Sphenoparietal Sinus (also known as Greater Wing of Sphenoid) Dural Fistula
A STEREO ANAGLYPH STORY — get your red-cyan anaglyph glasses and experience the beauty of stereo angiography
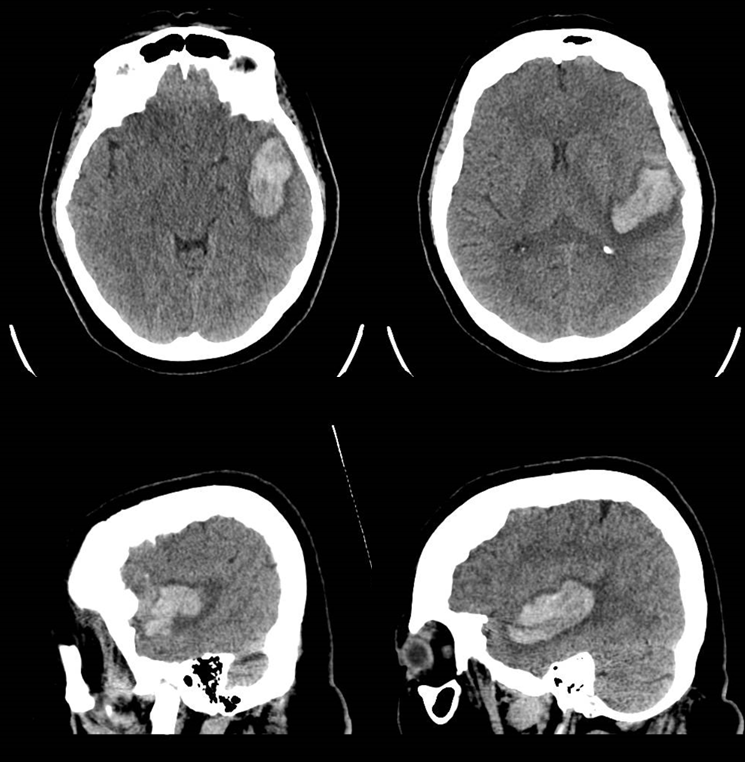
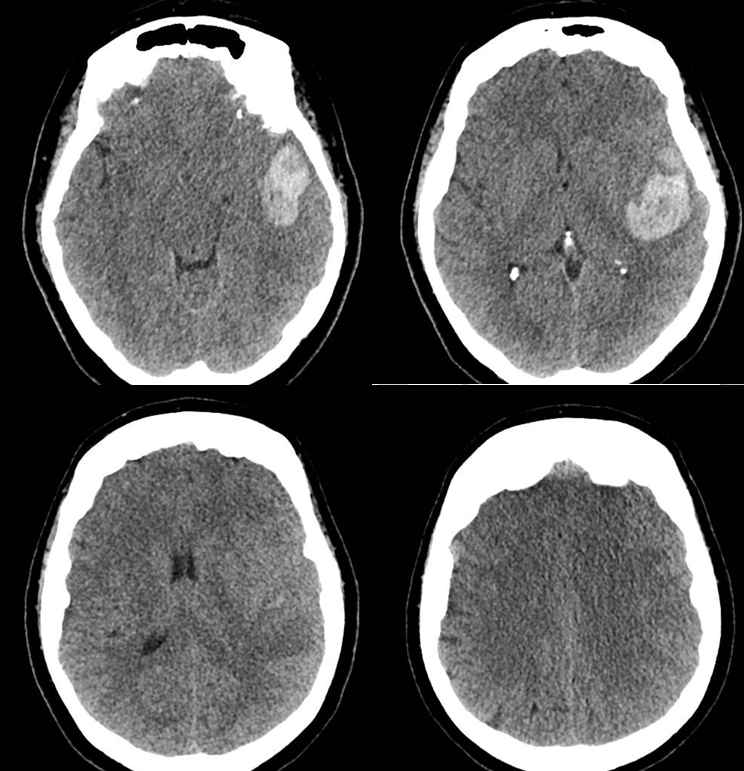
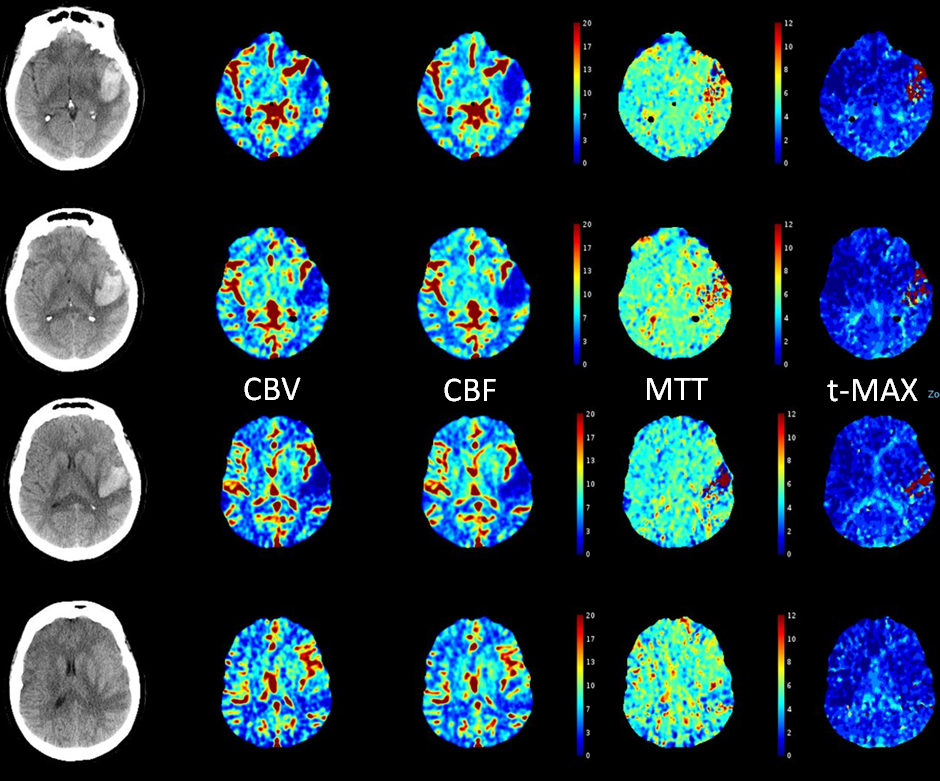
This is one of the rarest dural fistulas out there. However, as for all of them, regardless of location, the common theme is the same — degree of vascular congestion determines symptoms. This is reflected in the enduring value of Cognard and Borden classifications — the more cortical venous reflux, the more brain venous congestion, the more brain dysfunction, such as hemorrhage. Here is a case in patient presenting with a mixed aphasia. CT shows parenchymal hematoma
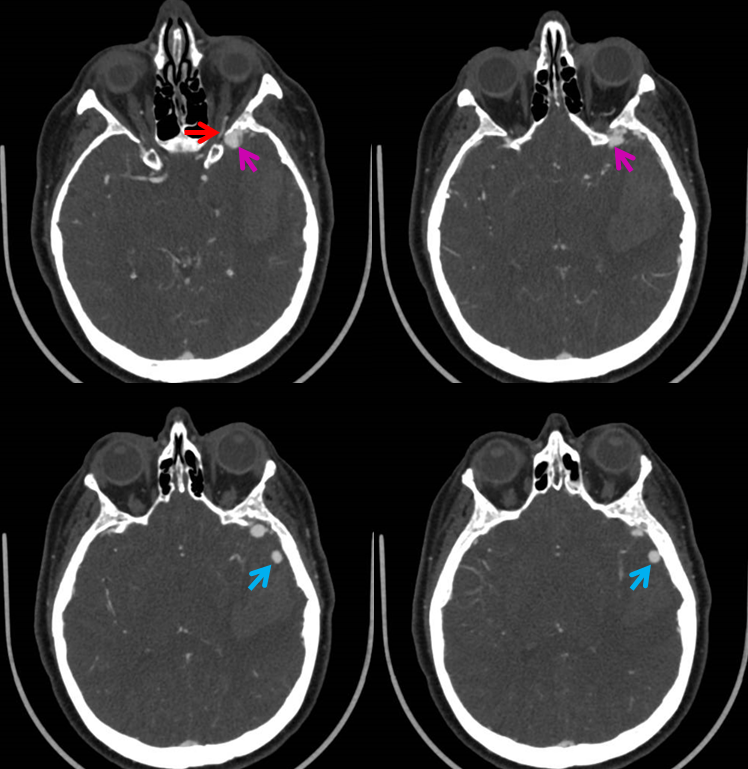
CTA (Ophthalmic artery = red; proximal venous pouch = pink; venous aneurysms = blue
This time, there are no arrows. We will let the pictures speak for themselves
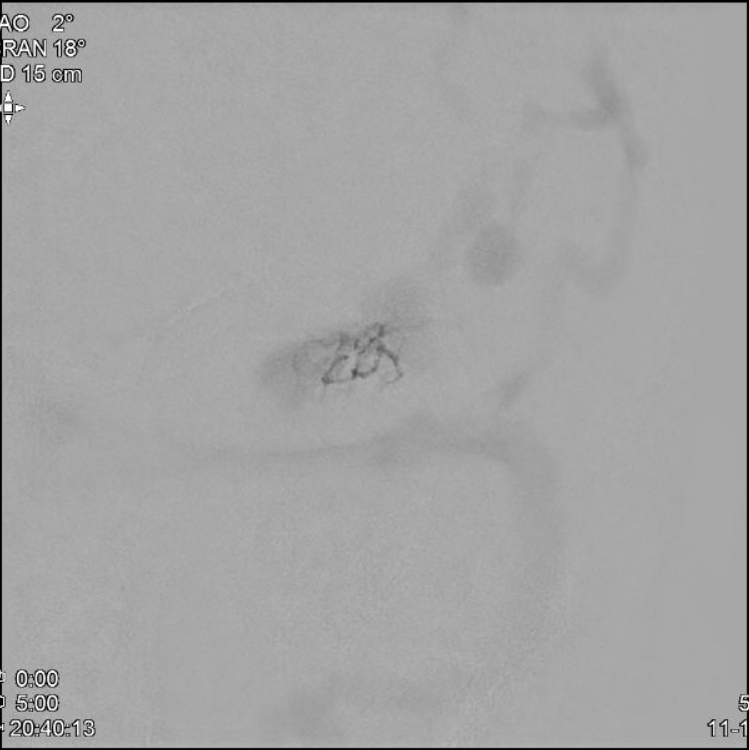
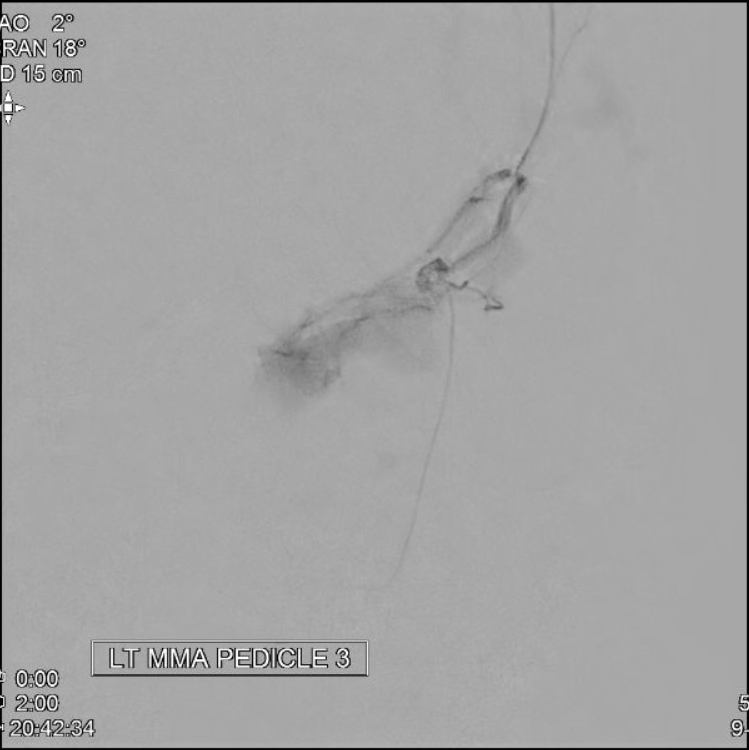
EMBO (non-stereos)
MMA pedicle 1 frontal
MMA pedicle 1 lateral

MMA Micro Pedicle 2


MMA Micro Pedicle 3

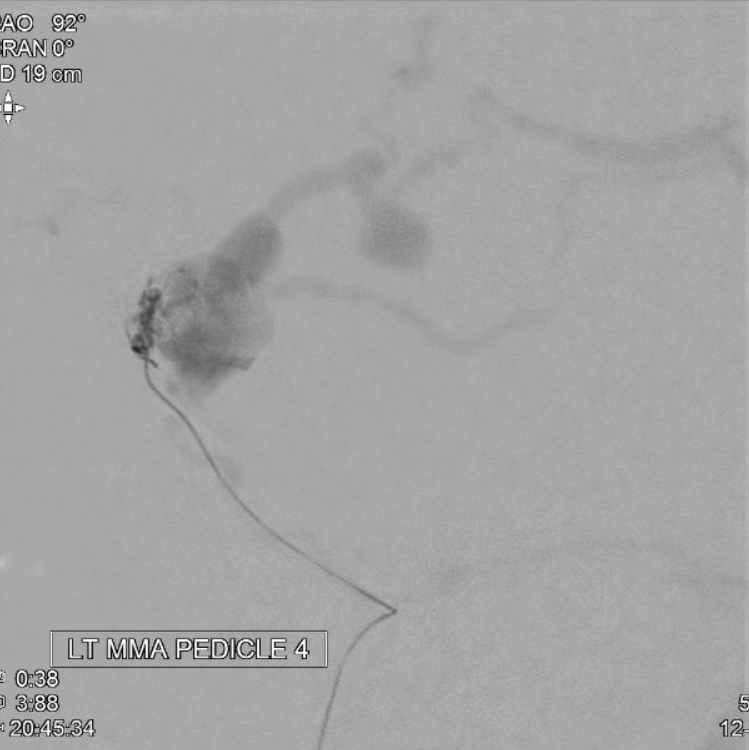
MMA MICRO PEDICLE 4

nBCA (50:50) PEDICLE 1


nBCA (50:50) PEDICLE 2
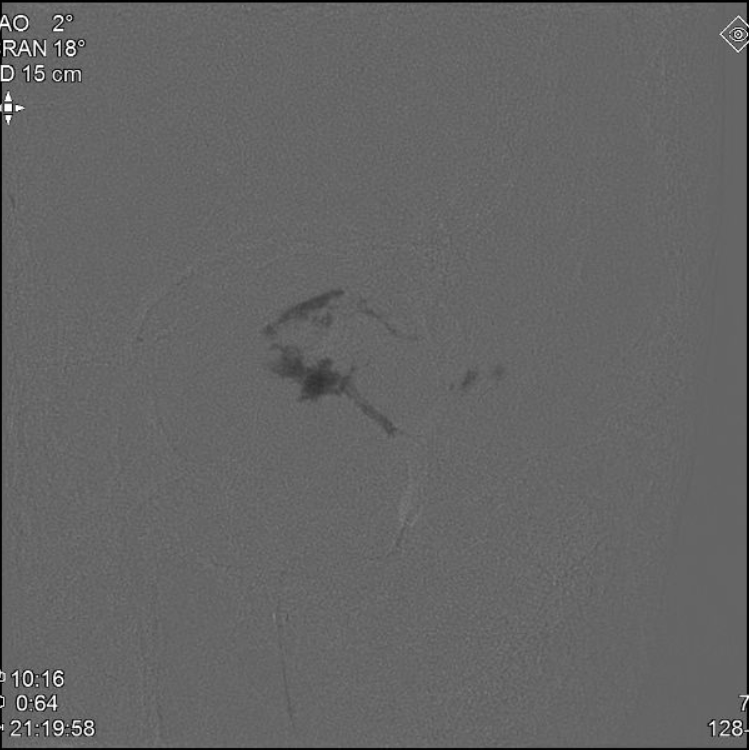


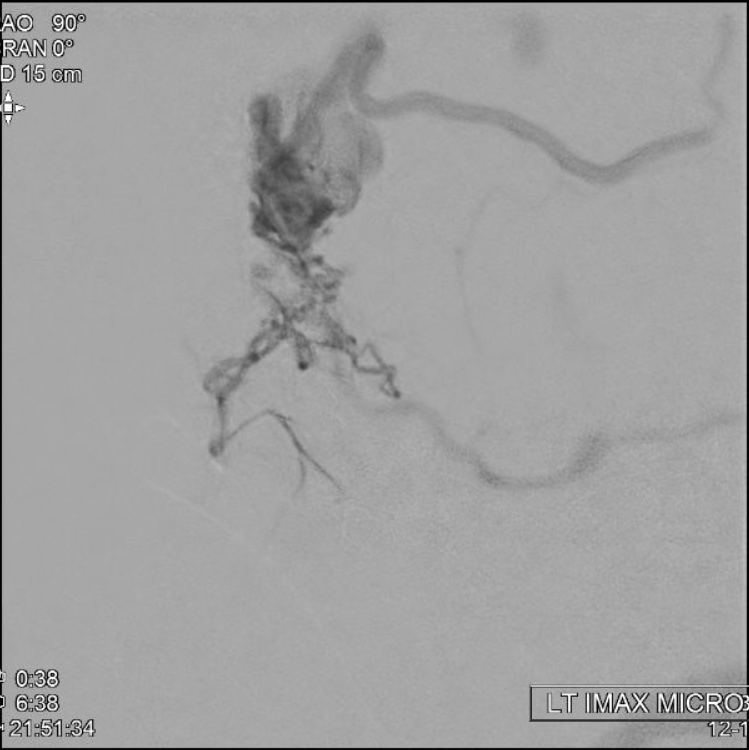
nBCA (30:70) IMAX


IMMEDIATE POST EMBO
IMMEDIATE POST CTA
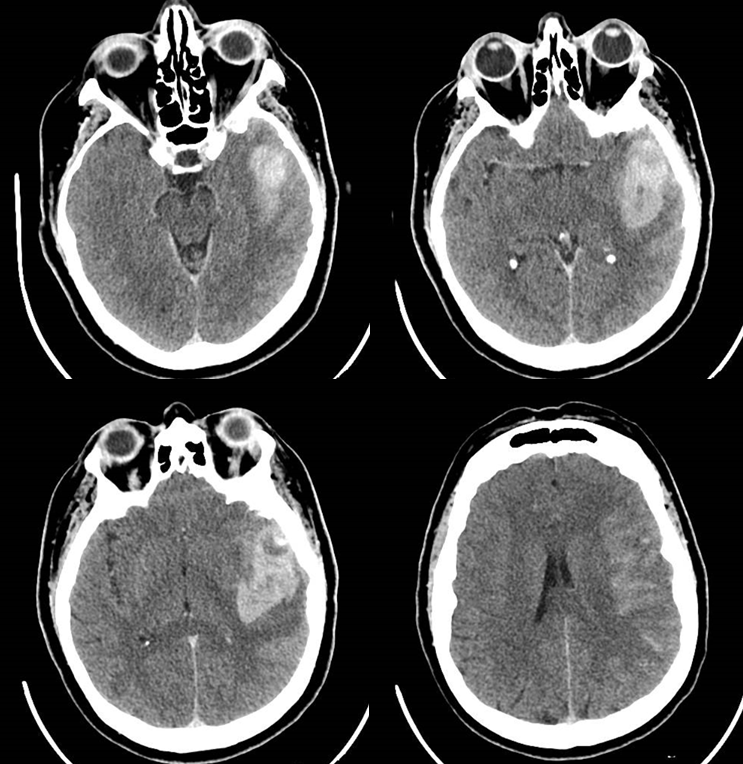
24 HOURS LATER
Bone windows. yellow = nBCA imax rotundum; purple = nBCA proximal venous pouch
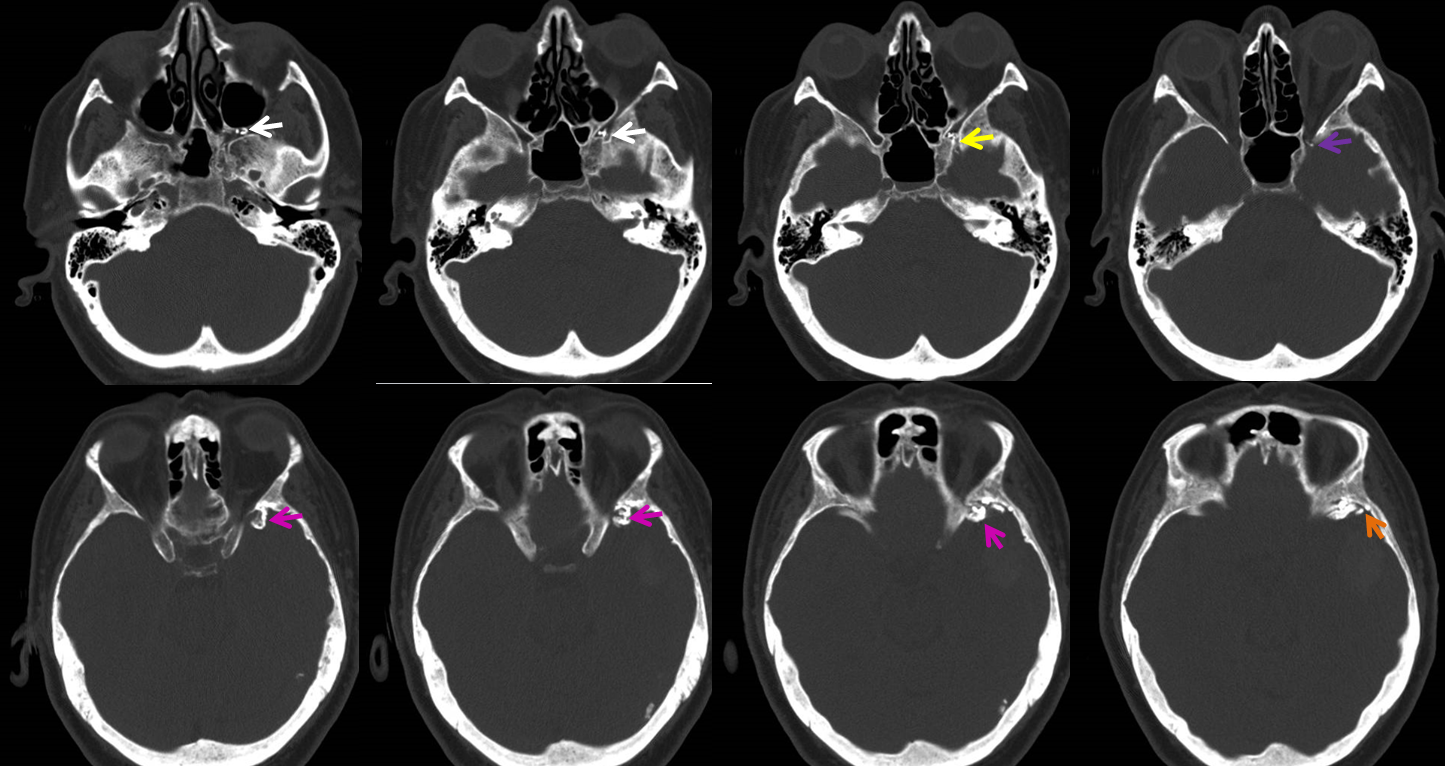
3 days later; nBCA = pink; residual opacification of venous pouch = purple; inferior sylvian vein = blue; the larger superior sylvian vein (the one with aneurysms) has thrombosed
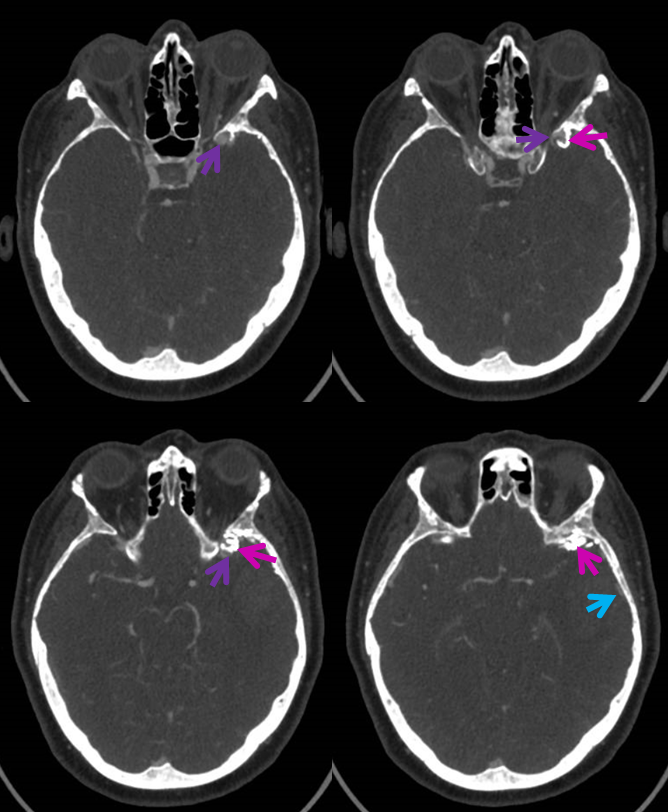
Angio two days later. Fistula progressed to occlusion. Temporal lobe drainage continues to proceed mainly via basal vein which empties in variant fashion via lateral mesencephalic vein into the superior petrosal sinus. Contrast is seen filling the venous fistula pouch in late phase, with no outflow
Venous phase PRE embo and POST embo images
The Labbe, previously used by the fistula (left image) is now seen in the venous phase of the brain (right). Hopefully things will continue to improve as hematoma resorbs and Labbe will be back in honest business
CT perfusion obtained for monitoring of spasm; post-perfusion venous phase, next day. No filling of venous pouch
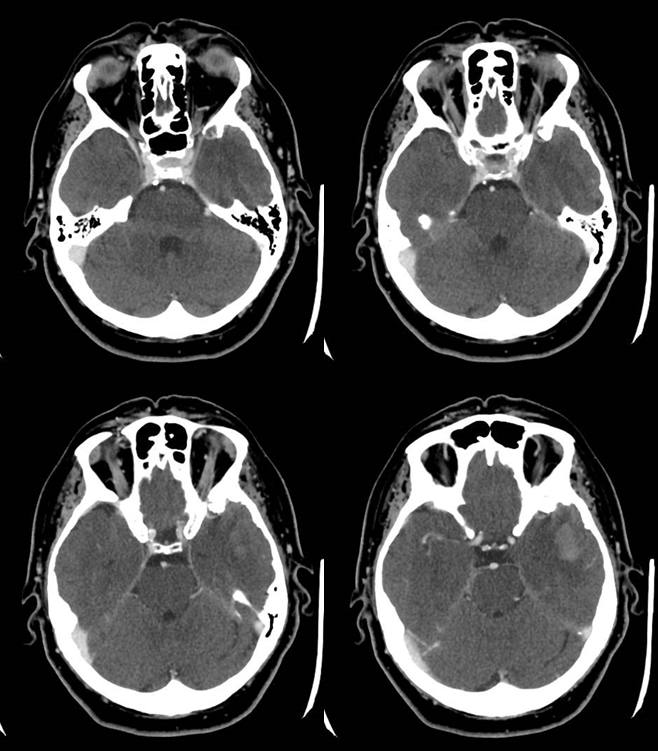
RAPID analysis. Interpretation requires knowledge of perfusion as in this setting evaluation of possible arterial hypoperfusion is coupled with venous congestion, so the dichotomized core/penumbra RAPID maps should be viewed with caution
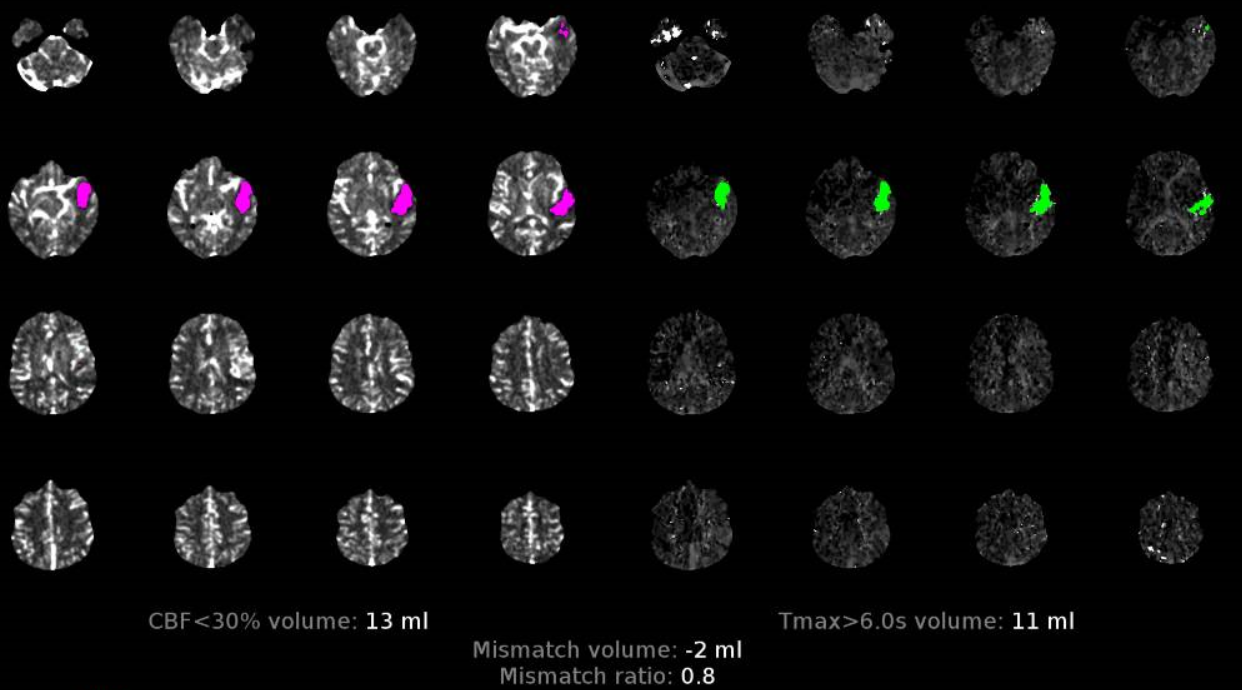
The effect of venous congestion in perfusion is to increase CBV, MTT, and Time to Drain (TDD). The latter is probably the most useful measure of congestion, however it has limited utility in LVO stroke and is not part of RAPID maps. In any case, the maps below show no evidence of either arterial or venous problem beyond the hematoma. Unfortunately, the area behind the hematoma is also ischemic (see matched CBV, CBF deficits extending a bit posterior to the back part of hematoma). However this is not a result of spasm (which would affect a much larger territory likely) and was a fixed deficit from the beginning.
Conclusion: Get those stereo glasses to see a great rare case
