The vast majority of spinal arteriovenous shunts are dural fistulas in men aged 50 and above. However, there are rare cases of multiple fistulas of various types. Many have underlying genetic conditions we know or are learning about. Usually, they do not fit the above demographic either. Here is a person (age and gender are withheld on neuroangio for confidentiality reasons), presenting with sudden onset neck and head pain.
CT head — the lesson is always look in the neck when there is no source for subarachnoid and/or intraventricular hemorrhage in head. CTA head was negative
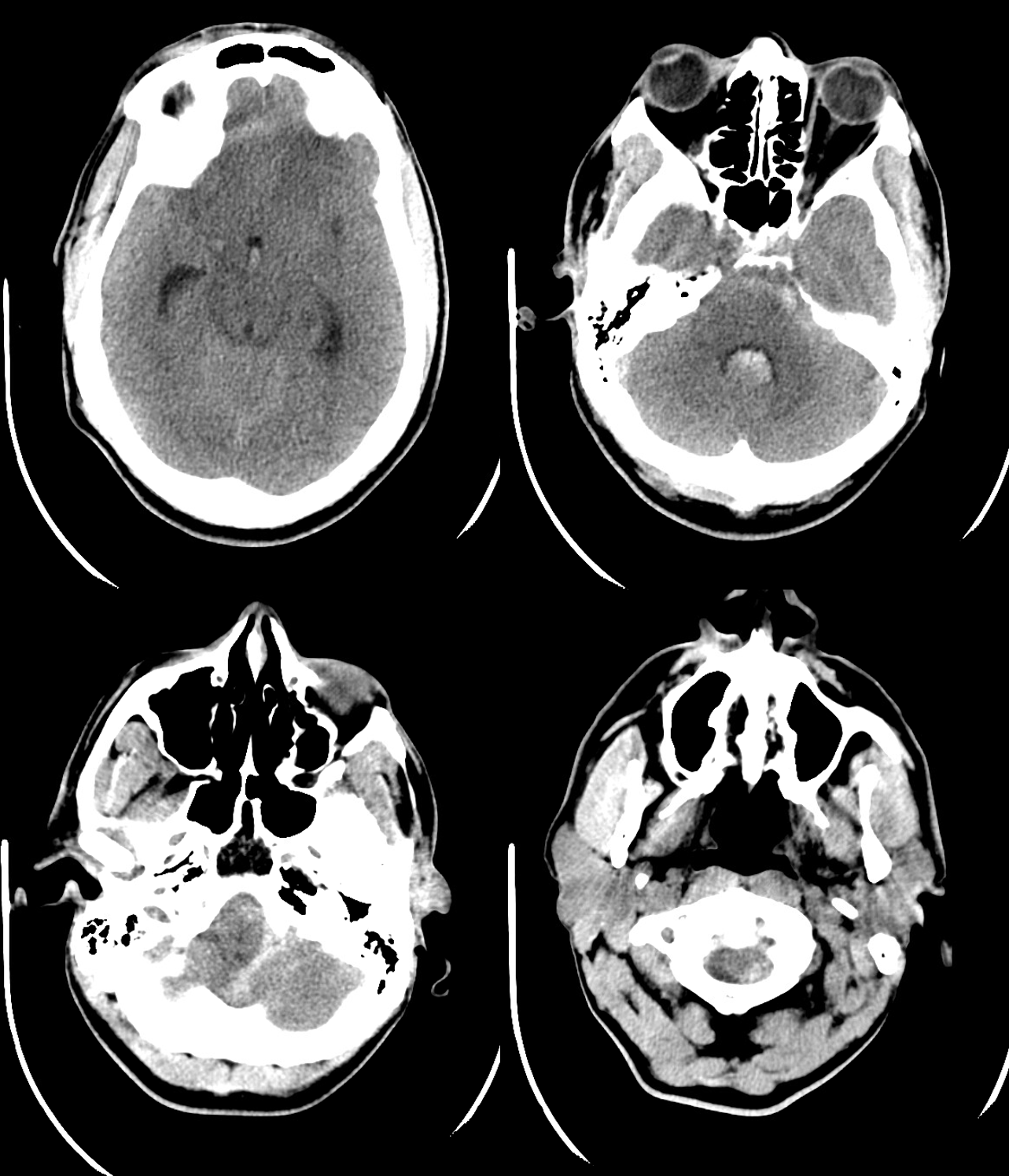
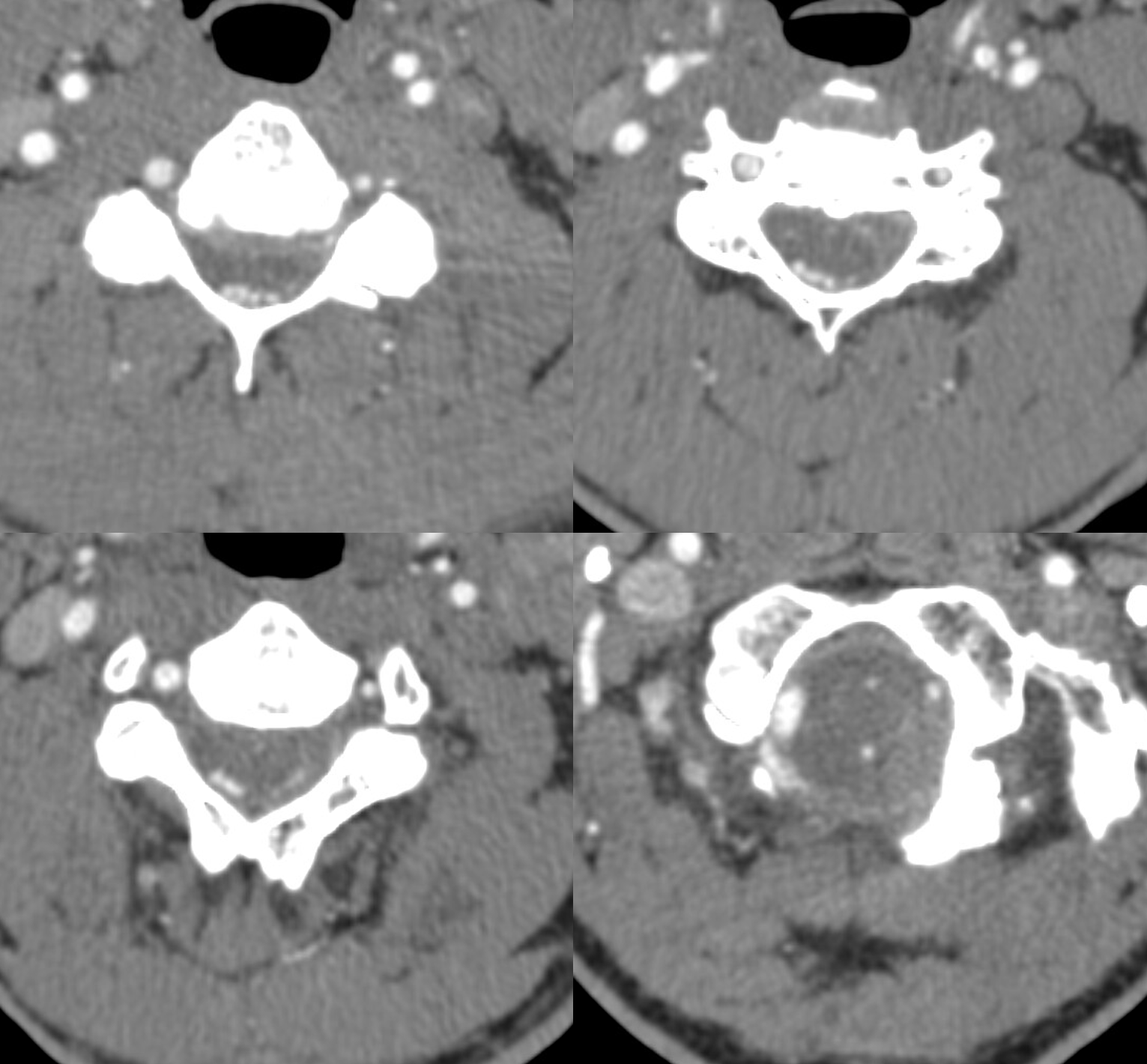
noncontrast neck ct was not done. Thankfully, though, a head and neck CTA was ordered
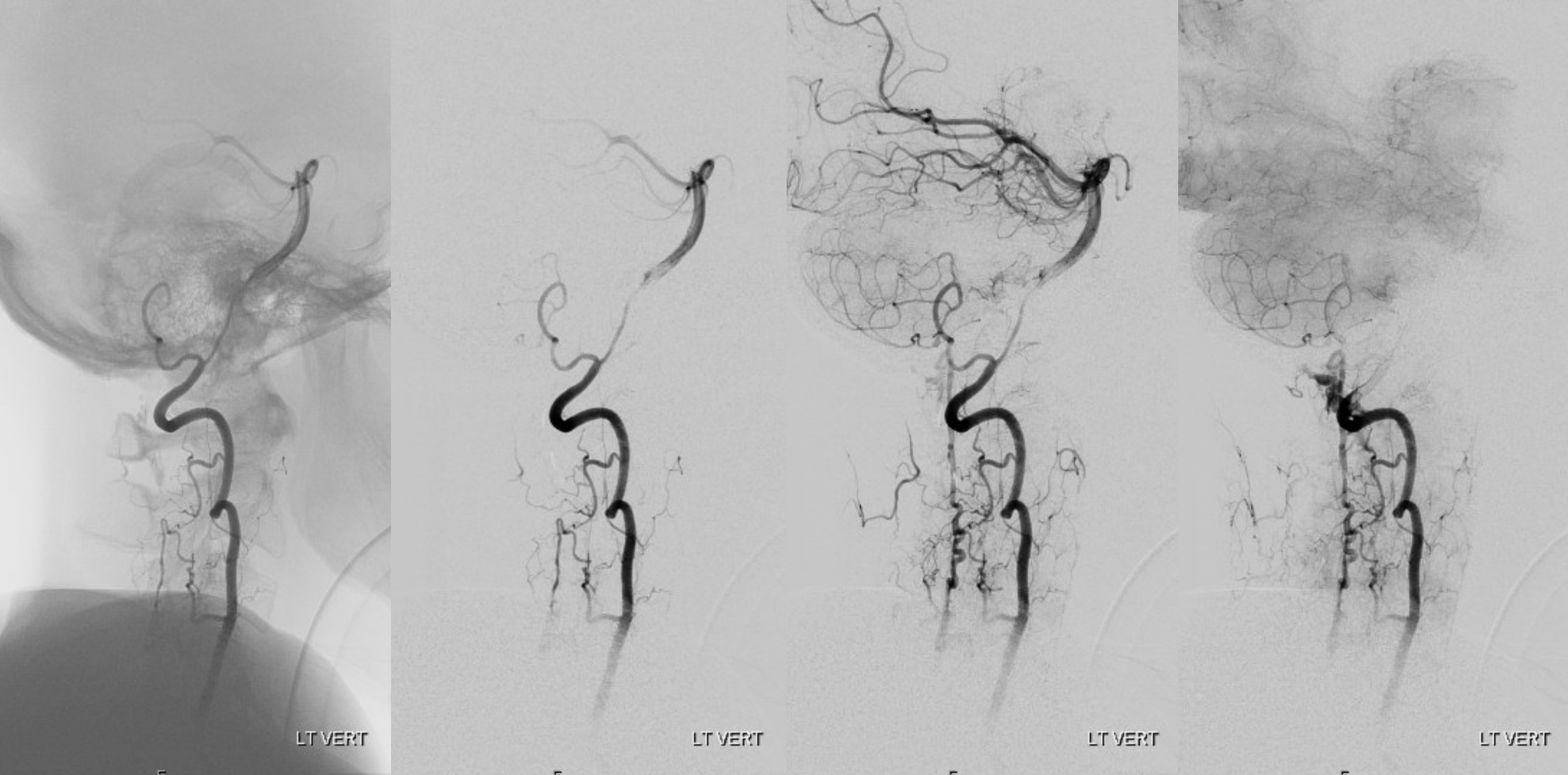
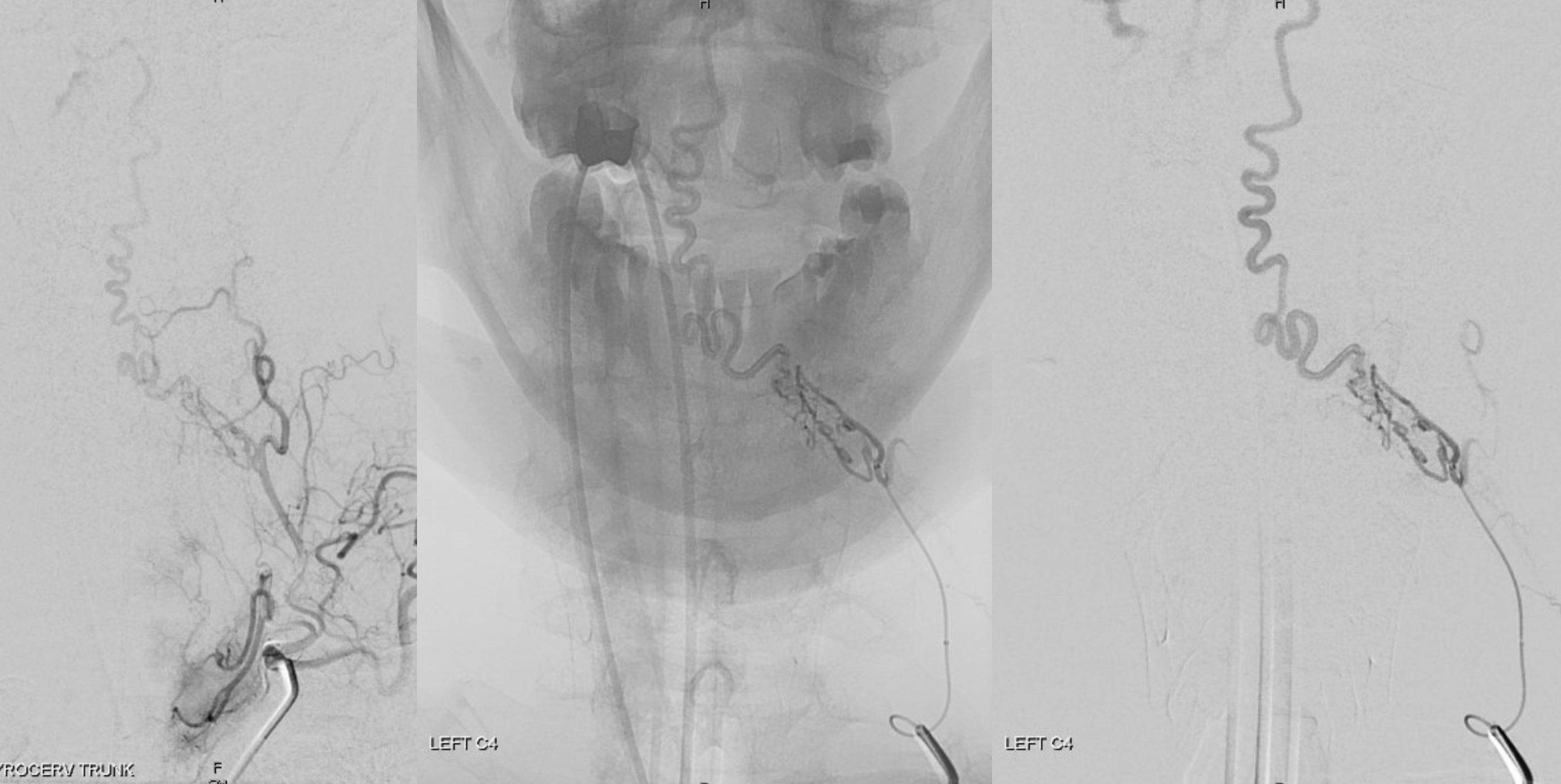
Right vert injection. There are two areas of premature anterior spinal vein visualization (C4 — white arrows and C2 — arrowheads). Note decompression of anterior spinal vein via left C8 radicular vein into the likely foraminal venous plexus (dashed white arrow). Also seen is premature visualization of the epidural venous plexus at right C4 area (black arrows). This could be either a separate epidural fistula at same level as C4 dural fistula, or a single epidural one with retrograde congestion of the spinal vein. This is hard to tell apart here.

Lateral — same arrows

Guess what? Magnified views — what other structure do we see now (open white arrows)

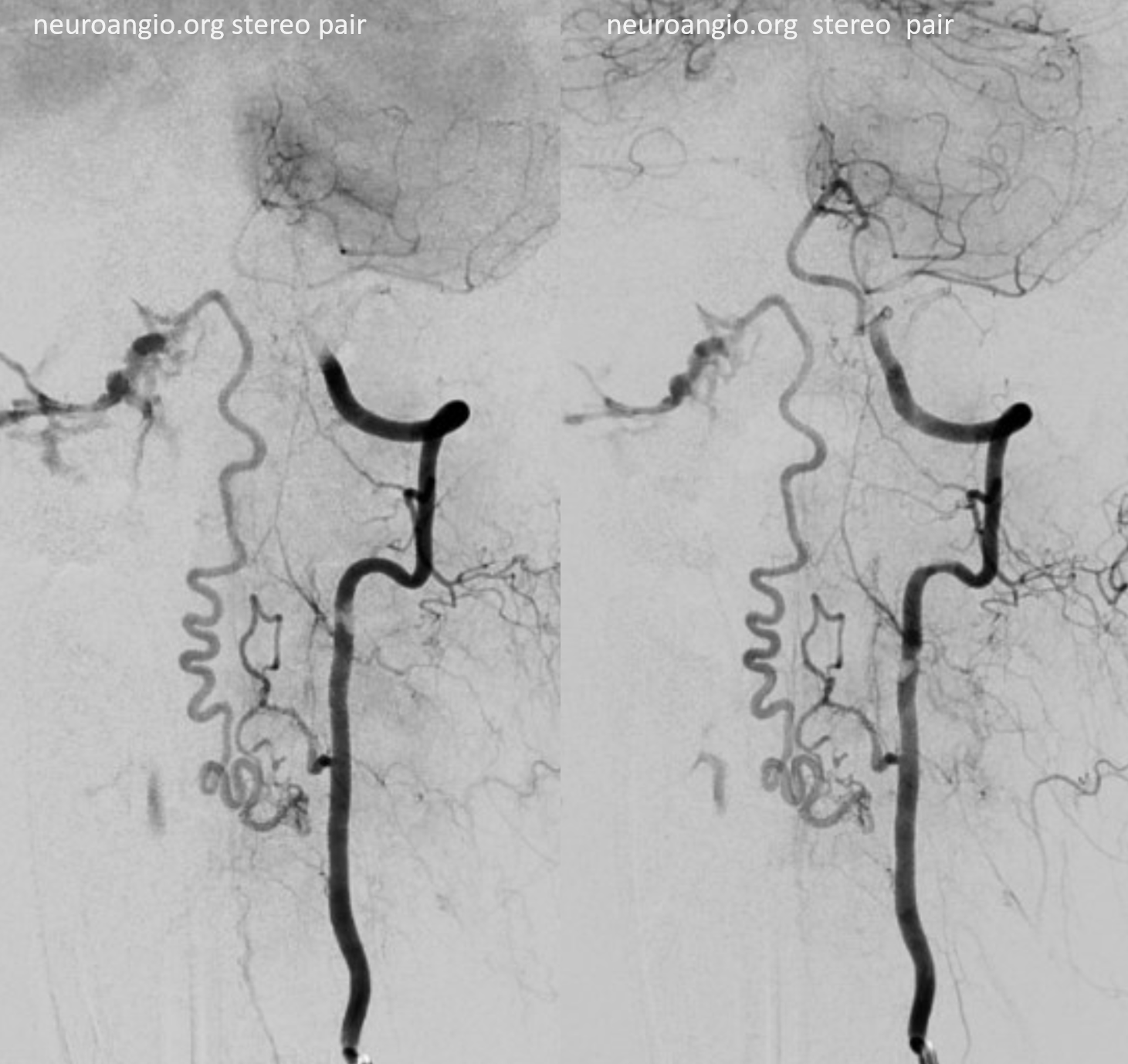
The other side — more is more… This is different kind of shunt — left C4 supply here. A longer kind of vessel (dashed arrow and arrowhead) opening into a venous-looking structure (ball arrows) which ultimately decompresses into the marginal sinus (ball dashed arrow). What kind of shunt is this?
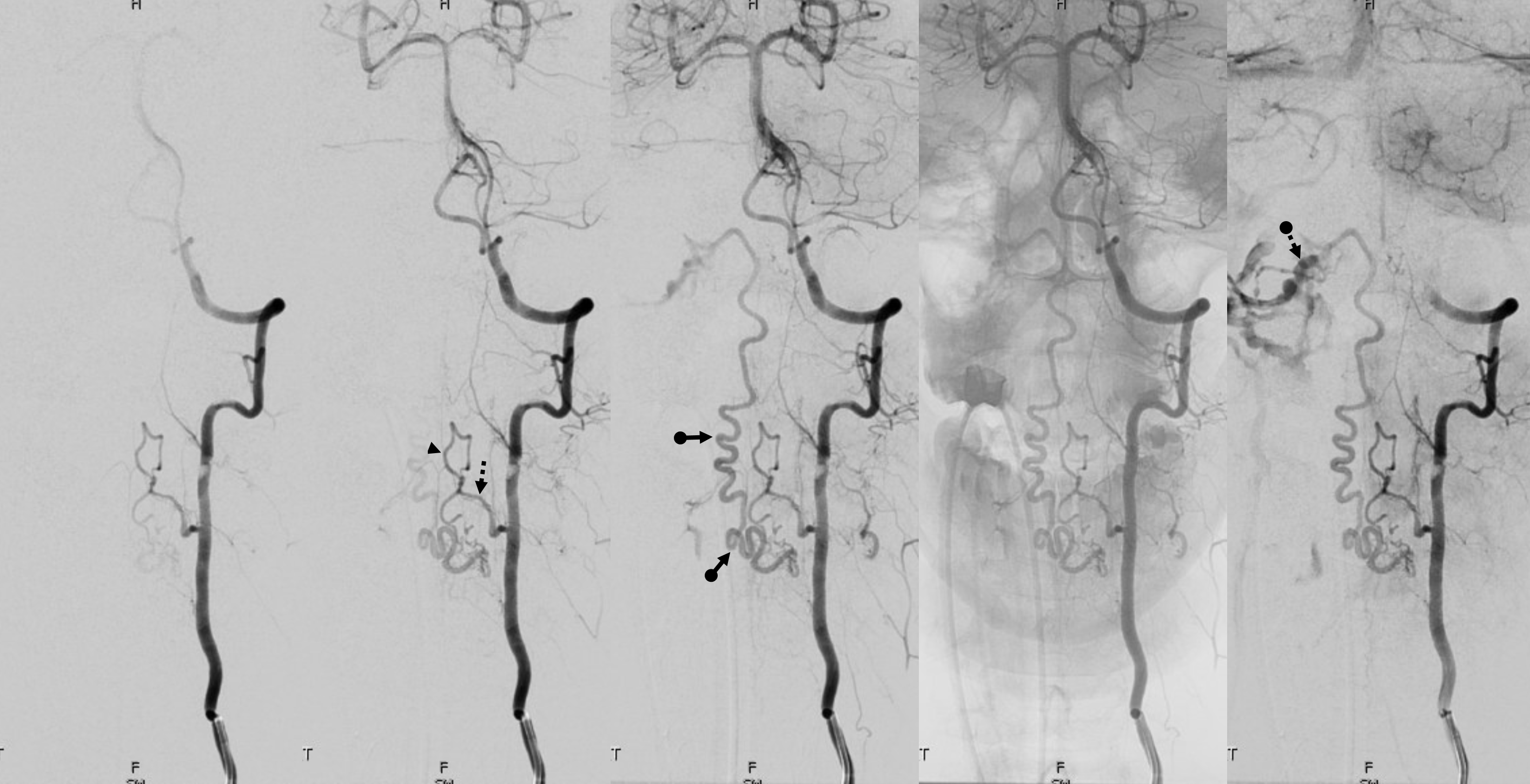
Lateral views. Note a very consistent observation here — anterior spinal veins cranially connect to the anterior pontomescencephalic / pontomedullary system (a direct continuation) and typically drain into the petrosal sinus (the collector of anterior group veins). Posterior spinal veins will open cranially into the marginal sinus or cervical epidural venous plexus (the two are homologous, marginal sinus being the cranial-most extension of the epidural venous plexus).
stereos
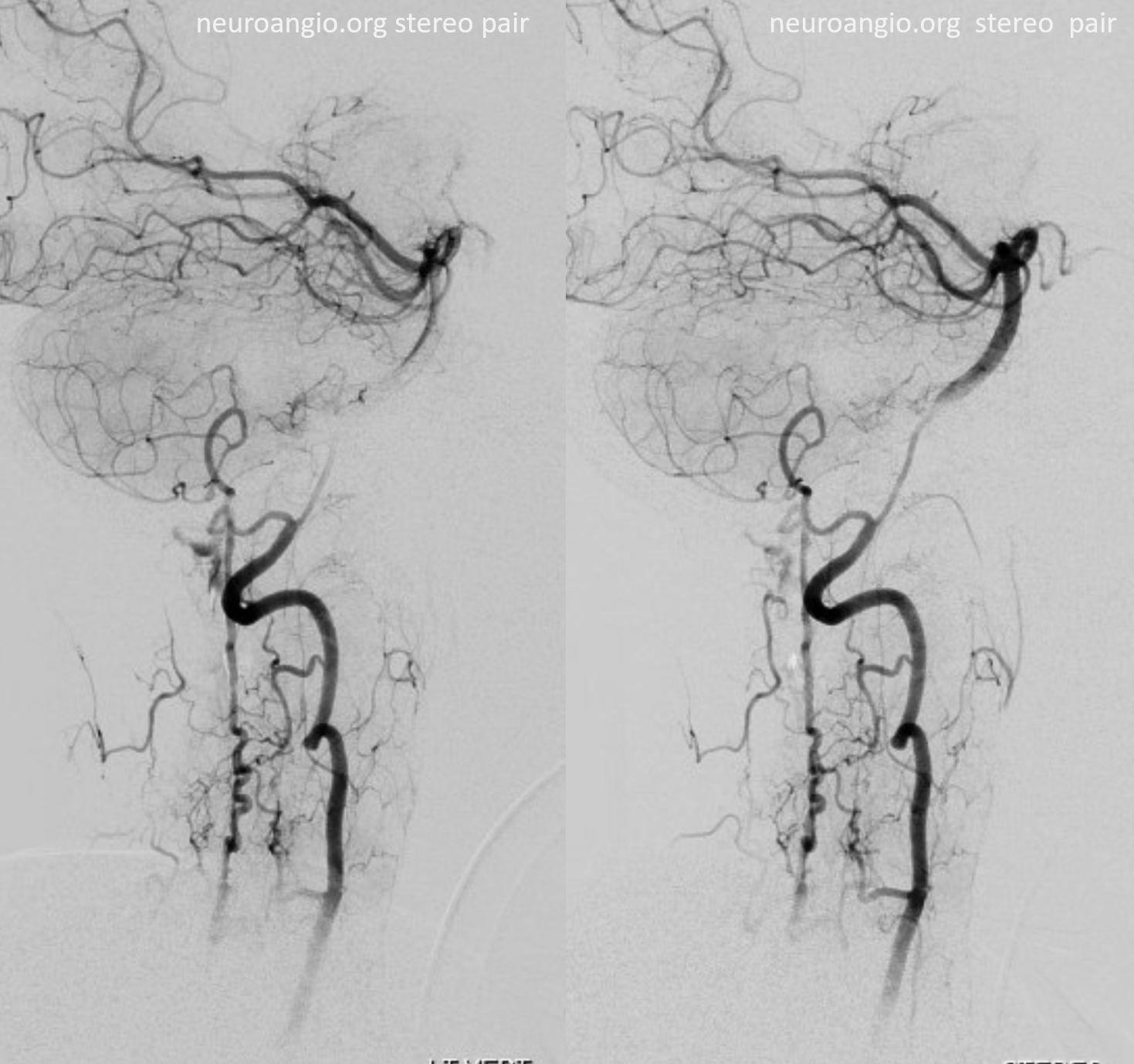
Magnified views. Guess what again! — now marked by black open arrows. In case you had any silly ideas. Yes, it is possible to catheterize the radiculopial artery beyond the radiculomedullary origin — but why would you given all the hazards seen so far?
Extra credit — what is the implication of contrast “slipstreaming” in the vein (ball arrows)
Finally, and critically, what structure is the arrowhead pointing to?
The answer to extra credit — what is going on here?
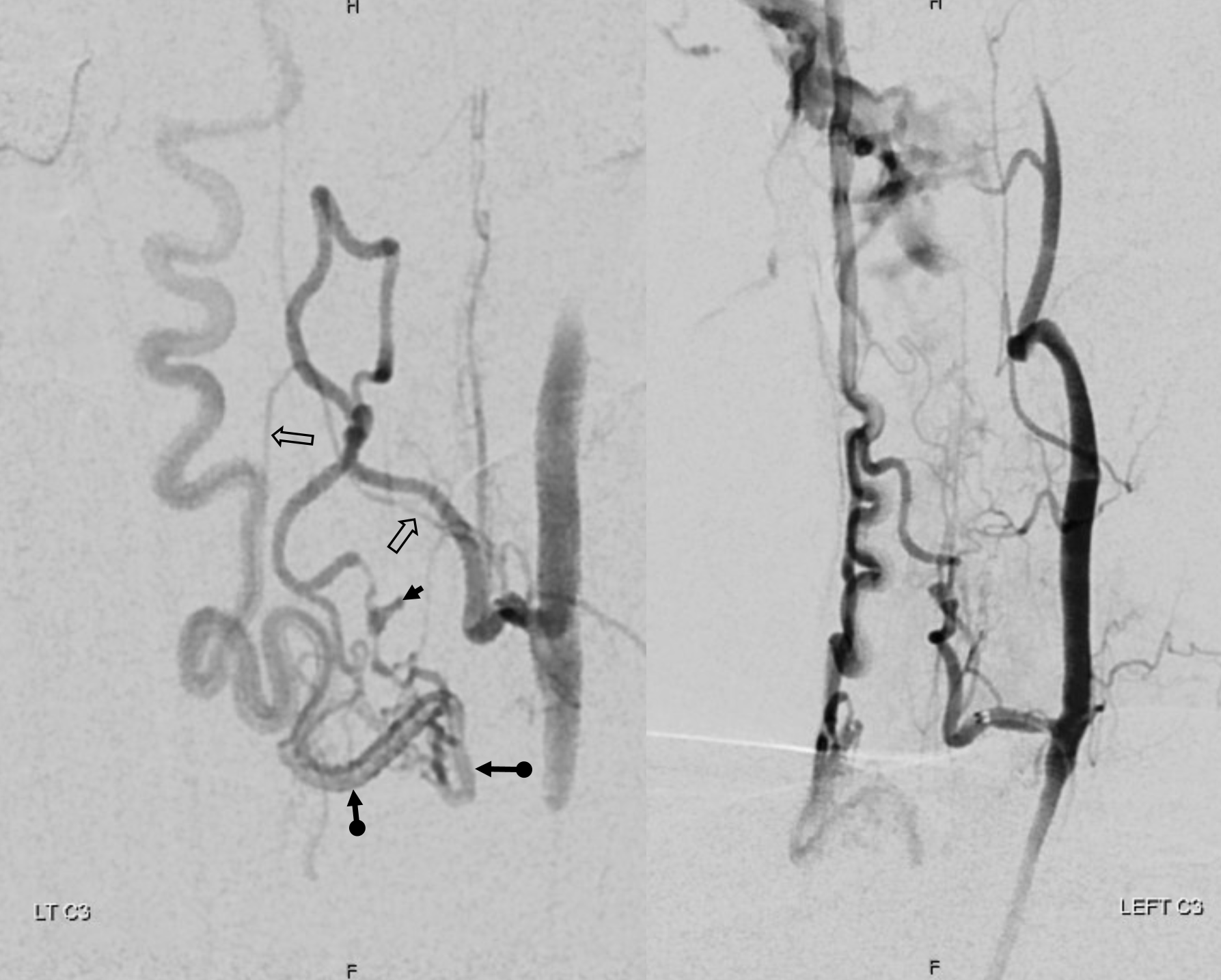
Of course, we need a DYNA.

Axial MIPs. The shunt is posterolateral (white oval)
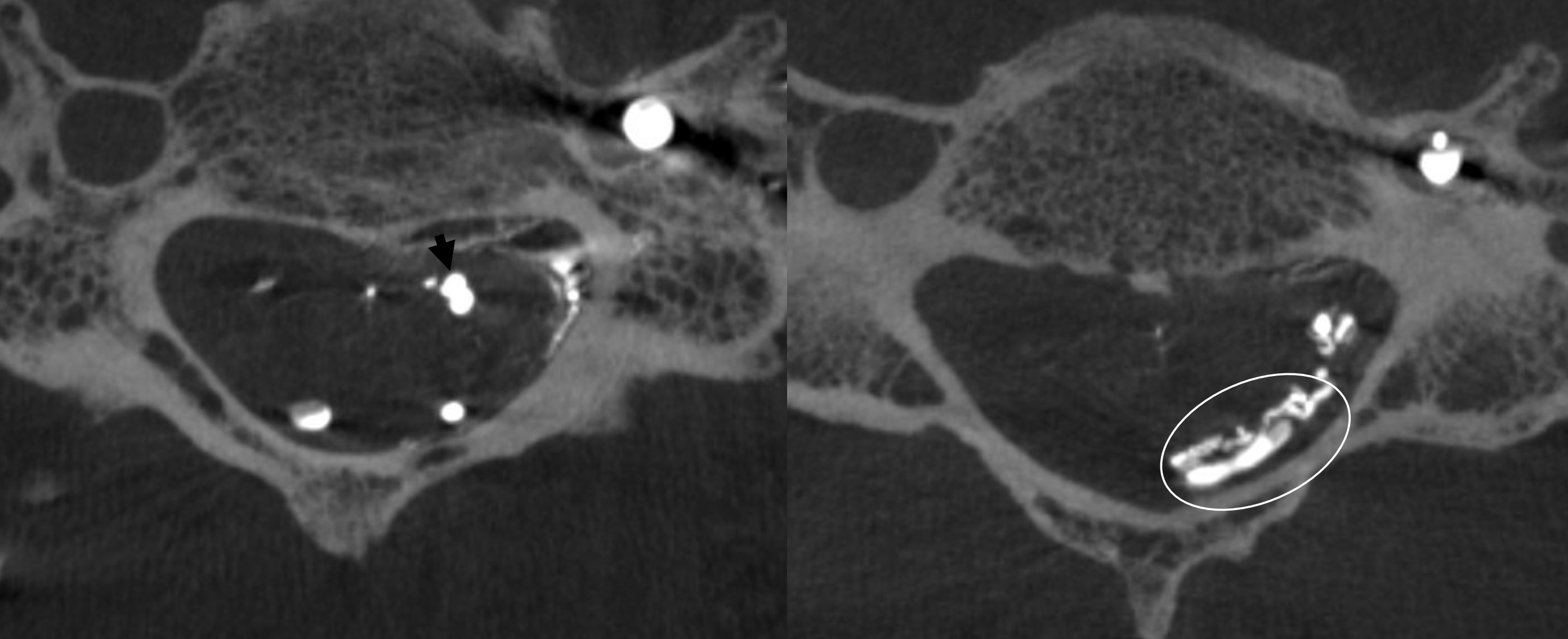
Right vert VR DYNA stereos. It is still not possible to decide whether this is an epidural shunt or co-existing dural and epidural ones. Ockham’s razor would have it epidural — and that is nearly always right in endovascular world.

Given the above, the obvious answer is surgical resection. Post-op views
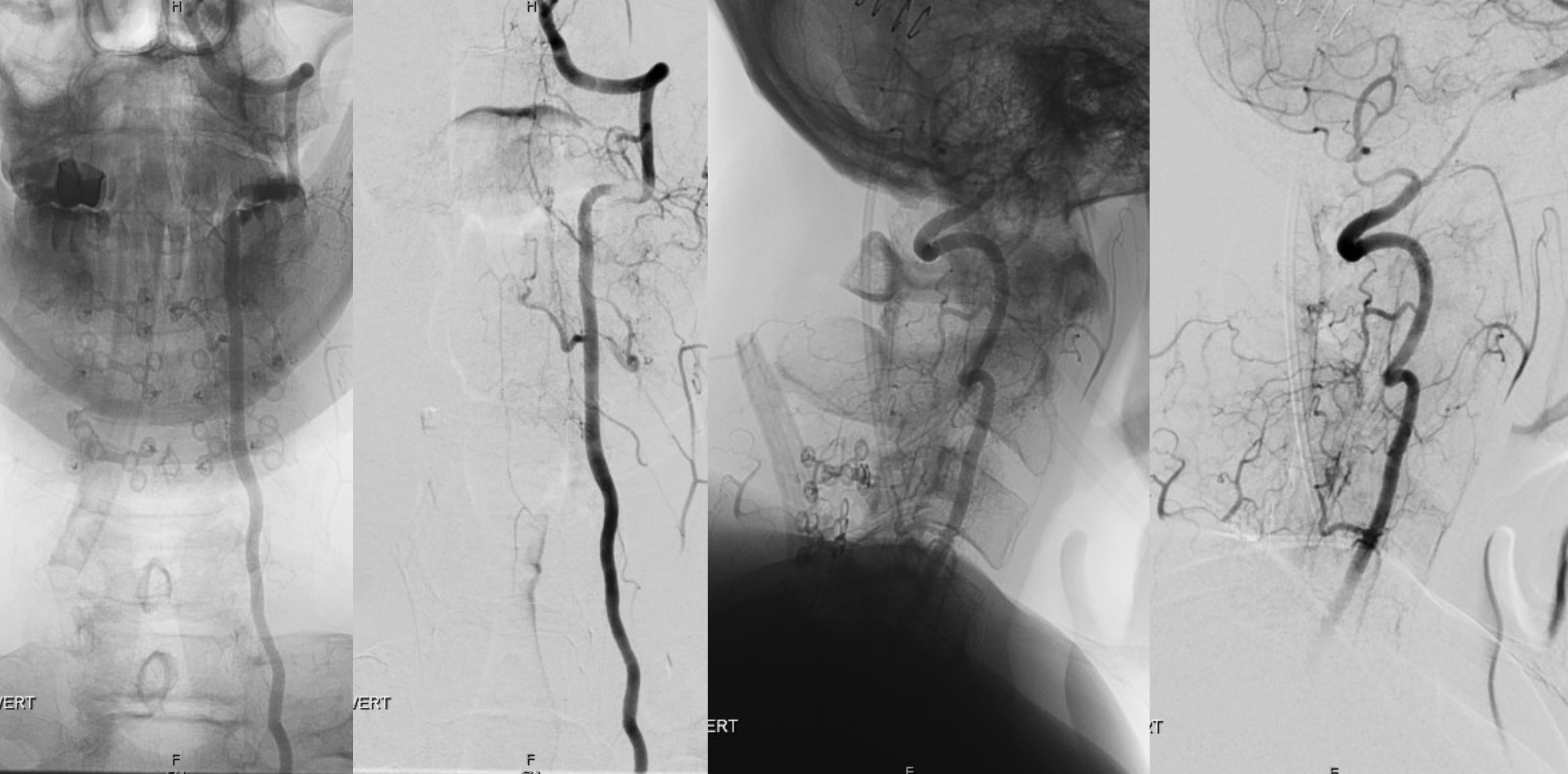
What is left?

What a great diagnostic case — an all in one of spinal vascular anatomy (well, almost).
