Case Courtesy
Mahmoud Elhorany, MD and Frédéric Clarençon, MD, PhD
Department of Neuroradiology. Pitié-Salpêtrière Hospital. Paris. FRANCE
Abbreviations
JF; Jugular foramen, APhA; Ascending pharyngeal artery, OcA; Occipital artery; VA; Vertebral artery, IJV; Internal jugular vein; ACV; Anterior condylar vein, HC; Hypoglossal canal, AIVVP; Anterior internal vertebral venous plexus, ACC; Anterior condylar confluence, SJB; Superior jugular bulb, IPS; Inferior petrosal sinus, IPOV; Inferior petro-occipital vein, LCV; Lateral condylar vein, VAVP; Vertebral artery venous plexus; PCV; Posterior condylar vein, Coc; Condylar canal, SCS; Sub-occipital cavernous sinus.
Case Presentation
The point here is that the condylar region (the part of the skull base and occipital area that lies lateral to the foramen magnum, runs laterally up to the jugular foramen (JF) and includes both the inside and the outside of the occipital bone) is an important area that looks like a cross road, containing critical nerves and vasculature. Additionally, it is the point of directing the encephalic venous drainage from intracranial to extracranial through multiple complex venous channels.
The arterial supply of this region is fed mainly by branches from the:
- Ascending pharyngeal artery (APhA)
- Occipital artery (OA)
- Vertebral artery (VA)
The cranio-cervical junction or condylar region is drained mainly by two venous systems depending on the position:
- Vertebral venous system in the upright position.
- Internal jugular vein (IJV) in the supine position.
The intracranial-extracranial venous connections through the condylar veins (anterior, posterior and lateral) are the following:
- The anterior condylar vein (ACV) lies in the Hypoglossal canal (HC) in association with CN XII and neuromeningeal trunk of ascending pharyngeal artery
It connects the anterior internal vertebral venous plexus (AIVVP), basilar plexus and the marginal sinus intracranially with the anterior condylar con?uence (ACC) extracranially.
The ACC is a venous pouch located at the extracranial opening of the HC. It represents a venous crossroad connecting with superior jugular bulb (SJB), inferior petrosal sinus (IPS), inferior petro-occipital vein (IPOV), in addition to ACV.
- The lateral condylar vein (LCV) connecting the vertebral artery venous plexus (VAVP) intracranially with the ACC extracranially.
- The posterior condylar vein (PCV) lies in the condylar canal (CoC) in association with neuro-meningeal branches of the OcA.
It connects the SJB intra-cranially with the sub-occipital cavernous sinus (SCS) extra-cranially.
- However, the PCV has four variants according to the intracranial connection: jugular bulb type (67%), sigmoid sinus type (25%), occipital sinus type (6%) and anterior condylar vein type (3%). PCV drains into SCS extra-cranially.
To the best of our knowledge, only 4 cases of arteriovenous fistula (AVFs) involving the PCV have been reported so far. Two cases presented with pulsatile tinnitus, and two with subarachnoid hemorrhage. [1-4]
In contrast to rarity of PCV fistulas, AVFs of the ACV are more common than those of PCV, with ~ 120 cases of the former documented in the literature, with a wider spectrum of symptoms including pulsatile tinnitus, intracranial hemorrhage, myelopathy, orbital symptoms and cranial nerve palsies. [5]
Management of condylar type fistulas is highly challenging: arterial approach is associated with potential for cranial nerve palsy and/or migration of the embolic material into the vertebrobasilar system via dangerous anastomoses (mainly the so-called “odontoid arch”).
Therefore, the transvenous approach is often preferred to the arterial one, to avoid the previously mentioned risks. Coils, Onyx or glue can be used. However, coil embolization may be preferred to avoid potentially uncontrolled migration of liquid embolic agent through dangerous anastomoses, reducing risk of spinal cord arterial supply compromise, and cranial nerve palsy. Coils could be combined with Onyx or glue, especially in high-flow fistulas, to reduce flow and prevent inopportune migration of the liquid embolic. Coils should not be densely packed to avoid postoperative cranial nerve palsy, especially for AVF located in the hypoglossal canal.
Herein is an illustrative case of posterior condylar DAVF. This patient presented with pulsatile tinnitus on right side and had right parietal headaches.
Diagnostic DSA revealed DAVF:
The fistula was supplied by meningeal branches from the neuromeningeal trunk of the ascending pharyngeal artery, by trans-osseous branches of the occipital artery and by the anterior meningeal branch of the vertebral artery on the right side. The AVF was drained by the PCV, which was probably partially thrombosed with no connection with the SCS and presented a reflux in the ACV, then ACC and finally in the jugular bulb (Fig. 1 and Fig. 2). Thus, the PCV presented a rare anatomical variation; it was not connected directly to the SJB, but to the ACV.
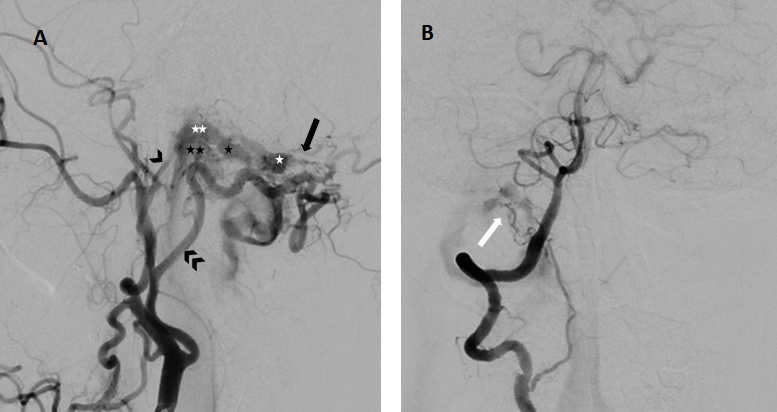
Figure 1 — right external carotid artery DSA; lateral (left) and frontal (right) projections.
Arterial feeders to the shunt point are seen: osseous branches (black arrow) of the occipital artery (double black arrowhead) and meningeal branches from the neuro-meningeal trunk the of ascending pharyngeal artery (black arrowhead). The shunt point involves the posterior condylar vein (white asterisk), which drains secondarily in the anterior condylar vein (black asterisk), then in the anterior condylar confluence (double white asterisk) and finally in the jugular bulb (double black asterisk). The fistulous point is also supplied by the anterior meningeal artery from the distal V2 segment of the right vertebral artery (white arrow).
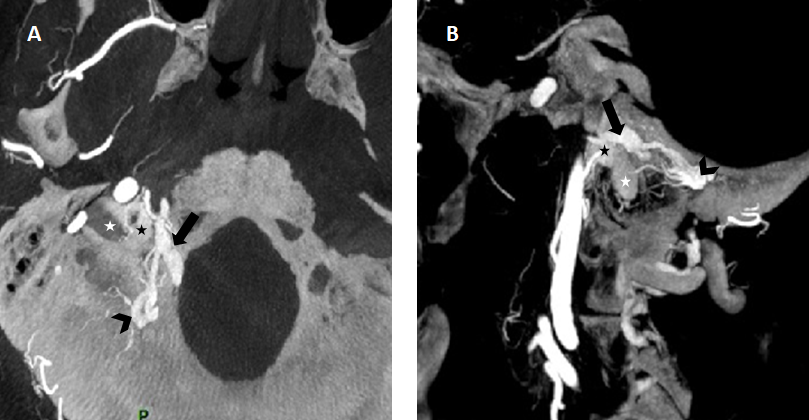
Figure 2 — reconstructions from the 3D rotational angiography injected through right external artery (A: axial and B: sagittal reconstructions) showing the venous drainage pathway of the fistula with a shunt point located along the wall of the posterior condylar vein (black arrowhead), with reflux in the anterior condylar vein (black arrow), then in the anterior condylar confluence (black asterisk) and finally in the jugular bulb (white asterisk).
Embolization
We chose embolization of the fistula by coils through transvenous approach (Fig. 3). Tri-axial system was navigated through the right IJV. Thereafter, the microcatheter was navigated through the ACC, then the ACV until the nearest point of the shunt, in the PCV. Multiple coils were then deployed until complete occlusion of the PCV to effect cure of the AVF, without technical issue or complication. The patient experienced quick resolution of her symptoms (tinnitus and headache). DSA 8 months later showed no fistula recurrence.
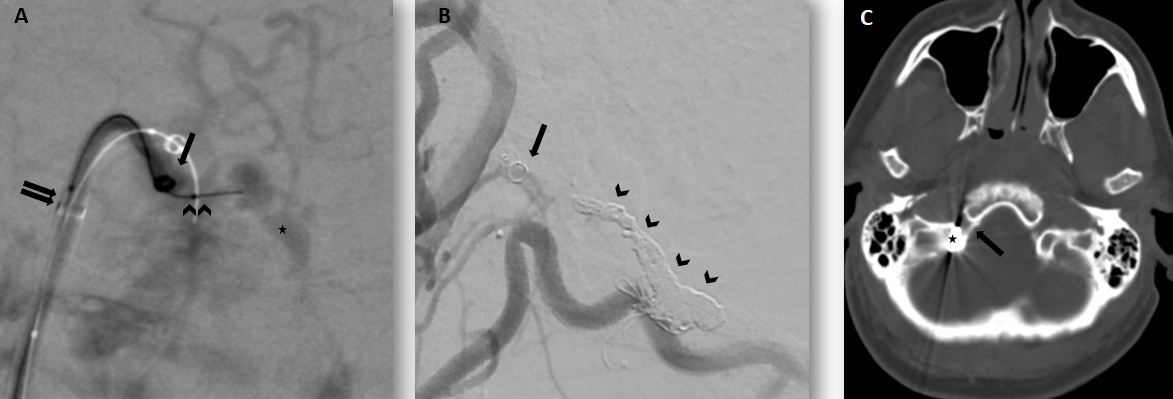
Figure 3:
3A. Road map injected through the right external carotid artery; postero-anterior projection
Transvenous approach by direct puncture of the right internal jugular vein using a tri-axial system; Neuromax 6F long sheath (double black arrows), Sofia 6F (single black arrow) and a Headway Duo microcatheter navigated over a Traxcess 0.014’’ micro guidewire (double arrowhead) navigated toward the posterior condylar vein, location of the shunt point (black asterisk).
3B. Post-embolization right external carotid artery DSA; lateral projection showing the coil mass (black arrowheads) and the complete occlusion of the AV fistula. Note the residual opacification of the anterior condylar vein (black arrow).
3C. Post-embolization unenhanced CT scan showing the coil mass within the condylar canal, which contains the posterior condylar vein (black asterisk) and which is located posteriorly and laterally to the hypoglossal canal, containing the anterior condylar vein (black arrow).
References
- Kiyosue H, Okahara M, Sagara Y, Tanoue S, Ueda S, Mimata C et al. Dural arteriovenous fistula involving the posterior condylar canal. AJNR American journal of neuroradiology. 2007;28(8):1599-601. doi:10.3174/ajnr.A0606.
- Mondel PK, Saraf R, Limaye US. Acute subarachnoid hemorrhage in posterior condylar canal dural arteriovenous fistula: imaging features with endovascular management. Journal of neurointerventional surgery. 2015;7(7):e26. doi:10.1136/neurintsurg-2014-011273.rep.
- Maus V, Soderman M, Rodesch G, Kabbasch C, Mpotsaris A. Endovascular treatment of posterior condylar canal dural arteriovenous fistula. BMJ case reports. 2016;2016. doi:10.1136/bcr-2016-012384.
- Shambanduram SS, Devarajan Sebastian LJ, Jain N, Garg A, Gaikwad SB. Management of a rare case of posterior condylar canal dural arteriovenous fistula presenting with subarachnoid haemorrhage: A case report and review of literature. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences. 2018;24(2):206-9. doi:10.1177/1591019917743703.
- Takemoto K, Tateshima S, Rastogi S, Gonzalez N, Jahan R, Duckwiler G et al. Onyx embolization of anterior condylar confluence dural arteriovenous fistula. Journal of neurointerventional surgery. 2014;6(2):e13. doi:10.1136/neurintsurg-2013-010651.rep.
