Case of Dr. Eytan Raz
To understand intracranial dissection is no easy task. While oftentime the diagnosis becomes more certain with time, prospective identification, especially during acute stroke code, is often difficult. However, this is of vital importance, since any manipulation risks extending the dissection, this making things worse, not better.
Below is an in-depth study of a single case, which encapsulates many findings and clues about dissection. True to neuroangio.org approach to anatomy, detailed study of one case is often better than lumping together a bunch with a cursory review of each, thus making the whole worth much less than sum of the parts.
Presentation is left MCA syndrome, with no underlying stroke risk factors. This, of course, is often unknown during acute stroke codes. In this case, history was available. So, that’s already reason to be on guard to suspect an unusual cause

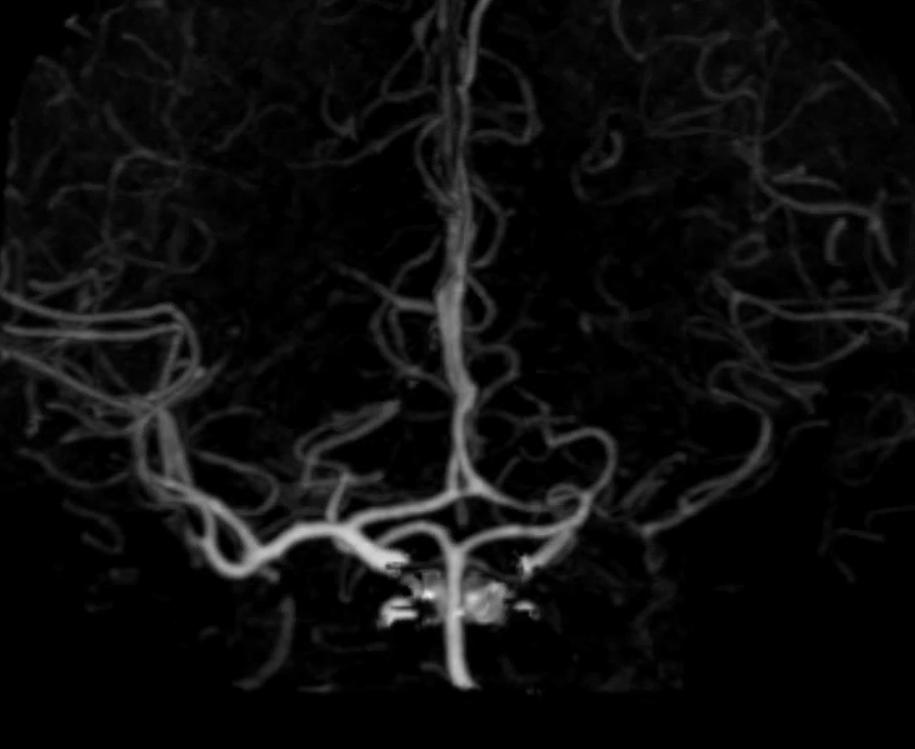
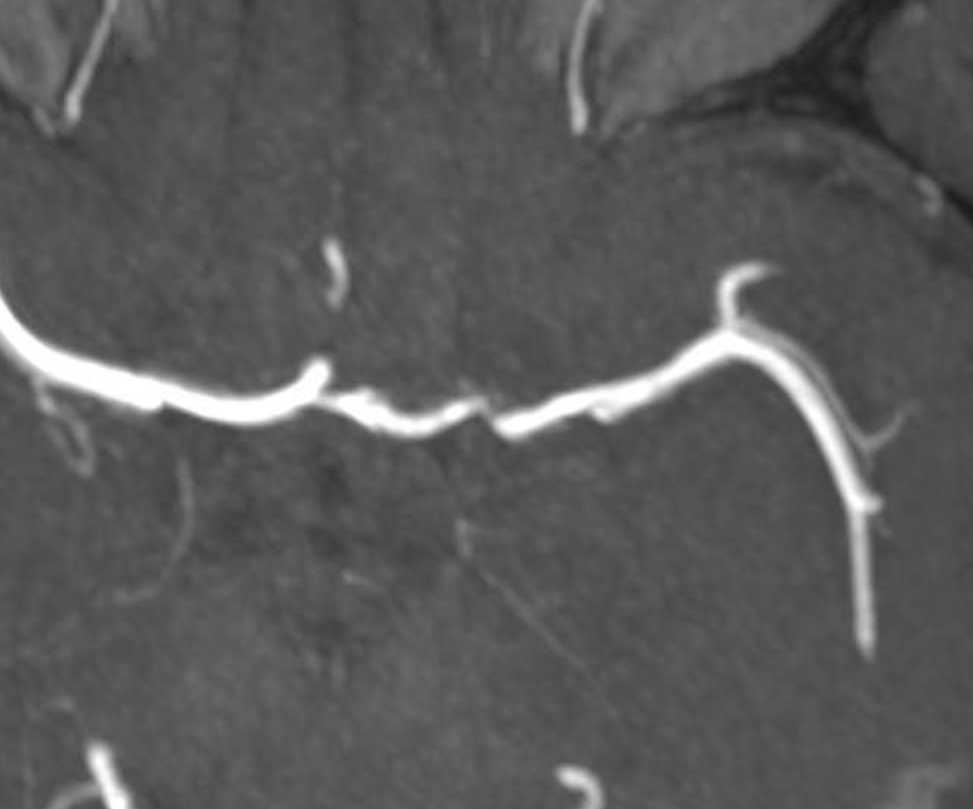
CTA shows no obvious cutoff — this is atypical (though certainly not unheard of) for an embolus
Perfusion is not helpful in diagnosis of cause here, and certainly correlates well with clinical status and CT / CTA
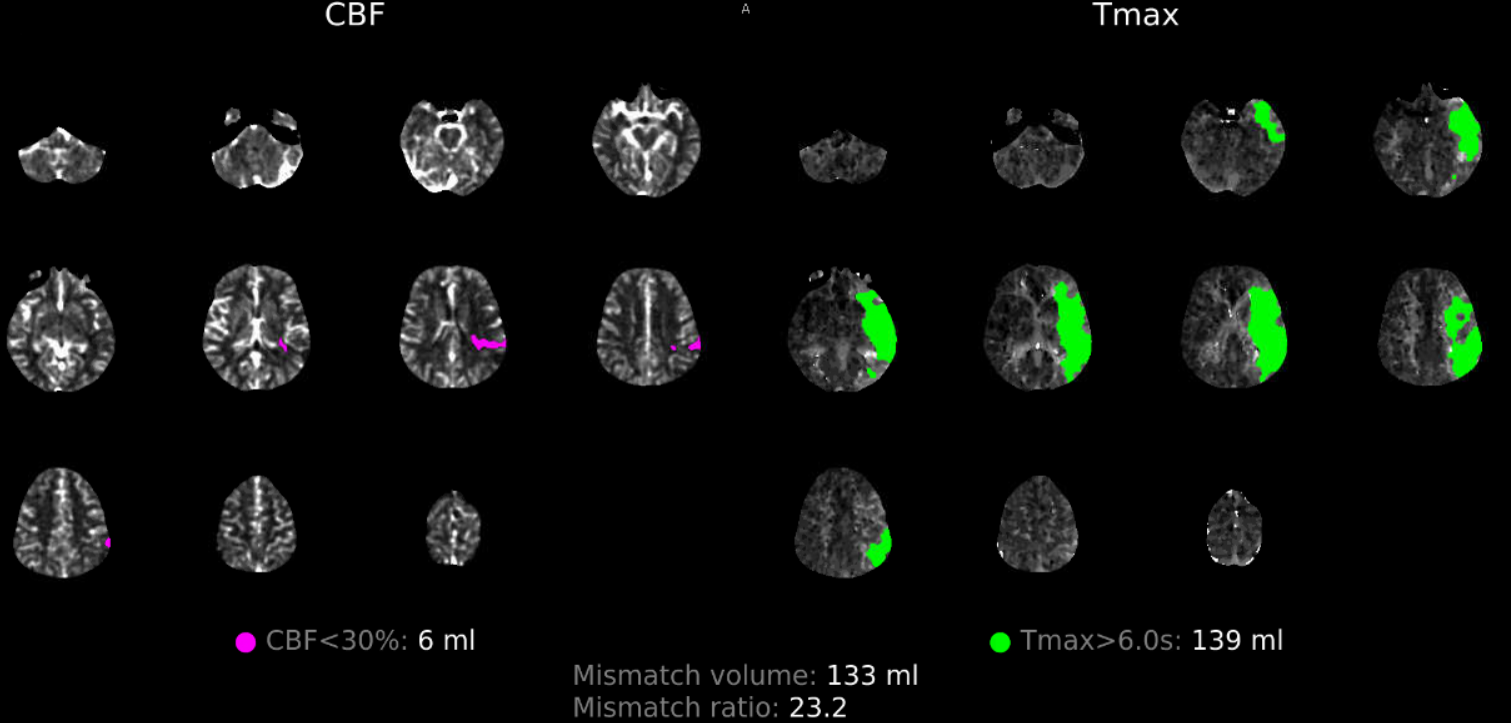
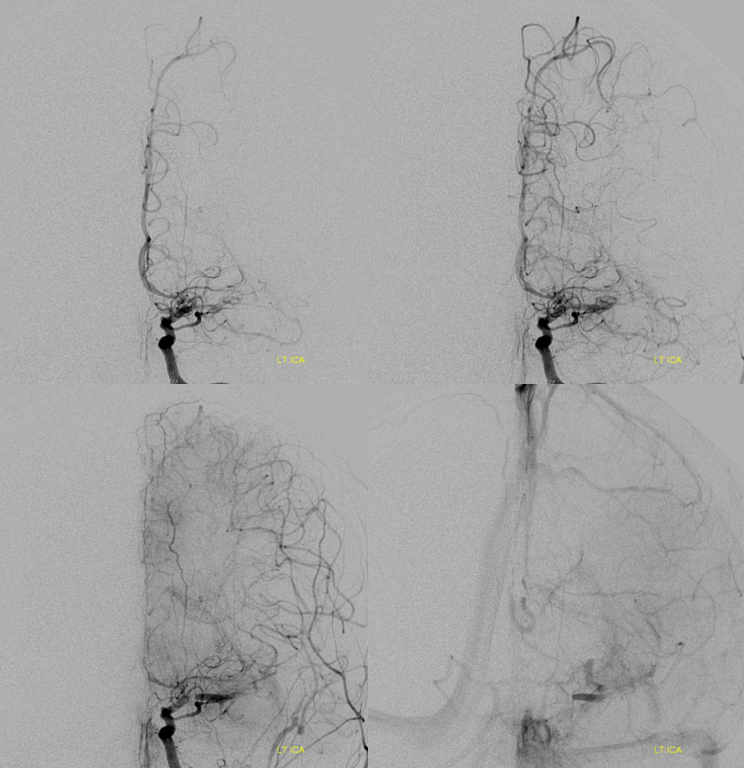
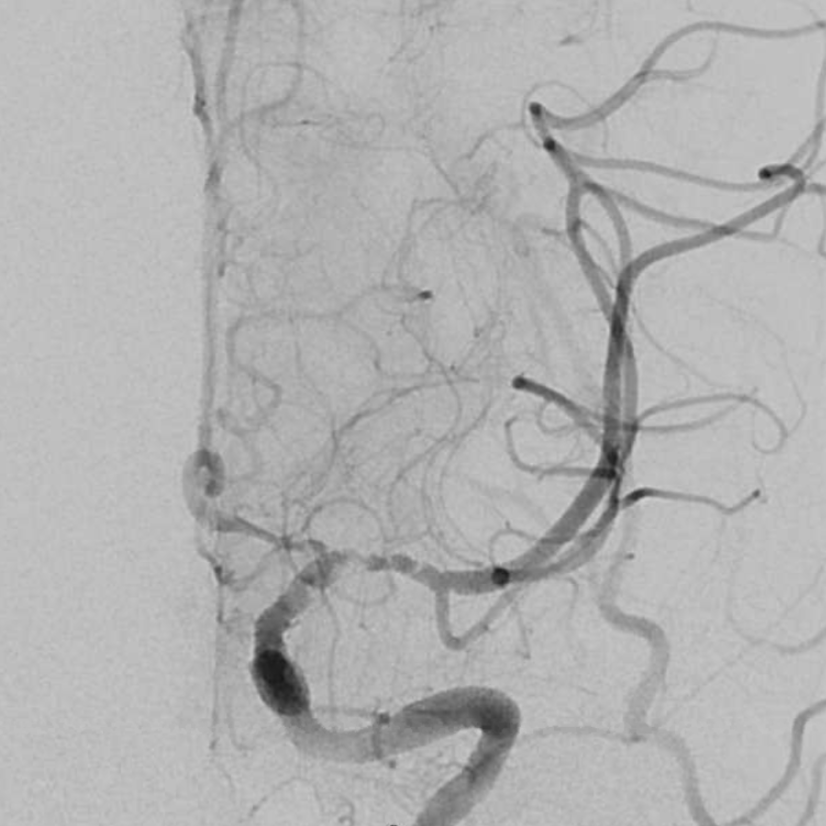
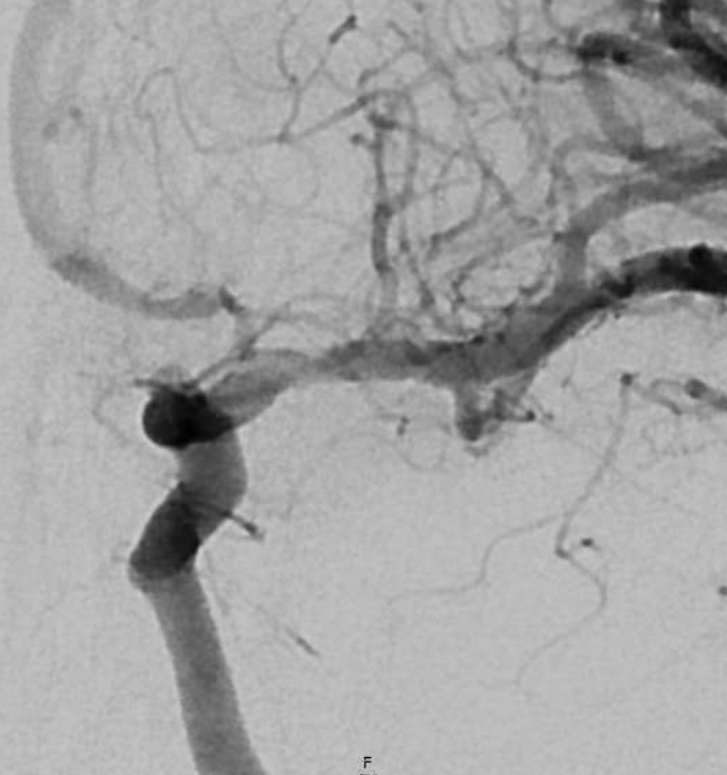
Angio — the clue here is slow antegrade filling of the MCA, consistent with a subocclusive lesion (lots of leptomeningeal collaterals are present also, thankfully).
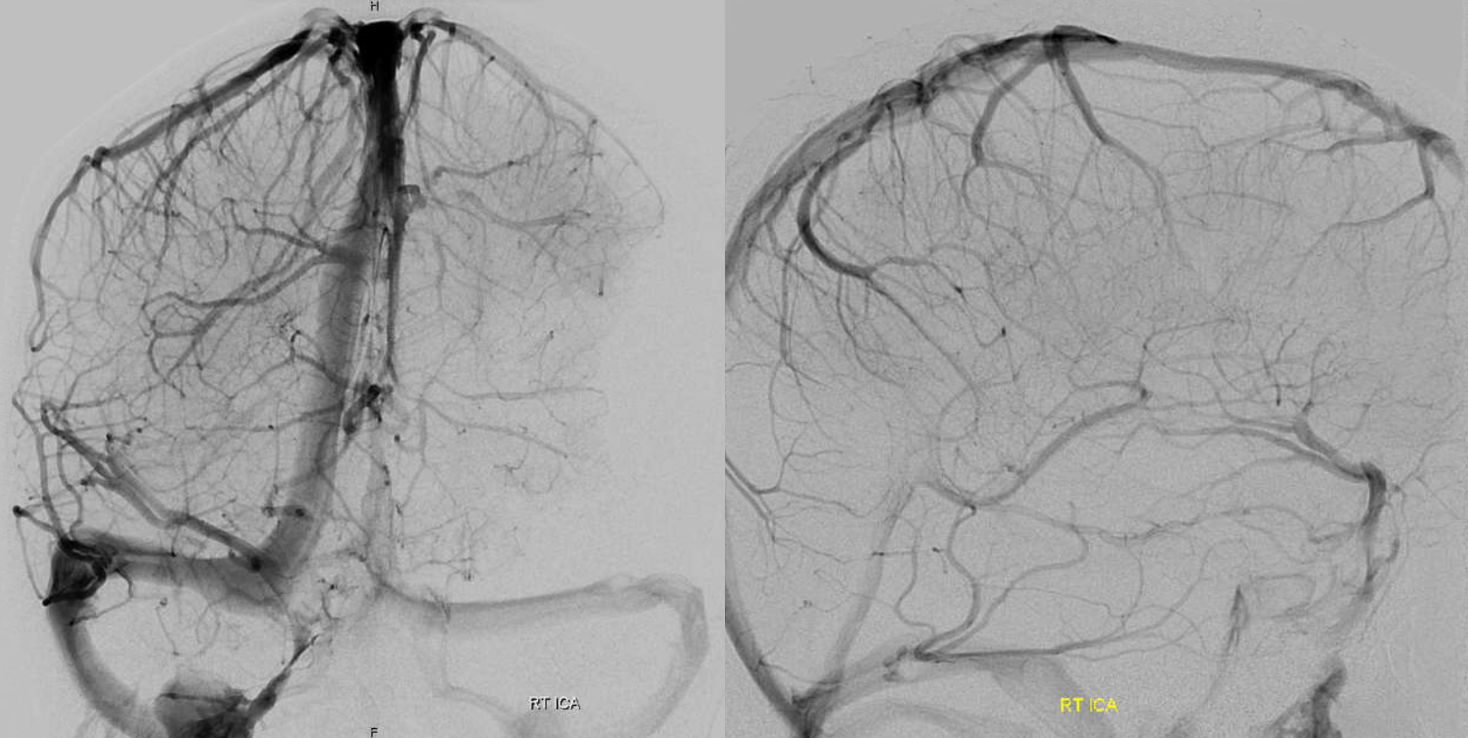
The biggest clue, however, is contrast stasis in portion of the M1 (bottom images). What causes that? Not something we see with either embolus or athero. The likely cause is stasis in the dissection flap, with contrast slowly filling the flap and remaining inside.
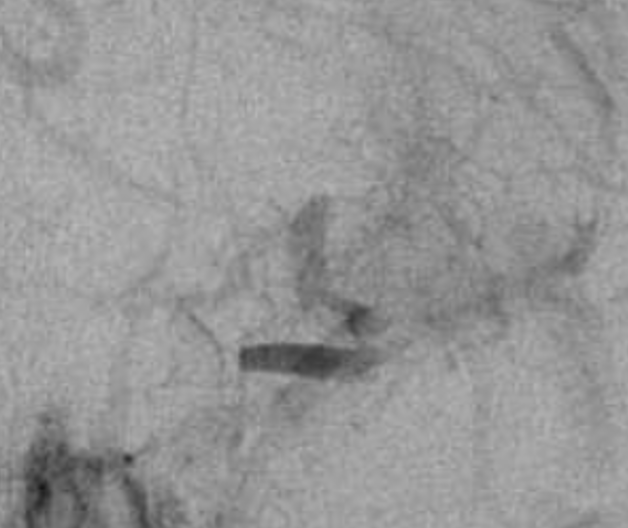
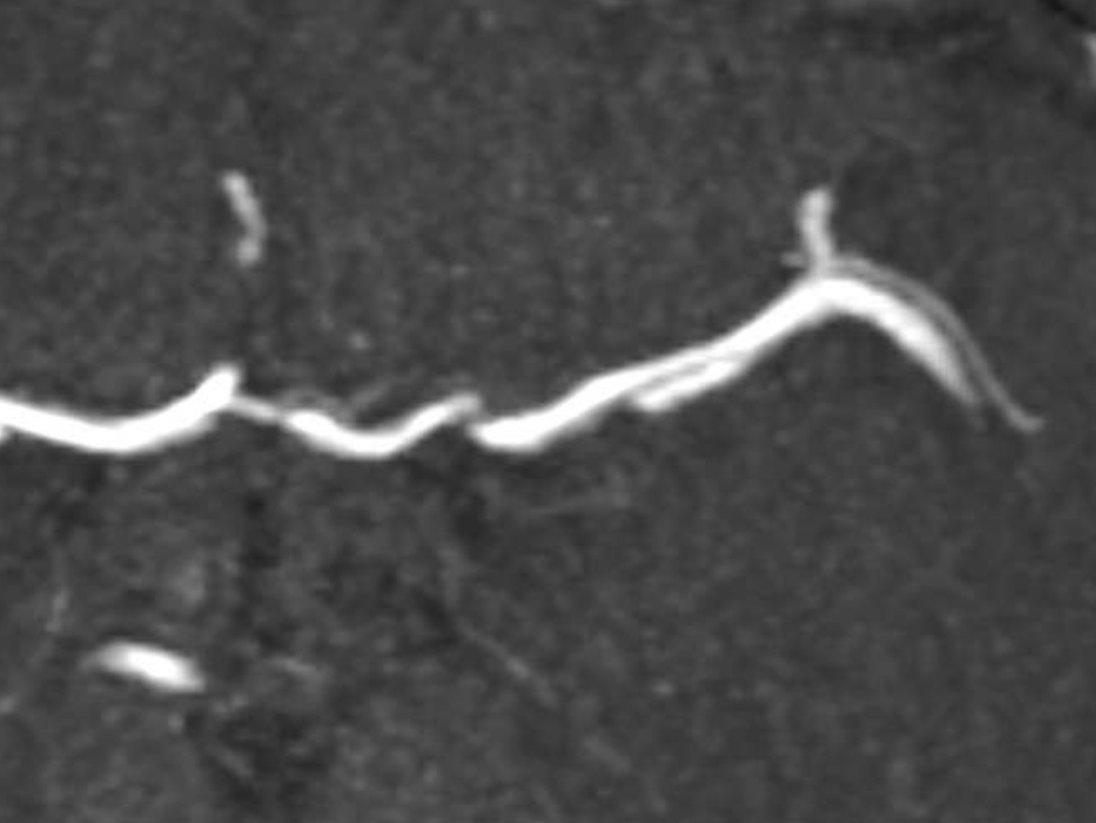
Magnified image below. We are certainly not saying that this is a sure sign of dissection, or that this is easy to recognize prospectively. It very much is not. However, the warning signs are here
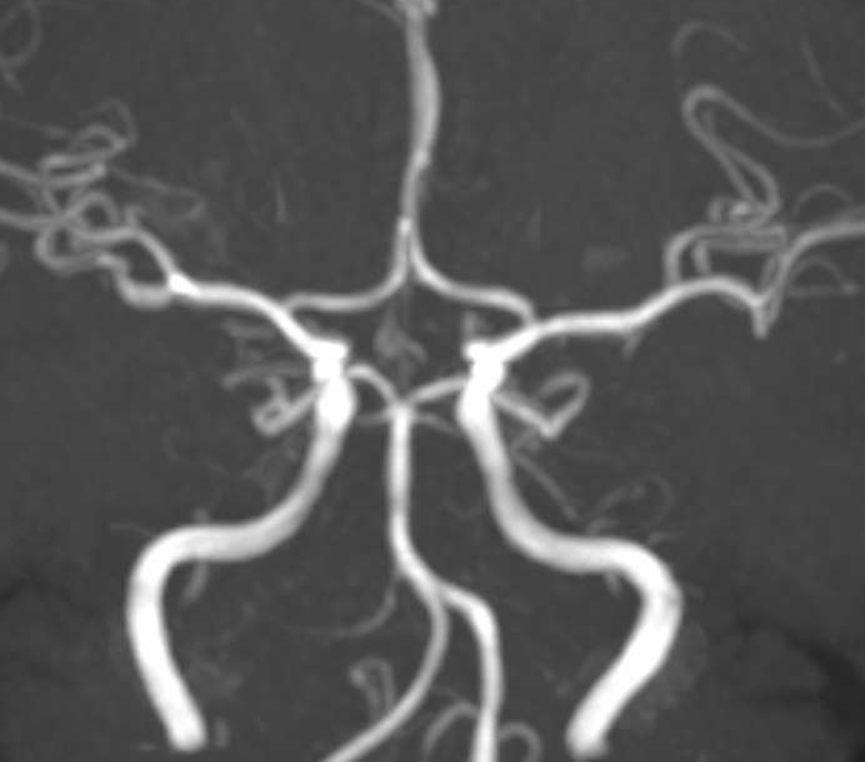
Here is another one — several years prior, there was a normal MRA. This can be helpful if the differential is atherosclerotic disease.
Now what? We go into the ICA (above are CCA images) and take another picture — no different
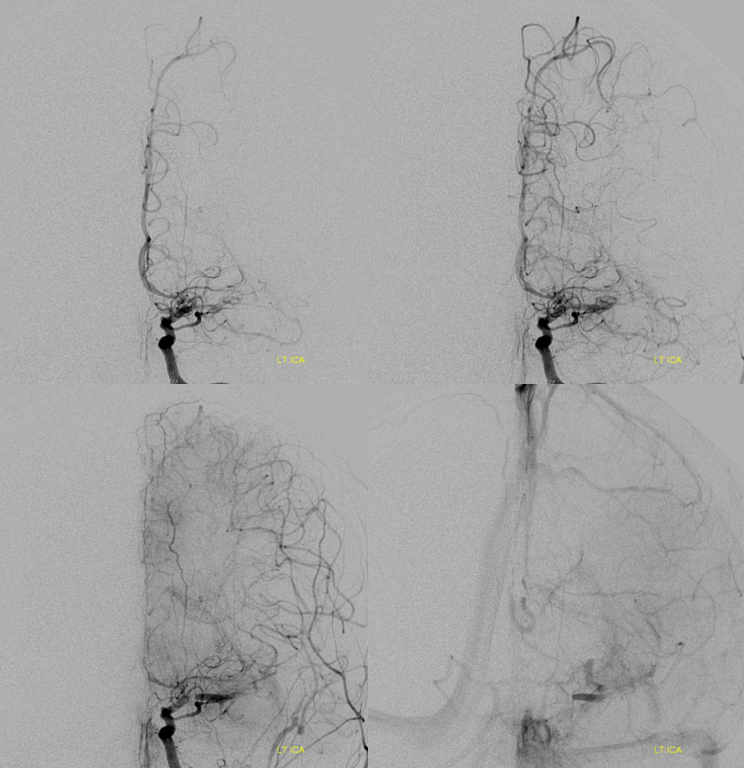
A Sofia 6 is advanced into the petrous segment and another image taken — see below.

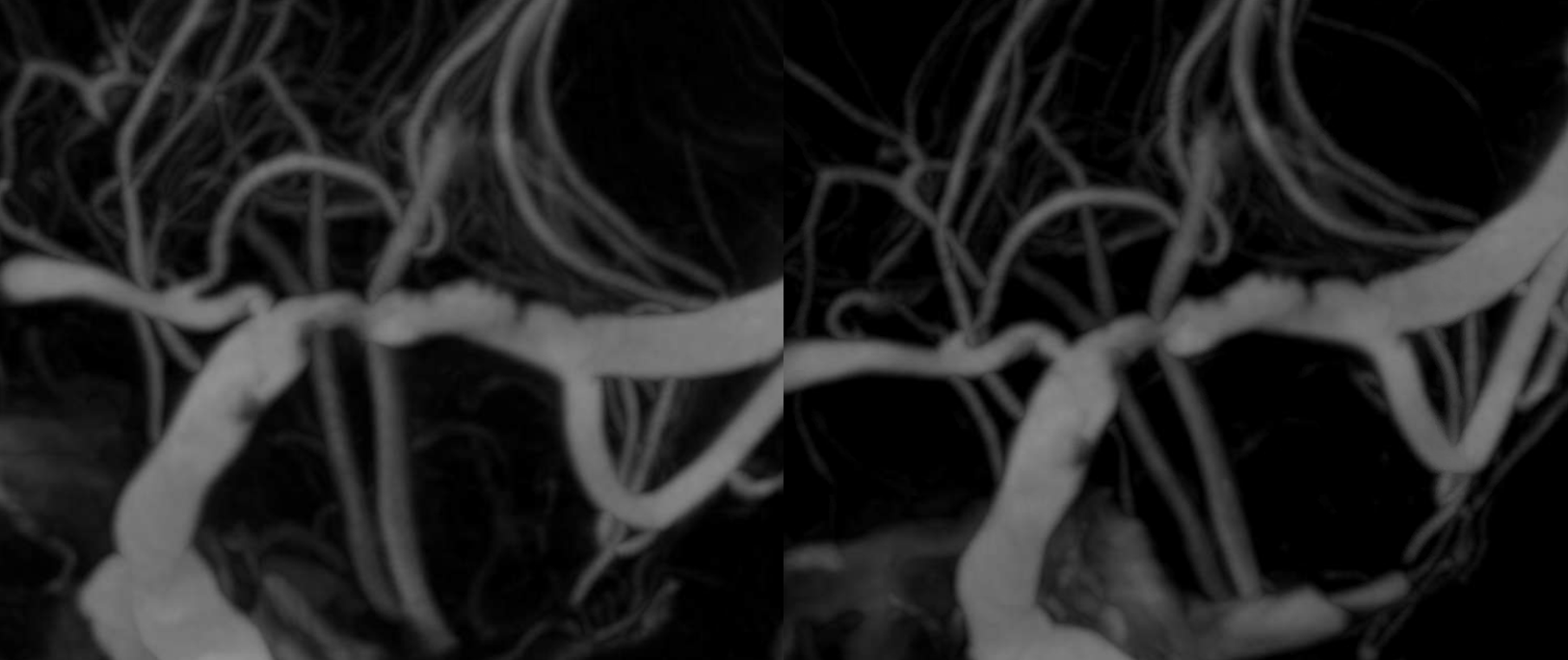
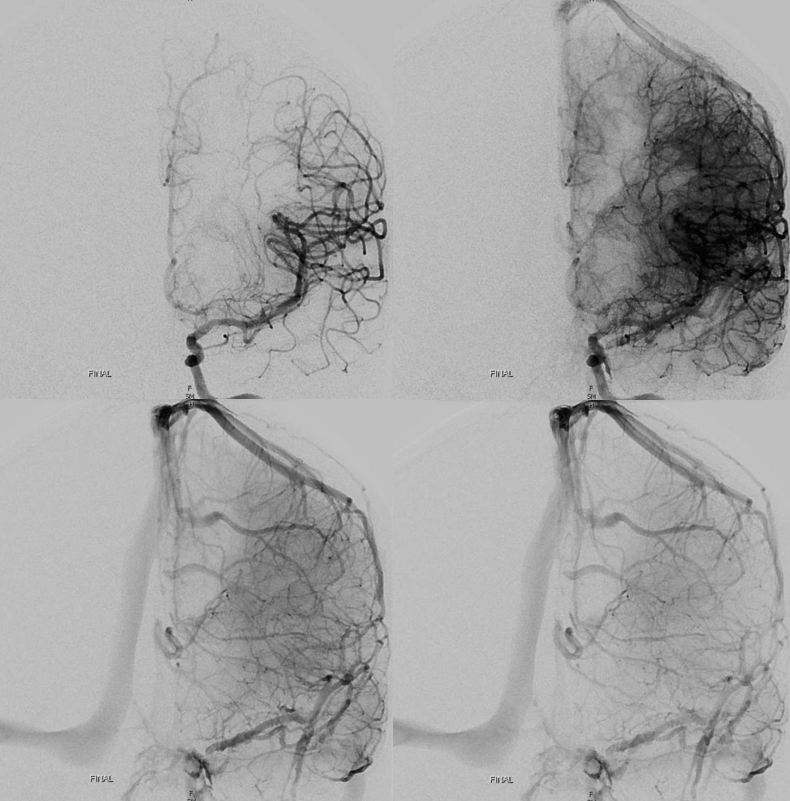
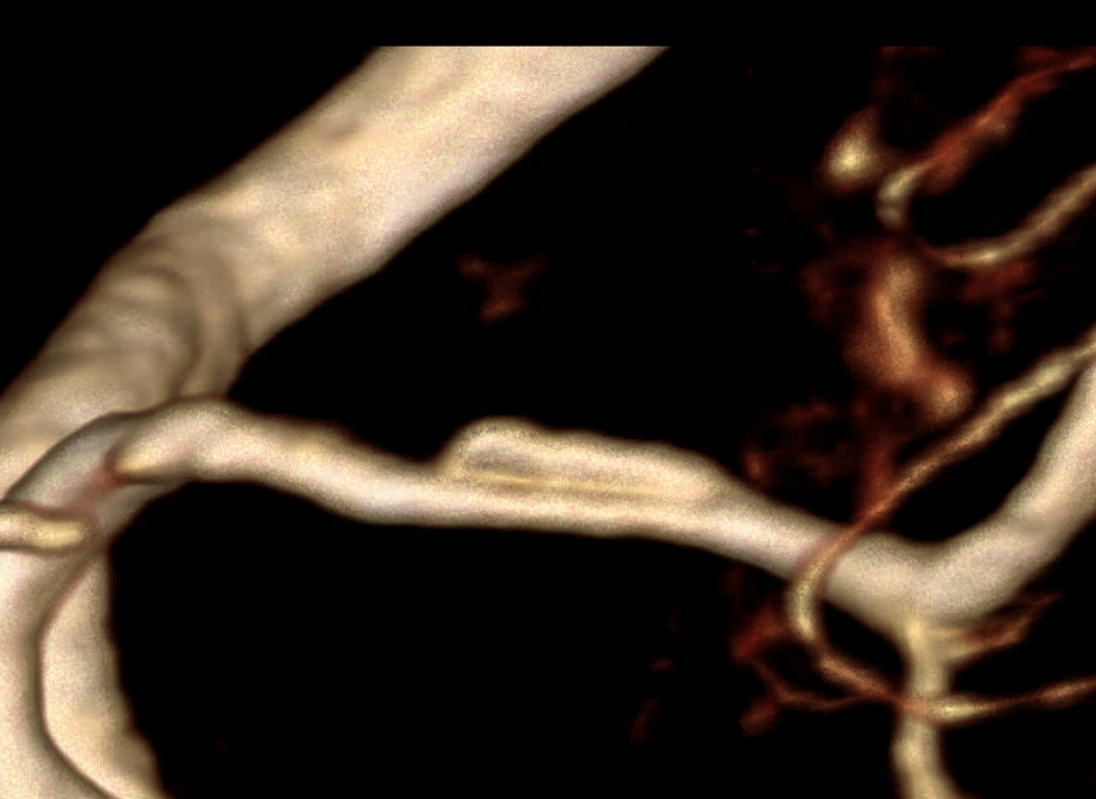
What happened? Did the force of injection dislodge some thrombus and reopen the vessel? Possibly. That is another clue — acute intracranial dissections can evolve literally in front of our eyes. Now we have an open vessel with some subocclusive filling defects at the carotid terminus.
Also notice diminished caliber of the proximal A1. These are very important clues. First, in our experience intracranial dissections have a predisposition to start at the carotid terminus. They either extent into both M1 and A1, causing A1to be narrow, or the narrowing is reactive. In either case, this pattern is another strong clue.
So, now we have a likely dissection, with subocclusive thrombus at site of intimal tear. What to do? If at this point we are convinced that this a dissection, we should give lots of antiplatelets and possibly stent. We prefer not to stent, just like we don’t stent extracranial dissections, unless there is no other way to maintain antegrade flow. However, what if we are not convinced — in this case, the standard maneuver is thrombectomy. For dissections, this s a treacherous move, as it can easily extend / worsen them.
In this case, we elected thrombectomy. Retrospectively, this was probably not the thing to do. The point is that prospective diagnosis of dissection is no walk in the park. We did however go very gently with the Sofia — probably the gentlest aspiration catheter out there, size for size.
Things seem to look not too bad post aspiration thrombectomy. There is irregularity now in the whole M1 but that might be spasm. The A1 stenosis seems worse also, but that could be spasm too…

After a few minutes — now its not good. A1 better, M1 worse. Is it worsening spasm? Extension of dissection? What to do?

Here, we do the right thing — give a bit of verapamil and wait. Its not nothing to give a vasodilator into a newly opened territory, but we are keeping pressure low and overall this seems like the right thing now.
Look below — the M1 is better for sure after verapamil — except for that distal segment. Its asymmetrically narrow, and there is still filling defect in the very proximal M1 . This picture is also something we see with dissections — touching them can make it worse.

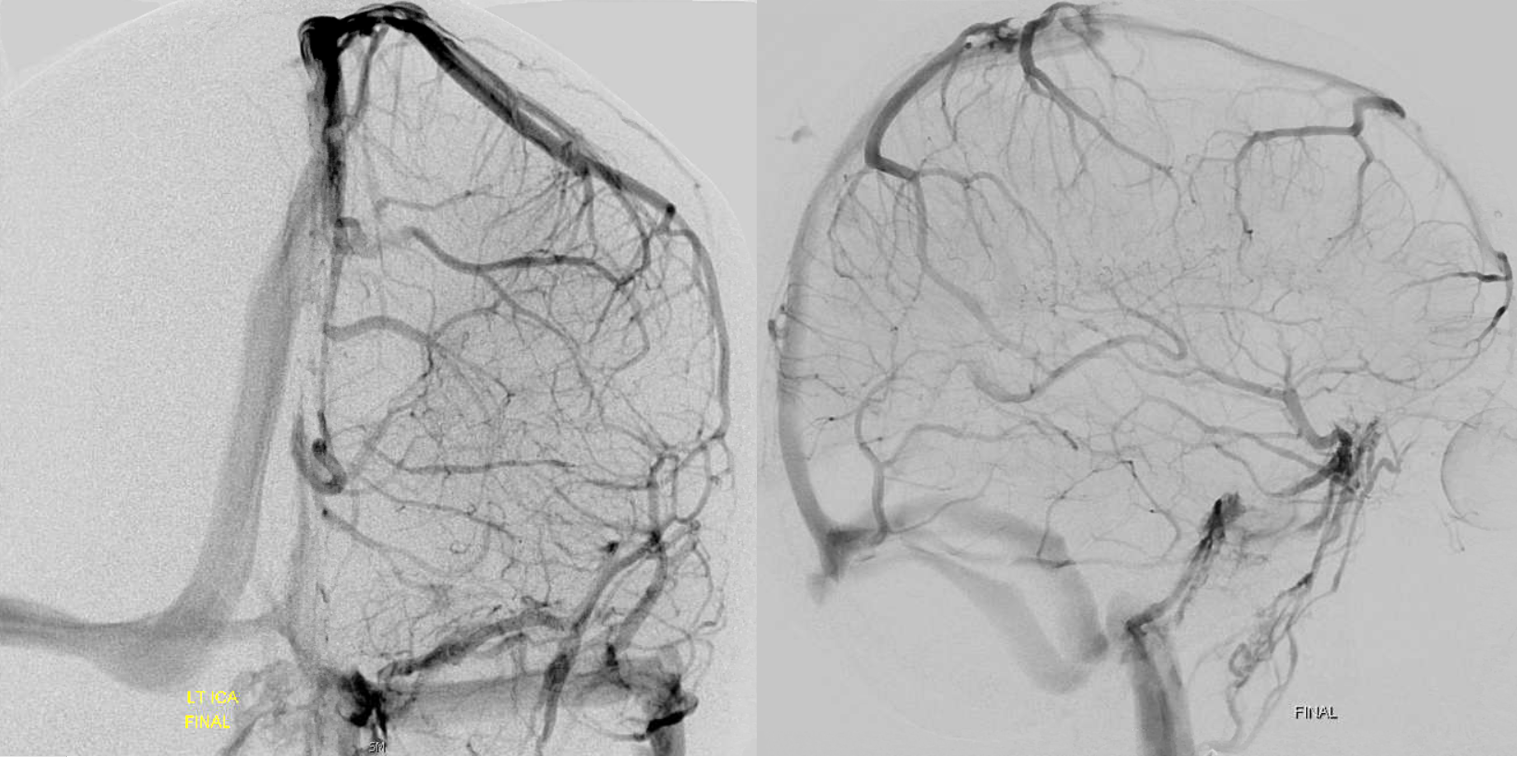
Final after some more waiting and intravenous integrilin — looks like the best so far. There are however residual signs — the A1 narrowing is persistent and is an important clue throughout. Also, the proximal M1 is not normal — there is less contrast density there. Why? This is where the flap it, flattening the vessel.
No DYNA is available for the above study.
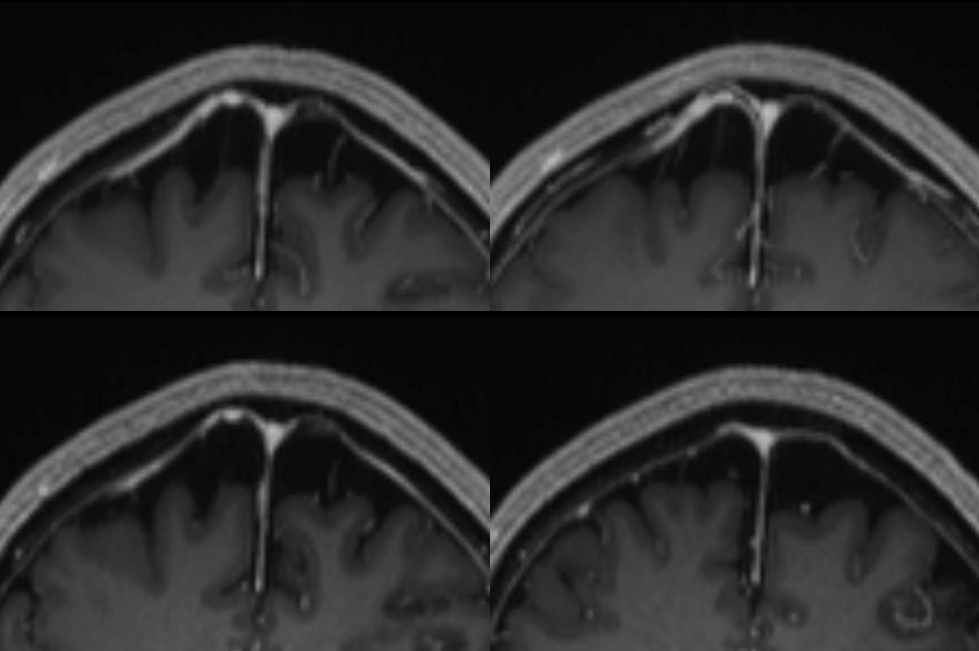
The patient improves, and worsens the next day (was on heparin overnight). This is another question — how to manage them medically in acute setting. If there is a major flow issue, probably anticoagulation is best. If there is not, it may be better to go heavy on antiplatelets to keep acute clot from re-forming. There is no literature to help, so we go by what we typically do for extracranial dissections. In this case, the heparin was not what we typically do, and it shows below.
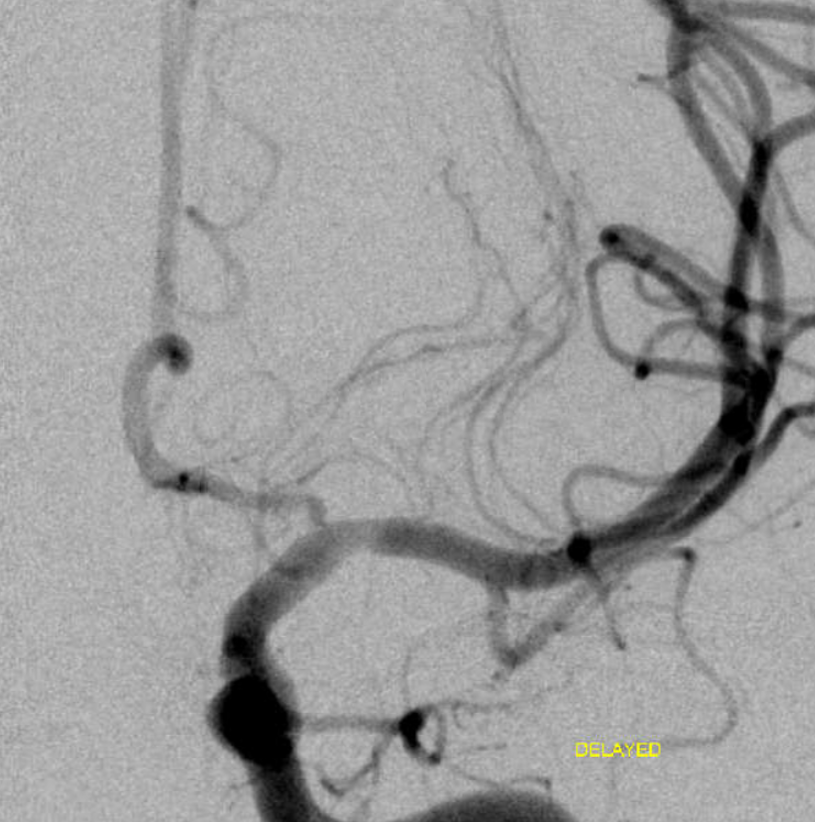
This is the next day’s angio. There is nothing like time to help figure things out. Here, the important clues are that both A1 and M1 abnormalities are longer in length — the dissection is progressing.
Now we have opportunity to get a DYNA
See again that bite in the upper distal M1 ?
By this point, we are sure that we don’t want to touch the MCA again, except if we need to cross it to stent. Some IA integrilin seems to work to get rid of clot.
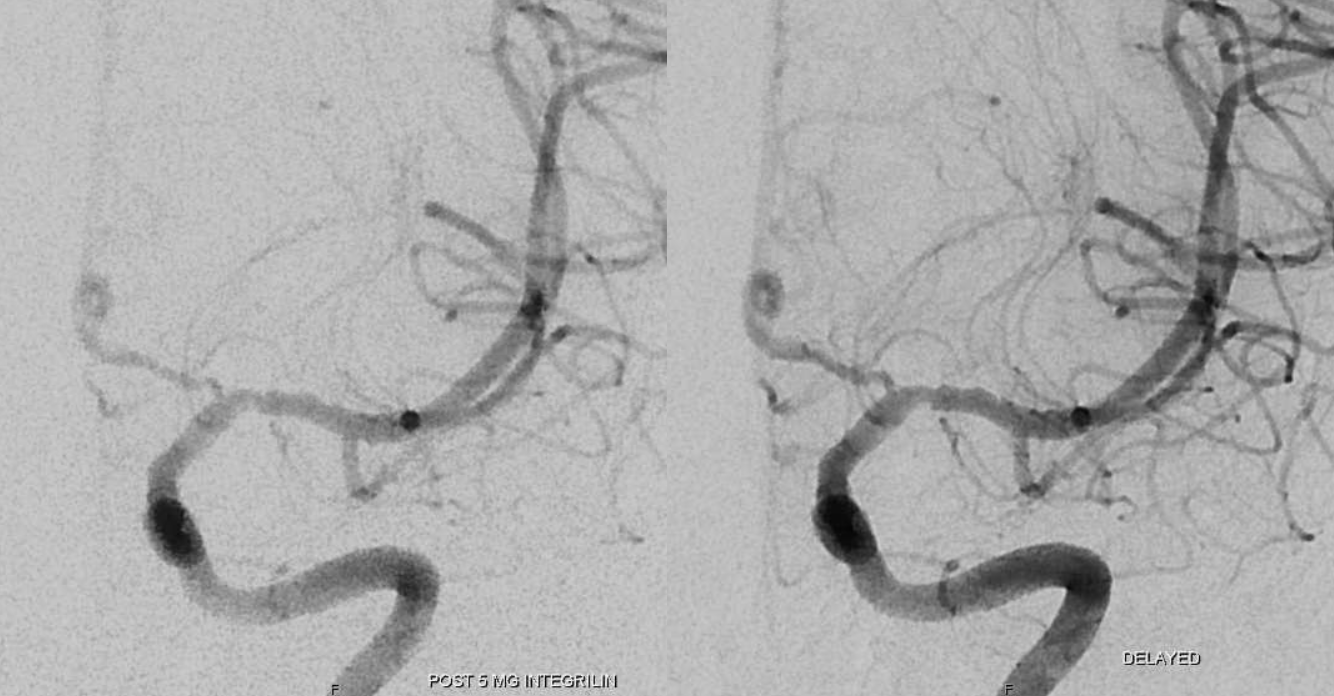
Post integrilin DYNA shows the location of the flap.

Final post 2nd angio/embo
Again, pay attention to the A1 segment — not because ACA perfusion is at stake — there is an ACOM here — but because the A1 is a consistent clue here. Not that we cant have A1 athero, of course we can. But it is not as common as this dissection-related smooth proximal stenosis, and there is no athero anywhere else.
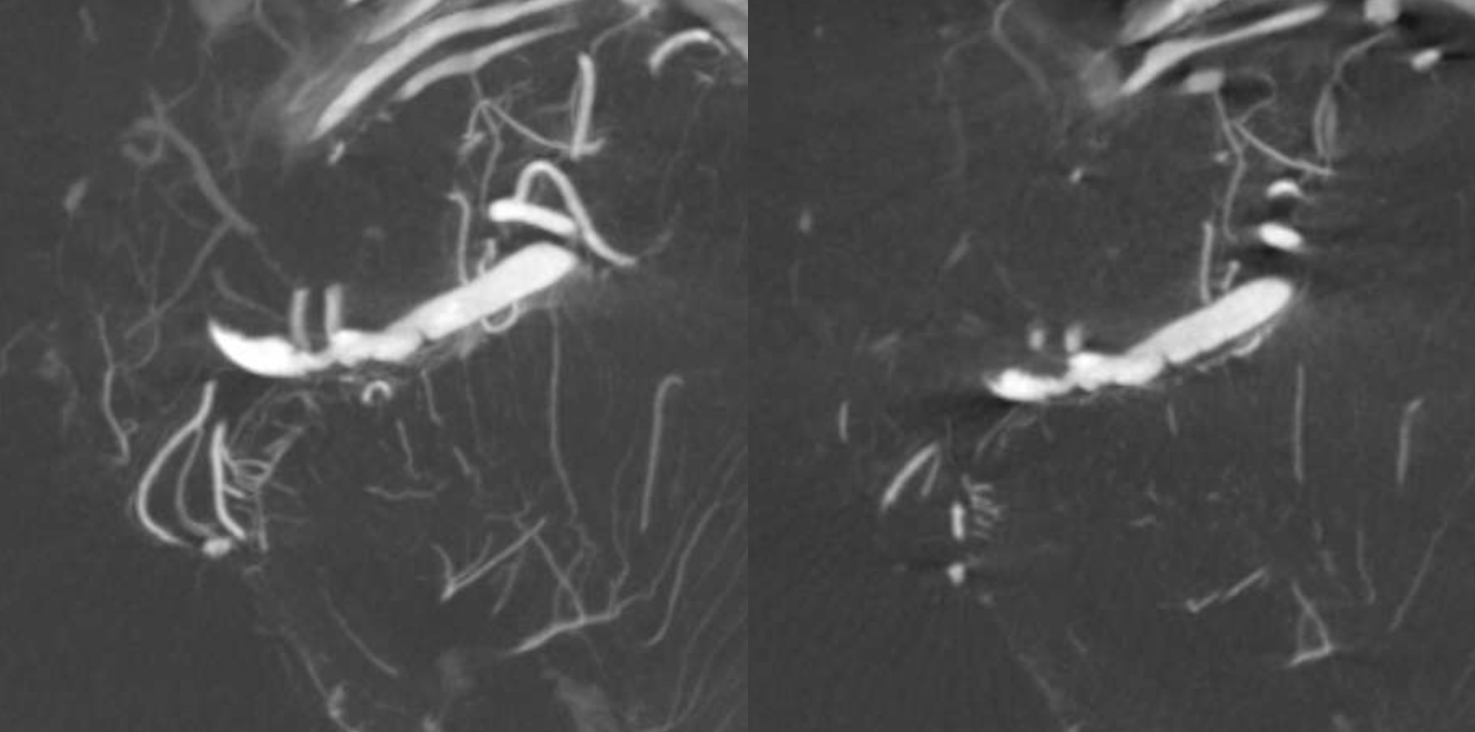
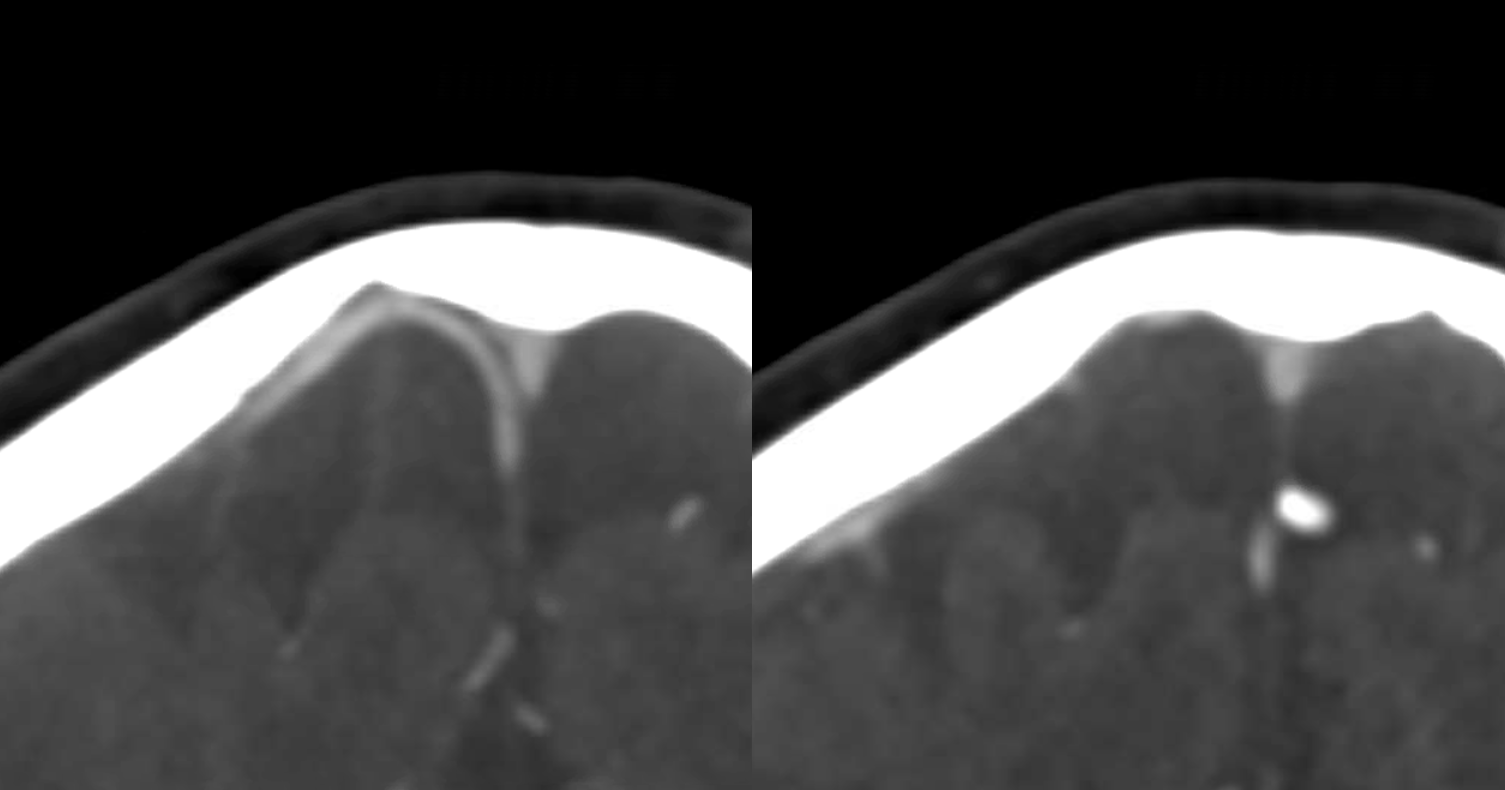
So, now we go to MRAs — this one is 2 days after second angio — Look at the vessel — there are clues here also
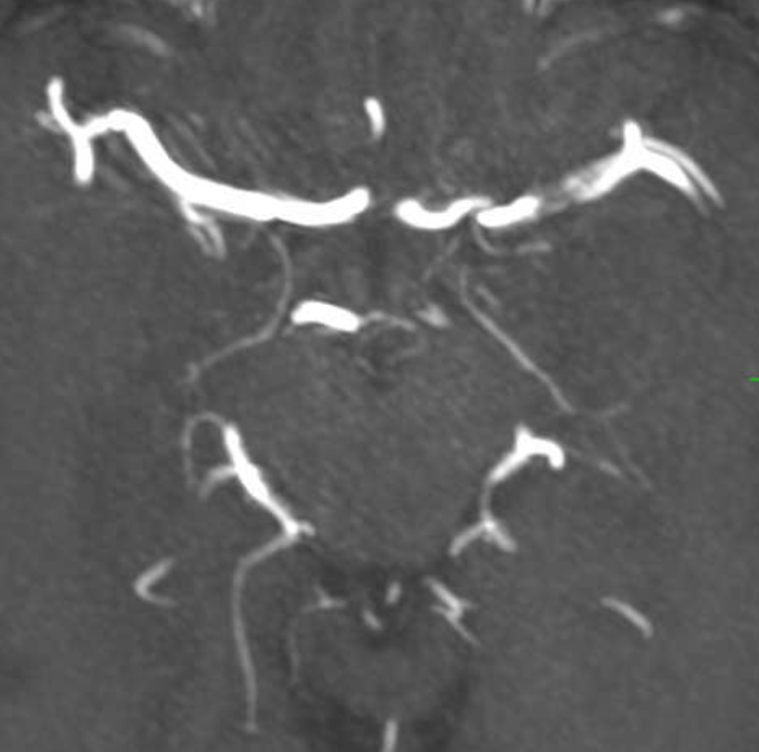
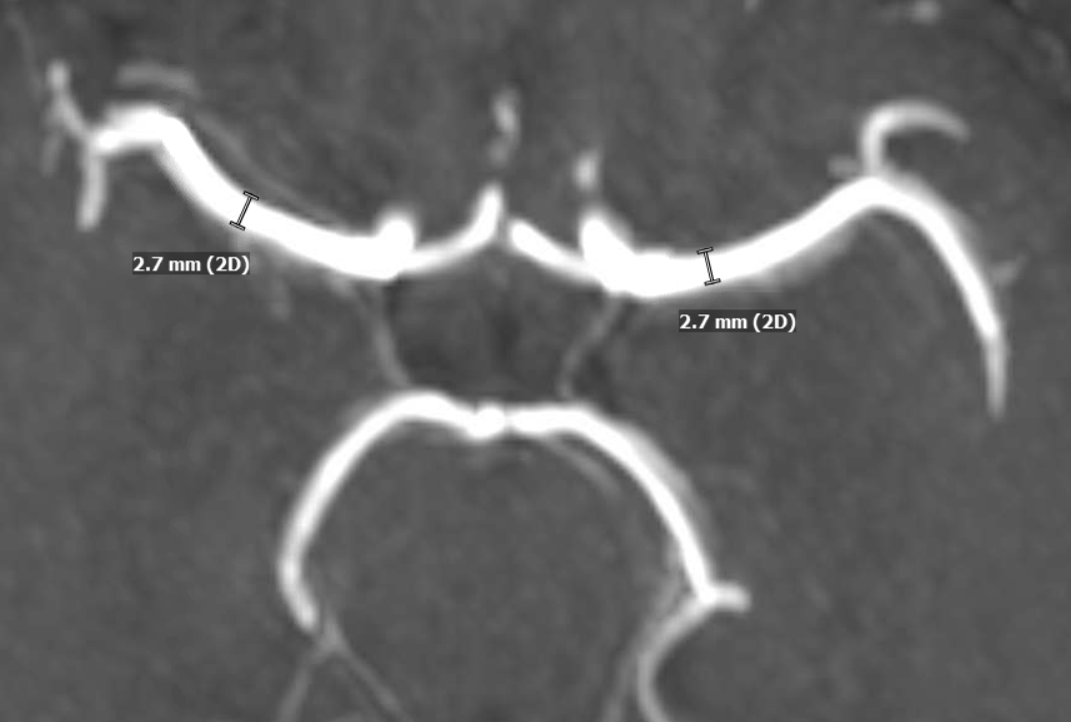
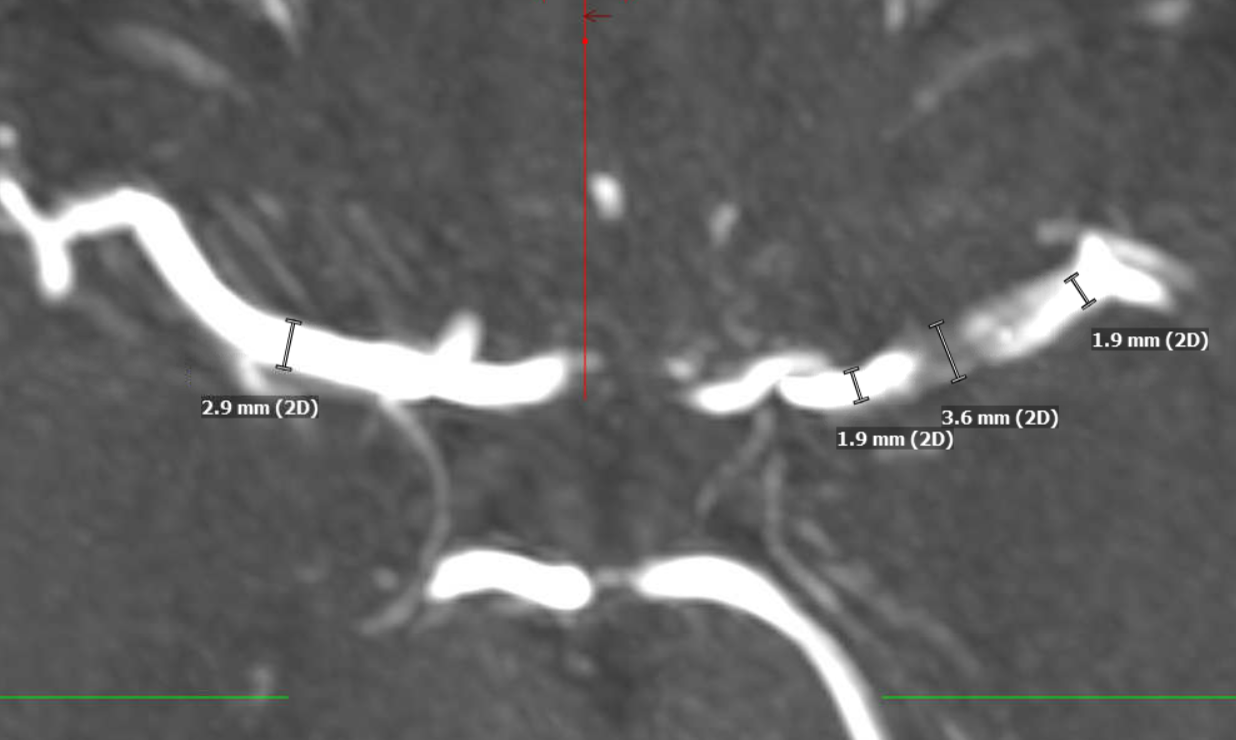
The major clue is vessel size. On the remote MRA, both MCAs were the same caliber. Now, the right is same, but proximal and distal left M1 is smaller, while the mid-segment is larger in caliber than the 2.7 mm baseline. Intracranial dissection segments often have larger caliber lumen on MRA. This is not T1 shine through — unlike extracranial dissections the false lumen frequently dissects back into the true lumen, creating two lumens.
The larger vessel caliber on MRA is distinctly different from athero, where the overall vessel caliber is larger, but lumen is smaller, and from noninflammatory causes such as Moya Moya, where the whole vessel is smaller.
Another 4 days later there is another MRA — the findings are becoming more obvious
Another two weeks go by — things are looking better — the mid-M1 caliber is decreasing — evidence of healing. The proximal A1 segment remains stubbornly narrow.
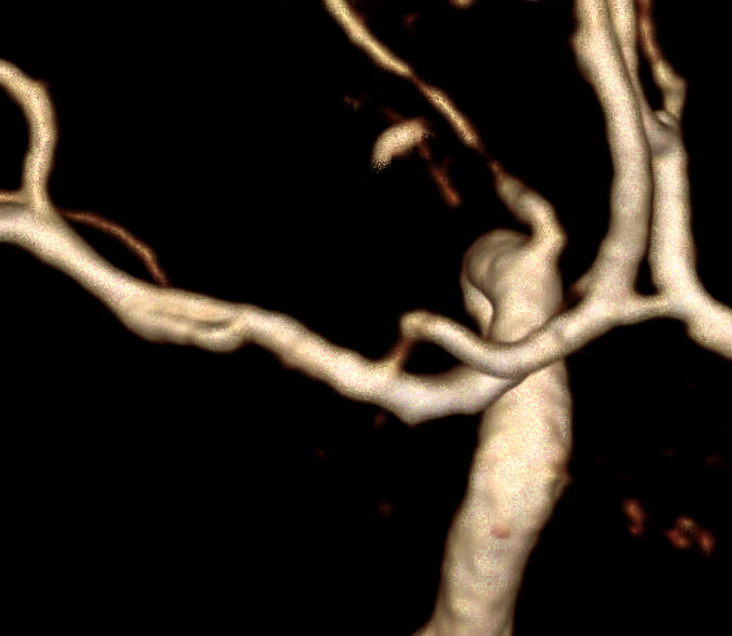
Finally, another few days later, and on a higher quality MRA — now i think we can convince the remaining skeptics that there is a flap here, with two lumens — nothing like time to solve a mystery
Volume rendered image. The overall M1 caliber proximal and distal to dissection remains diminished. This is expected to improve.
The VR view from the front is deceptive, except for the A1 stenosis. Notice also a diffusely smaller caliber of the left M1

It takes a view from above and back to show the two lumens.
Finally — and completely unrelated (!!) — good venous images of parasagittal dural venous channels / venous lakes — because we care about these also, and have good visualization. Also present is dual left superficial sylvian venous drainage — via emissary veins and into the paracavernous sinus.
Movie of one of the DYNAs, including venous drainage
Now, back to the dissection. What lessons can be learned? Many. The important ones are to keep a healthy but not too paranoid index of suspicion about possibility of dissection for all the reasons outlined above, and tread very carefully — it is all too easy to make them worse.
