Case courtesy Drs. Peter Kim Nelson and Eytan Raz
 Prior cases 1, 2, and 3 showed relatively simple superselective embolizations. This one is a very long case, and equally instructive.
Prior cases 1, 2, and 3 showed relatively simple superselective embolizations. This one is a very long case, and equally instructive.
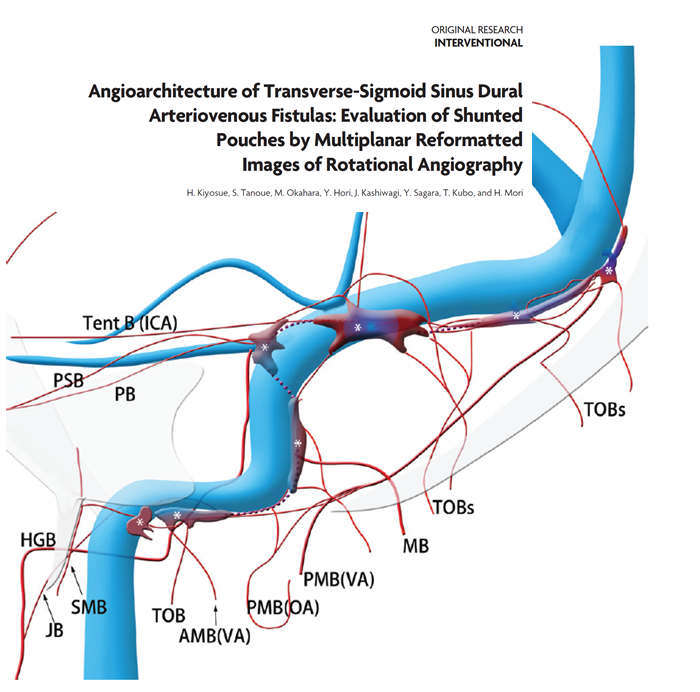
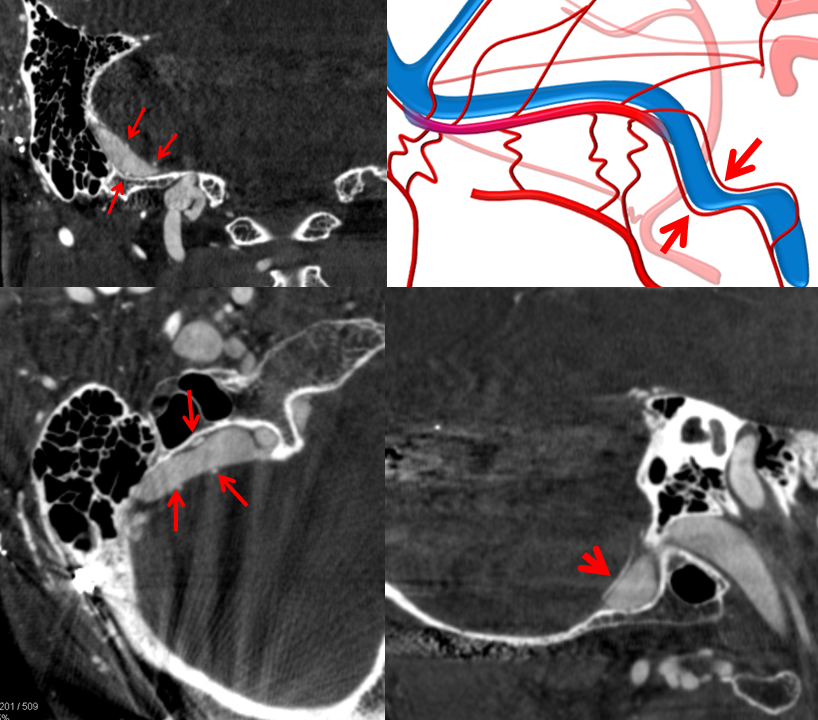
The principle is the same — arteries in walls of dural sinuses play key role in supply of dural fistulas. These arteries (artery of sigmoid, transverse, superior sagittal sinuses for example) form a network along sinus walls. See Meningeal Arteries page for more info.
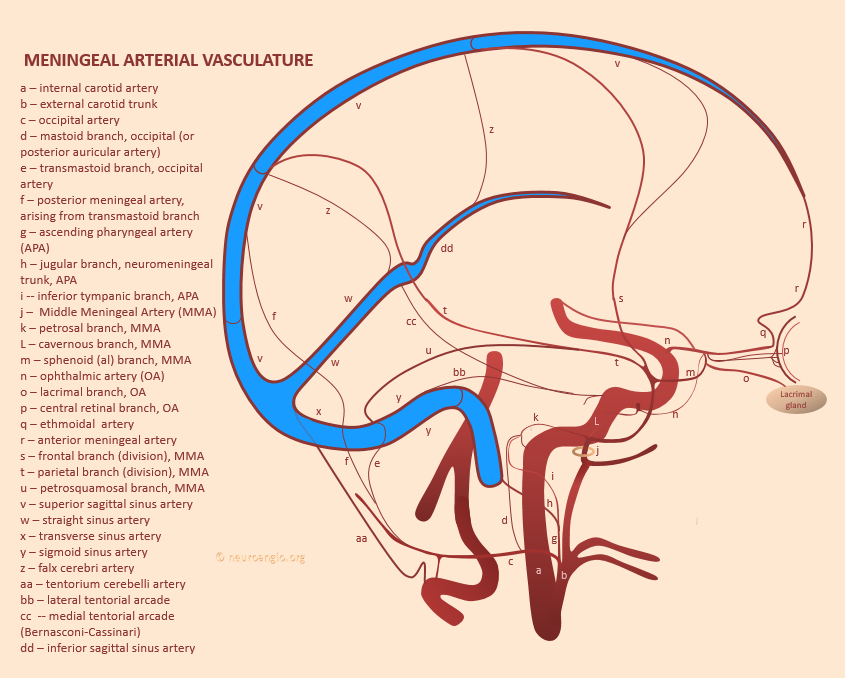
Here is another view of this idea
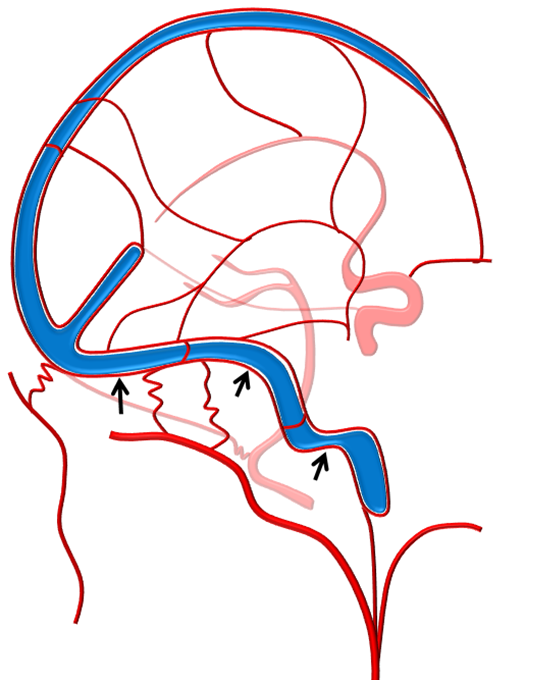
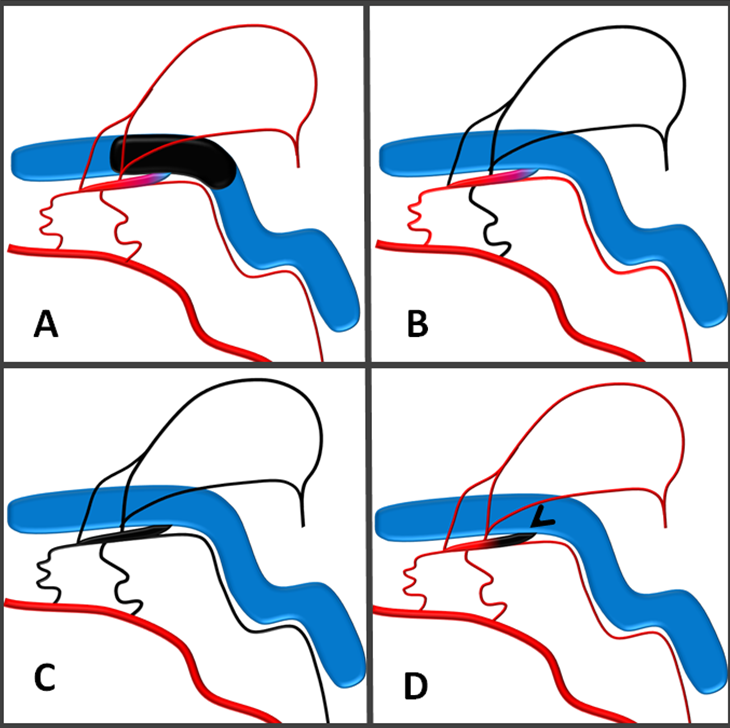
A simple dural fistula often consists of a channel in the sinus wall (red arrow), onto which myriad occipital, MMA, ascending pharyngeal, MHT etc feeders converge. This common channel communicates with the sinus proper in a single location (black arrow).
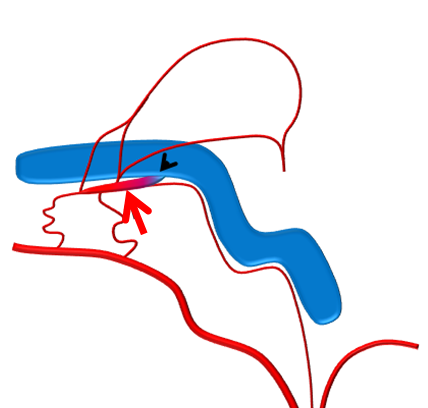
A more complex fistula looks something like this, with several openings of this common channel into the sinus proper
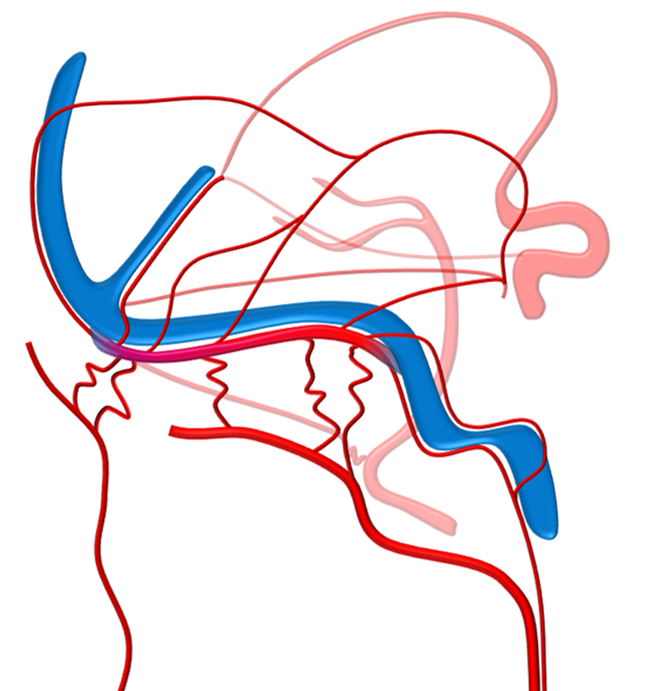
Once this is recognized, superselective treatment with preservation of the sinus proper by closing the channel is possible (D), avoiding unnecessary sinus sacrifice (A), and without the small but real hazards of transarterial embolization (B, C). The main hazard of transarterial approach being incomplete embolization (B)
Here is a complex case which absolutely required superselective embolization.
The existence of common channel in sinus wall was first reported by Mironov. More complex fistulas consisting of “shunted pouches” — a similar idea — was reported by Kiyosue, Mori et al.
Below is a complex example of a case that absolutely required superselective embolization.
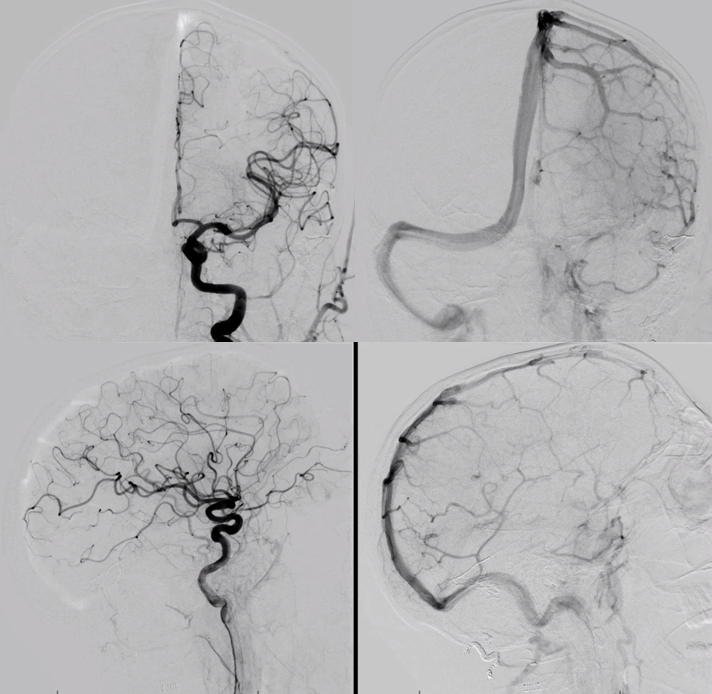
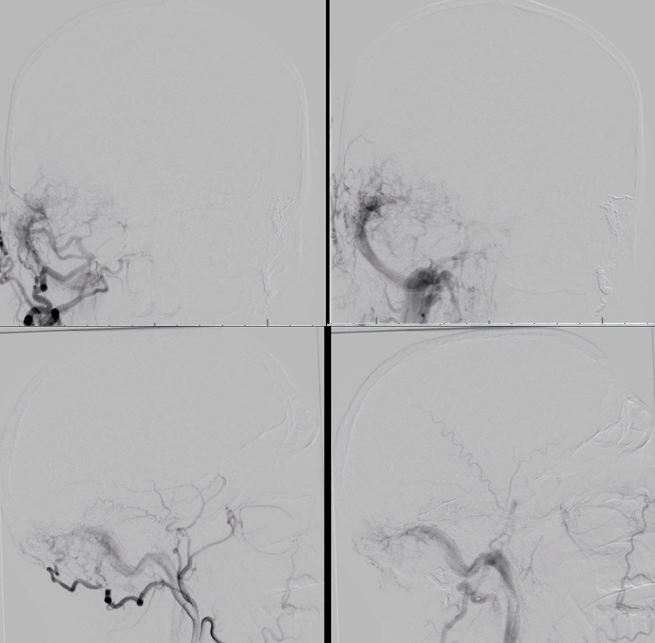
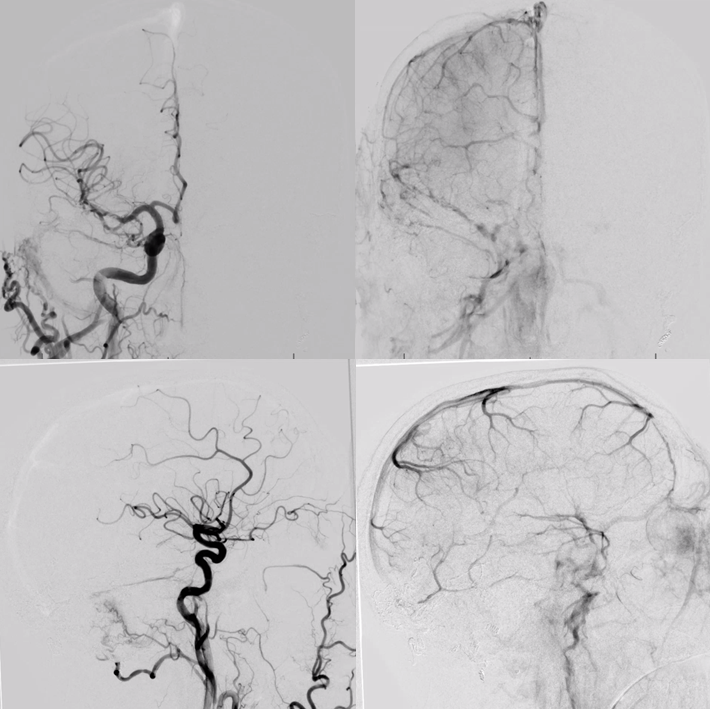
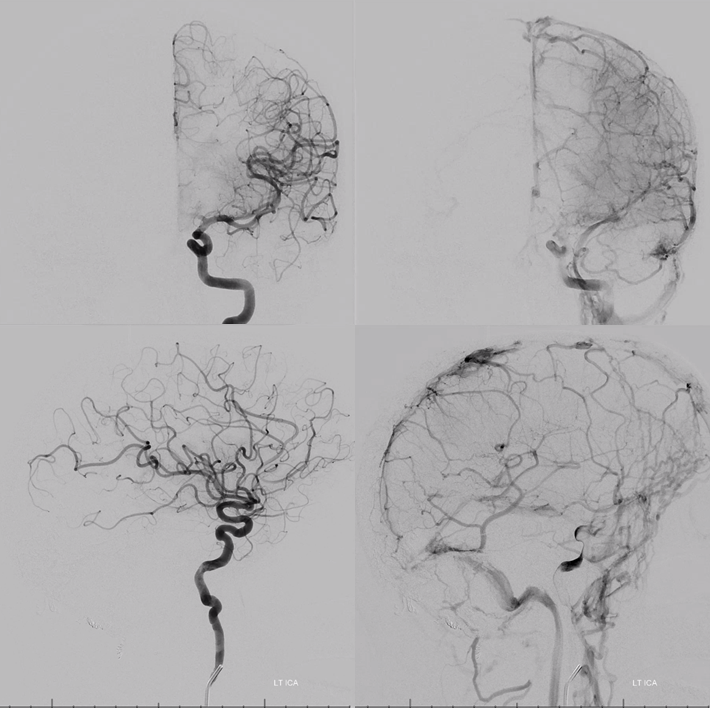
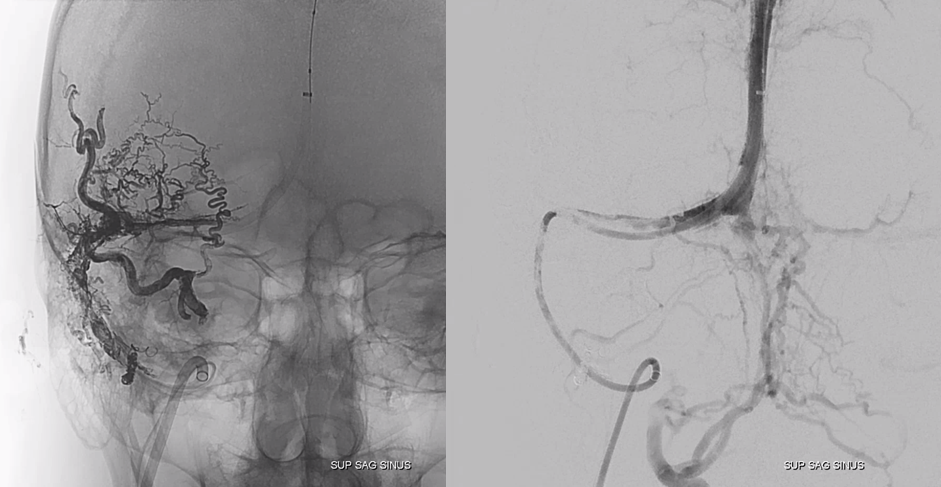
A left sigmoid high grade dural fistula
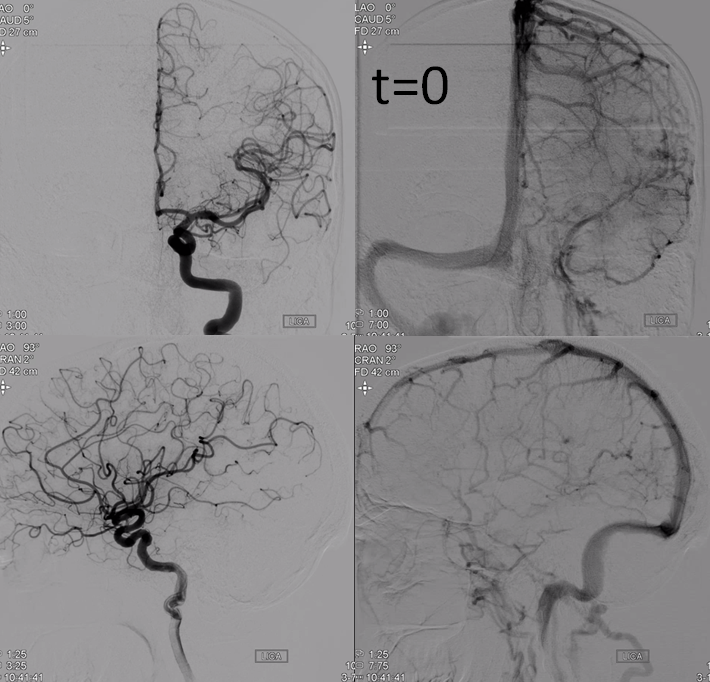
Trapped sigmoid sinus with cortical reflux
Distal external views
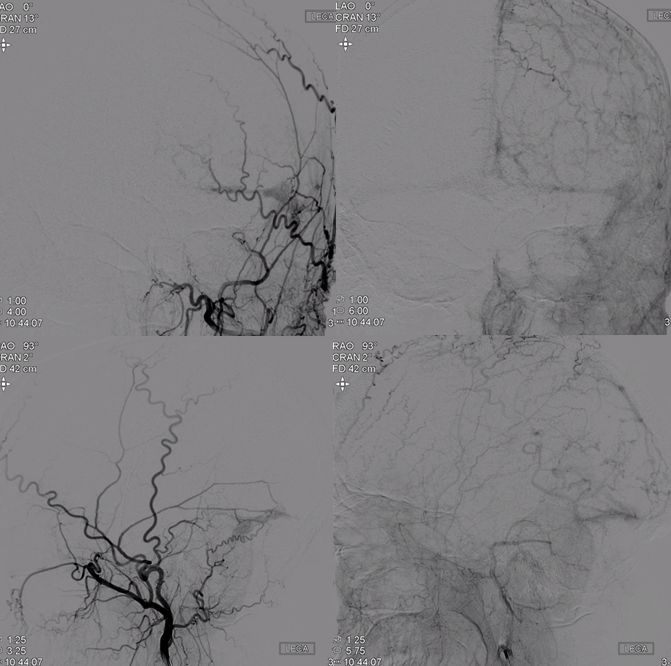
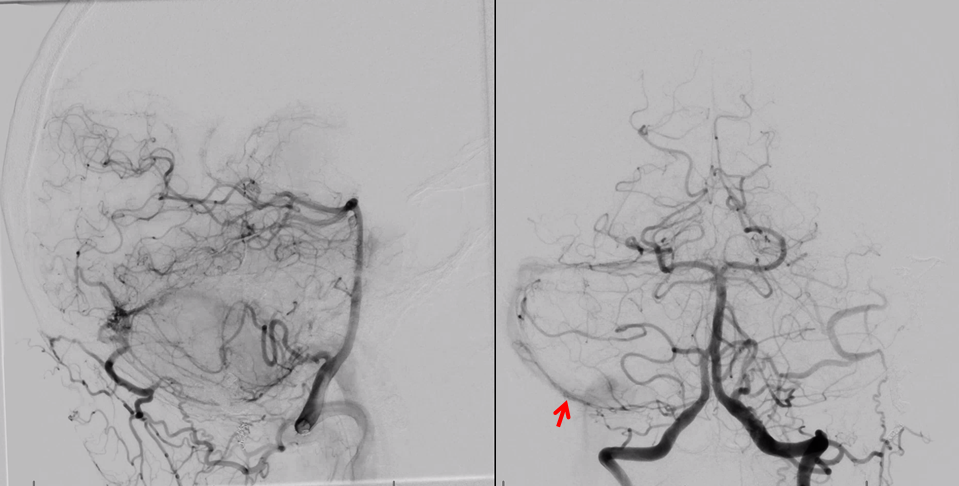
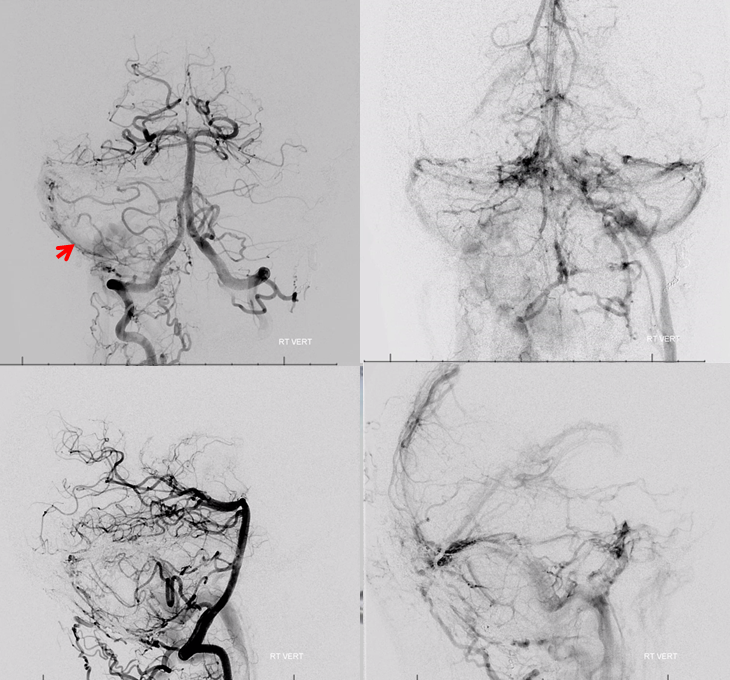
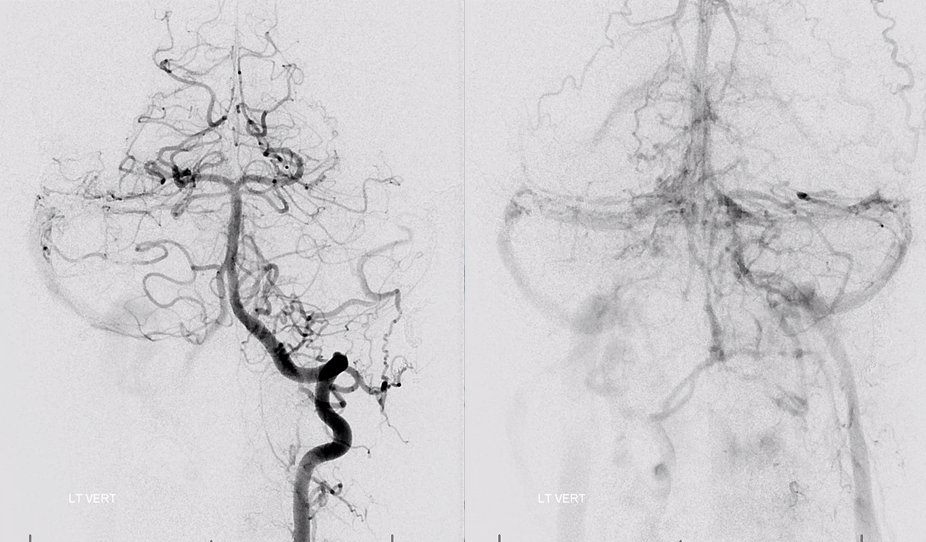
Vert shows the almost ubiquitous proximal sigmoid sinus artery (red arrow, normally branch of the ascending pharyngeal jugular division) and venous congestion with rerouting of cerebellar drainage into the anterior (petrosal) group (see Posterior Fossa Veins for more info)
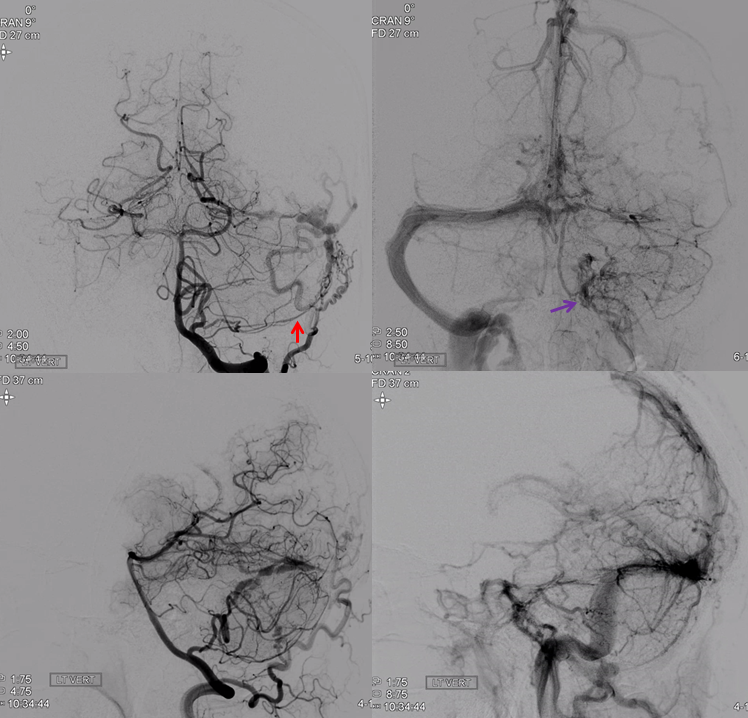
1 month later patient presents for embolization. More congestion
Usual transarterial treatment is performed, first by a proximal occipital attempt and then by a more successful penetration of the fistula into the sinus from the MMA. The fistula is cured.
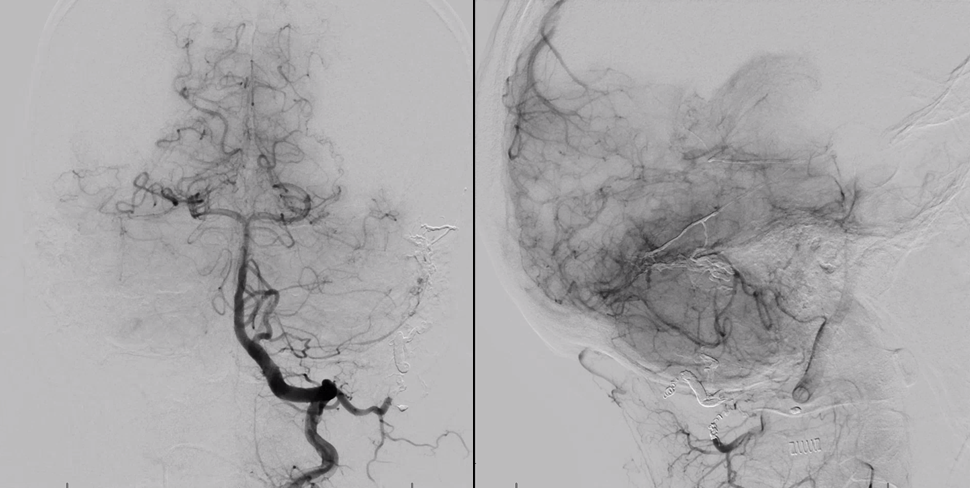
Six months later, something very interesting and very good happens — the proximal left sigmoid sinus has recanalized and is now draining the Labbe
Unfortunately, there is a new right sigmoid sinus fistula. The brain is also using the right transverse / sigmoid sinuses (see above)
Vert injection shows, again, artery of the sigmoid sinus (red arrow), now on left
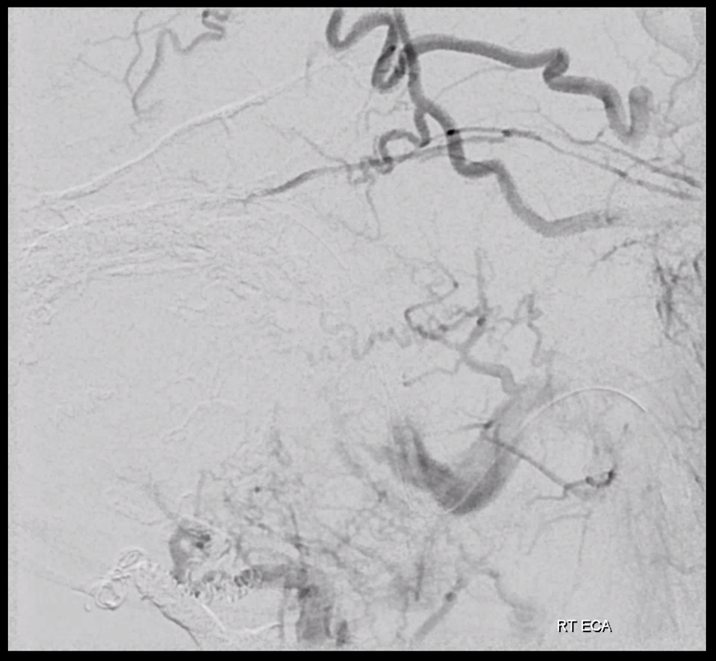
Superselective injection to show MMA supply, including proximal petrous branches that often supply CN VII
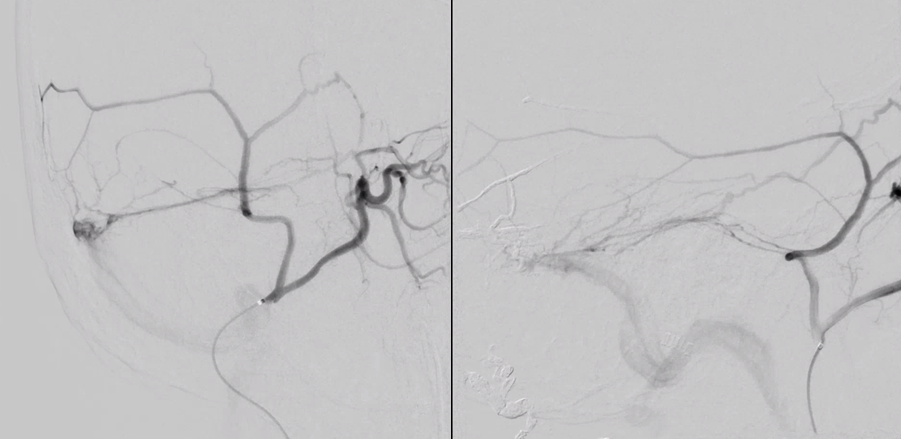
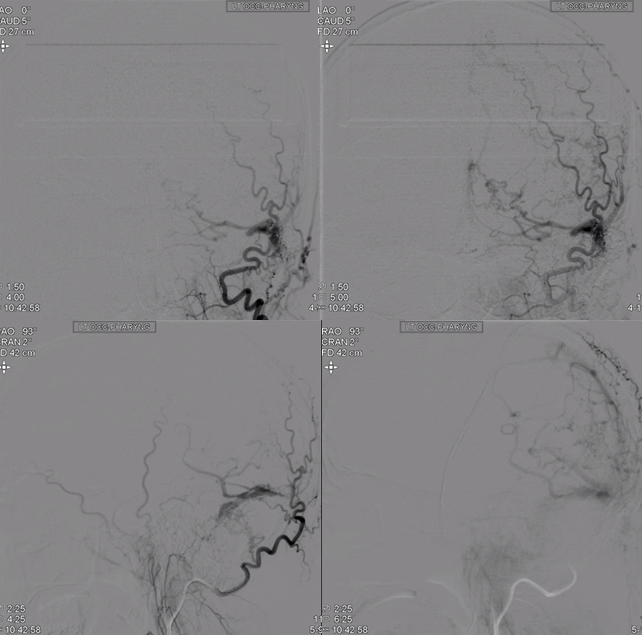
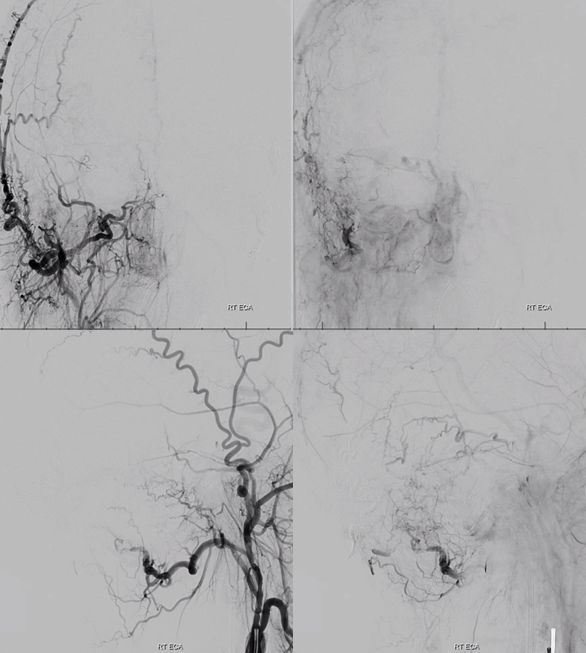
What to do now? Again, transarterial embolization. See all that Onyx on the right? Most of it is nowhere near the fistula. Fairly safe when you are in distal occipital and petrosquamosal MMA, but still unnecessary.
And also insufficient. The two disadvantages of transarterial embo are arterial complications (cranial nerve palsy, stroke) and incomplete embolization. It is frequently not easy to close the fistula hole or holes this way, even for experienced operators. This fistula is still alive. Supply now comes mainly from the jugular division of the ascending pharyngeal (lower left image). Wisely, the operator stops and does not endanger CN IX, X, and XI
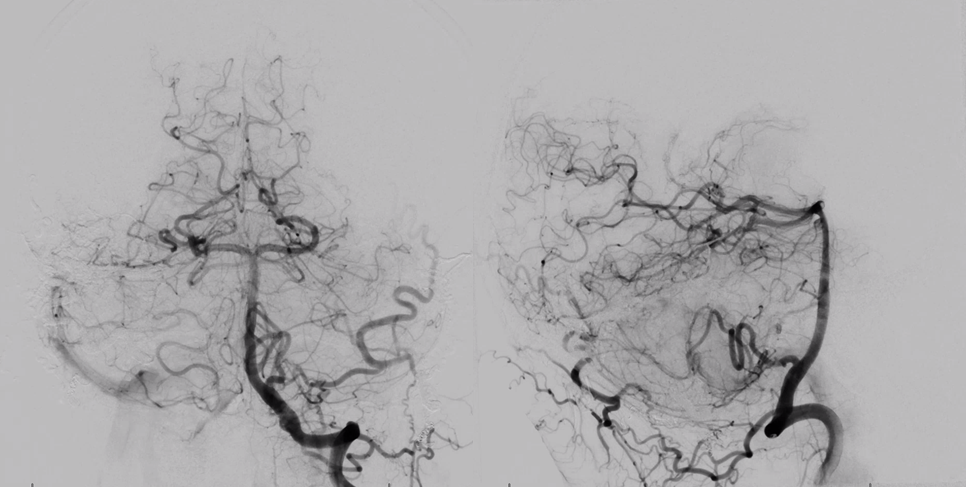
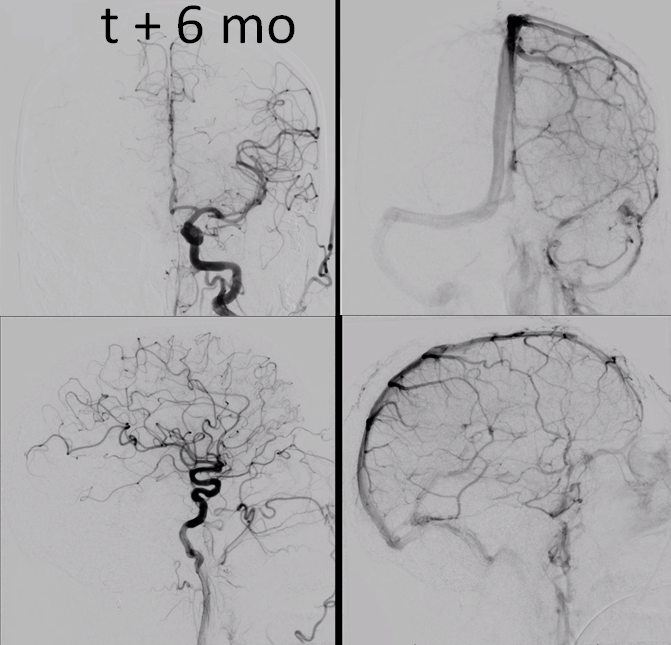
What now? Wait, of course. Sometimes, wait works and fistula closes spontaneously. Unfortunately, this one does not. Five months later
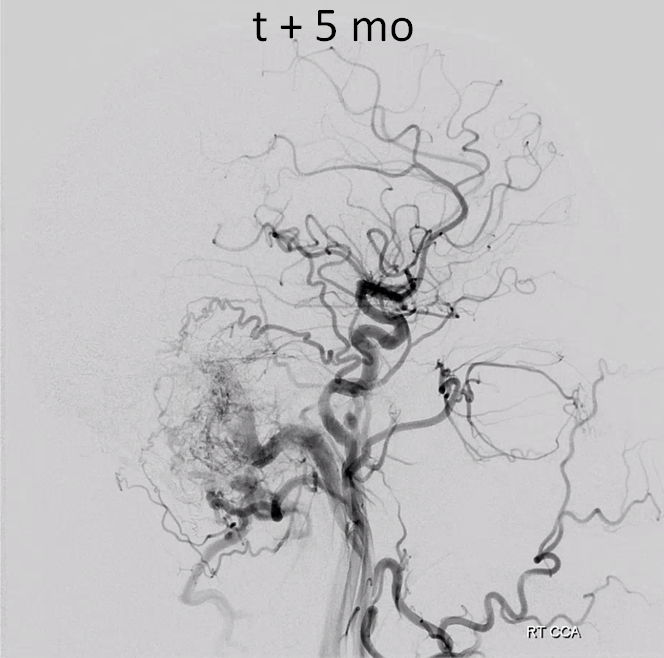
What to do? Sinus sacrifice is a very bad option. More transarterial does not seem promising at all. Here, the key is a good diagnostic angiogram to understand what options are.
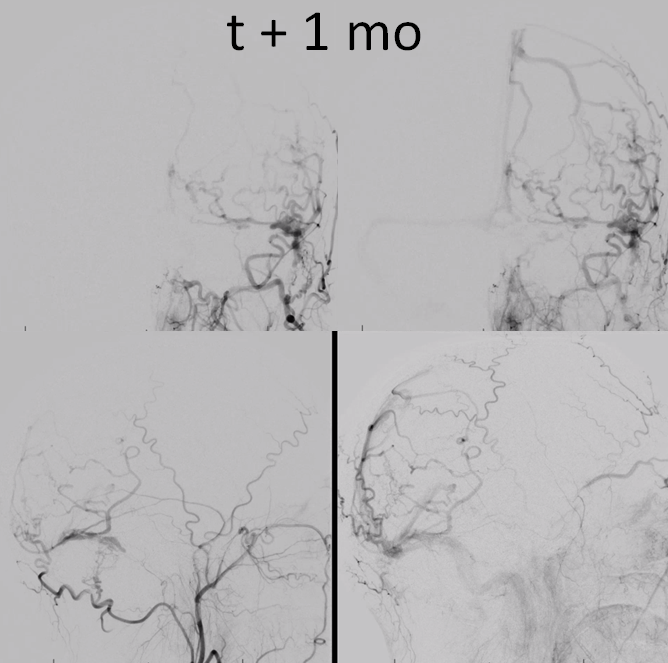
The brain is still using the right sinus
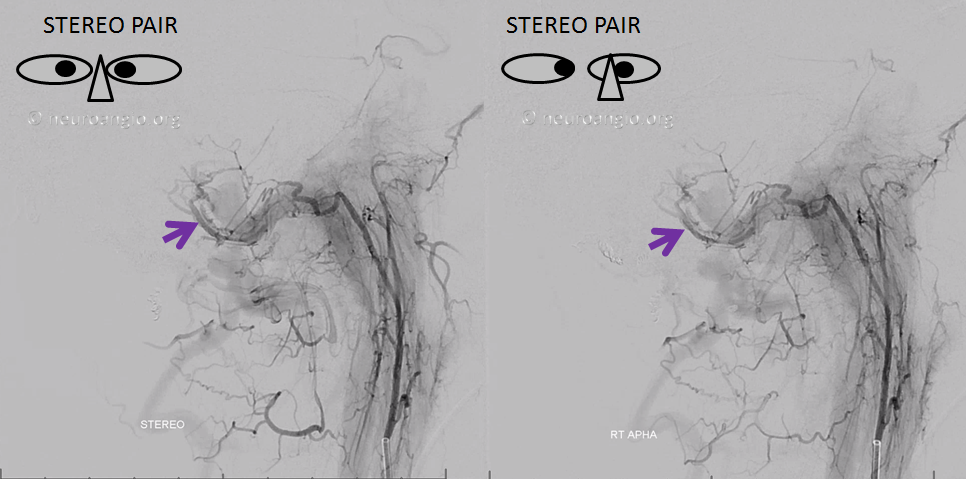
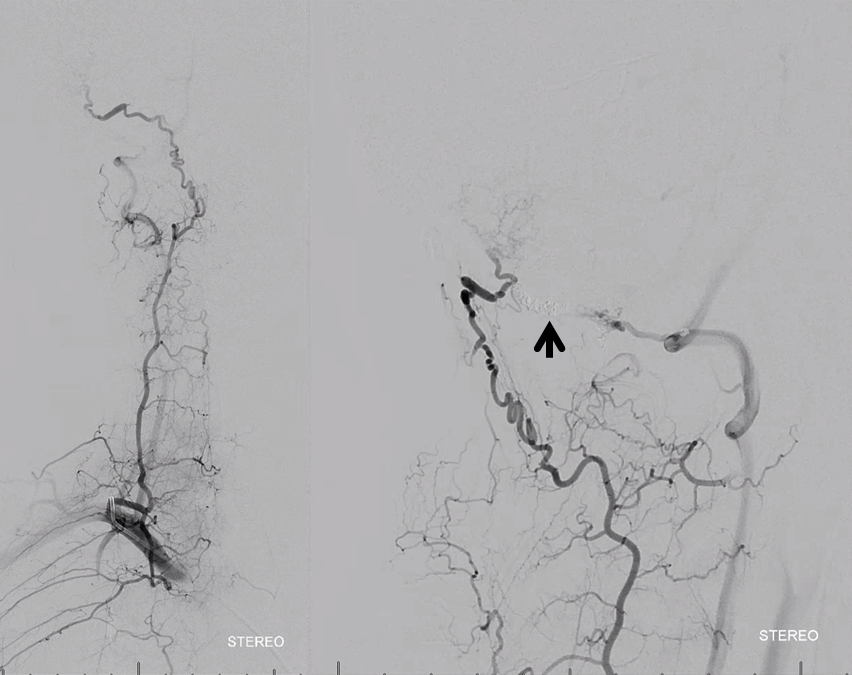
Occipital injections start to suggest a strategy. See the pouches marked by purple arrows. Those are in the wall, outside of sinus proper
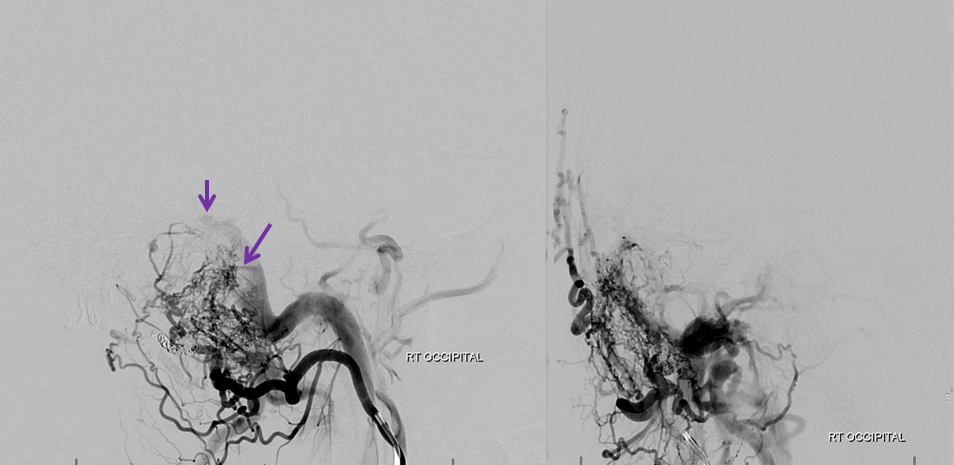
Distal ECA injection also looks promising. Most pouches are below the sinus, just like this one.
How can we resist getting a stereo view?
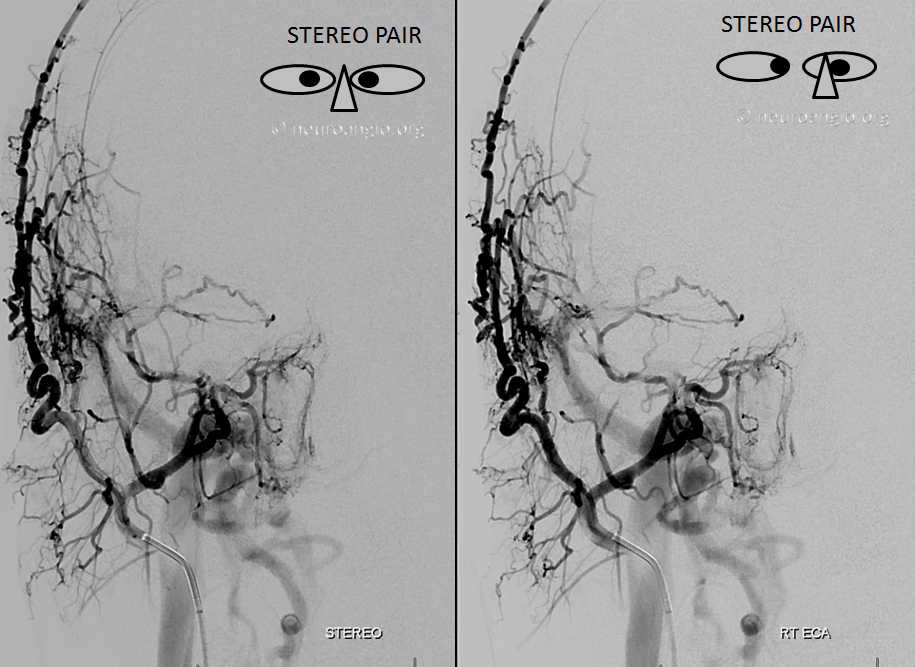
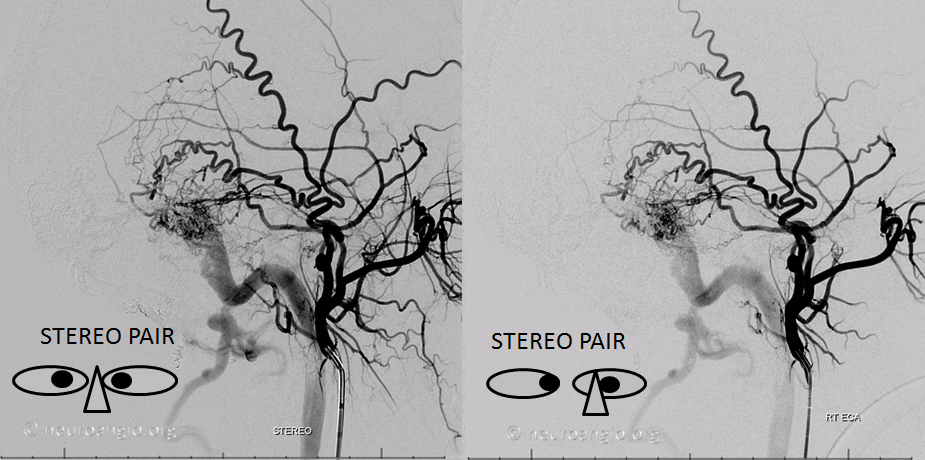
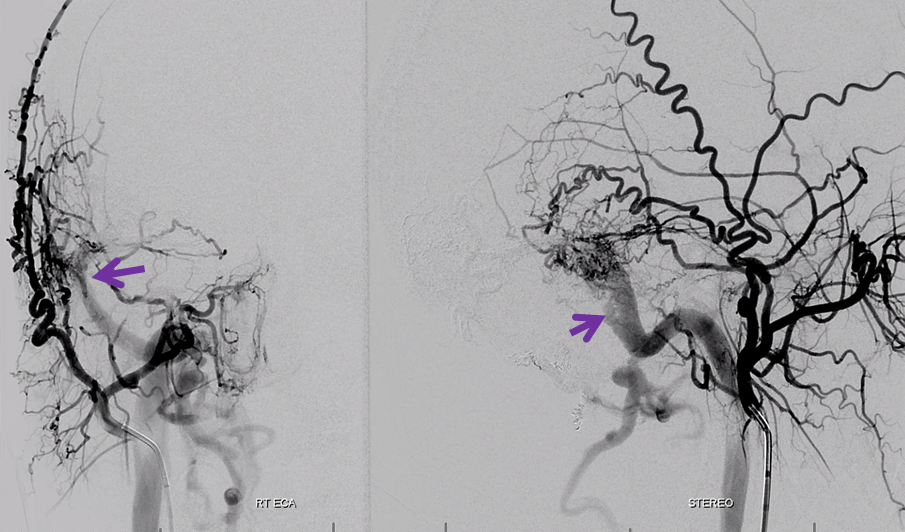
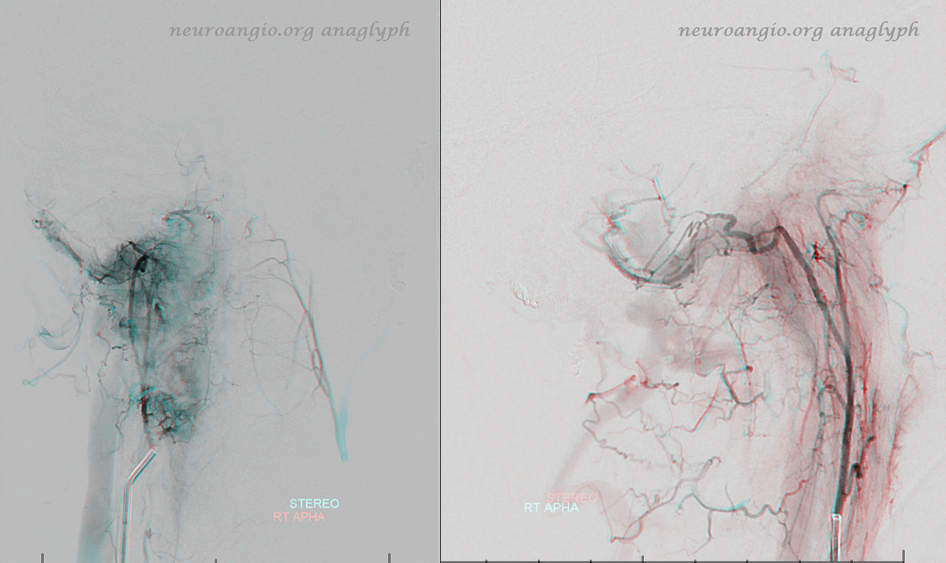
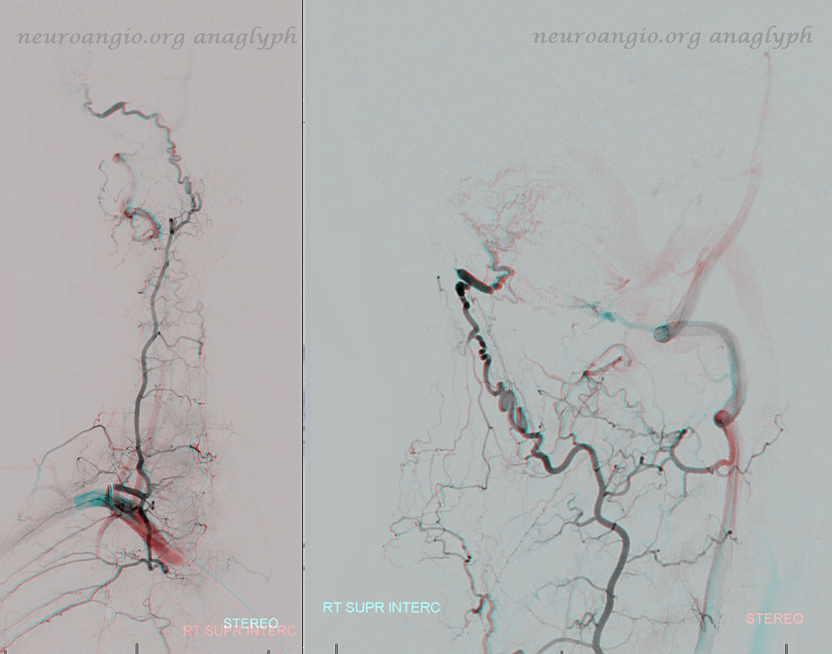
Very helpful stereos. With all that prior Onyx around, DYNA CT is not going to be pretty. Ascending pharyngeal jugular division is alive and well, supplying a more proximal sigmoid pouch (purple)
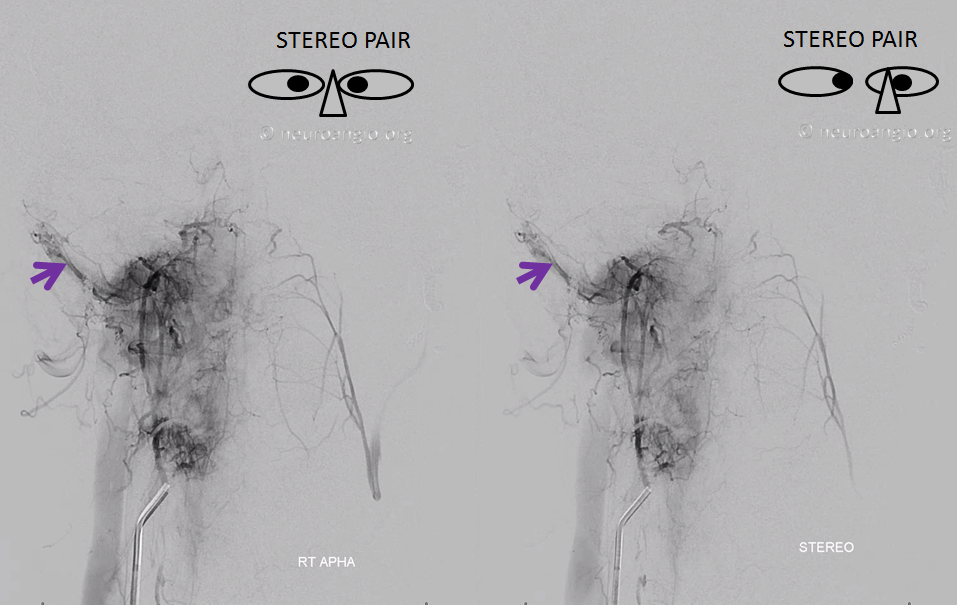

Anaglyph stereos. Get those red-cyan glasses here. See more anaglyphs here
Deep cervical injection shows reconstitution of distal occipital territory post prior proximal coil occlusion (black arrow). Another demonstration of proximal embolization futility, and a beautiful connection to the supreme intercostal system supplying the upper intercostal arteries.
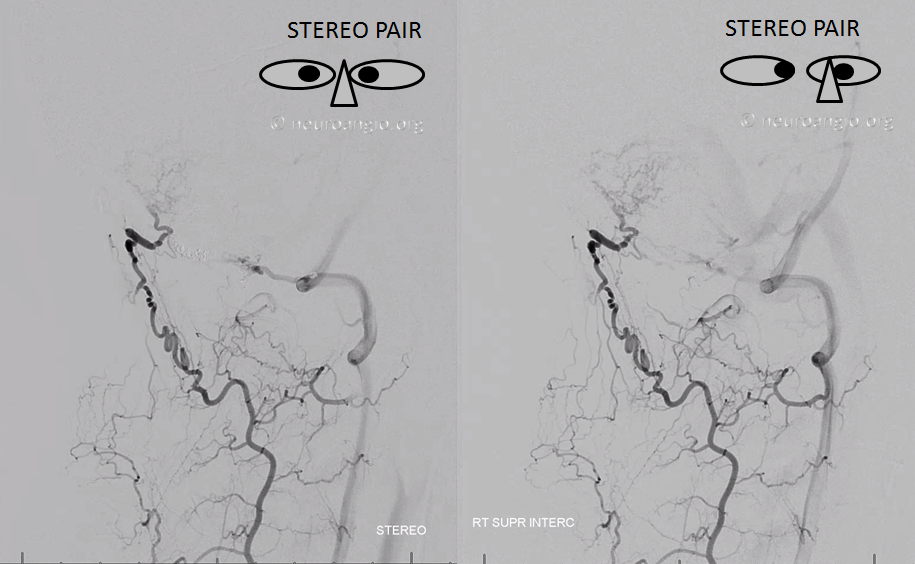
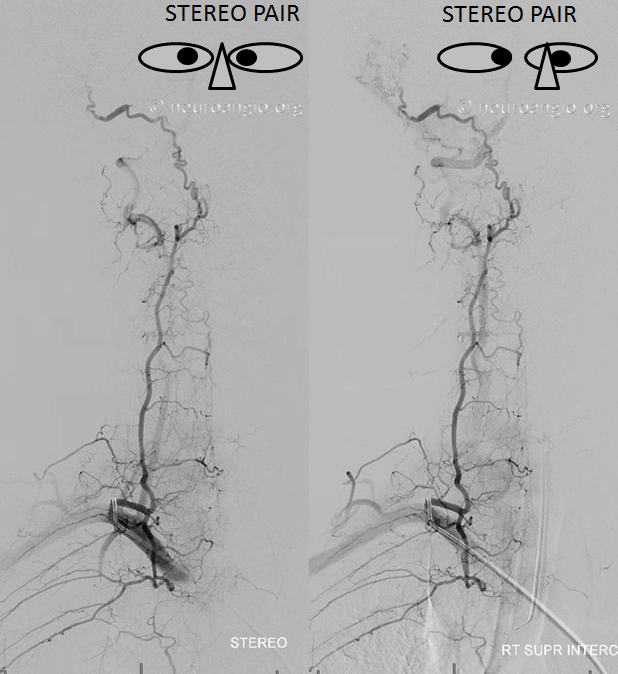
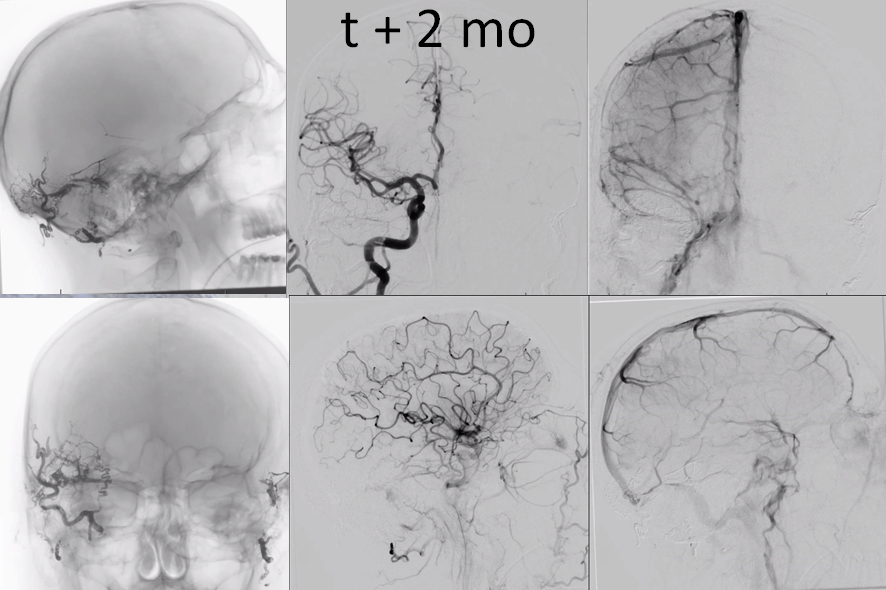
Now back to business. Left sigmoid sinus still open. great.
Posterior fossa also needs the right sinus.
So, in summary… Look at how nearly identical these images are, both theory and practice in perfect agreement. What’s not to like?
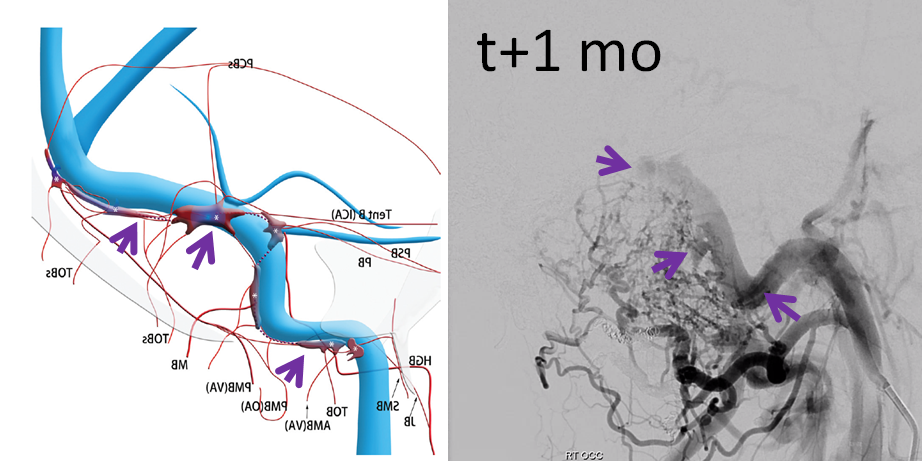
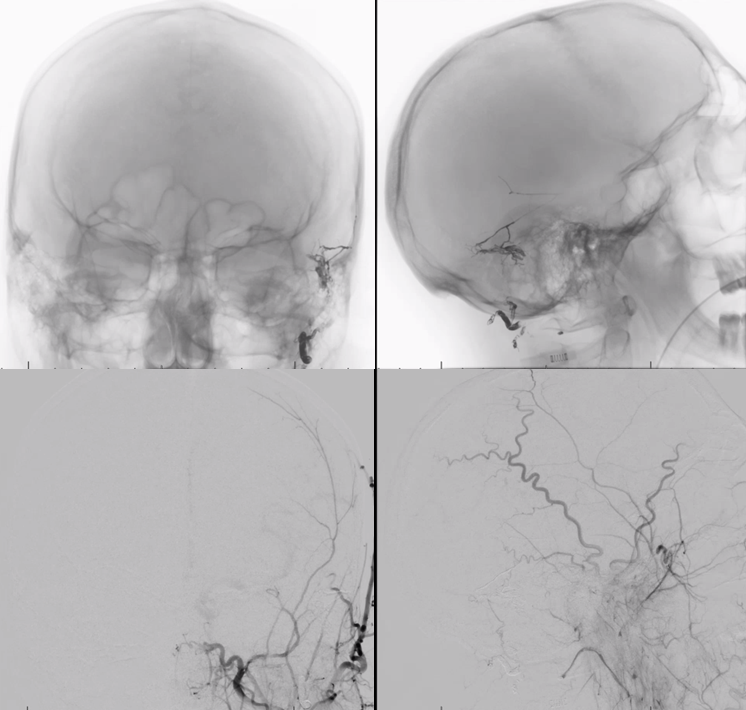
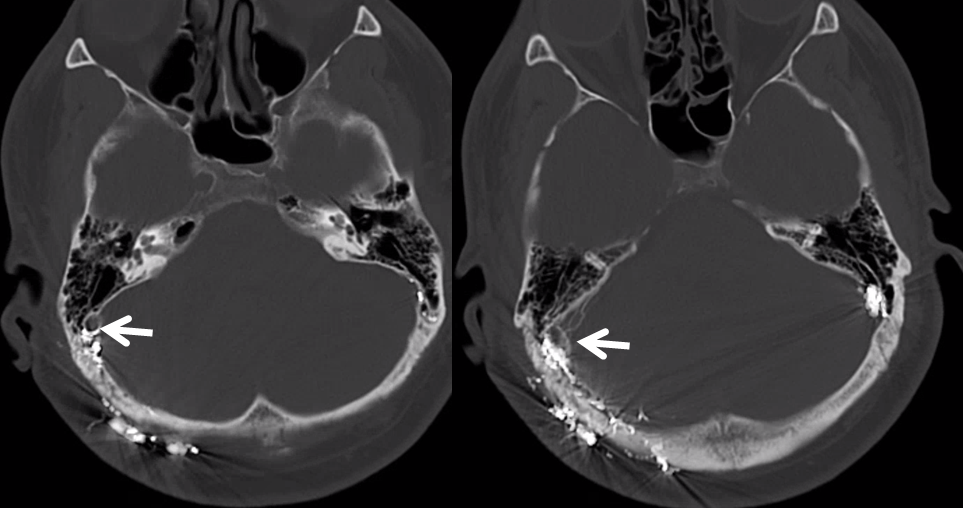
Dyna CT is significantly affected by Onyx, but we can still see the proximal-most pouch near the bulb (below)
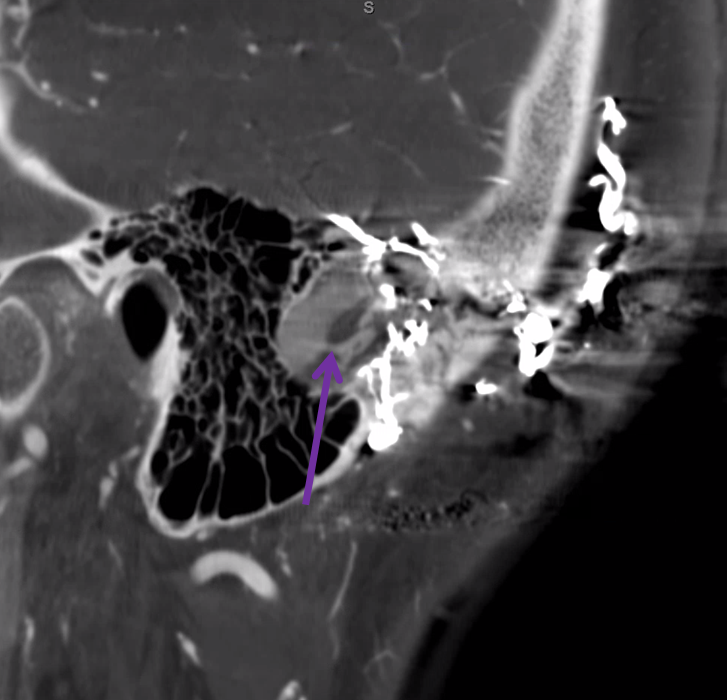
Again, look at how perfectly these images agree with each other
Here is a DICOM scroll of the same. Not good to see the pouches because of too much Onyx. But very good to see jugular division ascending pharyngeal branches in jugular foramen and in the sigmoid sinus wall. Also notice Onyx material in the sinus wall from prior Occipital injections towards the top.
Finally, we are ready for treatment. It takes a lot of diagnostic work to know what to do. Without good diagnostic angiography, superselective treatment is not possible.
So, how does superselective transvenous embo work? The idea is to get into the sinus wall channel, or channels, from the venous side, and close them, while sparing the sinus. For a simple fistula, like cases 1, 2, and 3 , a single microcatheter and some coils or Onyx is ok. Here, it takes more.
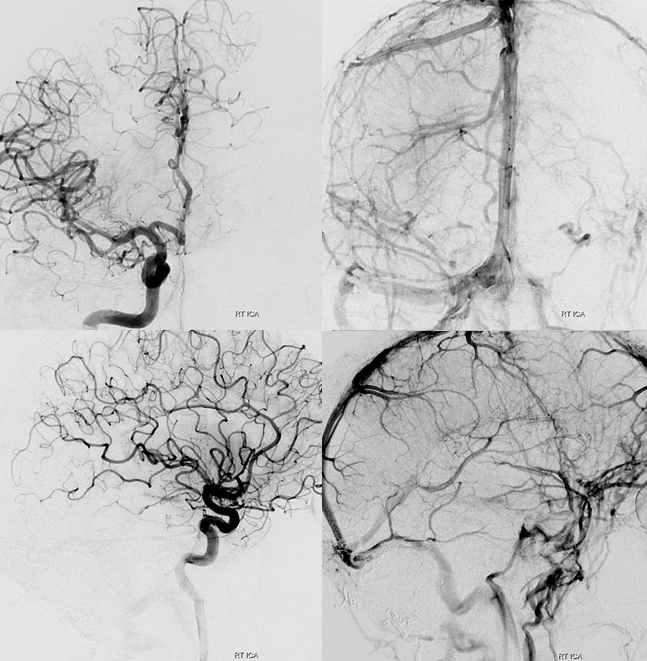
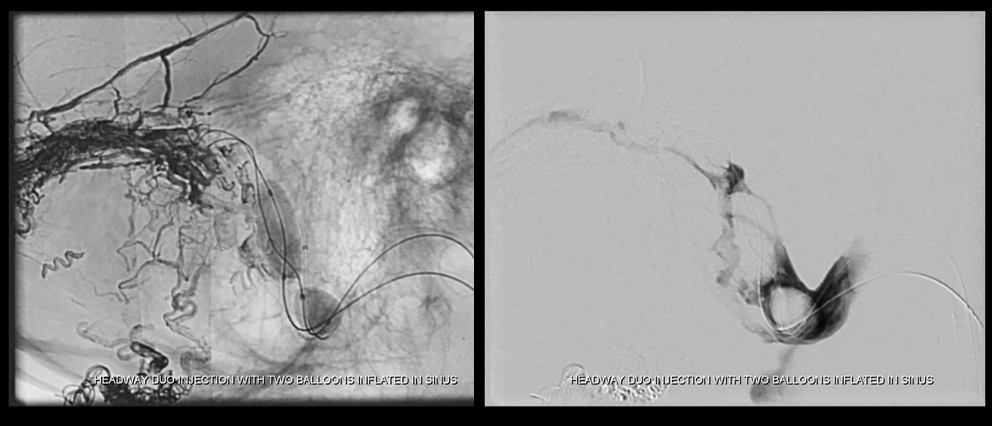
Setup: Two NeuronMax in the right IJ
Two 7×15 Transform balloons in the sigmoid sinus for protection (we don’t have Copernic balloons here)
Two microcatheters to access two separate sinus wall channels, one proximal, one distal. In this case, one catheter was a Scepter C, another was a headway duo.
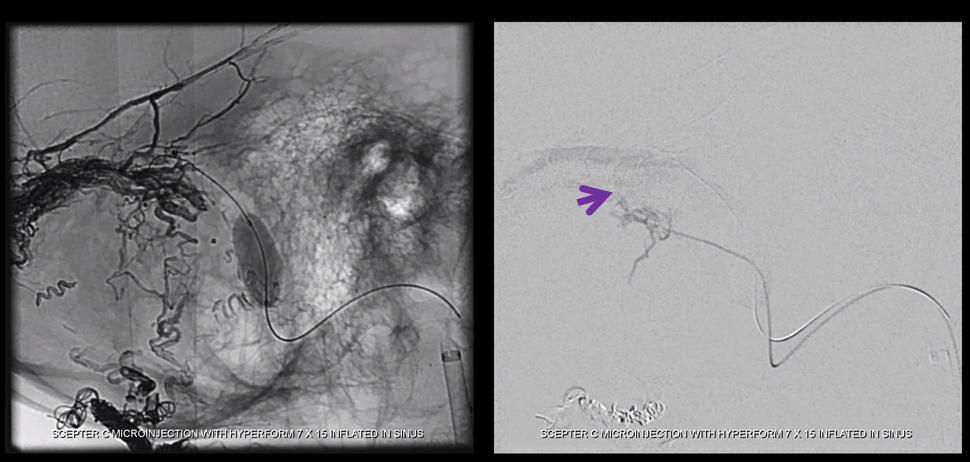
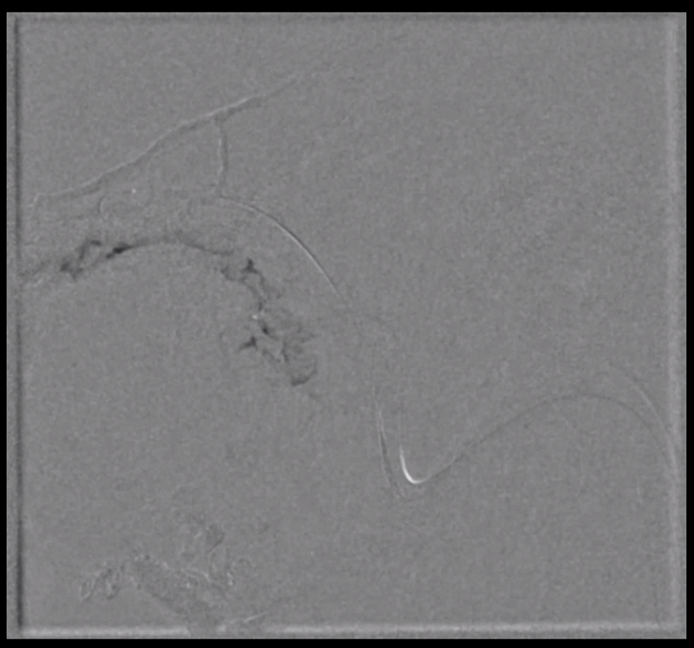
Below is an image of the Scepter in the main sinus wall channel (one we saw best from ECA injections)
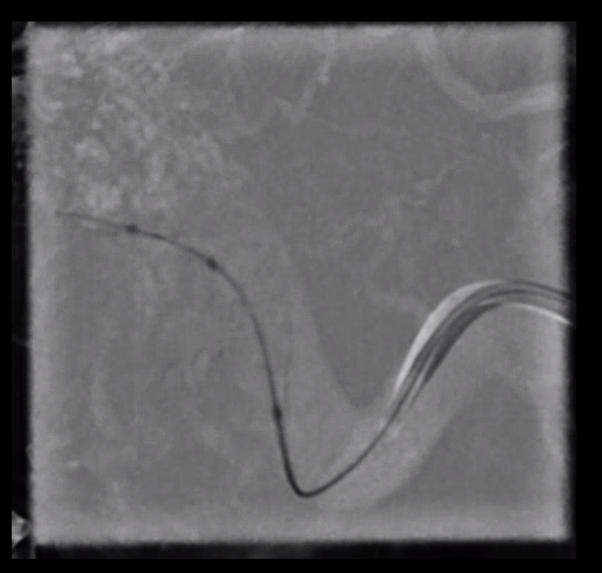
Test injection, see retrograde opacification of some Occipital tributary

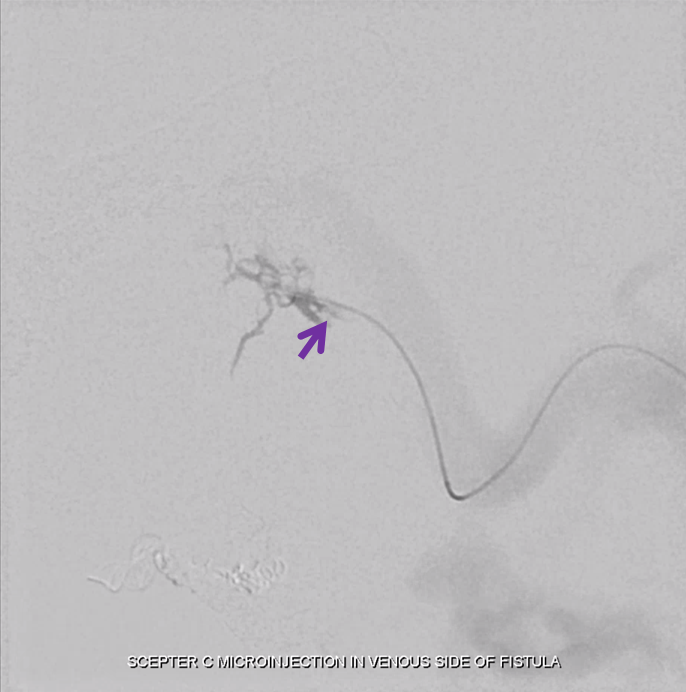
Now come the 7×15 Transforms. The proximal one is subocclusive
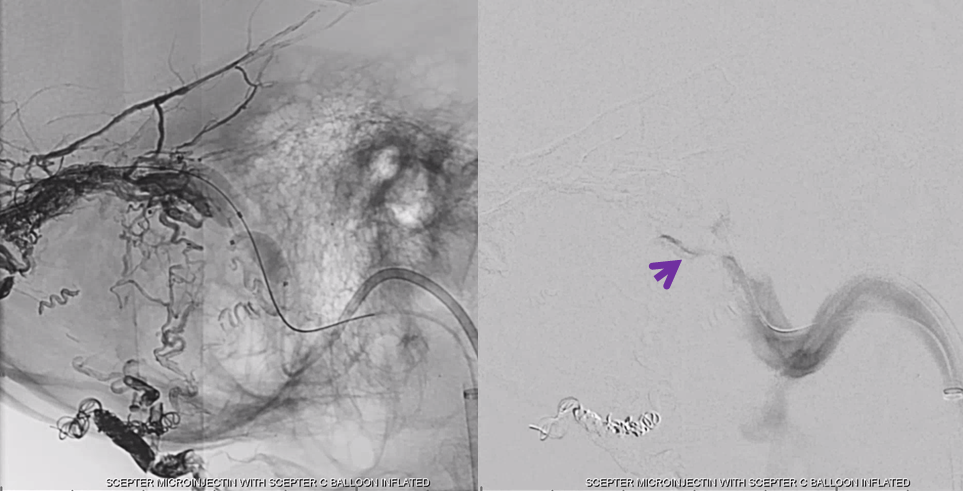
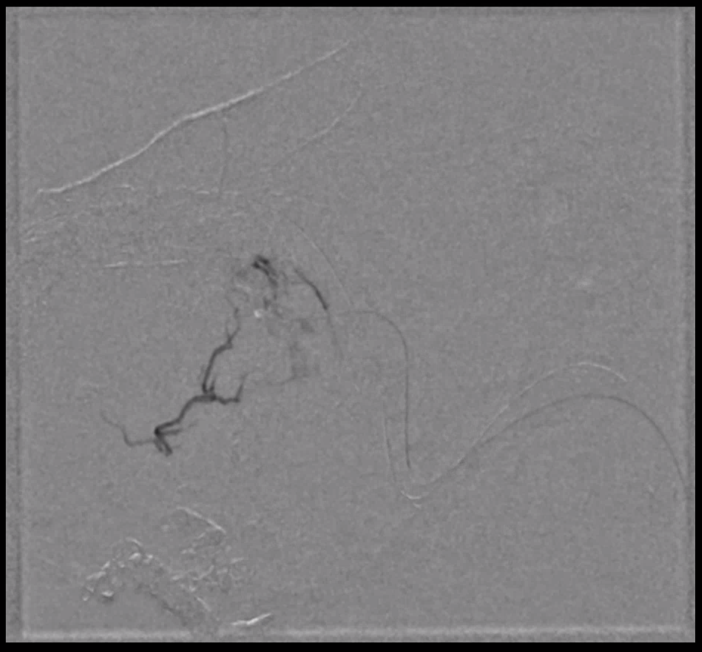
Inflation of proximal balloon positioned across the outflow of our channel, then inject channel to see another, more distal connection of this same channels with the sinus (arrow)
Finally, we put the Headway Duo into the more proximal channel (white arrow)
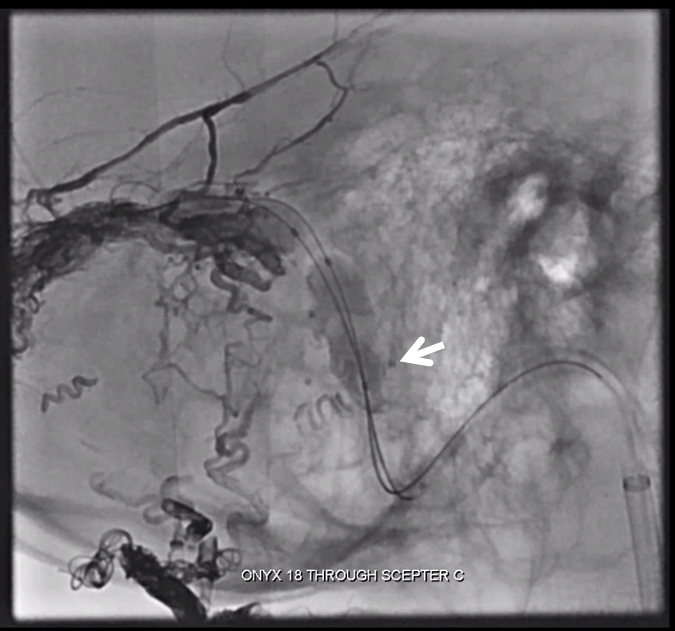
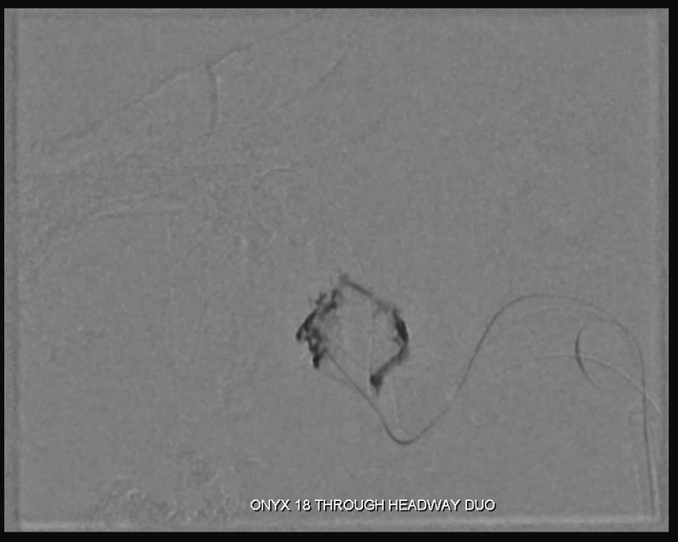
Now we Onyx (18). See how Onyx permeates that sinus wall network. Much more effective than any transarterial embo can achieve.
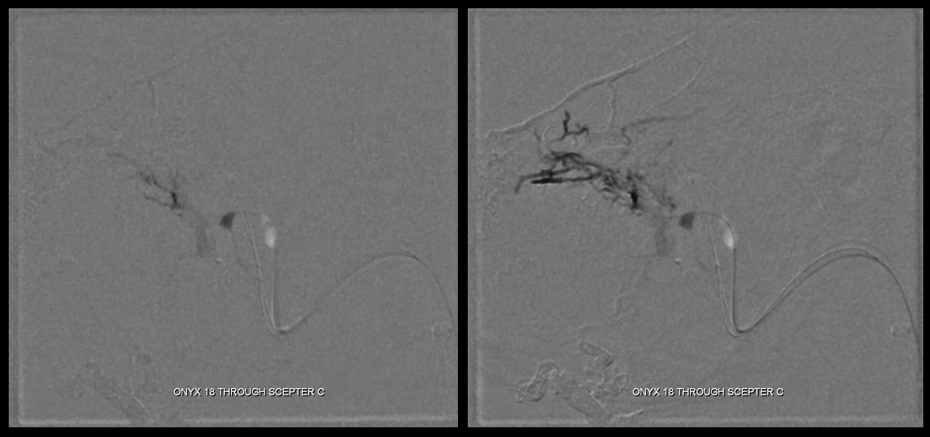
Keep going. Balloons need to be repositioned as onyx enters sinus proper through fistula holes between wall and sinus
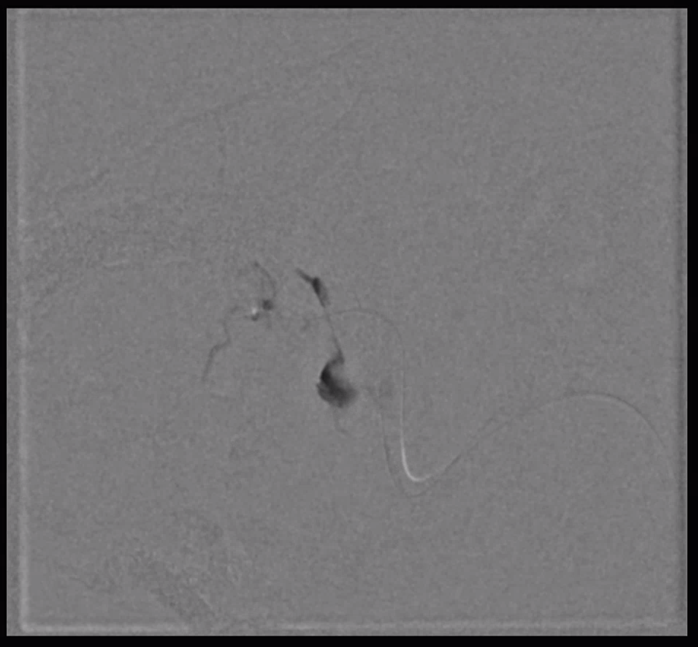
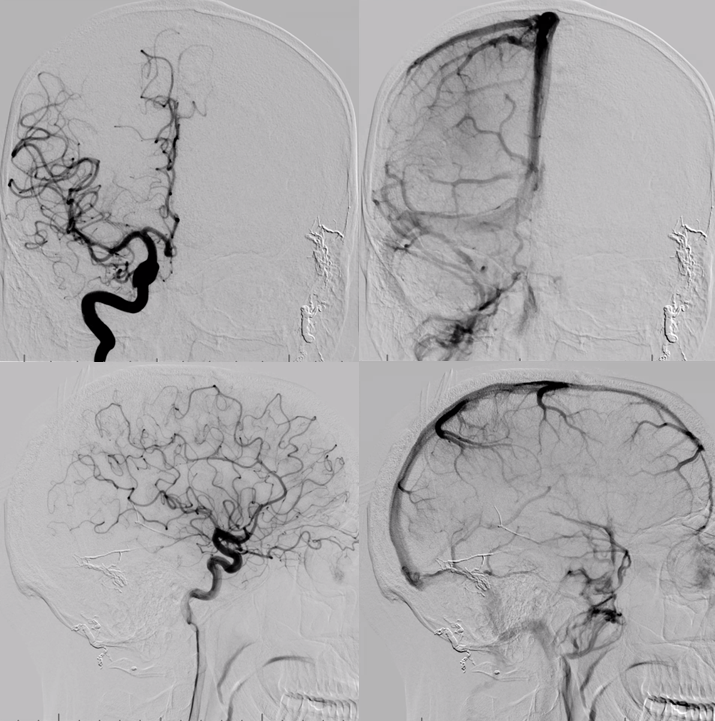
Control ECA injection. Almost done. Some very proximal sinus shunt left. This are is particularly dangerous to embolize trans-arterially, as it risks jugular foramen cranial nerves and the hypoglossal canal. Transvenous is much safer.
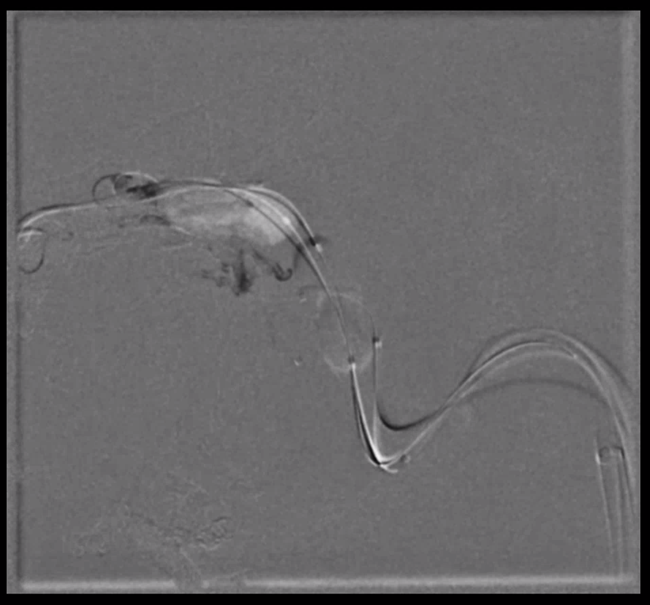
Reposition Transform balloon, inject from Duo to see the remaining sinus wall channel.
More Onyx
Fistula closed
So is the sinus…
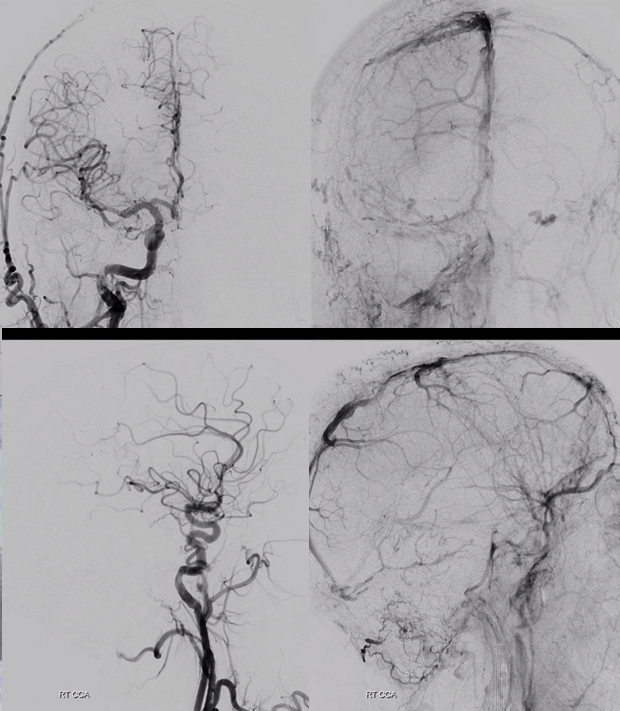
Failure? Of course not. It is not hard to go through the partially Onyx-filled sinus with either an 014 wire or an 035 glide, if need be. Here, we have a Sofia 5 in the superior sagittal sinus.
Now we deploy two Precise carotid stents across the diseased sinus segment. This was the plan all along. This sinus is far too sick to survive without a stent. The sinus is now open.
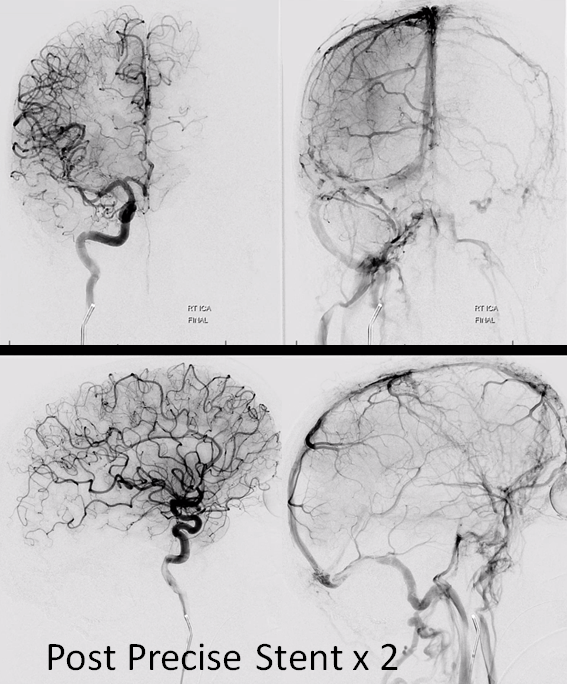
Cant see the stent? Neither could we. With this much Onyx cant see anything. Thankfully, it does not take much to open a Precise.
Even the left brain is now using the right transverse/sigmoid outflow. Cerebellum finally looks happy.
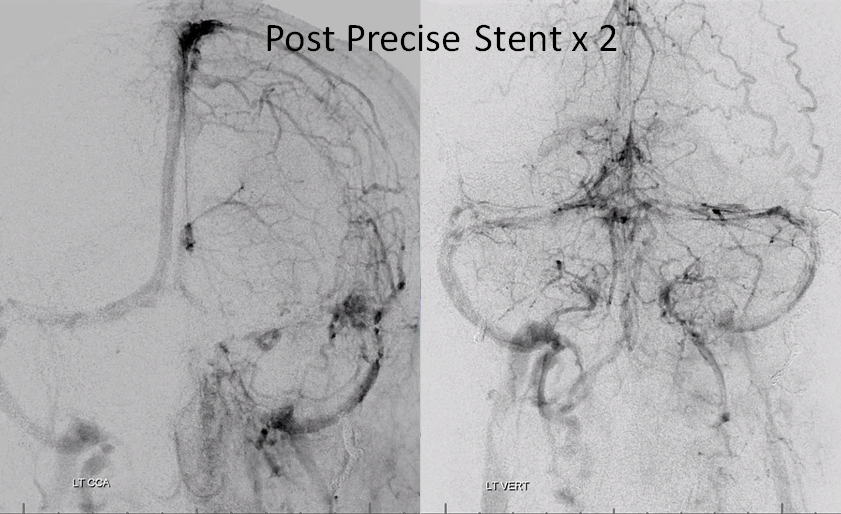
Indeed, the stents are there
Summary:
Superselective transvenous embolization is the best way to treat many sigmoid sinus fistulas. It is an ideal strategy — preserving sinus without transarterial approach, highly effective for closing the fistula. See how little Onyx it takes, and how effective it is when coming from the venous side? Sure, it does not work for every case — especially for higher grade ones, where the sinus is too diseased or closed. For low grade ones, where this treatment works more often, it is an ideal low risk choice.
Other examples:
Literature:
Mironov A. Selective transvenous embolization of dural fistulas without occlusion of the dural sinus. AJNR American journal of neuroradiology 1998;19:389-391
Piske RL, Campos CM, Chaves JB, et al. Dural sinus compartment in dural arteriovenous shunts: a new angioarchitectural feature allowing superselective transvenous dural sinus occlusion treatment.
Caragine LP, Halbach VV, Dowd CF, et al. Parallel venous channel as the recipient pouch in transverse/sigmoid sinus dural fistulae. Neurosurgery 2003;53:1261-1266; discussion 1266-1267
Shapiro M, Raz E, Litao M, Becske T, Riina H, Nelson PK. Toward a Better Understanding of Dural Arteriovenous Fistula Angioarchitecture: Superselective Transvenous Embolization of a Sigmoid Common Arterial Collector. AJNR Am J Neuroradiol. 2018 Sep;39(9):1682-1688
