Part of angiographic technique series
Intraprocedural complications are an inevitable reality. The goal is to minimize their incidence by best practices and to know how to address them when they take place.
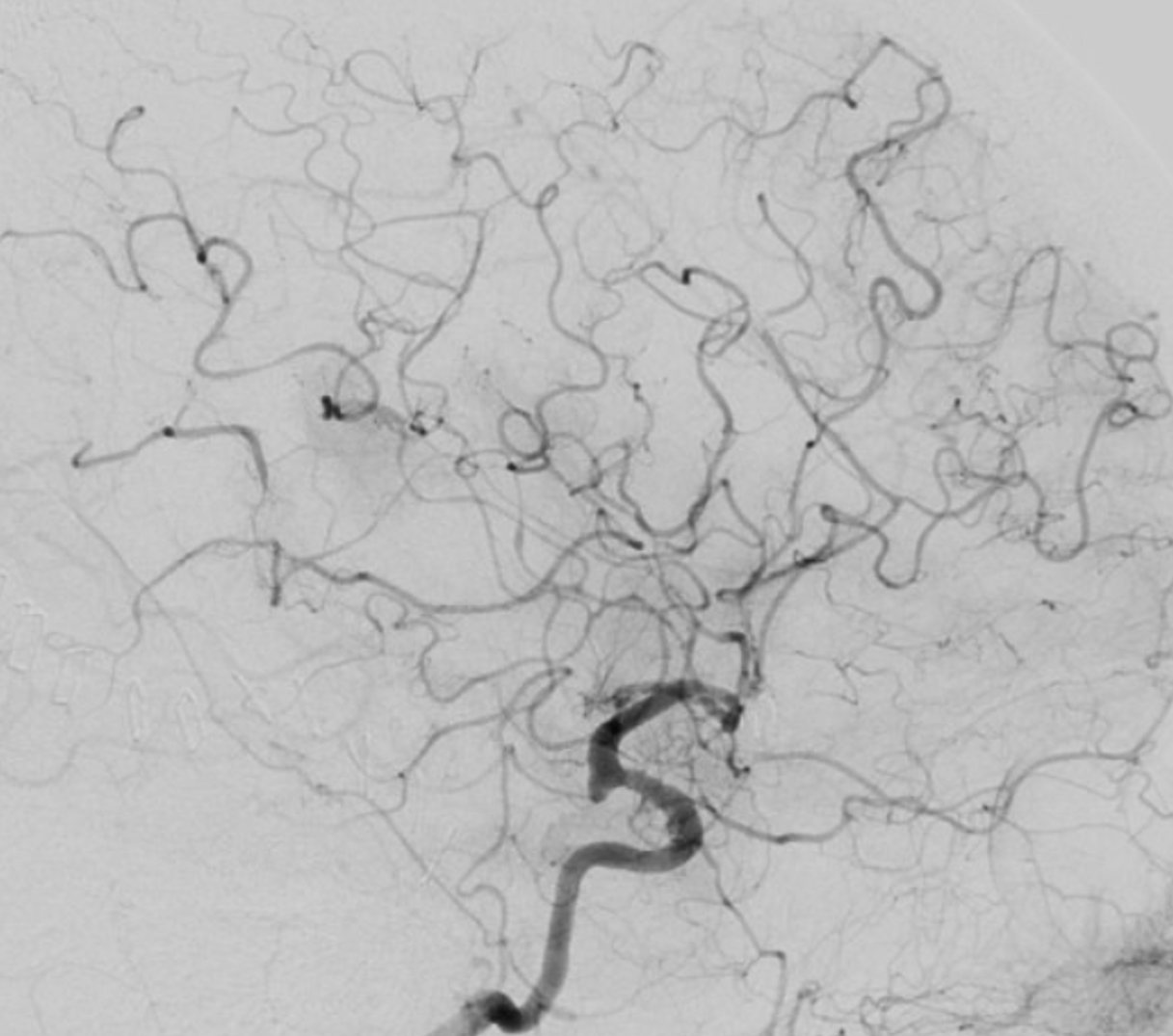
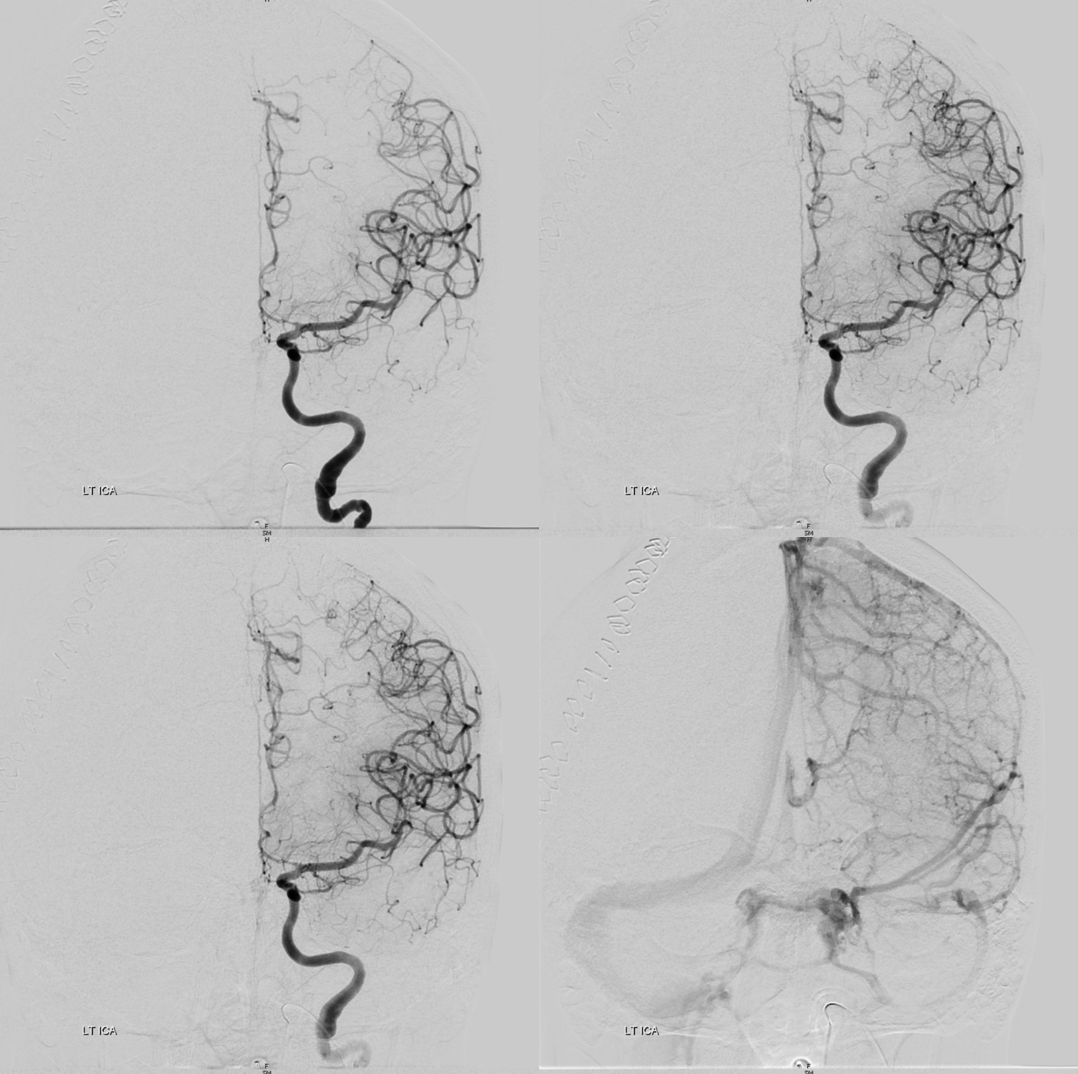
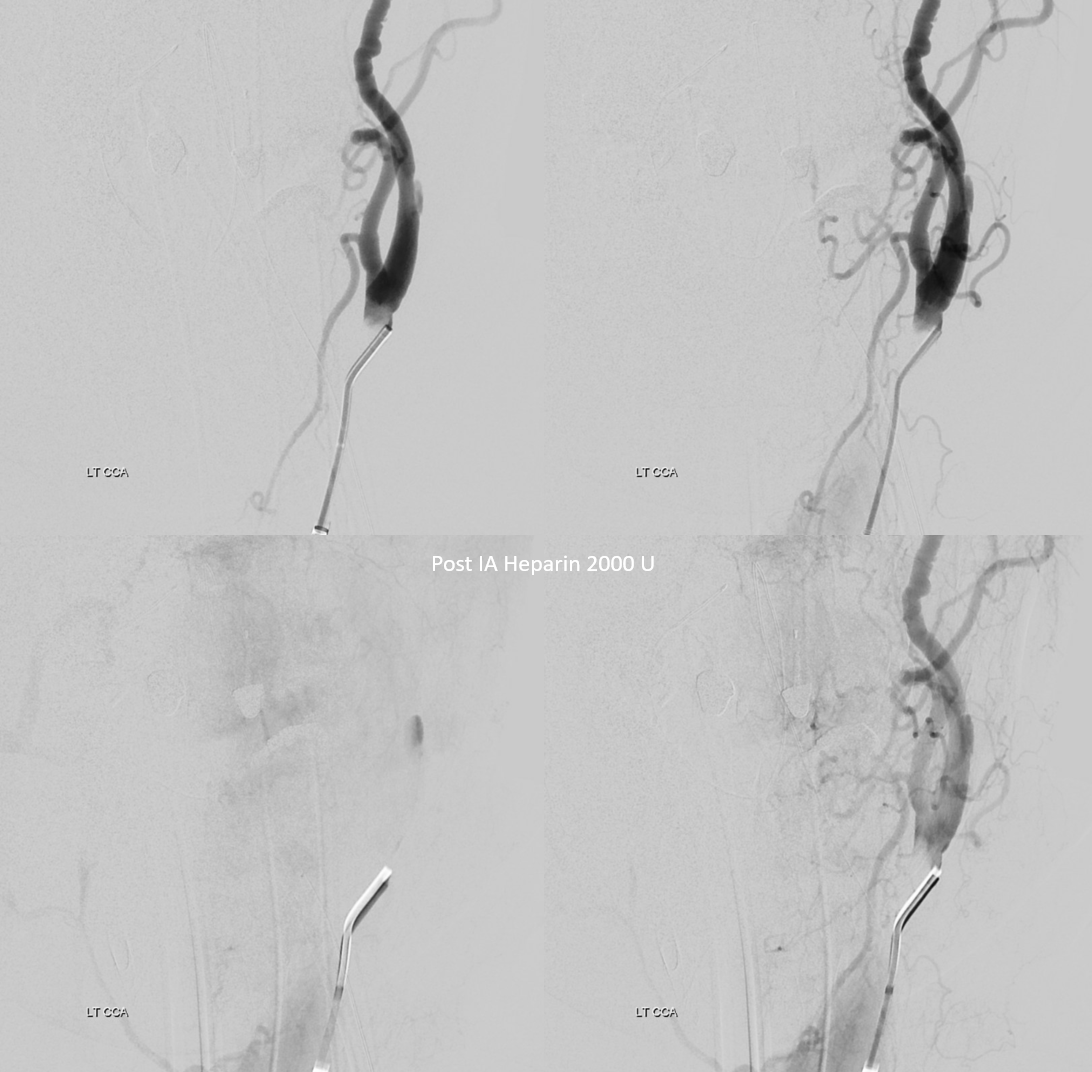
In this case, an intraprocedural embolus was a result of prolonged catheterization in difficult anatomy, in setting of recent subarachnoid hemorrhage — a known highly pro-coagulant state. Can you see the embolus?
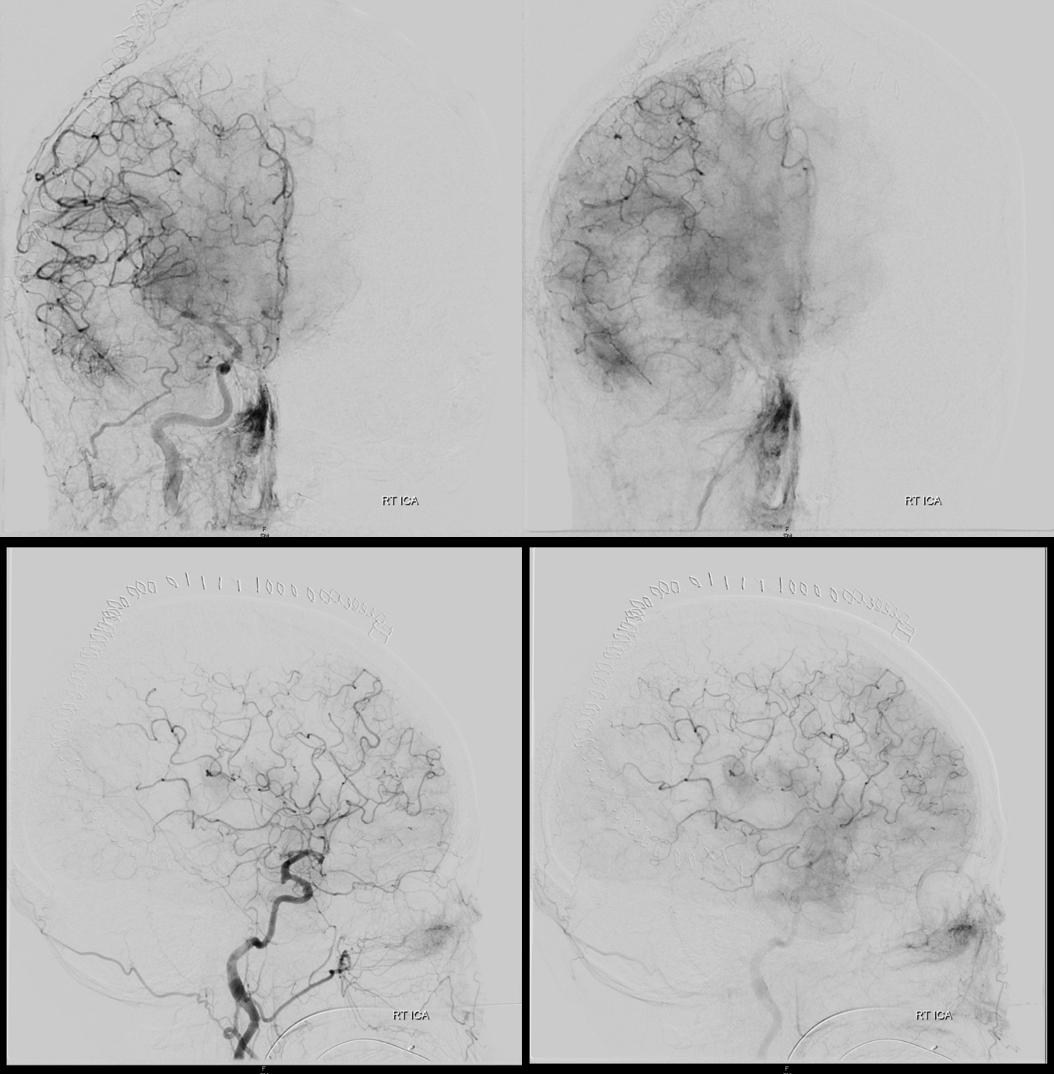
Close up view
A few minutes later
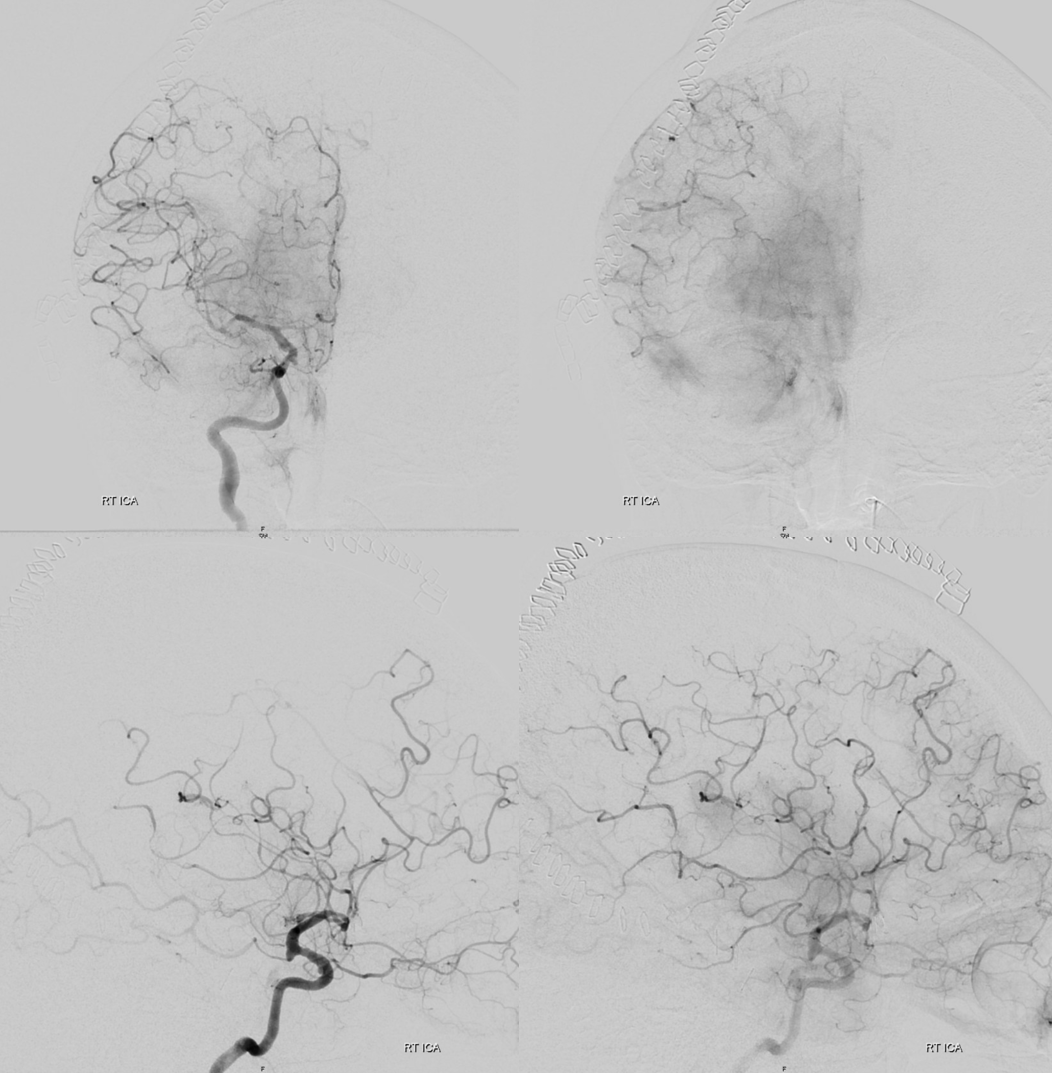
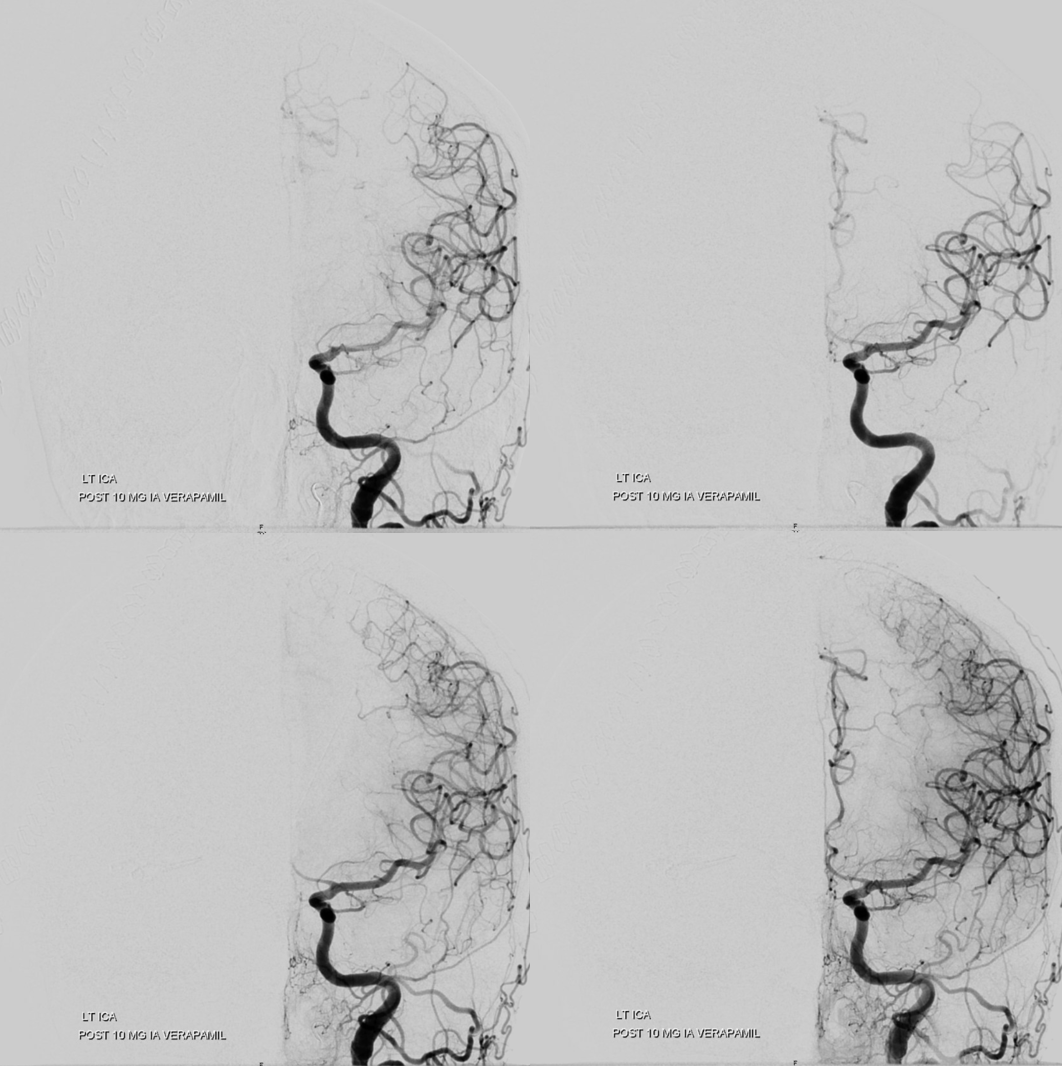
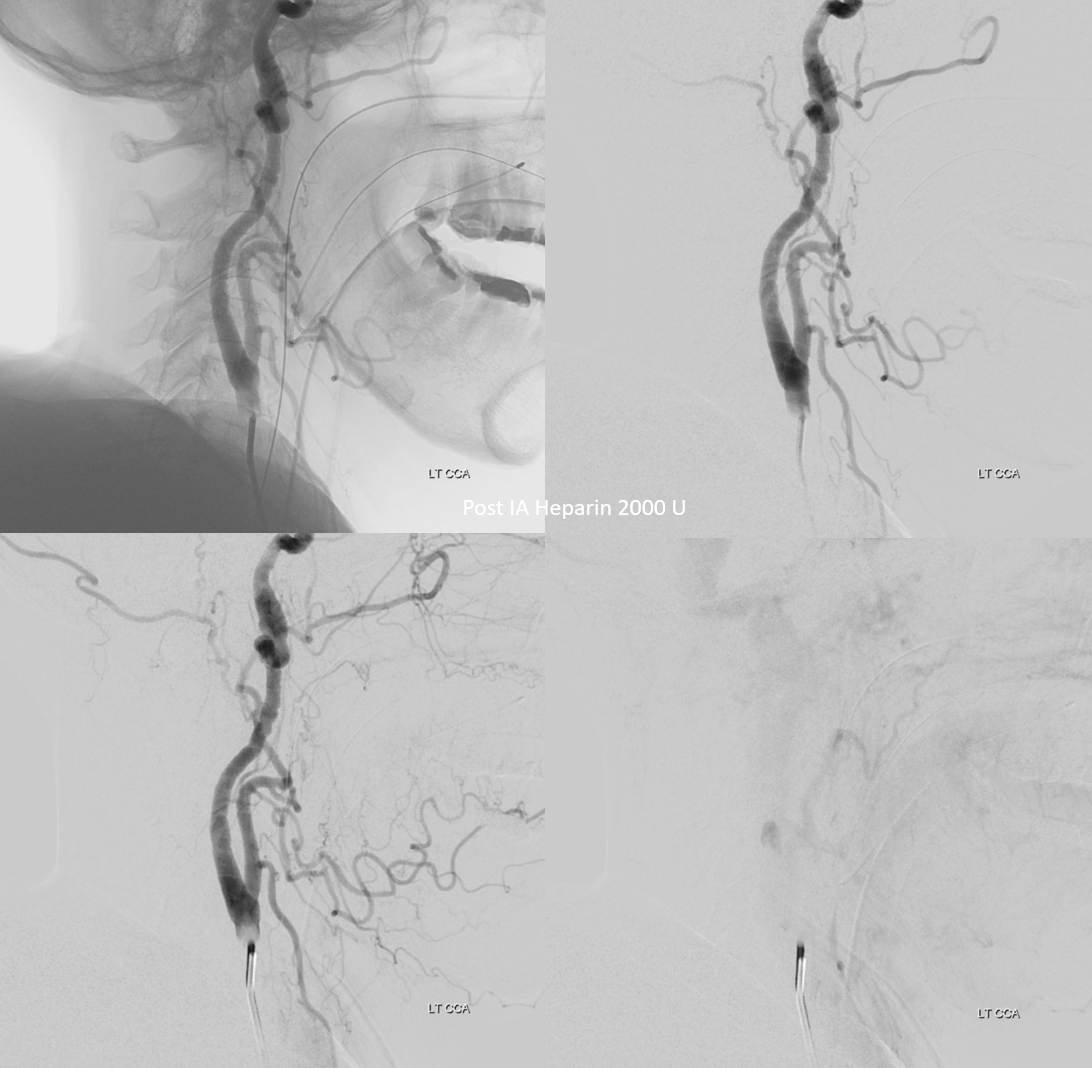
How to manage? In unruptured case, intra-arterial 2B3A inhibitors are highly effective. In this case, with a ventricular drain and hemicraniectomy, probably better to avoid it. There is also serious vasospasm present. We gave IA Verapamil and 1000 U IA heparin. After 10 min, the thrombus dissolved spontaneously. At least half the time, this is not enough and IA antiplatelets or thrombectomy are required. If this were necessary, superselective catheterization of the occluded branch to “lace” the clot with antiplatelets maximizes efficacy. In complete occlusion cases, there is no flow to take the drug to the clot. Its not magic — drug needs to contact clot for it to work.
Notice improvement on frontal images also
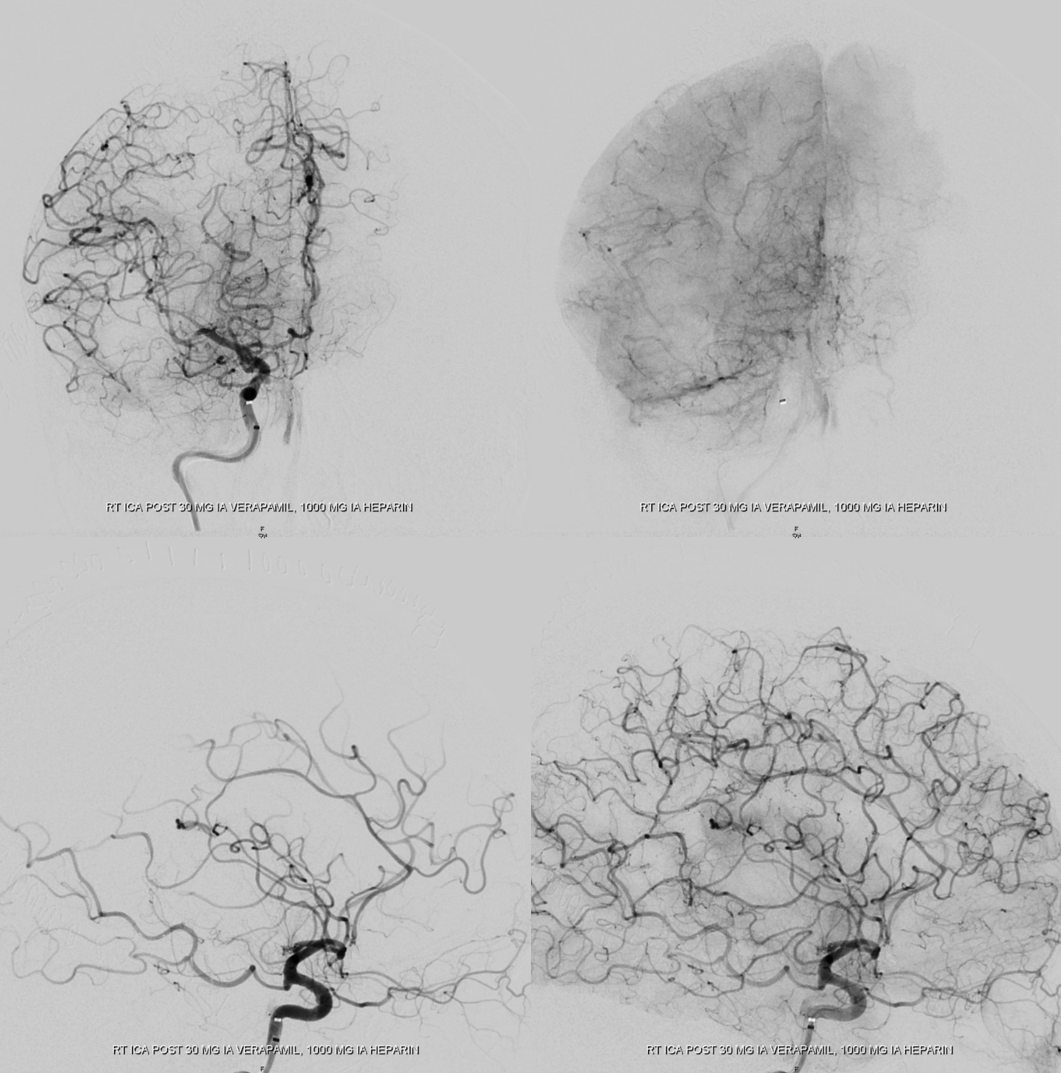
Now to the other side
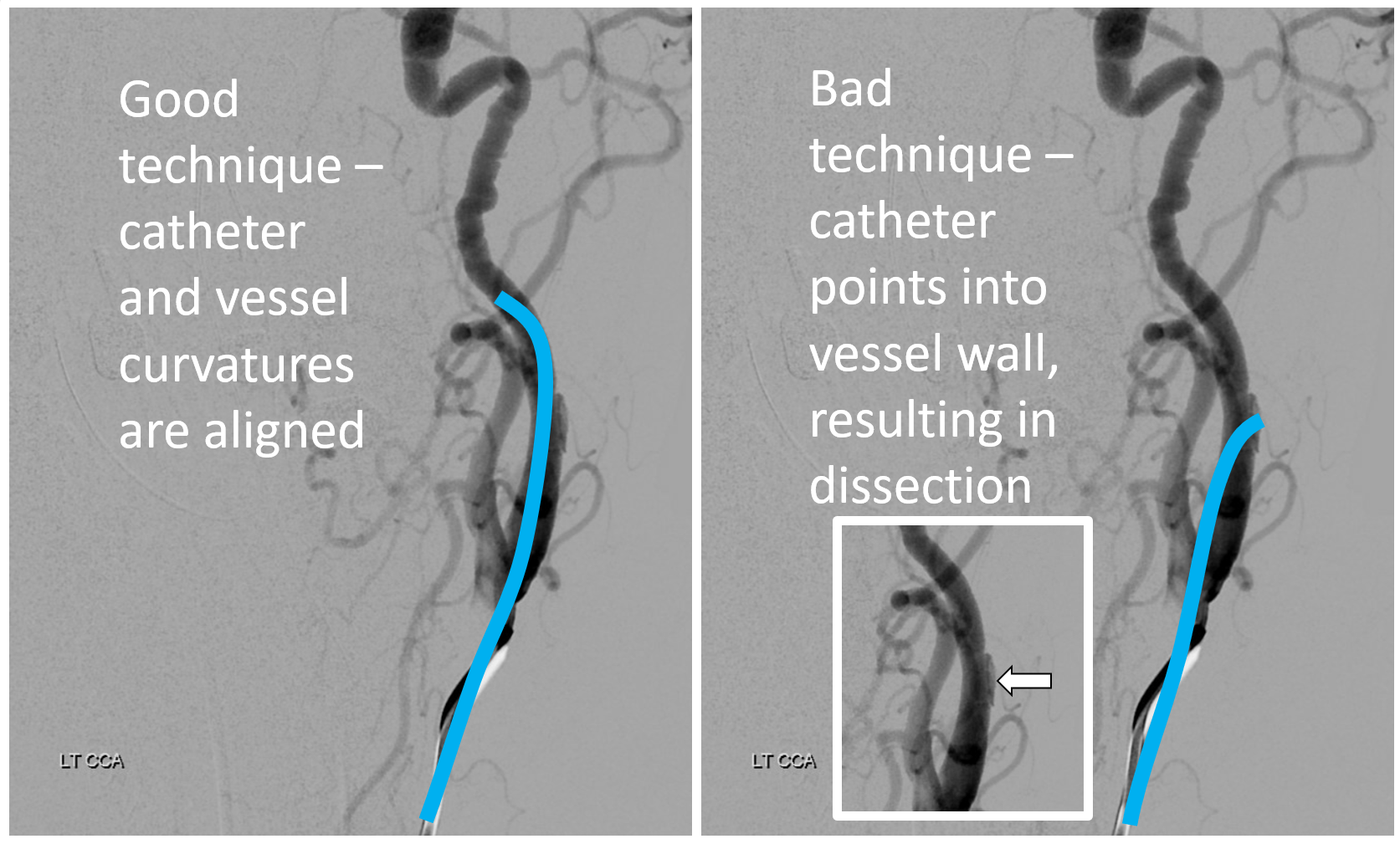
Another injection — notice the difference? IA verapamil was given in-between, but that is not the problem. If anything, the MCA looks better. What is the problem though?
Now you see?
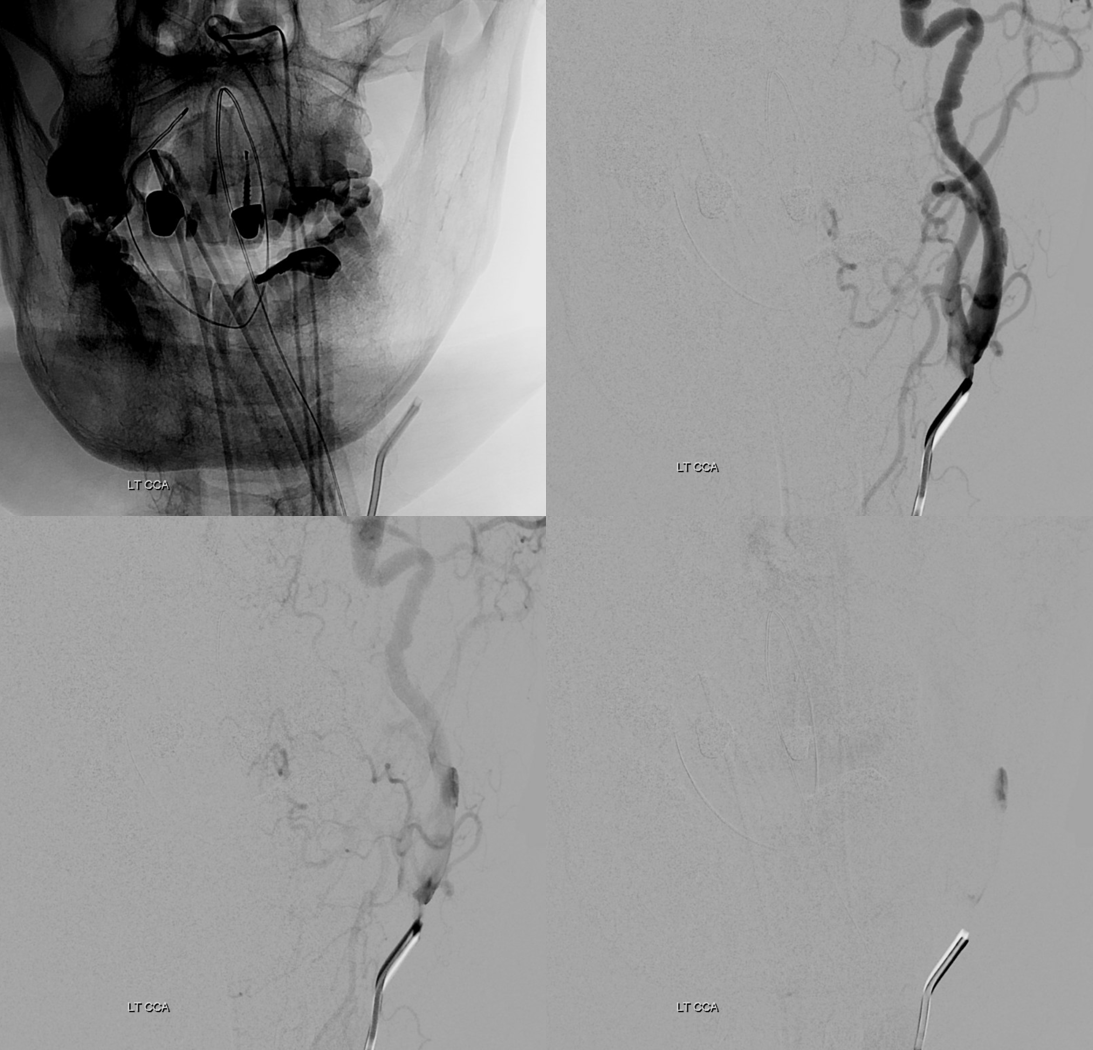
Mechanism is having catheter against the outer wall, not aligned with the vessel. Notice anything else in these images? Neither the catheter nor wire touched the upper cervical ICA — all of that is pre-existing
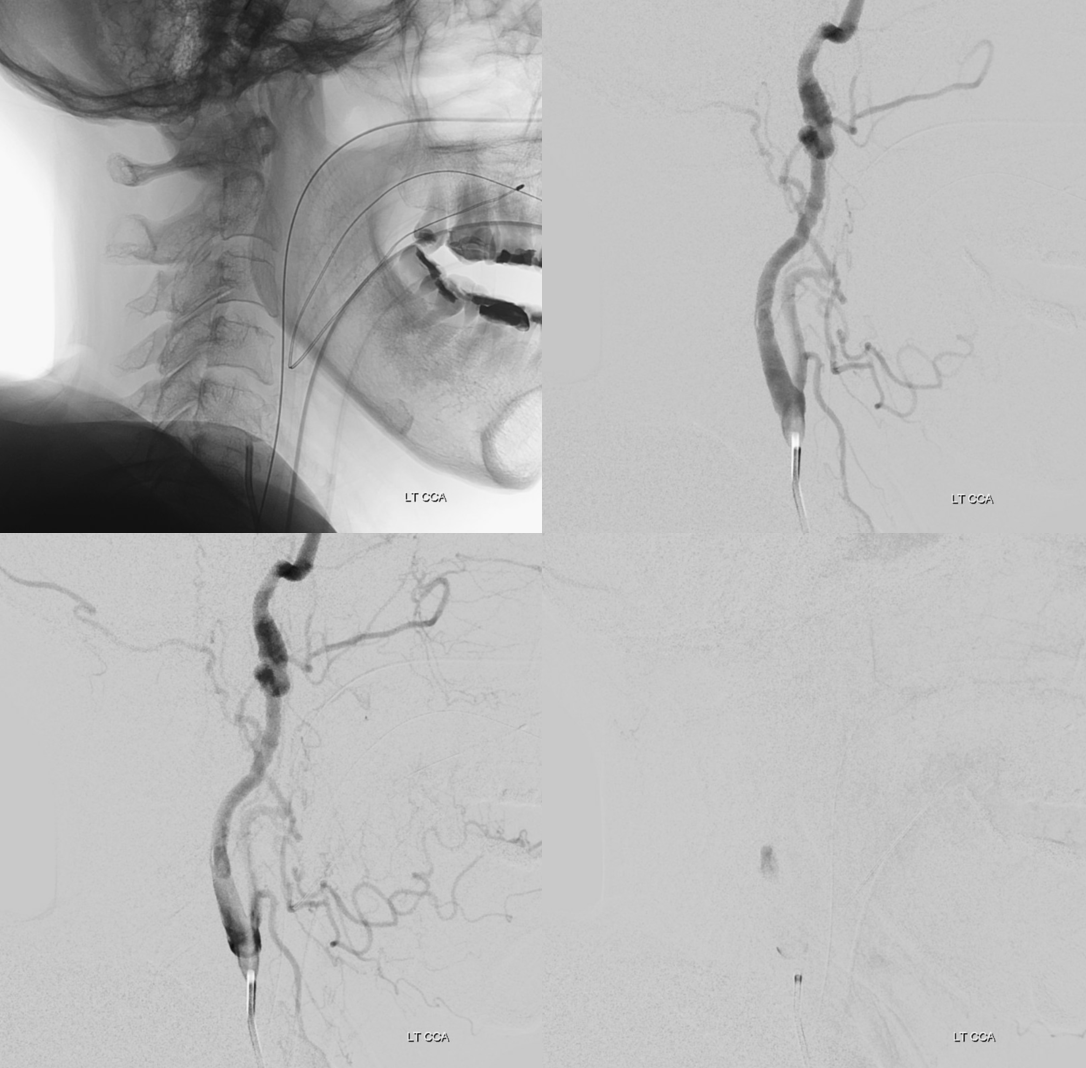
Now to deal with it? Staying calm. Giving some IA heparin, and aspirin (rectal) — looks stable below
Check the head — make sure there are no emboli
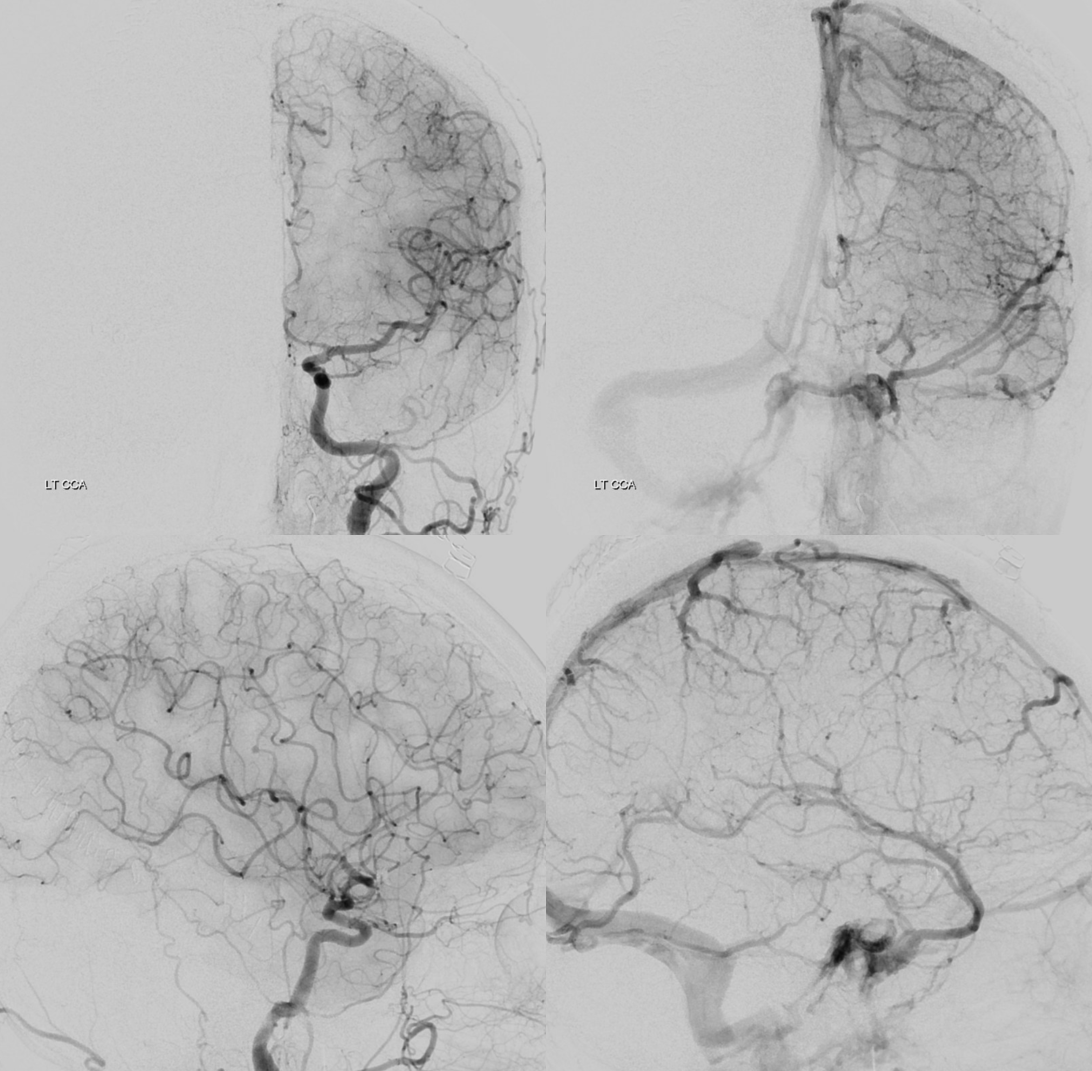
A week or two of aspirin is usually enough for small ones like this one
More complication management — see “Case Library“
