Lateral Spinal Artery / Posterior Spinal Artery of the Upper Cervical Spine and Cervicomedullary Junction
Most health care professionals have never heard of the lateral spinal artery. Some have heard of it but are not sure whether or not it exists. Located on the lateral aspect of the upper cervical spinal cord and the cervicomedullary junction, it is not a region commonly exposed to the OR lights, and so direct visualization is not common. Nevertheless, the lateral spinal artery (two, in fact –left and right) does exist, and is an important vessel from both embryologic and pathophysiologic perspectives.
Confusion regarding the lateral spinal artery is created by the nomenclature. Shouldn’t we just call it “posterior spinal” like we do everywhere else? Probably would have been better to do that and get rid of the confusion rather than follow punctilious rules. Because, strictly speaking there is a difference. For the purists out there, the “posterior” spinal artery is located posterior to the dorsal nerve rootlets. Lateral spinal one is anterior / ventral to them and in-between the dorsal and ventral ones. Really just on the lateral aspect of the cord. There you have it now.
Many texts depict the spinal cord as supplied by one large anterior spinal artery and two smaller posterior spinal arteries. This is horseshit. The posterior spinal arteries are in reality highly variable and often discontinuous channels — except at the rostral and caudal ends of the spinal cord, where the larger bulk of cervical and lumbar enlargements leads to more need for a beefier arterial presence. At the caudal end, the posterior spinal arteries are sometimes called “rami cruciantes“. At the rostral end, the lateral spinal artery usually serves the function of posterior spinal artery (see Spinal Arterial Anatomy Page and Vertebral Artery page for important background information).
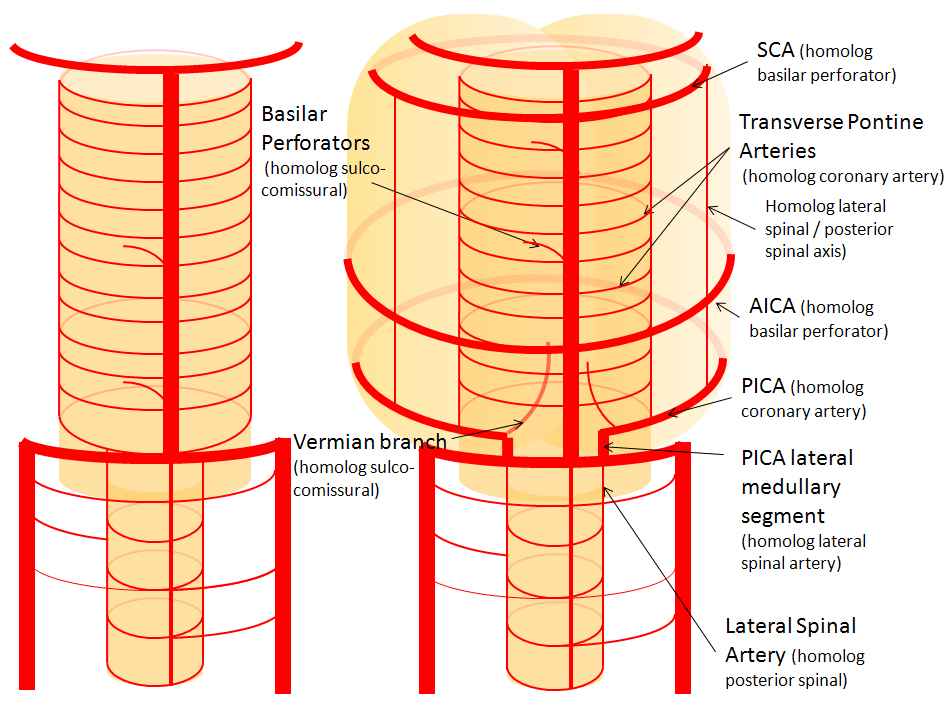
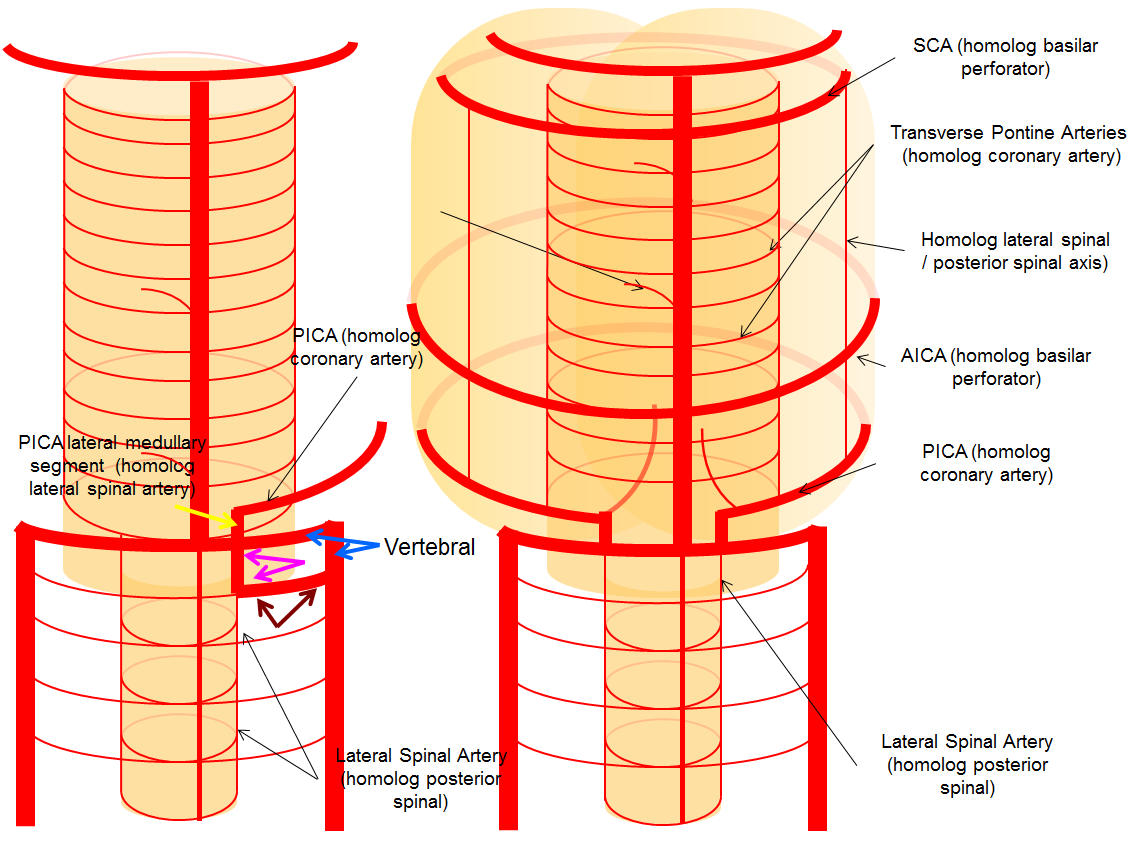
Cranially, the lateral spinal artery is related to the PICA in a very important way. The PICA is, embryologically, a cervical rather than cerebral, vessel. It is, so to speak, secondarily recruited to supply the cerebellum in the “higher” species. However, its primary territory is the lateral medulla. The same thing happens more cranially, where out of a large number of pontine perforators one or two may be selected to also supply the cerebellum, and are thus known as AICA vessels. The AICA is simply a pontine perforator vessel which has captured cerebellar territory. By analogy, we come to a radical idea — the PICA is a hypertrophied lateral spinal artery, participating in supply of the natural lateral spinal artery territory (lateral medulla) as well as the cerebellum. In reality, this is nothing too radical — we know that organisms tend to adapt existing vessels to new needs rather than developing brand new ones. The lateral spinal, being on the lateral aspect of the cord, evolves to supply the cerebellum, while the ventrally-located anterior spinal artery evolves into the basilar artery, whose hypertrophied branches ultimately take care of the upper cerebellum and posterior cortex. One can often see small vessels “originating” from the medullary loop of the PICA and running along the lateral aspect of the cord — which are interpreted as PICA giving rise to the posterior spinal artery. The embryology suggests the opposite — it is the little lateral spinal artery which is the parent of the relatively gigantic PICA.
This insightful theory allows one to understand many PICA and vertebral artery variations. For example, a C1 or C2 origin of the PICA is simply a prominent lateral spinal artery giving rise to the PICA. Occipital origin of the PICA is a case of radiculopial artery arising from the occipital artery and ending in the PICA. “Duplicated” vertebral artery with an intradural segment — the latter is the lateral spinal artery.
The PICA-lateral spinal continuum is an important collateral pathway in reconstitution of the PICA following upper cervical vertebral occlusion (usually dissection-related).
Illustrations
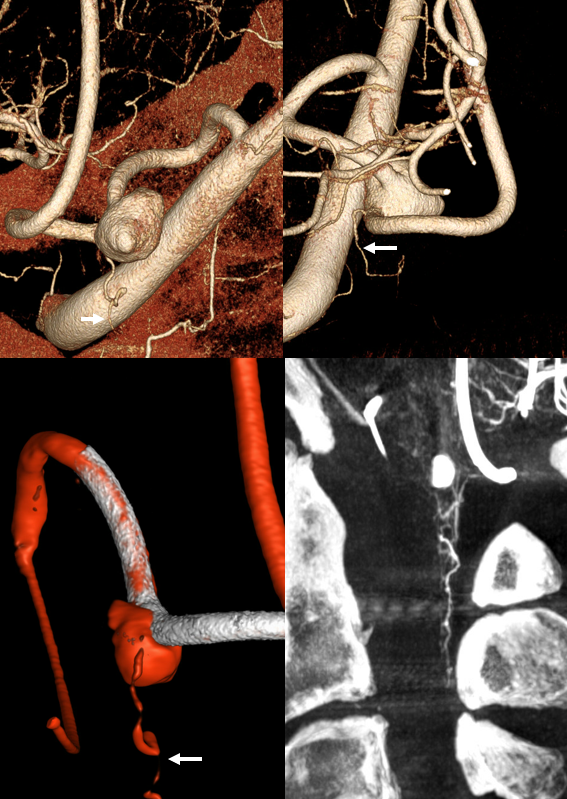
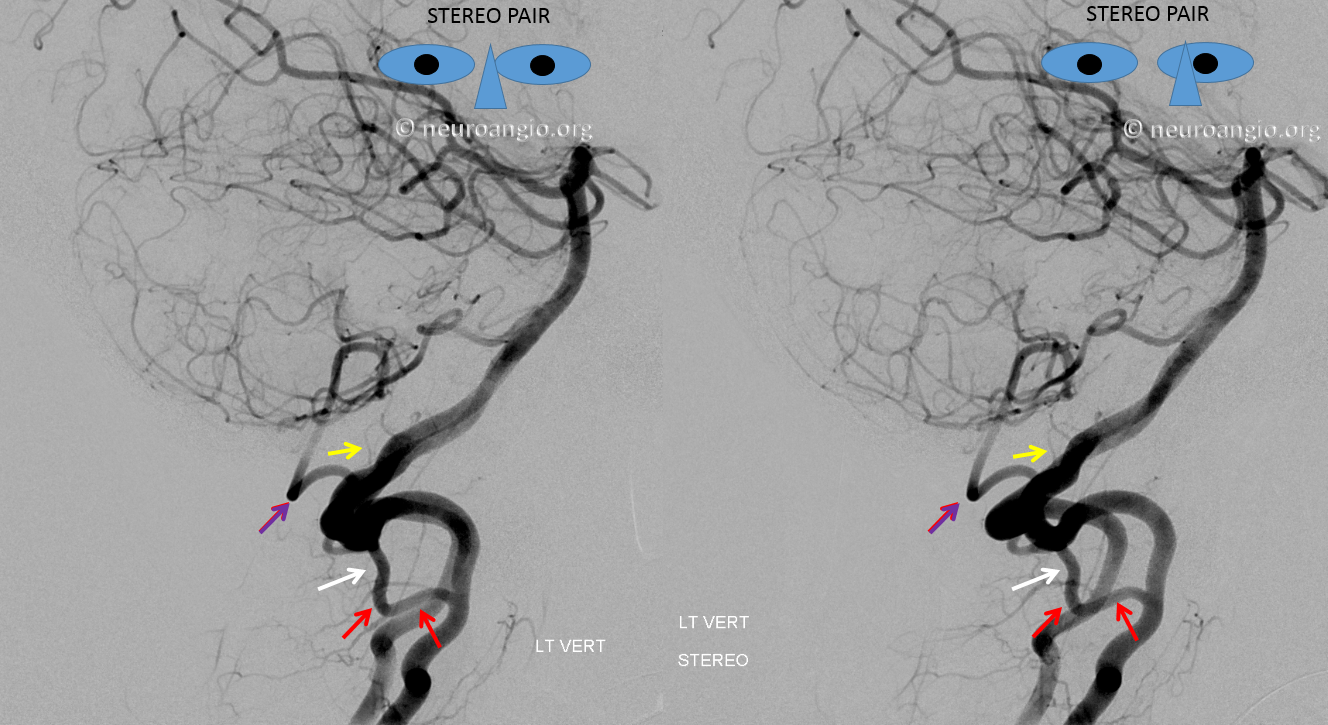
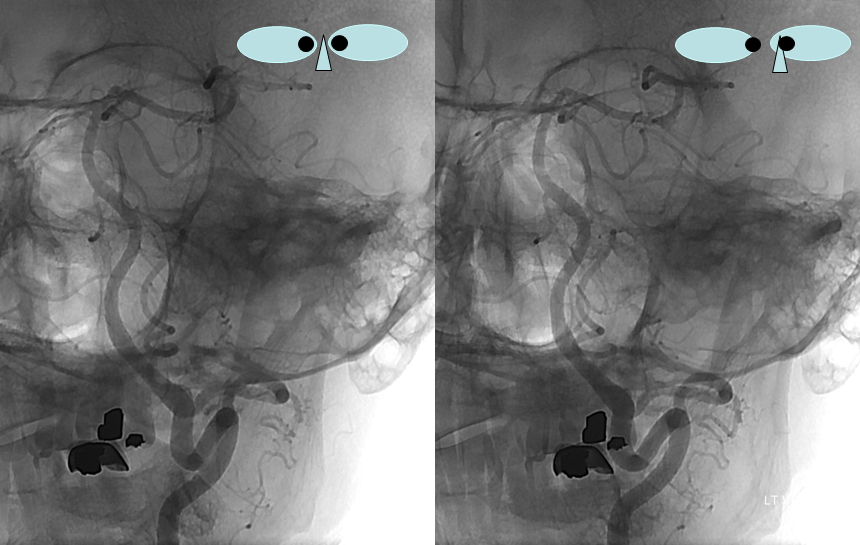
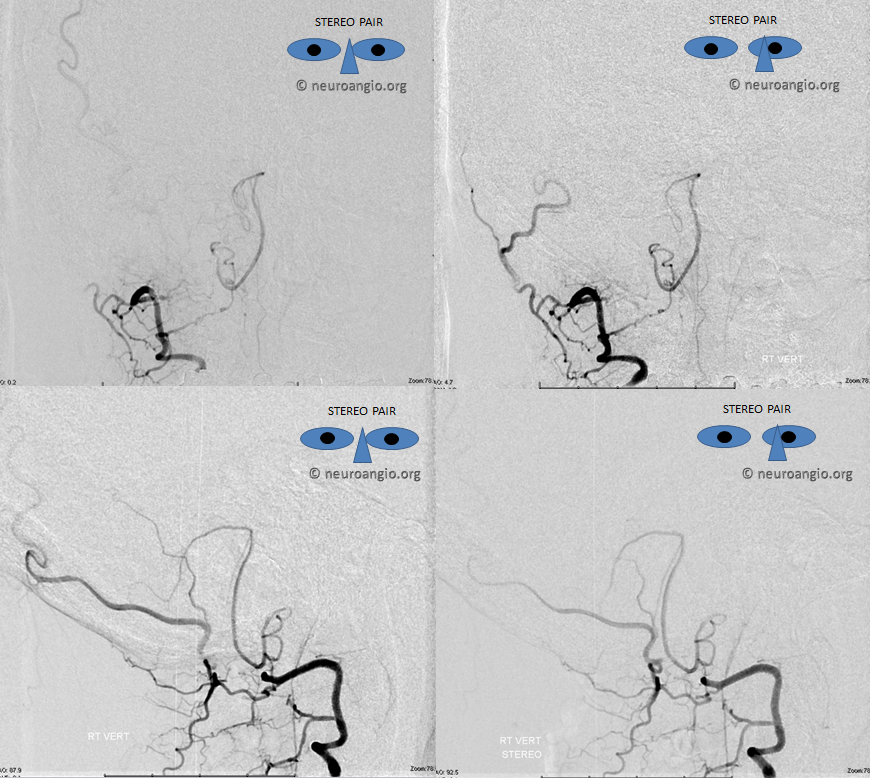
Perhaps the largest lateral spinal artery we’ve seen. Notice typical location at the posterior aspect of the cord on lateral views and an off-center, lateral location on the frontal views. One should always suspect, if an artery is unusually large, that it might be supplying fistula. In this case we did not see a fistula. Also, it would be somewhat unusual if there was in fact a fistula not to see other sources closer to the fistula site, which would need to be located at the lower end of the artery.
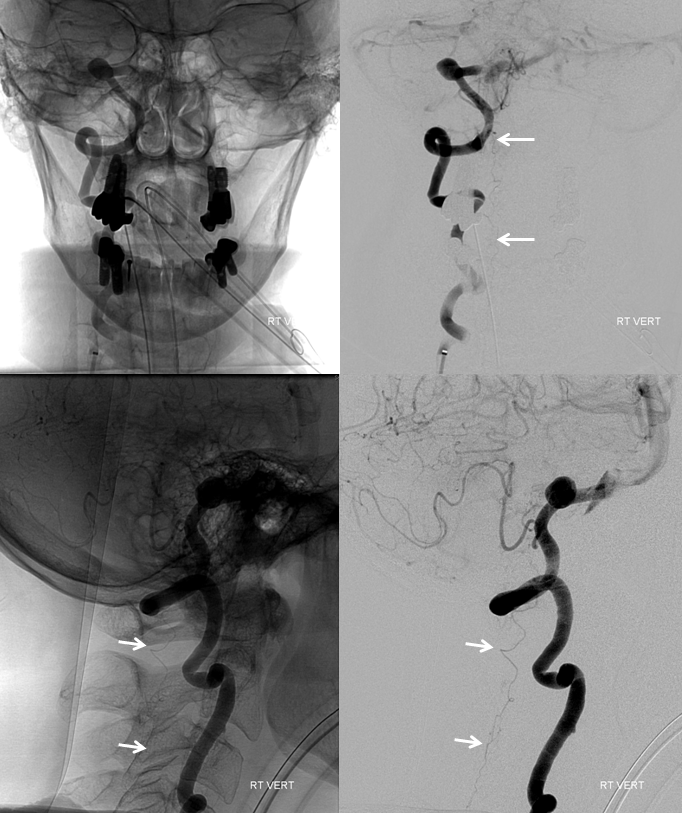
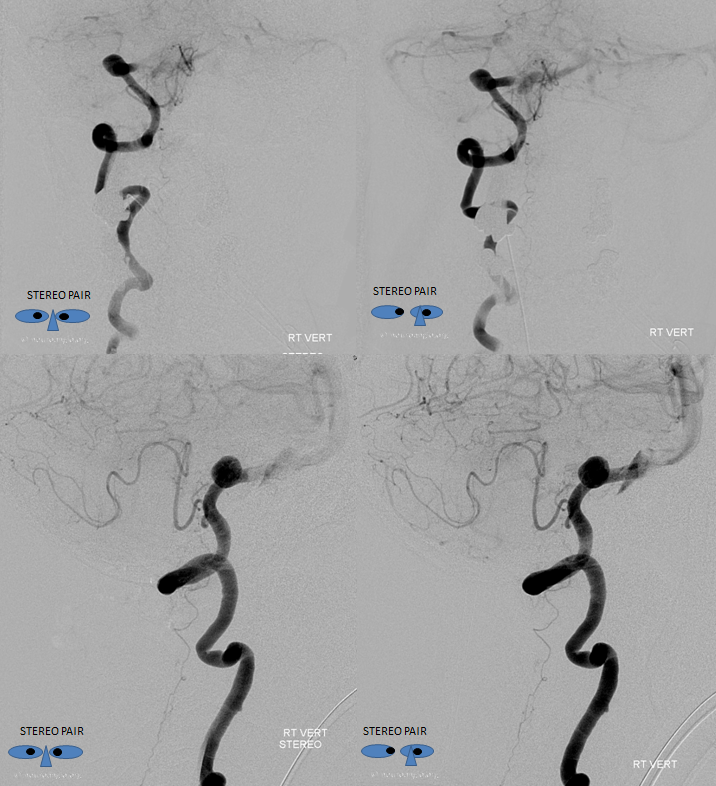
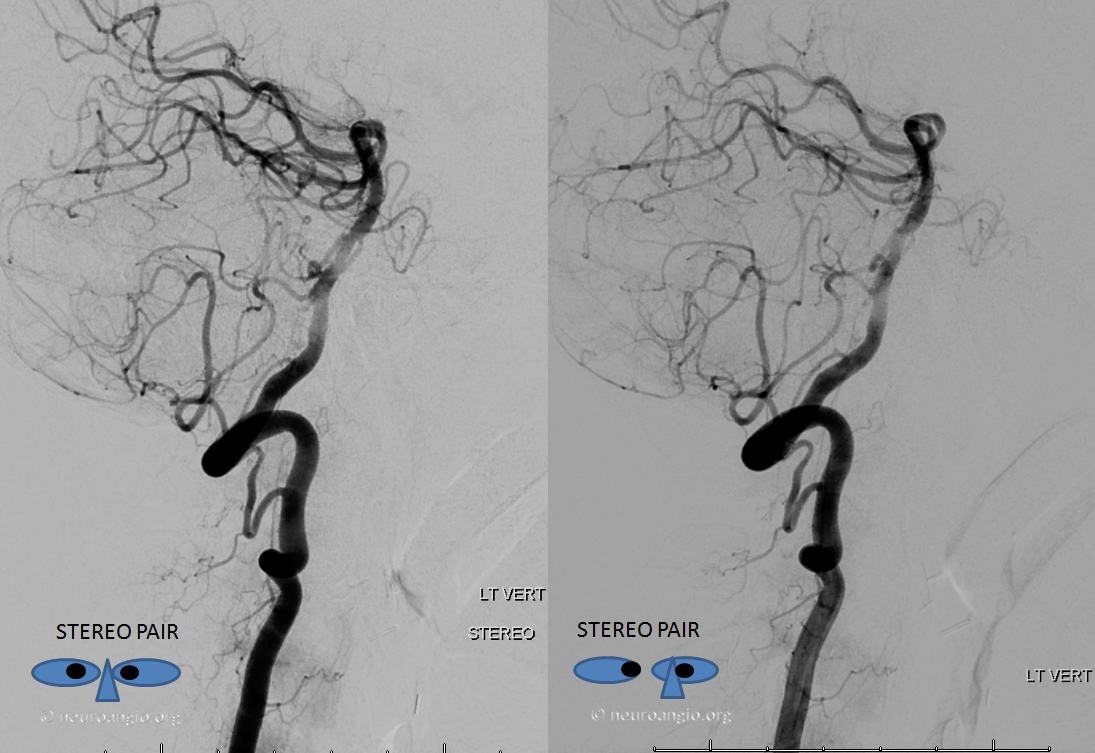
Obligatory stereo images, complements of neuroangio.org Learn to view stereo!
Anaglyph stereo
After Pipeline embolization of the aneurysm, there is a bit of spasm in the vert. A stronger injection allows for visualization of the anterior spinal artery (yellow) near the VB junction, which happens to arise from the left distal vert and therefore is only seen from the right with a strong injection. This case was done by Dr. Eytan Raz via a right radial artery approach, together with Dr. Eric T. Aaltonen. The arch was truly terrible, and we were very happy to go radial here. A 5F navien from radial into the upper cervical vert, and a Phenom 027 for delivery.
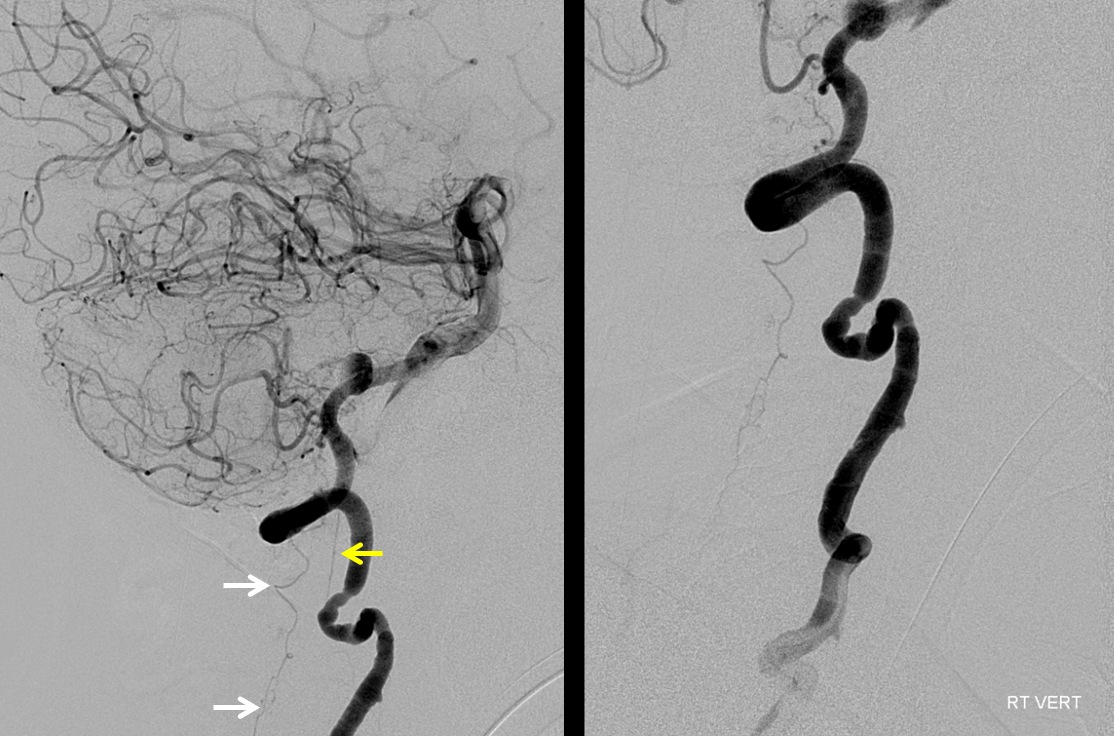
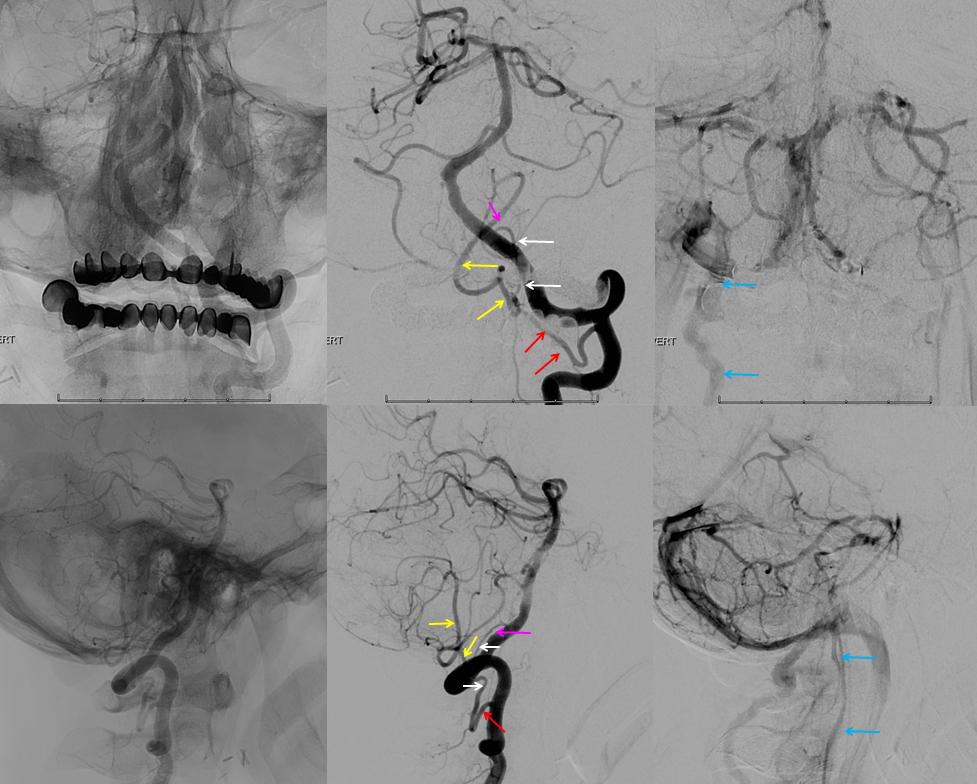
Anterior and posterior (aka lateral) spinal arteries
Look at this! Ridiculously “one-sided” origins of all three major systems — the anterior spinal and both posterior spinal arteries are supremely well-seen — originating from distal right vert (asa) and both PICAs (posterior spinals). This is most unusual. Frontal views show duplicated upper cervical asa (white arrowheads), long contiguous posterior/lateral spinal arteries (dashed white arrows), and faintly seen sulco-comissural arteries (black dashed arrows)
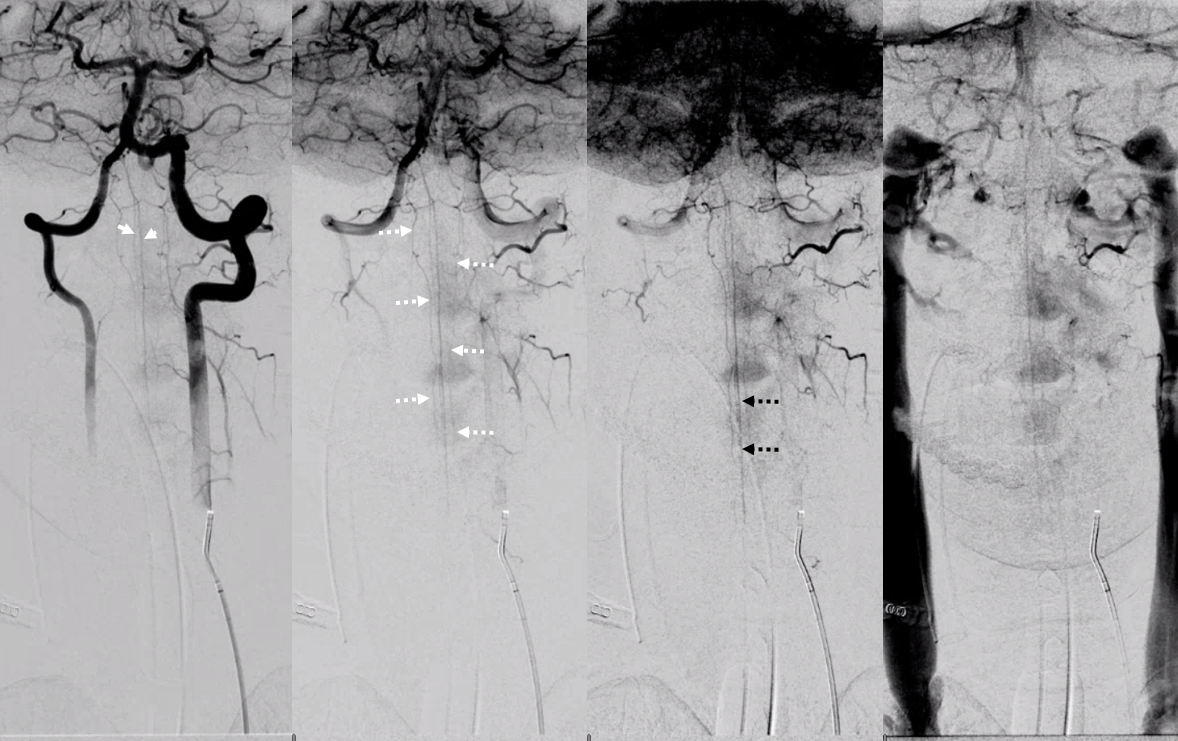
Lateral views show extremely well the posterior spinal axis (white dashed arrows), the position of spinal cord in the osseous spinal canal (leftmost image), a beautifully seen faint line of sulco-comissural vessels terminating in the depth of the ventral median sulcus (black dashed arrows), and circumferential / transmedullary spinal veins (black arrowheads)
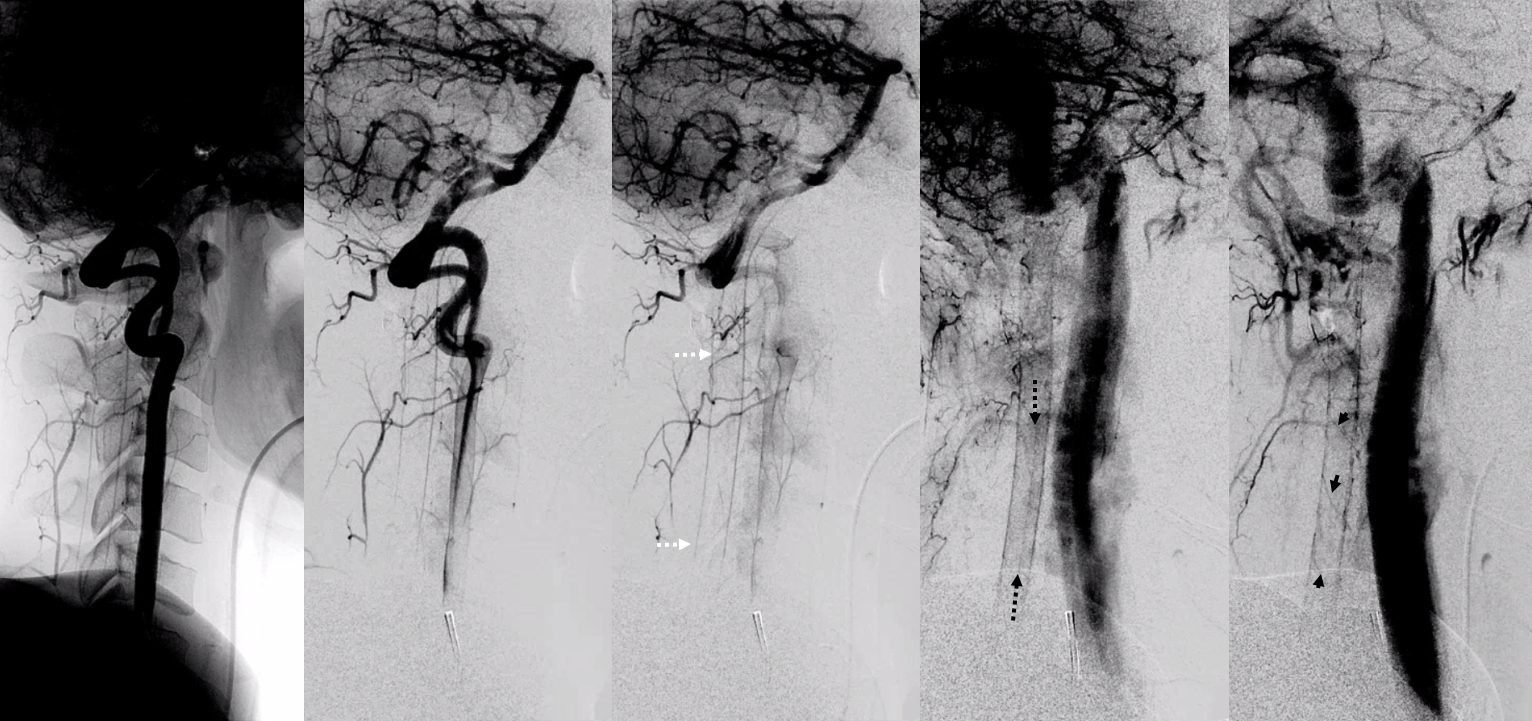
Rotational angiography/DYNA shows bilateral vert origins of anterior spinal axis (white arrows) and lateral / posterior spinal arteries (dashed white arrows) with several prominent coronary arteries — short arteries running transversely along the circumference of the cord (white arrowheads), opacifying the posterior cord (black arrows)
Anaglyphs
DYNA Illustration
Another case of large lateral spinal on the left, coexisting with a prominent upper cervical anterior spinal on the right. No pathology. DYNAs can be fantastic for this.


PICA origin posterior/lateral spinal artery
We’ve been showing them off vert mostly but there is PICA/lateral spinal homology and they do come of PICA — especially when the latter origin is classic proximal intradural.
Not much can be seen from 2-D DSA
However, the DYNAs show the vessel well. Again, be careful when you think of PICA sacrifice — get a high quality image to see what’s going on before you sack’em
Here is a nice case of a bihemispheric PICA stroke — see full case “Bihemispheric PICA stroke with Lateral Spinal Artery PICA reconstitution” on the Instructive Cases page
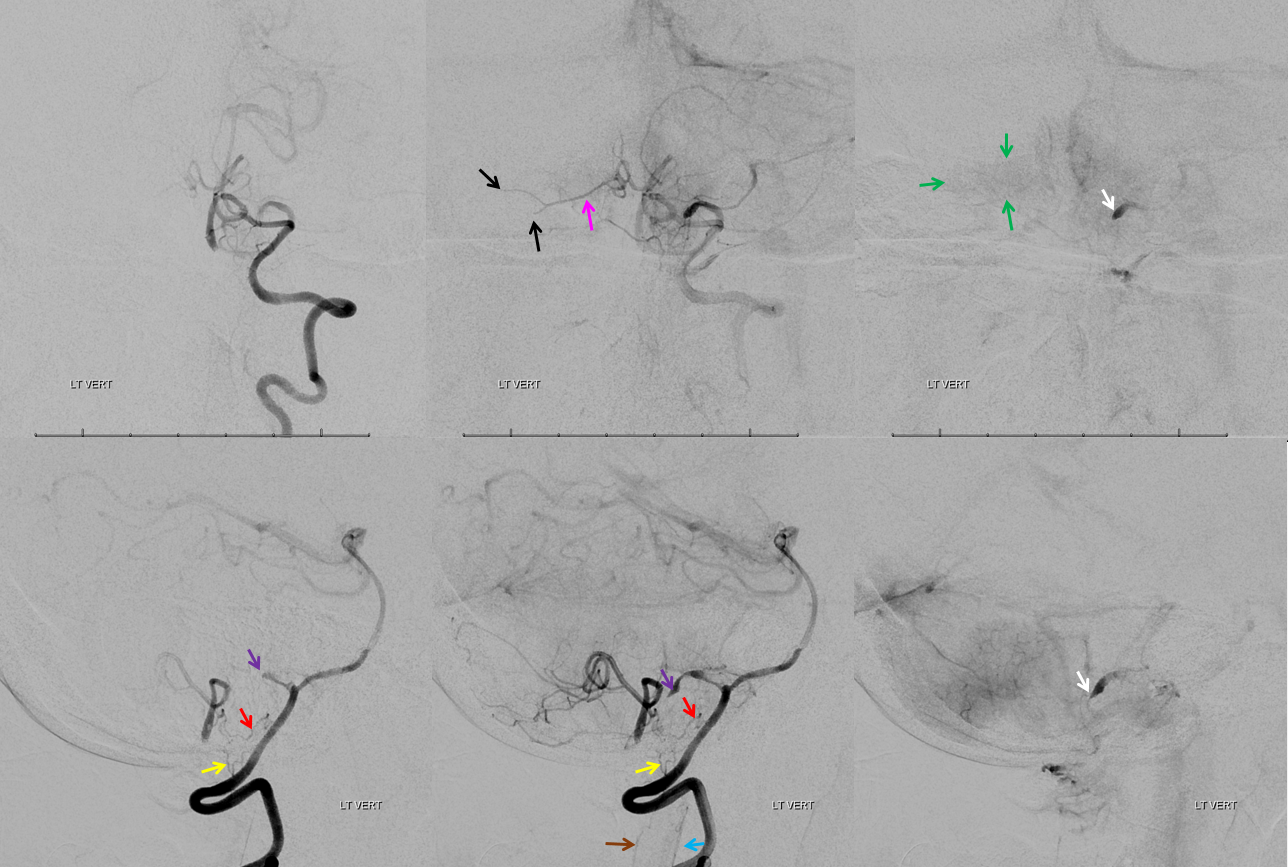
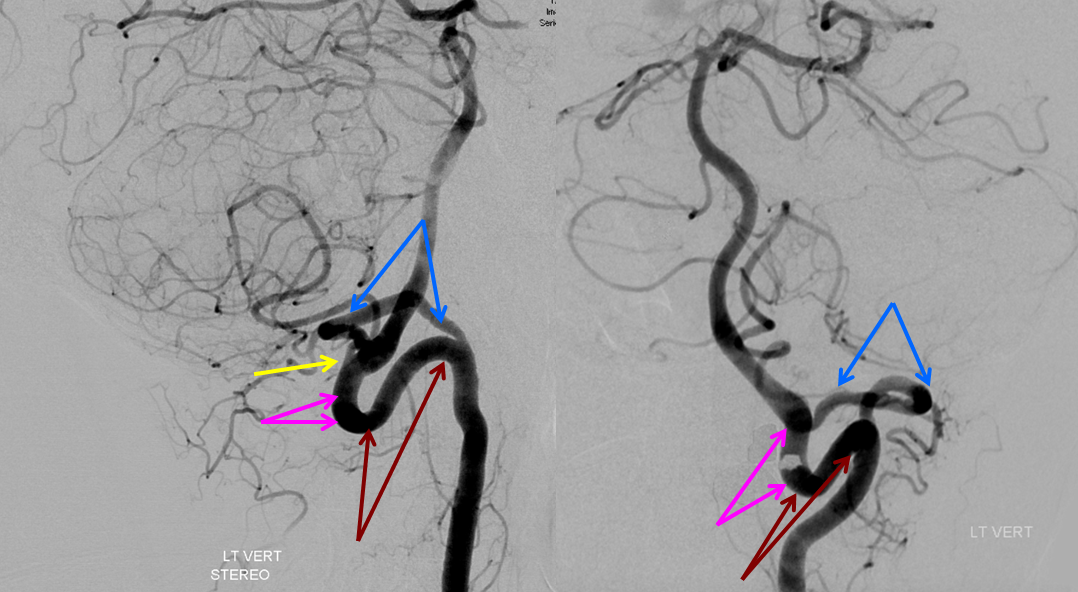
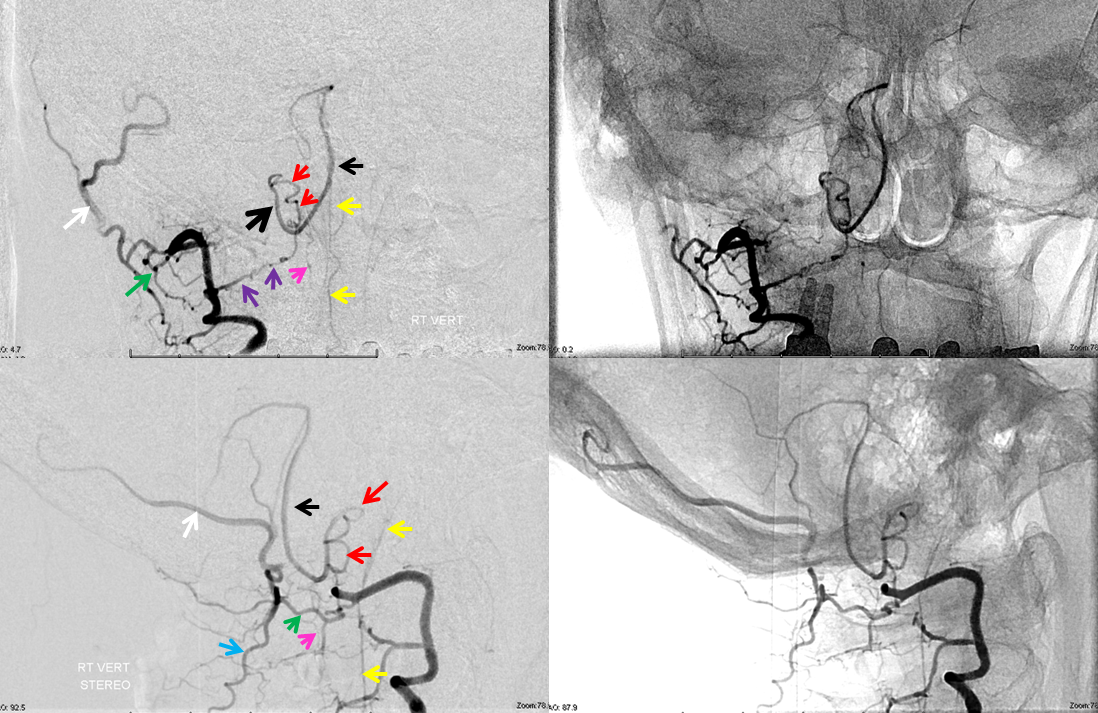
Frontal and lateral angiographic views show occlusion of the left PICA (white arrow) beyond the medullary segment (purple arrows). Notice clot in the proximal medullary segment, best seen on lateral views. The is a dominant large PICA with variant bihemipheric supply (pink and black arrows). Notice truncated appearance where black arrows are corresponding to distal embolic occlusions. the parenchymal blush is outlined by green arrows. How is the PICA reconstituted — the most common way it is — via the Lateral Spinal arterial network at C1 (yellow) and proximal intracranial (red) segments (also see examples below). Notice inferior component of the lateral spinal artery (brown arrow) just below its C1 segment (red arrow). Brown arrow points to the more typical length of the lateral spinal artery, when seen angiographically. The anterior spinal artery is shown by blue arrow, and is of course anterior to the lateral spinal artery. This kind of reconstitution has a propensity to form flow-related Lateral Spinal Artery Aneurysms so follow up is needed.
Lateral/Posterior Spinal Arteries
Finally, here is the rare threesome — anterior, lateral, and posterior. It just so happens that both lateral and posterior are supplied via a single trunk off the PICA (so really its in the lateral spinal family here). The anterior-most vessel (ventral to the ASA) is the odontoid arcade
Not telling you what the arrows are — that’s the homework

Axial DYNA images — stop and scroll thru individual frames
Extradural (C1) origin of PICA — the most common PICA origin variant – angiographic views of C1 origin PICA (red arrow), and diagrammatic representation of this disposition, highlighting the lateral spinal origin of PICA. The red arrow points to the lateral spinal portion of the PICA.
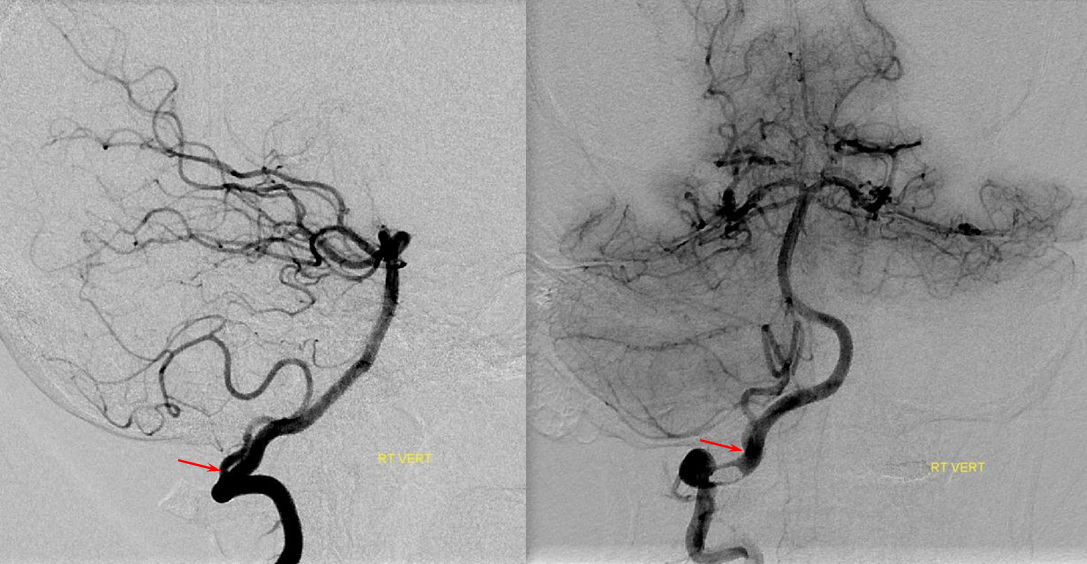
Diagram of the same
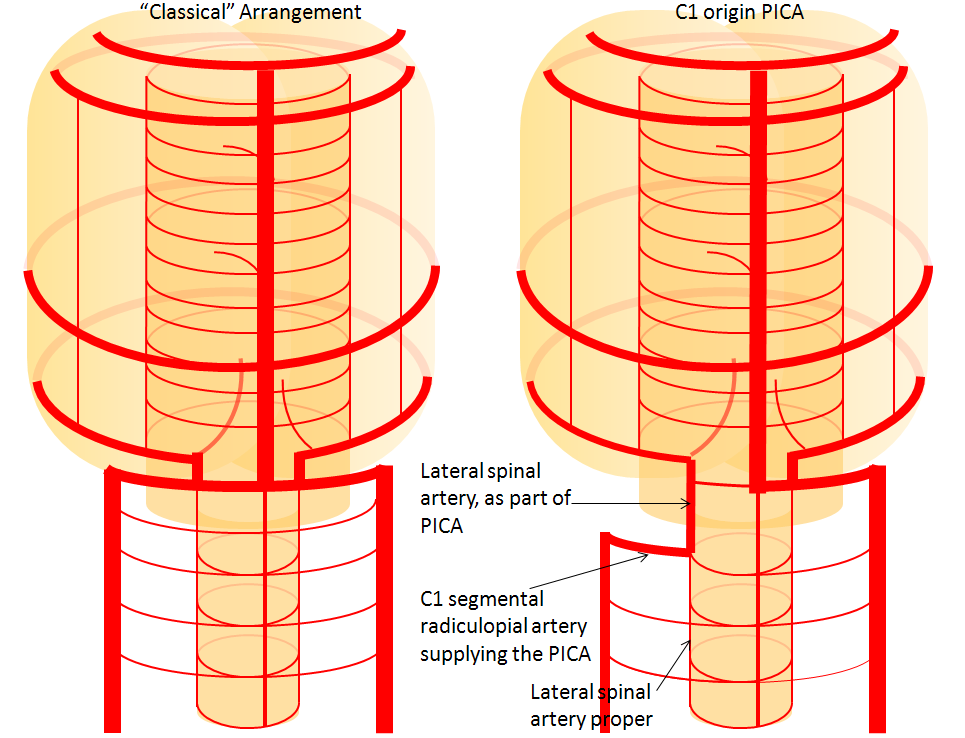
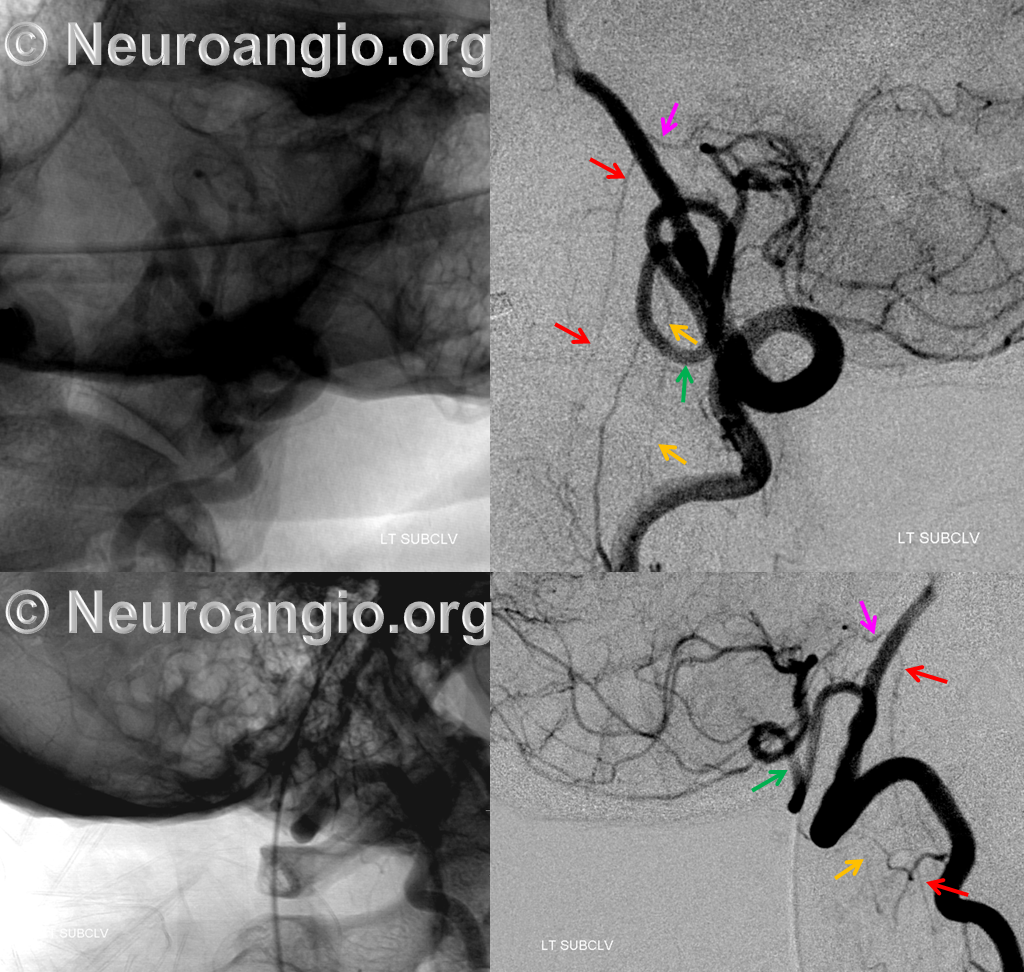
C1 origin PICA with medullary segment “perforator” at classical PICA origin — illustrating the concept of PICA relationship to the lateral medullary artery, and the role of segmental organization. In this patient, dominant PICA originates at the C1 segment (red). As is often the case in such situations, the medullary territory normally supplied by the PICA is now under control of a small medullary “perforator” (yellow) which takes off at the location where classical “PICA” would come from. The clinical implication of this arrangement is that occlusion of C1 origin PICA may not produce the classical lateral medullary syndrome; — the clinical deficit in such cases is congruent with the vermian and cerebellar hemispheric PICA territory and extent of collateral support. A related situation is a well-known AICA-PICA variant, where AICA captures a variable amount of PICA territory, including hemispheric and vermian, but almost never the lateral medullary segment.

Below is another beautiful example of C1 origin PICA (green), “giving rise” to the lateral spinal artery (yellow), which shows the embryologic relationship of the PICA to the lateral spinal. The “true” location of the PICA is shown by the large lateral medullary perforator branch (pink) arising from the intracranial vertebral artery. The upper cervical portion of the Anterior Spinal Artery (red) also arises from the same level.
C2 PICA Origin
This one is less commonly seen, but is no different than C1 in principle — just a lower origin lateral spinal homolog. Again, it is key to understand that 1) lateral medullary supply will not come from the PICA, but will arise directly from the vert, and 2) the cervical PICA may contribute to supply of the lateral cord as the lateral spinal artery, and so must not be sacrificed without extreme caution. The red arrow points to the radicular C2 branch (or strictly speaking radiculopial since it is connected to the lateral spinal artery) which connects the vertebral artery to the vertically-oriented lateral spinal artery (white arrows); the tonsillar and distal PICA is in purple. Most of the time, the whole vessel arising from the vert would be called “PICA” or “C2 origin PICA” however it is important to understand that it is in fact a c2 radicular branch supplying the PICA proper via the lateral spinal artery.
Anaglyph stereo
Lateral stereo view shows the lateral medullary perforator (yellow) in location of the classical PICA origin; the remaining arrows are the same as for the above image.
Anaglyph stereo
Stereo native image, demonstrating PICA arising below C1, at C2 segmental level — the red arrows in this case point to the C2 radiculopial artery which connects the lateral spinal to the vert, just like a radiculopial artery would connect the segmental artery in the thoracic spine to the posterior spinal artery there.
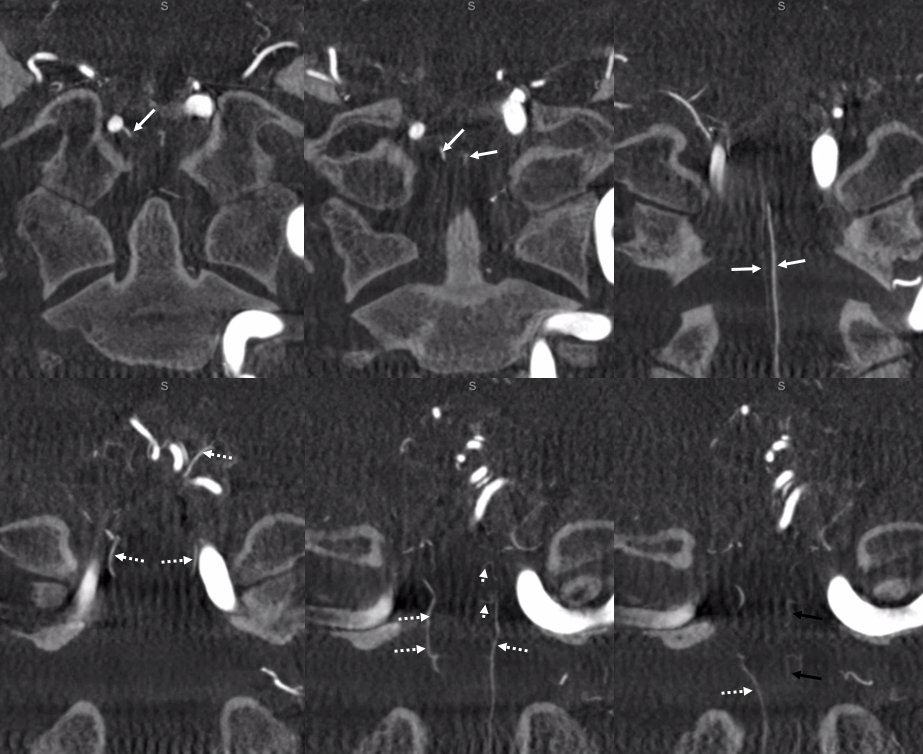
Another illustration of C2 origin PICA is below. This one is very nice because it better demonstrates the “classical origin of the PICA” sometimes called the bulbar branch (pink), with the downgoing lateral spinal artery (white) connecting to the C2 radicular branch(red). So, the network is simply lateral spinal artery extending from the classical PICA region (bulbar branch) to the C2 radicular branch (the lateral spinal embryologically extends to the C4 level). The distal PICA is yellow. Venous phase images show a nice vertebral venous plexus (blue)
Stereo images of the same patient, PA
Lateral
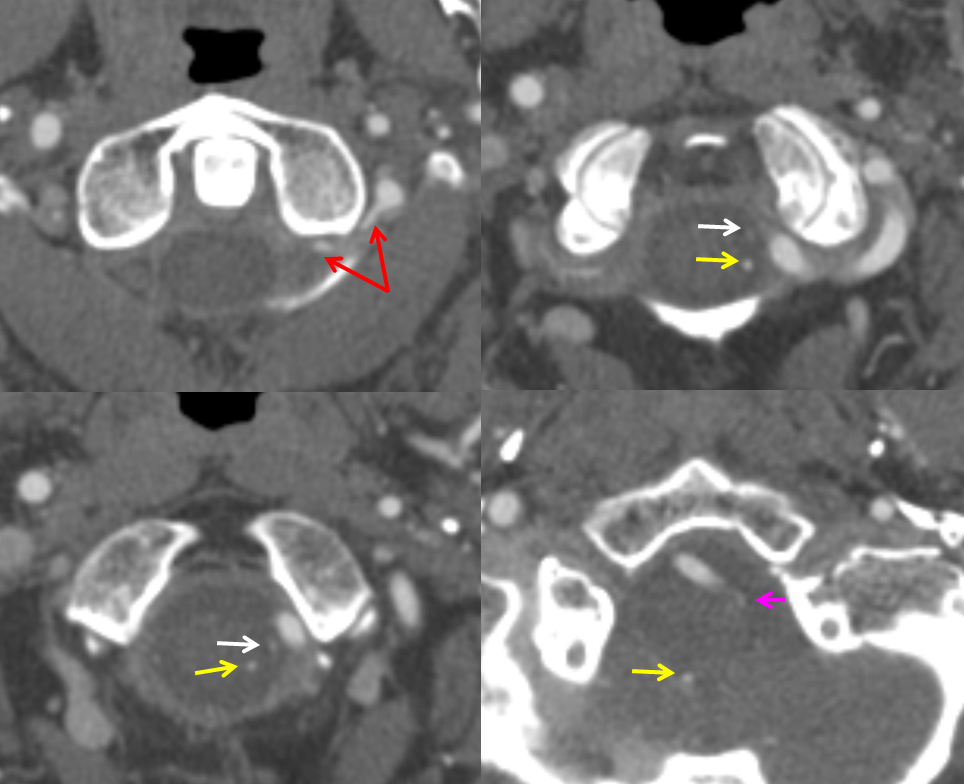
CTA of the same patient, showing the same vessels with same color arrows, from bottom to up
Vertebral Artery Duplication
Another variant explained by the lateral medullary artery artery is “duplication” of the Vertebral Artery, where in addition to the “normal” vertebral artery there is another, intradural channel (brown and pink arrows), re-connecting with the vertebral artery proper more cranially. The additional intradural channel is the lateral spinal artery (pink), while its connections to the vertebral artery are radicular (or technically speaking radiculopial, brown arrows) arteries.
Below is an example of this very disposition (same color arrows as the illustration above)
These images can be better appreciated in STEREO, in AP and lateral native and subtracted views.
Anaglyph stereo

Anaglyph stereo
Pathology — Lateral Medullary Artery Reconstitution of the PICA
The embryonic connection between the lateral spinal artery and the PICA can make a difference between having a PICA infarct and not having one — or not having as large a PICA infarct as would happen otherwise. Although the PICA territory is potentially quite large, the most clinically eloquent part is a relatively tiny lateral medullary area — the famous Wallenberg syndrome and its lesser known variants. The Wallenberg syndrome is most commonly produced by occlusion of the vertebral artery at the level of PICA origin. Depending on size of PICA, AICA-PICA balance (see PICA and AICA pages), and PICA-SCA balance (see SCA page) this kind of occlusion produces variable-sized cerebellar infarcts. However, it is exceptional for PICA-AICA or PICA-SCA collaterals to be robust enough to save the lateral medullary region — the most proximal part of PICA. However, not all vertebral occlusions at PICA level produce clinical symptoms; other times, these symptoms are of lesser severity than would be expected from a full lateral medullary stroke. Salvation often comes from the lateral spinal artery reconstitution of the PICA — a misnomer again since PICA is in fact a branch of the lateral spinal. Just like the posterior spinal artery is supplied by the radiculopial arteries (see Spinal Arterial Anatomy), so is the lateral spinal artery. We already saw from the above illustrations how vertebral duplications and C1 and C2 origins of PICA are related to the lateral spinal artery — the connections between vertebral artery and lateral spinal artery come from C1 or C2 level radiculopial arteries.
In cases of upper vertebral artery occlusion which endangers the PICA, reconstitution of the same can come in form of C1 or C2 radicular (radiculopial) connection to the lateral spinal artery and then from lateral spinal to the PICA. In the acute setting, this collateral is usually not sufficient to save the cerebellum, but may be enough to carry the all-important lateral spinal portion of the PICA.
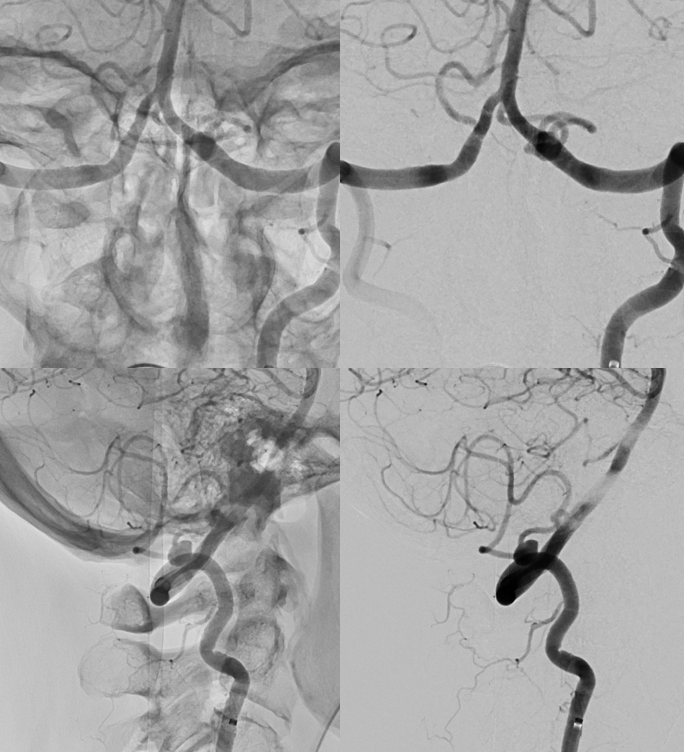
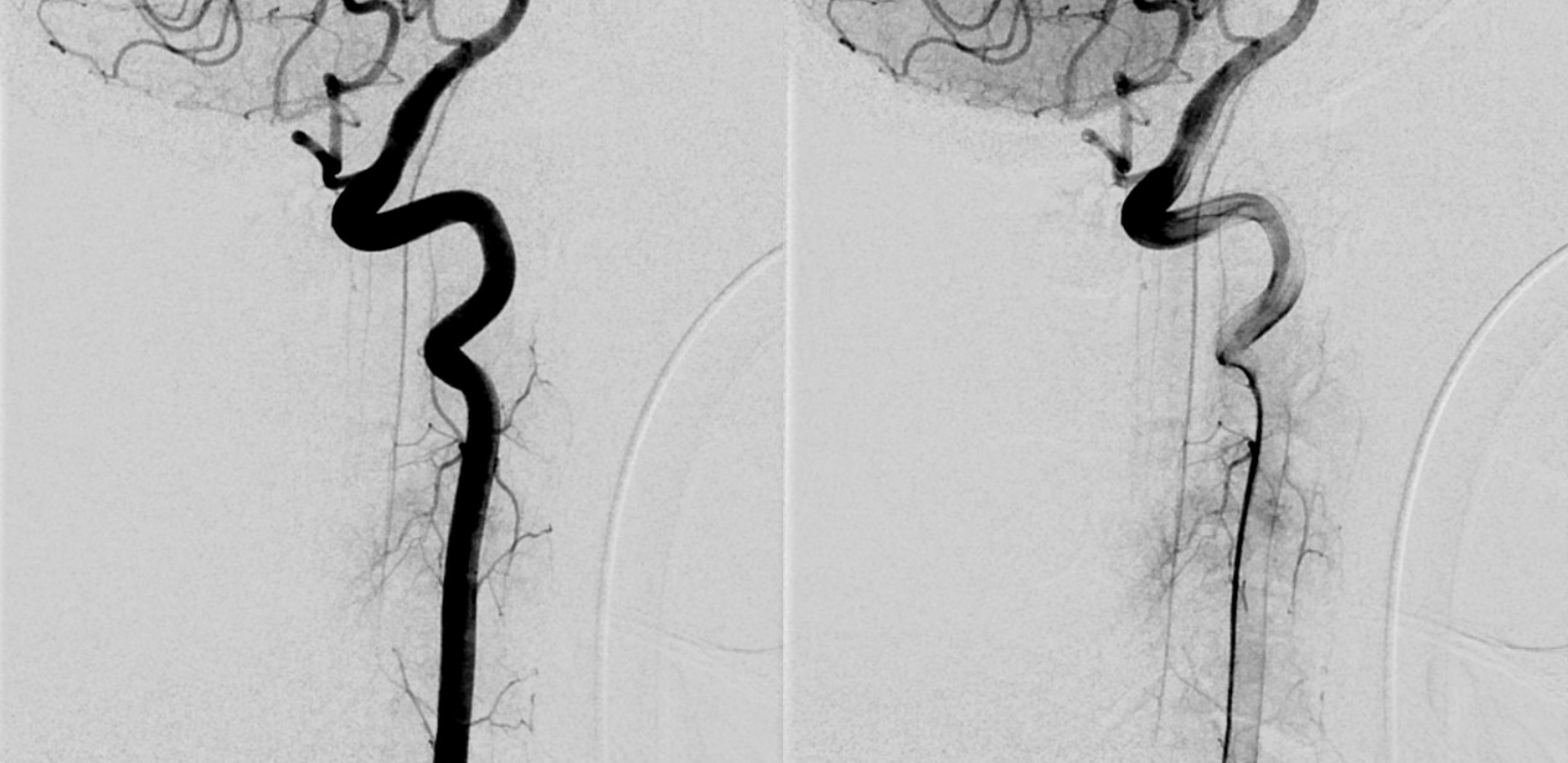
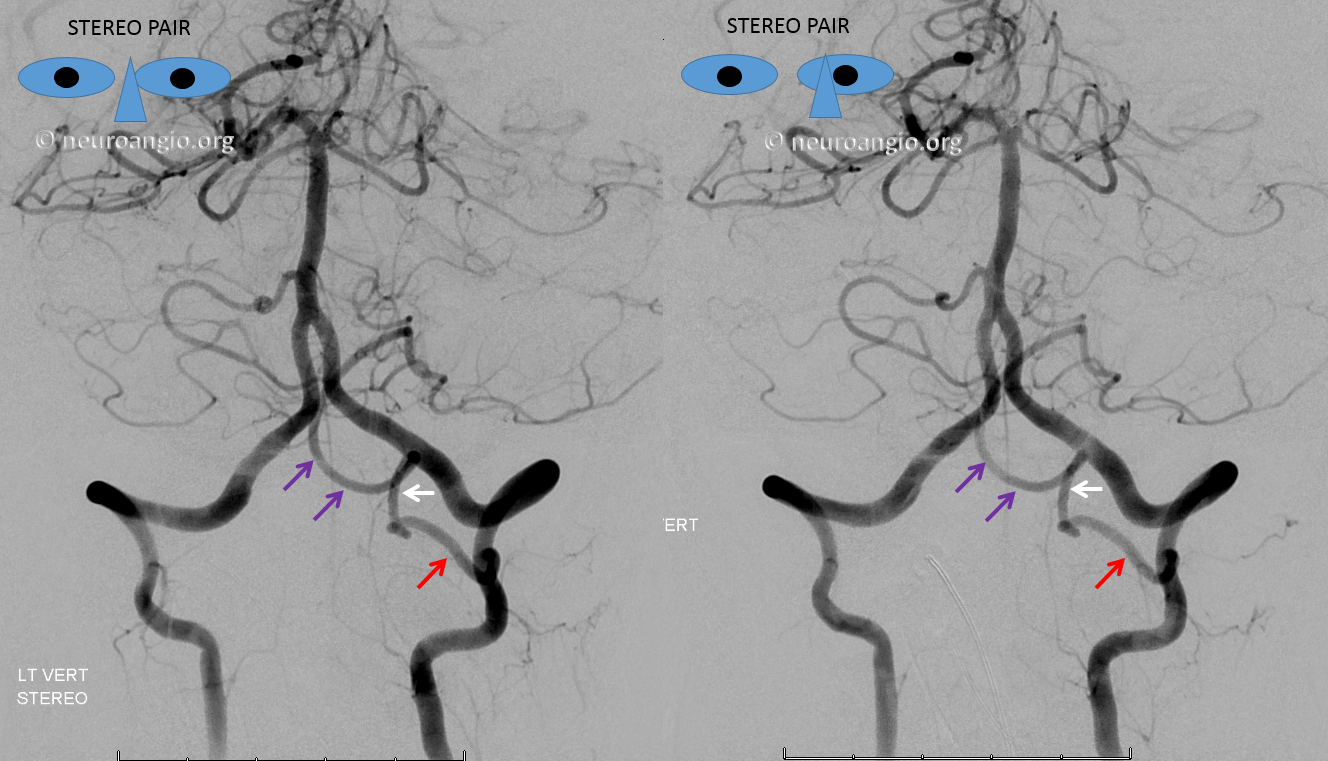
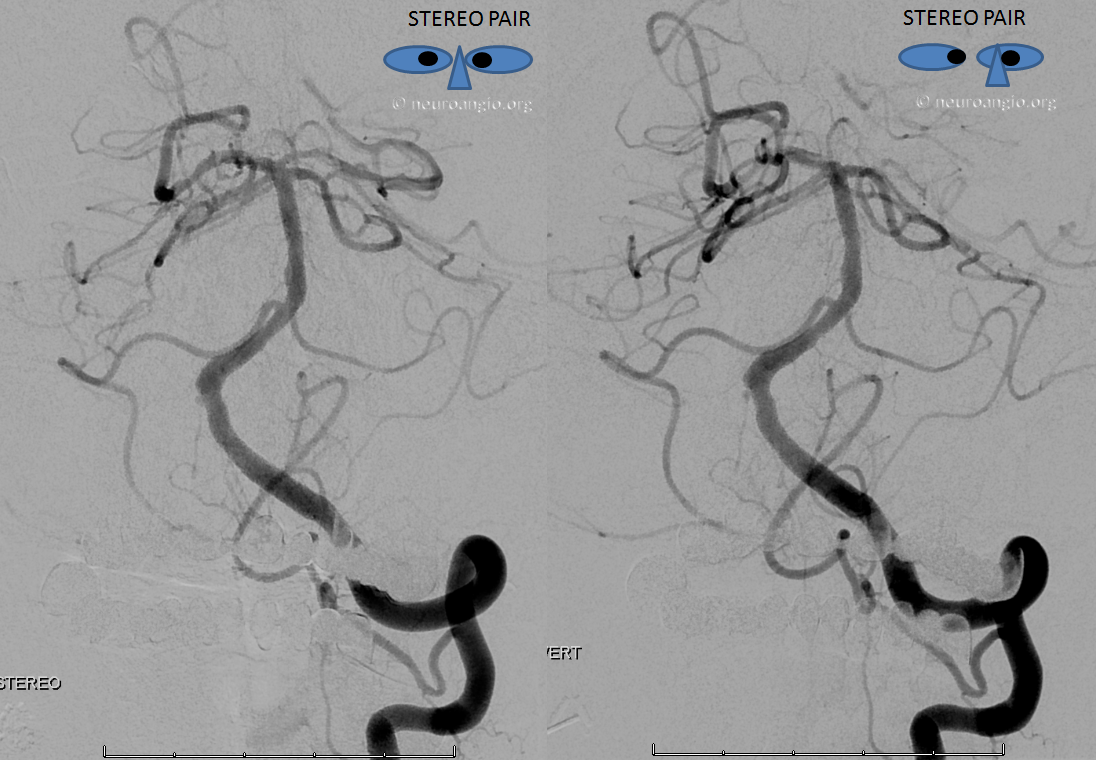
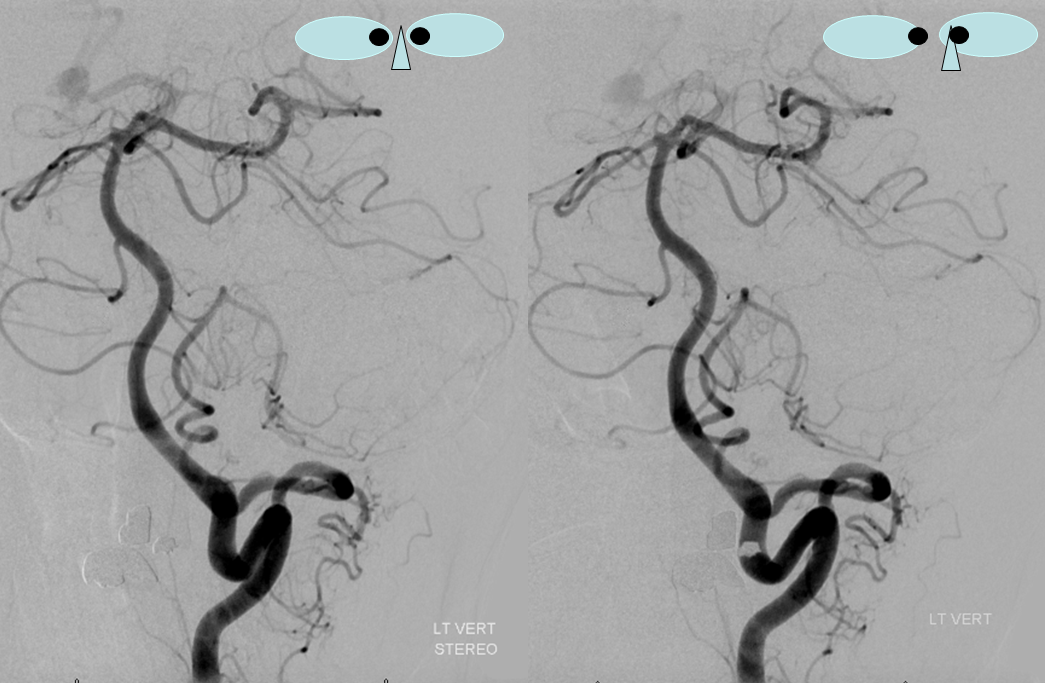
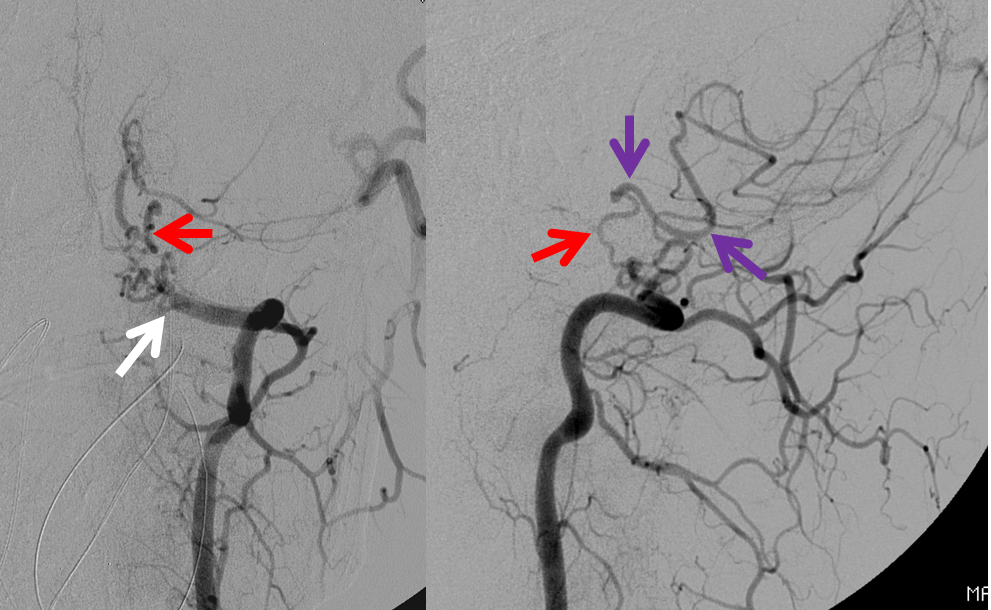
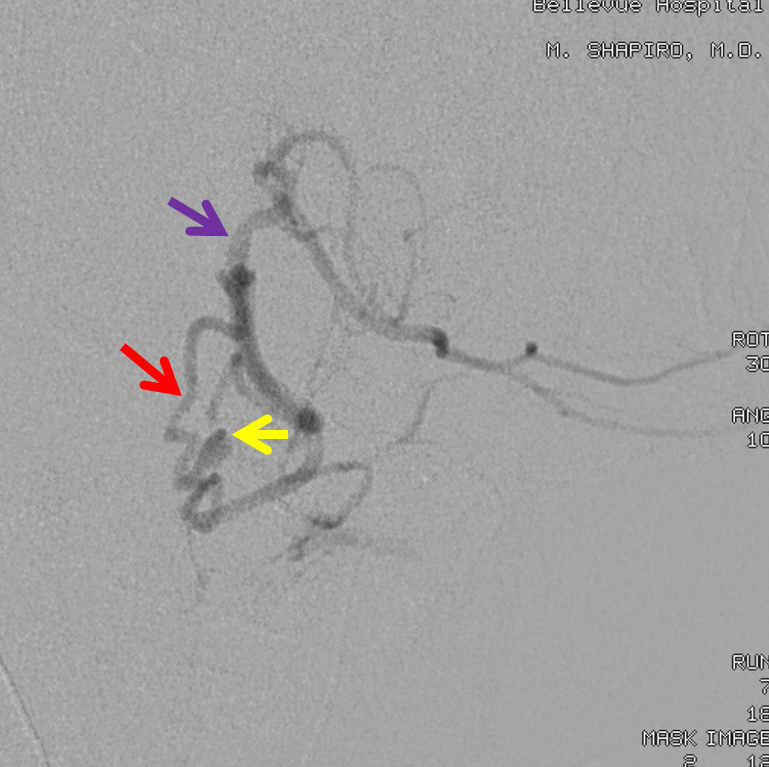
In this patient, the right vertebral artery is occluded just below the foramen magnum due to dissection. The C1 radiculopial artery (purple) connection to the lateral spinal artery (red) allows for reconstitution of the vermian branch of the PICA (black). The lateral spinal artery below the C1 radiculopial branch is marked with the pink arrow. Notice also presence of the anterior spinal artery (yellow) perfectly contrasting its anterior and medial position to that of the spinal artery. The C1 radicular branch (purple) is in effect the radiculopial artery is acting as a radiculopial artery, homologous to radiculopial supply of the posterior spinal arteries at the thoracic and lumbar levels (see Spinal Arterial Anatomy) The C1 muscular branch (green) opacifies the occipital artery (white) and deep cervical artery (blue).
The indispensable STEREO pair
Example 2 — vertebral dissection with lateral spinal reconstitution of the PICA and lateral spinal artery aneurysm
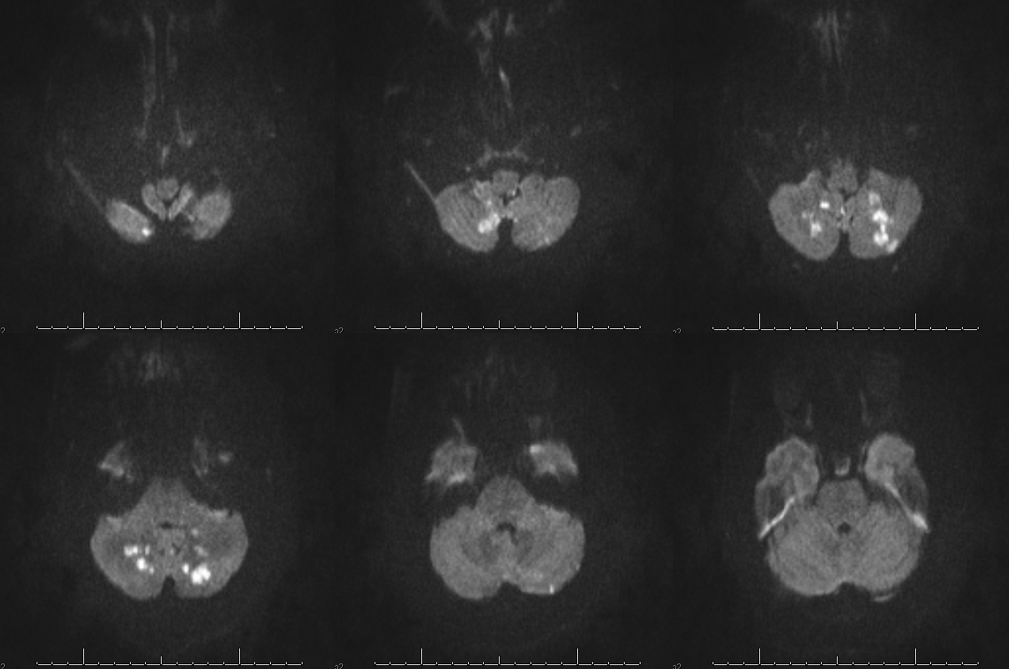
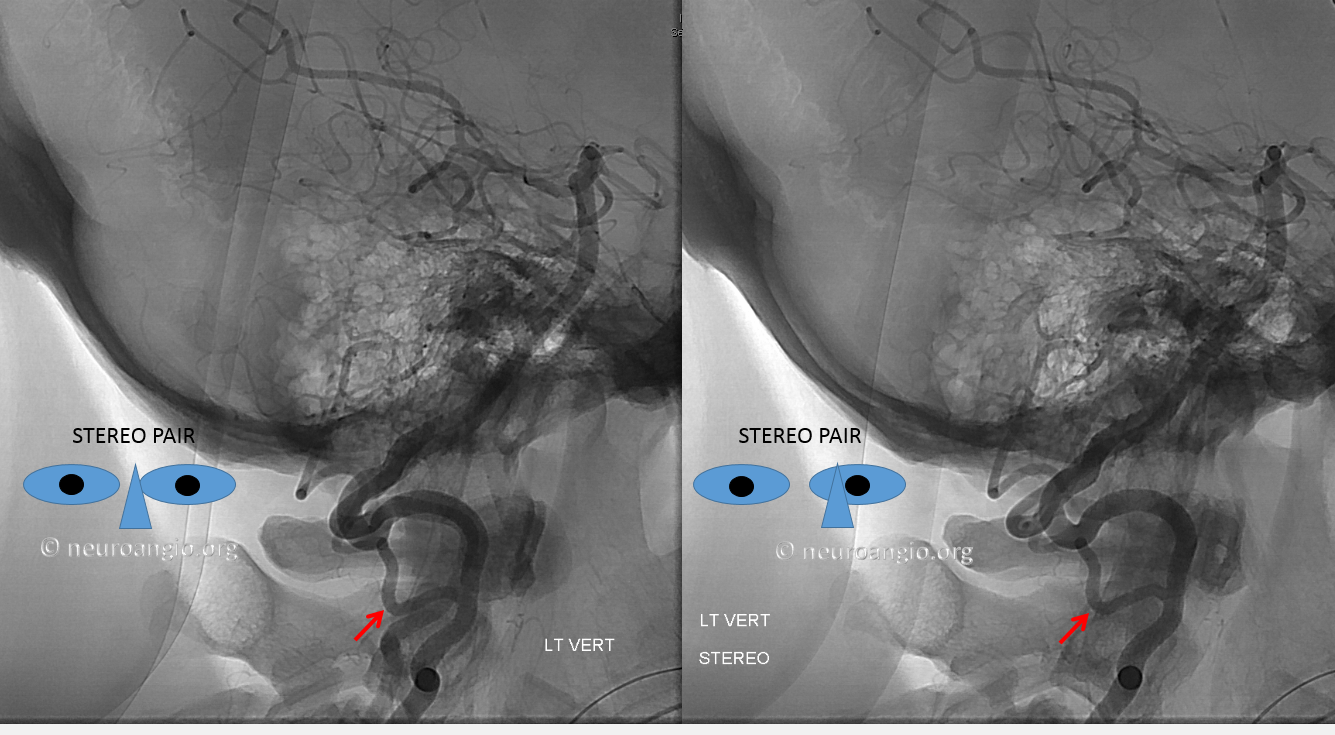
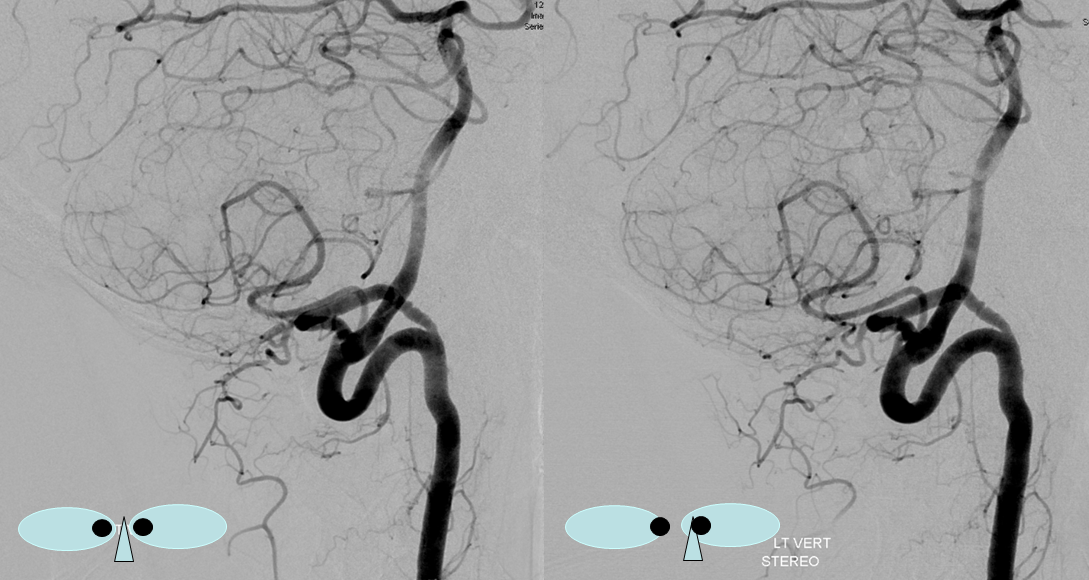
An individual with a passion for weightlifting dissected his left vertebral artery, sustaining a then-asymptomatic PICA territory stroke, as seen below. Notice sparing of the medullary segment, as any self-respecting asymptomatic PICA stroke would. This is exactly what we discussed above — while PICA occlusion can produce a cerebellar stroke, the lateral medullary territory may be spared — usually via the lateral spinal artery
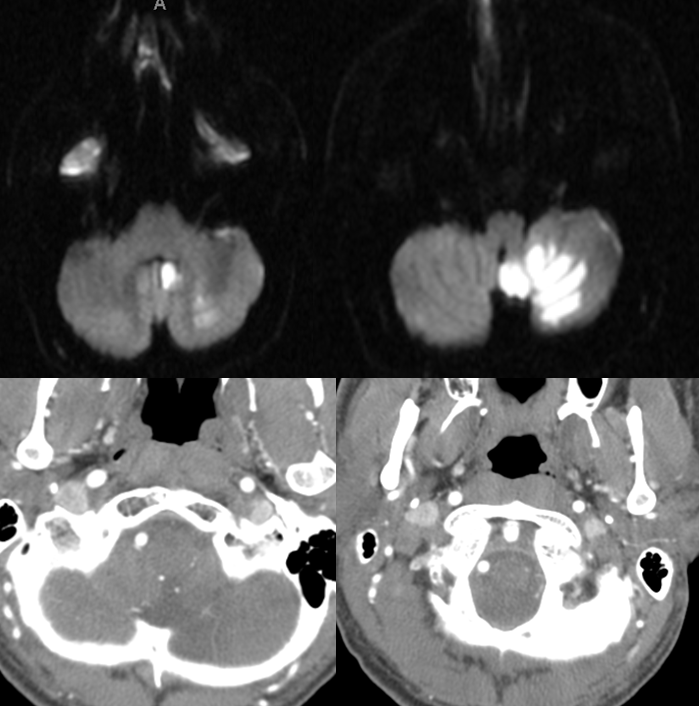
Several years later, the patient presented with subarachnoid hemorrhage in the posterior fossa (see Lateral Spinal Aneurysm page). Angiogram shows persistent vert occlusion (white arrow). The PICA (purple) is being reconstituted by the lateral spinal artery (red)
Microcatheterization demonstrates an aneurysm (yellow) of the lateral spinal artery (red), presented in lateral stereo projections.
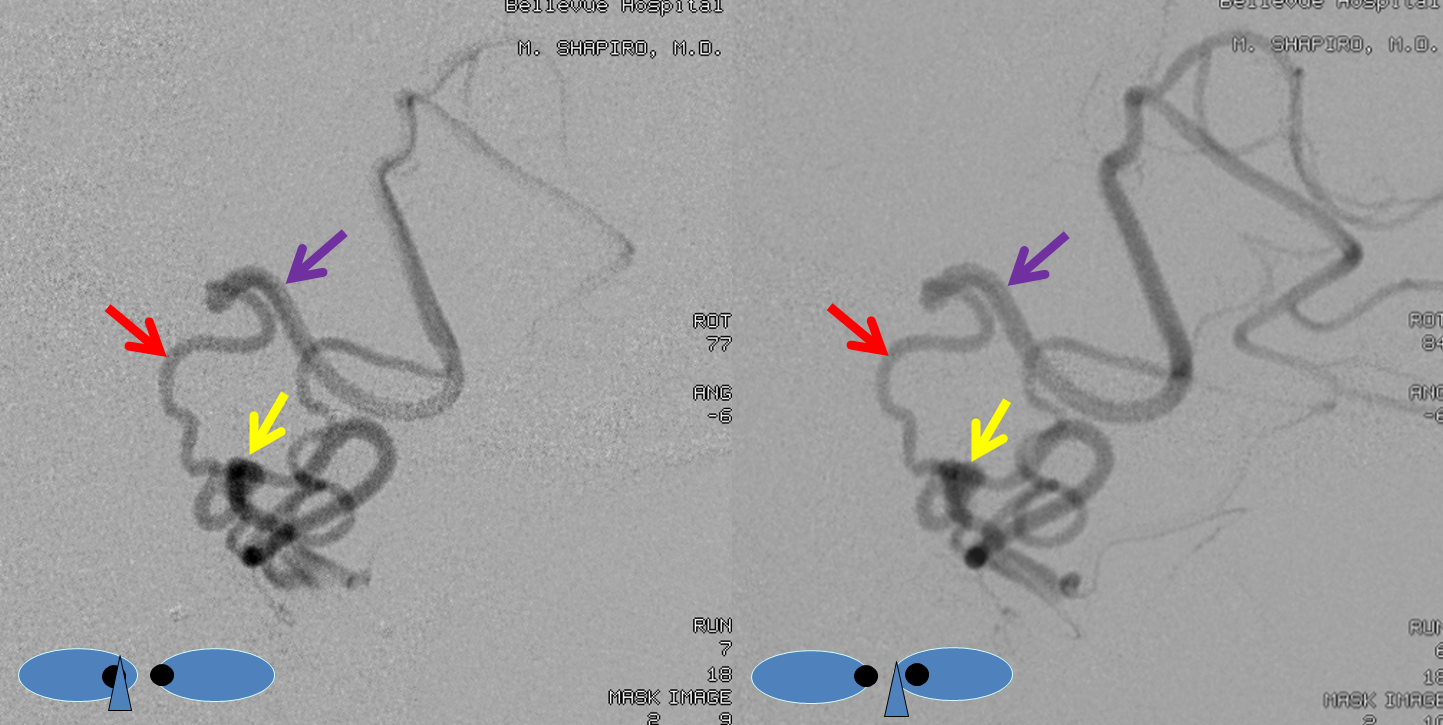
The same aneurysm (yellow) in LAO, for clarity’s sake. Pathophysiology of aneurysm formation is likely related to flow demand, although extension of dissection into the lateral spinal can’t be totally excluded.
For treatment, see Lateral Spinal Aneurysm page.
Conclusions:
Lateral Spinal Artery is essentially the same vessel as the posterior spinal artery, with a different name reflecting its more constant presence and unique role in the region of upper cervical spine and cervicomedullary junction. The PICA, embryologically a cervical rather than cerebral vessel, is essentially a hypertrophied branch of the lateral spinal artery, secondarily involved in supply of the cerebellum in “higher” species. Its pure lateral medullary territory corresponds to the Wallenberg syndrome in cases of occlusion. Many variations in PICA origin and upper vertebral artery anatomy can be understood when PICA is considered as a branch of the lateral spinal artery. PICA reconstitutions by the lateral spinal artery in cases of PICA origin occlusion can save the patient from developing a lateral medullary syndrome.
Further Reading:
Seminal paper by Lasjaunias group: https://www.ncbi.nlm.nih.gov/pubmed/4020445
Questions/Comments/Complaints: Here is the place
