Glomus tumors are rare, and the majority do not present with isolated pulsatile tinnitus. In other words, other symptoms are usually present in addition to pulsatile tinnitus. In fact, if PT is the only symptom of a presumed glomus tumor, it should give rise to a though that perhaps it is not glomus after all. Some dural fistulas can look a lot like a glomus, believe it or not. We have seen more than a few misdiagnosed that way. If it is in fact a glomus, usually other symptoms are present as well. Nevertheless, Glomus Jugulare and Glomus Tympanicum tumors are well-known to cause pulsatile tinnitus. Standard MRI with contrast and MRA are very good for picking up these tumors, except perhaps a small glomus tympanicum. Temporal bone CT has historically been even better than MRI for glomus, especially glomus tympanicum — an unusual situation since for most tumors MRI is a better test. In other words, if you’ve had a negative temporal bone CT and negative MRI brain with contrast, the chances of having a glomus tympanicum or jugulare are pretty much zero.
What is a glomus? Glomus tumors are part of “paraganglioma” family of tumors. There are different types throughout the body. Most are “benign” but can be locally aggressive and pretty much all of them require treatment. Symptoms depend on location and endocrine activity. Glomus jugulare ones grow in the jugular foramen, and therefore present with symptoms related to destruction/invasion of adjacent structures. The classic for Jugulare is CN IX-XI dysfunction, because these are the closest ones. Next come either VII, VIII, or XII, depending on whether it grows up (VII and VIII) or down (XII). By the time there is PT, other problems related to those nerves (swallowing issues, tongue paralysis, facial nerve paralysis, hearing loss) are also present.
The mainstay of glomus treatment used to be surgical resection. It still says that on more than a few medical websites that have not been updated in a few years. Nowadays, many are treated by “gamma knife” — a type of stereotactic radiation that minimizes radiation exposure to adjacent tissues and maximizes zap to the tumor. It is highly effective but takes time to work (months). PT symptoms may not improve for some time after gamma knife, and may do so gradually. However it is probably worth waiting rather than having your head cut open unless you really have to (because sometimes surgery is the right option still and a consultation with a true expert is a good idea). Particle embolization of the tumor can be effective in minimizing PT until radiation effects kick in, but this is typically not done because PT is tolerable enough to wait.
Why does glomus cause PT? Because it is so damn vascular. These tumors have such tremendous blood supply that the ear is literally hear blood flow through the tumor if it is large enough and close enough to the ear. Which is also why surgical resection of these tumors is usually not possible (or is very difficult) without preoperative embolization. Embolization is a procedure where blood supply to the tumor is blocked to make it less bloody during surgery. Various embolization agents are used, depending on location, experience, personal preference, etc.
Glomus tumors can have endocrine activity. A minority will secrete catecholamines and present special challenges during both embolization and resection due to catecholamine-related blood pressure instability
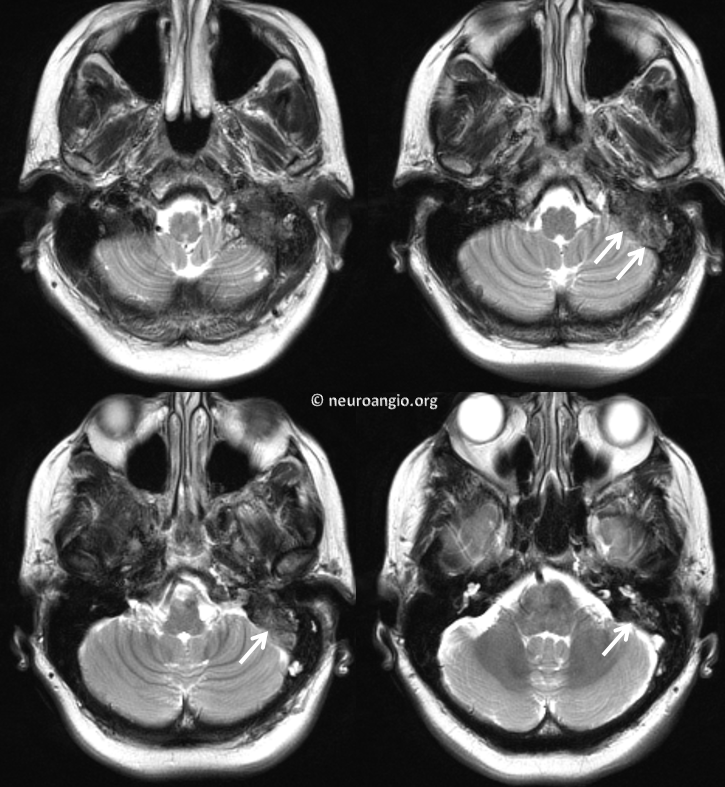
Here is a typical glomus tumor in a patient presenting with facial nerve palsy and pulsatile tinnitus. In this case, PT was actually the first sign of tumor. This T1 post-contrast image shows enhancing tumor (arrows) extending out of the left jugular foramen
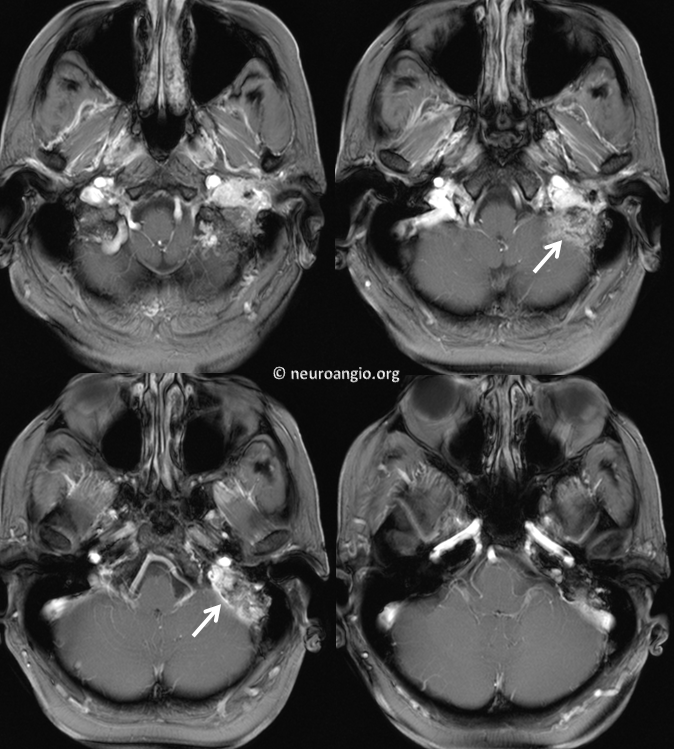
T2-weighted images have a heterogeneous appearance. The right lower image is a classic “salt and pepper” look
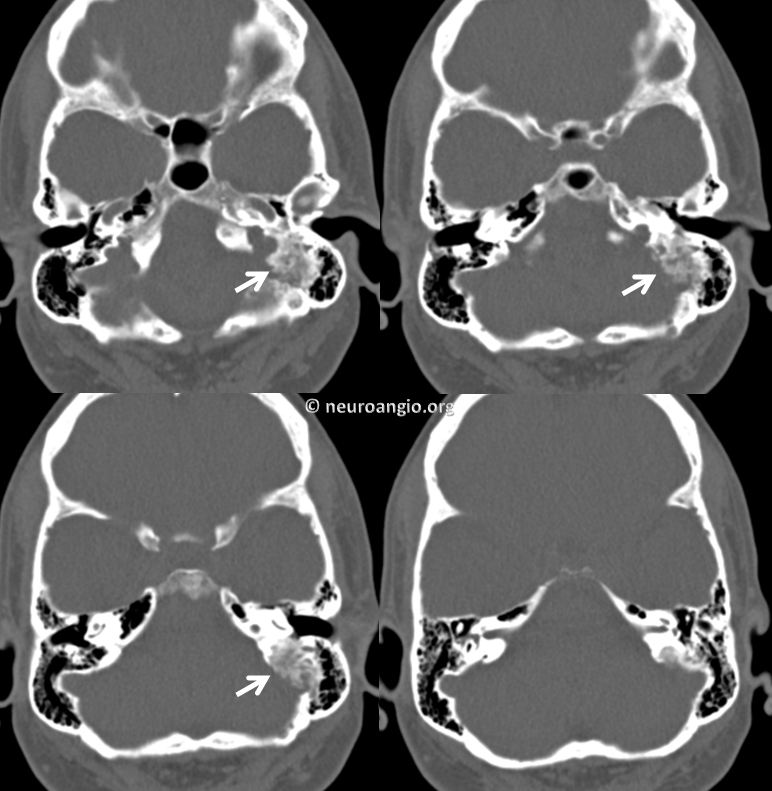
Temporal bone CT images show permeative and destructive appearance to the mastoid bone on the left (arrows) compared with normal right side
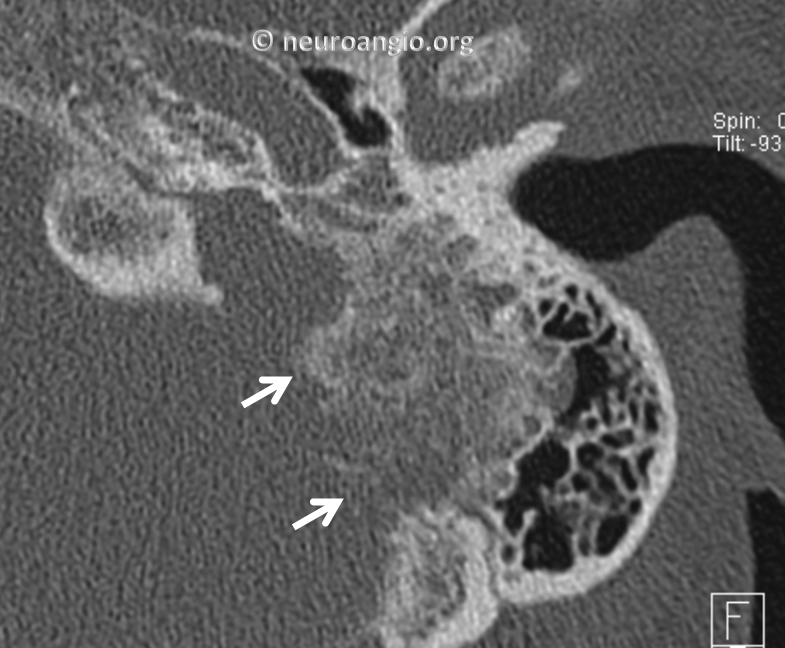
Bone algorythm reconstructions of left side only show the tumor really well
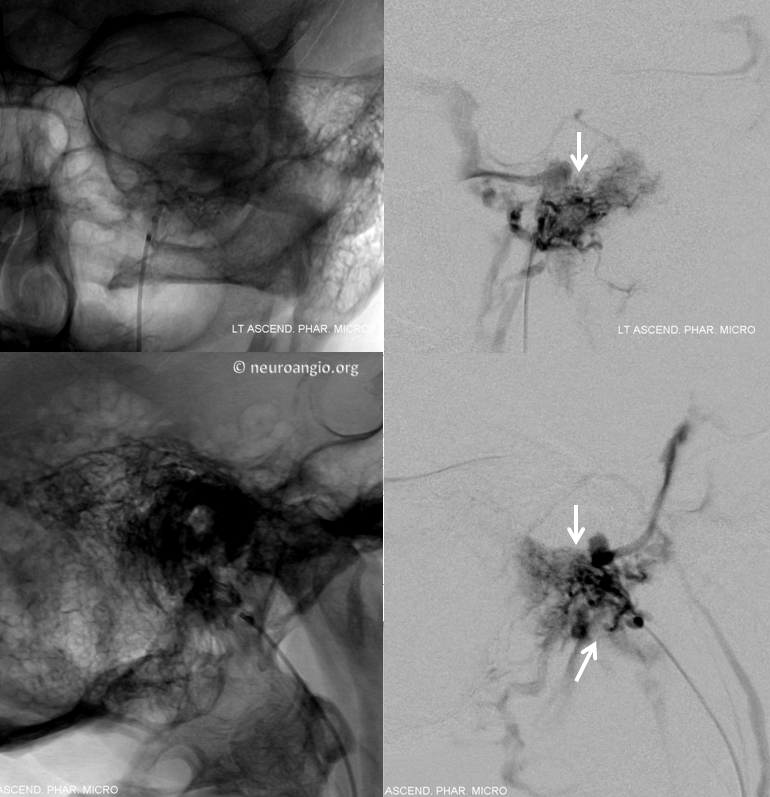
Angiography shows classic intensely vascular mass with left ascending pharyngeal artery supply
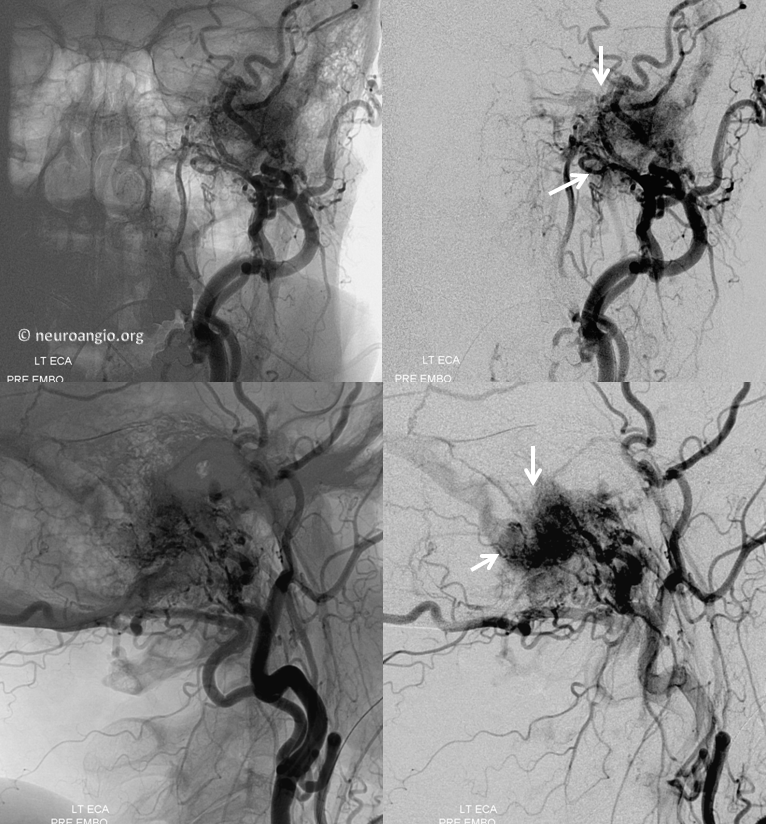
Microcatheterization of the neuromeningeal trunk of the ascending pharyngeal artery, followed by small particle embolization (see Techniques Preoperative Tumor Embolization for lots more cases, unrelated to PT)
Post-embolization external carotid injection, tumor blush is gone. Various trunks have been embolized with small particles and subsequently closed with various coils
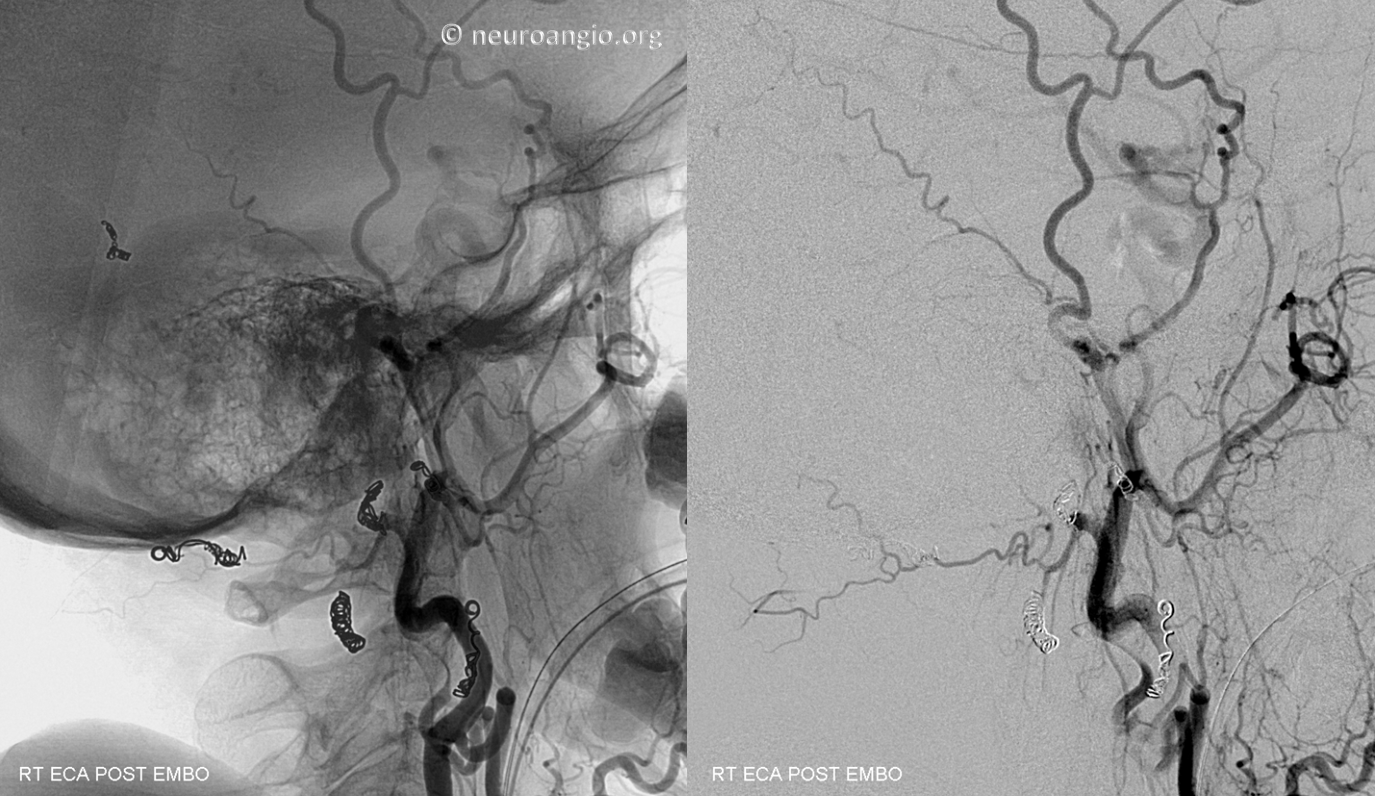
Common carotid injection to further show no residual tumor vascularity

Post-resection CT scan, with fat packing of the surgical cavity (white arrows) and a craniectomy plate (black arrows) in place

