Ethmoid Fistula Tranvenous Embolization
Case courtesy Dr. Cinthi Pillai and Dr. Eytan Raz, with Dr. Jeffrey Farkas showcasing a similar case in the NY Embo Club.
Transvenous embolization of dural fistulas is well-established, particularly for sigmoid, cavernous, and condylar types (see Dural Fistula Embolization page for various examples). Other dural fistulas are primarily managed by various endovascular means — transvenous, transarterial, or combined. The ethmoid dural fistula, located in the cribriform plate, and typically supplied by ethmoid branches of the ophthalmic artery, with primary venous drainage into a cortical vein rather than directly into a venous sinus (thus its increased hemorrhagic potential), is the only fistula i am aware of that still requires surgery as a primary treatment modality. The main reason is reluctance to perform transarterial embolization via the ophthalmic artery. That is a well-justified reason, if a potentially safer alternative, even if surgical, exists. However, surgery is not altogether benign — most cases require opening of the frontal (paranasal) sinus, which can lead to a number of issues — not usually as bad as blindness, but not pleasant either. There is however another way — transvenous. It can be technically challenging, because approach is long and usually tortuous. Catheters may not be long enough to reach anterior cranial fossa via femoral approach and navigation of frontal vein is not straighforward. However, we believe that it can and perhaps should be the primary option for ethmoid dural fistulas. When not feasible, surgery is a well-established backup.
In this case, transarterial nBCA embolization was attempted via a prominent and somewhat unusual middle meningeal route. When it proved insufficient, transvenous closure was achieved with jugular venous access, followed by catheterization of the anterior superior sagittal sinus using a 5F 115 cm Sofia distal support catheter, microcatheterization of the fistula with a headway duo, and closure with bare platinum coils . Case performed primarily by Dr. Eytan Raz
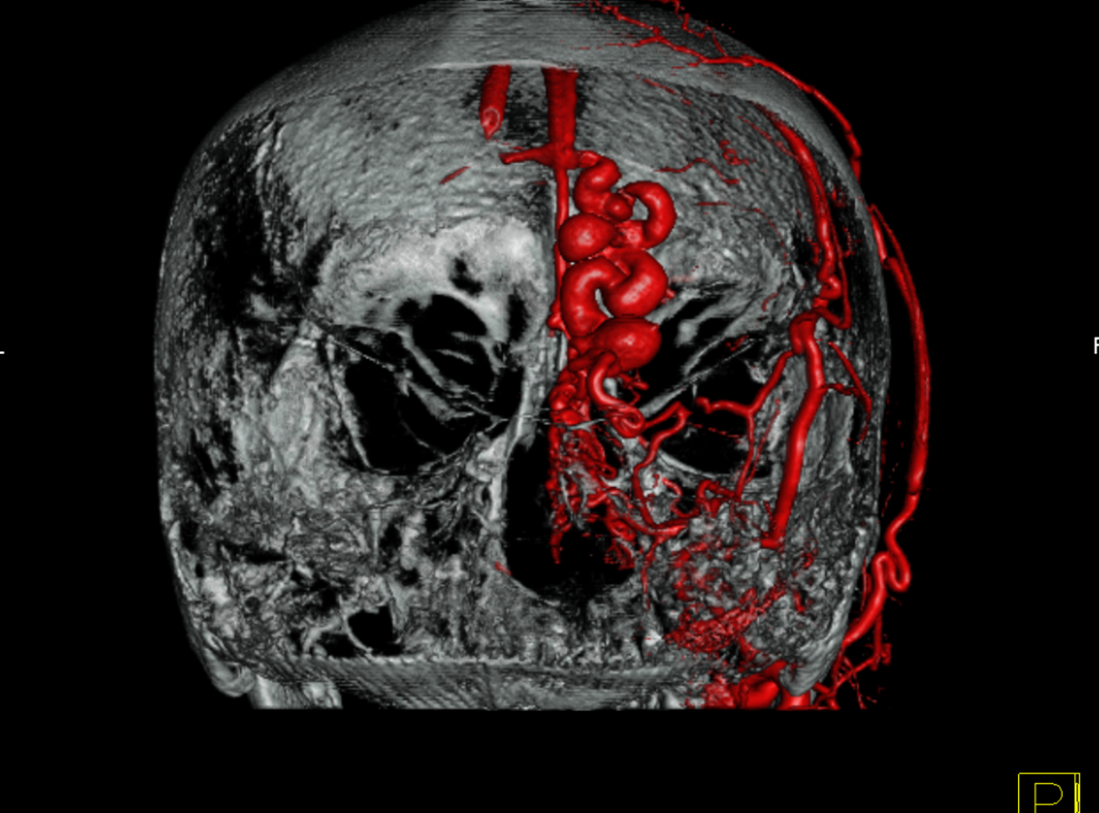
Patient presents with increasing headaches. Notice remote hemorrhage at right frontal base
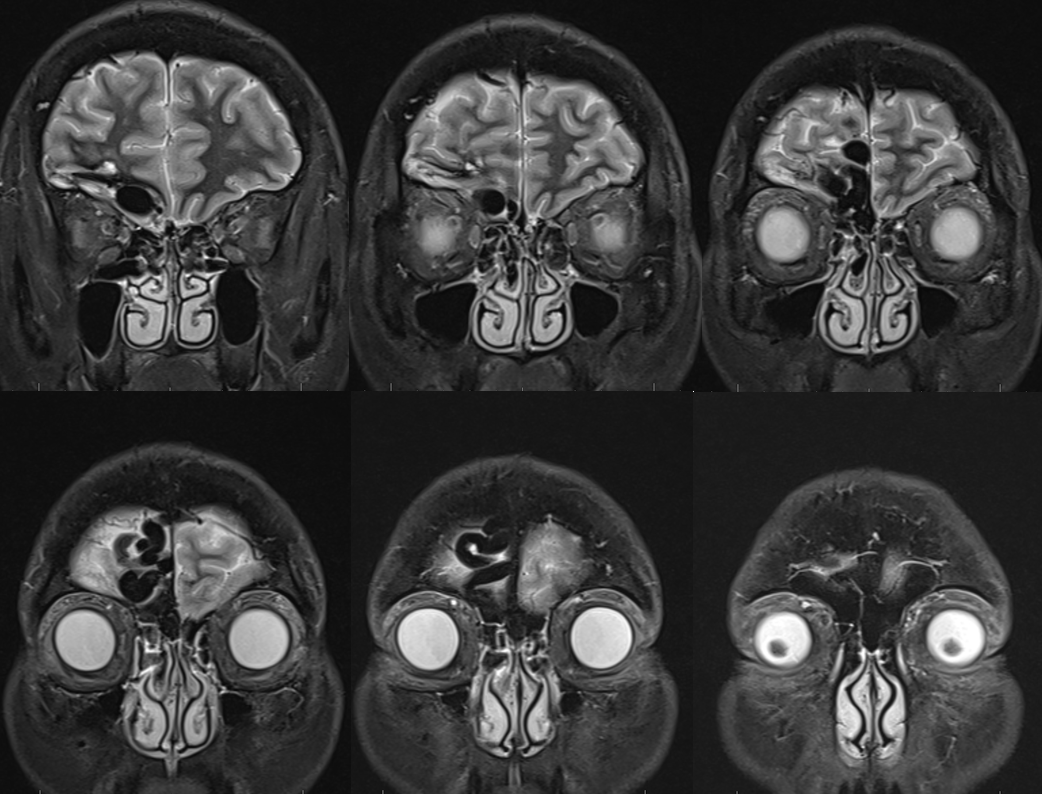
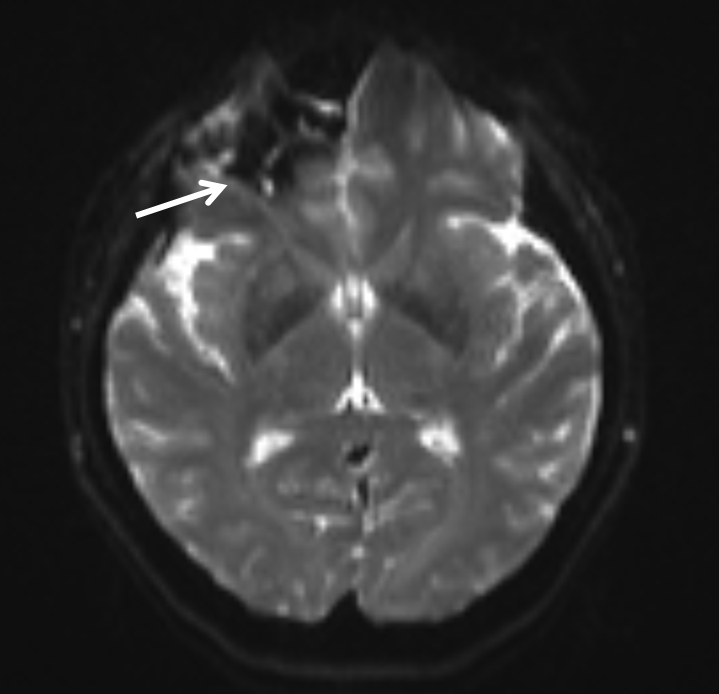
FLAIR with hemorrhage marked by black arrow. A subdural collection also seems to be present (white)
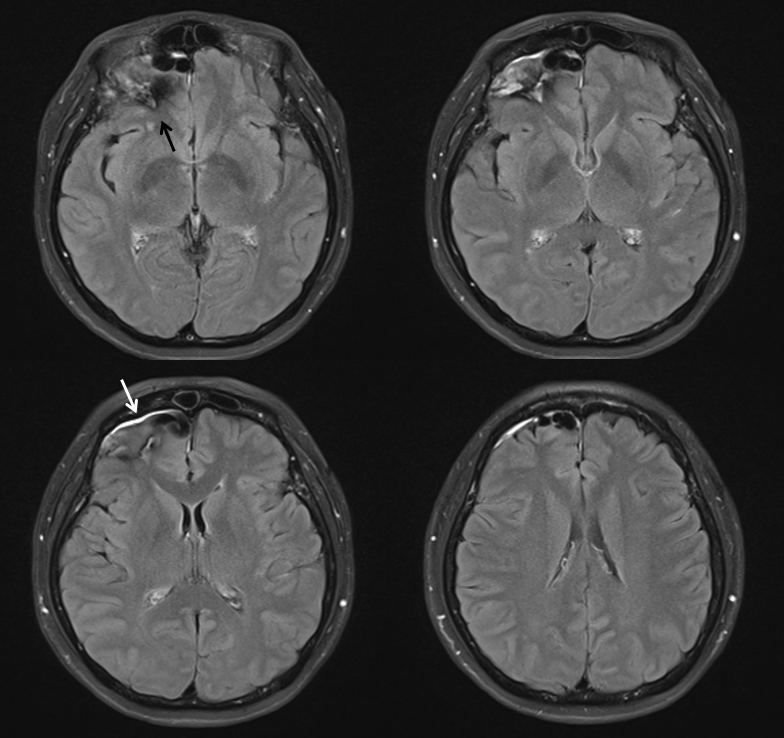
Hemorrhage on T0 of diffusion
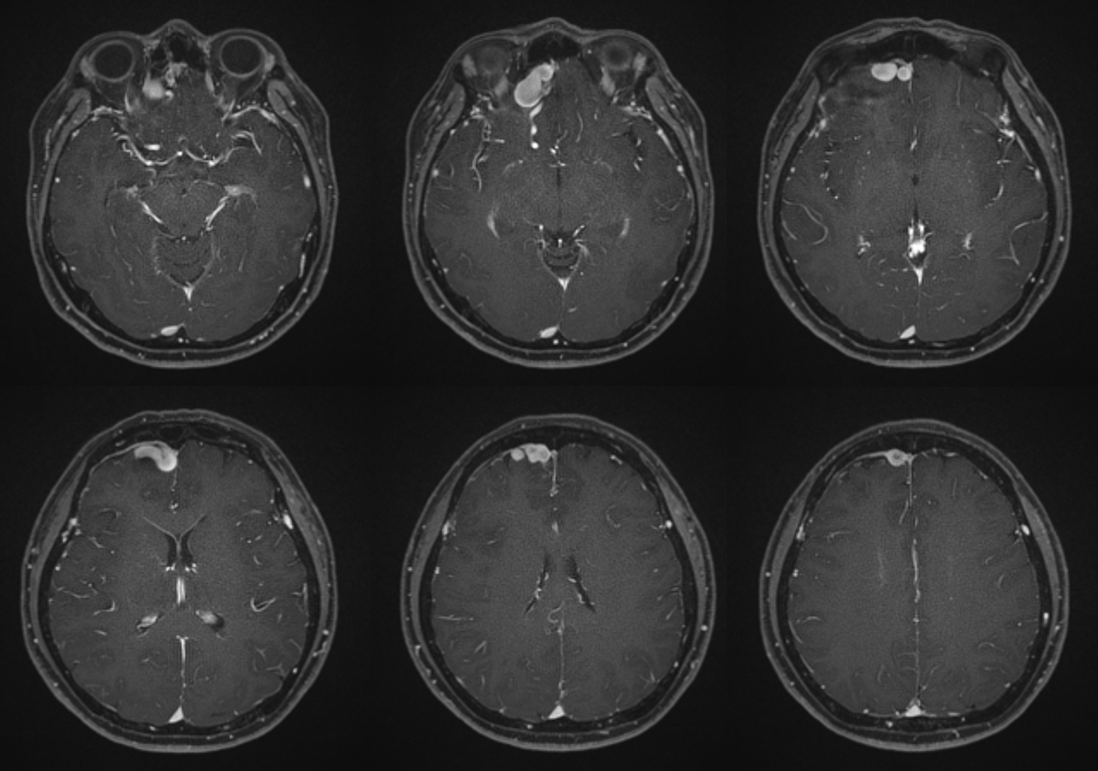
A subfrontal vein (not marked) extends posteriorly along the right gyrus rectus, in addition to main drainage via markedly tortuous and etcatic anterior frontal vein
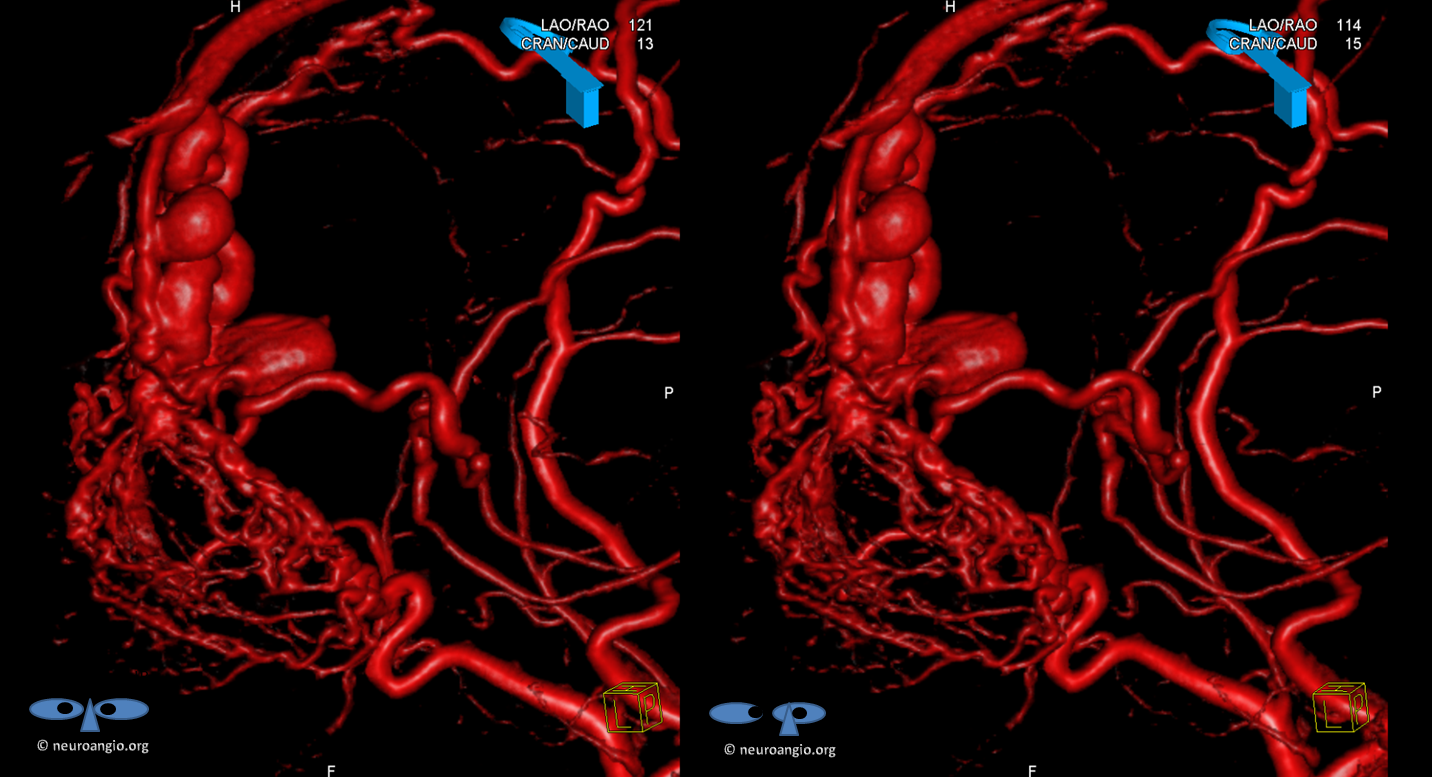
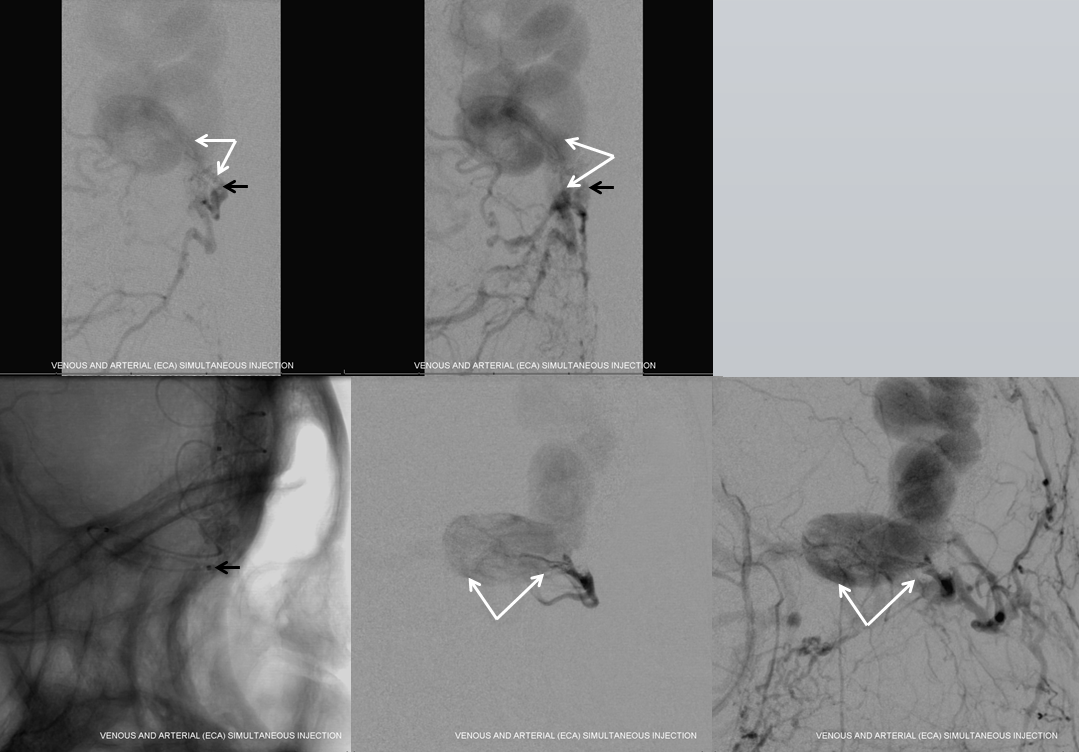
Right CCA injection shows unusually prominent middle meningeal artery (black) supply of the fistula via a beautiful anterior falcine vein (white arrows) which runs in the wall of the superior sagittal sinus
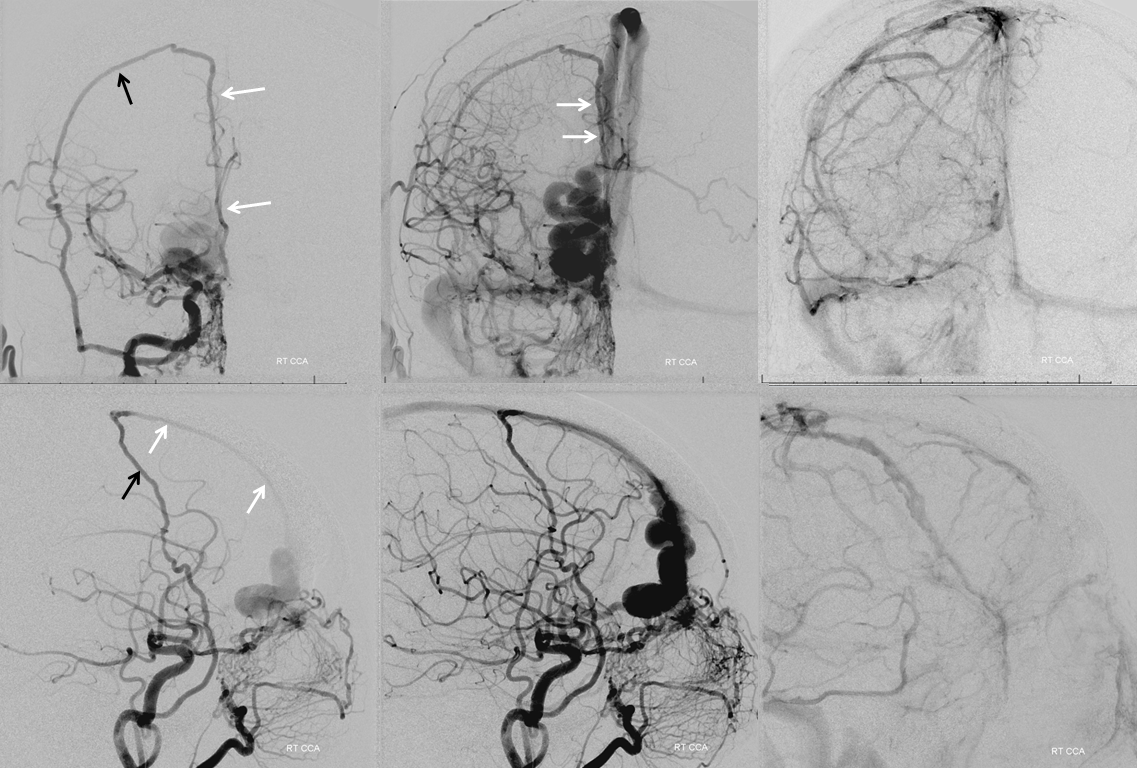
Stereo views, awesome
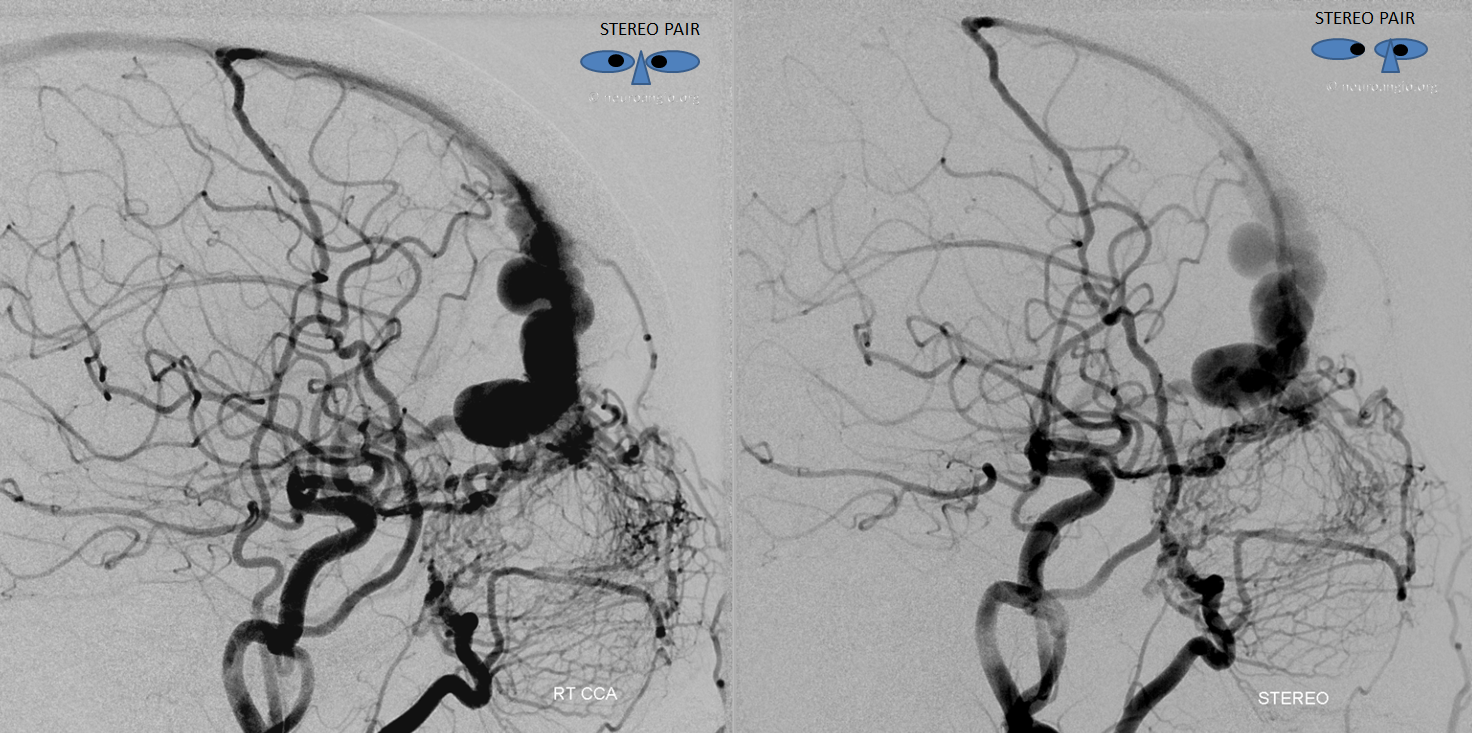
Key image of venous drainage. The main draining vein into the superior sagittal sinus is easy to see. There is however also present an anterior cerebral vein (white arrow) which was seen earlier on the T1-post MRI running along the right gyrus rectus. This vein drains into the basal vein (black) as well as into the right middle cerebral vein (purple) and then into the superficial sylvian veins (blue), one of which is connected to an anterior frontal convexity vein (pink) that drains into the sagittal sinus. The rest of superficial sylvian veins (blue) drain into the superior petrosal sinus (not shown). See superficial venous system and deep venous system pages for more anatomical info. This image is key to understanding cerebral venous congestion caused by this large fistula
Stereo images of venous drainage are amazing
Stereo views of right ICA injections. The right ophthalmic artery to ethmoid arteries connection is hypoplastic, which is why the normally dominant ipsilateral ophthalmic is not contributing much in this case
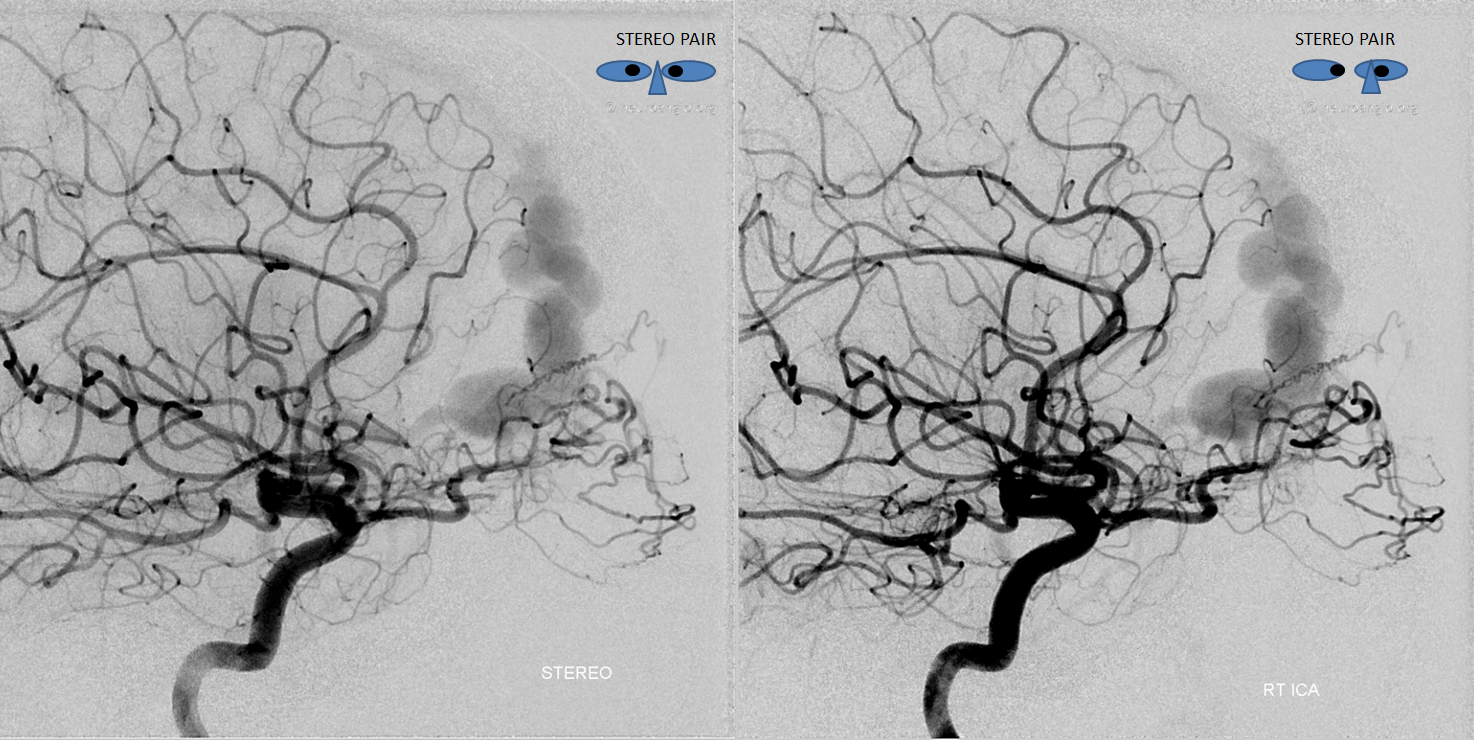
The right ethmoid arteries, and therefore the fistula, are primarily supplied by the external system, including the MMA and multiple septal arteries arising from the sphenopalatine branch of the IMAX
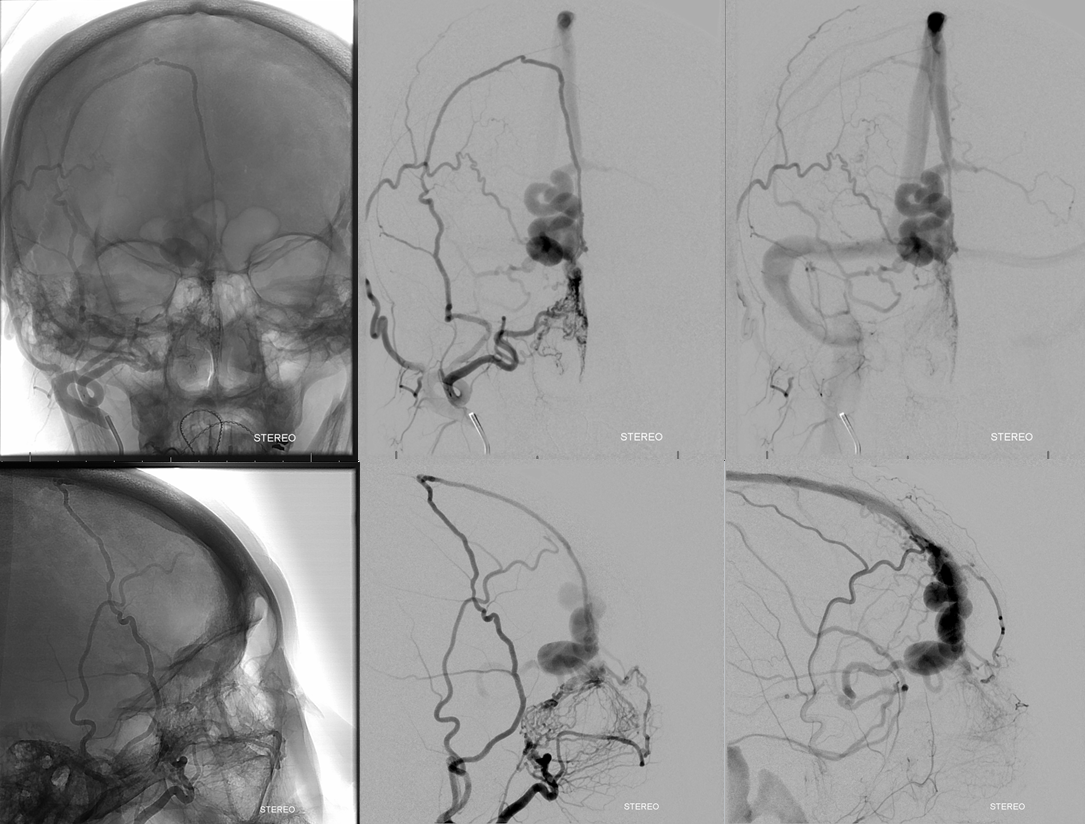
Stereo views of right external carotid injection
Left External carotid injection. The same right ethmoid arteries are also supplied by the septal branches of the left IMAX. Makes sense
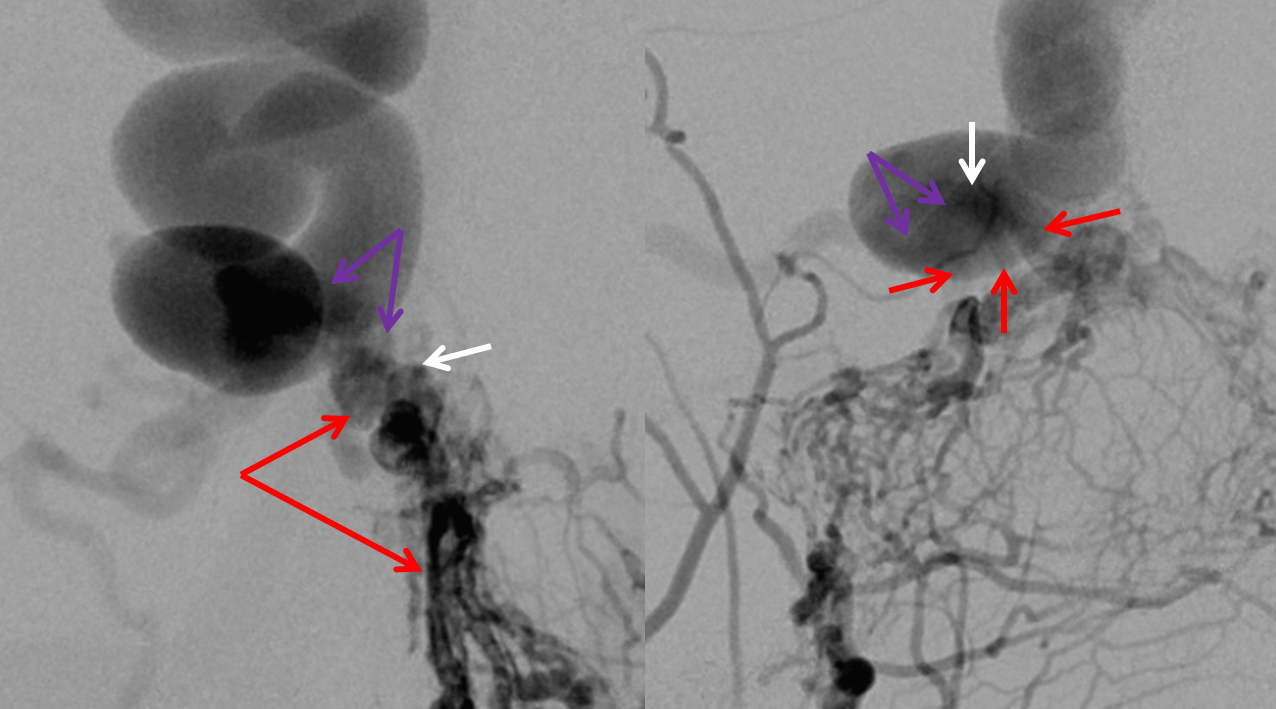
A close-up view of the fistula region is key to understanding what’s going on. We believe that most fistulas are single-hole arteriovenous connections. They look complicated angiographically but most are really only one hole. Our treatment strategy supports this view. Red arrows show dilated arterial ethmoid channels converging on one hole (white arrow, best seen in lateral view). The proximal draining venous segment is purple. Many would disagree with this assessment. Our strategy is to place embolic material, whatever it is, at the fistula and into the proximal draining vein.
View from the back
Volume rendered views. Various arterial contributors are labeled with white arrows. The proximal draining venous segment is purple, anterior frontal vein running along gyrus rectus is yellow, and proximal venous aneurysm is blue.

Stereo views, medial to lateral
Similar views with similar color arrows including bone (dual volume reconstruction.) Crista Galli black arrow

Stereos
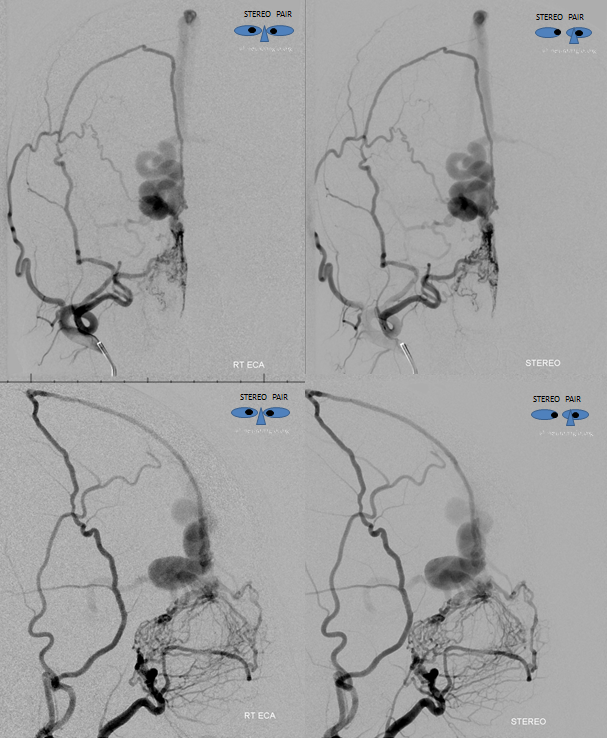
First, a relatively distal position is achieved via catheterization of the MMA
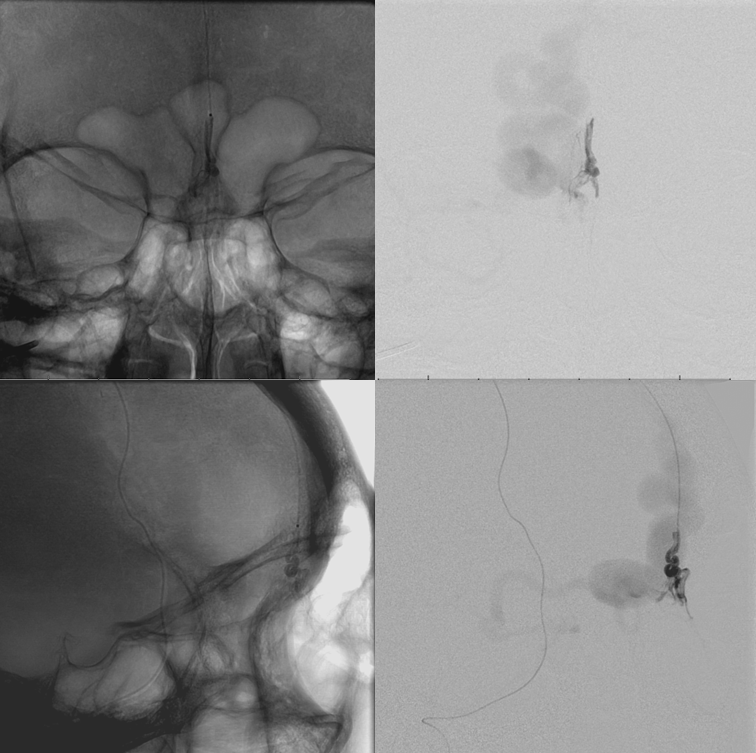
nBCA cast — although the fistula is penetrated with some nBCA deposition into the venous system (white), it is not enough
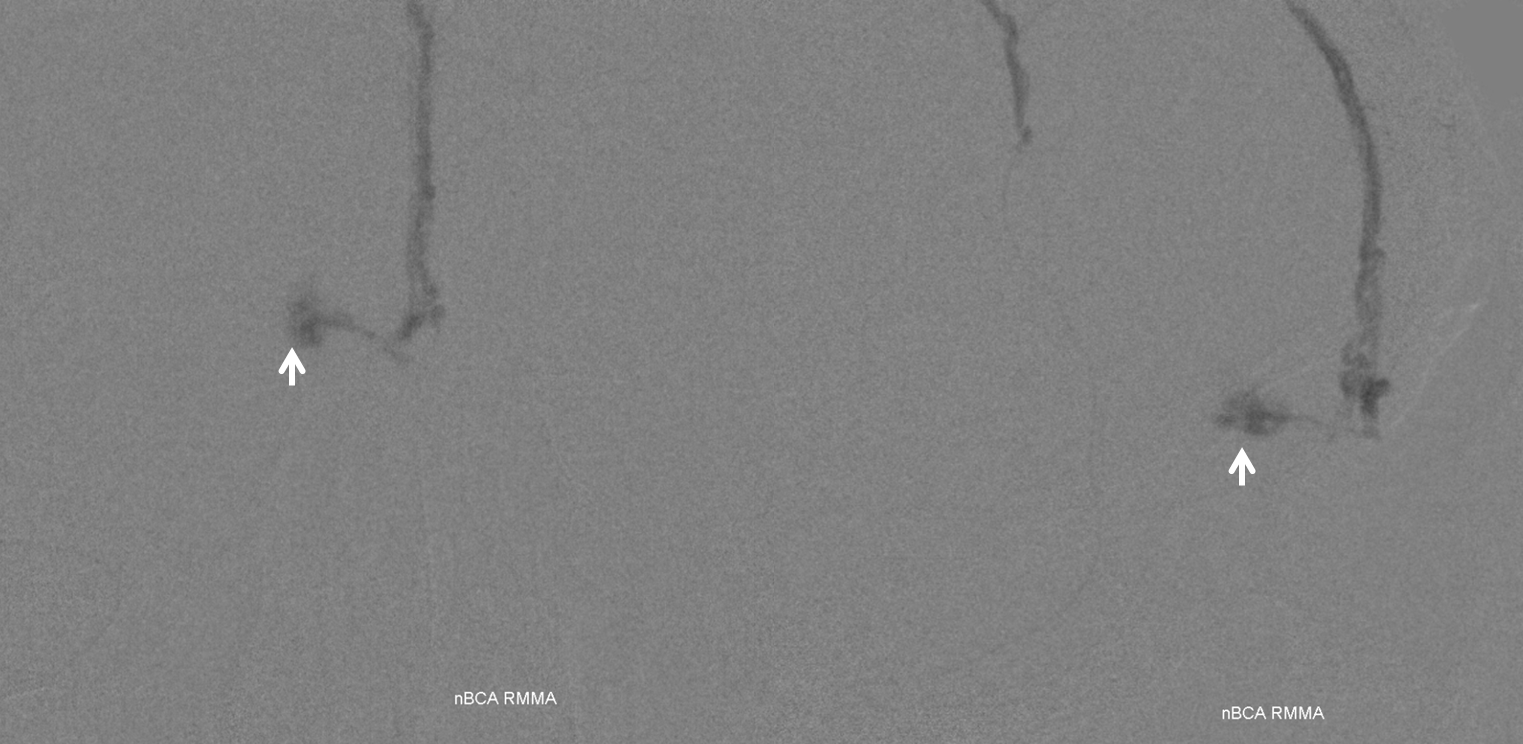
The fistula (white arrows) is still very much alive
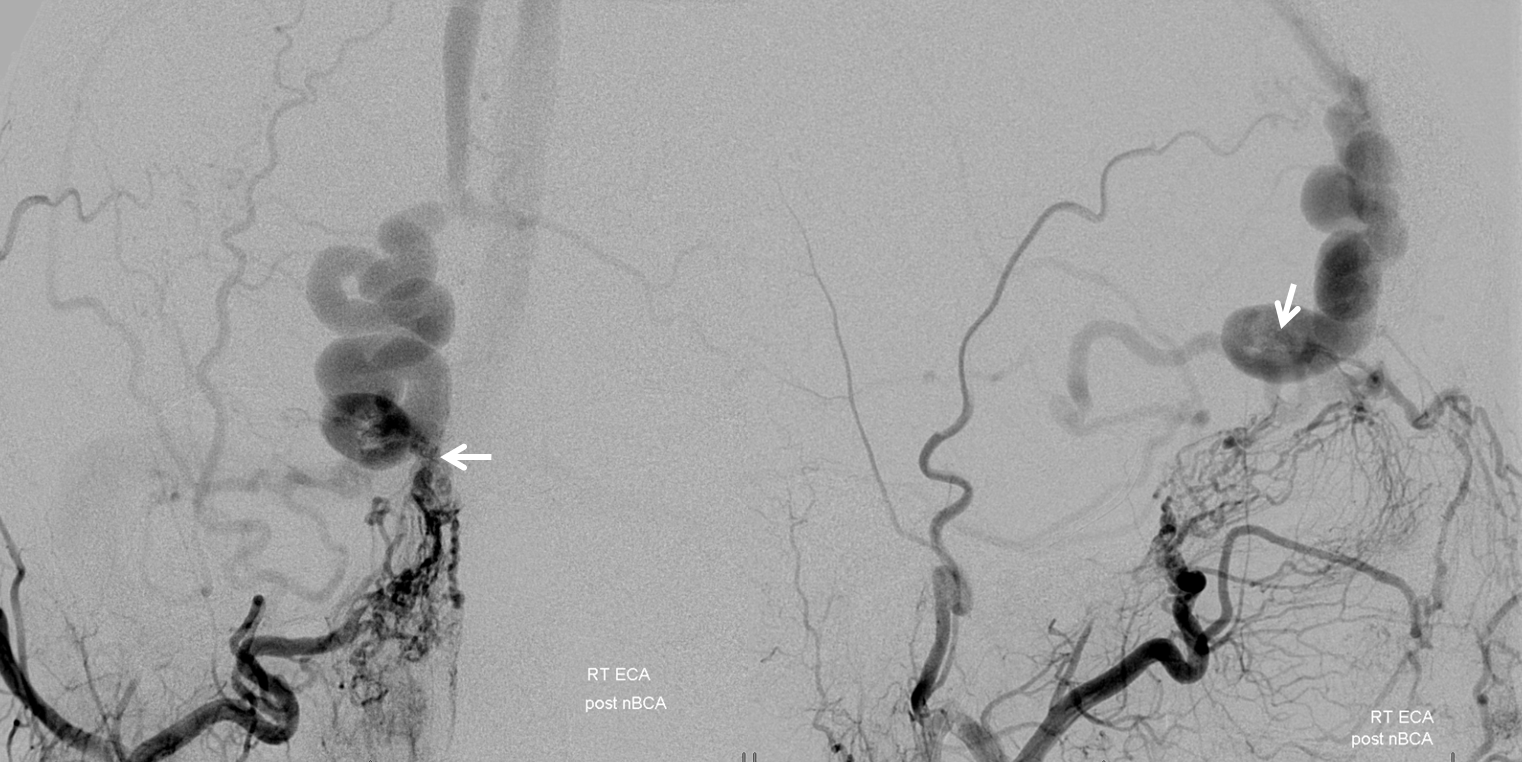
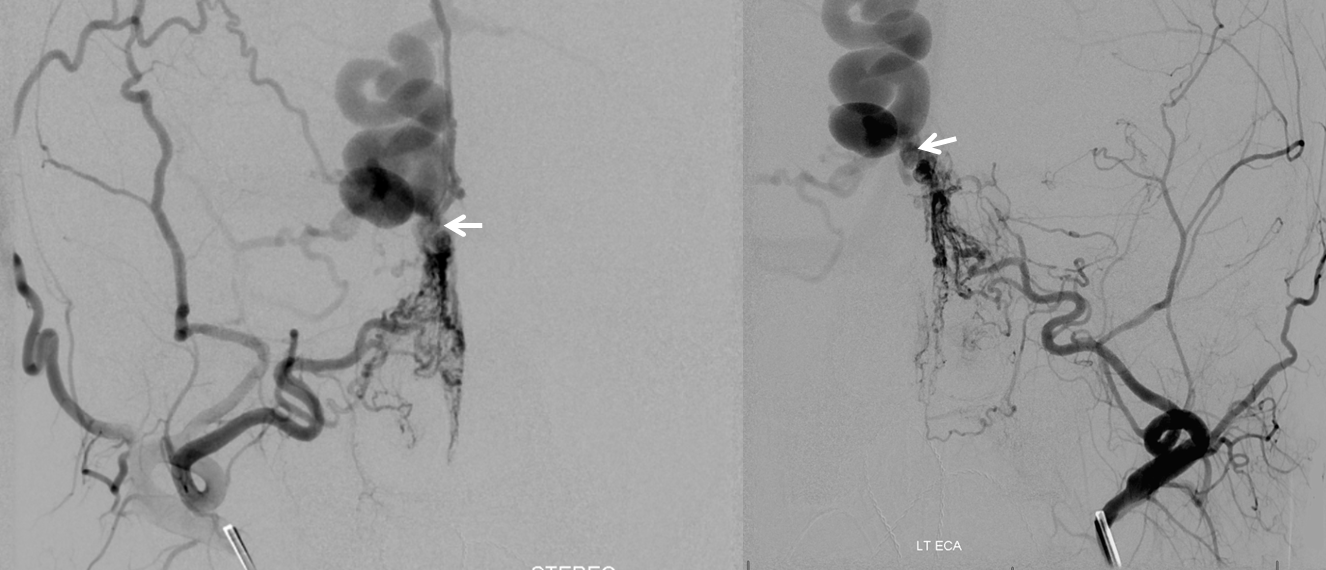
Another frontal view of the fistula (white arrows) from both right and left external injections
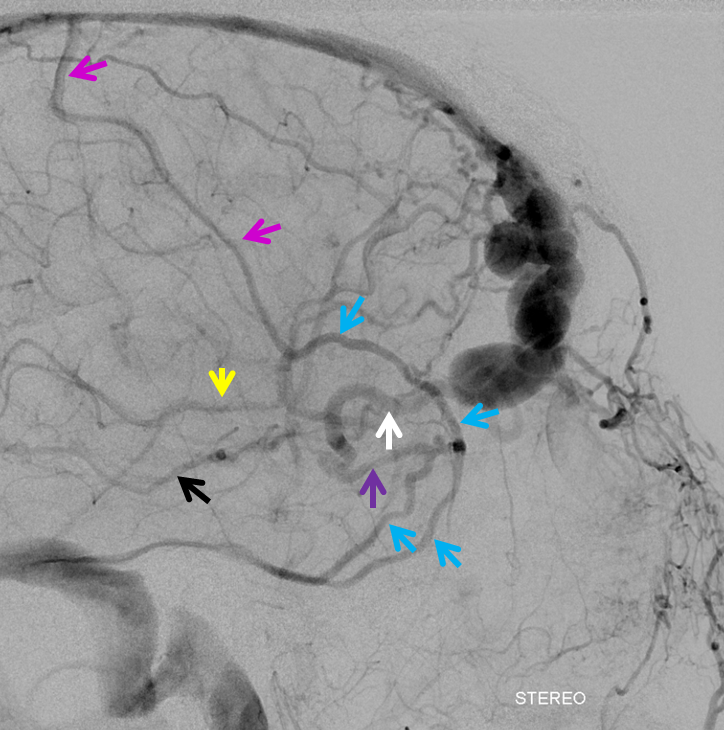
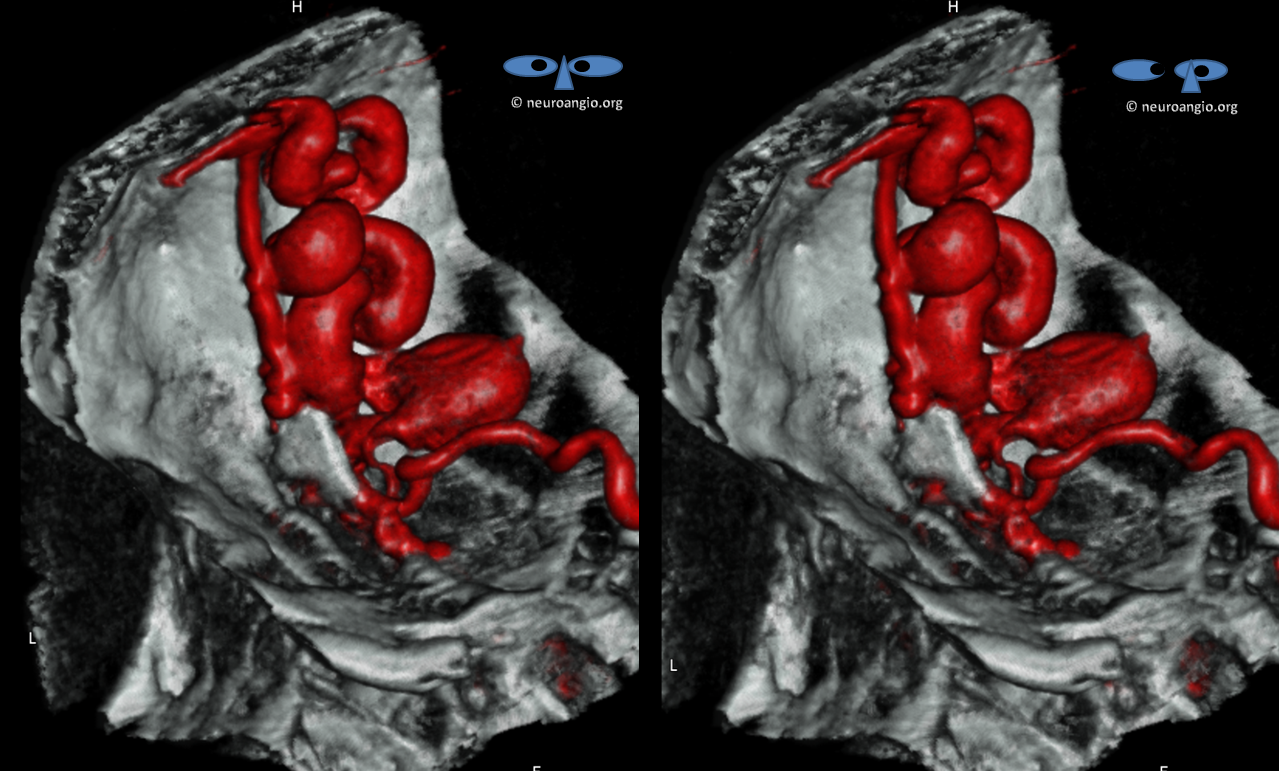
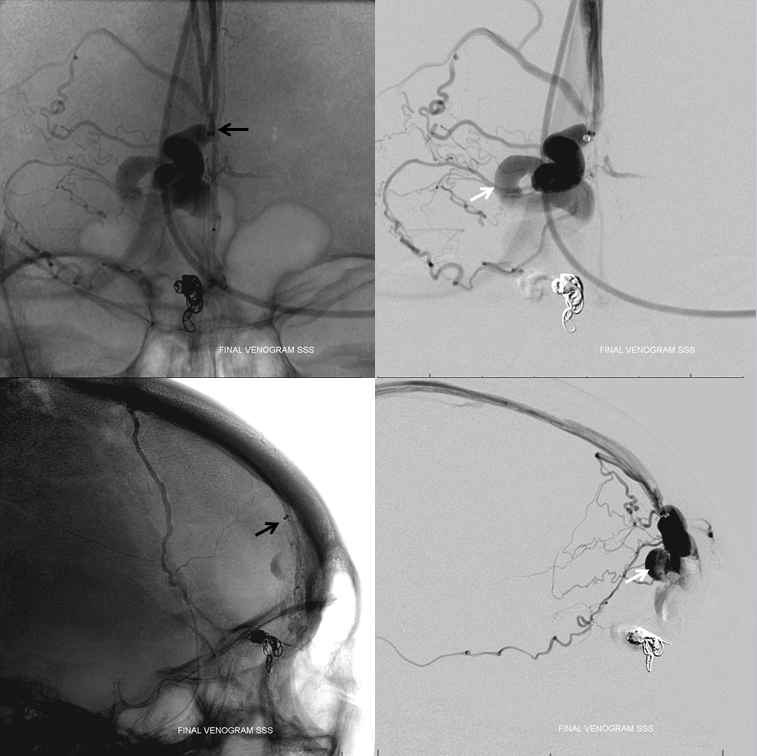
Transvenous access. A 5F short sheath is placed partially into the LEFT jugular vein, facing up, under ultrasound guidance, by Dr. Jonathan Gross of vascular interventional radiology, who is much more adept at jugular venous access than we are. Next, a 5F Sofia 115 cm catheter is navigated over Headway Duo and Synchro 14 Soft into the anterior aspect of the superior sagittal sinus, just to the point where dominant frontal vein drains into the sinus. Then, via right external carotid arterial roadmap, the vein is retrogradely catheterized all the way to the fistula. This was achieved by a combination of skill and luck, with the headway duo hubbed against the 5F Sofia at the end. The tip of catheter is marked by black arrow. The catheter is located in arterial pouch, having traversed the fistula point. White arrows show location of proximal vein where coils are to be placed
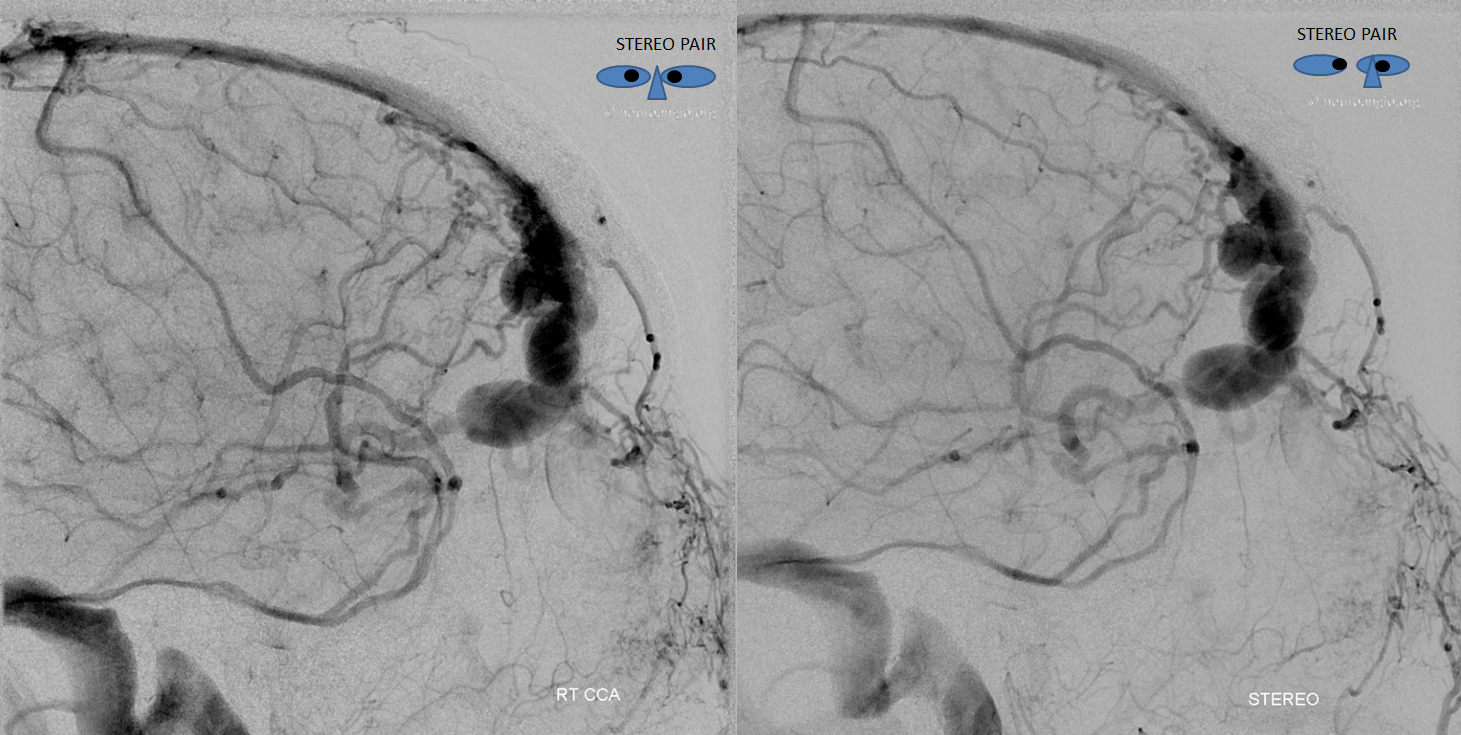
Coiling views, with reference images below showing location of coils in proximal vein and fistula (white arrows)
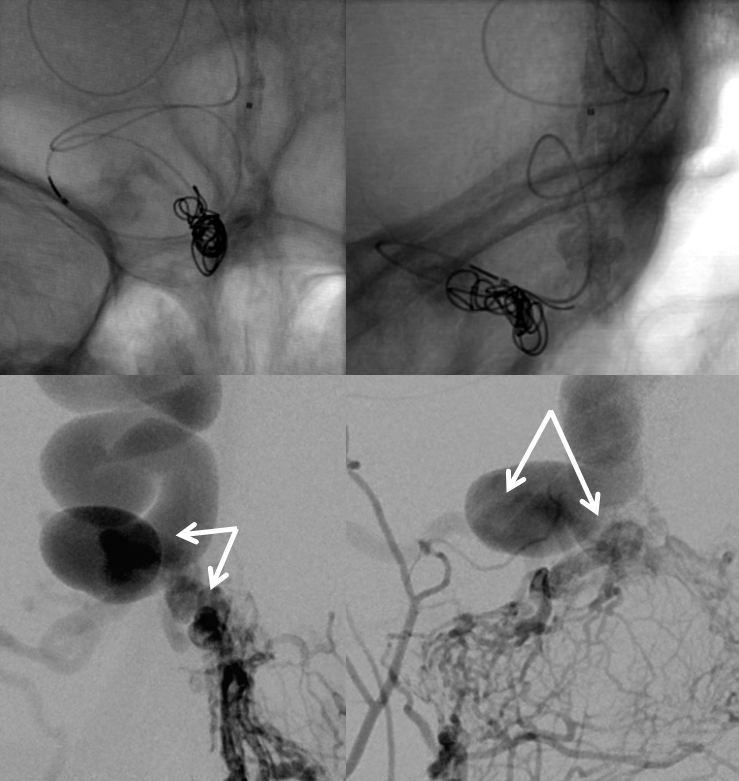
Post-coil frontal right external views. Part of coil mass traverses fistula and protrudes into the arterial side below

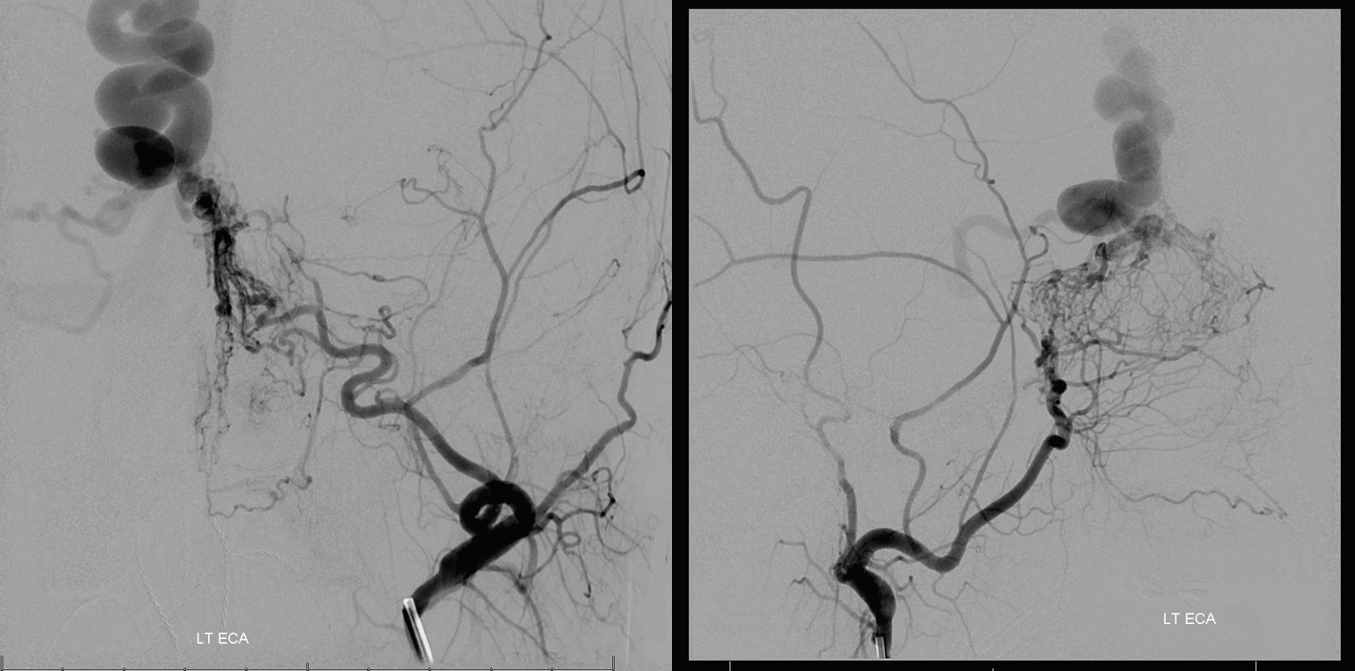
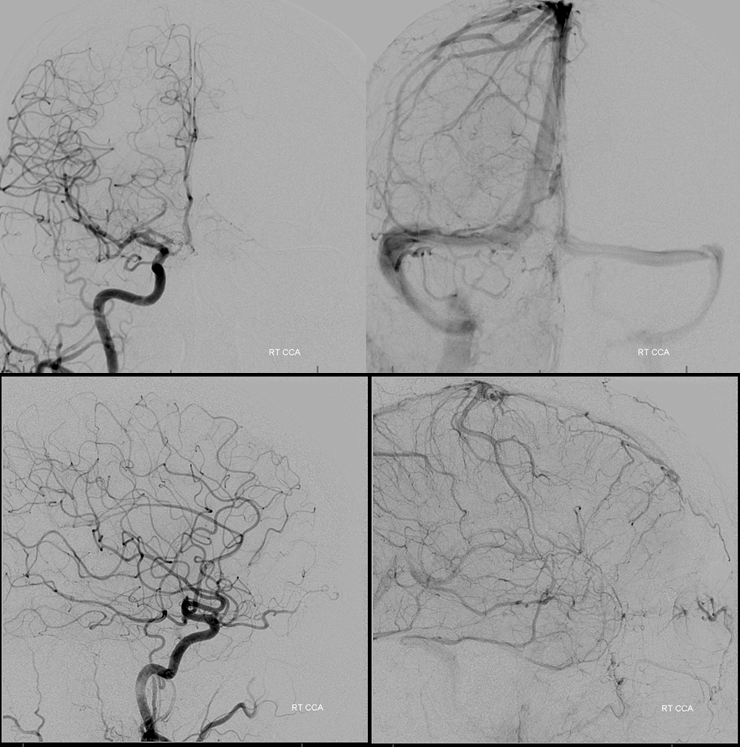
Right common carotid artery views
Left external carotid artery injection, with stasis in now non-fistulous ethmoid arteries
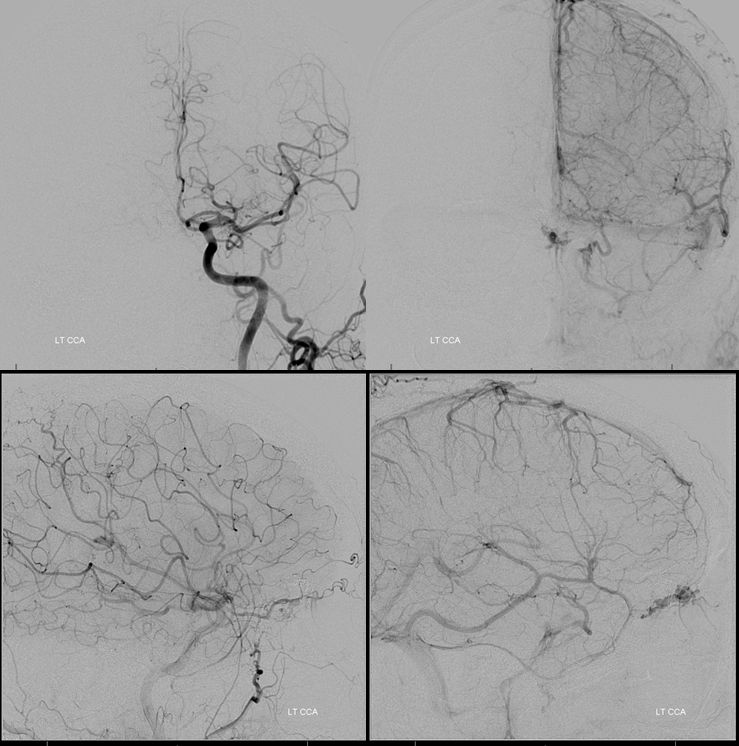
Finally, an unnecessary but instructive injection of the 5F Sofia in the anterior aspect of the superior sagittal sinus, demontrating contrast stagnation in the large, now non-fistulous frontal vein, with some retrograde reflux into frontal veins previously congested by the fistula
Further reading:
https://www.ncbi.nlm.nih.gov/pubmed/29180085
Other neuroangio pages:
