Case courtesy Dr. Eytan Raz
So, we are up to about 80% TICI 2b/3 for ICAs and M1s (this is 2018 now). Lots of talk about why we can’t get to 100%. Clot type, age, etc. All very important. Always better to take it out if possible. What does not get enough attention is acute intracranial stenting. Hard to imagine how acute stenting is going to be worse than a failed revascularization based on what we know now. Needs trial? Yep, that’s a really original thought. Sure, definitively needs trial, we agree. But what about now? The simple solution in many such cases is a stent. If it works, great. If it doesn’t, the antiplatelets can be reversed to allow for hemicraniectomy, safer trach, peg, etc. The reality is that stents have gotten much friendlier and simpler to use. There are a number of them that go though an 018 catheter and are really simple to deploy. The disadvantage is that they may or may not open against the clot. Or maybe its not a clot — could be dissection or intrinsic atheromatous disease. Then what? Salvage is possible but quite technically challenging and potentially hazardous. Which is why in these circumstances we prefer to use balloon-mounted stents. Off-label coronary stents. It is pretty amazing how flexible these things have become. And cheap. Much cheaper than self-expanding dedicated intracranial stents. They track almost as well as noncompliant balloons such as Gateway or Maverick. The short ones are particularly friendly. And if there are issues with going around the siphon, we as a field are now quite adept at putting a 5F catheter like Sofia right into the M1 to facilitate stent advancement. Only on rare occasions will a stent not reach the target with an intermediate catheter in the M1. The advantages of balloon-mounted stents are many. They are guaranteed to open. They do not foreshorten. They are easy to deploy and easy to see afterward. They come in drug-eluting varieties for atheromatous lesions, which we believe is useful. And they are so much cheaper. What’s not to like? Sure, even stents don’t always work. There is a potential added risk with antiplatelet requirements. Yet again, these don’t seen any worse than a TICI 0 outcome.
Here is an example of a patient with global right MCA syndrome. Head CT shows subacute right parieto-occipital infarct. This tells us two things. First, there may be a fetal PCOM. Second, there have been prior embolization events. So important to look at right cervical ICA
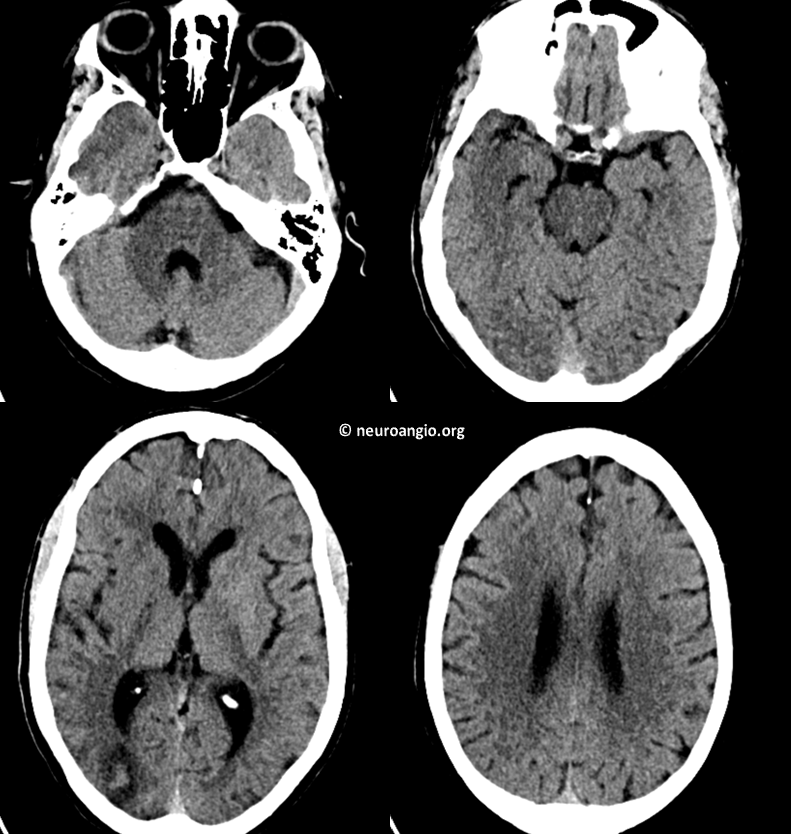
Typical Perfusion with decent upper division penumbra and likely proximal M1 occlusion based on lenticulostriate area flow deficit
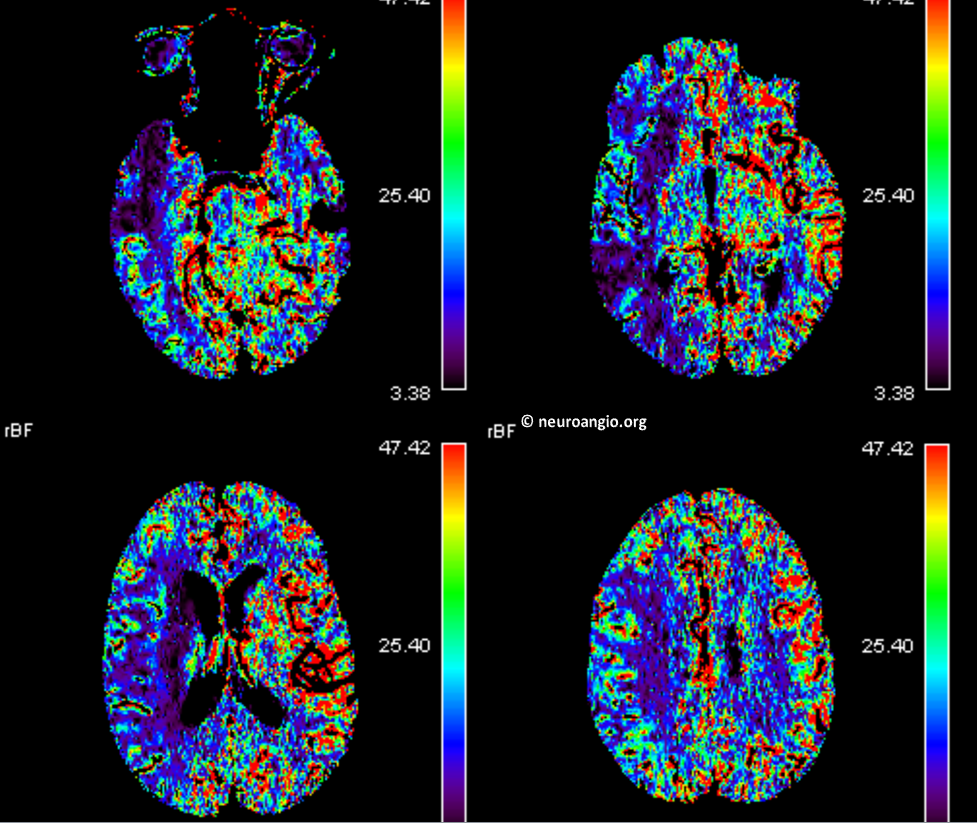
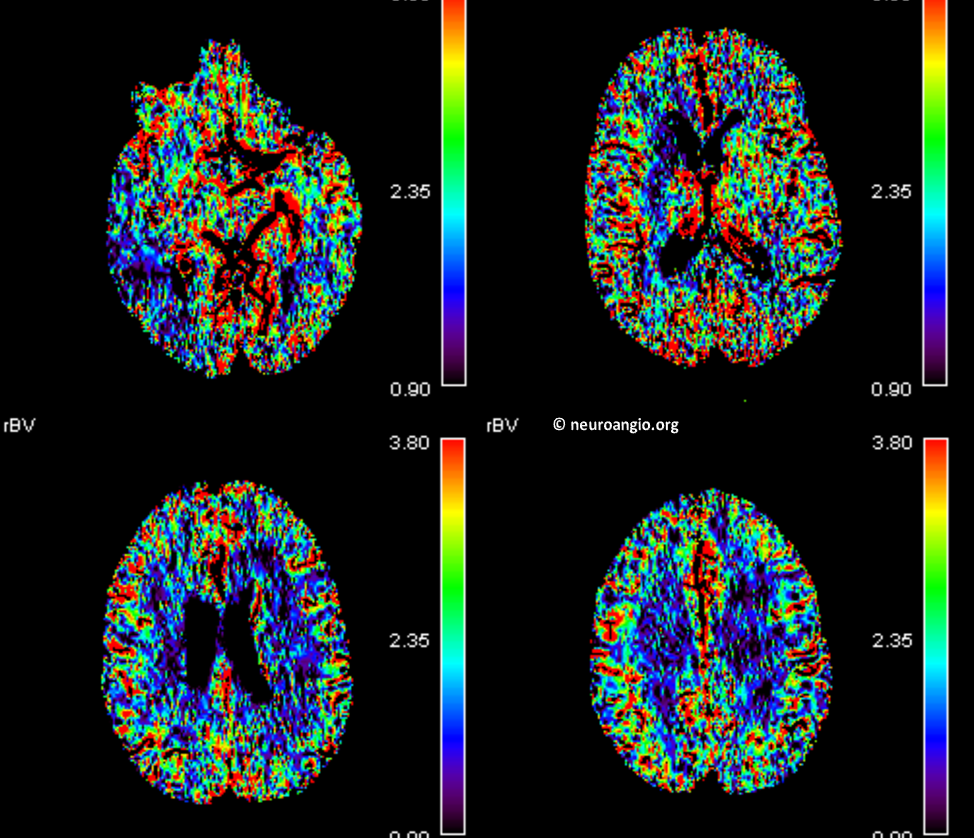
Volume maps below
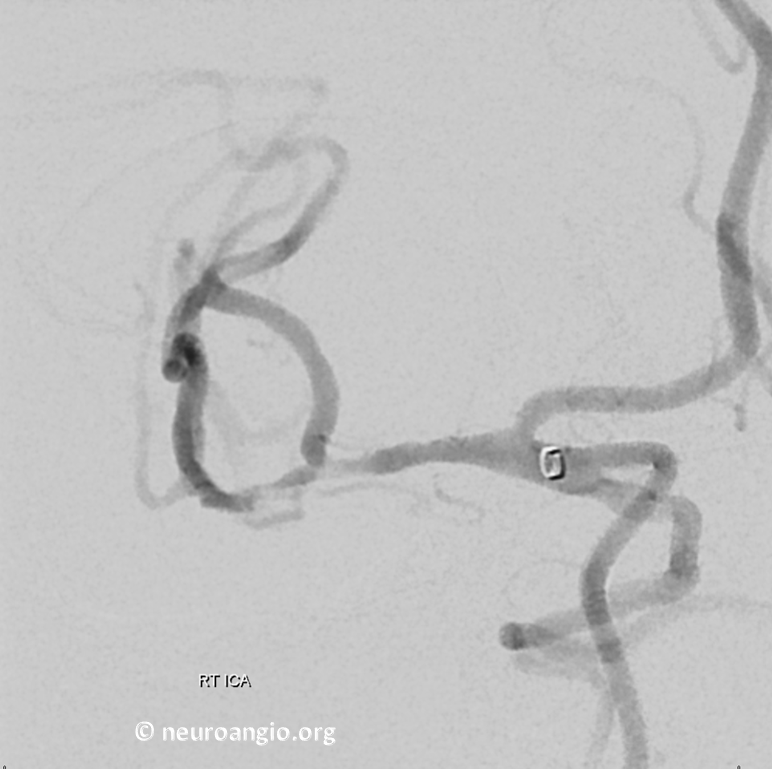
Angio of M1 occlusion
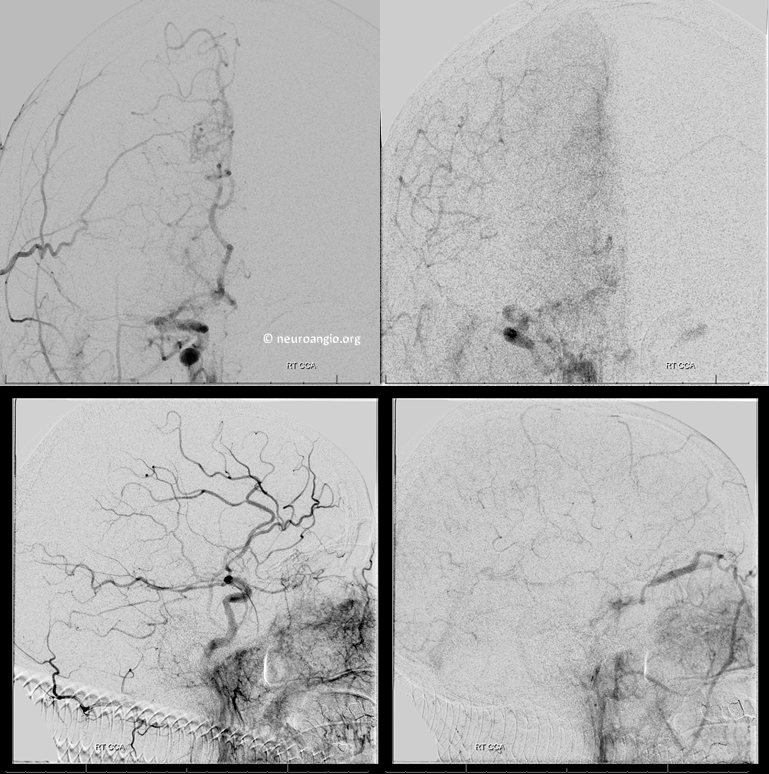
The cervical carotid was normal. Below is our standard straight suction Sofia 070 approach
First pass TICI 3
Time to go home? We usually don’t. We wait about 5-10 minutes and re-image. Here’s why
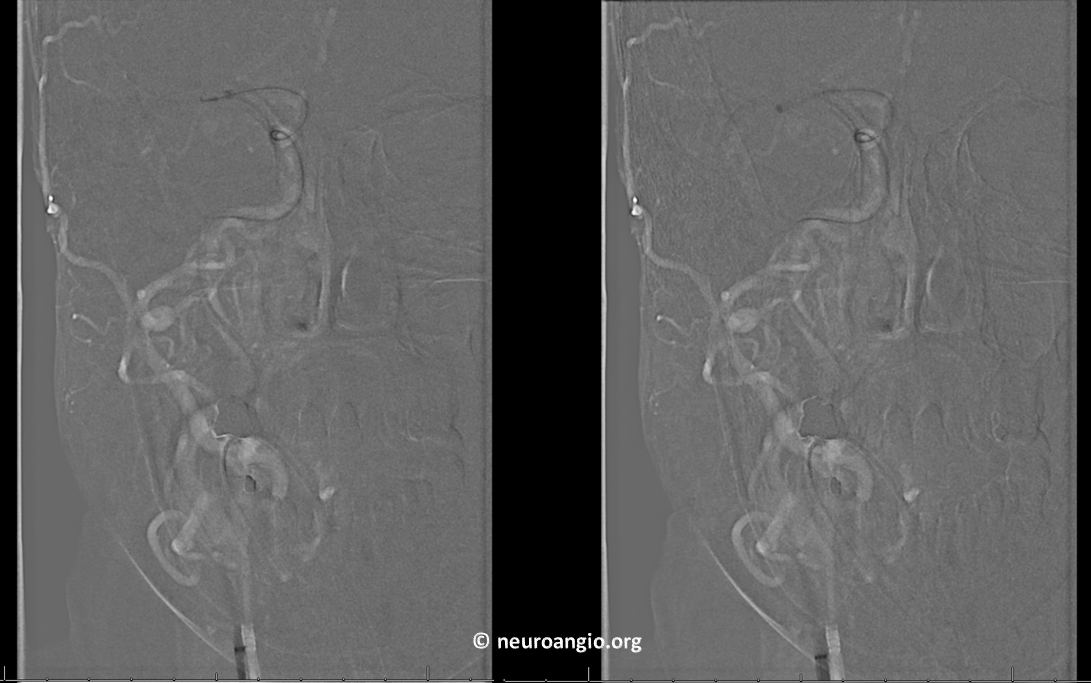
Looks like clot re-forming or something else going on. Could it be a dissection? Focal athero in otherwise clean vessels. Damage from Sofia? Last one is pretty unlikely
A few minutes later…

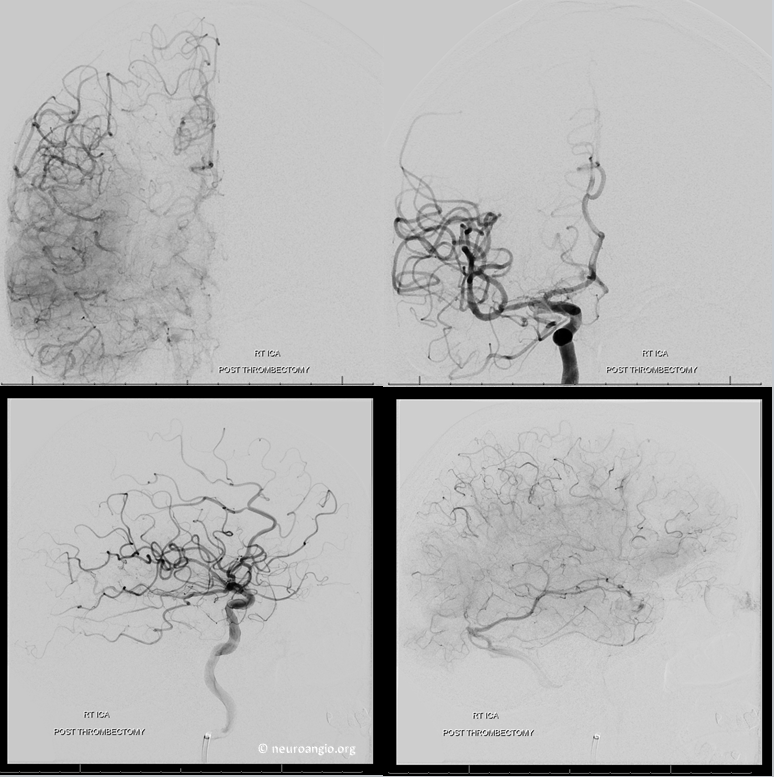
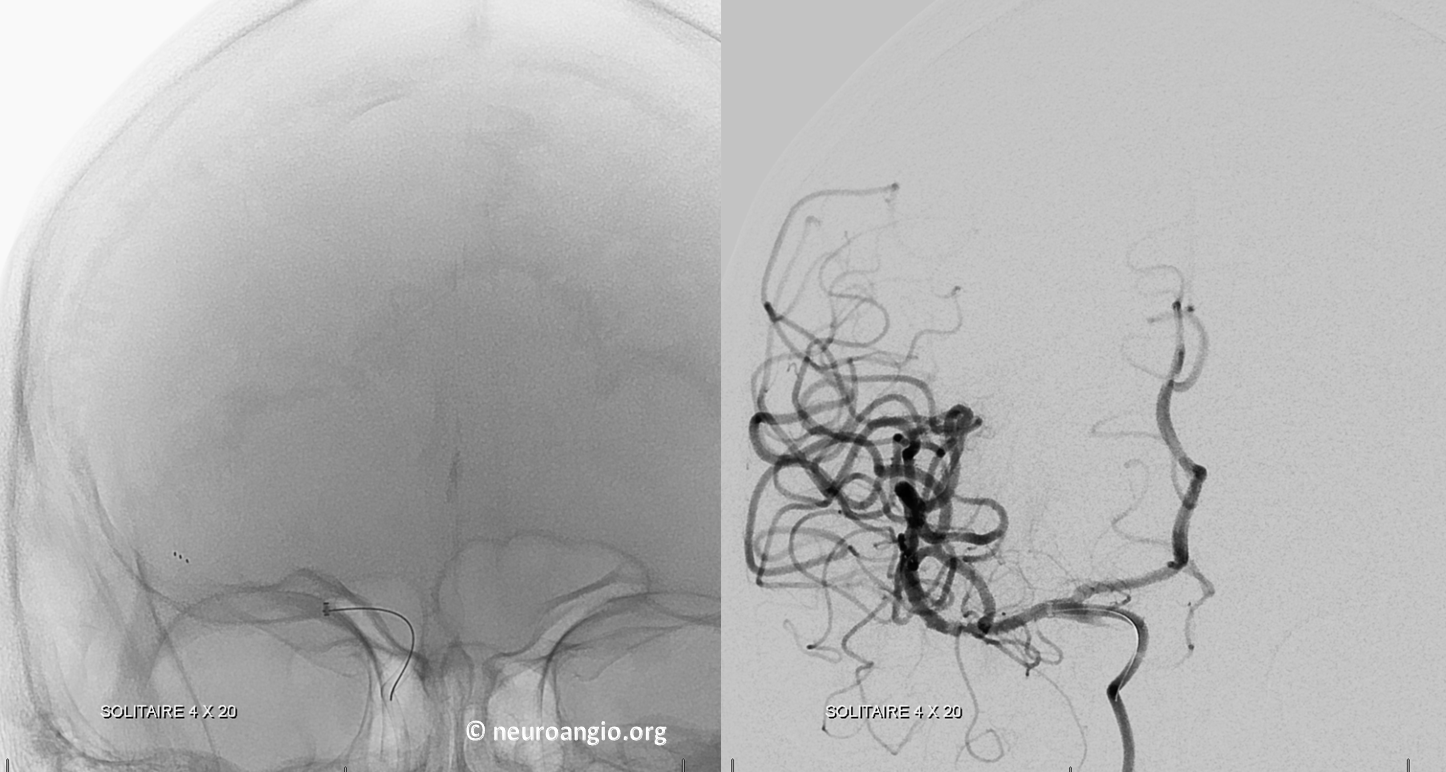
Had we gone home right after first TICI 3, everyone would have been scratching heads later. Now we don’t know why clot is re-forming, but we know what to do. Solitaire is next. Full re-perfusion with solitaire in place
Post Solitaire

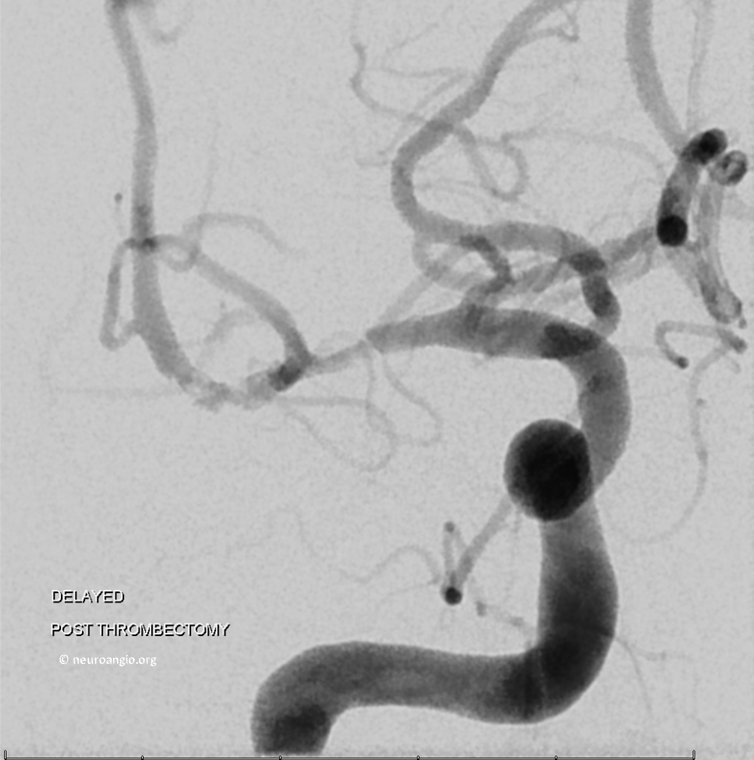
Delayed Post Solitaire.
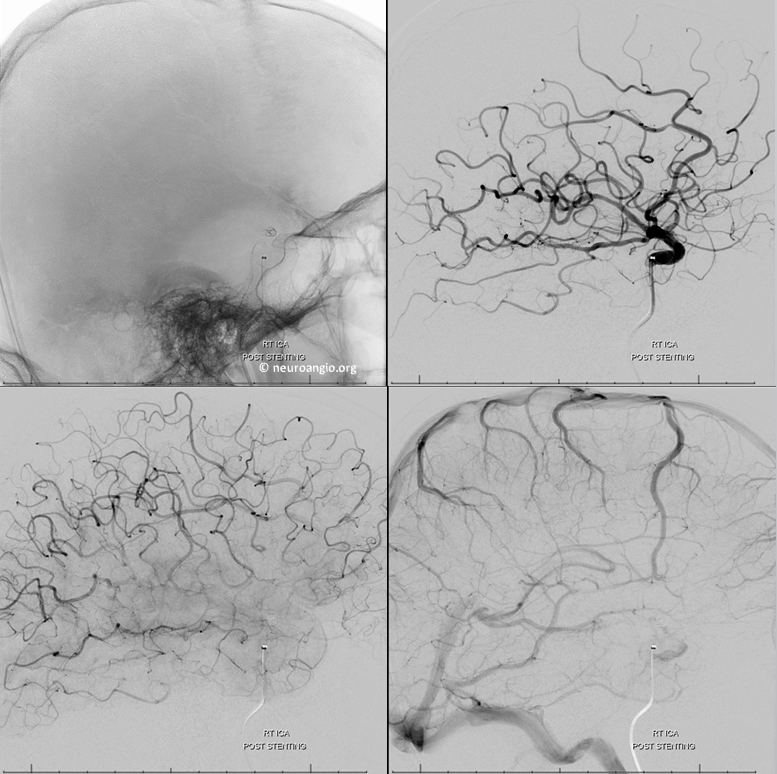
Time for the stent. This is a 2.5×16 mm Promus Premier stent. Our flavor of choice these days. The shortest is a 9 mm but even 16 goes in easy. Notice Navien 5F in carotid terminus to help with stent navigation. A softer 5F catheteter will likely do just fine also. It can’t be too long though, because coronary stents usually have shorter delivery systems. Check before you go.

Global post frontal views, back to TICI 3
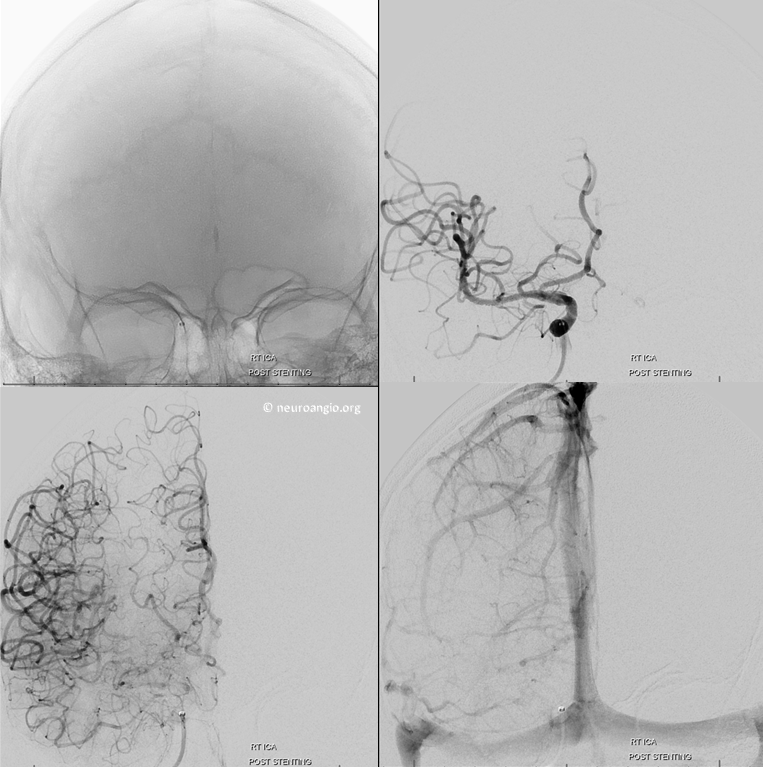
Lateral
CT post. Contrast in dead gyri
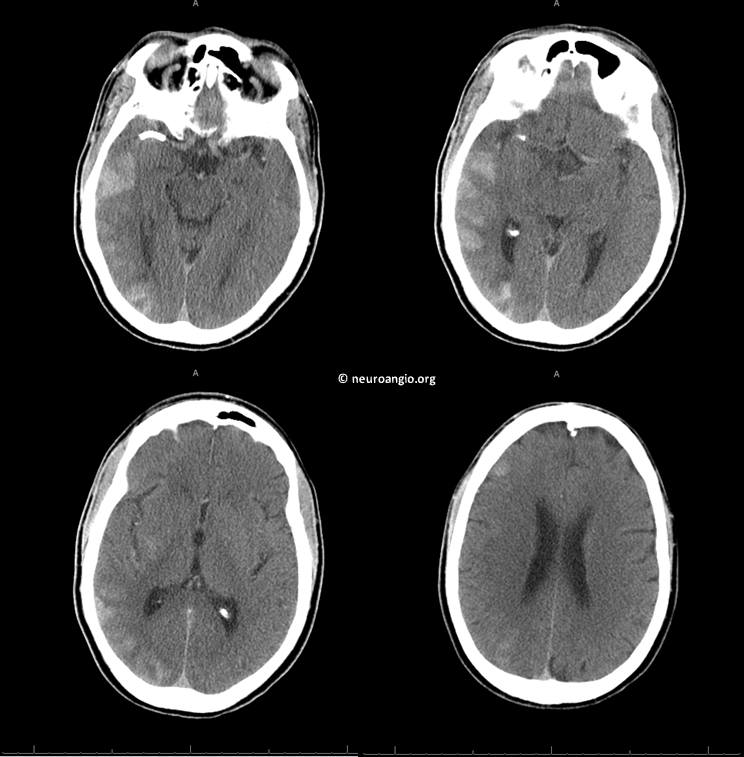
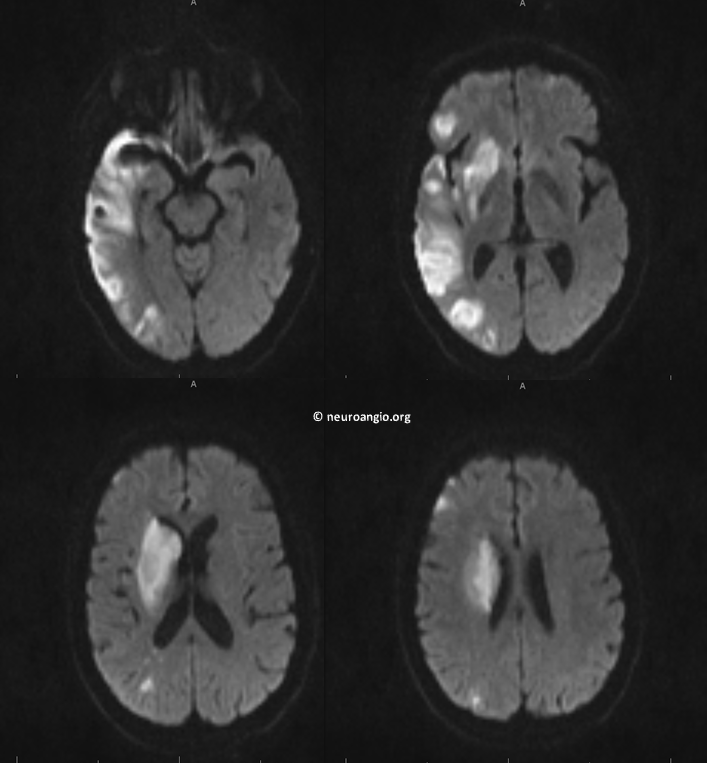
MRI on day 3 post-procedure. Looks just like CBV perfusion maps. As good as one can ask for. No hemorrhage. Patient is antigravity on the left. What’s not to like?
Further reading?
Check out Korean experience below. Sure, they got more intrinsic disease than we here do. Stents don’t always work, for them or for us. However, in this publication at least, the outcomes are better with stenting. We have had the same experience.
Bibliography:
