Case done in conjunction with Dr. Howard Riina
As shown in several cases (click on link 1) dural fistula embolization can be safely, effectively, and elegantly accomplished in a superselective manner which both preserves the main veins and venous sinuses and minimizes nontarget embolization of remote arterial feeders. The success depends on identifying the very proximal receptacle of the fistula, which is frequently an artery in the wall of the dural sinus. This method has been applied successfully in sigmoid and condylar (jugular) locations and in others. While some cases are relatively simple Grade 1 fistulas the idea of identifying a recipient pouch upon which a myriad arterial feeders converge and closing this pouch selectively to take the fistula down in a “magic bullet” way can be applied to complex cases as well. Here is one example of a jugular or condylar fistula initially mistaken at a different location for a glomus tumor. The patient underwent a preoperative angiogram and particle embolizaiton before recognition of its true pathology. It is a long but instructive case, meant to be studied in detail
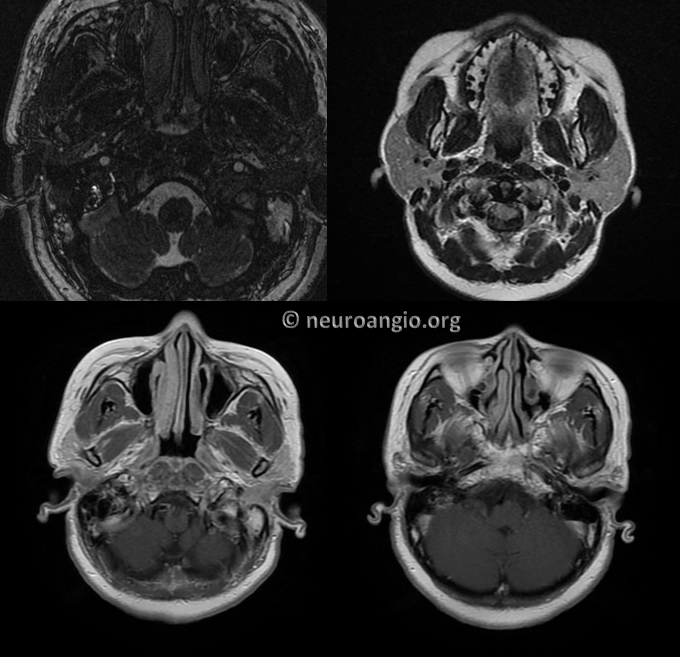
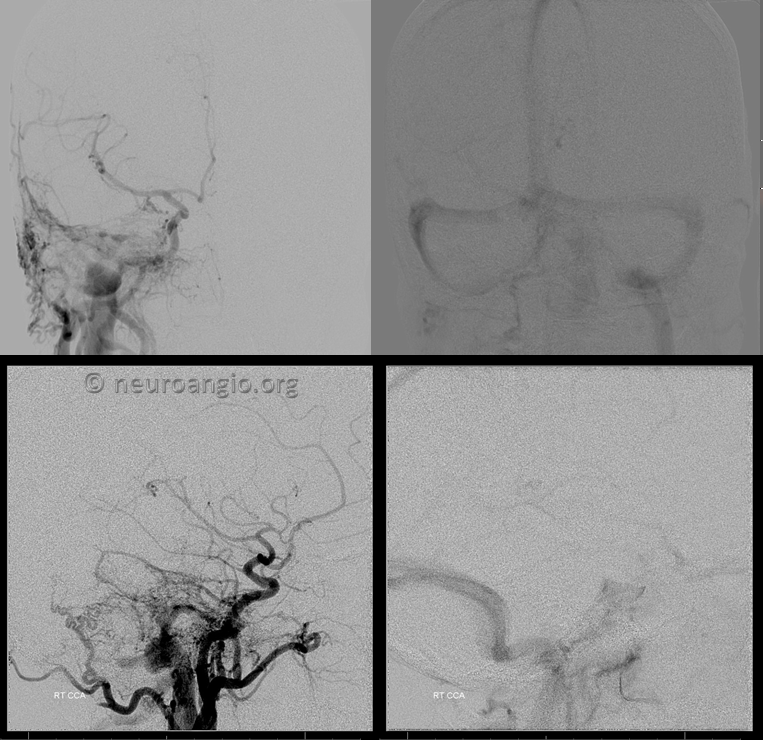
The right sigmoid and jugular are open. Minimal MHT contribution via lateral tentorial arcade
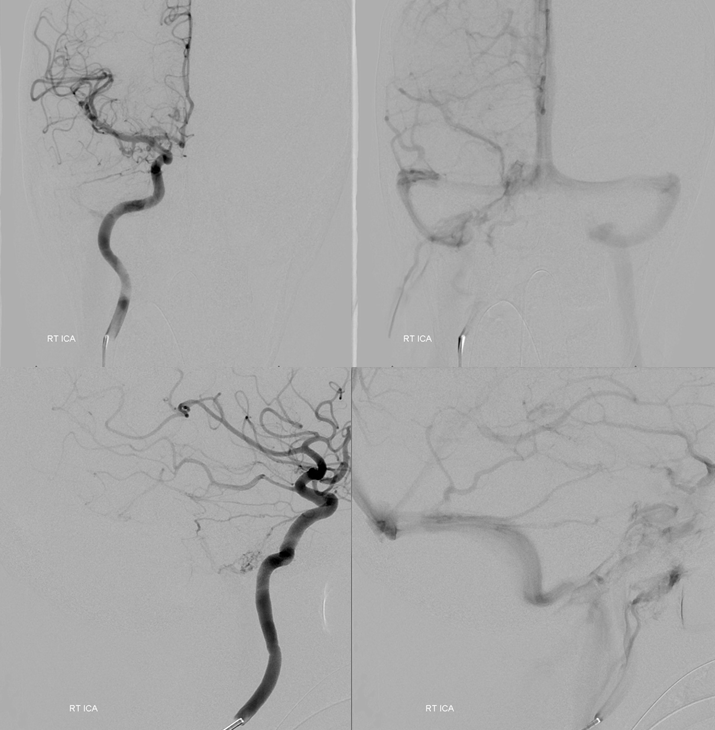
Ascending Pharyngeal supply
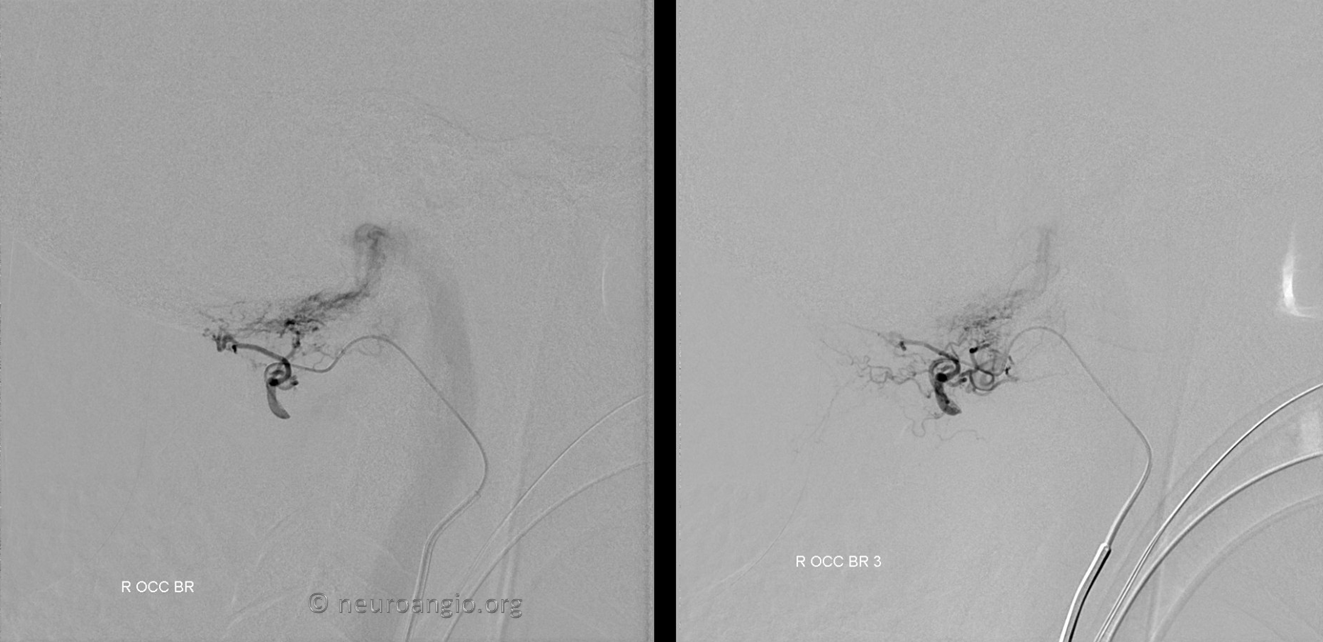
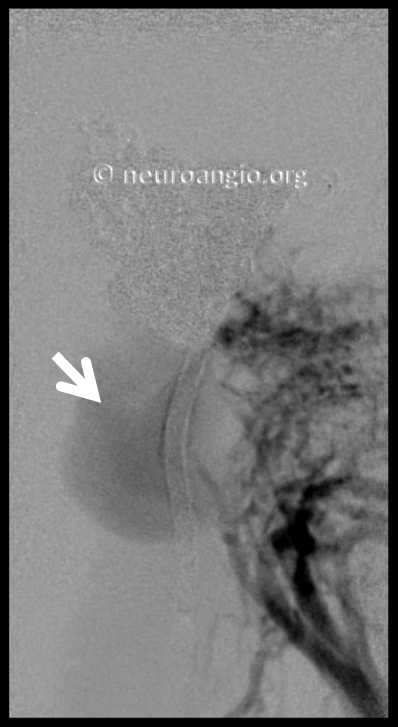
Small occipital feeder shows location of shunt at the condylar region
Ascending pharyngeal subselective injection. The recepient pouch ultimately targeted in the future is already visible (not marked)
Vert supply via odontoid arcade and posterior meningeal artery

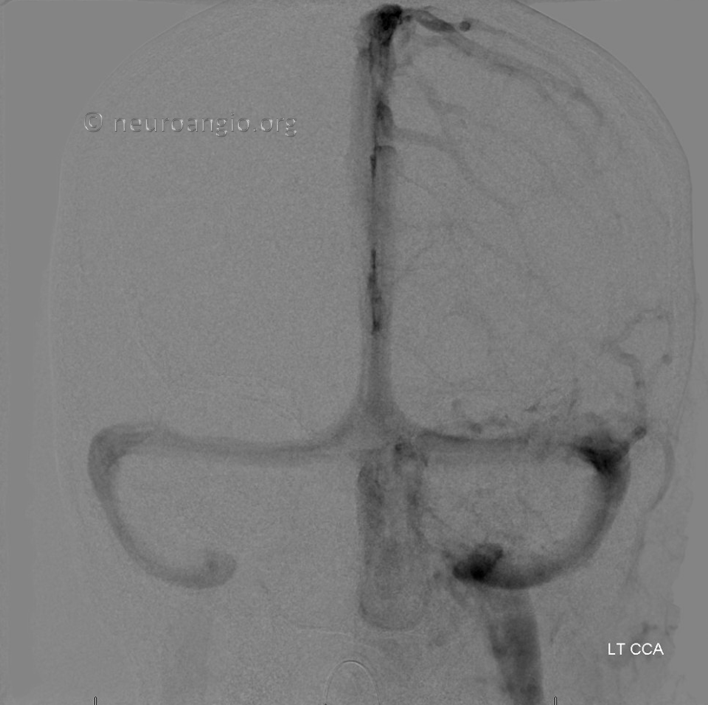
Nothing from left (other pictures not shown) and patency of right sinus outflow
Attempted resection was aborted due to bleeding

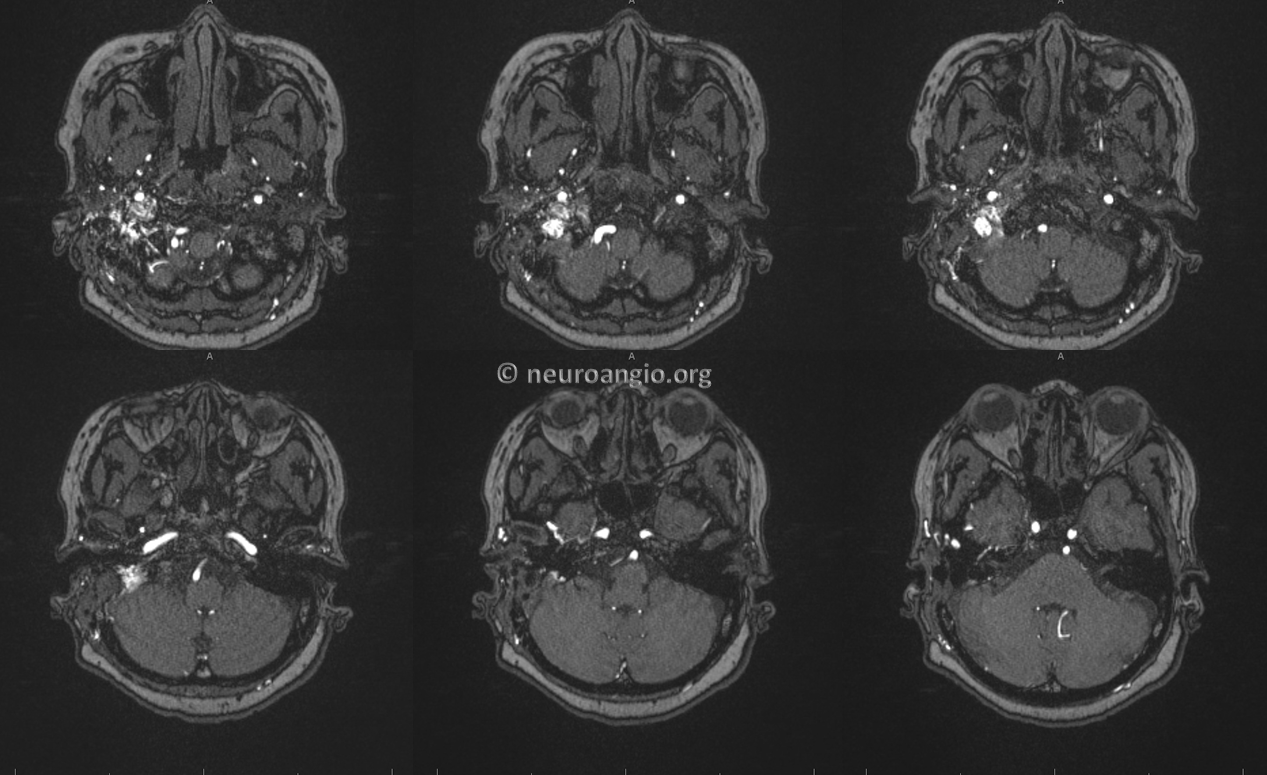
MRA several months post resection. We will come back to this set of images
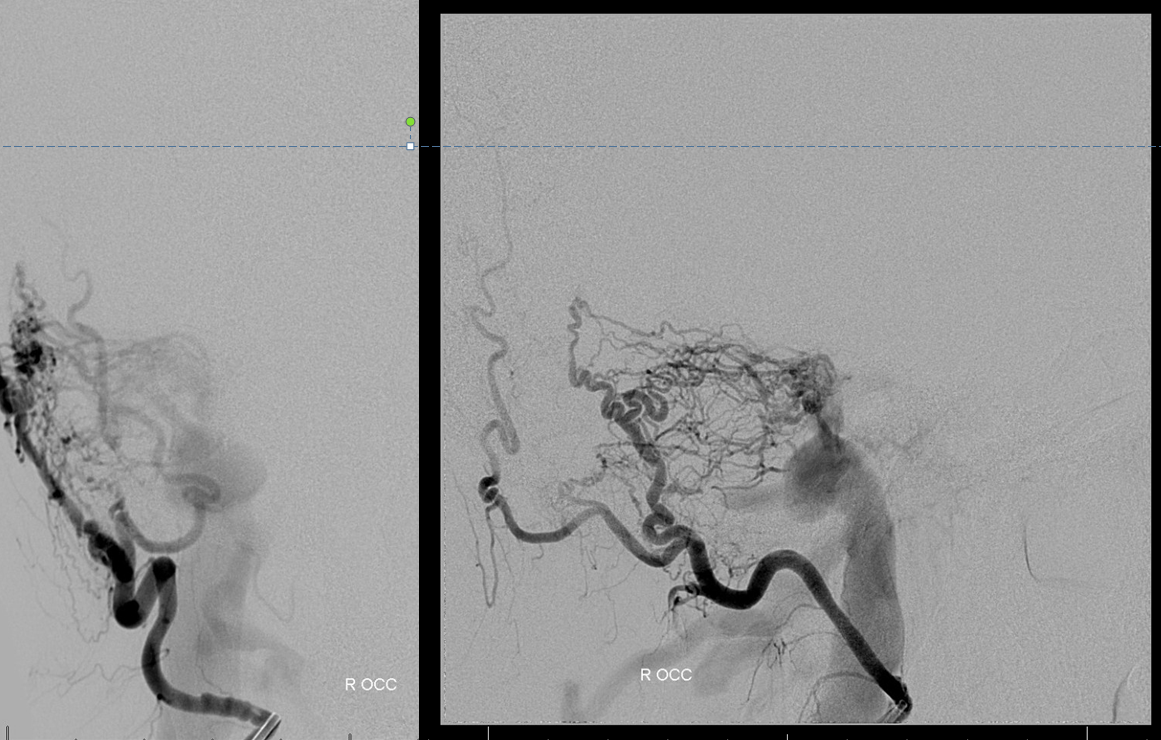
Now we are ready to attack the lesion as a dural fistula. There is much more supply now but sinus and jugular remain open
Ascending pharyngeal injection shows a new channel outlining the internal auditory canal which is likely post-surgical change.
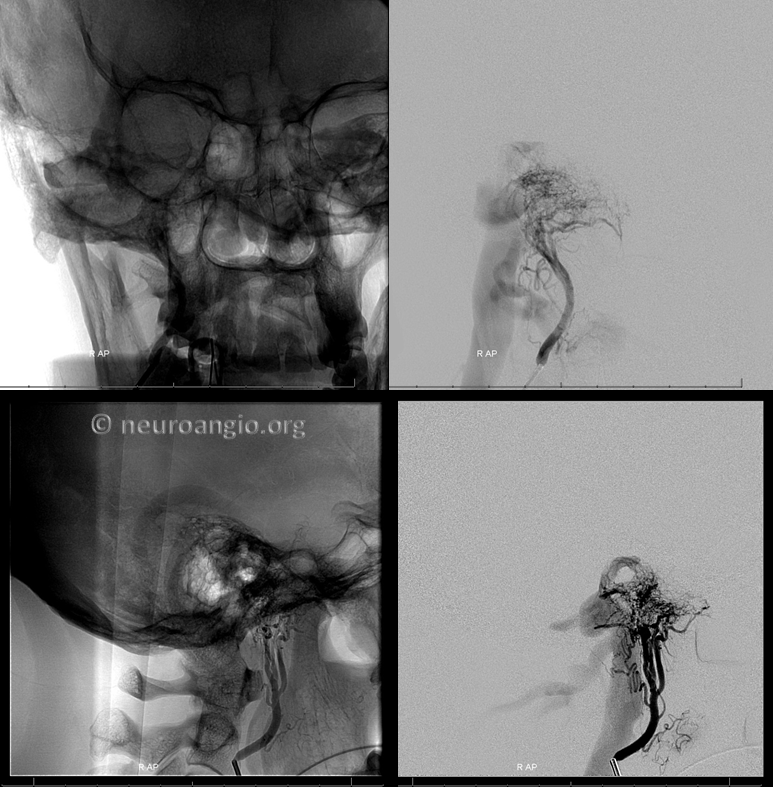
Extensive middle meningeal contribution has developed
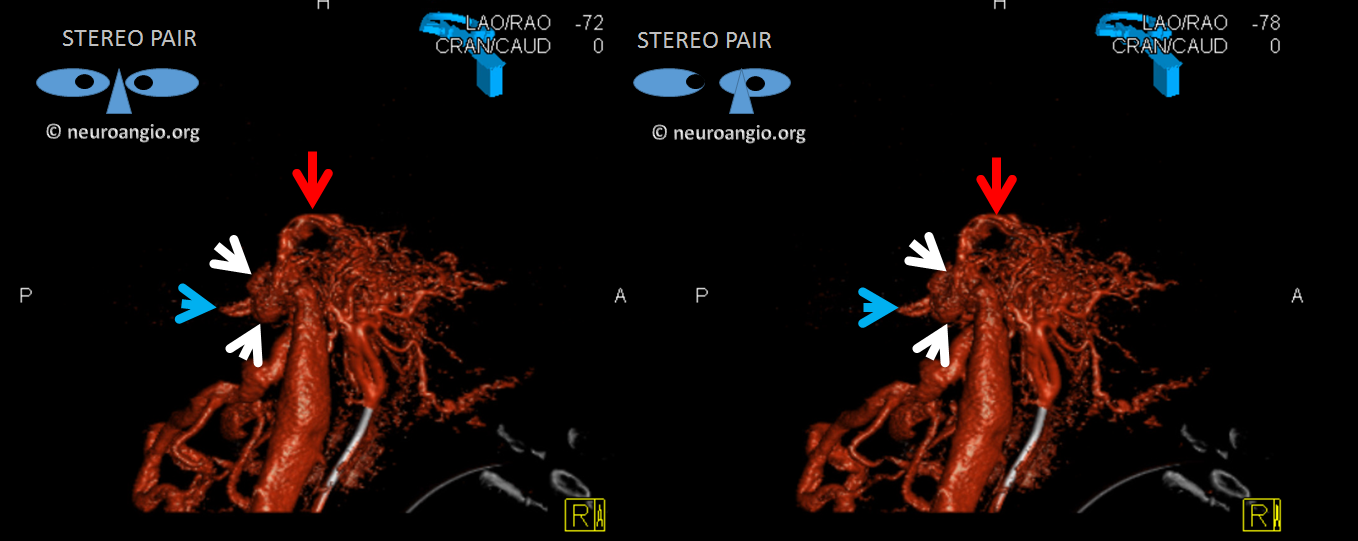
Stereo views
Occipital is not a good arterial embolization target, but in this case shows best location of the shunt
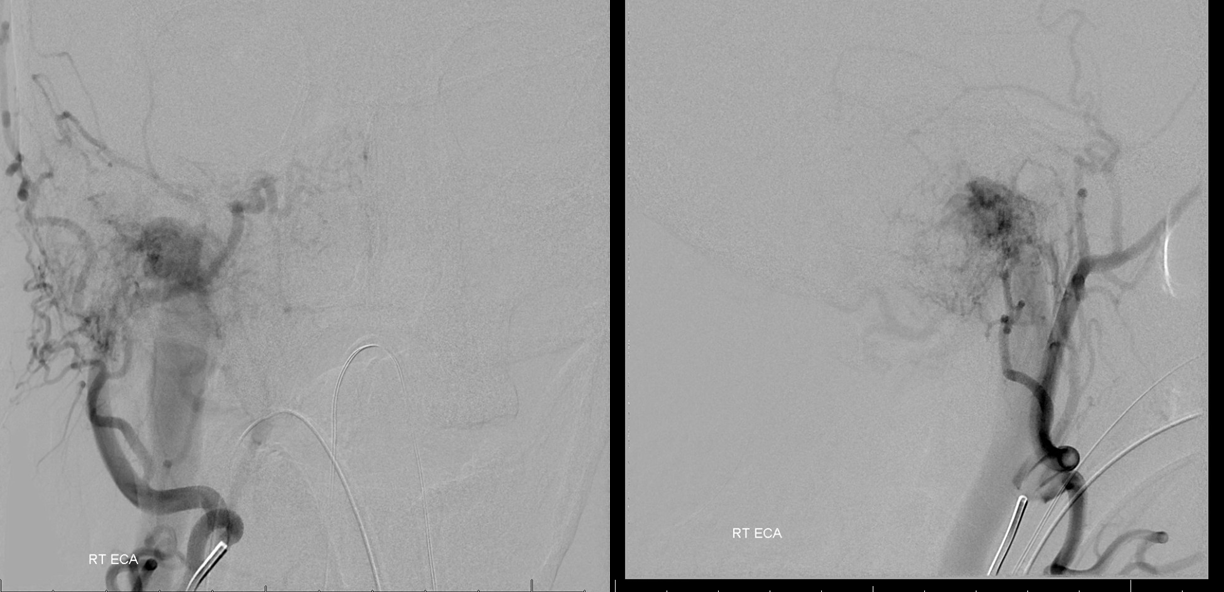
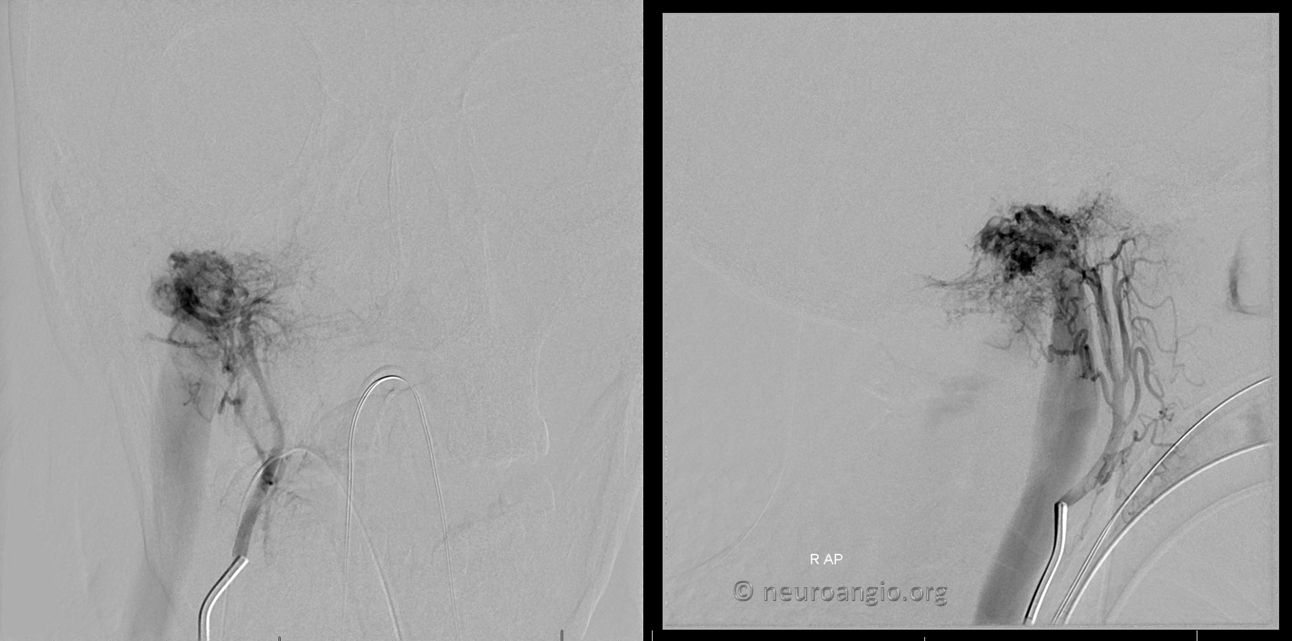
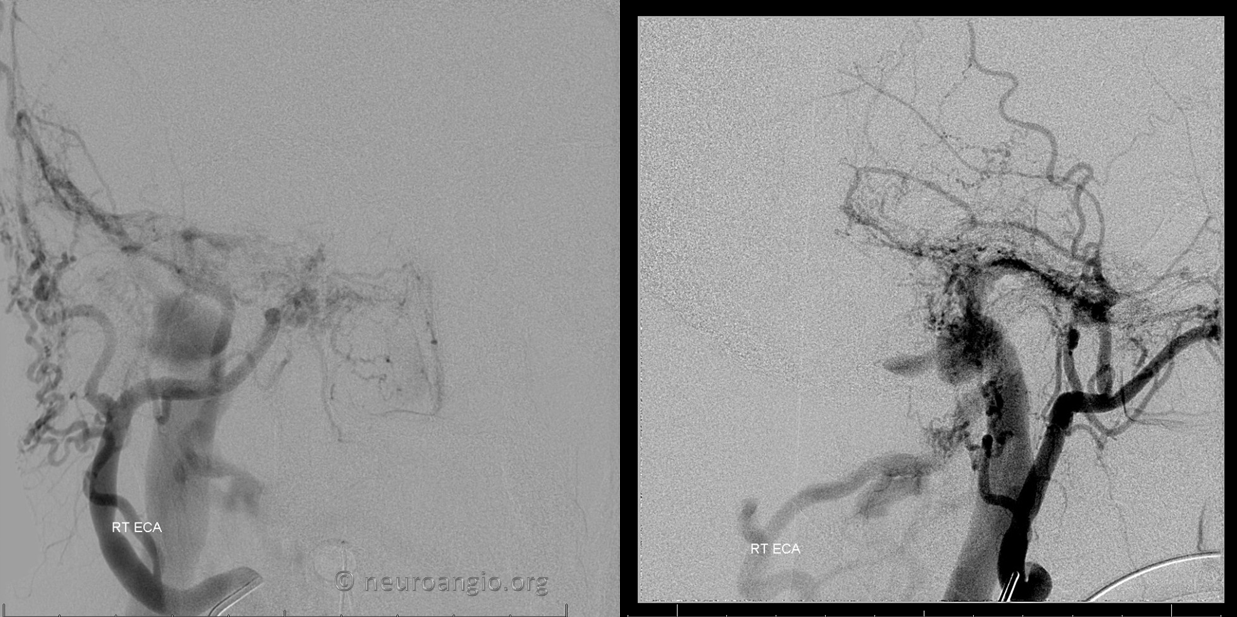
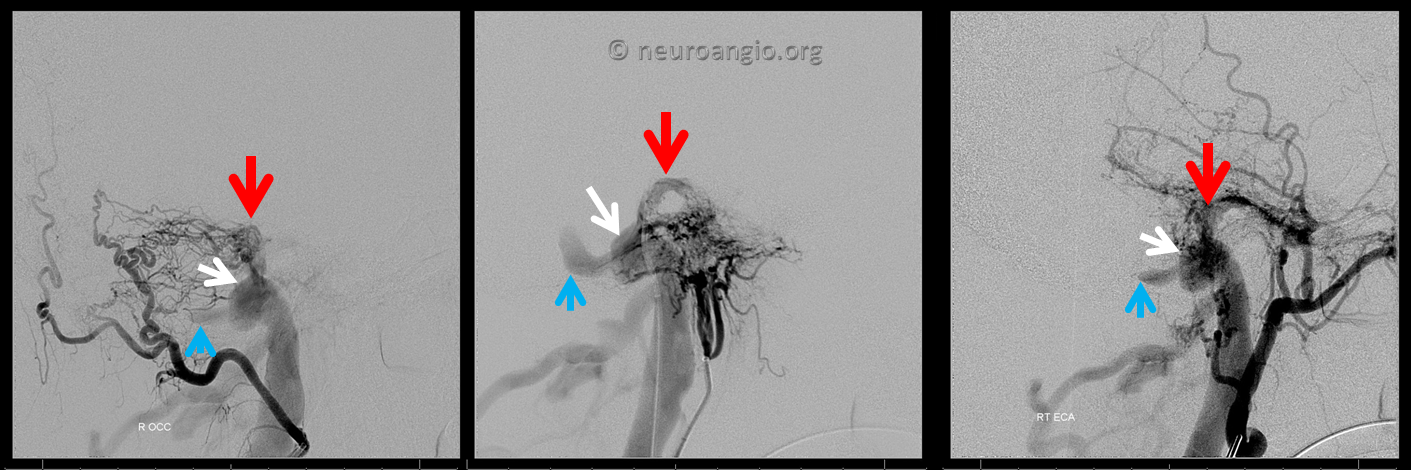
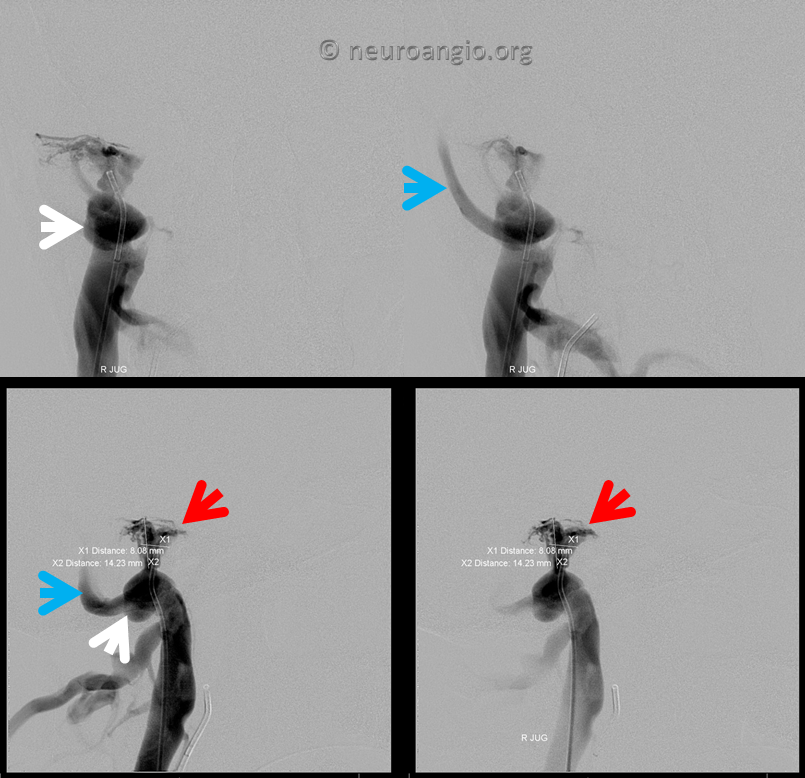
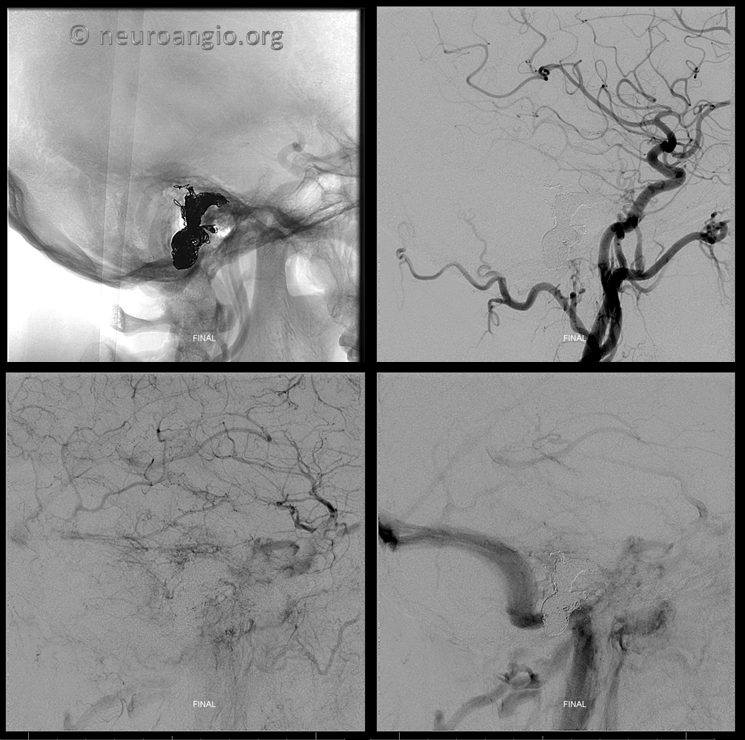
Now lets look at everything together. This ascending pharyngeal injection is key to understanding the fistula angioarchitecture. We see a channel (absent before surgery) above ths IAC (red arrow) as well as reflux into the proximal sigmoid sinus (blue arrow). White arrows point to a curious structure which is superimposed on the sinus in this lateral view
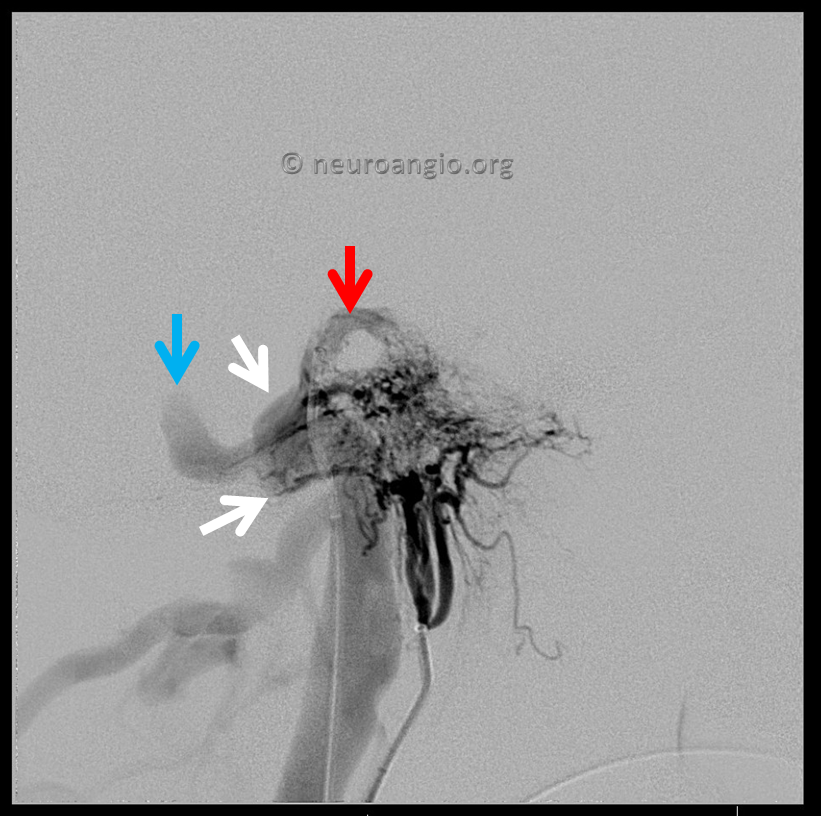
Now, when we look at these three injections we see the same structures in all of them. This kind of analysis helps identify the embolization target. The strategy is to come from the venous side and close (by coiling here) the pouches into which the fistula drains — these are marked by red and white arrows and represent areas where the myriad arterial feeders come together. The fact that these pouches are seen on all three injections shows them to be sites of arterial feeder convergence.
A rotational angio is done and some beautiful images are generated, but the idea comes from careful DSA analysis
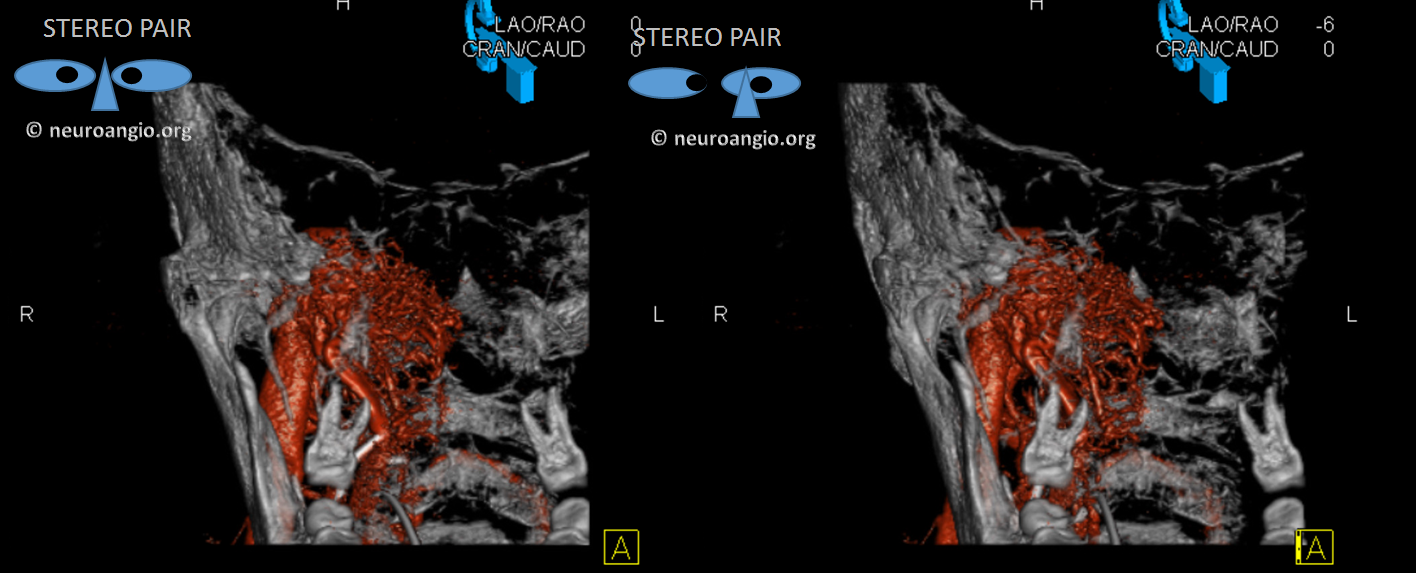
A stereo set without bone shows where small arteries converge on target pouches
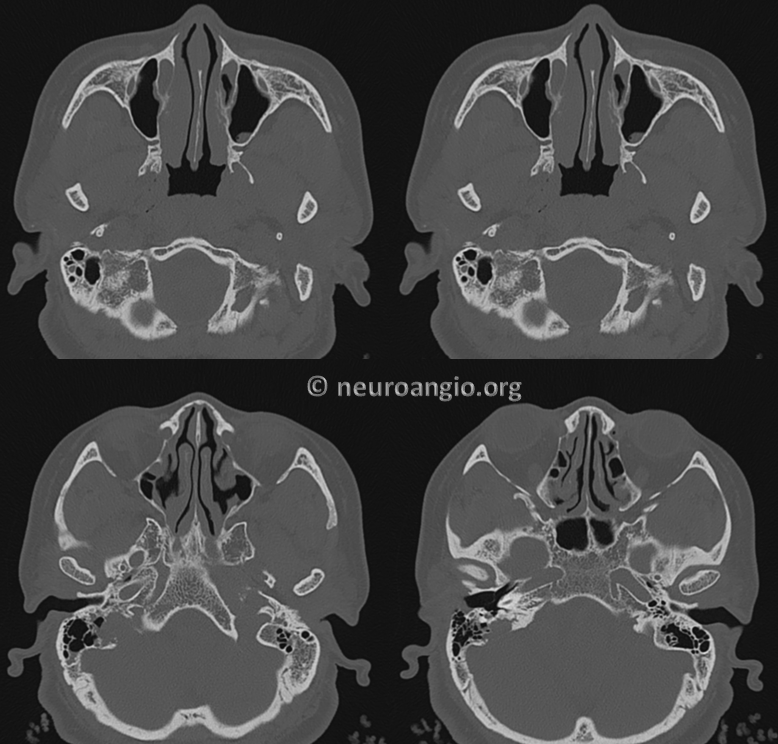
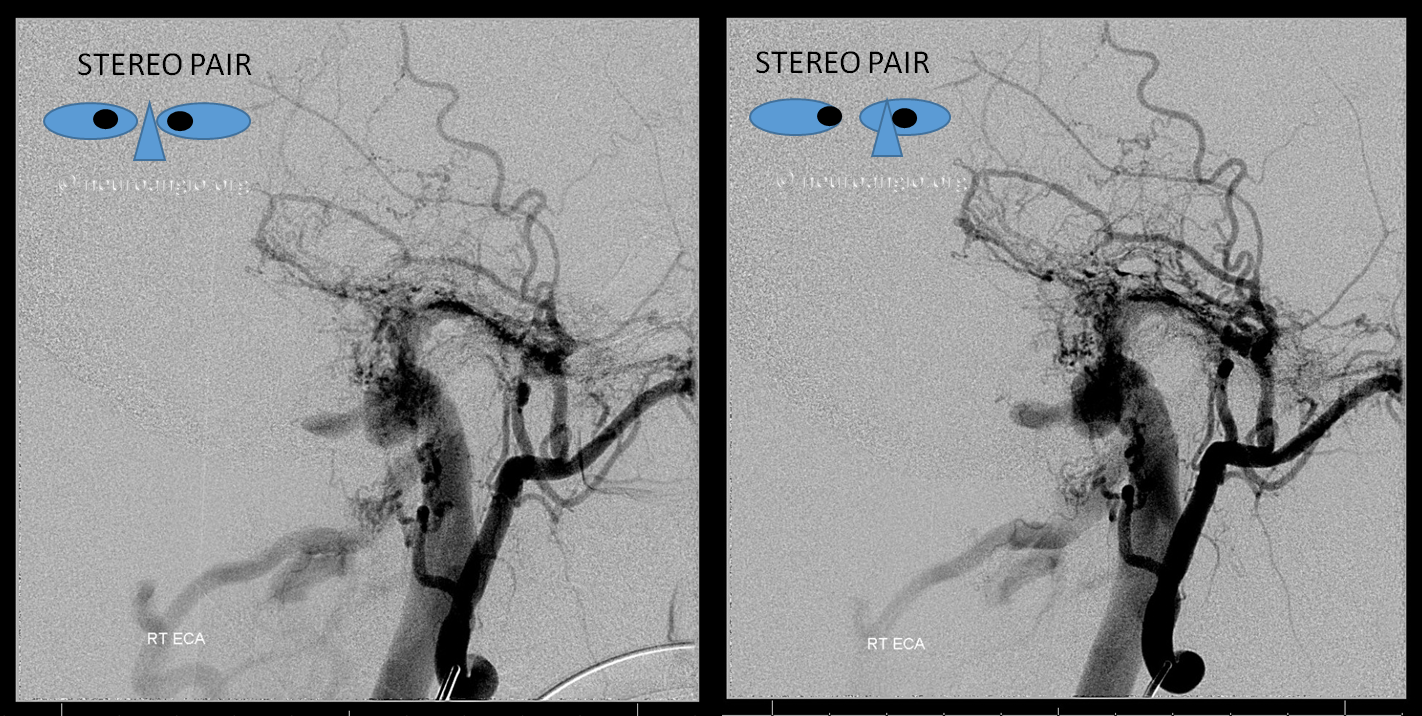
Now lets go back to look at MR. This is the art of being a neuroradiologist — how to look at a fistula from the standpoint of an interventionalist, to understand flow and angioarchitecture. There is a lot information on the MRI and MRA that is often under-appreciated. For example, here we see the upper portion of fistula drainage (red arrow) above the IAC and, more clearly, identify a strange-looking structure lateral to the jugular bulb (white arrows). This is not something we usually see in normal anatomy.
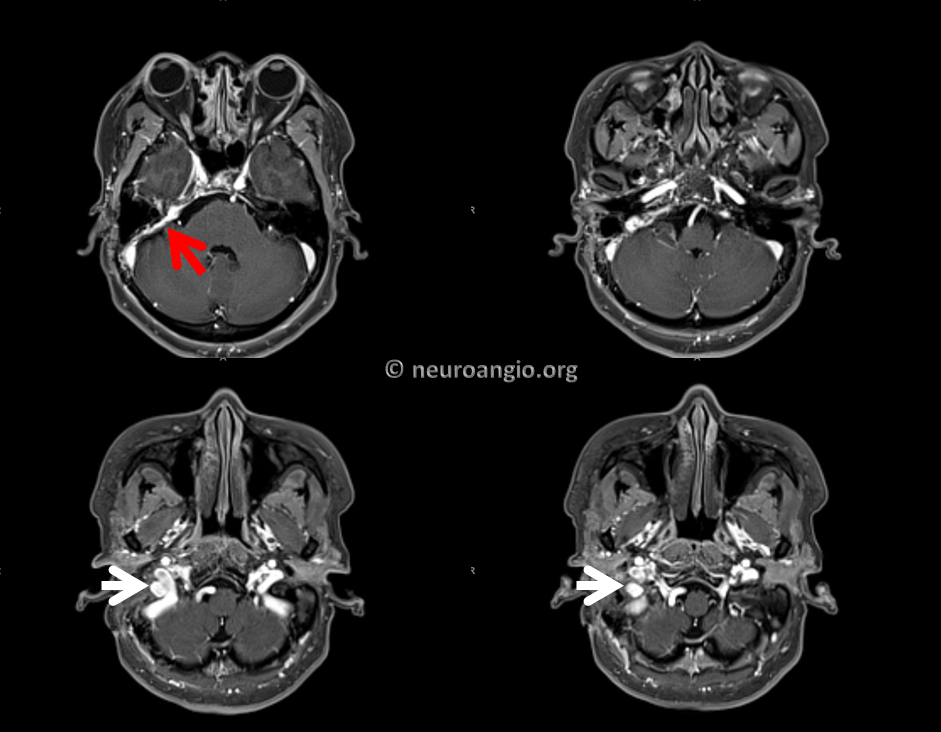
Here is the MRA — look at the tremendous amount of flow-related enhancement in this pouch (white arrow) compared to predictably absent flow signal in the jugular bulb which we know is patent. When looked at in this way, the MRA suggests that the pouch lateral the jugular bulb (white arrow) is the common receptacle of the myriad arteries feeding the fistula and the target of embolization. It also looks separate from the jugular bulb and worth a subselective embolization attempt.

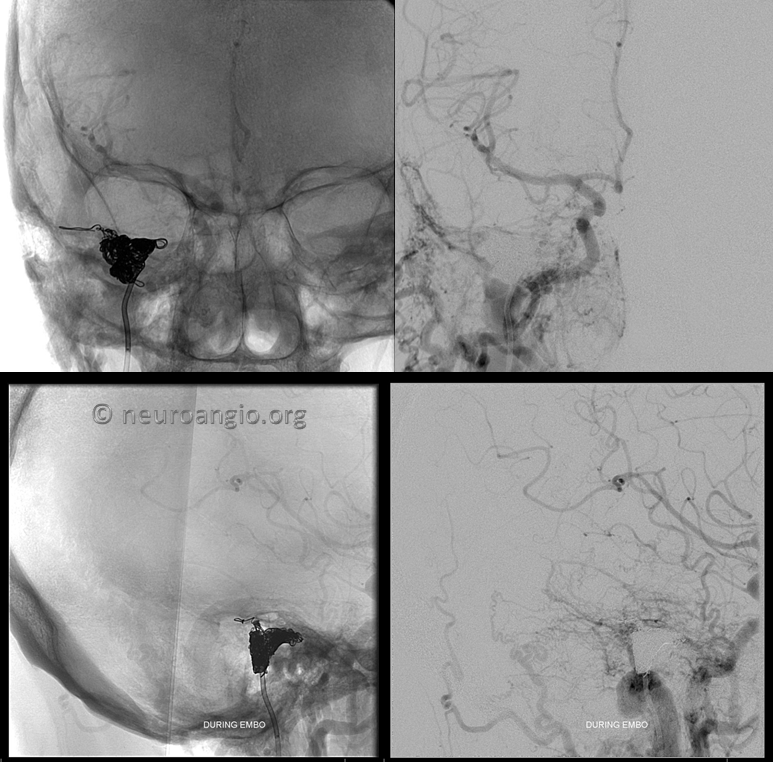
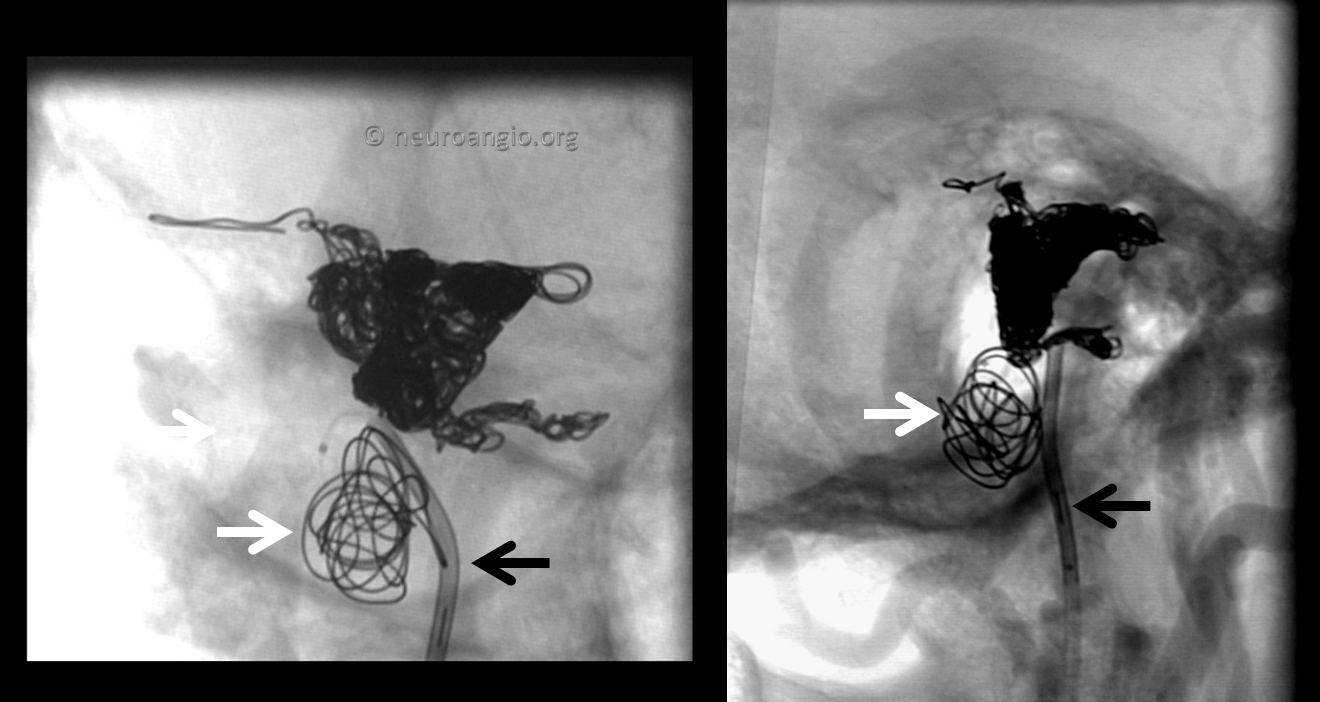
Between treatment and strategy, treatment is easier. Venous access is obtained. The target pouch is defined from the venous side
We start with the upper red arrow one

The middle meningeal contribution is now closed. The pouch lateral to the jugular bulb is next
Most of the supply is coming from occipital which dilutes this ascending pharyngeal injection
Fortunately the coils are staying in that pouch. The Vert catheter (black arrow) defines the location of the jugular vein and bulb, medial and anterior to the pouch.
Post-coiling. The fistula is gone and the jugular remains open.
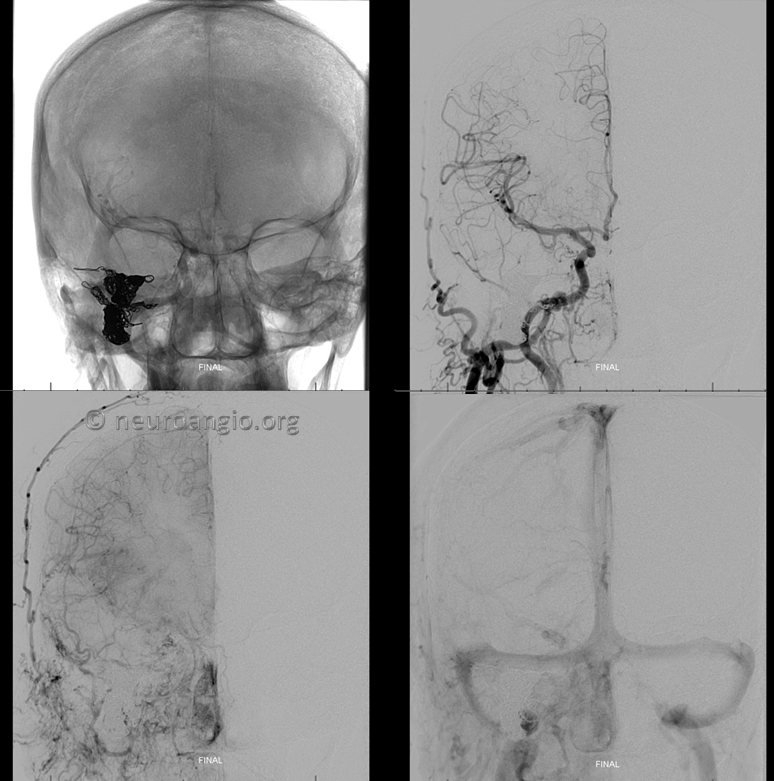
Lateral Views
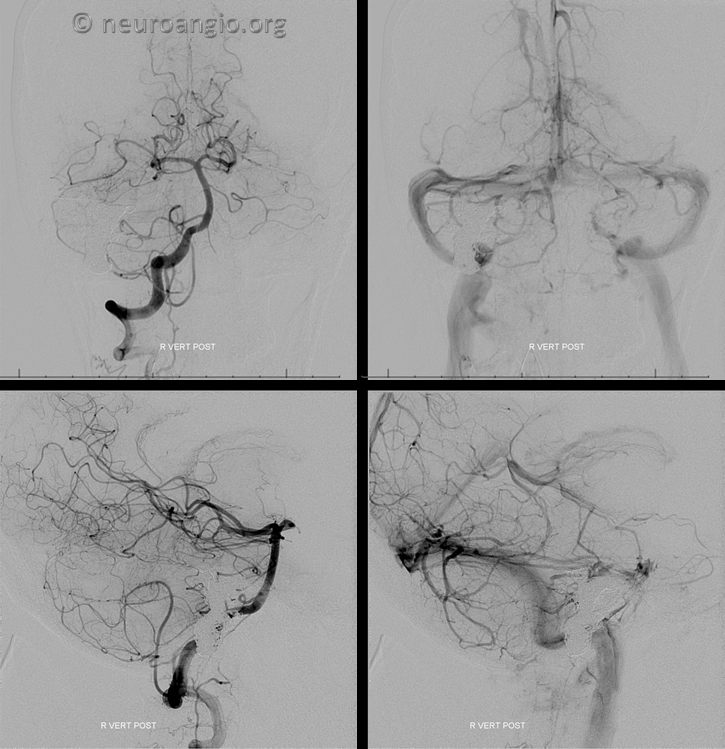
Control vert views. Nice patency of the sinus and jugular
Conclusion: The most important thing about dural fistula treatment is to understand where the fistula is. The location of fistula defines the embolization target. Frequently these targets are pouches alongside major veins or sinuses or vessels inside sinus wall. These can be superselectively embolized from the venous side with preservation of the sinus/vein and without risk associated with transarterial liquid embolic use.
Additional Cases
Literature
Mironov A. Selective transvenous embolization of dural fistulas without occlusion of the dural sinus. AJNR American journal of neuroradiology 1998;19:389-39
Piske RL, Campos CM, Chaves JB, et al. Dural sinus compartment in dural arteriovenous shunts: a new angioarchitectural feature allowing superselective transvenous dural sinus occlusion treatment. AJNR American journal of neuroradiology 2005;26:1715-1722
Caragine LP, Halbach VV, Dowd CF, et al. Parallel venous channel as the recipient pouch in transverse/sigmoid sinus dural fistulae. Neurosurgery 2003;53:1261-1266; discussion 1266-1267
Kiyosue H, Tanoue S, Okahara M, et al. Angioarchitecture of transverse-sigmoid sinus dural arteriovenous fistulas: evaluation of shunted pouches by multiplanar reformatted images of rotational angiography. AJNR American journal of neuroradiology 2013;34:1612-1620
Baik SK, Kim YW, Lee SW, et al. A treatment option for nontraumatic adult-type dural arteriovenous fistulas: transarterial venous coil embolization. World neurosurgery 2014;82:417-422
