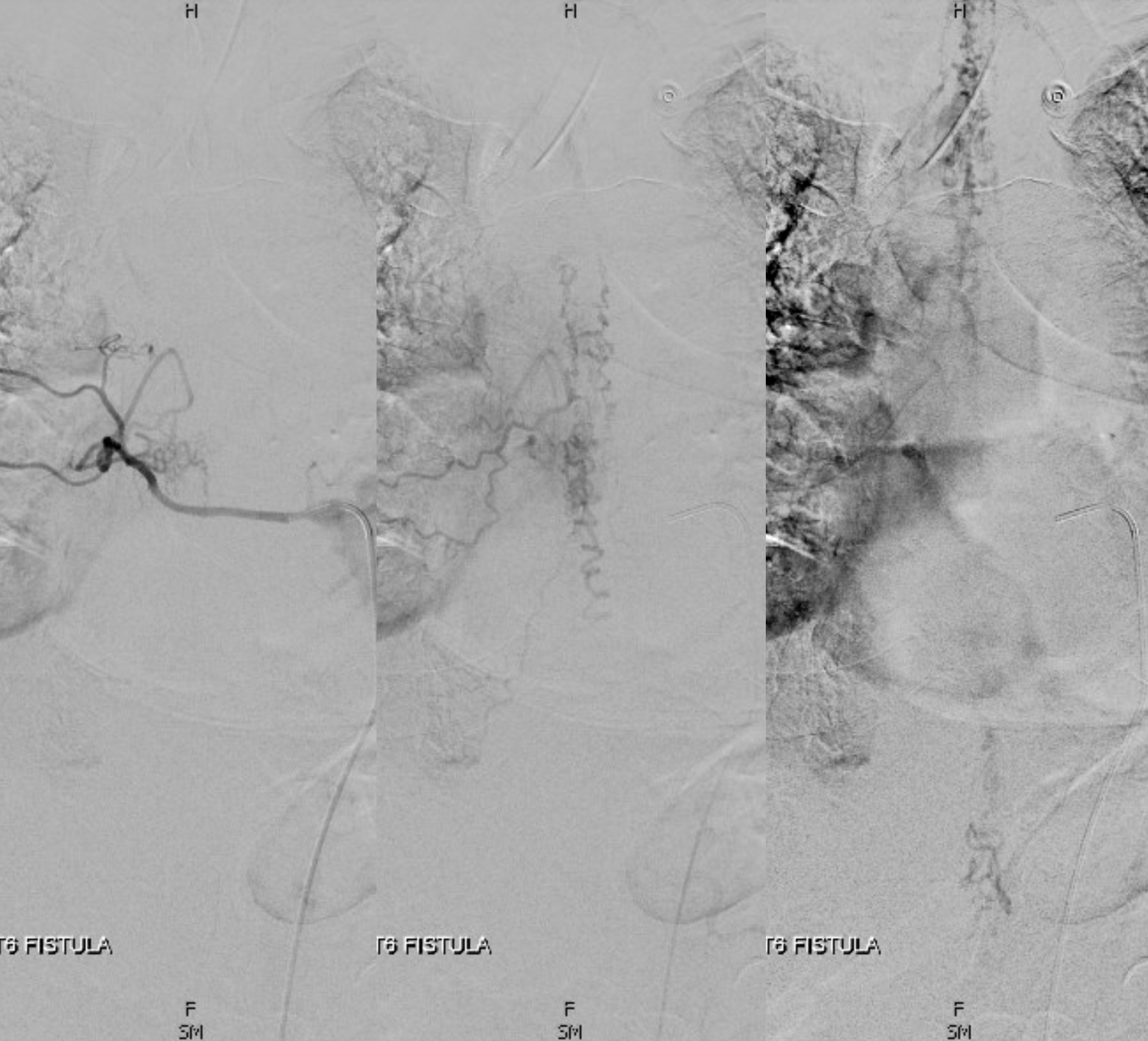
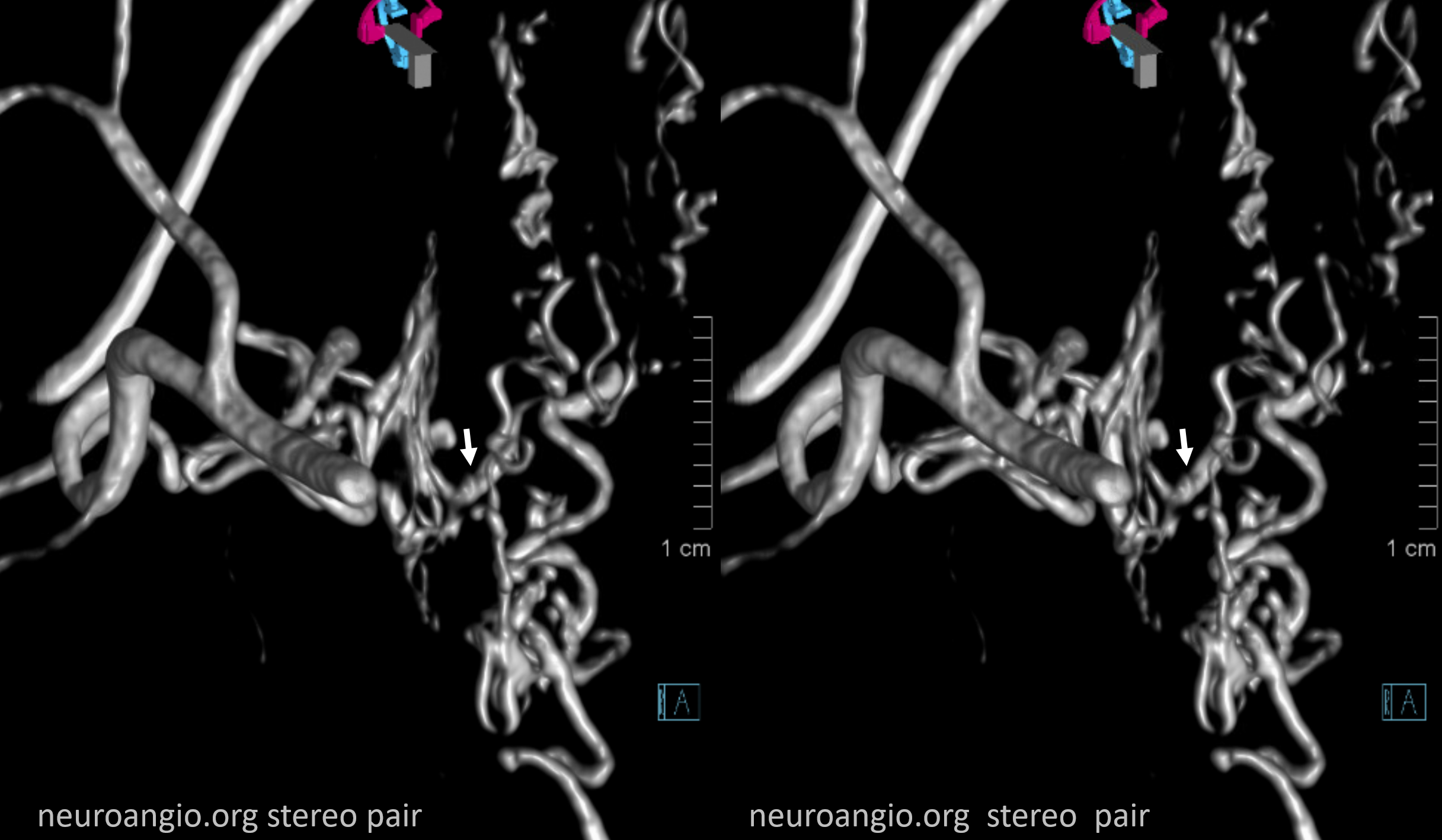
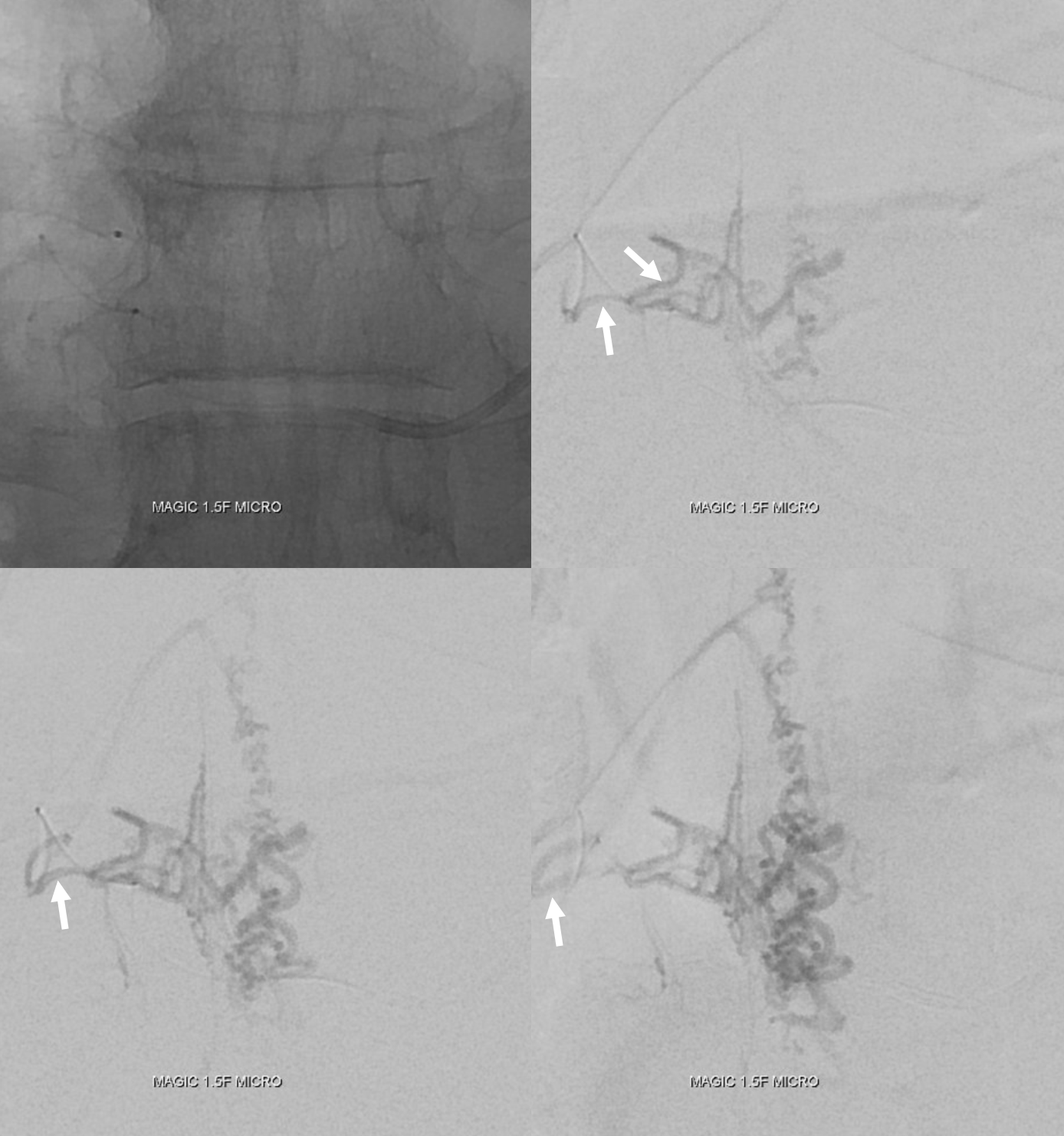
Cone beam (DYNA CT) can be extremely useful in establishing microarchitecture of the fistula (arrows point to “foot” of the radicular vein. This is the point that should be reached by liquid embolic for treatment to work
Movie
Coronal MIPs of radiculomedullopial left T6 DYNA CT
Detailed view points to DORSAL (POSTERIOR) epidural arcade connecting left and right sides (not the usual ventral epidural arcade).
Choice is Magic 1.5F and Hybrid .08
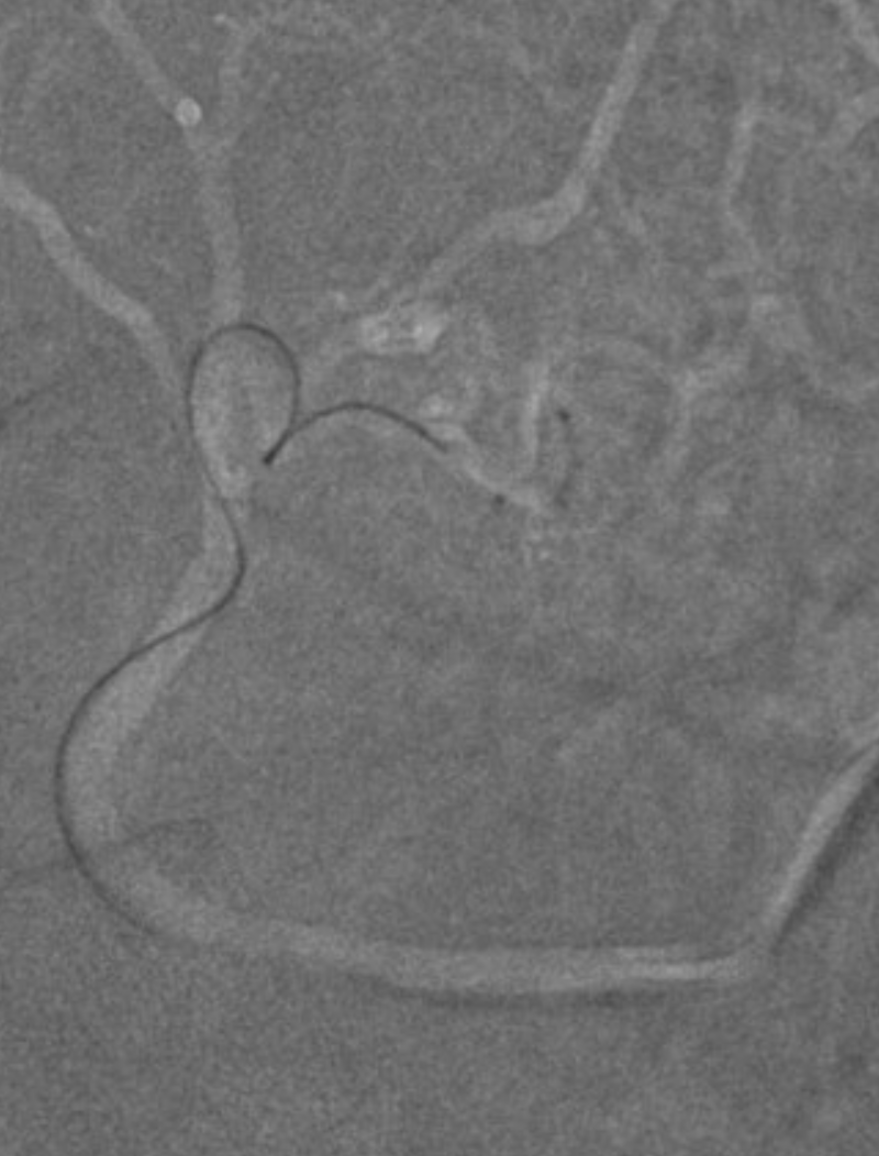
This is not a “wedge” or flow control position. So going deeper
The distal-most position is not “wedge either” — arrows point to reflux. This is NOT the optimal situation. Flow control is very important. Today we would have used Scepter mini for this, or switched to a larger caliber catheter — it is more important to have flow control than be distal. However, in this case took glue shot anyway. It worked, but was not optimal — not in terms of safety, but probability of occlusion is always lower without flow control
Movie of nBCA:Lipidol 1:3 injection, in real time. Predictably, the glue refluxes before reaching the fistula. Only with waiting and continued periodic injections does it finally advance to the foot of the vein. Given that there was no robust ventral epidural arcade i think the safety was reasonable.
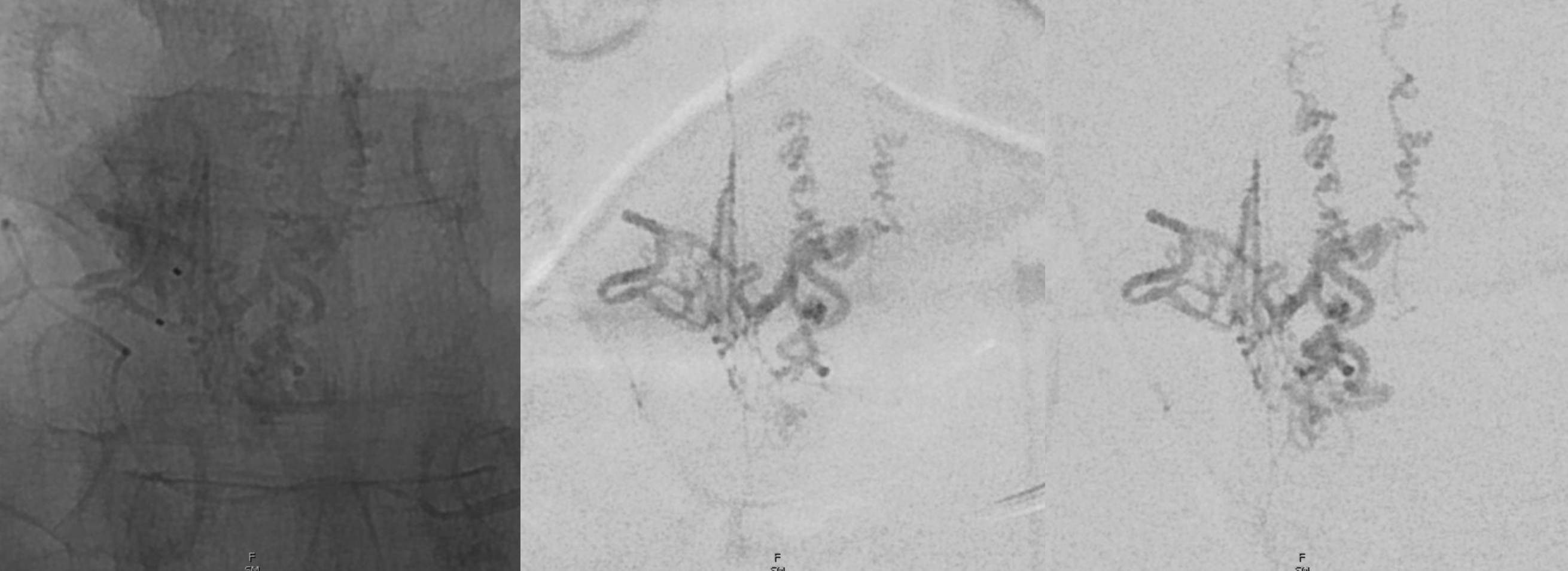
Glue cast
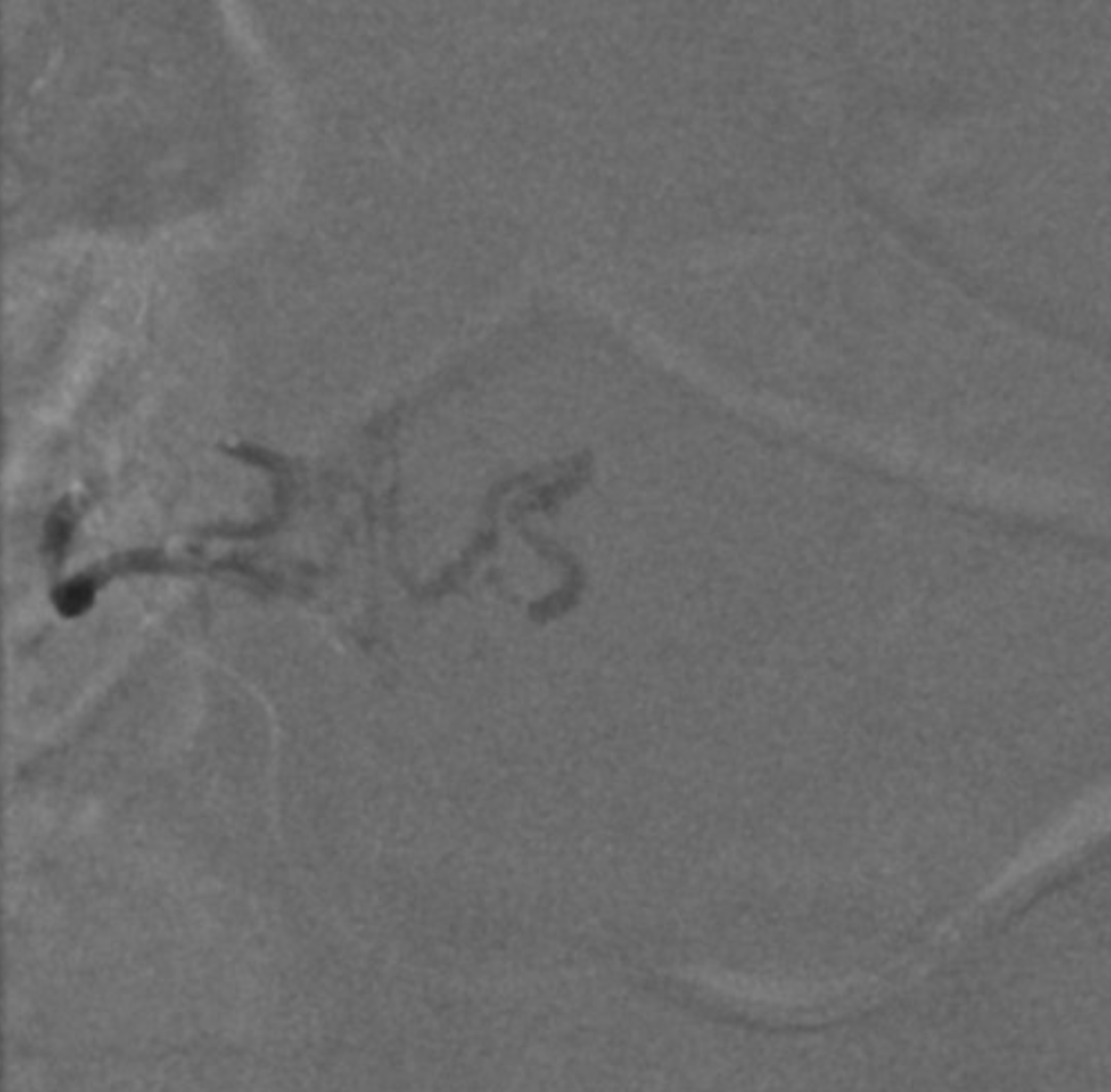
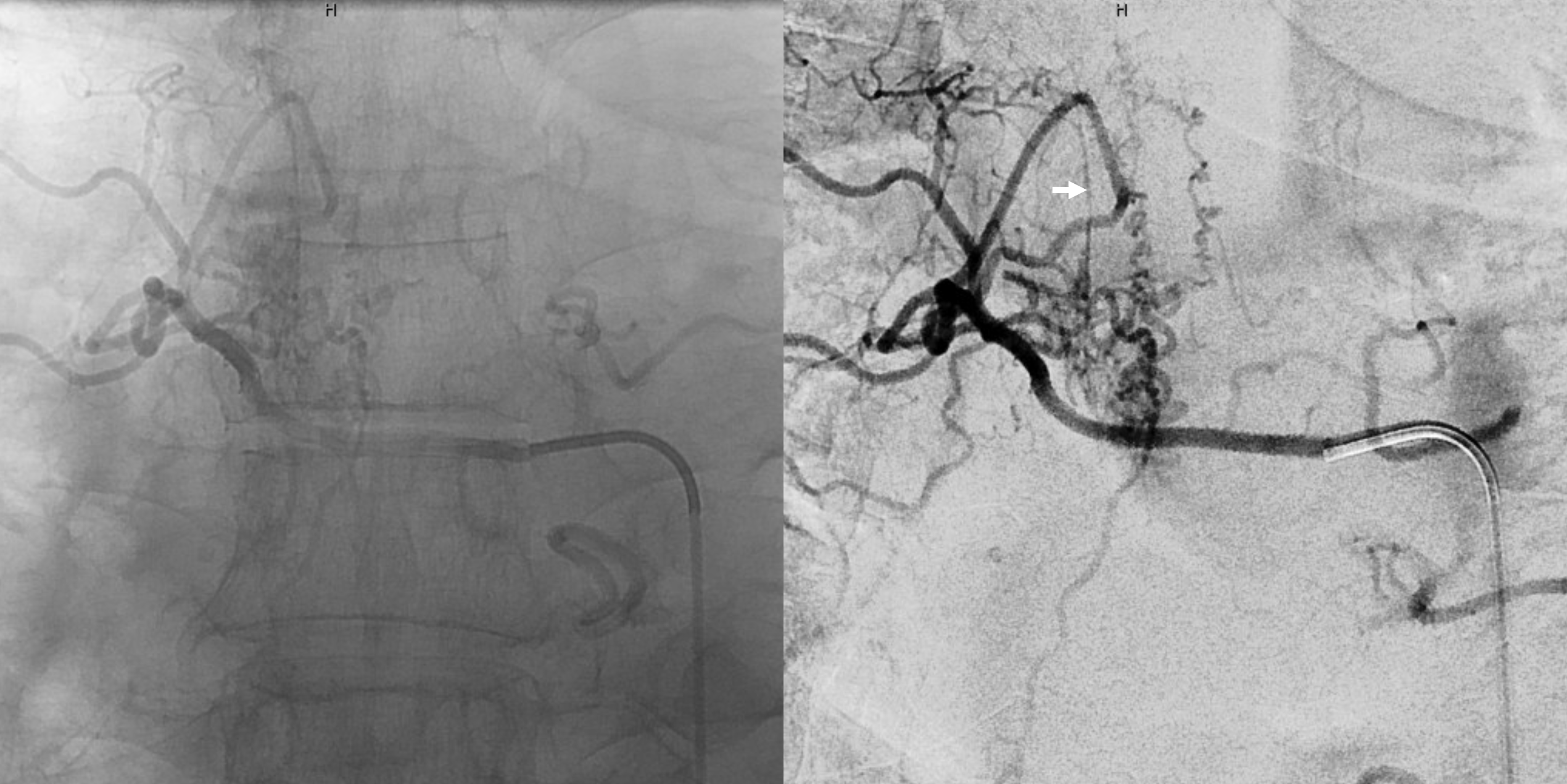
Post right T6 — note reflux into left side and faint asa

Left T6 — preserved anterior and posterior spinal arteries. Importantly, the cord veins previously parasitized by the fistula have now been “returned” to the cord — seen in their expected venous phase (oval)