Overview: The occipital artery (29, diagram above) most commonly, originates from the external carotid carotid artery, and sweeps a posterior superior course under the skull base, towards the back of the head and upper neck. It is mainly concerned with supply of upper neck muscular elements. This somewhat humble disposition, however, belies its important embryologic and functional roles as a conduit between the anterior (carotid) and posterior (vertebral) systems. This is aptly illustrated in frequent connections between the occipital and vertebral arteries at C1 and C2 levels, and in the proatlantal variant (which is, simply, an occipitovertebral anastomosis with hypoplasia of the more proximal vertebral artery). The longitudinal functional nature of the vessel is further demonstrated by its frequent association with the ascending pharyngeal artery where, perhaps 20-30% of time, both vessels originate from a common pharyngo-occipital trunk. Another potentially important contribution of the occipital artery can involve structures related to the facial nerve and mastoid bone. From an interventional standpoint, the occipitovertebral anastomoses must be kept in mind, particularly during embolizations. Aggressive small particle occipital artery embos can also produce skin necrosis, or result in postoperative wound healing issues. On a different note, its a very good place to stick a stiff exchange wire into — no better.
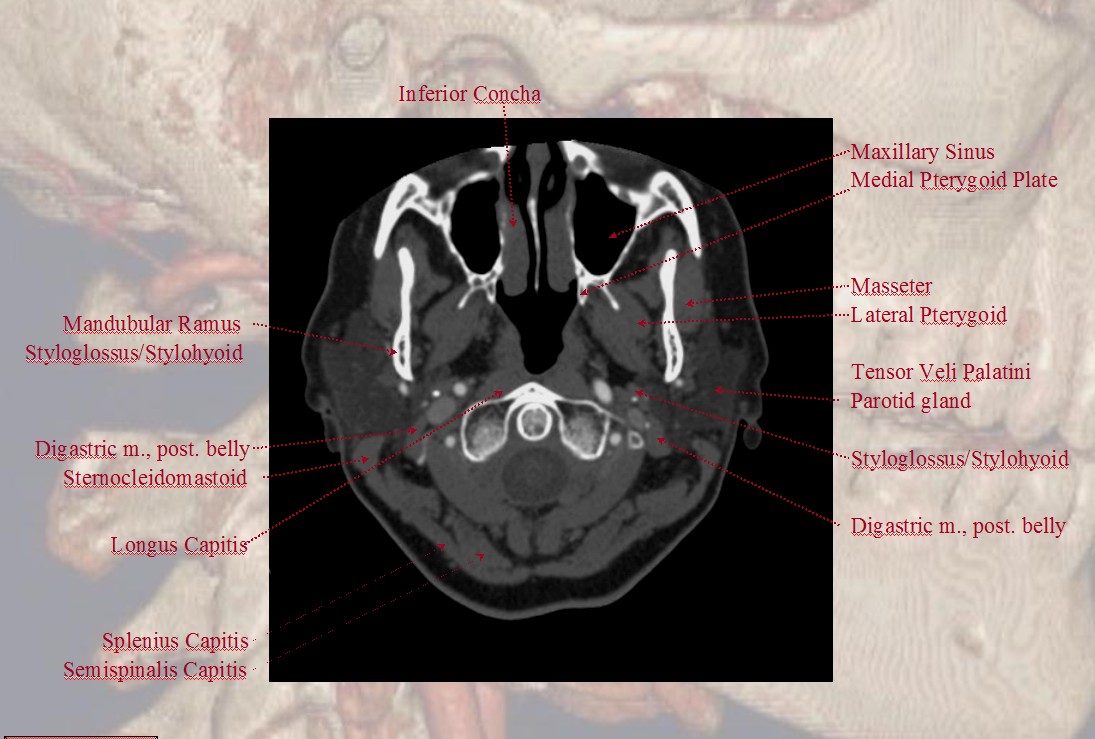
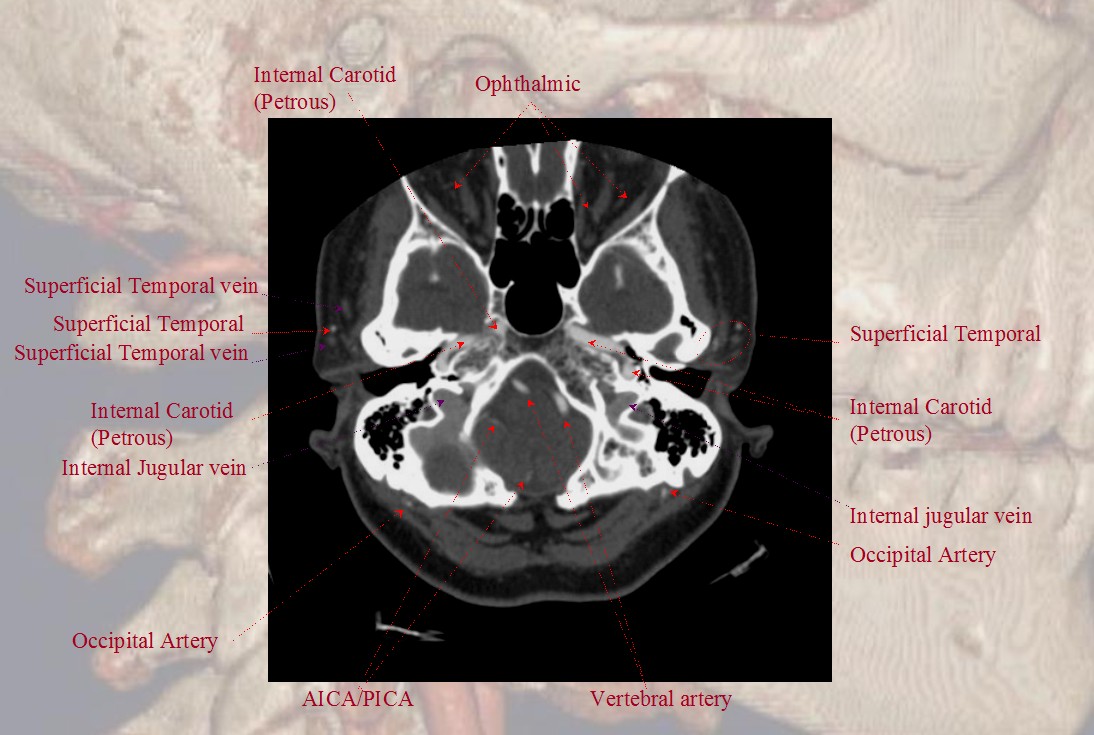
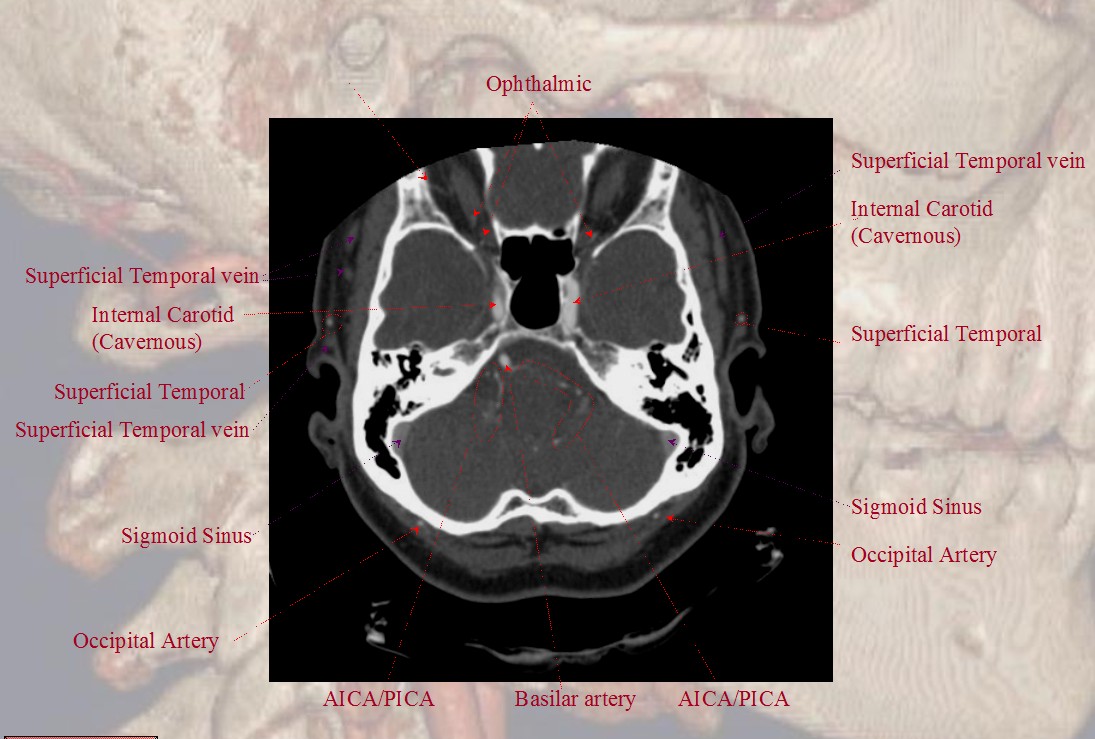
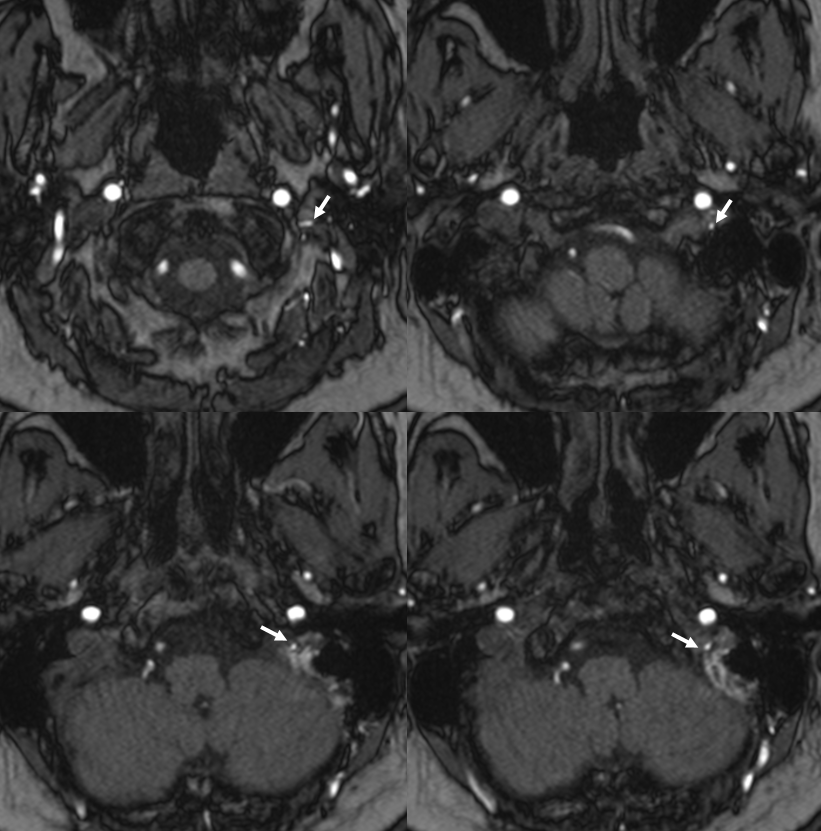
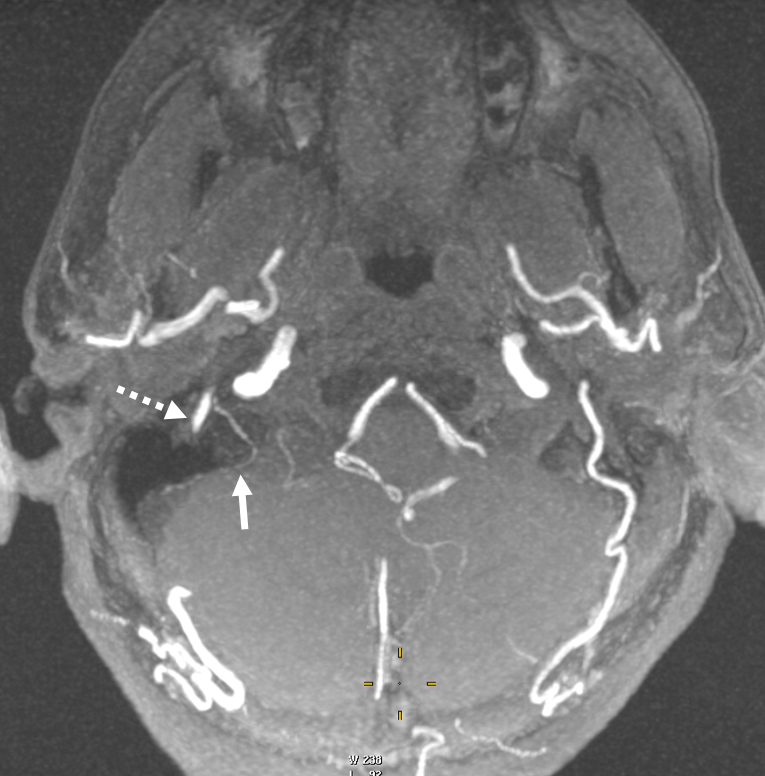
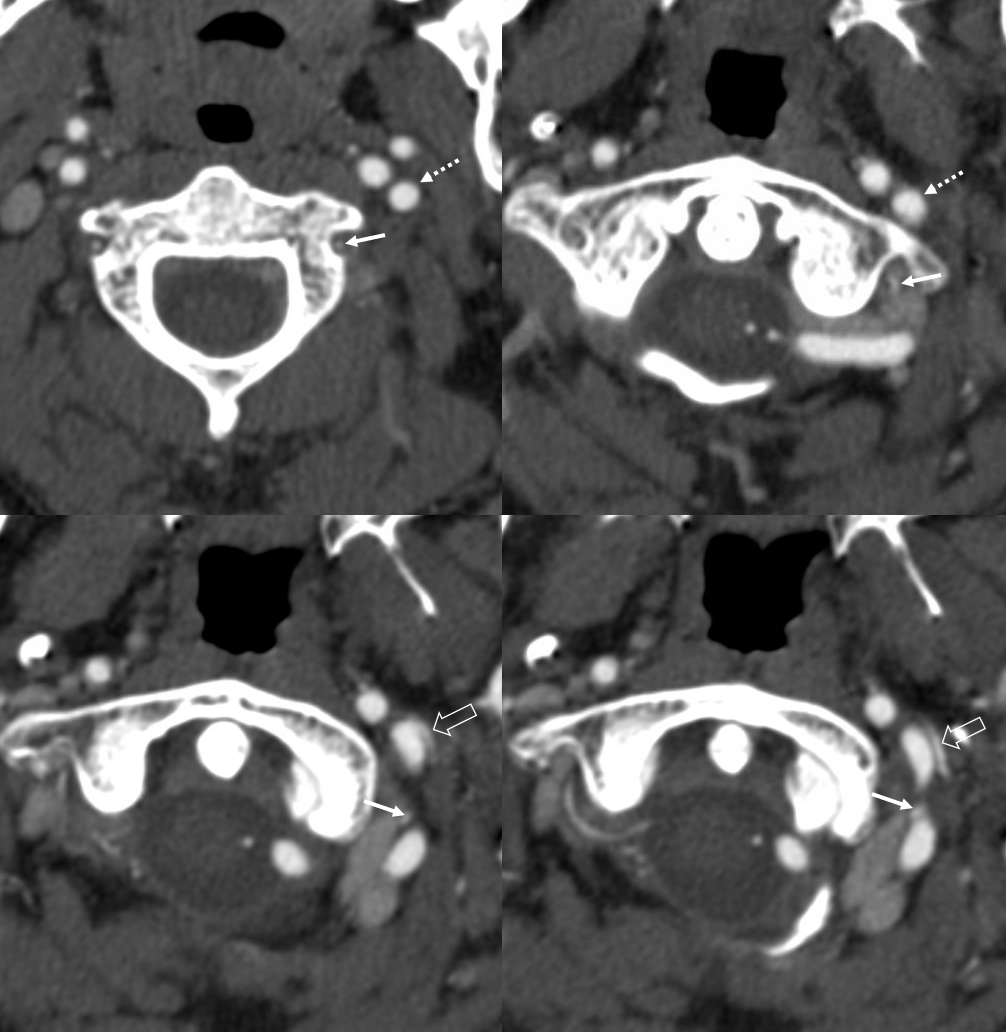
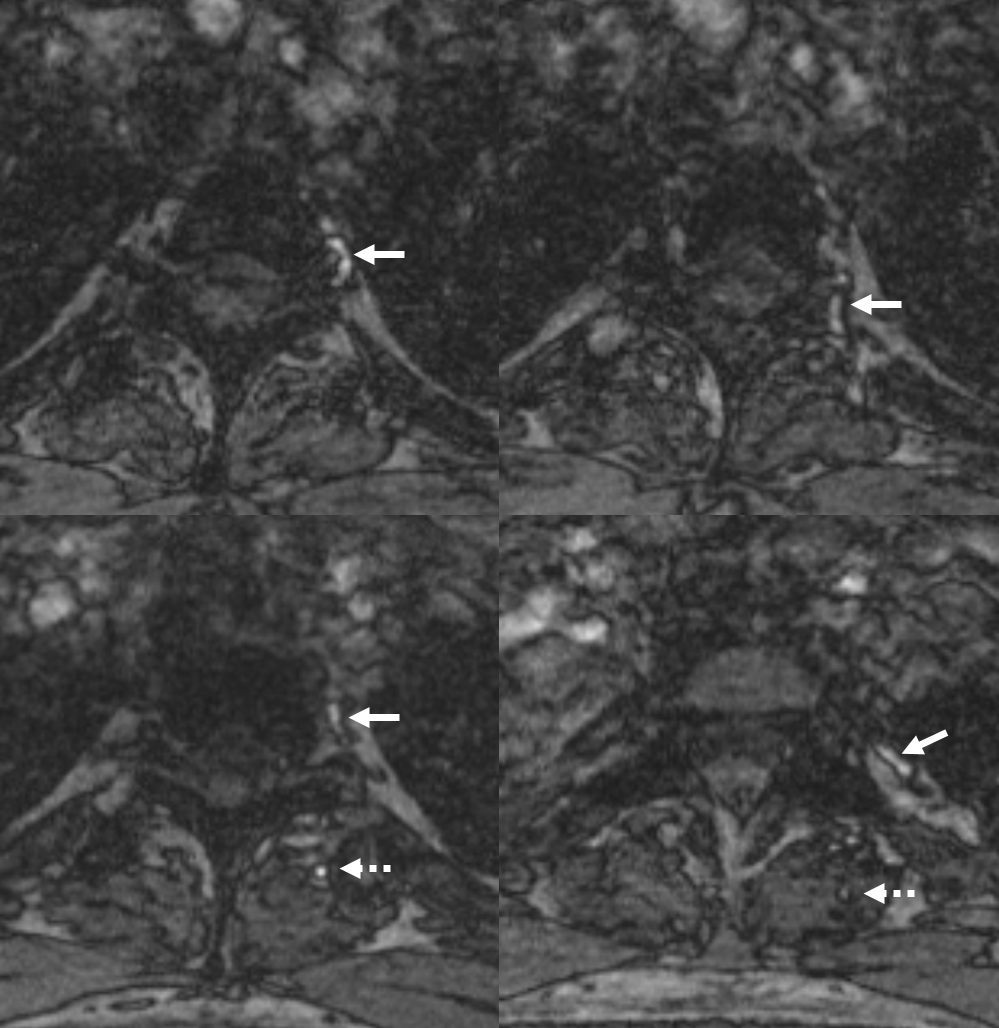
Cross-sectional Imaging — Select Axial Images of the neck, demonstrating the course of the occipital artery (in this patient), and its particular relationship to the digastric muscle. For a full set of CT angiographic images, consult CT Angio Vascular Atlas section.
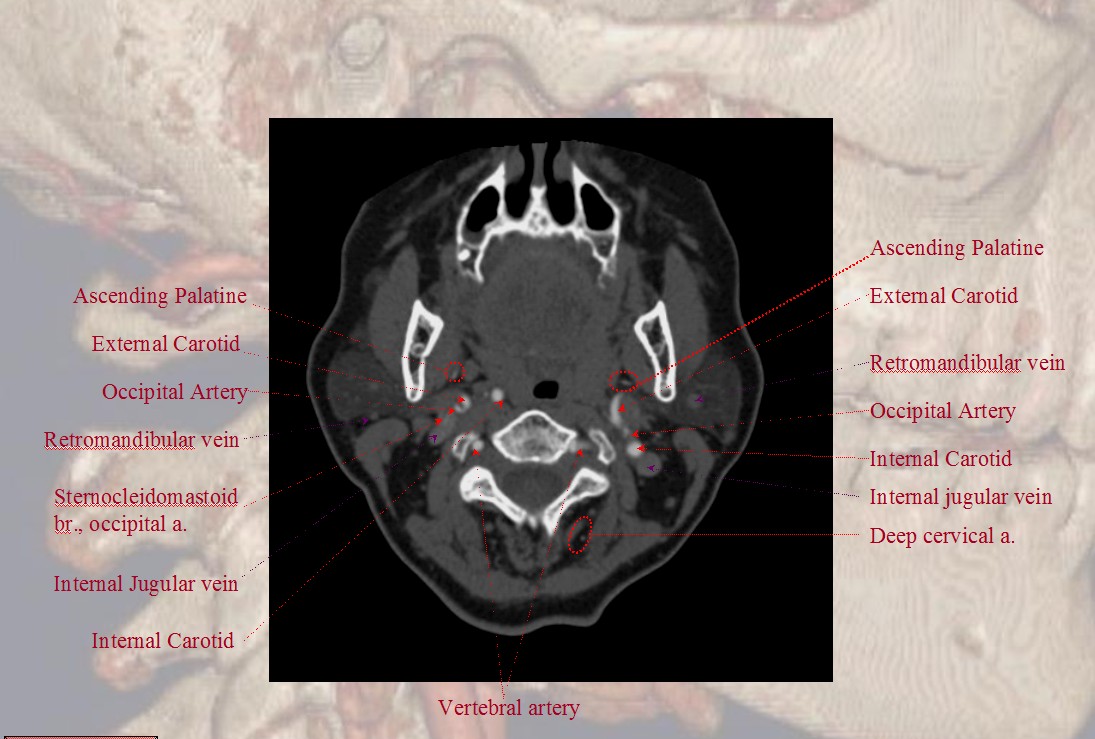
The Occipital Artery ostium projects posterior and typically lateral in relation to the parent vessel
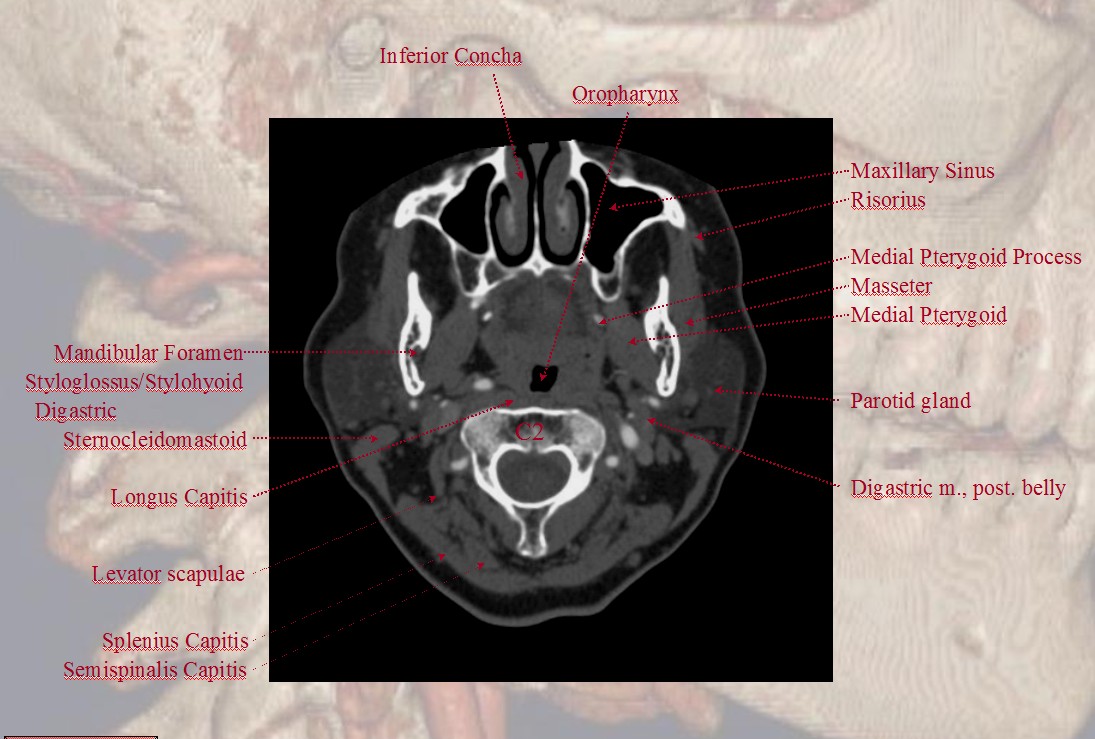
Some anatomical landmarks; the occipital artery passes deep (along the medial aspect) of the digastric muscle
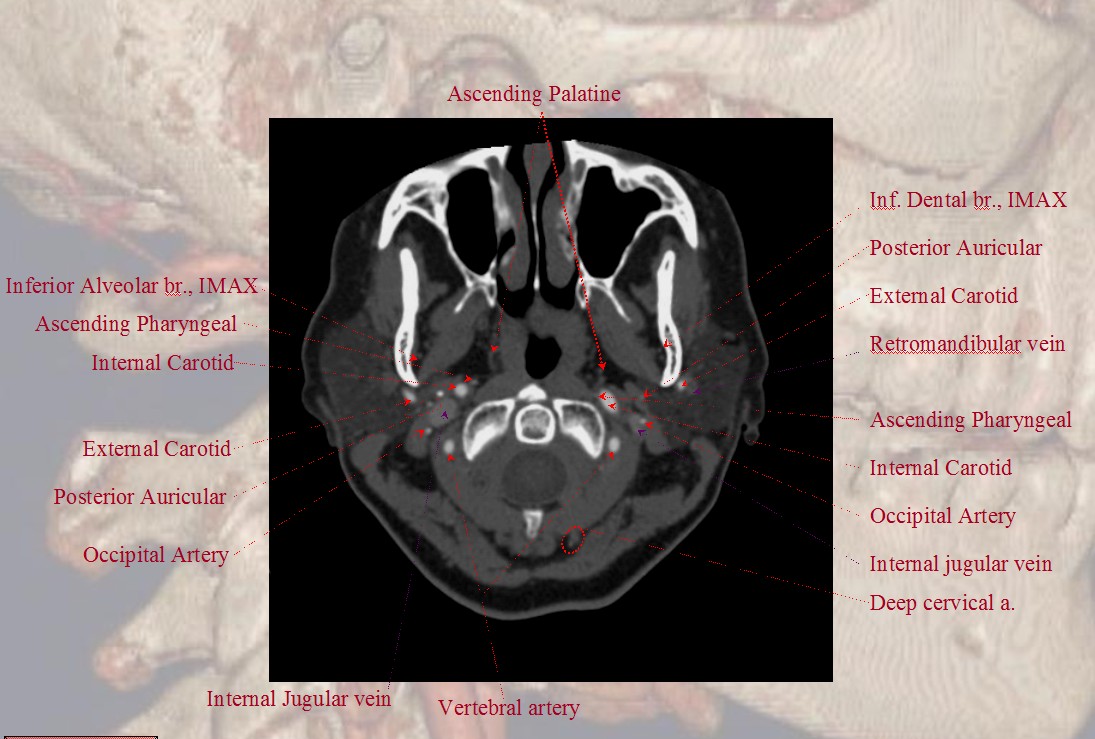
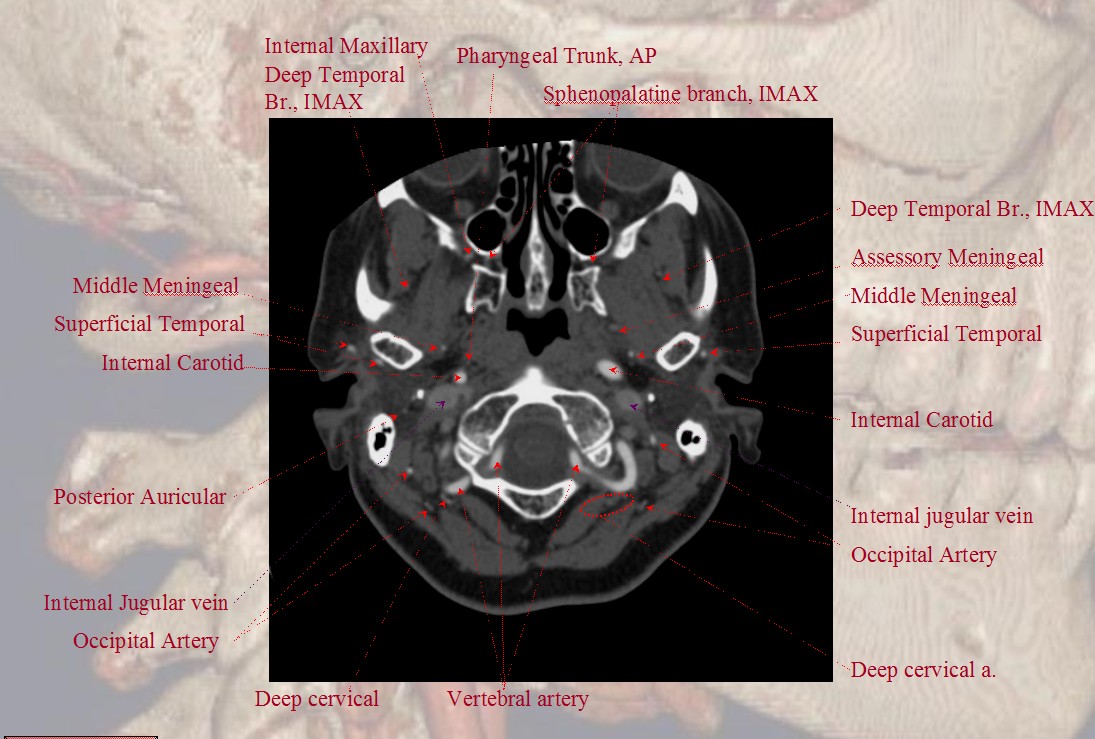
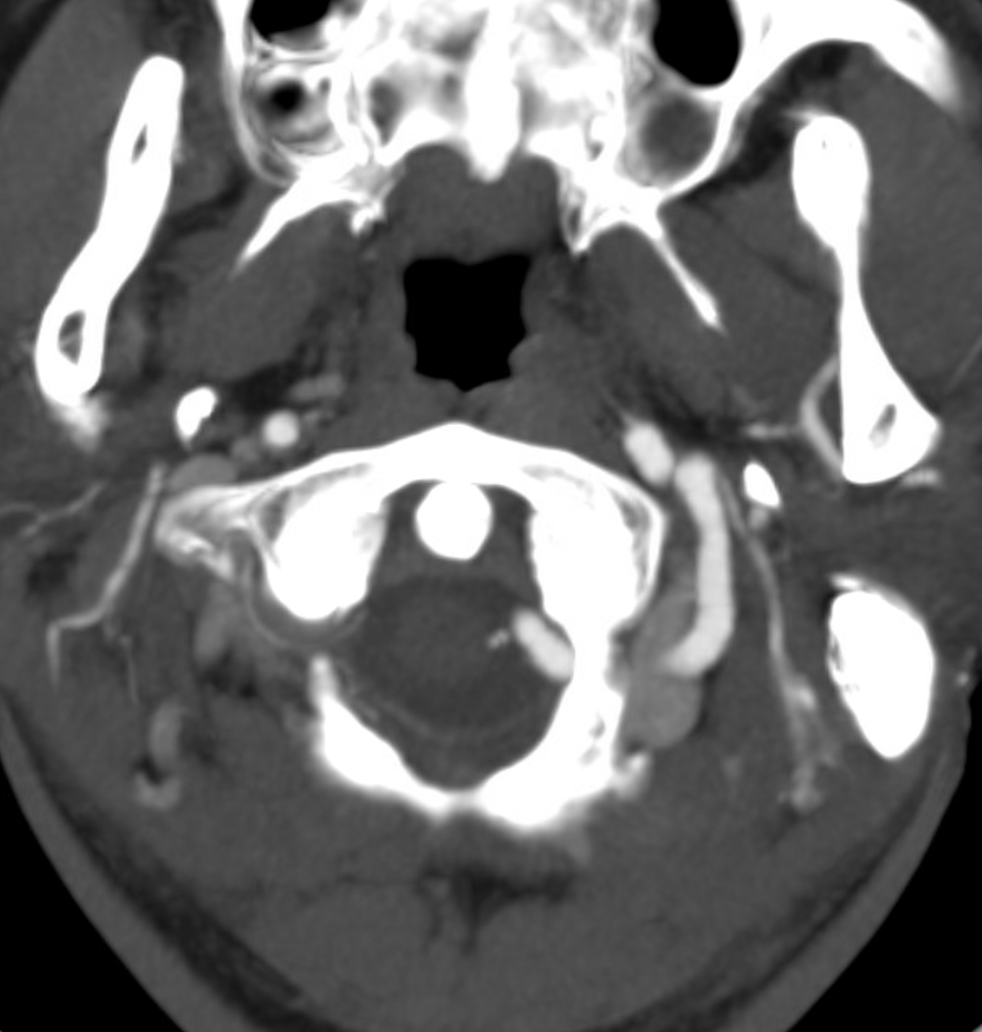
Notice proximity of the occipital, deep cervical, and vertebral arteries at the skull base, where anastomoses via the 1st segmental artery are common.
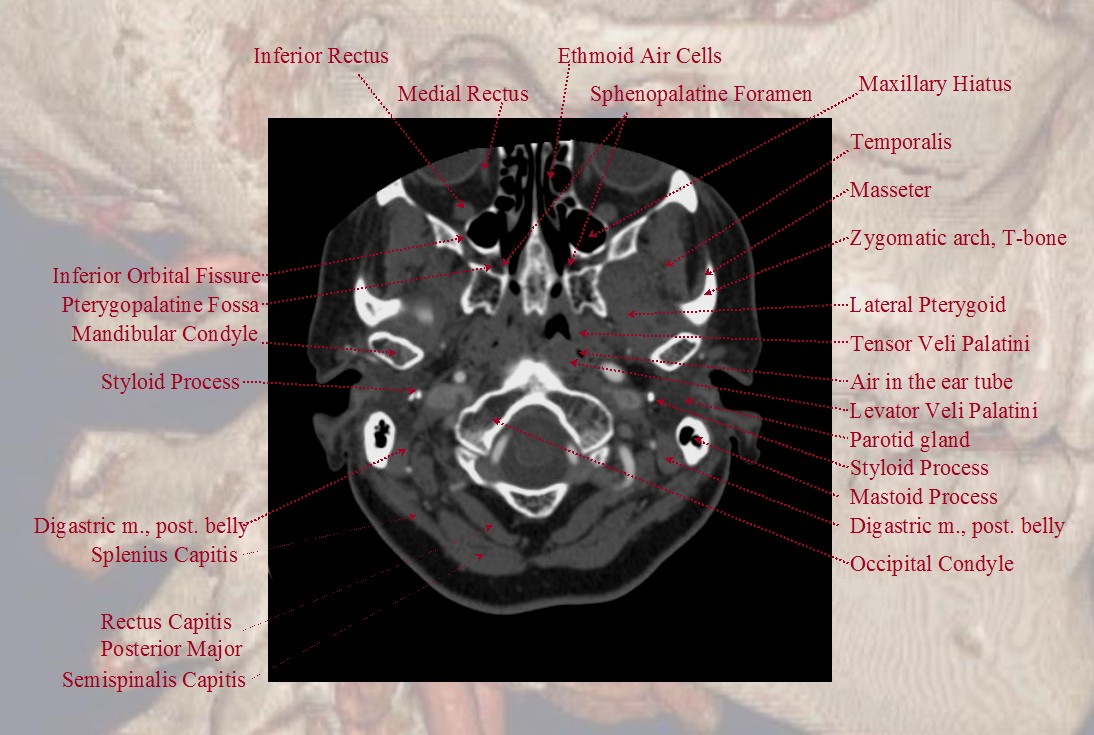
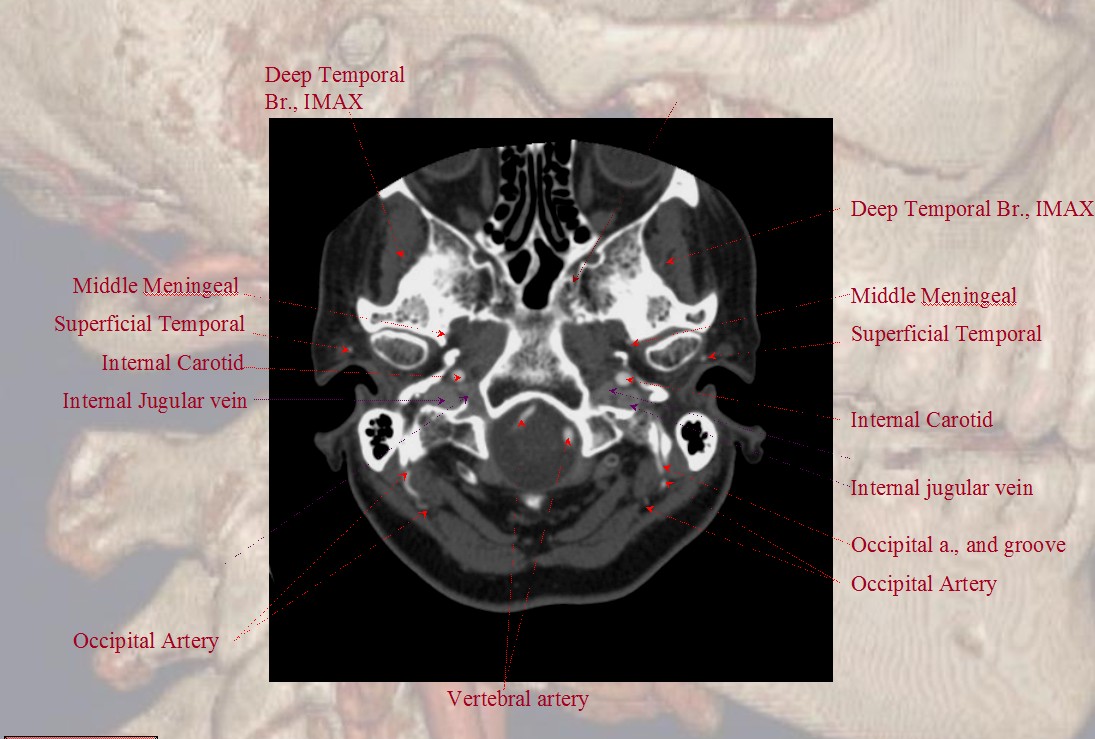
A shallow groove can be seen on the undersurface of the mastoid bone sometimes, made by the occipital artery as it curves posteriorly. The occipital artery stays with the digastric muscle until its insertion.
Vertebro-occipital anastomoses
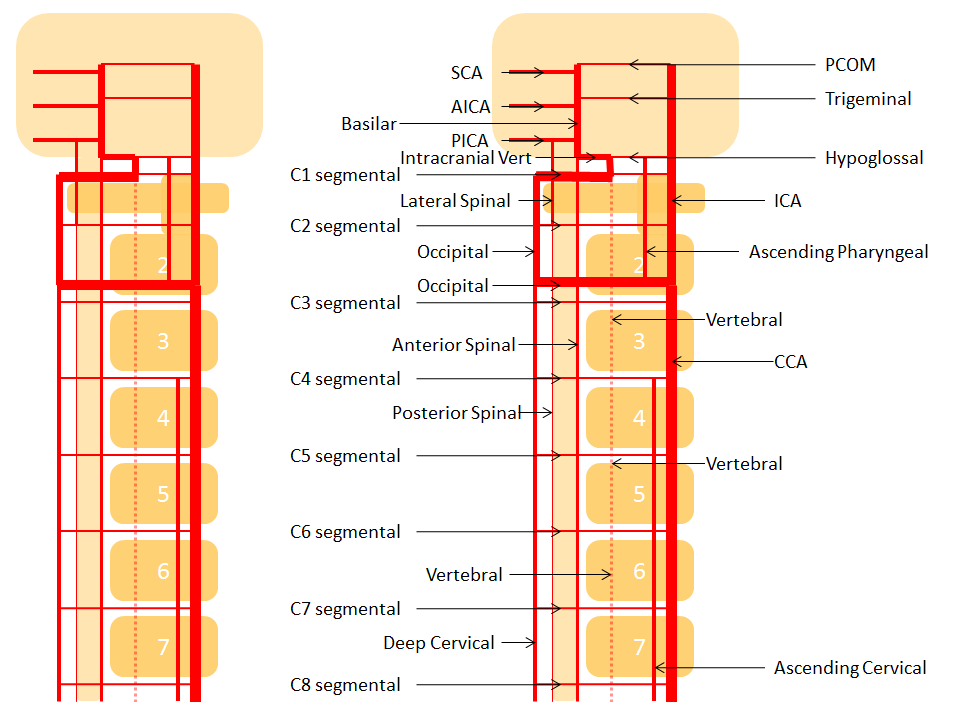
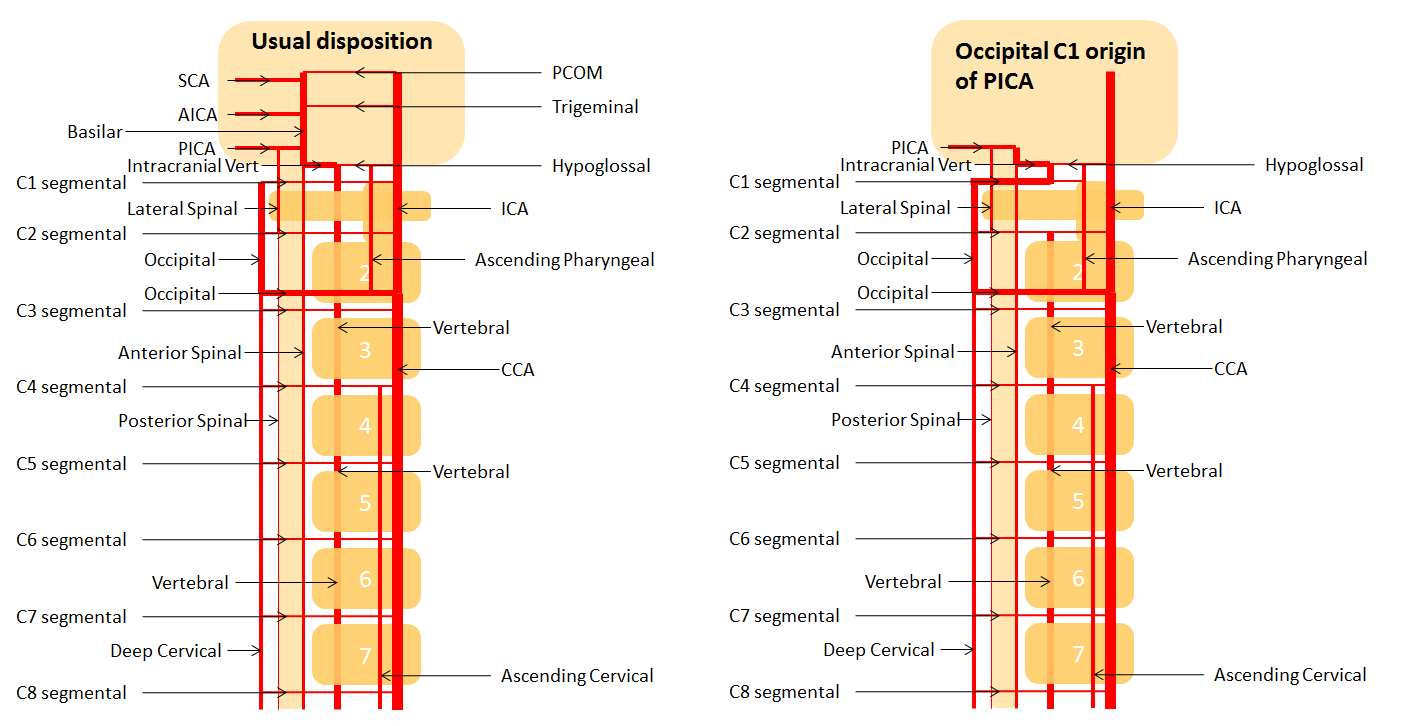
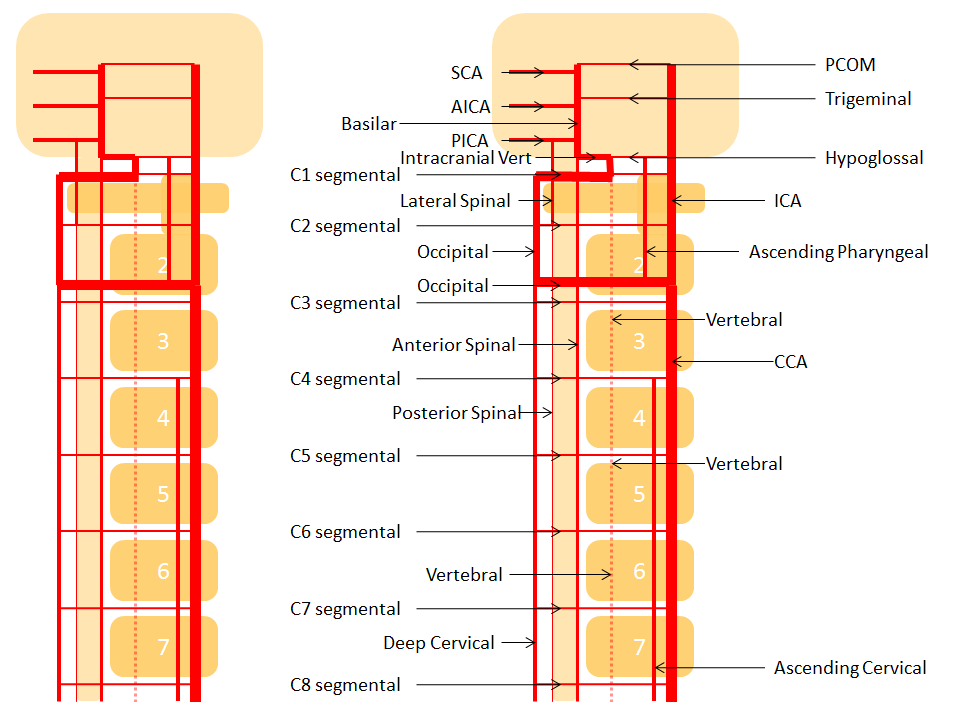
The vertebral artery communicatates with the occipital via C1 and C2 (segmental) branches, which typically supply adjacent muscular and ossesous elements. In this sense, the occipital is part of a larger network of cervico-vertebral connections between the occipital at C1 and C2, the deep cervical at C3 and C4, and ascending cervical at C5 and C6 (for example, the C5 level entry of vertebral artery into its foramen is, in fact, proximal vertebral hypoplasia with ascending cervical reconstitution via the C5 segmental artery).
For a full discussion of the longitudinal system and segmental vascular organization, see Vertebrobasilar Artery,Vertebral Artery, Basilar Artery sections.
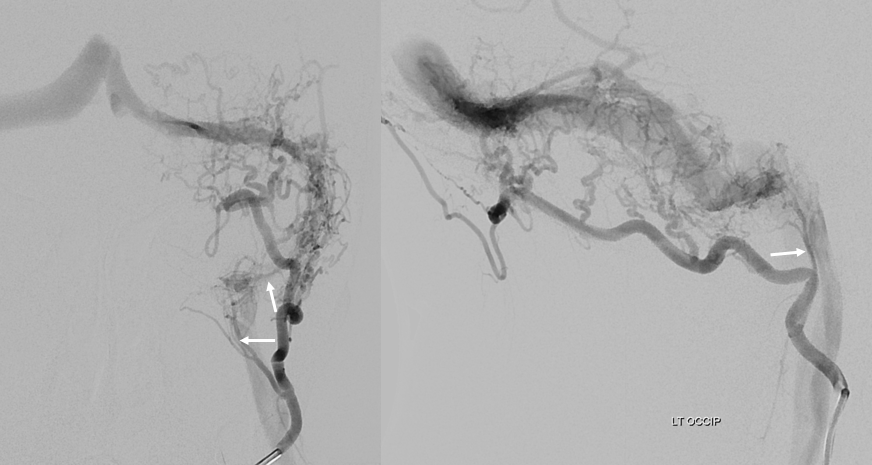
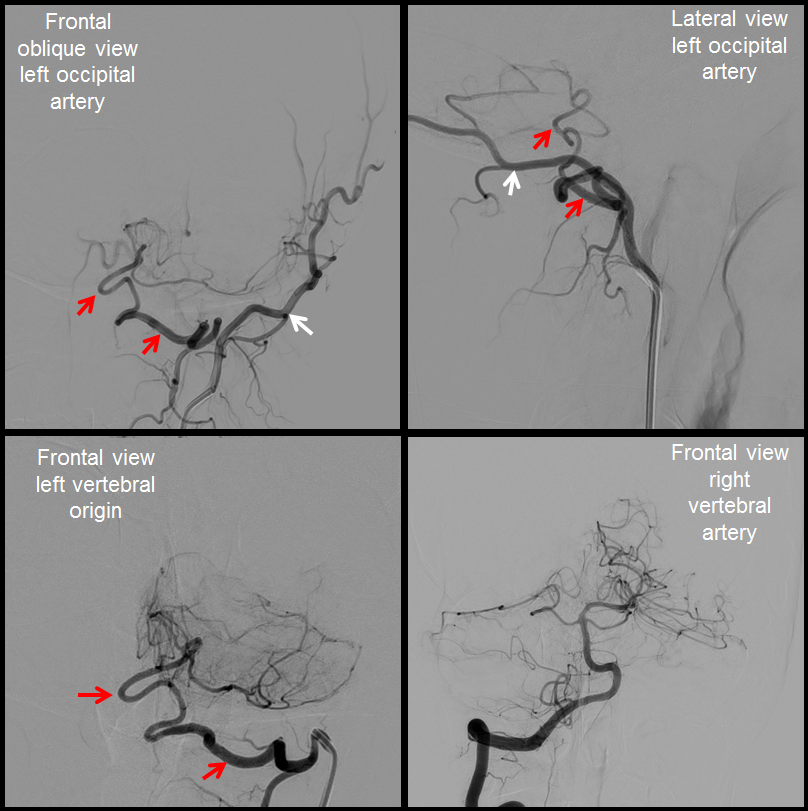
Examples:
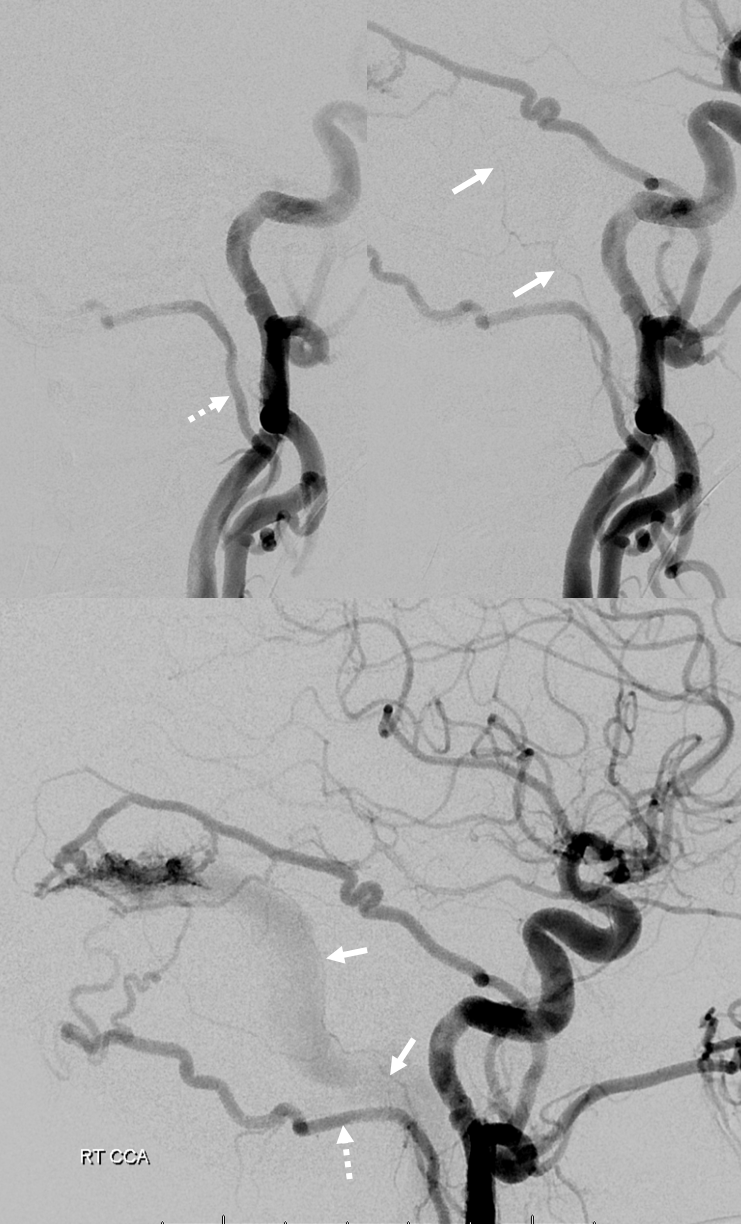
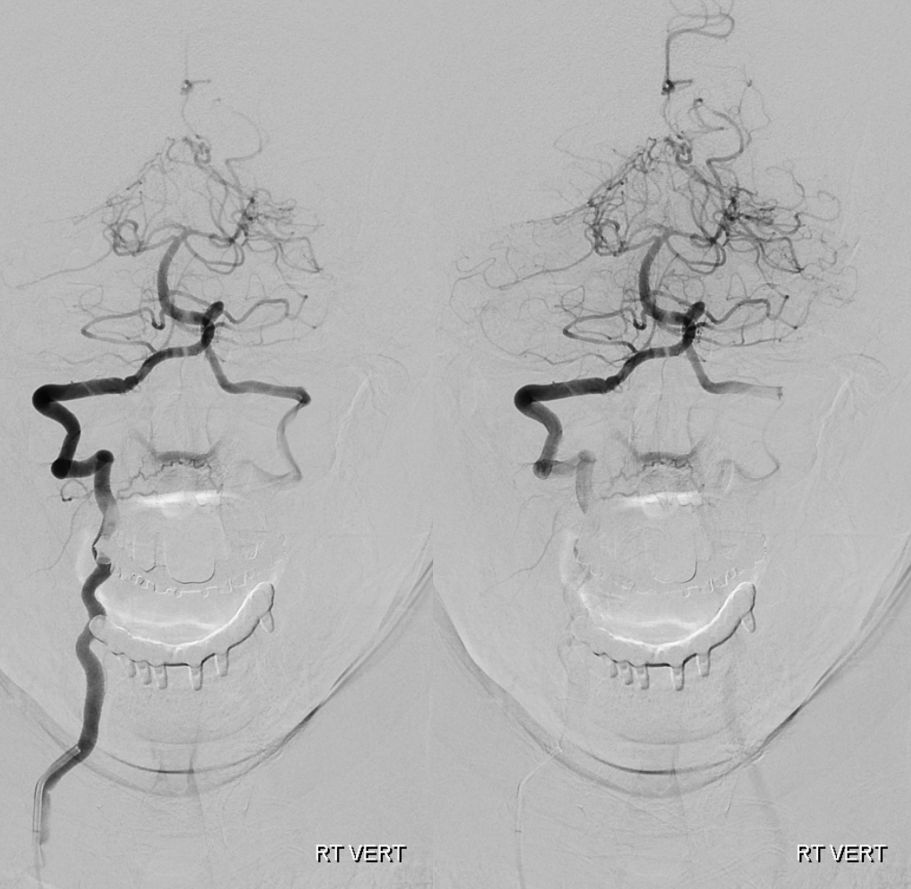
1) Vertebral origin of occipital artery — relatively commmon (~1%) — a large C1 segmental artery supplies occipital territory, in setting of relative proximal occipital hypoplasia.
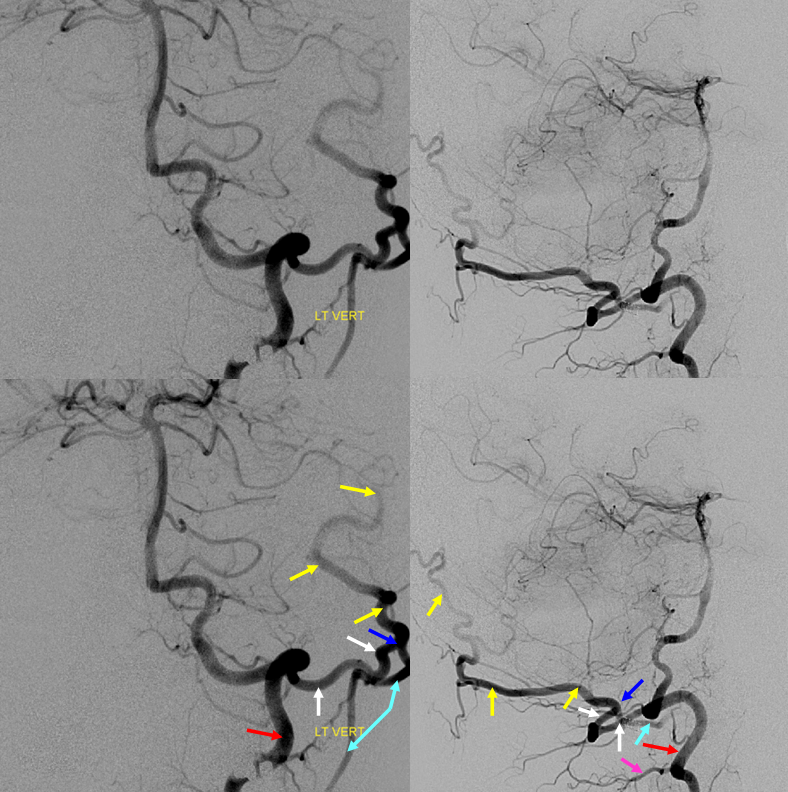
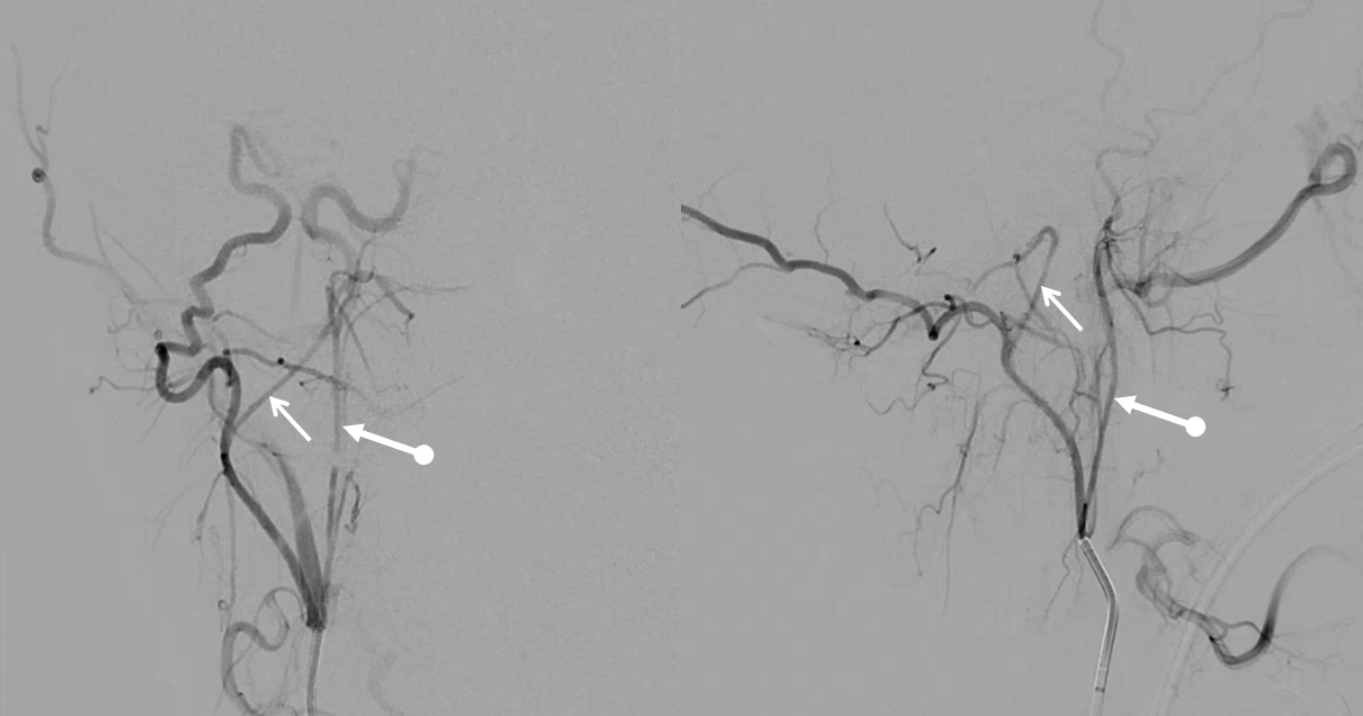
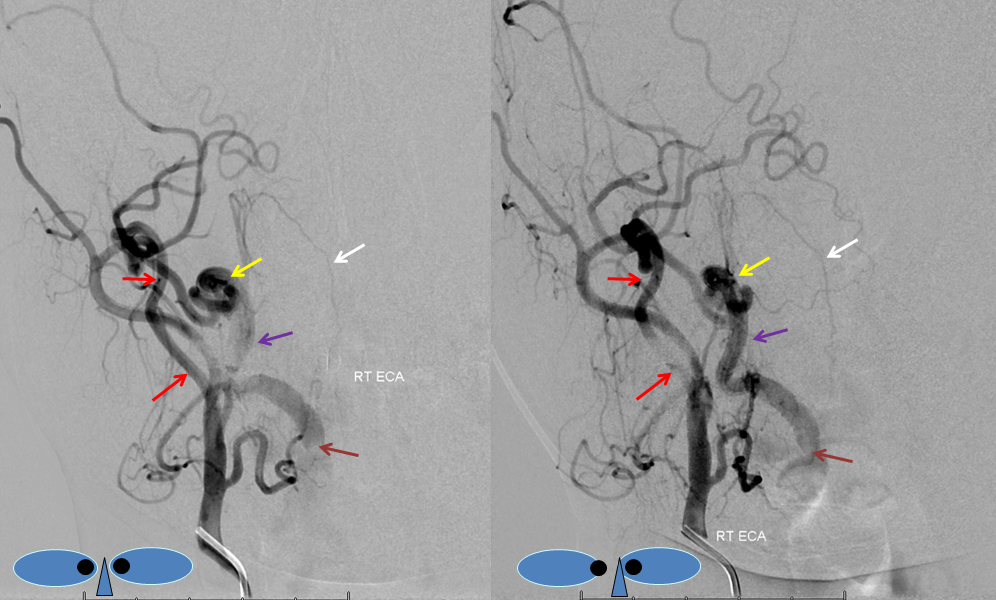
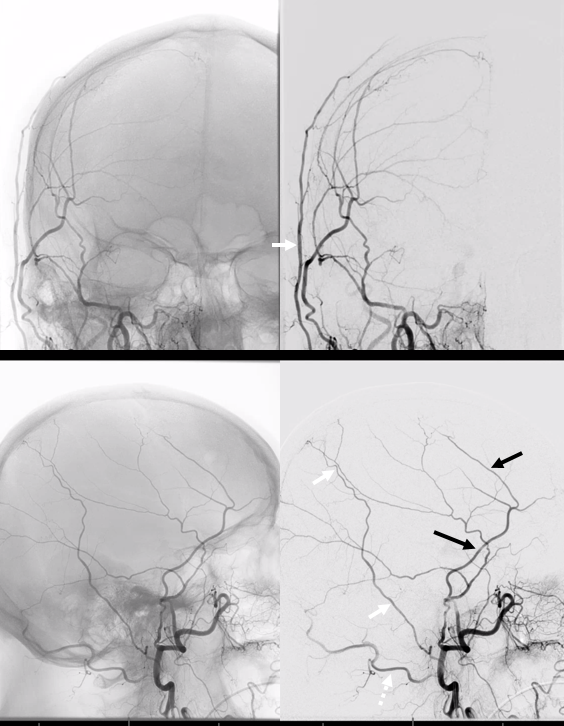
Unlabeled (top) and labeled (bottom), AP (left) and lateral (right) injections of left vertebral artery (red), demonstrating a prominent C1 segmental branch (100 master diagram, white arrow) supplying the occipital artery (yellow). The anastomosis between the C1 and occipital is marked in blue. Contrast reflux demonstrates hypoplastic occipital proximal to the C1 branch (light blue).
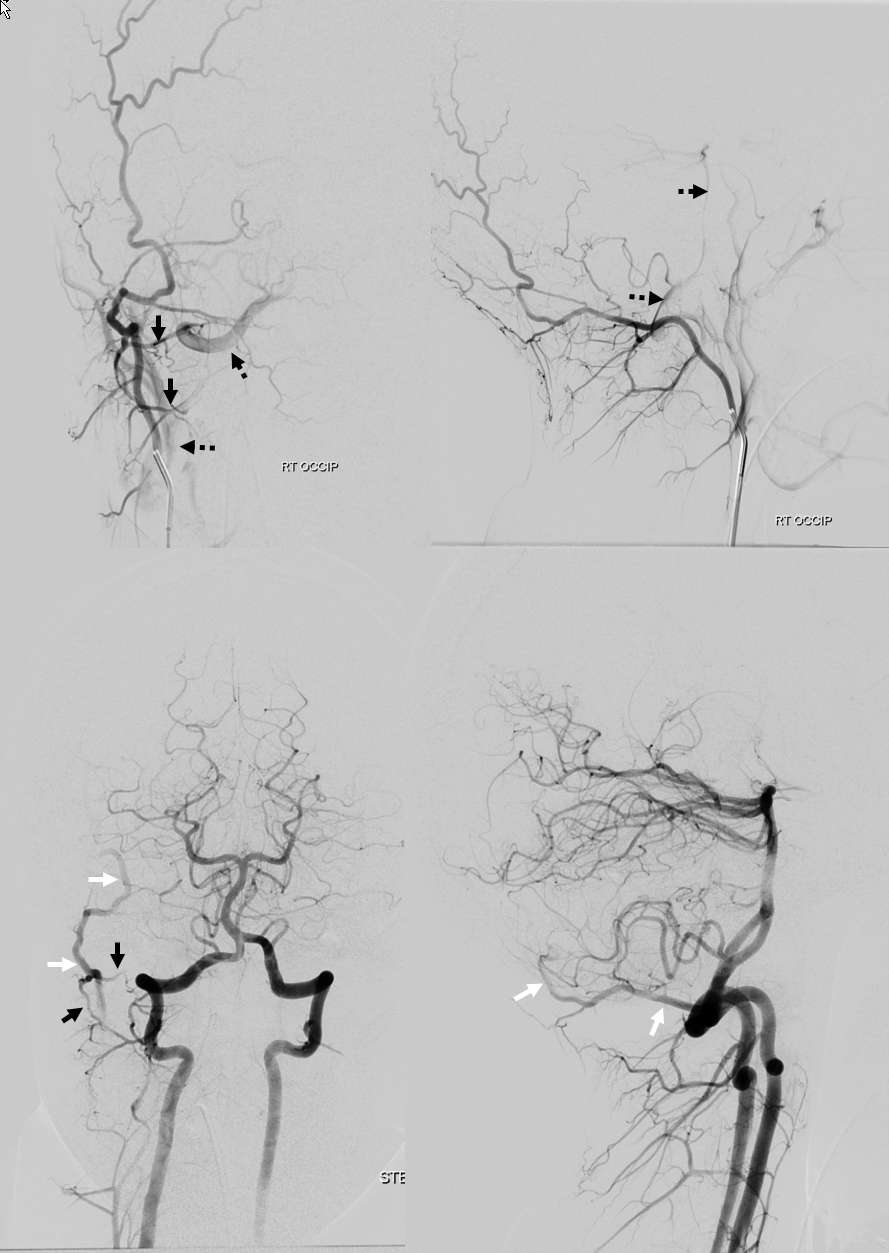
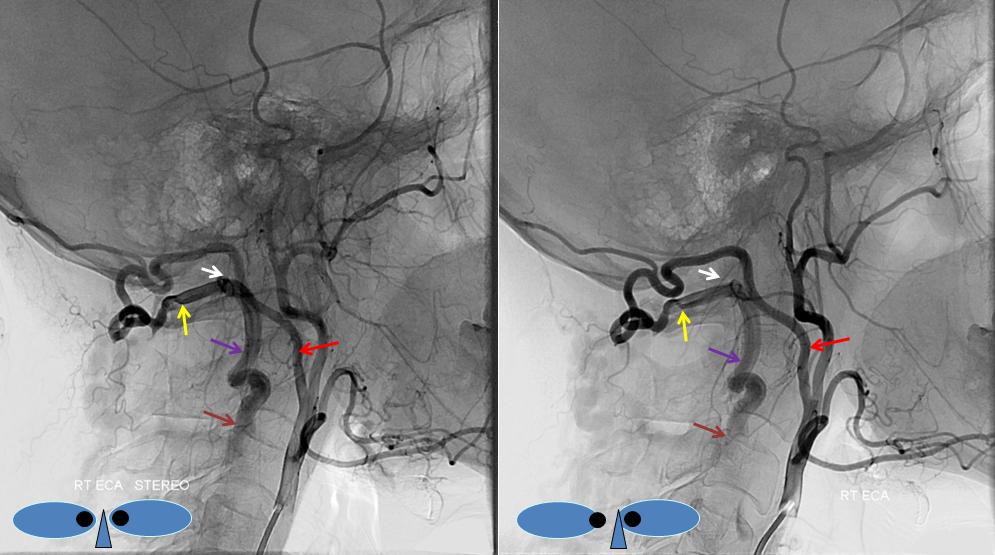
Another example — injections of occipital artery (top) and vert (bottom) show C1 and C2 muscular branch connections (black arrows) between the occipital (white arrows) and vert (dashed black arrows)
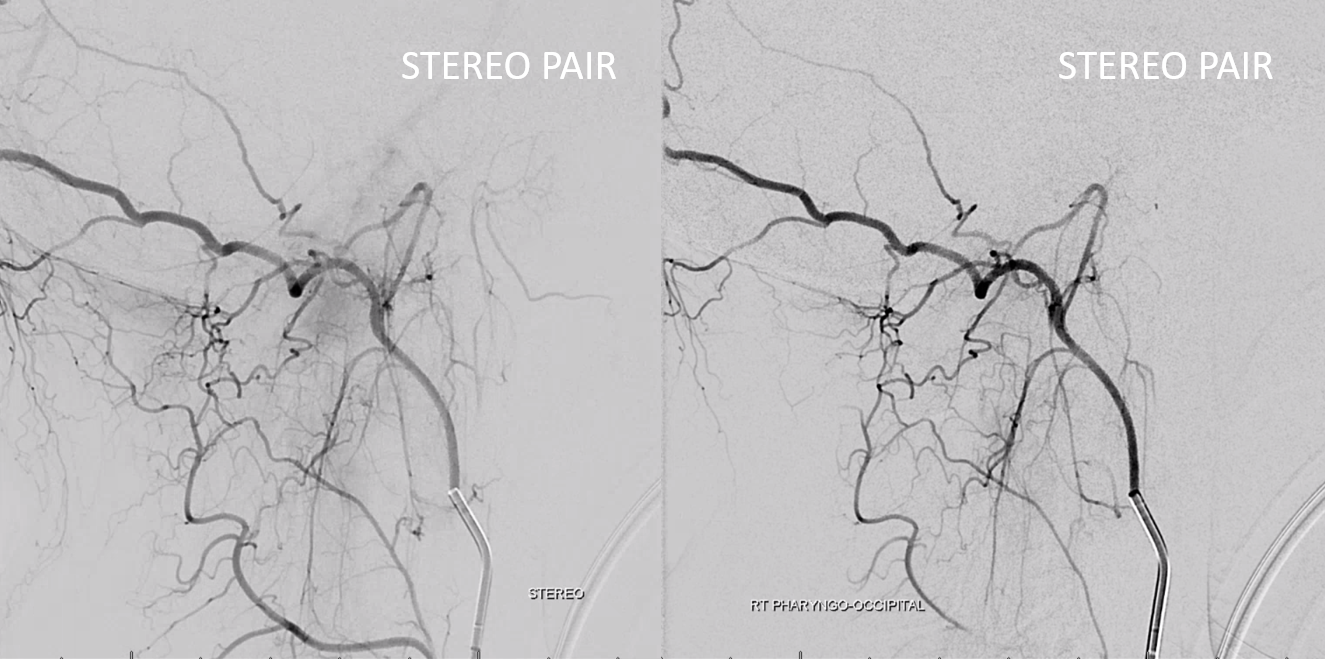
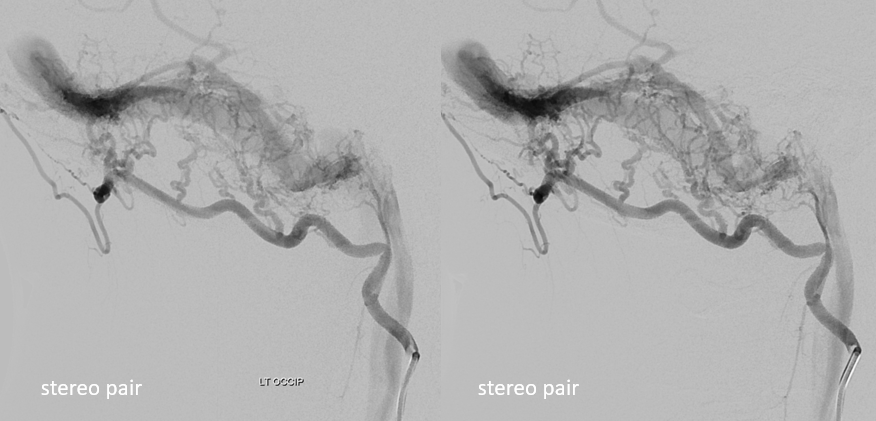
Anaglyph stereos of same
Carotid Origin Occipital Artery — rare variant
Pharyngo-occipital trunk (red) origin from the internal carotid artery. Occipital is yellow, and AP is pink.
Mastoid Branch (28)
The occipital artery almost invariably participates in supply of posterior fossa dural structures via transosseous channels originating from its mastoid branch. When the transosseous branch is large enough (i.e. gives rise to supply of posterior meningeal region), its corresponding hole in the skull is recognized as the “mastoid foramen”. The territory supplied is usually posterior to petrous pyramid base, in region of sigmoid sinus. Consequently, dural fistulas of the sigmoid sinus usually demonstrate a component of occipital supply. Usually, middle meningeal and ascending pharyngeal arteries represent more fruitful venues for transarterial embolization.
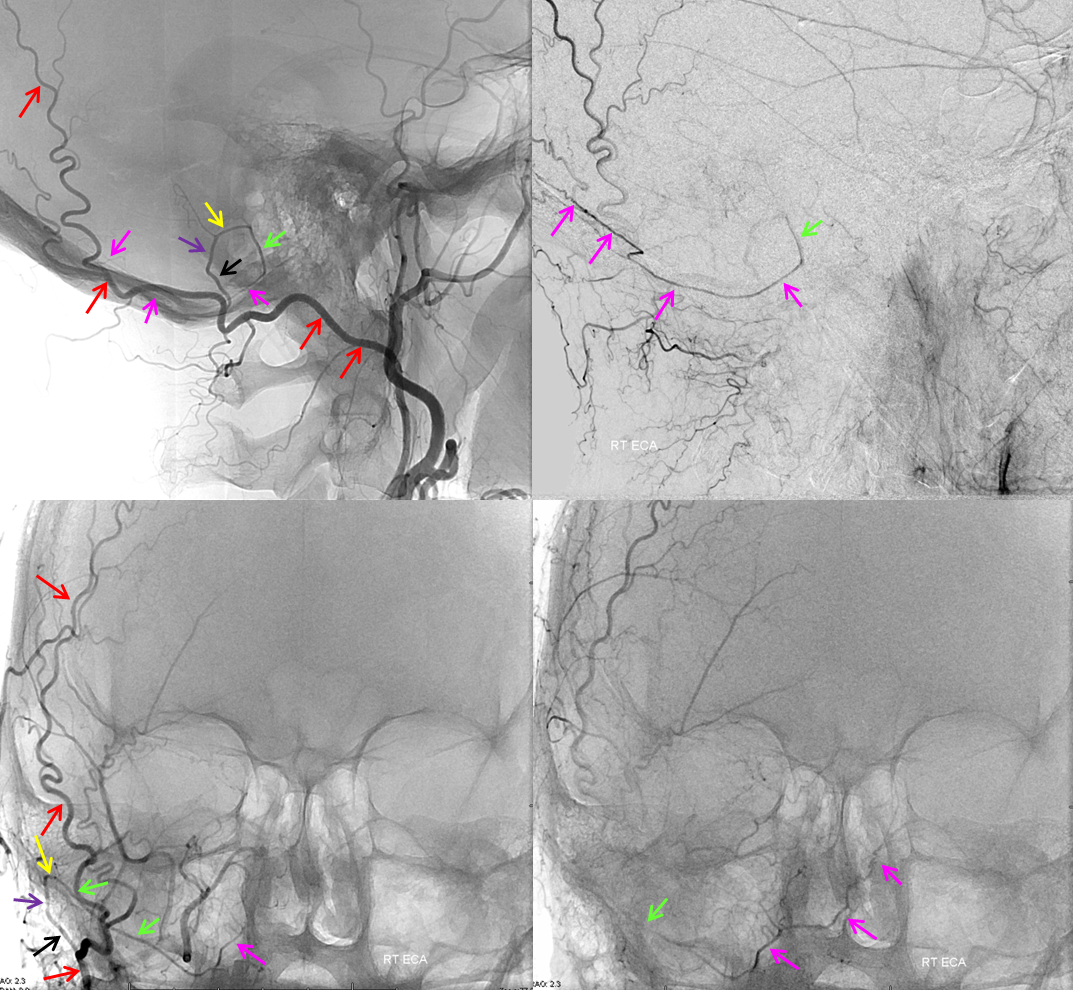
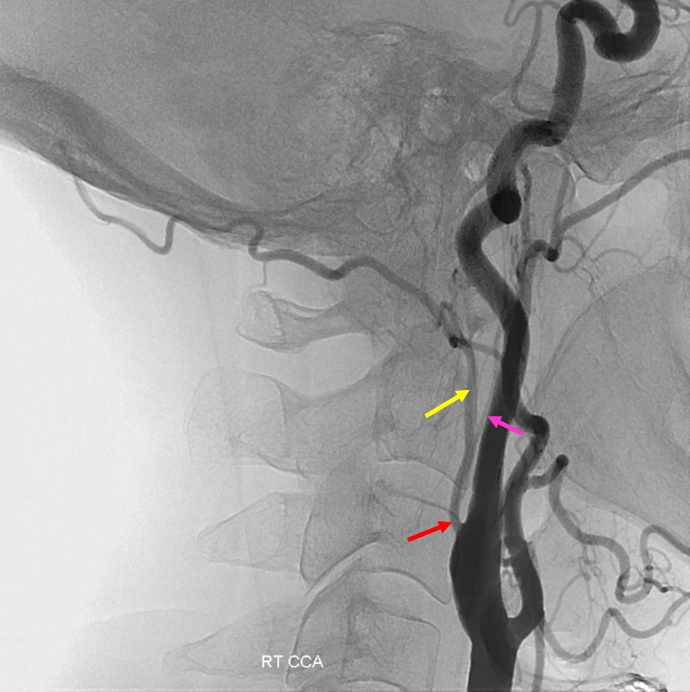
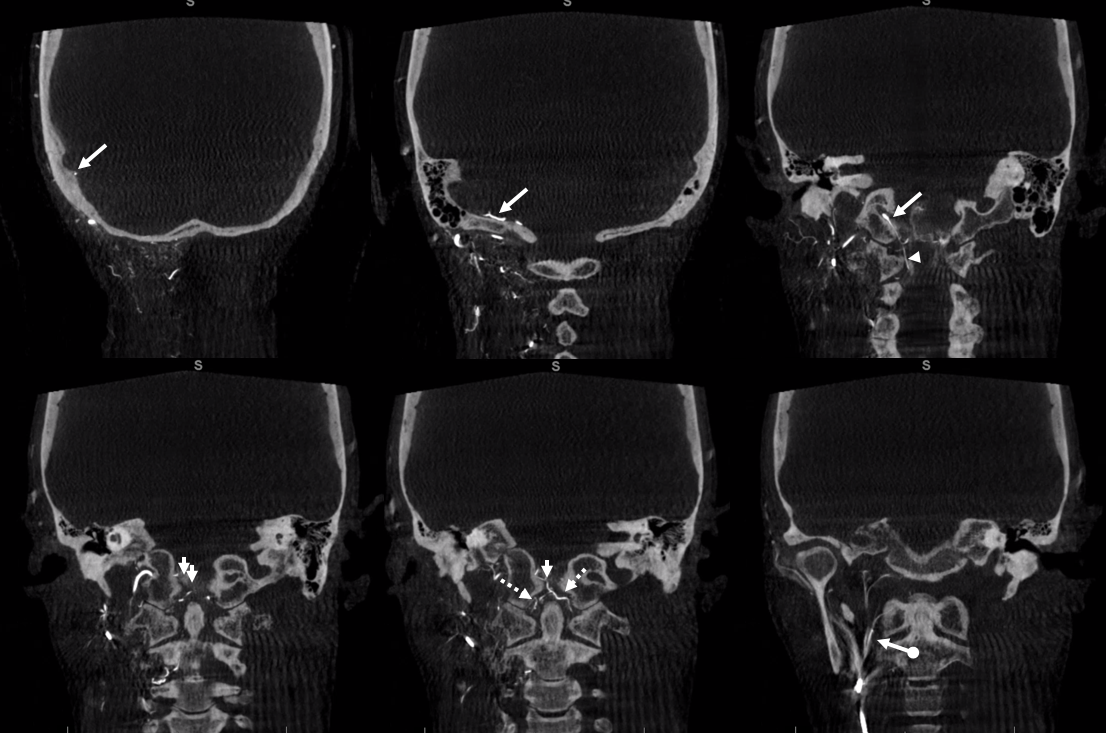
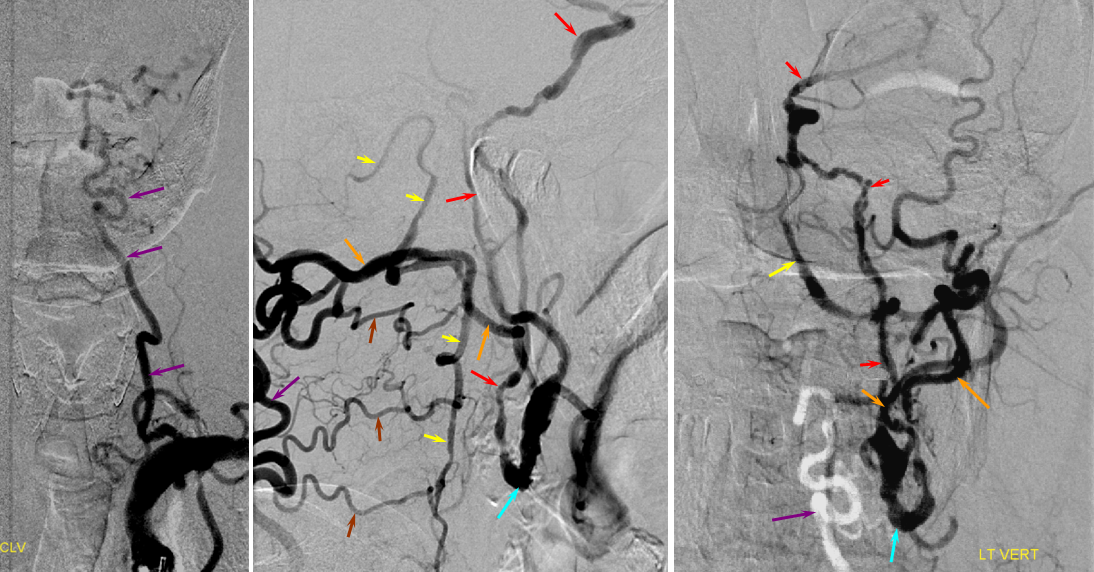
Mastoid branch supply of the posterior meningeal artery. Non-pathologic role of occipital artery (via its mastoid branch) in supply of dural structures is demonstrated in this patient, where the OA (red) gives gives rise to posterior meningeal artery (green and pink). The mastoid branch consists of a short extracranial segment (black), followed by transosseous segment (purple). The intracranial portion consists of a short anteroinferior dural segment (yellow), and a long medial segment (green) towards the lateral aspect of the foramen magnum, and then heading superiorly (pink) as the posterior meningeal artery.

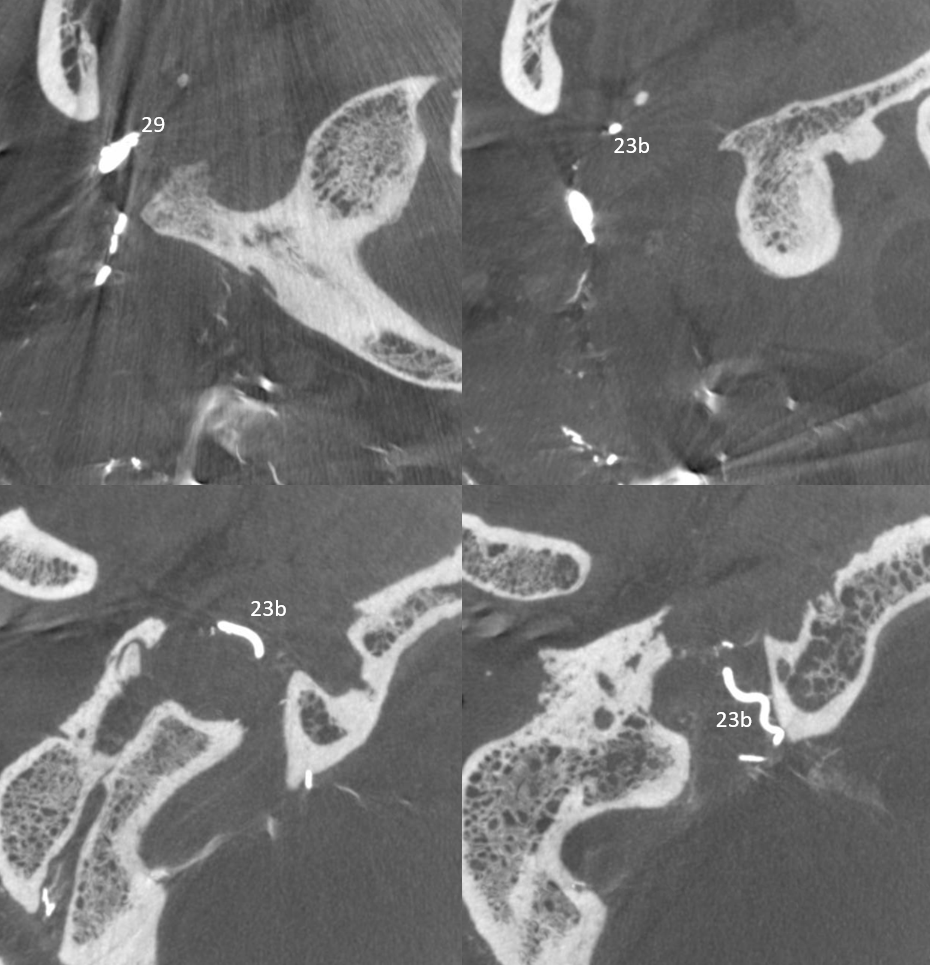
Mastoid Foramen. Same patient. The extracranial (black) and intracranial (white) openings of the mastoid foramen are defined by the transosseous segment (purple) of the mastoid artery.
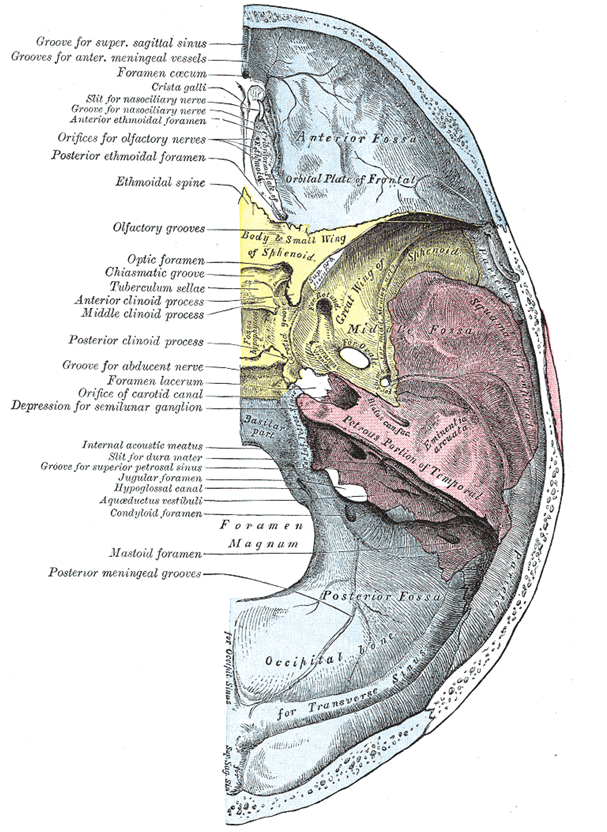
Gray’s Anatomy Plate 135. Although the mastoid foramen is drawn and labeled here, the posterior meningeal grooves arise from the condyloid (condylar) foramen which, when it exists, transmits the jugular branch of the ascending pharyngeal artery (in this specimen, the source of posterior meningeal artery supply)
Occipital – Ascending Pharyngeal Complex
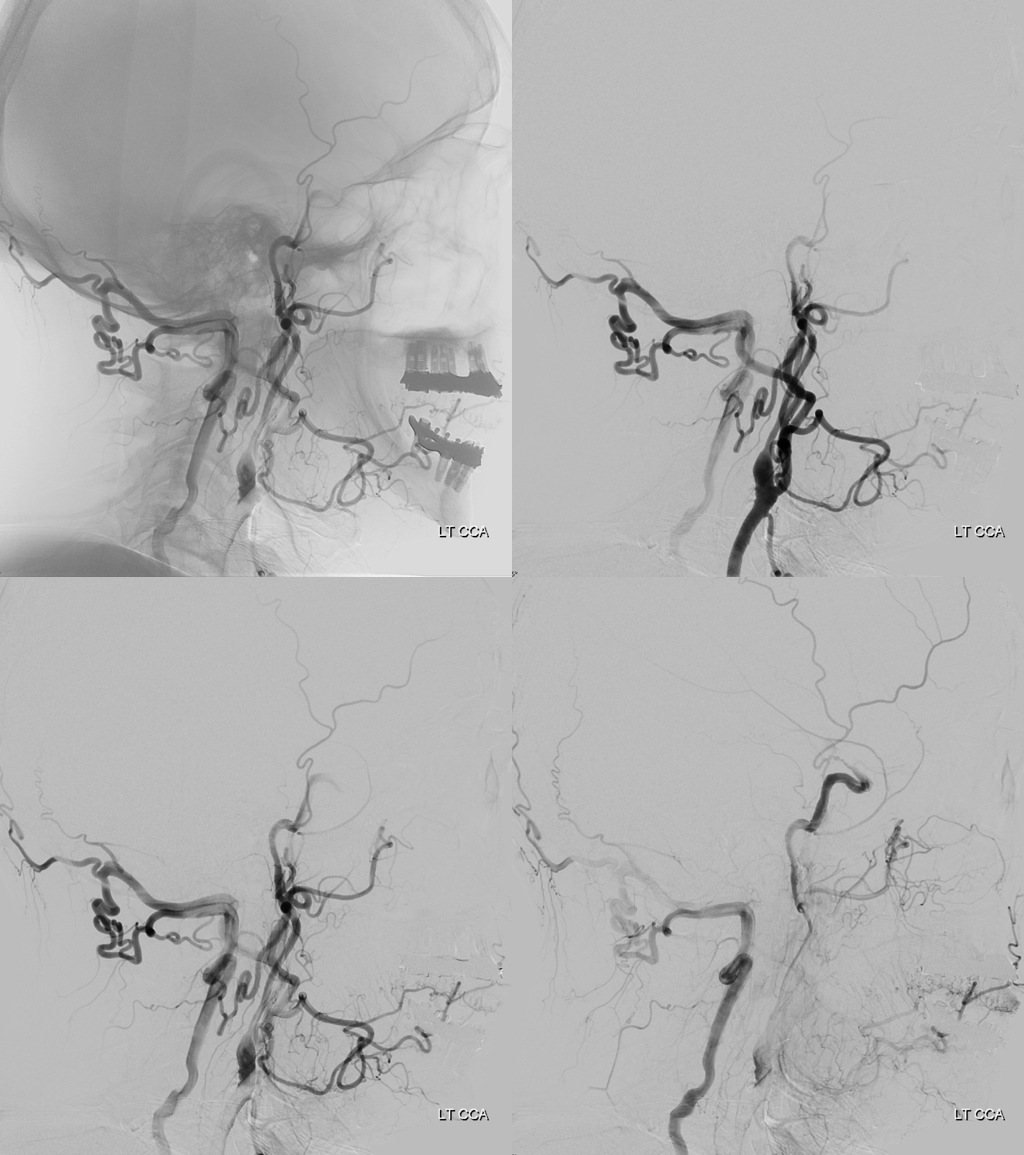
The relationship between occipital and ascending pharyngeal arteries is of extreme importance (see ascending pharyngeal page for complementary info). The ascending pharyngeal artery can “arise” from the occipital, known as pharyngo-occipital variant. However, perhaps more importantly, the ascending pharyngeal itself is responsible for various territories — the main parts are pharyngeal trunk and neuromeningeal trunk, with latter subdivided into jugular and hypoglossal divisions, entring the skull through their respective foramina. A number of variants are encountered in practice — for example separate origins of neuromeningeal trunk from occipital and pharyngeal from ECA, jugular or hypoglossal division origin from occipital with rest off ascending pharyngeal, etc. The picture below shows some but not all of these variations.
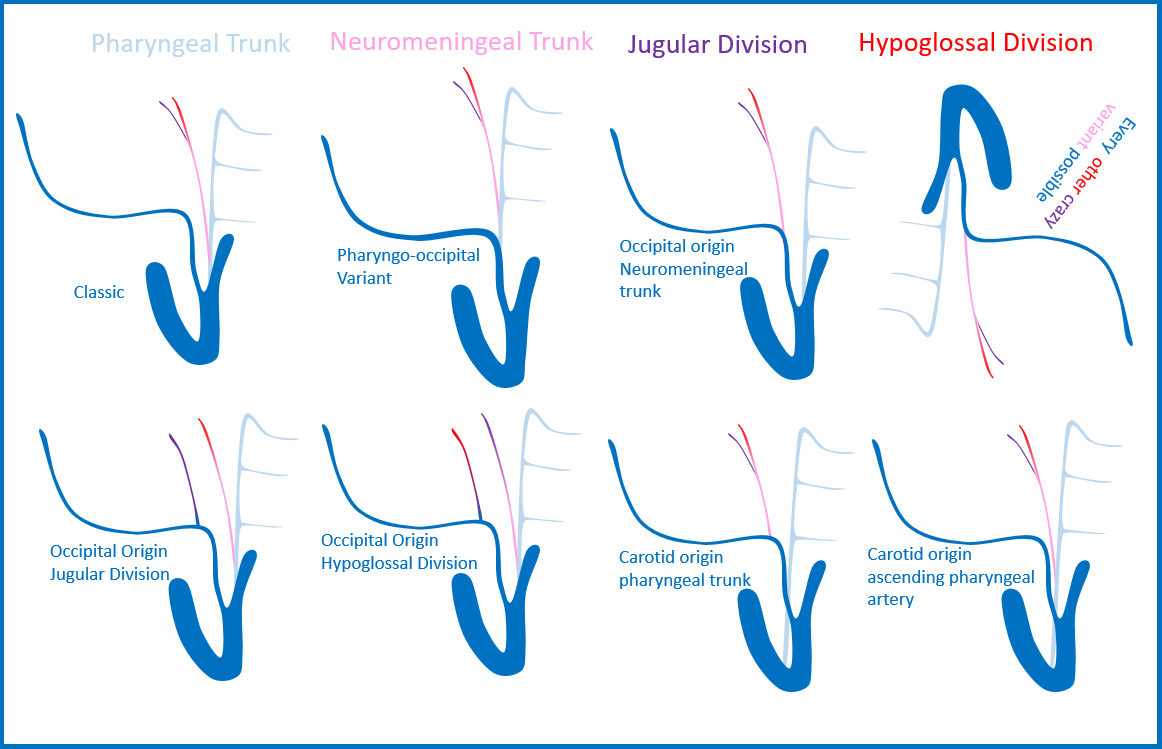
You get the idea. The practical lesson here is to know that isolated branches from occipital artery (jugular, hypoglossal divisions) can supply their corresponding cranial nerves, even if the ascending pharyngeal seems to be basically present. Below are some examples
Occipital origin hypoglossal division
Separate origins of pharyngeal trunk (ball arrow) and hypoglossal division (white arrow) from the occipital artery. The hypoglossal contributes to supply of posterior meningeal territory (a.k.a. ascending pharyngeal origin of posterior meningeal artery)
A diagnostic catheter position distal to the pharyngeal trunk isolates the hypoglossal division (white arrows), which opacifies the odontoid arcade (dashed arrows) via several anastomoses (white arrowheads) inside and outside the skull
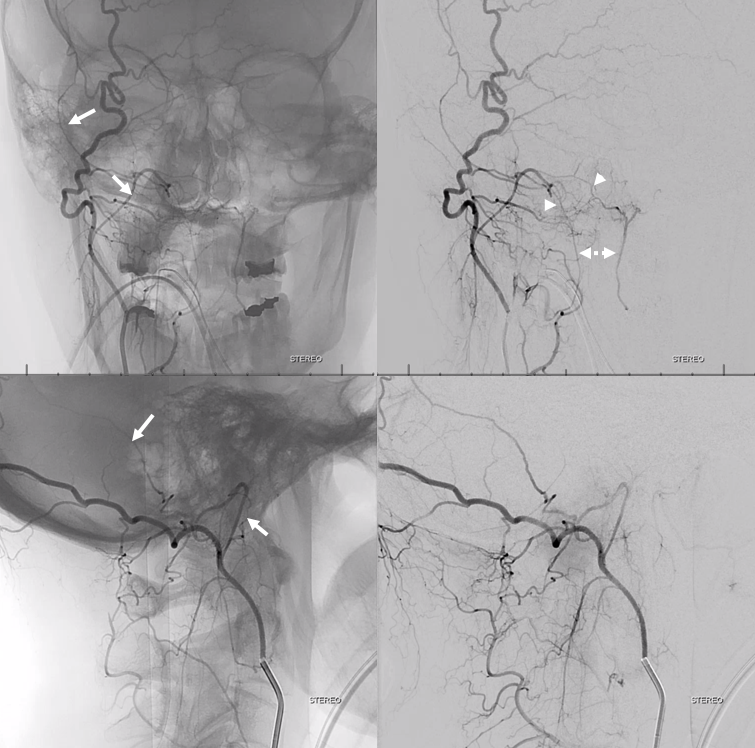
DYNA CT — same arrows as above. Notice the posterior meningeal artery in the groove of the sigmoid sinus (aka artery of sigmoid sinus — see meningeal arteries and middle meningeal artery pages for more info)
Cross-eye stereos
Anaglyph stereos
Another example — another nasty meningioma
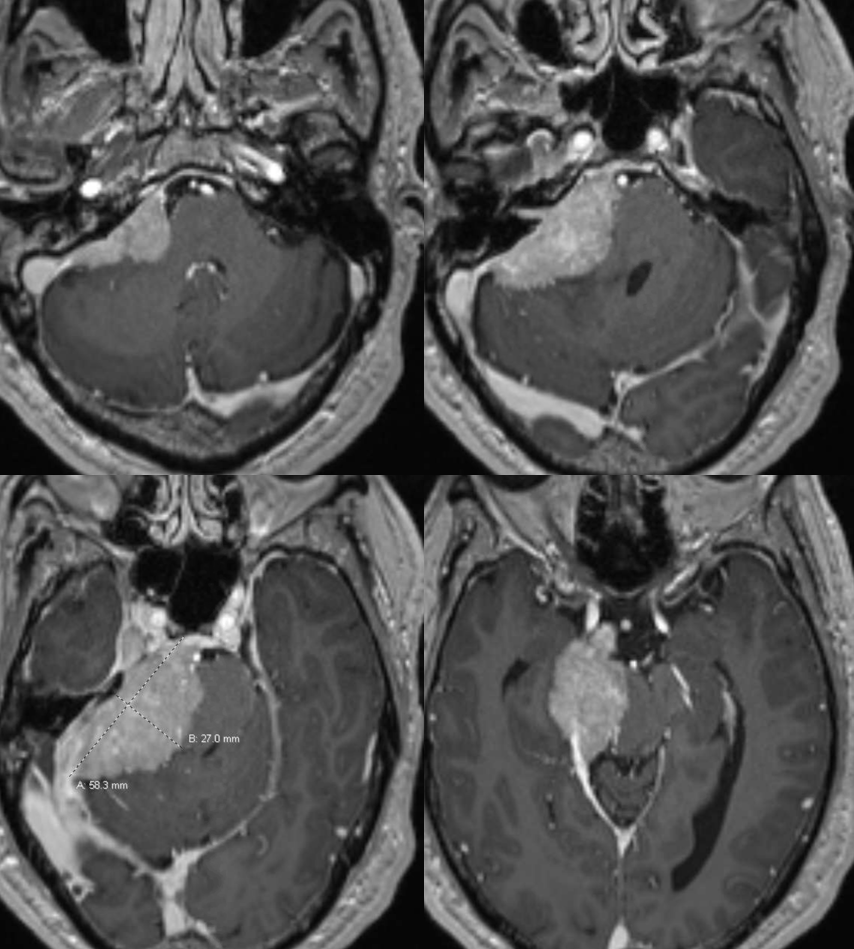
Jugular division (23b) origin from occipital (29) artery
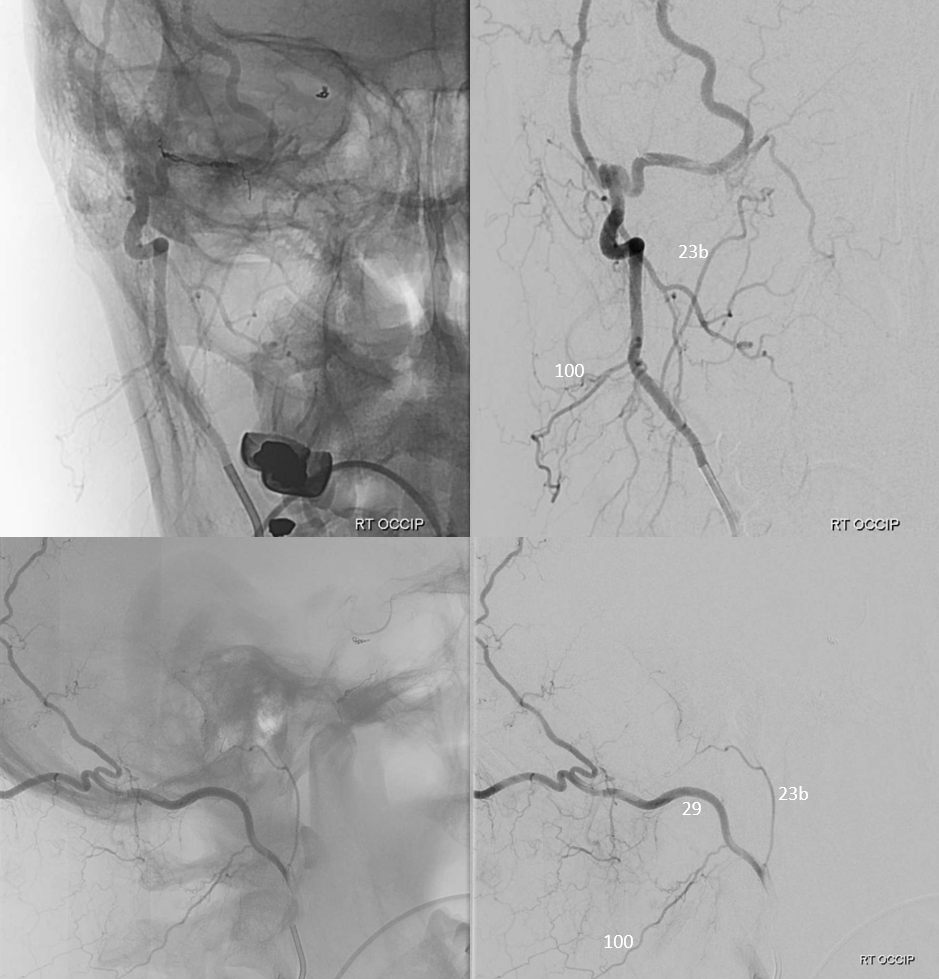
Axial DYNA MIPs
Another example:
Movie of DYNA CT — both jugular and hypoglossal divisions are off occipital — supplying posterior fossa meningeal tissues. Nice odontoid arch connection with hypoglossal. You can scroll through individual movie frames.
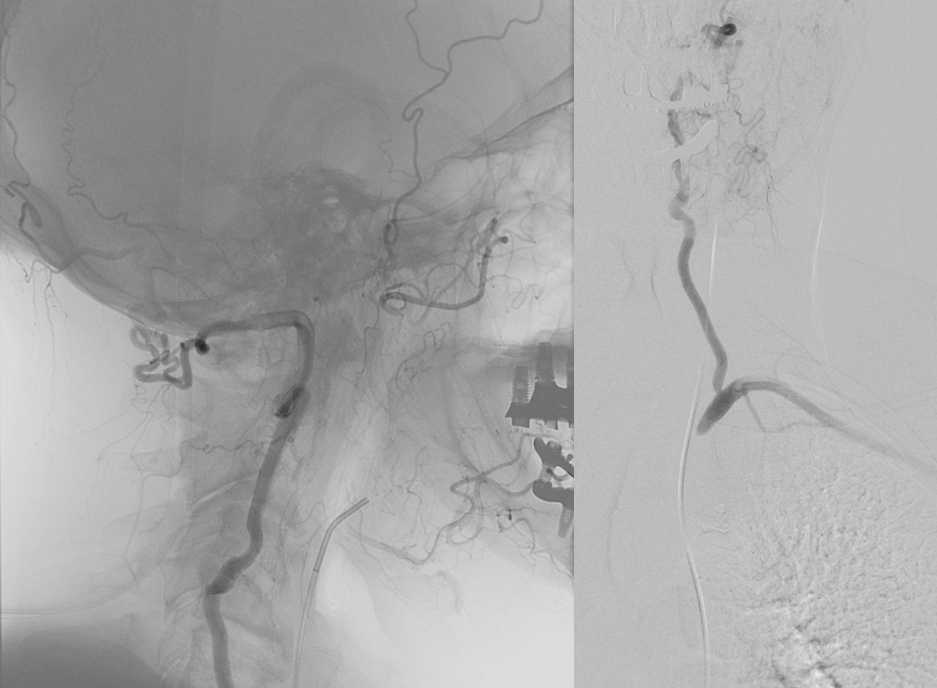
Sigmoid Dural Fistula
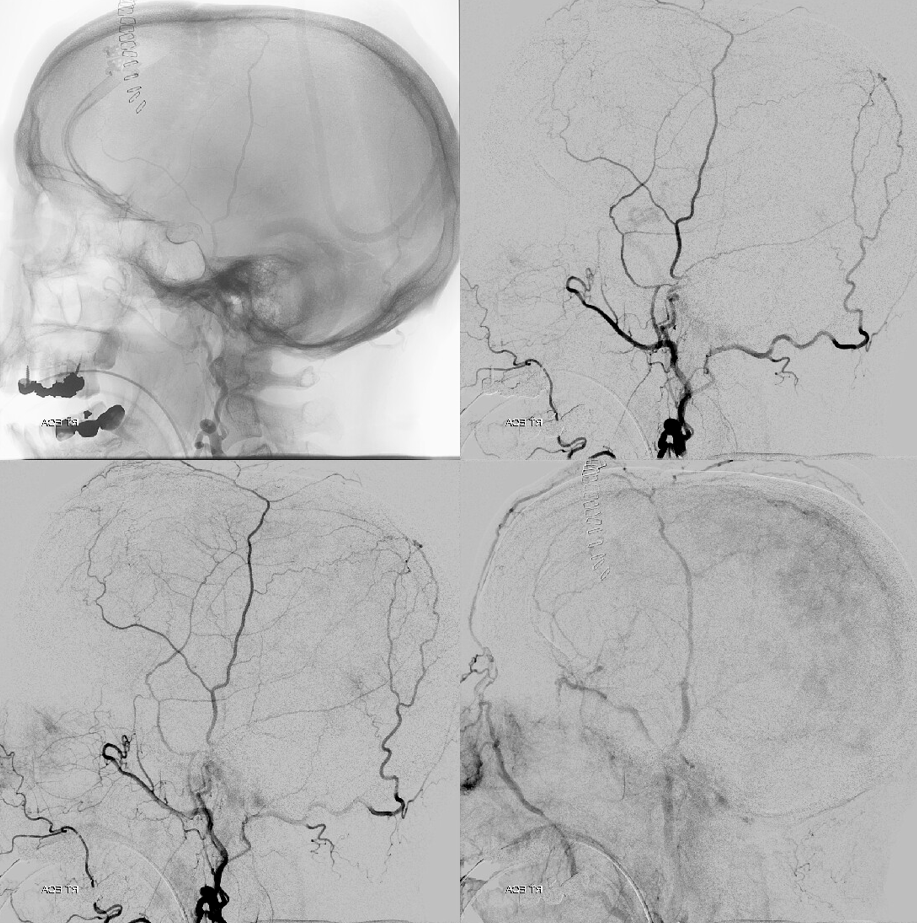
Another example — this time jugular branch is one arising from occipital — also dural fistulas. MRA
Angio — jugular division superimposed on sigmoid/jugular outflow
Cross-eye stereos
Another example of the same — jugular division — again running in the wall of sigmoid sinus
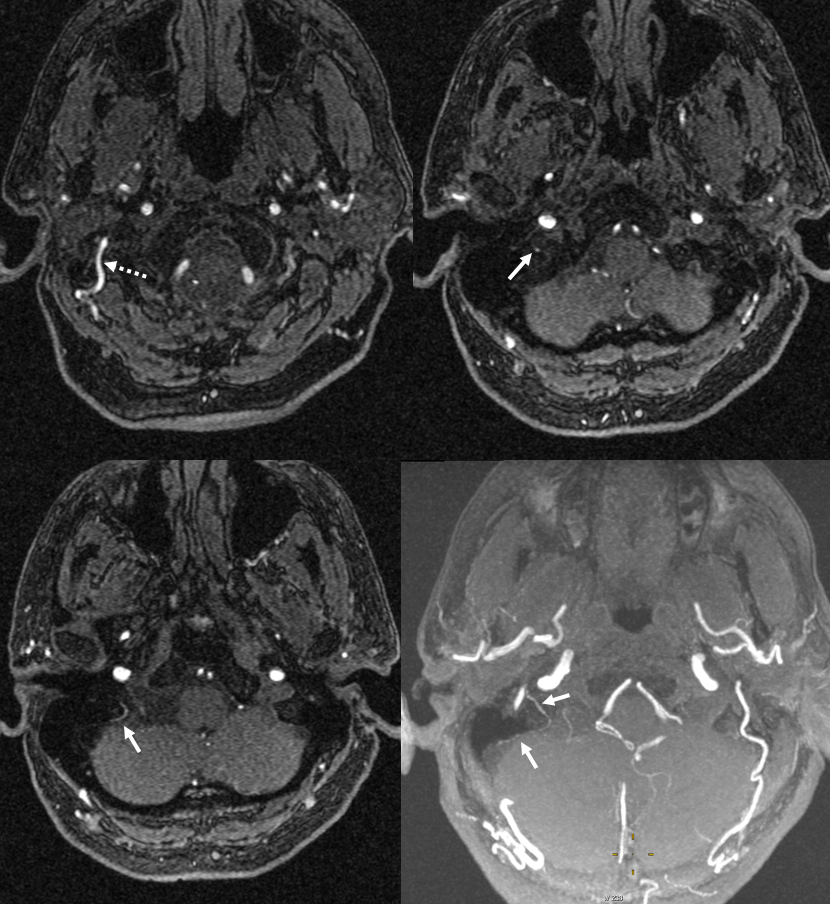
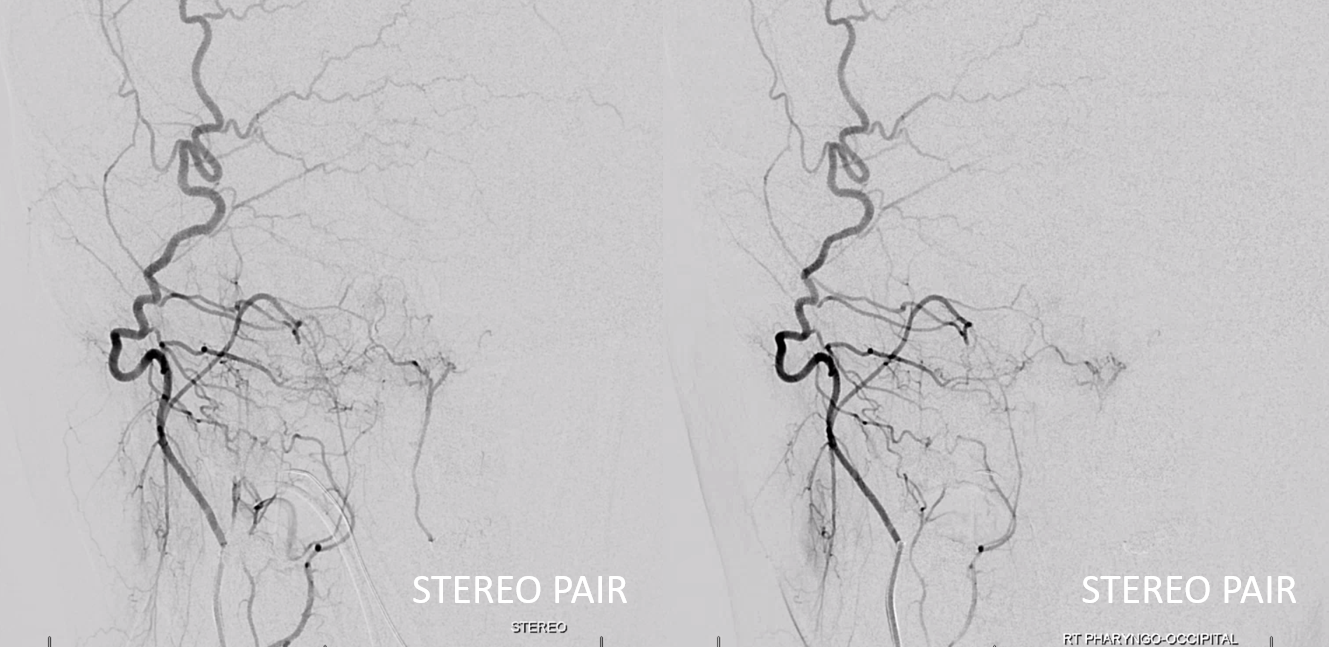
Occipital is marked by dashed arrows
Angio — nice parallel with sigmoid sinus
Occipitocarotid anastomoses and Common Carotid Occlusion
Proatlantal Artery
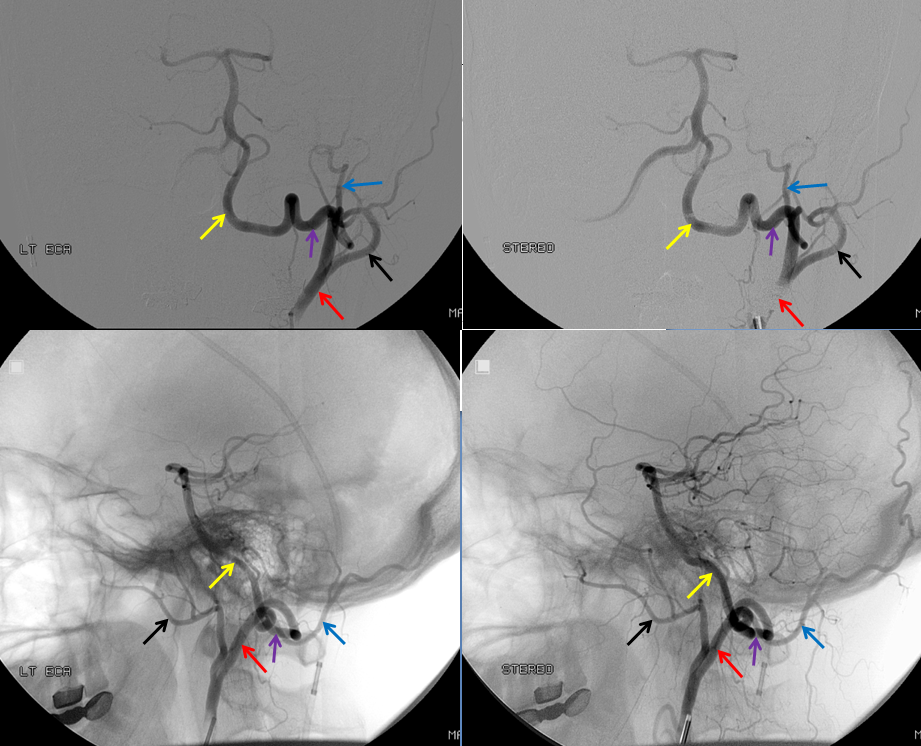
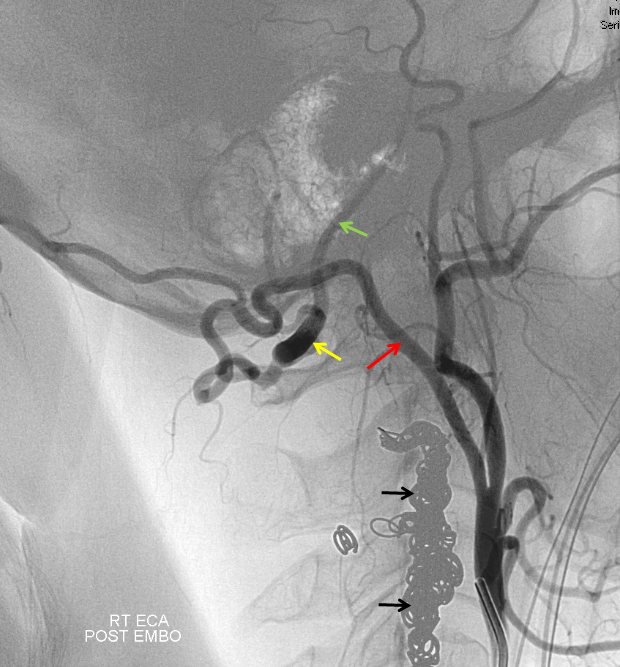
Embolization of the fistula has been carried out, with coils in the vert (black). The occipital (red), via the first segmental artery (yellow), now opacifies the vertebral (green) in antegrade fashion, a la Proatlantal I artery.
Occipital Artery Subclavian Steal
Here is a similar situation — subclavian steal. However, the patient is asymptomatic. Pressures in both arms are the same. Why — well, the C1 vert-occipital anastomosis and ascending pharyngeal artery musculospinal anastomosis provide the bulk of steal flow into the left vert, so the right vert is barely involved.
Actually, as it happens, this left vert is not even a vert — its one of those ascending cervical homologs since it enters the vertebral foramina at C5 level — see below — but that is just another embryology touch. Notice also some additional reconstitution of the subclavian artery distal to the “vert” — there is some unopacified inflow coming in. What is it?
See MRA neck — any idea what those vessels are?
Occipital-Superficial Temporal-Posterior Auricular Balance
The posterior auricular artery is probably the most ignored ECA branch. It is however there — and frequently supplies the mastoid branch that goes into the mastoid foramen and forms part of the facial nerve arcade (together with petrous branch of the MMA). So it is useful to know about it.
The posterior auricular is usually in balance with occipital and superficial temporal arteries. When occipital and STA are large, posterior auricular is correspondingly small. In the case below, the STA territory is limited to the frontal scalp (black arrows). The parietal scalp (normally supplied by the parietal branch of the STA) is instead taken over by the posterior auricular (white arrows). The occipital is dashed white arrow
Supply of the Meninges
The Traditional Occipital Contribution to meningeal supply is via the Posterior Meningeal Artery — responsible usually for the temporo-occipital area or the posterior fossa (all those occipital connections to sigmoid dural fistulas for example are in the temporo-occipital region). However, there are important exceptions. In this case of subdural hematoma embo, the occipital ends up supplying a lot of parietal meningeal territory via a large transosseous branch. The full case is here. Some select images are below
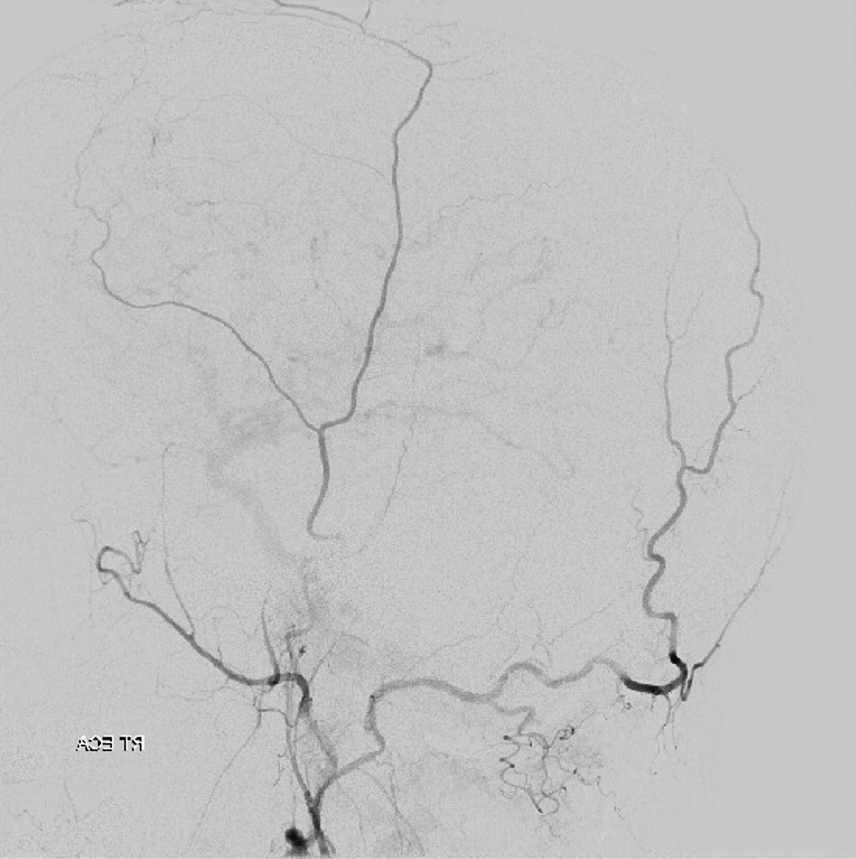
Global ECA injection
MMA injection with portion of parietal meninges not visualized
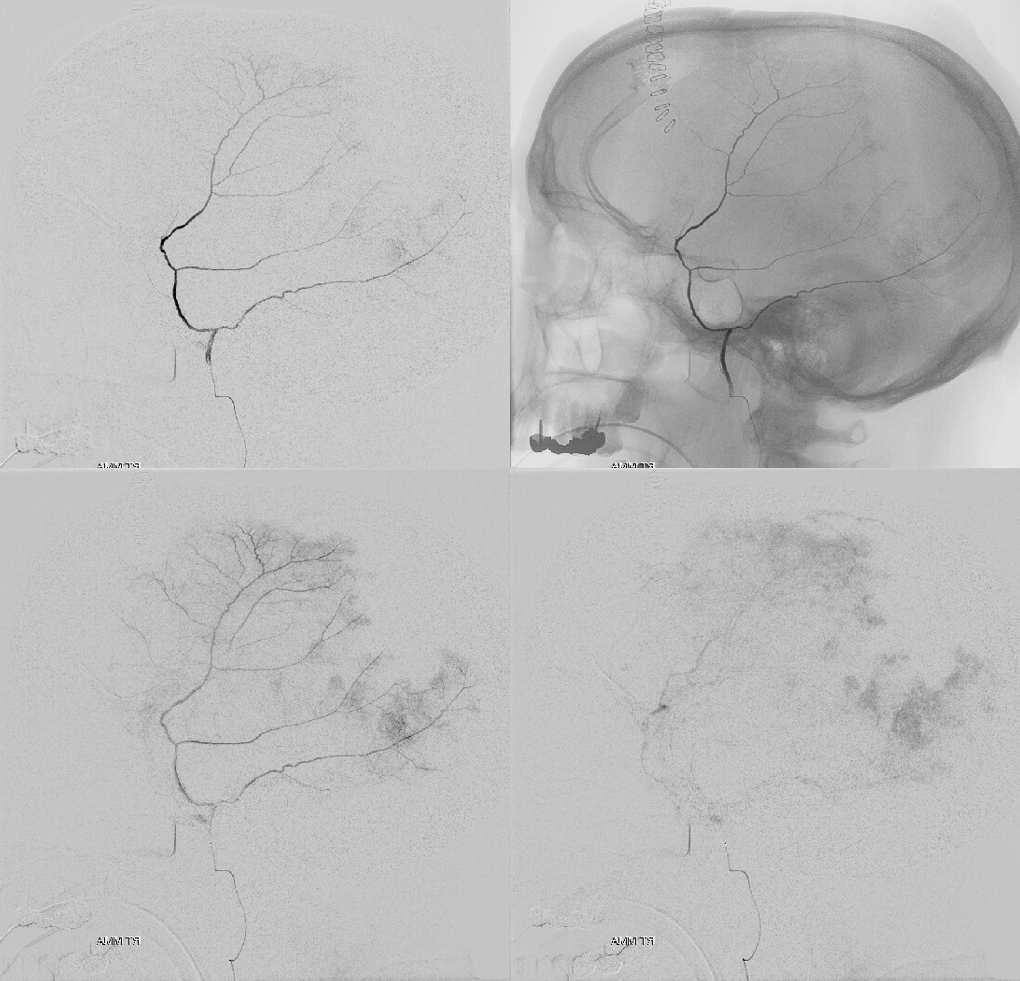
Occipital Injection
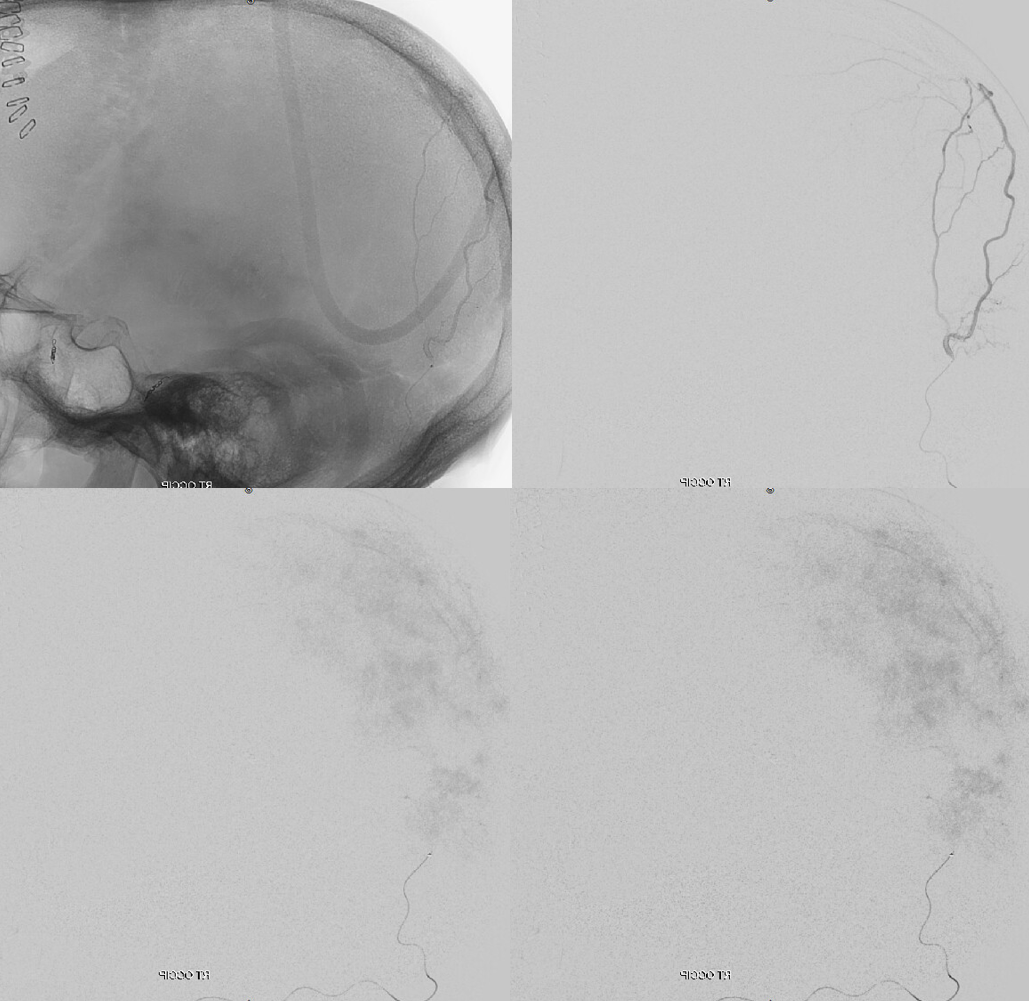
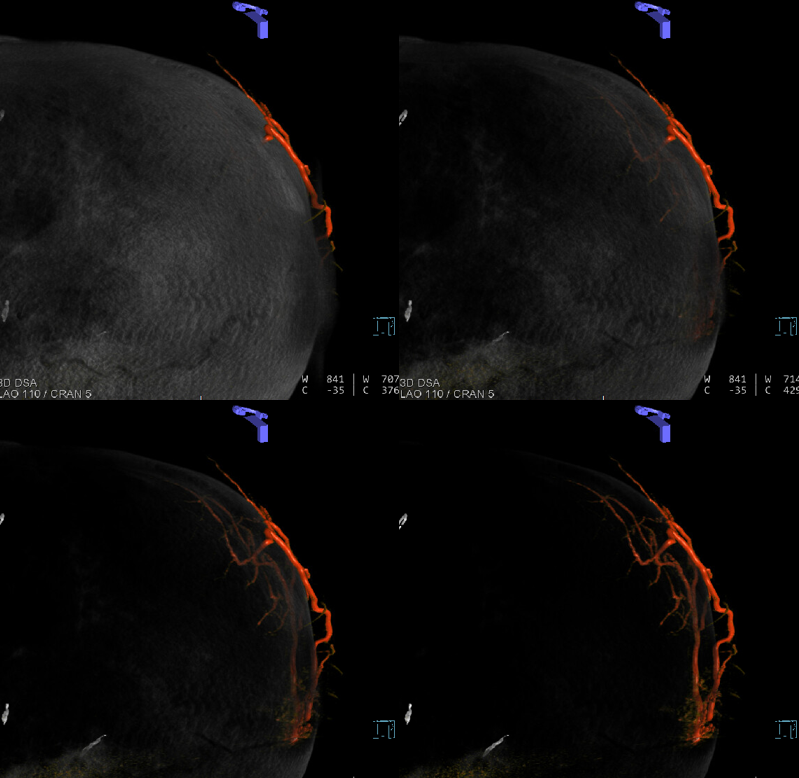
VR images of progressive bone removal to show transosseous branch
Final headway duo position
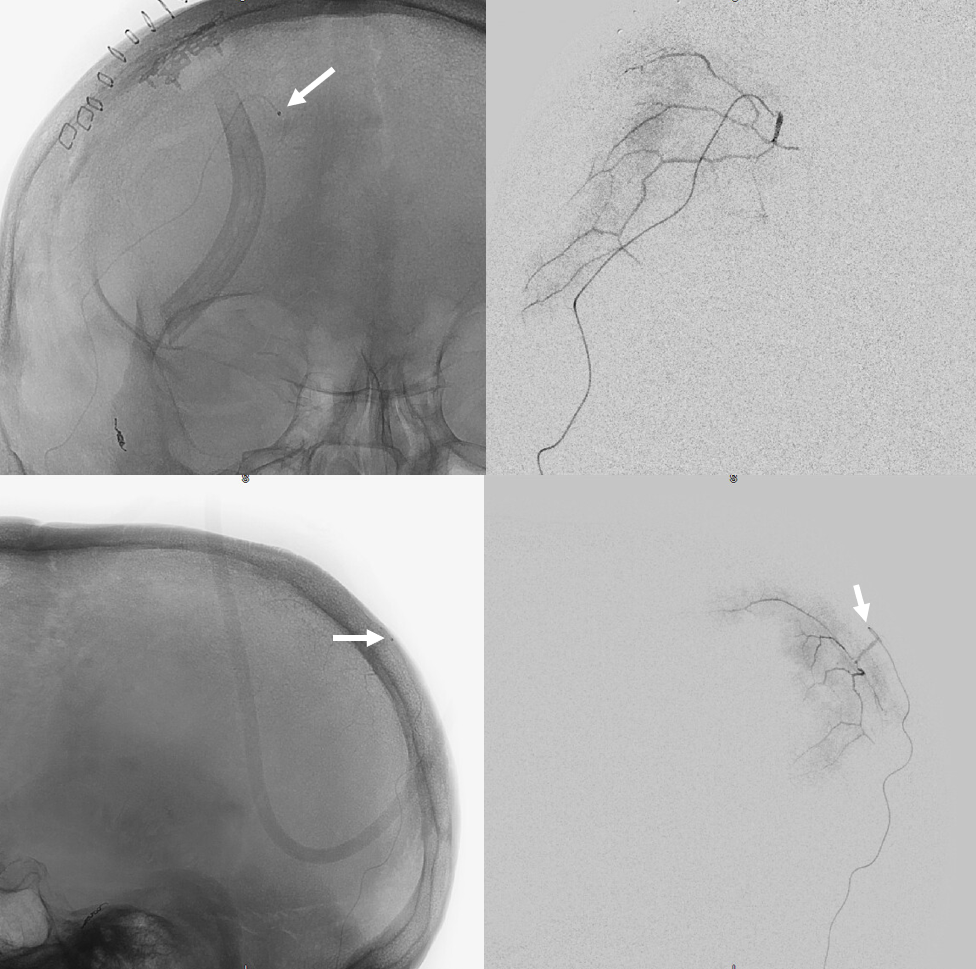
Post embo