In collaboration with Dr. Chandra Sen, Dr. David Gordon, and Dr. Eytan Raz
The dominant supply of a meningioma is determined by its original location. With continued growth, meningiomas will recruit additional sources, closely corresponding to their location and embryologic disposition of the host. For example, a sphenoid wing meningioma may receive dominant supply from the ILT, the middle meningeal, or accessory meningeal arteries, depending on which vessel was the pre-morbid dominant supplier to the area of subsequent tumor origin. In a patient with recurrent meningeal variant, for example, dominant supply will arise from the ophthalmic artery.
When it comes to petroclival meningiomas, it is thus reasonable to expect multiple sources of supply. The ascending pharyngeal artery, particularly the jugular branch of the neuromeningeal trunk, will nearly always be contributing, as will the ipsilateral ILT or MHT. Large petroclival meningiomas will often have bilateral MHT or ILT supply — usually the ipsilateral branch is the ILT, and contralateral is the MHT (because MHT has medial / midline territory, while ILT is by definition inferolateral).
The notion that both MHT and ILT are always off limits for tumor embolization is not in agreement with the ultimate goal of effective devascularization. First, the territory these branches supply is no more “dangerous” than other branches which are routinely subjected to particle embolization. In fact, the petrous branch of the MMA, with its supply of the facial nerve arcade and petrosal nerve, or the neuromeningeal trunk of the ascending pharyngeal artery, which supplies CN 9, 10, and 11 (jugular division) and 12 (hypoglossal division), are as eloquent as MHT or ILT supply to CN III, IV, V, or VI. Second, it is just as easy, and perhaps easier, to get into “dangerous anastomoses” trouble with MMA or AP (vertebral, carotid, ophthalmic connections) as it is with ILT or MHT. In a certain sense, dangerous anastomoses during ILT and MHT are actually easier to monitor — basically watching for ipsilateral carotid reflux, and contralateral carotid with MHT (inferior clival / hypophyseal branches, vestiges of the primitive maxillary artery) and ophthalmic branches during ILT embo (monitoring for anything going ventral).
If a tumor has extensive ILT or MHT supply, and if the operator decides not to proceed with embolization of these pedicles, it is probably best to consider as to whether it makes sense to embolize the tumor at all, since a very partial embolization accomplishes no medically useful purpose. In our experience, the incidence of cranial neuropathy with particle embolization of these trunks is no higher than with takedown of the ascending pharyngeal — meaning less than 5%. Whether or not this kind of risk makes sense depends on tumor location and overall treatment goals. Again, for embolization to have an effective role it must be considered as part of an overall treatment package — the more risk is assumed by embolization the less risk is taken during surgery. Where that balance should be depends on mutually agreed upon pre-procedural goals.
From a technical perspective, the MHT is generally easier to catheterize than the ILT, because the former is located at the posterior genu and is thus easier to engage,whereas the latter usually comes off the lateral wall and curves posteriorly, making it doubly difficult to catheterize. Small particles can be used with nearly all microcatheters.
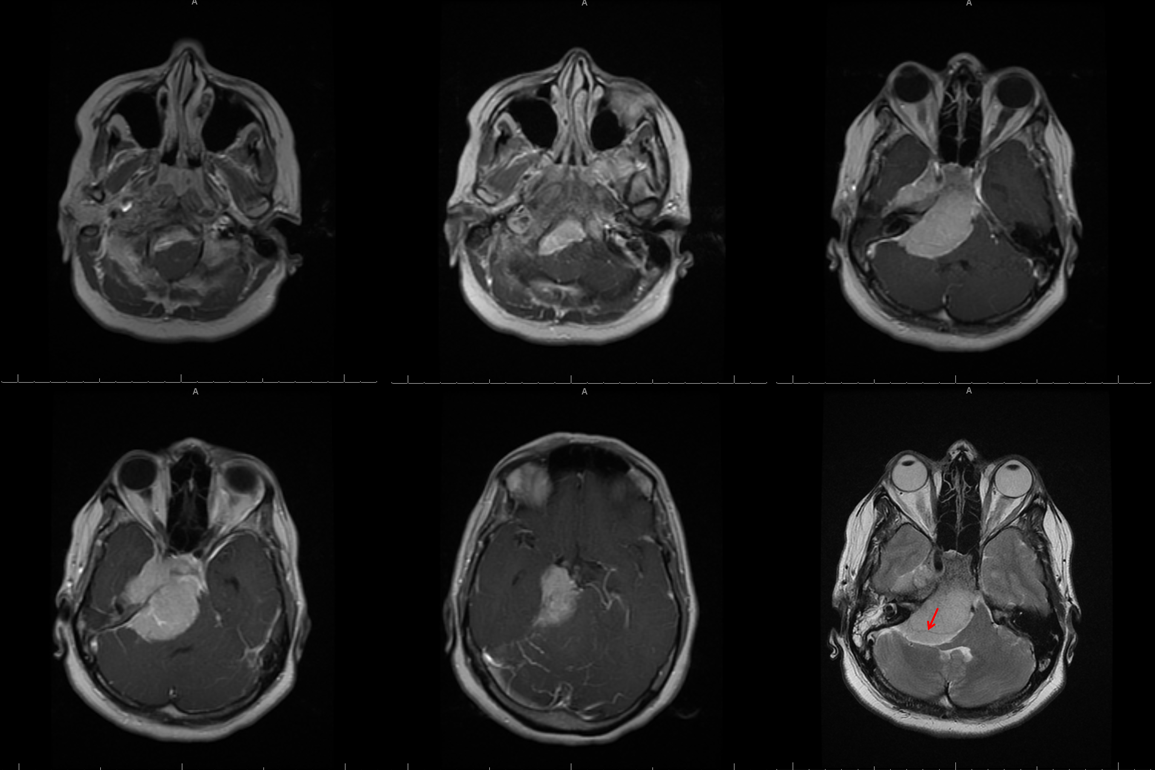
This patient presented with progressive imbalance; asymptomatic hearing impairment was noted on subsequent workup. Notice a vessel running through the tumor (red arrow, T2 image — this is the AICA)
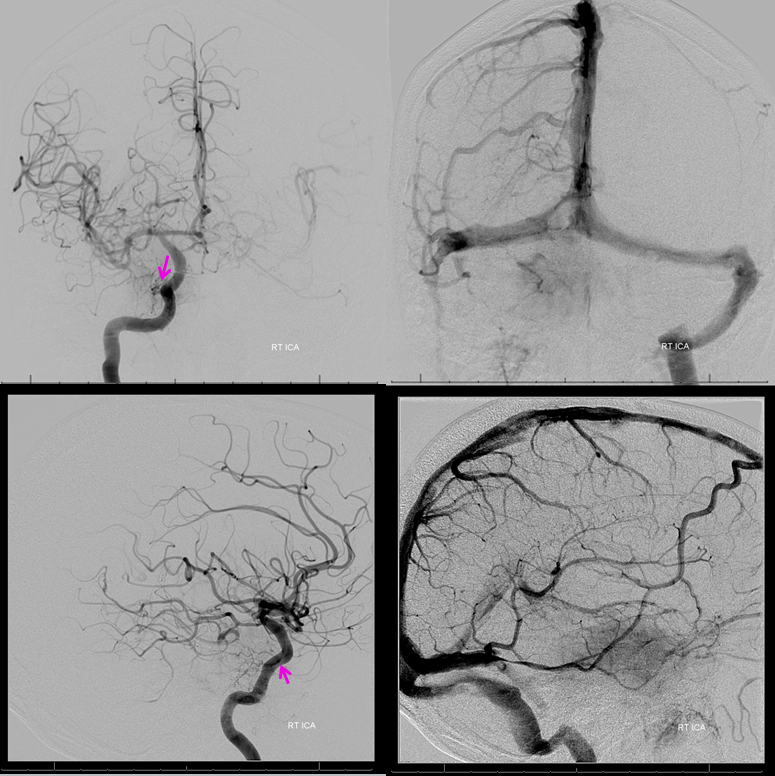
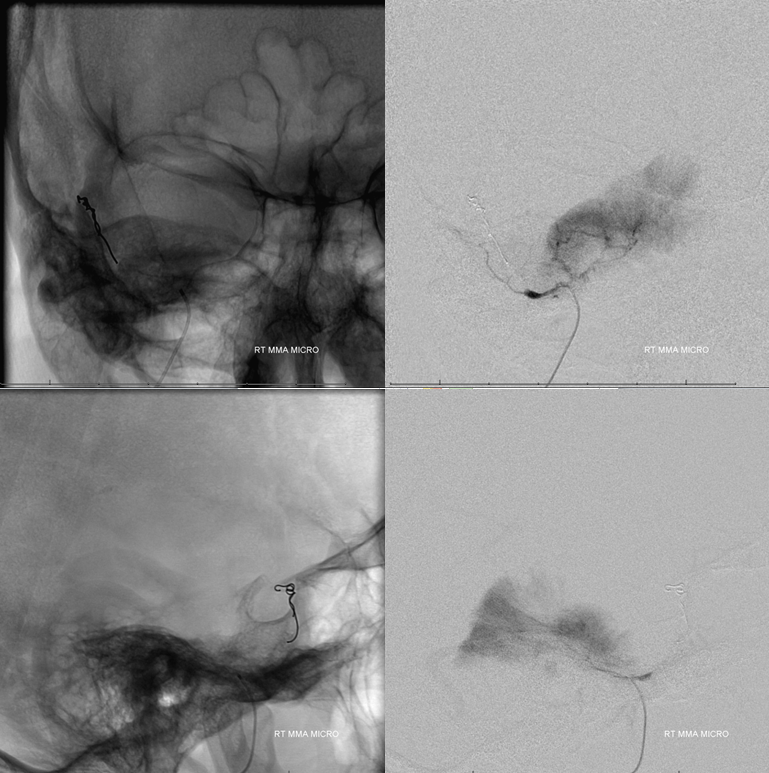
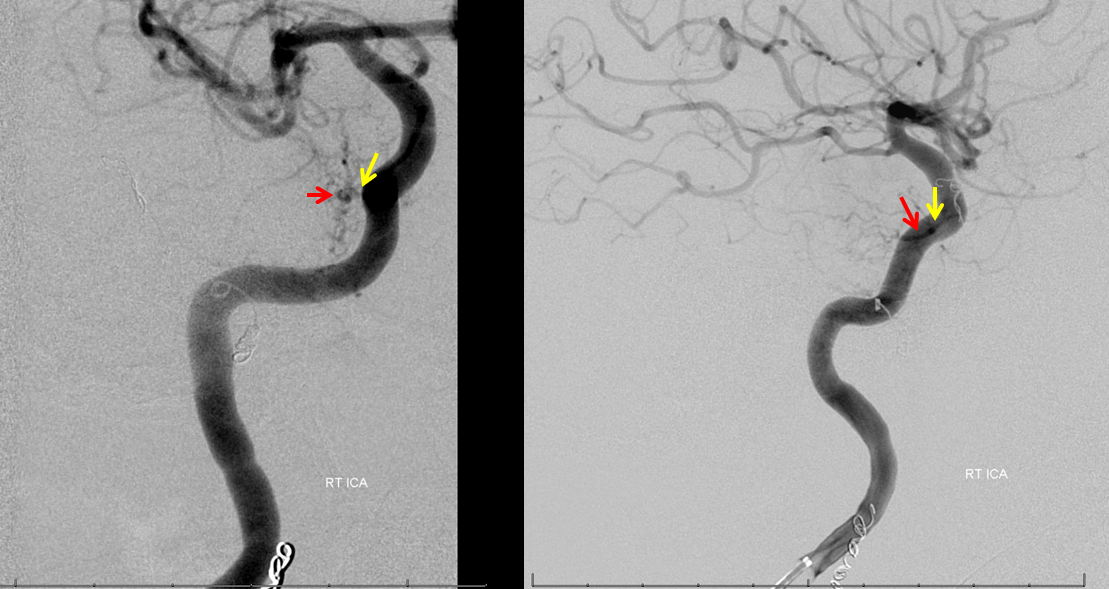
Right ILT supply from ipsilateral ICA (notice how the vessel curves backward). Right jugular bulb and vein are closed. There is a well-developed torcular and a right emissary vein present.
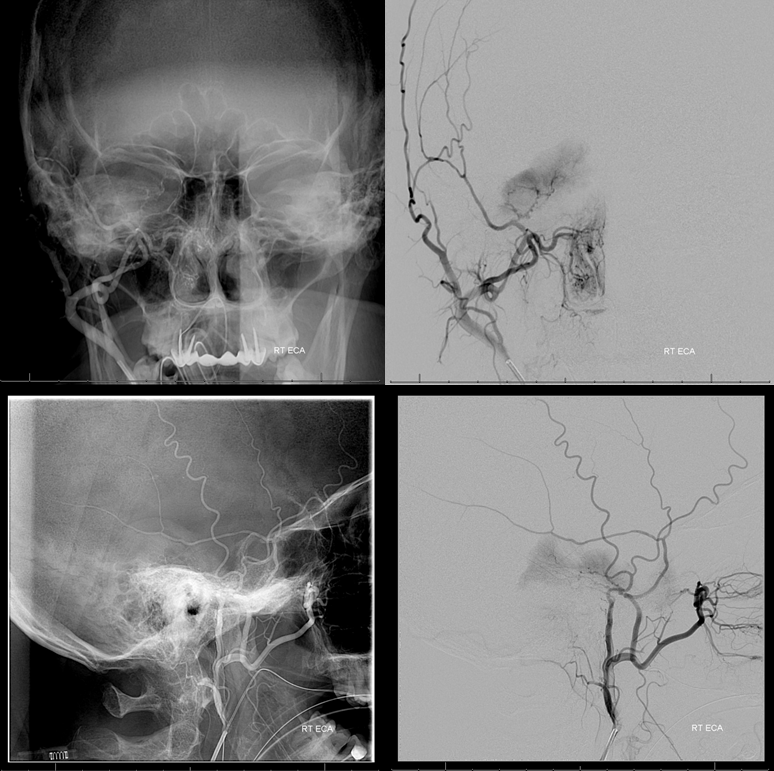
Petrous branch of the MMA (facial and petrosal nerve territory). Notice small foramen rotundum branch contribution (not marked)
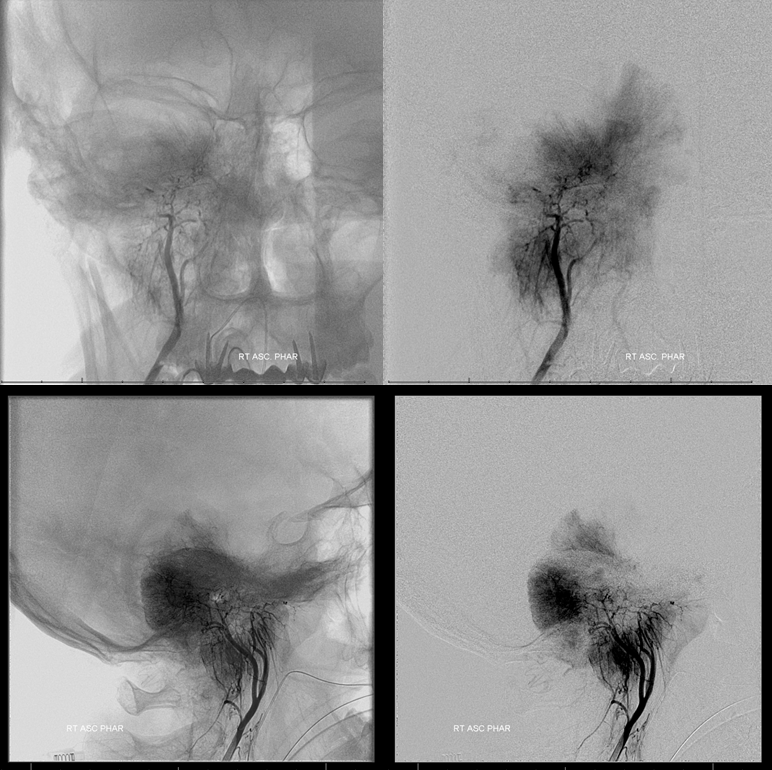
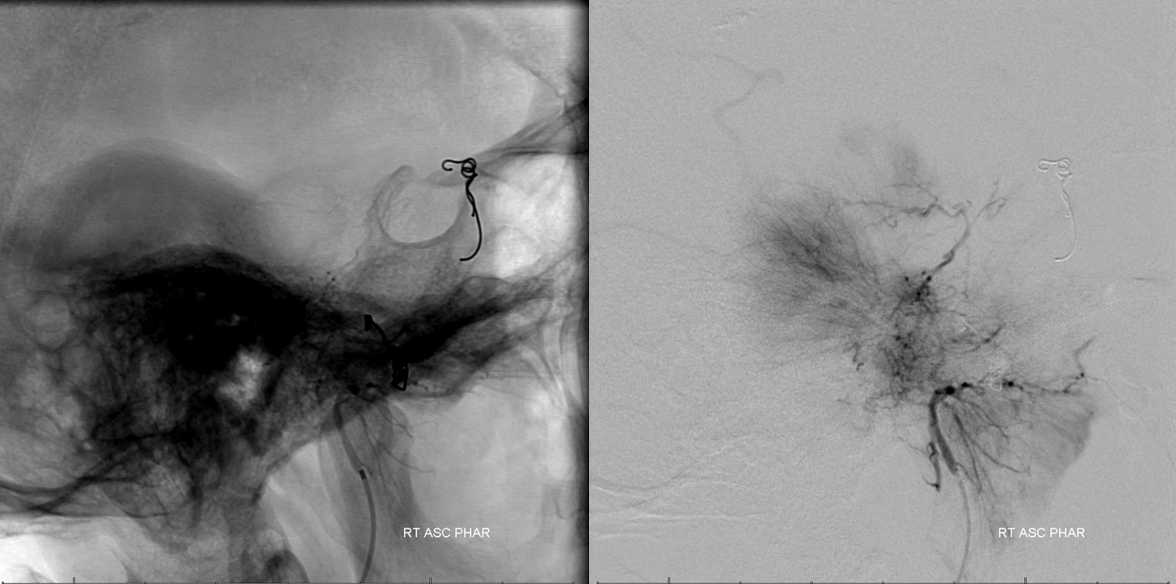
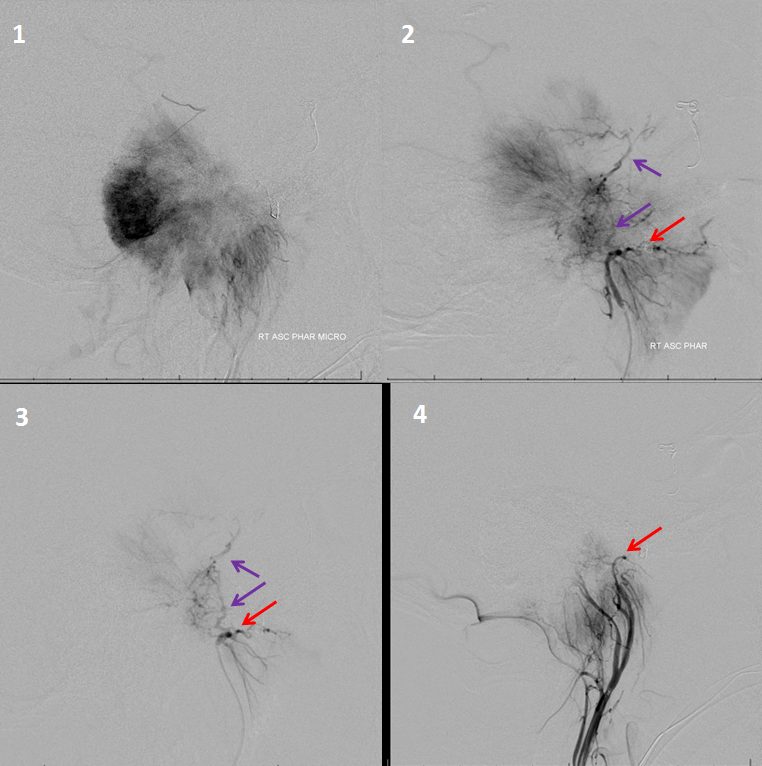
Dominant supply from the right ascending pharyngeal. The extremely dense contrast uptake of the posterior (dorsal) portion reflects its exclusive AP supply, which means that embolization will be particularly effective there.
Contralateral MHT supply
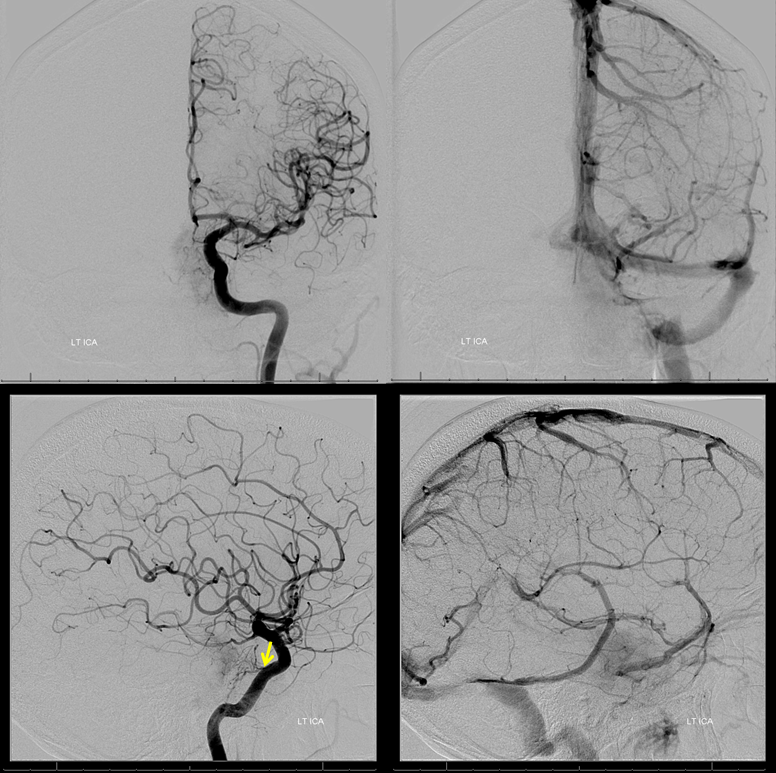
Left ECA with minimal AP supply

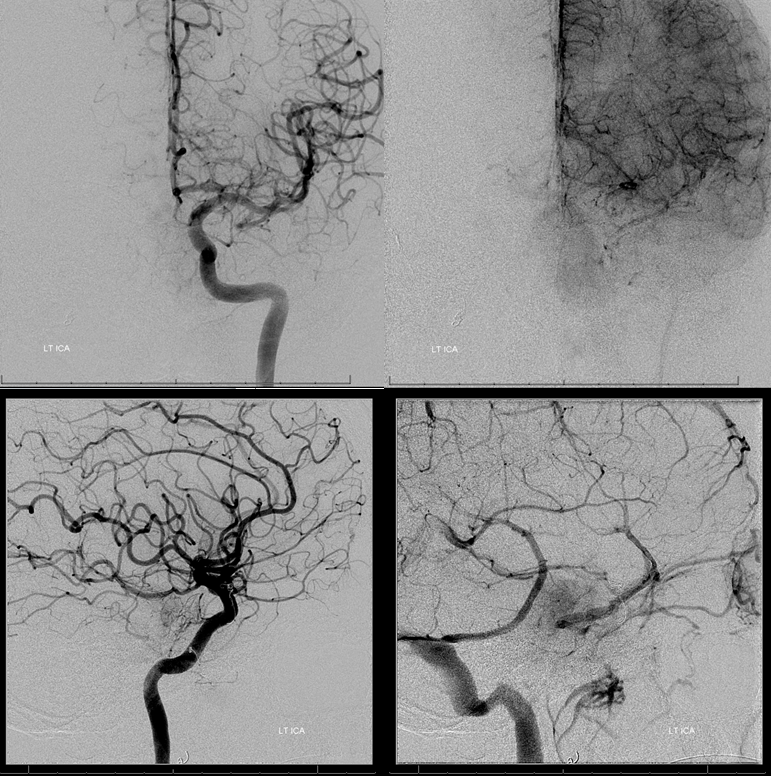
Arterial and venous images of posterior fossa injection are critical to understand shifts and identify vital vertebrobasilar structures. Even if no embolization is done, angiography will substanitally enhance pre-surgical planning. Note, in this case, size and position of the right AICA (red), shifts of the basilar, vertebral, and SCA/PCA. Right jugular is closed. The midbrain and pons drain into the left petrosal vein and into the left cavernous sinus (purple). The upper segments of the anterior mesencephalic vein, the interpeduncular vein, and contralateral basal vein are seen in the venous phase (none marked, see Venous System pages). Notice opacification of orbital veins (black), attesting to increased intracranial pressure. There is no pial supply to the tumor, which is very good. The odontoid arcade (green) supplies the portion of tumor at and below the foramen magnum.
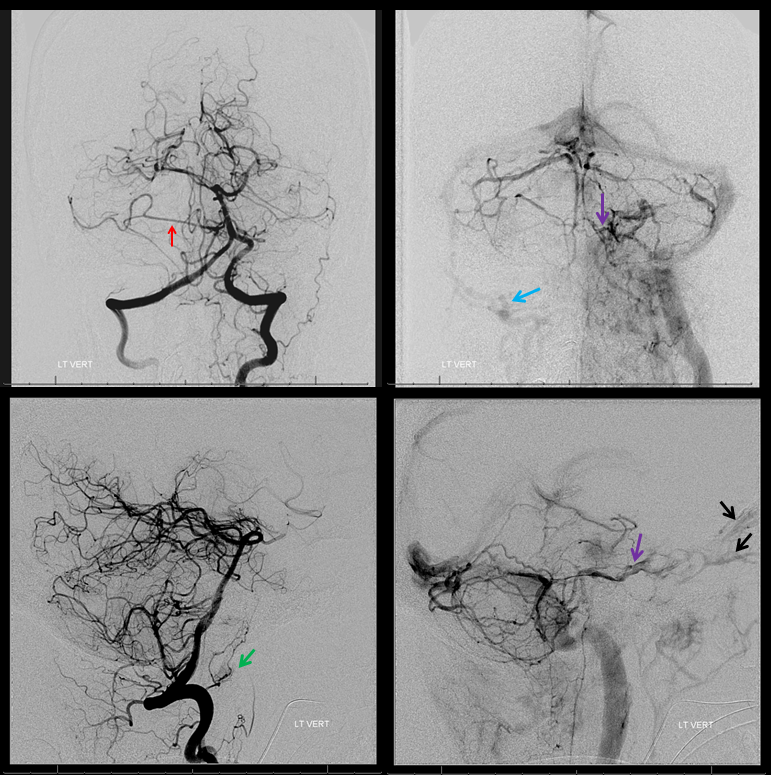
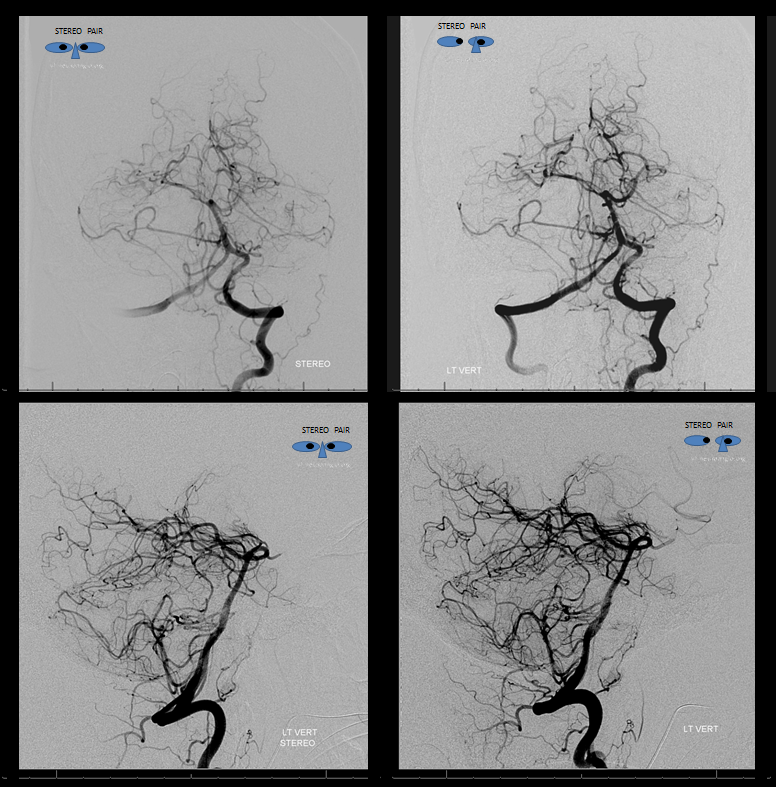
Stereo views are invaluable here.
Venous phase stereos
Time to start working. Closing distal MMA with a pushable fibercoil allows for petrous branch embolization from a more proximal position, with small (45-150 micron) followed by medium (150-250 micron) particles.
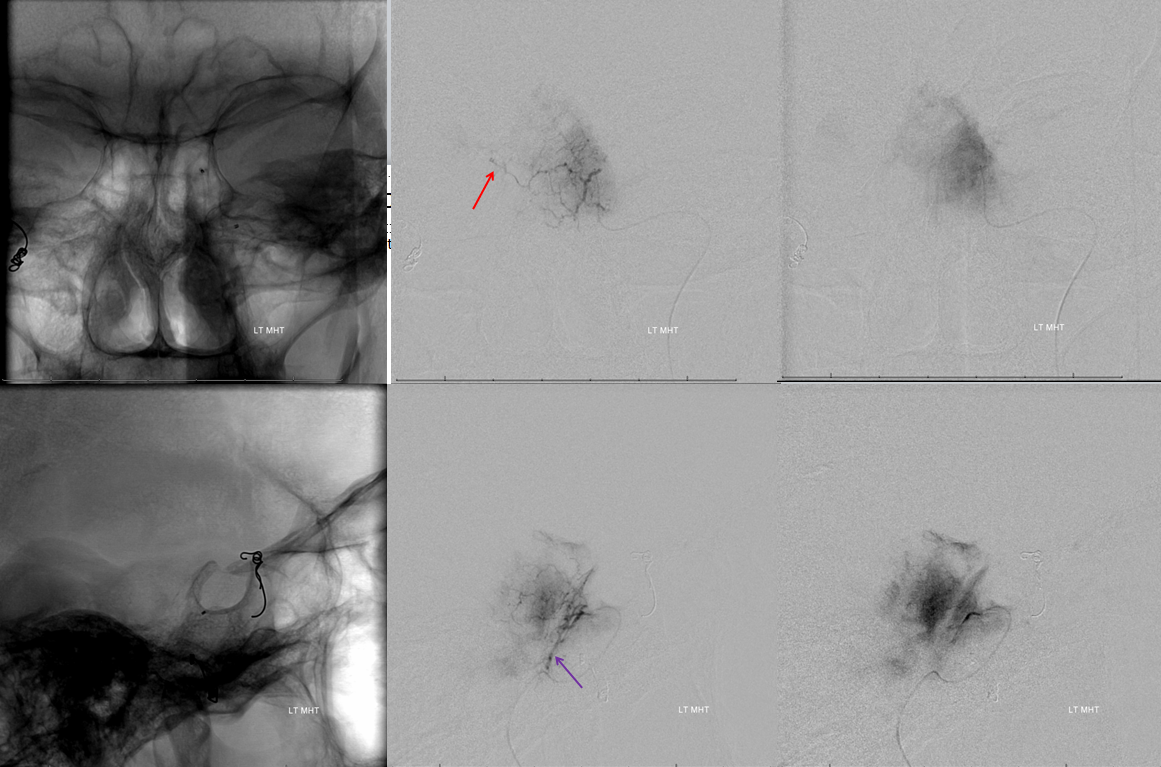
Next is ascending pharyngeal

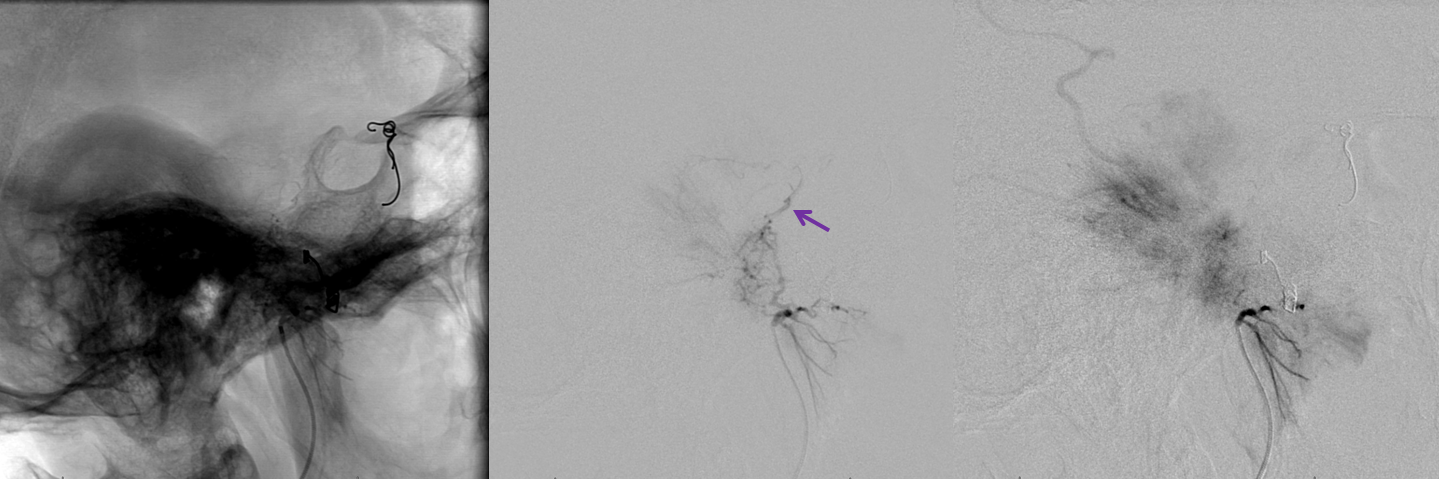
Periodic DSA runs show progress of embolization. Closure of primary tumor bed territory supplied by a given pedicle often “opens” or exposes other territories, which can be very helpful, as these territories can sometimes be more difficult to catheterize. Notice how in the injection below a more superior portion of the tumor, not seen on the original injection above, is now visible. This area is supplied by the MHT/ILT.
Later on during embolization. The clival branches are still visible (purple)
End of ascending pharyngeal embo. All of this was done with 45-150 micron particles
The image below shows progressive devascularization of the AP supply, including some secondary MHT/ILT territory embolization. Purple arrows point to the jugular division and clival branches; red to the superior pharyngeal branch. The posterolateral pharyngeal wall is richly collateralized and will tolerates reasonable embolization
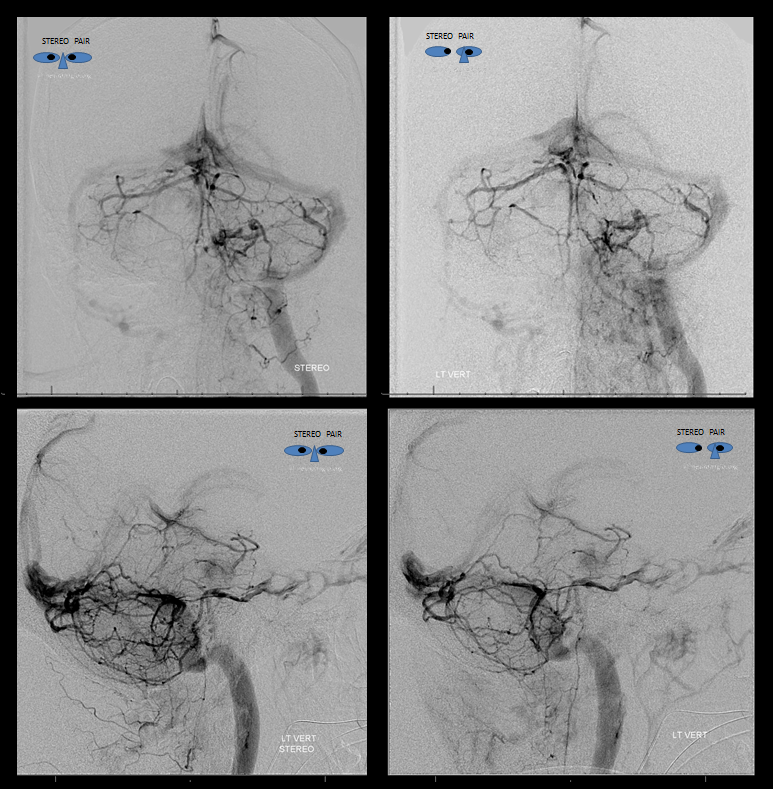
Right ILT consists of proximal medial-to-lateral portion (yellow arrow) and more distal ventral to dorsal portion (red arrow)
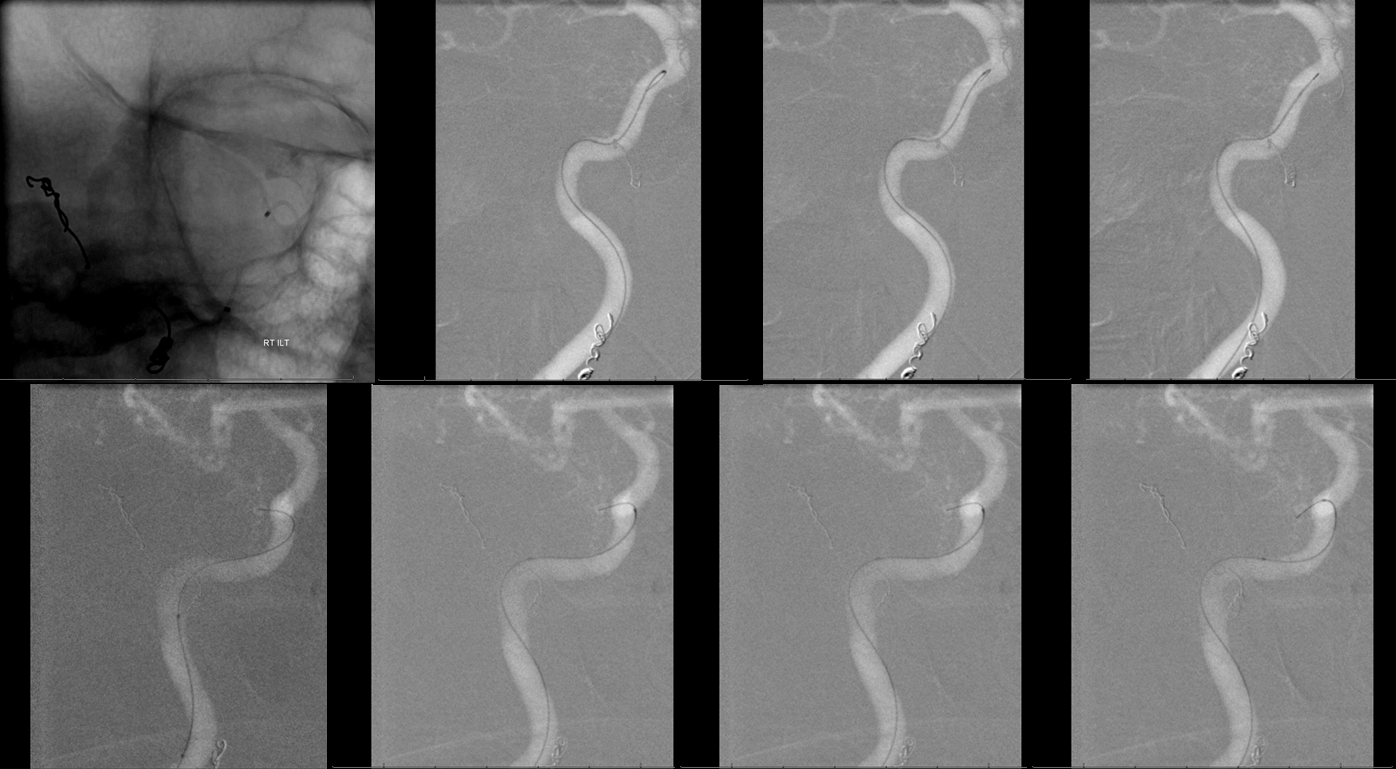
A reasonable position was achieved using Synchro soft 014 wire and a steam-shaped Echelon-10 catheter. A marathon can be used as well, if only small particles are going to be injected
ILT micro-injection. Notice re-visualization of the petrous MMA branch (red)
Post-embo right ICA. There is still an ILT blush, but substantially reduced.
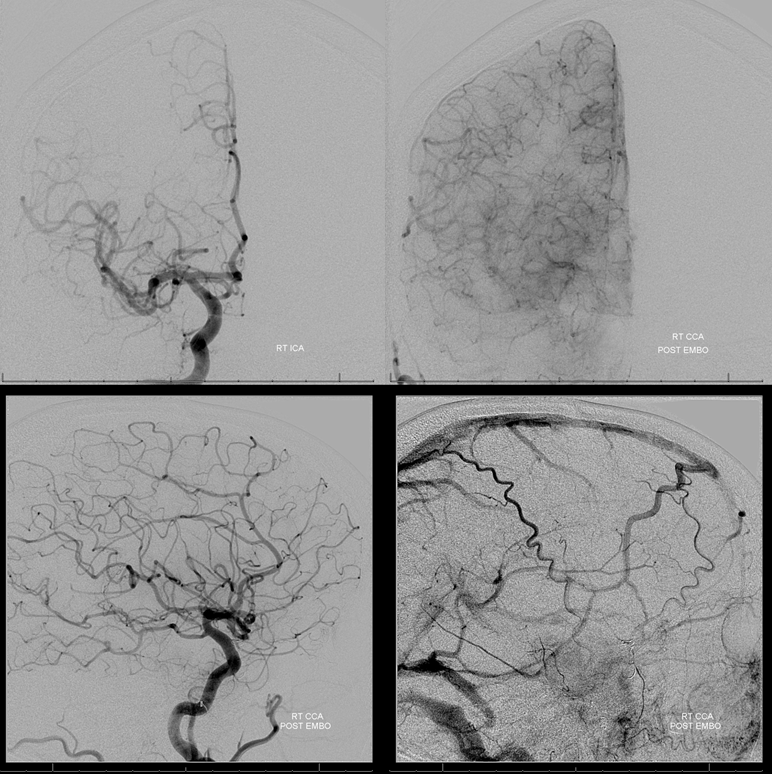
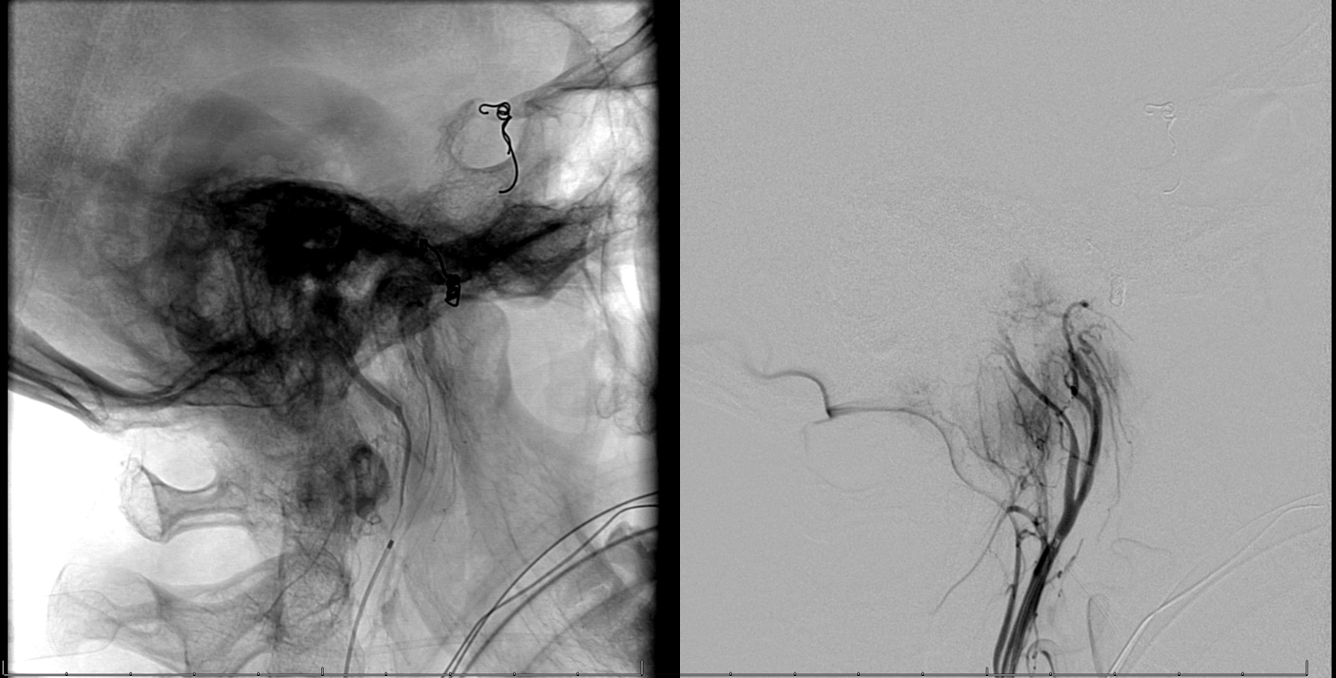
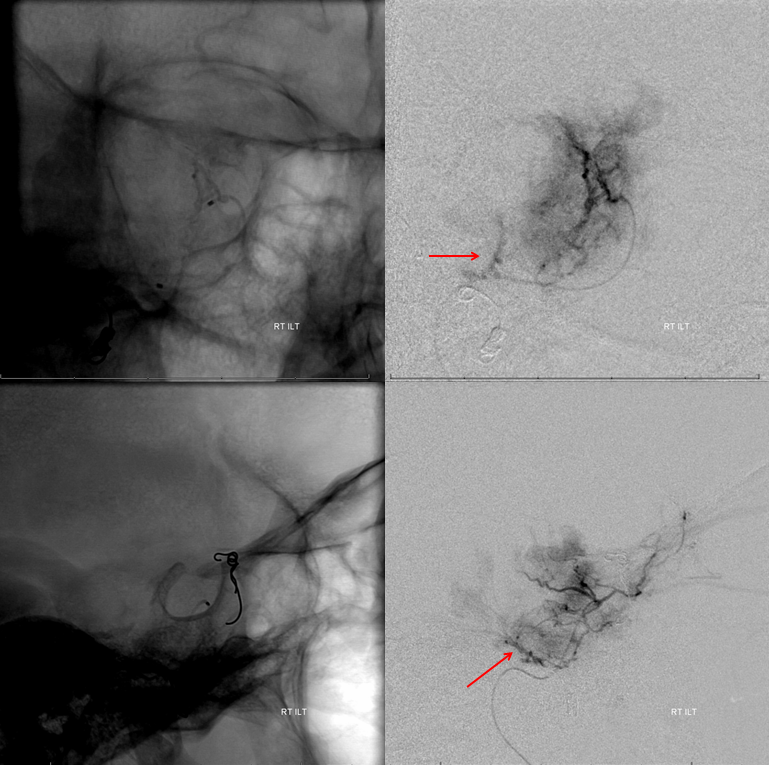
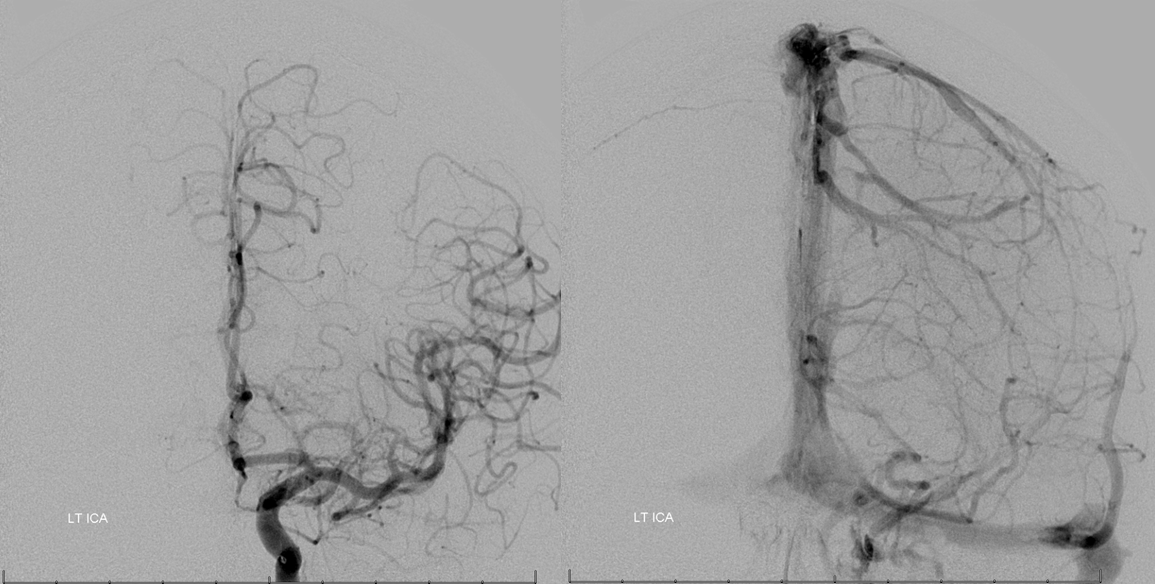
Left MHT contribution is alive and well
Catheterization is possible with a straight SL-10 catheter

MHT micro-injection. Notice inferior pituitary branch to the contralateral MHT (red, primitive maxillary artery remnant) as well as clival branch (purple) previously seen via the AP
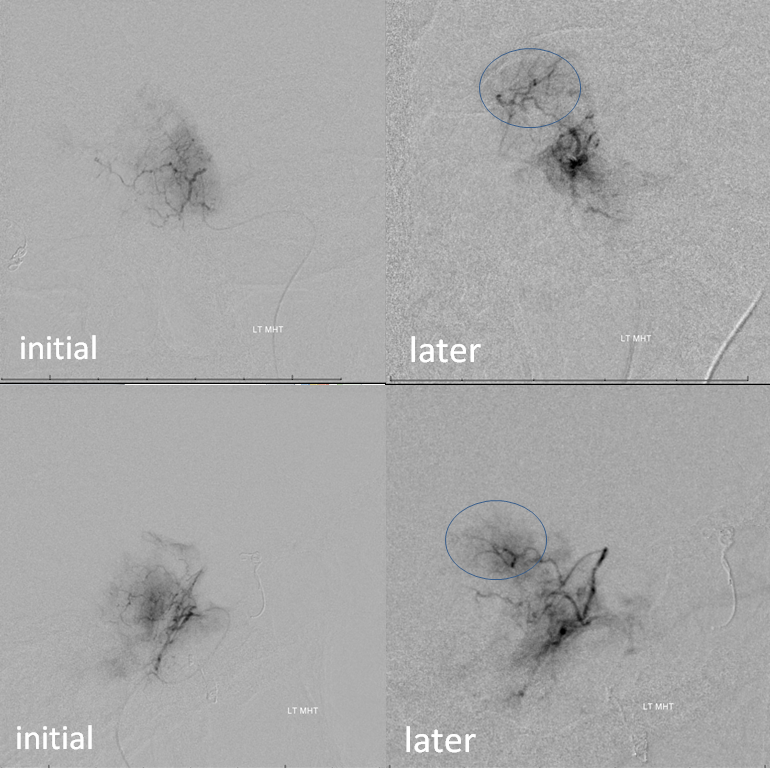
Progressive embolization opens up more posterior territory previously seen via the ascending pharyngeal route (blue oval, see also image 2 in the AP embolization sequence)
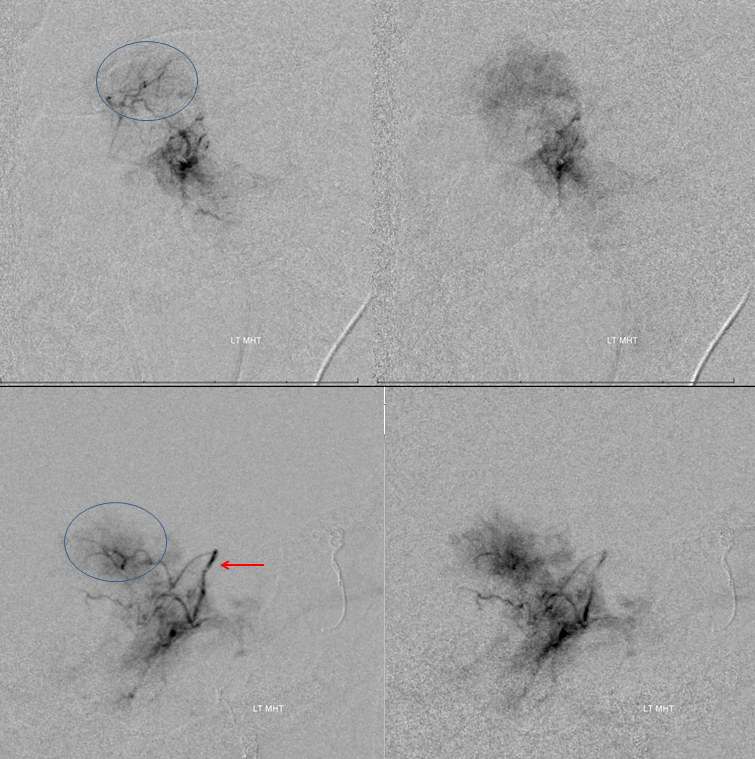
Another illustration of the same
Final post-embolization picture. The MHT was closed with a coil after particle embo to prevent near-term recanalization. Only frontal image is taken to minimize radiation exposure (more dose was accumulated in the lateral plane due to its preferential use during particle embolization)
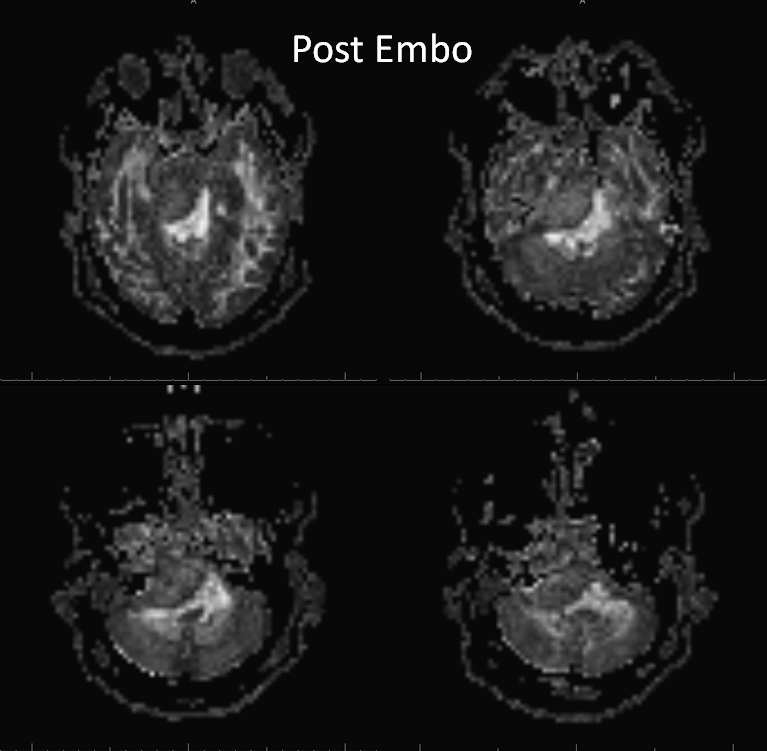
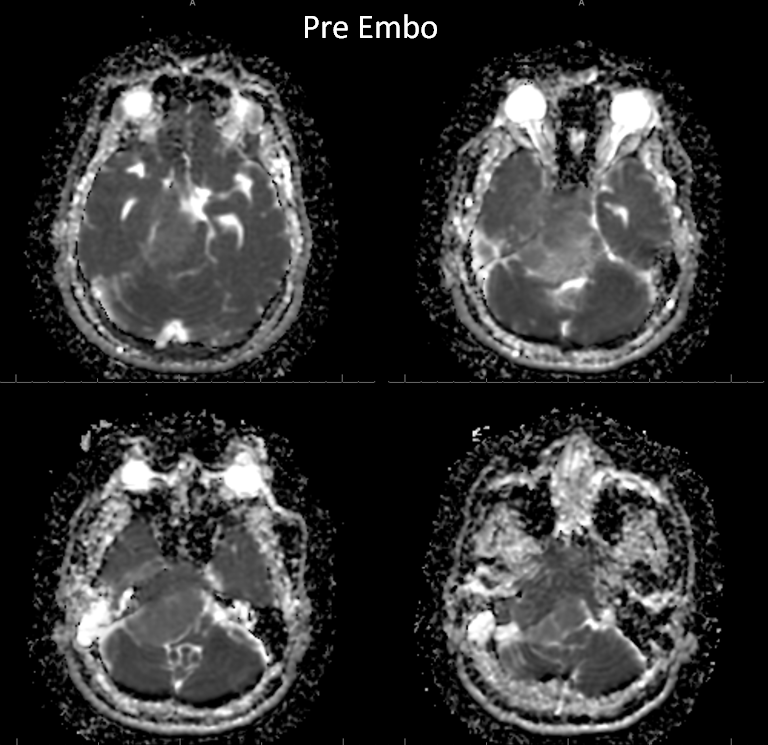
Post-embolization MRI can show both desirable and not so desirable embolization effects (brain emboli). Post-contrast sequence is good to show necrosis, and ADC maps will demonstrate more restricted diffusion in well-embolized areas
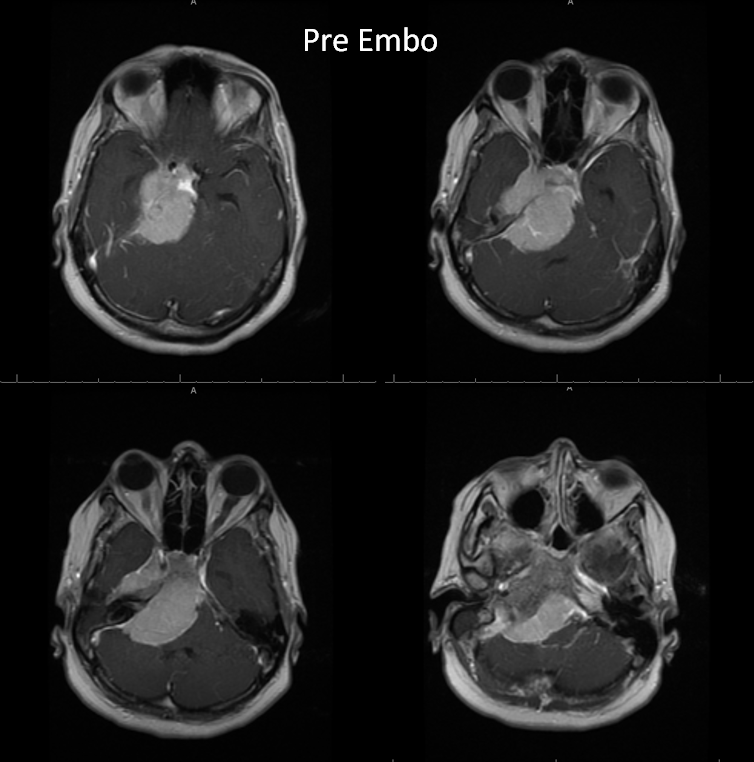
Here is post-embo T1, with overall decreased enhancement and areas of nonenhancement compared with the preoperative study (allowing for differences in MRI equipment and technique)
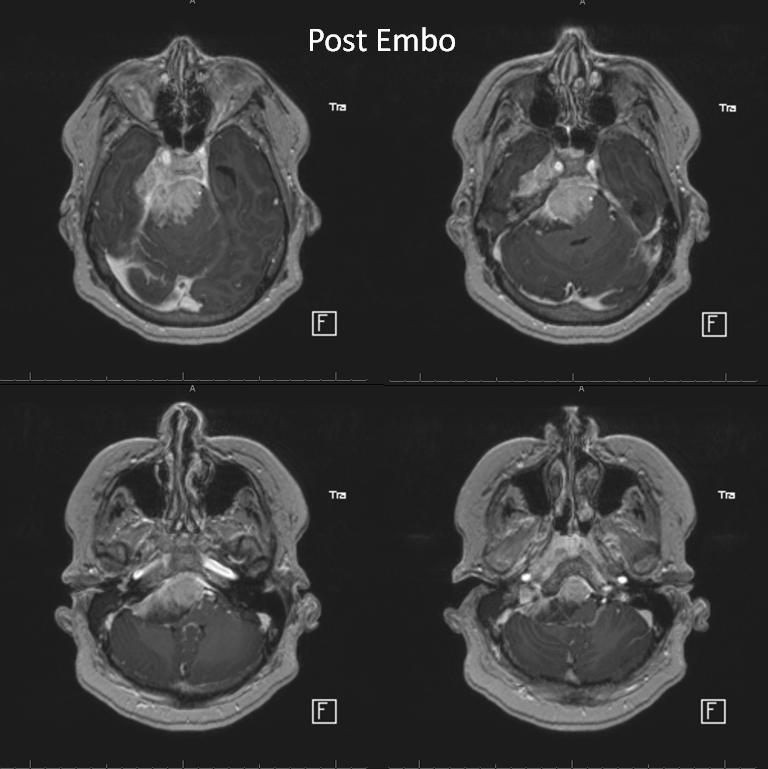
Pre-op study
Post-op ADC
Pre-embo below
Back to Techniques Preoperative Tumor Embolization Page
