Together with Eytan Raz, MD PhD
A www.youtube.com/neuroangio narration of this page — BANANA BITES — is here
A nice case to show options for carotid revascularization. And another good perfusion case — you know how we use perfusion as diagnostic tool to understand occlusion site and flow consequences rather than for penumbra/core estimation and patient selection. Pictures will tell story….
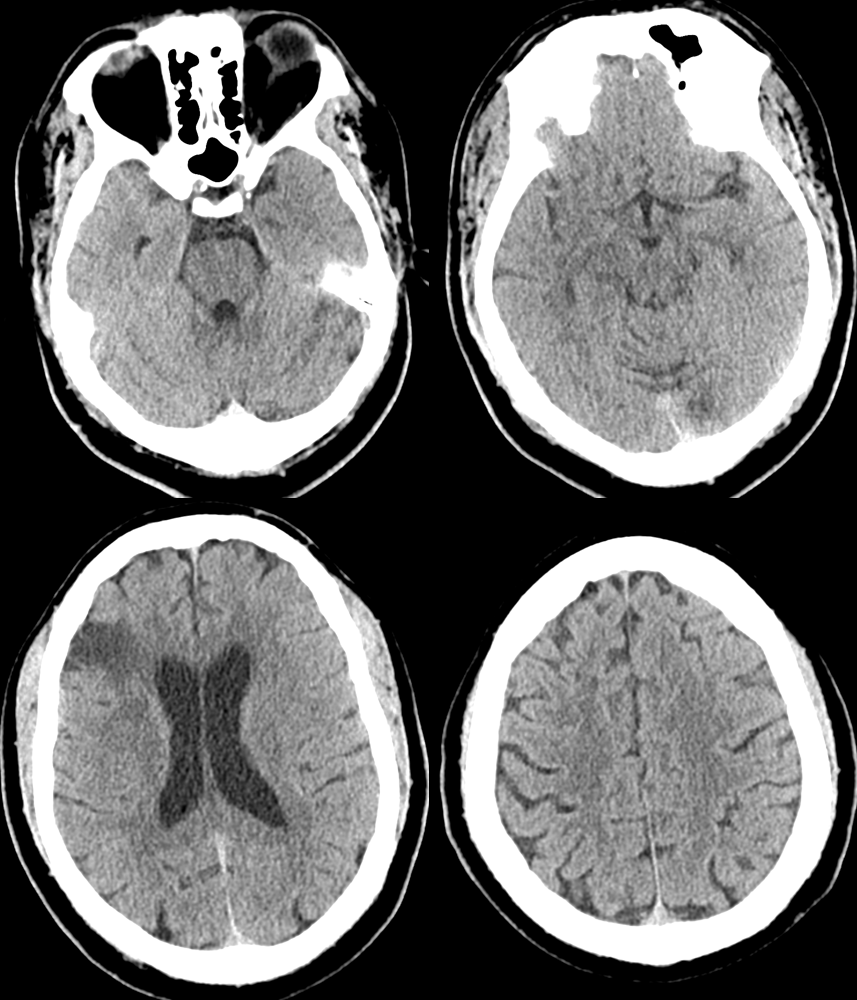
Patient presents with NIHSS 1-3 fluctuating — mild language issue and field cut
Perfusion — strange picture maybe. Movement? Something else? Always look at individual maps and source images if not sure
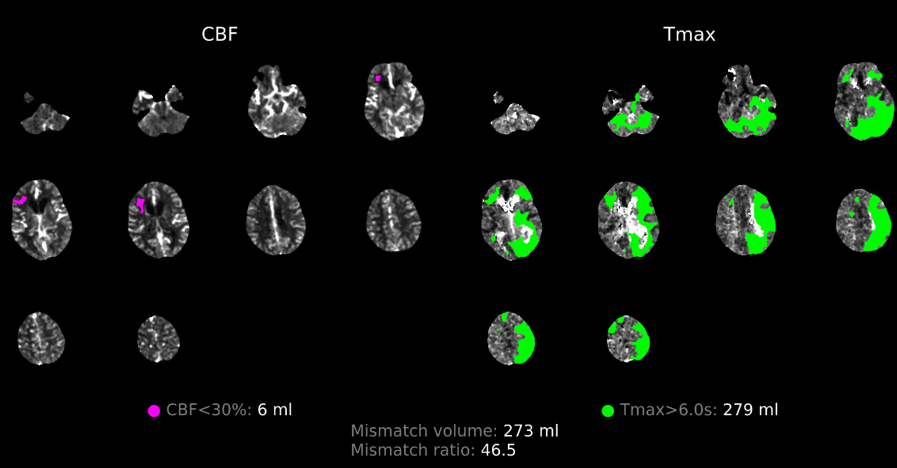
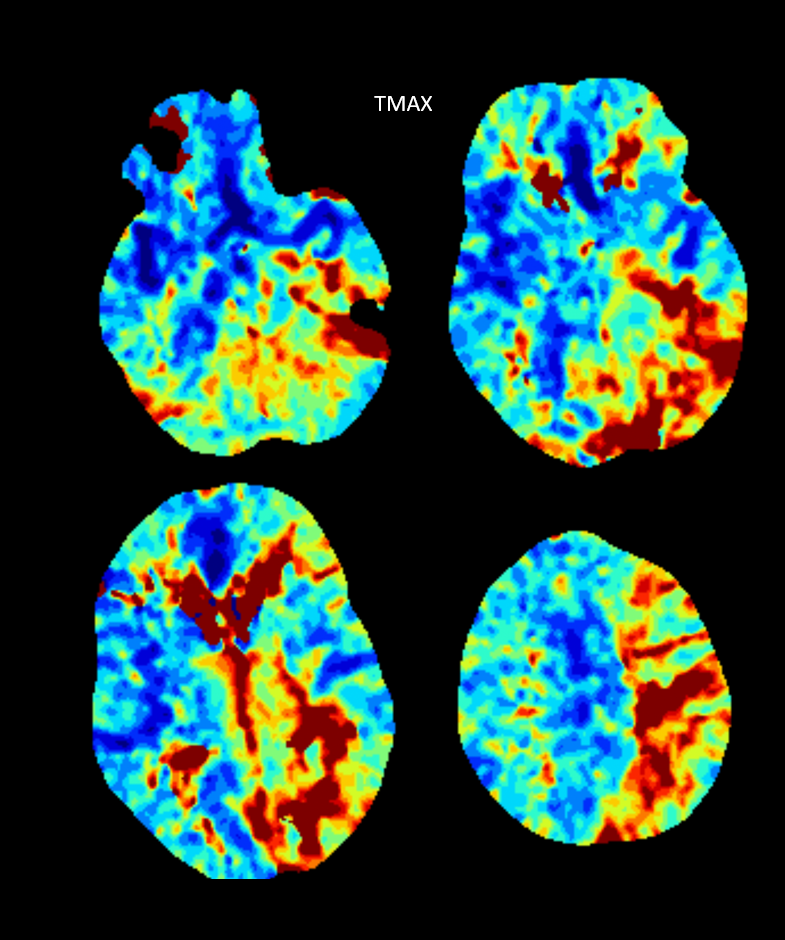
Maps looks pretty real — including occipital and upper cerebellar flow issues — tmax maps are best for that
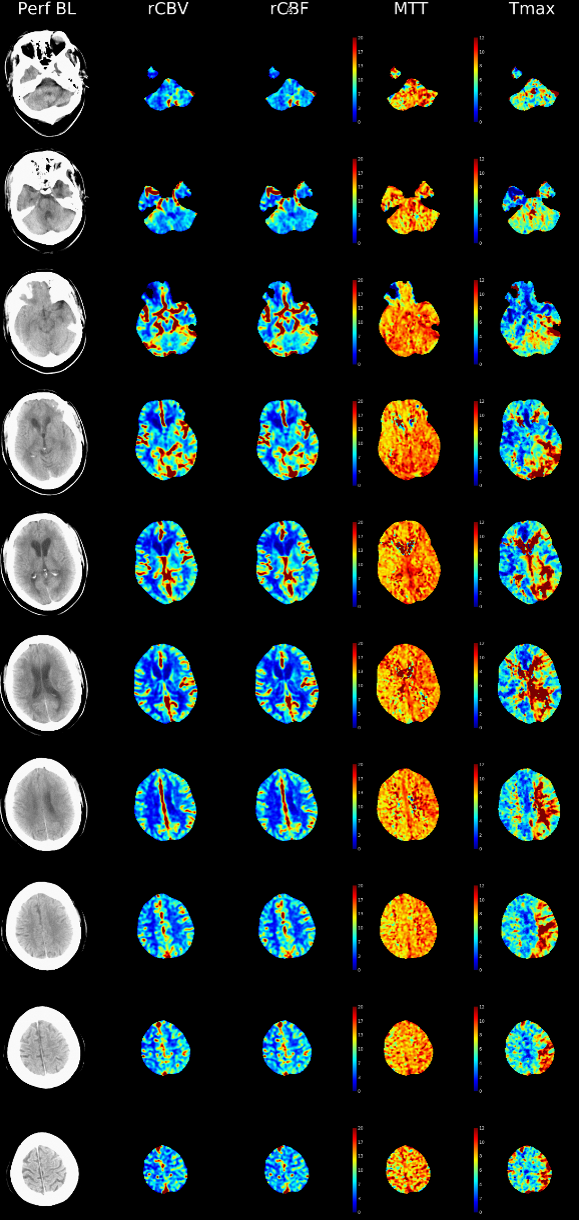
Tmax Maps super sensitive to flow alterations — we use them primarily — its not about flow/volume differences — its about knowing where occlusion is and what territory is affected
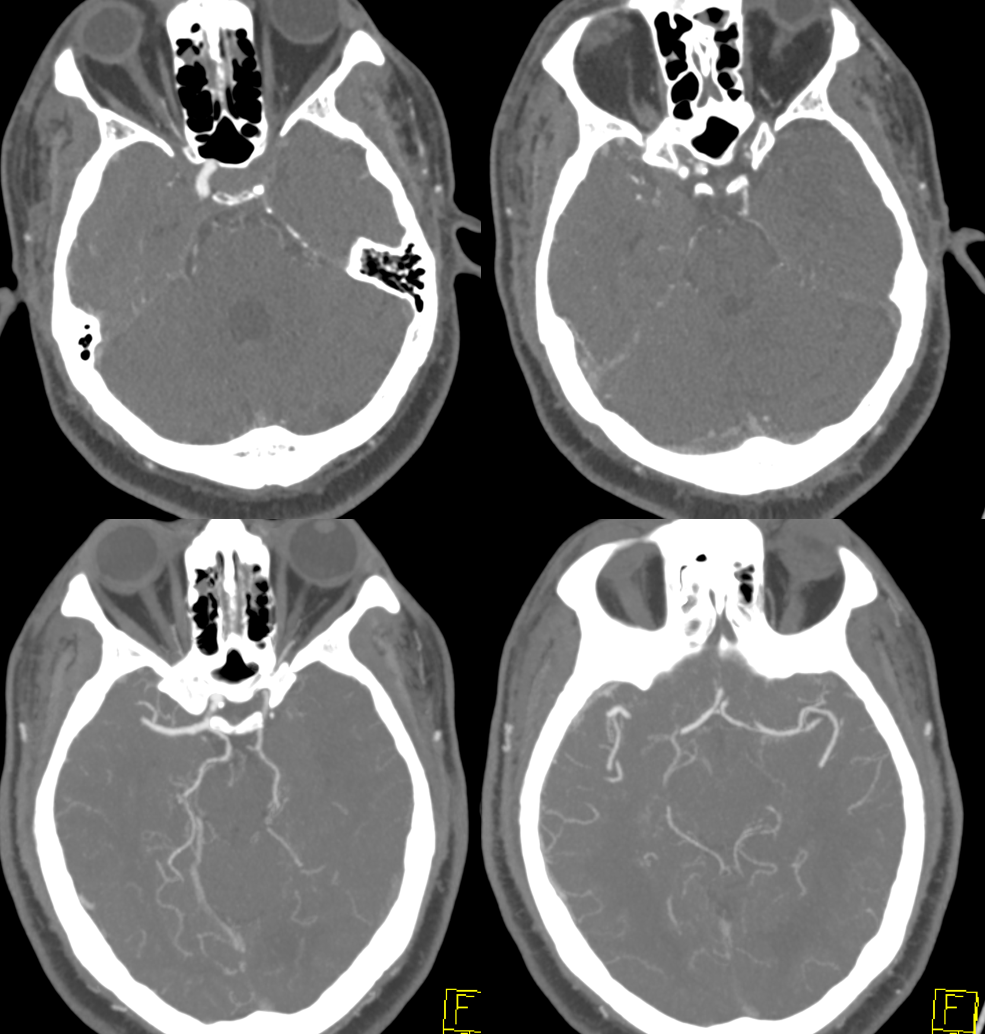
CTA shows left carotid occlusion. There are bilateral large PCOMs and small P1s. Which means they cant help the left hemisphere. Support comes from a small ACOM and likely ophthalmic — notice its slightly larger on left.
The moral is that between perfusion, when used as a diagnostic study, and CTA you see very nicely what’s happening
Patient is stable overnight. Next afternoon aphasia worsens and there are new mild motor issues. Given small size of ACOM and large left ICA territory (including PCA) this is not surprising.
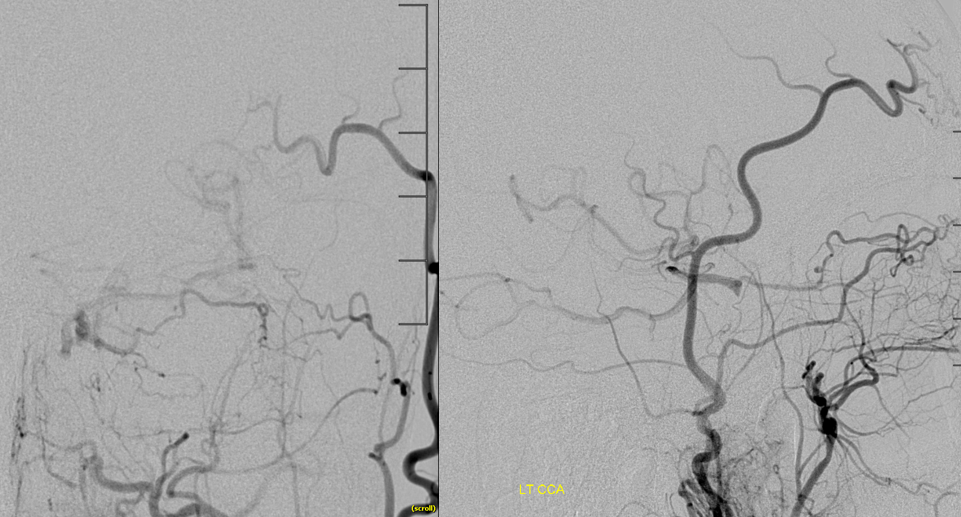
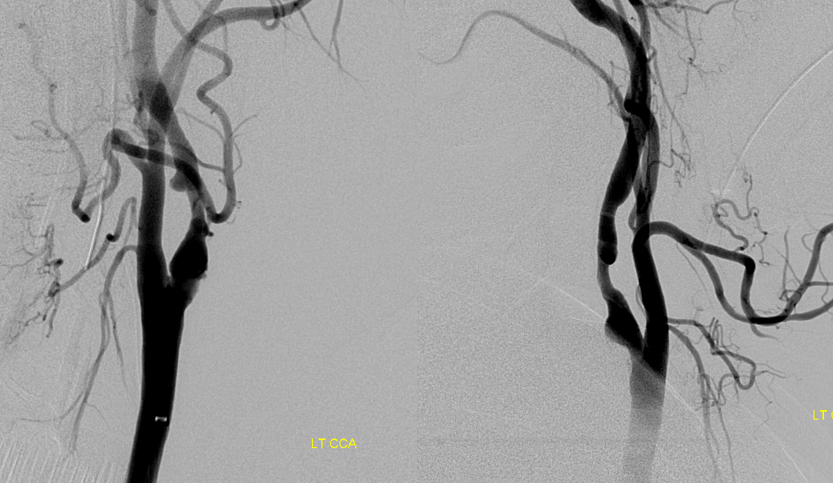
Now he is going for revascularization. Angio — RT and LT vert injections — basilar is small and irregular — likely combo of developmental small size and superimposed athero
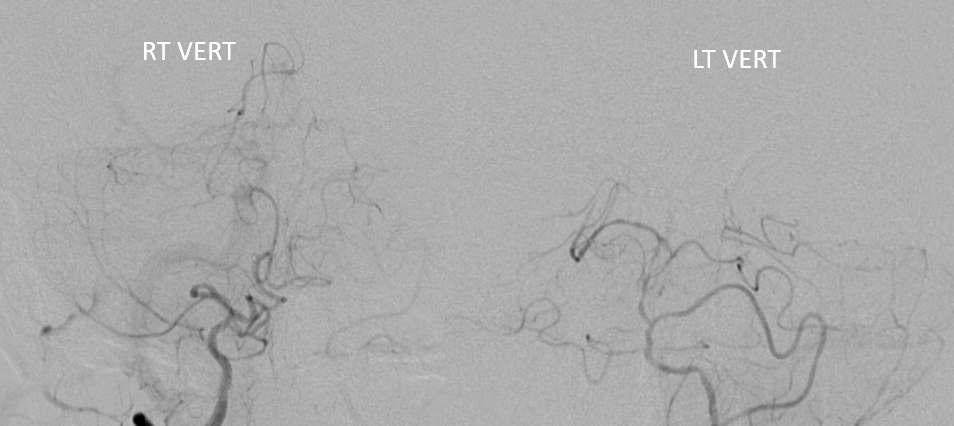
Right CCA injection — as suspected small ACOM /A1 are not enough for left side
Carotid stump — does not look like pseudo-occlusion — there is plaque / clot at the origin
Ophthalmic tries hard — see fetal pcom
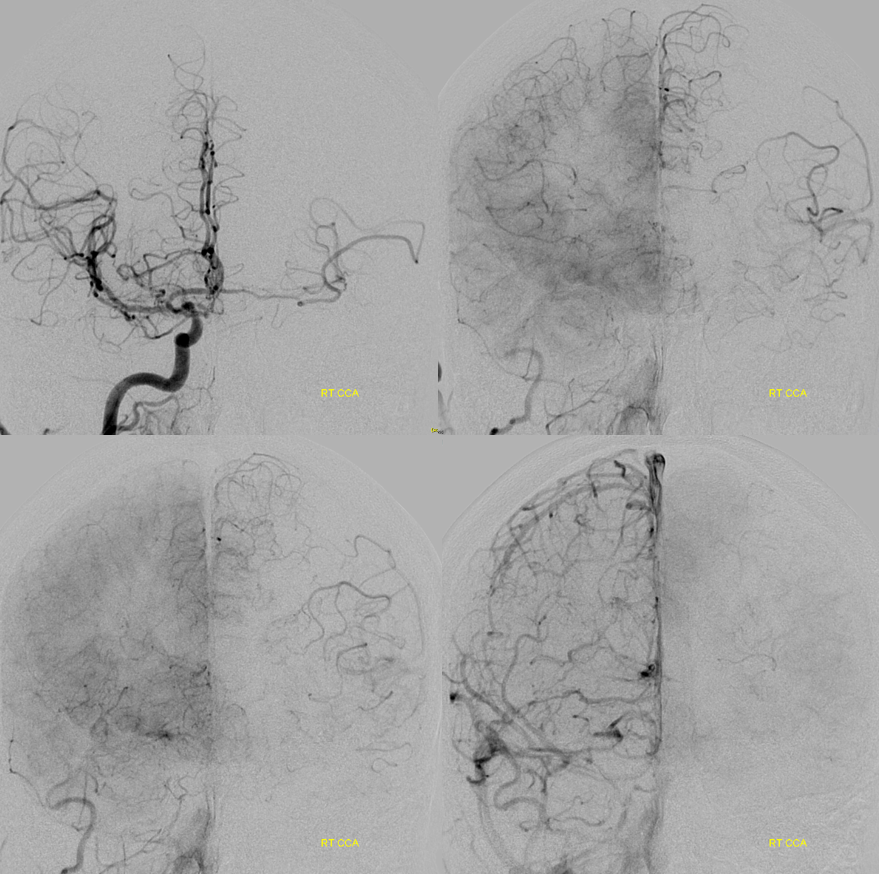
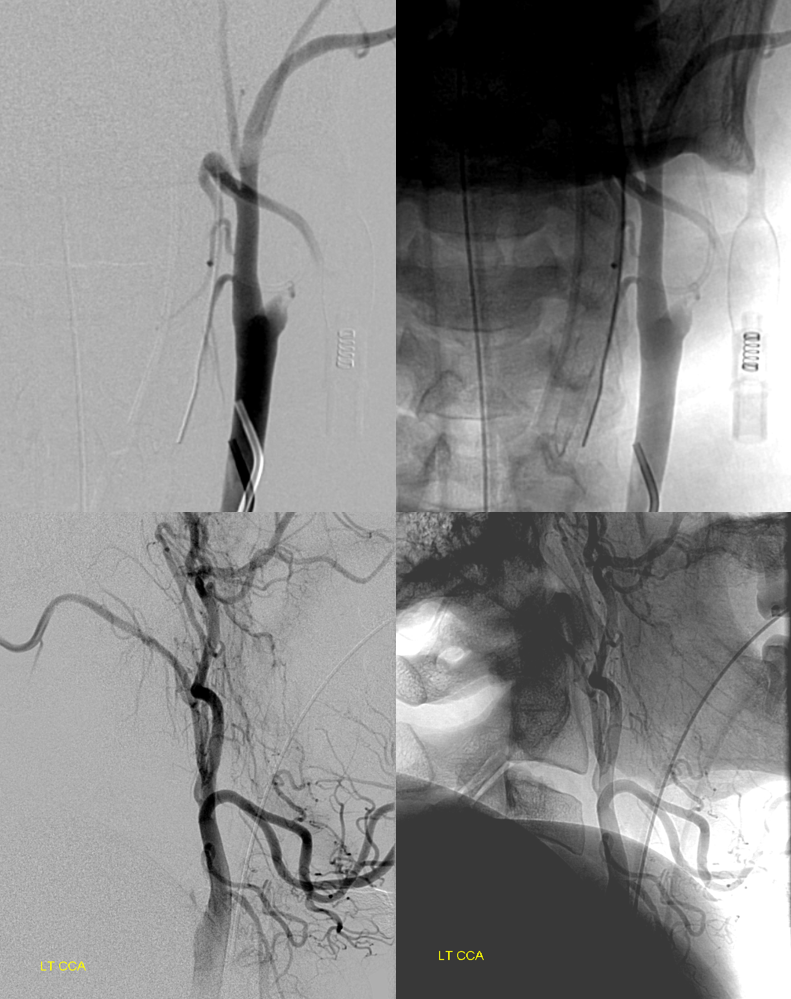
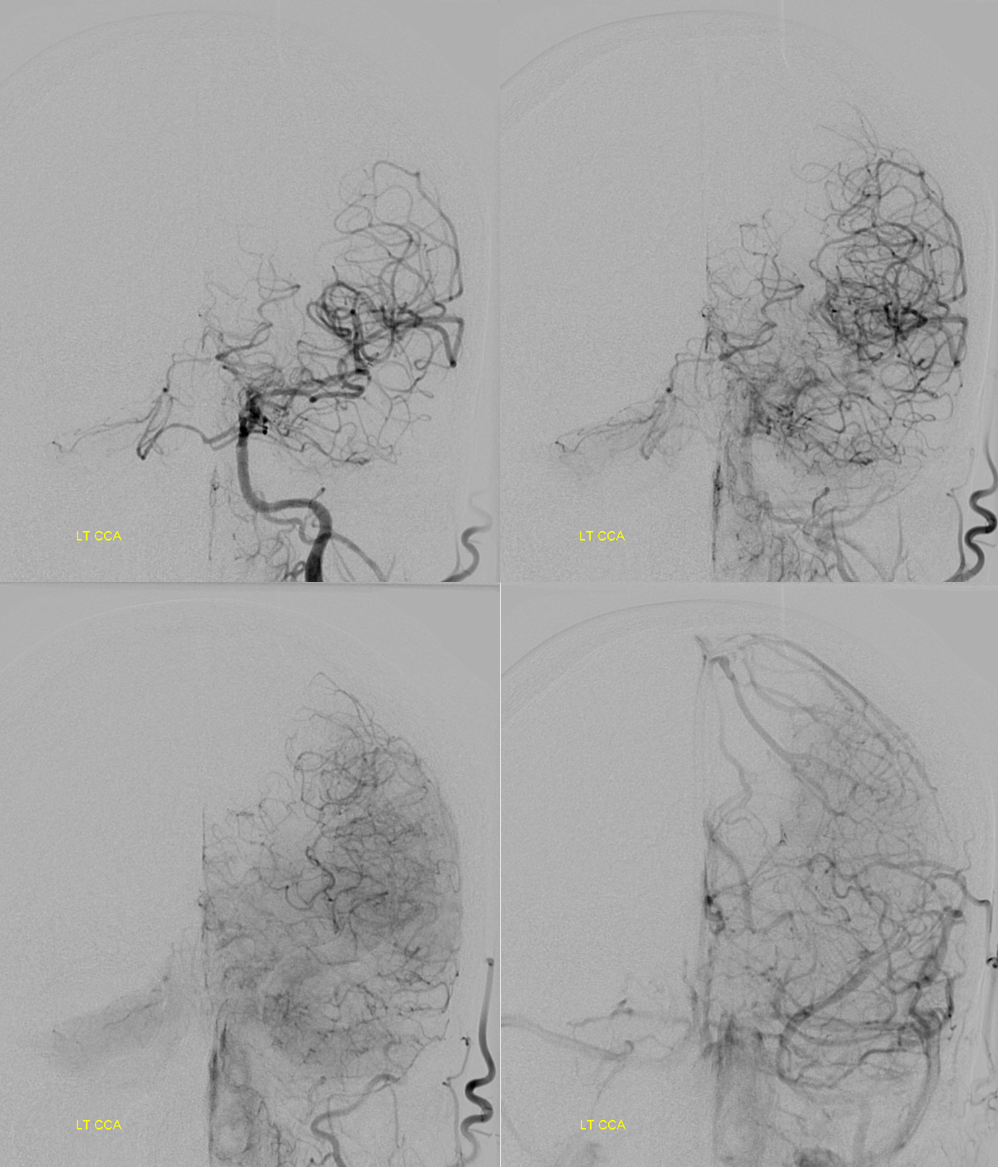
Many ways to reopen a carotid. Major concern is always the same — releasing clot to float north. How to protect it? Sometimes pushing sheath like Shuttle through the occlusion is enough — it will be occlusive there. Another is using a balloon guide — we do this here. A Walrus is advanced into the proximal ICA and balloon inflated across origin to both protect ICA and maintain critically necessary ECA flow

The walrus is NOT attached to a line and left open. A Sofia 6 is repeatedly taken thru walrus to aspirate the ICA — several pieces of clot came out. When Sofia is advanced to supraclinoid segment, we finally have blood return. Angio shows no new occlusion
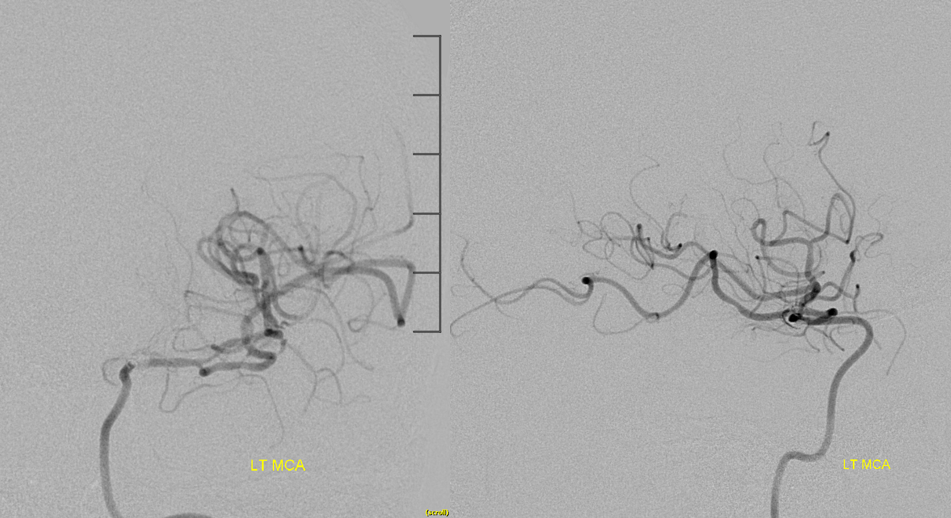
Moving Sofia proximally — no emboli. Notice how that PCA also supplies much of upper cerebellar territory via the P1 retrograde flow (arrows)
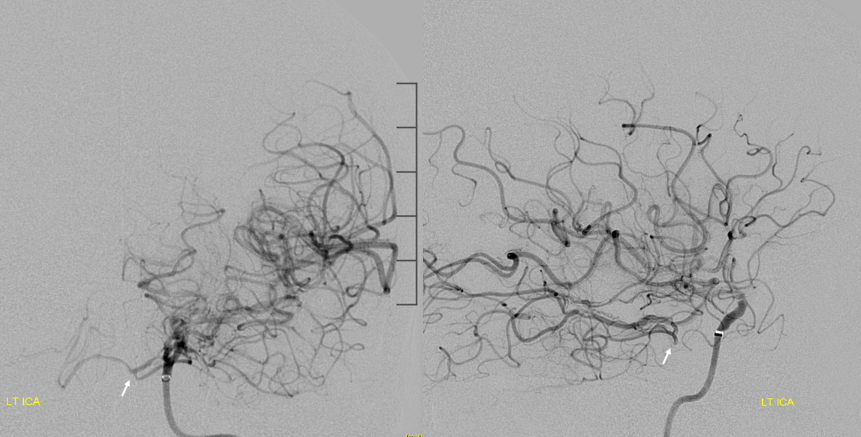
The ICA is clean. Now what? deflating Walrus balloon might release clot into the ICA if there is any clot below the balloon. Unlikely but not impossible.

We put a Scepter 4×10 in, inflate it to protect the ICA, and after that deflate the Walrus balloon

Then, we can advance walrus to the scepter and aspirate on walrus to remote anything that may have floated up there.

Why not use a filter wire instead of Scepter, especially if we may stent. Because they suck, and balloons don’t. If you really need embolic protection, balloons are much better — just minimize inflation time.
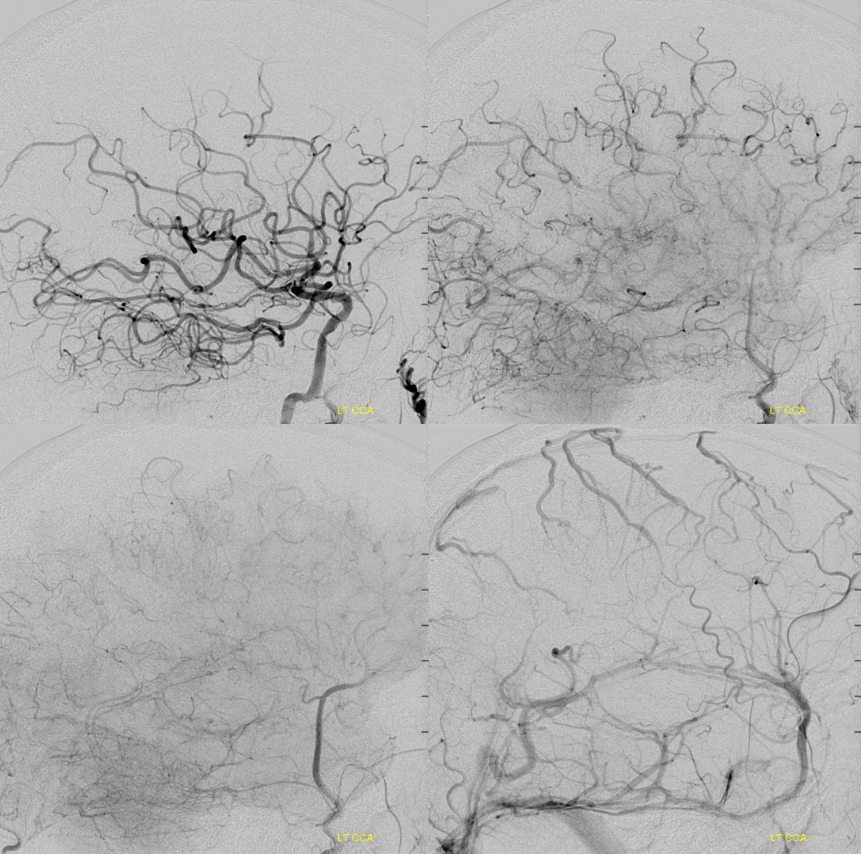
And here is post angio — see how the upper cerebellum is supplied by the PCOM — retrograde P1 flow into top of basilar — just like perfusion! Another example of how perfusion shows the full extent of the problem, flow dynamics, etc. We didn’t use perfusion to make a go-no-go decision — the NIHSS did that. But, perfusion told us exactly what to expect.
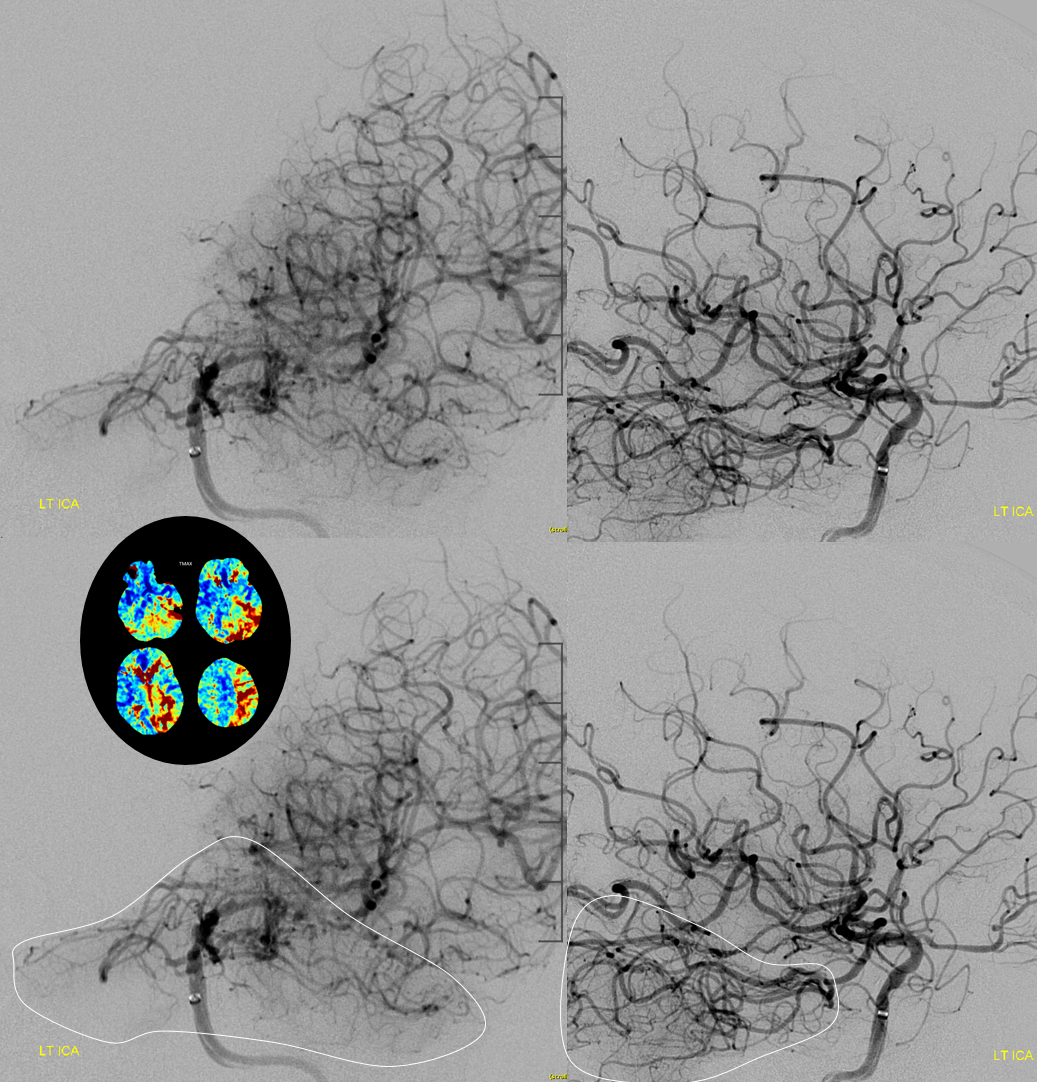
Post carotid bifurcation — we left this one unstented for later decision.
Final post
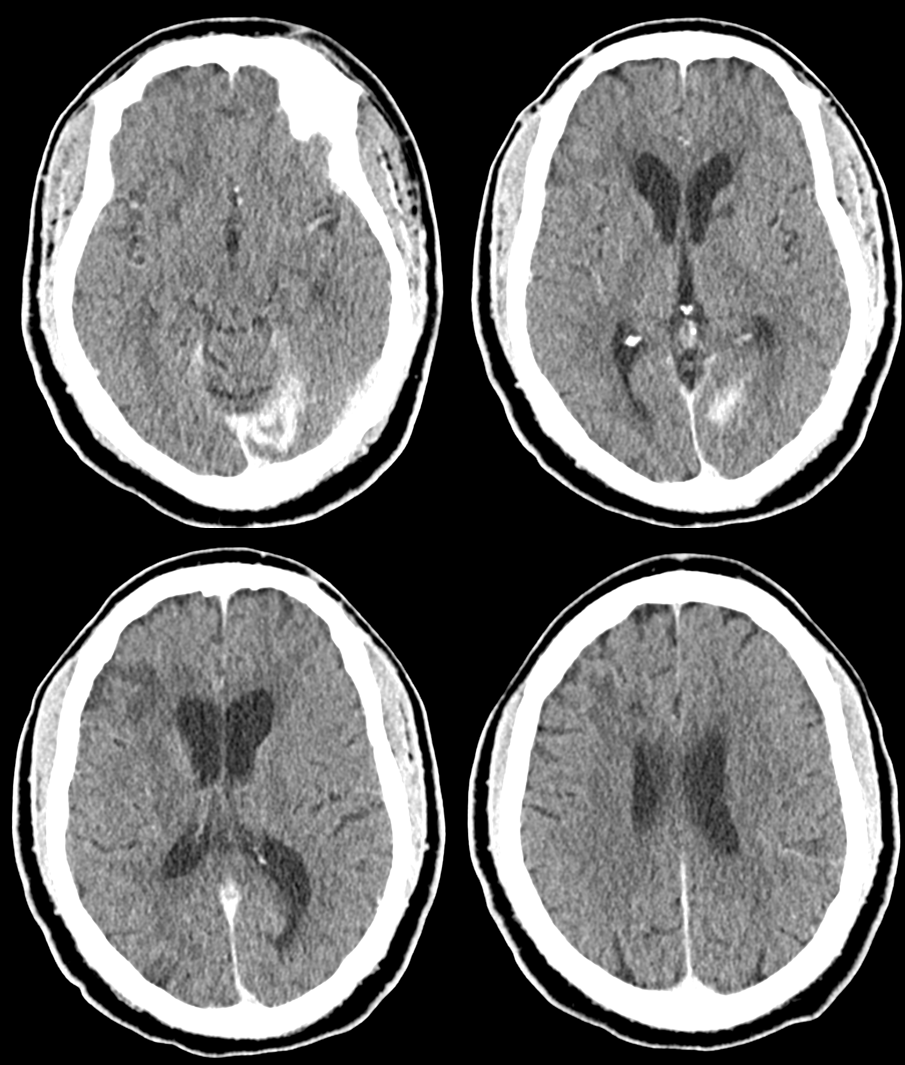
Post CT — the area with least collateral support (occipital lobe) in someone with a fetal PCOM is what got some damage. Rest is perfect
Points:
- Walrus or some other balloon guide carotid protection is an excellent option
- Perfusion as a diagnostic tool rocks, if you know how to use it
