This page is dedicated to Dr. Fedor A. Serbinenko

Yet, I am not sure how many care about BTO anymore. Pipeline killed the BTO star, or at least wounded it pretty badly. Nevertheless, I hope this will turn out to be a useful guide for those who do not do BTOs often. For those that do, this page is just a show of how we do it. I am sure its different from how you do it — in fact, I don’t think any two people do BTO the same way. Why we do it this way will be shown as we go along.
We do BTO under general anesthesia and rely on venous phase delay to give a dichotomized pass/fail grade. In our opinion it is as good or better than neurologic exam, with the advantage of being substantially shorter, thereby minimizing test occlusion times. In most cases the balloon is up for less than 3 minutes
So, here is the approach for the bread-and-butter internal carotid BTO, NYU style
- Place patient under general anesthesia
- Obtain dual arterial groin or radial access, or combination thereof
- Do at least 3 vessel diagnostic angiography — two internals and a dominant vert, or both verts
- Place your favorite compliant balloon into the petrous segment of the test ICA but do not inflate
- Place the second diagnostic catheter into the contralateral ICA
- Set up your frontal view to include both hemispheres
- Give as much heparin as you think you need
- Check with anesthesia regarding blood pressure — what is the pressure now relative to what it is at baseline. Most of the time, the pressure will be lower under GA, so that is your hypotensive challenge
- Obtain a roadmap of the vessel being tested
- Inflate balloon
- Do a run of the ipsilateral guide (on side of balloon) in biplane to confirm full balloon occlusion of the ICA and see potential ophthalmic, ILT, and other ECA-ICA collaterals. The more ECA-ICA collaterals there are, the worse the circle of Willis is and the more likely the BTO will be a “fail”
- Do a run of the contralateral ICA. Only frontal projection is useful. Make sure to inject enough contrast (10 ccs or so) and image the run well into the venous phase
- Reposition the contralateral ICA catheter into the dominant vert and do a biplane run of the head to see PCA / PCOM contribution to the side being tested
- Deflate balloon
- Do a run of the internal carotid artery after test to check for dissections, emboli, spasm, etc.
- Analyze images. We do our standard runs at 2 frames per second for the ENTIRE run. A delay of more than 1 seconds in venous phase between the open and the occluded hemispheres is a fail. There are many methods, ranging from this very qualitative one to some sophisticated quantitative approaches. It is not clear that any one is better than another, at least to me, and so many things change over time that extrapolating conclusions will always have some false negative rate. See examples below for clarity.
- Extrapolate this method to other sites of BTO — we rarely do ICA BTO now. However more often we do intracranial branch BTO (say someone has a mycotic aneurysm of the rolandic branch. Can this branch be proximally sacrificed?). Needless to say, the catheterization should be quite careful and balloon inflation also to avoid vessel rupture. GA is quite helpful for these, and familiarity with how to do interpret BTO based on images is equally important, since reliable clinical exam may not be available for different branches. Usually there is no need for dual catheter access as the collateral for the branch being tested is typically in the same territory as the parent carotid or vertebral artery.
Below are some examples
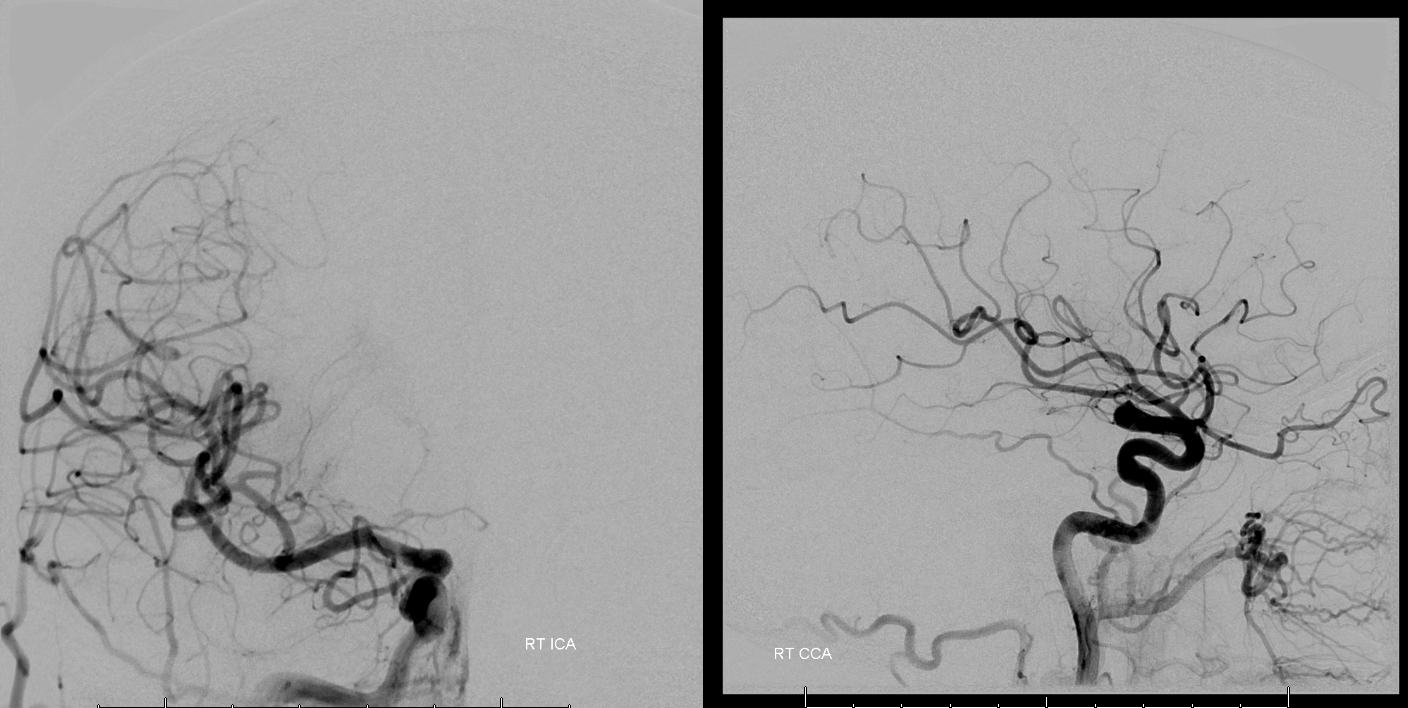
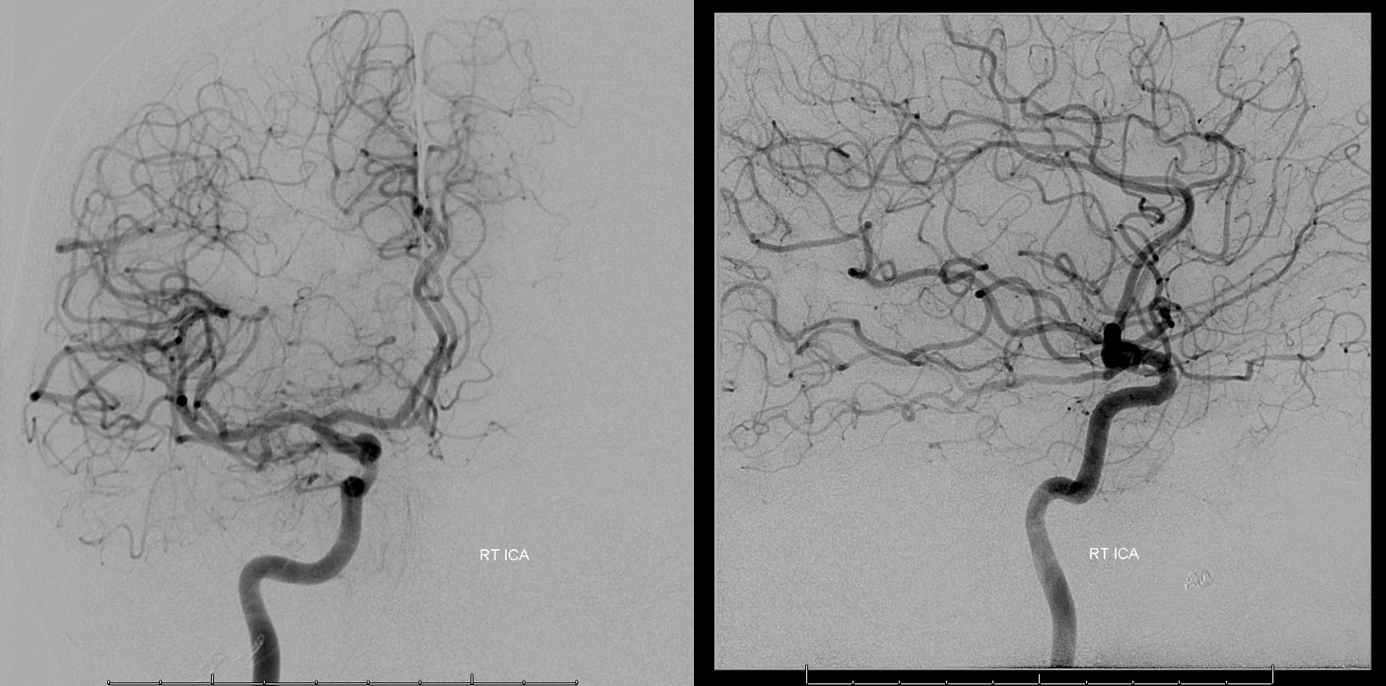
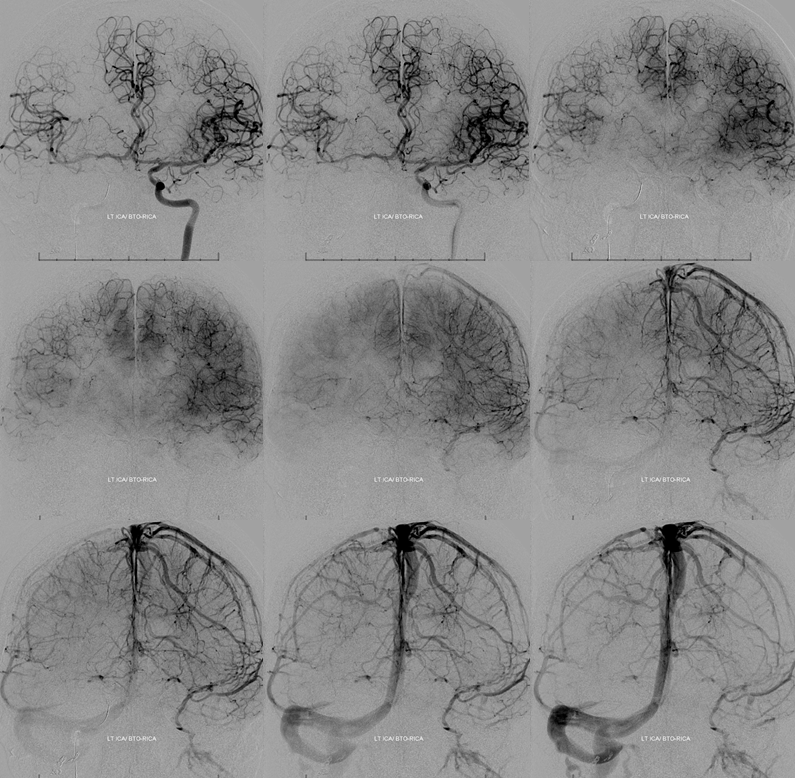
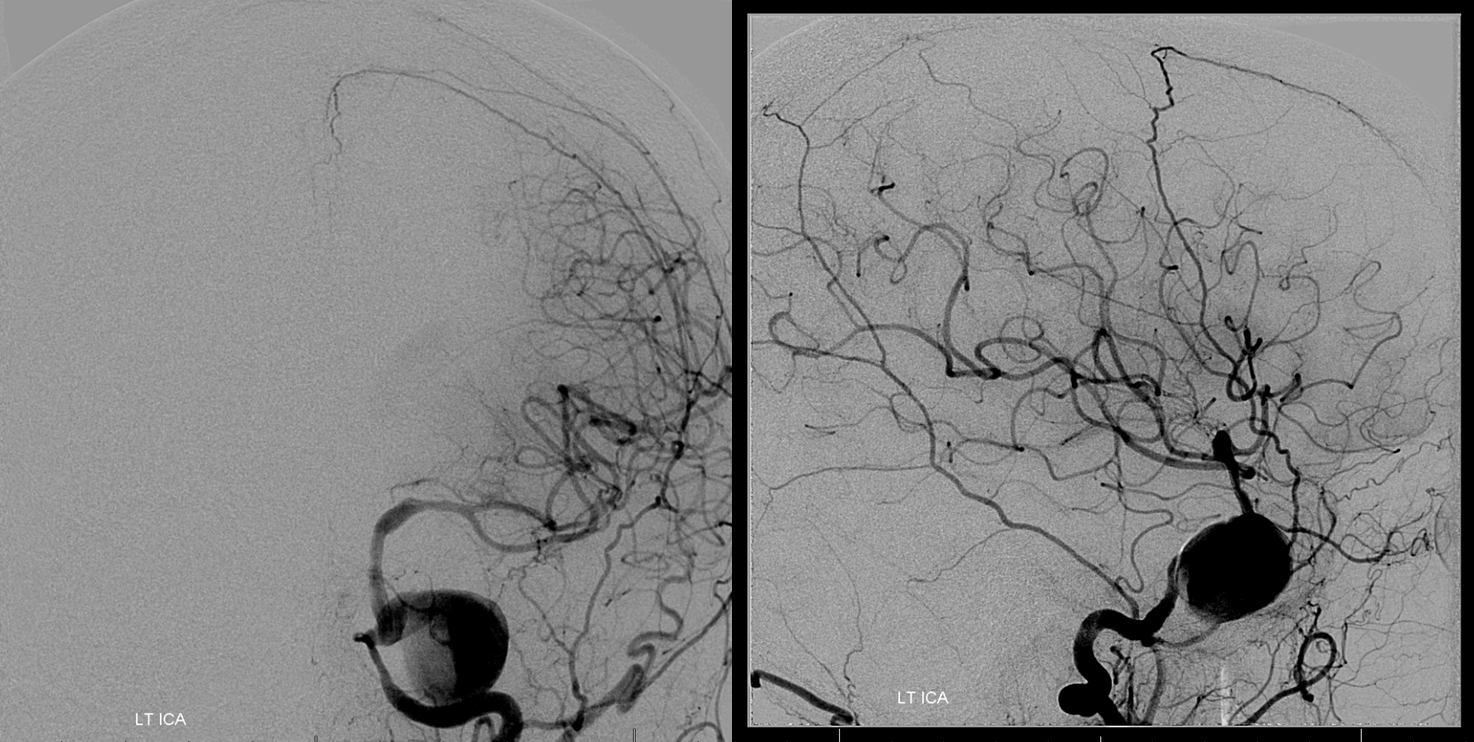
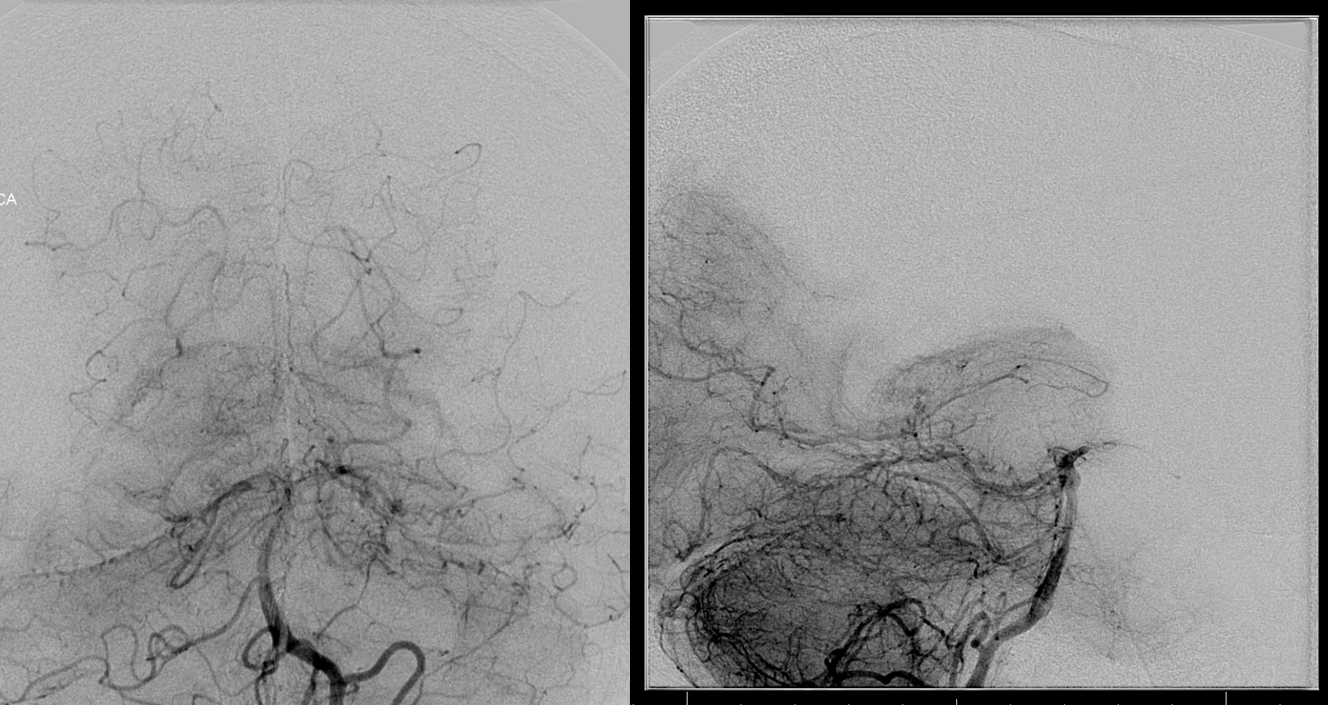
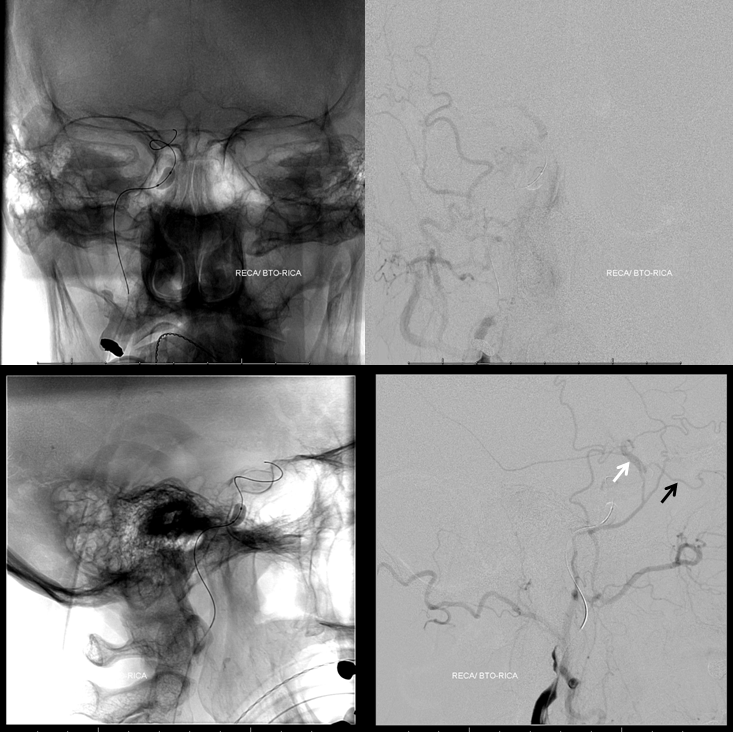
Case 1 — humongous glomus — preop BTO and embolization. Case courtesy Dr. Tibor Becske and Dr. Chandra Sen
Right CCA

Right ICA
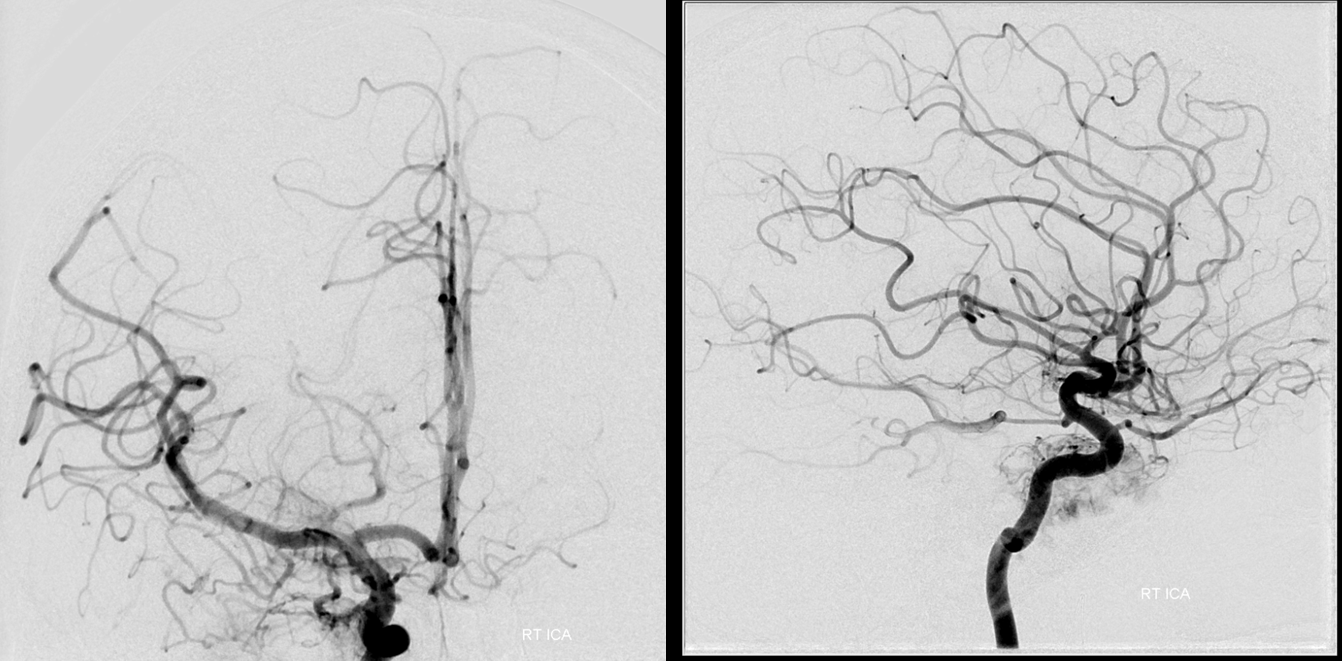
Left ICA — notice reflux into the right M1, flash-filling what looks like bilateral well-developed A1 segments and ACOM. That’s pretty much a BTO pass right there. Fenestrated MCA variant
Right vert — the dominant vert.
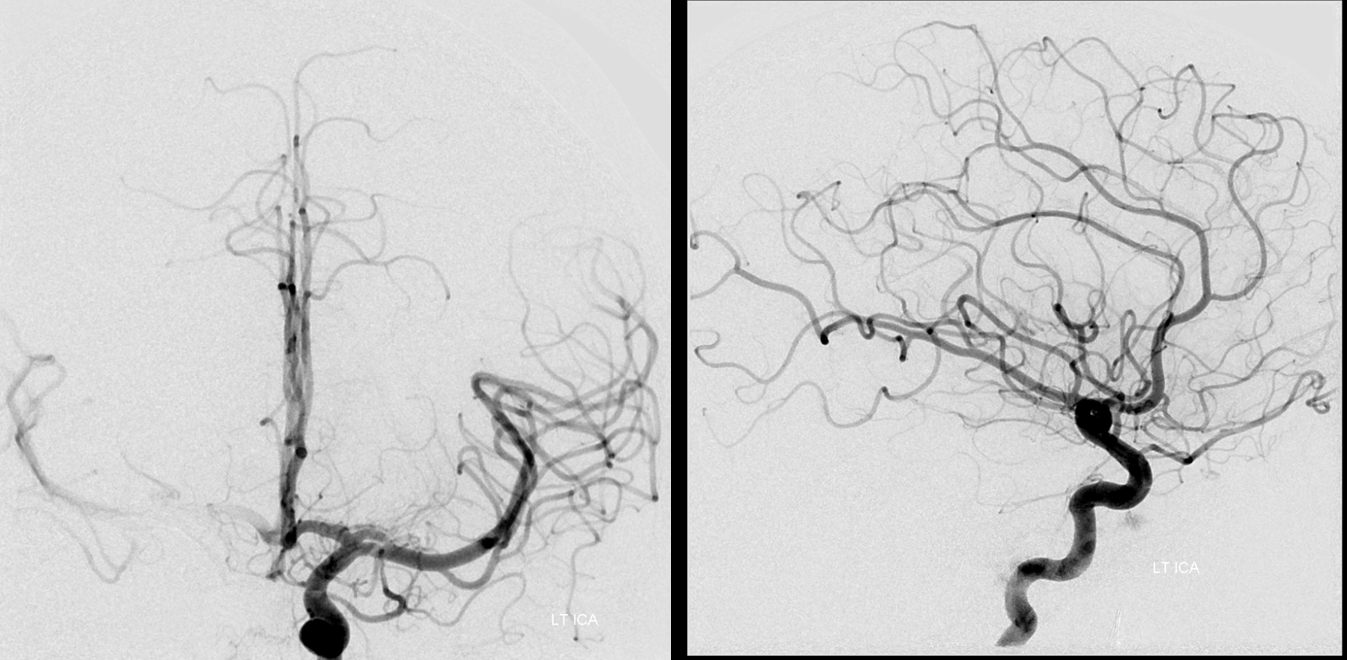
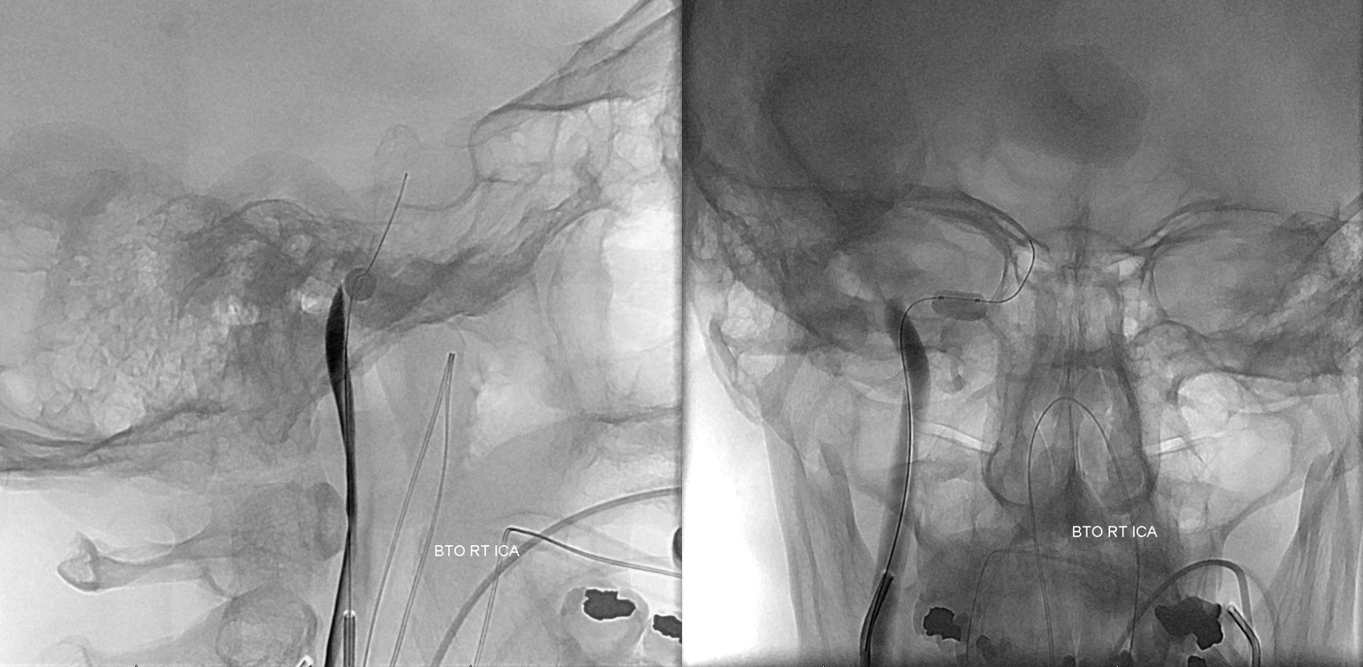
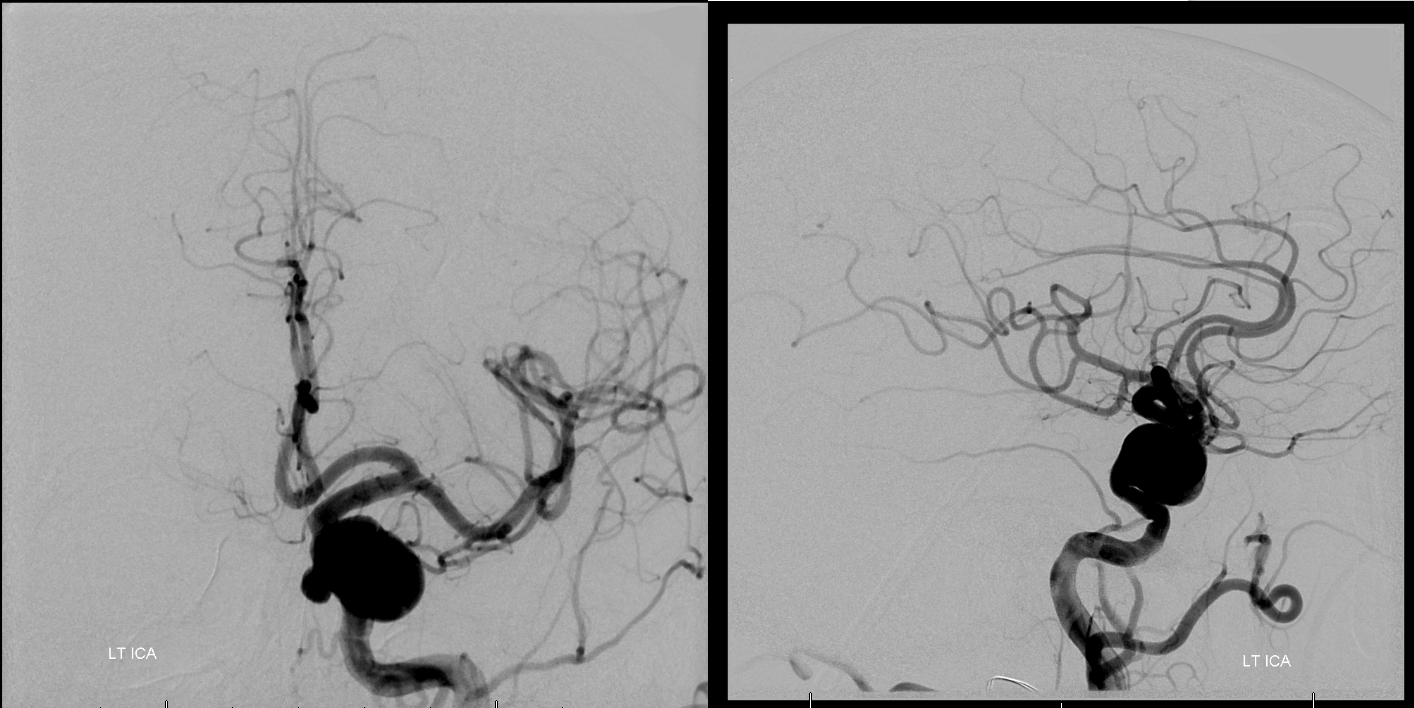
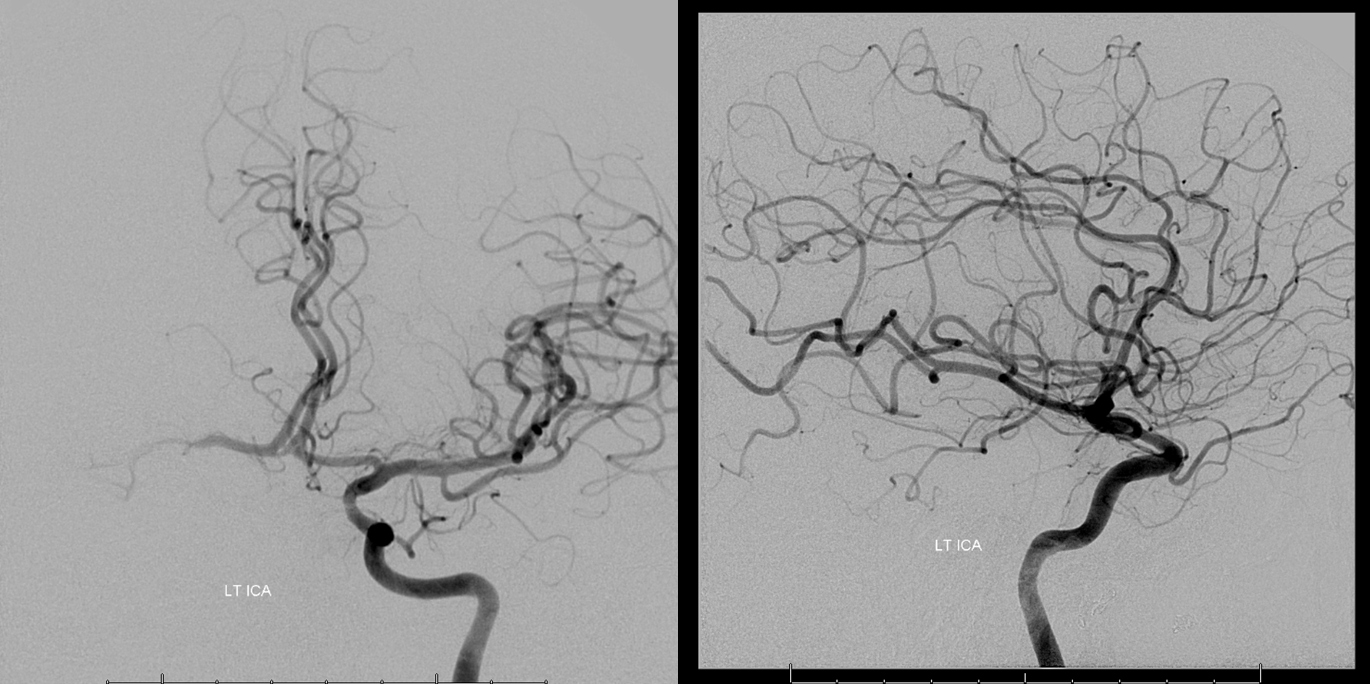
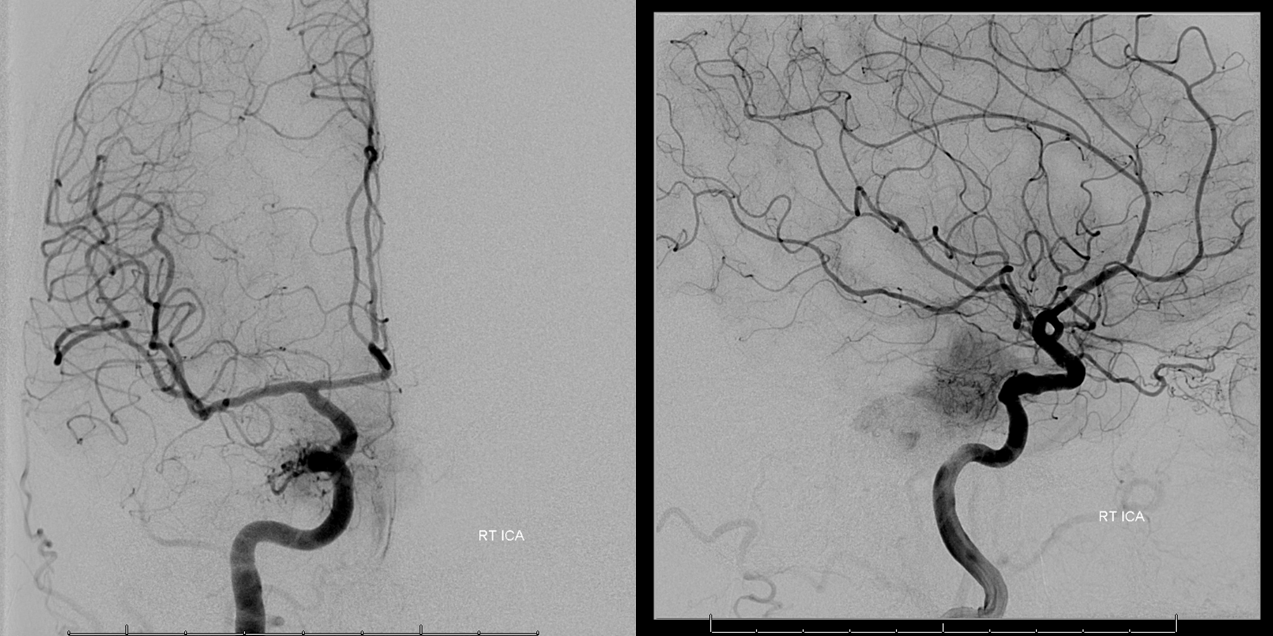
Balloon is inflated in the horizontal petrous segment — safest place — the bone protects against over-inflation and there is little chance of spasm here. Run through right ICA guide confirms occlusion. The ECA collaterals were not studied
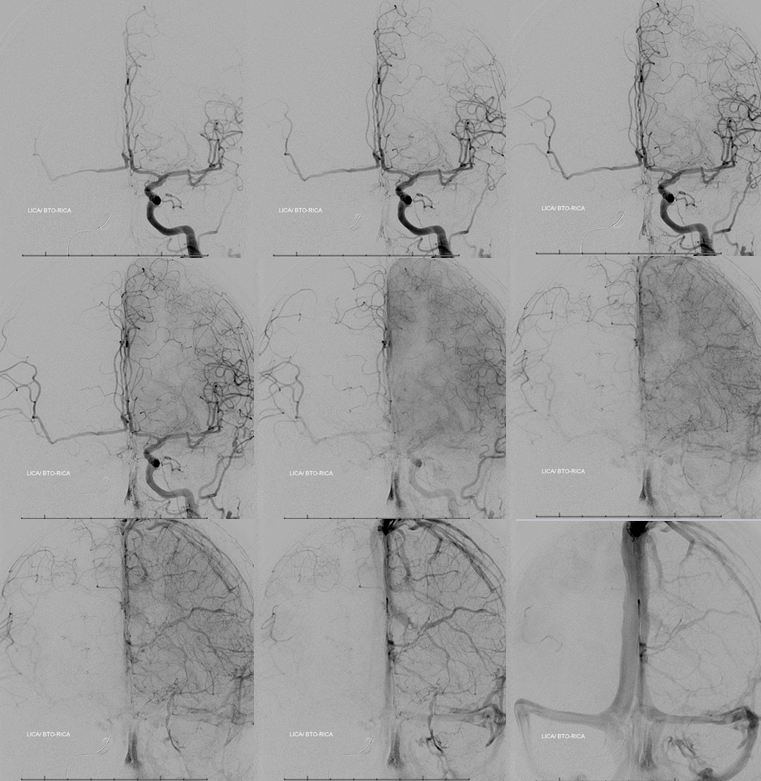
Left ICA run, frontal projection only. Key images here. Looks like a pretty good ACOM in the arterial phase. However, venous phase is a better judge. Notice that the whole right hemisphere is “washed out” — not as densely opacified as the right. Is that a problem? No. In fact, that’s great. Why? Because it means there is another source of inflow besides the ACOM — namely the PCOM. So, DON’T look at the degree of opacification. Look at the TIME curve of opacification. Look at the bottom two rows. See how the venous phase of the right hemisphere barely lags behind the left one — maybe by 1 frame. Sure, the veins are less densely opacified, but they are pretty much 1 frame apart from being in the same phase. The last row is the best one to judge that. That’s a solid pass. Also, isn’t it nice to have your BTO done under controlled conditions, without movement, letting you calmly do your thing and deal with any possible issues. That’s why we like GA so much. Plus, it usually offers a simultaneous hypotensive challenge.
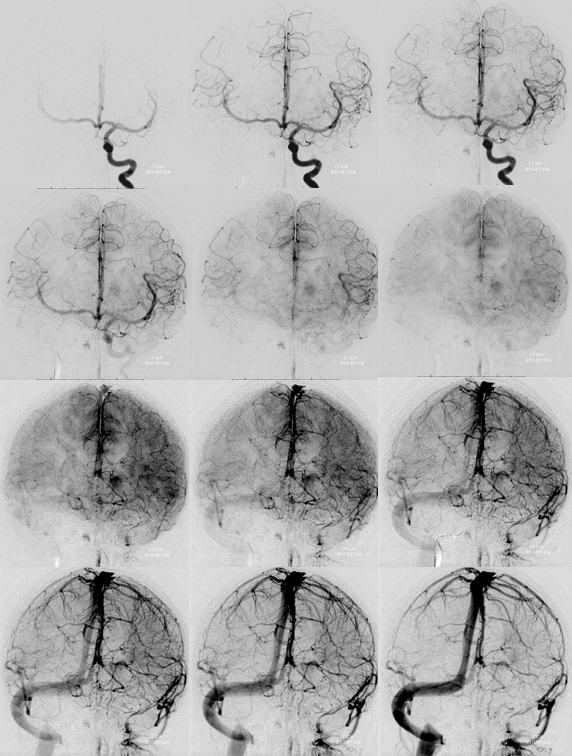
Done? Probably yes, in this case. However, it is always best to do a complete angio, unless there are major reasons not to. Which means repositioning from left ICA into left vert. Usually that’s pretty straightforward. There is nice support coming from the PCOM as well.
Lateral view. The PCOM would have been too small to carry the ICA alone, but together with the ACOM its a solid pass
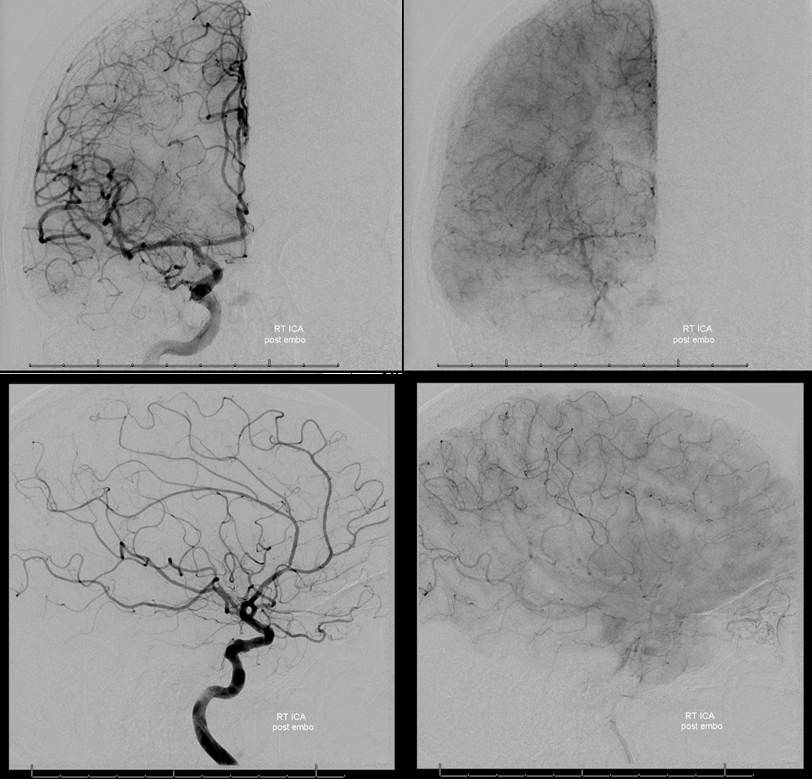
Post-embo view of the right CCA — see Technique Preoperative Brain Tumor Embolization page for more on how to achieve nice results like this one
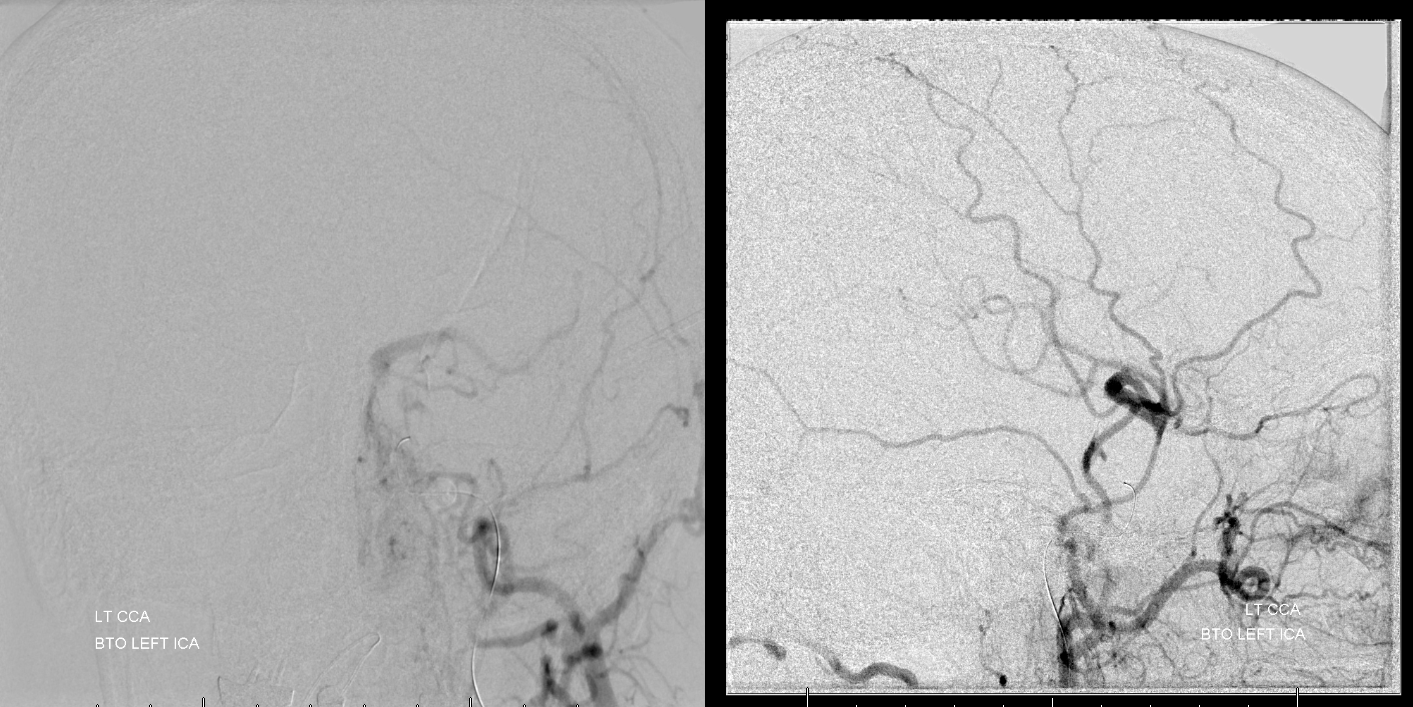
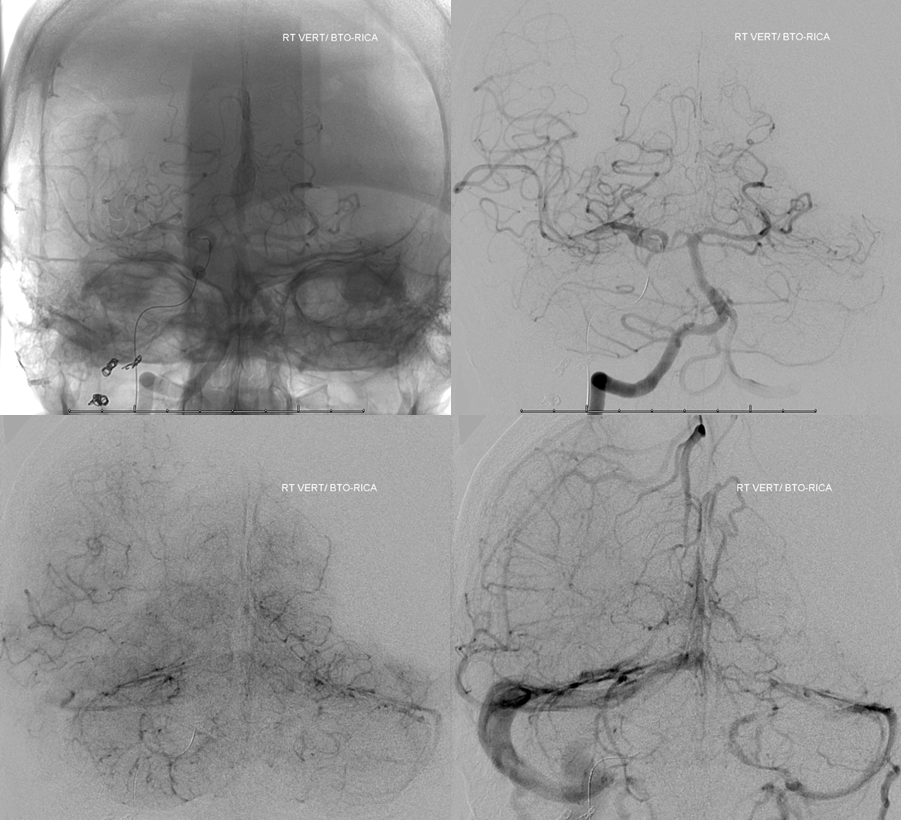
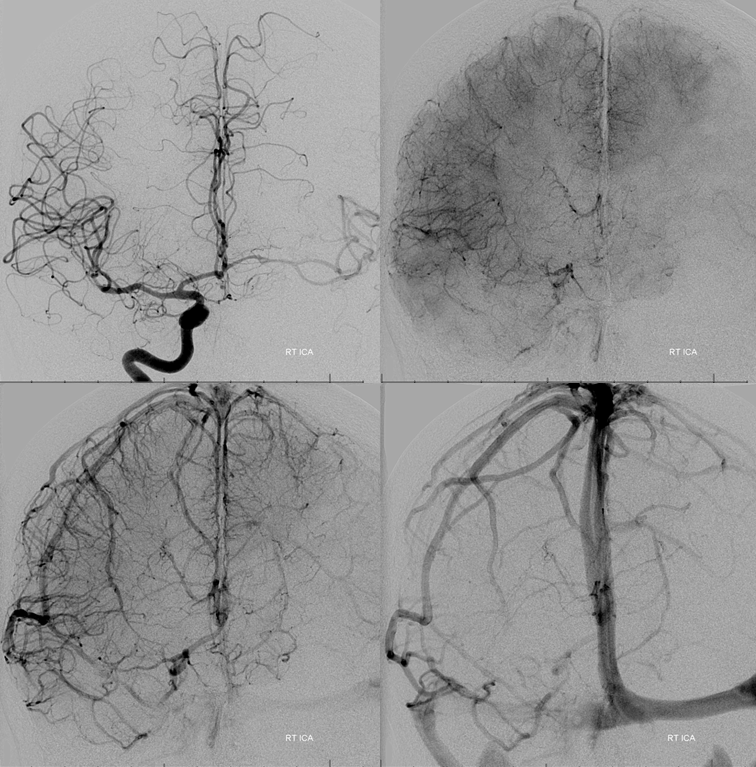
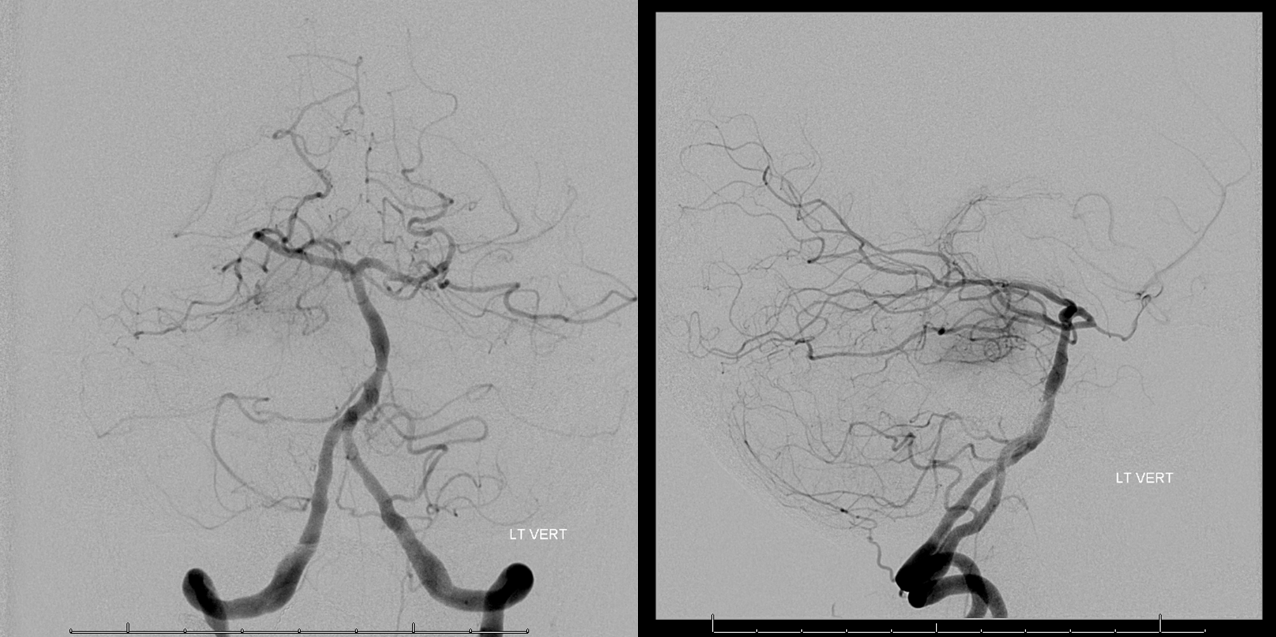
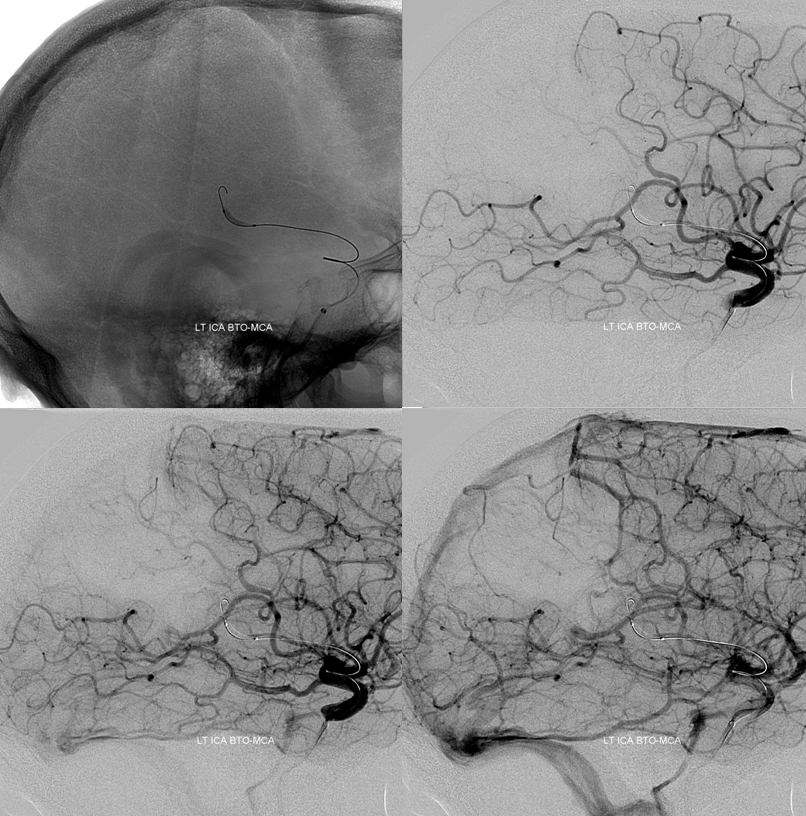
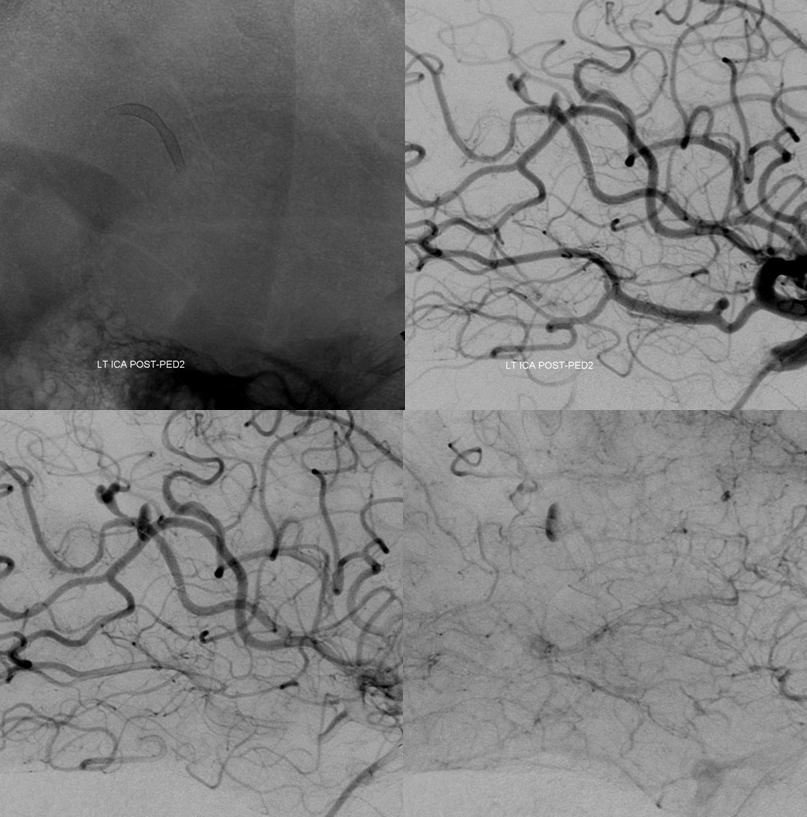
Case 2 — giant aneurysm
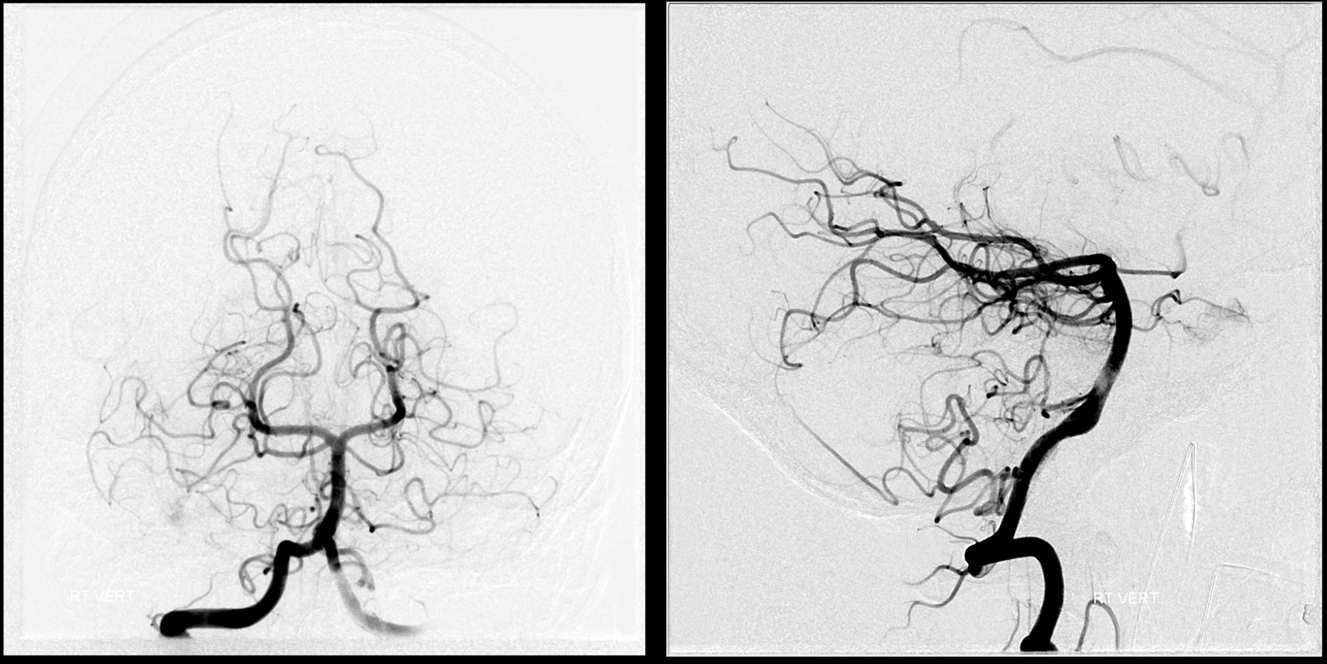
With enough experience, you kind of start to understand that most BTOs can be predicted on MRA or CTA alone. If someone has a hypoplastic A1 on either side and no PCOM on the side being tested, there is pretty much no way they are going to pass a BTO. If an MRA shows a complete circle of Willis, chances are they will pass. Sometimes it is hard to judge the size of an ACOM on an MRA or CTA. However the A1, P1, and PCOM segments are there for all to see. Here is a case of a BTO formally performed in light of unfavorable Circle of willis:
Right CCA — hypoplastic A1, no PCOM
Left ICA — dominant A1, no PCOM. This injection alone tells you there is pretty much zero chance this patient will pass a BTO
Vert. Again, no PCOMs
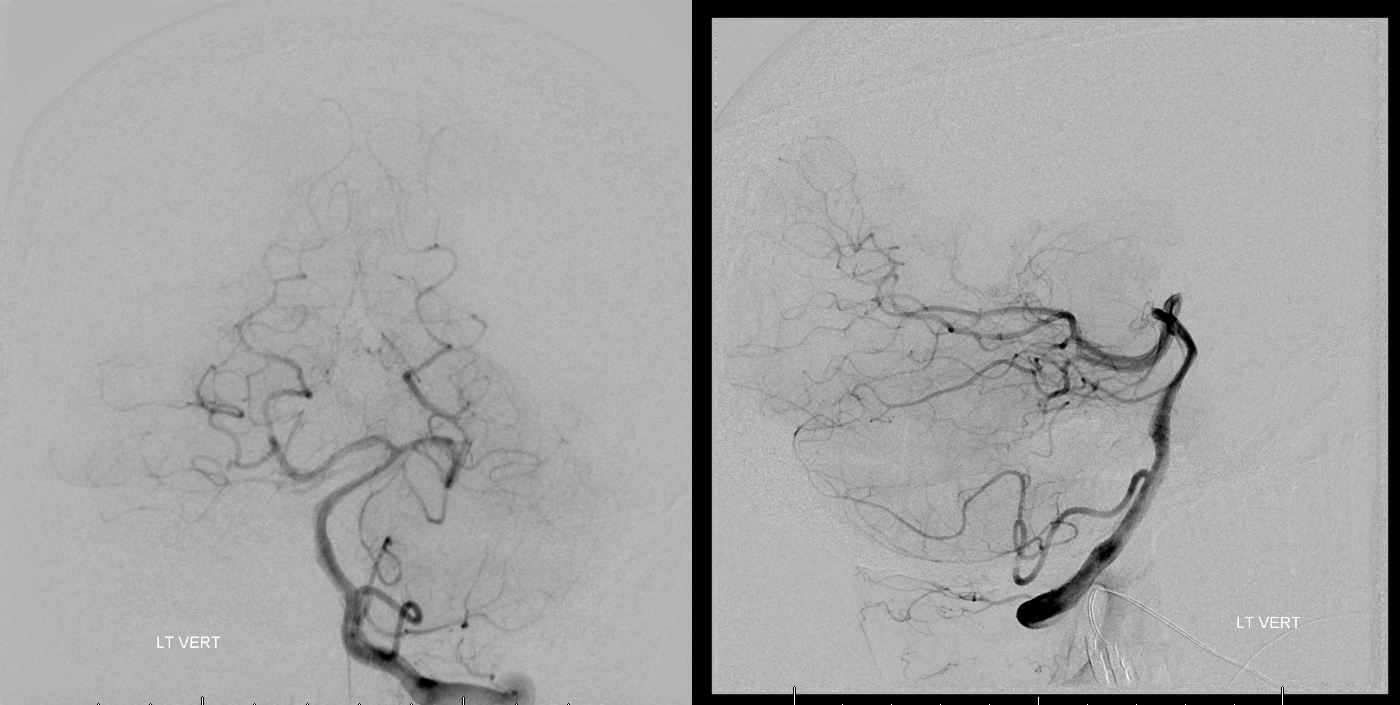
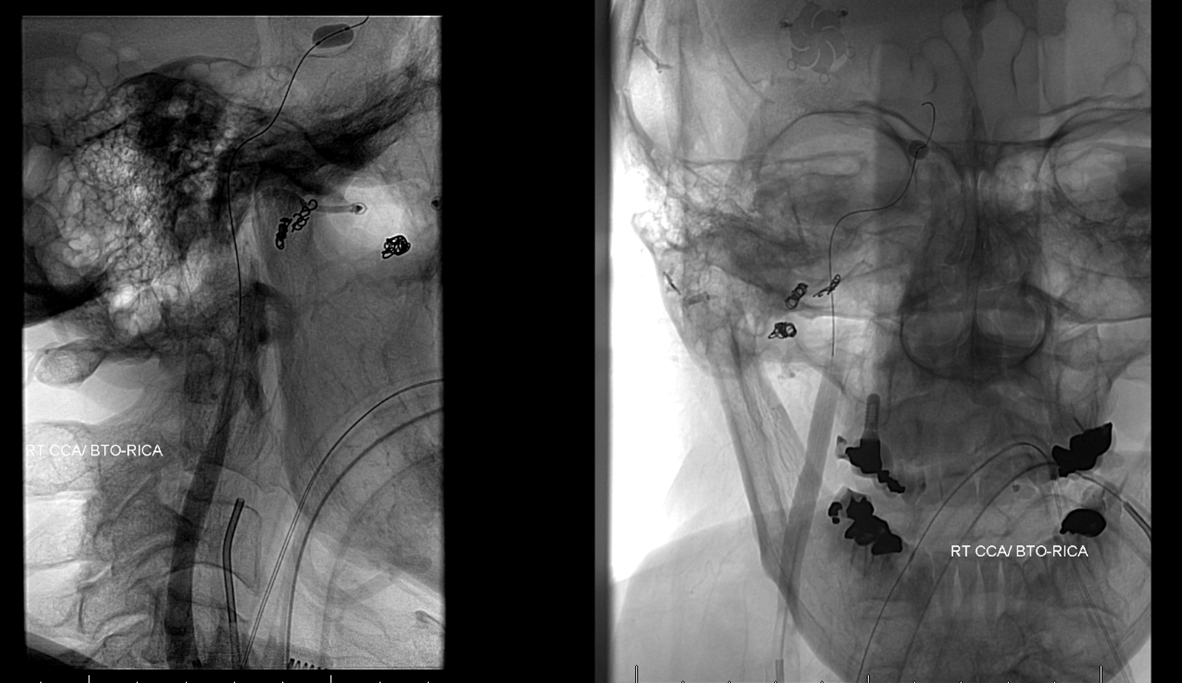
Balloon in petrous ICA
Ipsilateral guide injection of the left CCA. See how much the ophthalmic is trying. If the ophthalmic needs to work so hard, chances are its a fail
Right CCA — looks hopeless. Right A1 is just too small. Even the left ACA territory is a “fail” — on last image the right hemisphere is in late venous phase, whereas the left ACA territory is still in parenchymal phase. The left MCA gets pretty much no flow at all.
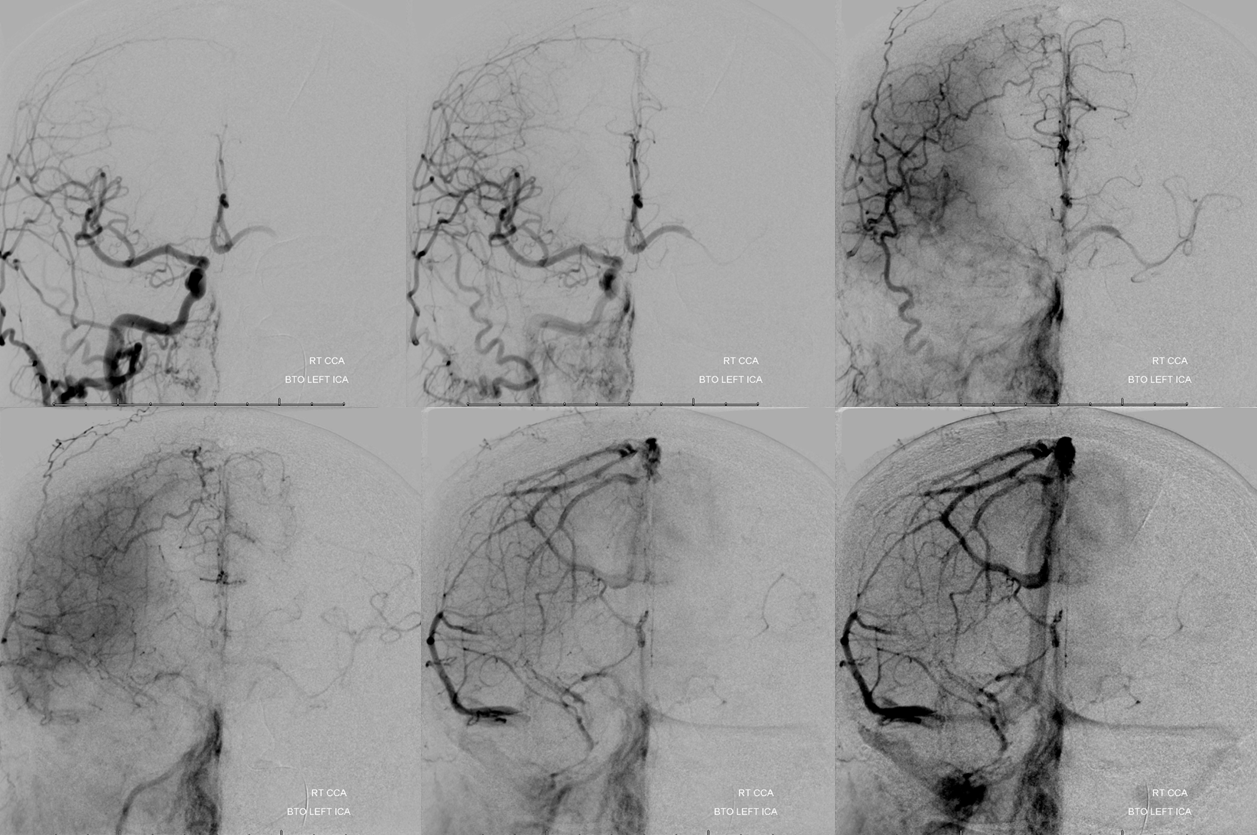
Left vert — we only did the lateral view to minimize frontal tube exposure, since this was going to be a pretty long Pipeline case.

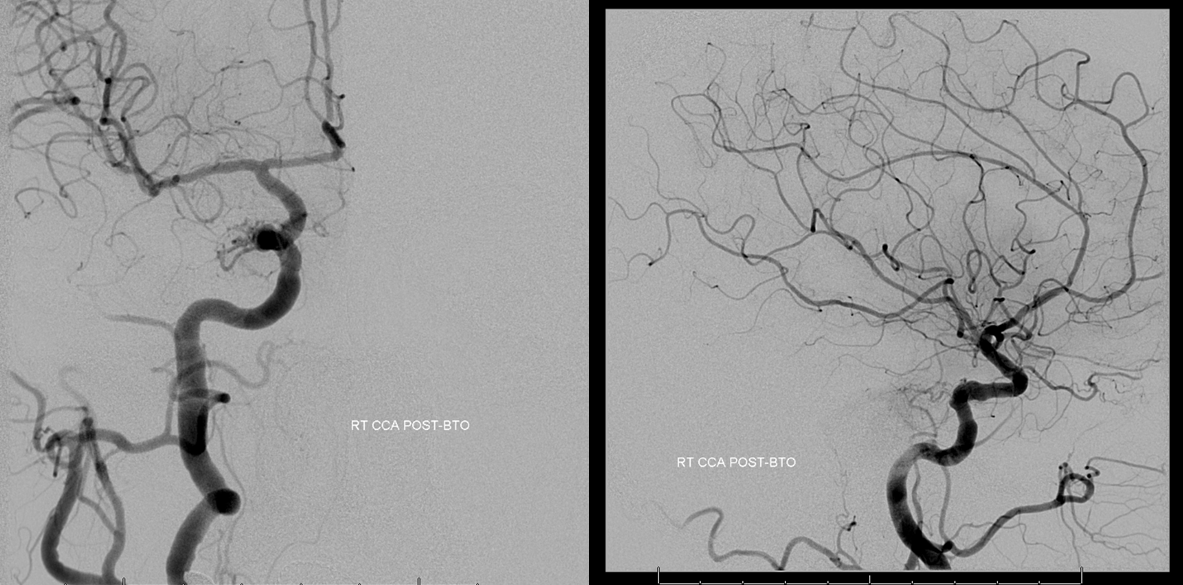
Post-BTO — always important to make sure there is no embolus or another problem
Post Pipeline. This was one of our very early cases. To me, it seems as though the Pipeline has reduced the number of BTOs we do by at least three quarters.
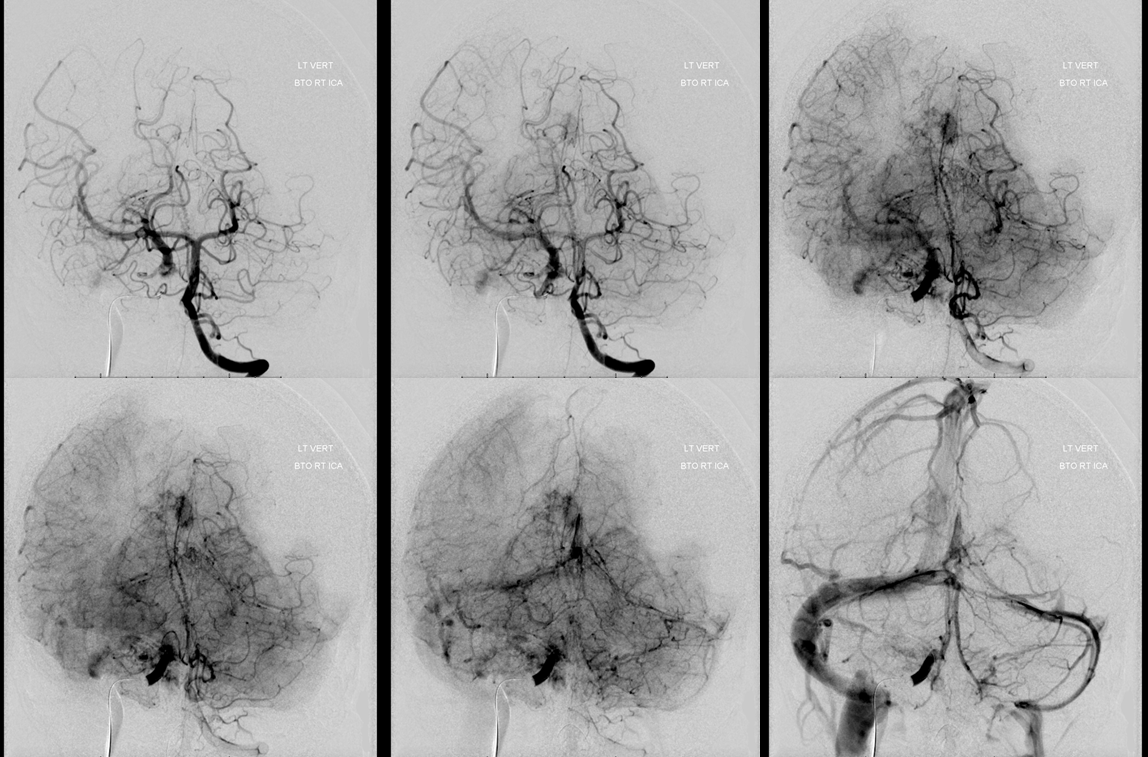
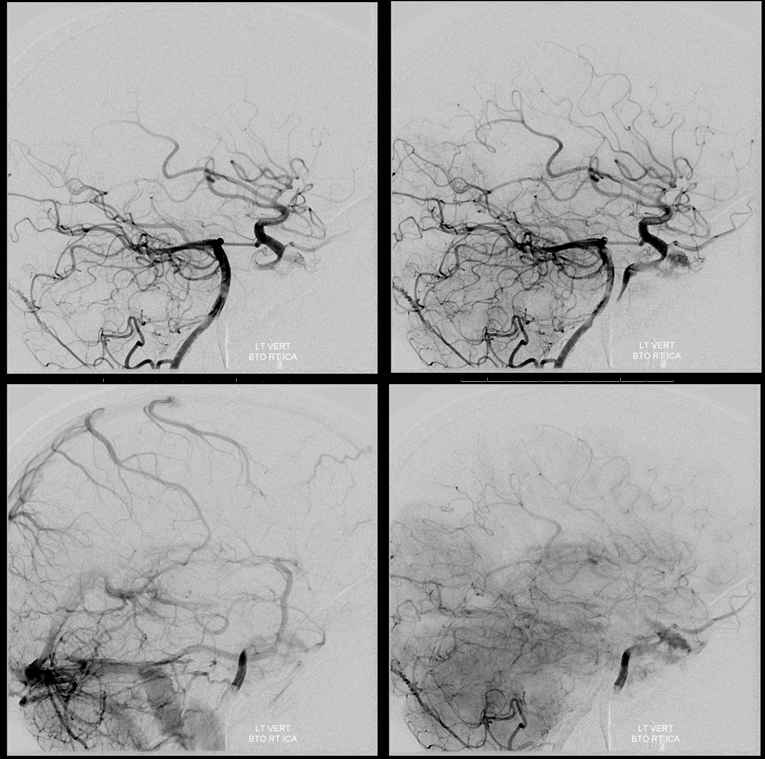
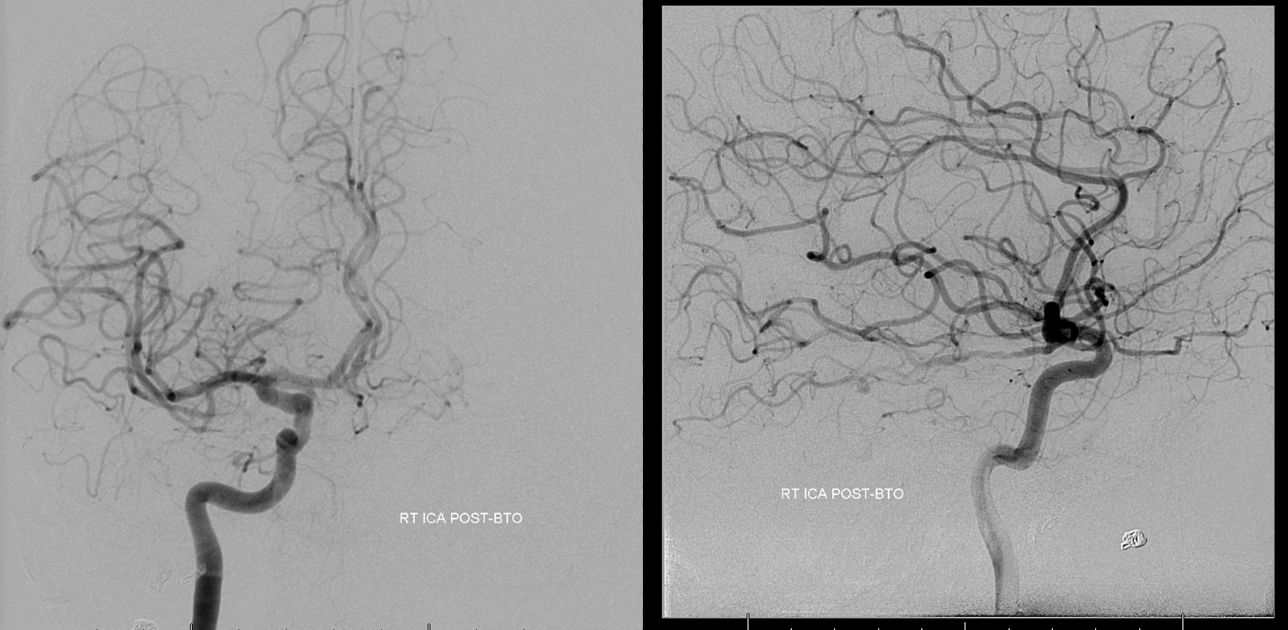
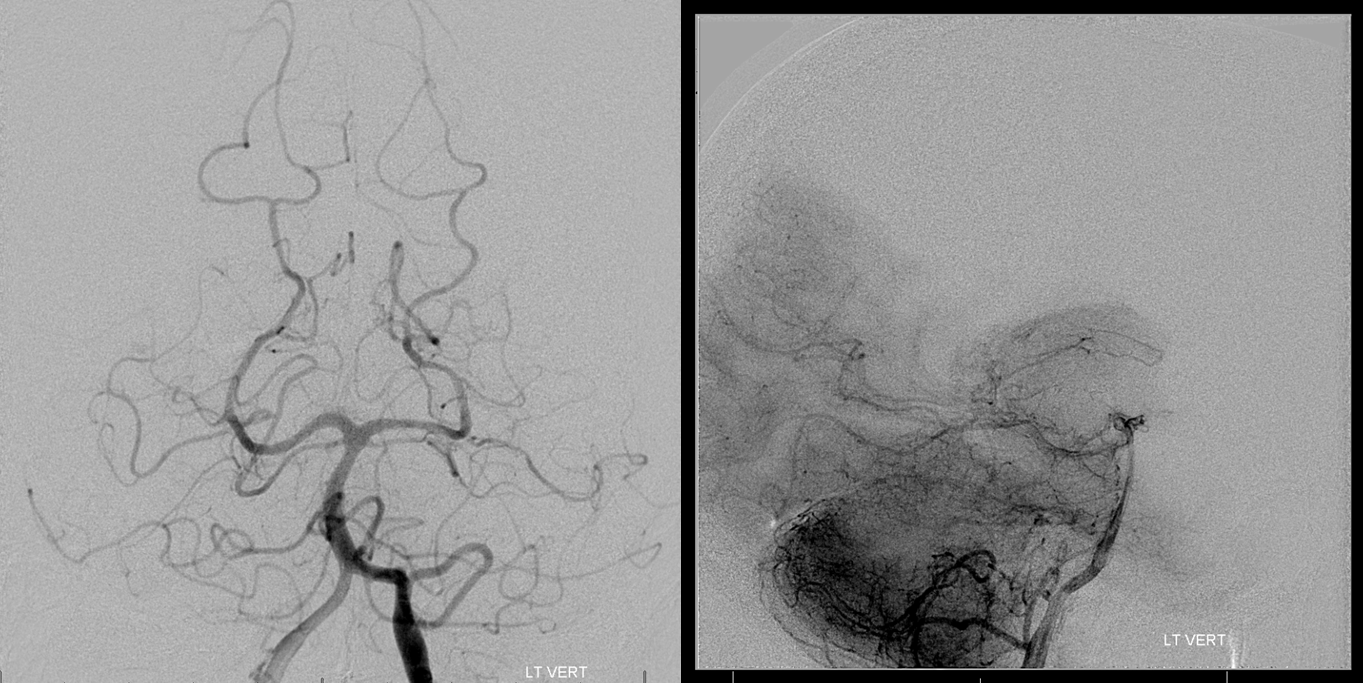
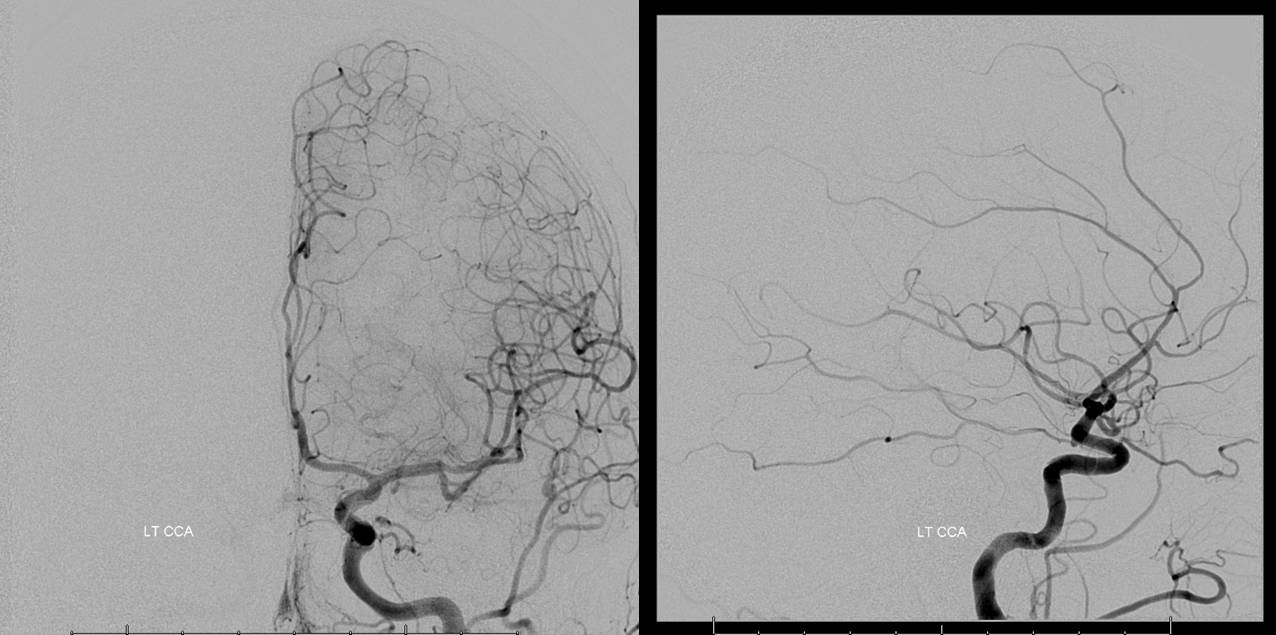
Case 3 — right cavernous sinus meningioma, hypovascular. Courtesy Dr. Peter Kim Nelson
Right ICA — see that nice PCOM with washout in the lateral image from the P1 segment (not marked, you should know). Looks pretty good. ACOM (fenestrated) looks good also.
Left ICA — see that nice ACOM with reflux into right A1 — its going to be a pass, 100% guarantee
PCOM is on the right — look for the invisible blue arrow
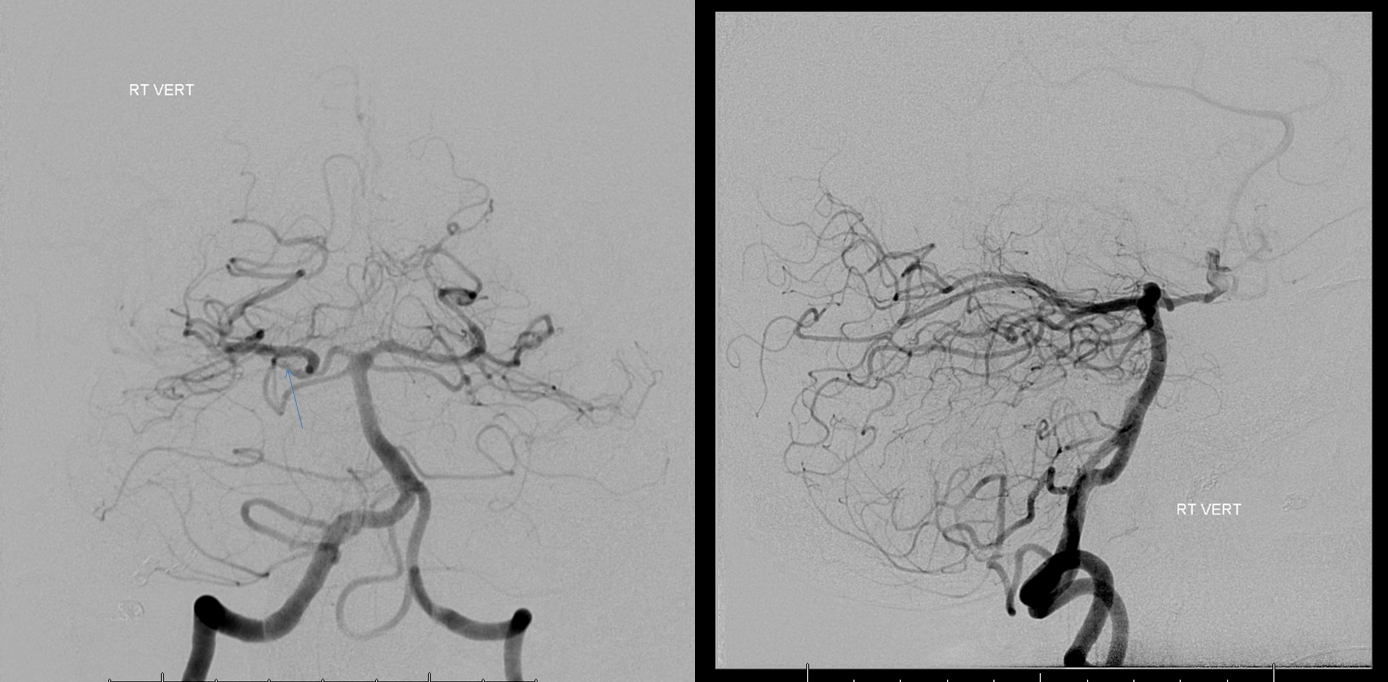
Same as case 1 — the density of contrast on the right is reduced due to inflow from the right PCOM, however the timing of contrast opacification is nearly simultaneous. There is a 1 frame (0.5 second) delay, which is a solid pass
Frontal vert
Lateral vert. The ACOM is so good the vert does not have to do much anyway
Post BTO check — all is well. So, starting to get boring right? At least more comfortable with BTO? That’s the beauty of our method — GA, no movement, standard views every time. Frankly, after seeing a few of these, you may be thinking there is not much science to it. I happen to think so, except for the few marginal cases here and there. With more experience, you learn how not to have so many marginal cases — its Pass/Fail, Doctor.
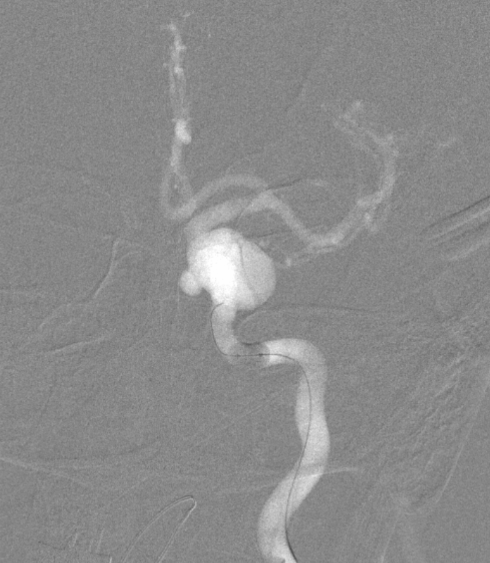
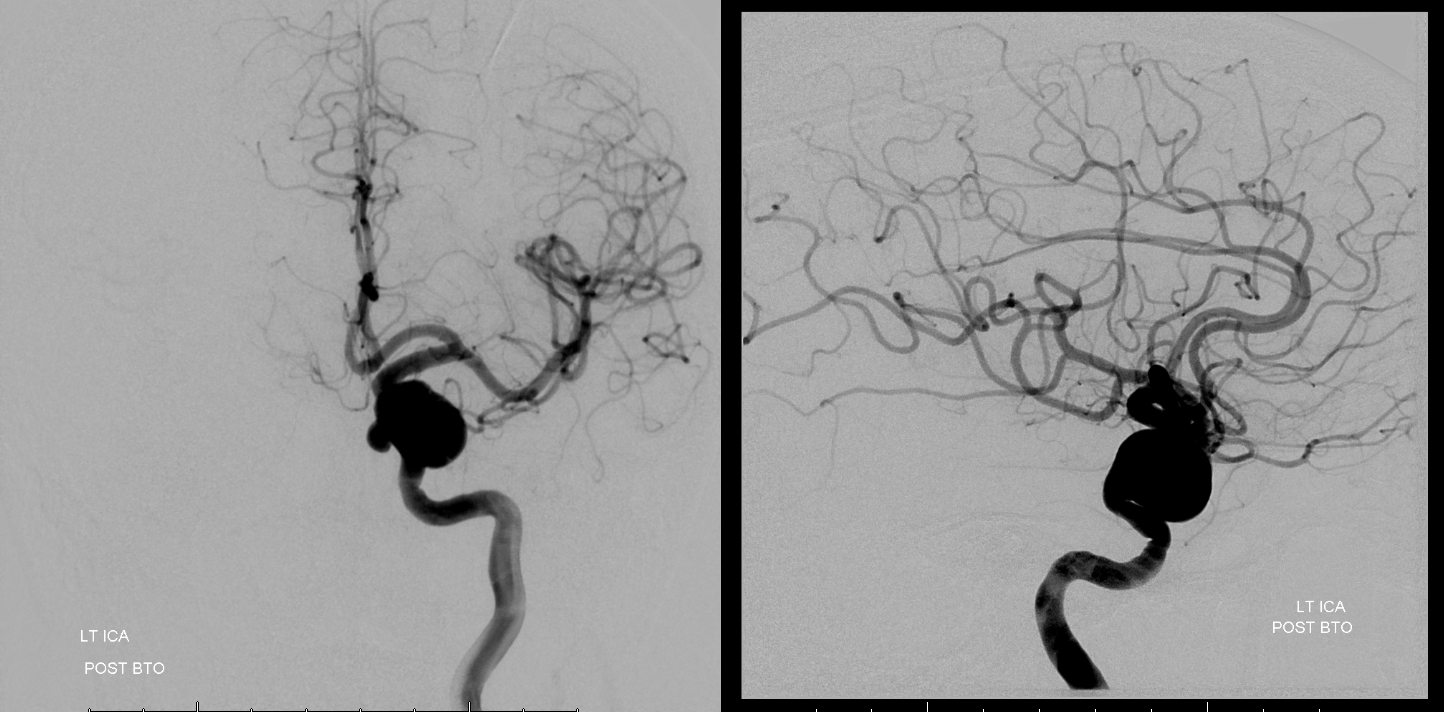
Case 4 — giant aneurysm. Marginal failure
BTO, in our view, is a semi-quantitative test. Others may disagree. Here is a giant aneurysm
Right ICA. Already there is redistribution of flow
Vert shows no PCOMs
BTO. We graded it as a fail because of slighly more than 1 second delay in parenchymal and early venous phases (blue frames). I think with some induced hypertension the patient may have done ok but there is no way to tell, and we should remember that this is dominant hemisphere with language areas in the most vulnerable zone. Nevertheless, this is an example of a close call.
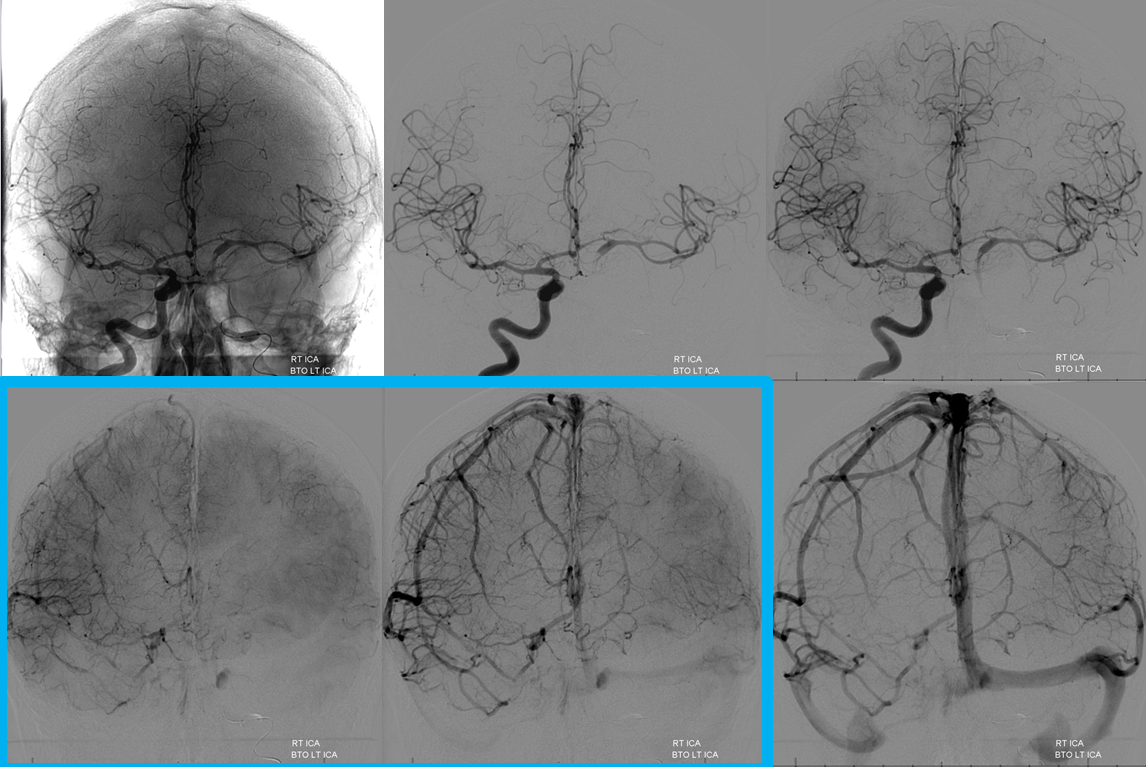
The vert is not doing much — another reason to suspect that collateral response is not going to be that robust at least in the near future should we choose to sacrifice the left carotid
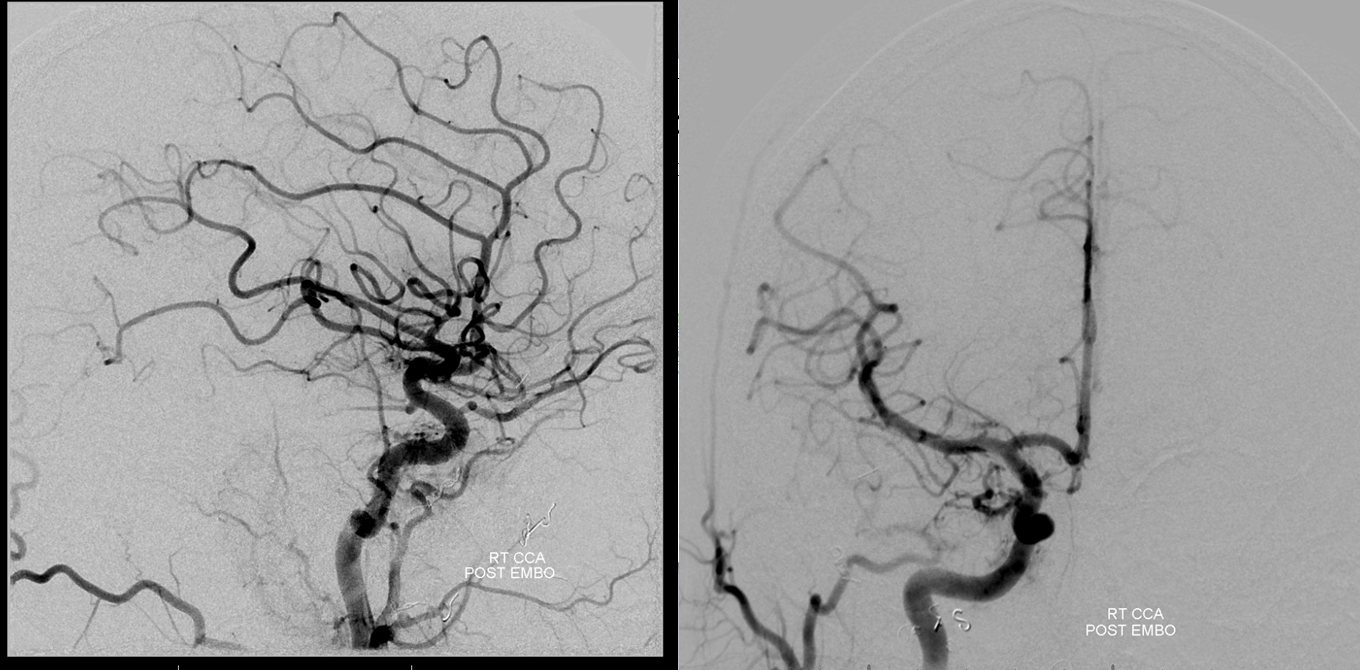
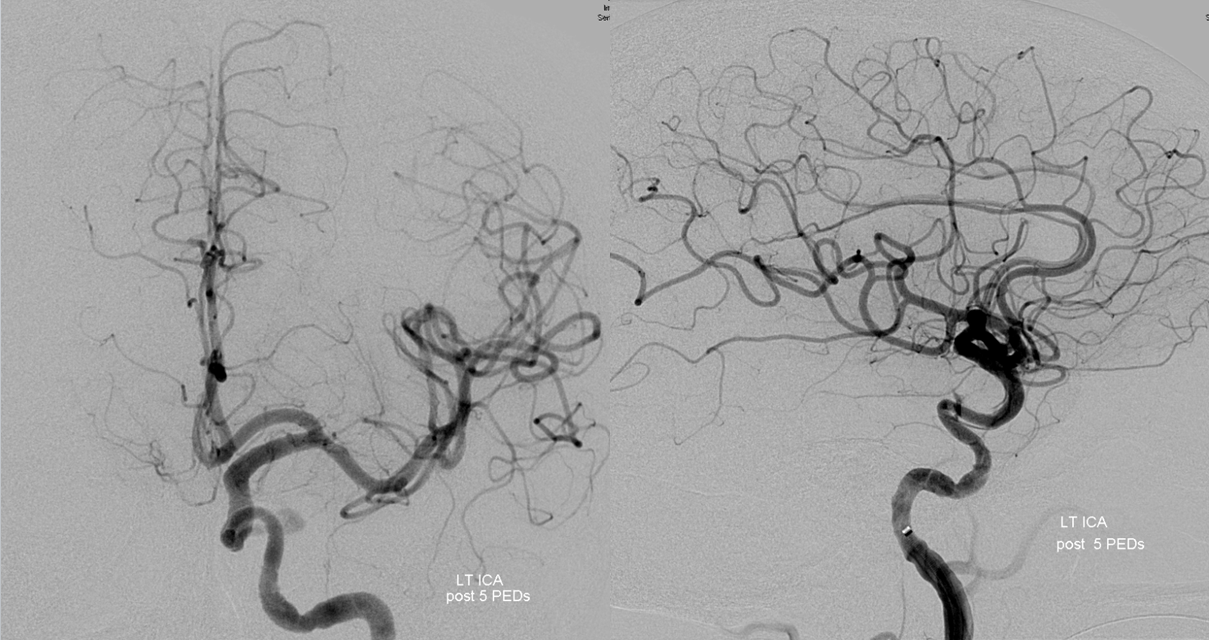
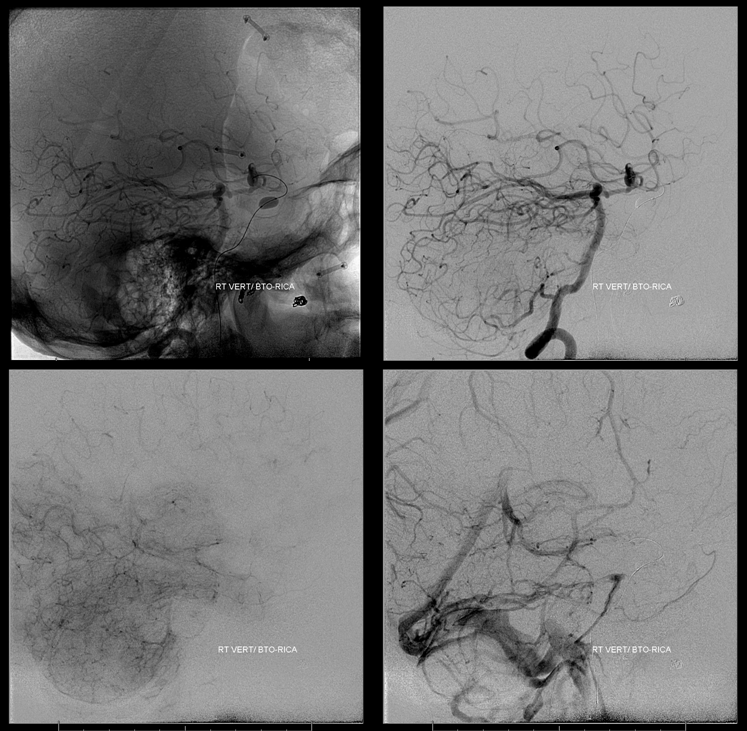
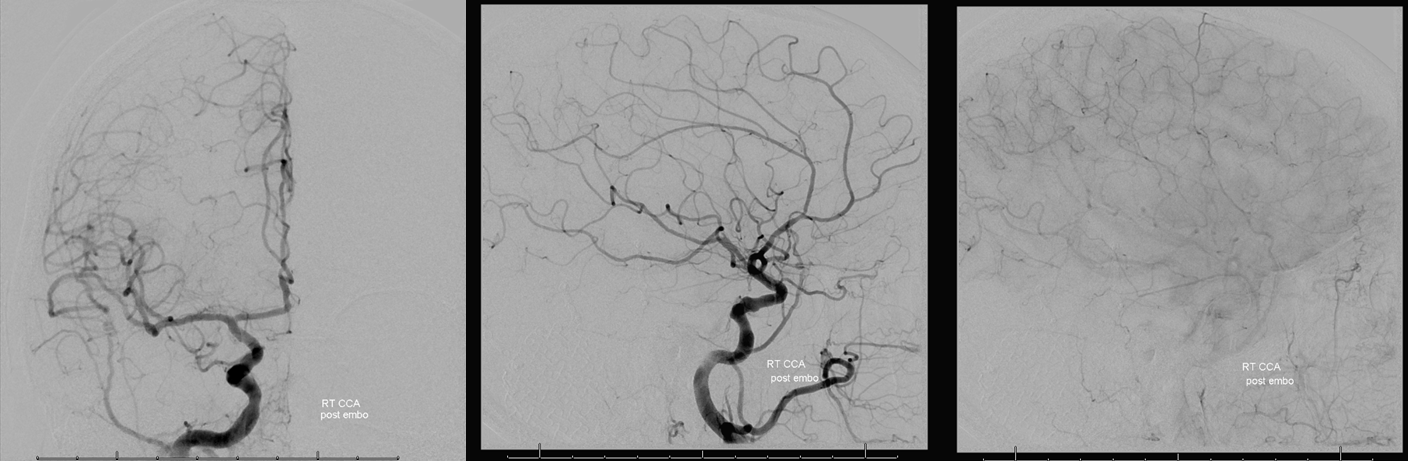
Case 5 — ugly petroclival meningioma, BTO and preop embo. Courtesy Dr. Peter Kim Nelson, Dr. Tibor Becske, and Dr. Ramesh Babu
Right ICA — look at that juicy MHT supply. For more cool preop embo cases, see Techniques Preoperative Brain Tumor Embolization Page
No PCOM, and looks like no ACOM — practically a fail from this injection alone
Vert — look at that athero. The PCOM is on the wrong side.
No ACOM here either, but we will demonstrate failure formally
Again, see that ophthalmic (black arrow) reconstituting the ICA (white arrow). Not a good sign
A total failure
We don’t even bother with the vert
Now for the cool stuff — MHT embolization. working projections

Selective MHT catheterization with the Marathon, Dr. Becske’s skill here. Zamatos! — that’s “juicy” in Hungarian
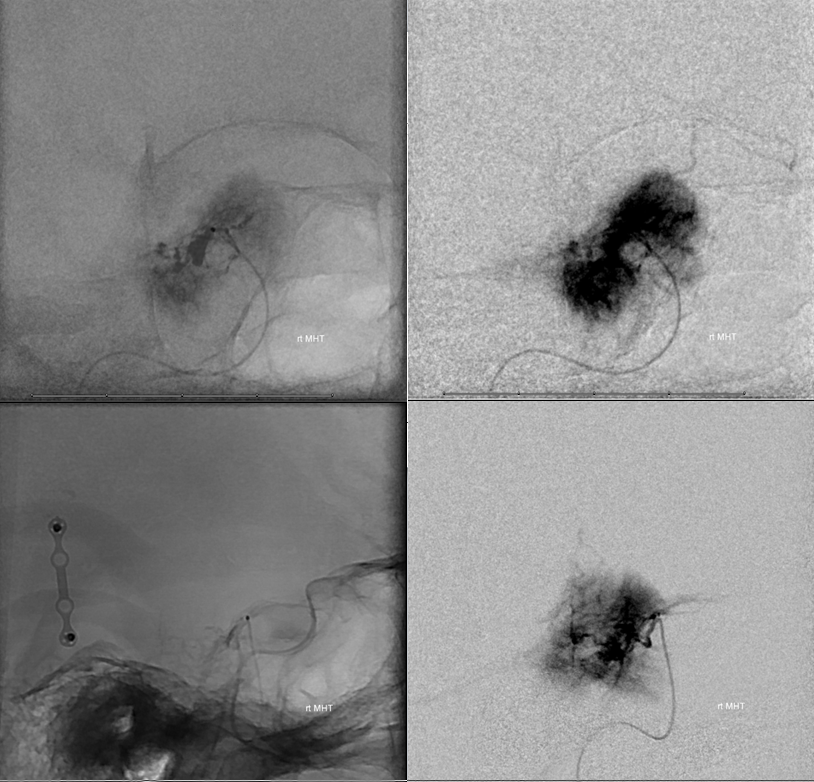
Post PVA embo. We like it like that. See other cases of MHT and ILT particle embo on Techniques Preoperative Brain Tumor Embolization Page
Right CCA to prove there is no external supply
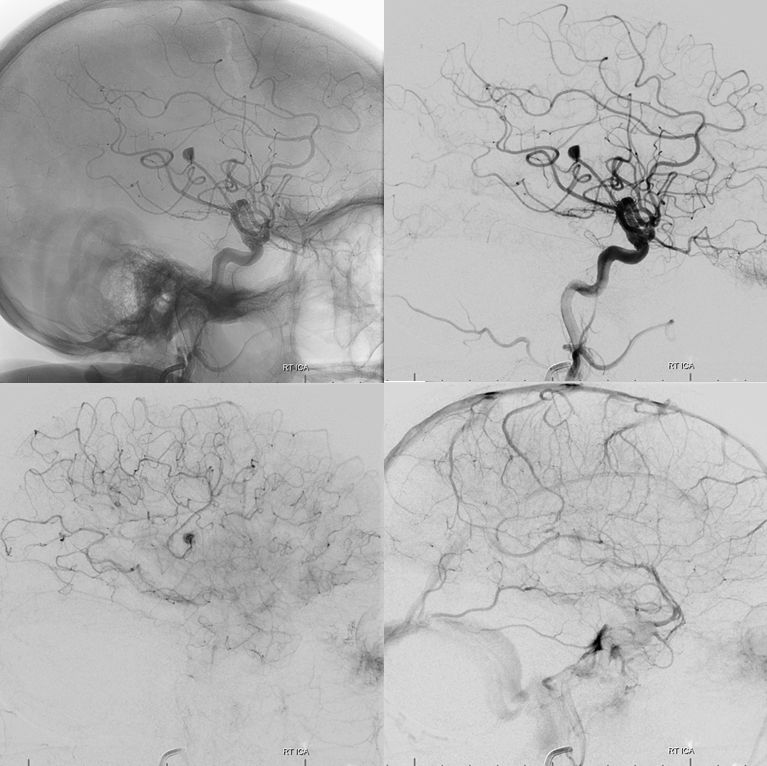
Case 6 — distal MCA aneurysm, courtesy Dr. Peter Kim Nelson.
Other than ugly tumors, we rarely do BTO for aneurysms anymore. I understand, some of you may be diehards for carotid sacrifice. It is an ever-shrinking group. However, for more distal aneurysms a BTO is not always a bad idea. For example, could the territory harboring this ruptured distal MCA aneurysm have decent enough leptomeningeal collaterals to just close it or should we Pipe? For a patient under GA, this kind of BTO is a very safe thing to do. Typically you only need to access one groin and inject one vessel. Sometimes a vert injection is necessary also if the territory being tested is inferior parietal, but otherwise no.
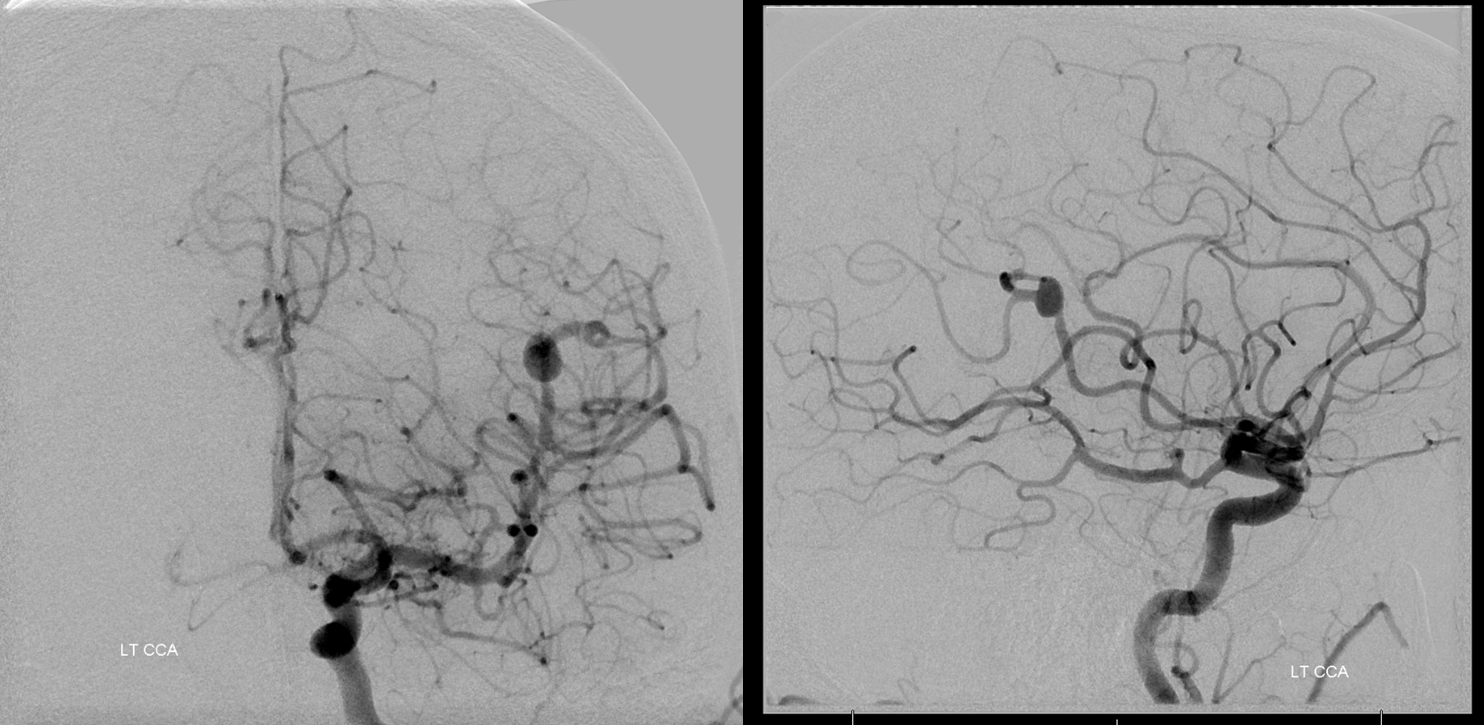
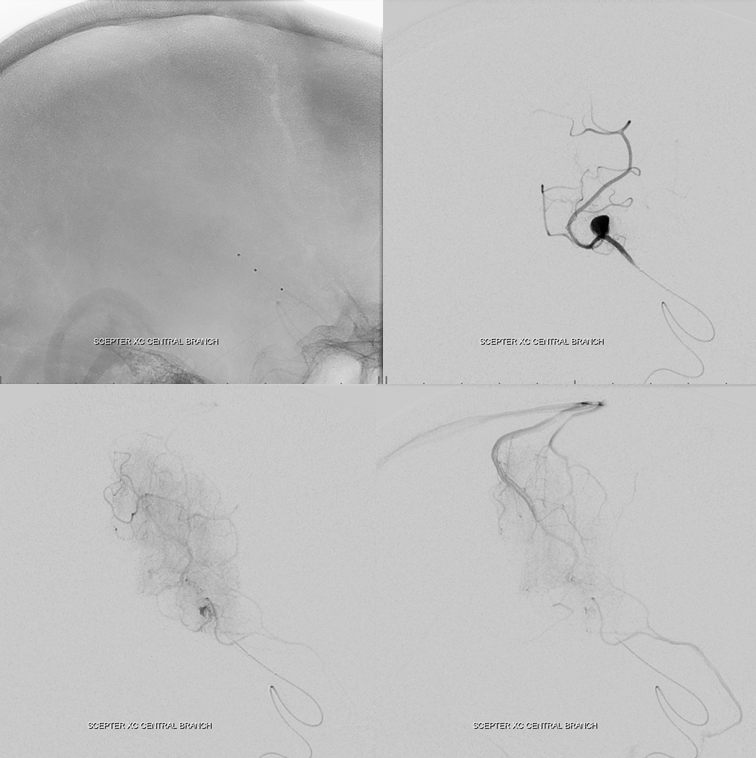
Microcatheter injection to best delineate territory. We did this and then went in with a balloon. Using a Scepter would have been even easier.
Just inflate the balloon proximal to aneurysm and do a run from the guide. As long as the A1 is well-developed, the ACA territory can be opacified through the guide and its leptomeningeal collaterals accessed. If the A1 is hypoplastic or the territory is inferior parietal, a second catheter in the contralateral ICA and/or vert may be necessary. This is a clear BTO failure
Post PED
So, lest you think these distal BTOs are always dismal failures, check out this…
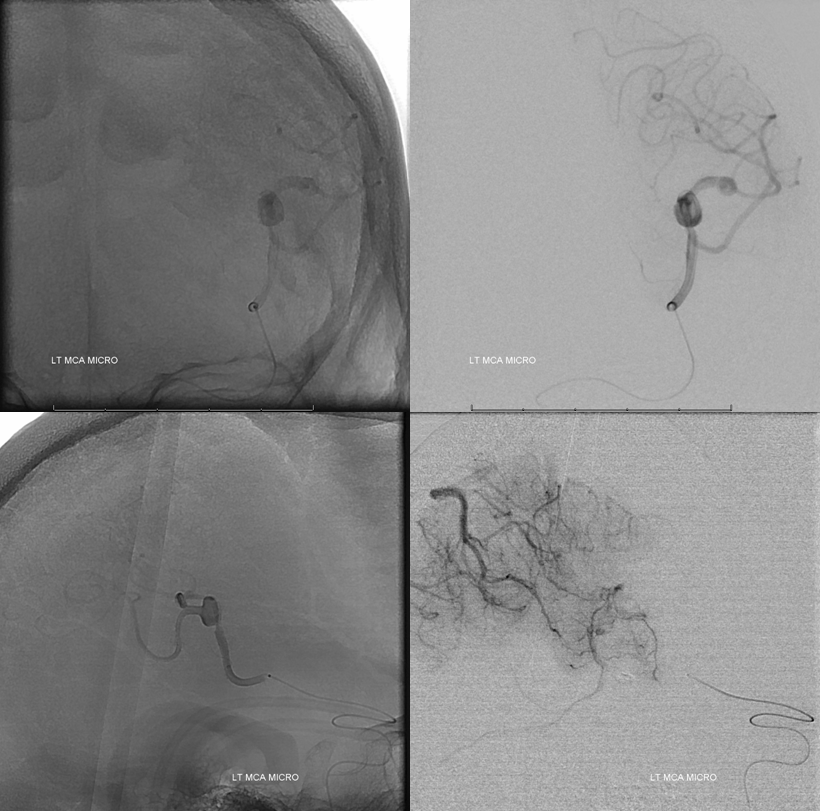
Case 7 Courtesy Dr. Eytan Raz
Another Rolandic branch aneurysm. Honestly, I think 99% of these end up in the Rolandic branch somehow (its not always the biggest branch, but it is by far the one most commonly involved)
Stereo
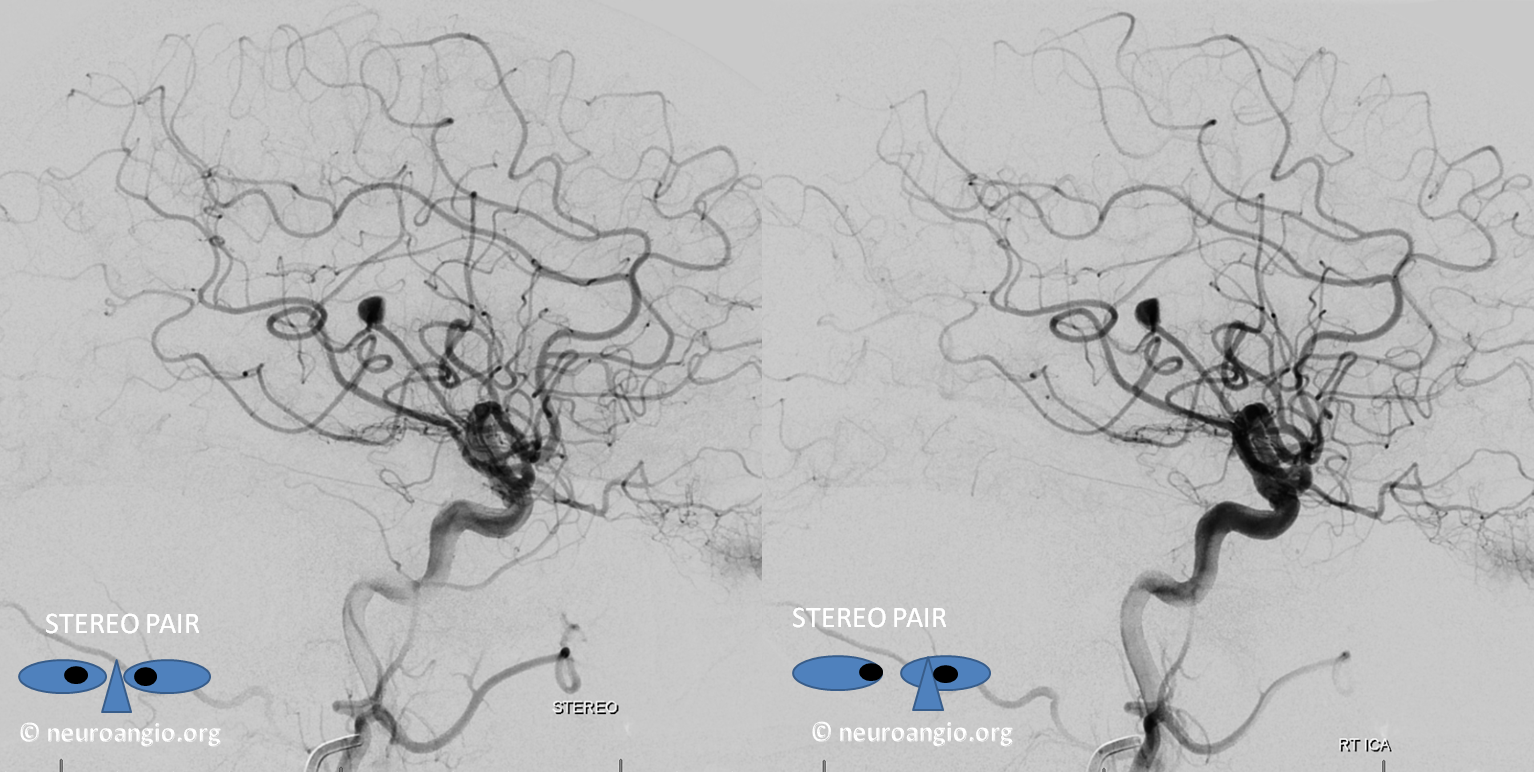
Scepter C injection of the proximal Rolandic branch. The Scepter is an excellent choice for BTO since it is highly navigable, can be used with all kinds of wires unlike the Transform and the Hyperglide/Hyperform family, and allows for injection through it should that become necessary. Its Rolandic branch all right.
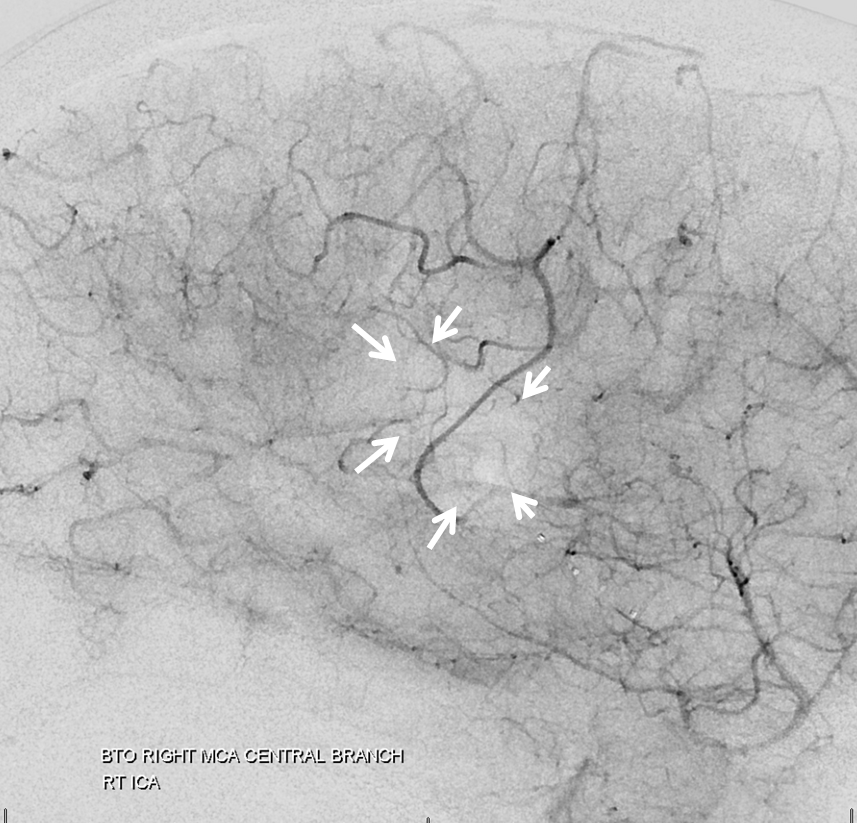
BTO. All you have to do is gently inflate the Scepter C (black arrow) and inject the 6F guide to see ipsilateral leptomeningeal collaterals. If the A1 were hypoplastic you’d have to put in a second catheter into the left carotid or, better yet, left ACA. Here we don’t have to. Notice excellent leptomeningeal collaterals backfilling the Rolandic branch (white arrows) all the way to the aneurysm (white arrowhead). Almost as good as it gets.
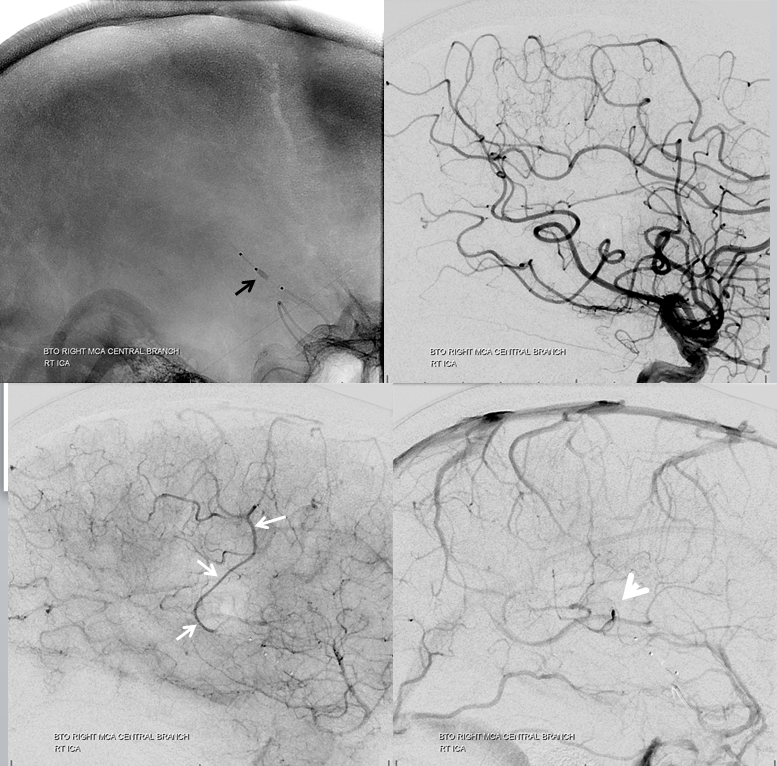
Nevertheless, it is not a perfect pass. The lucency outlined by the arrows below in parenchymal phase is probably not sufficiently supplied and perhaps a facial can be expected. Although technically this is a failure, I think its important to understand that there are exceptions to all rules. In less eloquent territory this would be a pass.
Case 8: A large left superior cerebellar aneurysm. Check out this page to find out why its not a PCA aneurysm. Nice stereos
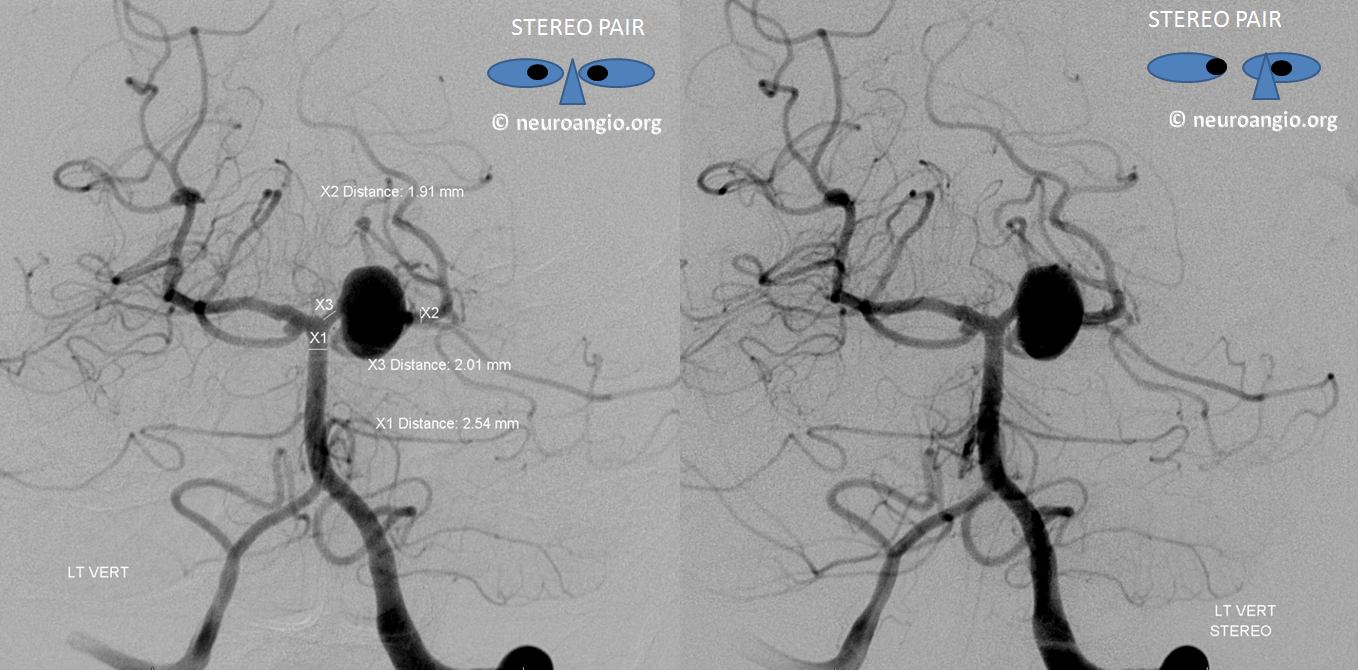
We considered coiling the aneurysm and thus sacrificing the left SCA. However BTO with Scepter SC in the proximal left P1 showed that there was no effective SCA reconstitution via the AICA or PICA. PCA reconstitution was not accessed given balloon position. BTO was a fail. See full case for more details. We piped it

That’st it folks. So far. Further reading? Sure, search “Balloon Test Occlusion” in whatever search engine you like best and get ready for confusion. If, however, you want to read a true masterpiece, look at the very first and still, in my opinion, the very best article on BTO

Related neuroangio pages:
Technique Preoperative Brain Tumor Embolization
Craniocervical Collateral Circulation
