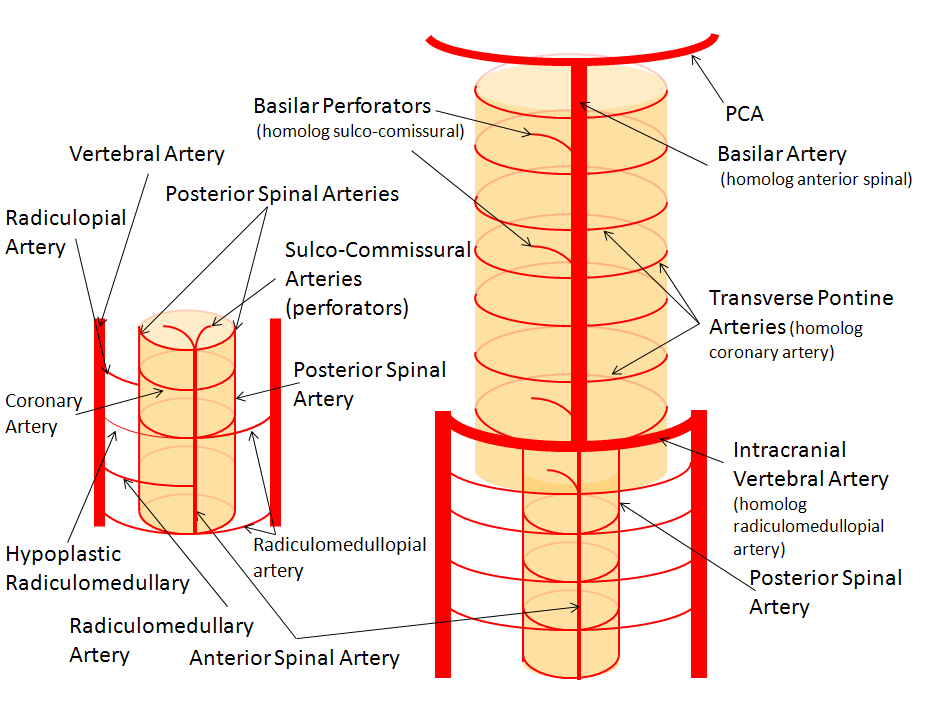
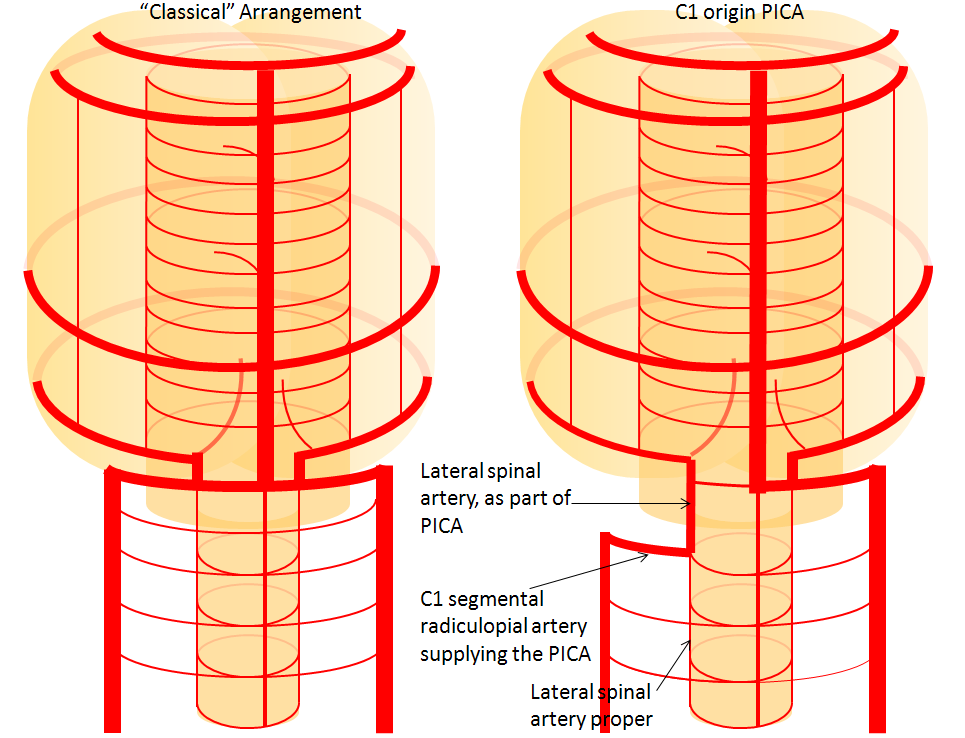


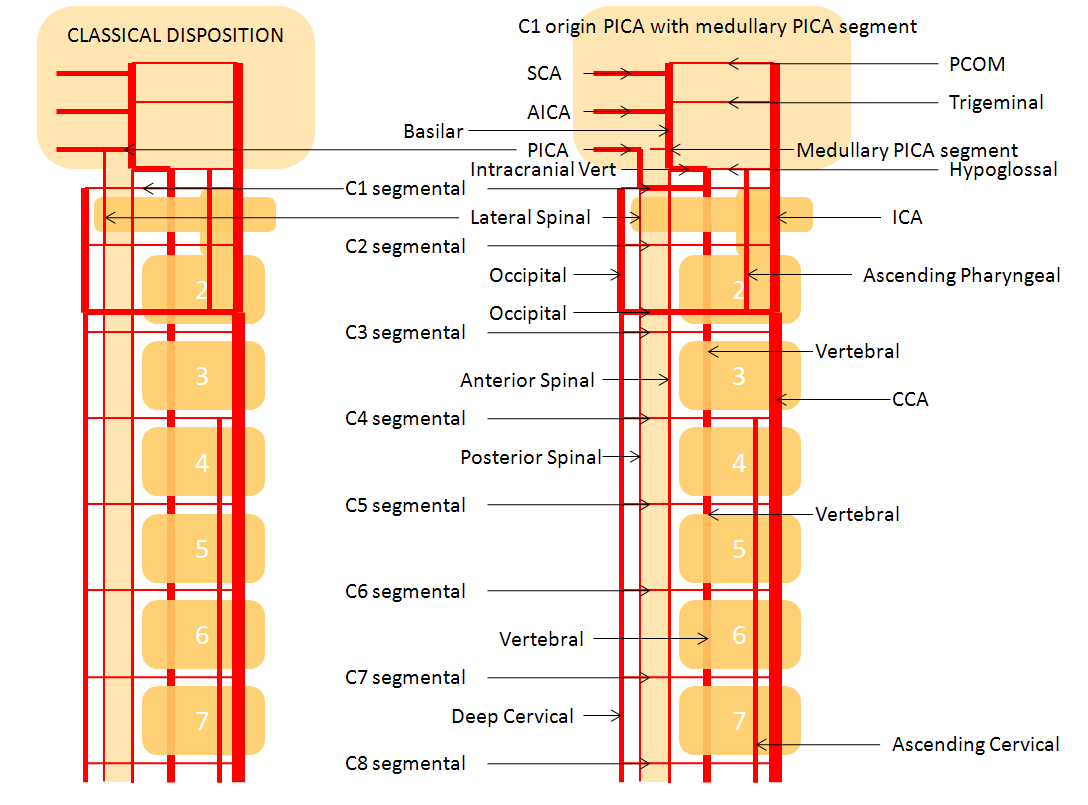
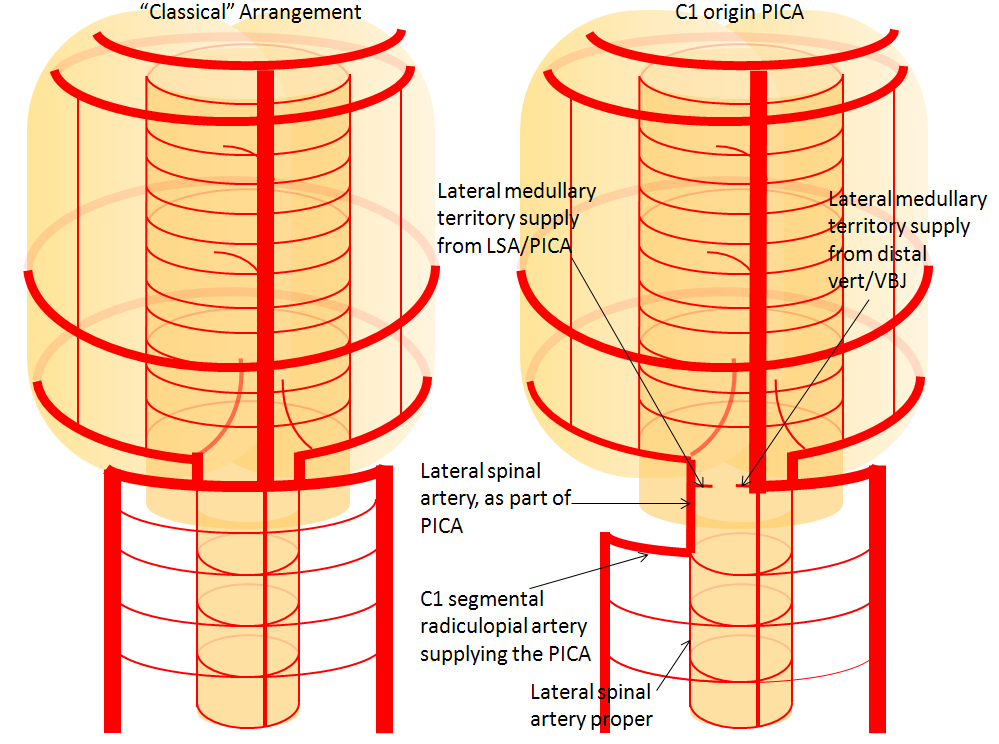

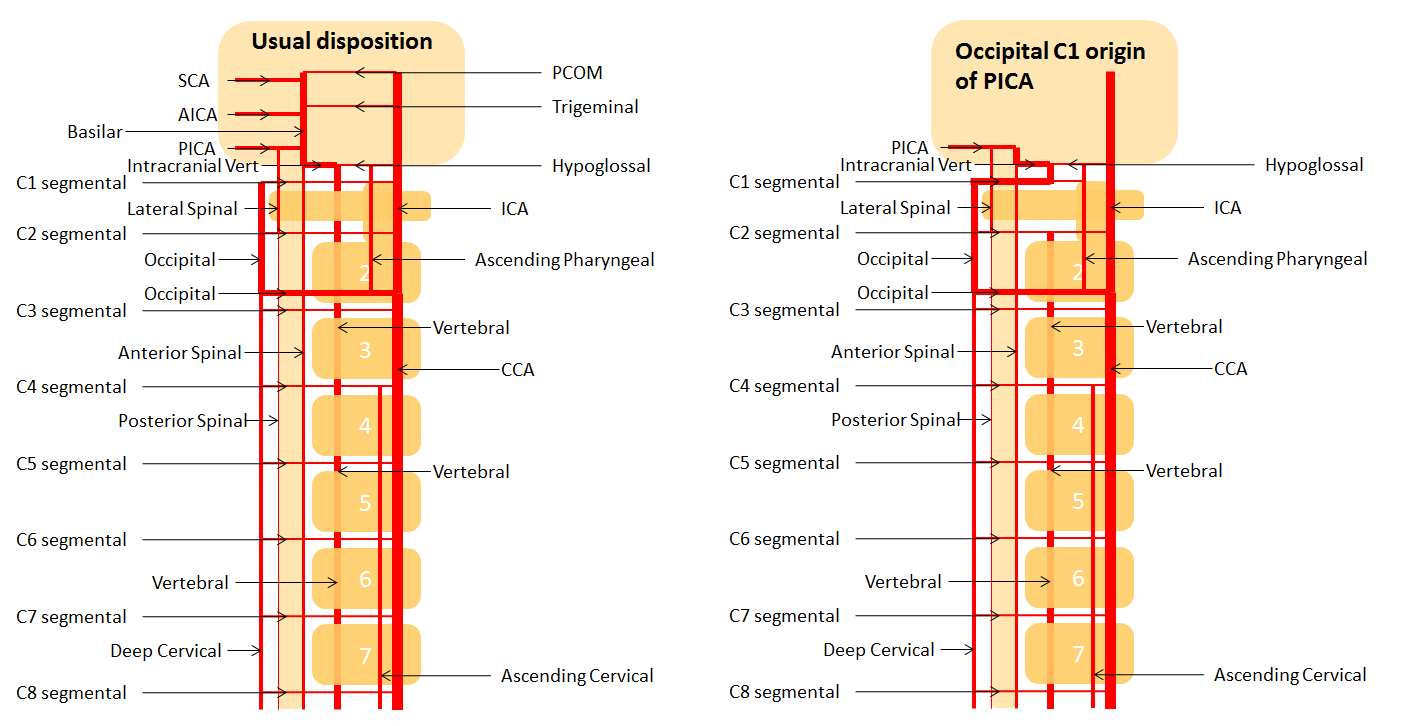
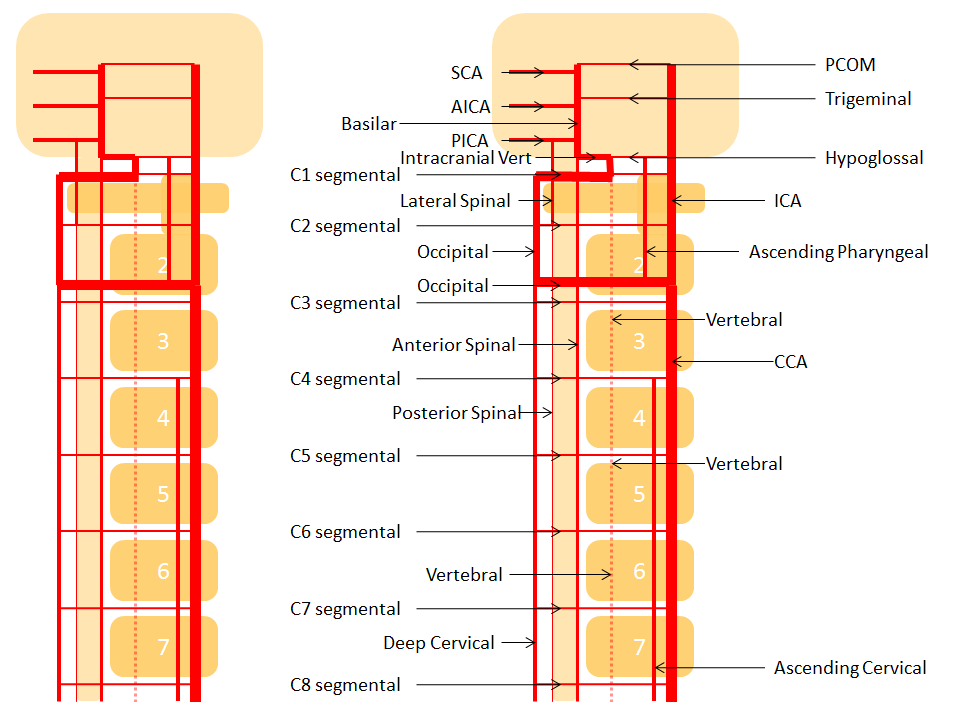
Lateral Spinal Artery / C1 radicular artery / PICA anastomosis
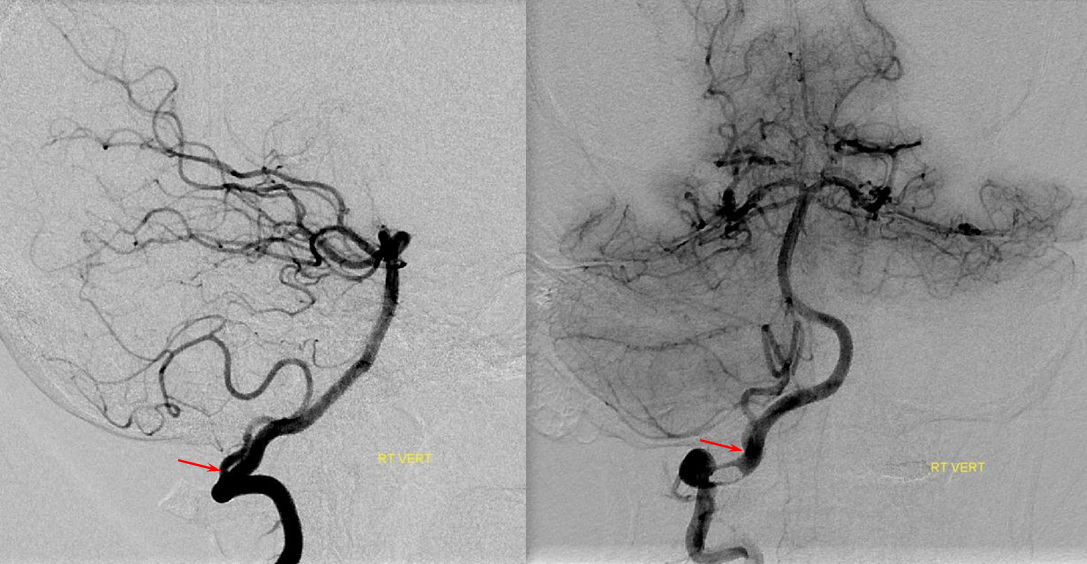
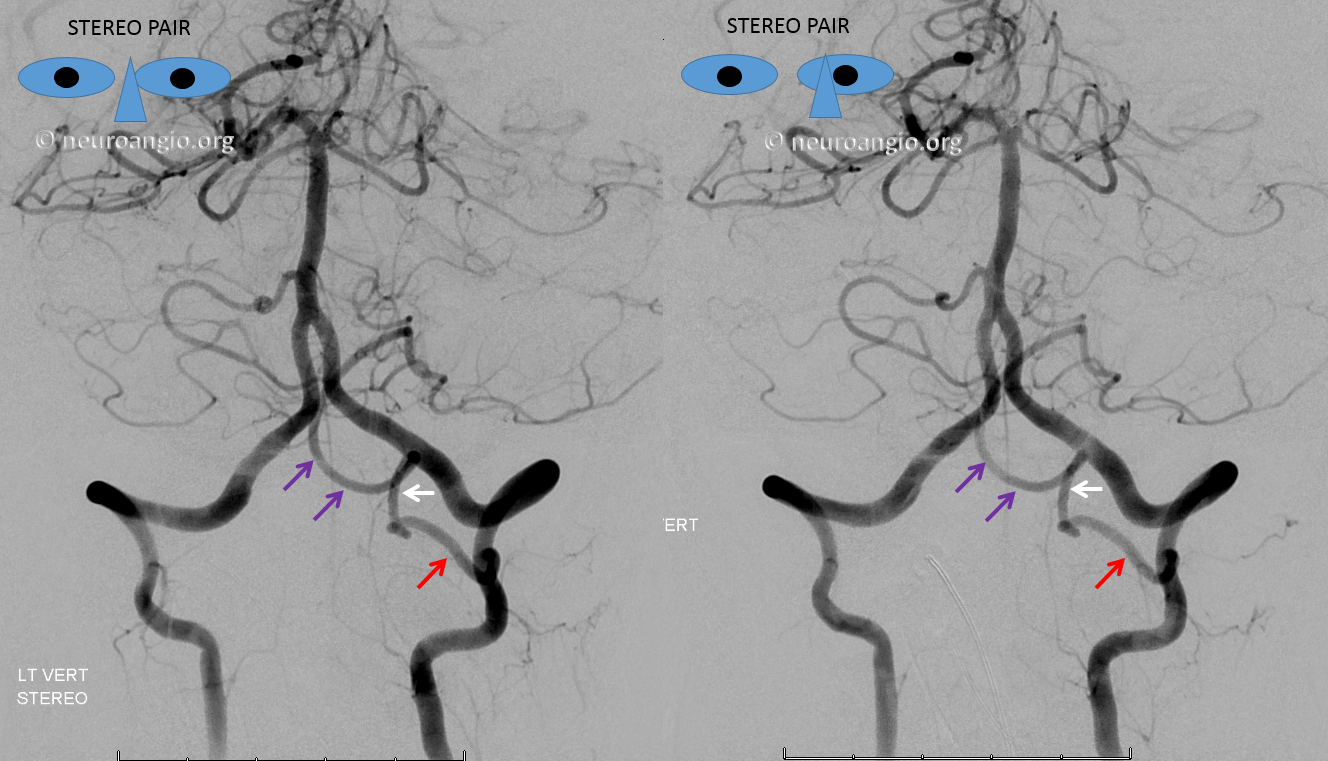
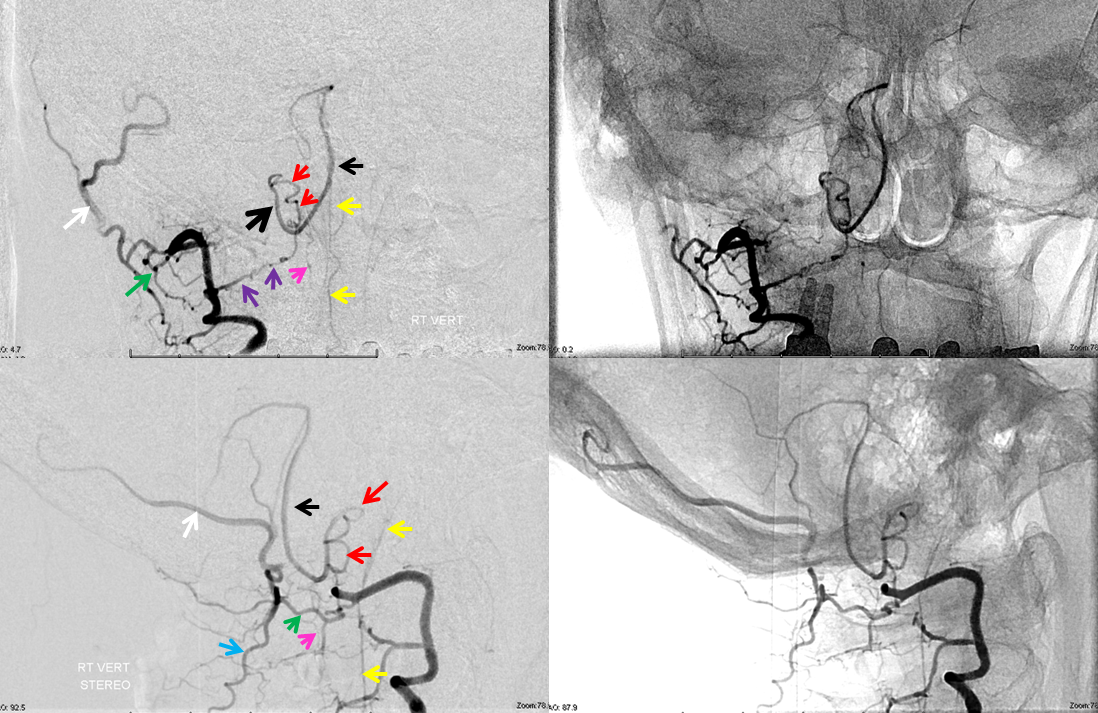
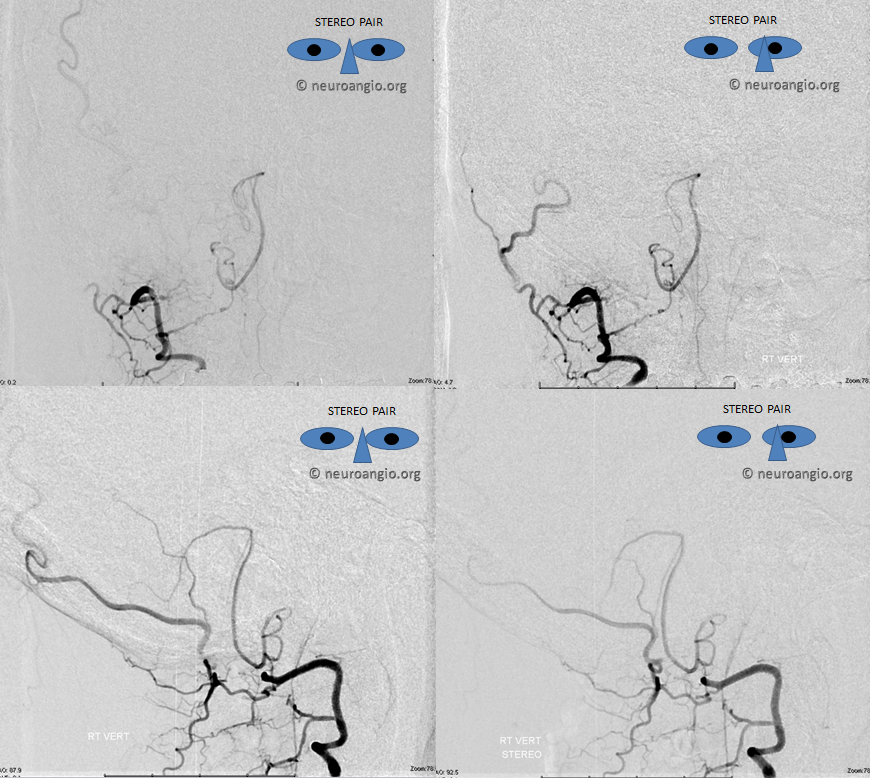
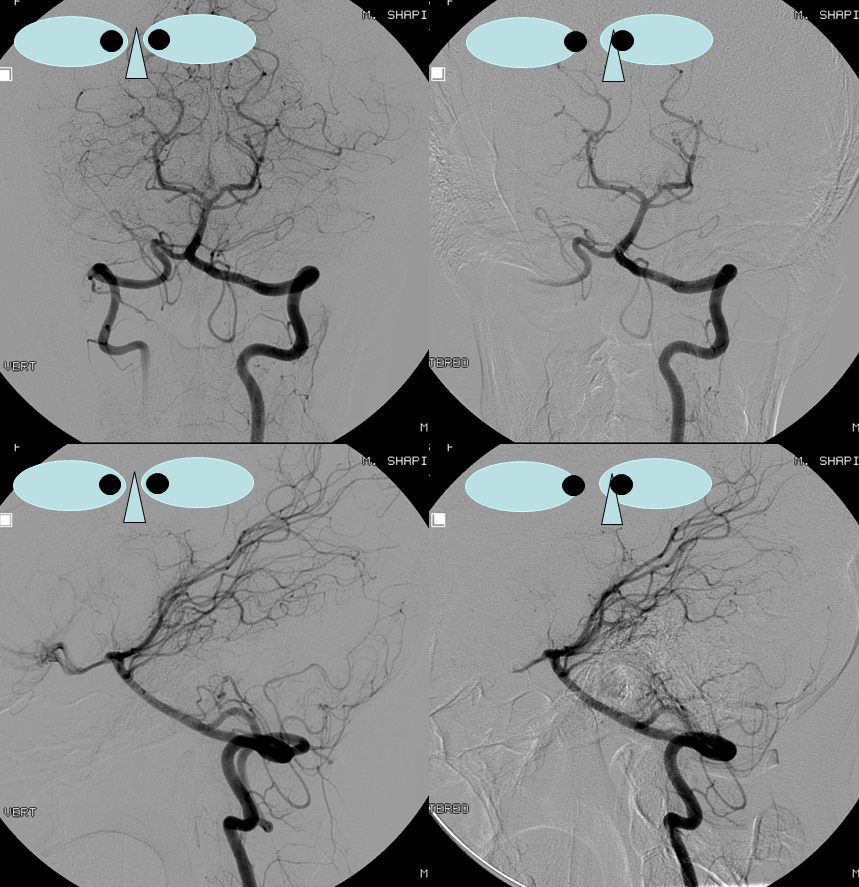
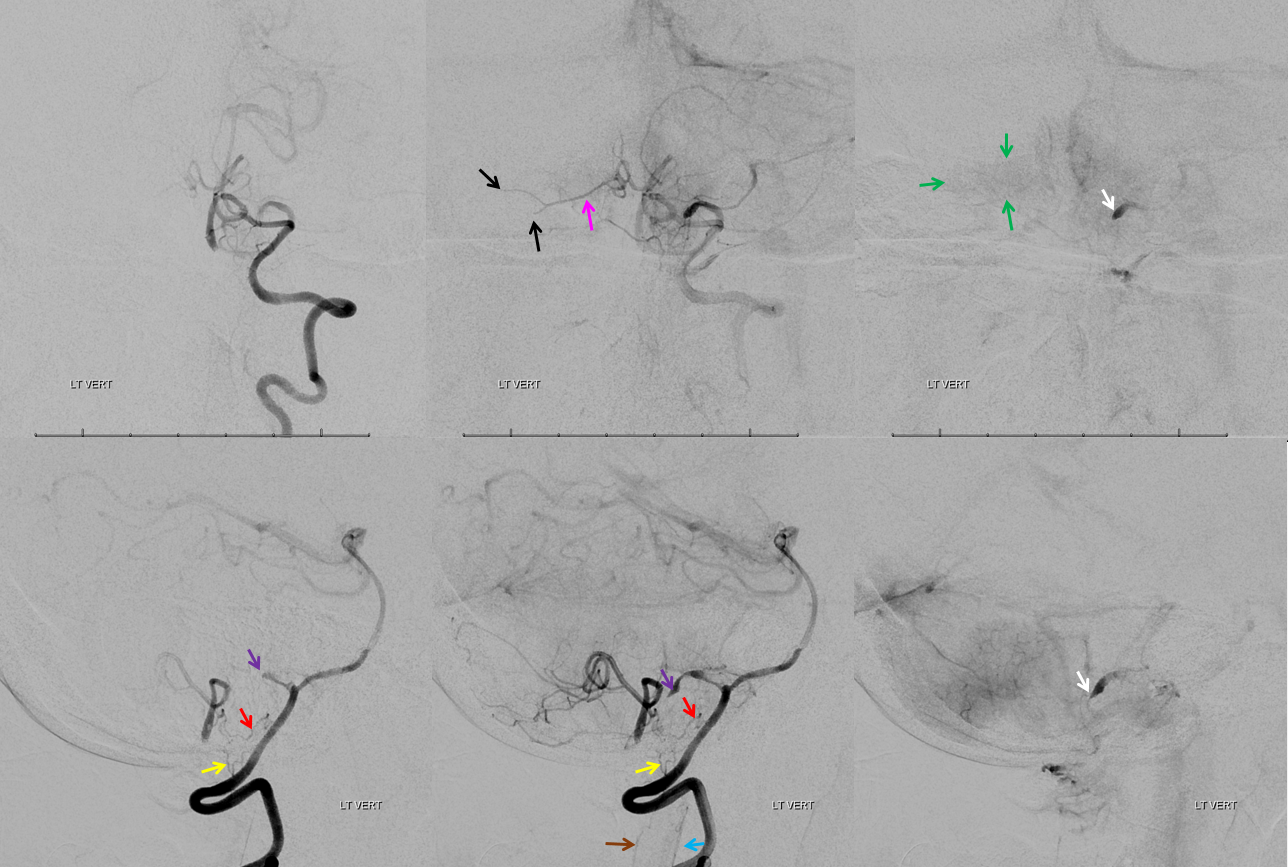
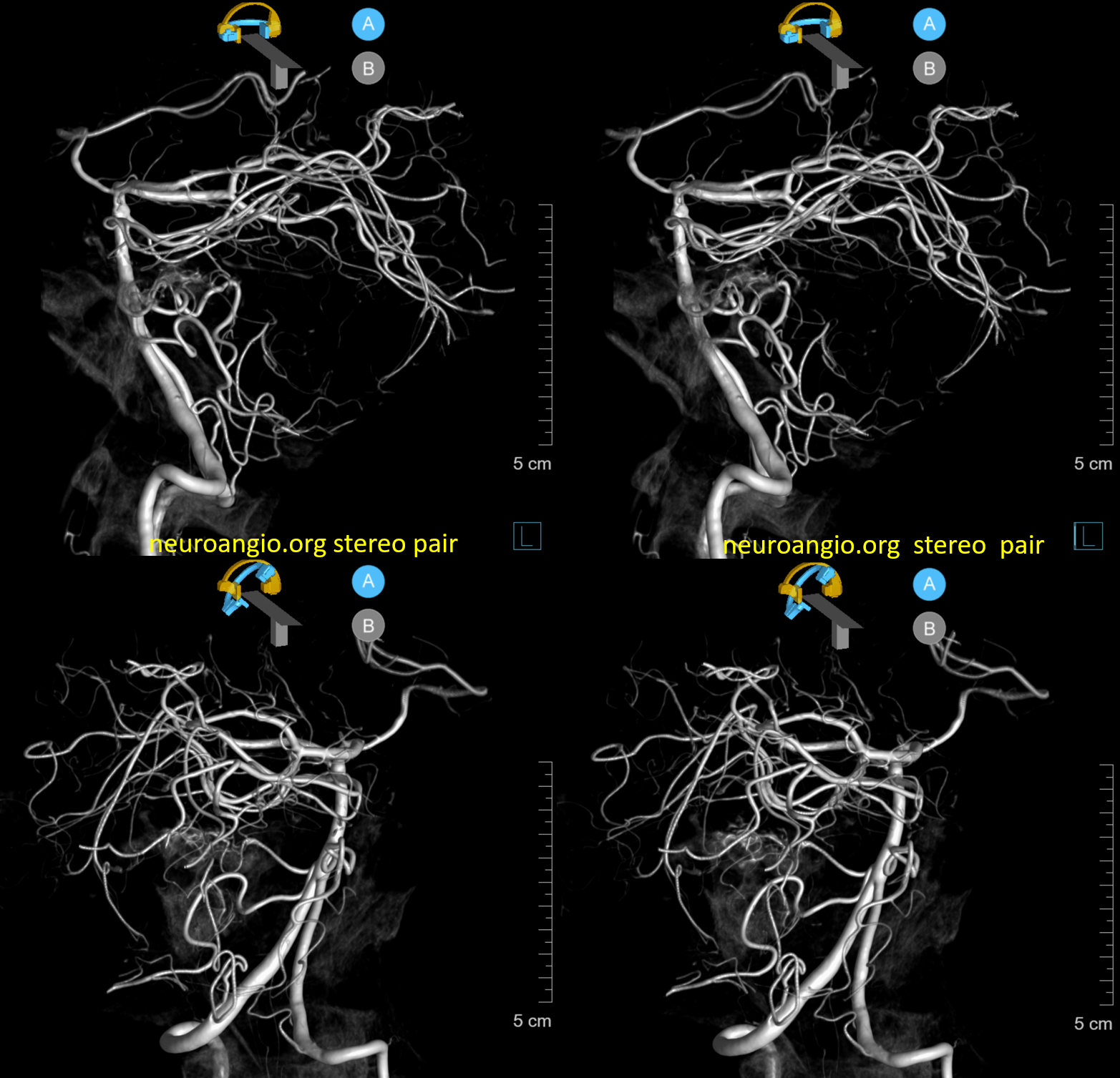
Lateral spinal artery is a pathway by which PICA can be reconstituted in cases of more proximal vertebral occlusion — again recognizing that PICA is a lateral spinal artery homolog — in effect an enlarged lateral spinal artery capturing territory of the cerebellum in addition to the lateral medulla. In this patient, the right vertebral artery is occluded just below the foramen magnum due to dissection. The C1 radiculopial artery (purple) connection to the lateral spinal artery (red) allows for reconstitution of the vermian branch of the PICA (black). The lateral spinal artery inferior to the C1 radiculopial artery is marked with a pink arrow. Notice also presence of the anterior spinal artery (yellow) perfectly contrasting its anterior and medial position to that of the spinal artery. The C1 radicular branch (purple) is in effect the radiculopial artery is acting as a radiculopial artery, homologous to radiculopial supply of the posterior spinal arteries at the thoracic and lumbar levels (see Spinal Arterial Anatomy) The C1 muscular branch (green) opacifies the occipital artery (white) and deep cervical artery (blue).
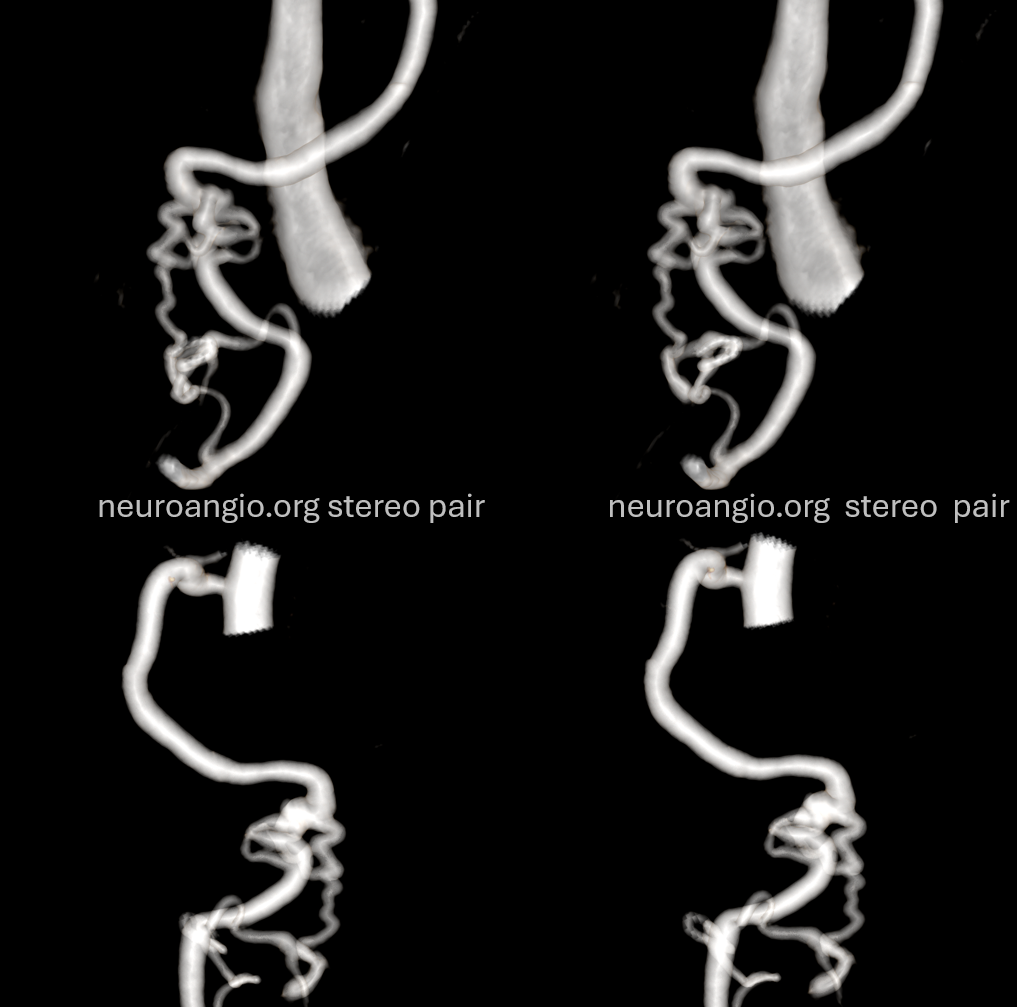
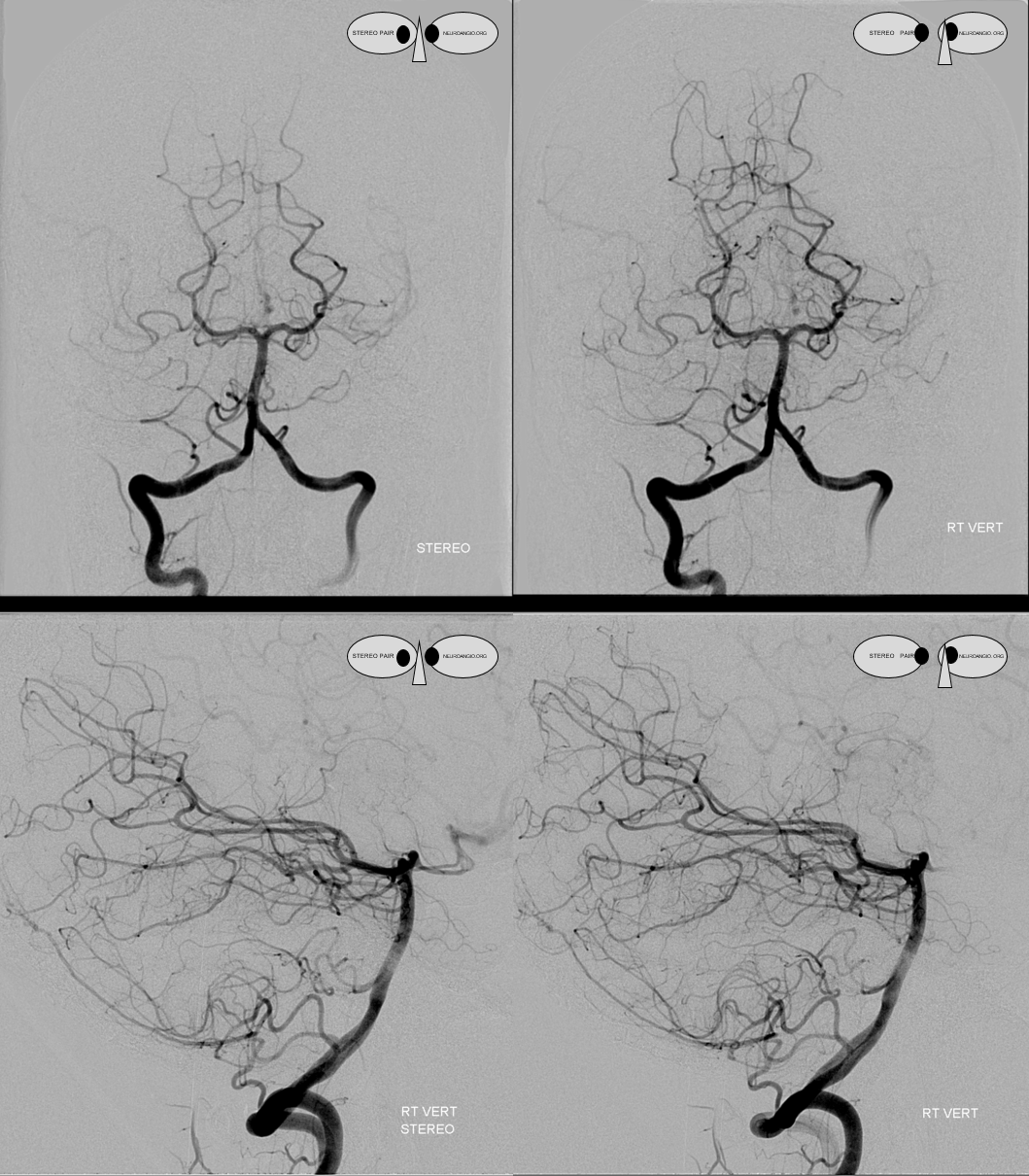
The indispensible STEREO pair
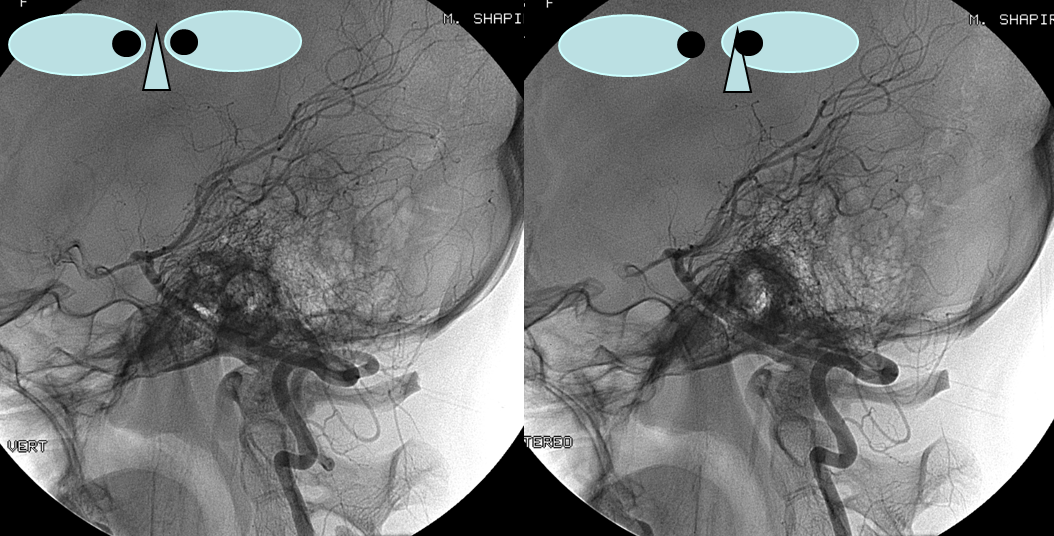
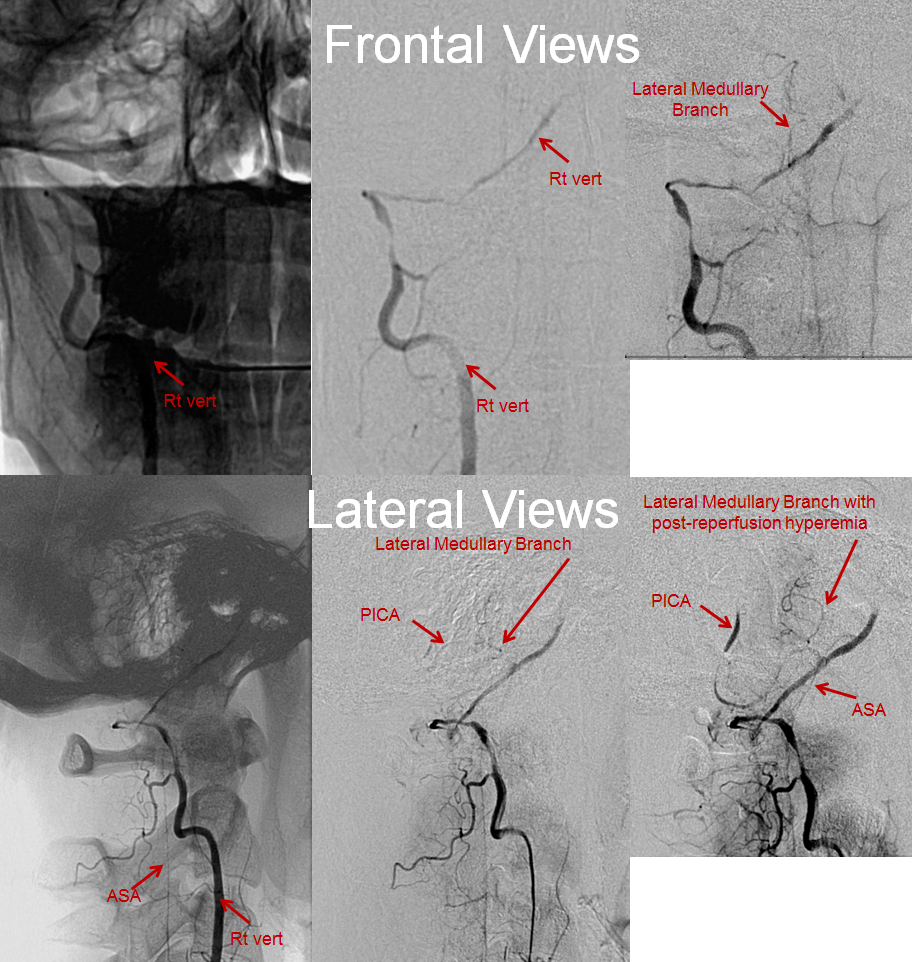
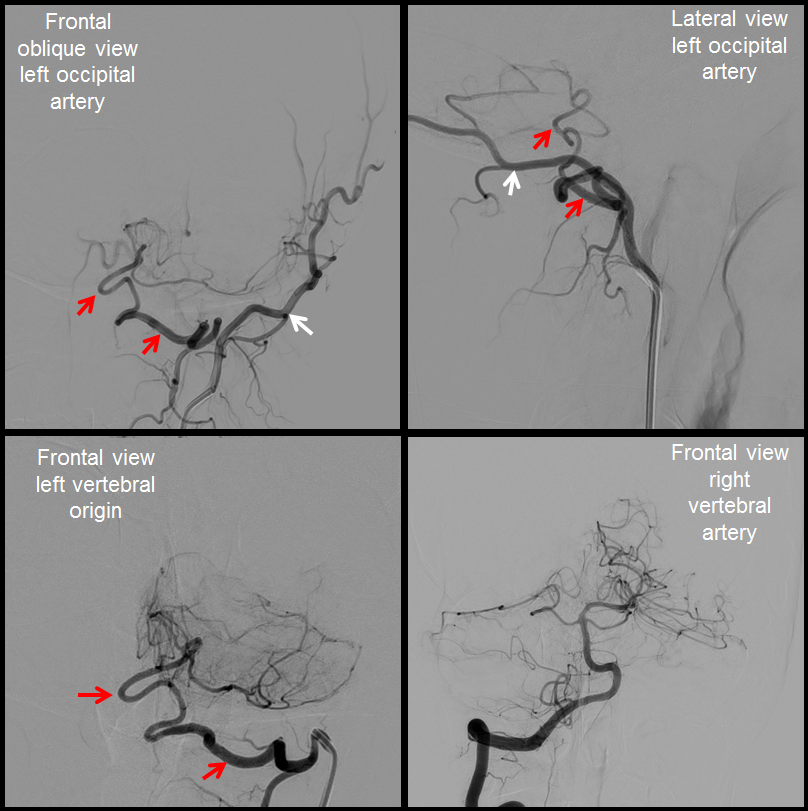
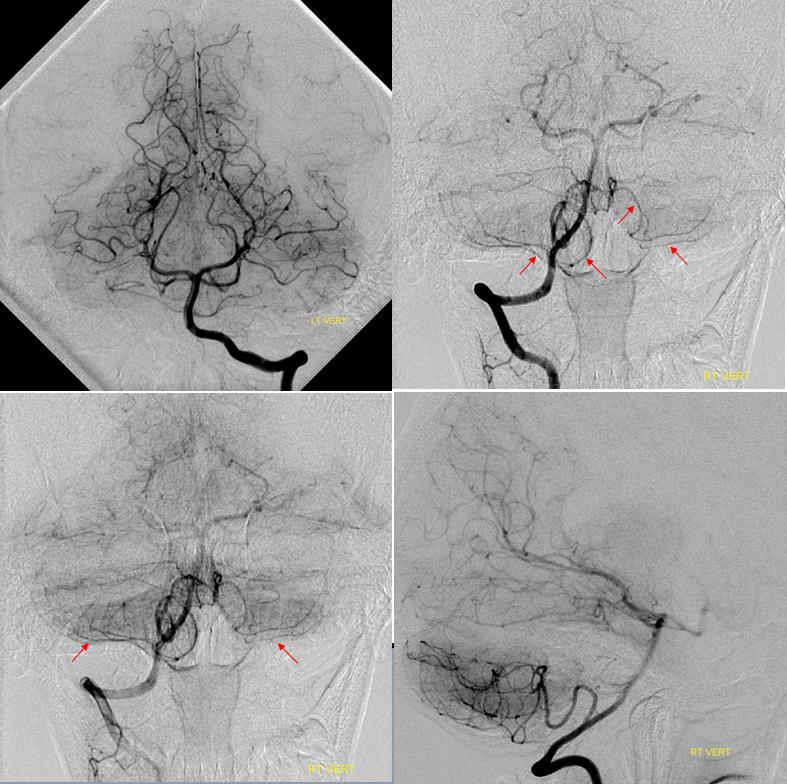

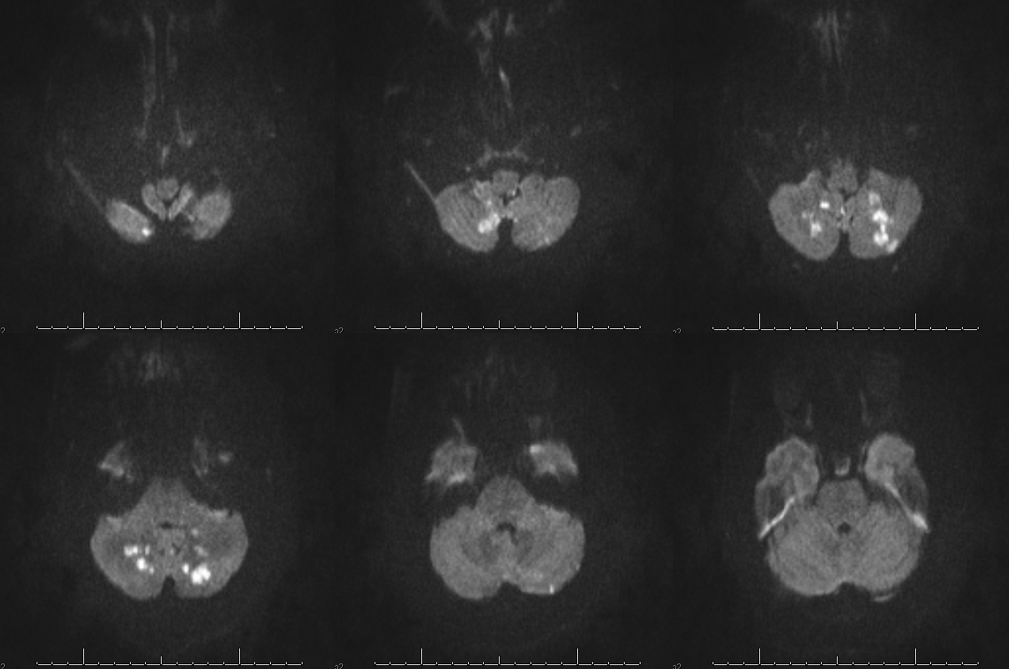
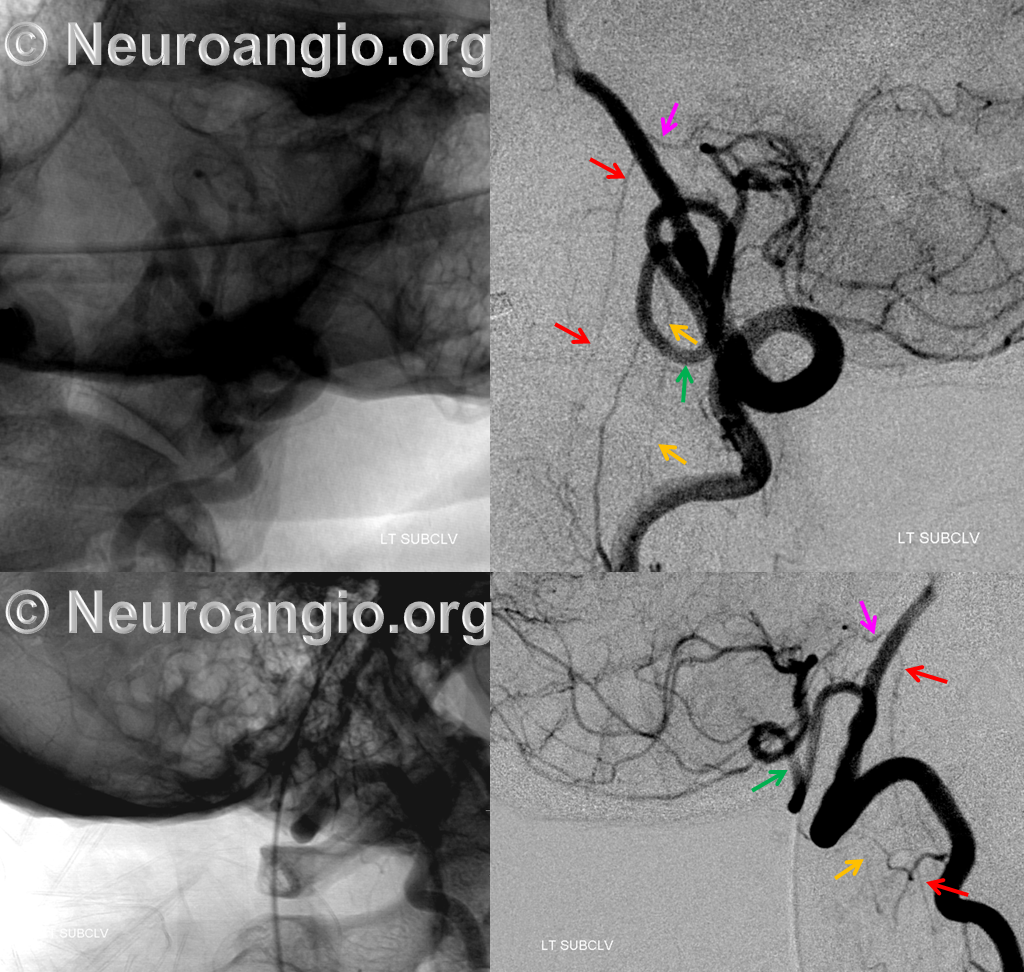
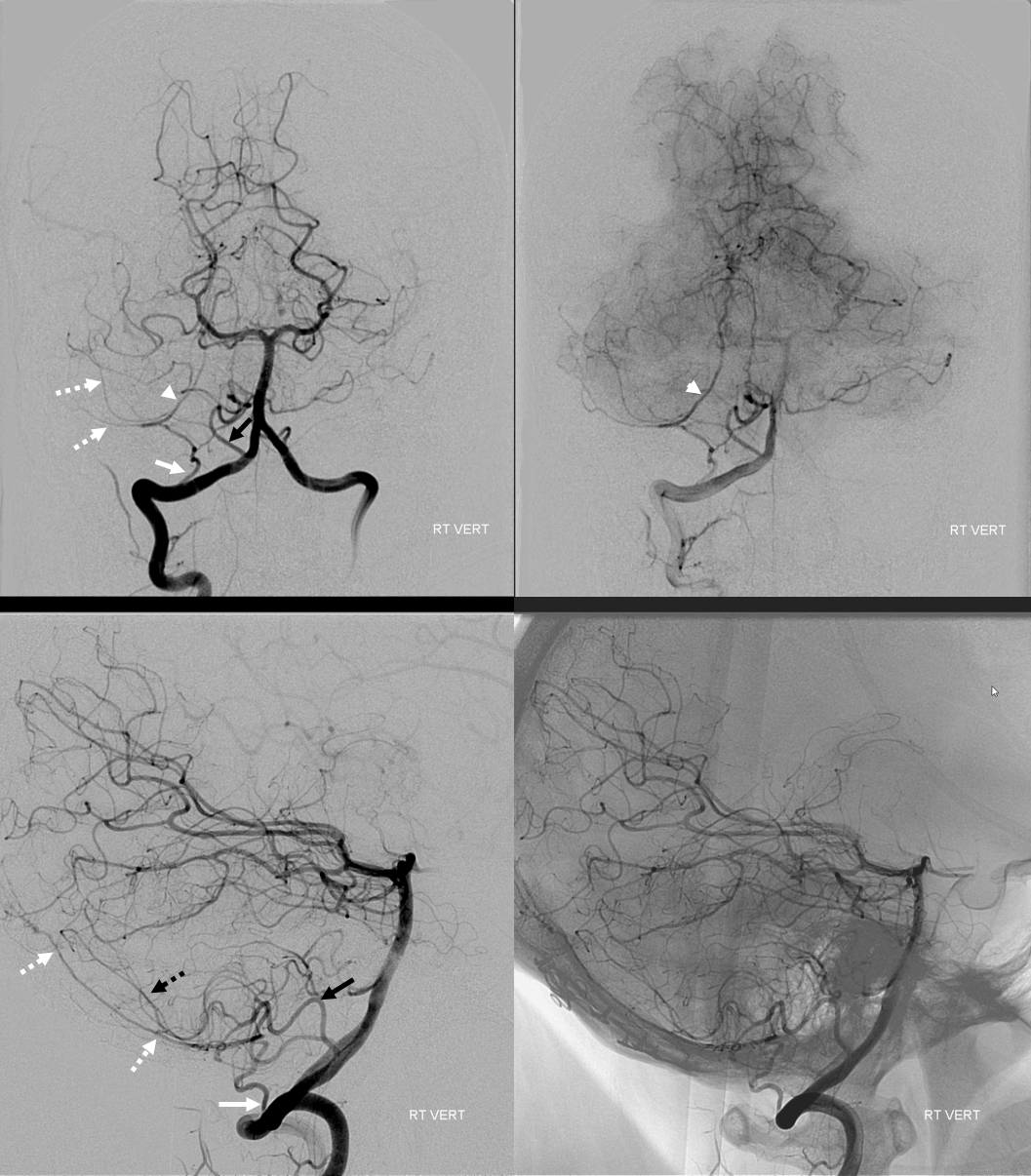
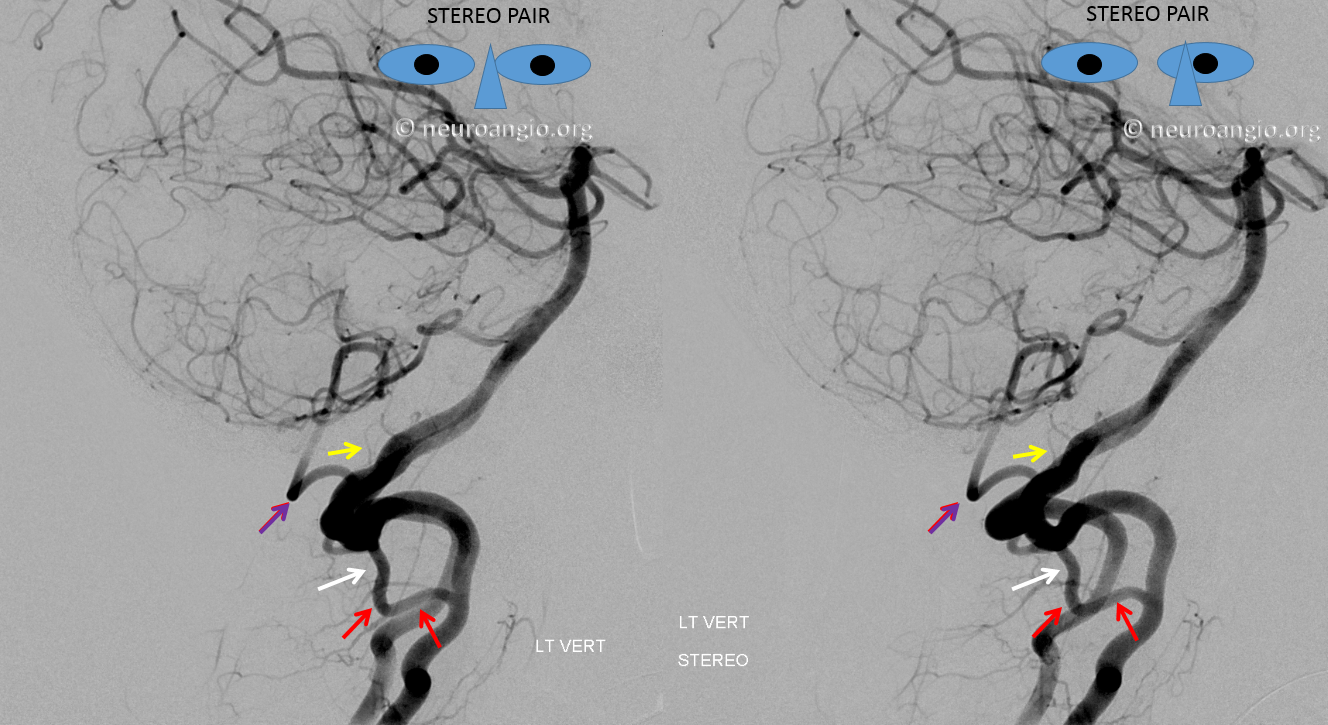
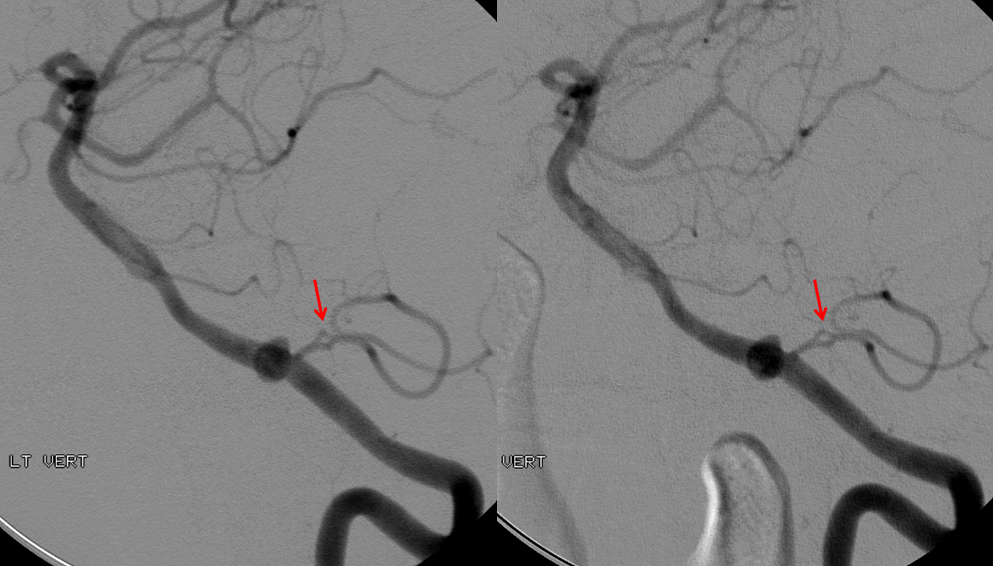
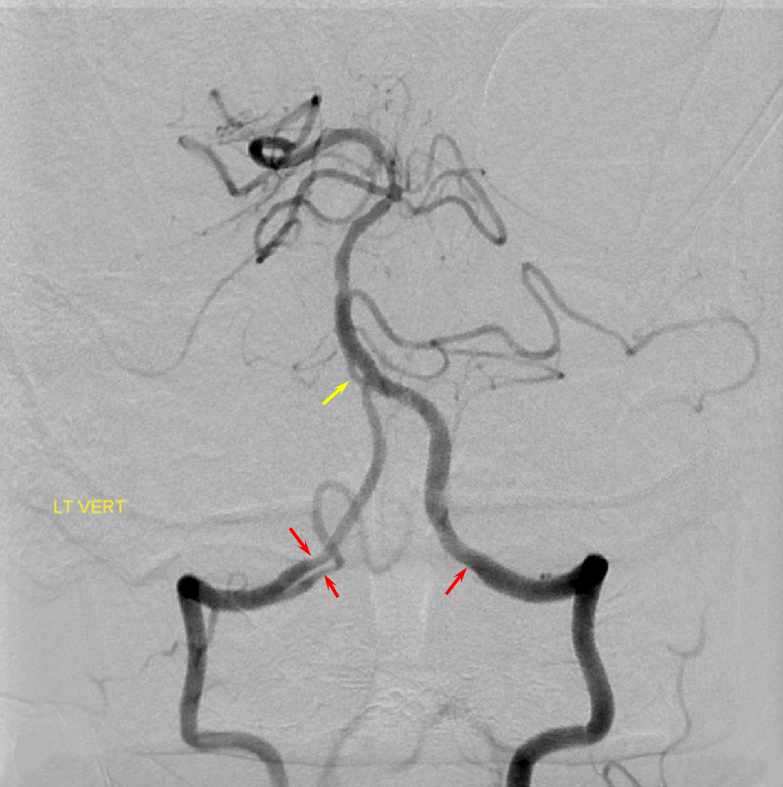
Frontal and lateral angiographic views show occlusion of the left PICA (white arrow) beyond the medullary segment (purple arrows). Notice clot in the proximal medullary segment, best seen on lateral views. The is a dominant large PICA with variant bihemispheric supply (pink and black arrows). Notice truncated appearance where black arrows are corresponding to distal embolic occlusions. the parenchymal blush is outlined by green arrows. How is the PICA reconstituted — the most common way it is — via the Lateral Spinal arterial network at C1 (yellow) and proximal intracranial (red) segments (also see examples below). Notice inferior component of the lateral spinal artery (brown arrow) just below its C1 segment (red arrow). Brown arrow points to the more typical length of the lateral spinal artery, when seen angiographically. The anterior spinal artery is shown by blue arrow, and is of course anterior to the lateral spinal artery. This kind of reconstitution has a propensity to form flow-related Lateral Spinal Artery Aneurysms so follow up is needed.
Third case with anaglyph stereos
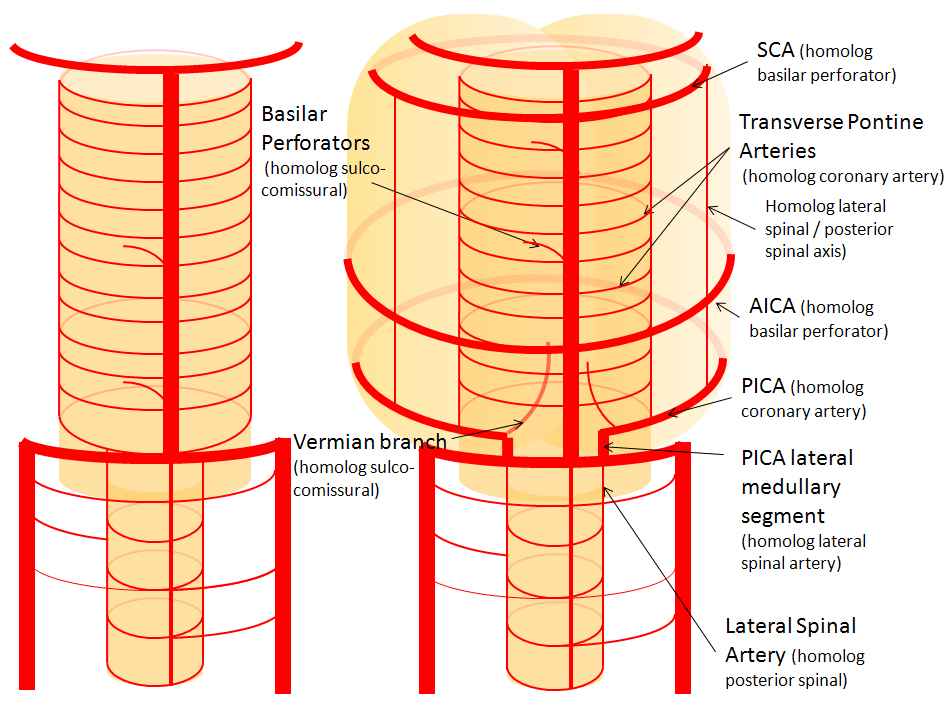
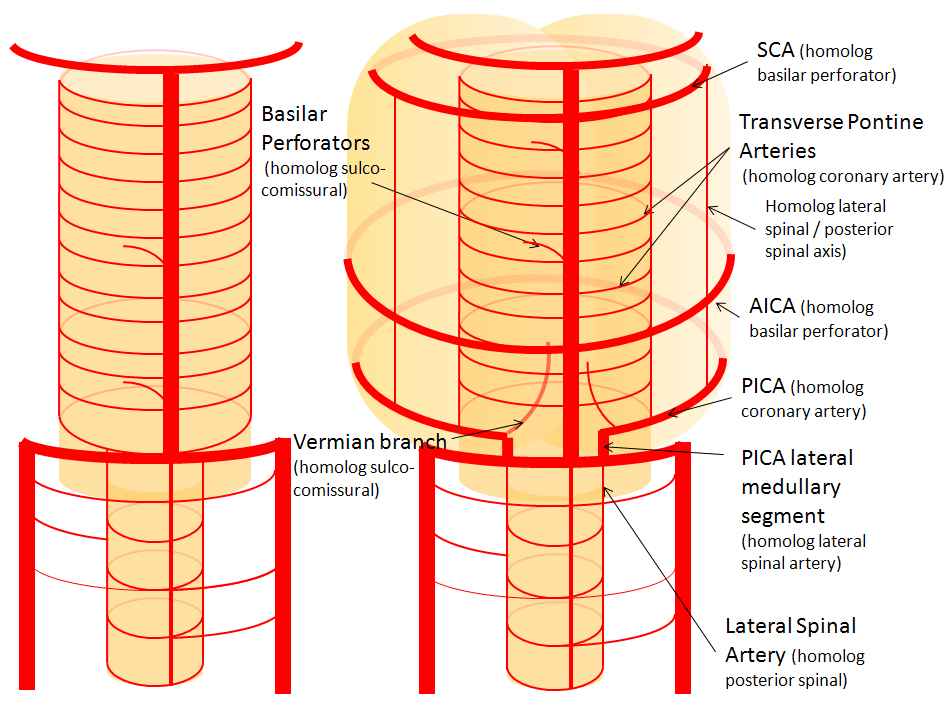
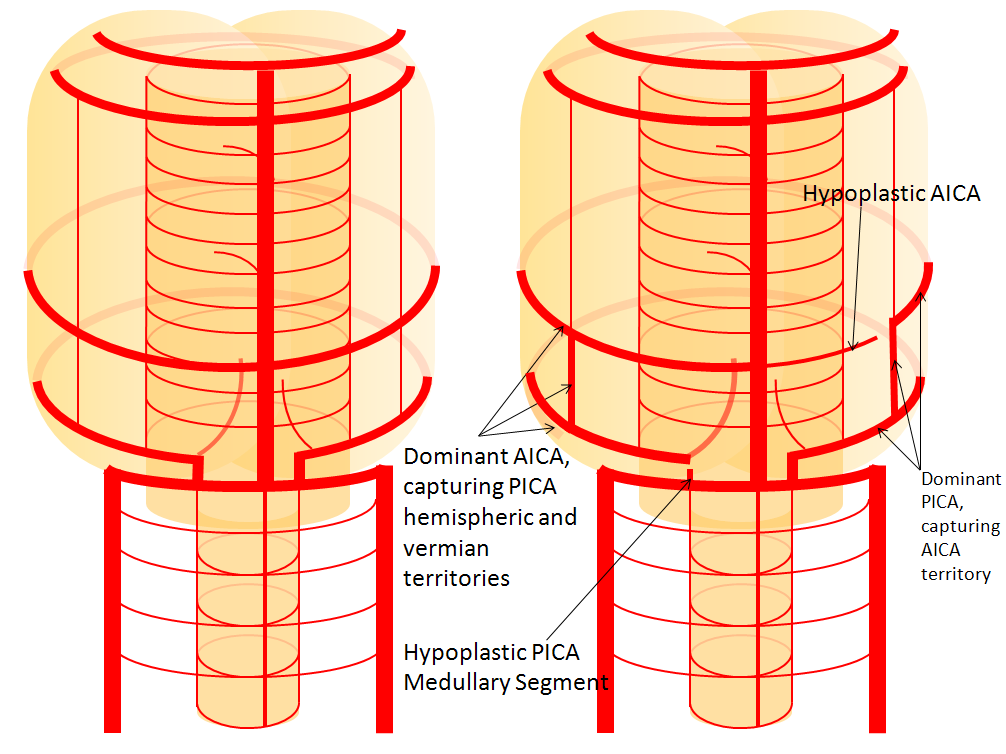
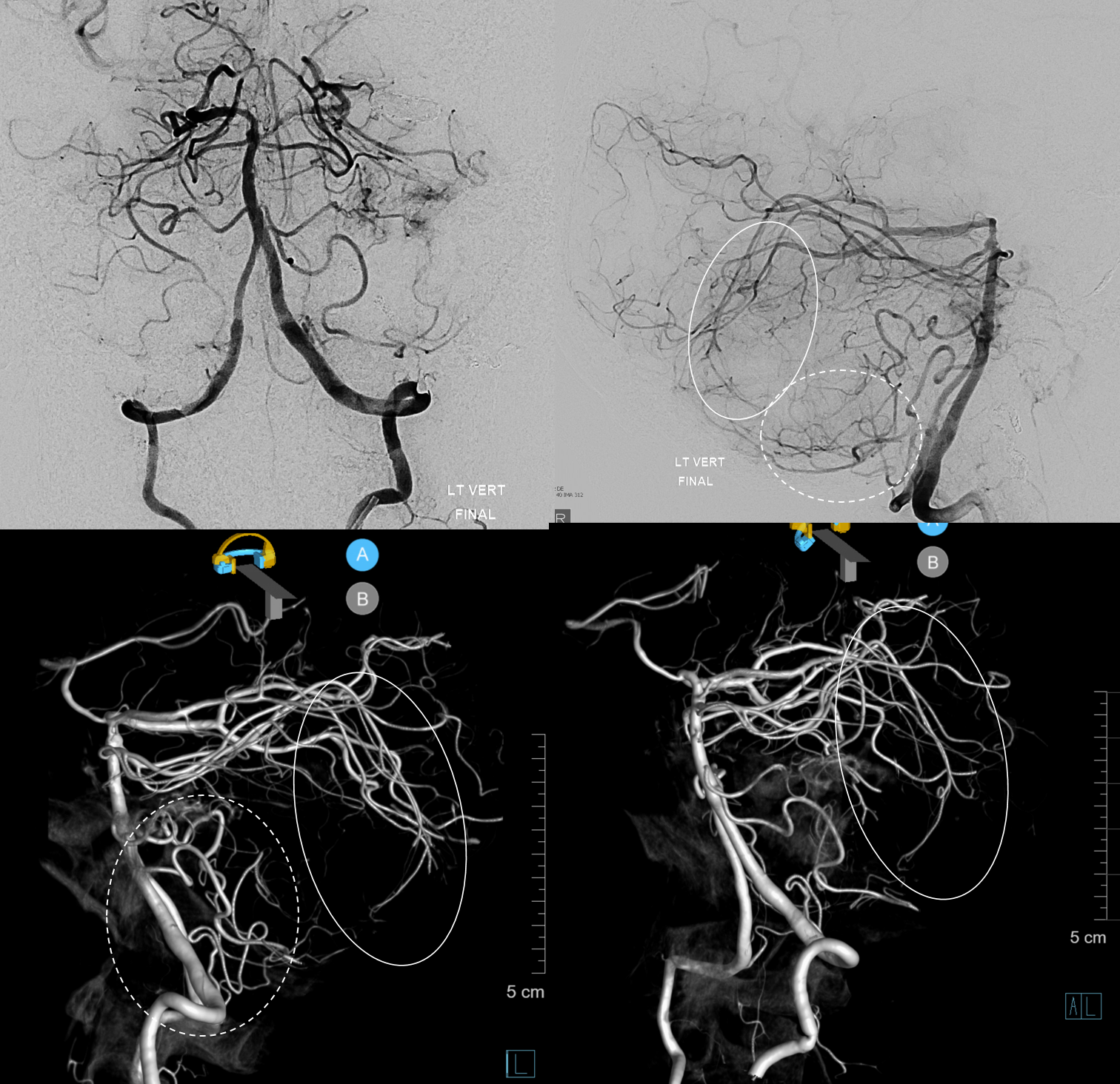
Dominant left PICA supplies left lateral hemisphere and vermis. Small PICA on right goes to lateral hemisphere only. Small AICAs supply the IAC area (they nearly always do). Both SCAs supply the lateral hemisphere territory of AICAs. In the end, its ![]() bumper sticker, and everyone here is actually happy
bumper sticker, and everyone here is actually happy

PICA – SCA Balance
Much less mentioned than AICA-PICA, but its real. The balance is mainly in supply of the vermis (AICA-PICA is usually lateral / hemisphere balance). The superior vermis is SCA, inferior is PICA classically. Below is an example of dominant SCA supply of vermis (solid oval), with a correspondingly small PICA (dominant AICA supplies hemisphere and some inferior vermis, dashed oval)
Stereos
PICA Fenestration
another curiosity, next to an unusual aneurysm arising distal to the PICA ostium. One should at least consider the possibility of dissecting pseudoaneurysm — an incidental finding in this patient. STEREO PAIR.
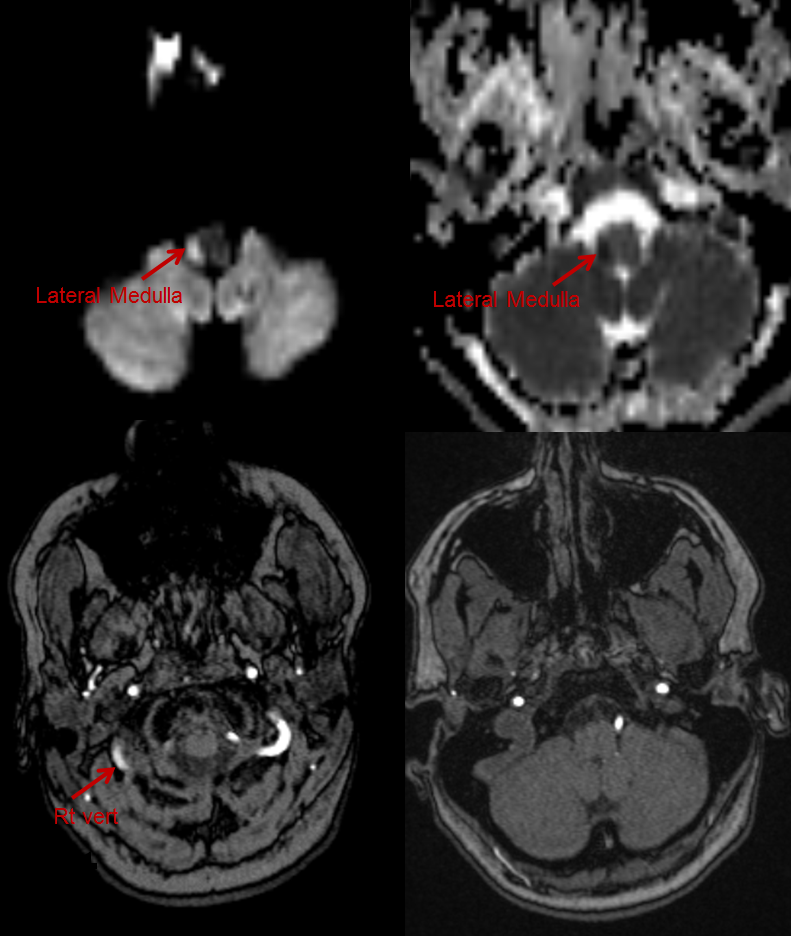
PICA Dissections
Quite common. Can happen at the ostium or more distally — usually at the tonsillar segment where the artery traverses the foramen magnum. Often present with hemorrhage and an obvious pseudoaneurysm, though sometimes aneurysm is not identifiable — see corkscrew vessels, pseudo-fenestrations (additional channels reconstituting post-dissected segment). Deconstructive treatment option is good if lateral/posterior spinals can be identified and risk-stratified. Reconstructive options favor flow diversion, especially when there is no hemorrhage.
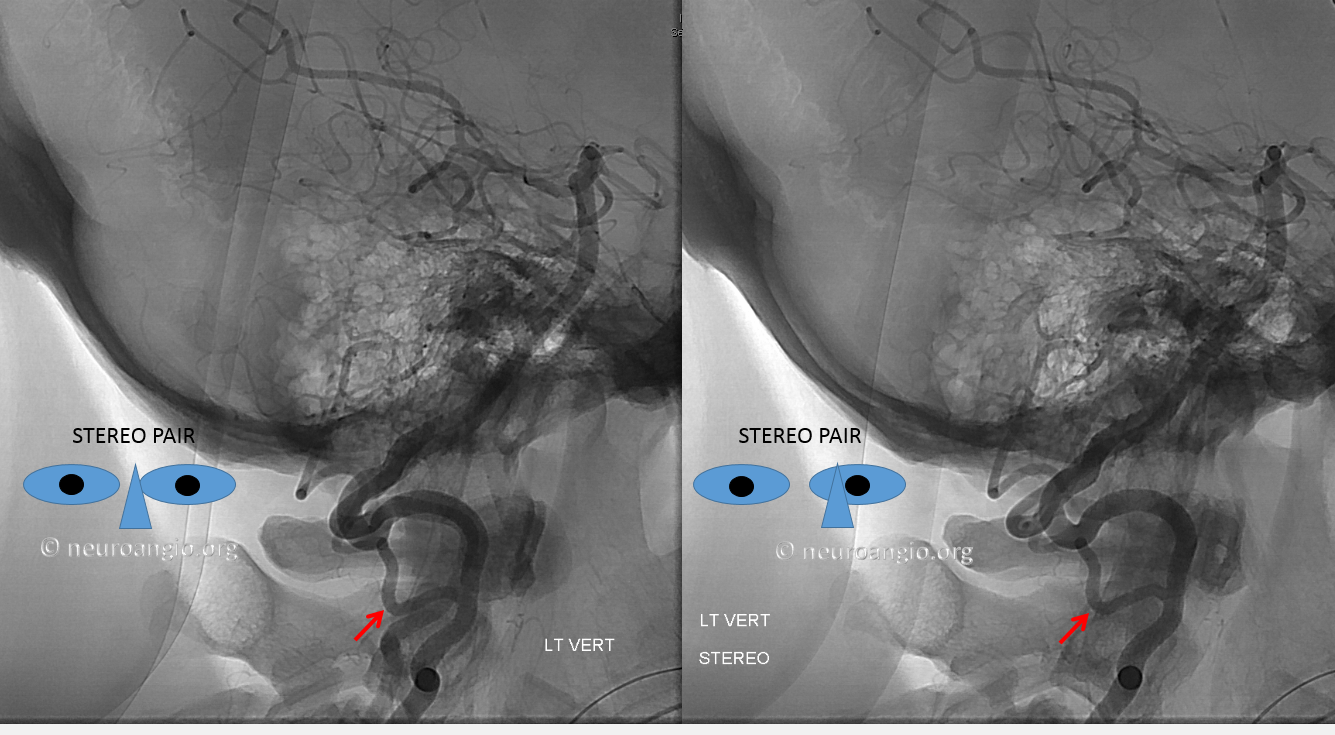
Here is an example of hemorrhagic dissection — hard to make diagnosis here, but can be suspected

More angio
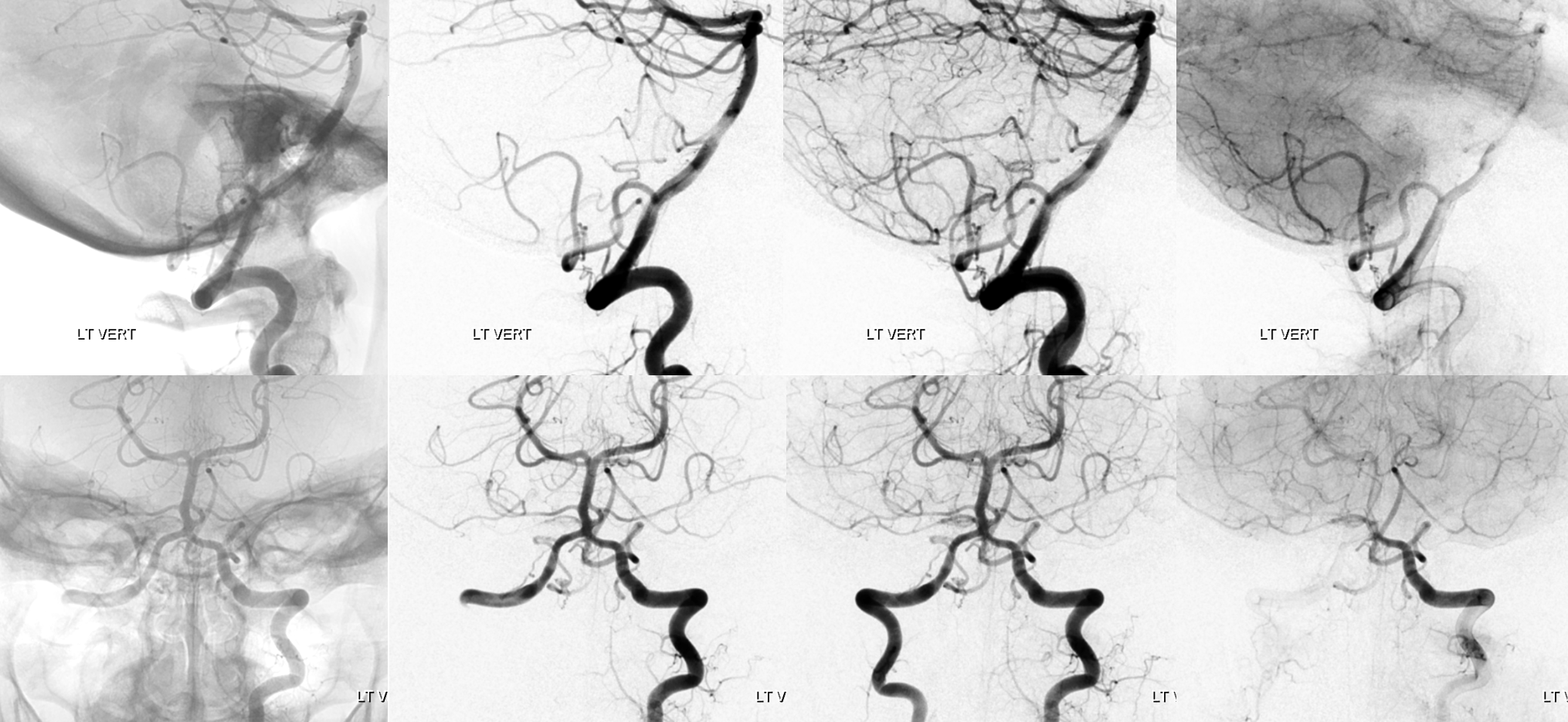
Not much to be seen in the standard DYNA — even the region of interest is not there

More suspected from a dedicated view of the standard recon
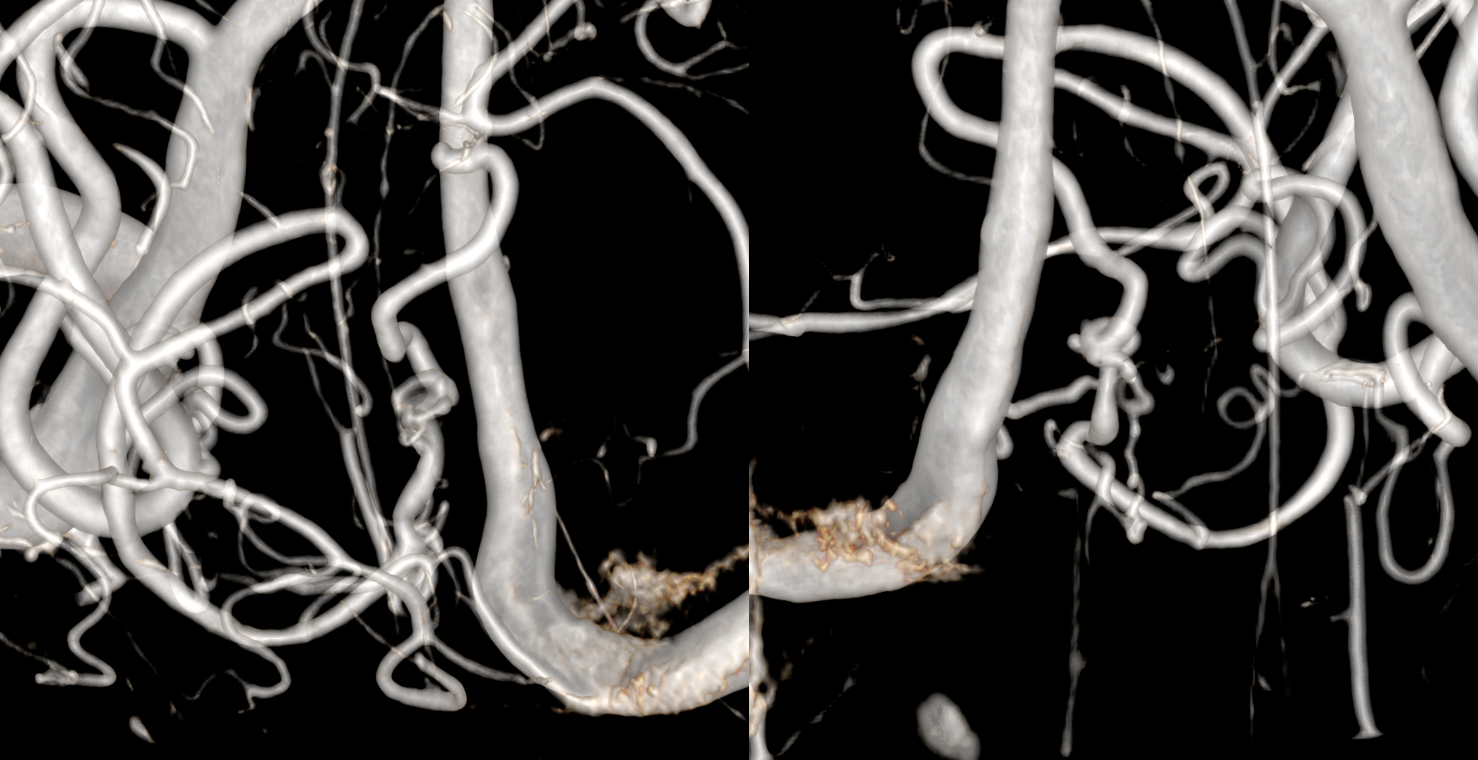
With more image manipulation, diagnosis is certain. That two channels reconstitute the distal PICA — strongly suggesting that the dissection has been around for some time, and hemorrhage likely comes from the hypertrophied new channels reconstituting the distal PICA — they used to be microscopic and are do not do well being many more times their intended size. This is a similar process to what is seen with hemorrhagic Moya Moya