With Roberto Flores MD
Scalp AVMs are high flow arteriovenous shunts. Typical supply is from STA and occipital arteries. Drainage into superficial veins. The diagnosis of AVM is not pathologic — it is based on morphology and angiography. This and other facial / soft tissue AVMs are not exactly similar to brain AVMs. Head/neck ones are acquired. Brain AVMs usually are not, or so we believe. Scalp AVMs are a mix. Some seem stable while most grow. Some grow very aggressively, with very bad outcomes. Where do they fall on the tumor spectrum? We don’t yet know. Genetic advances are always a promise . Because of all these uncertainties, our feeling is that they are best dealt with by aggressive surgical resection, taking out what looks like nidus and some tissue around (similar to margins). A preoperative embolization is often needed.
Presentation here is pulsatile scalp bump.
Some months later — predictably worse
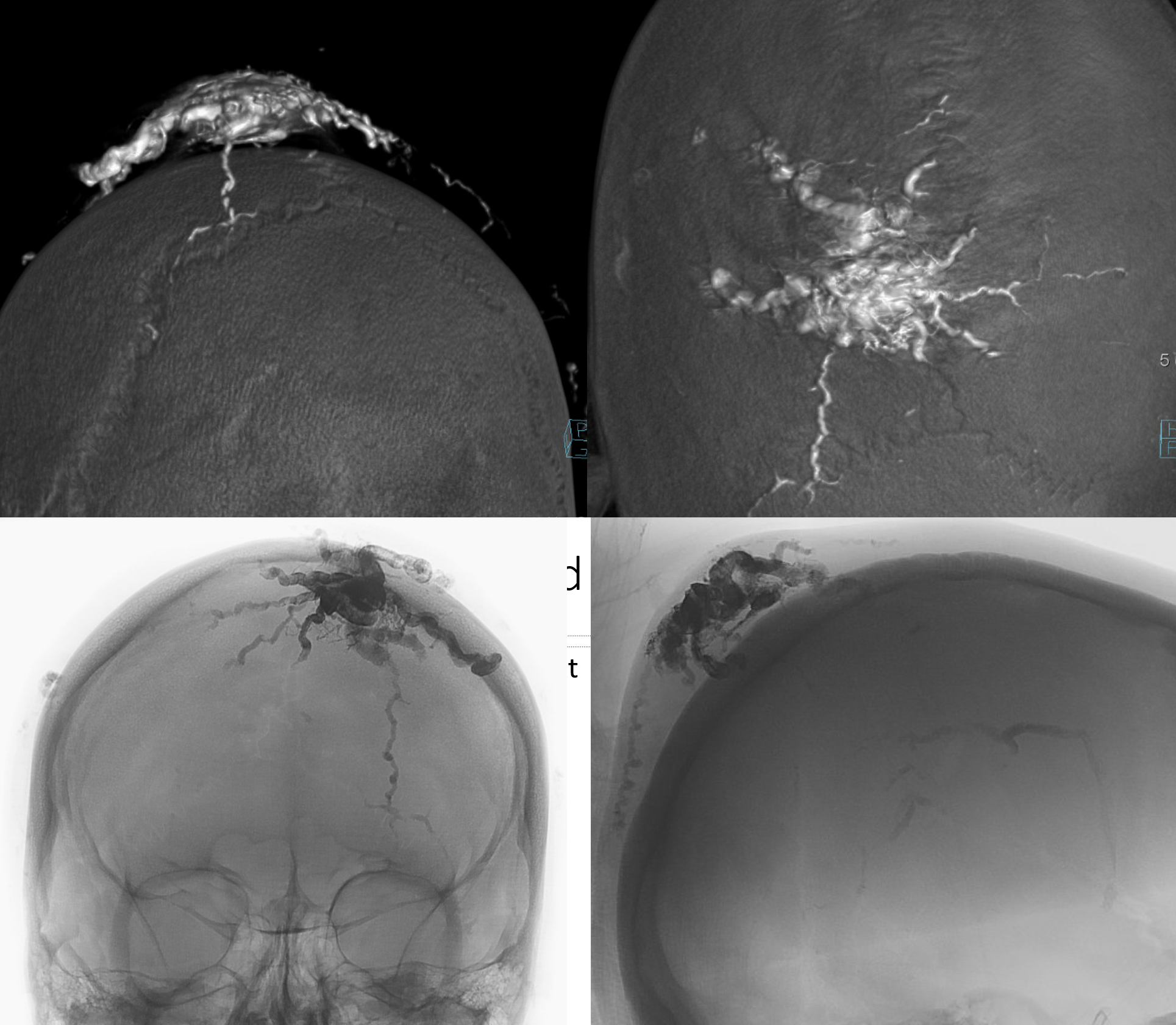
Angio — no supply from ICA. It is important to make sure however that meningeal vessels are not contributing — if yes its typically as part of occasional meningeal supply of scalp via transosseous foramina — see MMA page for more. The typical supply is here — occipital and STA. Drainage into scalp (superficial temporal) veins, then ECV, then jugular.
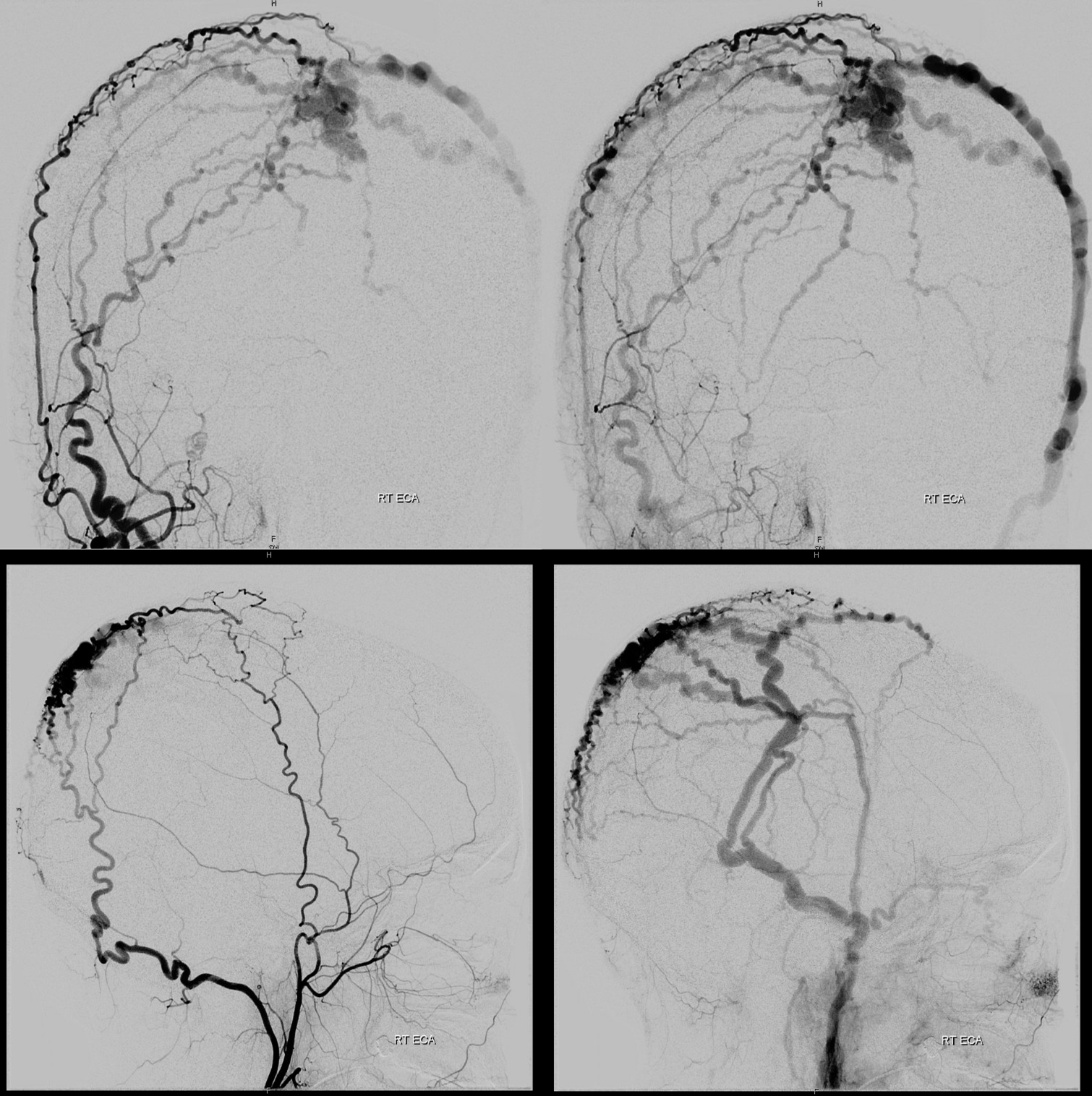
Left is worse
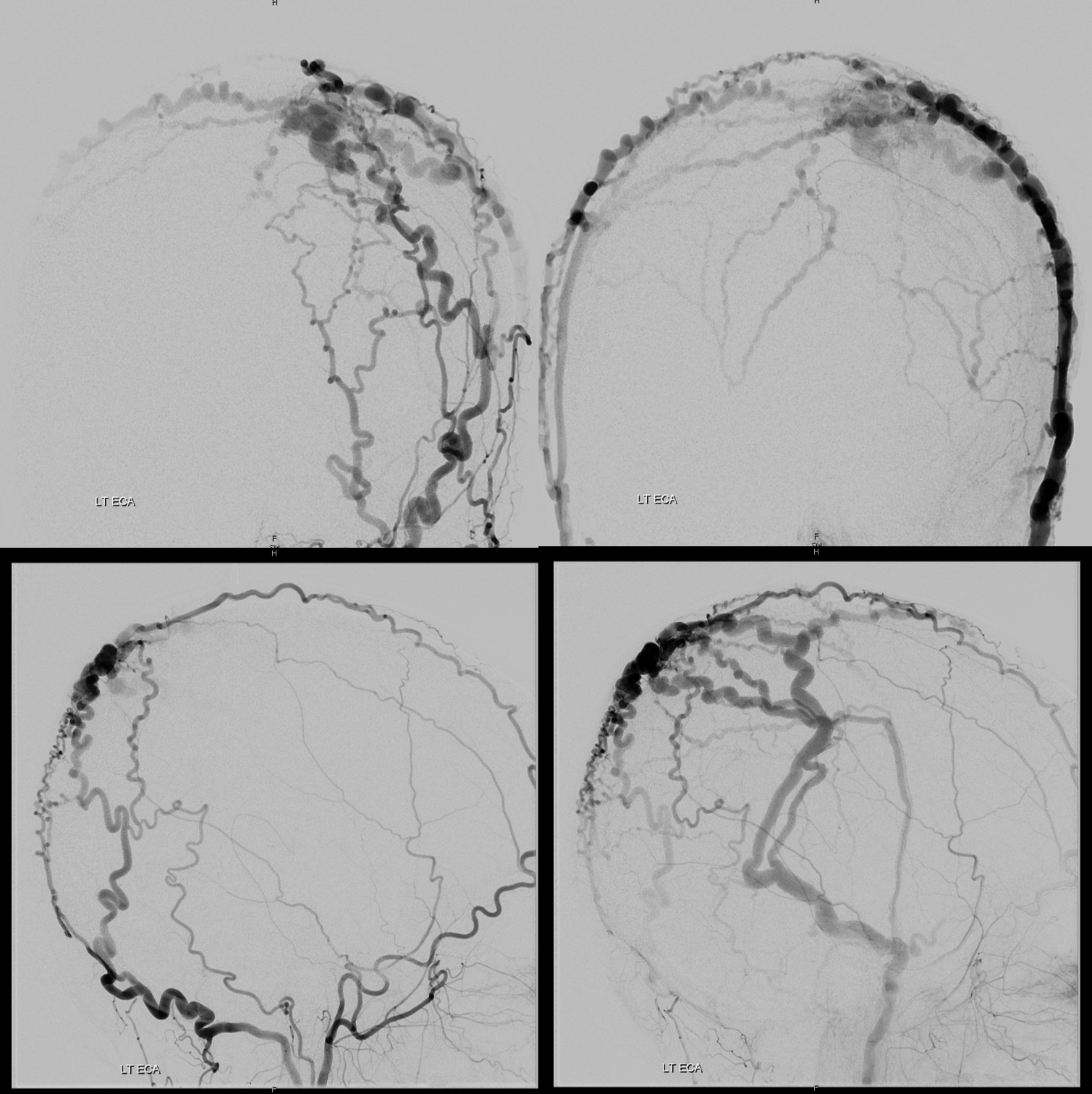
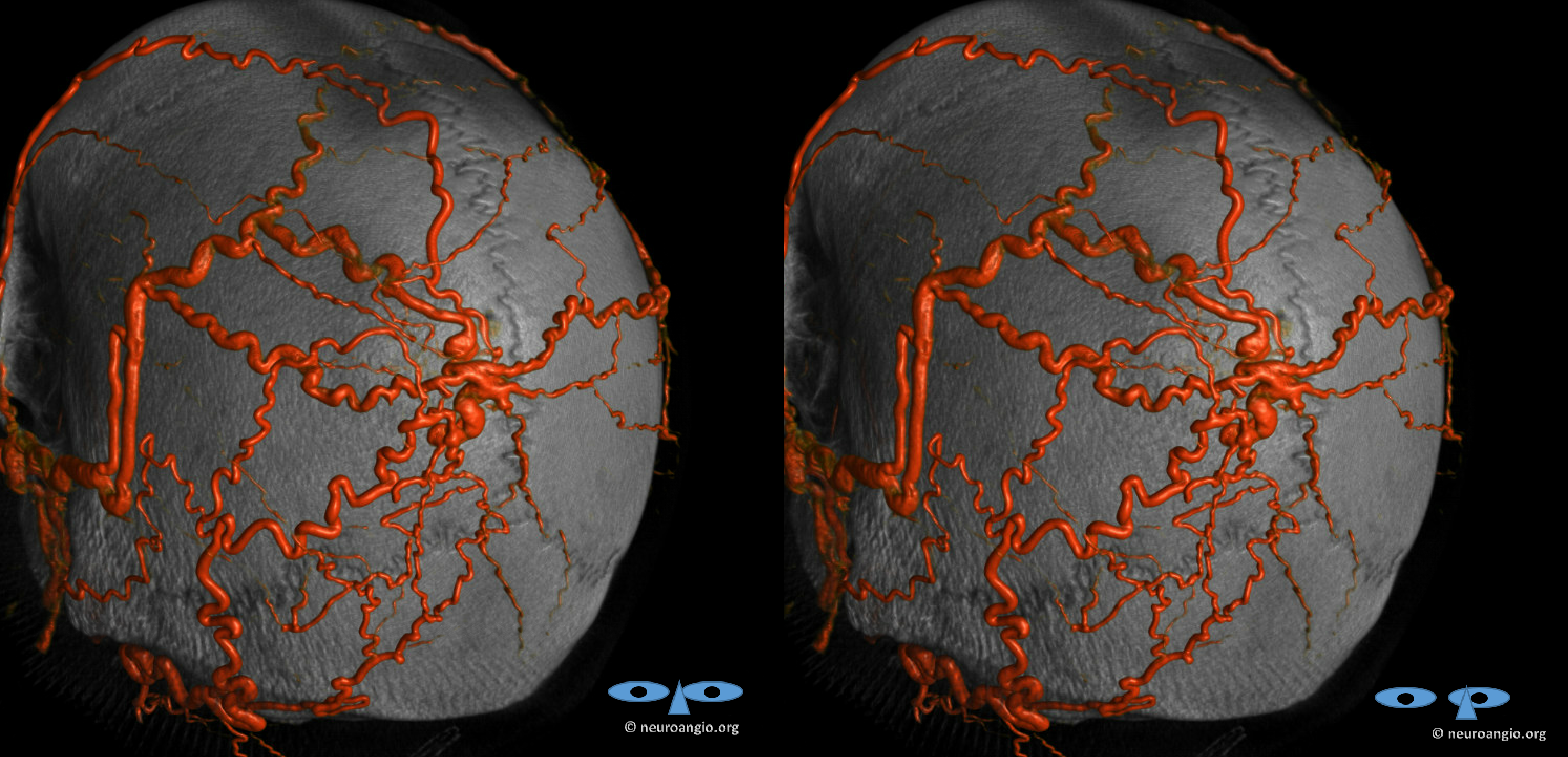
Stereos
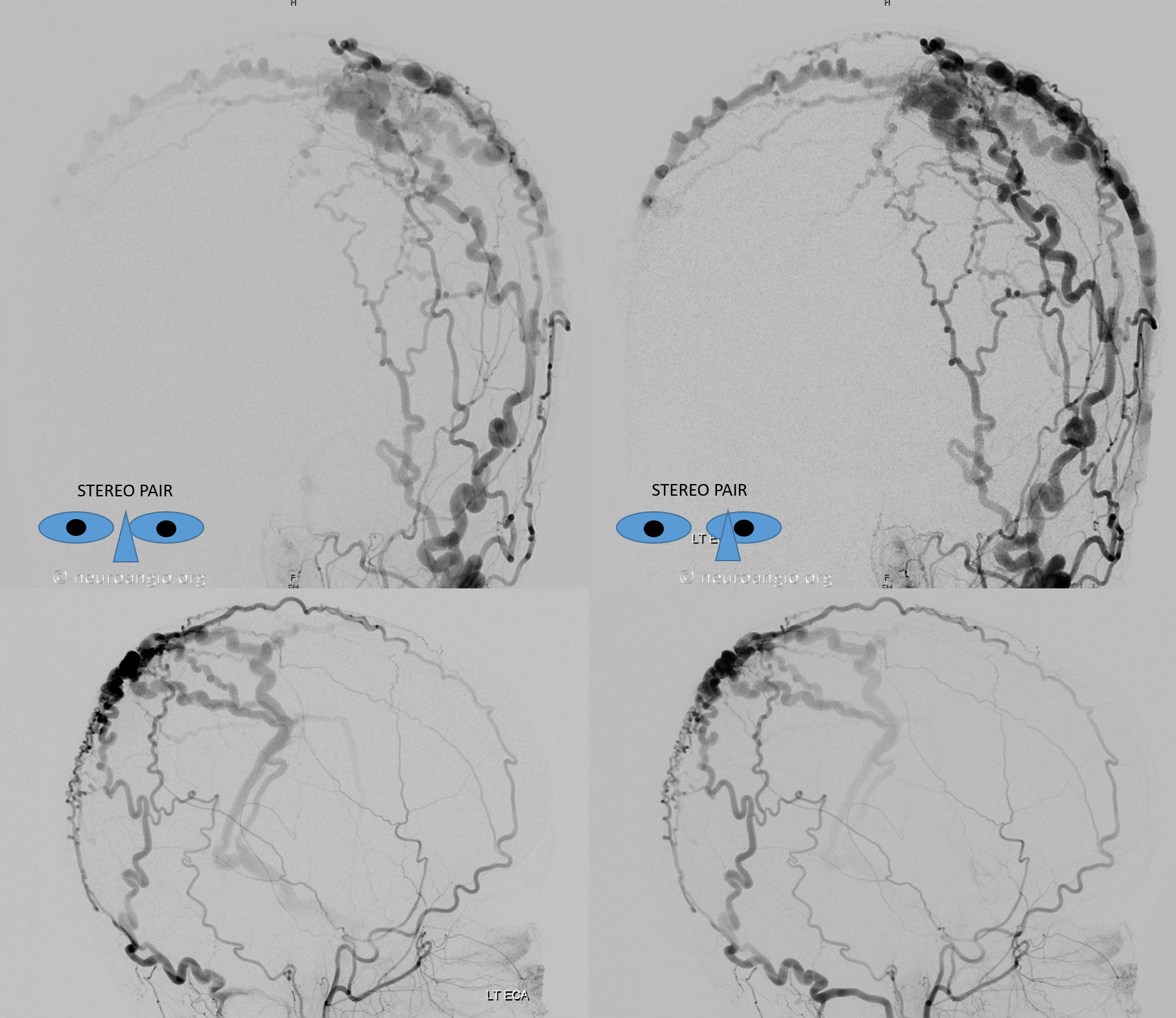
Anaglyph stereo
3D-DSA / Volume rendered / DYNA — important to get that if you can. Looks pretty insane huh…
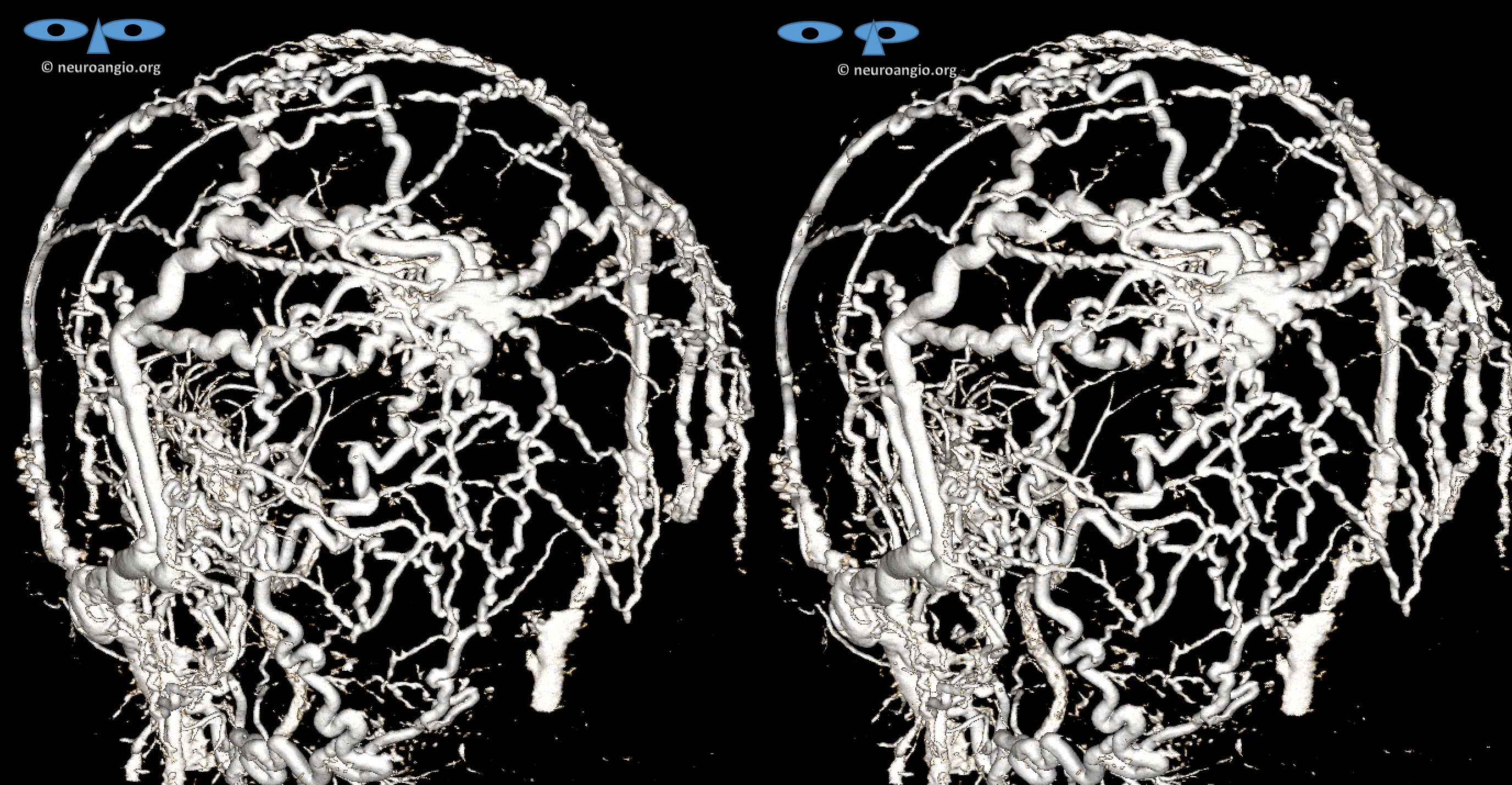
Anaglyph stereo
Not to worry. Lets see closer — another cross-eye stereo
Anaglyph stereo
Look closely — its simpler than it looks. All arteries are coming into one region, and all veins come out of it. The same principles we advocate for brain AVMs and dural fistula apply here — superselective embolization — just getting the nidus and some veins around it is enough. The target is in the oval
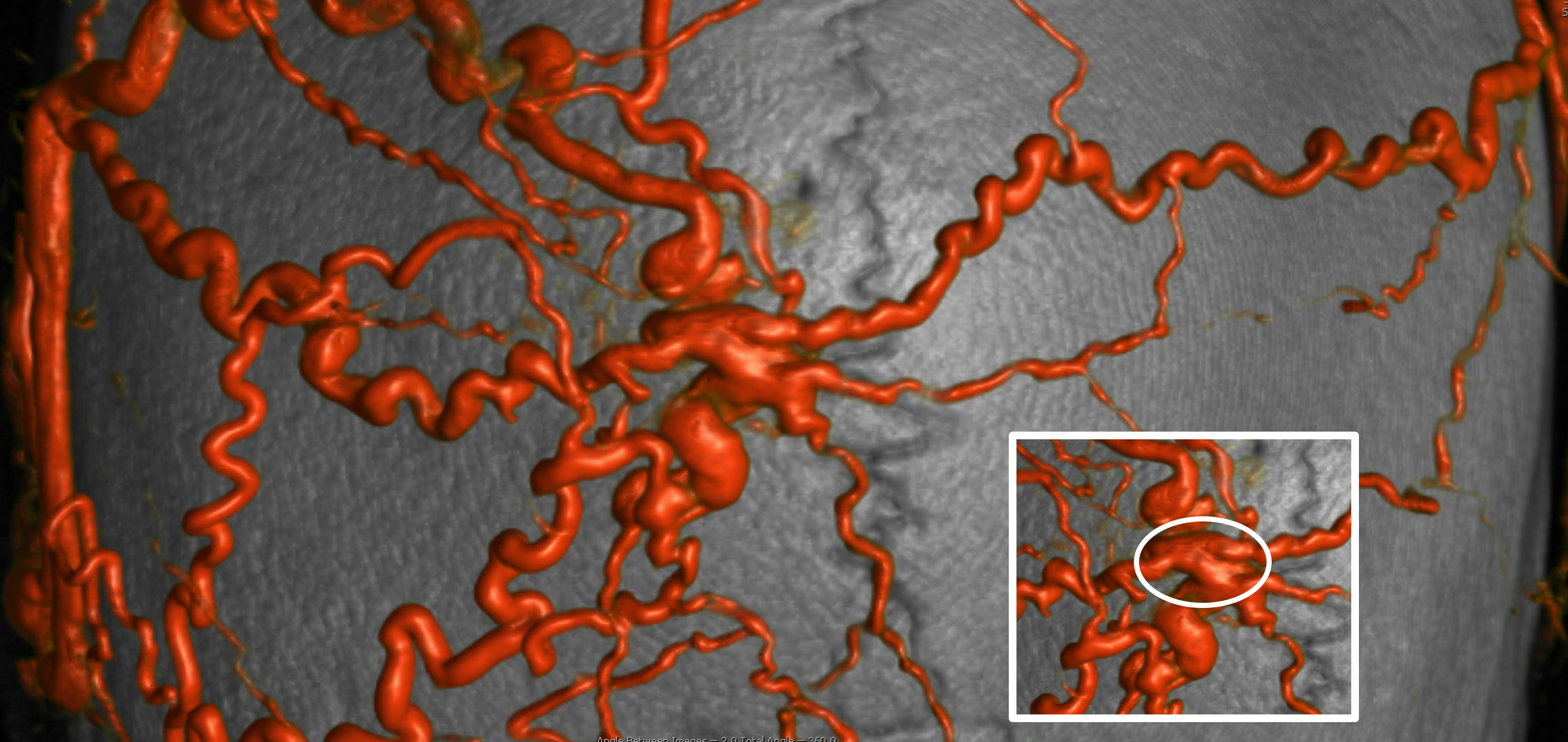
How to do it? Transarterial? Transvenous? Both? Direct puncture?
From among these, the worst is transarterial. Why? It will take a ton of catheterizations unless you get very lucky with onyx (which is not likely in the scalp), and any transarterial liquid embolic embo will take out skin, which will be nice to have for surgery. Some will just put coils into proximal arteries, which is OK, but will still bleed a lot. We prefer transvenous or direct puncture.
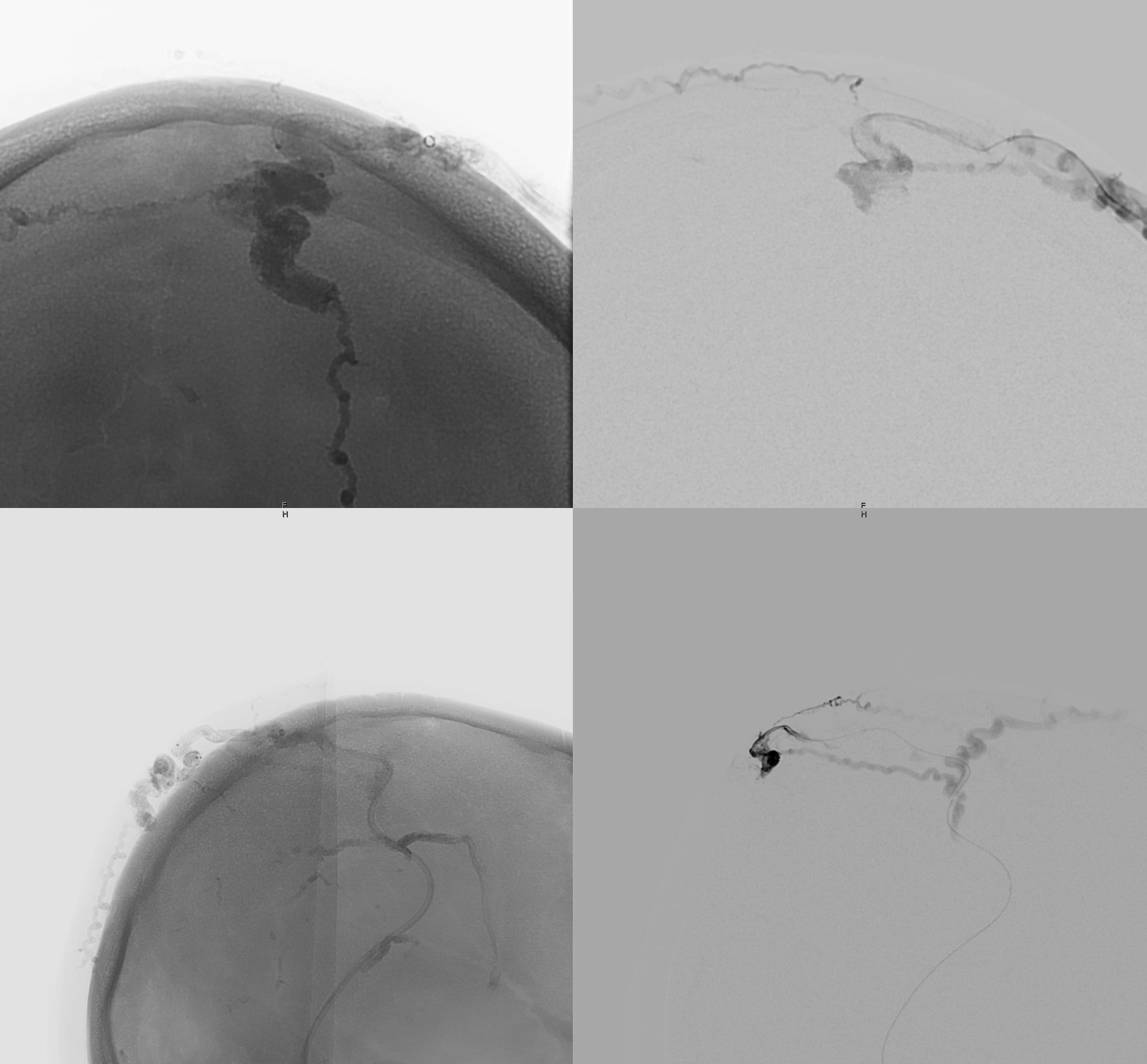
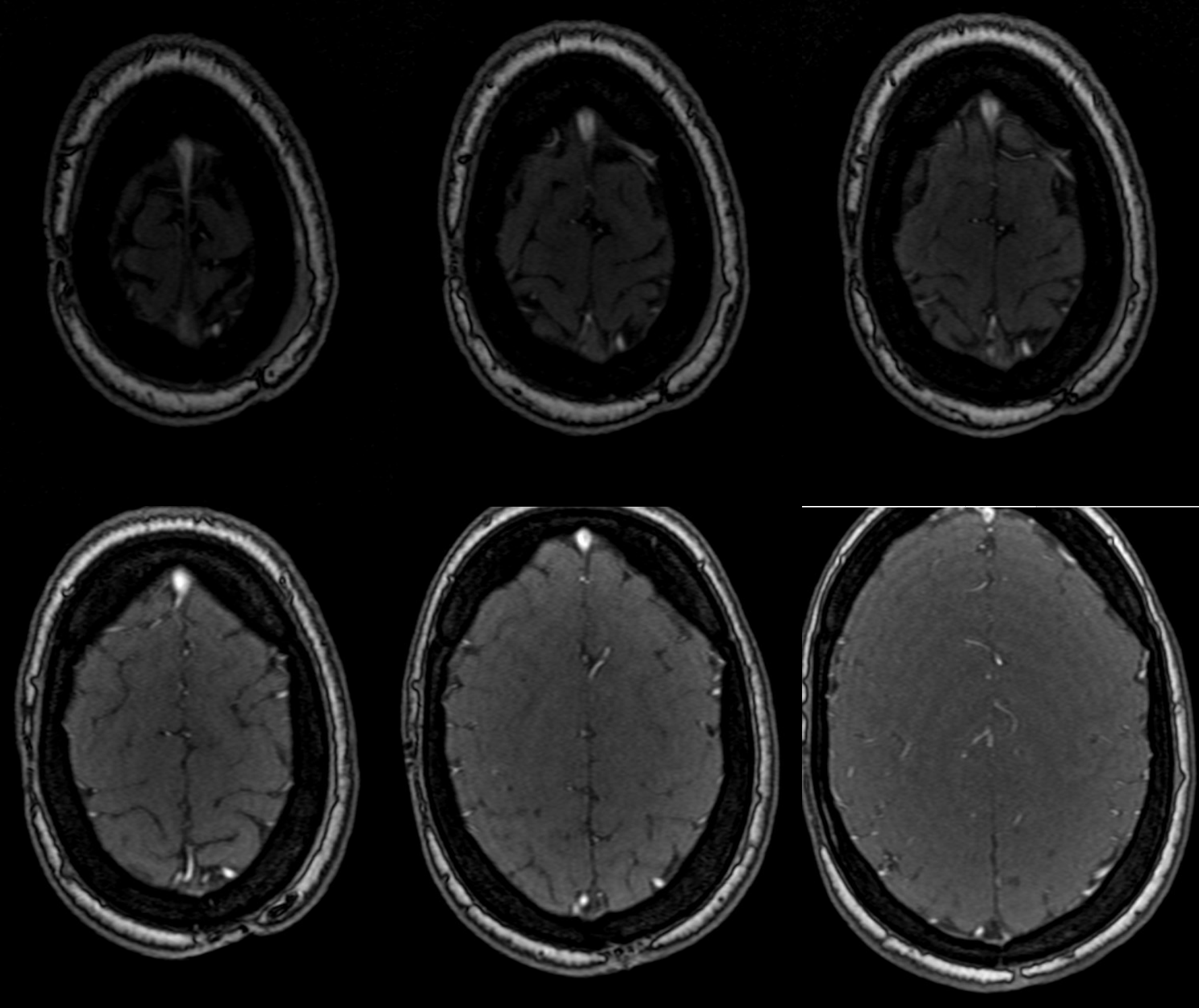
Below is transvenous approach. Important to have intermediate catheter support in the veins — we have a Sofia 5 with a BMX guide. The microcatheter is a Scepter XC — good to have that flow control option
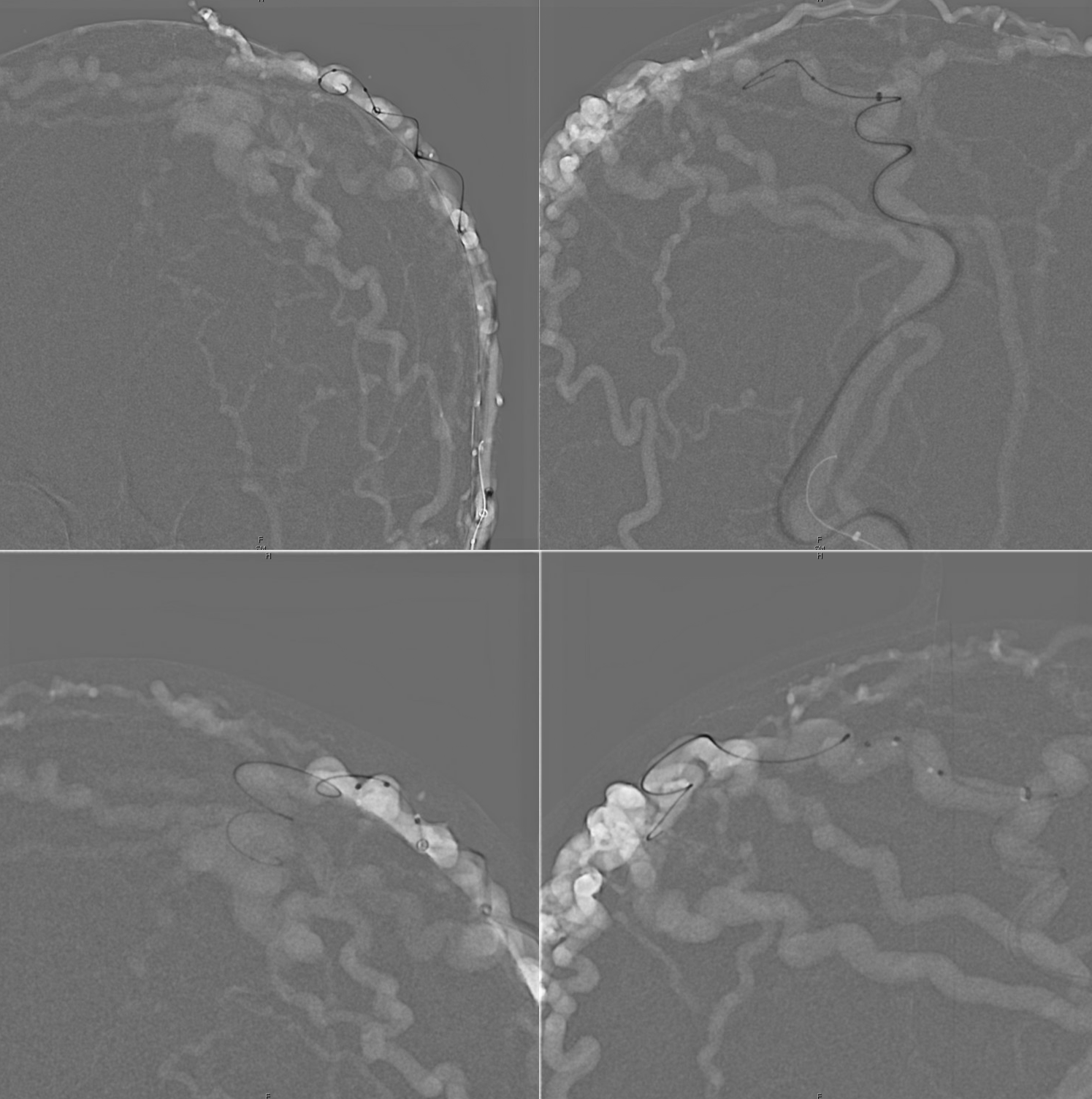
In position — corresponding arrows.
Top views are Scepter injection (fistulogram). Bottom are from the Sofia. To confirm good position.
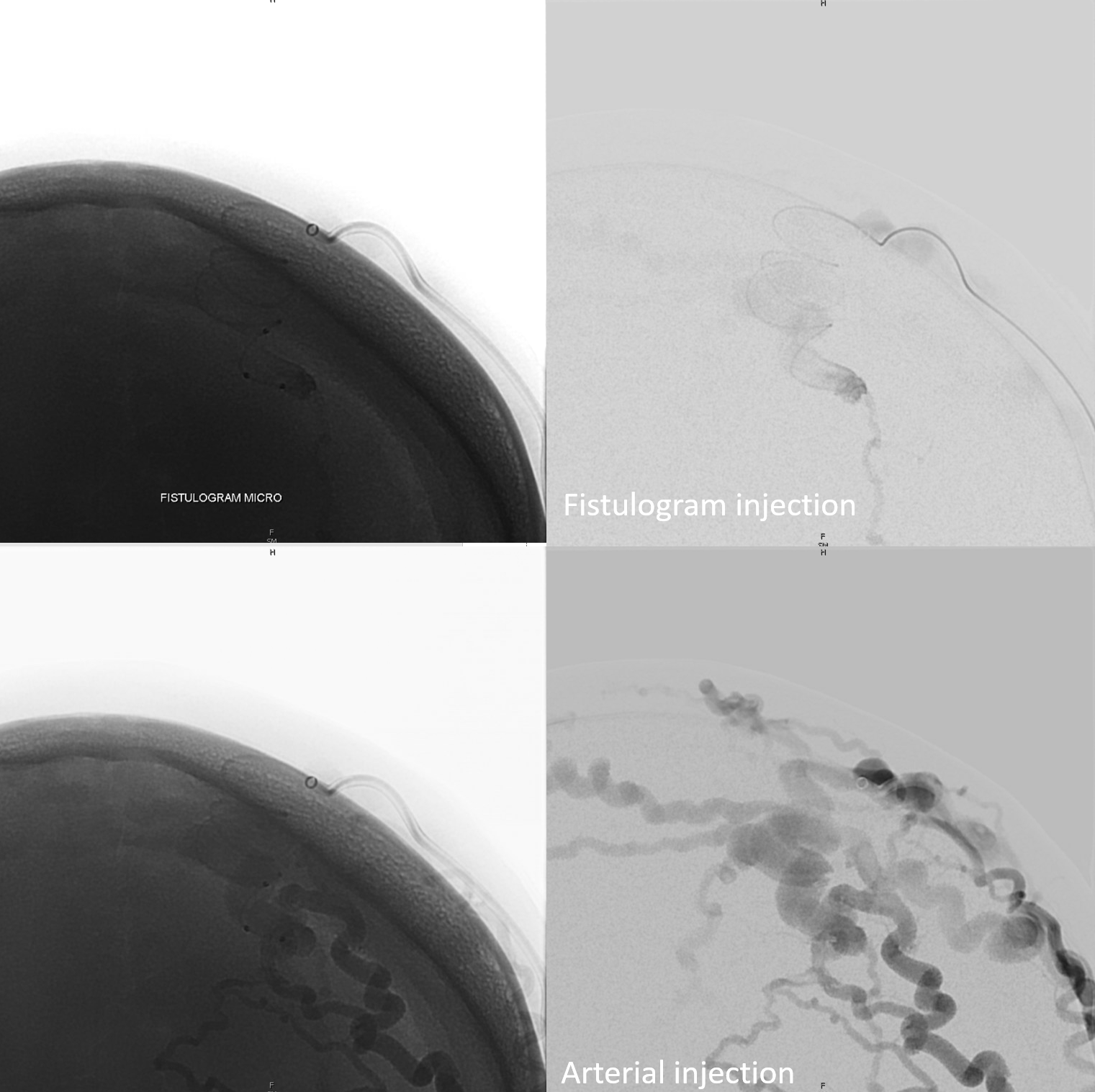
Inflating balloon
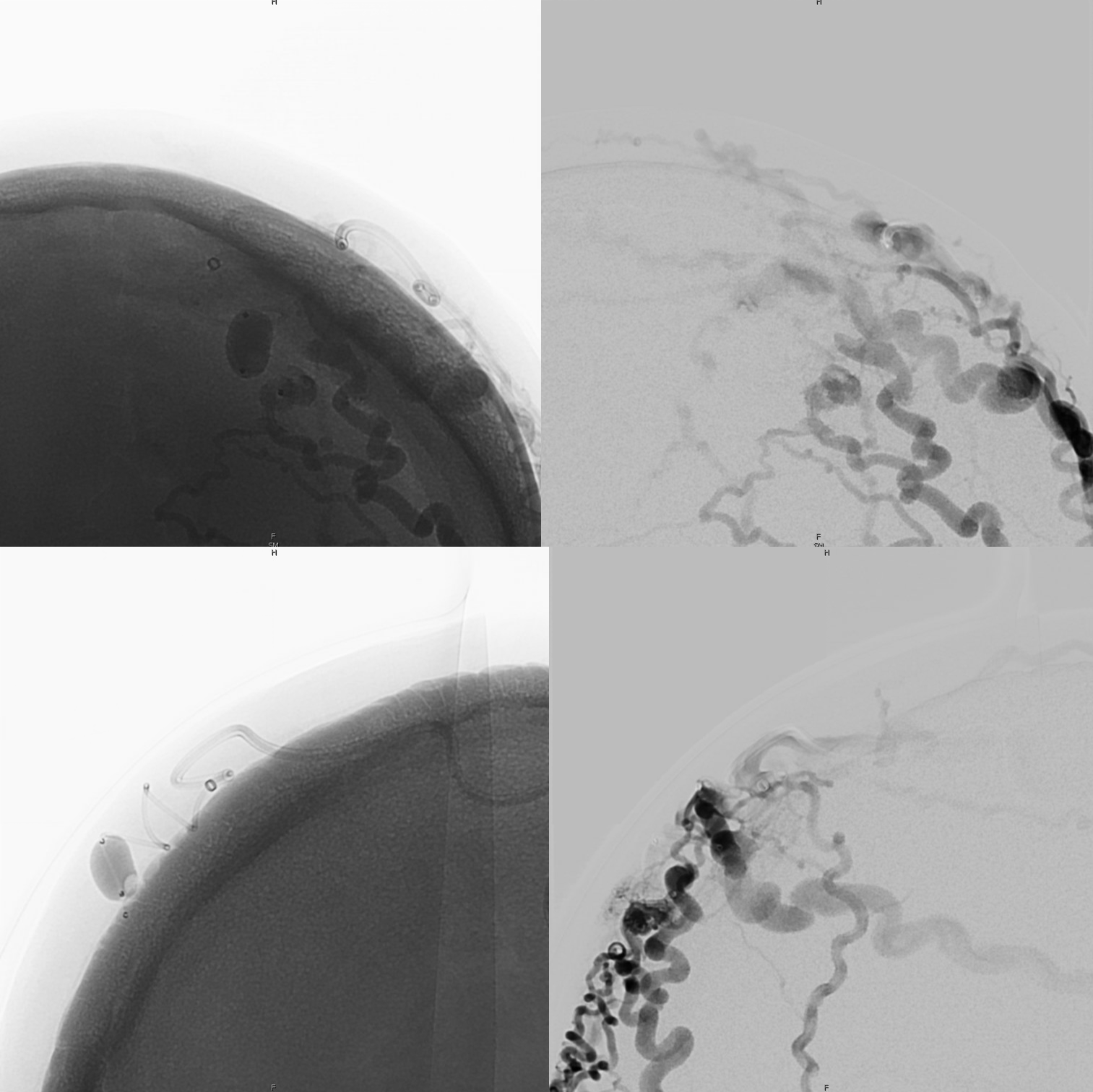
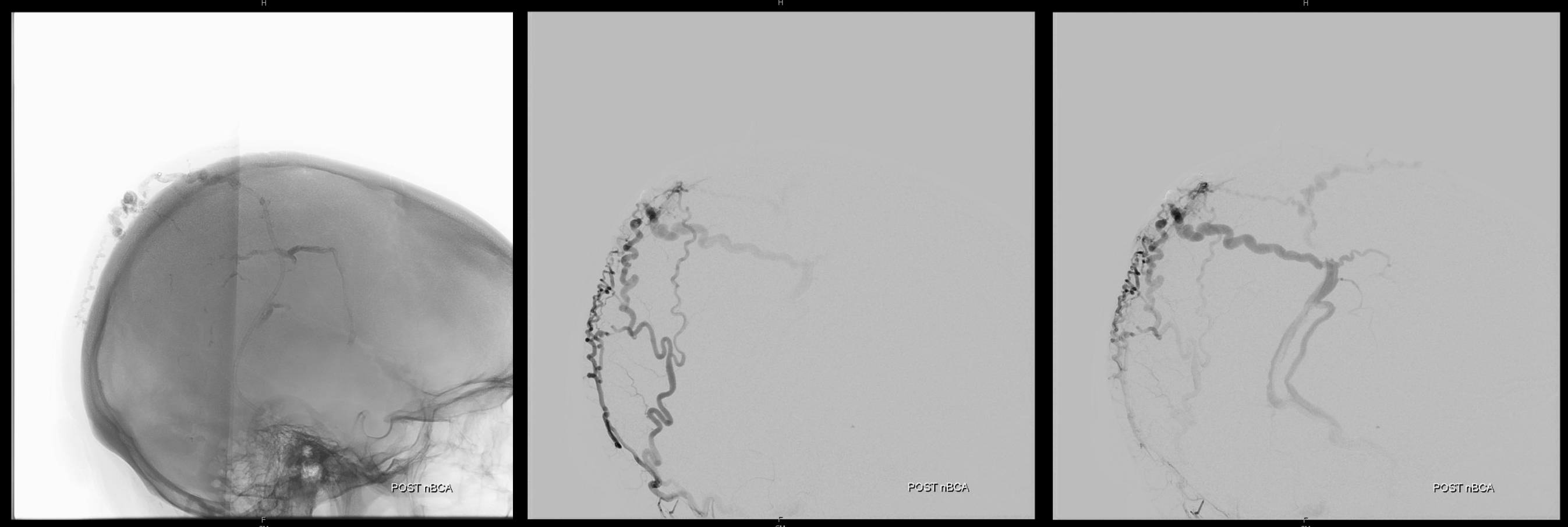
Here we make what turns out to be a suboptimal choice of using nBCA. When it works its great. But if often ruptures the balloon and control is lost — see image on right. The glue escapes into some scalp veins — which is no problem at all. But it we dont have good flow control now.
Still, its a very nice deposition.
Much better, but still alive
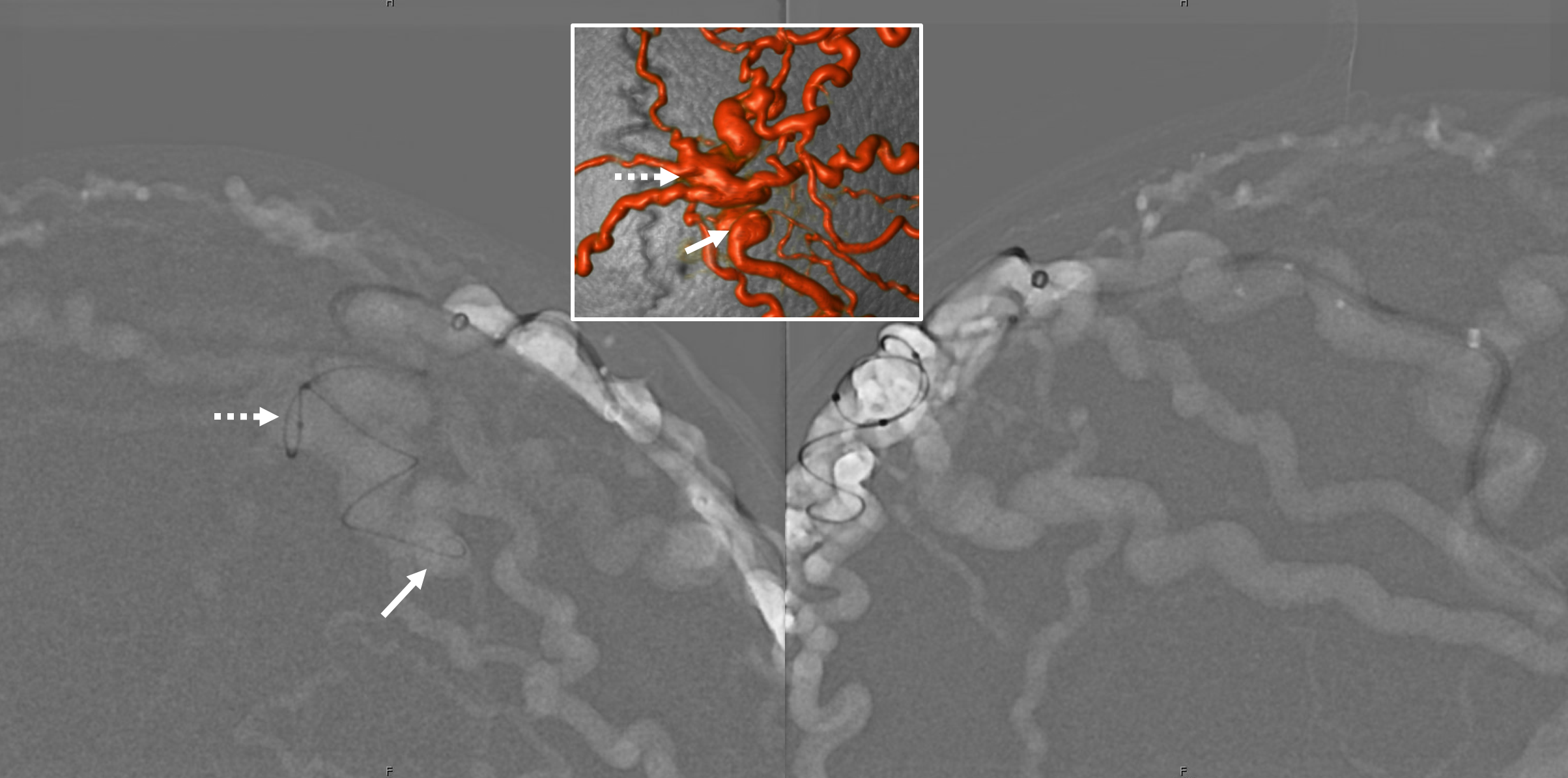
Second transvenous approach — via the next largest temporal vein
Fistulogram on bottom
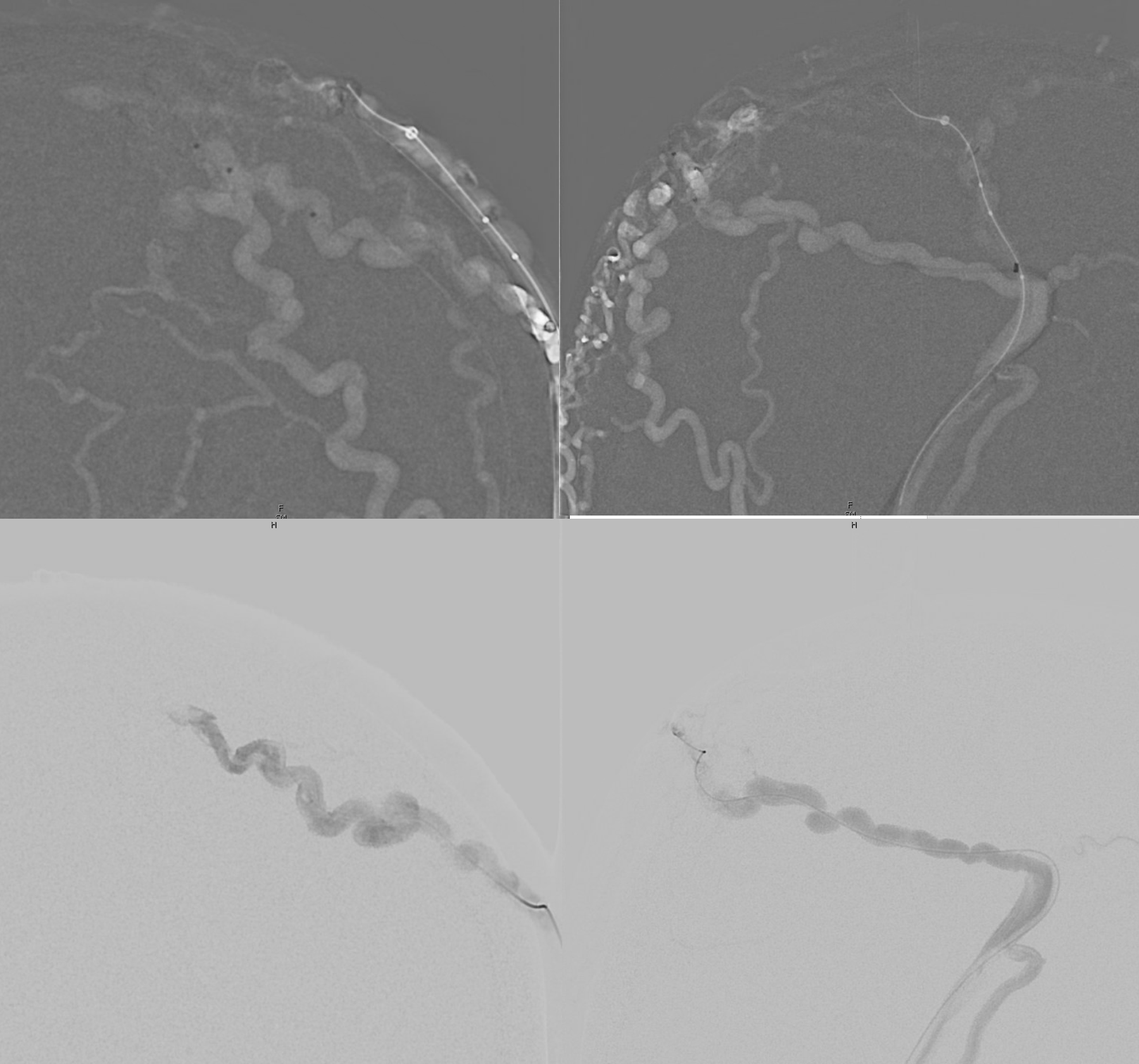
Balloon up. Now we will use Onyx — the other reason we didn’t want to use it is because of intraoperative cautery fireworks — that’s fine in the scalp though
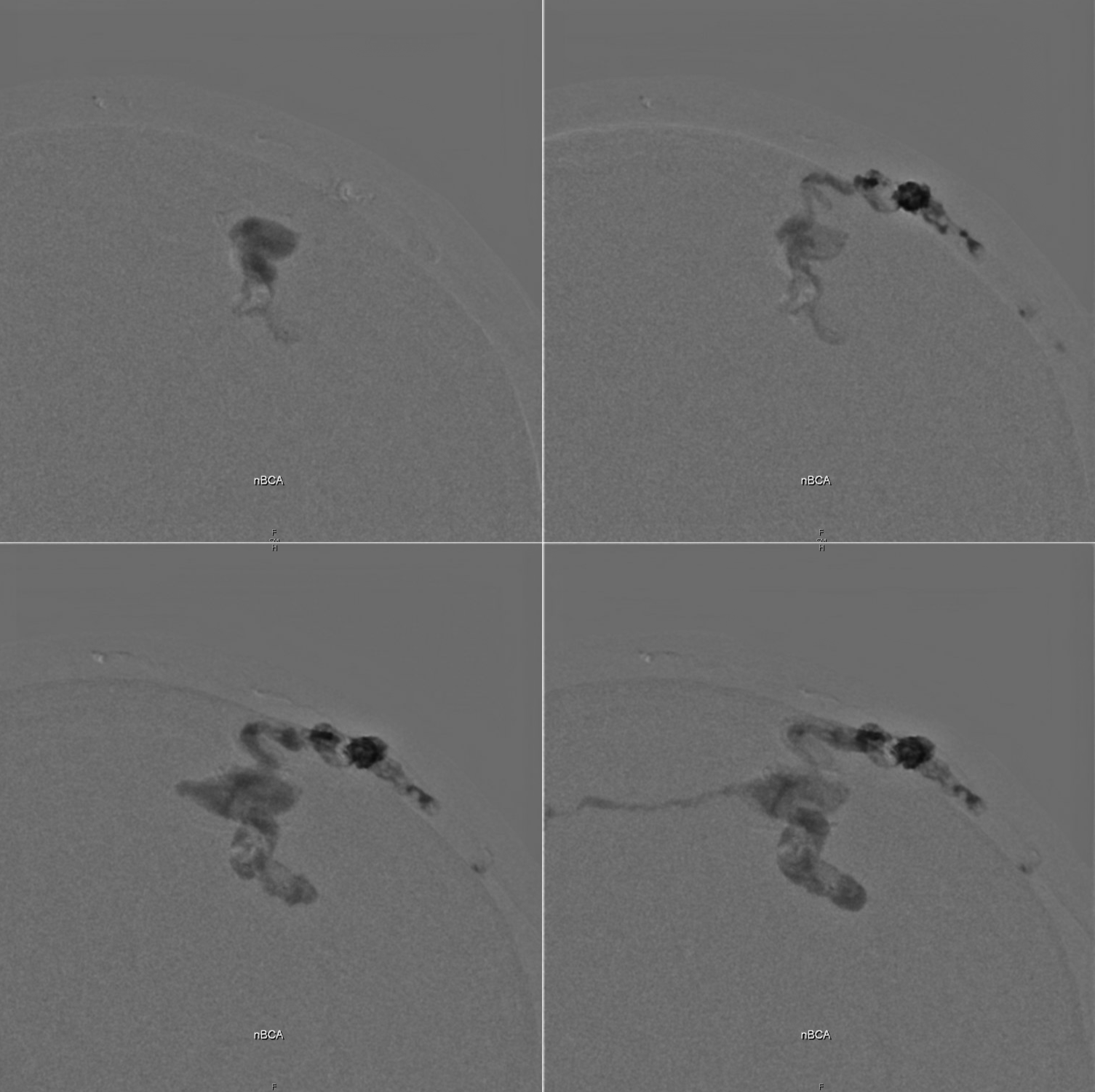
Onyx does its thing
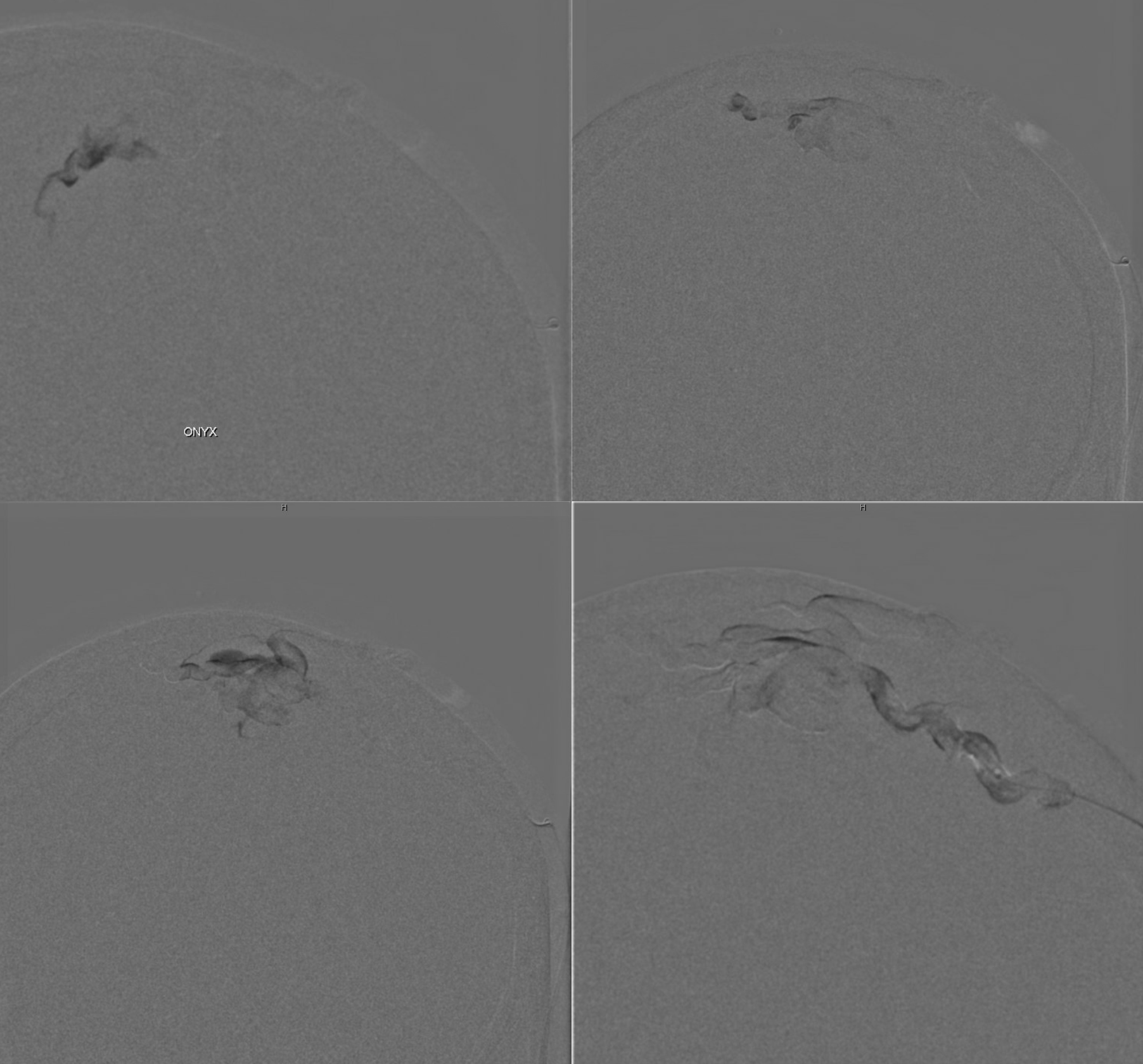
Still some left
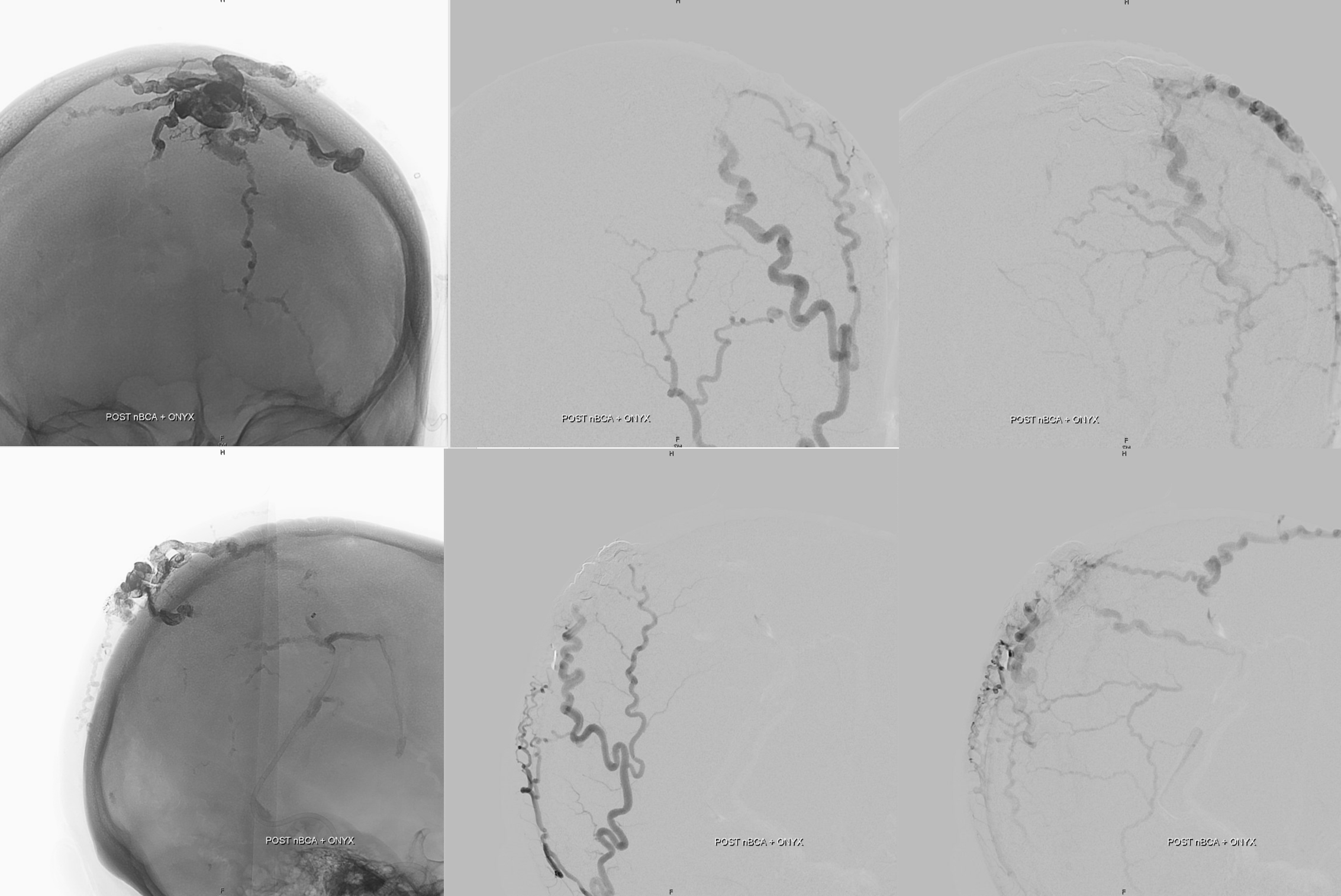
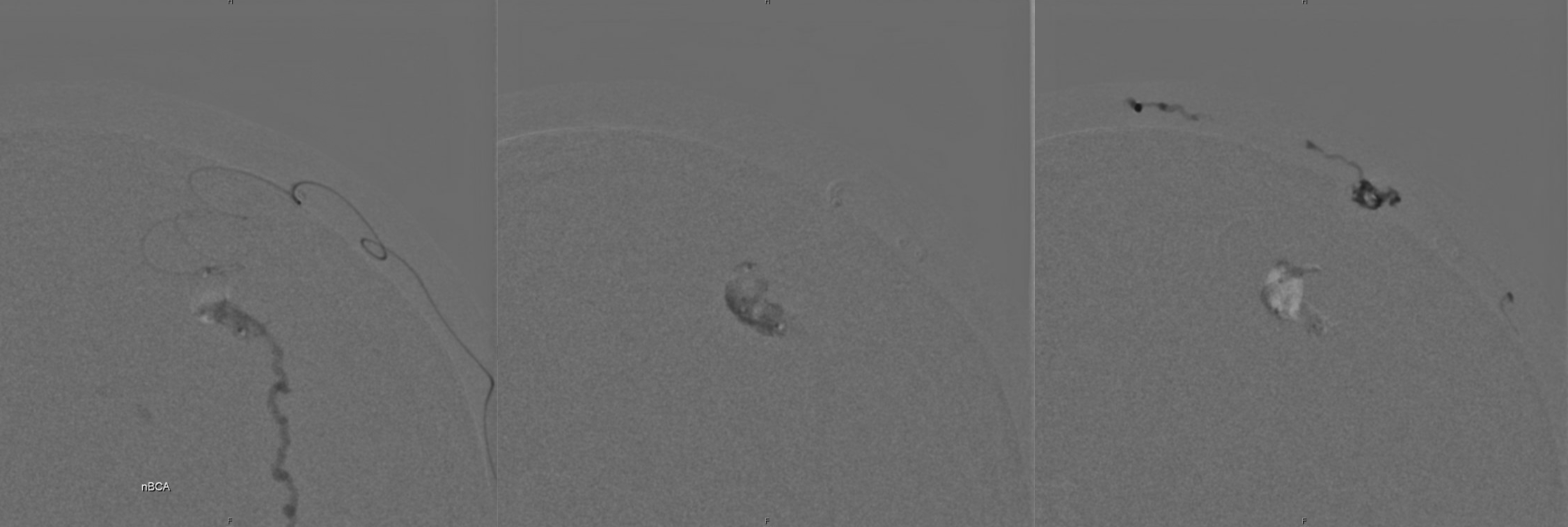
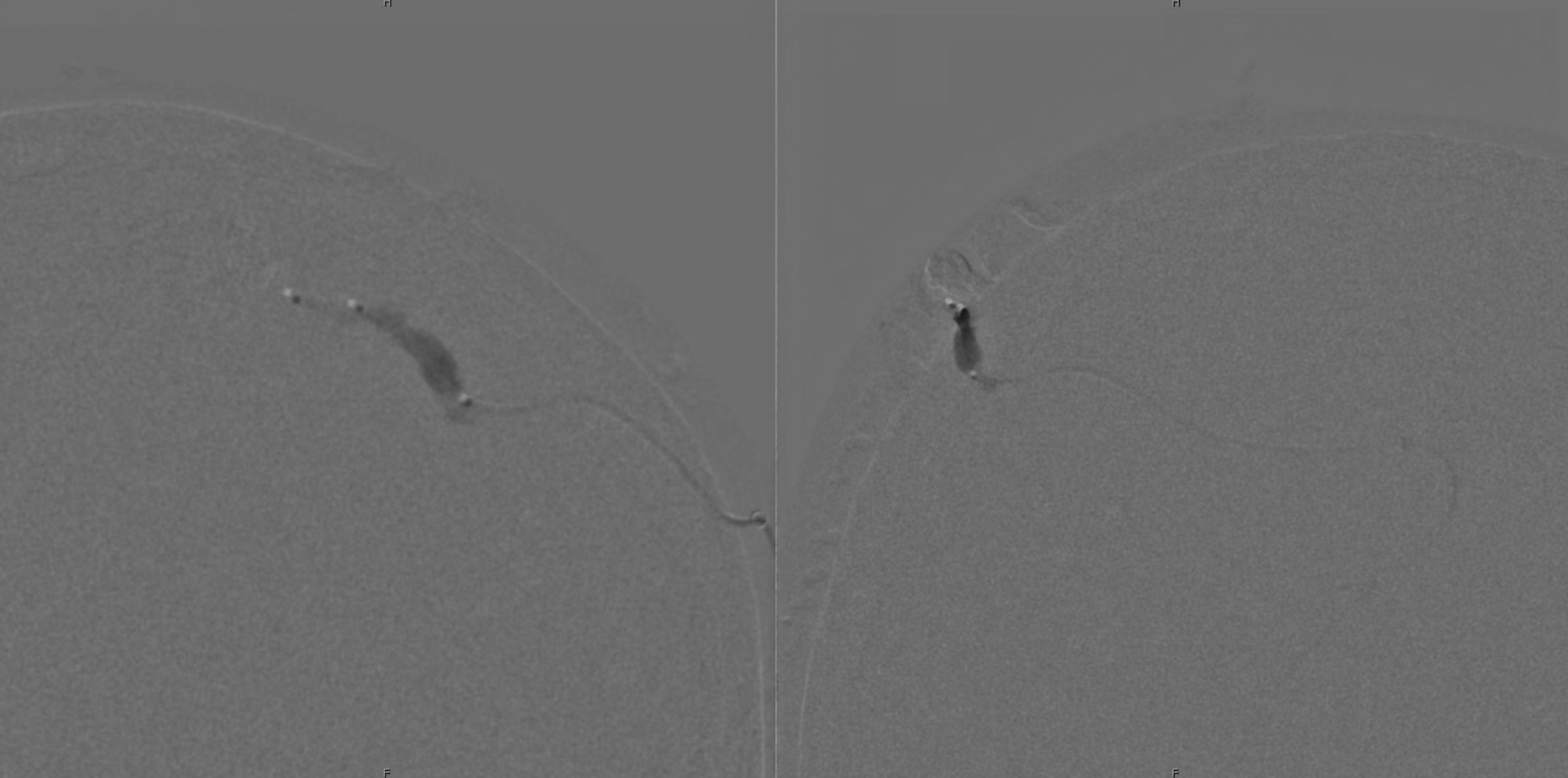
Now direct stick — simple technique — dilute nBCA (1:3 nBCA:Lipidol) in a 3 cc syringe. Under fluoro roadmap guidance, stick the nidus with a 20 or 22 gauge angiocath. When bright red blood comes out, inject glue. No need for any D5W lines etc — glue against blood will be fine in an angiocath pretty much always. Two shots — top and bottom
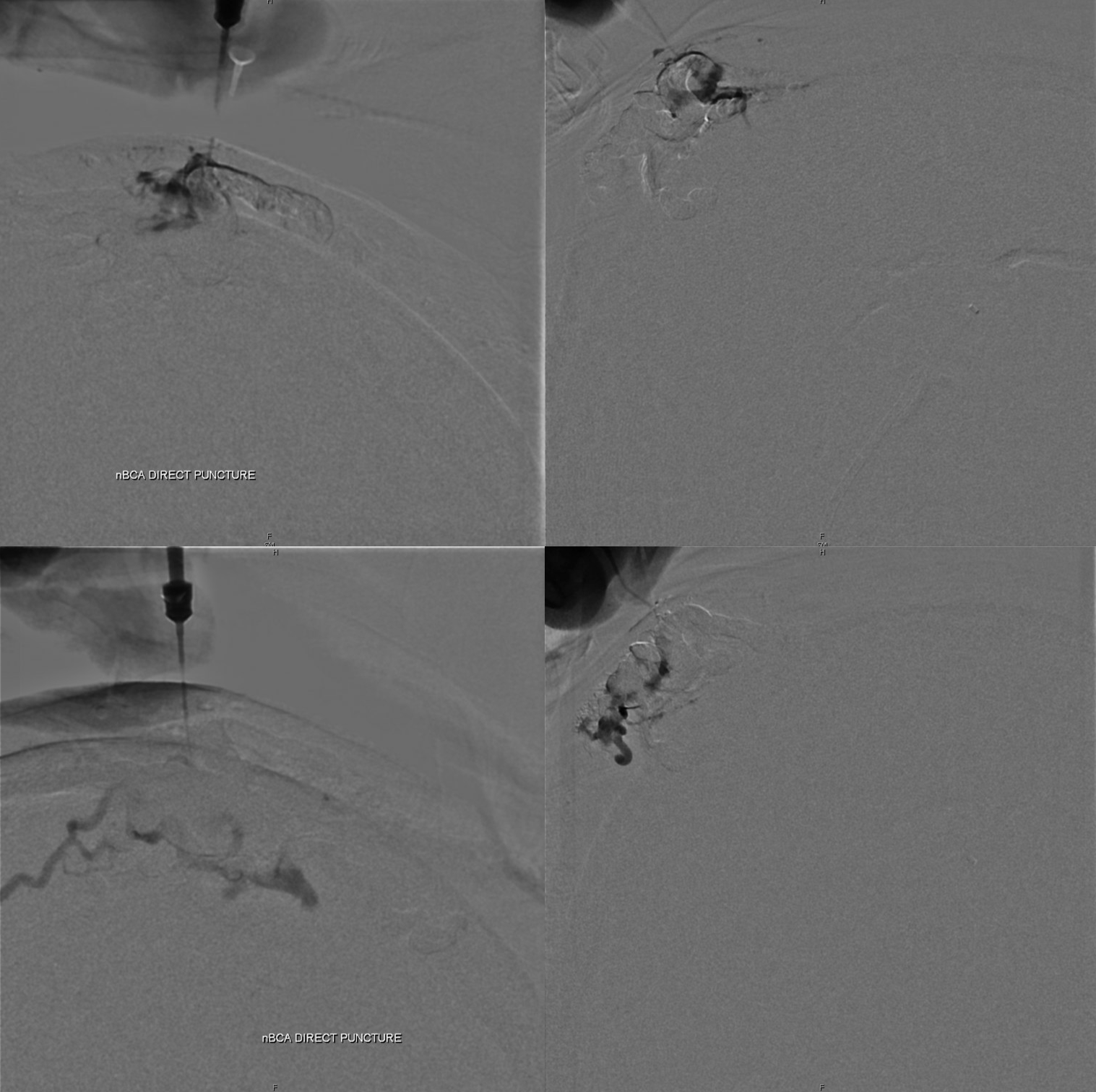
Post left ECA (top) and right ECA (bottom). Very little is left. Plenty enough for presurgical embo
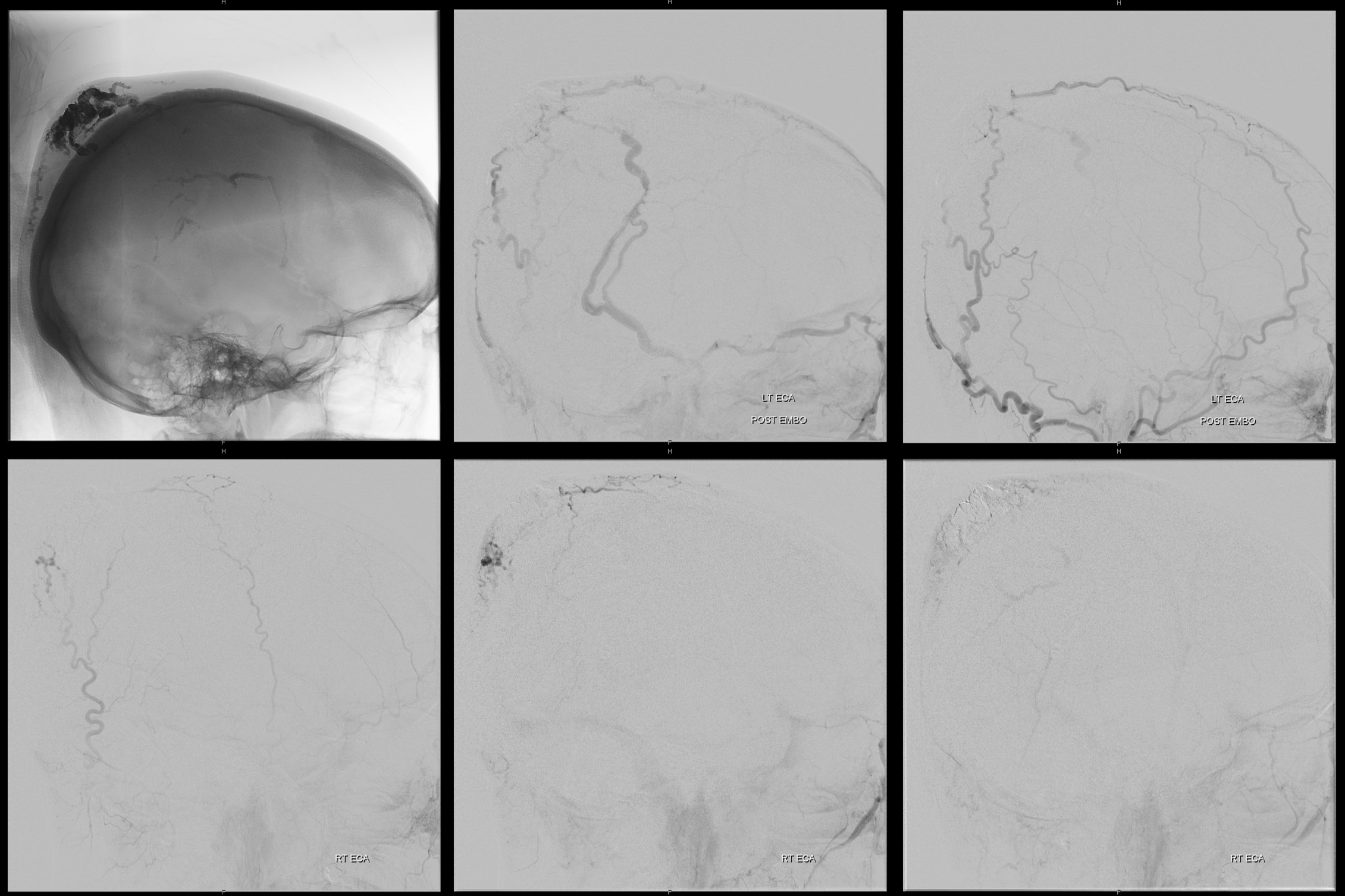
Picture of embo cast is very nice for surgeon. Can also tell with respect to cast where residual supply will be – 9 o’clock when looking from the back.
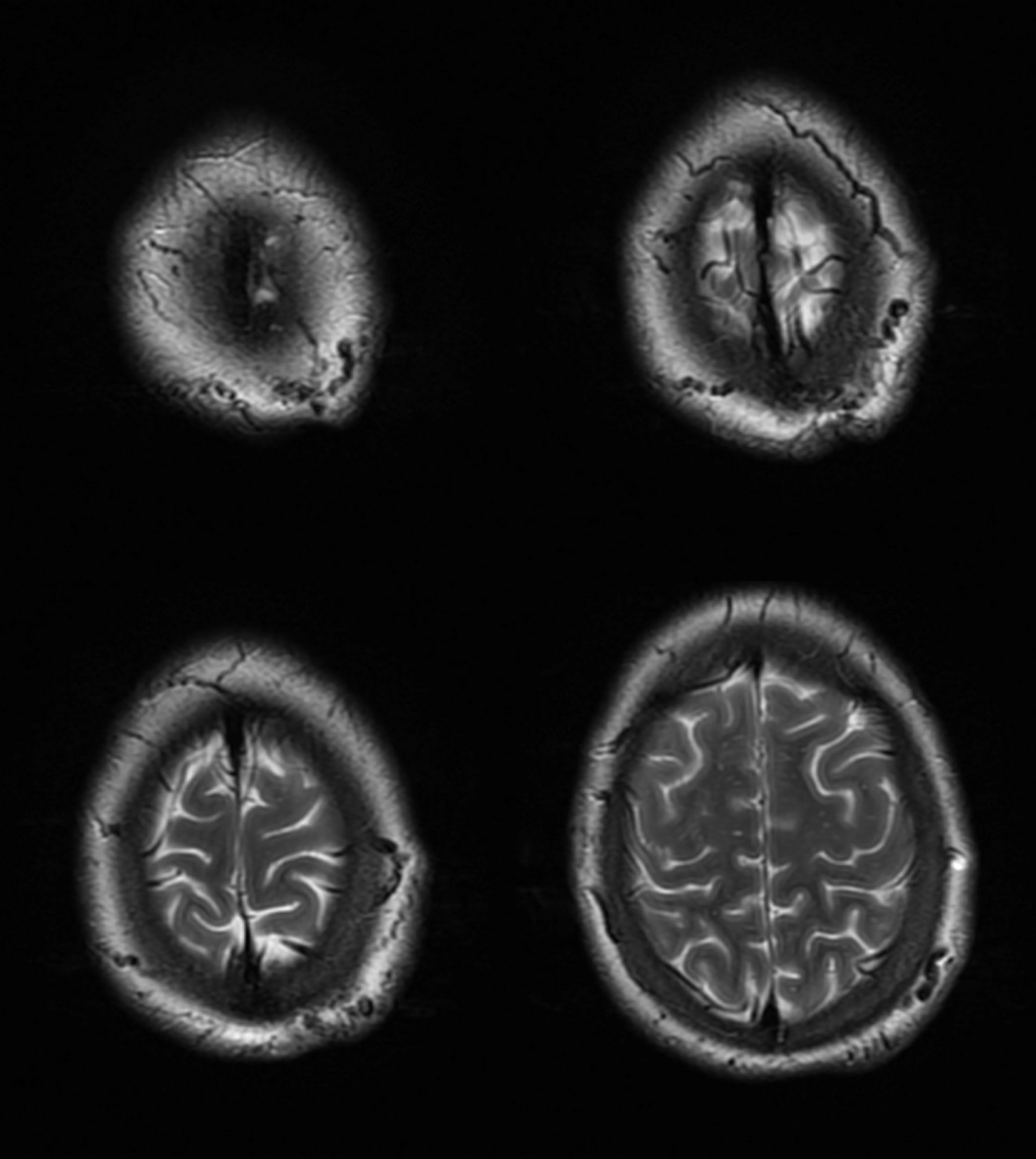
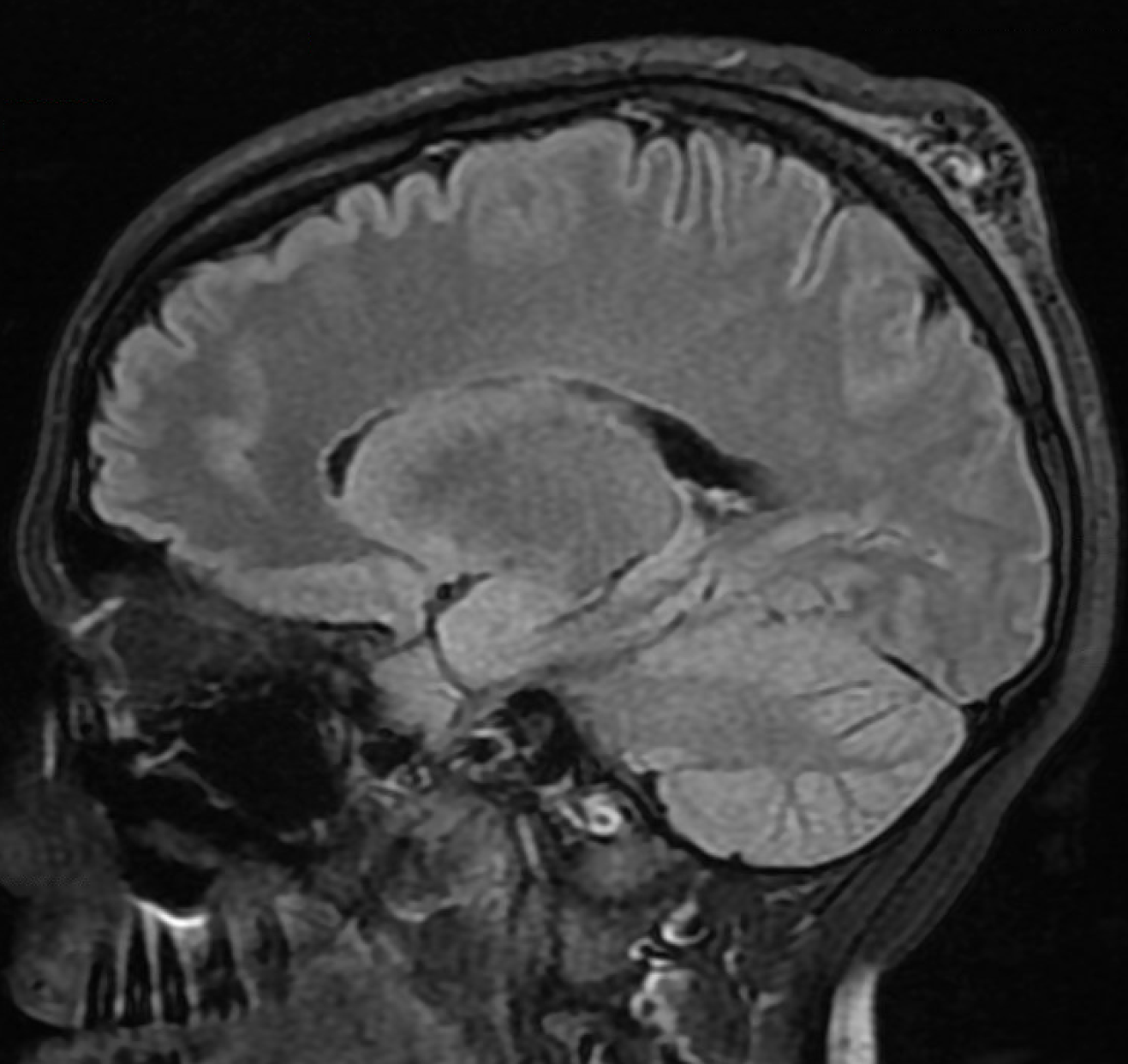
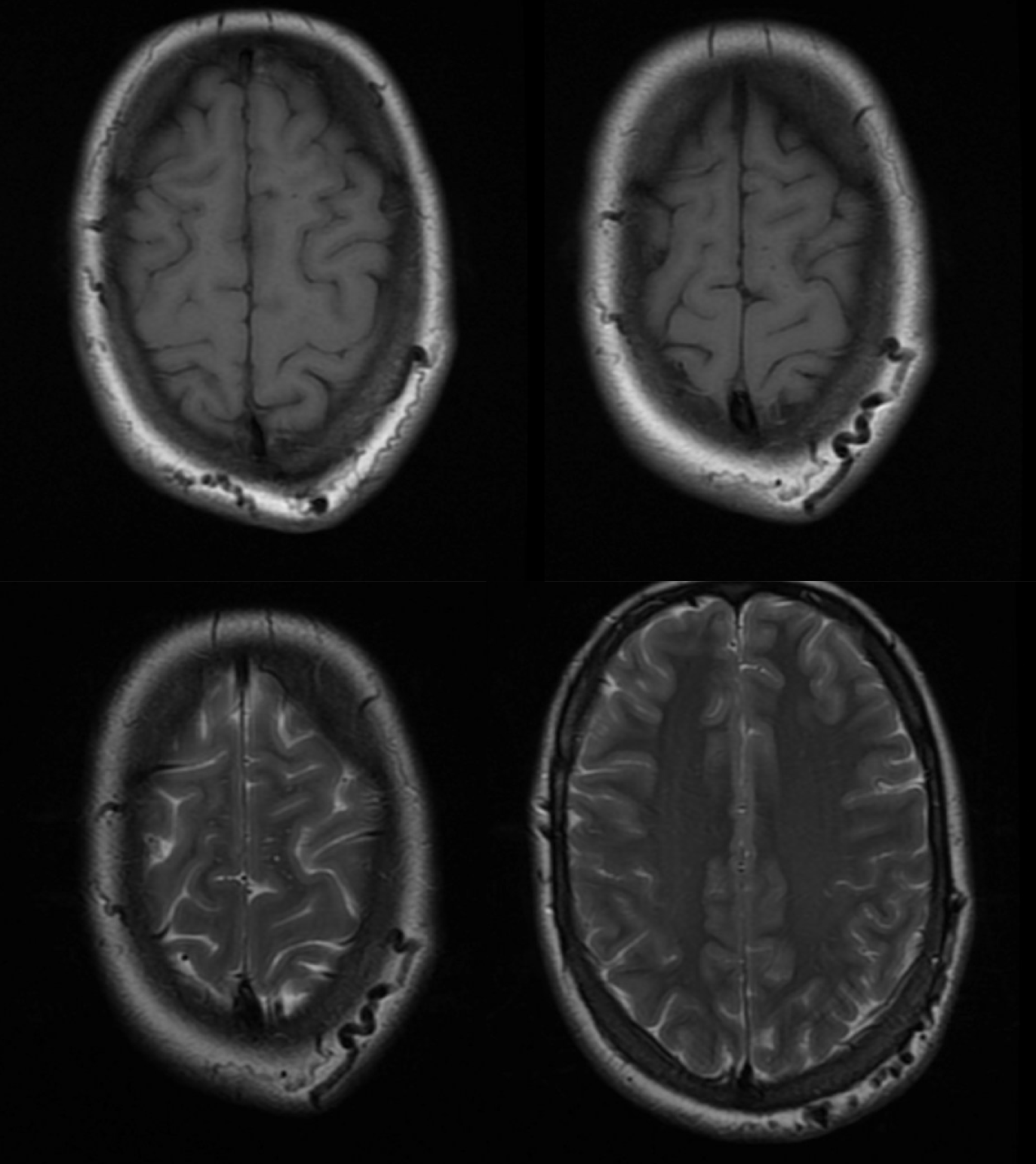
MRI/A 6 months post resection. No skin graft was needed
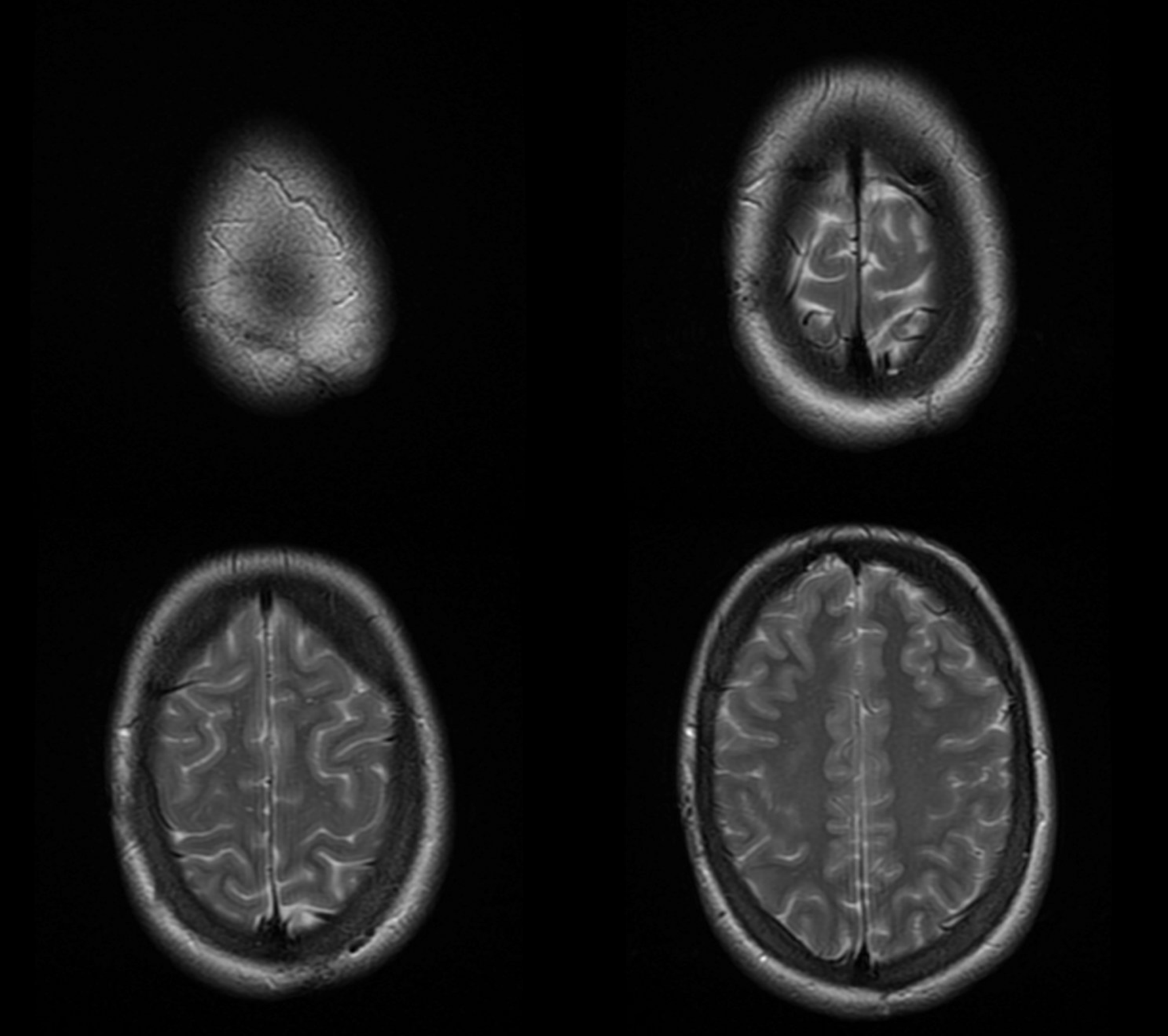
MRA — extended to vertex. Nothing to see.
Plan for delayed angio — at least one angio 12 months post or longer is rule for us. Just to make sure.
Other preop embos — see Case Archives, including Ear AVM, Orbital (Lacrimal Gland) AVM
Like it? For questions/concerns/referrals email neuroangio@neuroangio.org
