Almost always these have ophthalmic artery supply. For obvious reasons this is the least preferred route. Surgery has been the mainstay, but not anymore, at least not where we come from. There is usually an endovascular way — see transvenous route for example here. In this case, however, the patient has too many co-morbidities and coagulopathies for surgery, and ophthalmic is the only supply. So this is mostly a technical note on how to embolize thru the ophthalmic when u have to
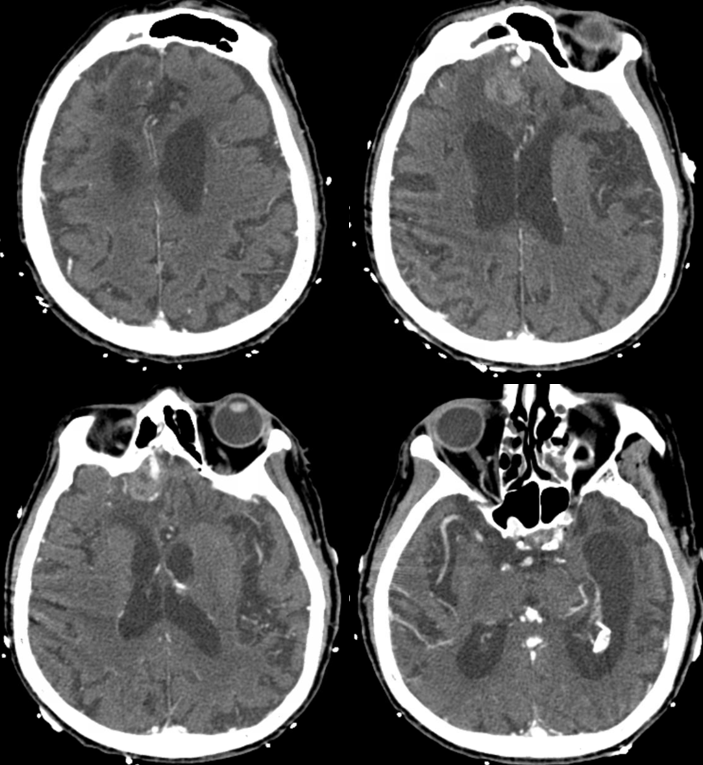
Presentation with hemorrhage

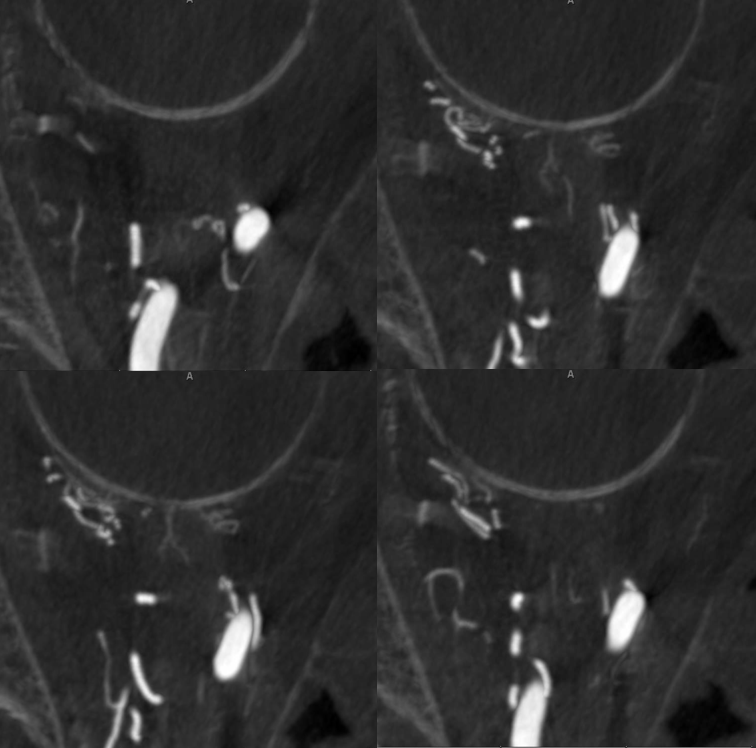
CTA — enlarged ophthalmic artery and ethmoidal-fistula looking frontal base veins
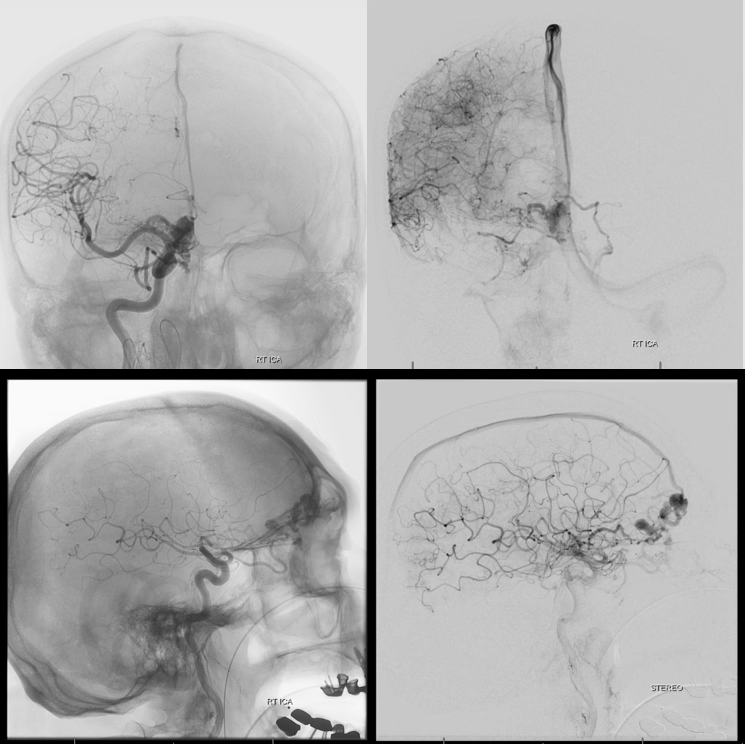
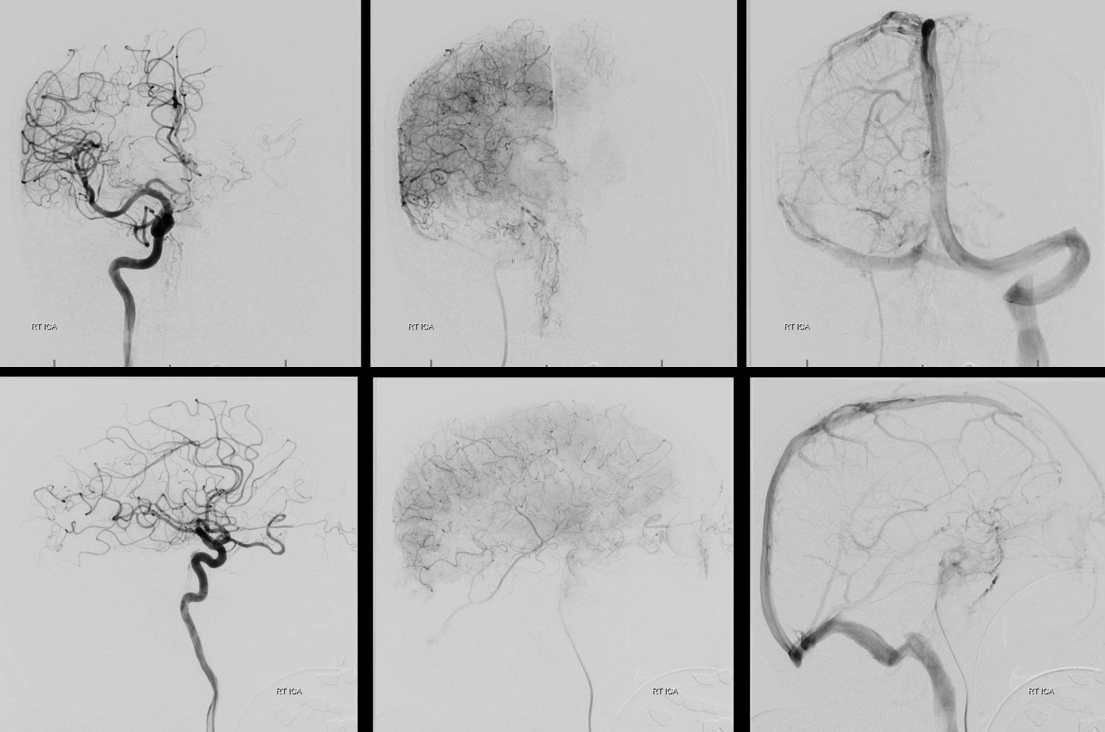
Rt CCA
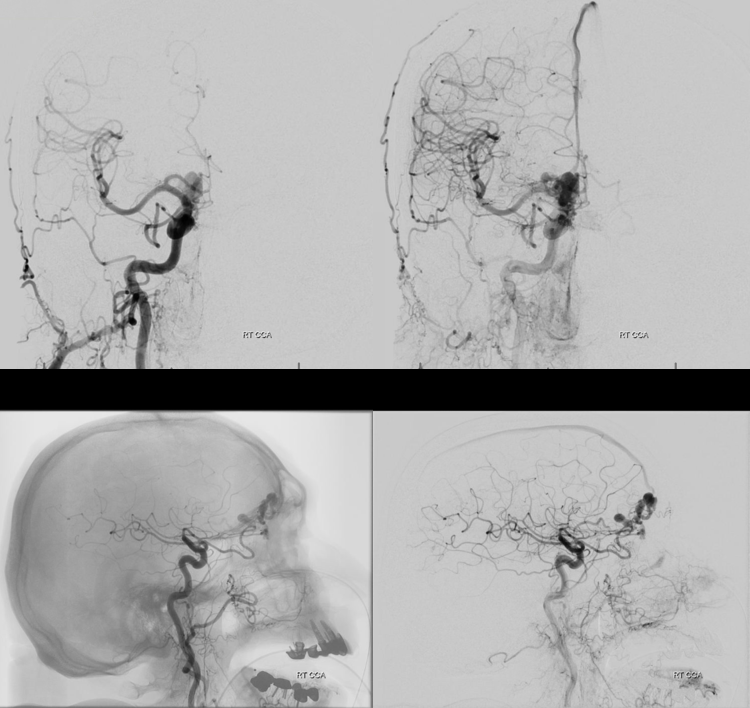
Virtually no external supply
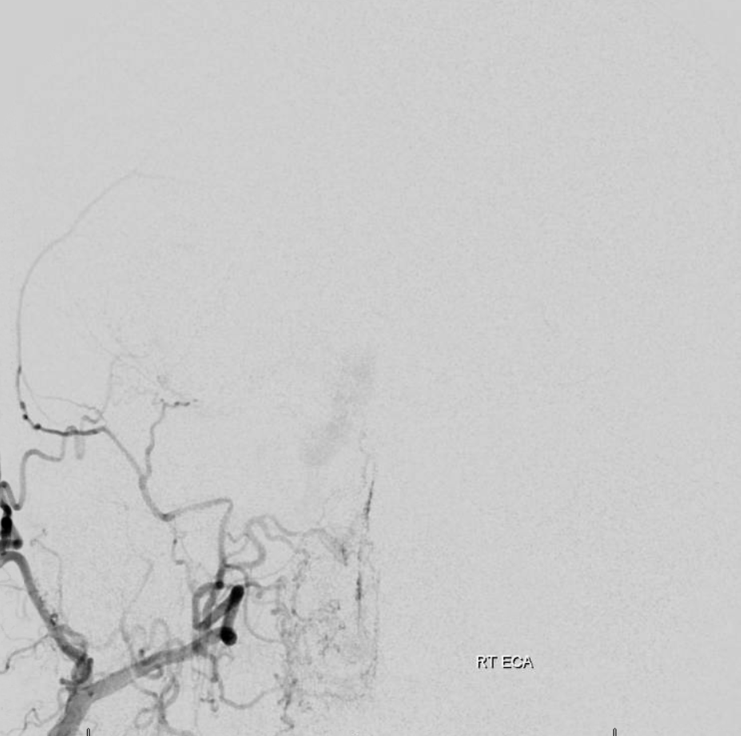
Nothing from left side either. Internal below. Notice bilateral congestion of frontal base veins
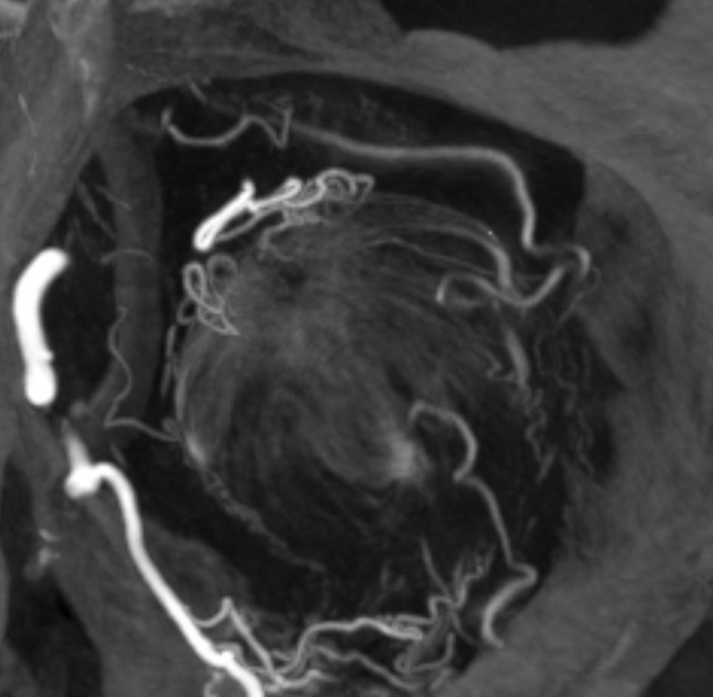
VR — notice stenosis at the level of cortical venous entry into SSS — arrow. Because of this stenosis, there is secondary congestion of frontal base veins (dashed arrows) as well as formation of venous aneurysm (open arrow) responsible for rupture. The smaller subfrontal vein is unlabeled
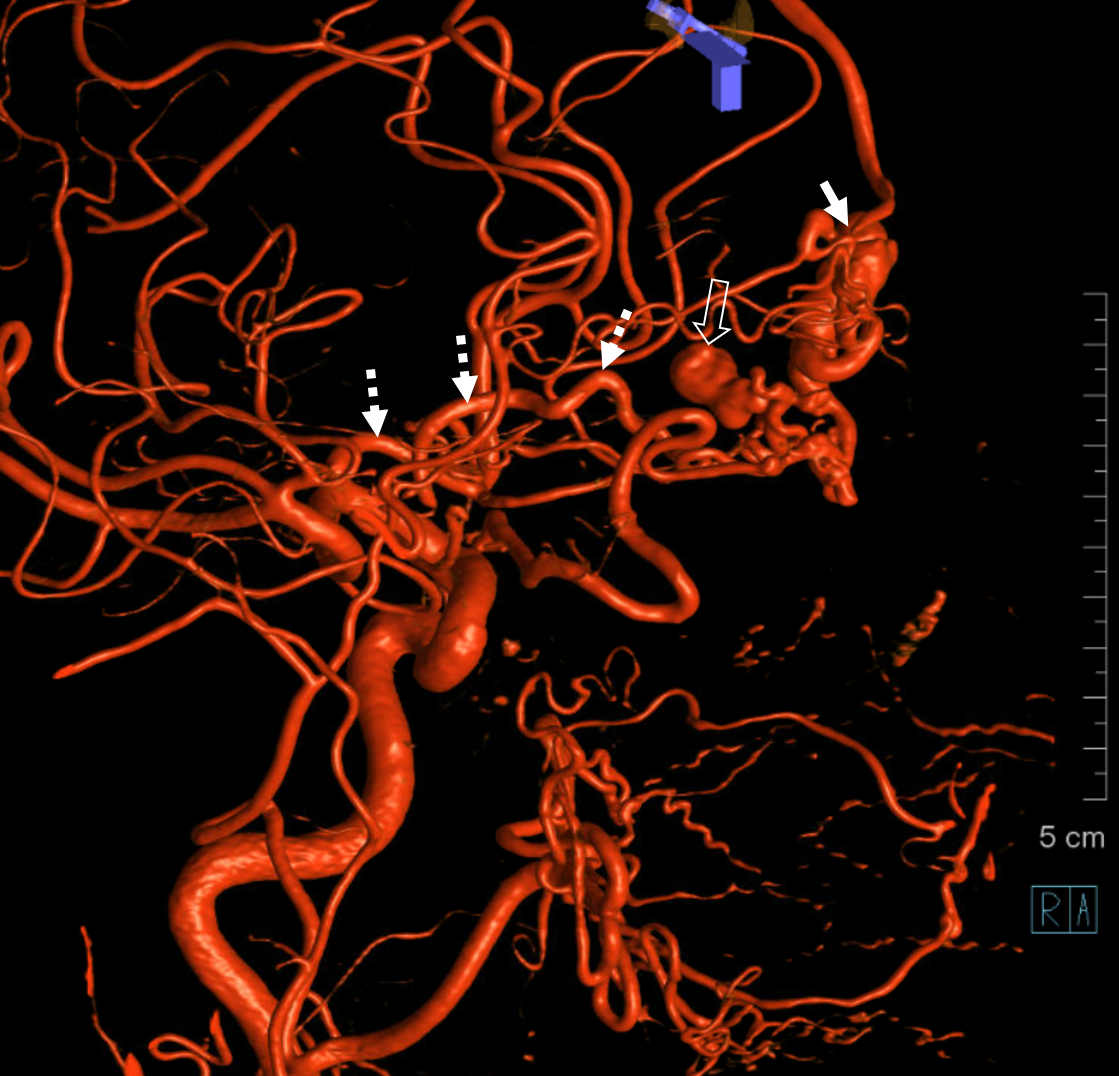
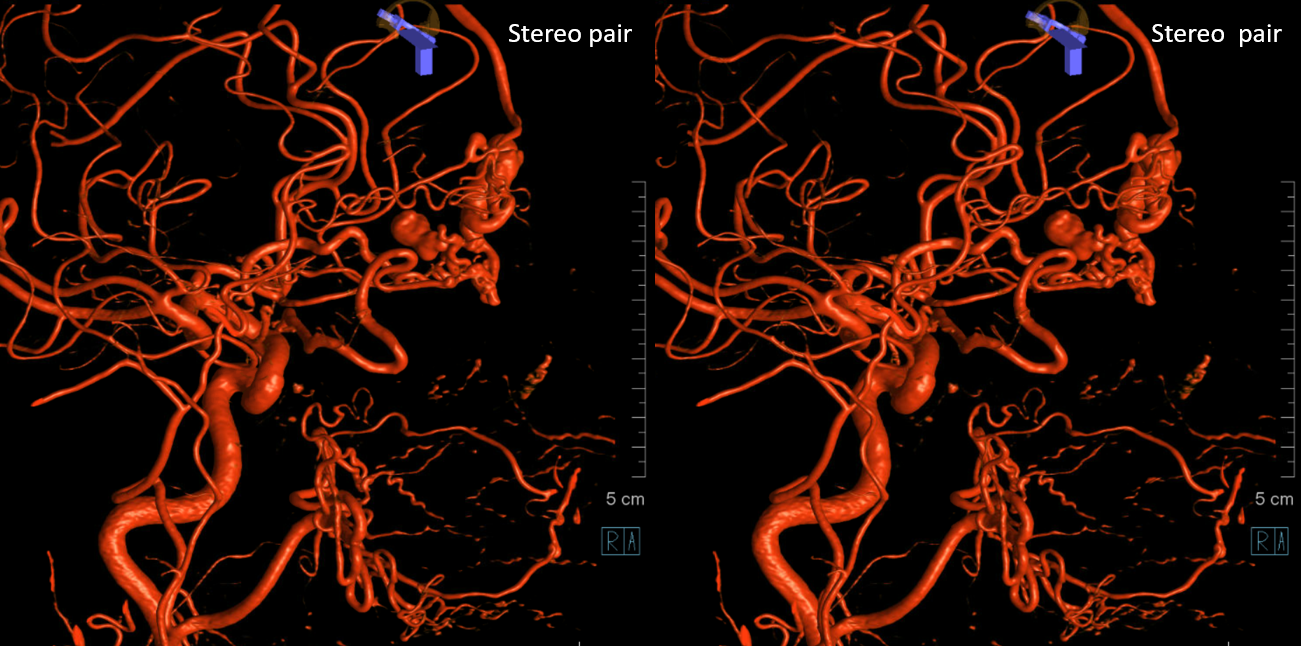
Cross-eye stereos
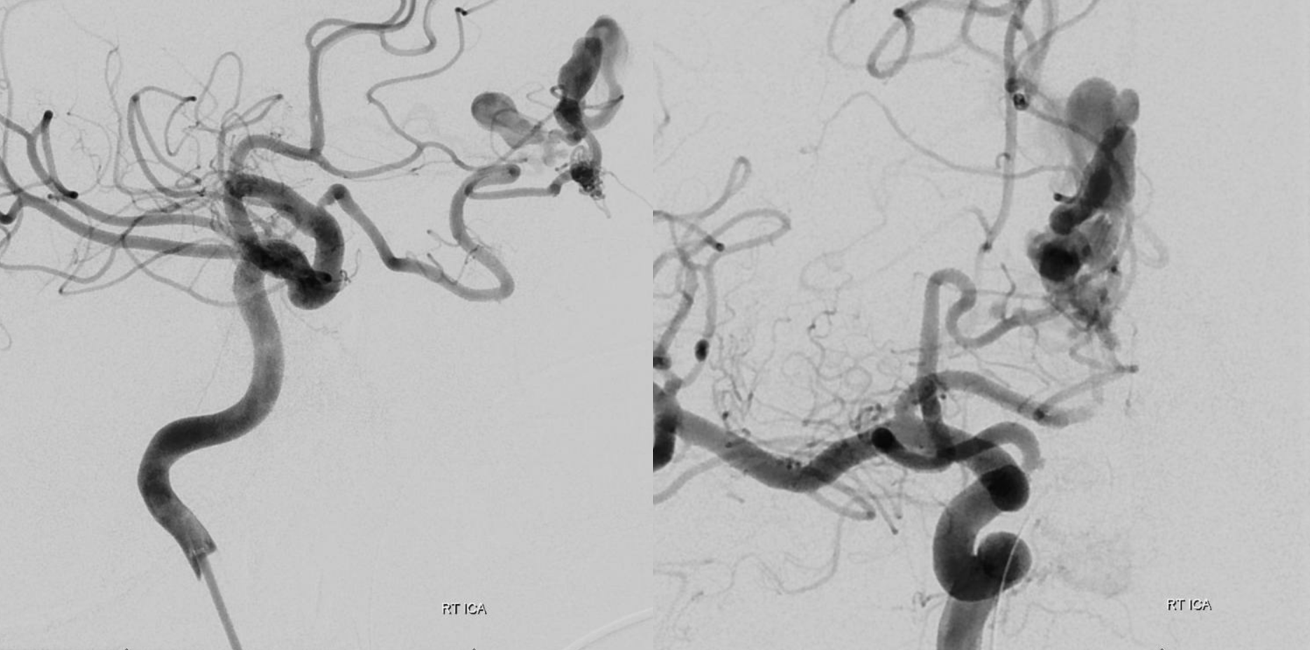
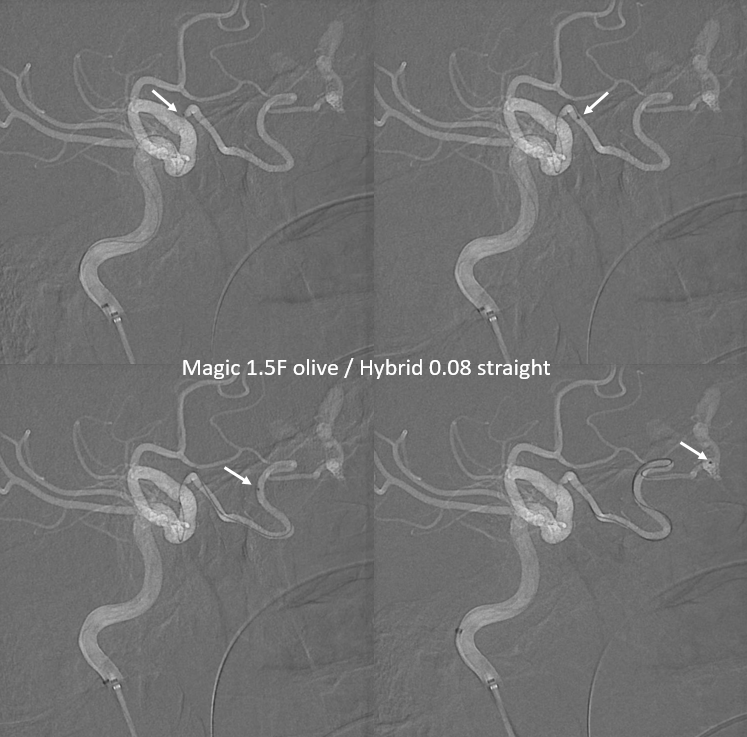
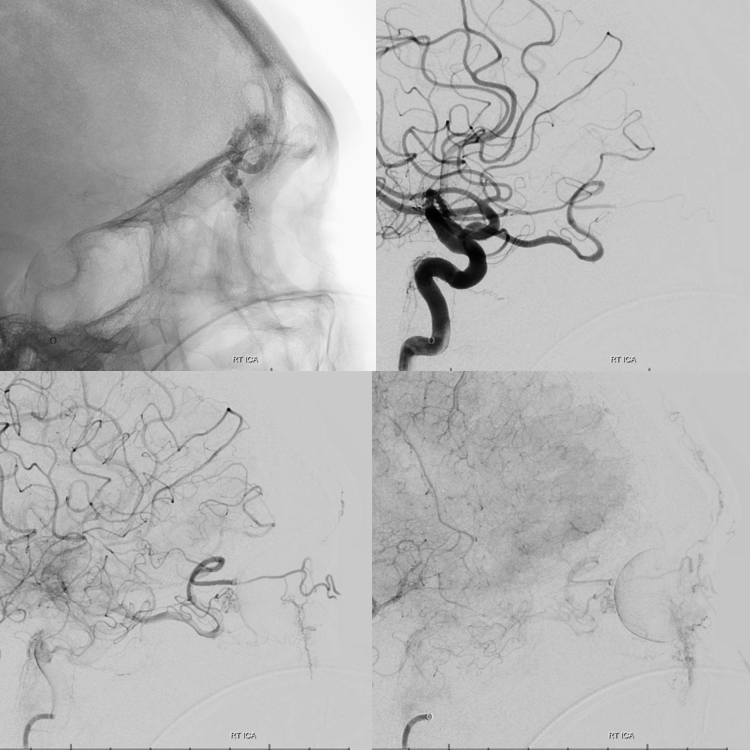
Working projection views. There is a stenosis at the ostium of the ophthalmic
Navigation with Magic 1.5F olive and Hybrid .08 straight wire. The Magic is ideal here, as it allows for minimum manipulation of the ophthalmic artery with wires, etc. — as long as the Magic is thru the ostium chances are it will do its magic and follow — as it does below. The Hybrid wire family is by far the best choice with the Magics, in our experience. The central retinal artery is expected to arise at the point where the ophthalmic takes a cranial turn — not labeled — see ophthalmic artery page for info
Magic micro injection
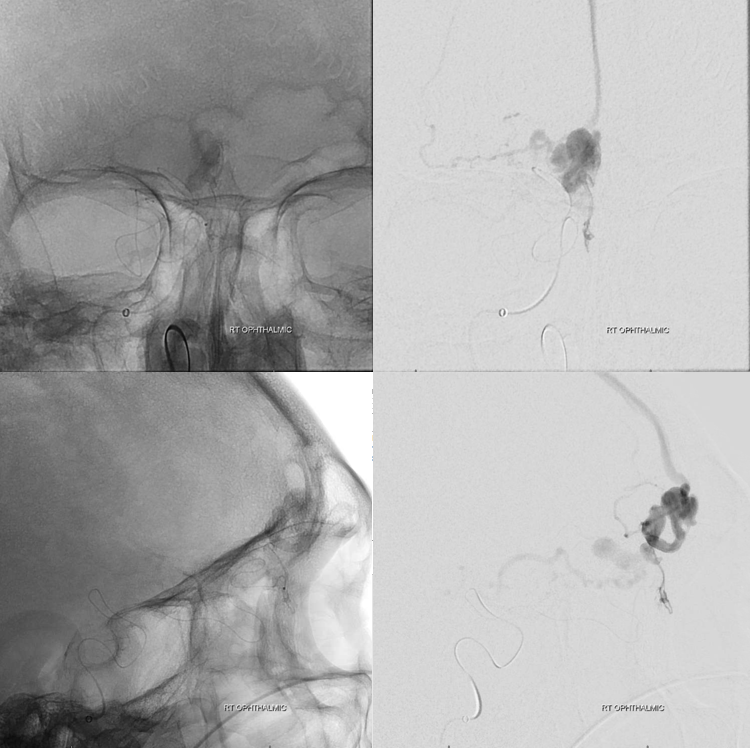
nBCA is the optimal choice here, not because we have a Magic. First, this is the only principal feeder, so we are not likely to have competing inflow prematurely polymerising the glue. Second, we do not want to create any plugs that would require us to do the type of Onyx “pull” in the ophthalmic. The idea is to use dilute glue to close the proximal vein without much reflux — not because reflux is bad per se — we have tons of “safety” here in the distal ethmoidal artery — but because reflux might make the pull more traumatic. Diluting glue also makes for an easier pull — less glue to hold the Magic
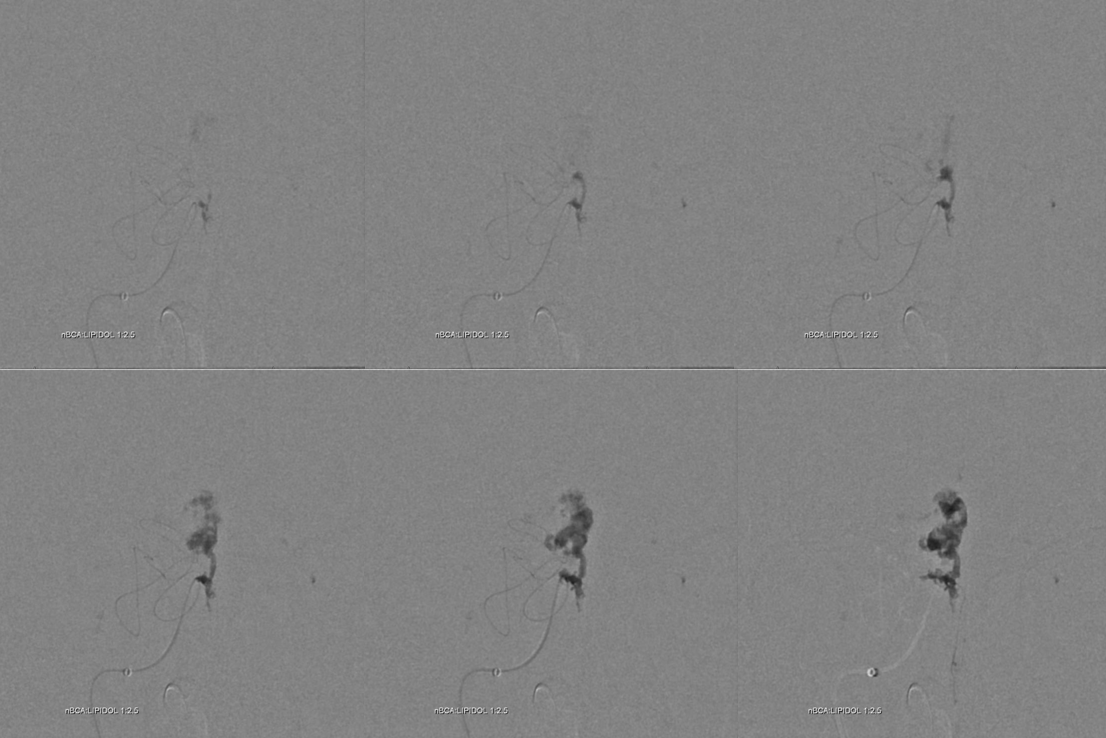
Below are frontal sequential images of glue injection, with an nBCA:Lipidol 1:2.5 dilution
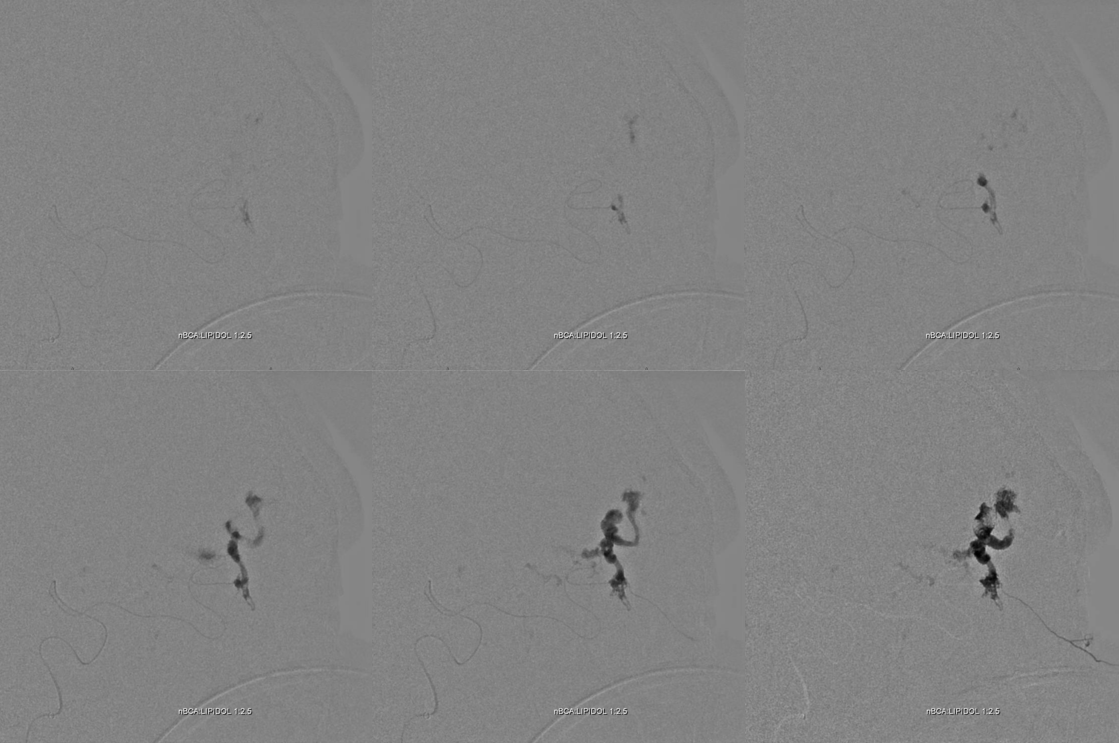
Lateral
Post
Post working projections — look at the beautiful visualization of the globe — the ophthalmic artery is enlarged, and now with no fistula outflow provides an excellent view of the orbital contents
Dyna CT thick MIP views of the globe — beautiful. Courtesy Dr. Eytan Raz. Look at those awesome vessels converging on the optic disk. Most are likely veins.
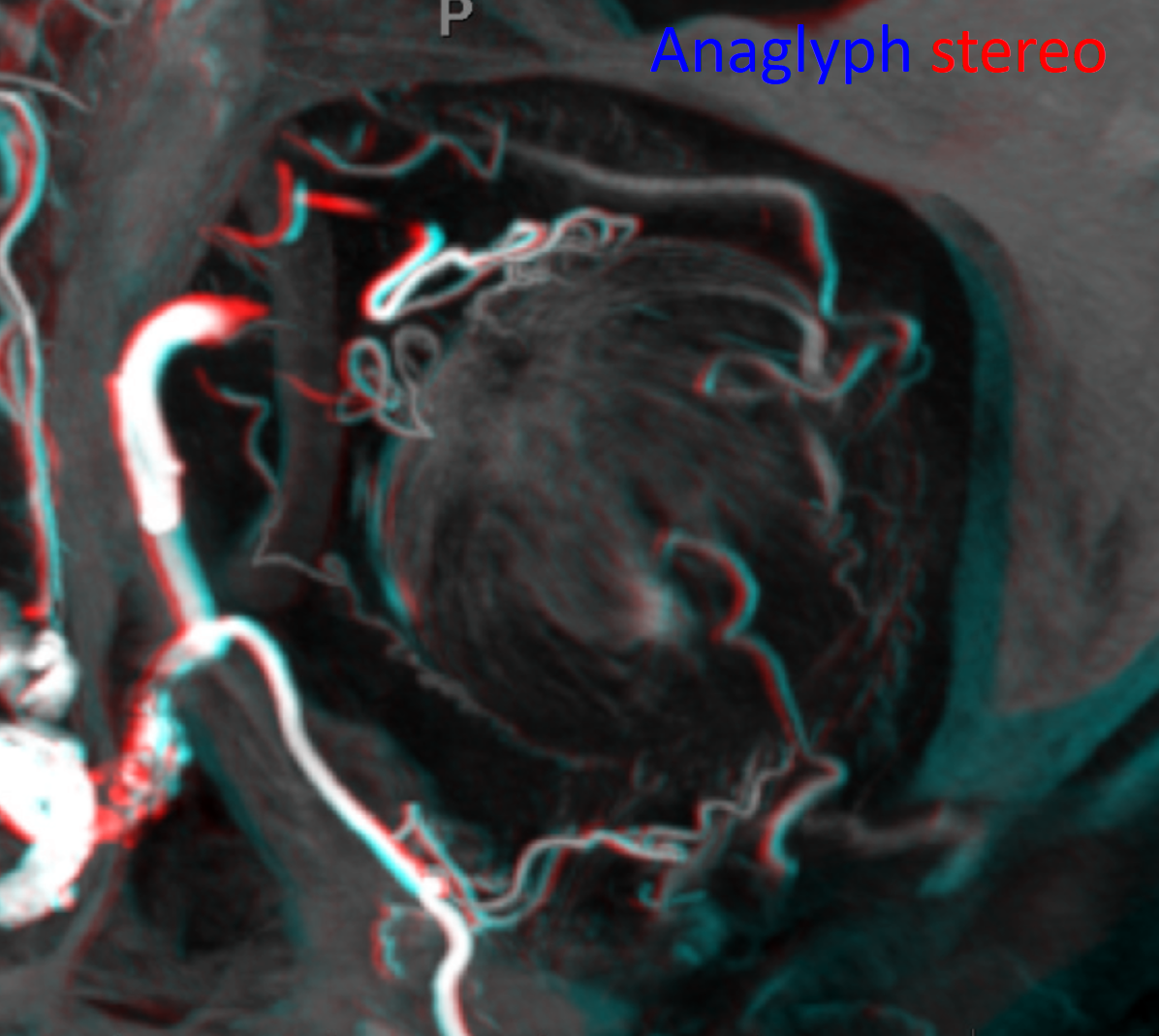
Cross-eye stereos
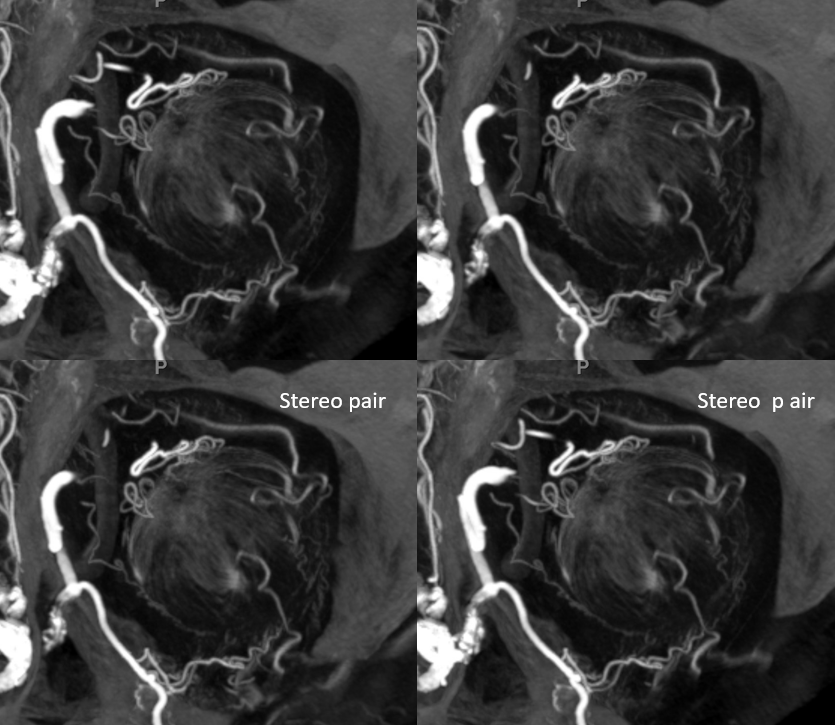
Anaglyph stereo view
A sagittal oblique view along the optic nerve axis beautifully shows a vessel inside the optic nerve at the level of optic disk
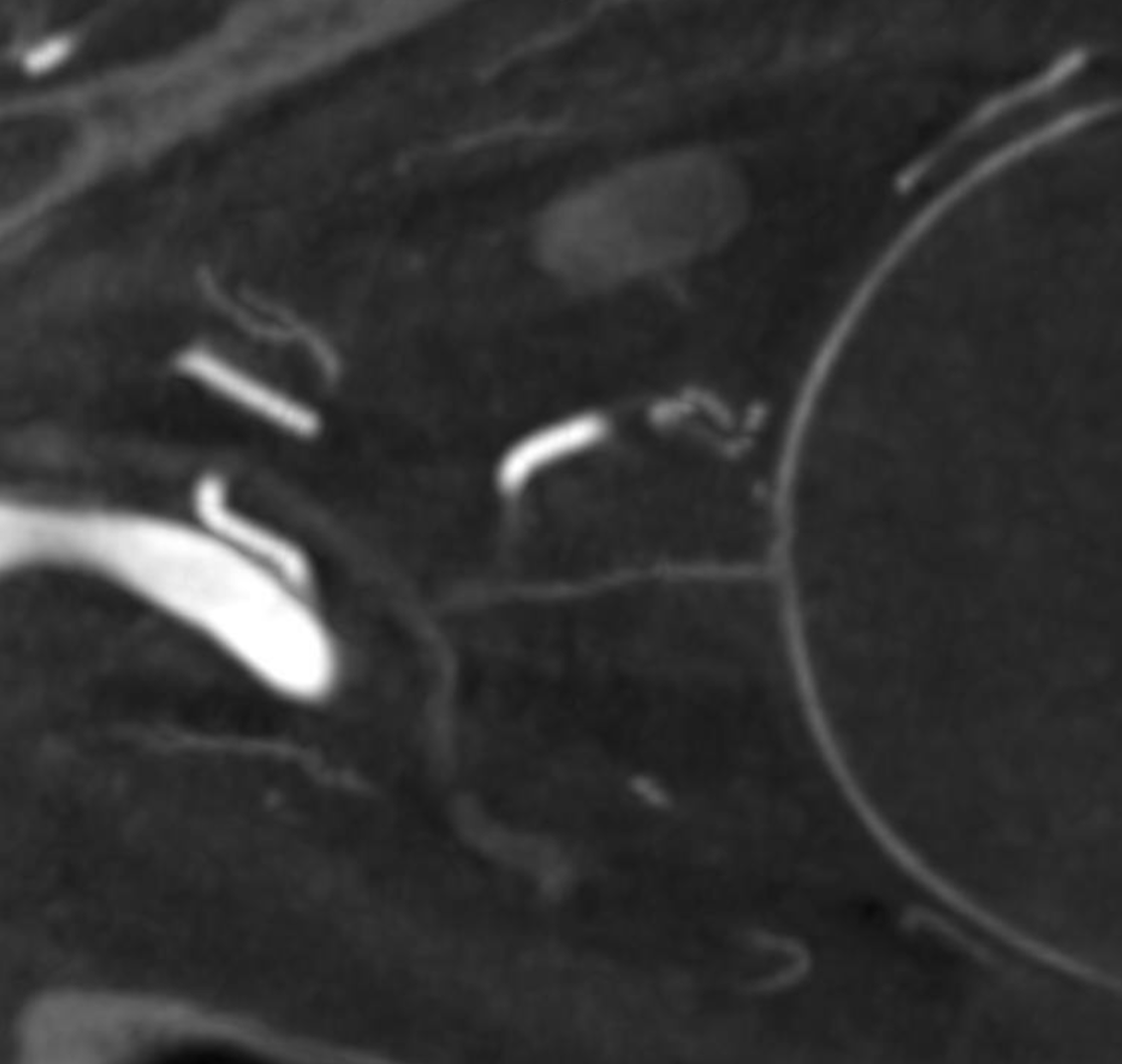
The axial views are a bit more complicated. The vessel seen above is probably a superimposition of central retinal artery (red arrows) and central retinal vein (blue arrows). The superimposed vessel is marked in purple. The optic disk is marked by white arrow
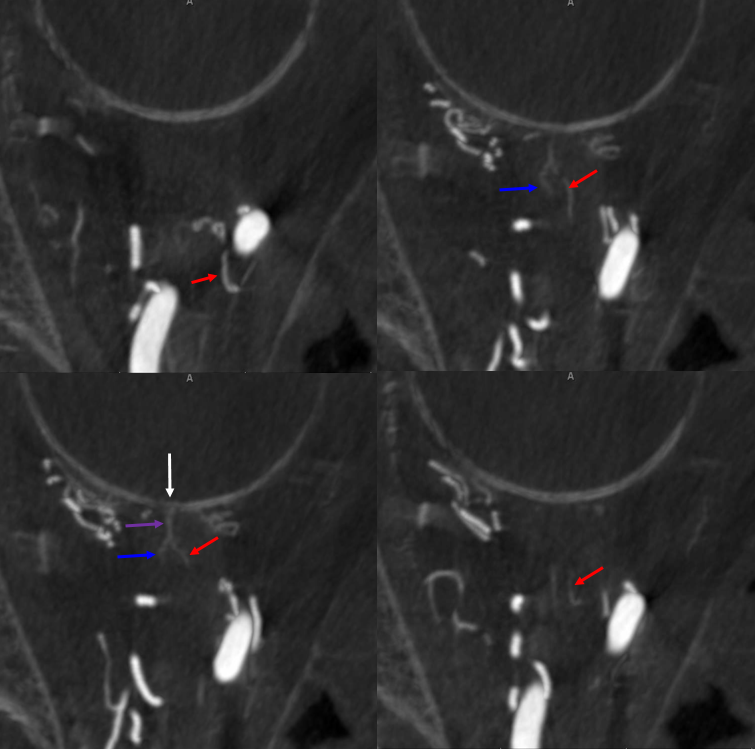
Same with no labels