With Drs. Benjamin Brush, Koto Ishida, and Erez Nossek
Venous sinus thrombosis is more a problem of parenchymal venous drainage than sinus itself. If blocked cortical veins can find drainage to other open areas such as cavernous sinus or SSS and contralateral patent jugular outflow, there is less of a problem than if veins have nowhere to go. Which is why straight sinus thrombosis is so treacherous — if it extends into the Galen the internal cerebral veins have very limited collateral potential for alternative outflow.
This patient presents with typical symptoms of this process — neuroangio witholds demographic and clinical information details for privacy reasons.
noncontrast CT top, CTV bottom. Right sigmoid/transvese/straight/Galen thrombosis. Notice patchy look in the sigmoid
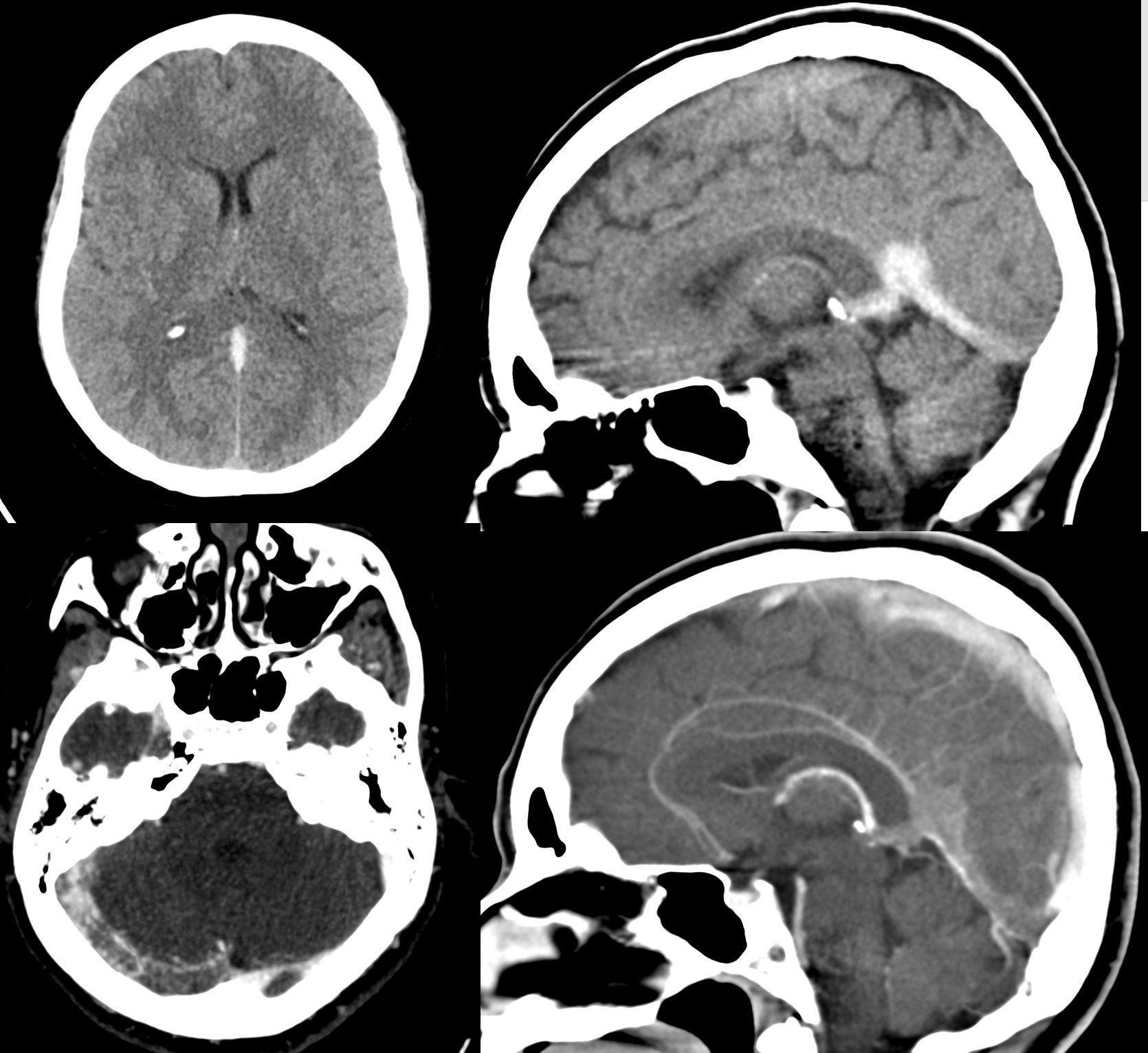
Nice example of dilated Internal Cerebral Venous tributaries on the left and very early hemorrhagic transformation in the left posterior limb
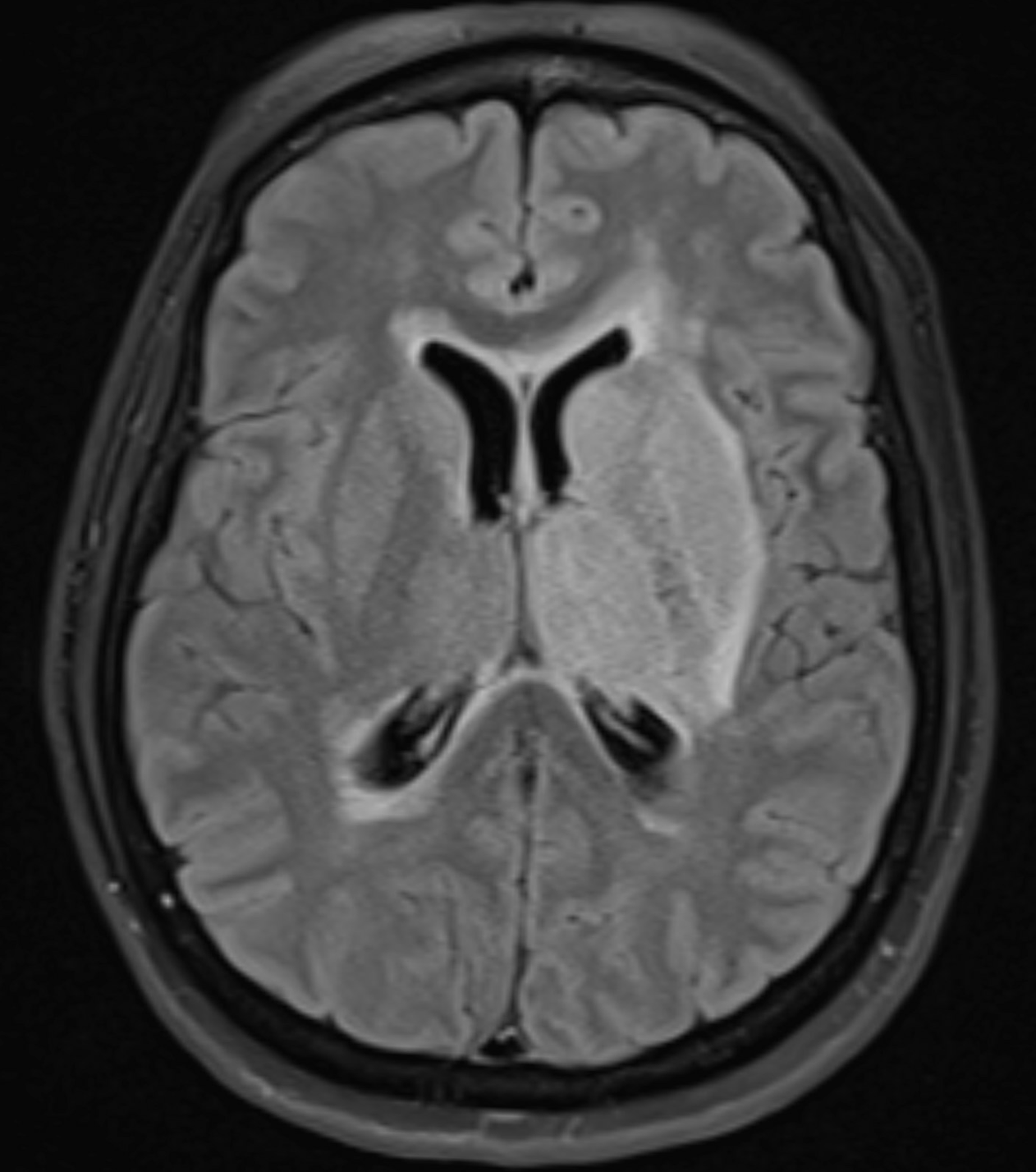
MRV — the sigmoid might be partially open?
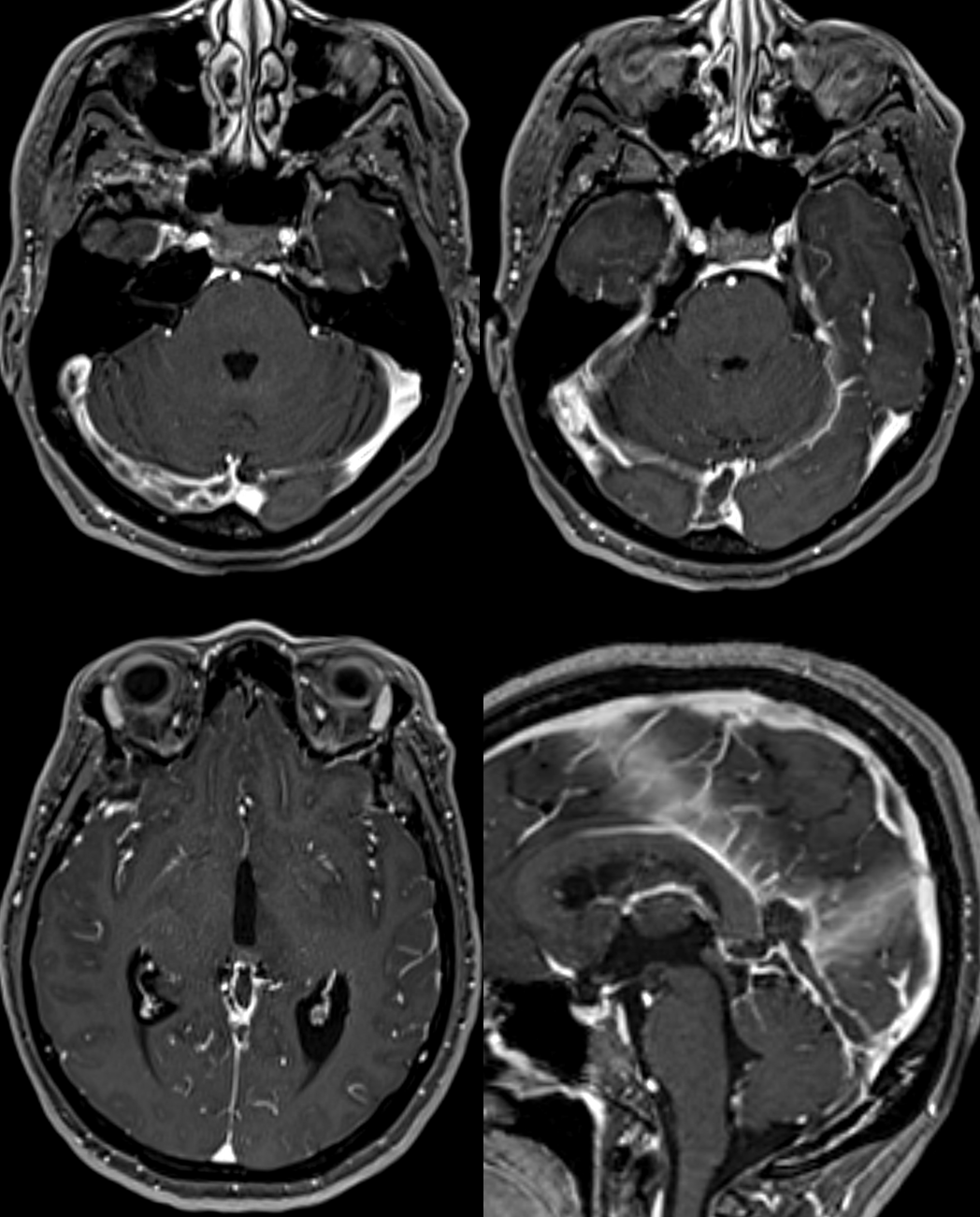
See the difference — right internal cerebral is visible — which means its better — and drains via small channels remaining in the straight sinus. The left internal cerebral is not seen at all — either thrombosed or very congested — worse in any case.
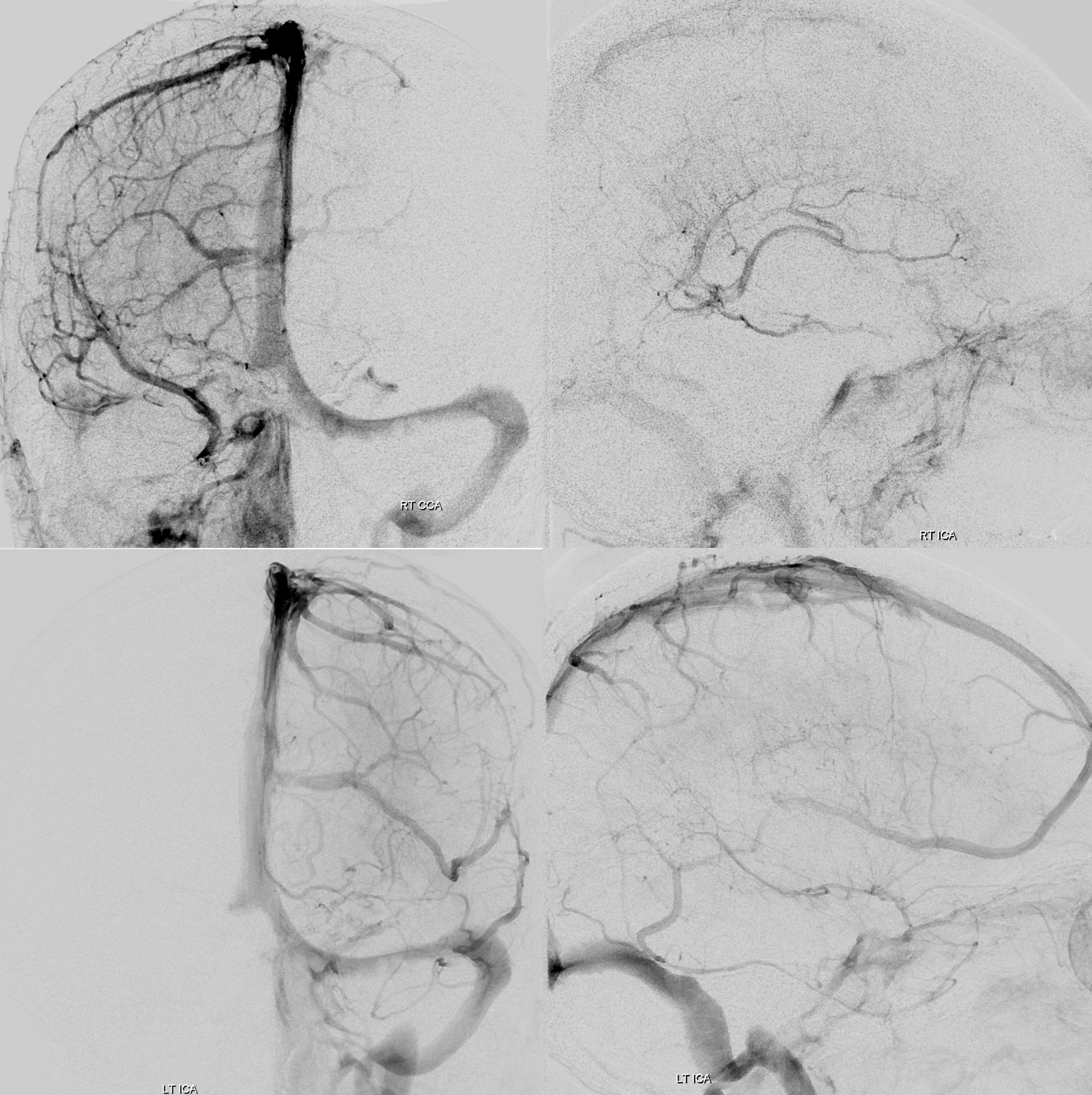
The right sigmoid is functional — via both the jugular and a mastoid emissary vein.
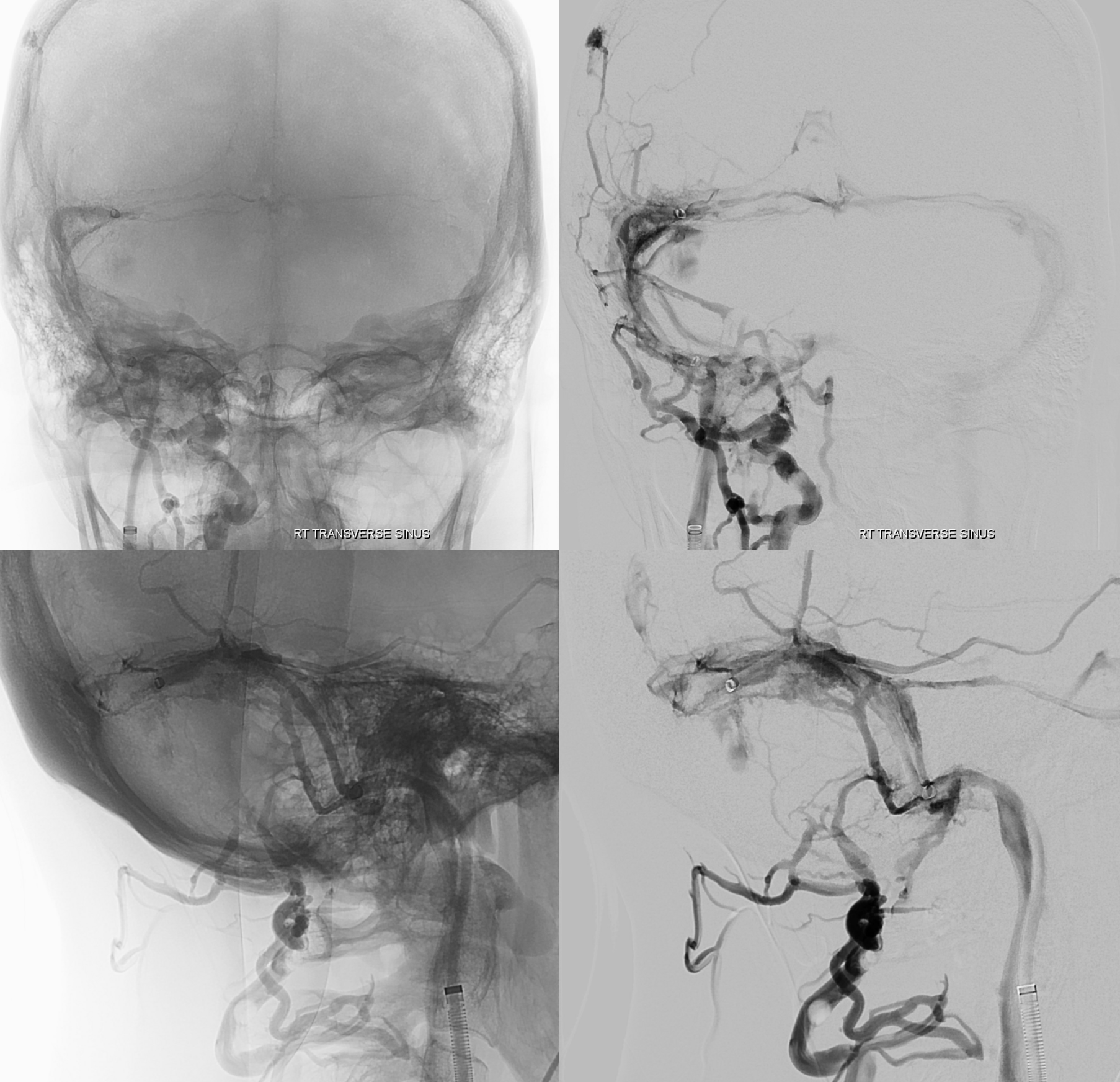
Zooms in the right sinus system — not much luck either aspirating anything or getting through to the torcular though
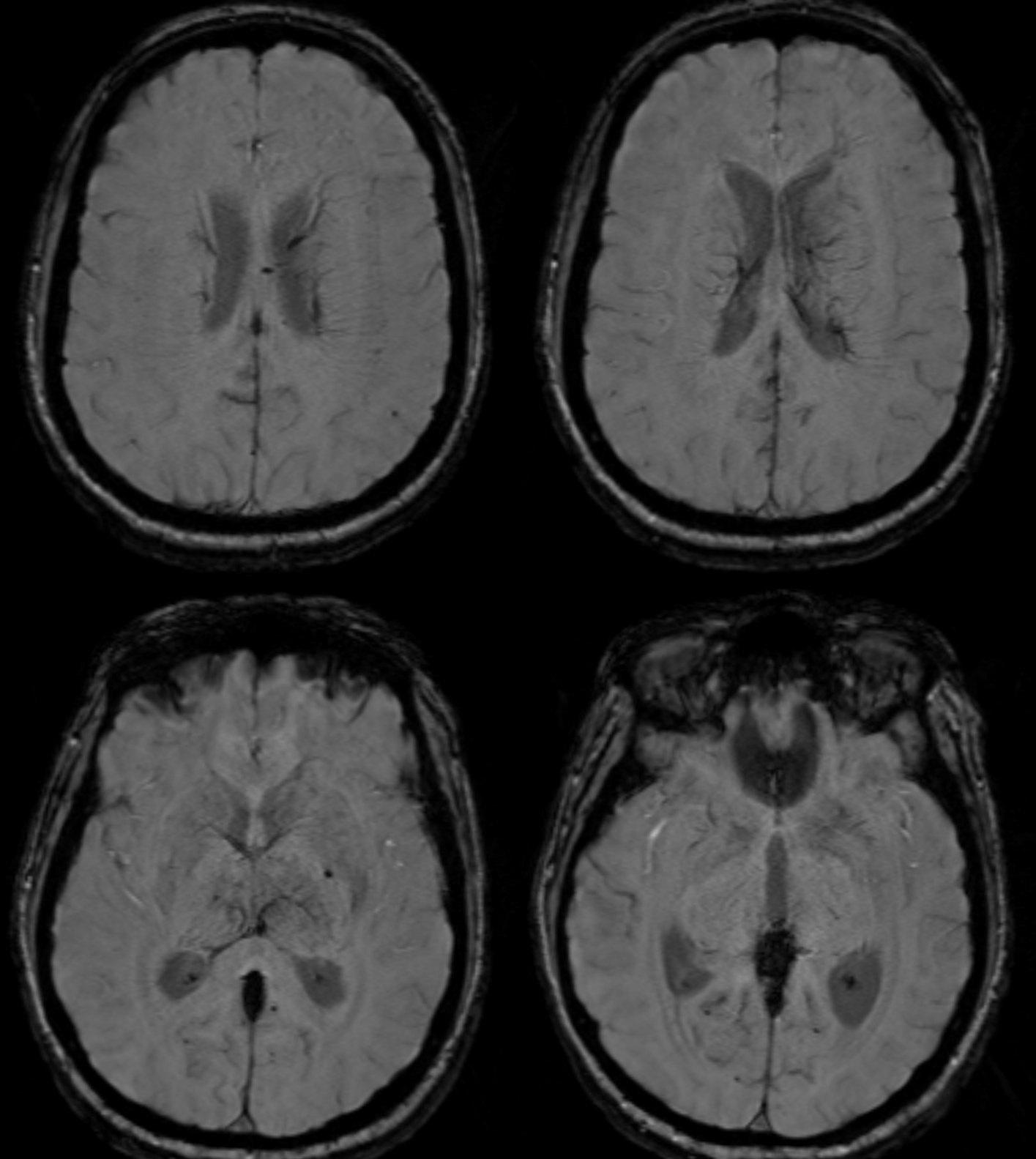
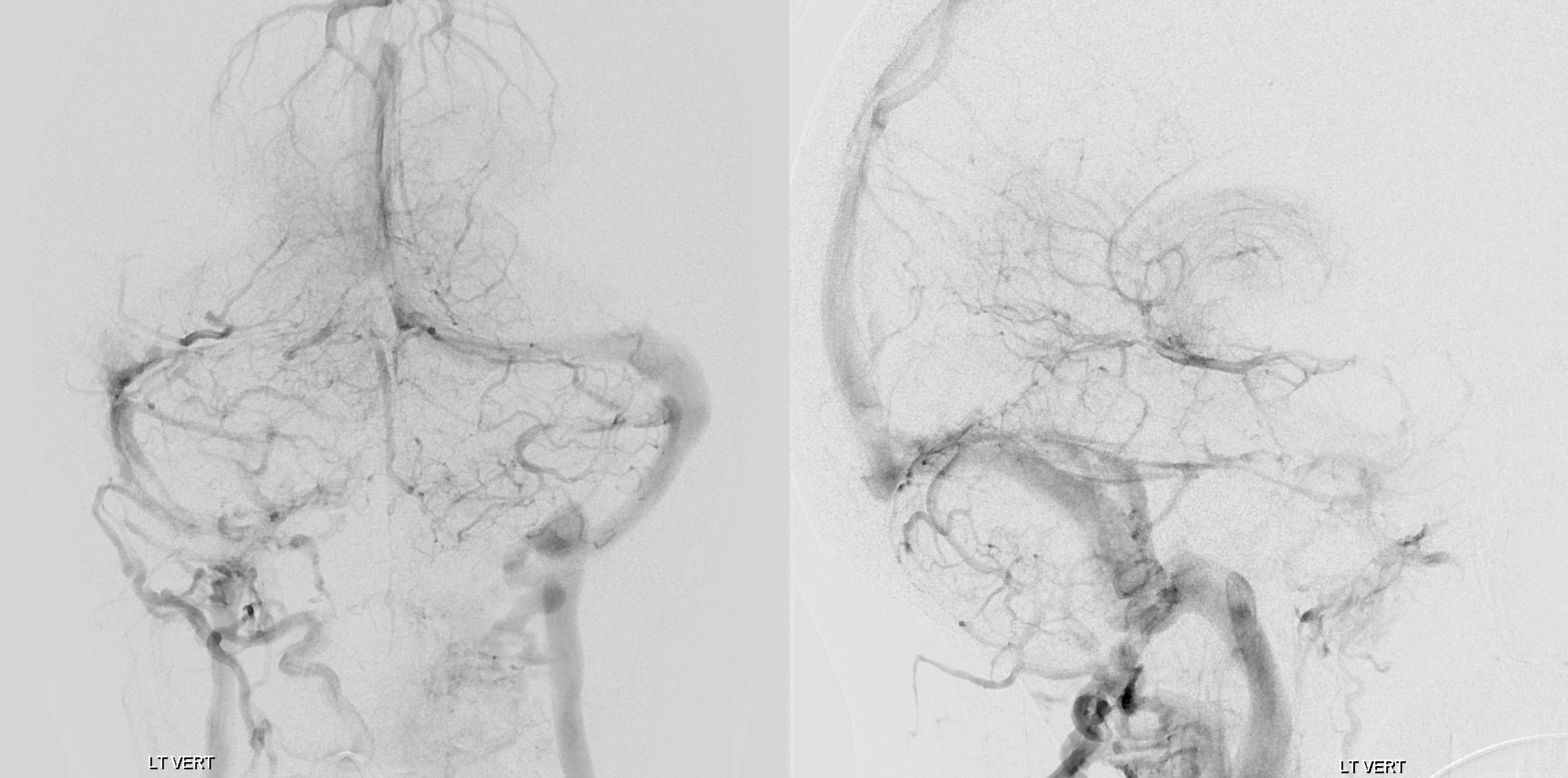
From the left — thankfully could get into proximal straight sinus with a 71. See all that clot? Some interesting things — the Rothenthal looking veins are not Rothenthal — they are dural veins in the tentorial margin.
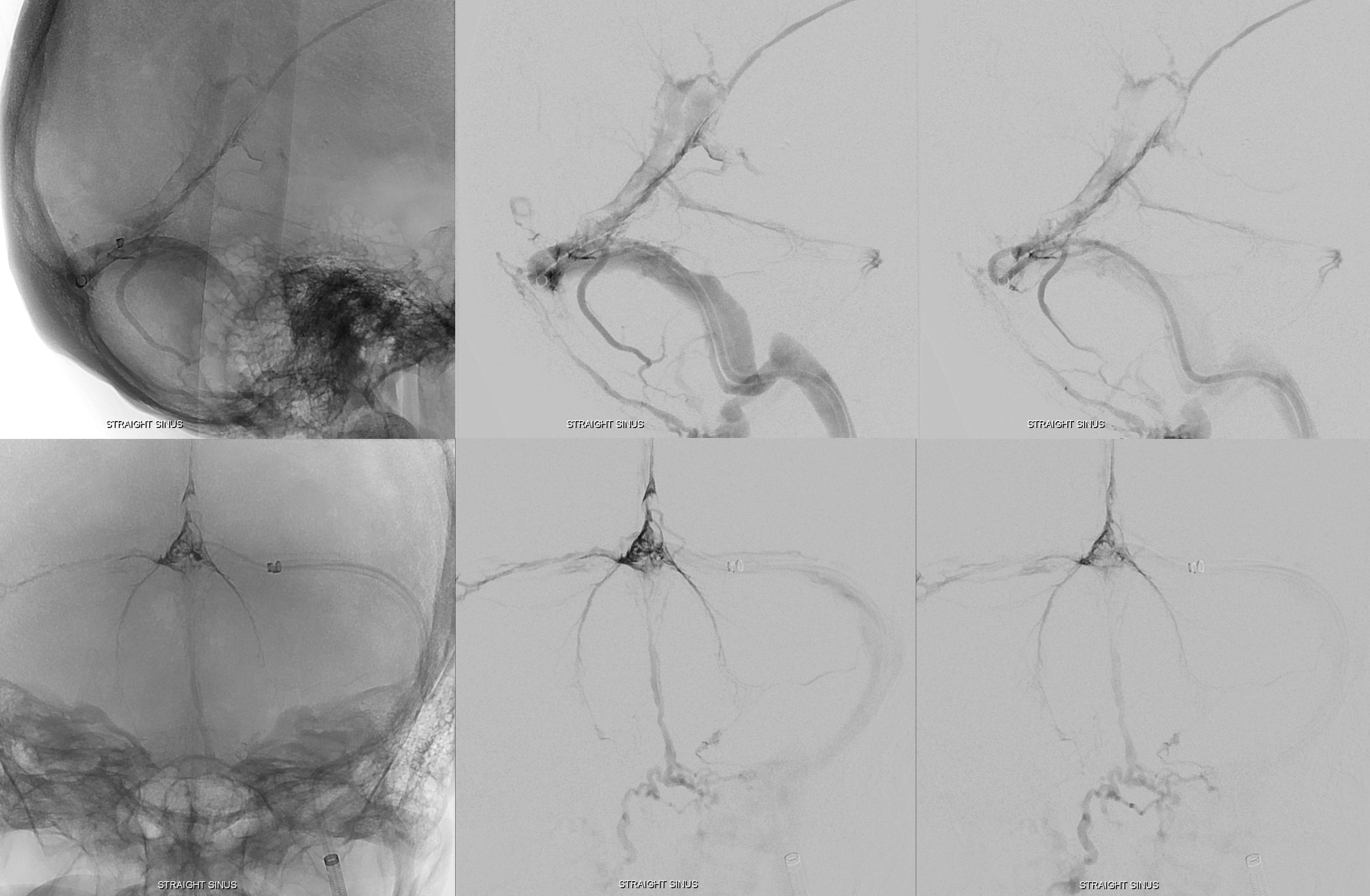
Were mananged to sneak a headway duo into the Galen thankfully

Not much outflow from here — mostly into the real Rothenthal.

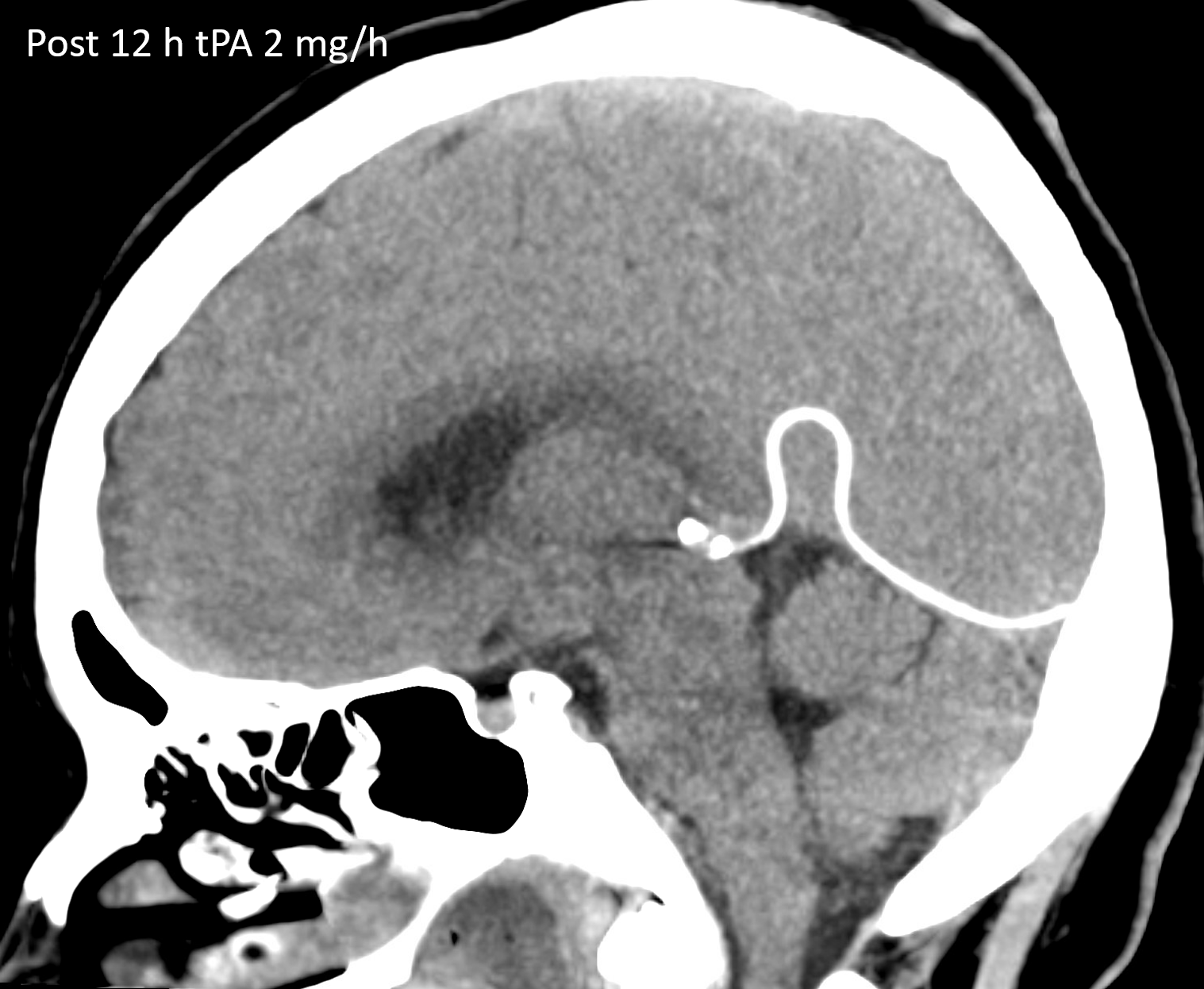
Protocol is 2 mg tPA / hr infusion (500 mg water/100 mg tPA, 10 ml/hr) with a 2 mg bolus. The venous sheaths and intermediate catheters are pulled into the cava and secured to the leg. It is essential that the infusion continue uninterrupted or the microcatheter might thrombose, though having all that tPA in there is protective. Oozing from puncture sites, including groin hematomas, may be encountered.
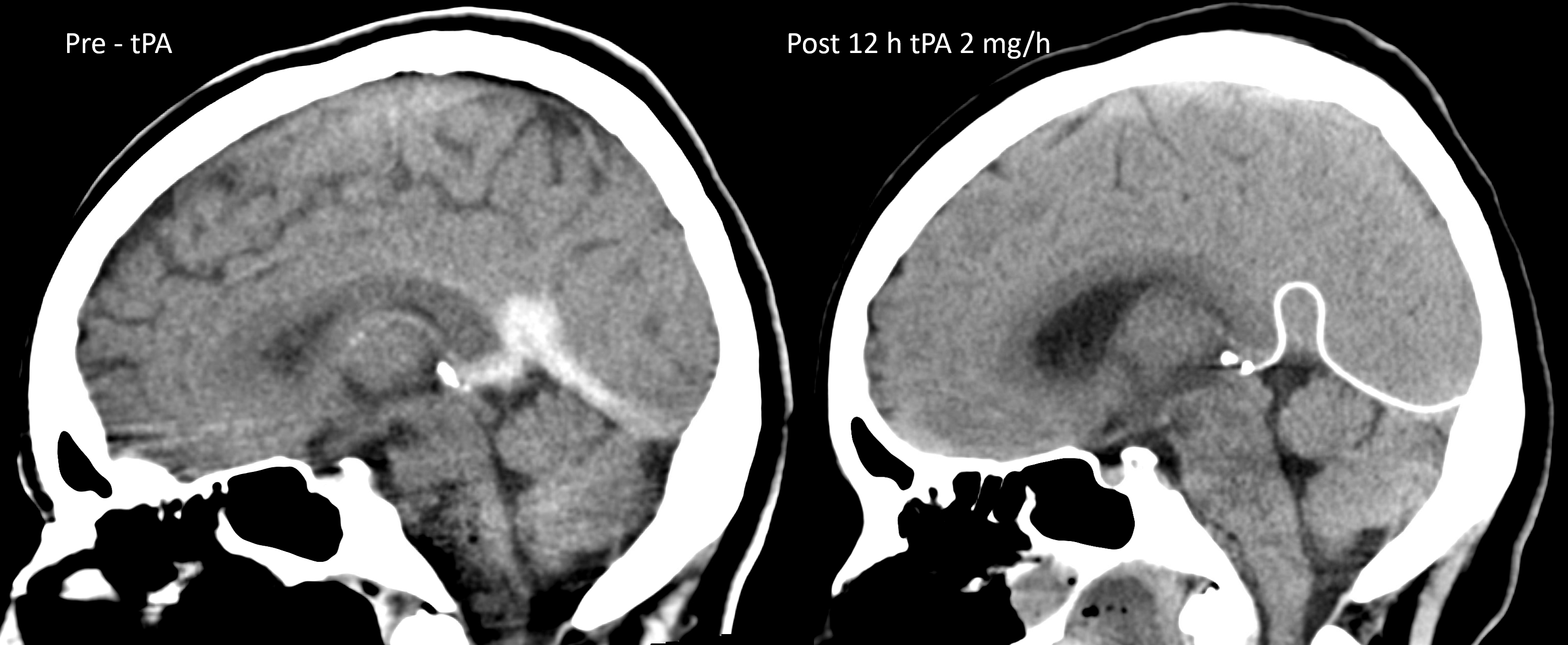
Since this is rarely done, there is no standard follow up. A CT in 12-24 hours is typical. In this case, a 12 hour post-infusion CT is below. MAGIC — all hyperdensity is gone!
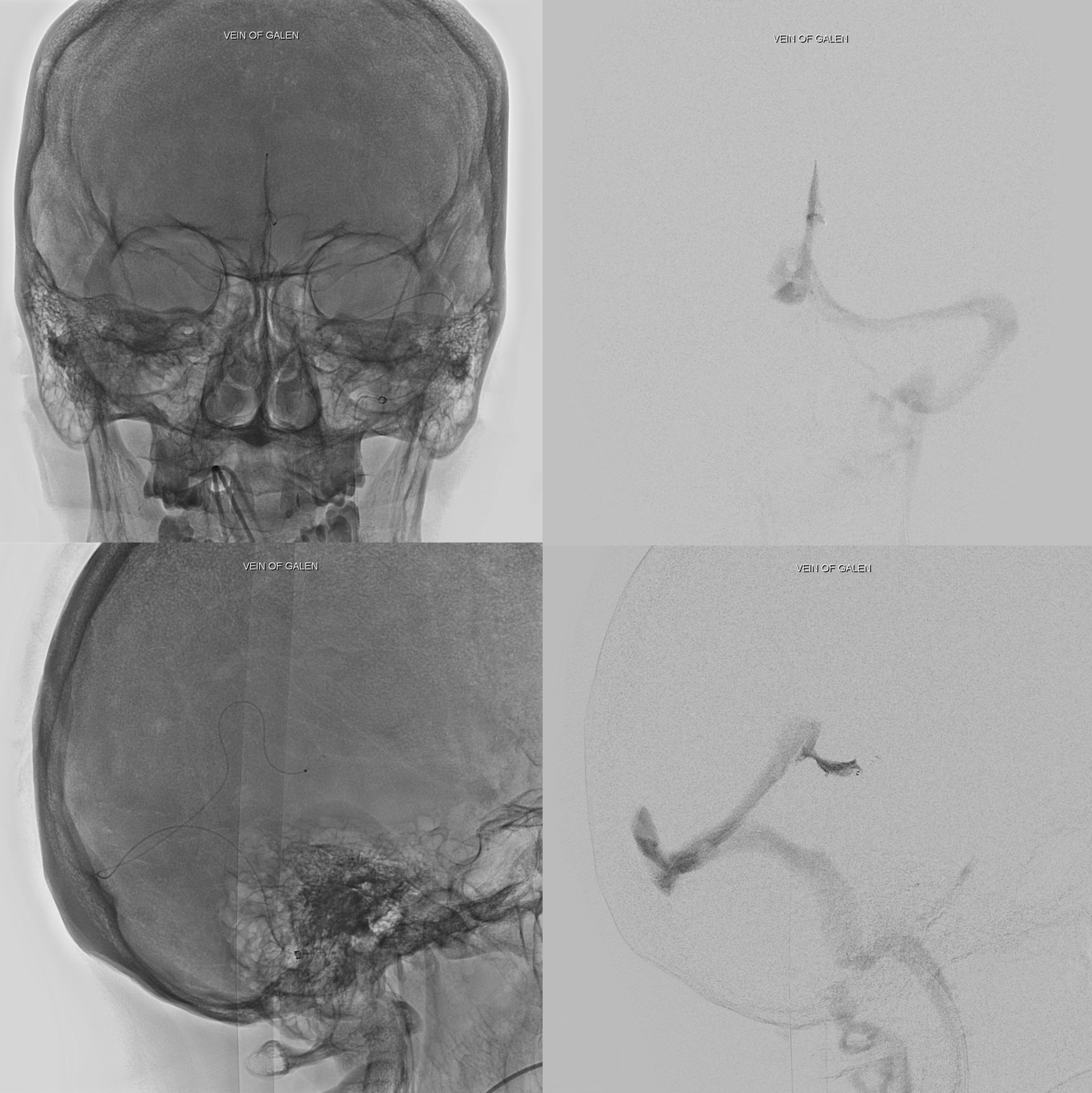
To check flow in the Galen, simply bring patient into angio suite and inject the microcatheter. All clot melted like last year’s snow.
The patient so well — extubated and discharged without a follow up CT… Not on our watch… but it is what it is. You will just have to take our word for it — it was super.
THE POINT IS THIS: This is a technically fairly simple, underused, and extremely powerful tool in management of venous thrombosis. Successful treatment of both cortical or deep venous and deep sinus thrombosis requires more than recanalization of the sinuses. Making a channel in the sinus without restoring deep or cortical flow into it will not help anyone. Mechanical thrombectomy without anticoagulation is likely to fail — the key is anticoagulation, clot lysis. Which means that direct tPA administration is what makes sense — and what worked here.
