Number 116a

A very consistentent artery within the Iternal Accoustic Canal (IAC) supplying the cochlea and vestibular structures of the inner ear — it is the artery of CN VII and VIII. Occlusion classically leads to hearing loss. The consistency of this (i.e. collateral potential) is unknown — based on various occlusions, iatrogenic or otherwise), that can be reasonably established in time, there collateral potential is not very good. Probaby the sparing of hearing is due to collaterals to the AICA, from which it usually arises. The artery itself likely has very poor collateral potential, similar to the central retinal artery.
Origin is from the AICA, near the famous AICA loop. Reports of direct origin from basilar may be tainted by the underappreciation that a key feature of the AICA is its ownership of the Labyrinthine artery. Catch 22. For example, when the PICA is highly dominant, what else has an AICA specifically to do? — so it will be small, and supply the Labyrintine and perhaps the subarcuate artery — easy to mistake for a “direct origin”? Whatever the case, occlusion of the AICA at the loop has a high probability of hearing loss.
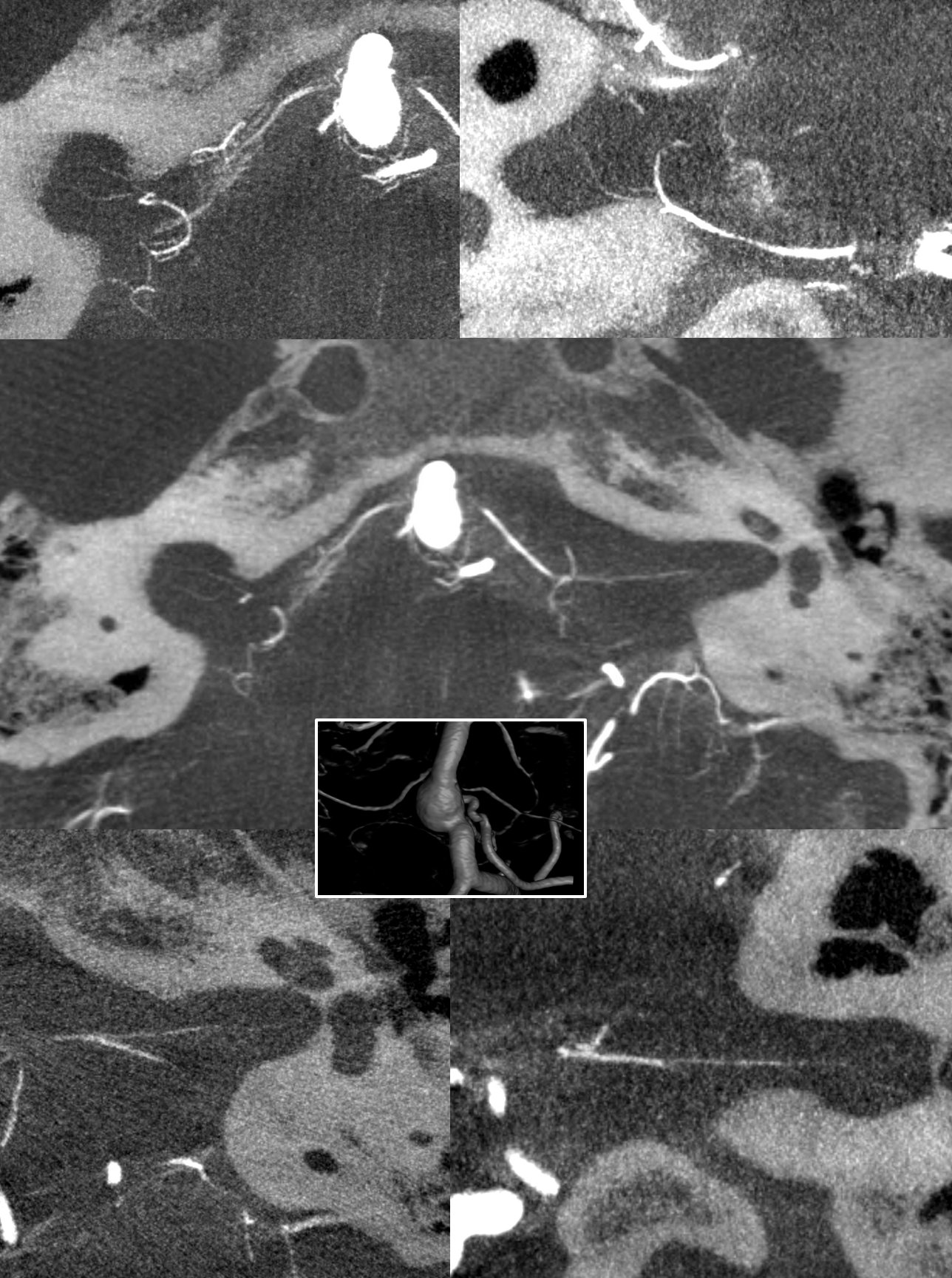
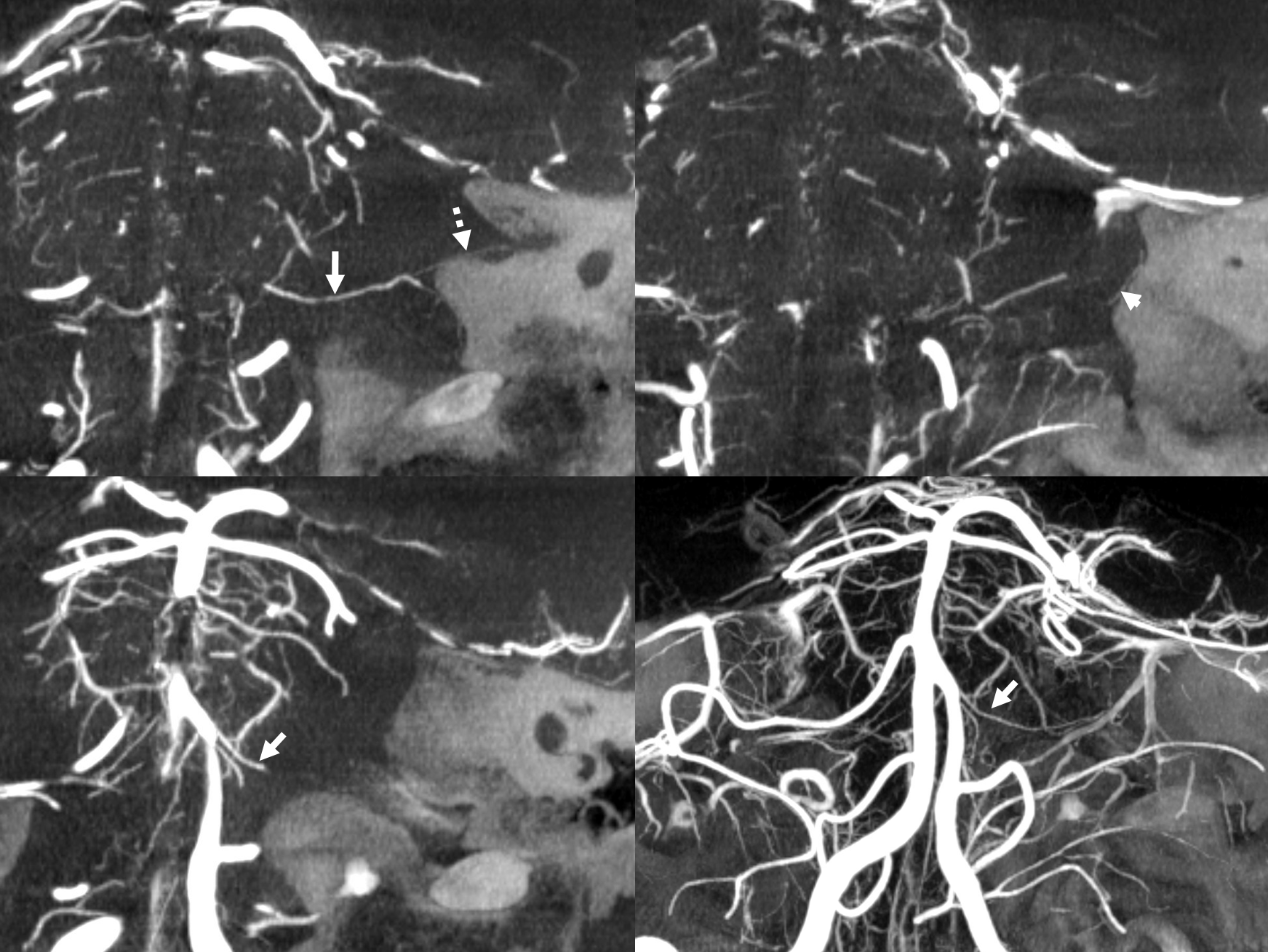
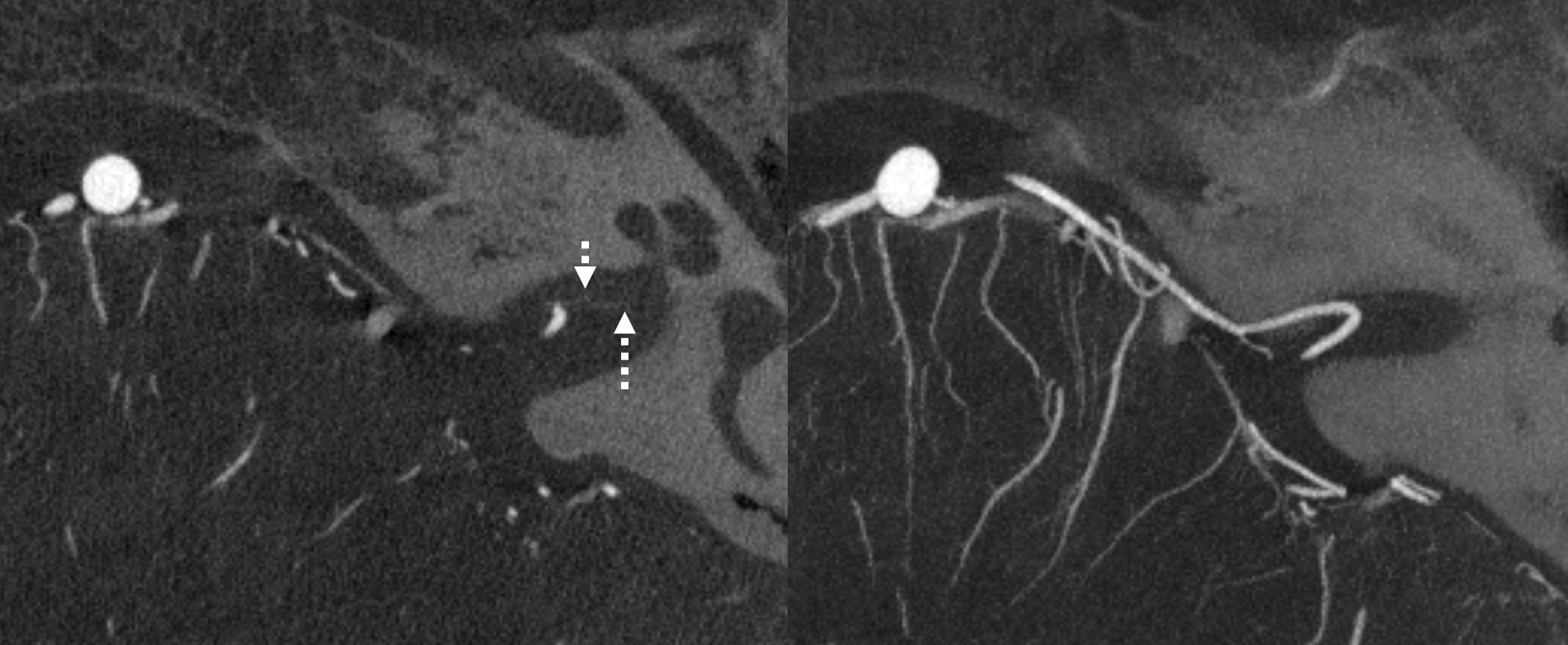
Visualization of the Labyrinthine artery is currently impossible without high resolution Cone Beam CT (HR-CBCT). With HR-CBCT, it is seen in over 50% of cases. Below are some examples:
with labels
Bilateral Labirynthine arteries in case of a midbasilar aneurysm. Small AICAs
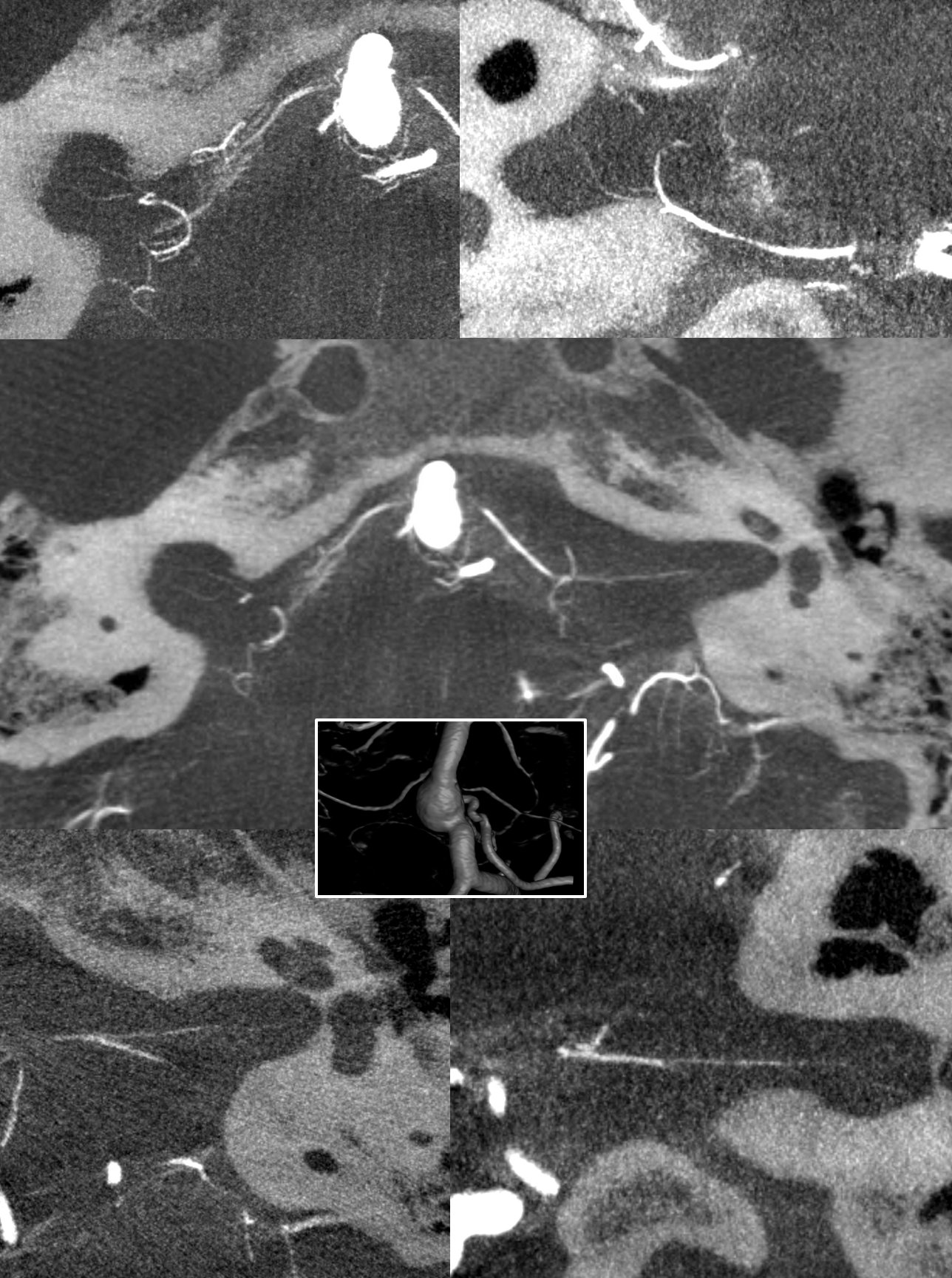
Another patient with bilateral prominent labiryinthine and subarcuate arteries
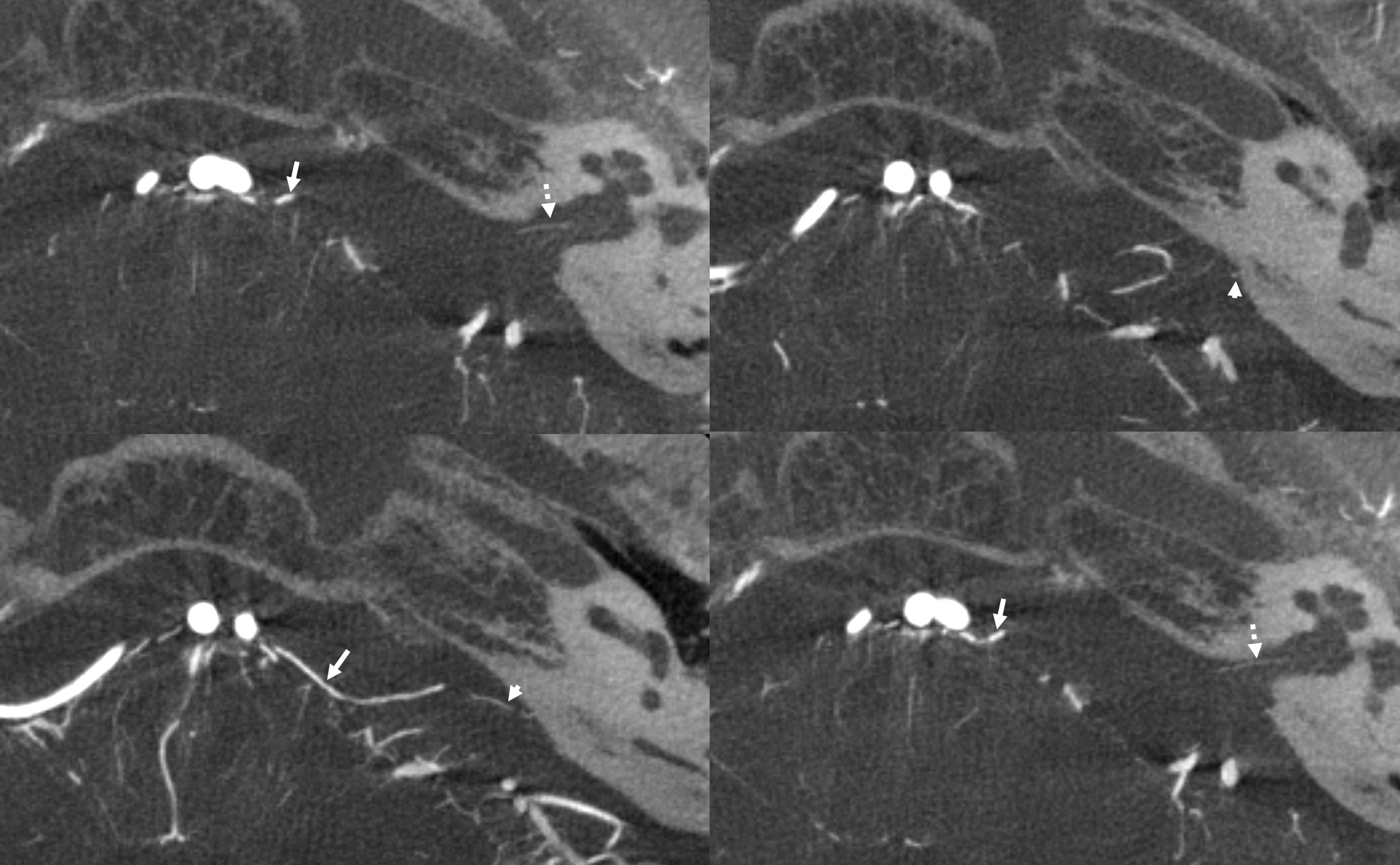
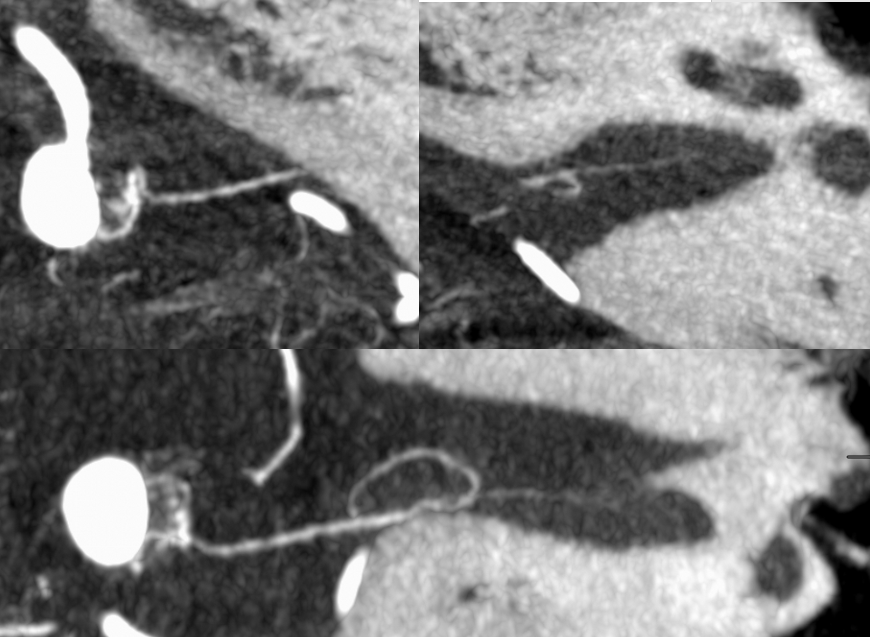
Left side — note branching — best seen in upper left coronal image — one branch to the cochlea, another to the vestibule.
Right side — branching resolution also
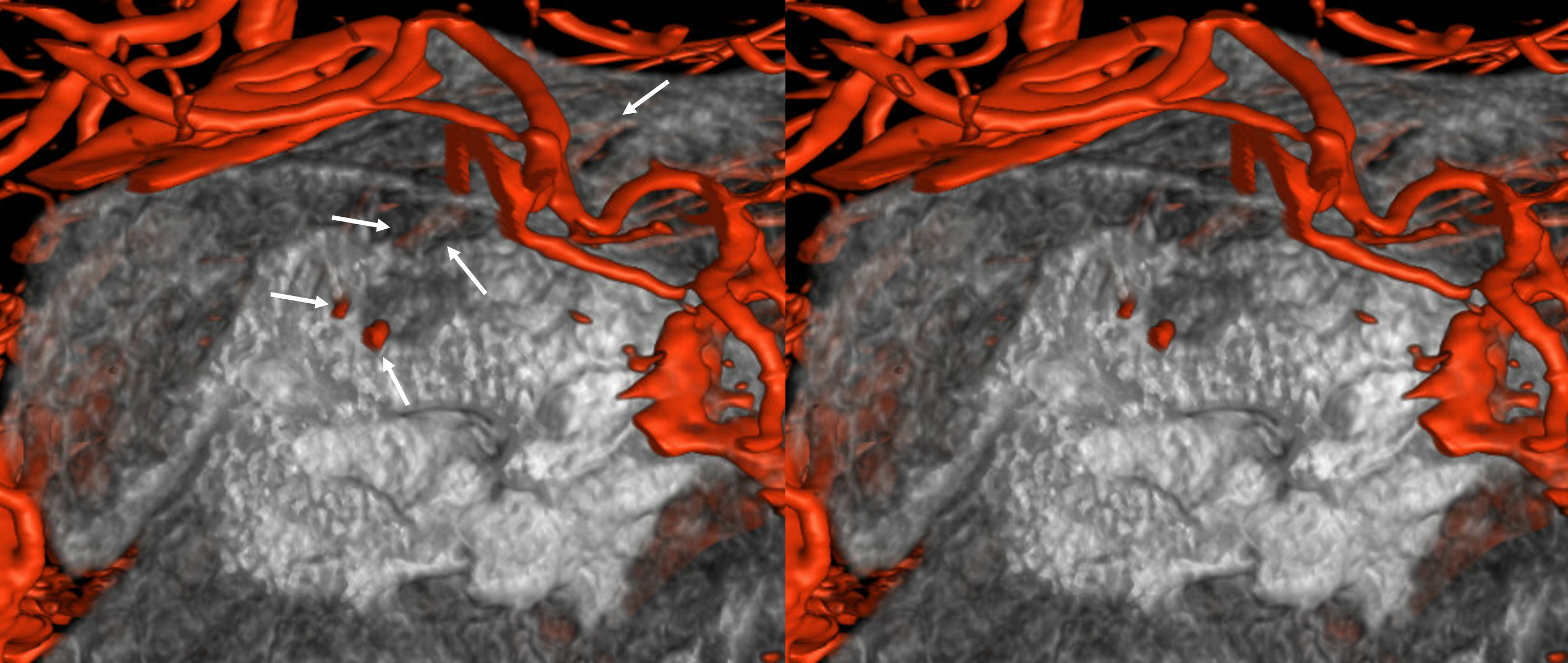
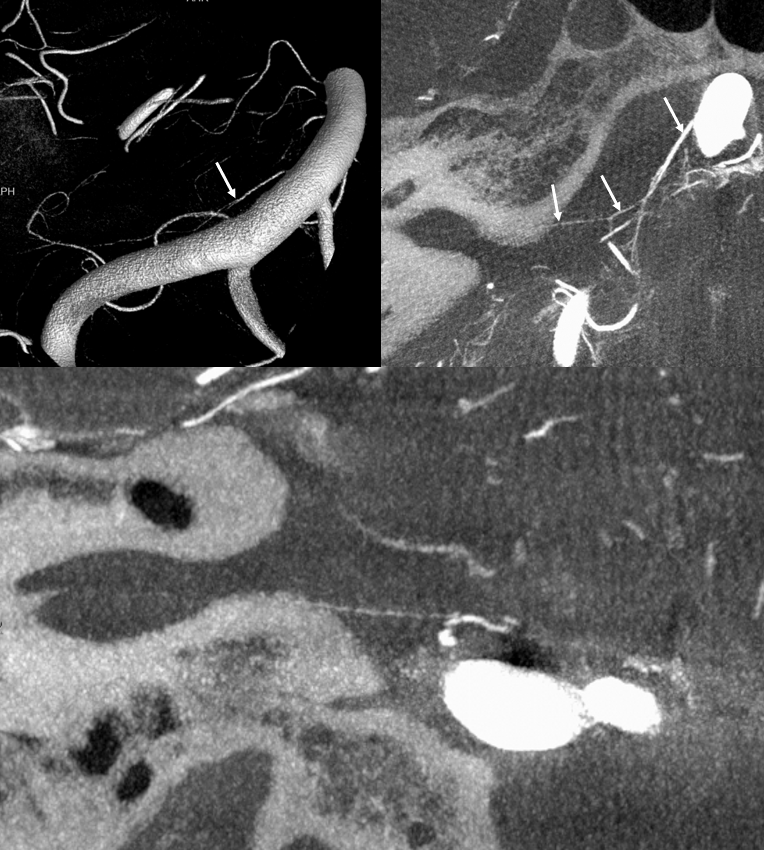
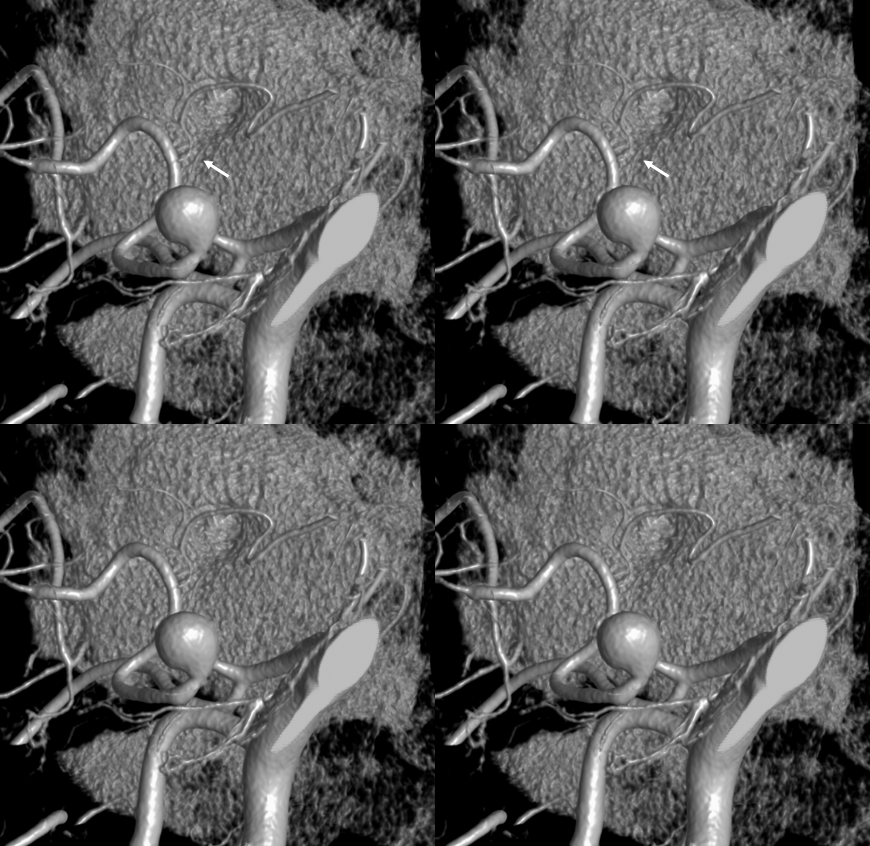
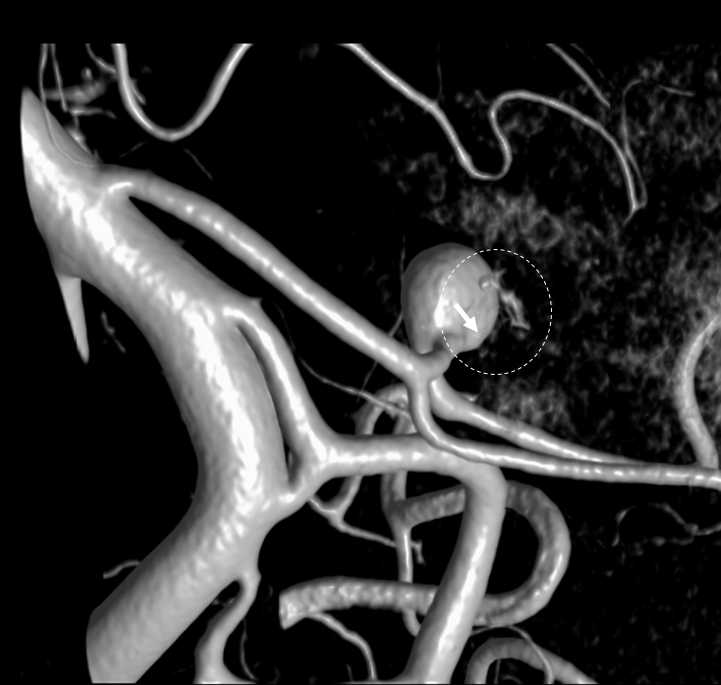
VR image of the same case as above. See the subarcuate artery (arrows) inside the petrous bone, below the arcuate eminence
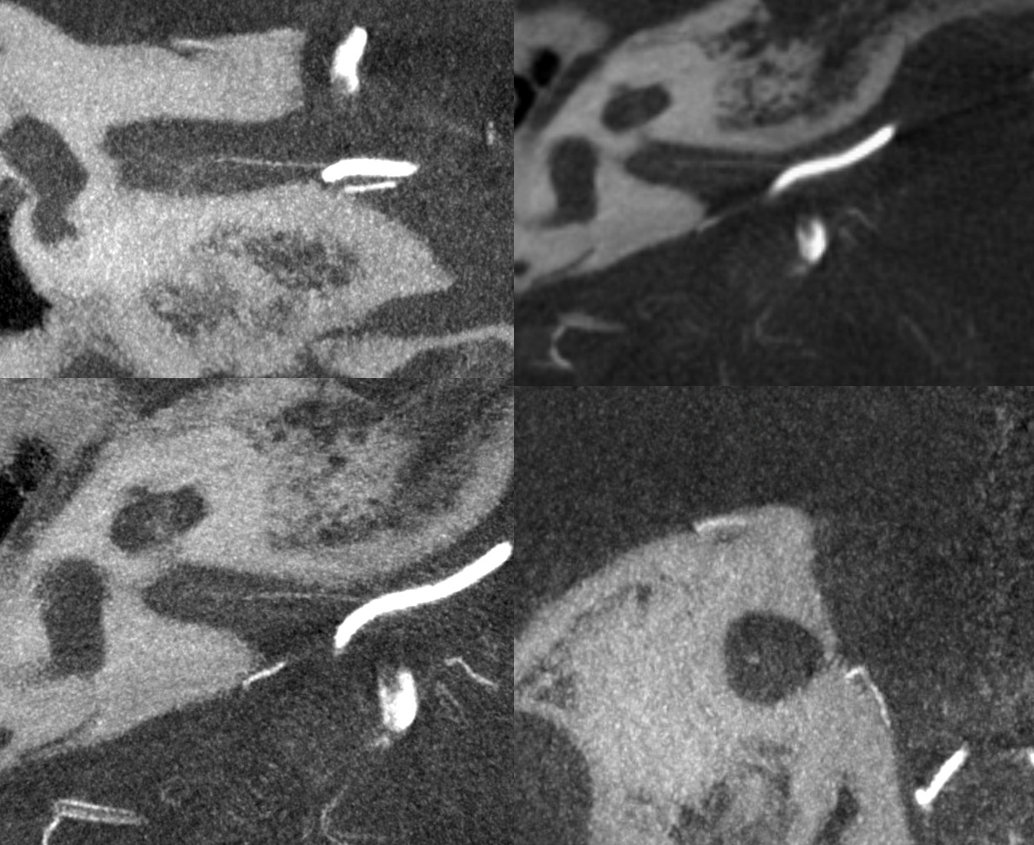
Hypoplastic AICA — what happens with that? There is the notion that labyrinthine artery may “arise” from the basilar artery directly. OK, thats one idea. That begs the question of what is AICA? How about a better idea — AICA is defined by the labyrinthine branch — whatever gives rise to that is the AICA. That’s precisely what happens when the AICA is “hypoplastic” — as in dominant PICA.
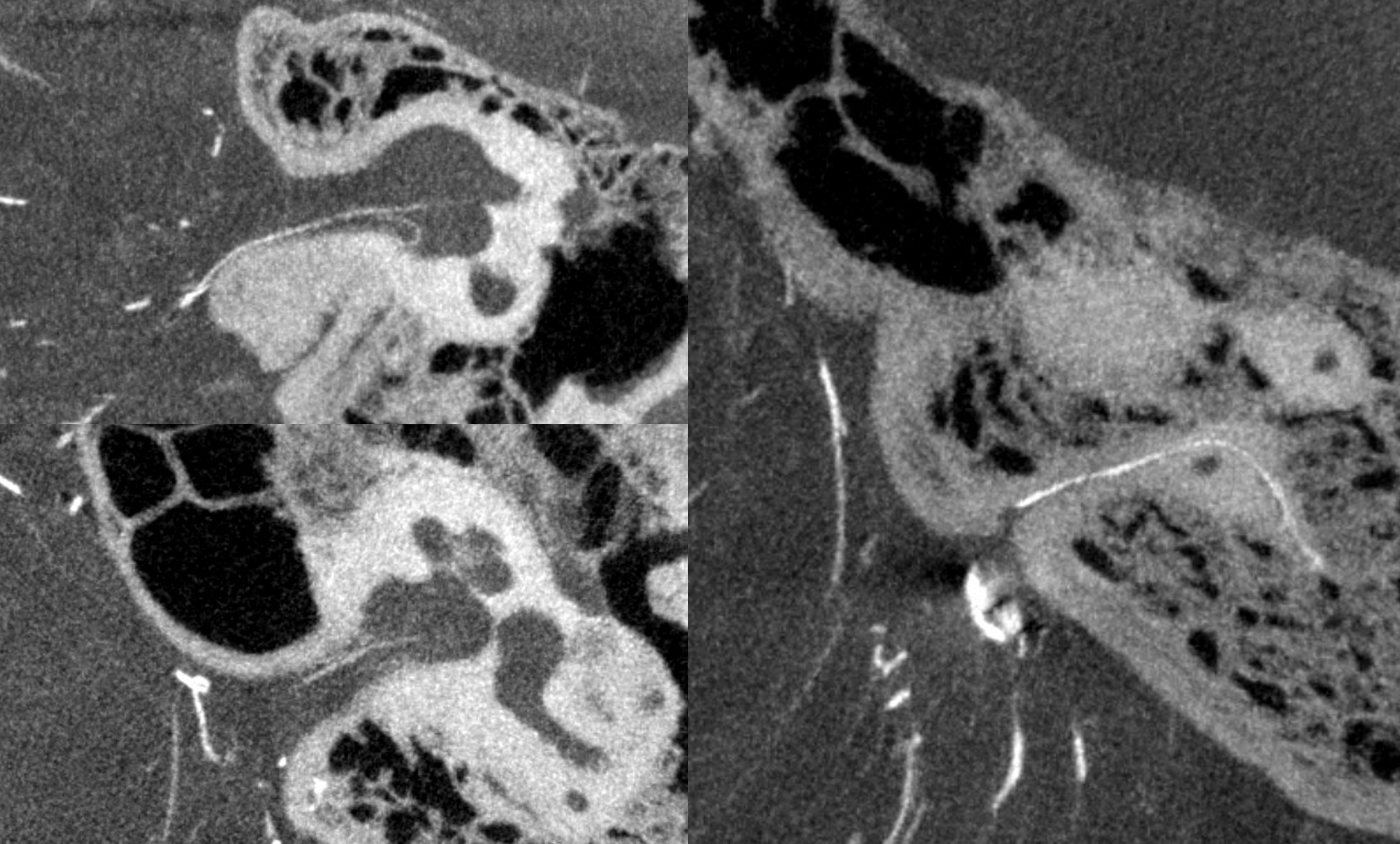
Left side — very, very “hypplastic AICA” — not identifiable on 2D-DSA at all. The open arrow points to an overlying branch of the PICA. This is not the AICA… There is no classic “AICA” at all

AICA is the one poined by solid arrows. Dashed ones are labyrinthine. Arrowheads are the subarcuate branch.
Axials
Another example of “direct AICA origin” from basilar — or more correctly the small AICA — its territory defined by labyrinthine supply — in setting of dominant PICA.
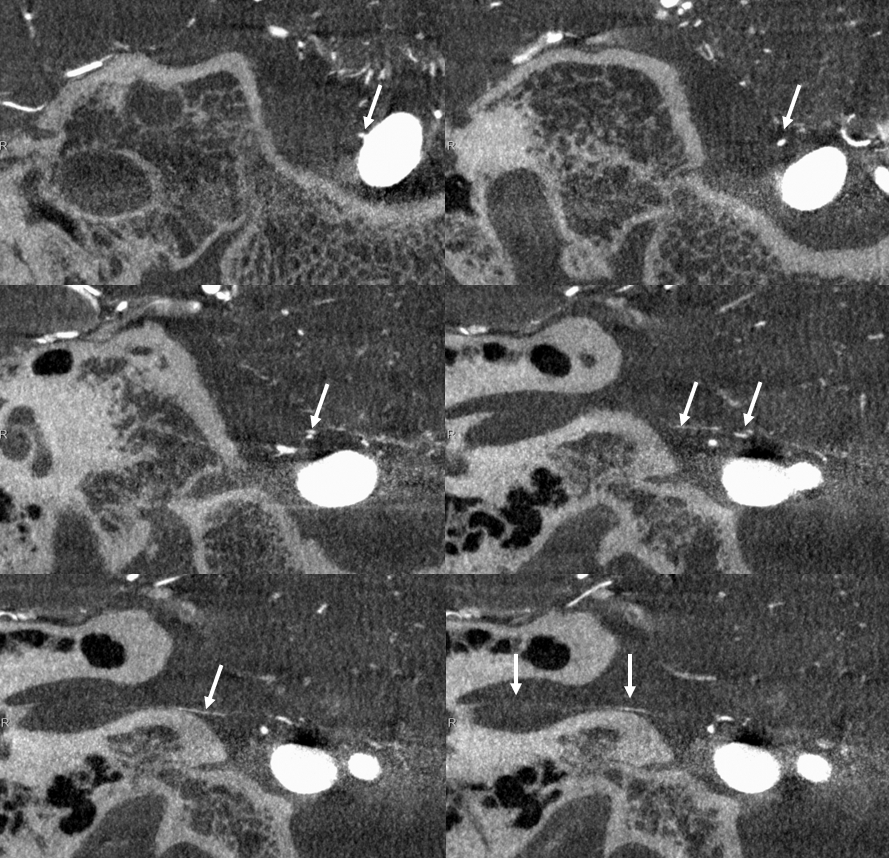
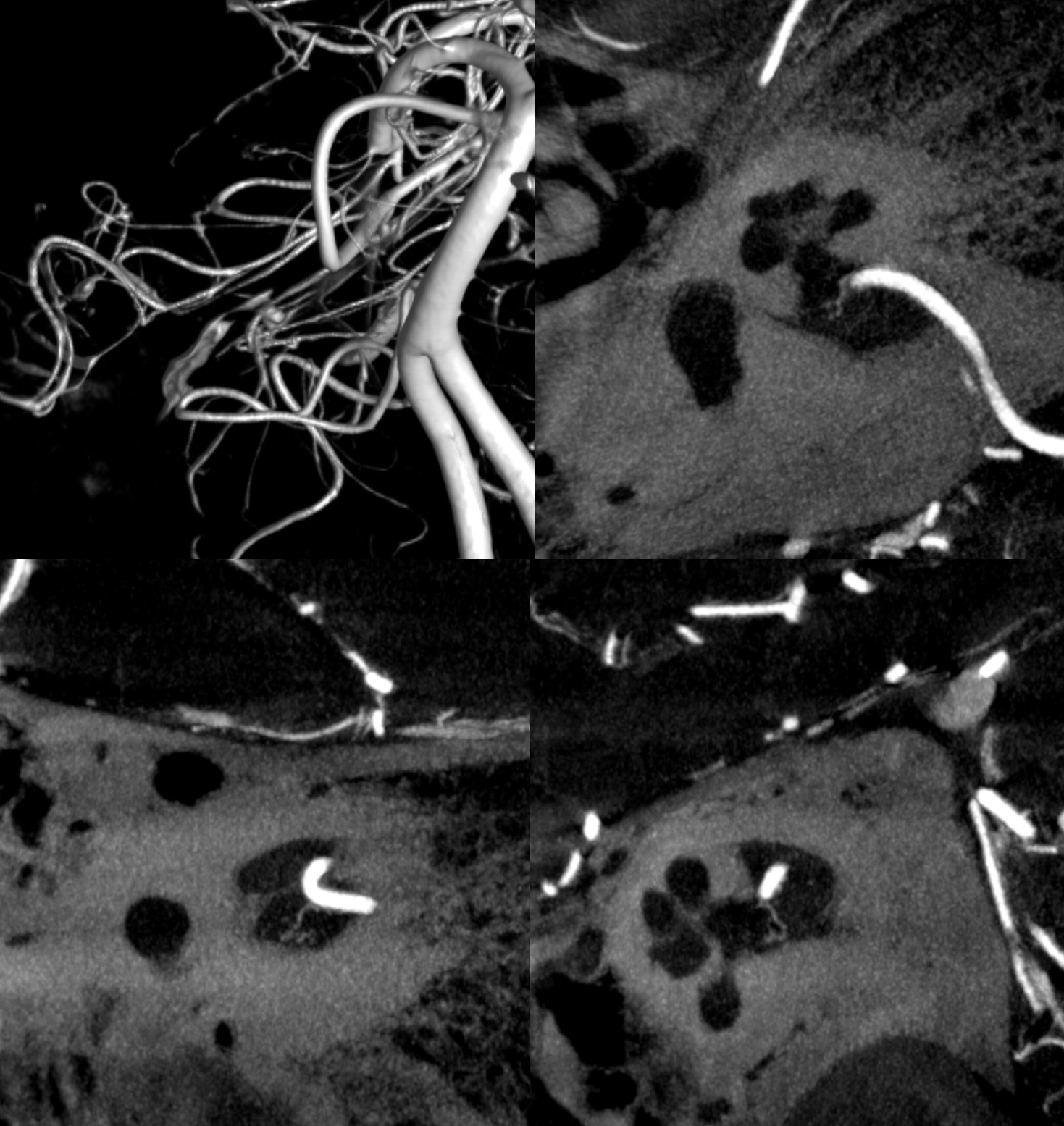
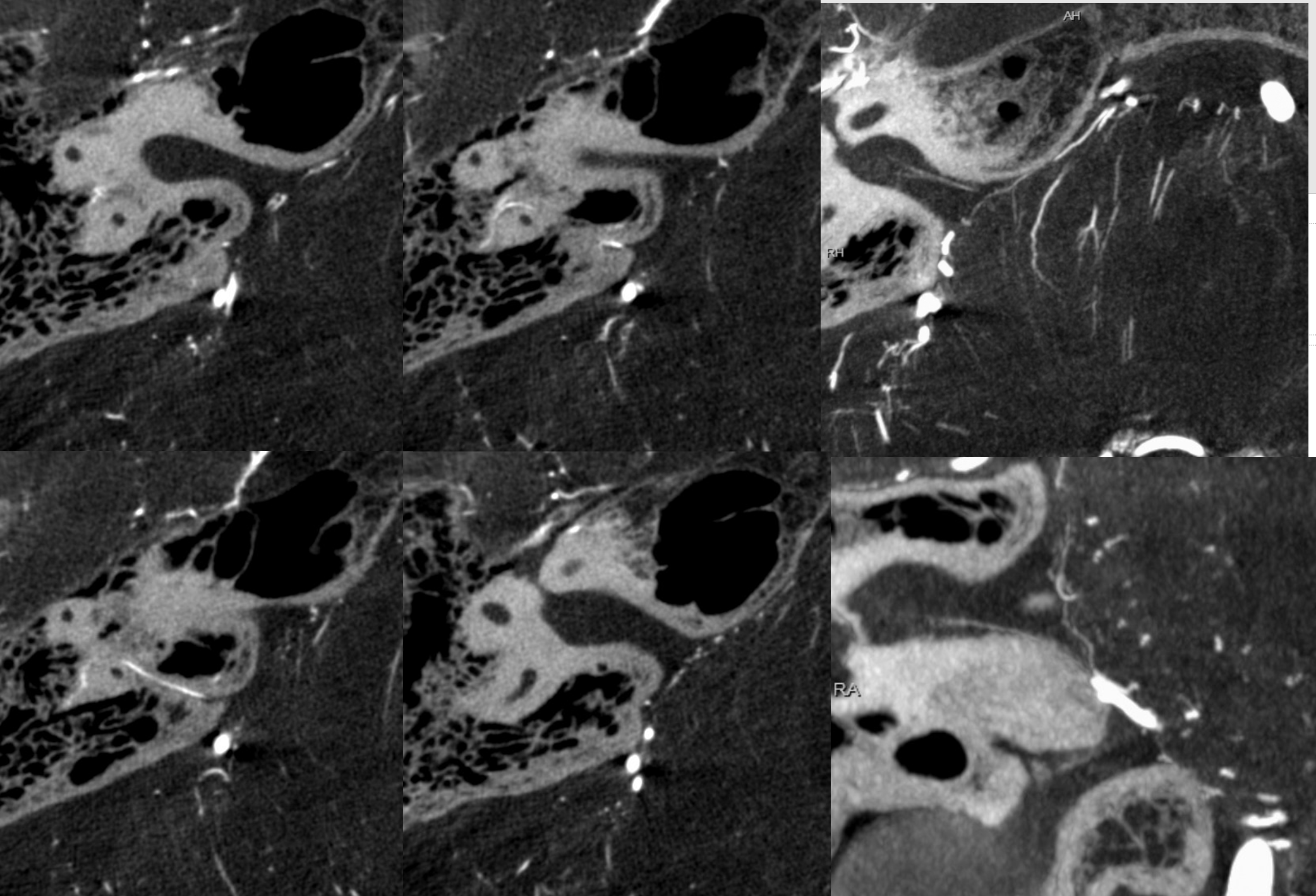
AICA Loop and The Labyrinthine Artery
That loop is forever blamed on tinnitus, dizziness, etc etc — being presented for some kind of surgical solution that pretty much is never endorsed by a reasonable surgeon. One of the dogmas being discussed is that the labyrinthine artery always comes from this loop. That’s of course usually true, and sometimes not. Here is an example the labyrinthine artery (dashed arrows) origin from proximal to a very impressive loop. Interestingly, a curious recurrent branch (arrows) does arise from the loop segment, heading back deep into the brainstem / middle cerebellar peduncle. Not what might be expected. The arcuate branch (ball arrow) also comes off proximal to the loop. Top images are without arrows. Nothing like looking…

On the left side, the same patient, all is well — origin is from loop (dashed arrows)
Clinical Significance — AICA Aneurysms
Below is CBCT visualization of the labyrinthine artery from a dedicated AICA injection by Eytan Raz. Not much can be seen on 2D-DSA…
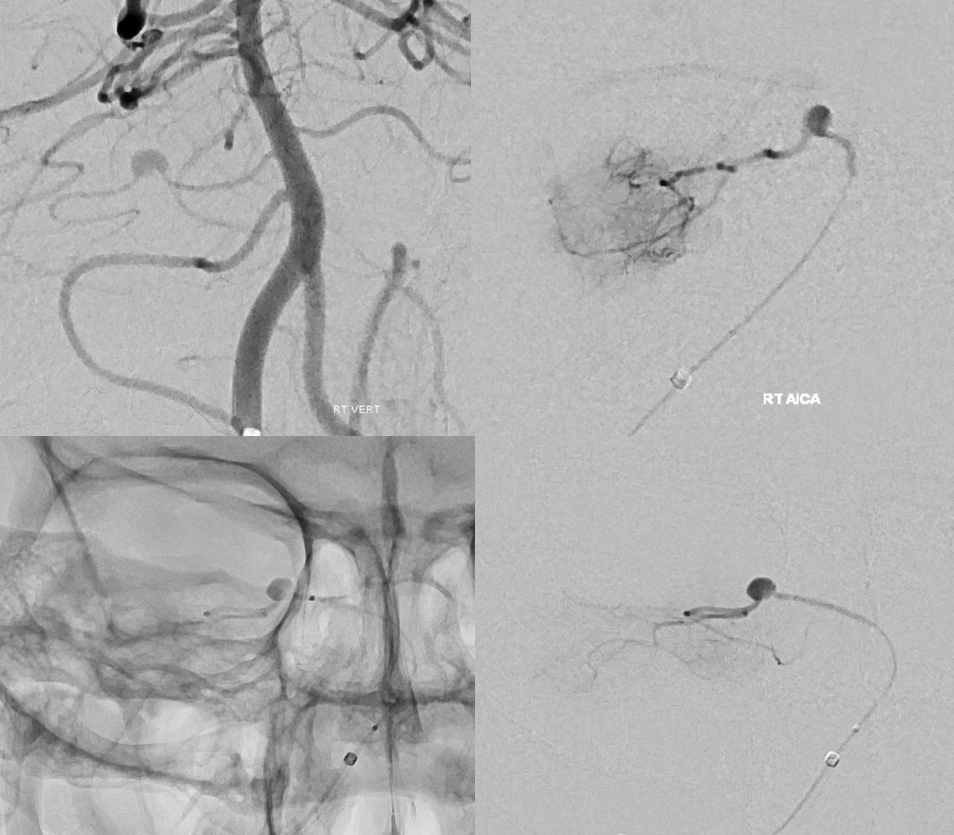
CBCT of AICA injection
Presumably, the labyrinthine artery can be seen on 7T-MRI (reference here). The question of whether this vessel could represent a larger vein rather than artery is unclear. The size of the artery on MRI would suggest that it should be readily seen on CBCT, which it is not… However, veins are well-seen on CBCT too, so questions remain.
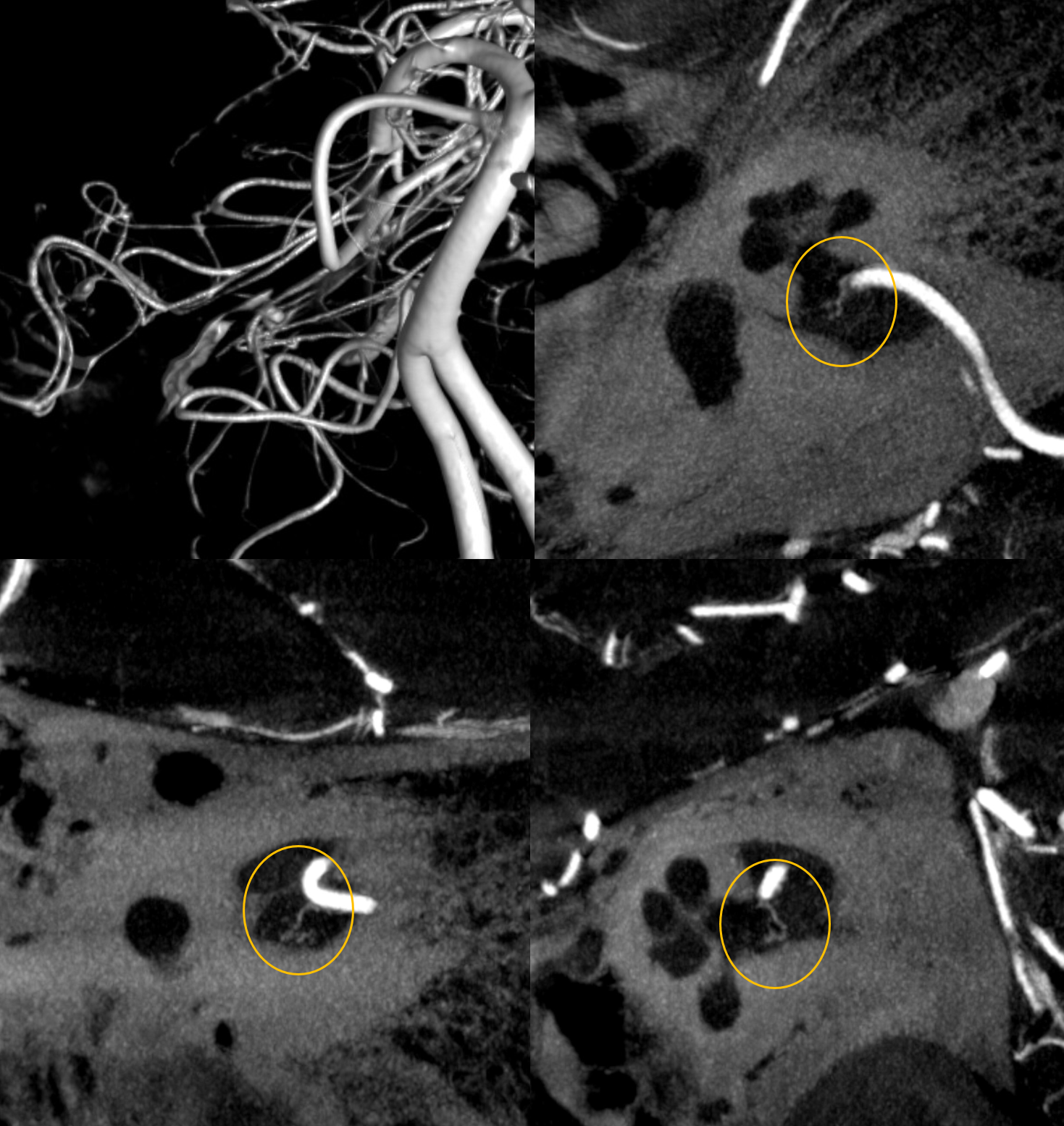
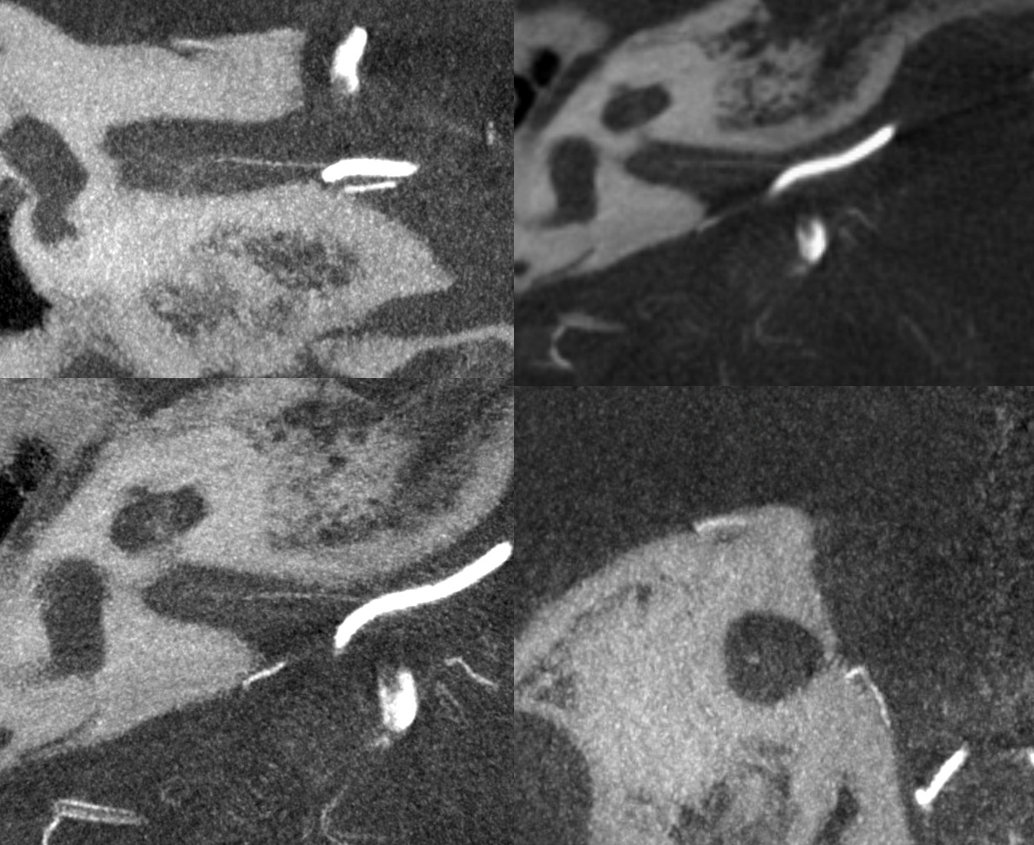
Labyrinthine Artery 2 — another excellent example — also with aneurysm. The point is that sacrifice of this aneurysm will likely leave patient deaf. On the other hand, some patients the these types of dissecting aneurysms have already lost hearing during the dissection. Some present with transient hearing imparment that recovers, presumably due to collaterals, or re-establishment of antegrade flow. Some, interestingly, loose hearing partially. We know very little about vascular deafness.
Stereo pairs below
Subarcuate Artery
Perhaps the most consistently seen “piodural” branch. Origin from AICA loop area also. In contrast to the labyrinthine artery, with which it is sometimes confused, the subarcuate artery does not supply CNVII or VIII. It is a dural or osteodural branch. Travels in the arcuate canal. Supplies adjacent dura and bone. Clinically significant, as it is pretty much always involved in supply of petrous apex dural fustulas.
This branch is not always present in surgical dissections, so prevalence is hard to estimate. On HR-CBCT it is perhaps seen in up to 25%. Usually very small. See dedicated page here.
