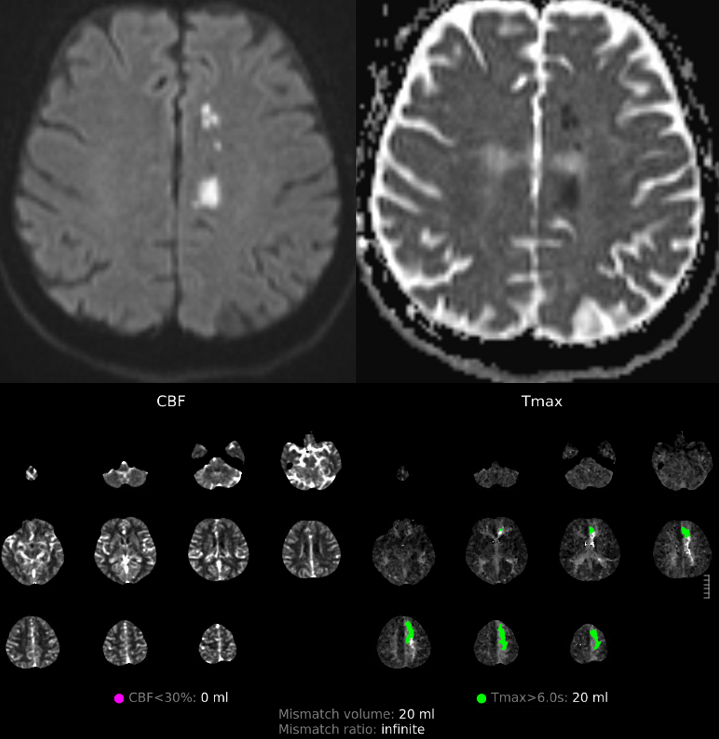
Subacute revascularization need not be limited to cervical ICA. Carefully selected (no large core, obvious perfusional state, favorable anatomy) lesions are legitimate targets. This is about 3-day old occlusion with perfusional weakness. A2 segments are anatomically favorable, since there is usually a gentle curveature present without serious angulation.
Case below shows that tools should be adapted to anatomy. We can’t always use balloon-mounted stents — though it is still possible to do that in A2 sometimes — see case here. Below is another matter…
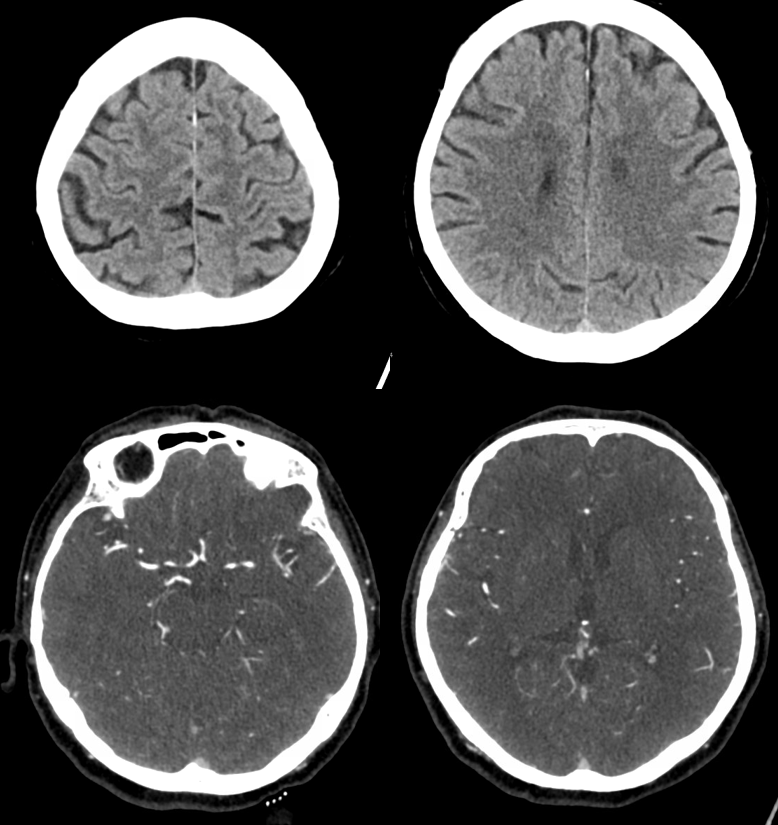
Challege here is significant A1 disease. Do we plasty/stent that also?
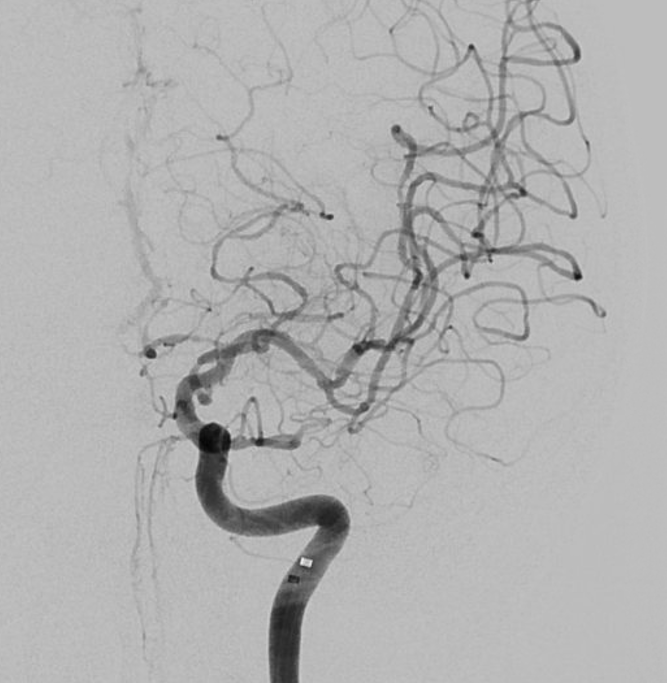
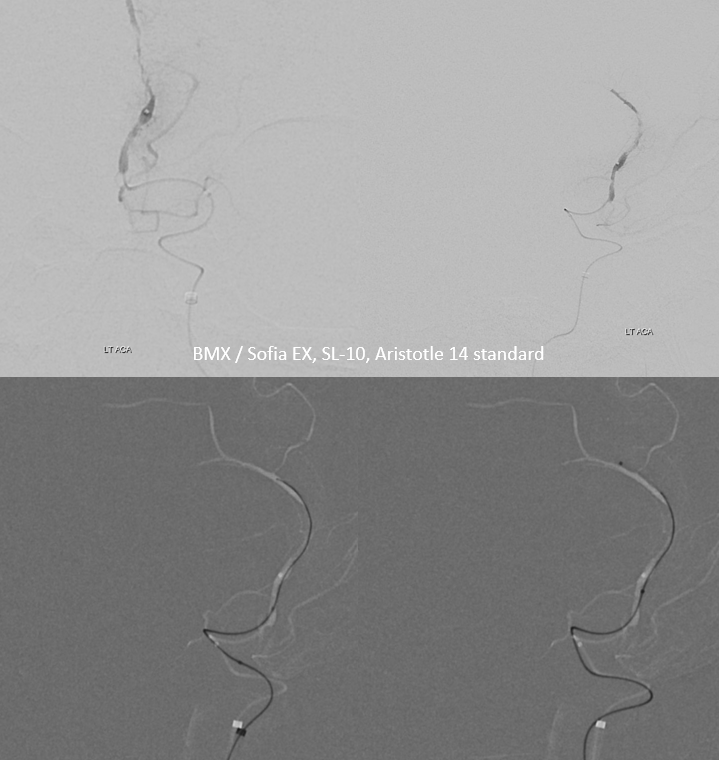
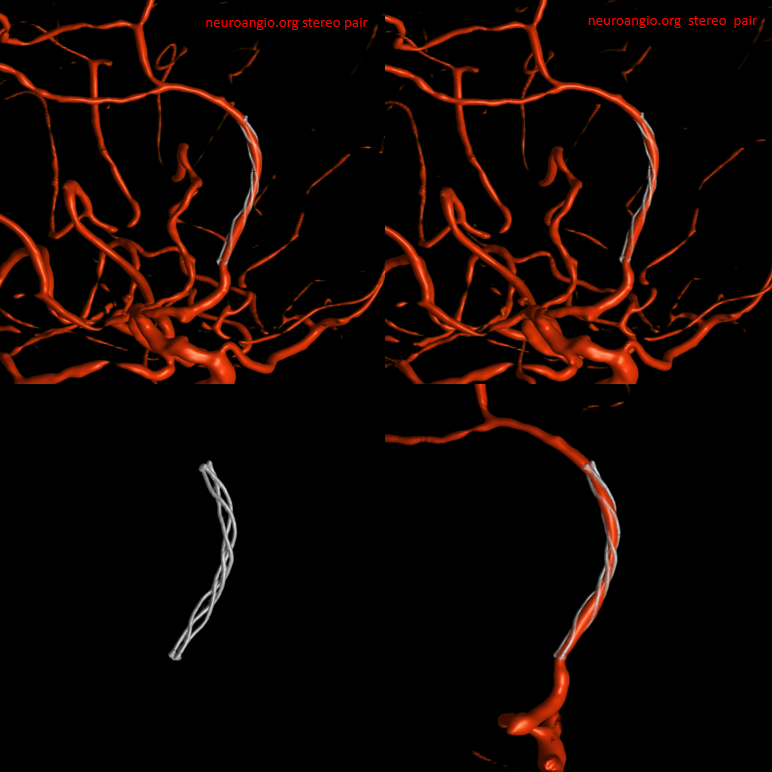
Low profile system is chosen due to anticipated A1 and other access difficulties. Setup is BMX, Sofia EX (115 cm), SL-10 (single tip), and Aristotle 14 standard. Traversing occlusion was not too difficult, but careful positioning of the microguidewire and slow advancement were still required. See how DSA from proximal A2 shows the path…
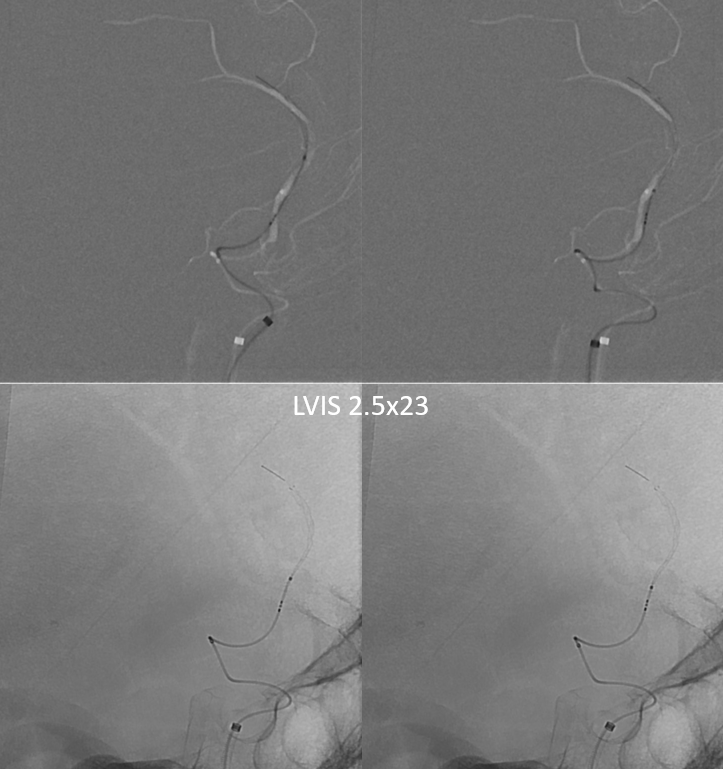
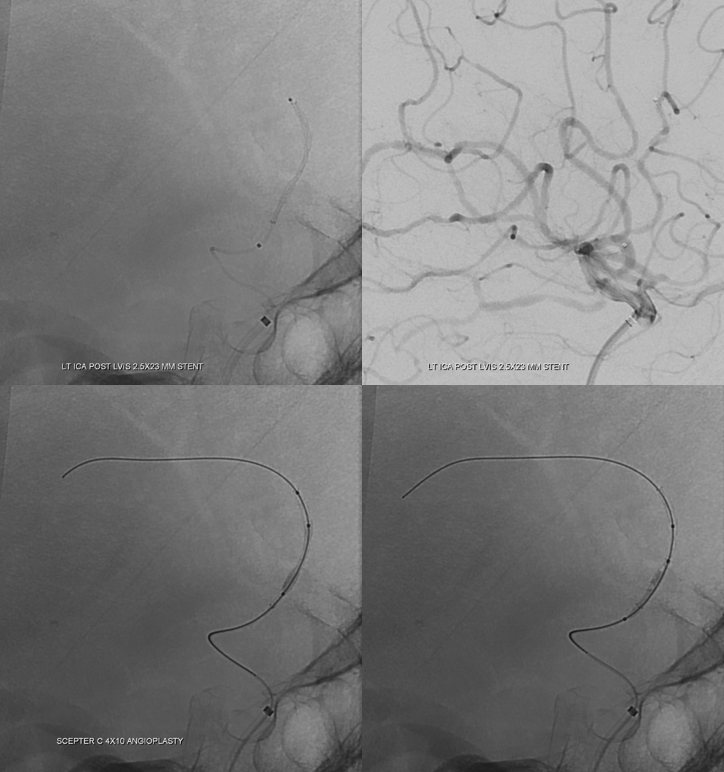
LVIS Jr was the plan from get-go. Certainly not the ideal stent for this, but in this anatomy this is the way in 2023. Images on bottom are done to make sure the stent is opening at stenosis level. Applying forward pressure on the microcatheter helps somewhat.
A post-deployment angioplasty was done after exchange of SL-10 for Scepter C. Probably would have worked to have the Scepter as microcatheter from beginning, but we were not sure if it would traverse the occlusion. Even though noncompliant balloons are obviously preferred for angioplasty, there the point is that it would be very difficult to get one up there in this case. So both LVIS Jr. and Compliant Angioplasty are examples of adapting to anatomy. As long as balloon is within the stent, and inflation is gentle, it can be done.
Angioplasty helped
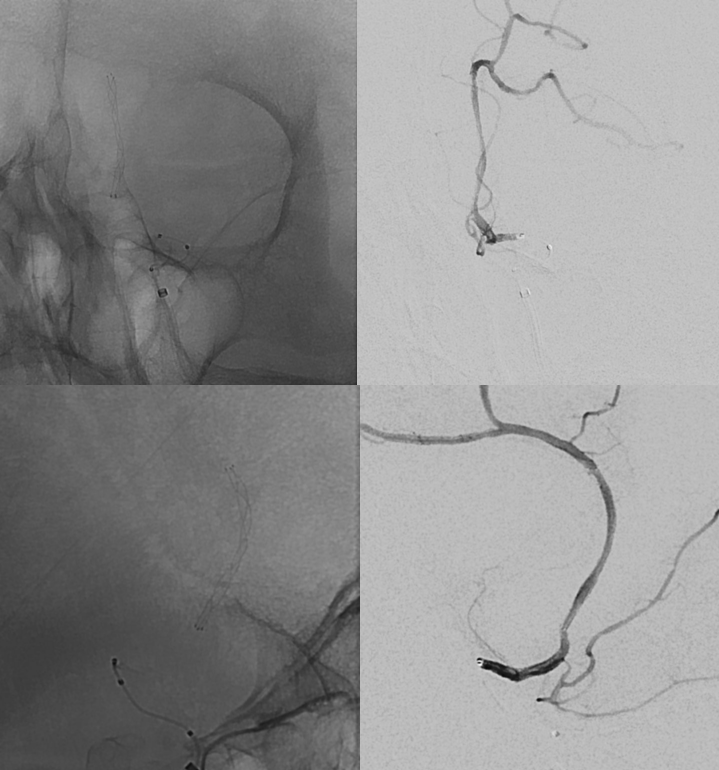
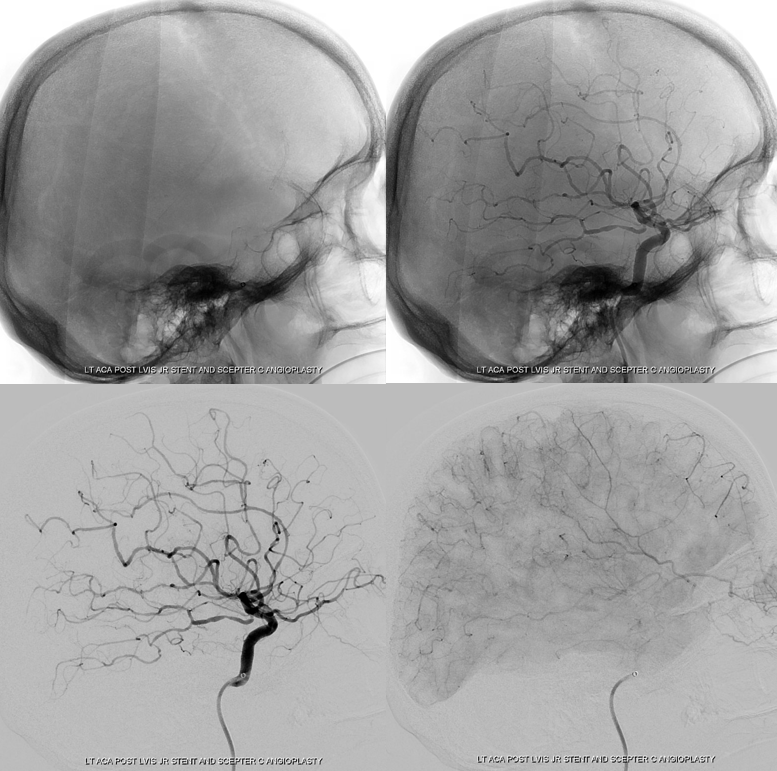
Still a bit slow in the frontal convexity, but much better than before
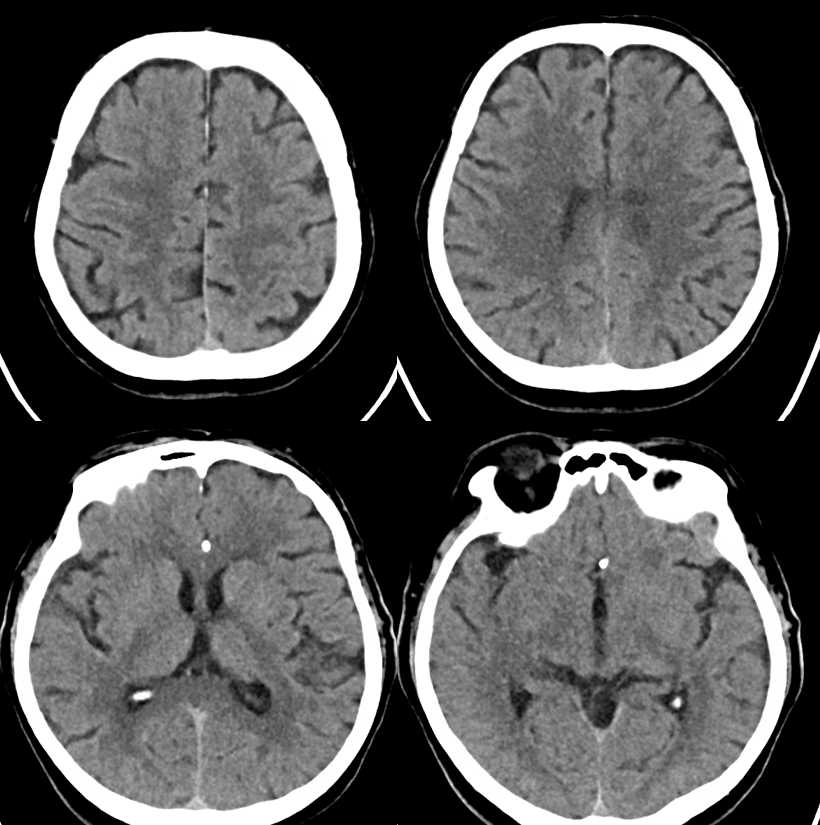
CT 2 days post