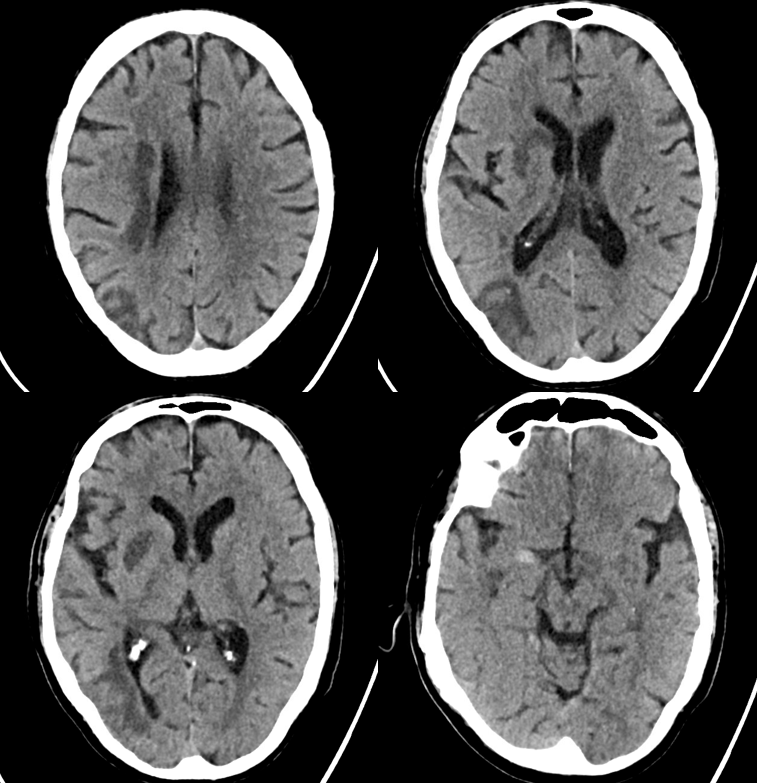
Increasing role for this kind of thing. Here is one example.
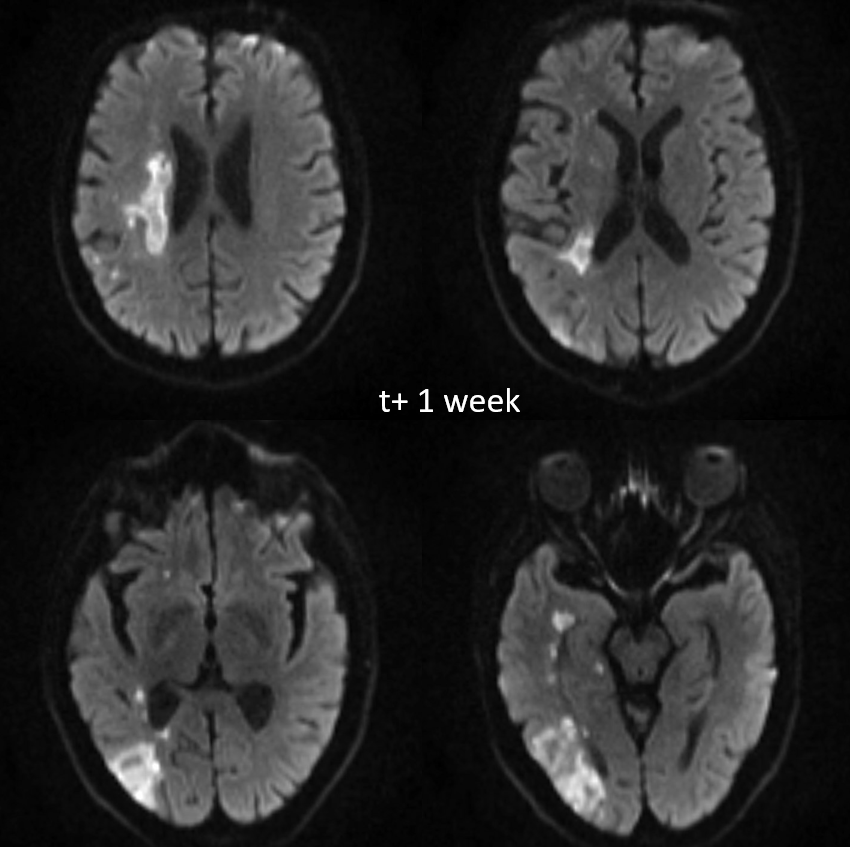
Progression of left-sided weakness over subsequent week
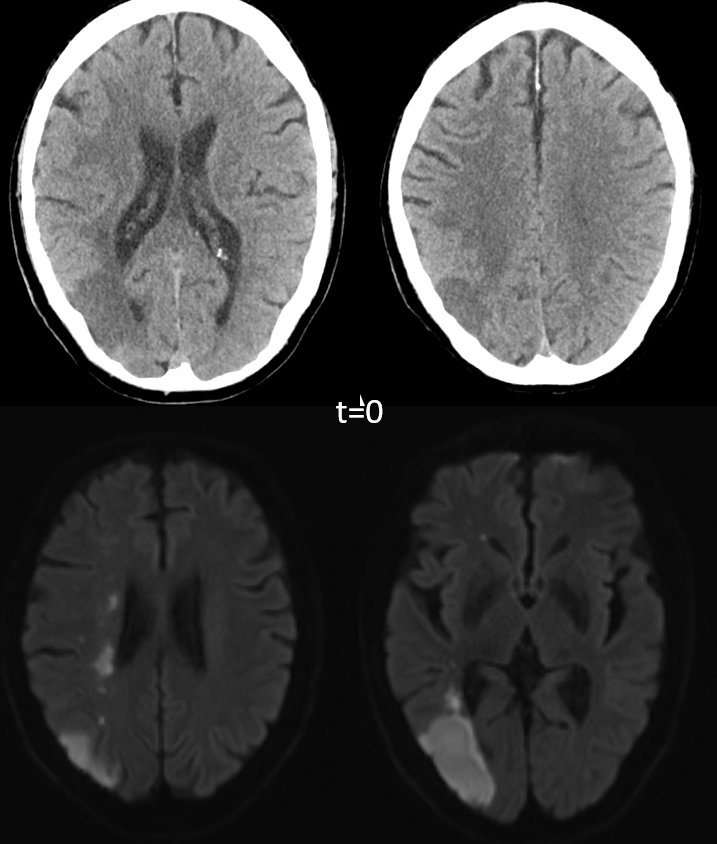
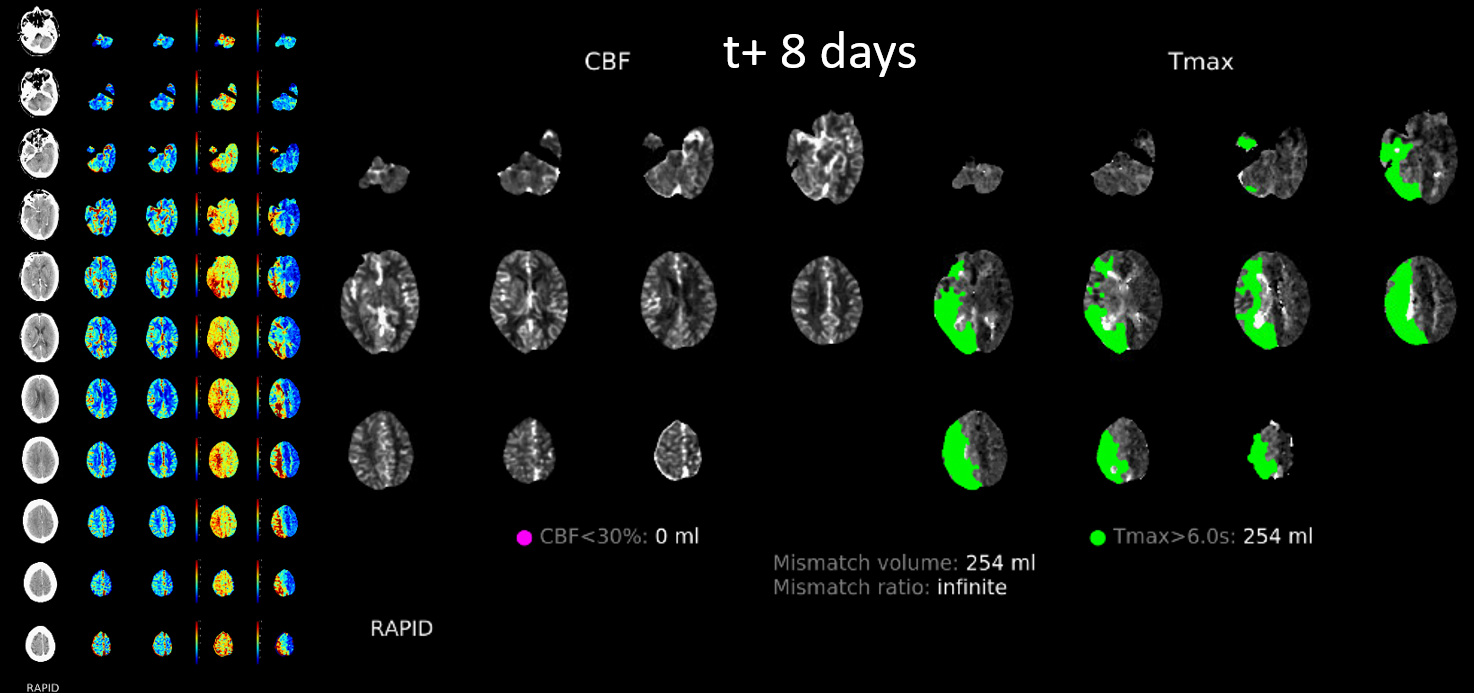
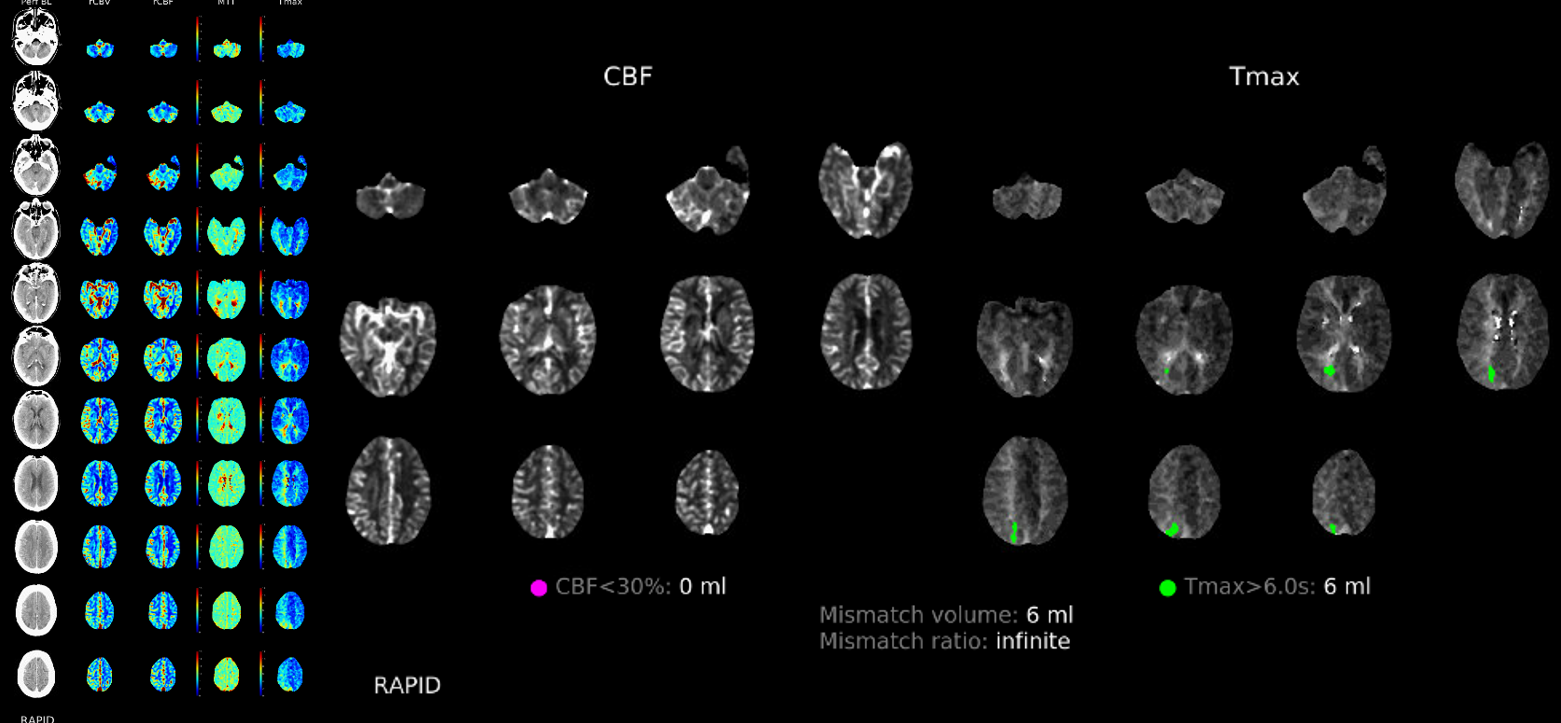
Now perfusion is done — very valuable, even without diamox, etc….
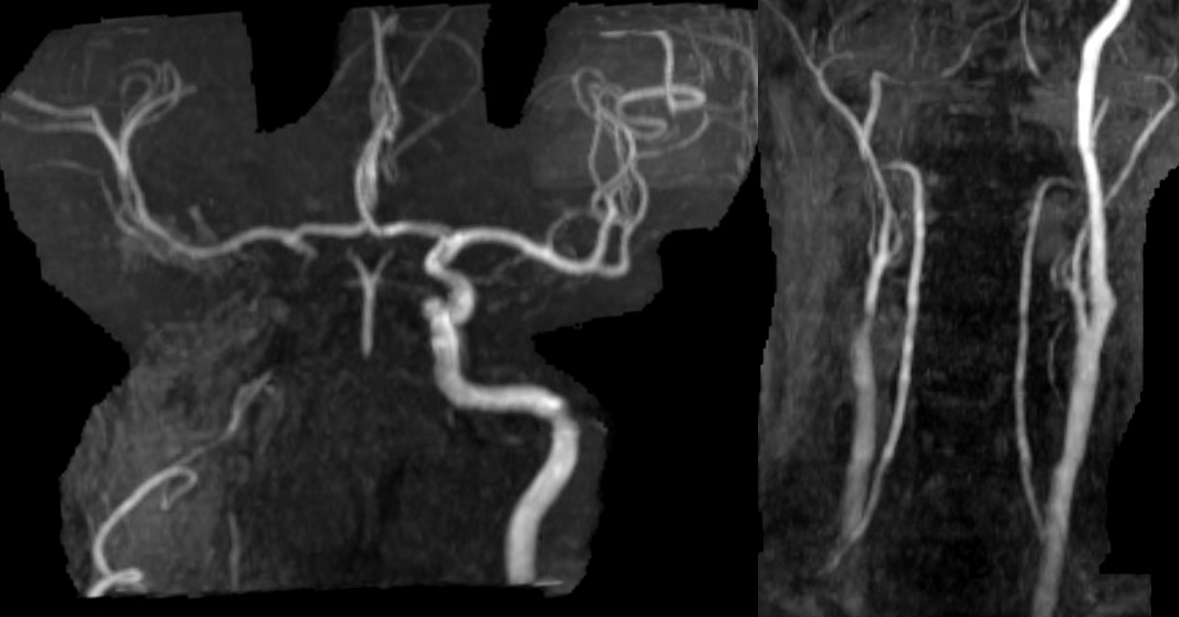
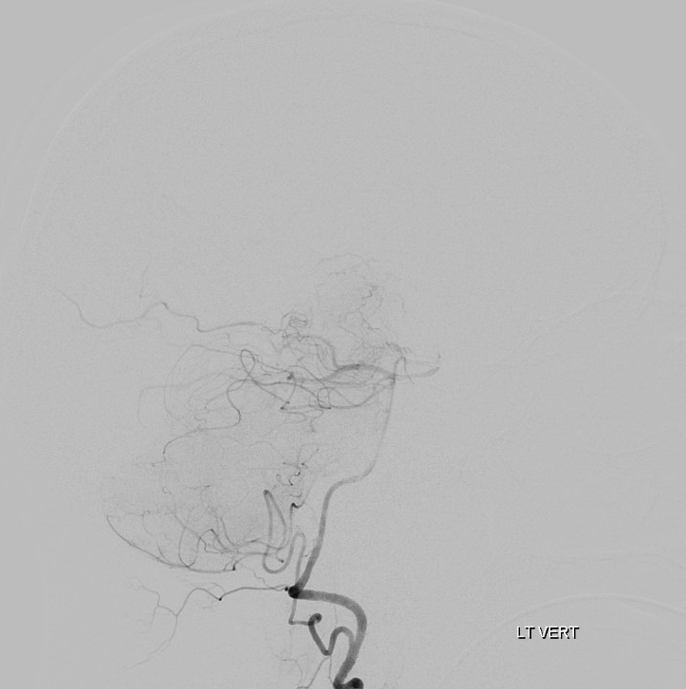
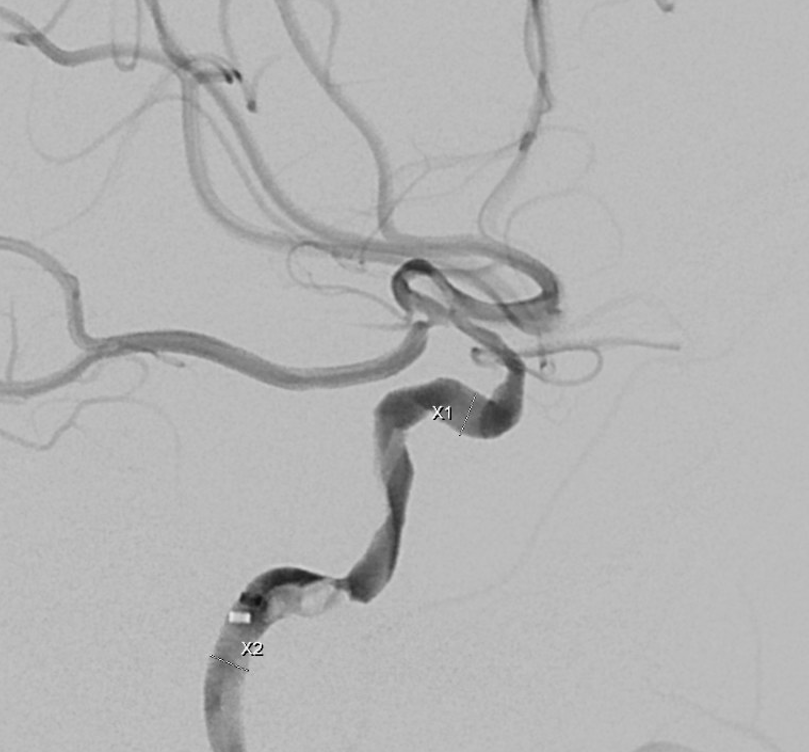
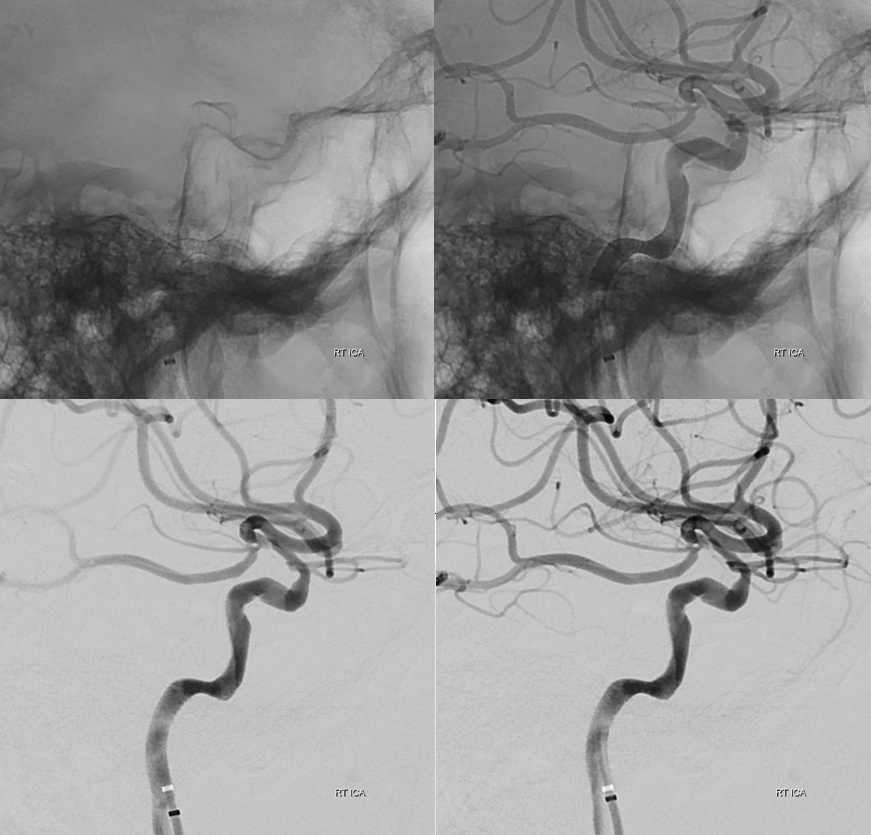
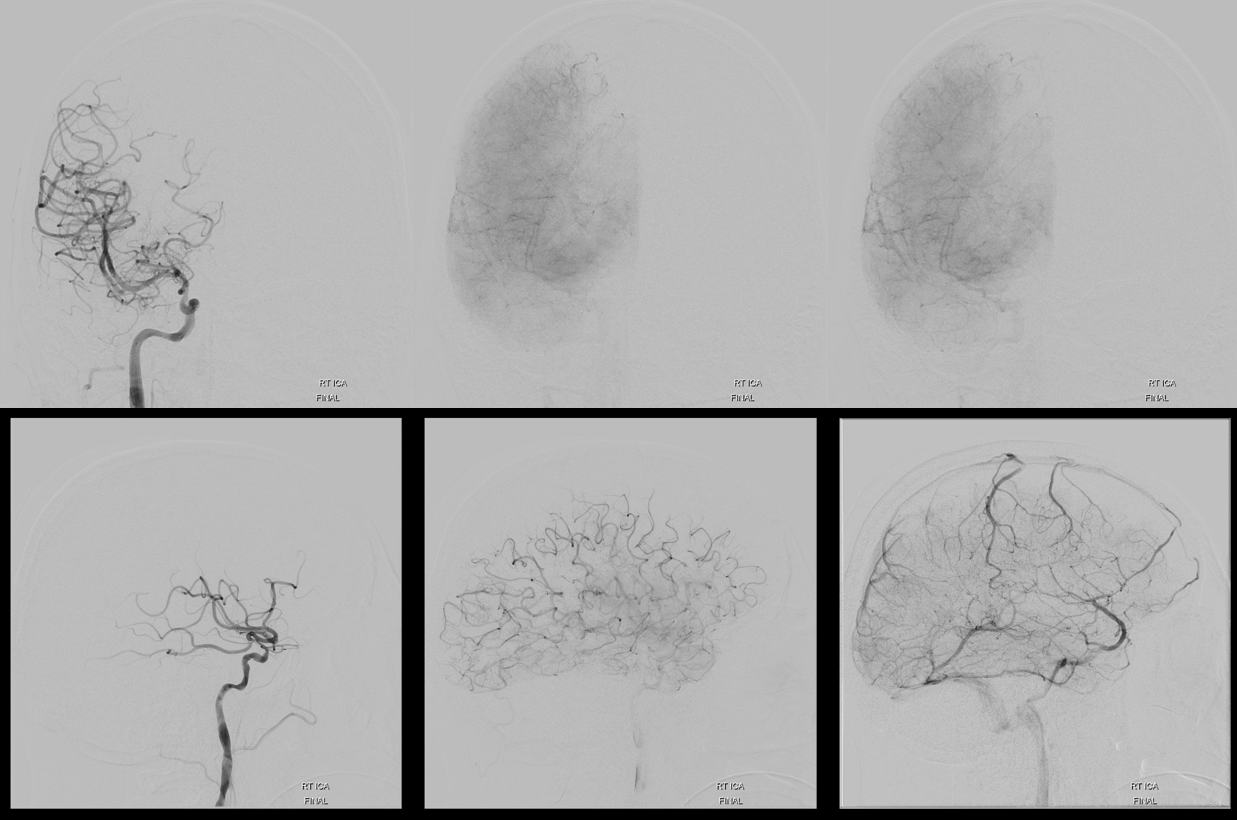
Extreme angiographic delay of right hemisphere. Fetal PCOM… Only slowly progressive occlusions can have this kind of delay without holohemispheric infarct
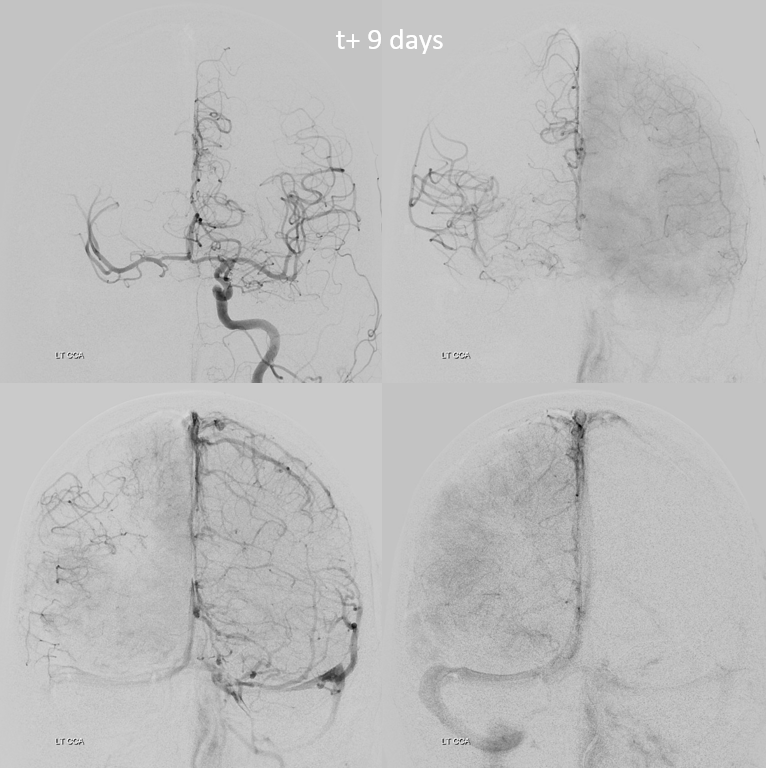
Tiny ACOM is carrying the week…

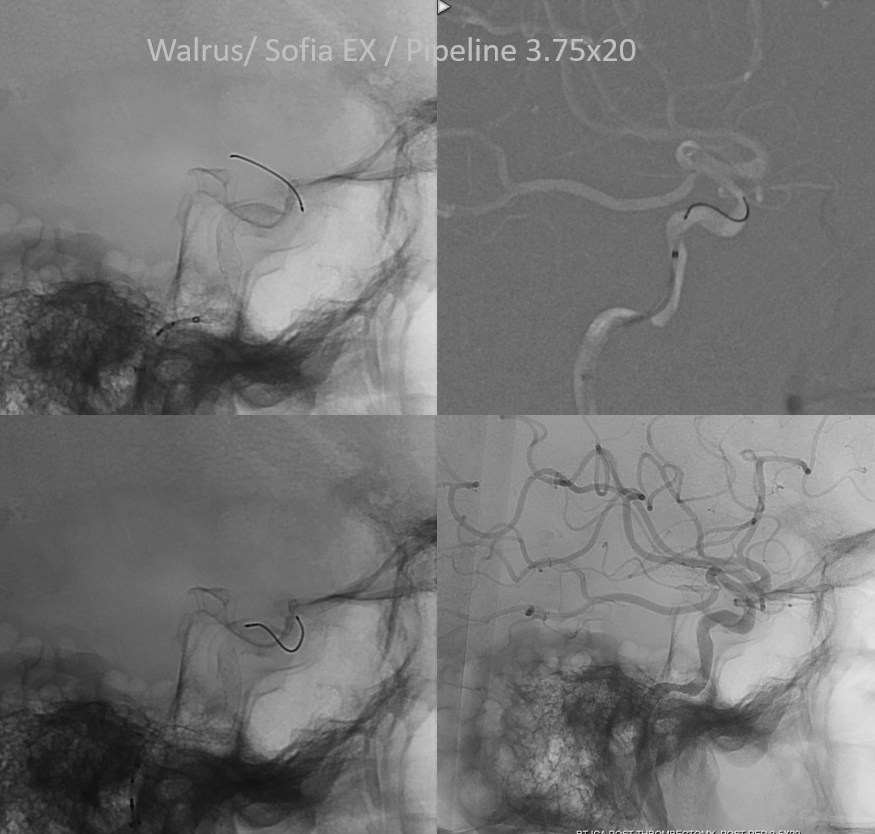
Important to have proximal flow arrest/ control to minimize distal embolus probability
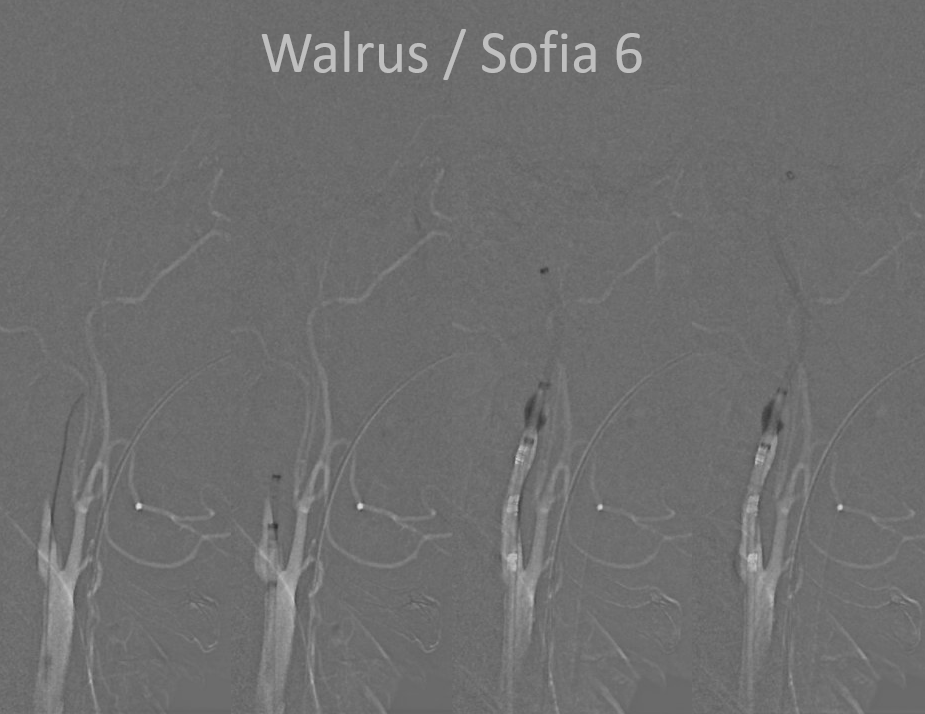
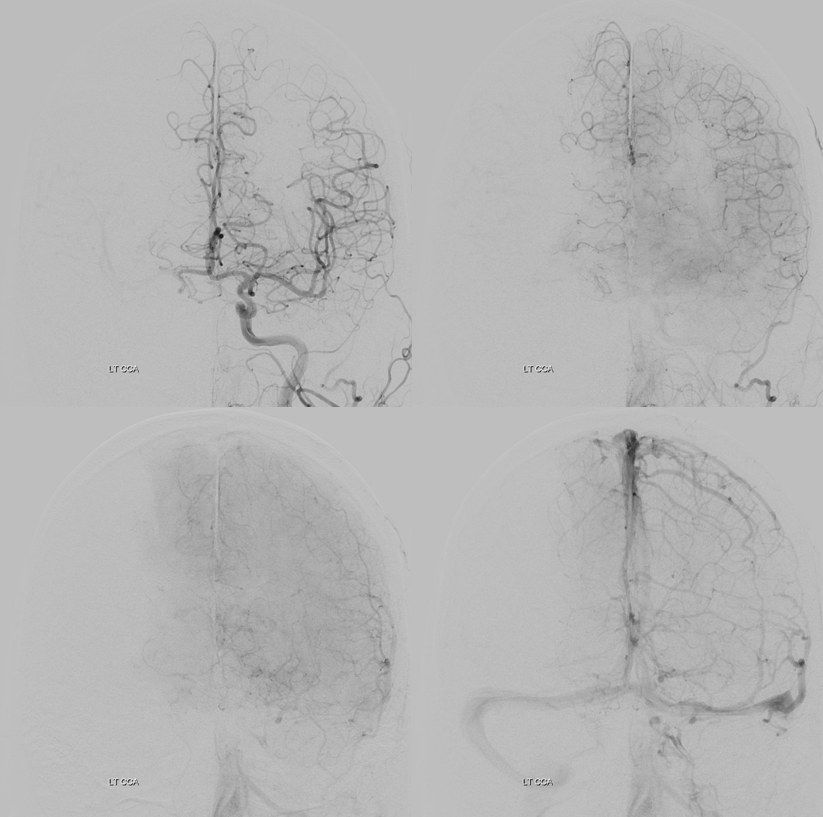
Bilateral access with left CCA roadmap ensures understanding of where wires/catheters need to go, especially in the intradural ICA. The occlusion seems to be at the proximal horizontal cavernous segment — wherever the Sofia stopped
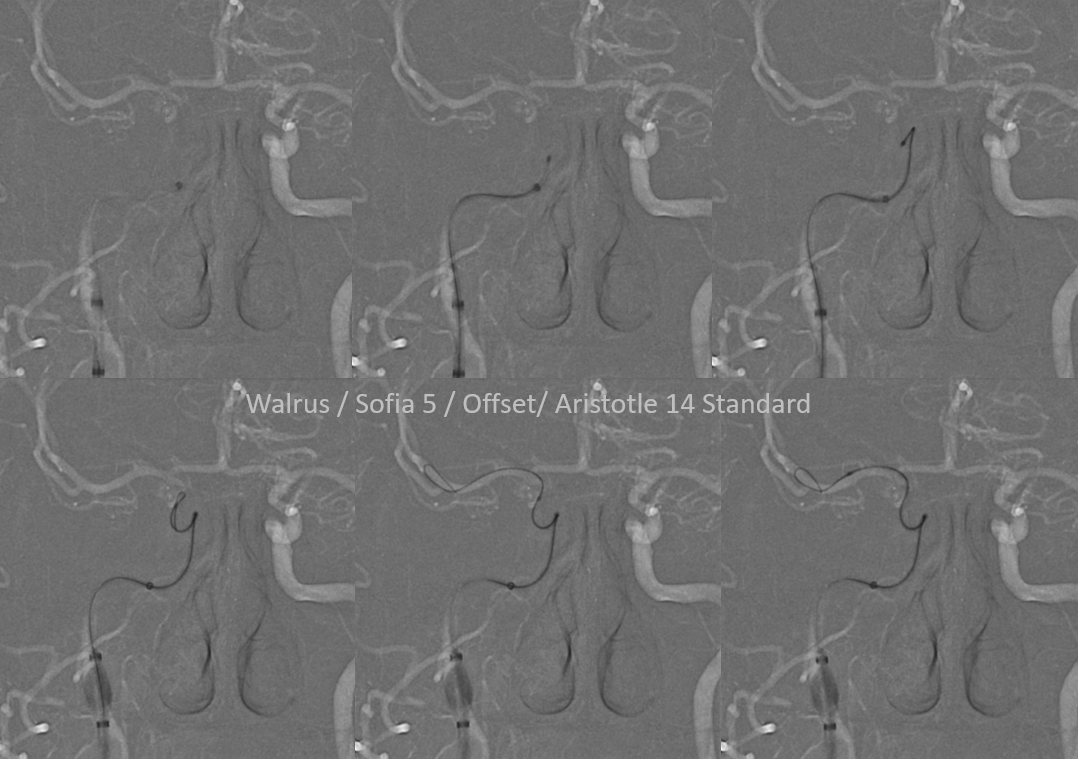
Lateral view is deceiving, since roadmap is of the left side…
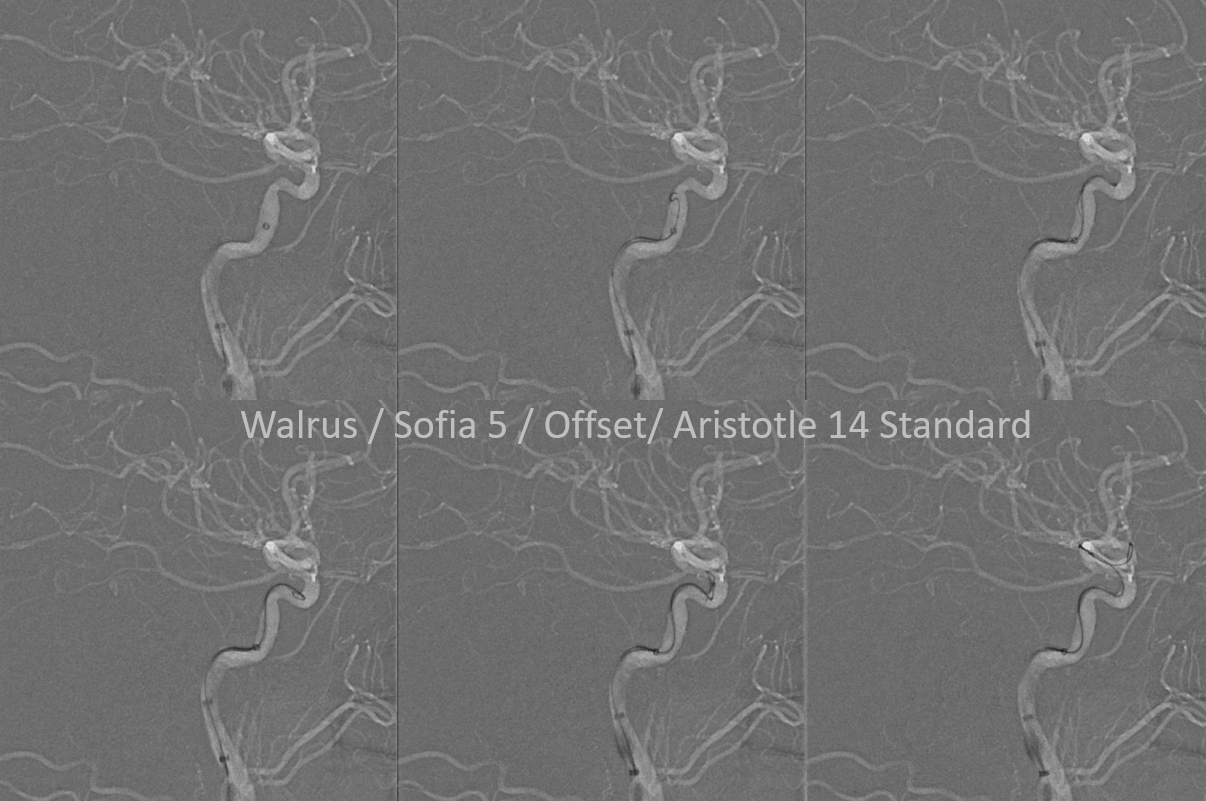
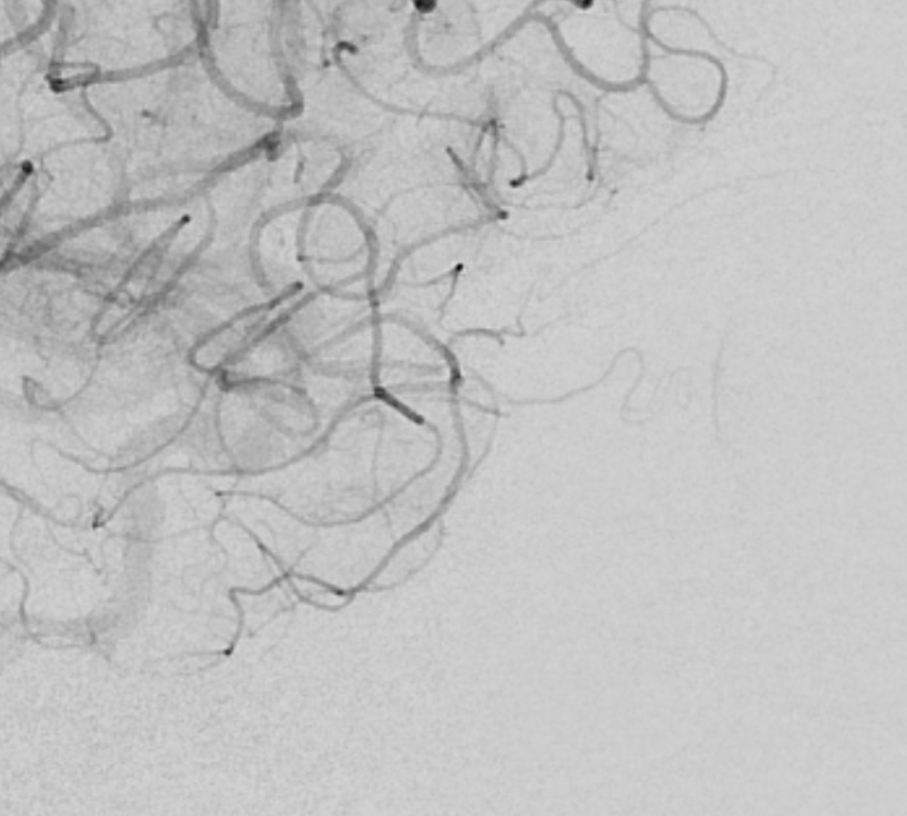
Flow restored, with lots of clot adherent to walls still…
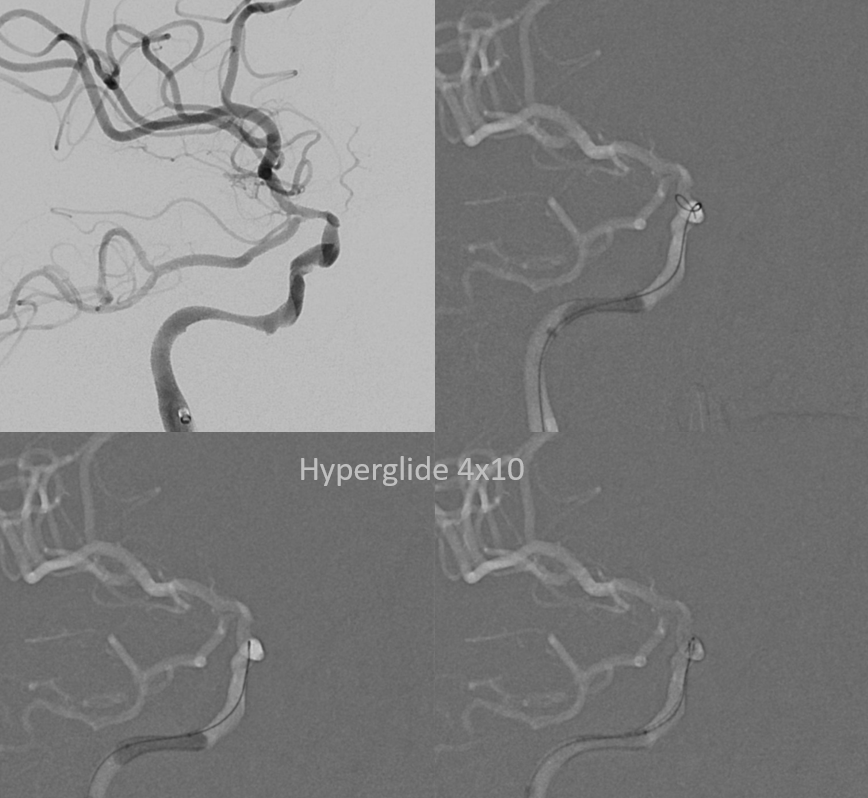
Can you recognize a cavernous segment dissection? Common occurence with delayed revascularization. As long as one is back into the right lumen intradurallly, its fine
Which stent to use? Can go with several balloon-mounted ones. Or single Pipe — good for keeping clot pinned to walls also
Compliant balloon angioplasty works somewhat — until it pops. No problem – just dont put any air in there
Not the whole dissection is covered by the Pipe — but its stable and still more flow there than in the diseased supraclinoid segment
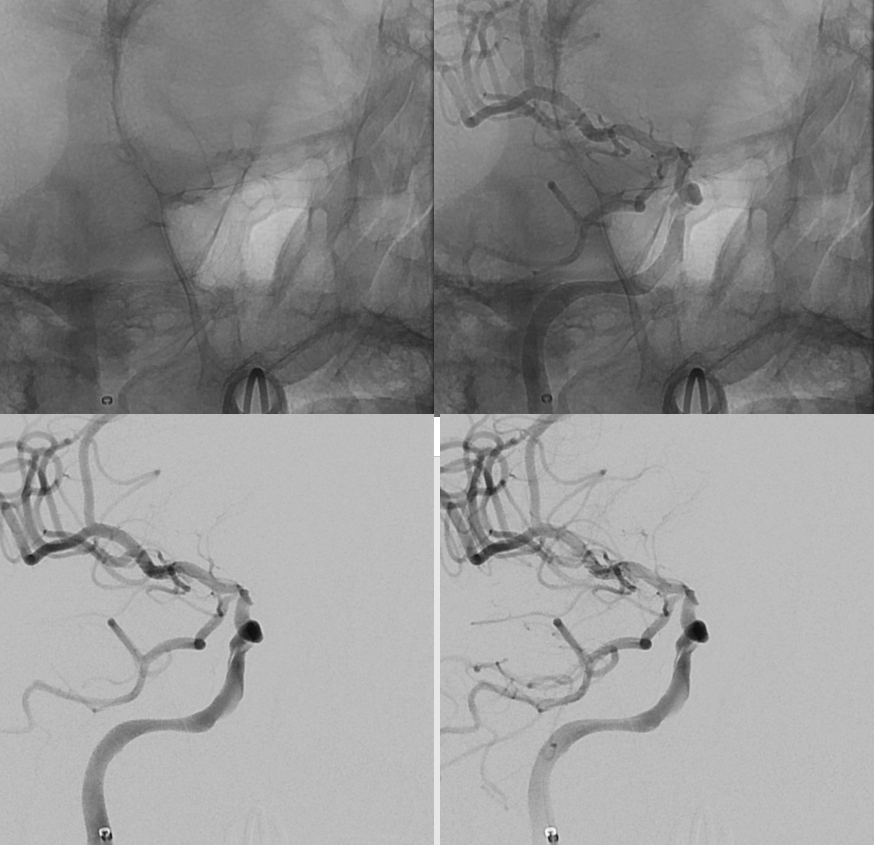
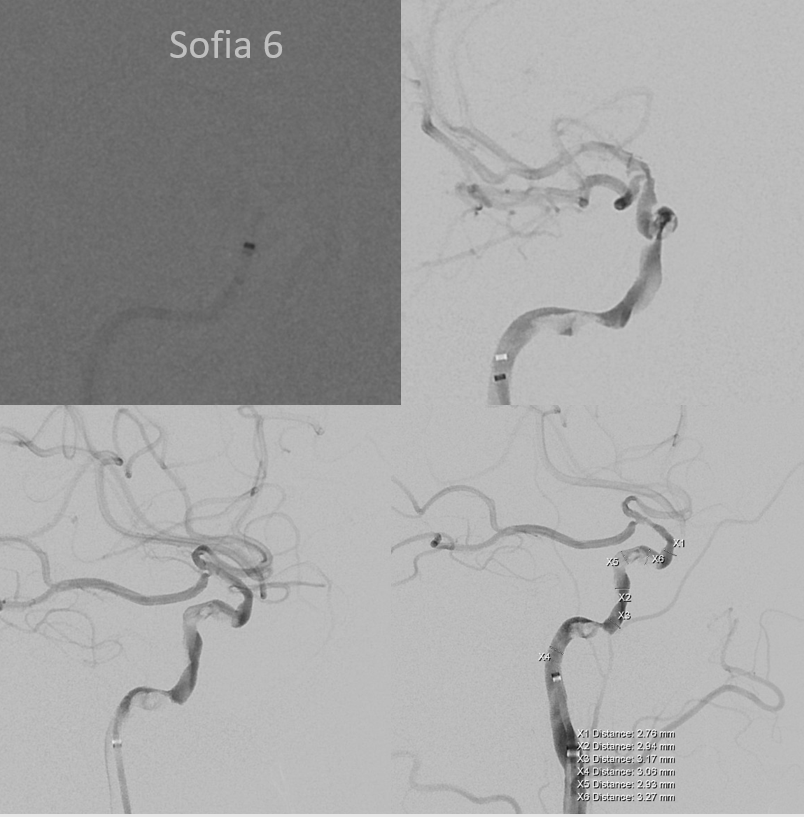
Note a very small branch to the globe. A short cilliary for sure, and maybe central retinal also. Part of the recanalization… And a bad thing, since retinal embolus is now a possibility.
Not perfect — there is residual moderate supraclinoid stenosis. Better is big enemy of good in these procedures. Much more flow now is antegrade — so leave alone now and not endanger the choroidal and fetal PCA with any silly thoughts of supraclinoid angioplasty or stenting
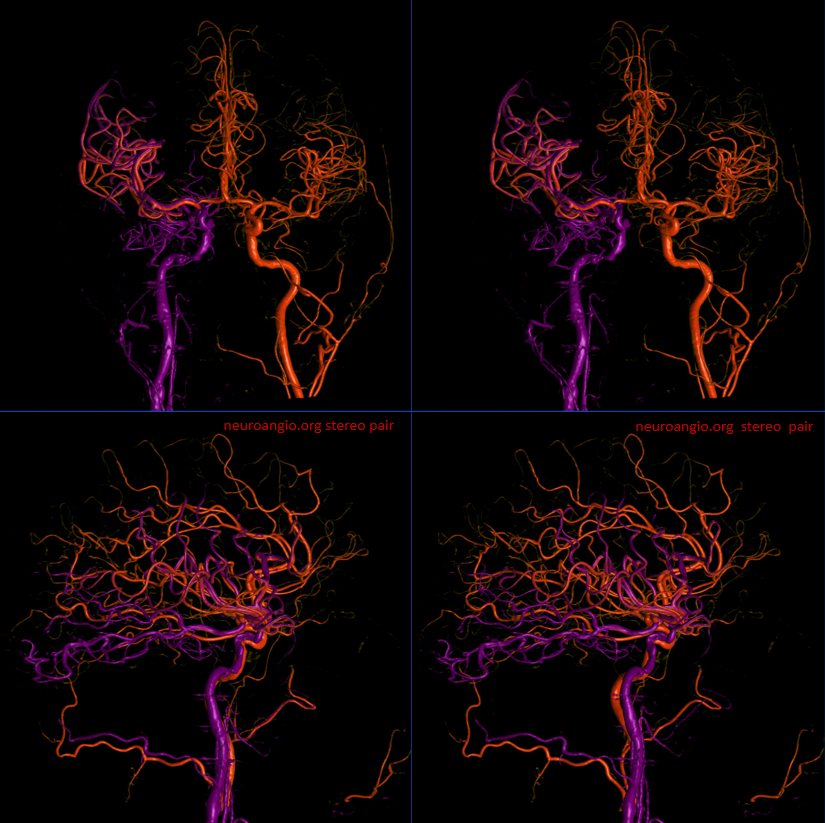
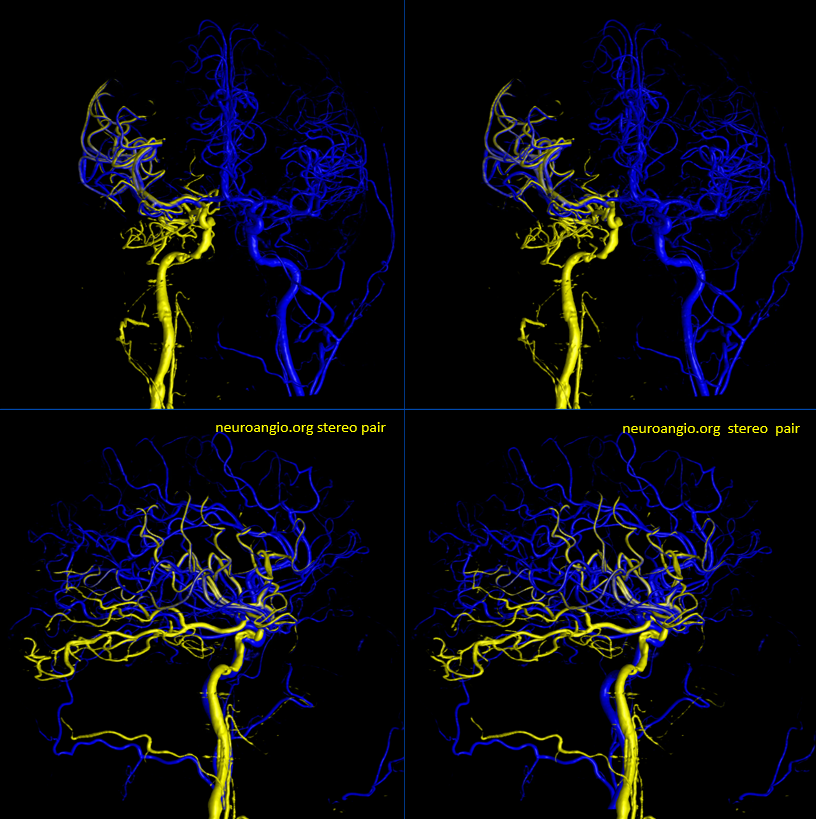
A 3D-DSA from the left before revasc, co-registered with 3D-DSA of the right ICA after revasc
Post Perfusion
Post CT