Dr. Huang and colleagues, particularly Dr. Hitoshi Fukusava, Dr. Tatsuhiko Ohta, and Dr. Toshio Okudera carried out seminal research on the topic of cerebral venous architecture. The venous system has historically taken a back seat to its arterial complement. Consequently many conditions which affect the venous system remained, and continue to be, less well understood than those of the arteries. The microarchitecture of the venous drainage was one such area; credit for advancing knowledge here goes to very large extent to Dr. Huang and his collaborators. Our current understanding of the DVA is a result of these insights.
The Medullary venous Malformation, now better known as the Developmental Venous Anomaly, or DVA, is seen in as many as 15% of brains on current generation MR scanners. It is a purely venous structure which drains normal brain parenchyma, and an incidental finding in vast majority of cases, with some rare exceptions.
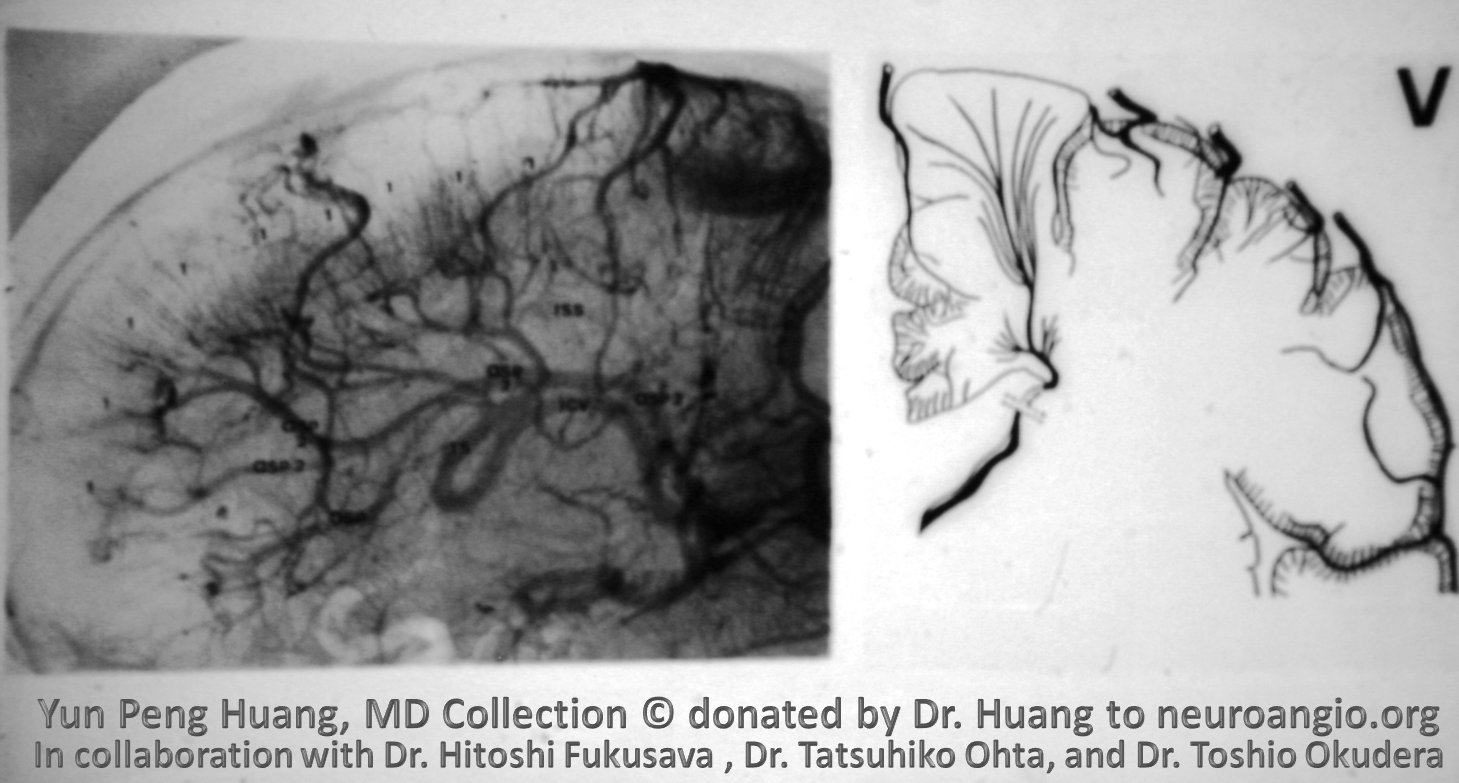
There is no consensus on how exactly DVAs form. Fundamentally, they seem to be aberrations in the “normal” balance between superficial and deep venous drainage systems, particularly involving the territory of the deep white matter. The superficial drainage apparatus consists of the extraparenchymal pial veins, cortical (subpial) veins, and superficial medullary veins located just underneath the cortex. The deep system includes subependymal veins and deep medullary veins which drain the bulk of white matter. Some anastomotic venous channels, known as transmedullary veins, traverse the entire distance between pial and ependymal veins. They appear to be more common in the embryonic stages, and their density seems to decrease with increasing thickness of the hemispheric parenchyma. The superficial and deep medullary territories represent, if you will, the watershed zone between the pial and ependymal collectors. When the balance of drainage is shifted towards either one, the vein or veins collecting the larger than “normal” territory is enlarged. This venous collector is the Medullary Venous Malformation of Y.P. Huang, with its name reflecting the nature and location of the malformation. The term Developmental Venous Anomaly presumes existence of some form of intrauterine event, resulting in anomalous development – one proposition was microthrombosis of either deep or superficial venous apparatus, requiring the other one to assume control of the at-risk territory. This intriguing hypothesis has not been proven.
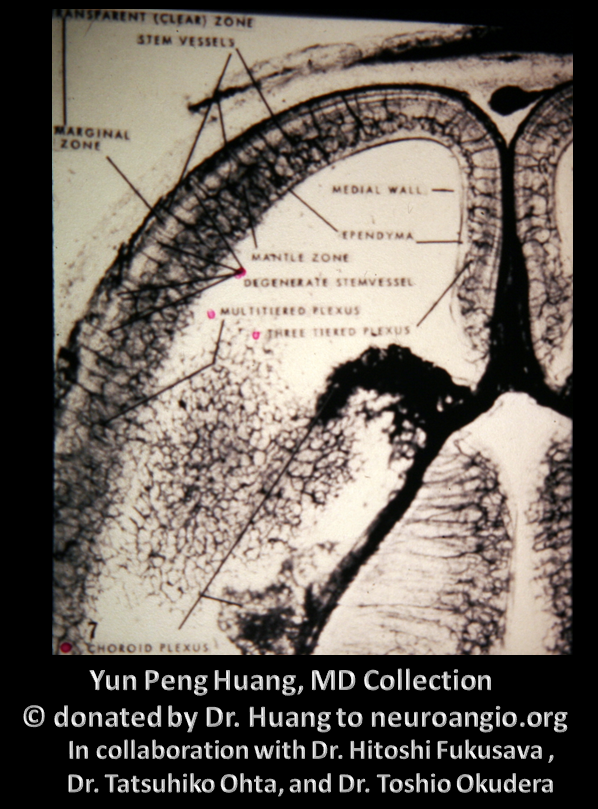
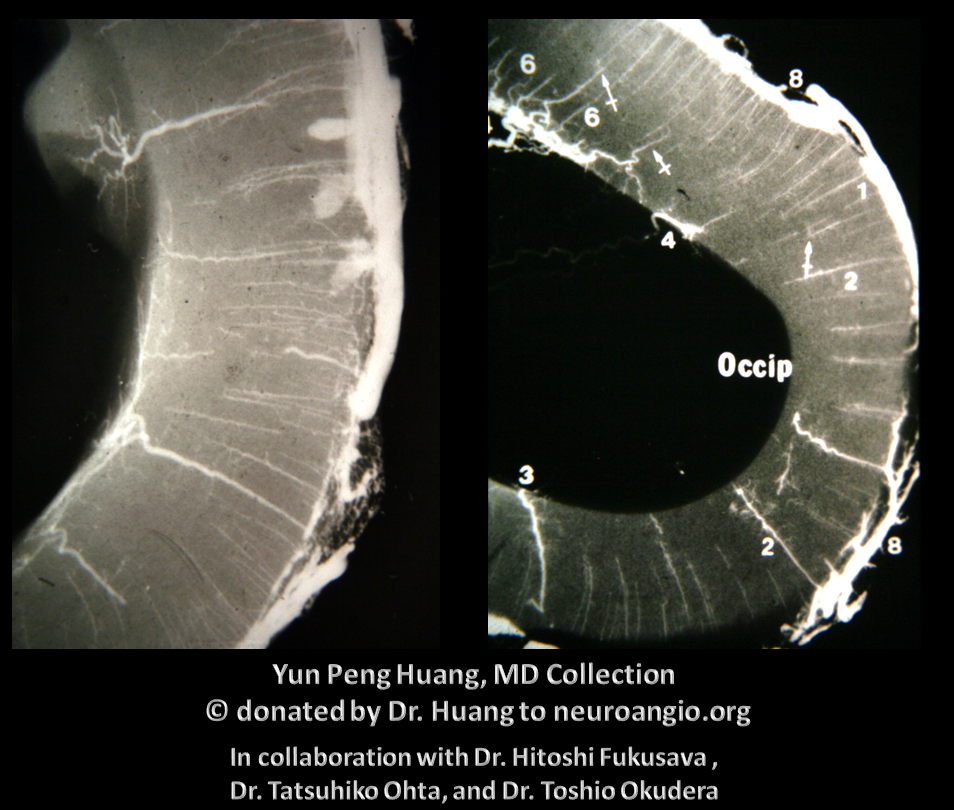
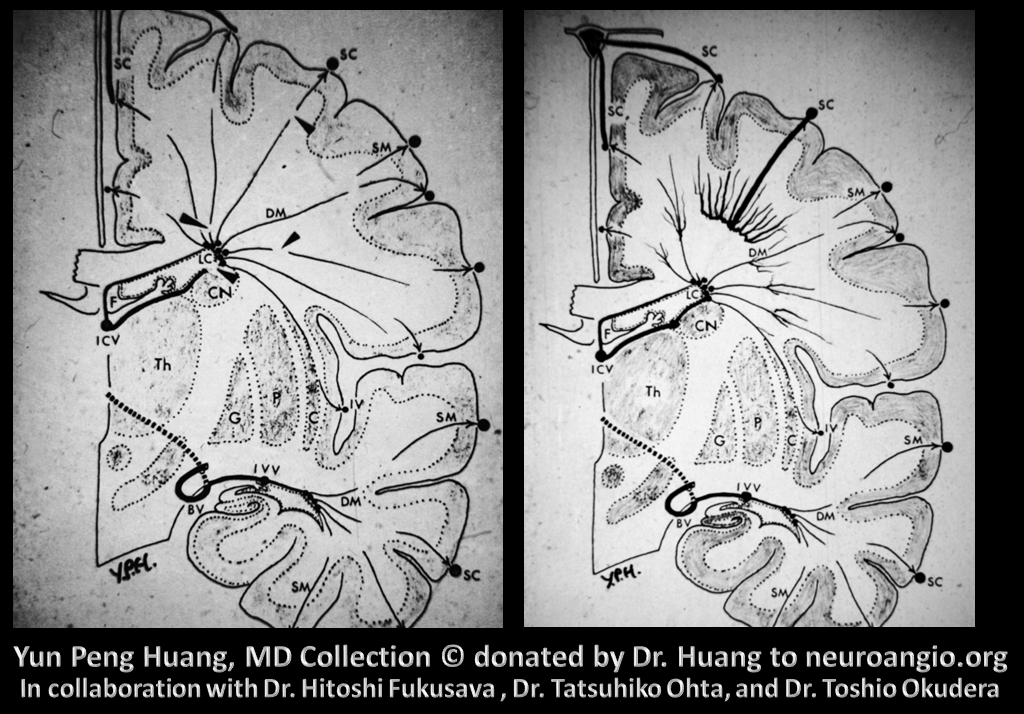
Venous drainage of cerebral mantle consists of superficial and deep veins
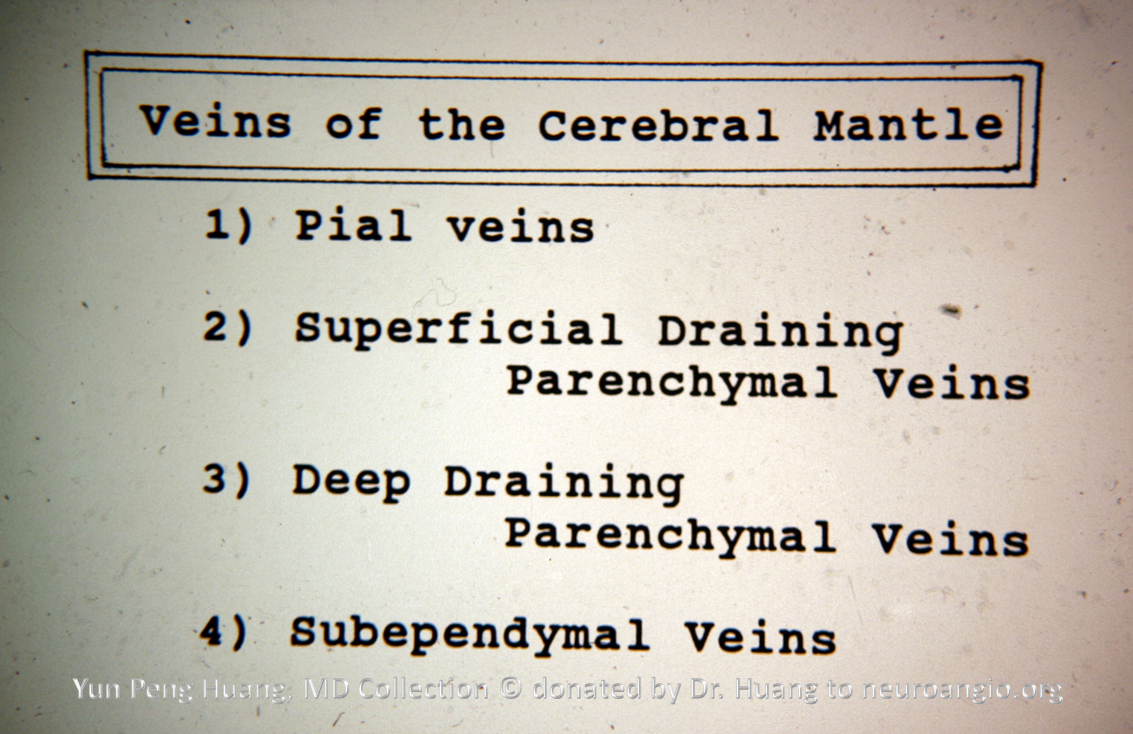
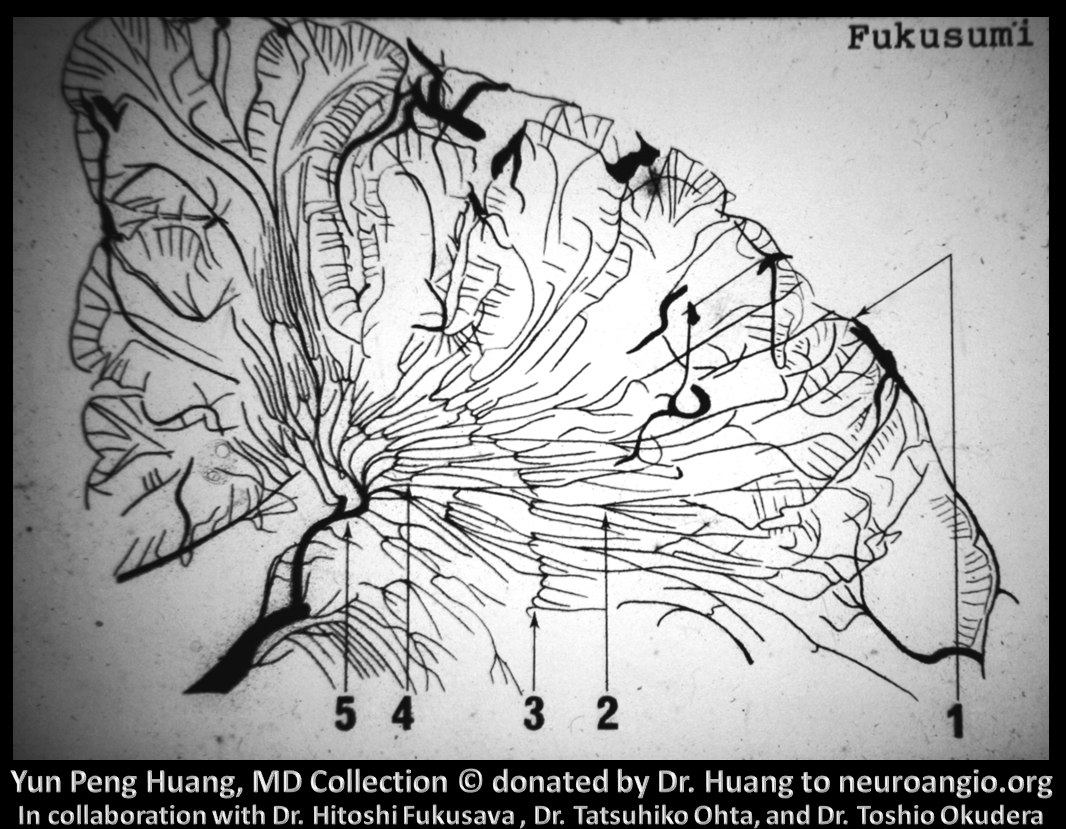
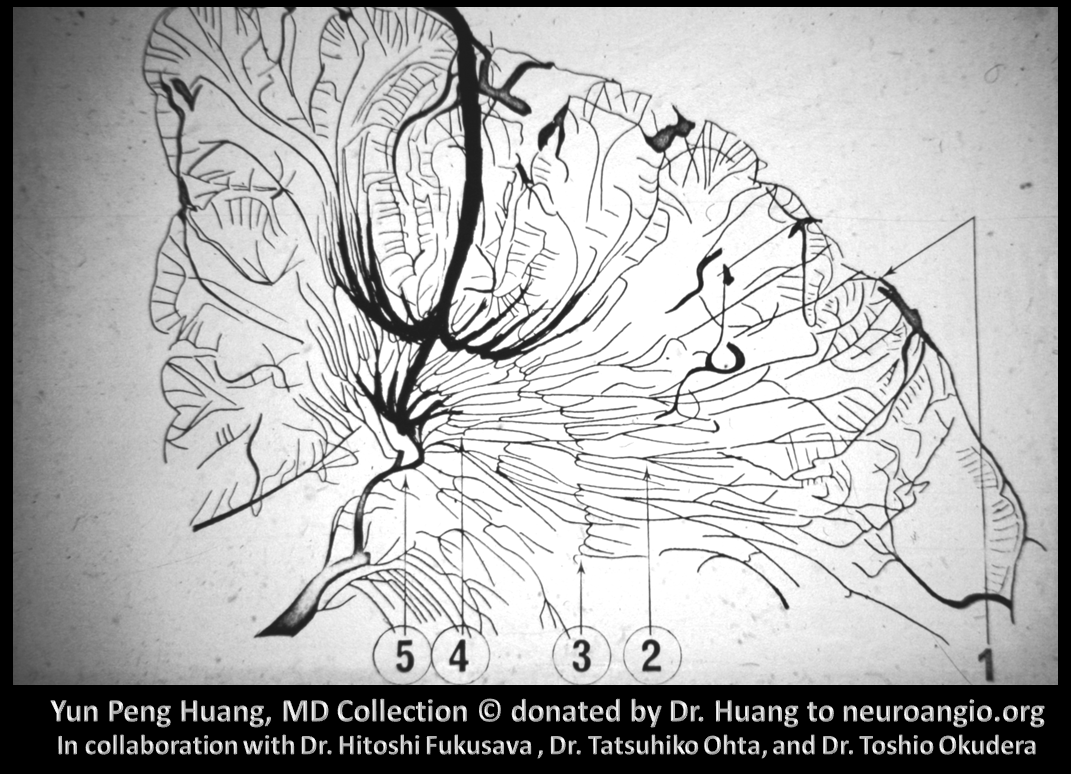
The deep draining veins (deep medullary veins in slide below) were further subdivided into for “Zones of convergence”. This subdivision, in my view, has clear anatomical validity; it is however not presently taught and has been effectively forgotten
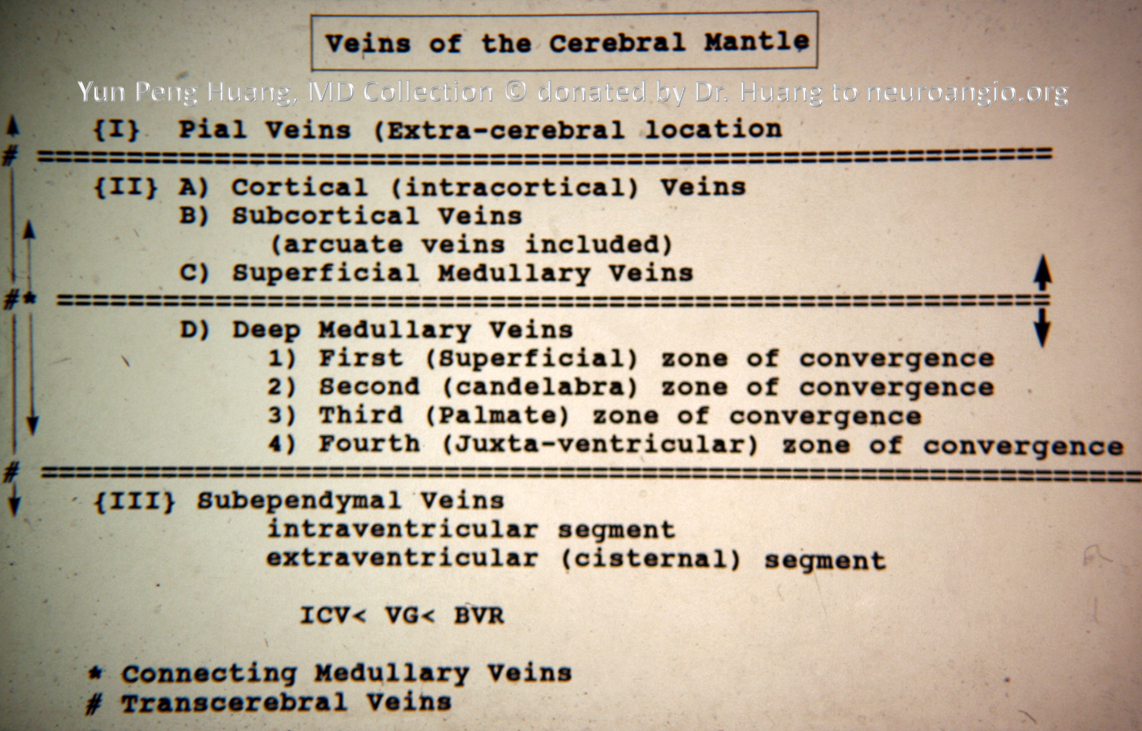
Another slide of the same concept
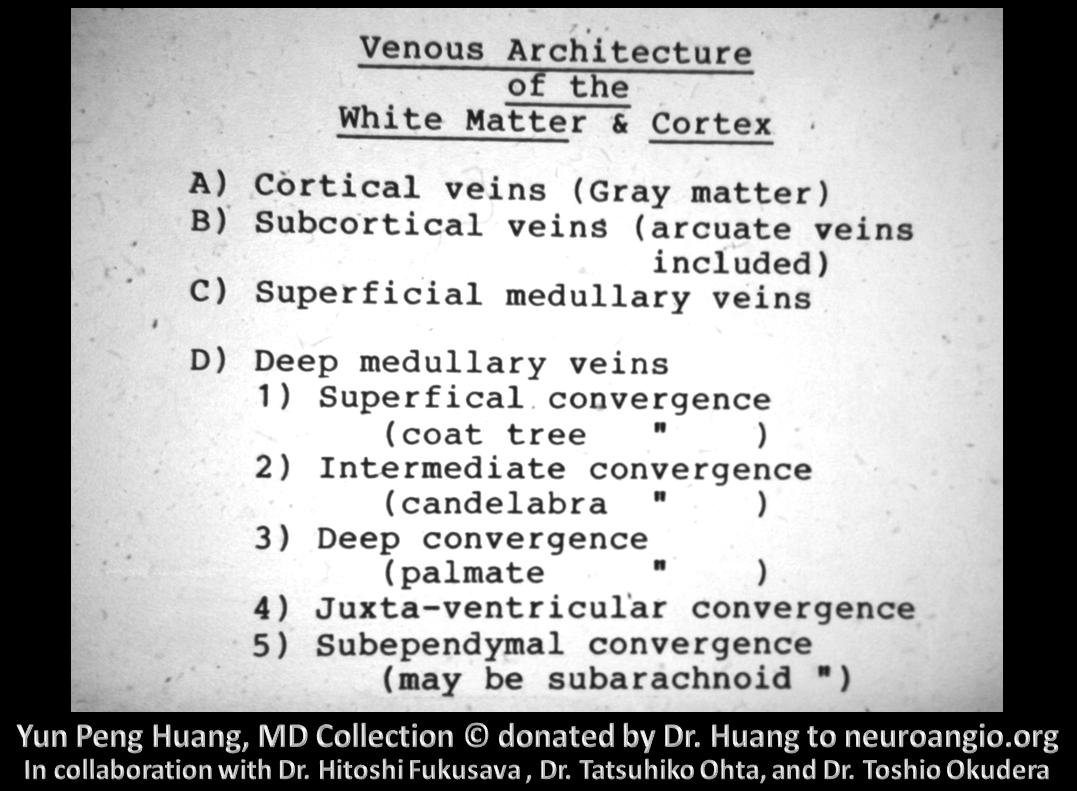
In the following image, the numbers correspond to those of the preceding slide.
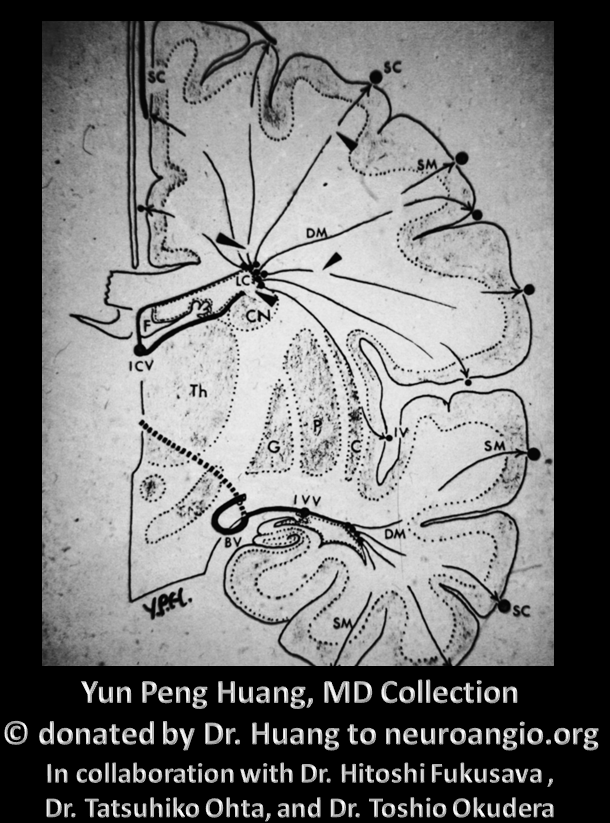
In this picture, DM = deep medullary veins, SM = superficial medullary veins. SC probably refers to surface cortical.
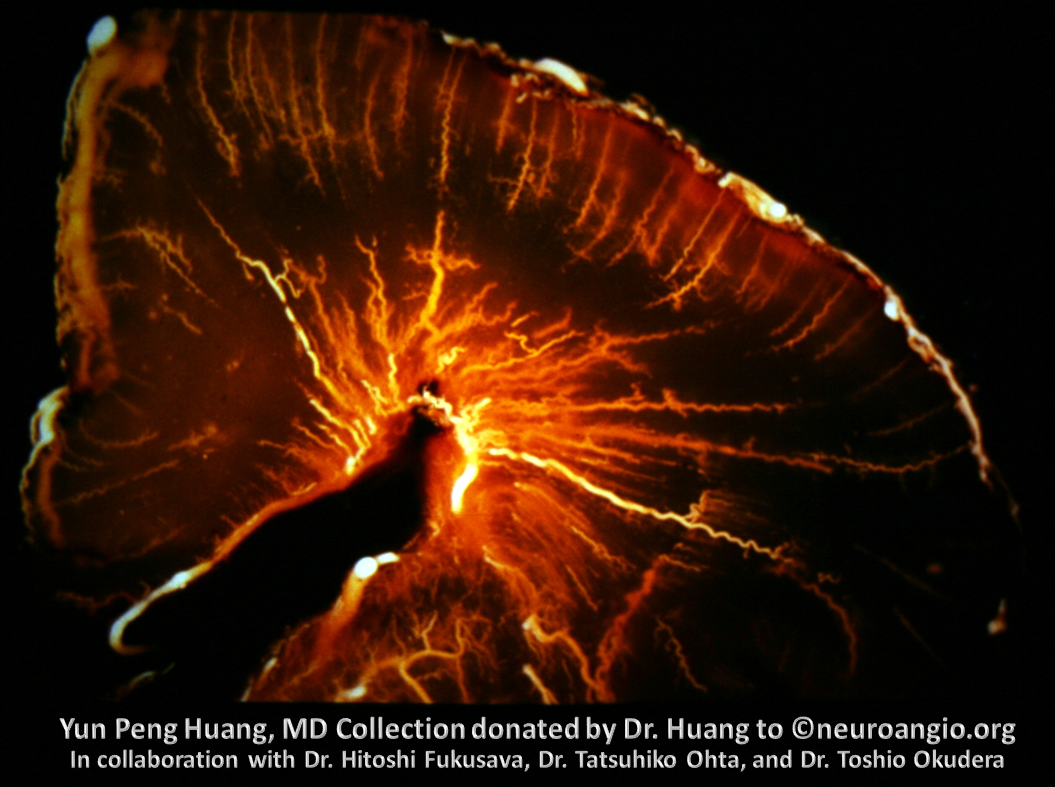
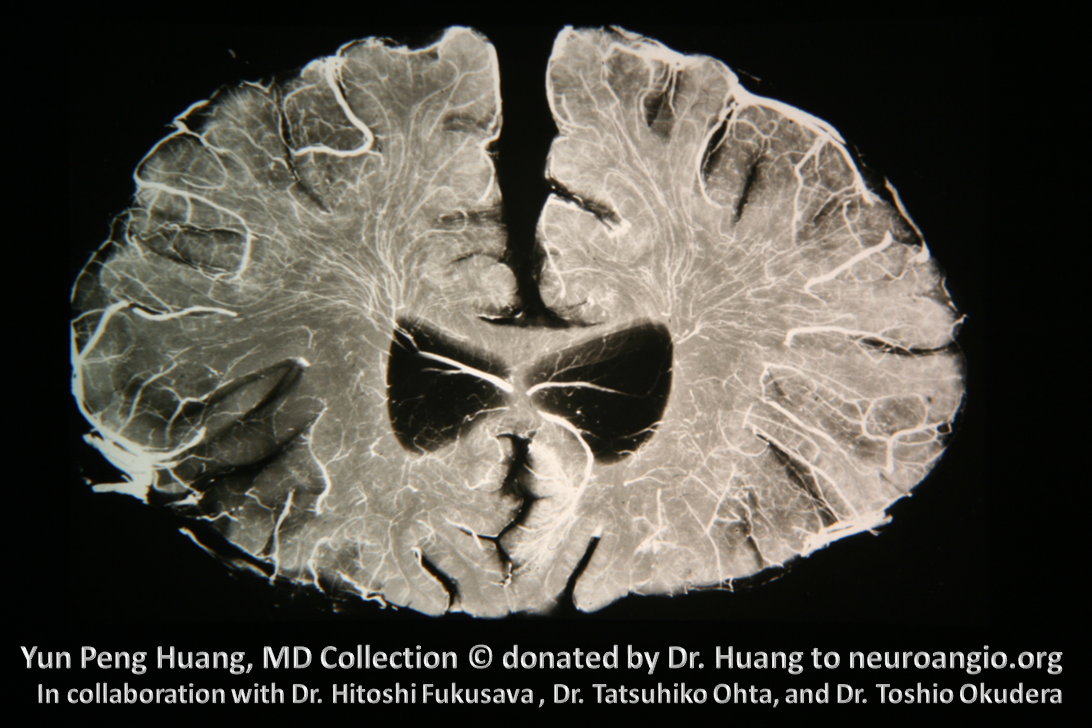
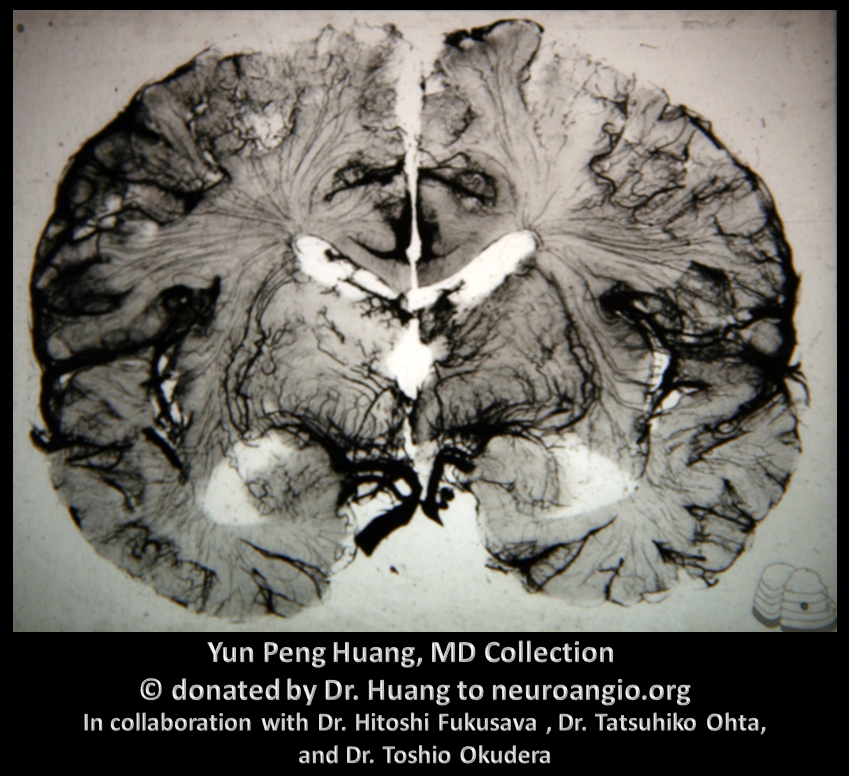
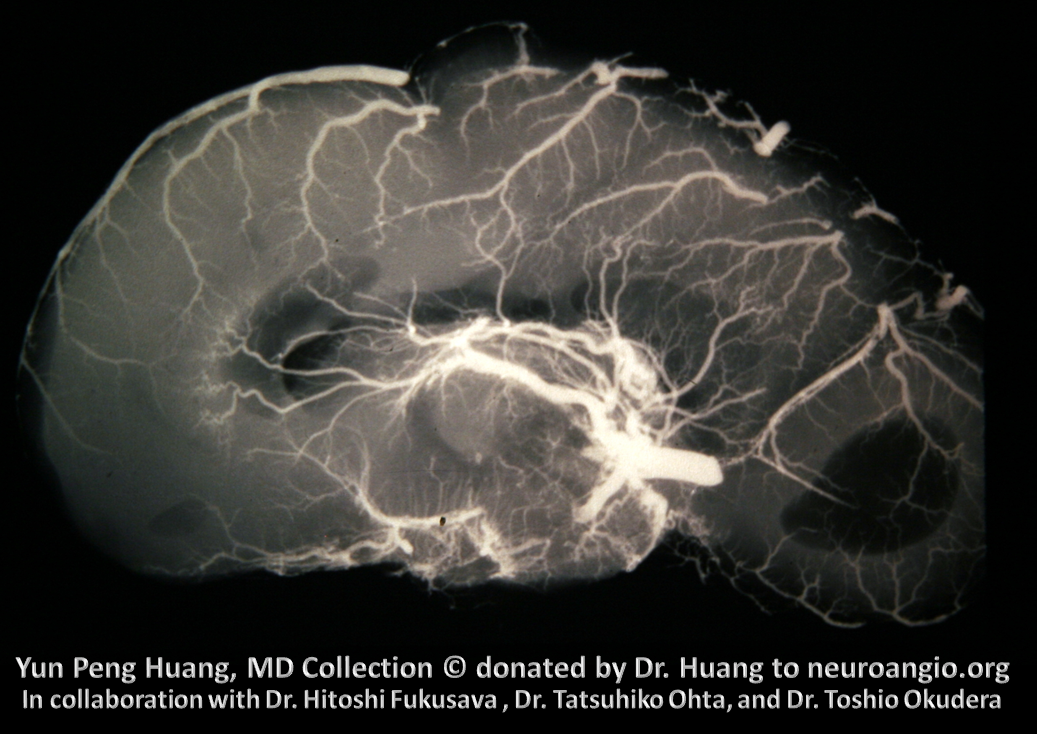
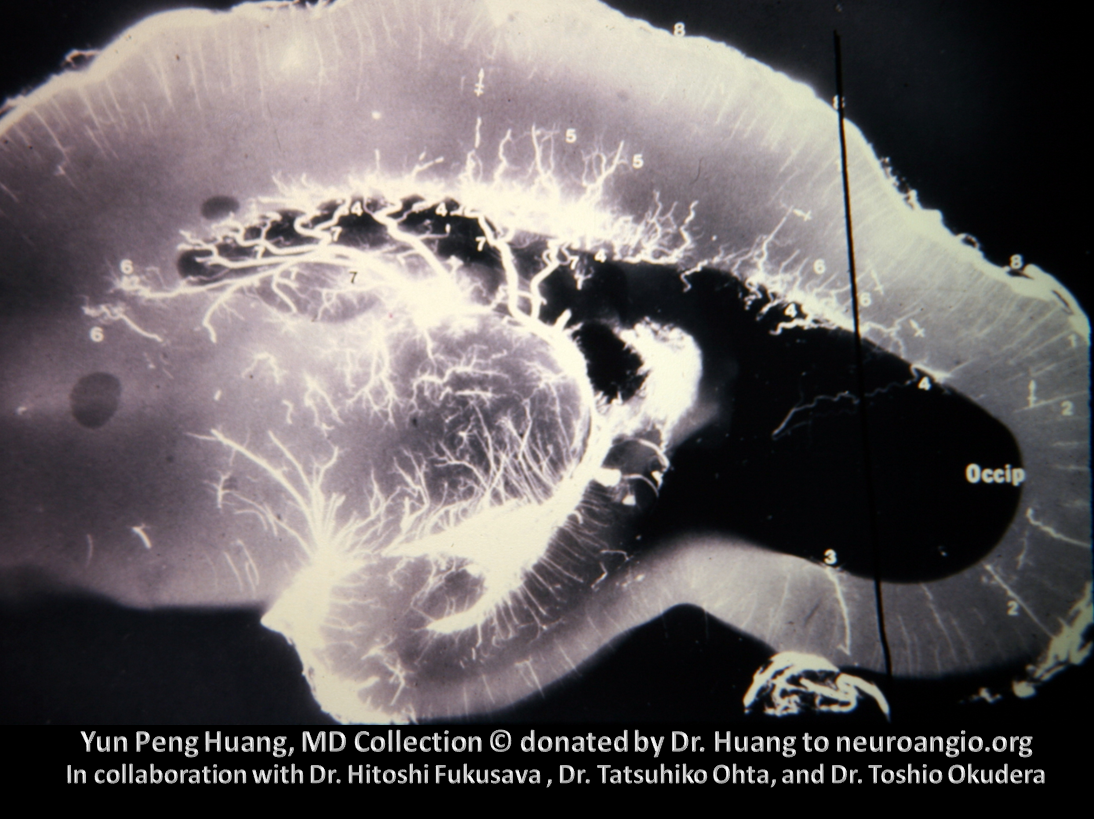
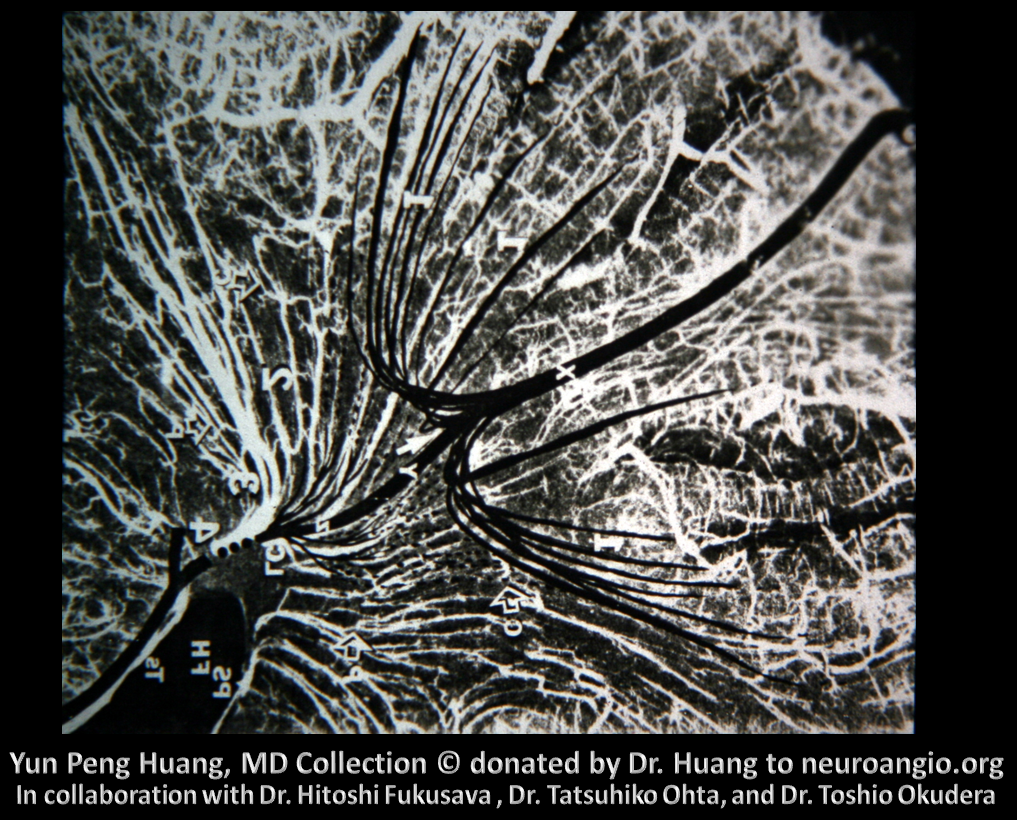
An x-ray of injected coronal section specimen exquisitely shows this venous apparatus
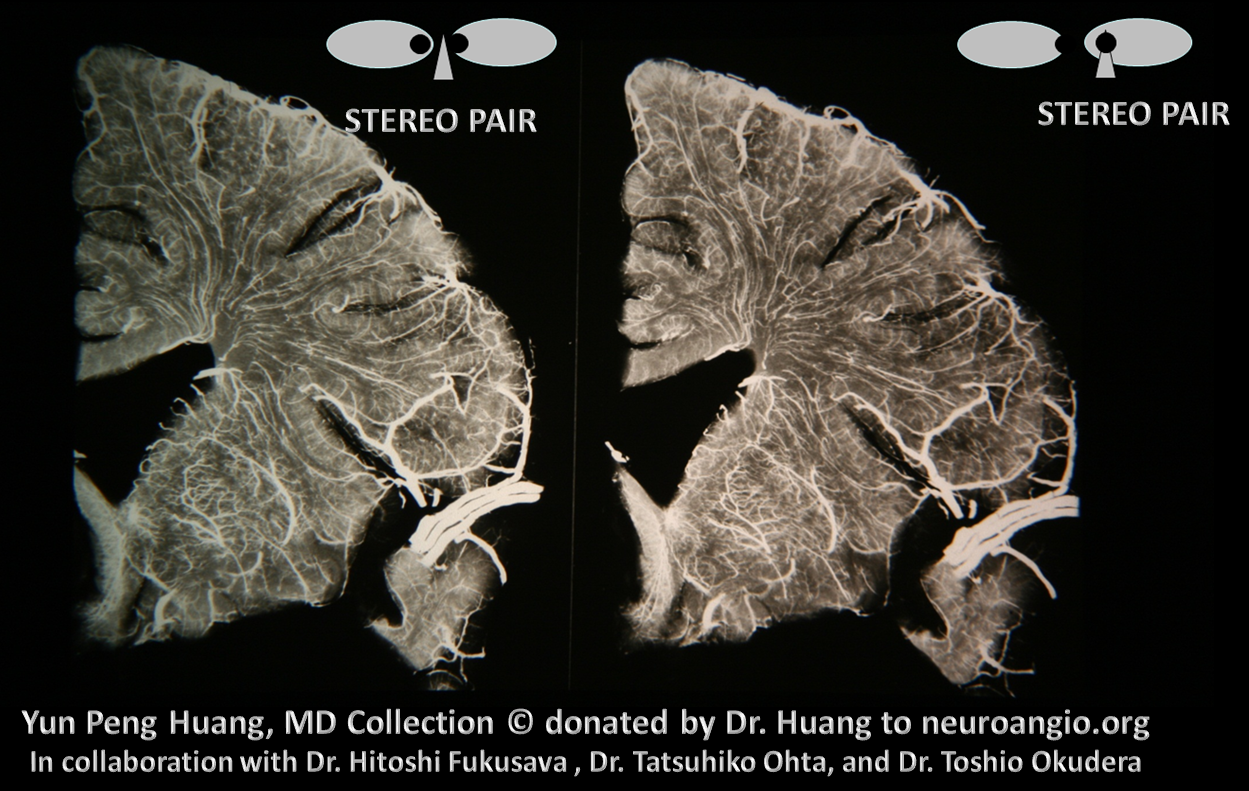
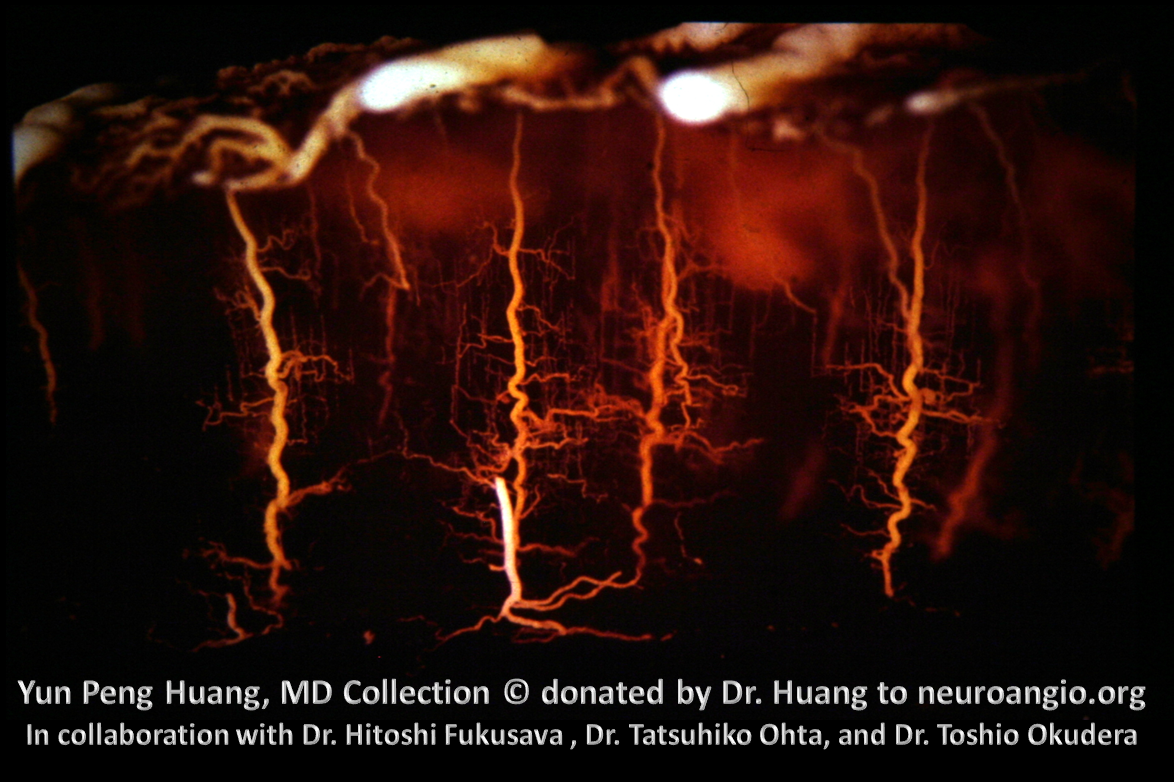
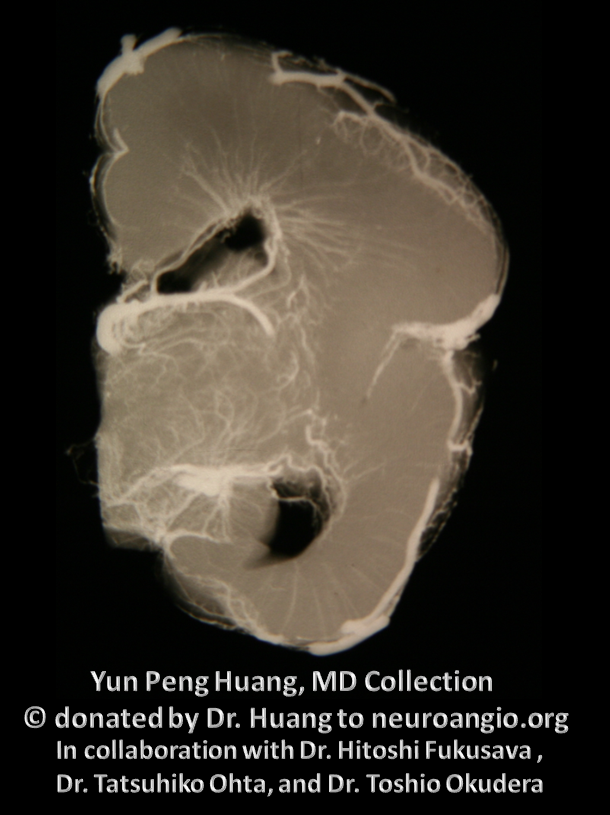
A beautiful stereo image. Notice how a few veins traverse the entire white distance between the pial and ependymal surface – the transmedullary veins.
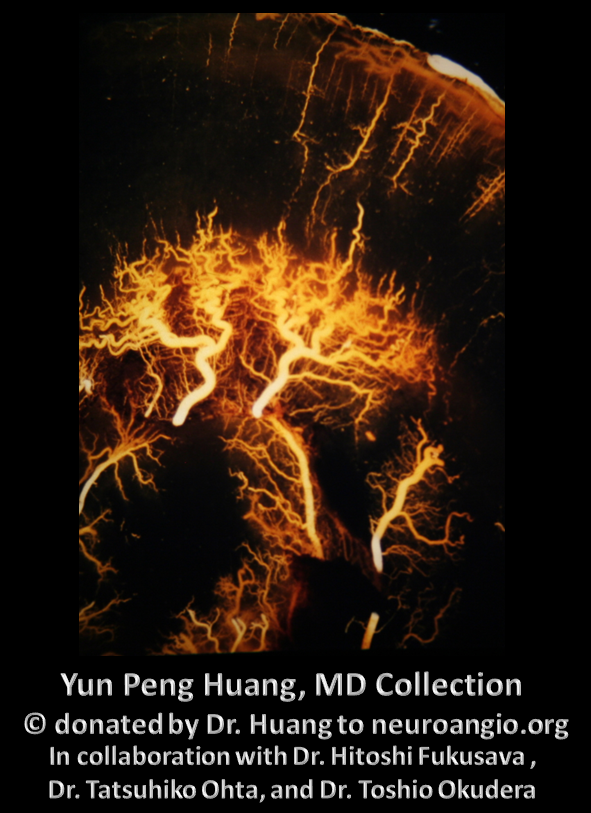
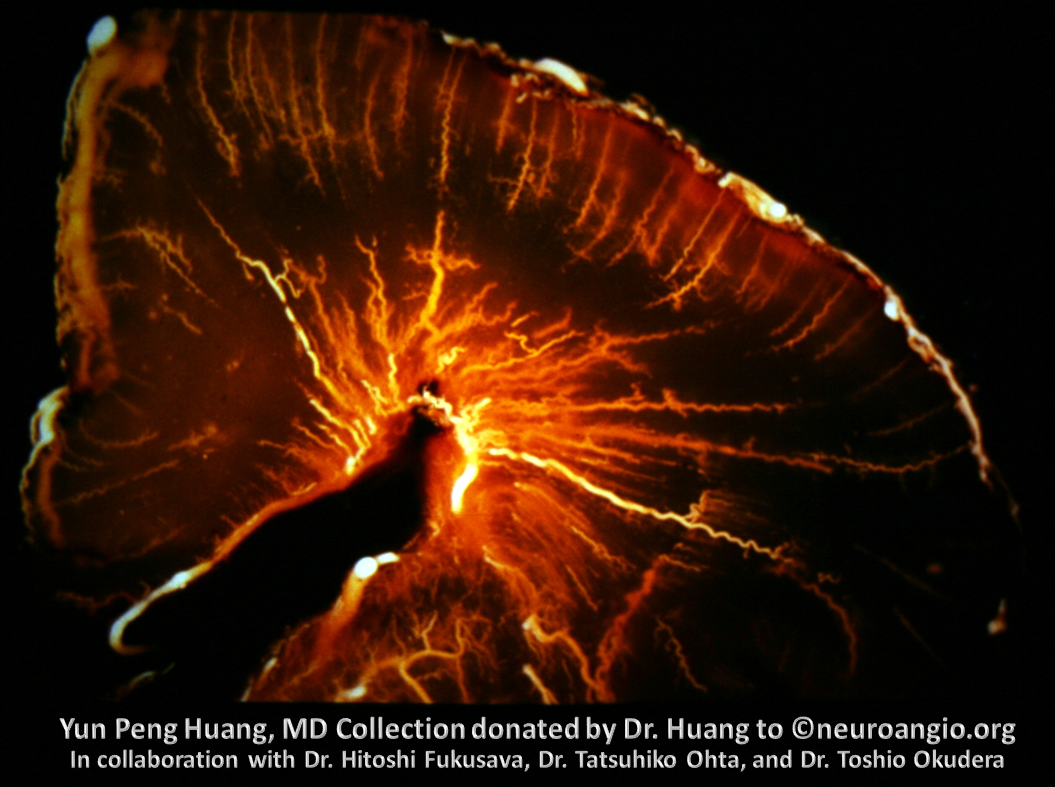
Another really gorgeous specimen of superficial veins
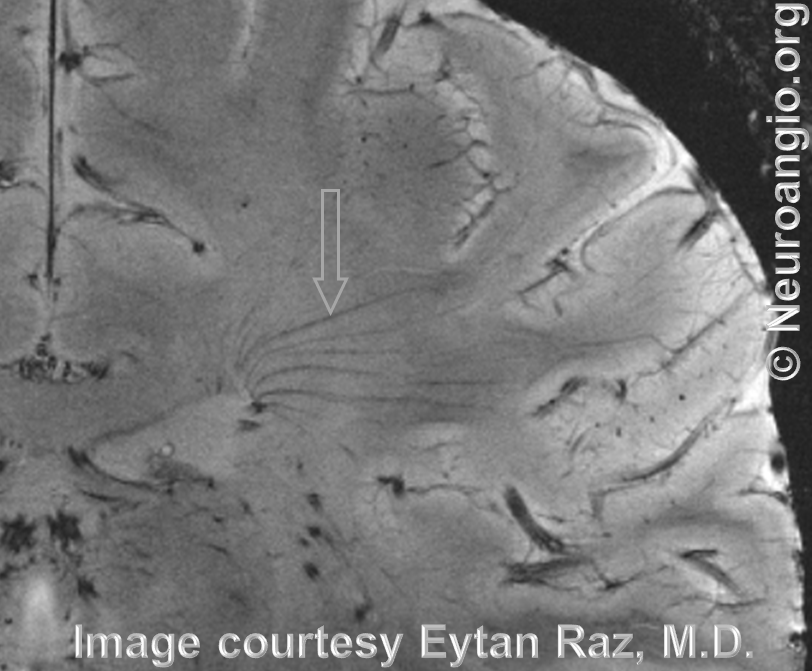
A momentary jump into the present — look at his amazing 7T MRI image of one of our own NYU very bright neurointerventional fellow, made by Dr. Raz. All veins — pial, superficial medullary, deep medullary (arrow), subependymal, ependymal, transmedullary — are seen here. We get the info, fellow keeps the brain — everyone wins.
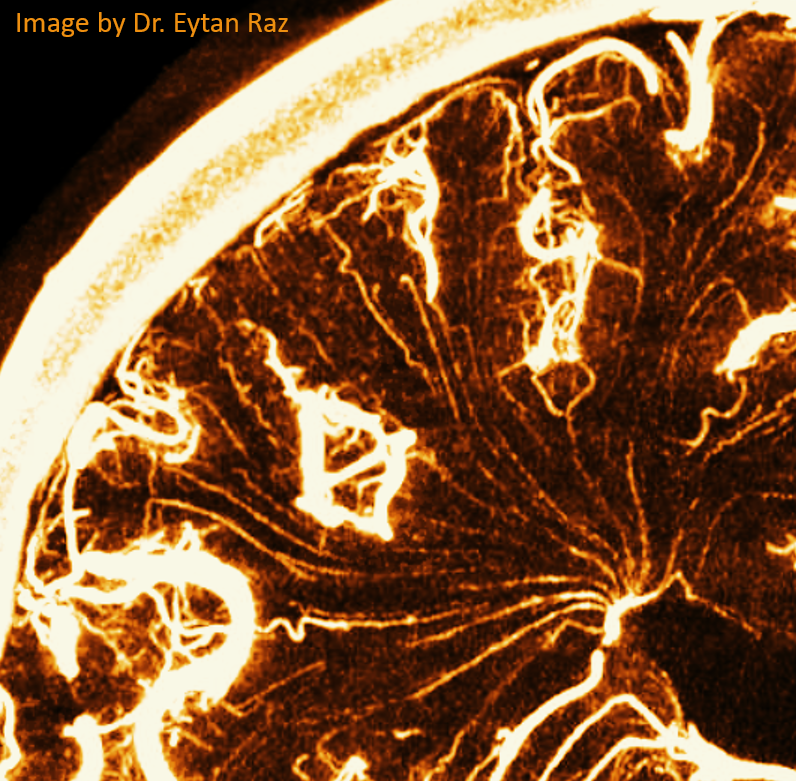
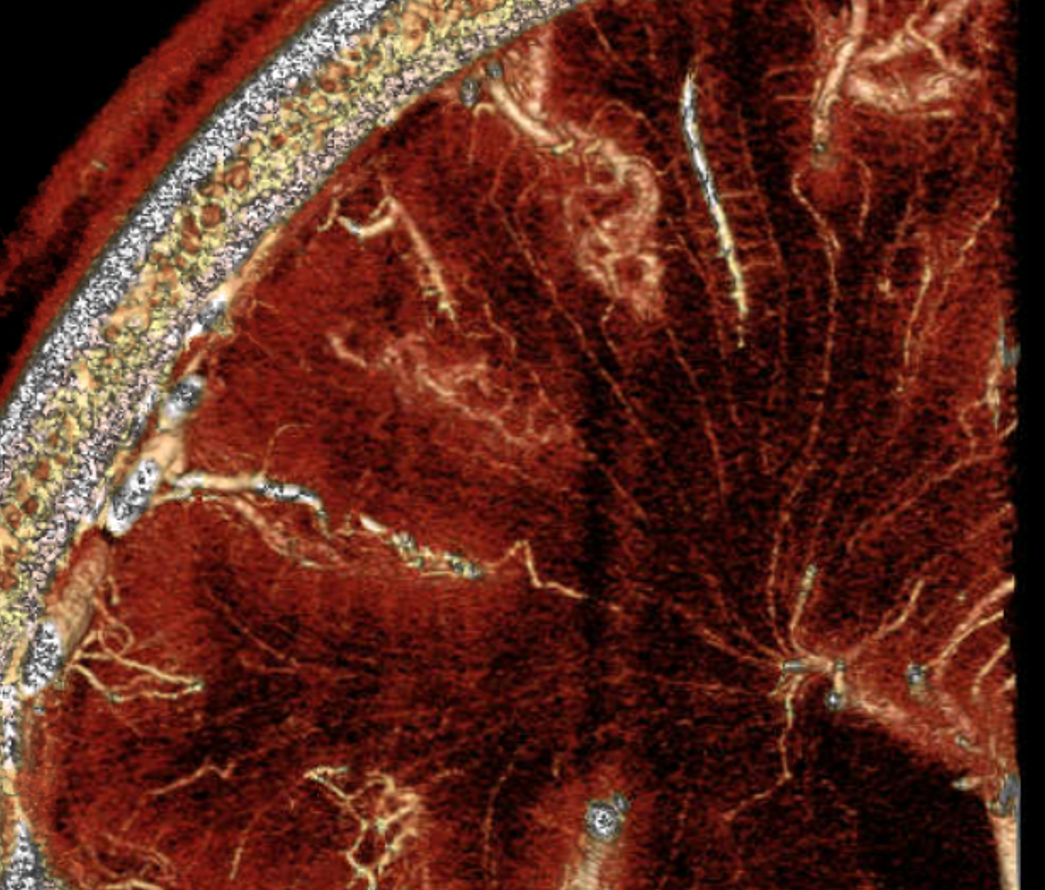
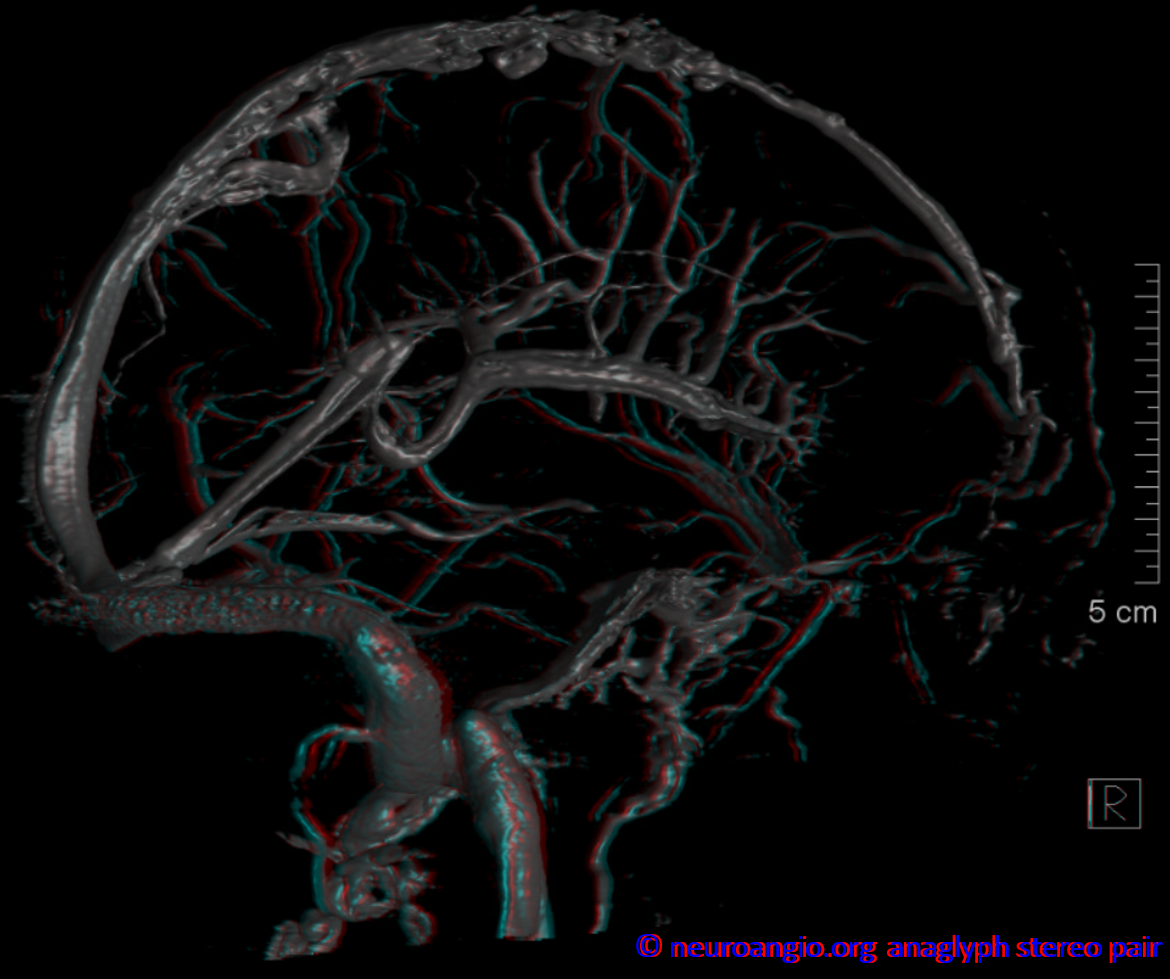
Now here comes flat panel imaging — DYNA CT in this case. Also courtesy Dr. Raz. The venous resolution is incredible — in vivo



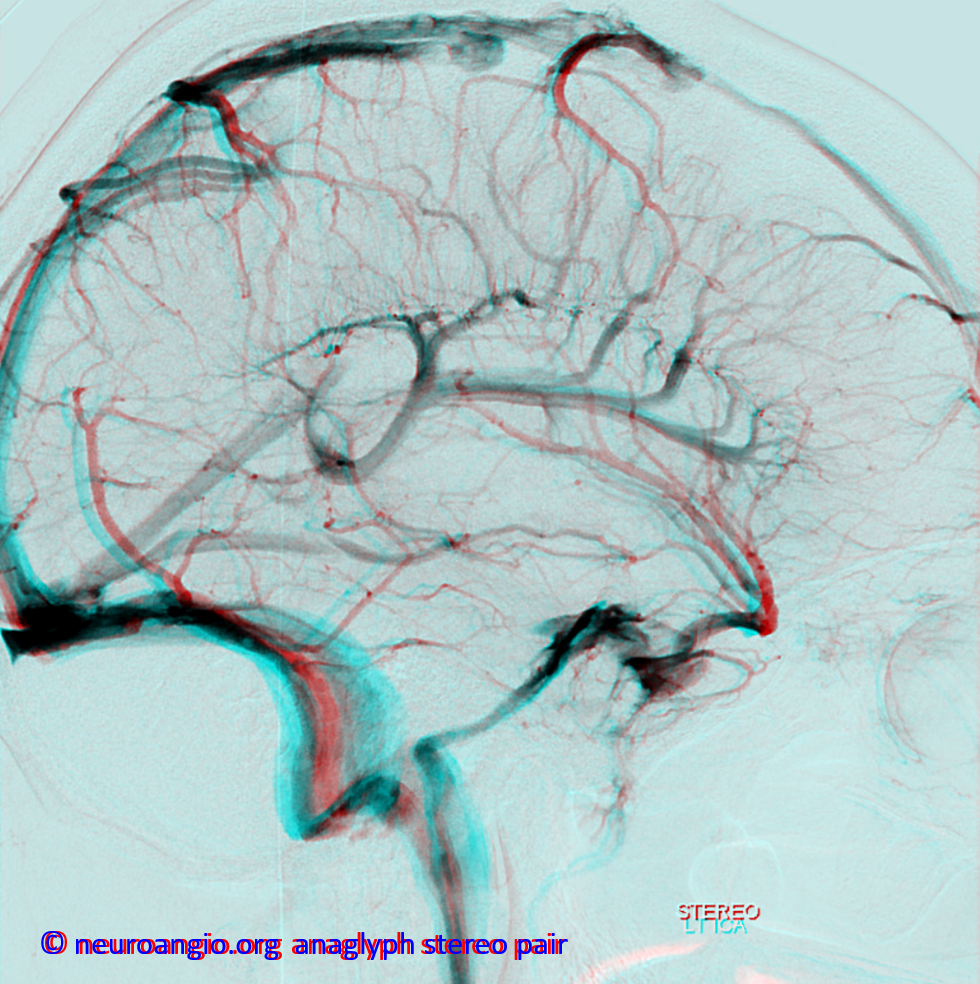
Anaglyph stereos
Back to Dr. Huang’s collection — beautiful depiction of the superficial venous collectors. Imagine what might one of these look like of the adjacent ones were absent – the remaining vein vertically-oriented vein would likely collect a larger territory o longitudinally-oriented tributaries — isn’t that what a DVA looks like.
A really spectacular image of both deep and superficial systems. Notice the taller, denser, and larger deep veins, reflecting the increased vascularity of the germinal matrix compared with the developing cortex in this embryo. Some of those deep tree-like collectors look almost like DVAs already
The high density of transmedullary vein is appreciated on this slide
In this specimen roentgenograph, some veins are medial hemispheric, others (particularly parieto-occipital) are transmedullary
Another specimen
The esthetic beauty is intrinsically valuable
Numbers 2 and 3 are pretty good
Another illustration
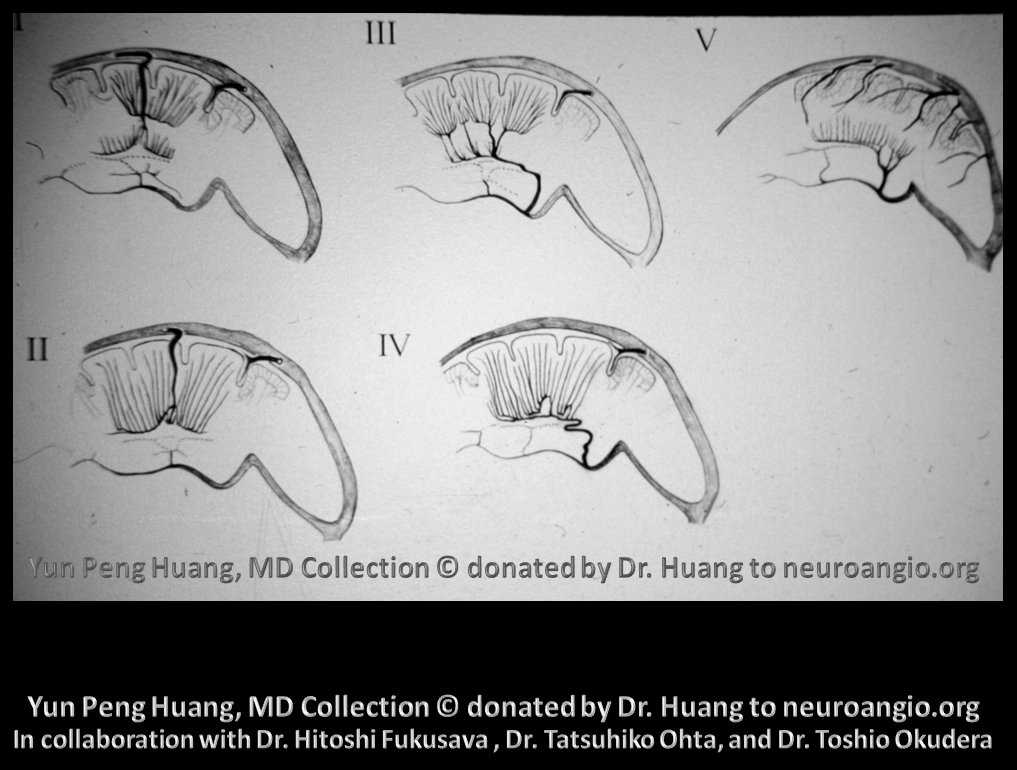
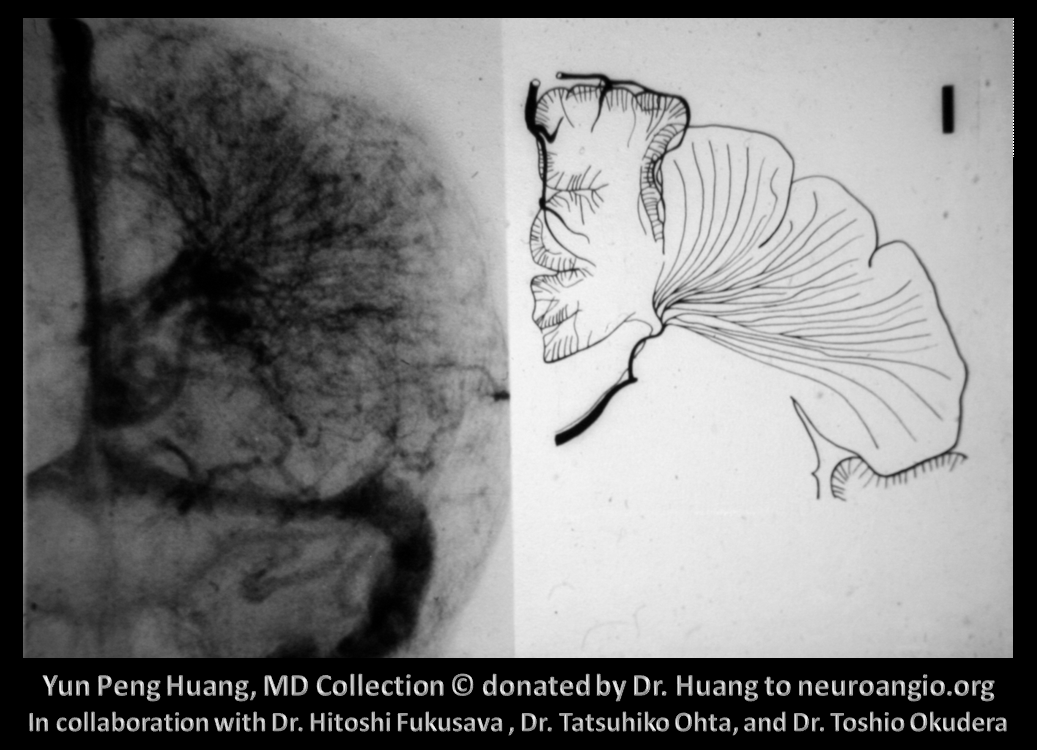
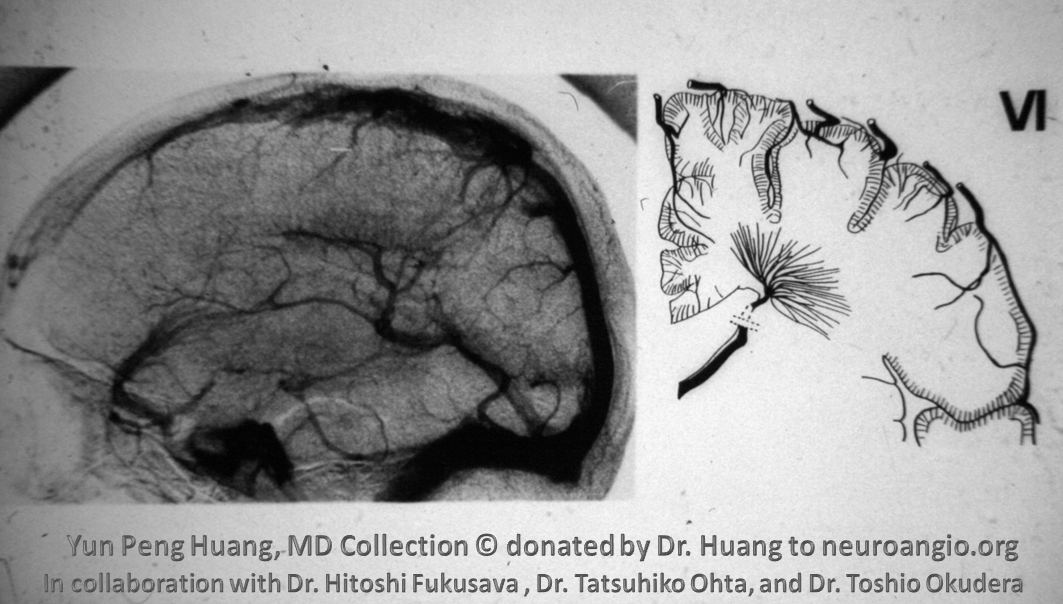
The concept of a Medullary Venous Malformation, or DVA, as a vein collecting more than its physiologic share of medullary territory now emerges. There are two types of DVAs depending on where the vein drains – superficial (I, II in the slide below) and deep (III, IV, V in the slide below). The majority drain superficially, assuming responsibility for drainage of the deep medullary territory which normally into the deep,subependymal system. Deep MVMs, or DVAs, collect tributaries of the superficial medullary area which normally would be served by the pial veins. This idea is illustrated in the slide below, although the Roman numerical nomenclature of the different subtypes is no longer in use.
See below
Same concept, deep medullary territory collected into the superficial system
Drawing over ex vivo specimen
Superficial Medullary Venous Malformation in pre-DSA era
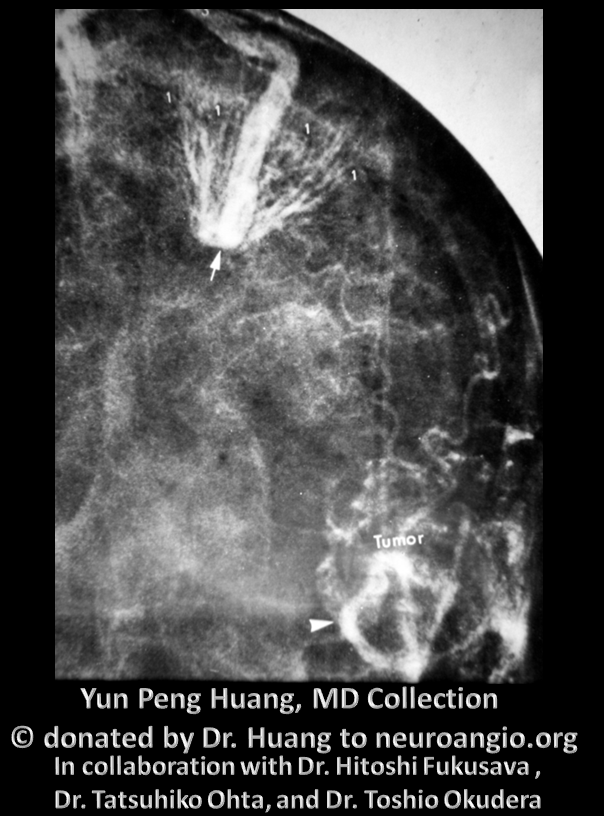
Extensive deep venous MVM — is this Sturge Weber?
DVA of the direct lateral vein
Extensive deep MVM-DVA collecting into the internal cerebral vein
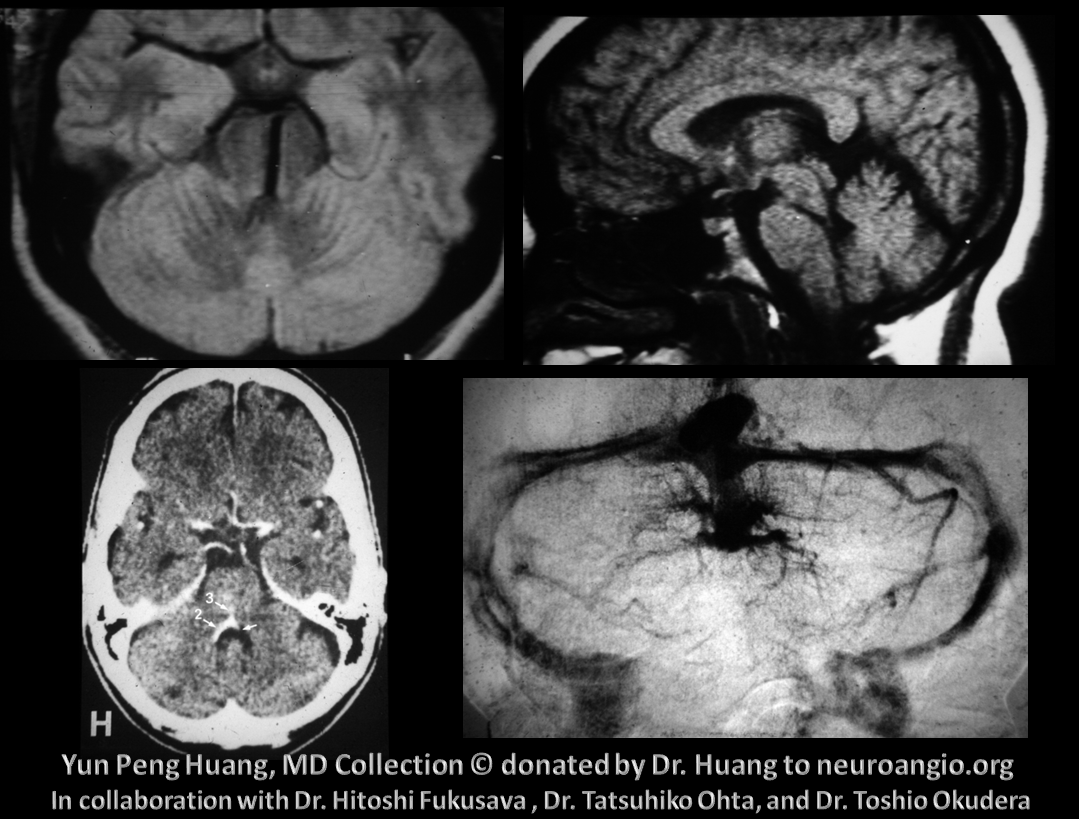
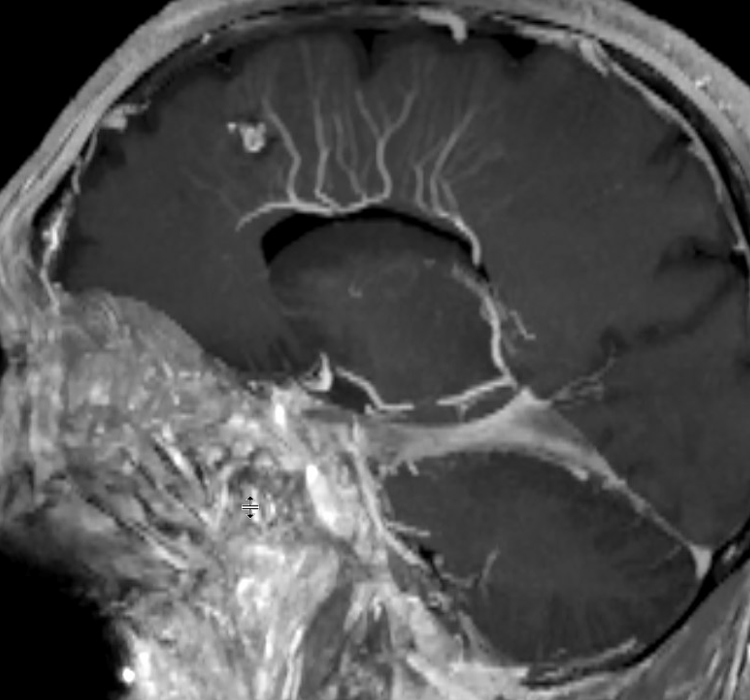
Cerebellar DVA with trans-pontomesencephalic drainage, highlighting presence of trans-medullary veins in the brainstem; similar transmedullary veins can be seen in the spinal cord.
Another remarkable DVA, showcasing basal ganglia/hippocampal drainage anastomoses with the cavernous sinus region via the uncal/basal veins
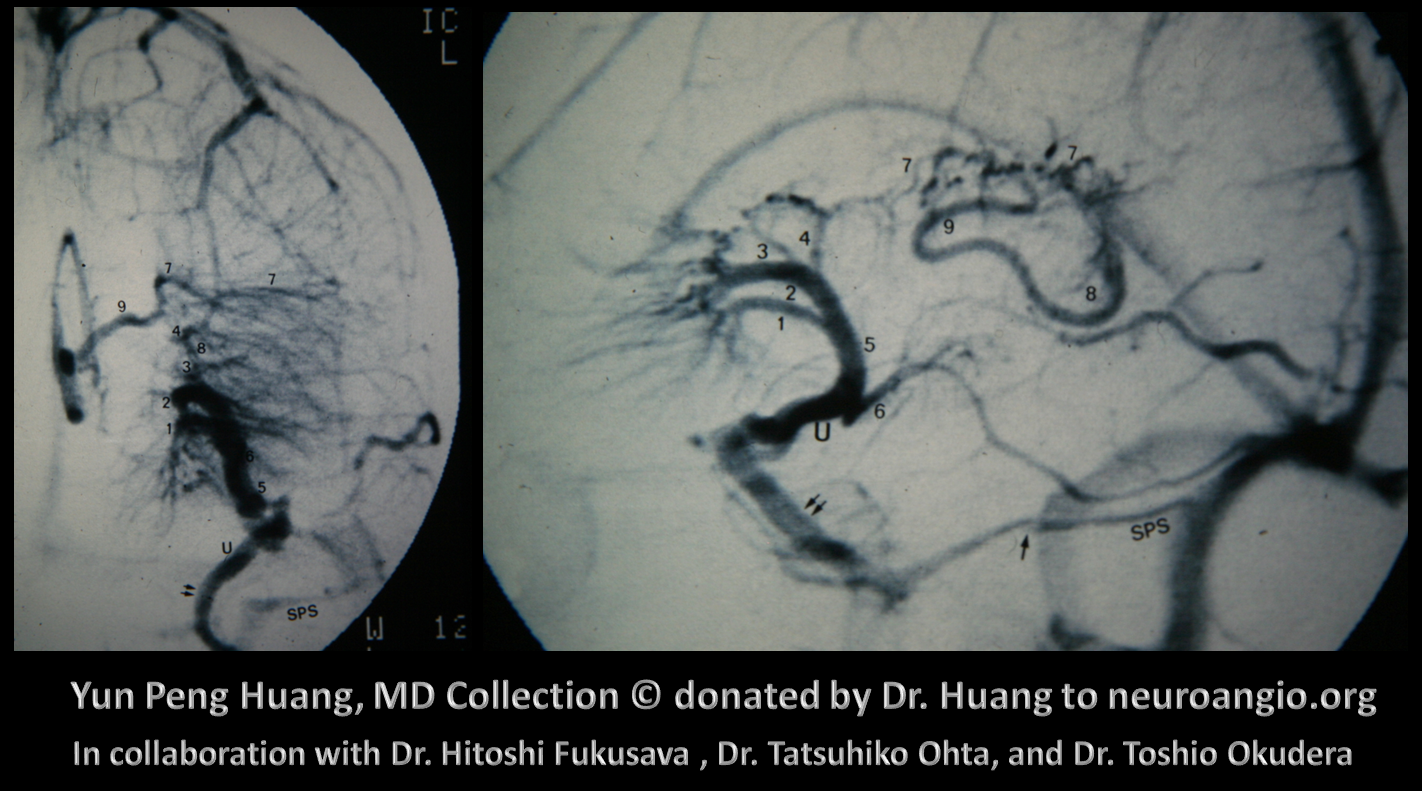
Essentially the entire internal cerebral venous system is collected into the basal vein, a unique structure which bridges the deep and superficial venous systems.
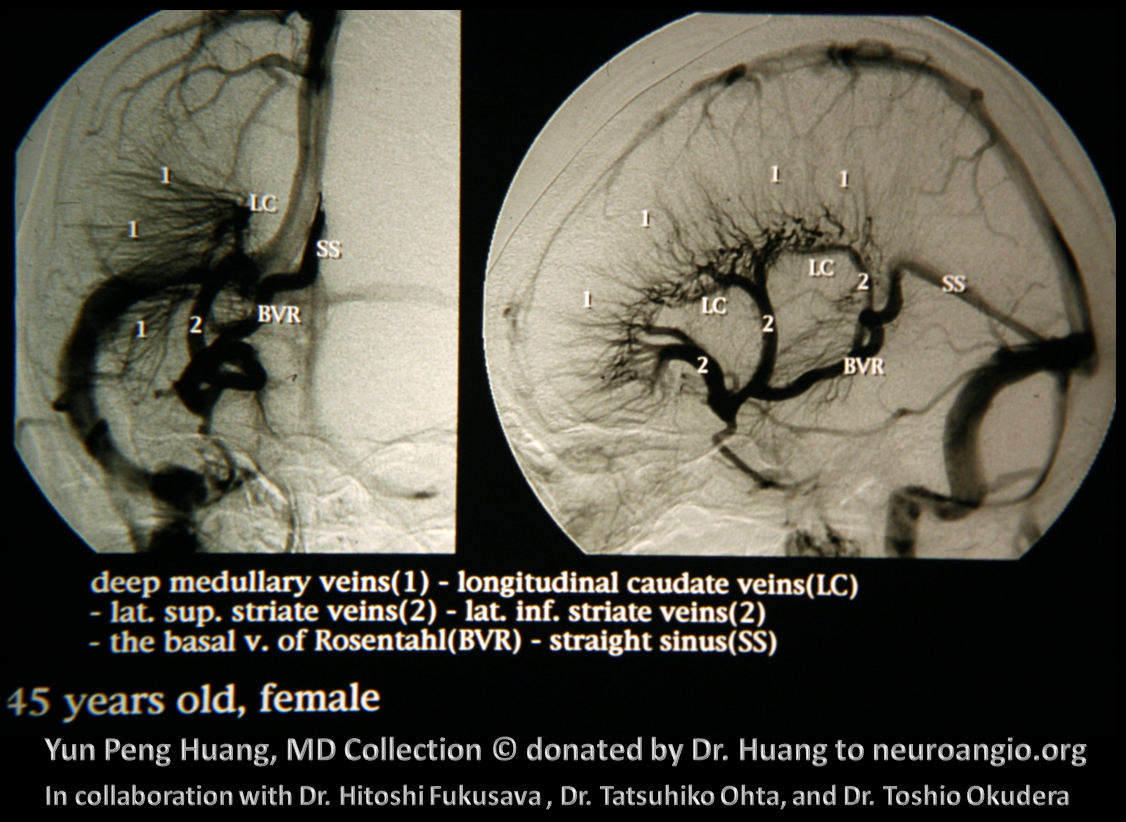
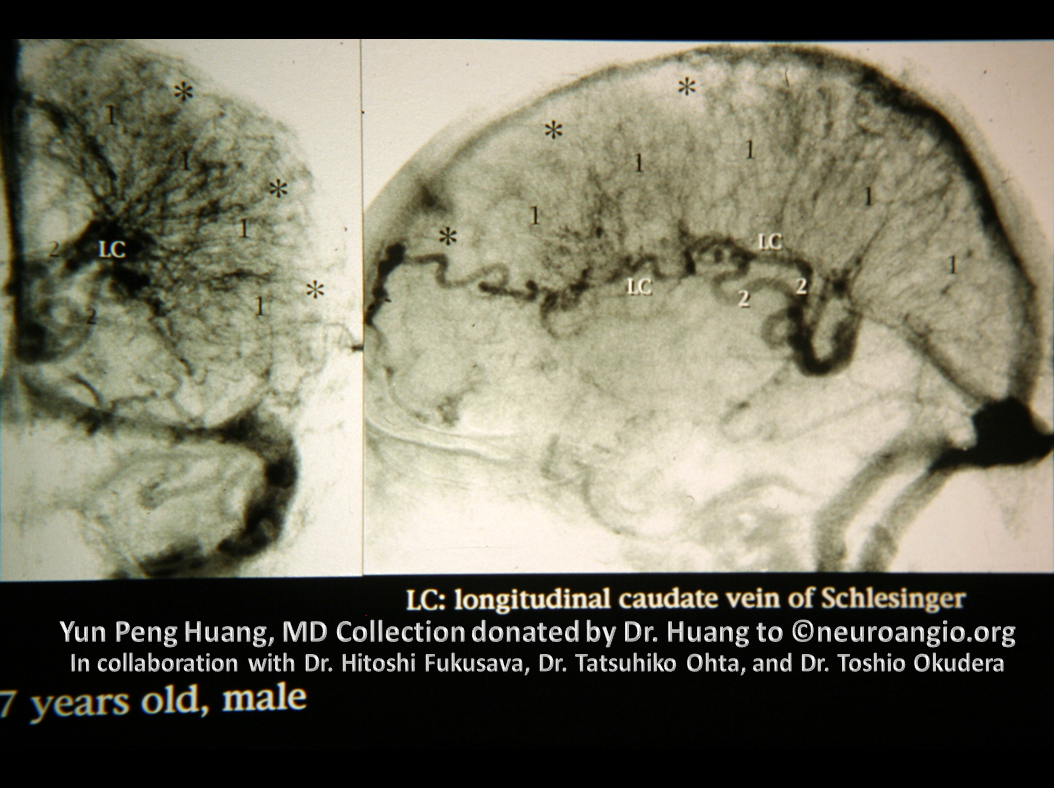
Large MVM-DVA of the longitudinal caudate vein (of Shlessinger)
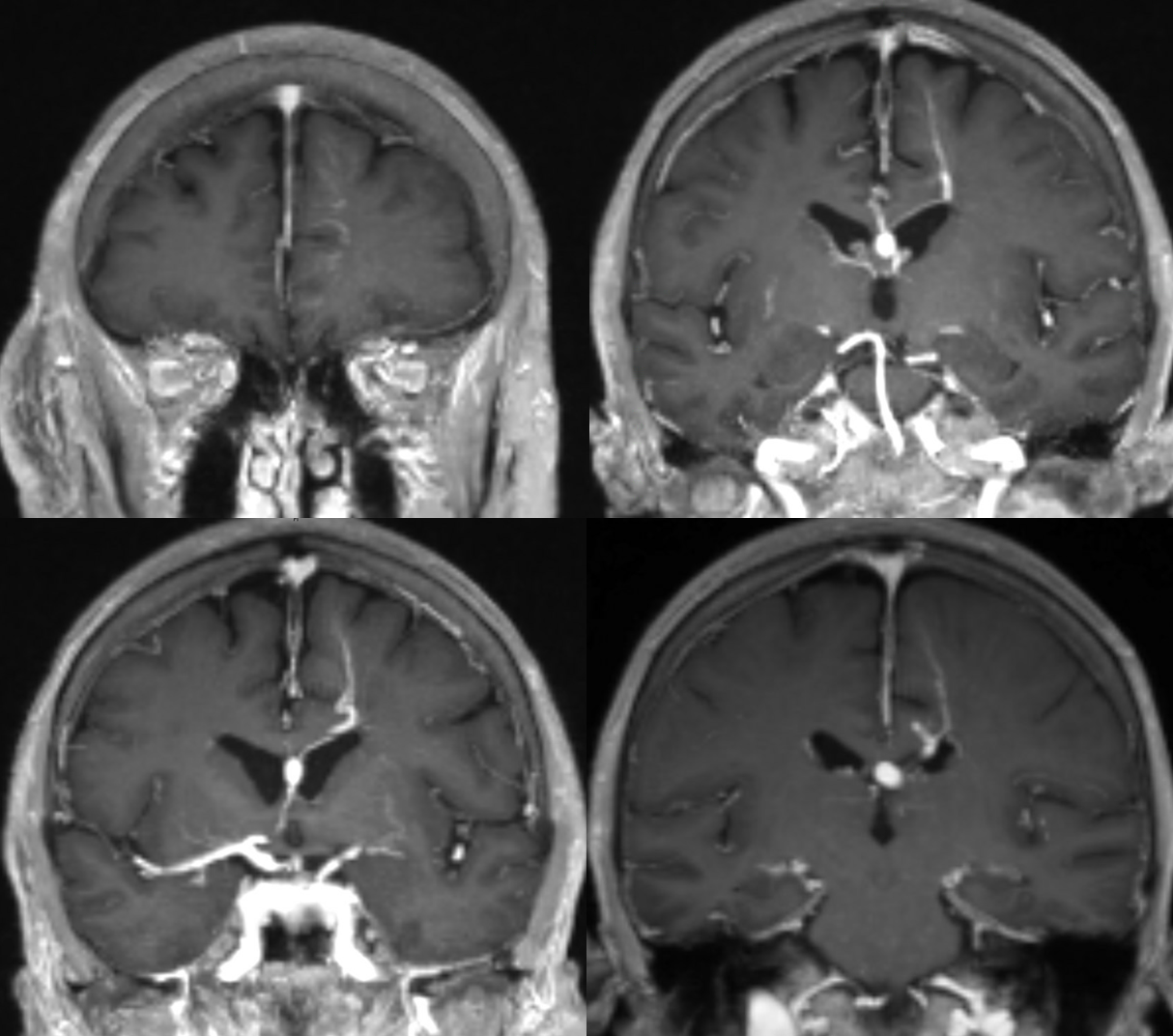
DVA deep-draining and Cavernoma MRI
Pons DVA
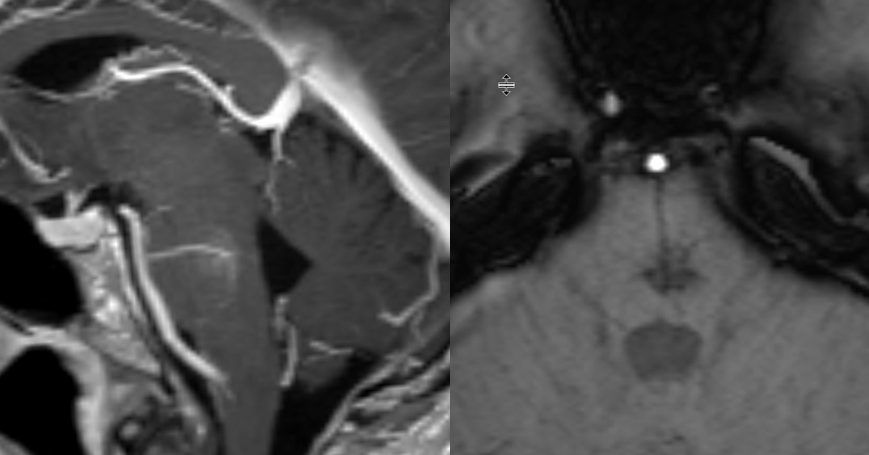
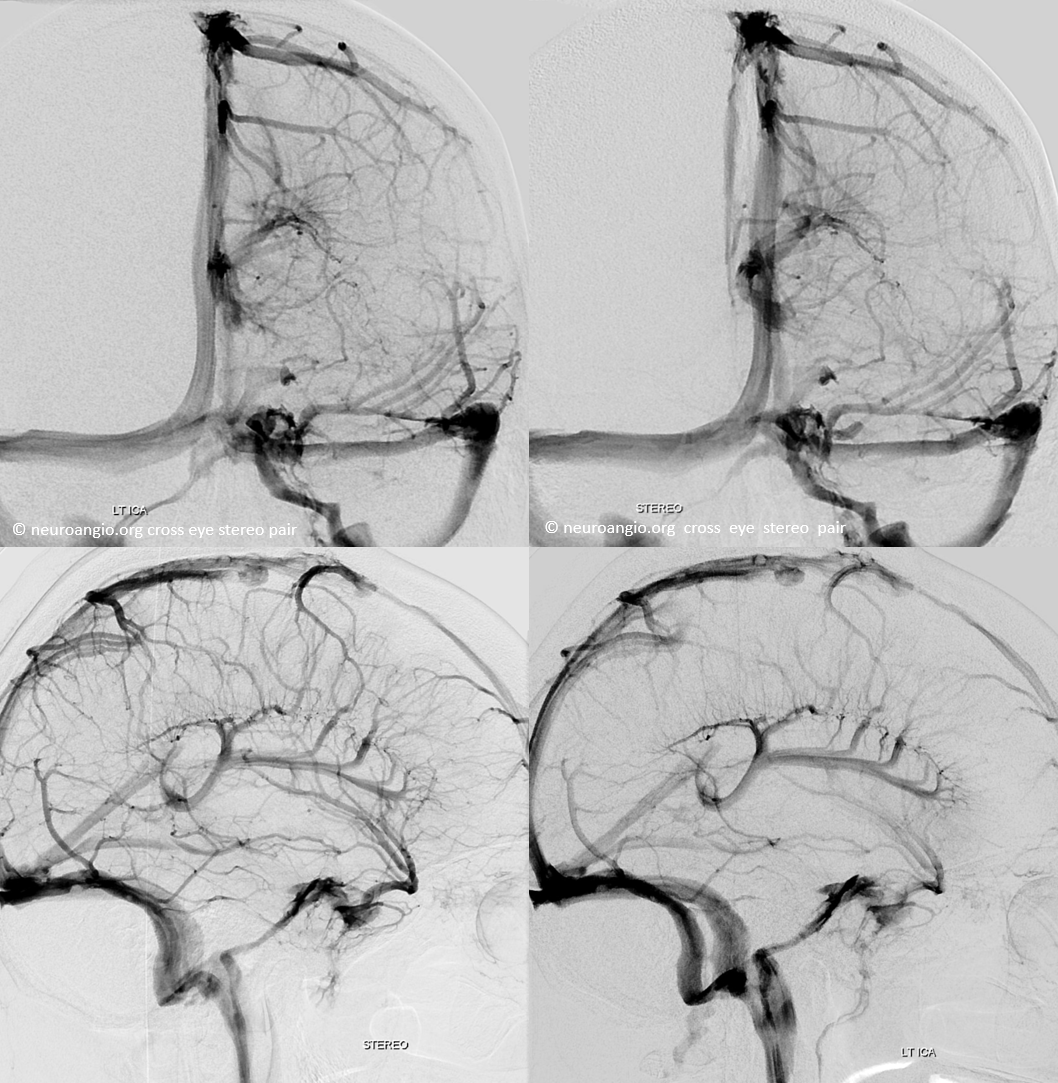
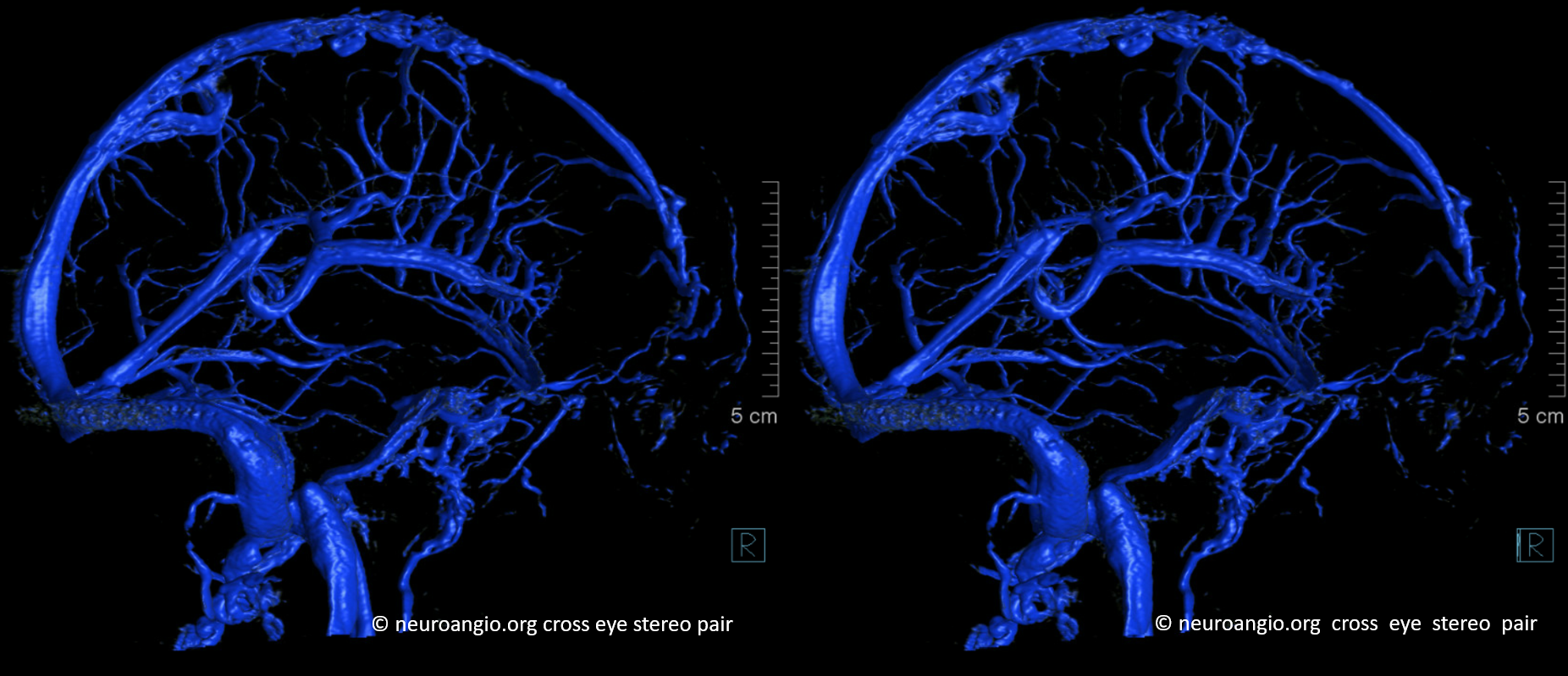
MRI-angio example courtesy of Eytan Raz
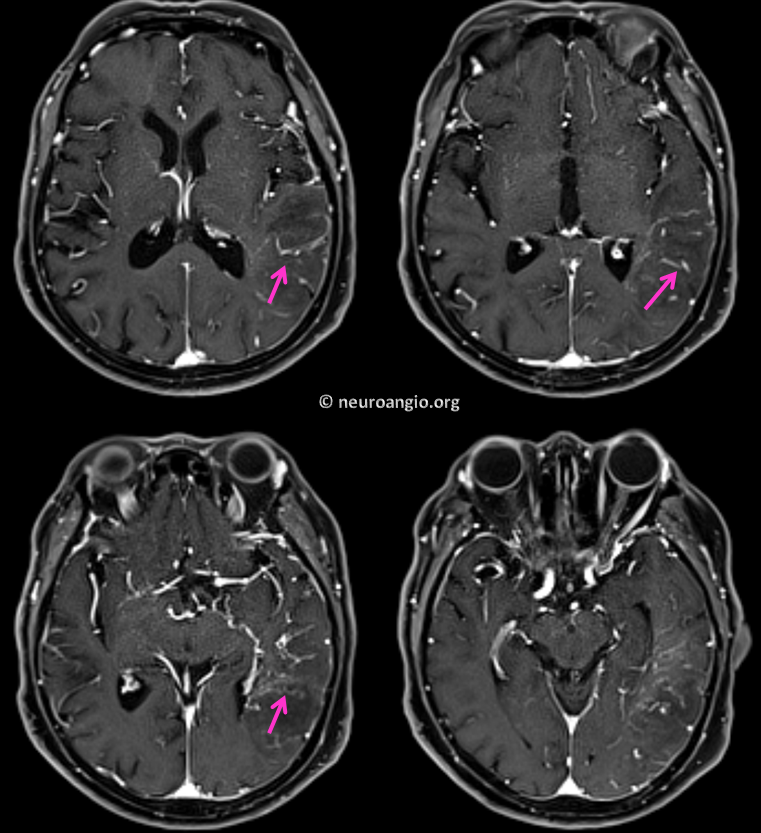
Excellent example of deep DVA — see how the medullary veins extend to the subcortical regions? The loss of balance between superficial and deep venous systems is the hallmark of DVA
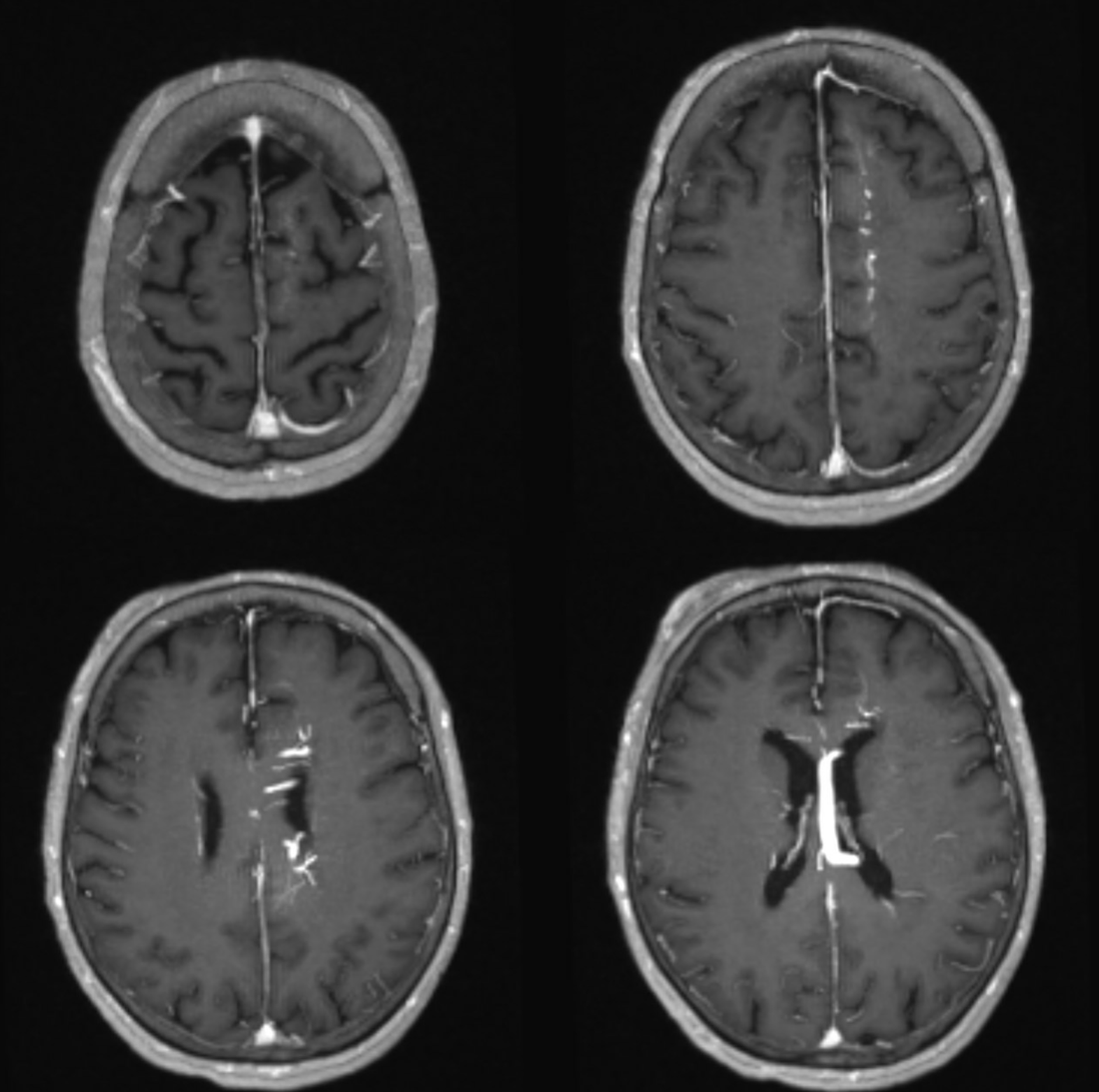
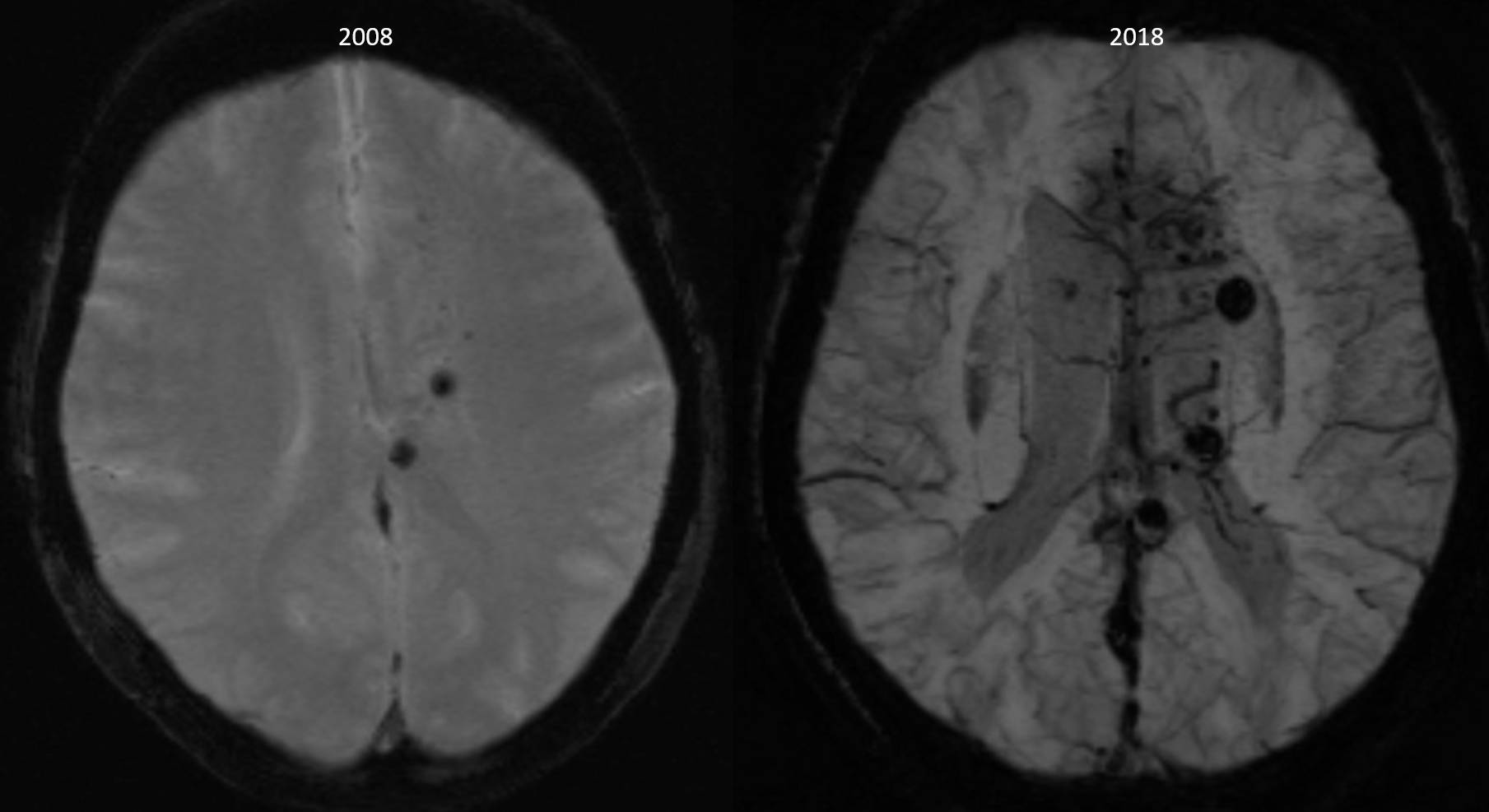
Much improvement in imaging over 10 years — and a few more cavernomas…
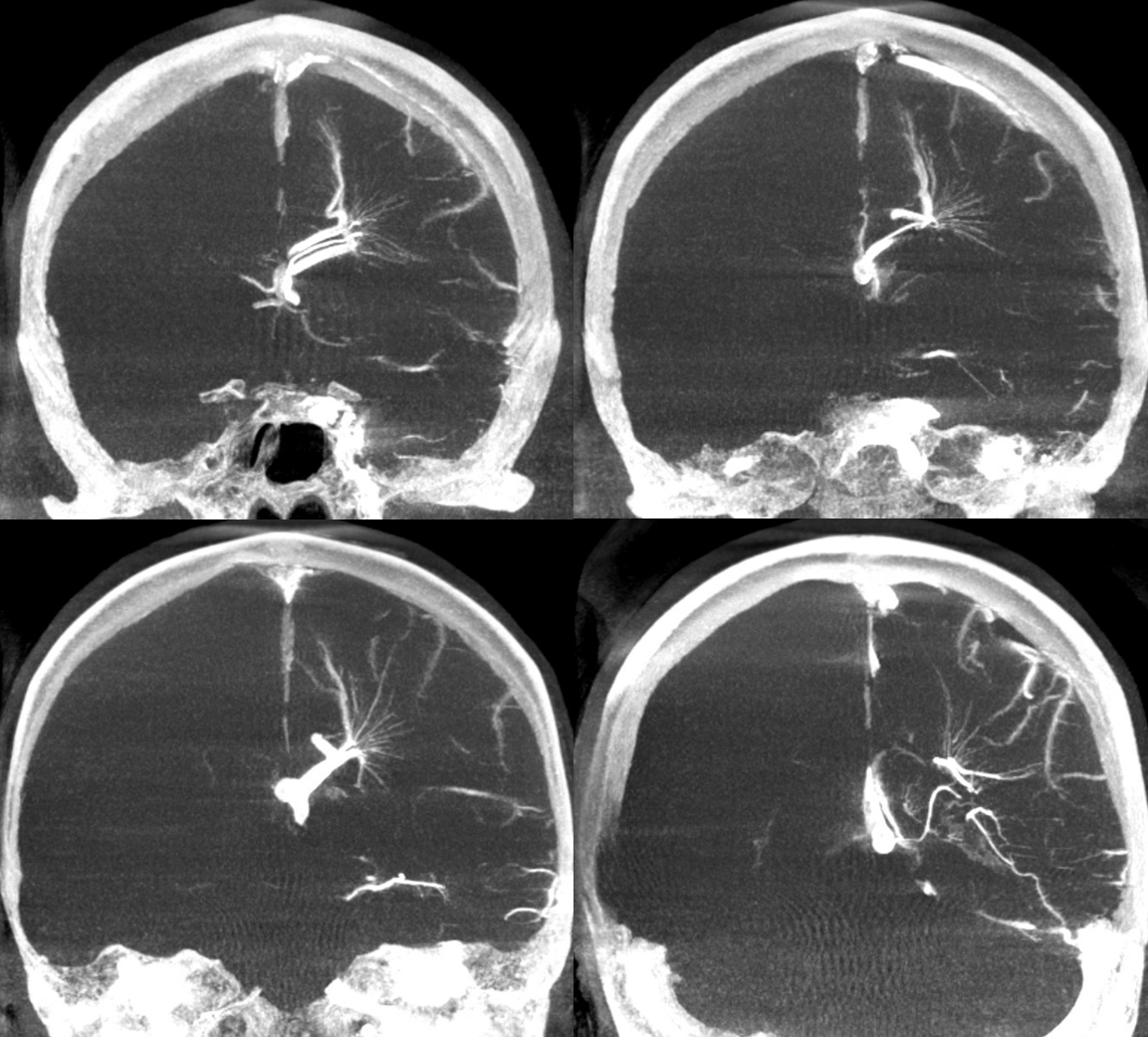
DYNA MIPs
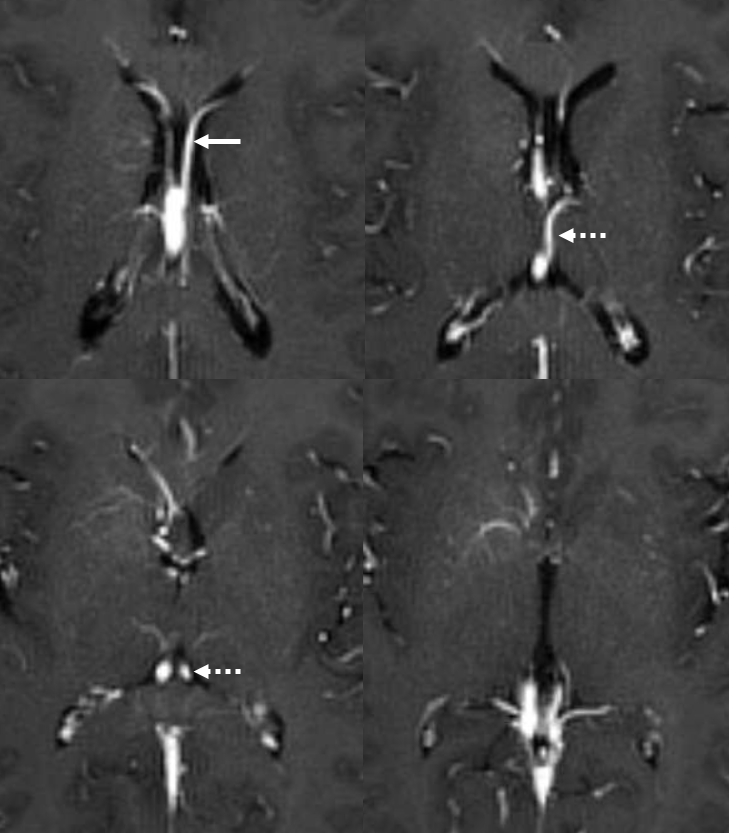
Variations abound — here is bilateral caudate / septal veins (left — arrow) draining into the right internal cerebral vein, while the left thalamostriate vein is the major tributary of the left internal cerebral vein (dashed arrow) — in a subject with a MVM/DVA
Modern Pathophysiologic Correlation
The recruitment of transmedullary veins in states of venous occlusion (such as venous sinus thrombosis) or venous flow-related congestion (such as dural fistulas draining into cortical veins) has been well-documented, and serves as a confirmation of the functional role of transmedullary venous pathways. Some examples are shown below, such as this case of extensive dural sinus thrombosis wth secondary recruitment of transmedullary veins (blue) draining into the deep venous system, and venous hemorrhage (green)
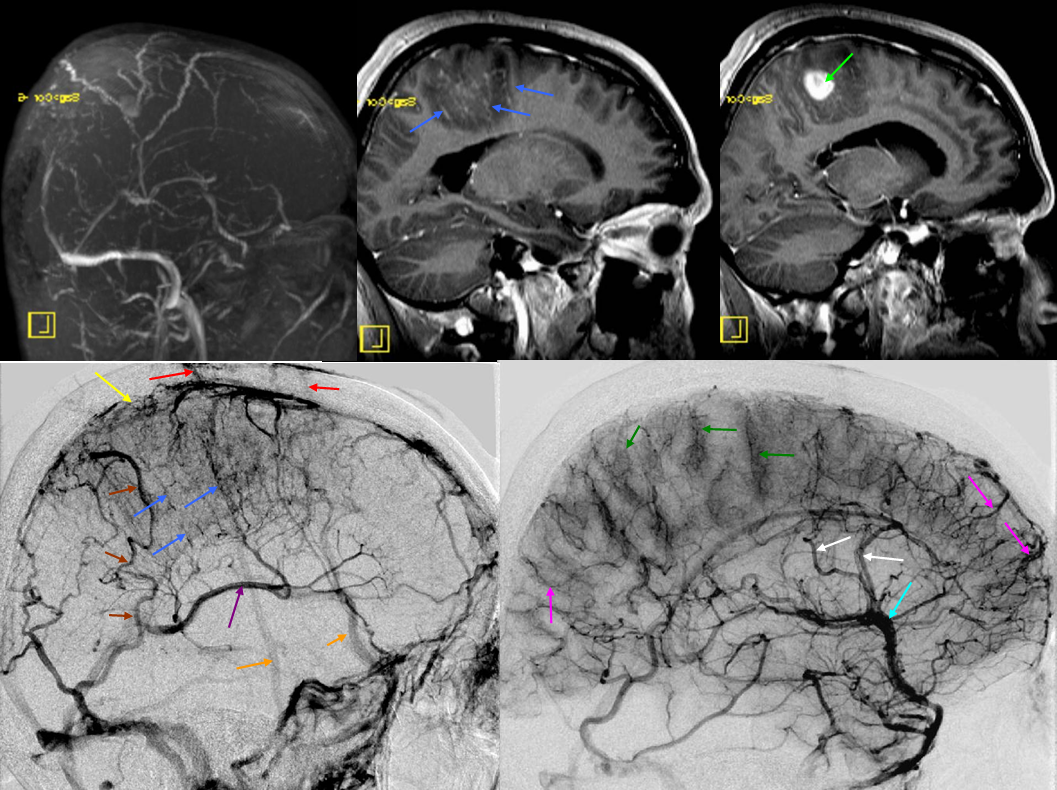
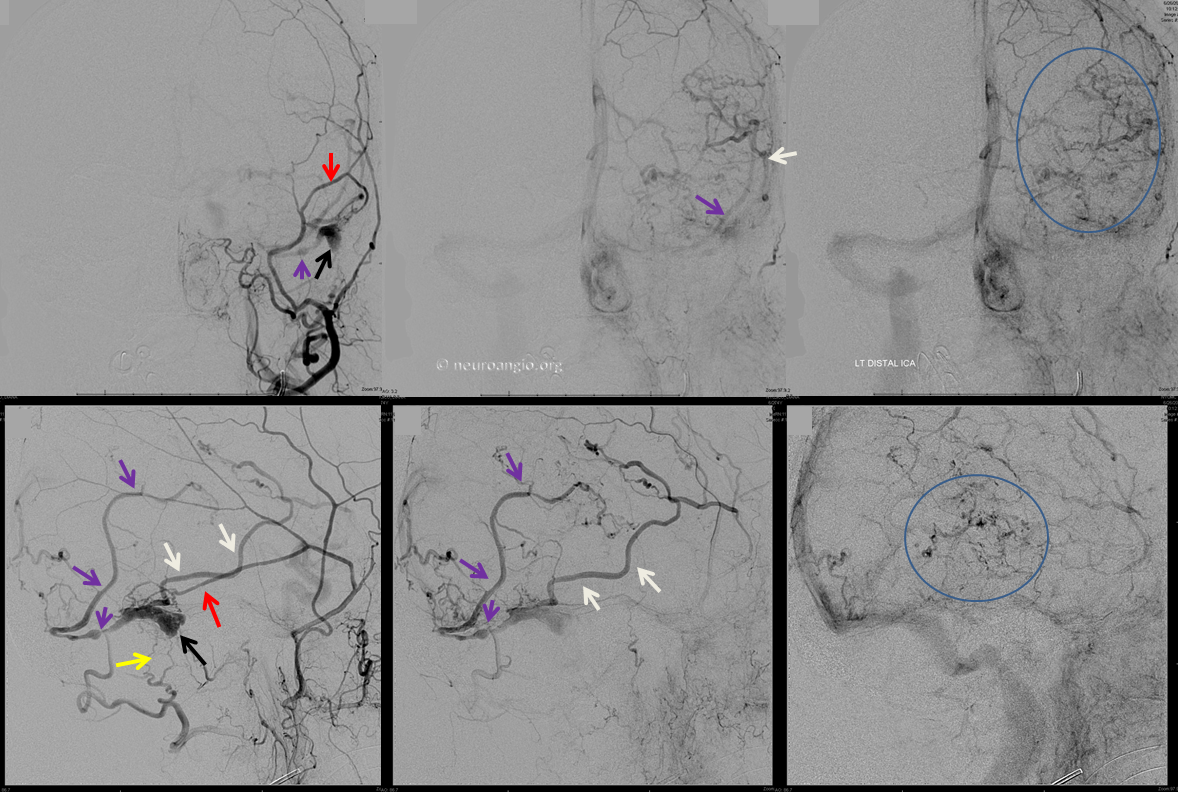
In this case of a sigmoid sinus fistula and occlusion of both proximal sigmoid and transverse sinuses, with exclusive cortical venous drainage and no effective pial collaterals into the SSS or cavernous sinus, the result is marked congestion with extensive venous infarction. The transmedullary veins are marked by pink arrows. The full case link is here, under the subsection Case Archives
Pre-embolization angiogram with transmedullary veins within the blue ovals
DVA Associations
Cavernous Angioma/Cavernoma: The association between DVA and cavernous angioma or cavernoma is well-known. The vast majority of hemorrhages in the neighborhood of a DVA actually come from an adjaent cavernous angioma. Why DVAs are associated with cavernous angiomas is not clear.
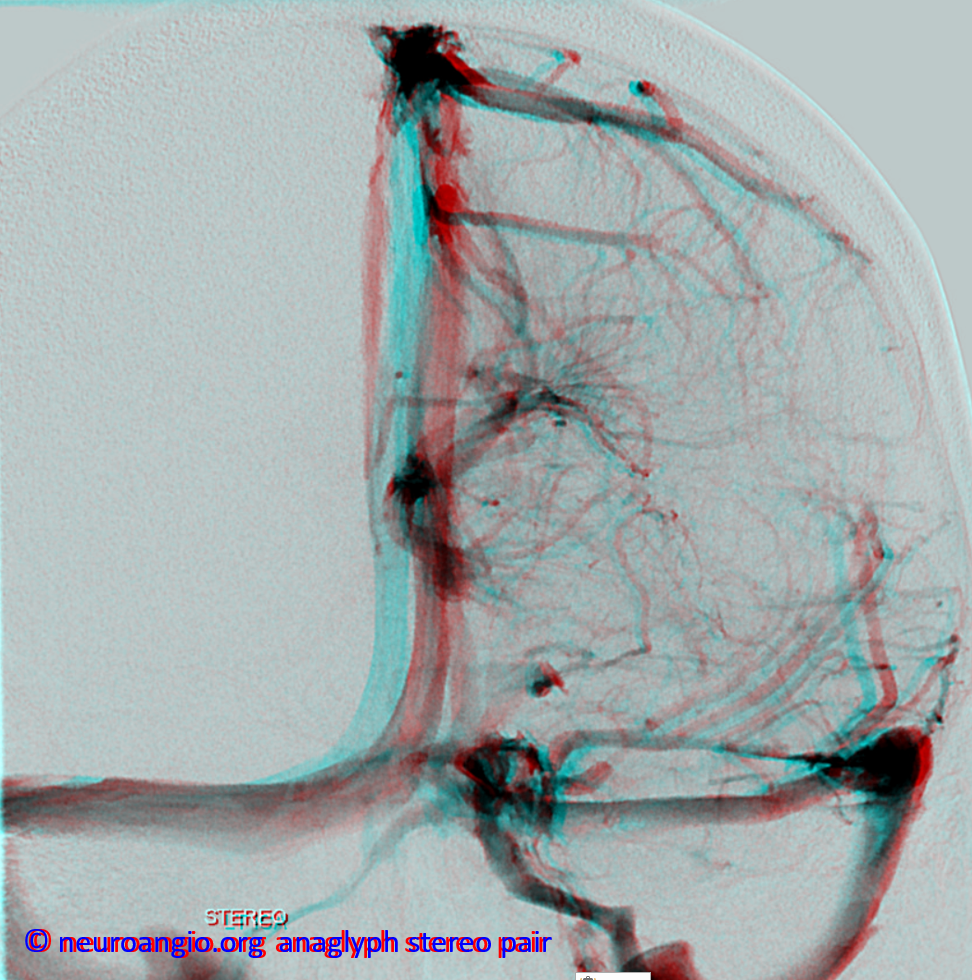
Dural Venous Sinus: A less well-known associateion is between a DVA and a dural venous sinus into which it sometimes drains (as distinct from drainage into cortical or deep venous system). Dural venous sinuses othen than the well-known and named ones (superior sagittal, transverse, etc) exist quite frequently — falcine sinus is one of them. There are several nice examples on the “Venous Sinuses” page. The dura has embryonic potential to house sinuses, and does, until most of these disappear. If a state whereby increased flow into a dural sinus is established, the sinus may persist — for example when a large cortical vein or DVA drain into the sinus. This is very important to keep in mind for the surgeon, who may inadvertenly injure the sinus while opening the dura — with the same consequence as would be injury to a major cortical vein. Here is an example of a frontal operculum DVA (blue) draining into a large dural sinus (white). Notice the flattened appearance of the sinus as seen on frontal views and a semi-transparent look on the lateral view — this is a very characteristic look for dural sinuses which are oval within the flat dura. Note also jugular vein stenoses at the C1 lateral mass level (brown) with compensatory hypertrophy of the emissary veins (purple)
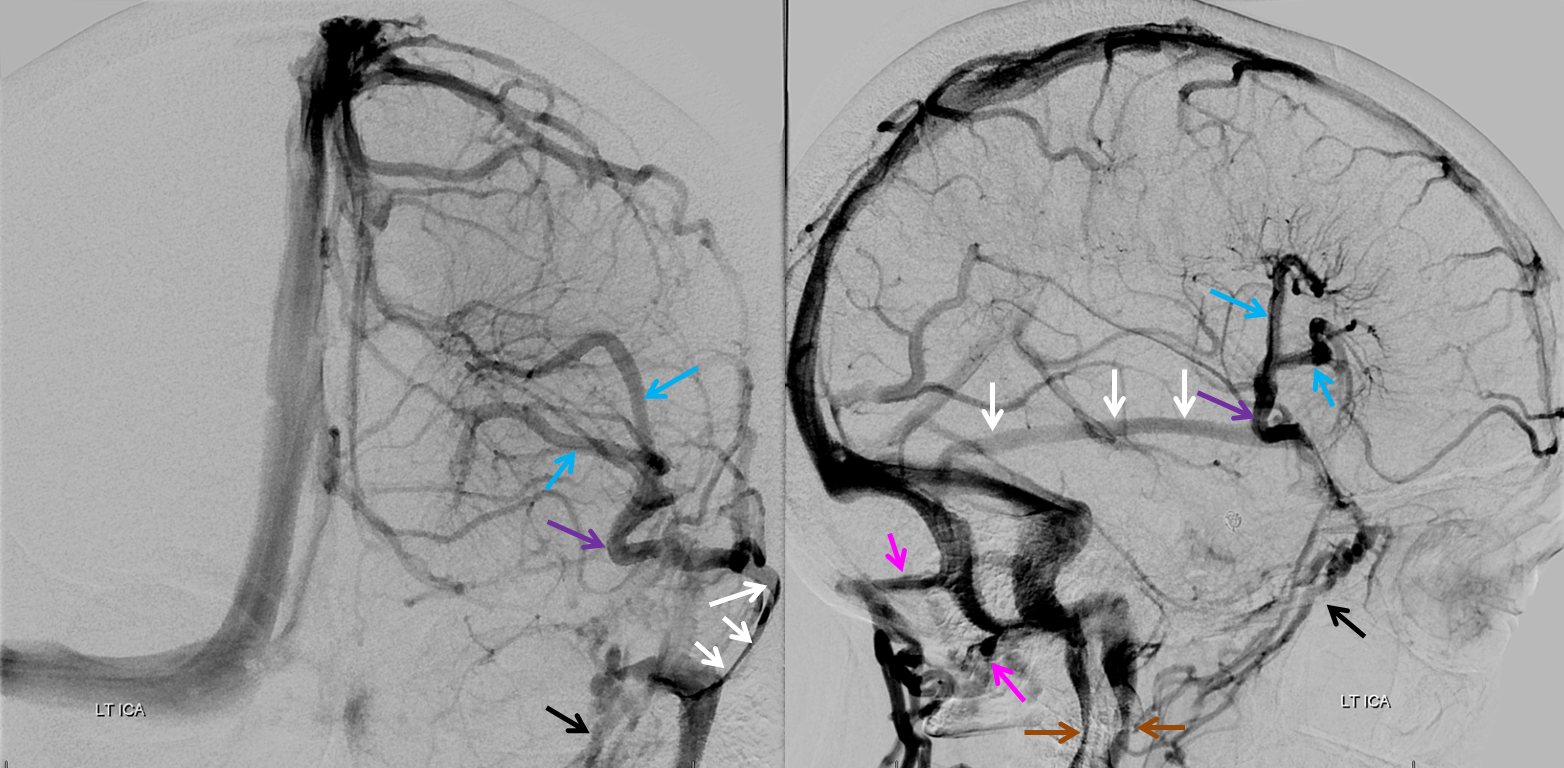
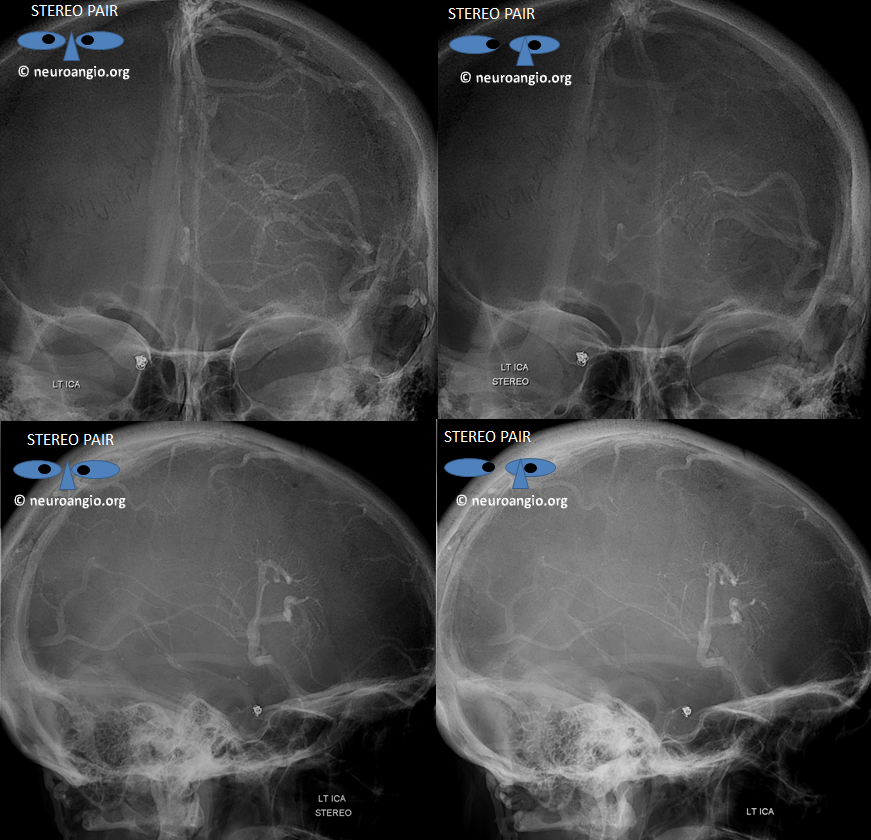
Stereo views
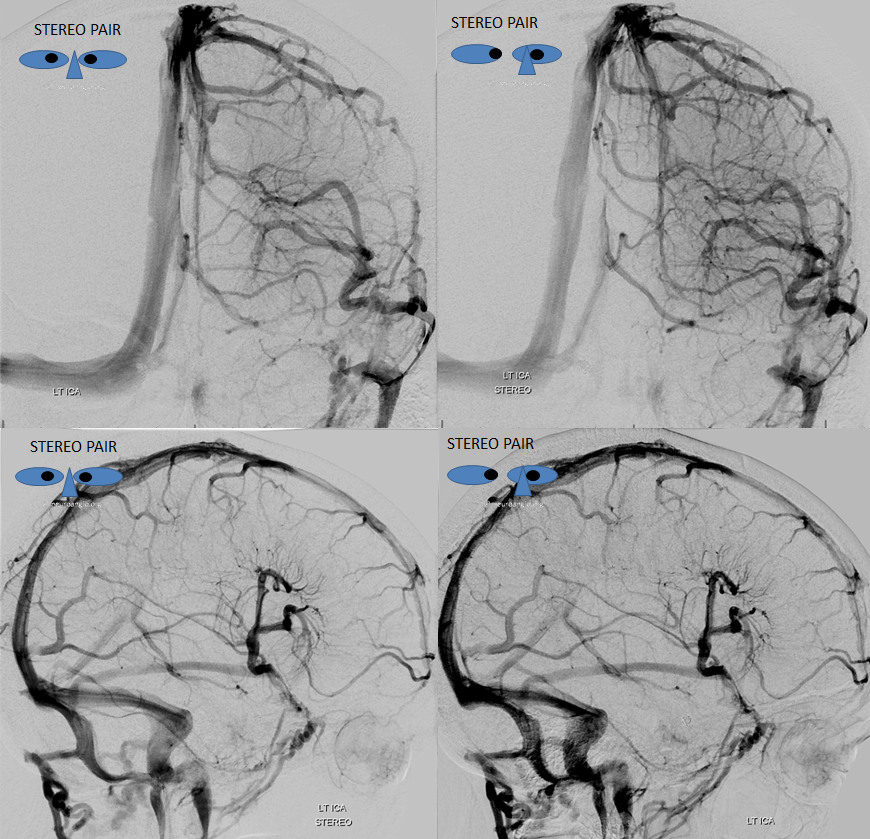
Native stereos
Conclusion
In large part due to worldwide adoption of the term DVA, Dr. Huang’s seminal contributions to our current understanding of normal and variant / anomalous / malformative venous drainage are not widely known to the current generation of trainees — an omission which neuroangio.org would like to see at least somewhat redressed.
Back to Yun Peng Huang Collection
Related neuroangio.org pages:
Further reading is here:
http://onlinelibrary.wiley.com/doi/10.1046/j.1440-1789.1999.00215.x/abstract
https://www.researchgate.net/publication/14072140_Venous_Architecture_of_Cerebral_Hemispheric_White_Matter_and_Comments_on_Pathogenesis_of_Medullary_Venous_and_Other_Cerebral_Vascular_Malformations
http://link.springer.com/article/10.1007/BF01743138
http://stroke.ahajournals.org/content/39/12/3201.full.pdf
Questions/comments contact here
