Patient Information Spinal Dural Arteriovenous Fistula (SDAVF)
This page is intended as a source of information for patients suspected of or having been diagnosed with a spinal dural fistula. Please remember to read the “Disclaimer” section — none of this information may be used to diagnose or treat any disease. This is for general information purposes only.
Should you need more information, or if you are a patient wishing to make an appointment, you can write to me directly or call the office, both of which are listed in the “Contact Us” section. Our group at the NYU Langone Medical Center is one of the premier neurointerventional centers in the world.
“Fistula” means abnormal connection between two structures that are normally not connected. An arteriovenous fistula is therefore an abnormal connection between an artery and a vein. Any part of the body can have a fistula. A spinal fistula, particularly spinal dural fistula, is usually an abnormal connection between an artery and a vein that are located near the covering of the spinal cord. This covering is called dura, and so the full name “Spinal dural arteriovenous fistula.” When a fistula forms, blood from an artery under high pressure and flow goes directly into a vein, which is a low pressure and low flow structure. Even though the dural fistula is usually not directly on or within the spinal cord, it nevertheless causes dysfunction of the spinal cord by congesting the venous system, as will be explained below.
Etiology (Reason why fistulas happen)
The reason spinal dural fistulas form is usually unclear. They appear to develop spontaneously, that is without any reason we can point to. Sometimes, a patient has clear history of significant trauma or surgery in the area which later develops a fistula. In most cases, however, we have no explanation why they form, so they are sometimes called “idiopathic”, meaning without identifiable cause. There is in fact a cause, we just don’t know it yet. Typically, the patients with fistula are in 50 years or older, and more often men (maybe as much as 5 times more common), but many exceptions to this are seen and really any age or gender can have a fistula.
Pathophysiology (How fistulas cause trouble)
The way fistulas cause trouble is by preventing normal spinal cord blood circulation. Normally, spinal cord is nourished by a number of arteries, from which blood goes to the capillaries from which it passes into small venules and finally into larger veins that run along the surface of the cord. These surface veins then drain blood out via connecting veins that go through the dura into still bigger veins which finally return blood to the heart. Because the veins which drain the spinal cord are connected to veins that sit on the dura, a spinal dural fistula vein can be connected, in a reverse way, to spinal cord veins. The veins near the fistula are under higher pressure and higher flow than they are used to. This causes congestion (backup) of fistula blood into spinal cord veins. The backup of blood prevents the spinal cord from draining the blood that goes to it, since spinal cord blood has to overcome higher pressures created by the fistula to exit the cord. This causes the spinal cord to swell and malfunction. As time goes on, the situation gets progressively worse. The veins which drain the fistula eventually become diseased and often cose down (thrombose). Why exactly this happens is not clear, but it has something to do with higher flow and higher pressures and different chemical environment than the veins are normally designed for. Failure of these draining veins worsens already existing spinal cord congestion and makes symptoms worse. Irreversible damage to the spinal cord (myelopathy) eventually results. The patient may end up paraplegic (unable to move legs), impotent, and unable to control bowel and bladder.
The length of time between formation of the fistula and symptoms can be quite variable. Initially, the fistula is probably asymptomatic (no symptoms). Most fistulas, however, grow over time, — NOT in the same way a cancer grows, but by hypertrophy (enlargement, rather than neoplasia or new growth) of additional arteries leading to the fistula. As spinal cord swelling gradually develops, most patients start to have some problems with leg weakness, back and leg pain, and issues related to their bladder and bowel. Weakness can be of different types (upper vs. lower motor neuron, or both), and the patient may feel either stiff in the legs, or wobbly, or any other number of descriptive terms. The bowel and bladder problems can also be vague, — a person may feel they cannot start urinating as well as they could, of feel that they cannot empty their bladder as well as they should, or may not feel the urge to urinate and therefore have some incontinence. Constipation or fecal incontinence can happen also. Other problems patients report are impotence, abnormal sensations in the legs, which can be very variable, such as pins and needles, numbness, burning etc. The problem with diagnosing the fistula early, before catastrophic dysfunction develops, is that at first the symptoms are usually nonspecific — meaning that they don’t for sure imply that the patient has a fistula. In fact, most people with symptoms of numbness in the legs or urinary incontinence don’t have a fistula. Obviously, if you are concerned, you should see a doctor, and maybe a specialist such as a neurologist or a neurosurgeon. These fistulas are not common, and even busy neurologists may only see a handful during their career. Most patients have symptoms of the fistula for one or more years before they are diagnosed. It’s usually not the doctors’ fault, again because these fistulas are rare and early symptoms are usually vague.
Diagnosis
The most common way a fistula is eventually discovered is by MRI. The patient, who has had a long history of some symptoms, continues to get worse and an MRI of the spine is eventually done. MRI of a patient with a dural fistula (see below) usually shows large veins surrounding the spinal cord. The cord may show evidence of swelling (edema) and enhancement if MRI contrast is given. Notably, even MRI can miss small fistulas, and we see patients who bring us old MRI studies where the fistula cannot yet be seen, but must have been there in retrospect. Also, the quality of MRI study has to be good. Not all MRI machines are equal, and newer machines operated by competent technicians are vastly superior to older ones.
Diagnosis
Once the diagnosis of fistula is made, the patient is referred for more evaluation and treatment, which is the time when we first see the patient. The next step in evaluation of the fistula is a catheter spinal angiogram. MRI studies do not show where the fistula is, only that one is likely present. To find the fistula, a minimally invasive procedure, — a spinal angiogram, is necessary. This is a procedure where a skinny but relatively long catheter is inserted into the aorta and many vessels which can give rise to the fistula are catheterized (selectively entered) under x-ray guidance. It may take a long time (4-6 hours) to find the fistula. For this reason, and because the patient has to be completely motionless during angiogram injections, we do spinal angiograms under general anasthesia (patient is completely asleep). Once the fistula is found, the anatomy of the fistula is evaluated to see if it can be treated.
Treatment
The vast majority of fistulas can be treated either through catheters (neuro-interventional techniques) or by surgery. Most are treated through catheter embolization, sometimes at the same time as the spinal angiogram, so that both diagnosis and treatment can be carried out during the same procedure. To treat a fistula, a very small catheter is inserted into the fistula or very close to it, and the fistula is plugged up with a glue-like substance. If this treatment is not possible, for one of several reasons, the patient can have the fistula closed by having special spine surgery. Overall, the vast majority of fistulas we see are cured through one of these two ways. Whether the fistula is cured by endovascular (catheter) or surgical means, the treatment should only be undertaken at specialized centers having extensive experience with this particular condition, as details of treatment are usually quite complex. The details of treatment are best discussed with the specialist who will be treating the fistula.
Prognosis and Recovery
Once the fistula is closed, spinal cord blood circulation gets better, but usually does not go back to normal. The patient’s symptoms may go away completely, partially, or not at all. The extent of eventual improvement depends on duration and severity of pre-treatment symptoms, individual anatomy, and other considerations. Overall, most patients get better. The converse is that, without treatment, virtually all patients get worse and will be eventually paralyzed. For this reason, we strongly recommend that essentially all patients with dural fistulas be evaluated for treatment.
Additional Information
Images
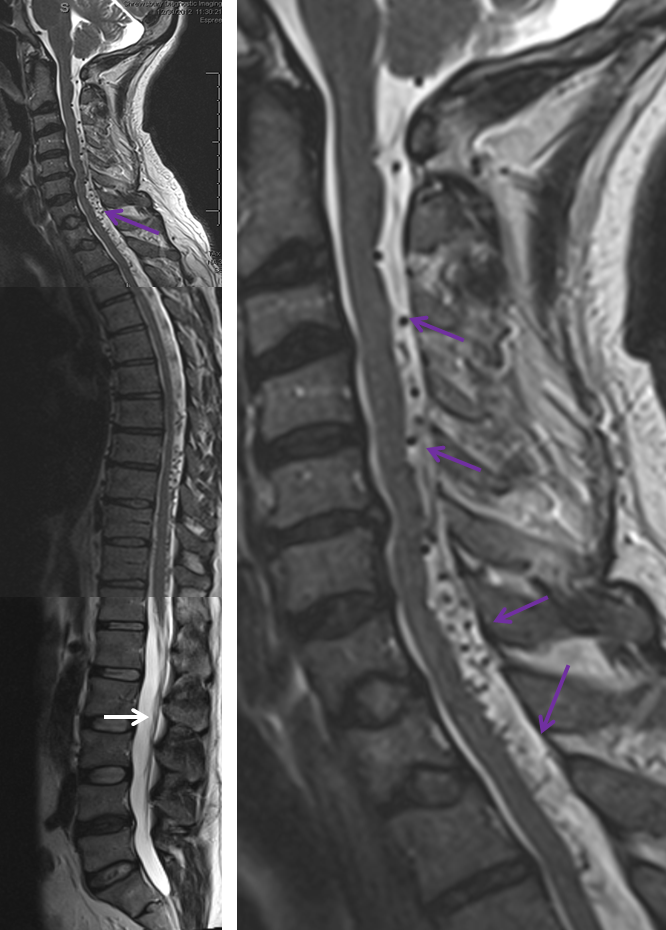
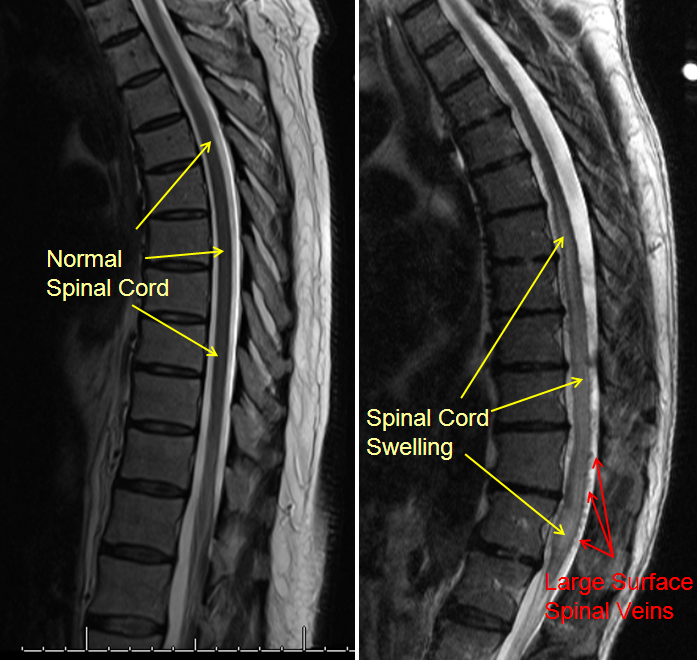
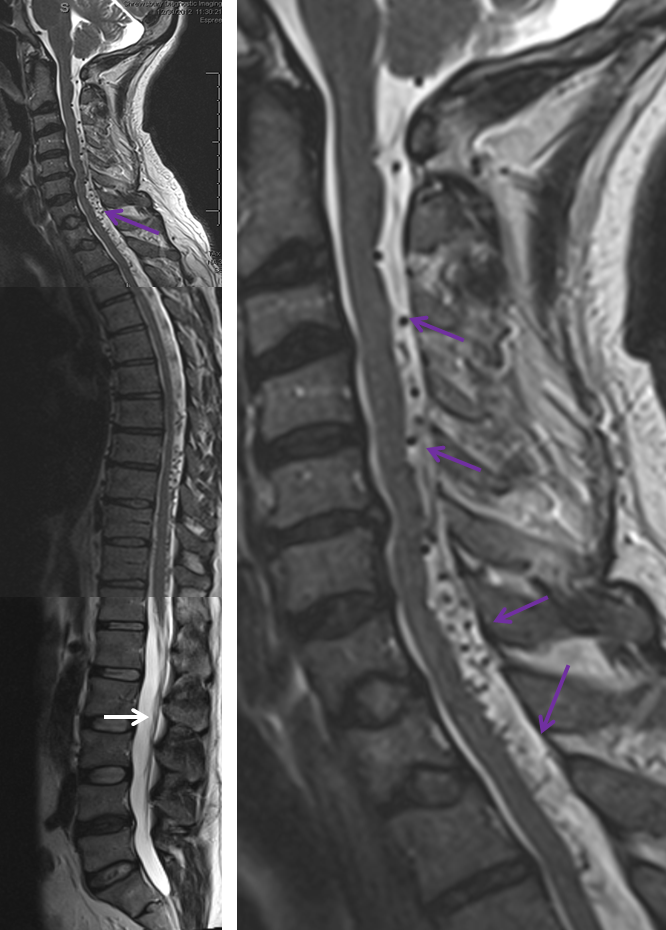
Below are images of normal spine MRI and MRI of patient with a spinal fistula
The LEFT midline image of the back shows normal dark appearance of the spinal cord with normal bright cerebrospinal fluid surrounding the spinal cord. Image on the RIGHTshows an area of brightness within the spinal cord, which represents cord swelling, or edema. A number of black dots are seen on the back surface of the lower cord, which are large tortuous spinal veins. The image on the right is very typical of a patient with a spinal fistula (either spinal dural or spinal intradural fistula)
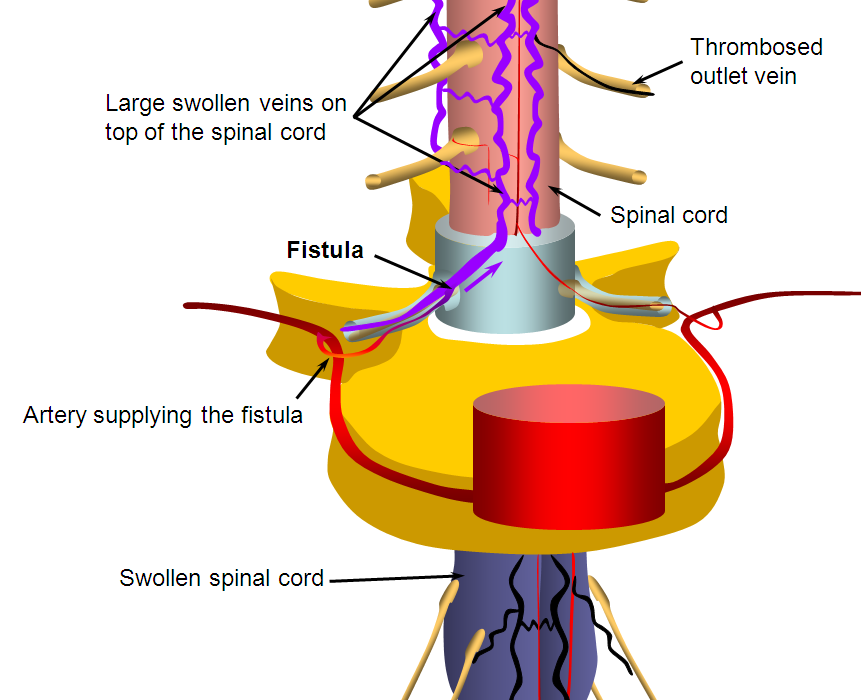
Spinal Fistula Diagram
This is a schematic view of the fistula, with large dilated veins on top of the spinal cord (which are labeled with red arrows in the MRI study above) and swelling of the spinal cord (same as yellow arrows on the MRI above)
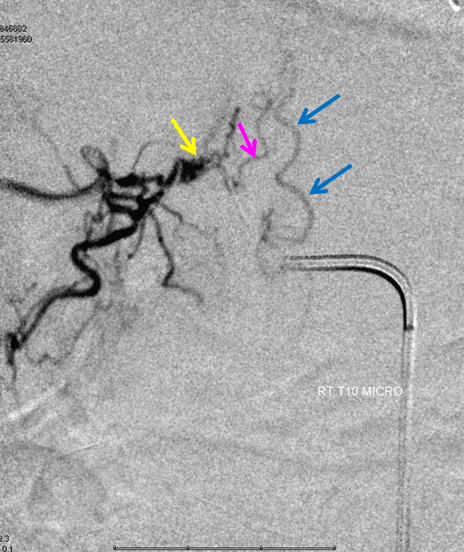
SITE OF FISTULA, CATHETER ANGIOGRAM
Right T10 (lower thoracic spine) injection shows a spinal dural fistula (yellow arrow) reversing flow in the radiculomedullary vein (pink arrow, the same vein as seen on the above diagram with the purple arrow below it) to opacify the spinal vein (blue arrows, same as “swollen veins on top of spinal cord” caption in the diagram above)
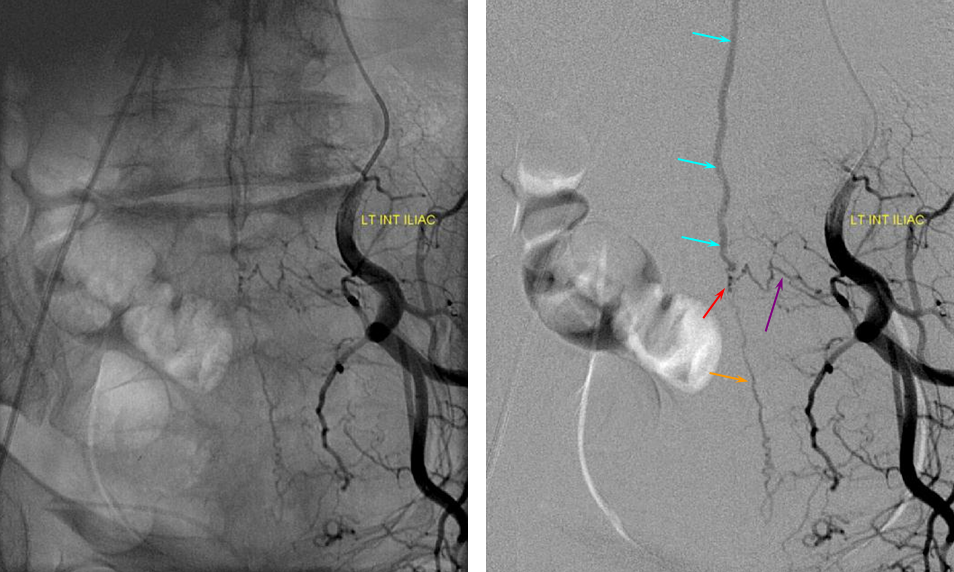
ILIAC ARTERY ORIGIN OF AV FISTULA
The fistula (red arrow) is the site of abnormal connection between the radicular arteries (purple and orange) and spinal vein (blue). This somewhat unusual fistula is supplied by an artery in the pelvis called the Iliac artery. The image on the left is similar to the one with arrows, except that bony landmarks can be seen.
Although most spinal dural fistulas arise near the nerve root involving the lower thoracic and lumbar spine, they are not infrequently unique and involve other locations which makes them considerably harder to find. In this particular patient, MRI of the spine showed extensive abnormal vessels near the top of the cord (cervical spine or neck area) — purple arrows. Notice lack of abnormal vessels at the bottom (white arrow), where they are normally most prominent.
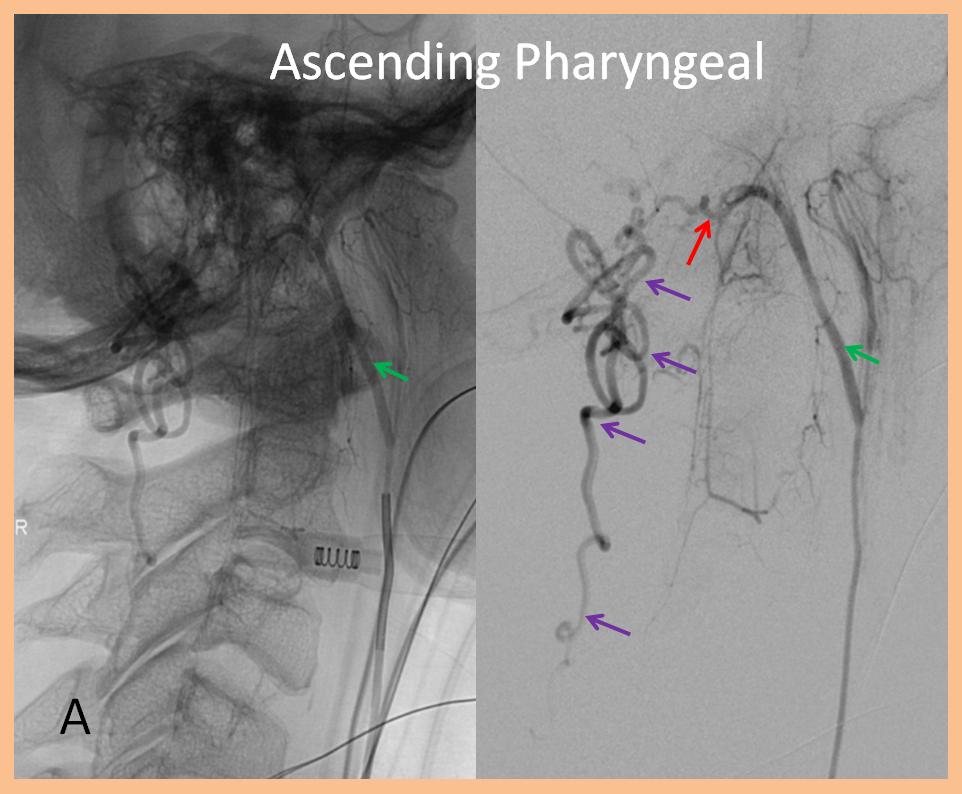
The fistula was ultimately traced to an artery in the neck that classically supports tissues of the skull, cranial nerves, and throat. In this particular case, the ascending pharyngeal artery (green) hypoglossal division (red) was opening into a fistula extensively congesting the paraspinal veins (purple), ultimately emptying all the way at the bottom of the spinal cord, near the pelvis.
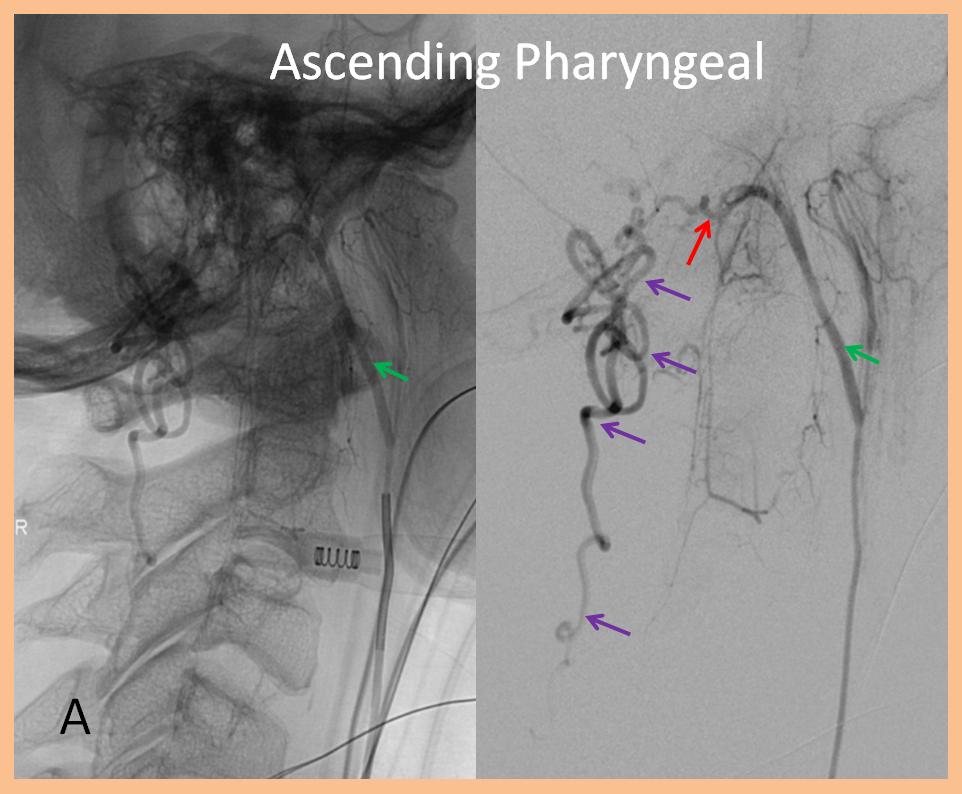
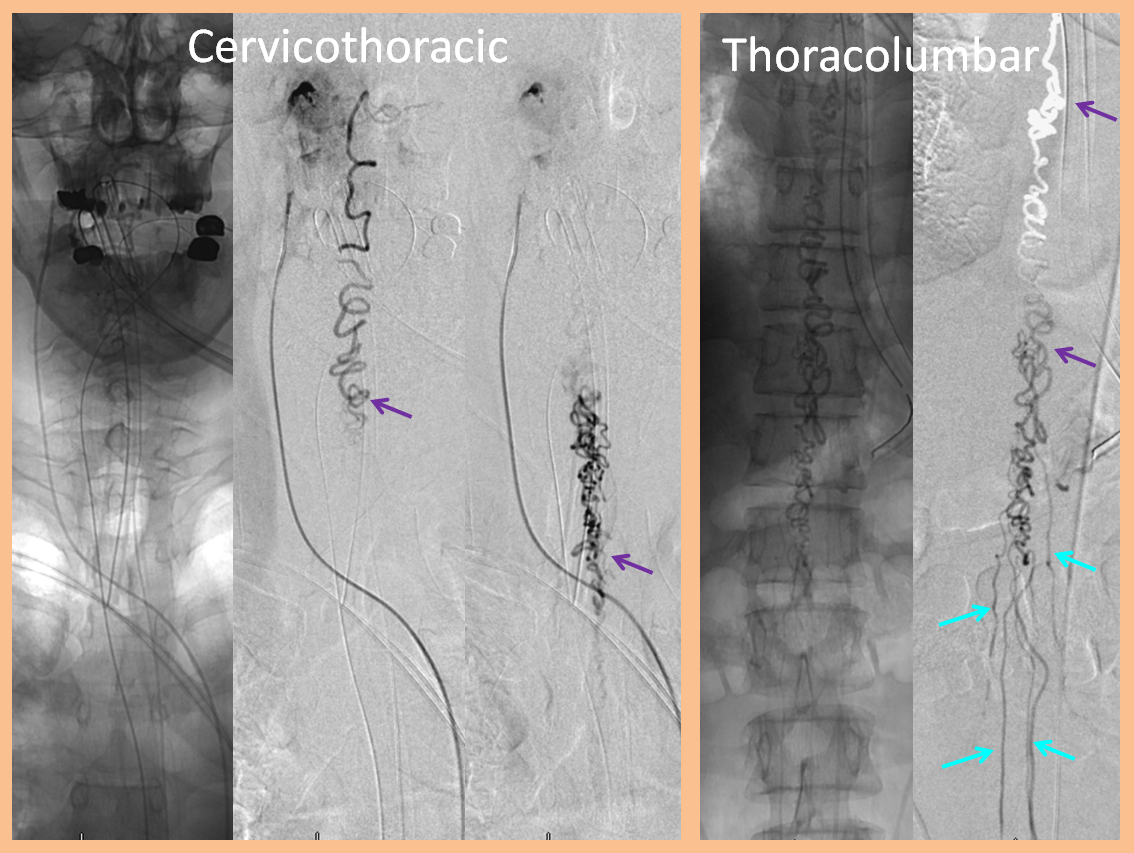
The images below, of the same ascending pharyngeal injection, show extensive congestion of the spinal veins all the way down to the pelvis.
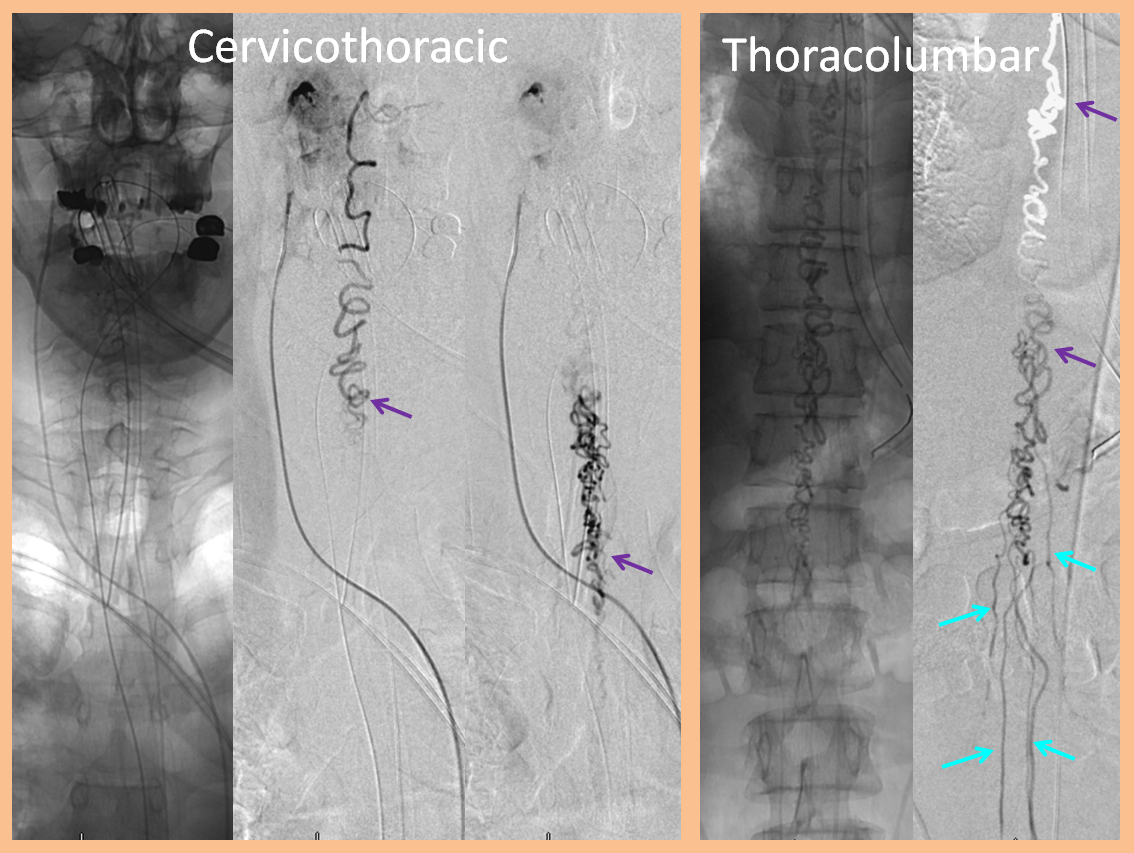
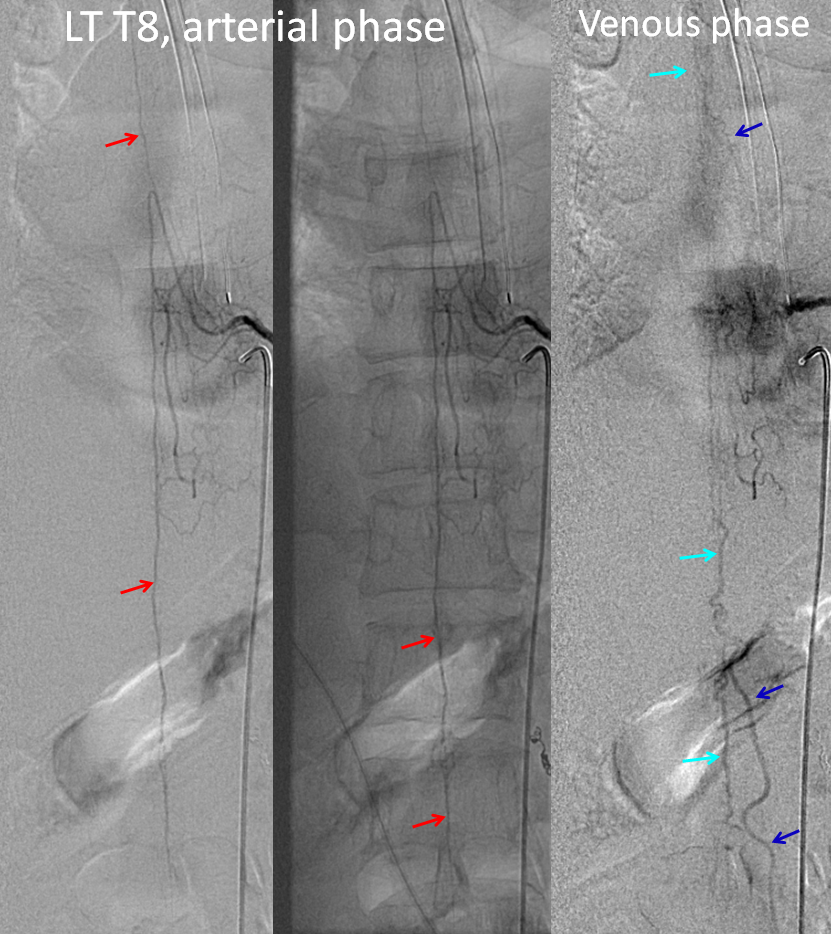
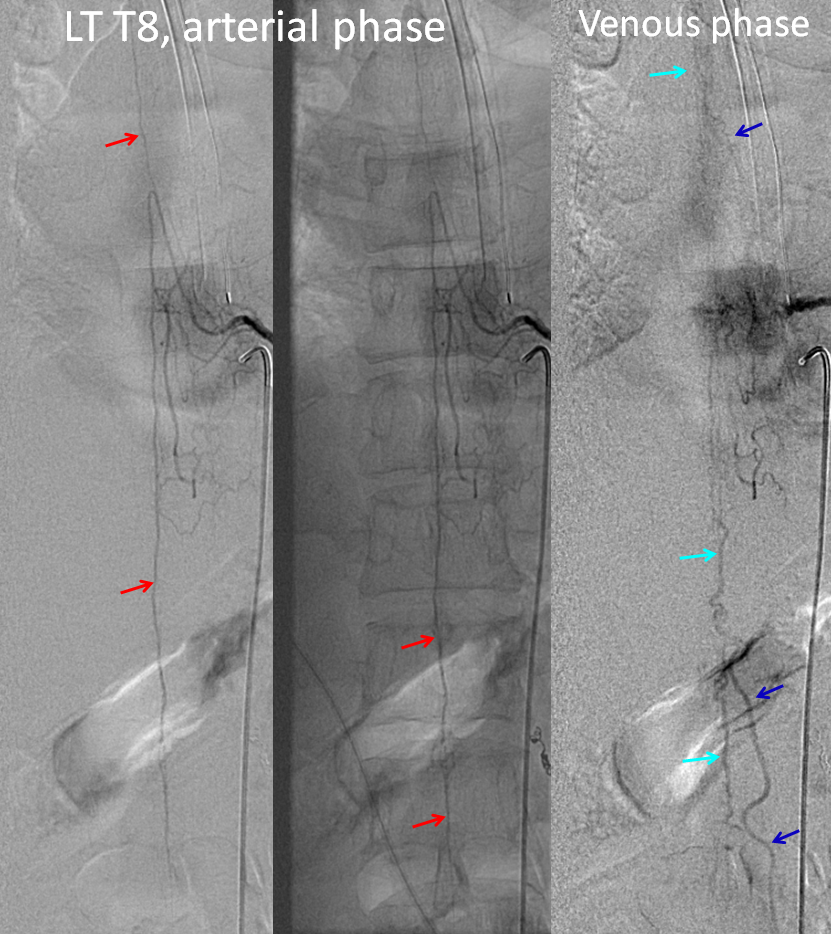
This fistula was treated by selective catheterization of the ascending pharyngeal artery and injection of nBCA (glue) to close the fistula while preserving spinal veins. Post-embolization injections of anterior spinal artery (red arrows) now visualize spinal veins (light blue) and their draining radicular veins (dark blue) in their normal venous phase.
Our role
Our Neurointerventional Radiology group specializes in performance of spinal angiography and transcatheter (endovascular) embolization of spinal vascular malformations, including spinal fistulas. We are located at the NYU Langone Medical Center, in New York City. As all centers of excellence, we function as part of a team of neurosurgeons, neurologists, rehabilitation specialists, and diagnostic radiologists, all of whom have extensive experience with vascular conditions of the spine. Regardless of where you may seek medical advice, we STRONGLY recommend that your evaluation and management be carried out at a major center with extensive experience in treatment of this condition, as details of diagnosis and therapy are usually quite complex. A number of excellent centers exist accross the US and elsewhere.
Contacting Us
For questions, or if you are a patient wishing to contact the center, use the “Contact Us” section to email or call.

Pingback: Spinal Cord Blood Flow Diagram - Smart Cord Blood Banking