Well… See the MCA page. What is an M2 exactly — in this case its functionally more like an M1 or at least a very dominant M2 — just more distal. Rhoton would call it M2. In terms of “penumbra” it may pass as an M3 — slowly progressive athero can induce a lot of leptomeningeal collateralization and limit extent of dysfunction. Lots of learn here.
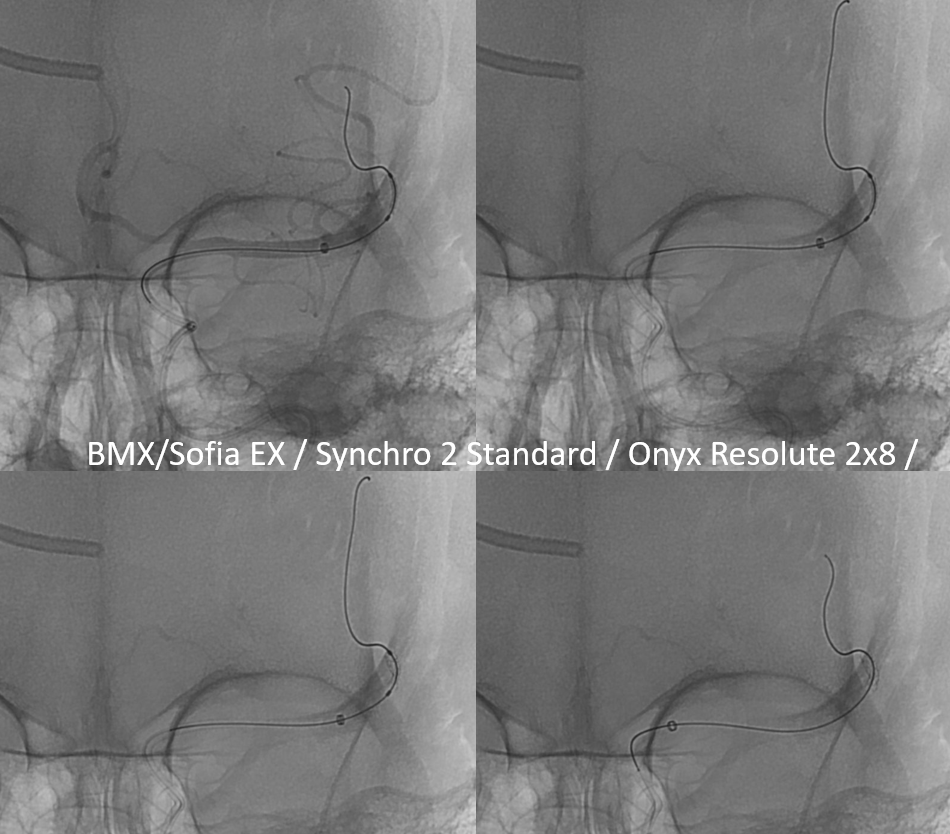
Presentation is with pressure-dependent / perfusional expressive aphasia. The small amount of penumbra in setting of a large proximal occlusion should make one think of intracranial athero
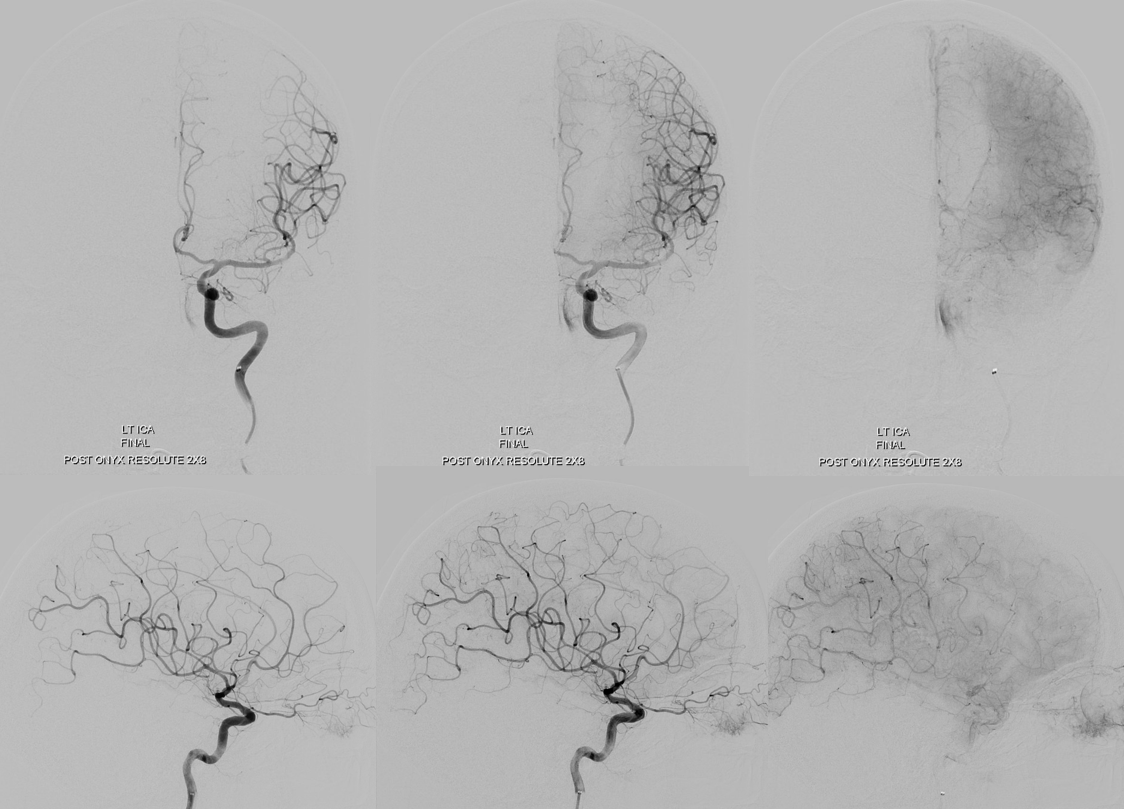
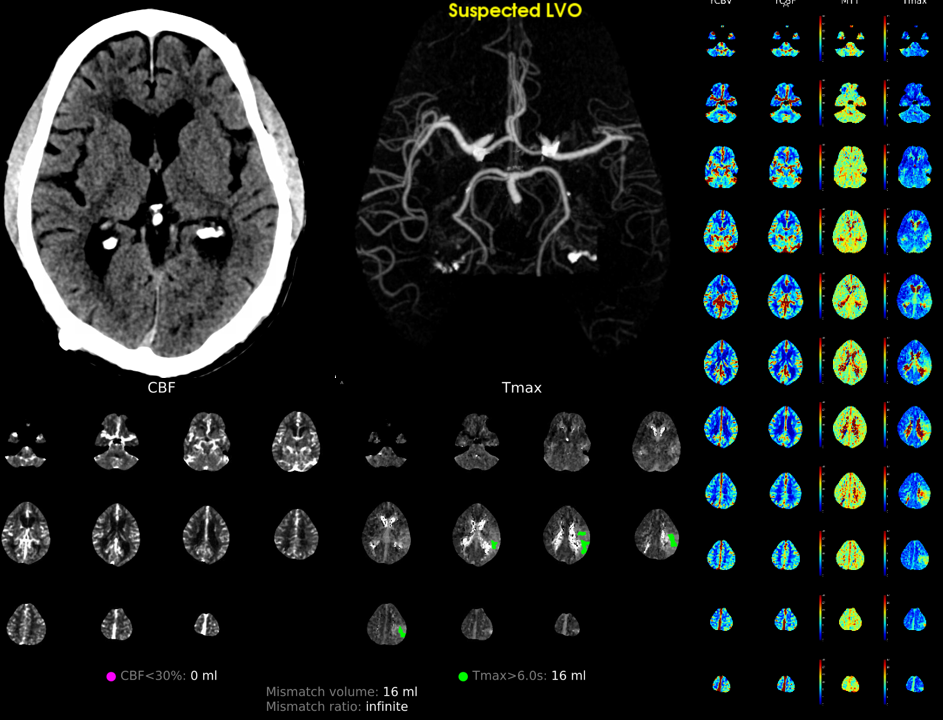 Excellent leptomeningeal collaterals
Excellent leptomeningeal collaterals
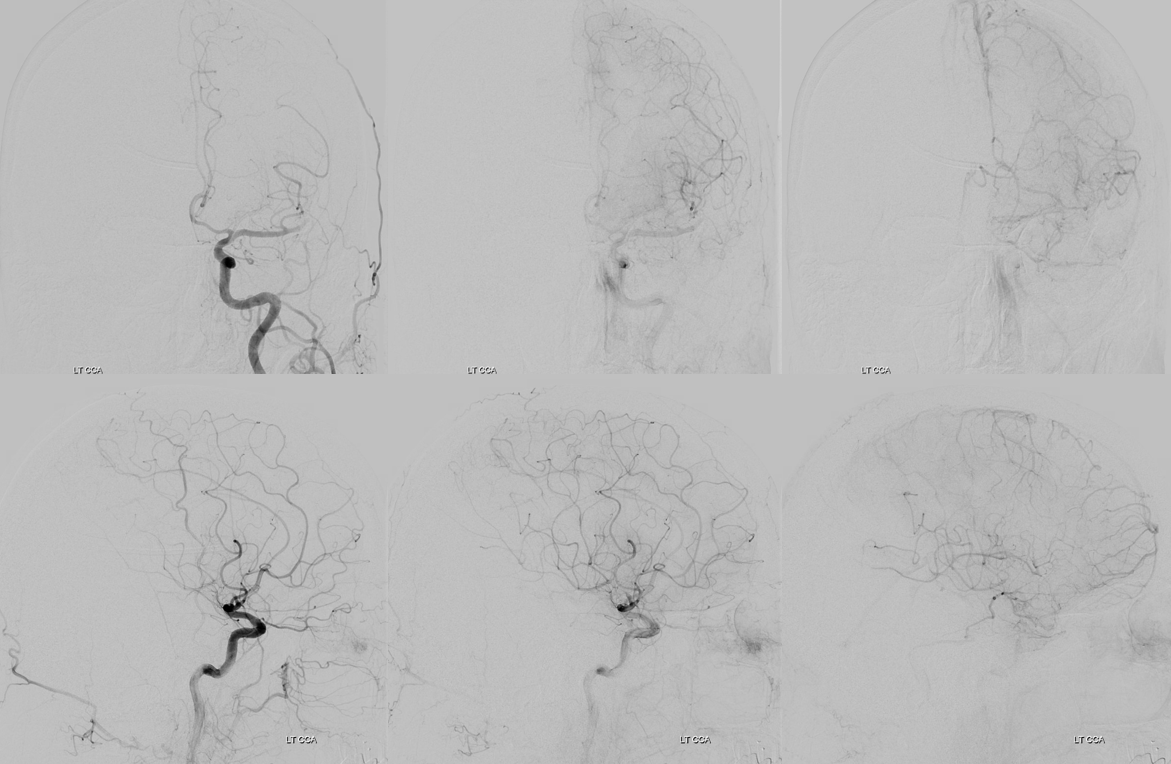
Another thing that favors athero is inability to make any progress in revascularization despite large bore catheter aspiration attempts. We tried aspiration twice with no improvement

Classic athero picture — the occlusion is not at a bifurcation / branch point. In this case lets stay its a mid-M2 of dominant inferior division. The Solitaire shows where stenosis, and where bifurcation is.
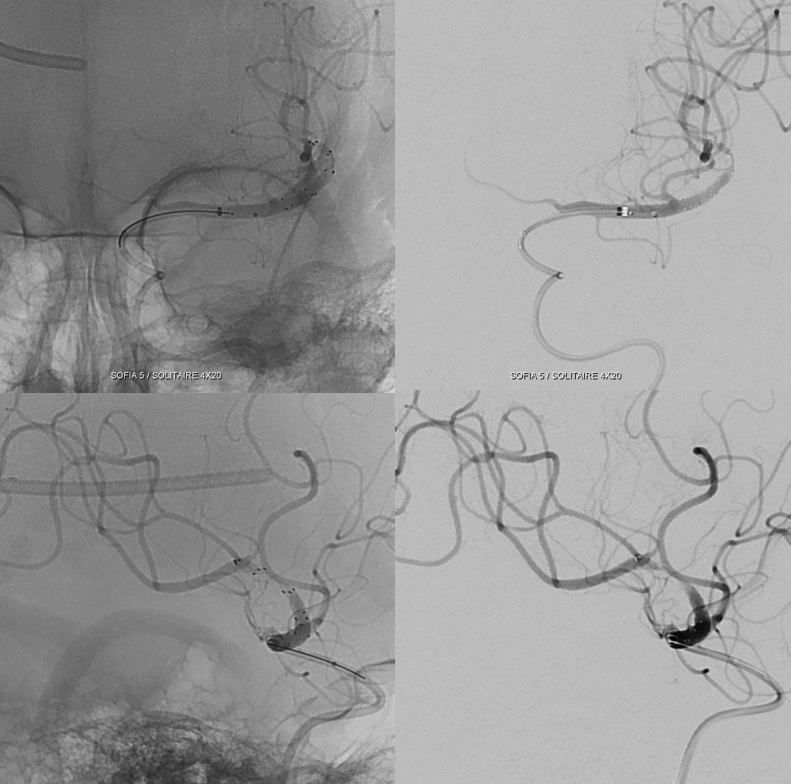
Yet another characteristic of athero — nothing retrived despite 2 solumbra attempts, with a small channel made through the occlusion that threatens to re-close
Measurements are improtant. The smallest diameter balloon-mounted stent we have in 2023 is a 2×8 (Onyx Resolute). The distal vessel is 1.4 mm but likely larger in reality (diminished caliber due to less flow demand now). So a 2 mm stent is reasonable.
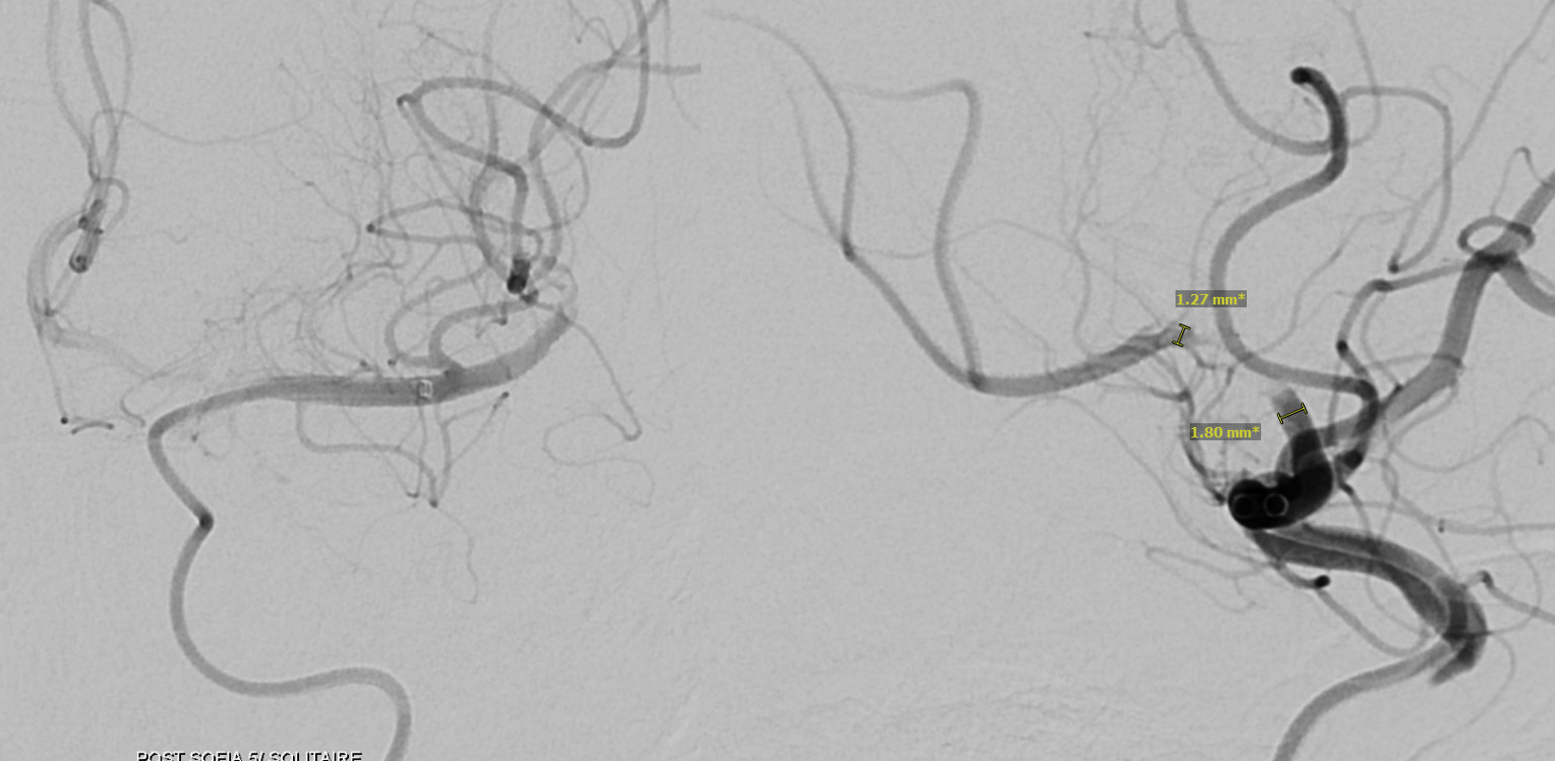
We inflate the balloon gently, to suboptimal size (3 atm), the deflate, check for perforation, then inflate again, to something like 4 atm. Check again. Better to go slowly.
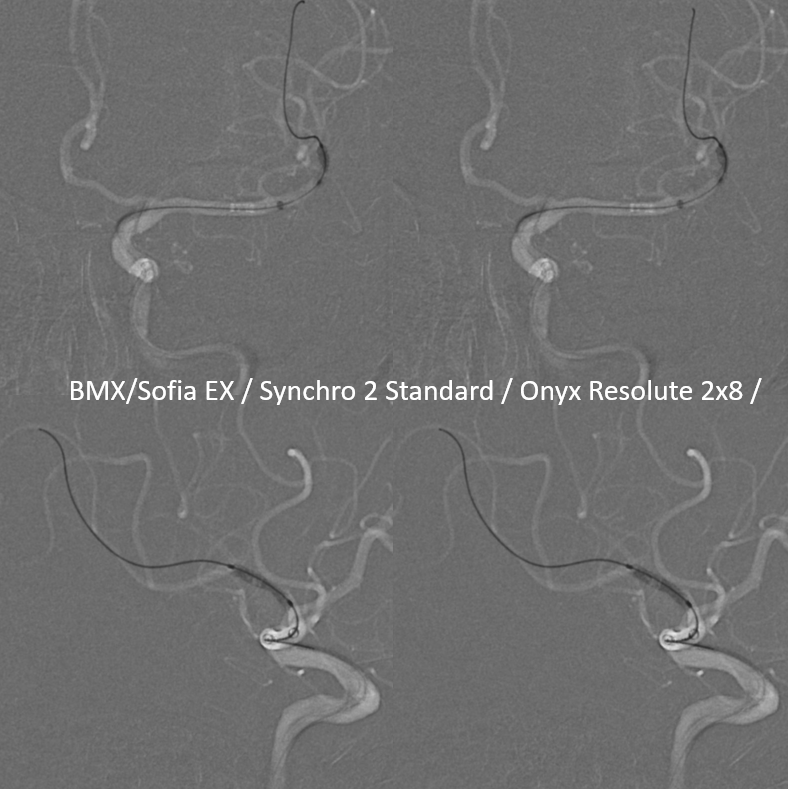
The ballon has to be inflated to at least 1 atm below nominal – underinflation will cause uneven opening of the stent. Worse still, the stent may not come off the balloon, and move proximally, as balloon is being withdrawn.
Almost done. See that waist at the level of stenosis. Need to inflate a bit more.
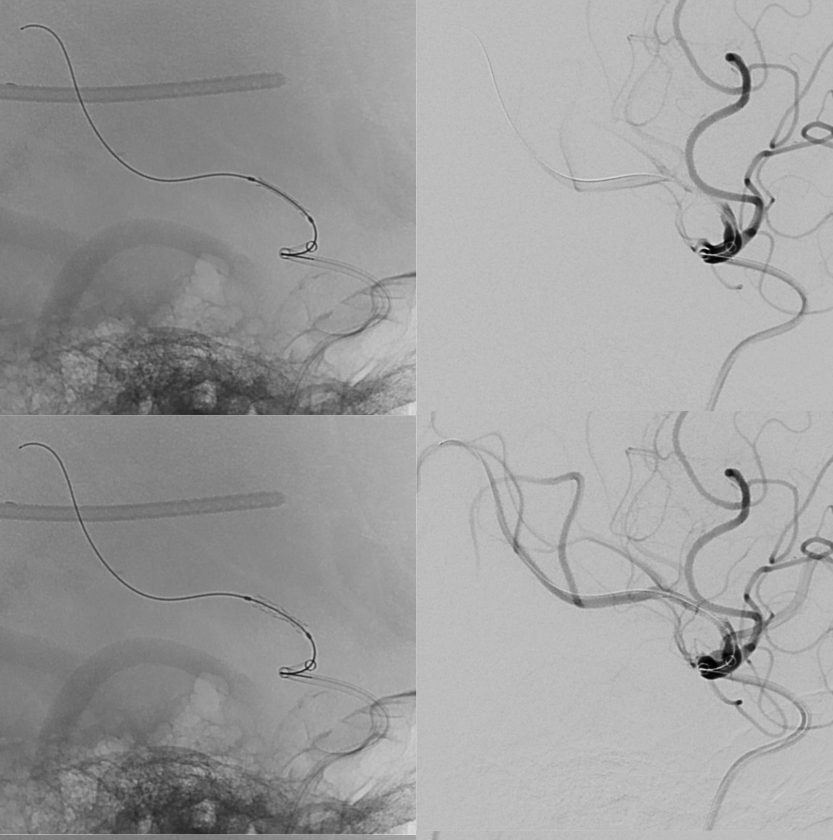
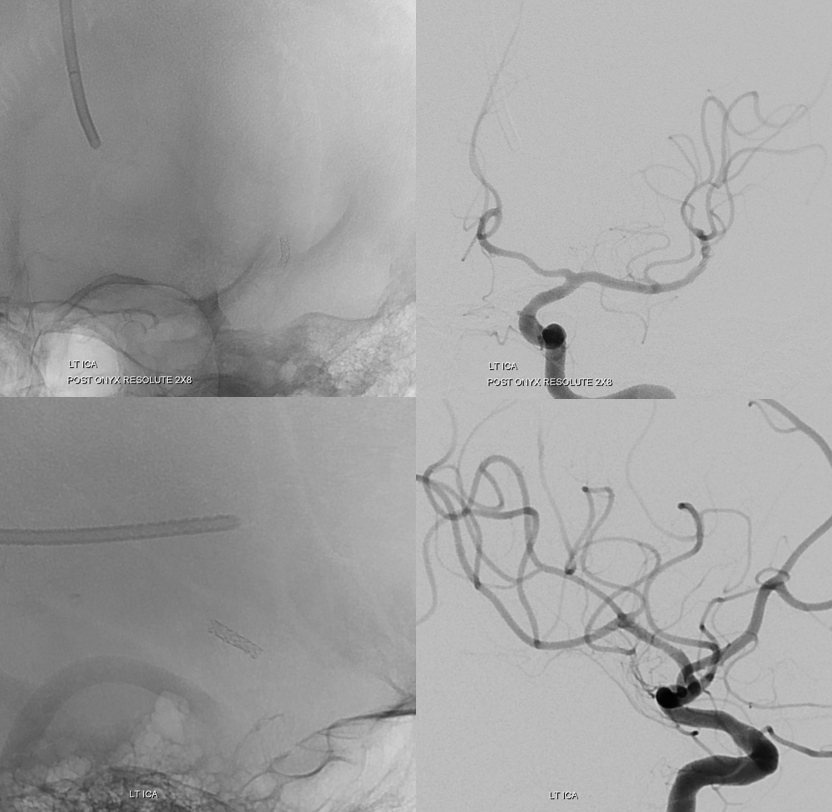
Post. Nice revasc.
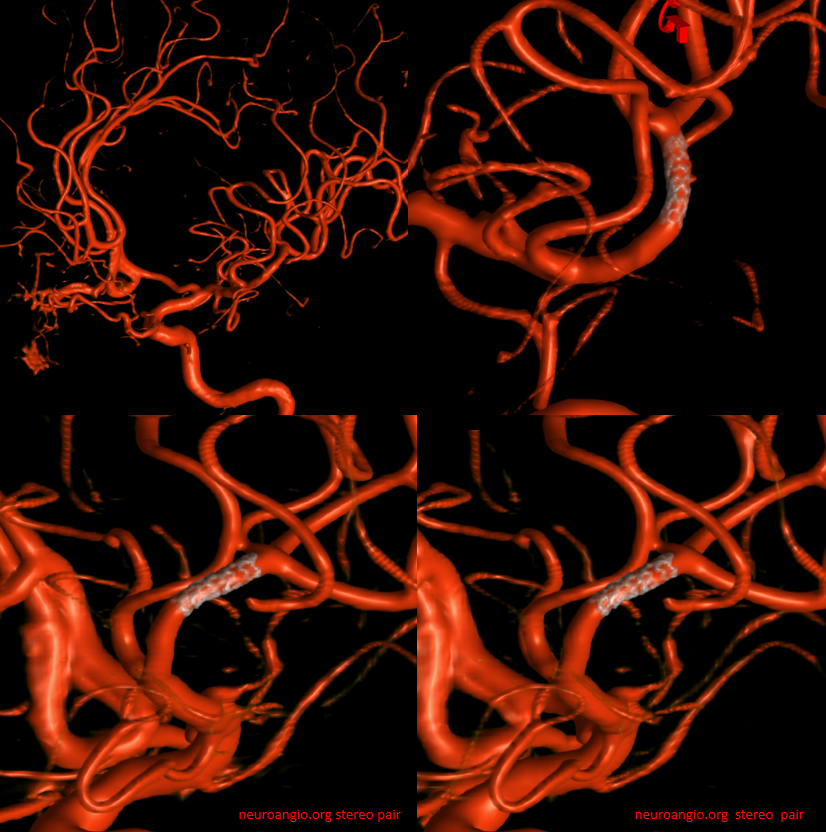
Good to look at the source images of the rotational angio / 3D-DSA we did to get those nice pictures above. What do we see? Typical subarachnoid / subpial hemorrhage in the fissure after Solitaire pull
What to do? Staying calm helps. There is no clinical change and no extravazation on angio. Reversing antiplatelets right away is not a great idea — the stent will close. Repeating DYNA after 30 min or so is a better option. Looks stable — better imaging is due to selection of the 70 kEv DYNA version, over the 109 kEv one above.

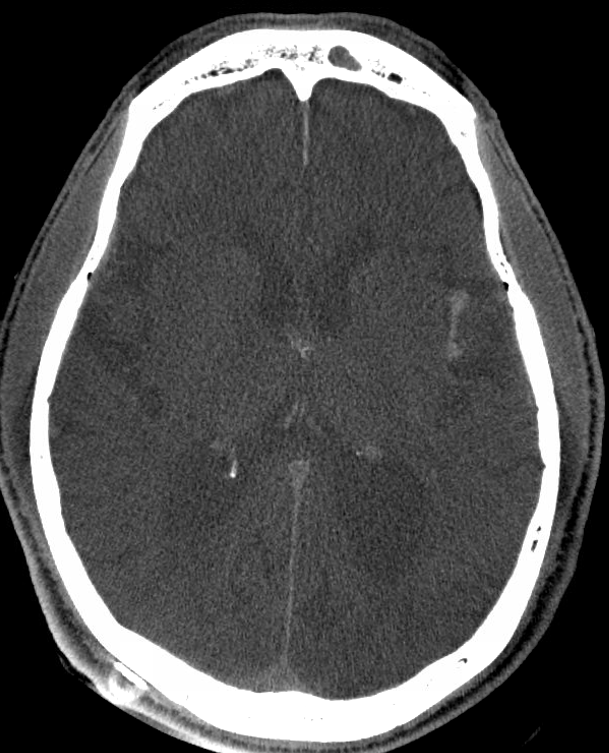
Holding some antiplatelets (integrilin drip) while maintaining some level of inhibition (PR aspirin) is usually the choice. Below are “real” CT scans obtained right after the procedure, and in delayed fashion. No more bleeding, resorption ongoing. 12 hours later we give Brilinta and start full dose duals

Post imaging next day
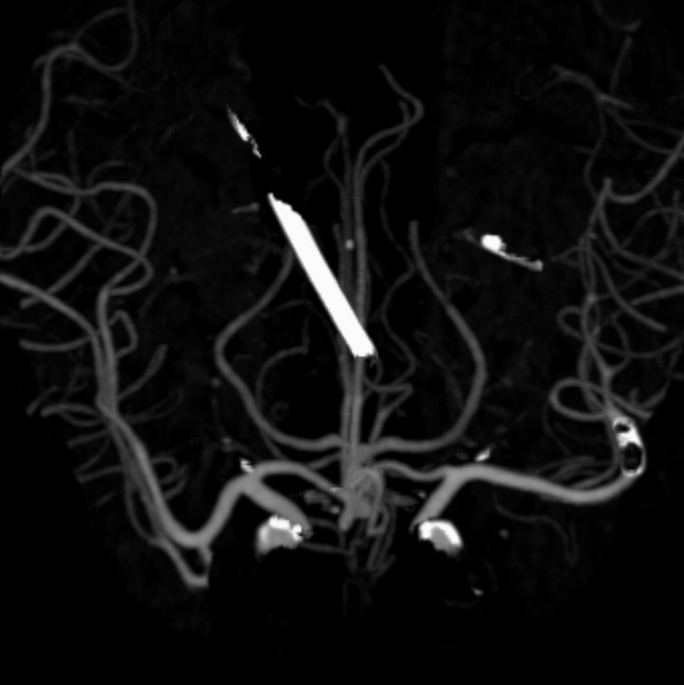
Yet, NOT ALL IS WELL WITH this case. Three weeks later, the stent re-occludes. What happens next? Click here to find out…
See other subacute revascularization cases on Case Library page
