Pipeline is by far the best device as of 2024 for unruptured paraophthalmic aneurysms. Safest and most efficacious. Still, at least 10% of cases are “failures” by strict criteria of aneurysm nonocclusion. For aneurysms less than 10 mm these angiographic failures are almost never clinical failures — aneurysms dont rupture and there are no peri or post procedural complications. Nevertheless, it is improtant to understand why treatments fail. It helps us succeed more in the future. The number one reason, by far, why properly implanted pipelines fail, is because of an outflow source — an artery that is incorporated into the aneurysm, with its outflow keeping the aneurysm alive as well. Its a complex topic, but thats the bottom line.
Most of the time, this artery is incorporated into the aneurysm to begin with (ophthalmic for example). Sometimes, however, it becomes secondarily incorporated, or part of a fusiform segment — as in the instructive case below.
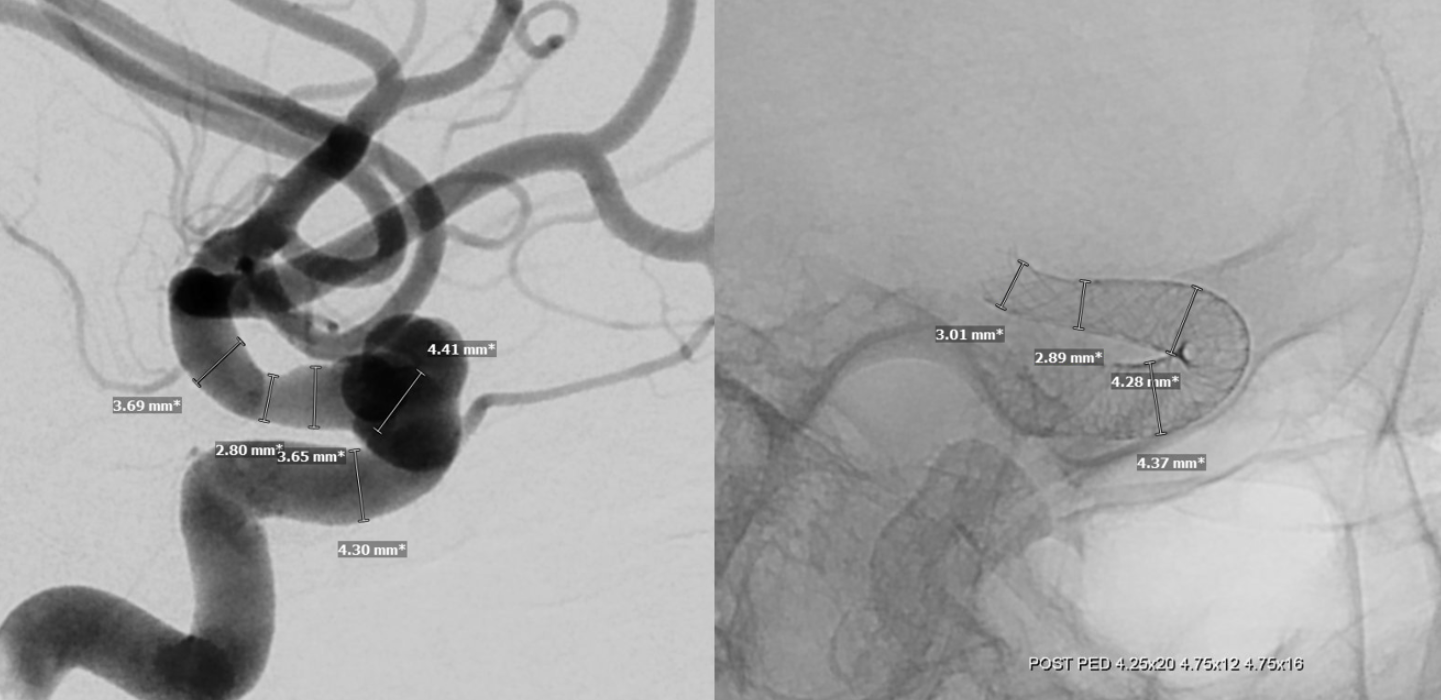
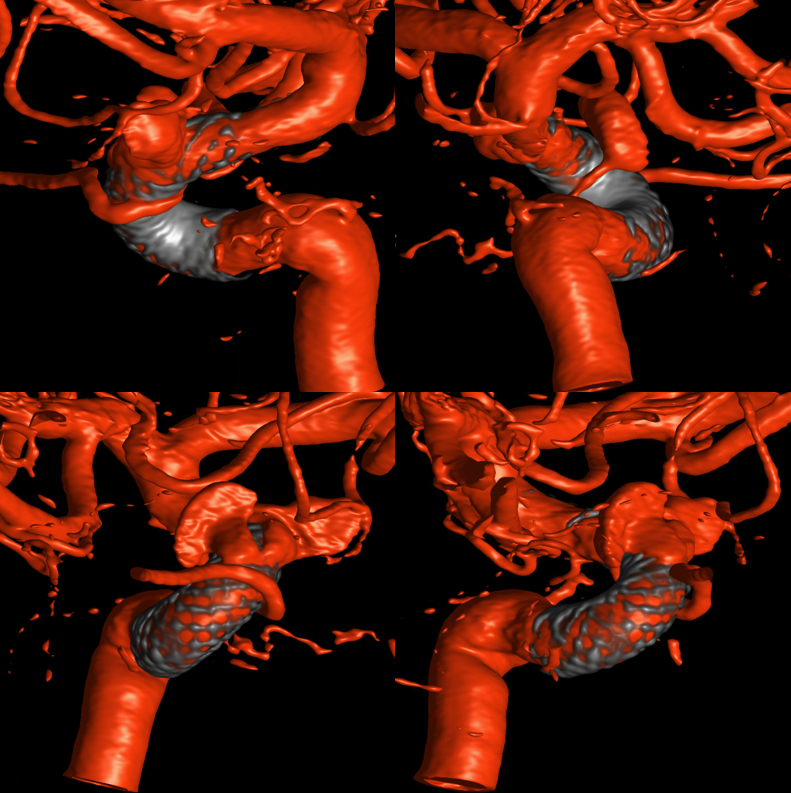
Here is an aneurysm. see DYNA images — dont try to count how many aneurysms there are. Its a silly task. The whole paraophthalmic segment is dysplastic and aneurysmal.
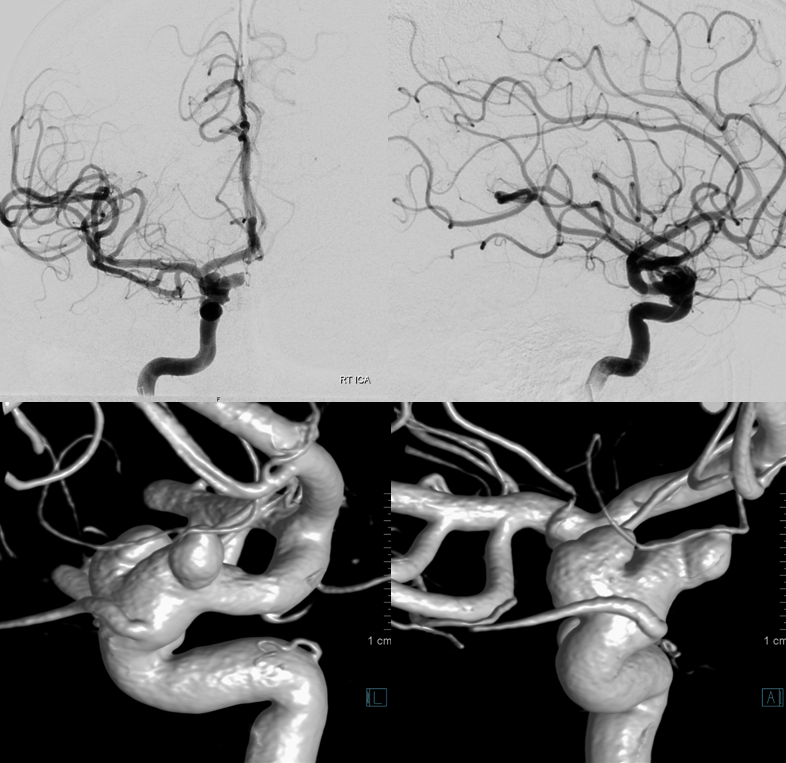
See how the origin of the ophthalmic is associatedi wth a bulging, fusiform dilatation of the ICA. That’s the problem. The PED will not appose it, even though it is the most flexible device on US market. I think a nitinol device would do better here actually, we just dont have them.
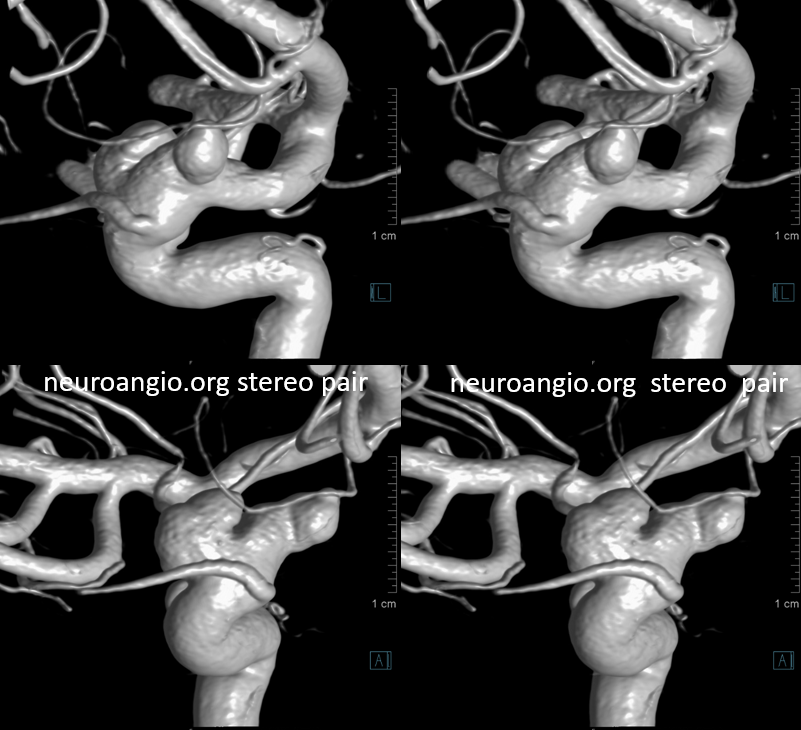
The other problem is a big mismatch between the distal landing zone and the aneurysmal segment. Sizing of the device should not be to the proximal landing zone but to the fusiform segment — to try to appose the walls there as much as possible
See how despite excellent technique the device diameter at aneurysmal sement is less than the wall. Thats what always happens in fusiform types — but here we have the ophthalmic…
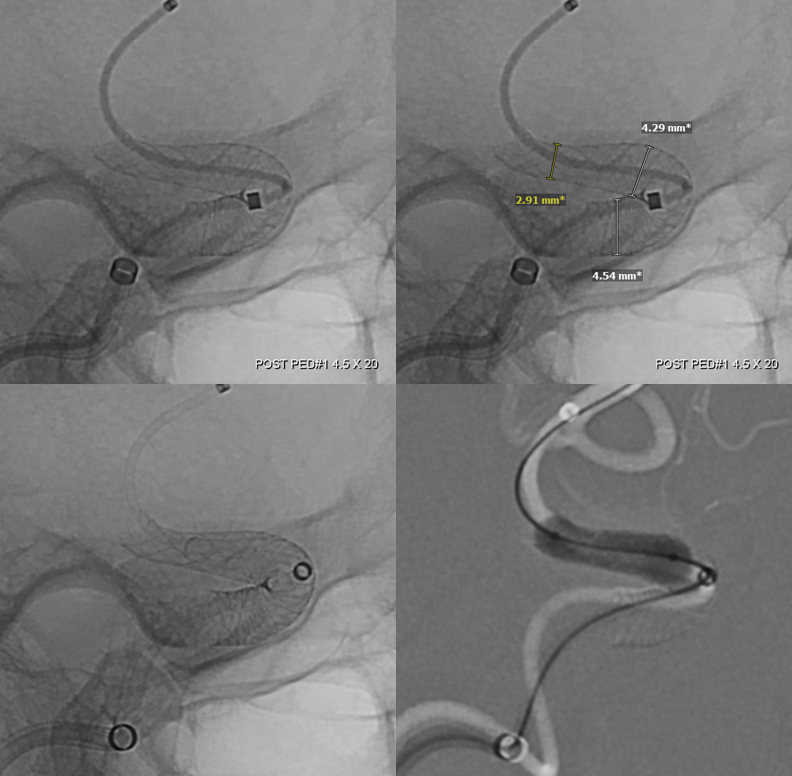
More devices are needed in this setting — to maximize probabily of success is what we think. Still…
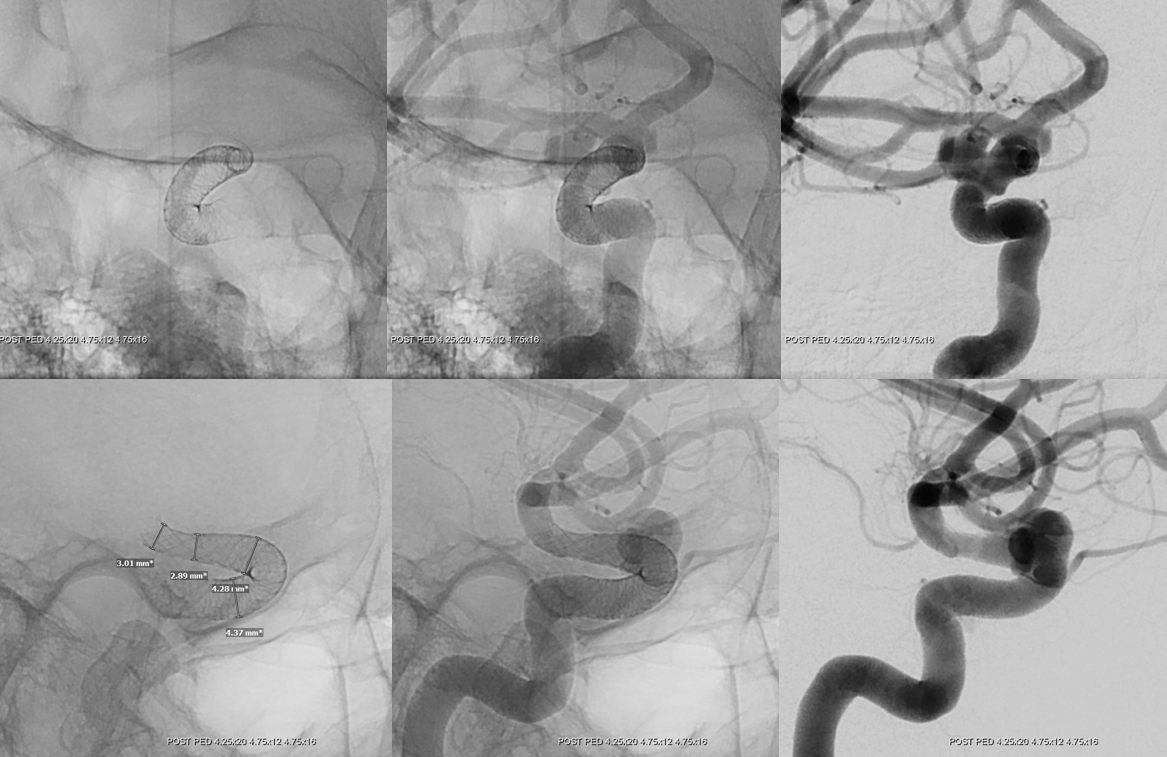
Pre-implantation dimentions on left, device construct dimentions on right
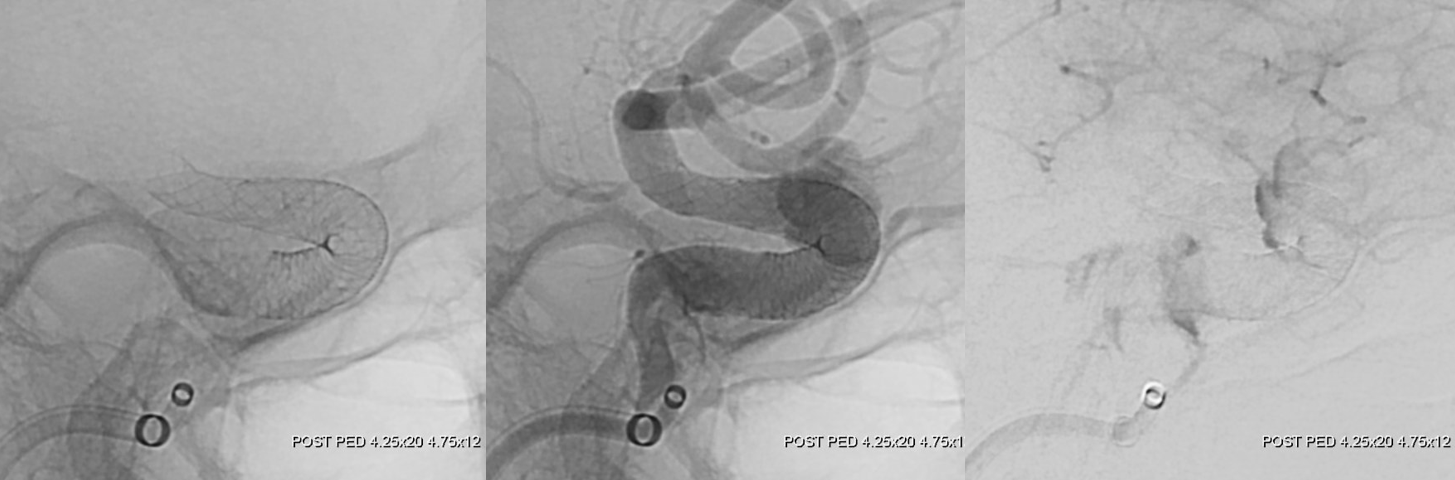
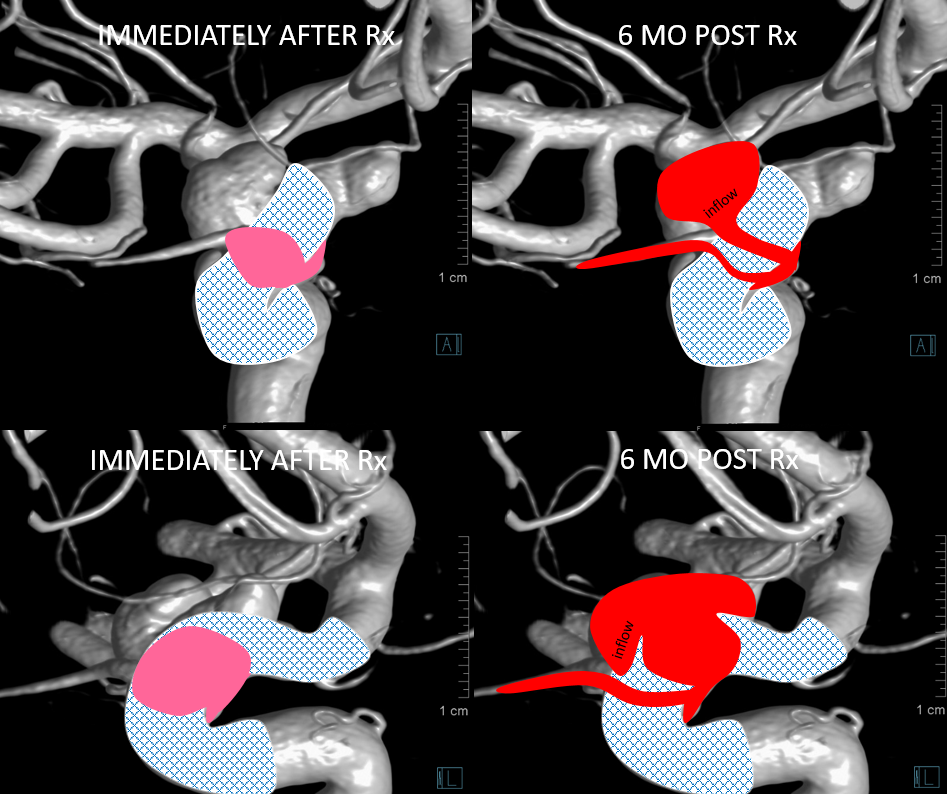
6 mo post
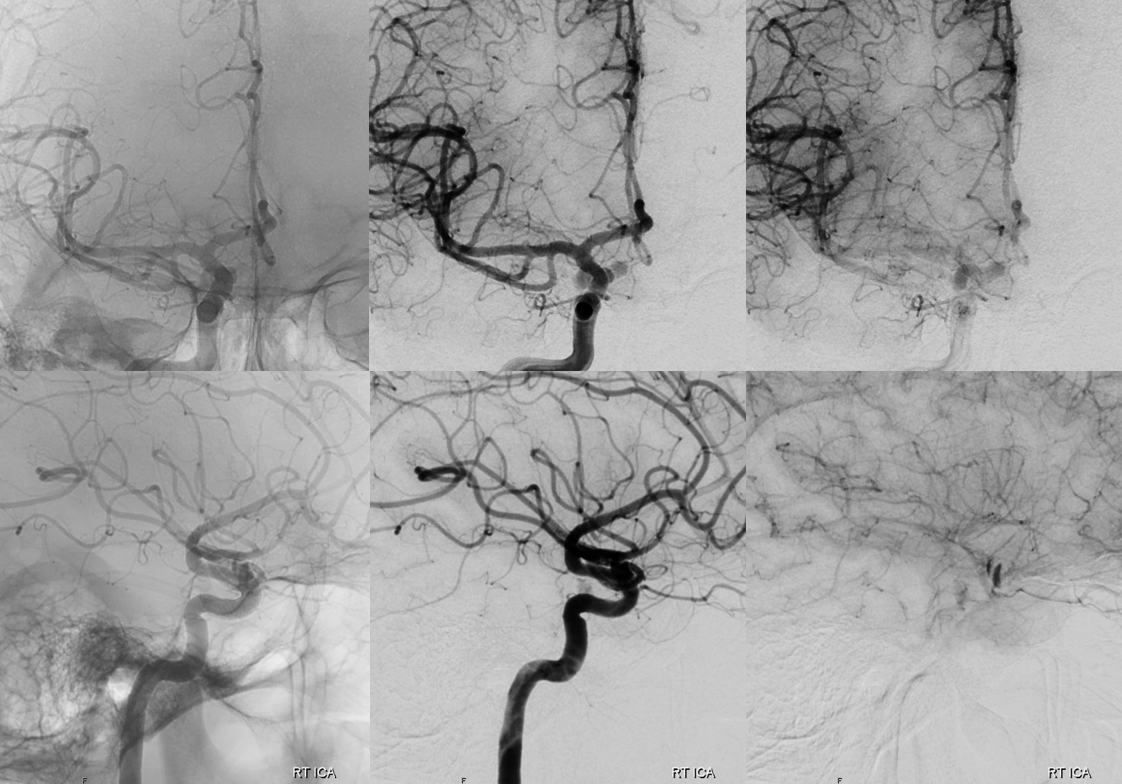
What happened?
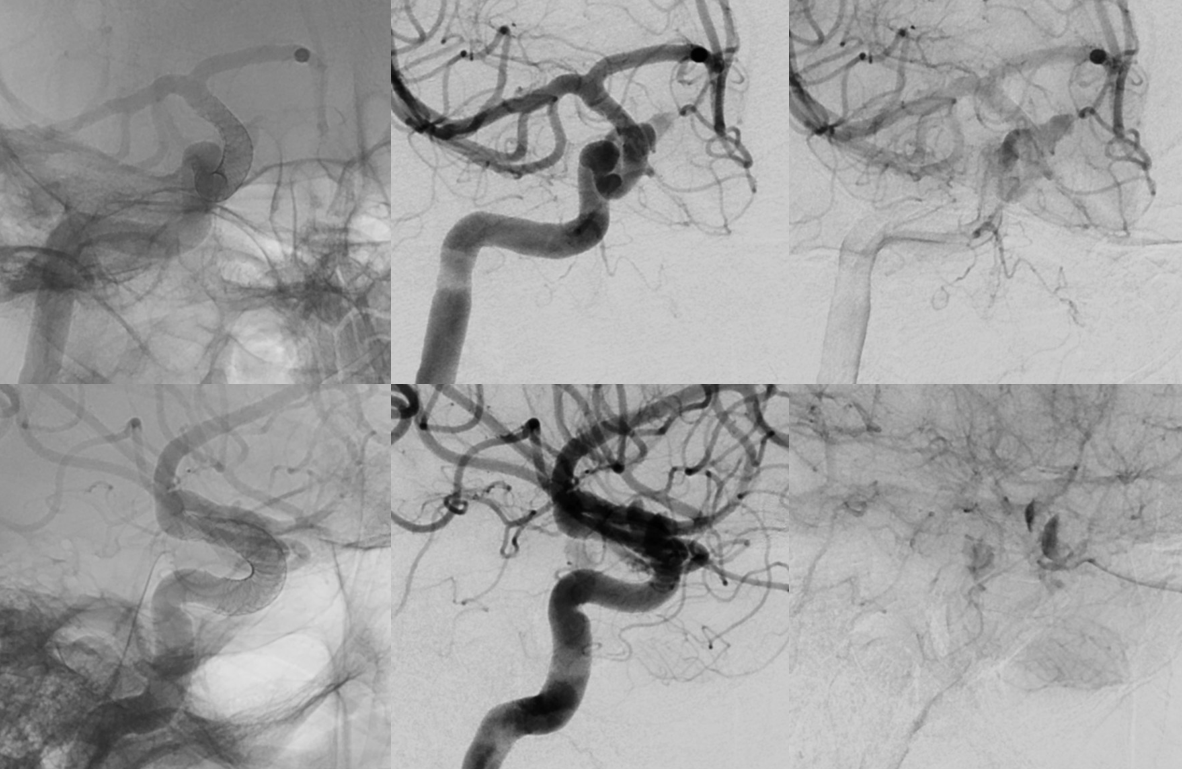
Ophthalmic secondarily incorporated into aneurysm backside. Anterior genu area of inflow, ophthalmic is the outflow.
This is the idea — post Rx there are areas of incomplete apposition of device construct to the wall (pink) due to fusiform nature of the segment. This results in device not apposing the ophthalmic artery ostium, which remains part of the aneurysmal segment outside of the pipeline construct. Over time, endothelialization / intimal overgrowth/remodeling correct much of the fusiform segment, however a new pattern of ophthalmic outflow maintains aneurysm patency
See Pipeline Device Aneurysm Selection Page for more examples
