An unusual kind of AVM, and an instructive case in spinal anatomy
Presentation is with progressive upper extremity dysfunction

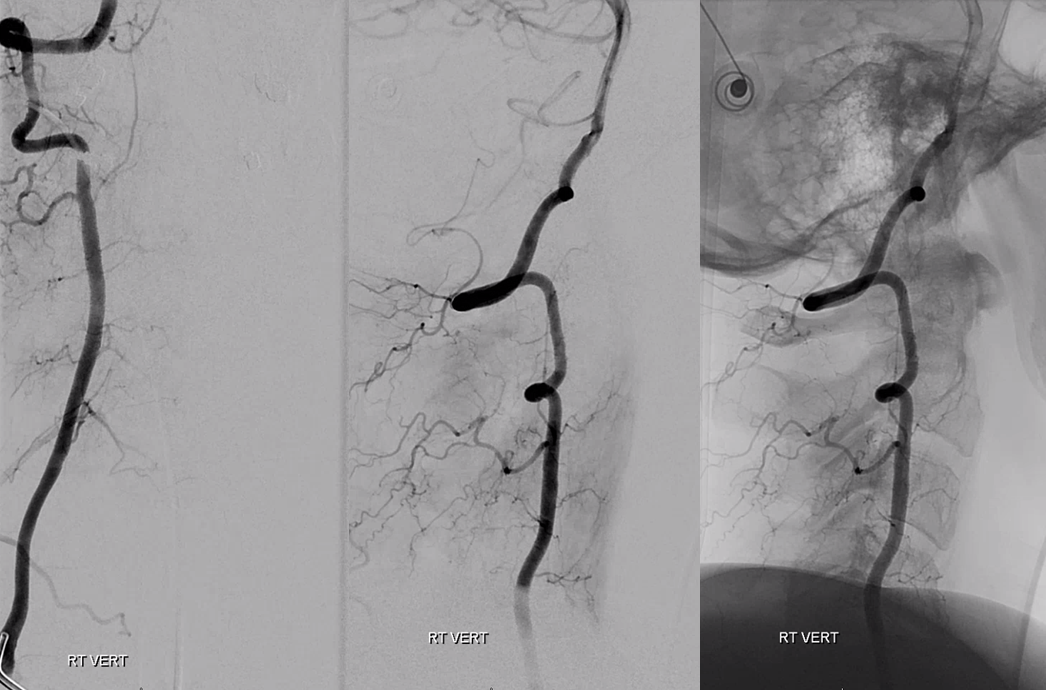
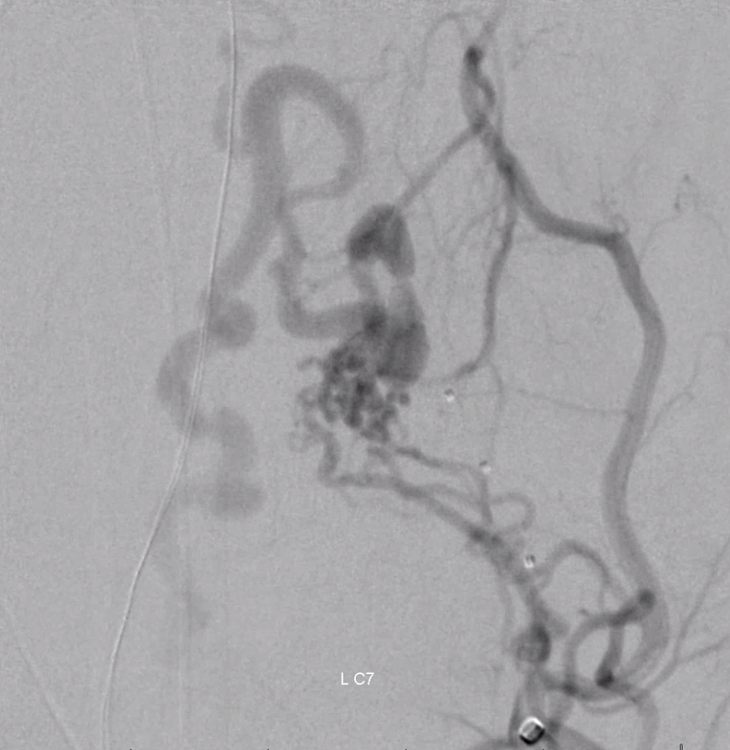
Important to image that ECA looking low

Look how those ultra-congested spinal veins have no caudal outlet, with outflow ultimately directed cranially into the upper cervical epidural venous plexus
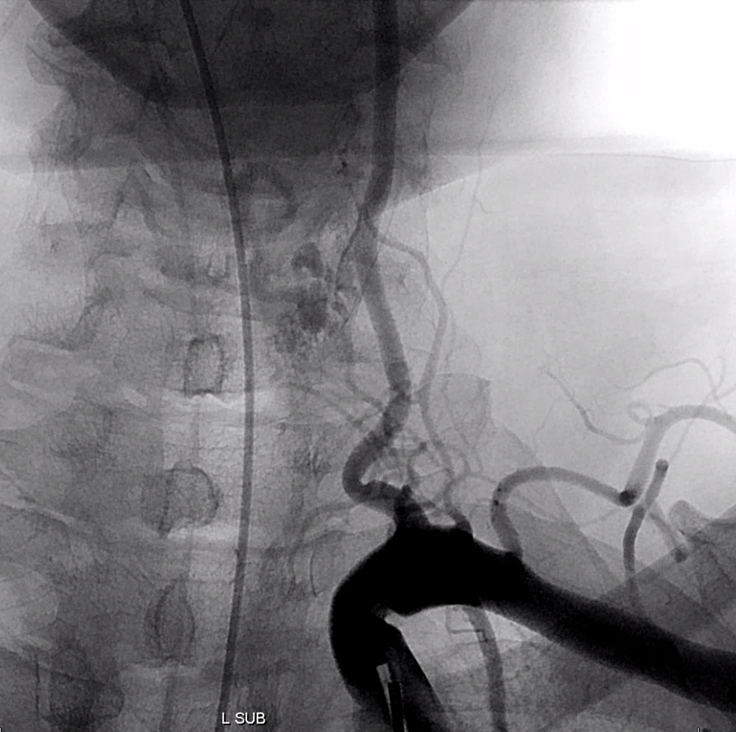
Off-midline nidus location
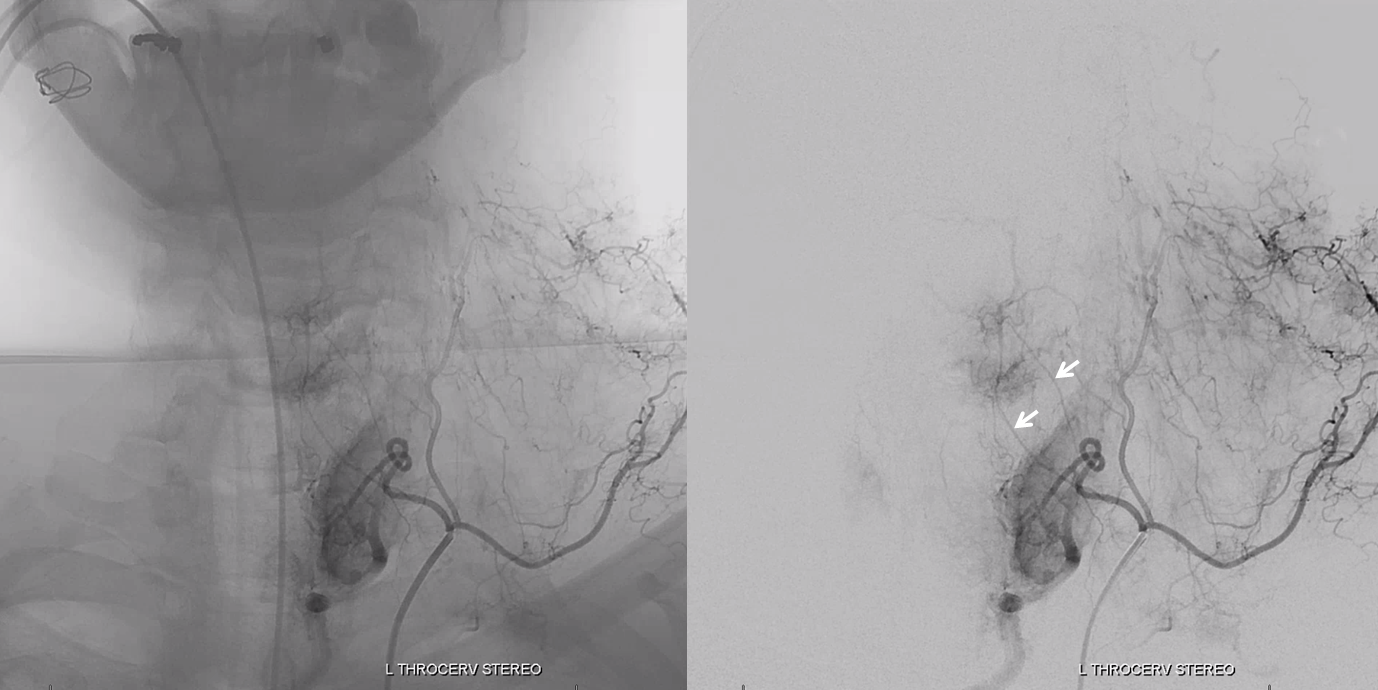
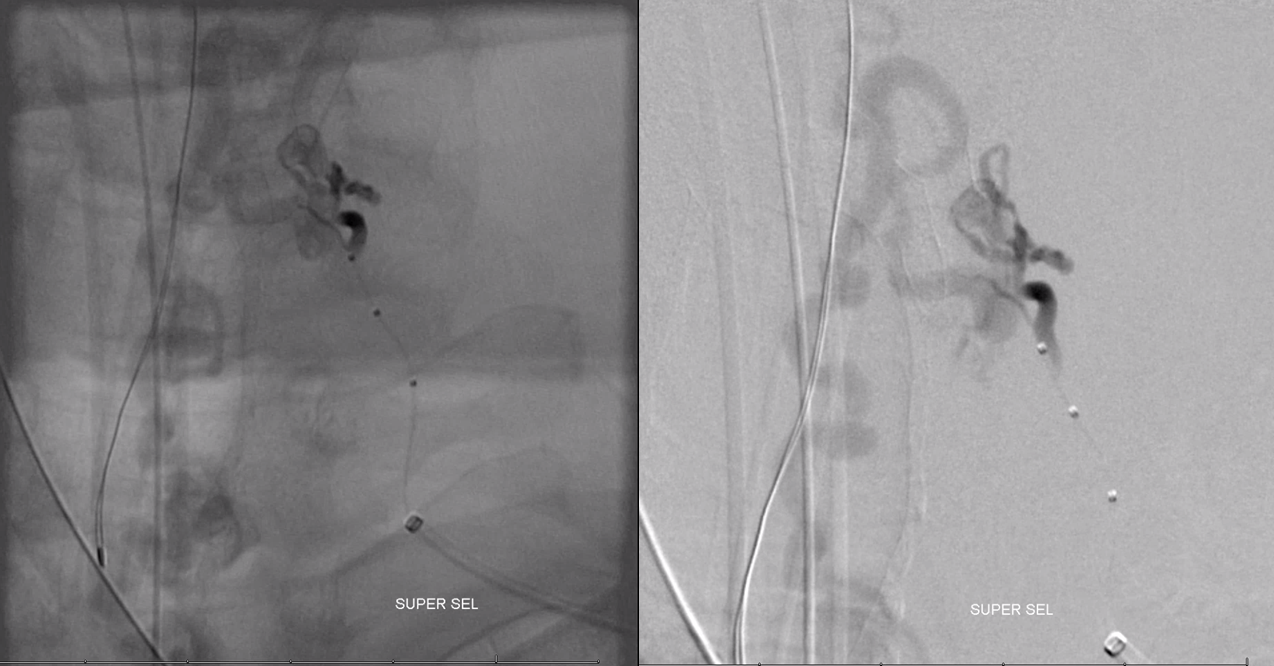
Stereos
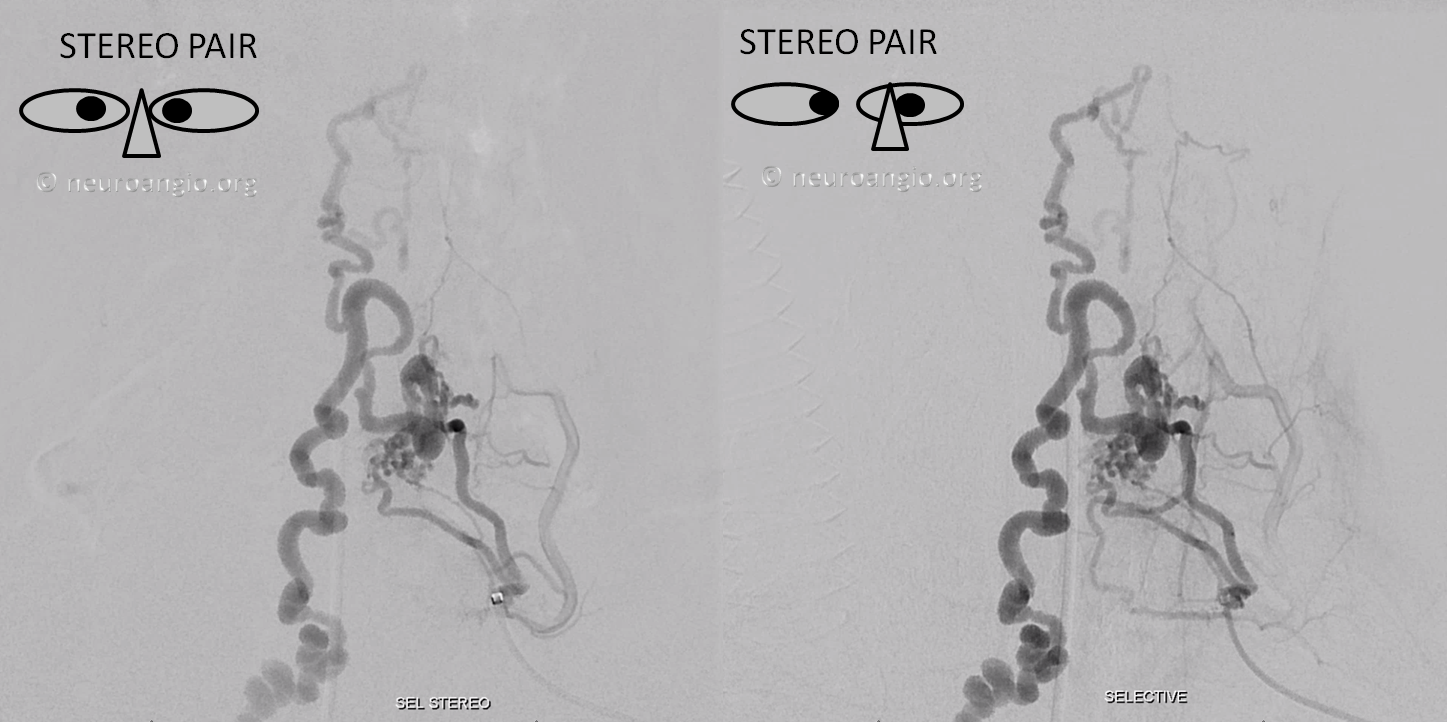
Anaglyph stereo

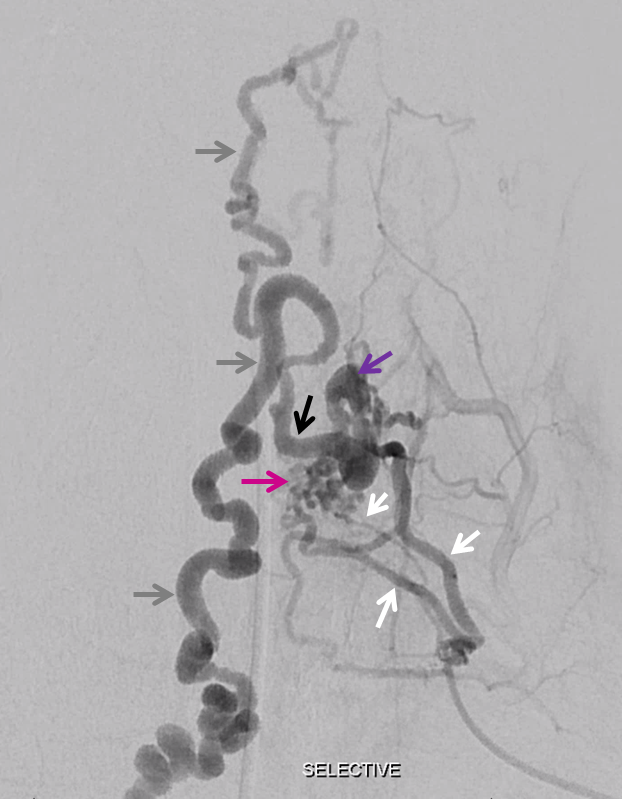
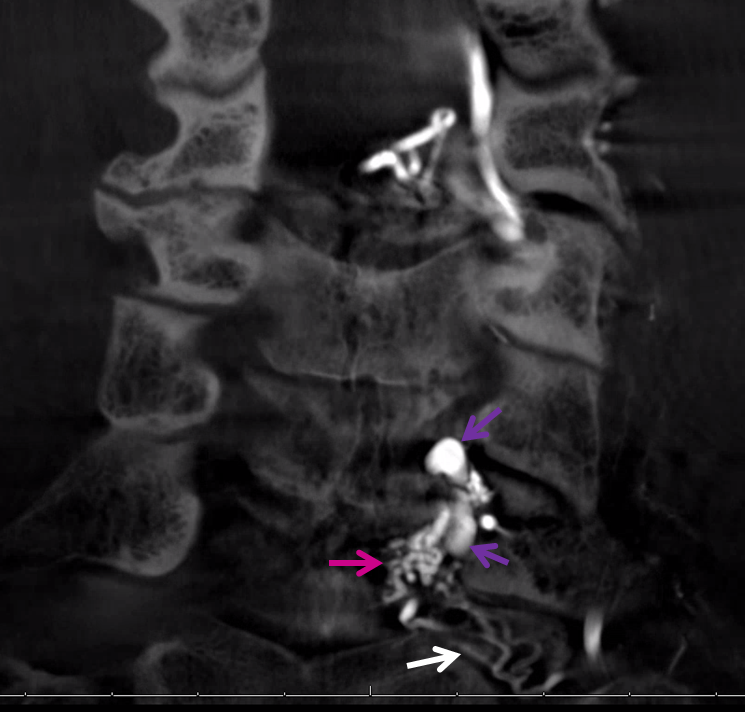
Several left C8 radicular arteries (white) supply nidus (pink), draining into single extradural radicular vein (purple), coursing medially (black) to open into and congest intradural cord surface veins (grey)
MIP Dyna CT coronals
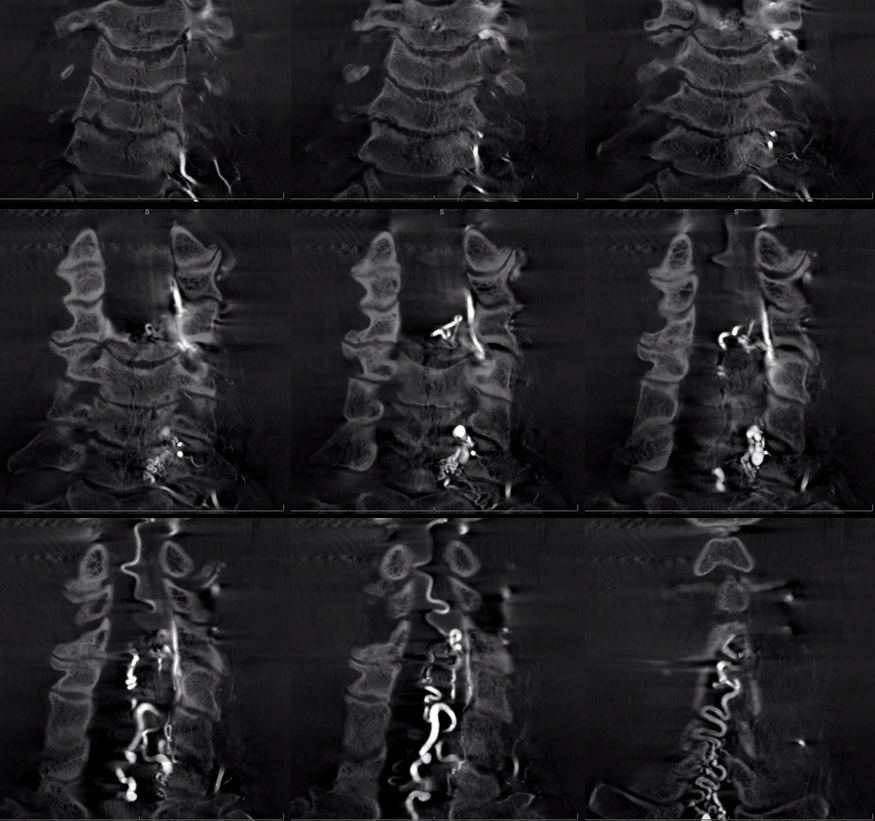
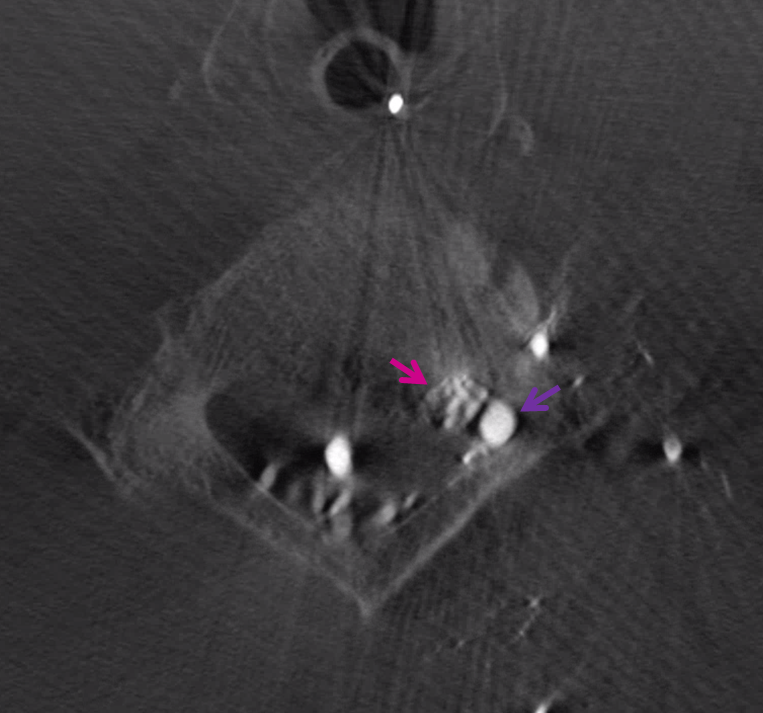
Axial Dyna CT source image, nidus (pink) and extradural proximal draining vein (purple). Also seen are multiple posterior spinal veins
Coronal MIP
Small anterior spinal artery (white) off mid-cervical vert is not opacified to level of AVM
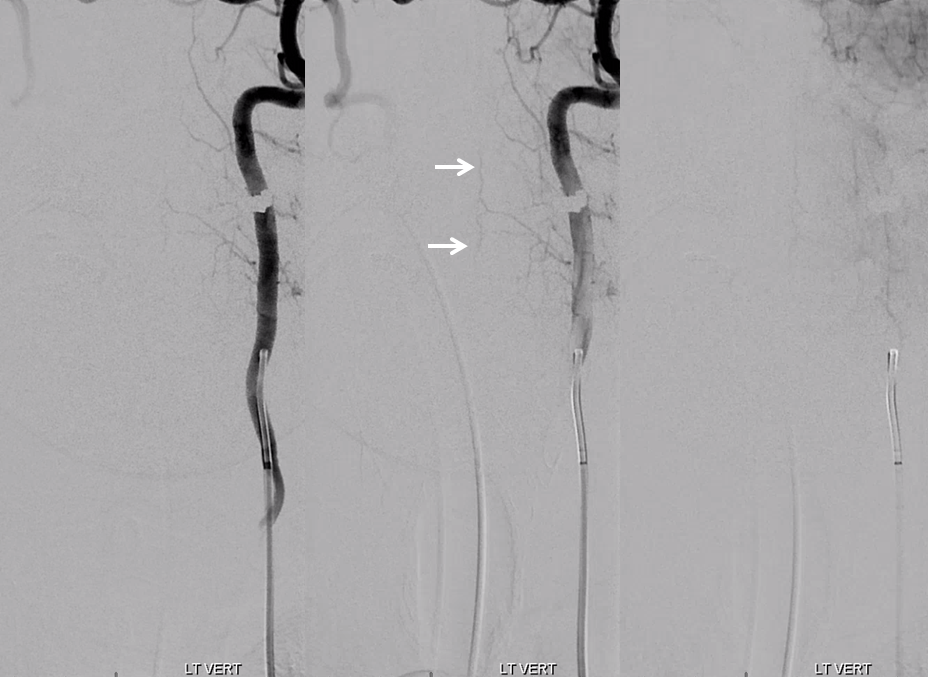
Ascending Cervical shows C7 and C6 radicular arteries (white arrows) which do not reach midline. Often these supply posterior / lateral spinal network
Some thoracic levels are injected in addition to those below. No anterior spinal is found
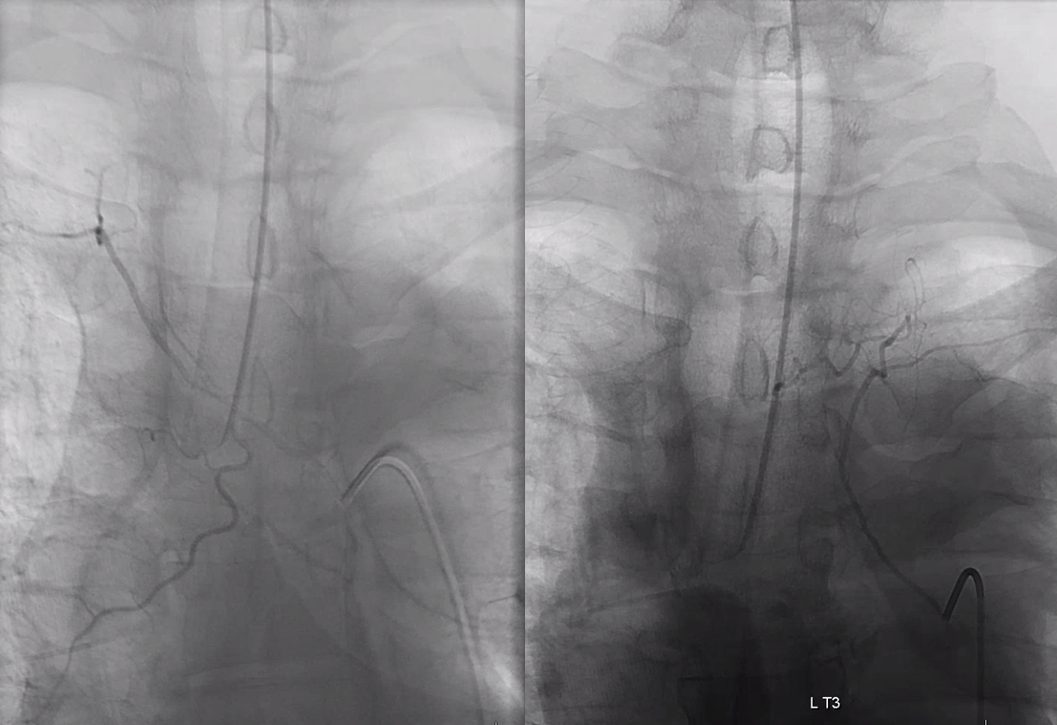
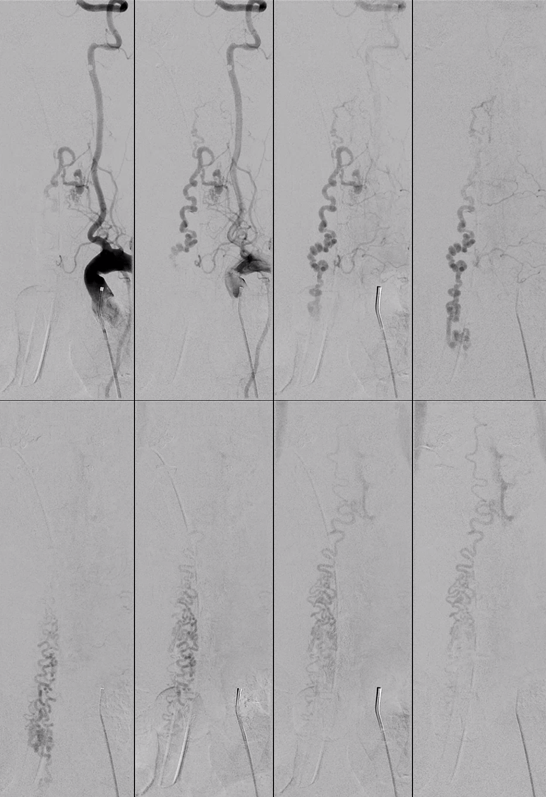
Embolization is highly effective when Scepter C is used to ensure proximal flow arrest. Pre-Onyx injection shows excellent probability of successful penetration into the vein
Injection of guide with Scepter C inflated outlines contribution from the other radicular arteries
Onyx cast shows excellent permeation of radicular supply as well as a cluster in the descending spinal vein at midline
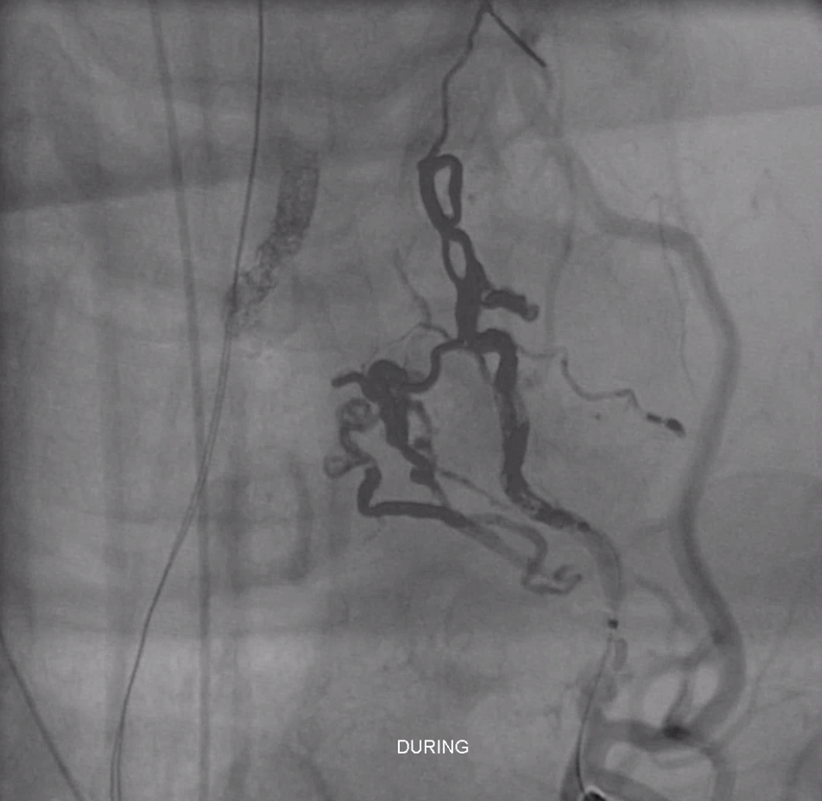
AVM seems dead
More Onyx is delivered

Looks great
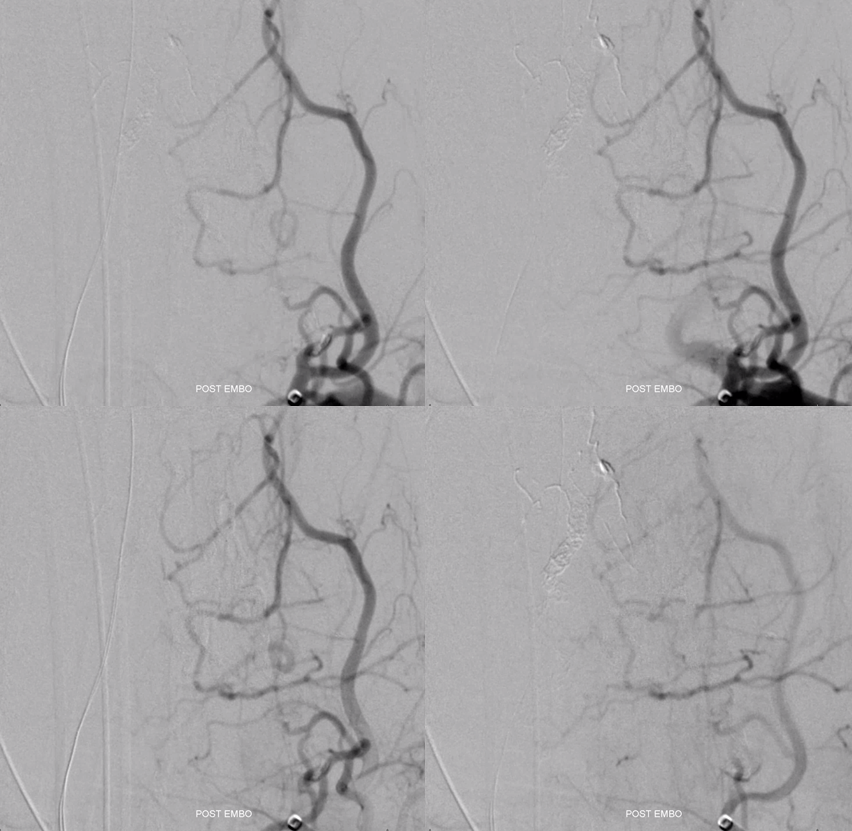
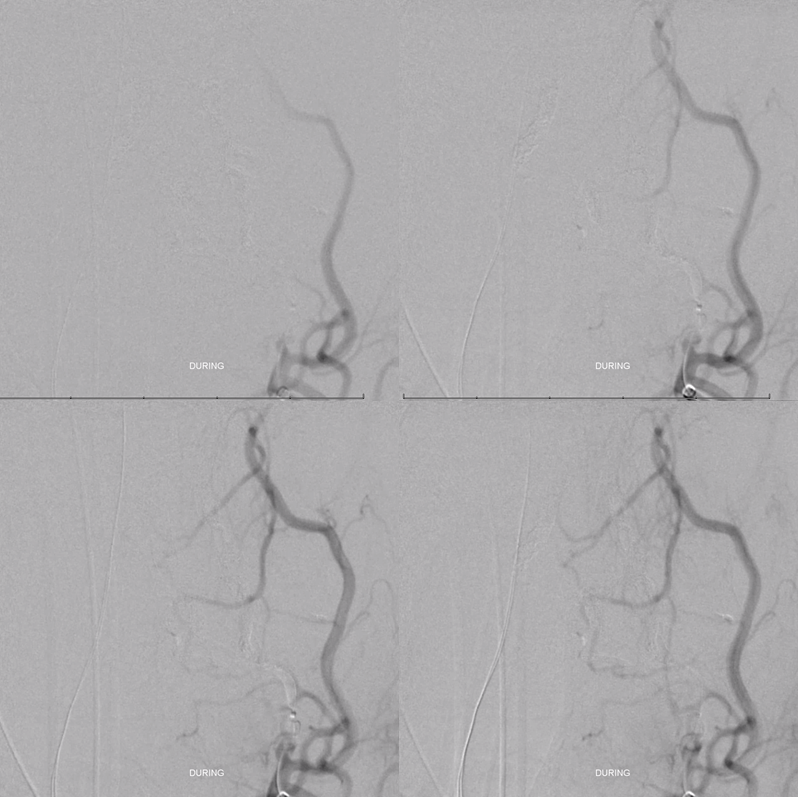
Post embo native view. Any concerns?
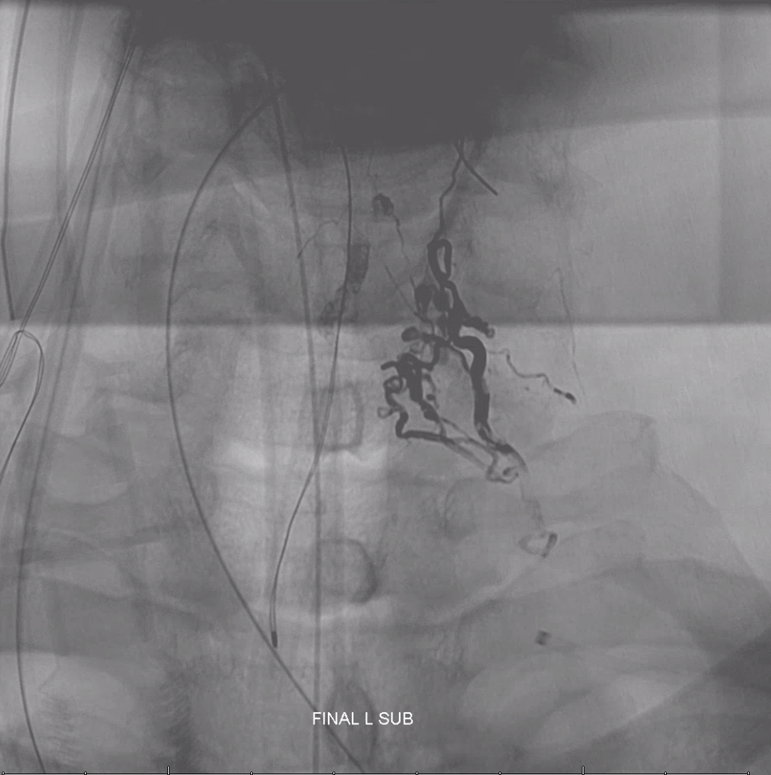
Notice Onyx material in location not visualized during any pre-embolization injections. Radiculomedullary arteries are white, anterior spinal is purple, and contralateral radiculomedullary is black. In the end, Onyx permeates the anterior spinal network. See Spinal Arterial Anatomy page for more anatomical details.
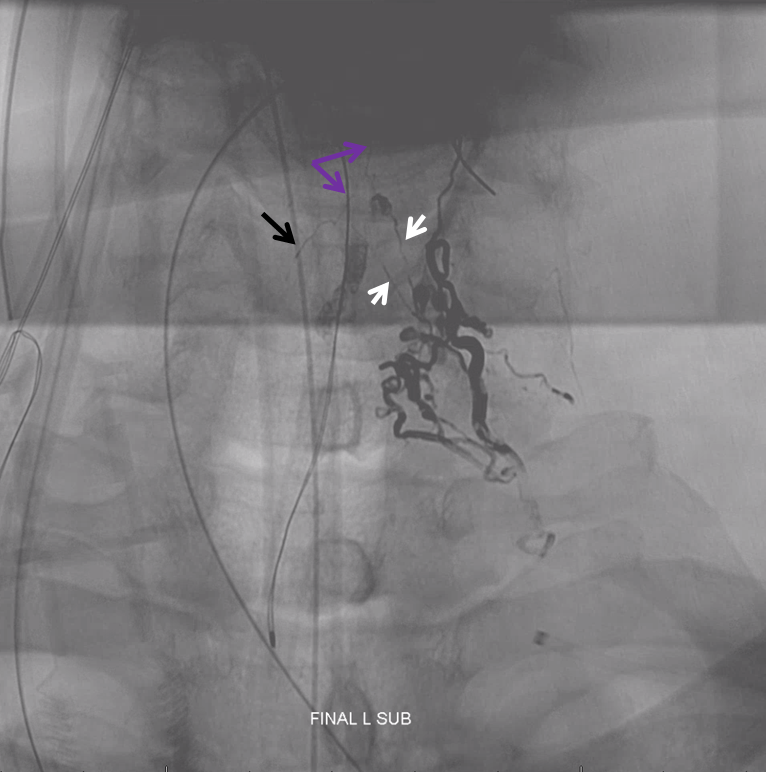
How does this happen?
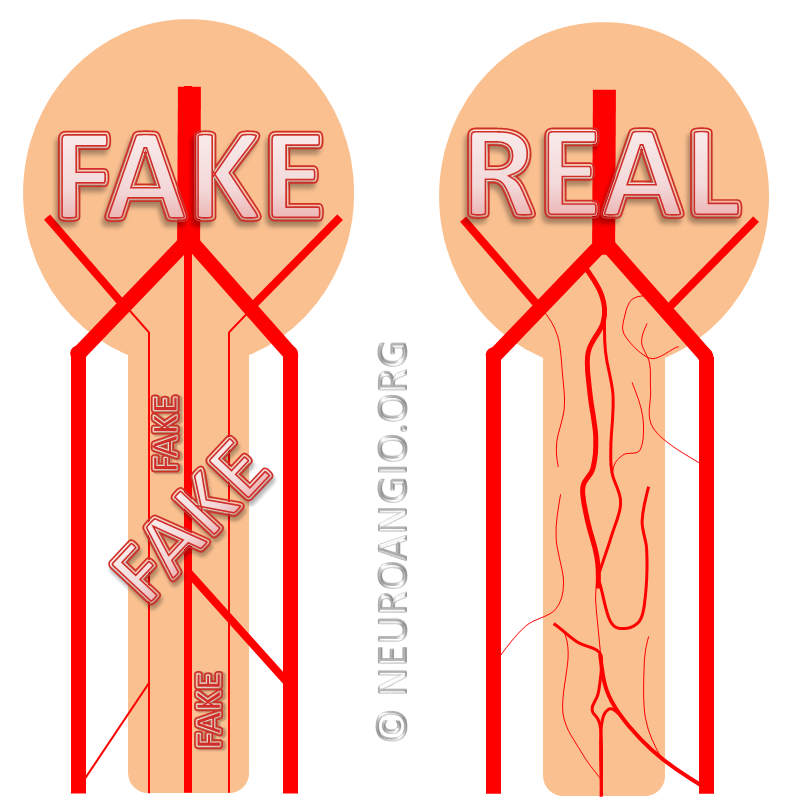
For several reasons. First, it is important to identify anterior spinal axis prior to any spinal treatment. Not all vessels were interrogated here — for example right thyrocervical, right deep cervical, right supreme intercostal, and left supreme intercostal. Perhaps spinal is coming from there. If not, one should be very suspicious that it is in fact arising from the same pedicle that supplies the AVM, and is not visible because of preferential contrast inflow towards the nidus. As the AVM is closed, possibility of anterior spinal penetration increases, as happens here. It is also important to know that, embryologically, small caliber connections between radicular arteries and anterior spinal system are very likely. We only call radiculomedullary those arteries we can see. Many are present but below angiographic resolution.
The patient emerges from anesthesia fully neurologically intact. Certainly, the Almighty can be Merciful. Unlike thoracic and lumbar spine, cervical cord arterial system can be much more distributive, with no major anterior spinal artery dominance and relatively well-developed posterior / lateral spinal arterial networks. For example, in up to 30% of normal spinal angiograms the anterior spinal artery is not fully demonstrated despite injections of all possible sources. Here, we happen to have had very good collaterals.
Here is a schematic, from our Spinal Arterial Anatomy page
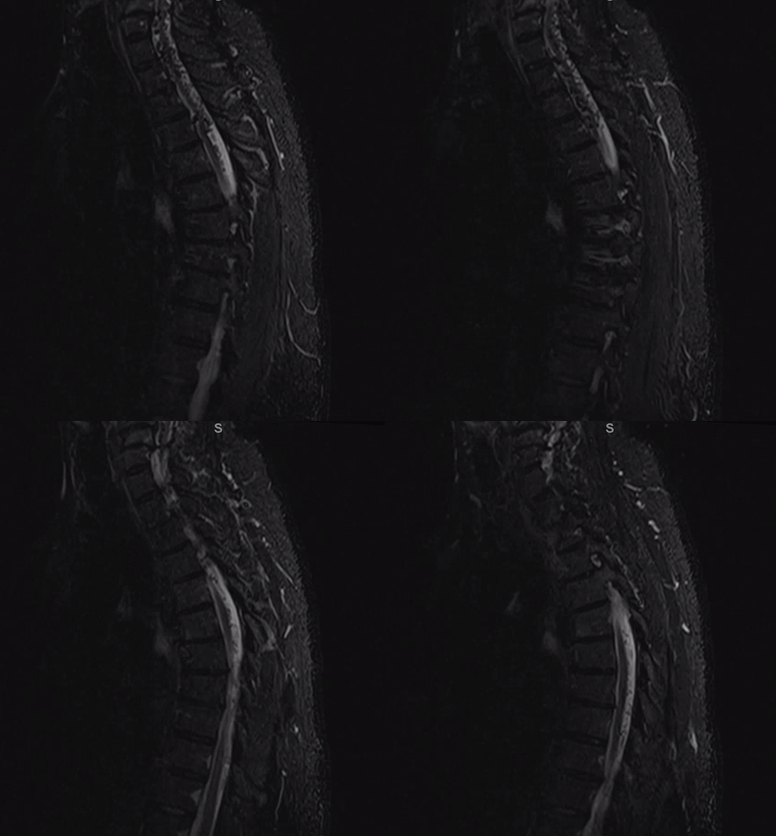
MRI day 1 post embolization already shows shrinkage of spinal veins, exposing impressive multifocal compression-related gliosis (white arrows)

Teaching points as above. See another case demonstrating extreme importance of pre-embolization identification of anterior spinal artery here
