A great case for craniocervical junction anatomy! Case performed in conjunction with Dr. Eytan Raz of neurointerventional radiology and Drs. Anthony Frempong-Boadu and Omar Tanweer of neurosurgery
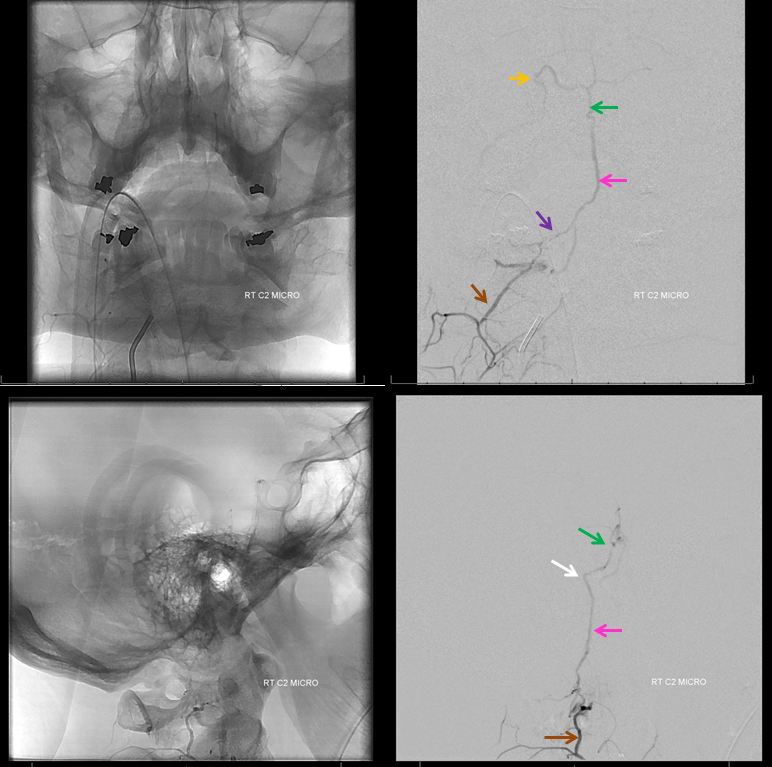
Patient presents with sudden severe upper neck pain and headache, photophobia. CT head negative. Catheter angiogram is ordered. Its a complicated case. Right vert injection shows an early vein (purple). It is not a normal structure at this point. The C2 nerve root (yellow) is likely supply. The innocent bystander odontoid arcade is white
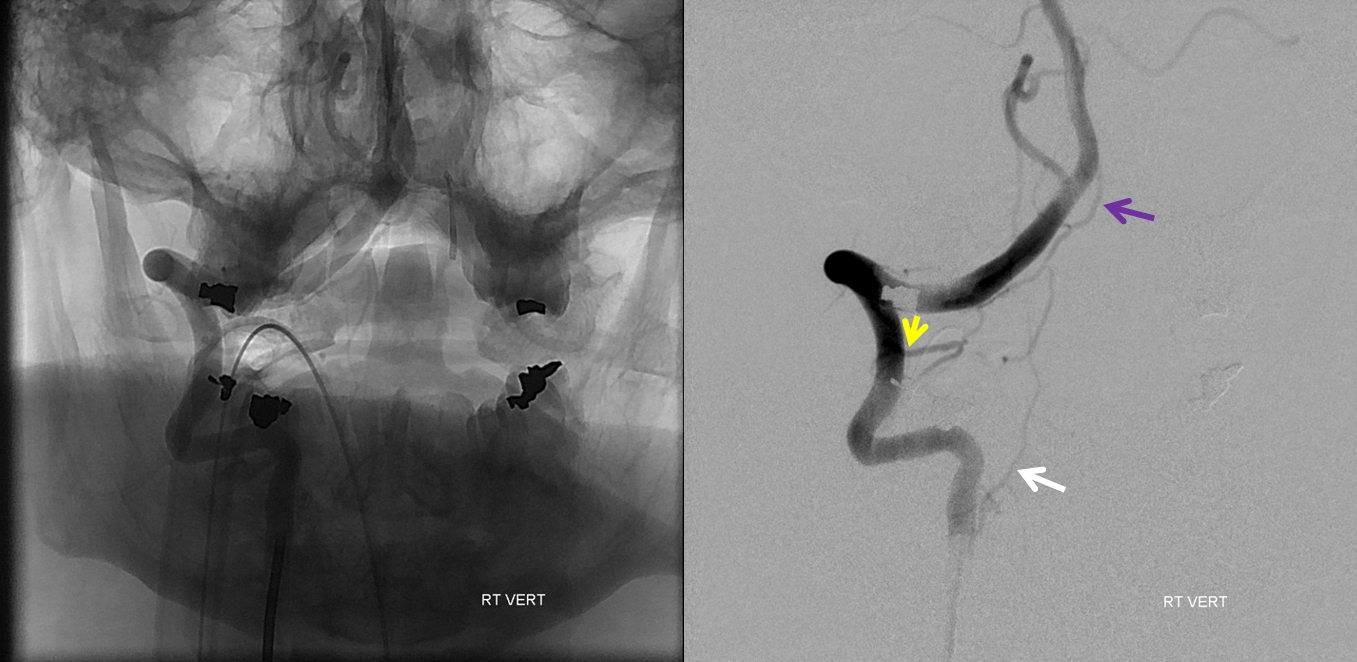
Lateral views. Same color arrows. Contrast is collecting in the dorsal epidural space (red arrows)
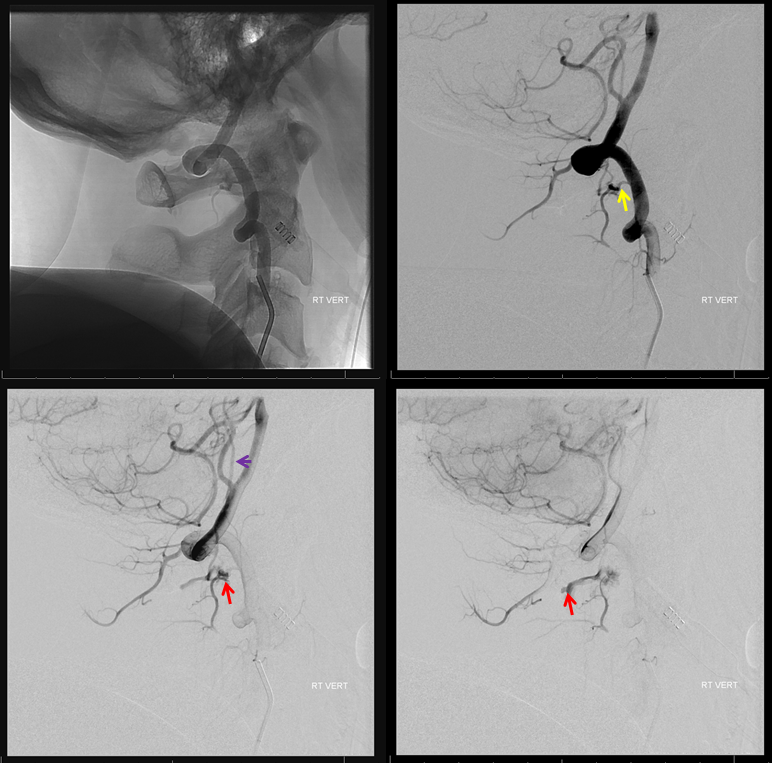
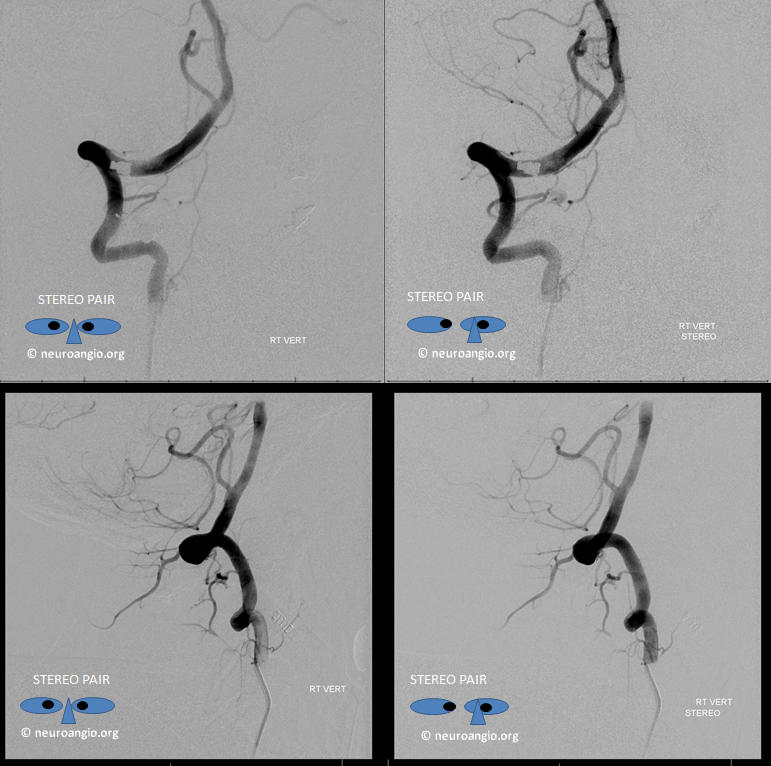
Stereo views
C2 segmental artery injection clarifies things a bit. The catheter tip is white. Retrograde opacification of muscular branch (connecting with deep cervical below) is brown. Also retrogradely opacified is the C1 branch (black). The fistula point is at the confluence of C2 and C1 branches (red). Proximal draining vein (C1 radicular vein) is purple. The premedullary vein is pink. Descending vein is blue (the one which drains into the epidural space)
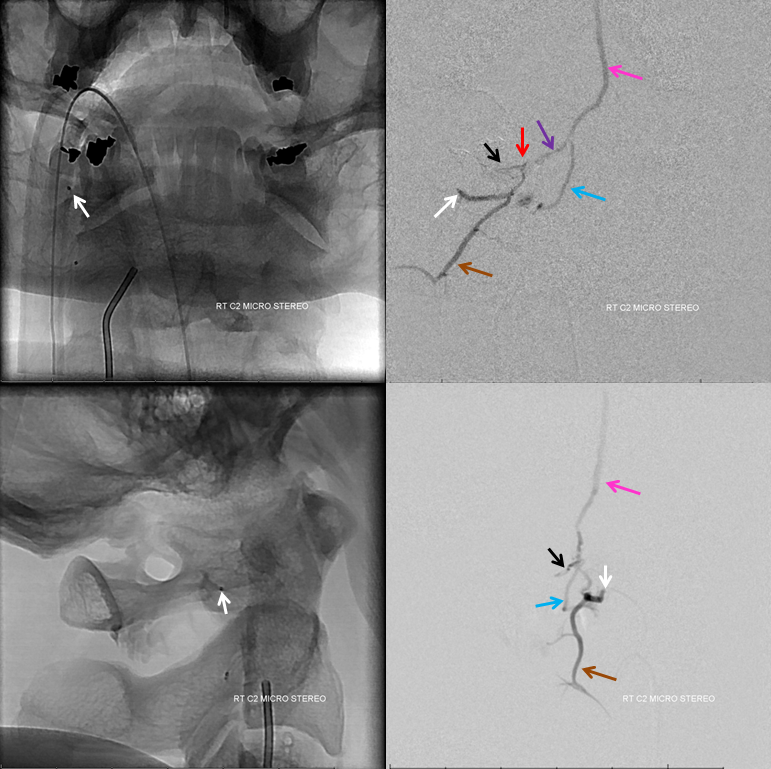
A stronger and longer injection better demonstrates cranial venous drainage into the anterior premedullary vein (pink) and onto the prepontine vein (green). Lateral pontine vein (yellow) ultimately drains towards the jugular bulb. The pontomedullary sulcus is shown by white arrow. C2 muscular branch is still brown.
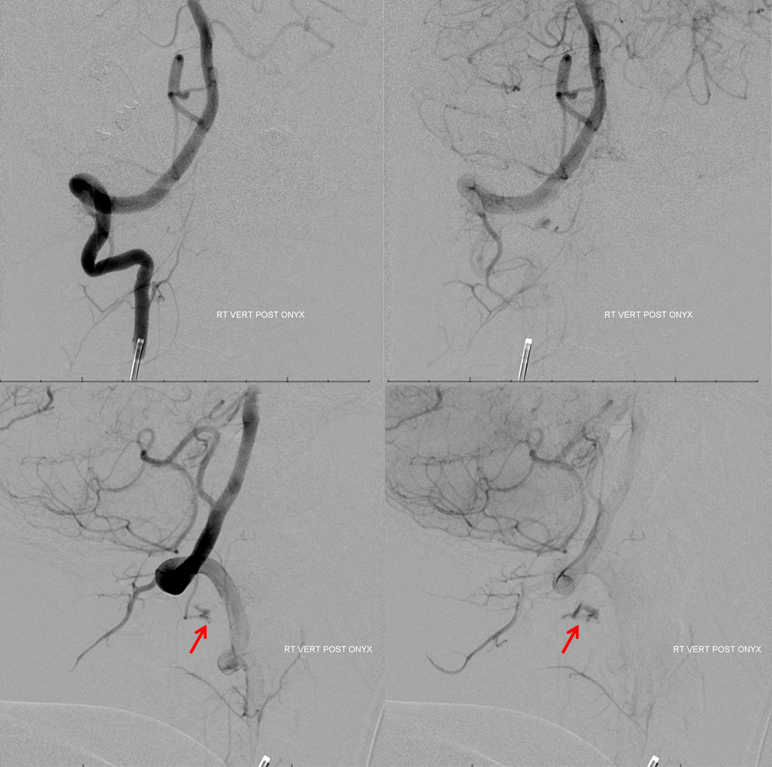
Given location we chose Onyx rather than nBCA. It did not reach the fistula before refluxing too close to the vert. The fistula is still alive with persistent drainage into the epidural space (red arrows)
We managed to perch the microcatheter (tip white arrow) in the tiny C1 branch ostium to get a picture. The descending C2 vein is blue. Reflux into the vert is red. Needless to say we did not feel too good about this embolizaiton position. We were also somewhat concerned about C1 level embolization because of the lateral spinal artery. It is never too far from this branch, and we turned out to be right.
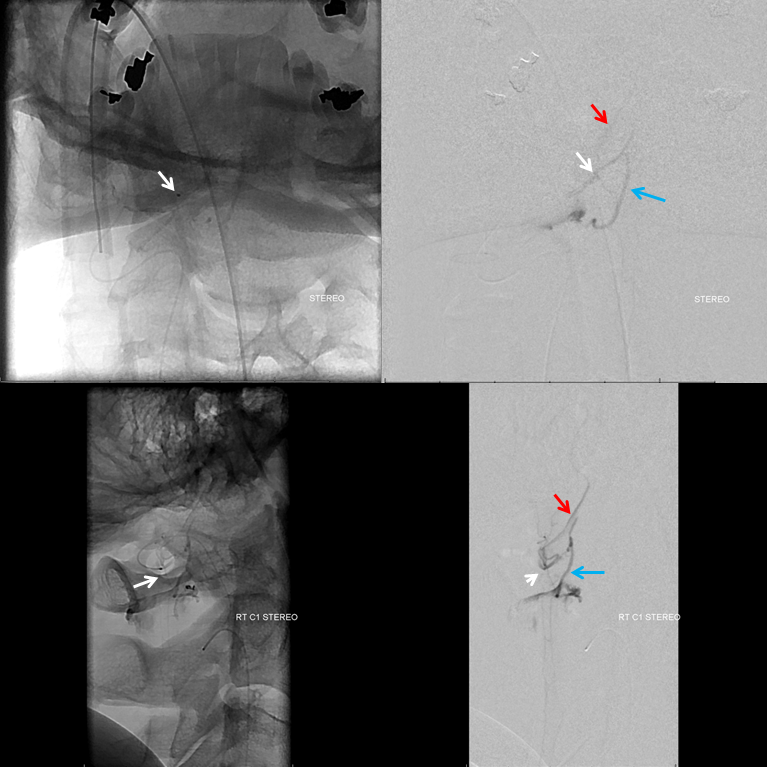
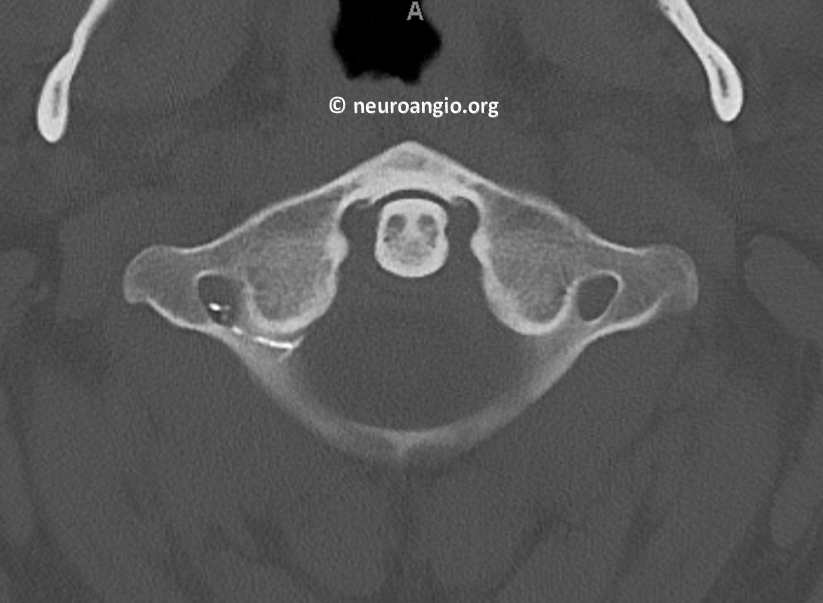
So, we decided to close the residual fistula surgically. We have the benefit of a hybrid Zeego room, which is key for small vessels like this one. C-arm is generally not enough. A post-embo CT shows Onyx in the C2 radicular branch.
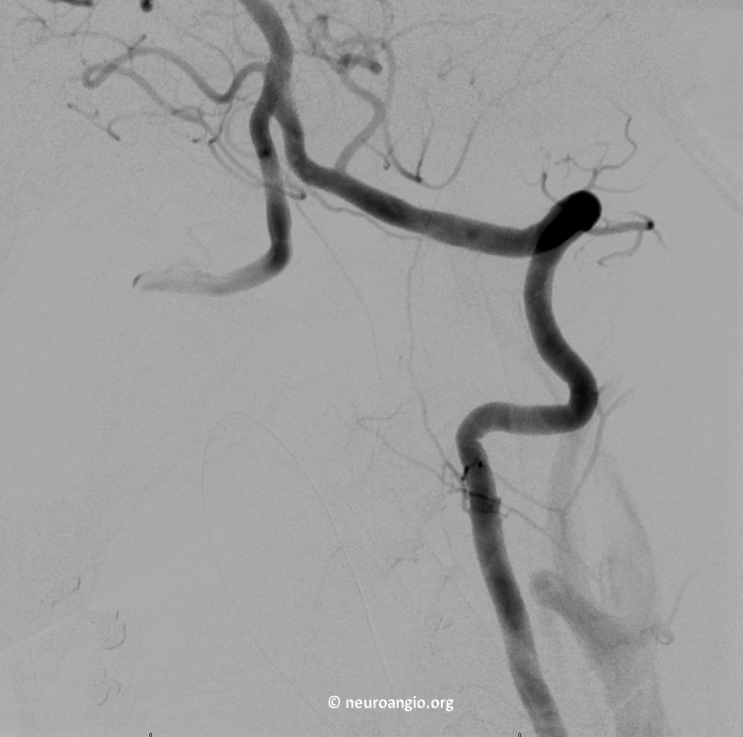
A pre-op right vert view (patient is prone, therefore the vert looks like its on the left, but it is not). Fistula is still very much alive and its cranial drainage is more visible. That’s what usually happens — unless liquid embolic permeates fistula point it will just recruit more of remaining arterial supply
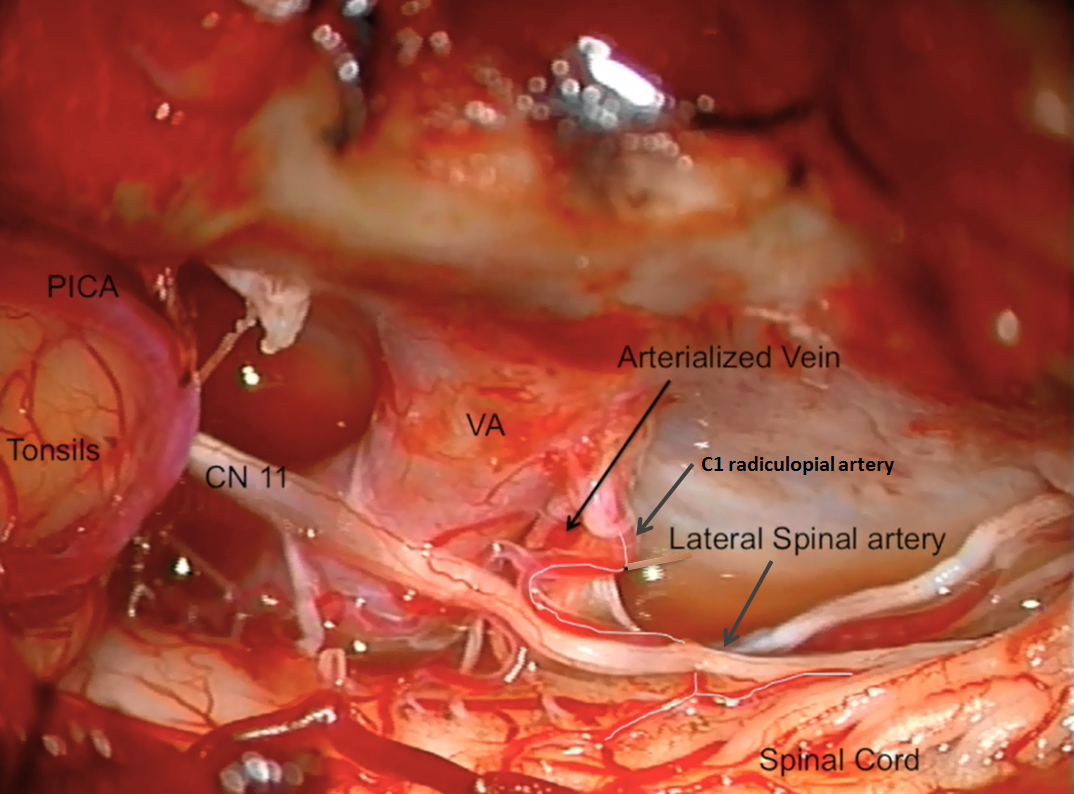
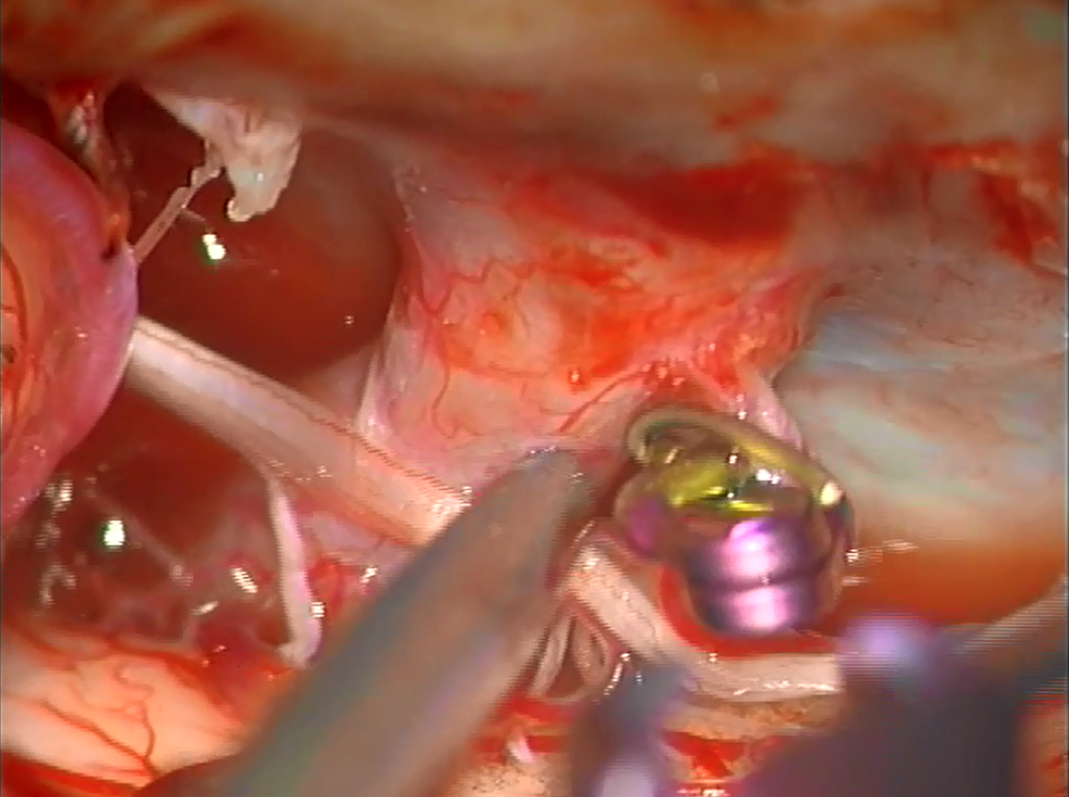
A beatiful intraoperative view, from posterior and right lateral. The very proximal intradural vert. Inferior to it are two vessels — one is the arterialized C1 radicular vein which is draining the fistula. However there is also another, which was not seen on the angiogram. It is our friendly C1 radiculopial artery supplying the lateral spinal artery. In most cases the whole thing would be named “lateral spinal” or posterior spinal, but technically the branch along the C1 nerve root which supplies the lateral spinal is the radiculopial branch. Either way, this picture shows why it is usually not a good idea to push Onyx or glue into the C1 radicular branch.
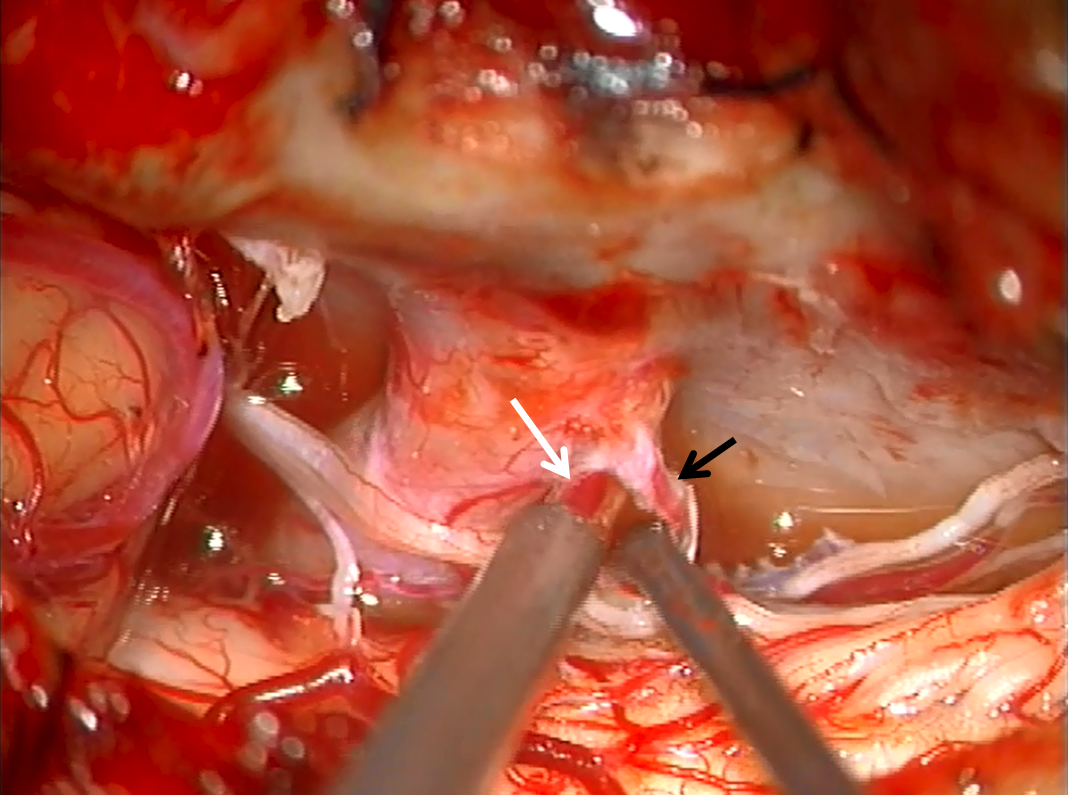
The sucker is on the arterialized vein (white) with the probe gently retracting the radiculopial artery (black)
IC Green injection showing the lateral spinal and some cord
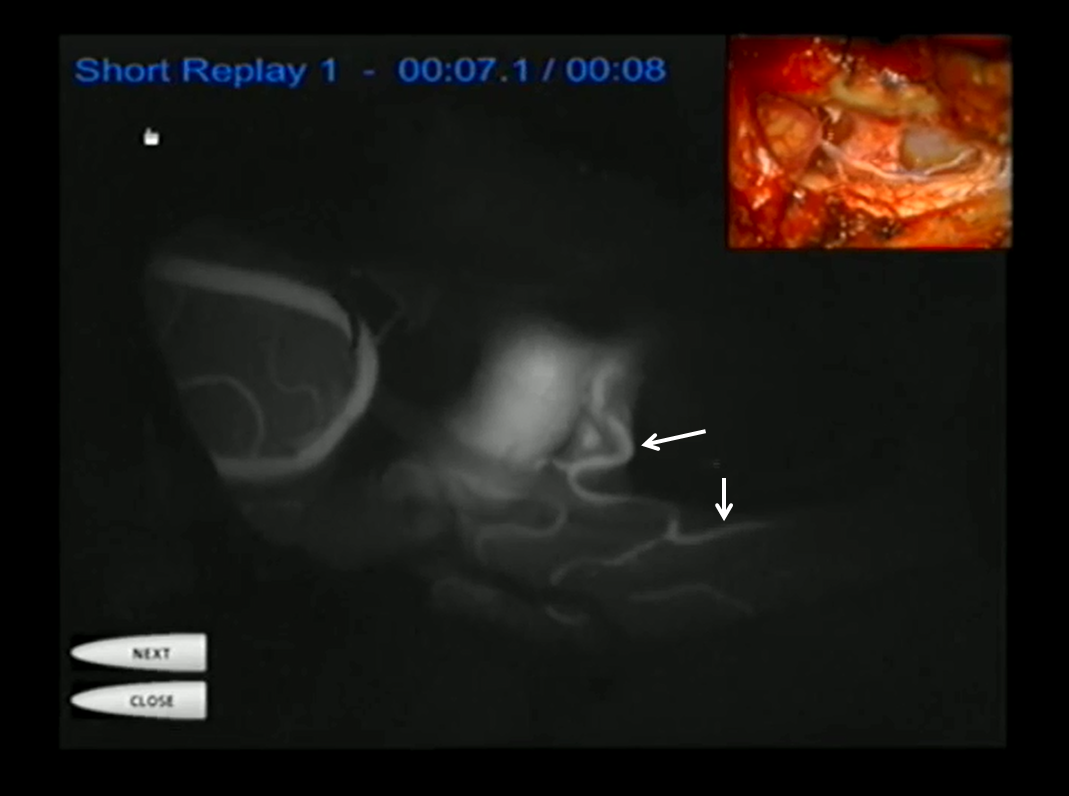
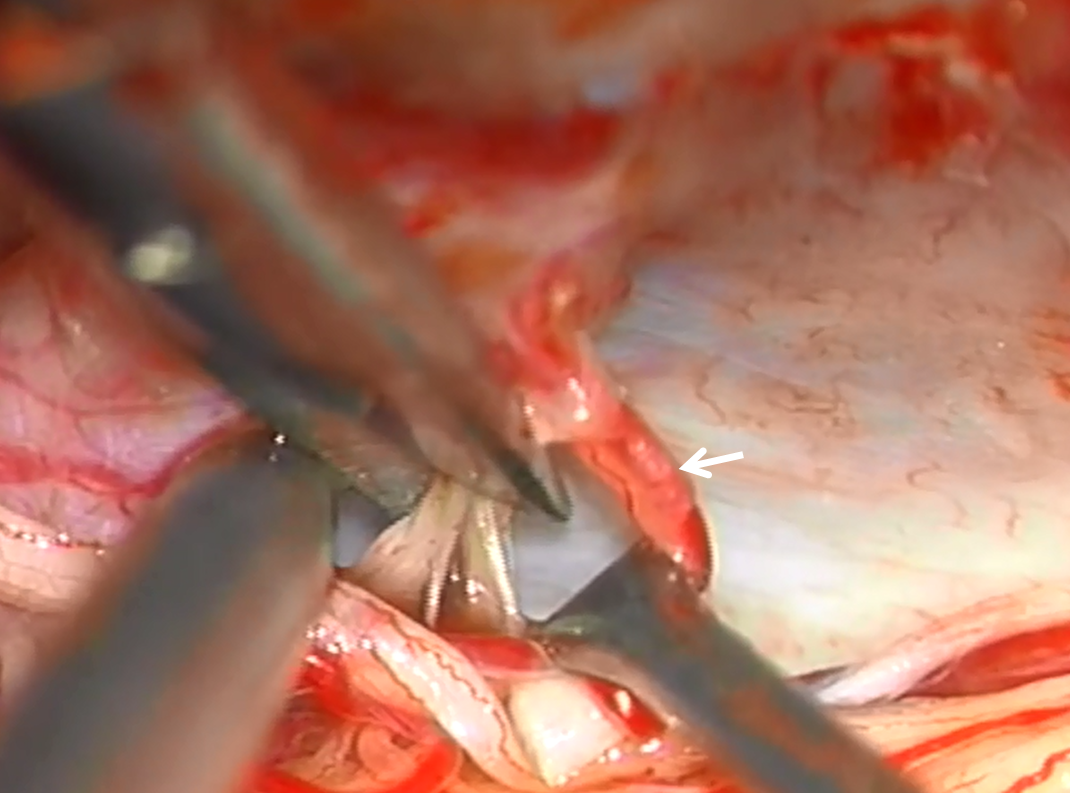
A temporary clip is placed on the draining vein.
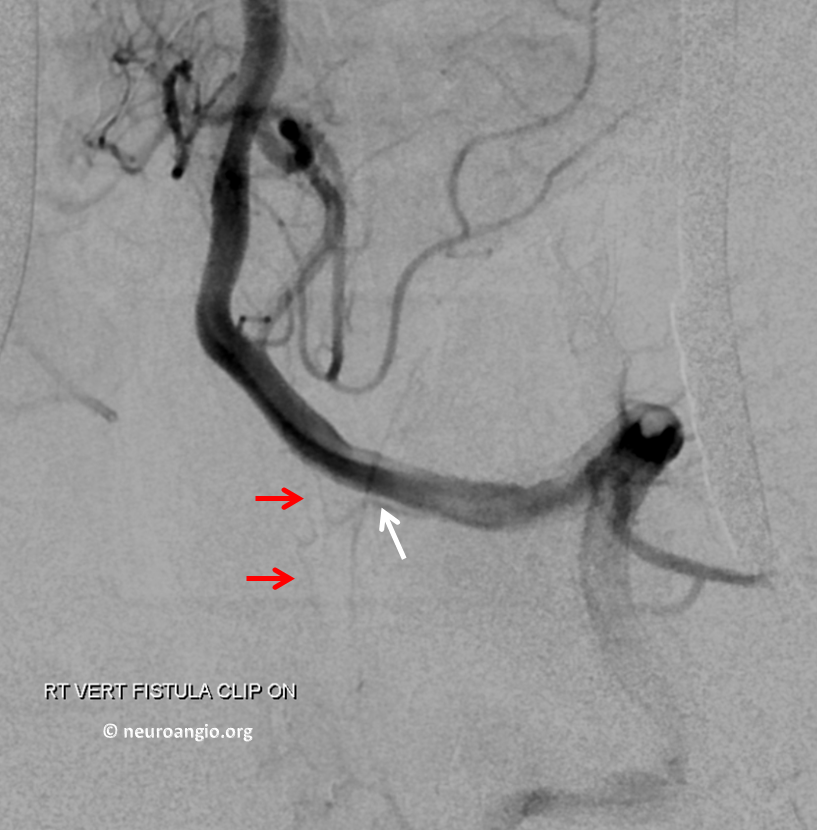
Now we shoot an intraop angio (clip white arrow)

The fistula is gone. But there is more. Now we see the radiculopial (white) and lateral spinal (red) arteries! Why? Probably because dissection and retraction of neck tissues allowed for better visualization. I do not think it is because of steal or competitive flow related to the fistula. For once, there is no reason to believe the body can’t supply both. Also, the lateral spinal did not look too starved under the microscope. Finally, the patient never had any clinical signs of lateral cord ischemia. But it is an angiographic correlate of what is seen surgically. Had we embolized from C1 position a lateral cord syndrome would likely have resulted.
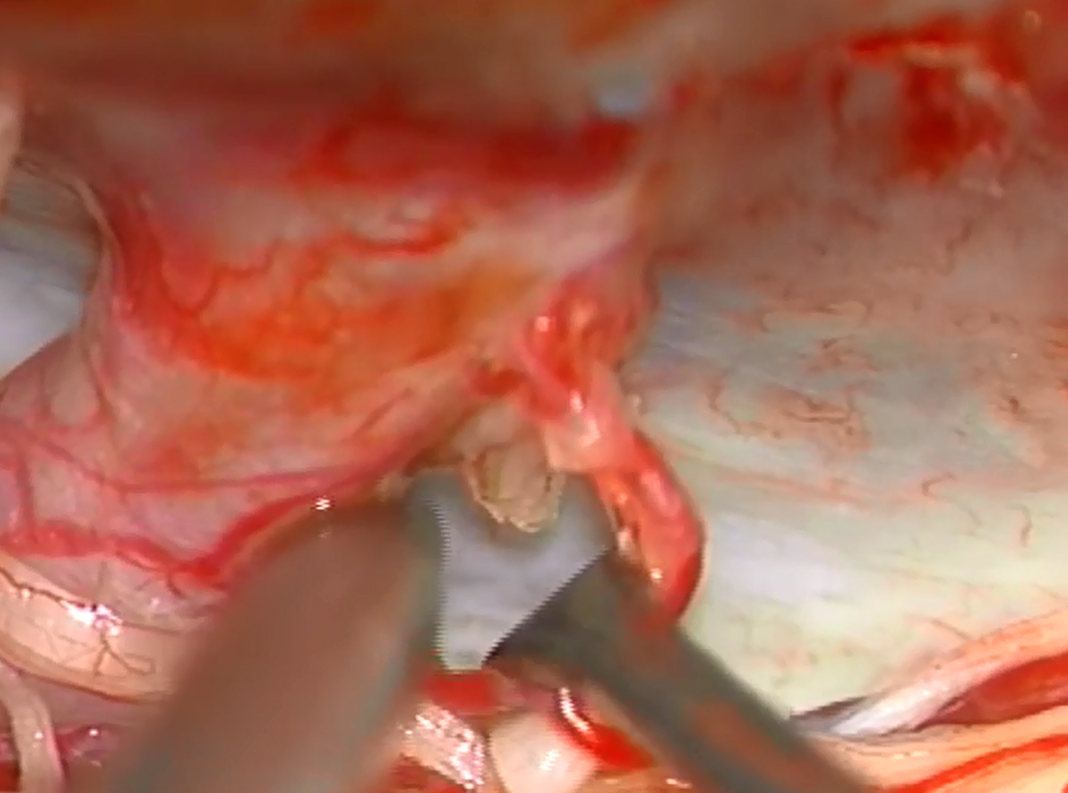
The fistulous vein is coagulated and ready to be divided. The lateral spinal contribution is intact (white arrow)
Good bye fistula
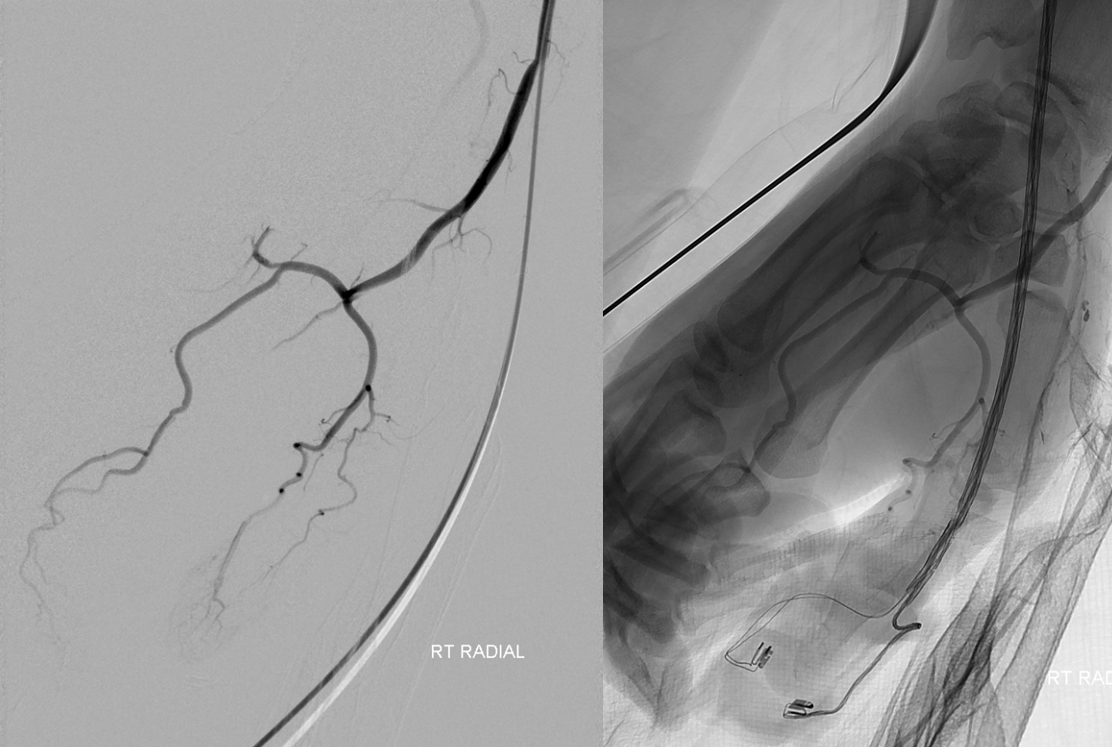
So, how do you do a prone intraoperative vertebral injection? One way is to put a long sheath into the femoral artery and bring it to the lateral aspect of the leg. But a much easier way is to go radial. In fact, all of this patients angiograms were done through the right radial approach. No femoral access ever. Much more convenient to do this in prone position.
Here is a YouTube Video, courtesy of Dr. Omar Tanweer
Conclusion: This is a case of small and perhaps complicated vessel anatomy in a critical location. They may not look very dangerous, but C1 and C2 branches are very treacherous because critical spinal arteries are never too far and lateral medullary and lateral spinal syndromes are some of the most frustrating deficits patients face in terms of persistent sensory disturbances. So, be careful.
See companion cases: Lateral Spinal Artery Aneurysm, Posterior Fossa Hemorrhage Hypoglossal Fistula
Other pages: Vertebral Artery, Lateral Spinal Artery, Spinal Arterial Anatomy
