Case Courtesy Dr. Keith DeSousa
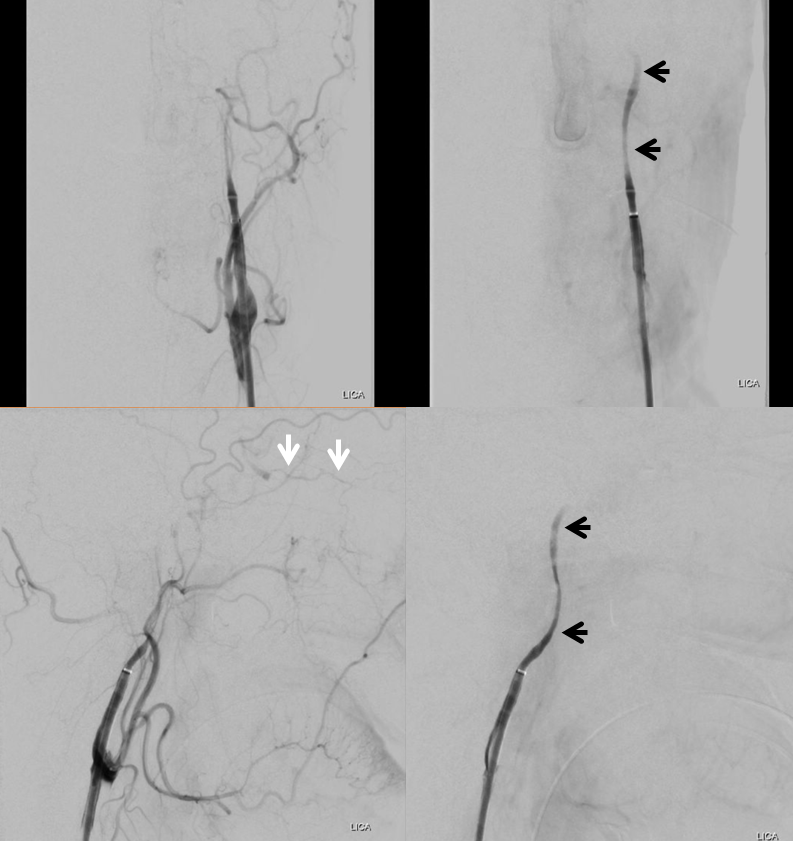
As of now, in 2019, most intracranial stents we place are in setting of acute stroke (not elective) and documented failure of prior maximal medical management. Here is one, with prior embolic-type frontoparietal convexity infarcts and left cavernous segment stenosis (arrows).
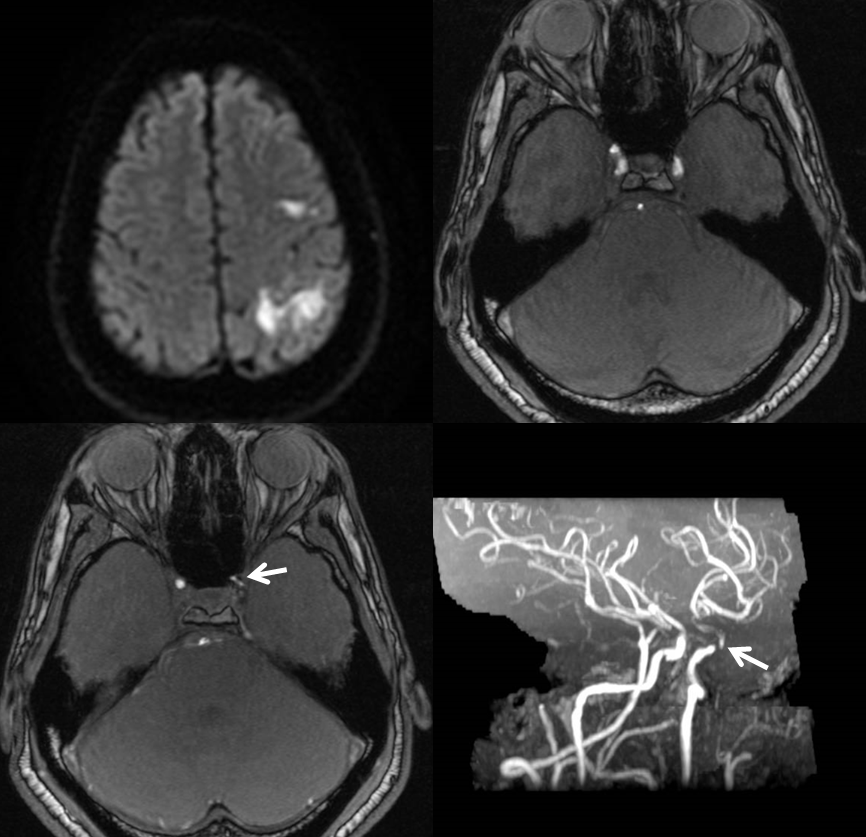
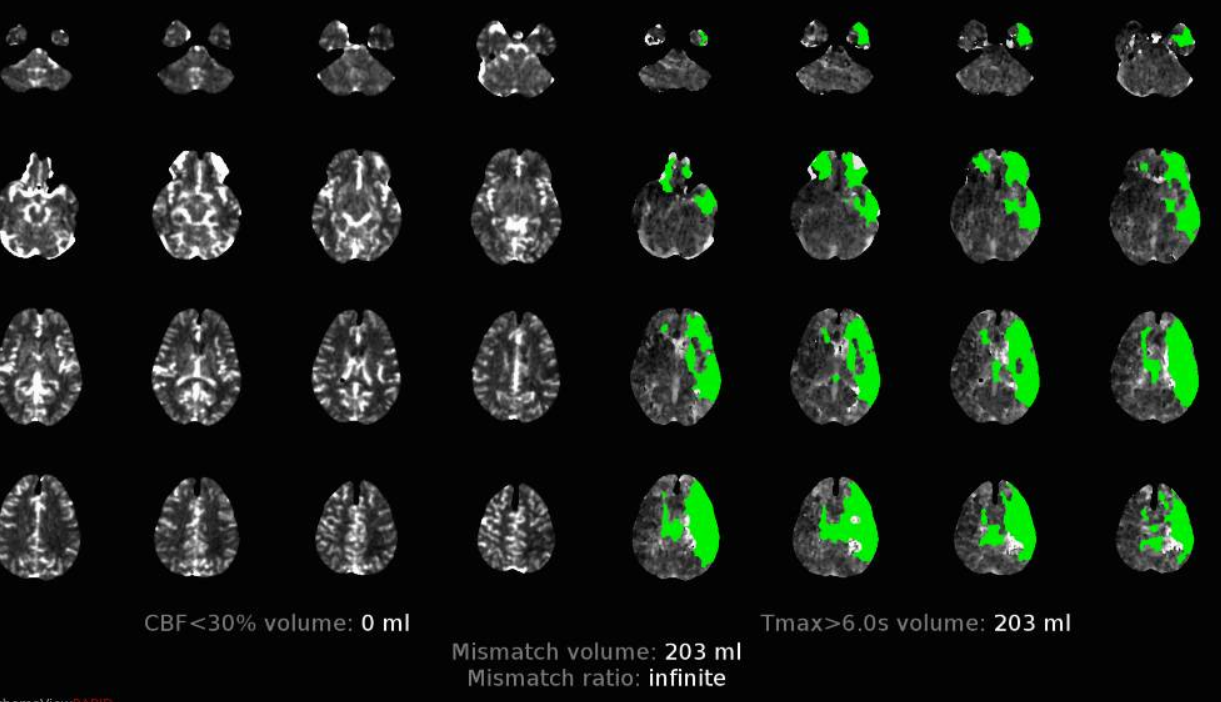
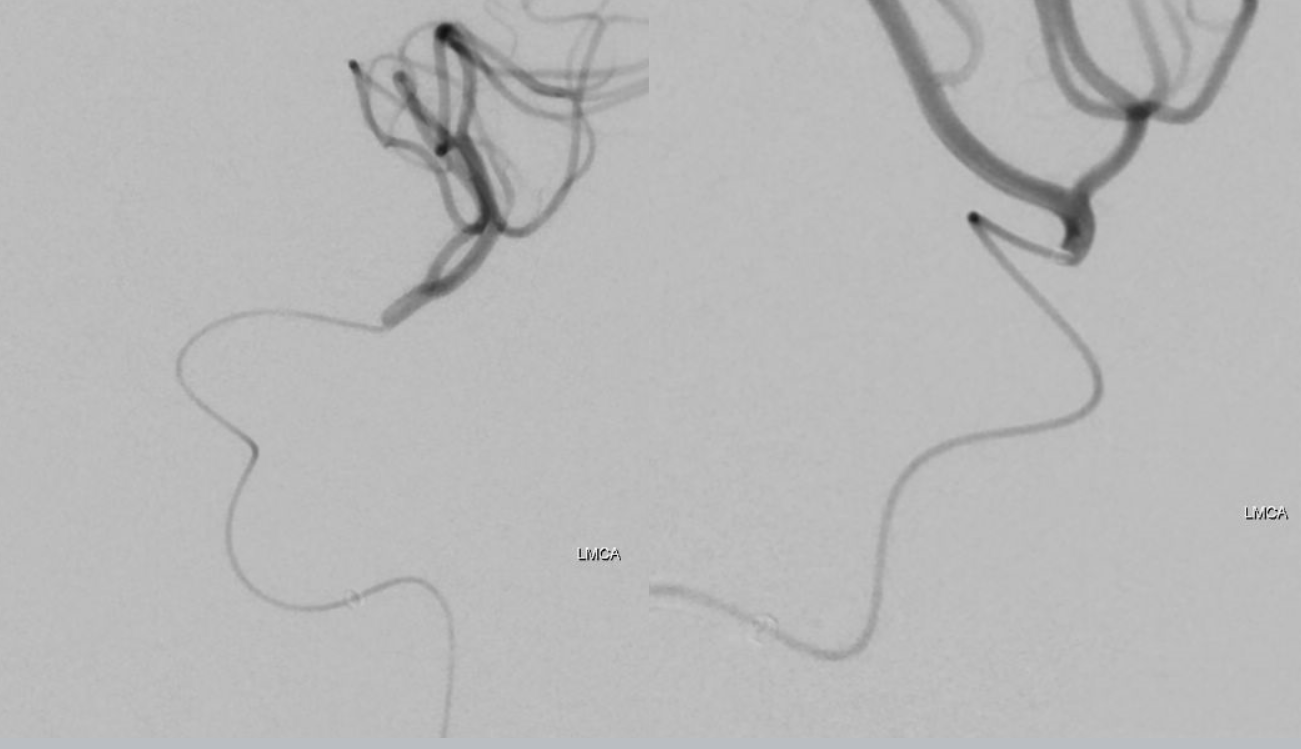
Three months later patient returns with left MCA syndrome. Notice involvement of right ACA territory, probably because of hypoplastic left A1 (see ACA page)
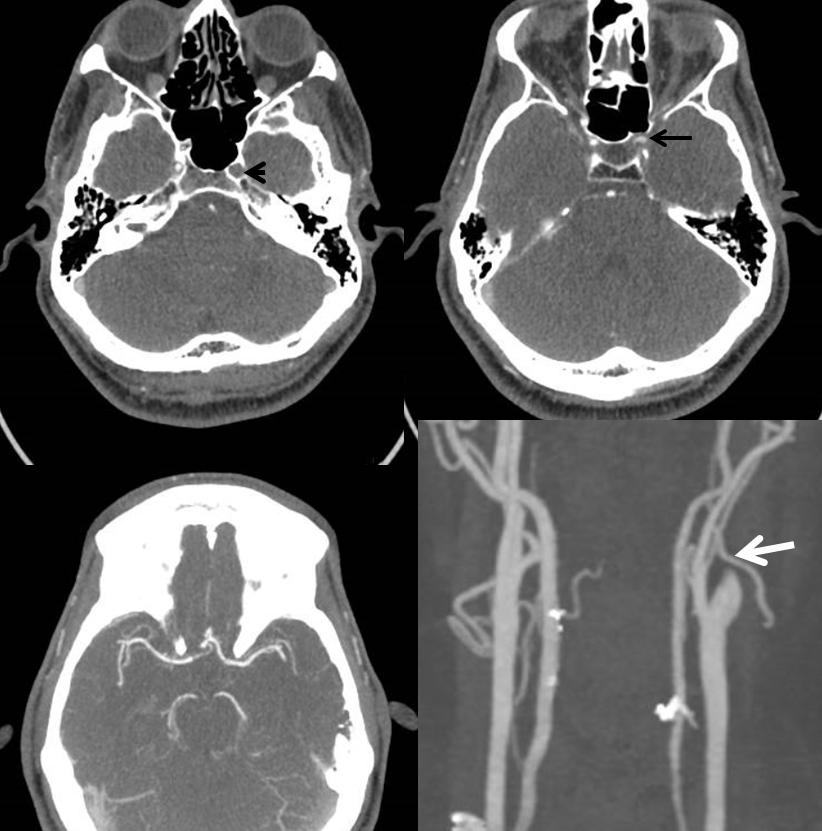
CTA shows no flow in the cavernous segment (black arrowhead), good flow distal to left ophthalmic (black arrow), patent M1, and “pseudo-occlusion” of left cervical ICA (white arrow)
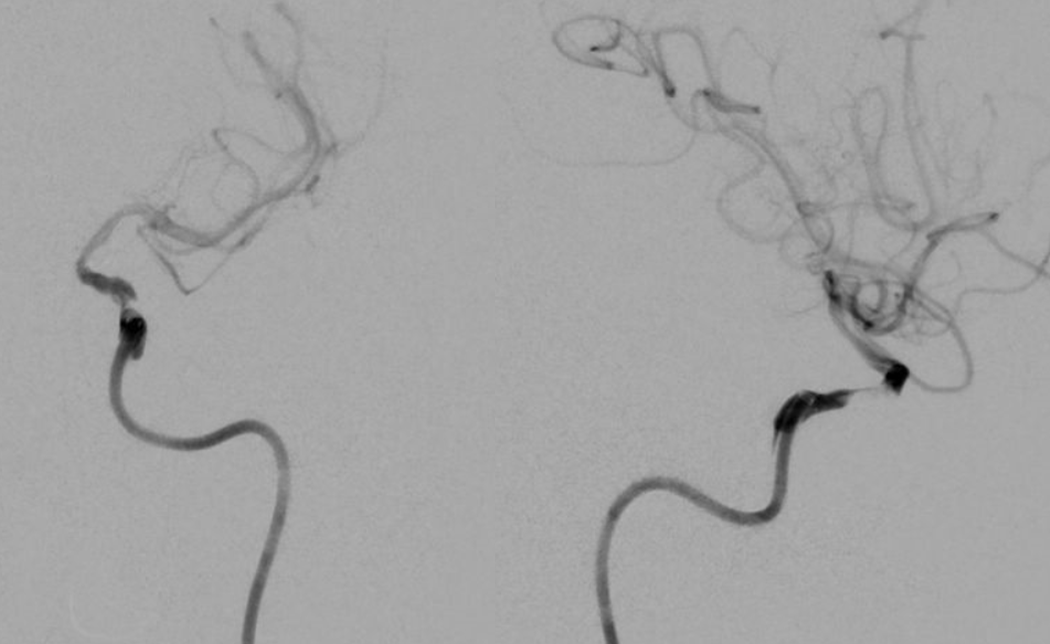
Important to angio collateral vessels in cases like these before rushing headlong into the left ICA. A few minutes make no difference with these kinds of collaterals, and the additional information is well worth it. Here is a nice demonstration of marginal collaterals, especially well seen by differences in the venous phase (lower right image). Also notice how the angiogram matches perfusion maps, with delay in right ACA territory because of dominant left A1.
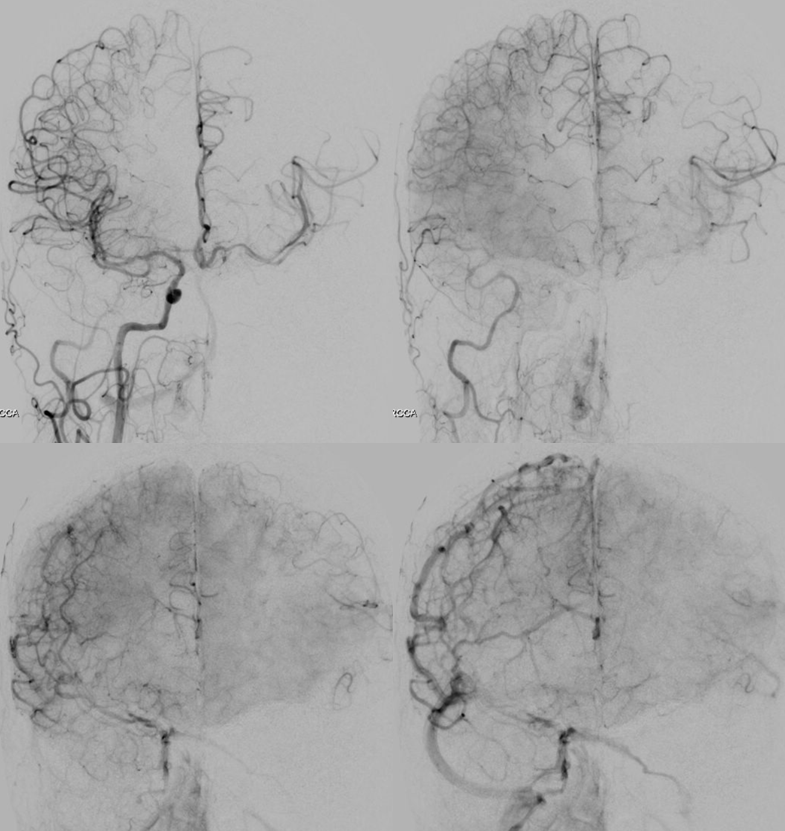
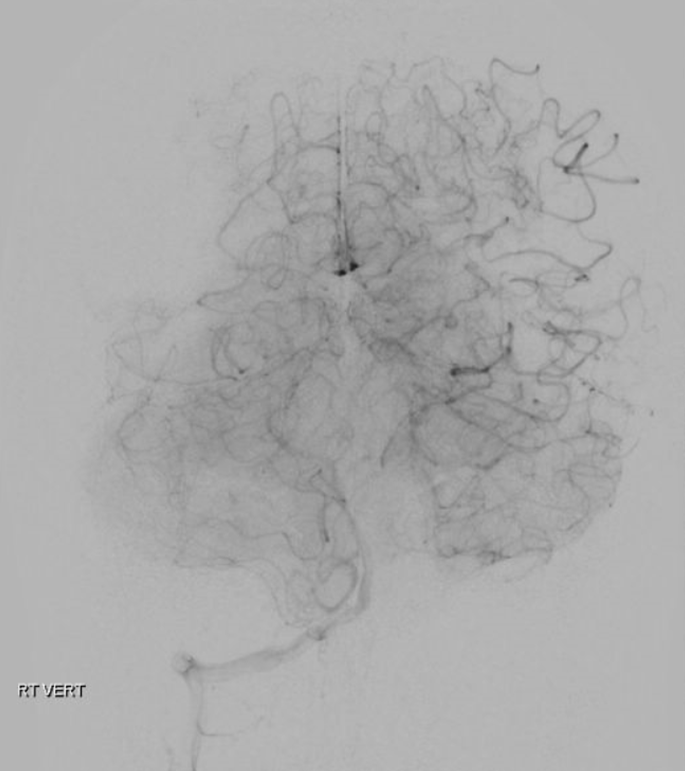
Vert leptomeningeal collaterals
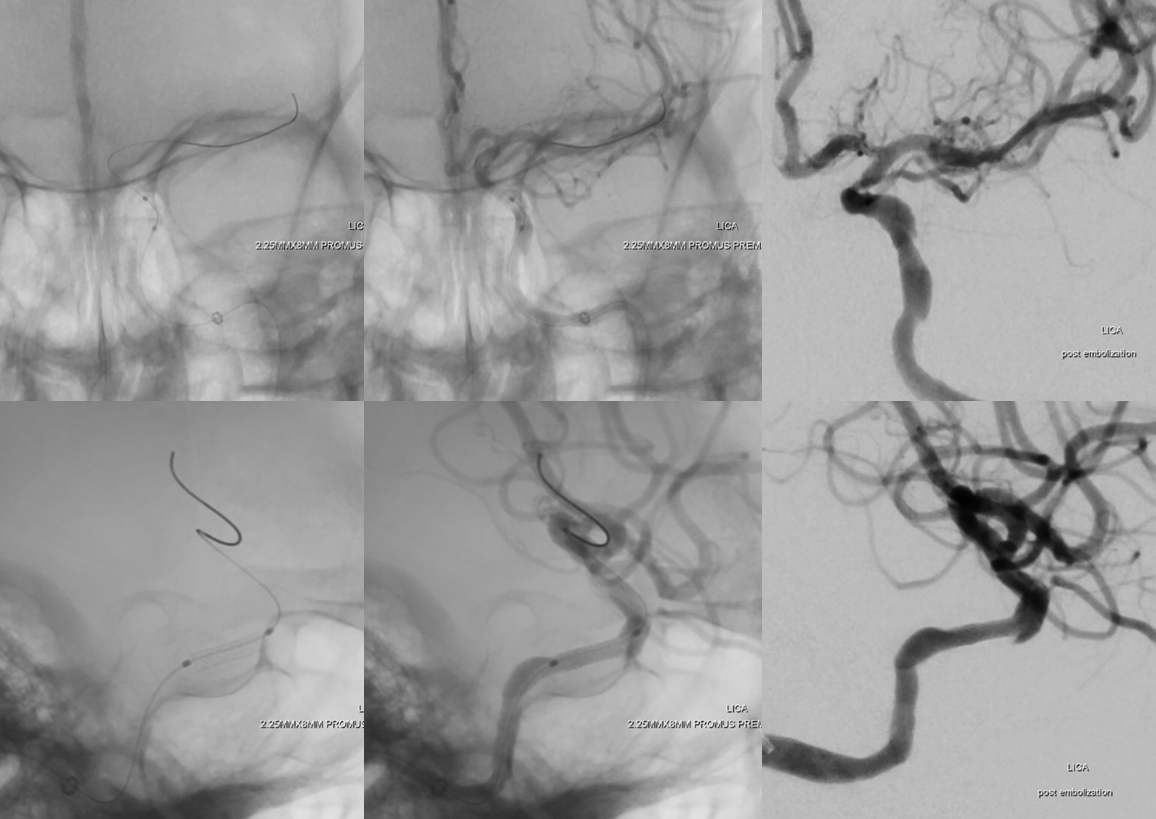
Setup is NeuronMax into proximal left ICA, then Sofia 6 115 cm (short one because stent delivery system is on short side, at 144 cm). Injections show the psudo-occlusion with delayed contrast progress into the upper cervical segment (black arrows). The actual occlusion is at the cavernous segment. Retrograde flow in ophthalmic (white arrows)
Sofia 6 is advanced into petrous and cavernous segments and about 3 mm long clot is aspirated. Then, traction is applied to Sofia under aspiration and the stenosis is traversed to aspirate whatever plaque/clot is there. Post-aspiration image below. Cavernous segment is perfect for stenting.
Magnified view prior to stenting.
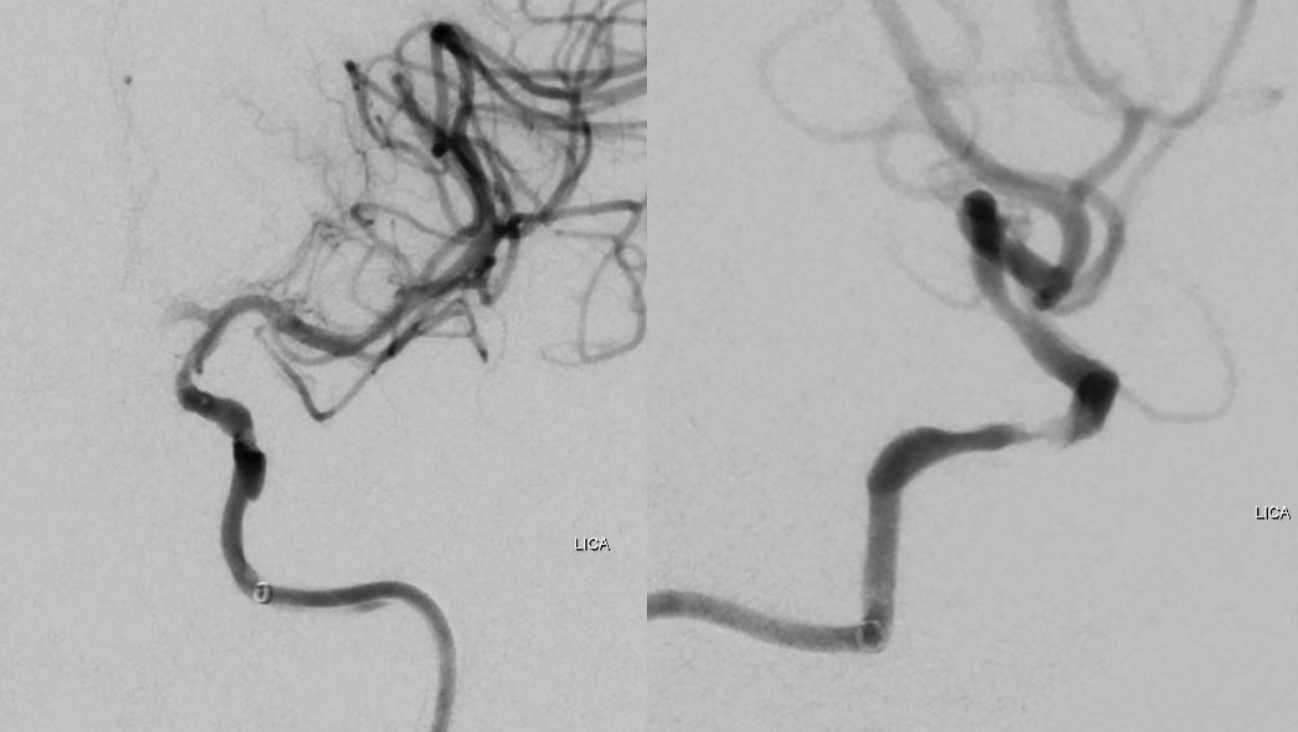
Distal access with Marksman. Why? To make sure we are in the right lumen in case there is a dissection at level of stenosis. We J-wire an 014 (Synchro) and pass the J thru the stenosis, followed by the Marksman. Then, we put in a 300 cm Transcend 014, remove Marksman, and deliver stent over Transcend. The simpler way is just to J-wire the transcend without Marksman. We prefer a 300 cm wire to maintain access.
We purposefully undersize these stents, even in cavernous segment. This is a 2.25×8 mm Promus, a balloon-mounted Everolimus-eluting coronary stent, used off-label. We very much prefer these Everolimus ones to Wingspan, Neuroform, or any other intracranial stent in this kind of setting. Short ones like this 8 mm are pretty flexible as these kinds of stents go and deployment is straightforward. Someday, flow diverters will be this easy also. Post deployment images below. We pulled back Sofia after advancing stent. To advance stent, Sofia is brought up right against the stenosis. Makes it much easier.
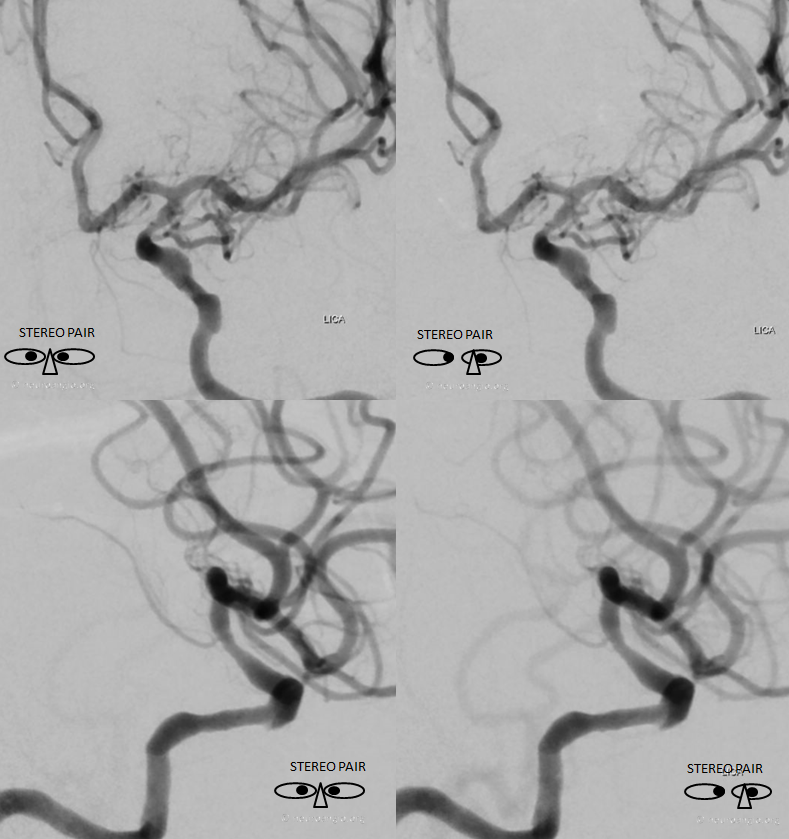
Stereos!
Anaglyphs
Global post. Tandem stenosis in the supraclinoid region is left alone. Ophthalmic is now antegrade. Hopefully that supraclinoid stenosis will behave.

