With Erez Nossek MD and Eytan Raz MD PhD
A very complex case highlighting our main message — aggressive aneurysms require aggressive treatment strategies. This is not for stent-assisted coiling
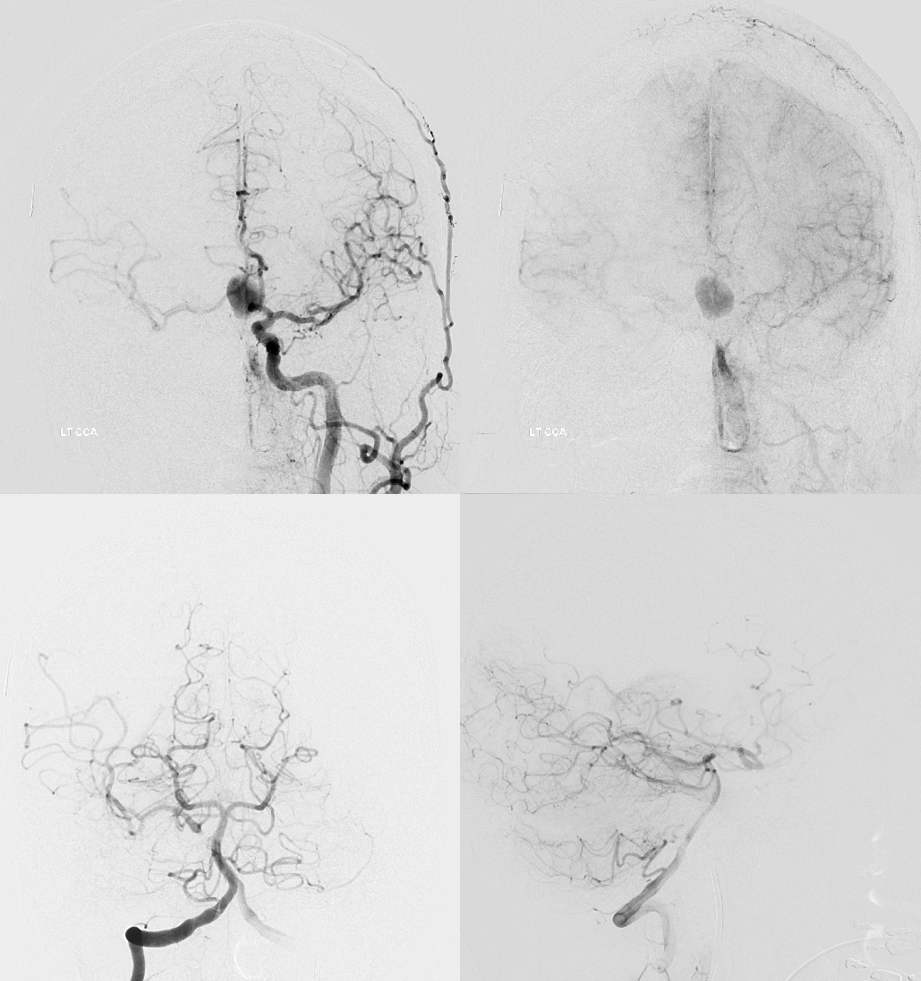
Giant ACOM
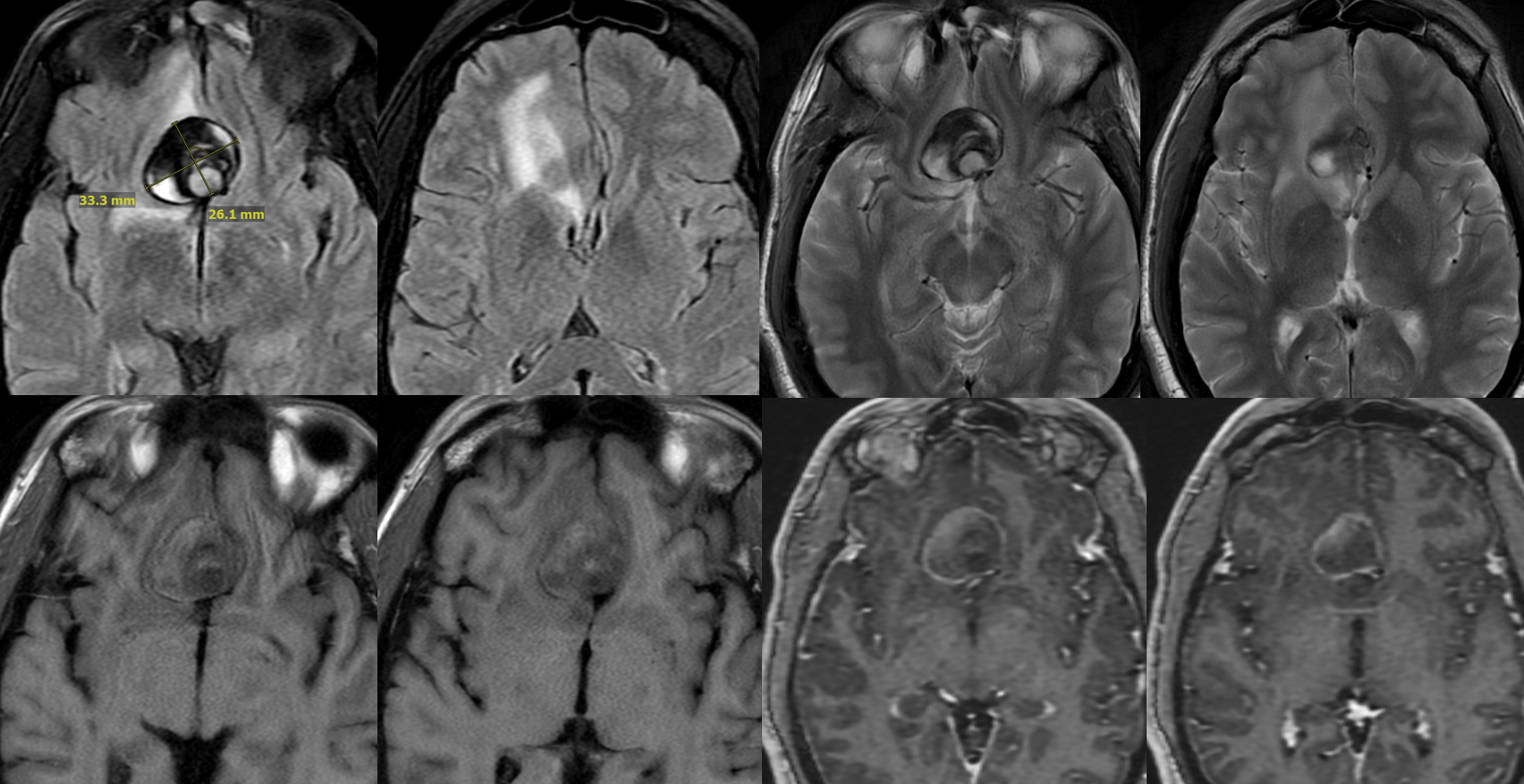
More problems? Yes

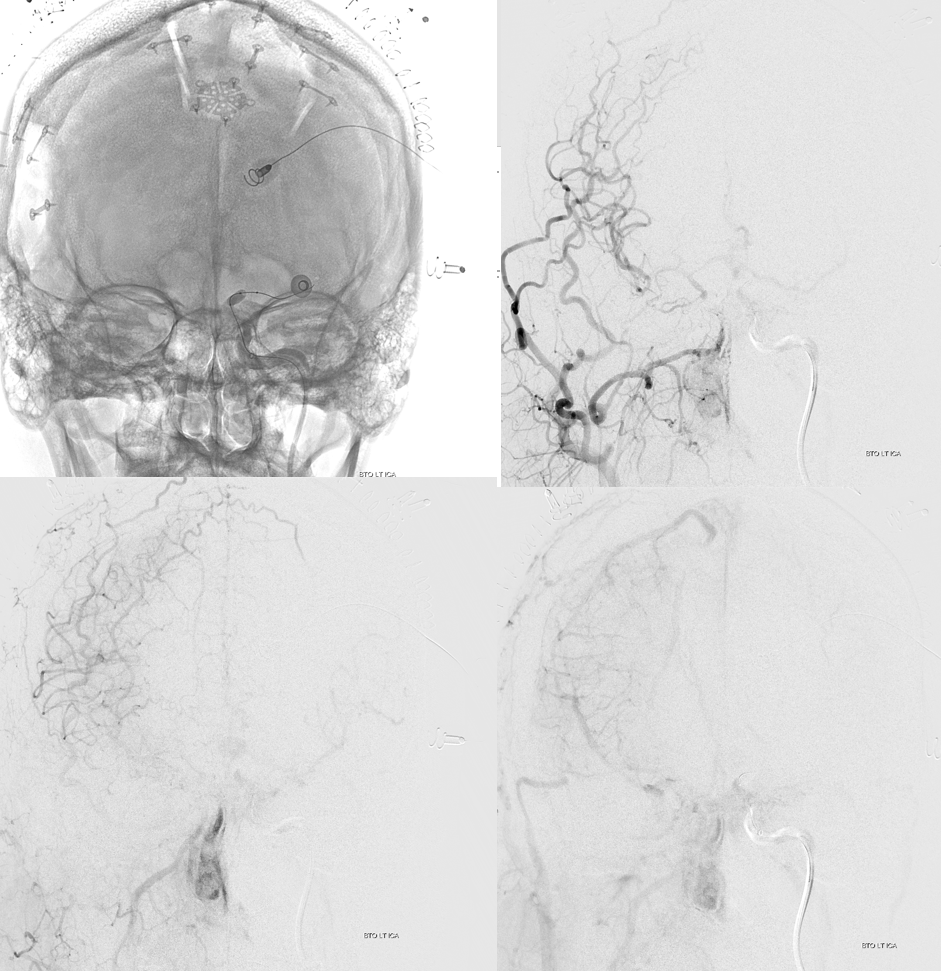
So far, we have a giant mostly thrombosed ACOM aneurysm with adjacent edema, a chronically occluded right cervical ICA, and right ACA dependent on the ACOM flow… Not easy
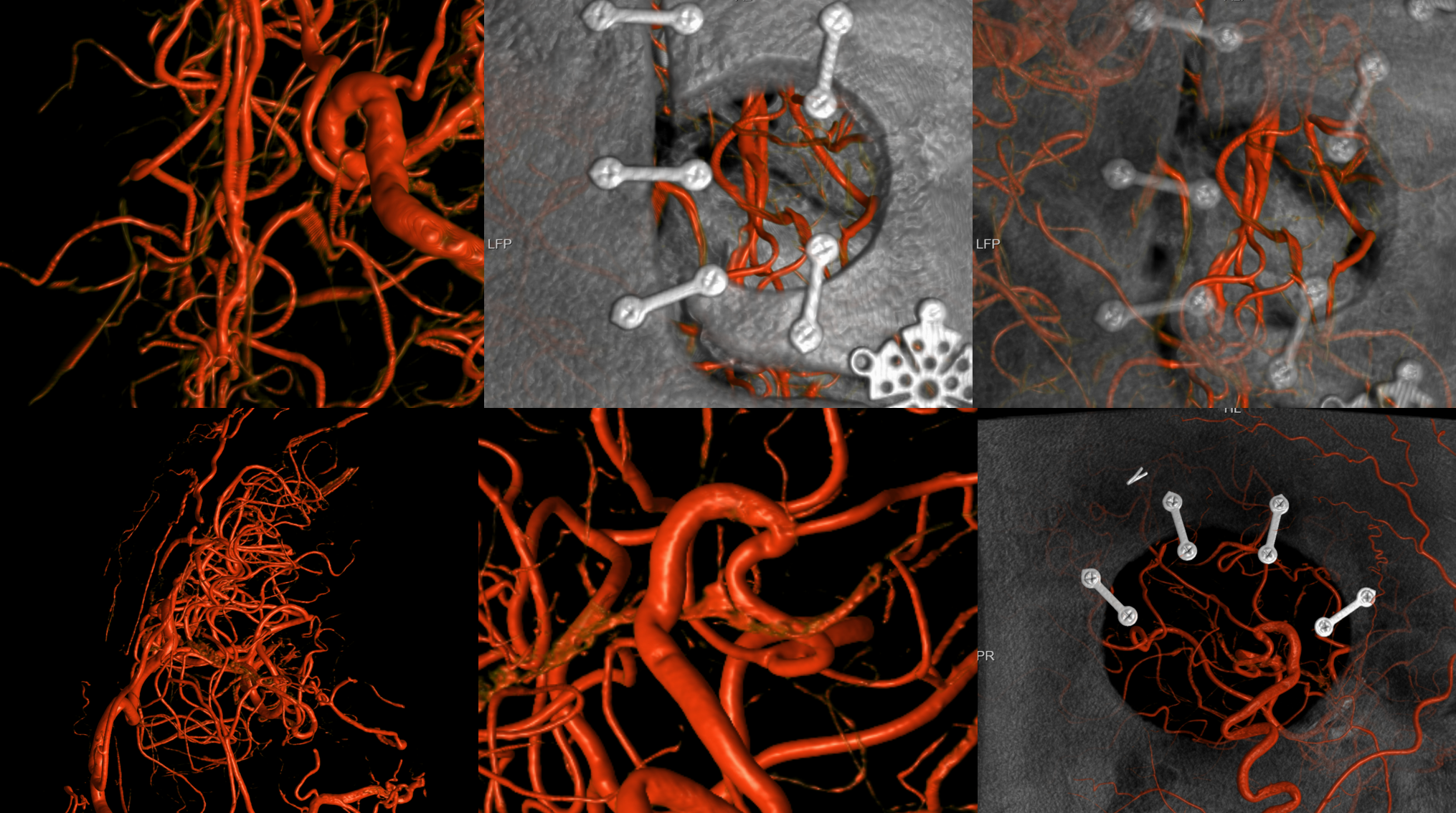
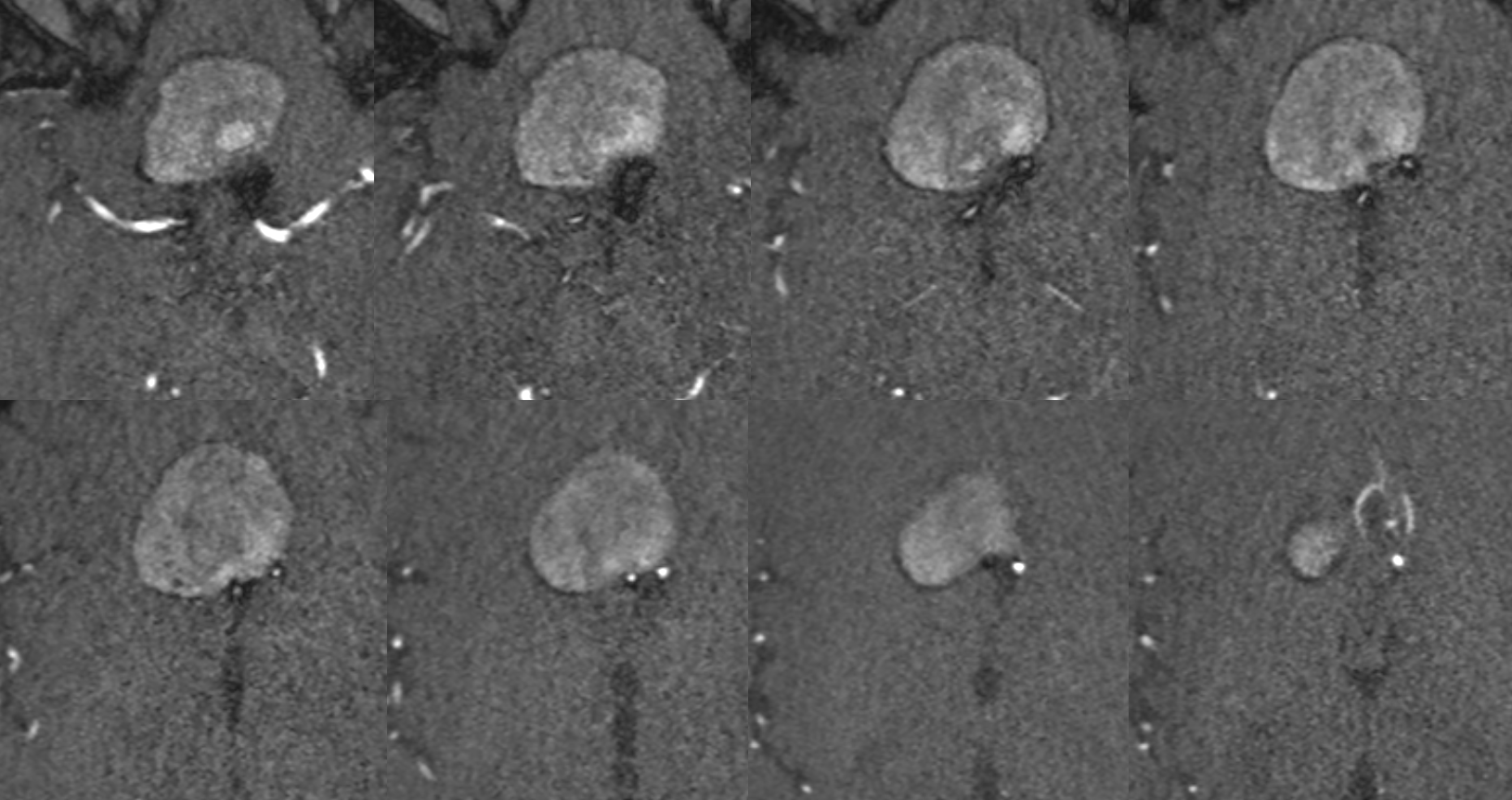
Spins are good
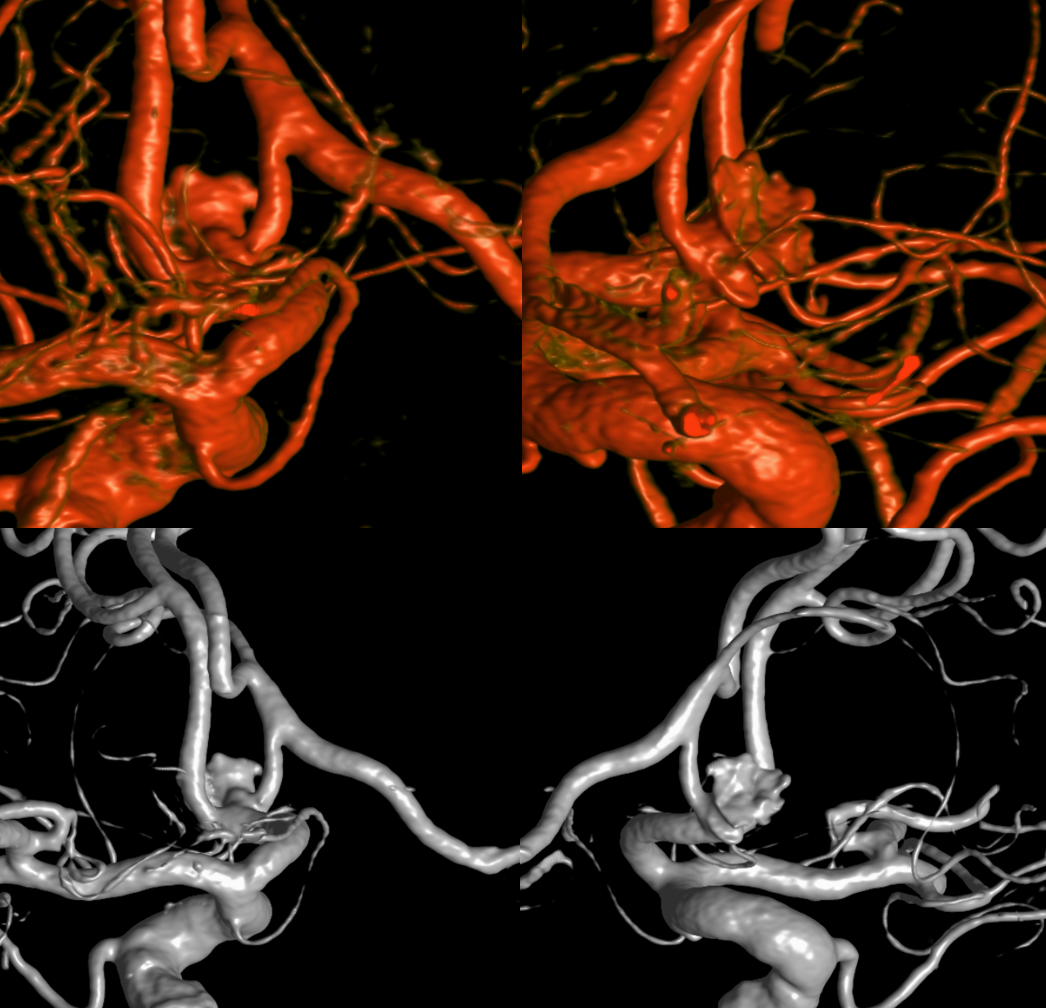
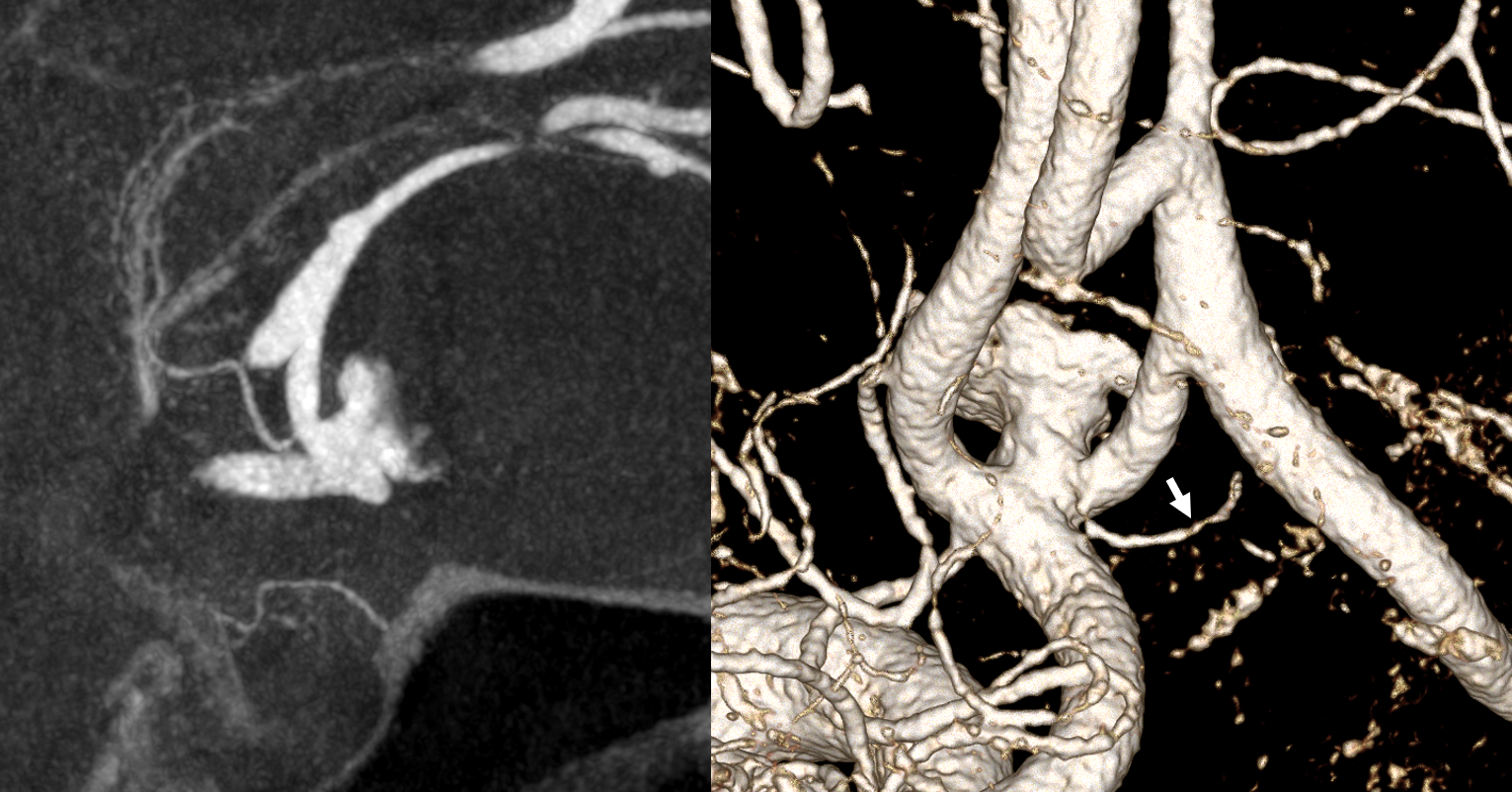
A secondary reconstruction and detailed analysis is better. What does arrow point to?
Spin
A better unsubtracted spin
What to do? We know what not to do — Coiling, WEB, stent-coiling — that’s the thing not to do. All that happens is you close doors on future treatments and the aneurysm continues to grow. So don’t fall for that. The strategy is staged treatment. First stage is to bring more flow to the right side with STA-MCA and ACA-ACA bypasses. Then we attack the aneurysm with more options.
1 mo later — open portion is larger despite same medication regimen

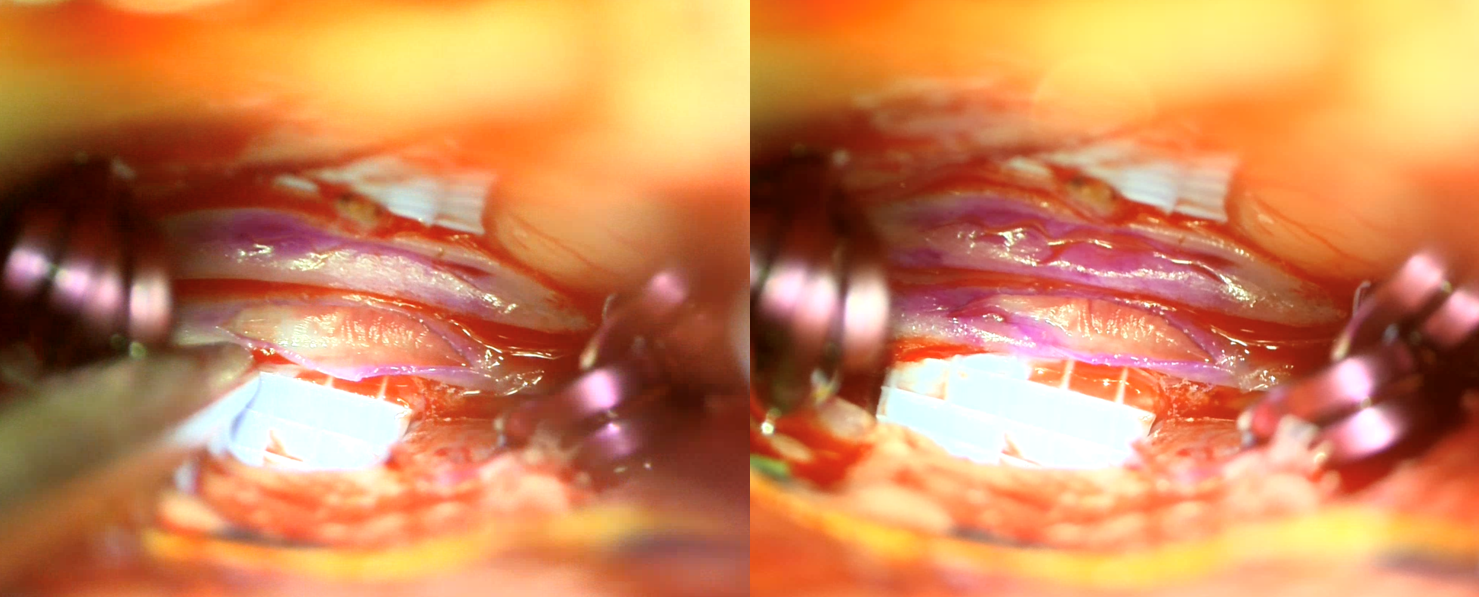
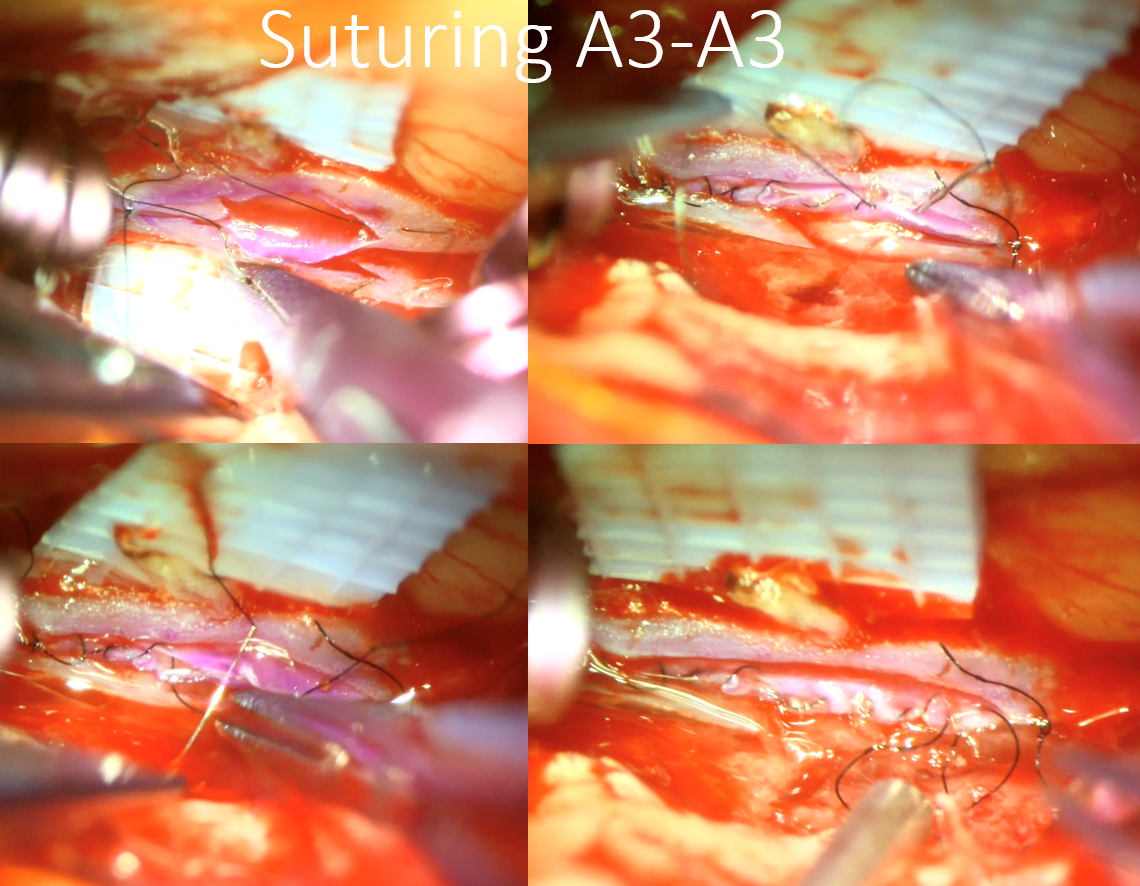
Preparing A3-A3 bypass
Harvesting STA

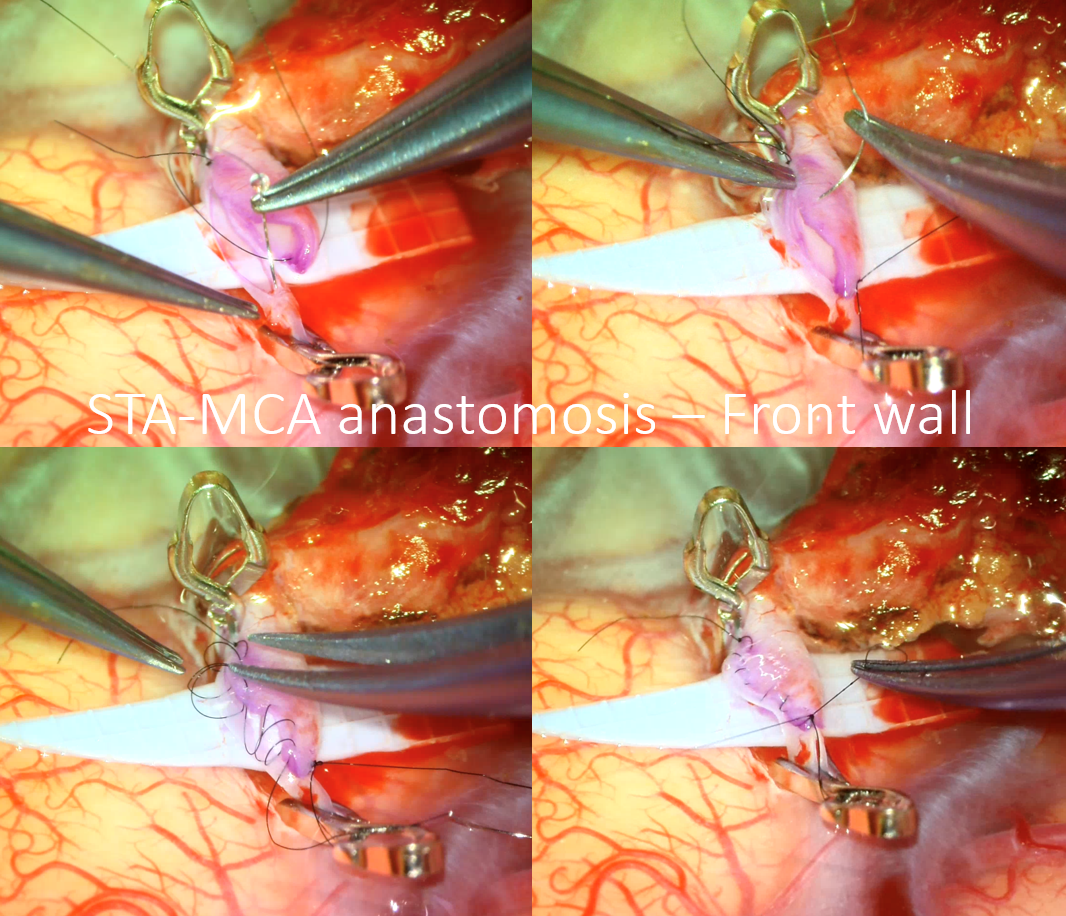
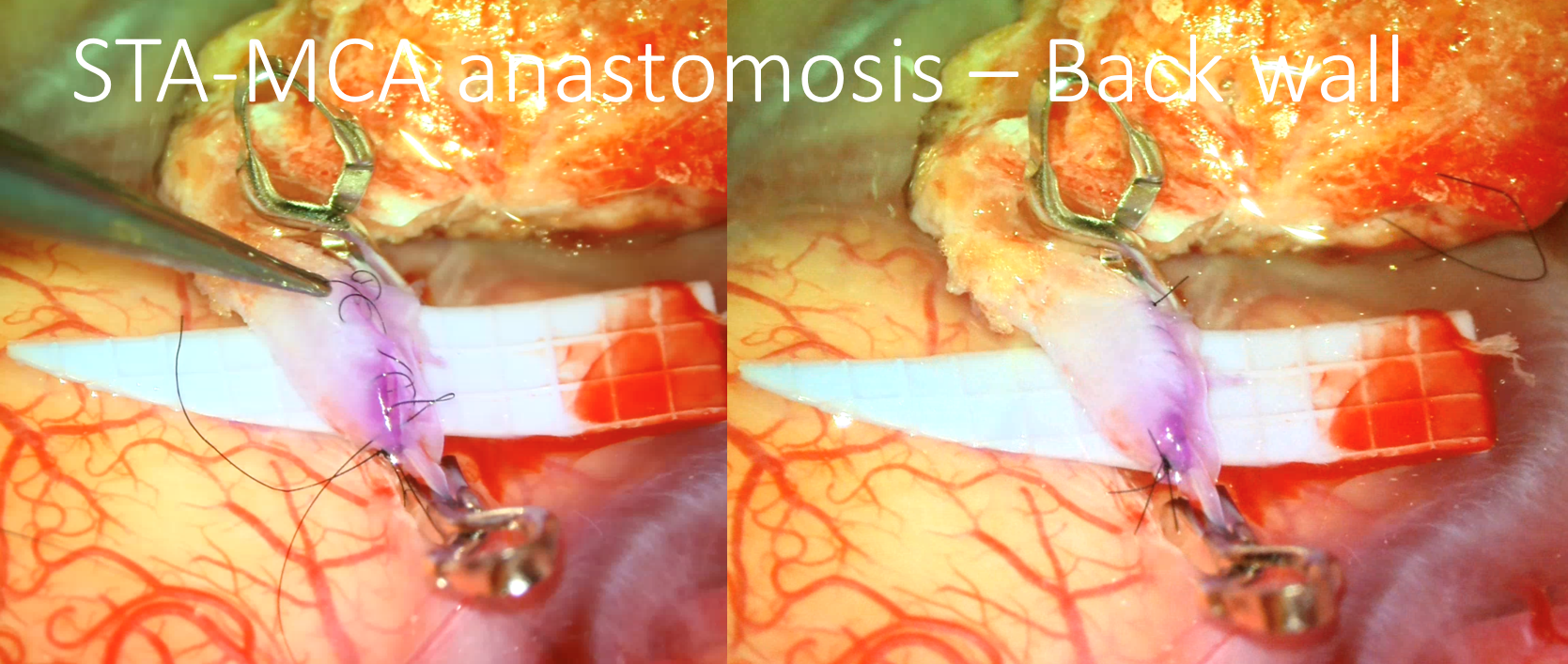
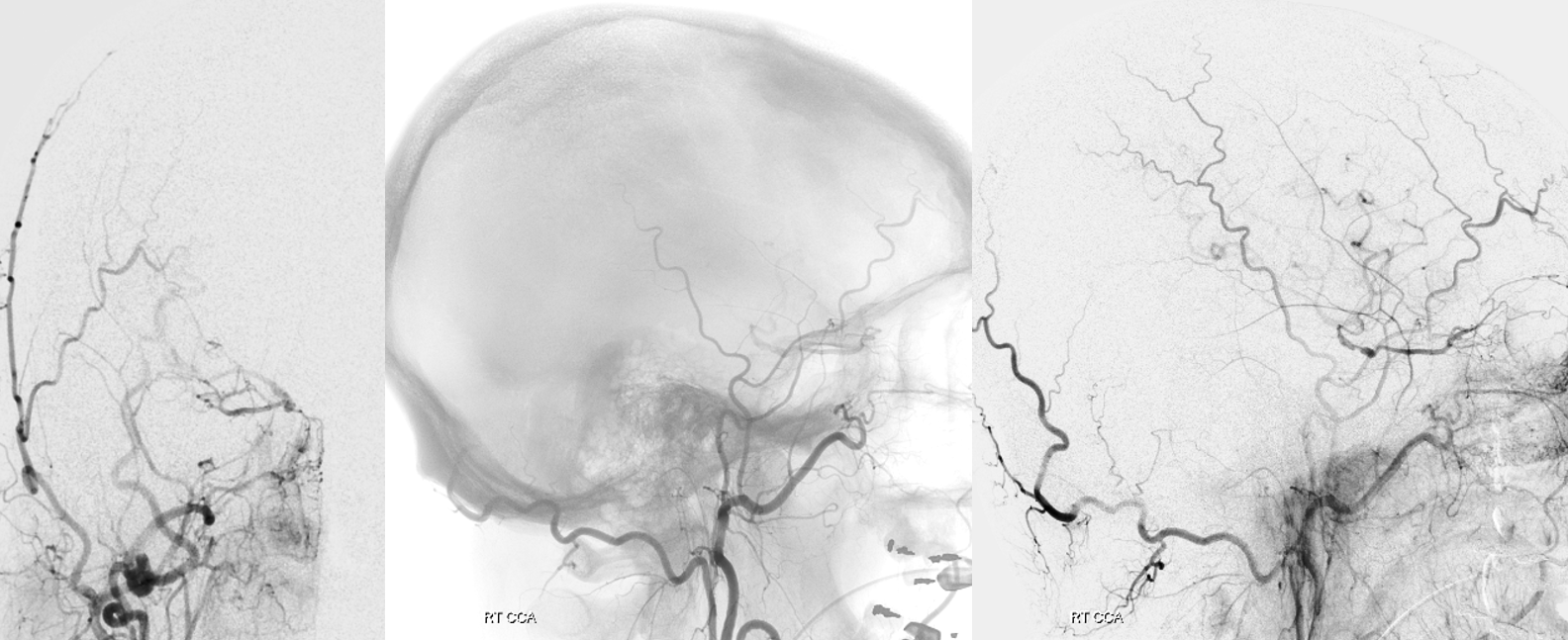
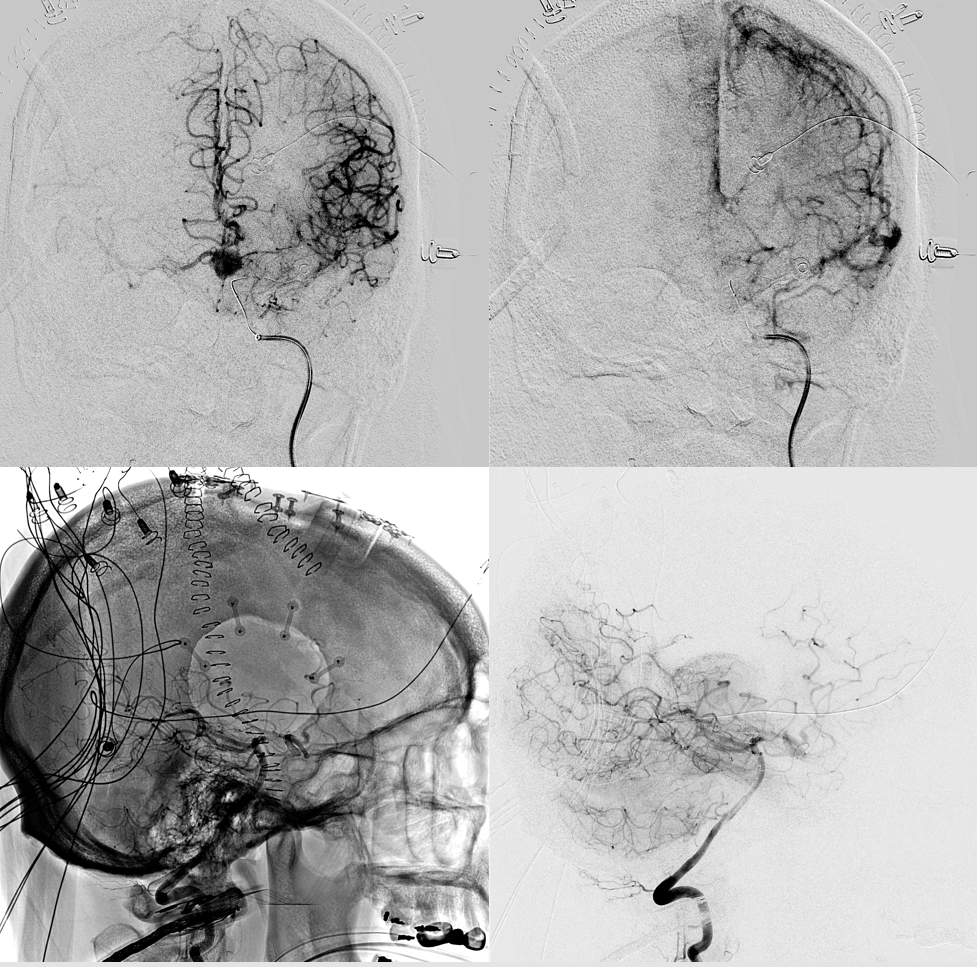
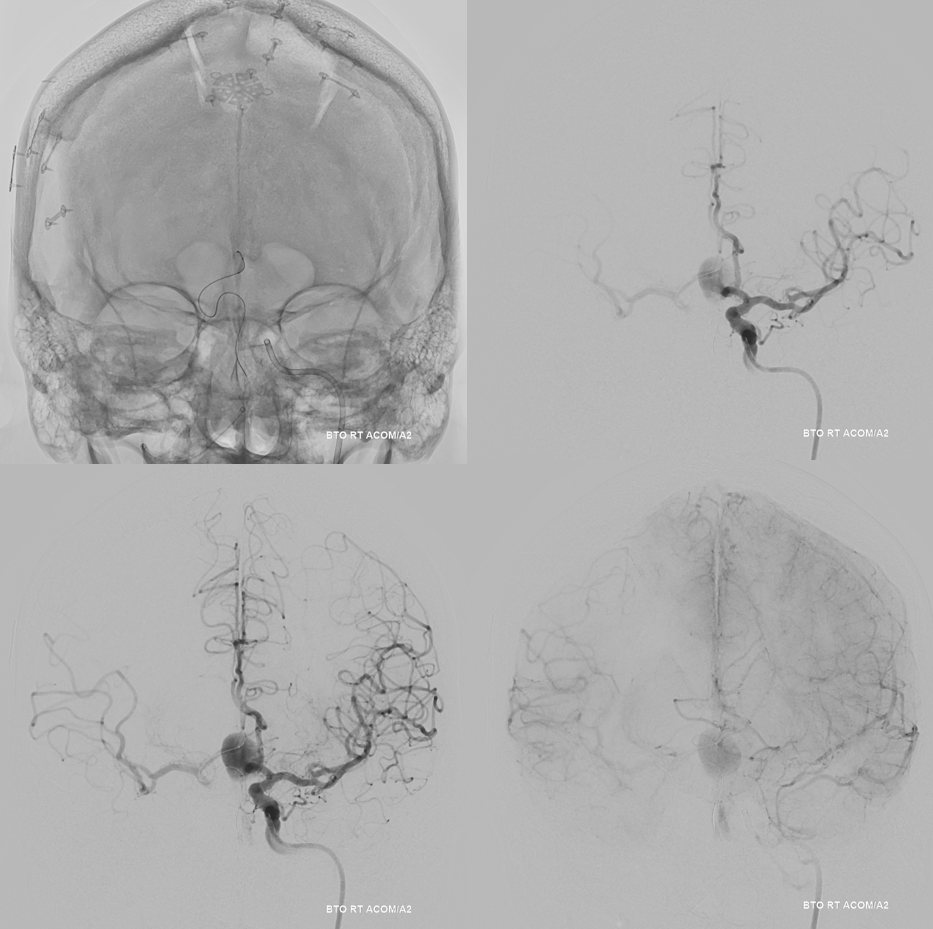
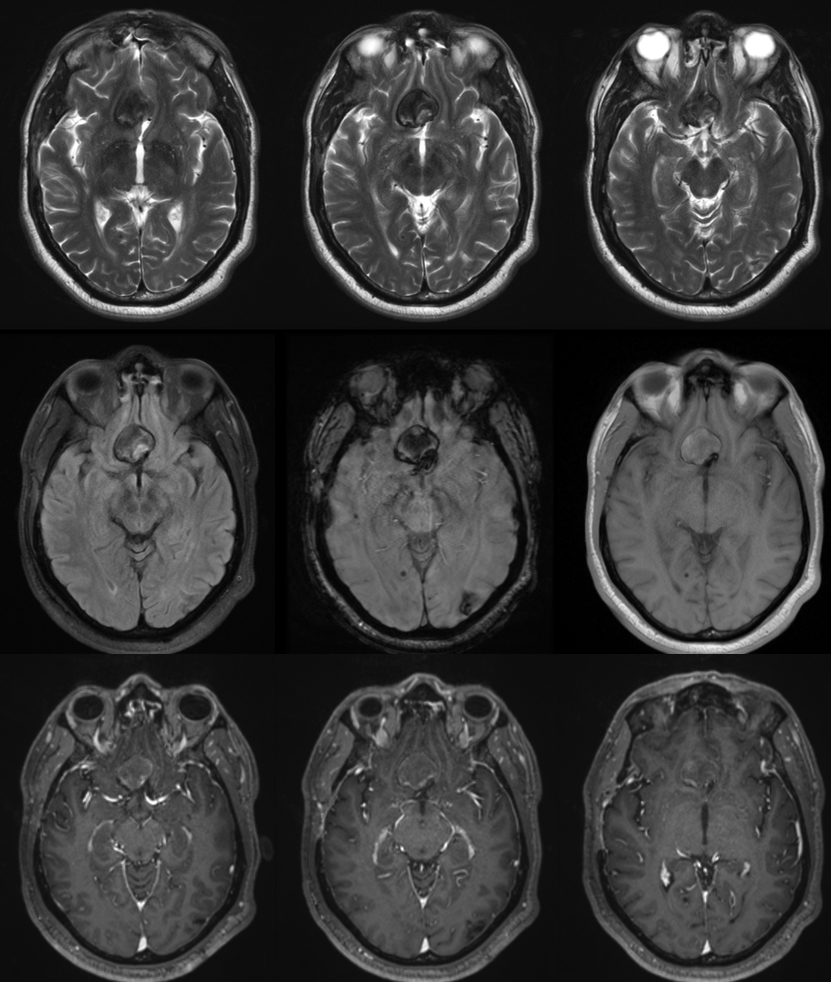
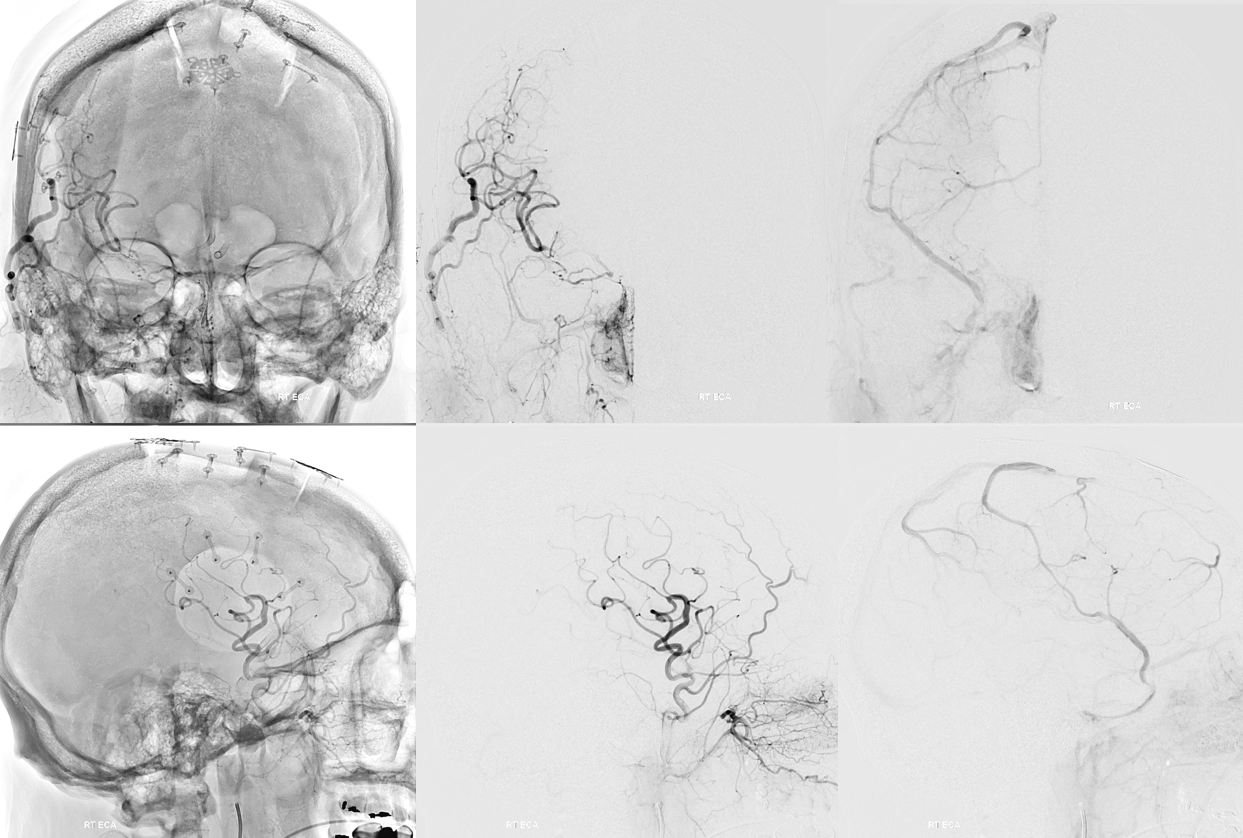
Angio intraop post bypass- STA-MCA working
ACA-ACA did not have flow at this point. Tested by a left A2 BTO. How does that test for bypass patency?
STA-MCA bypass, right ophthalmic, and right PCOM not enough to supply right ACA at this stage — tested by left supraclinoid bypass — what is the rationale there?
Now we decided to wait a few months
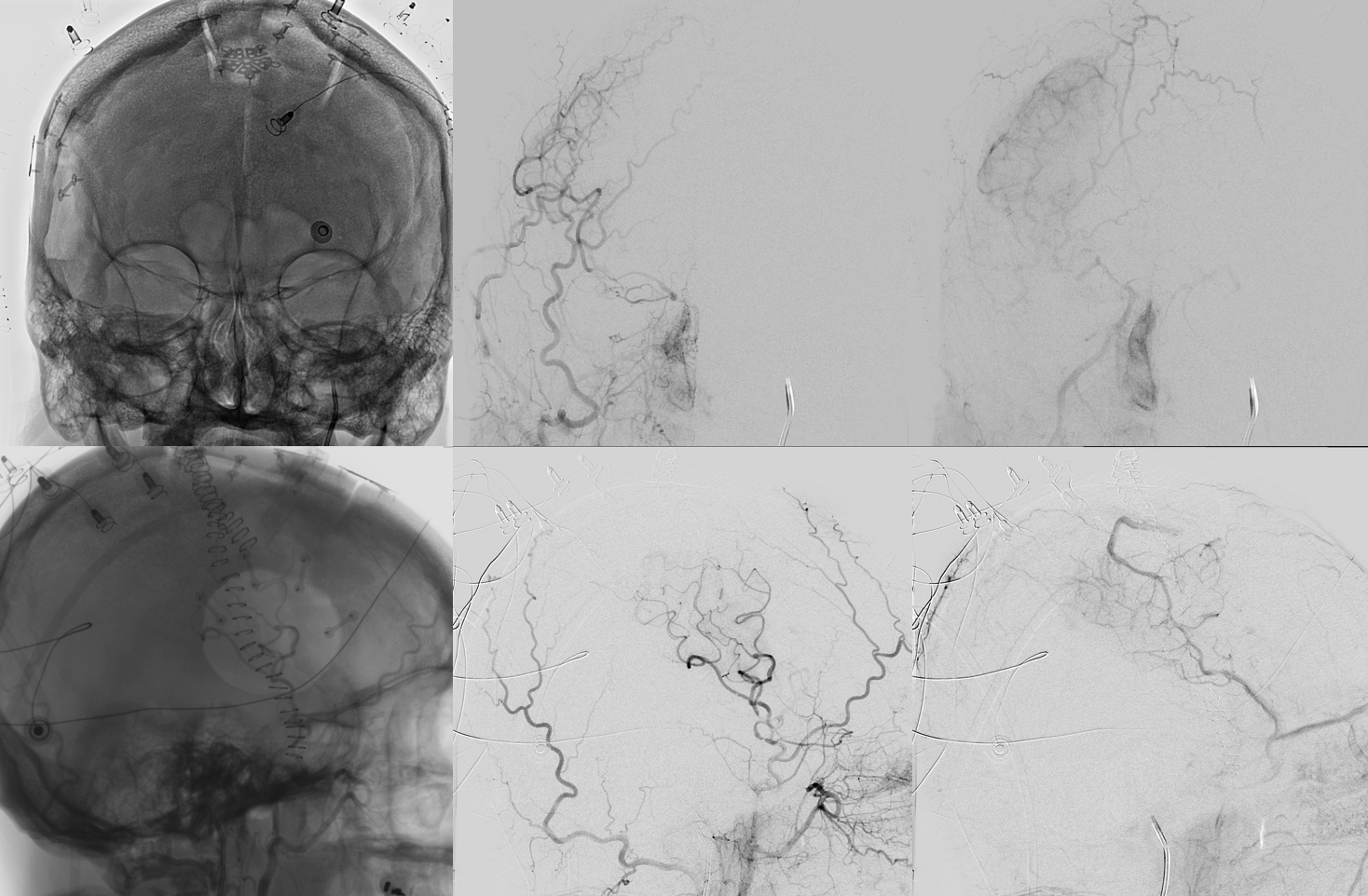
Bypass working even better
PCOM working correspondingly less. Ophthalmic no longer needed
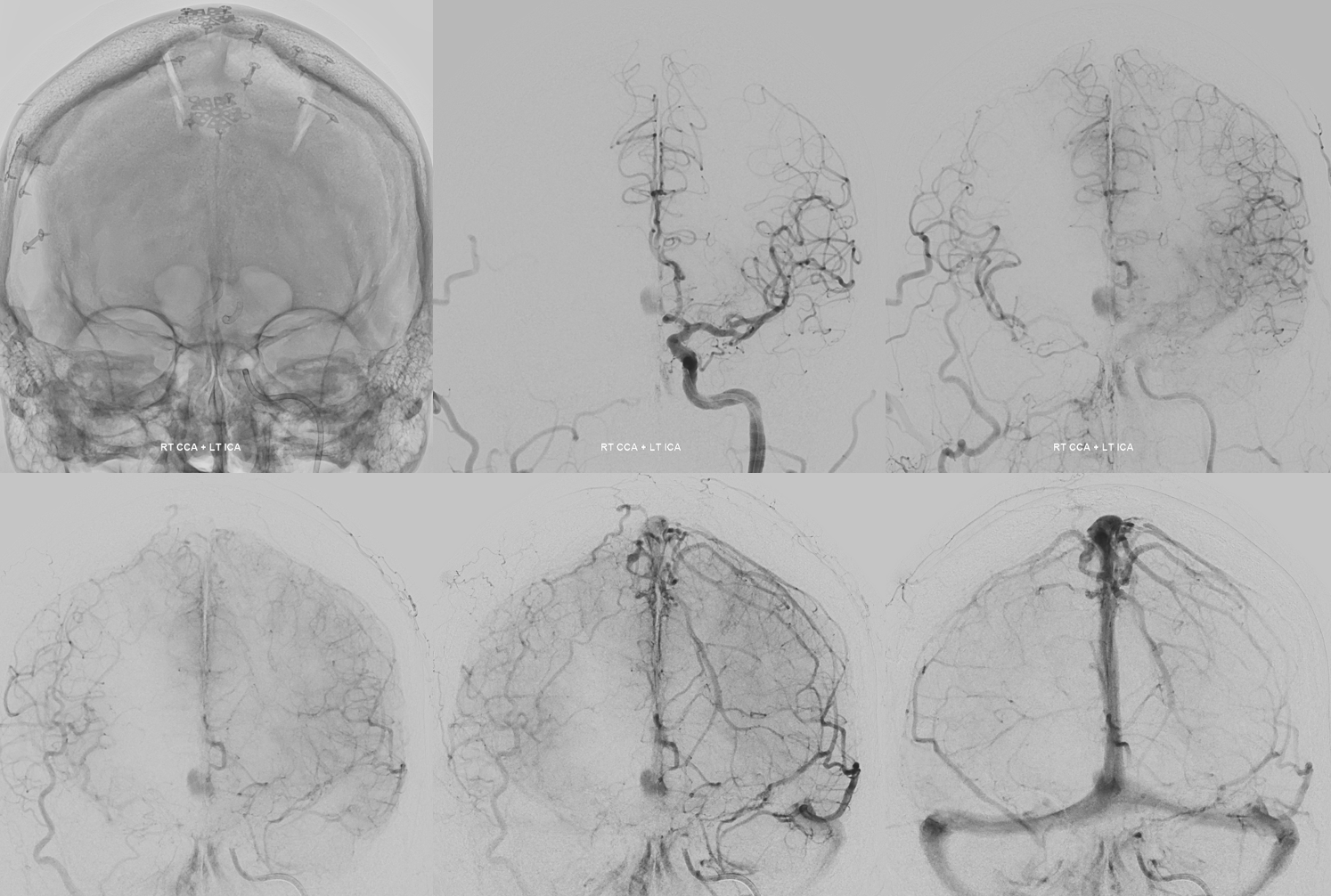
Bilateral CBCT Injections. A big bonus — the ACA-ACA bypass now seems to be patent! Cant see that from 2D images really at this stage. We did not realise this at first but became clear later
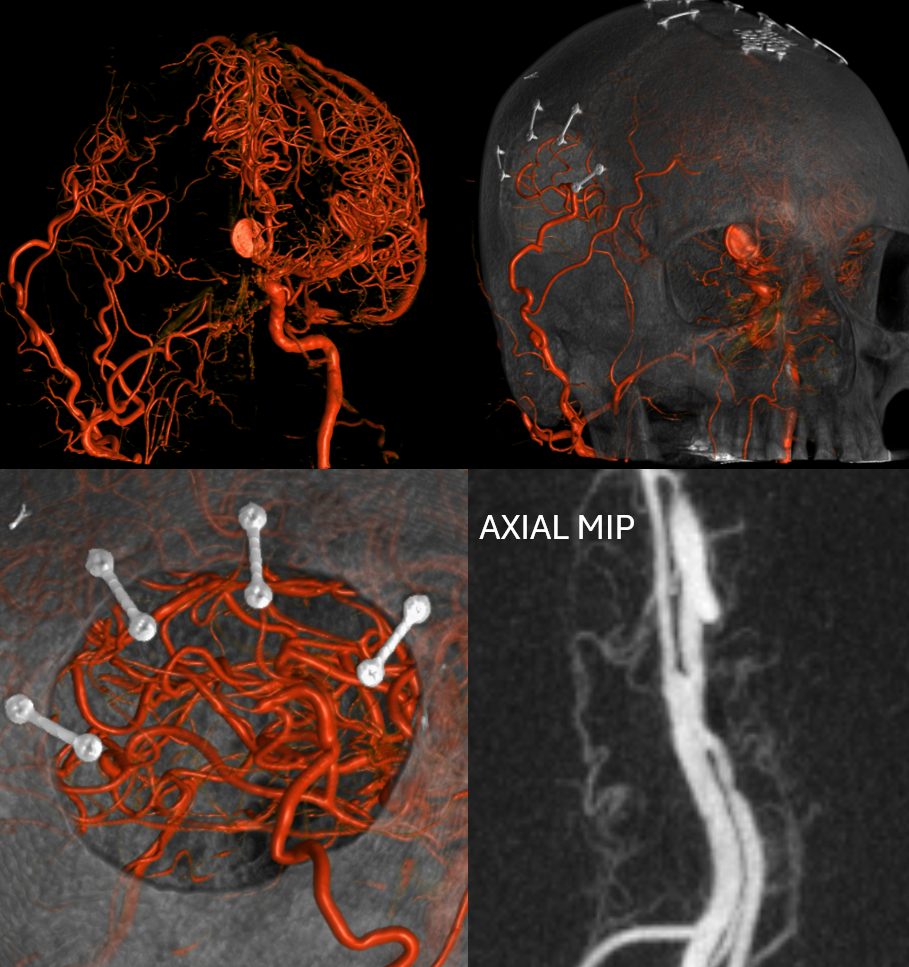
A3-A3 bypass more images

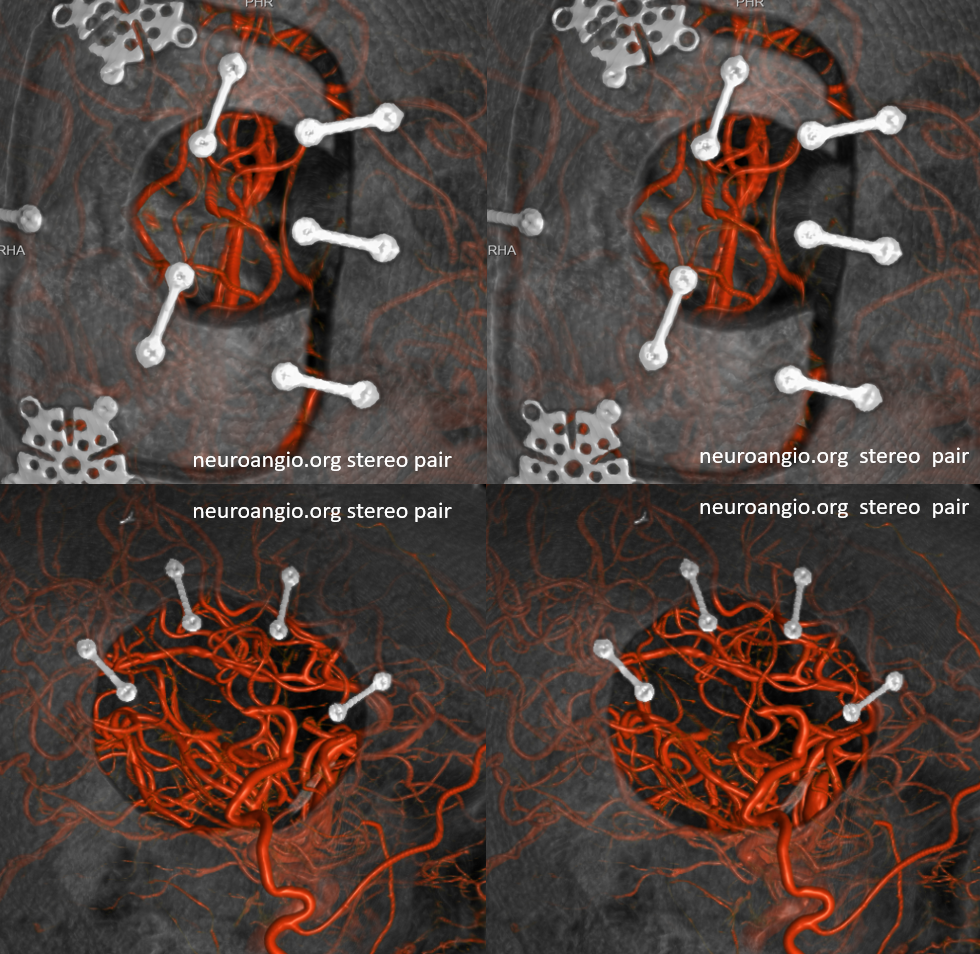
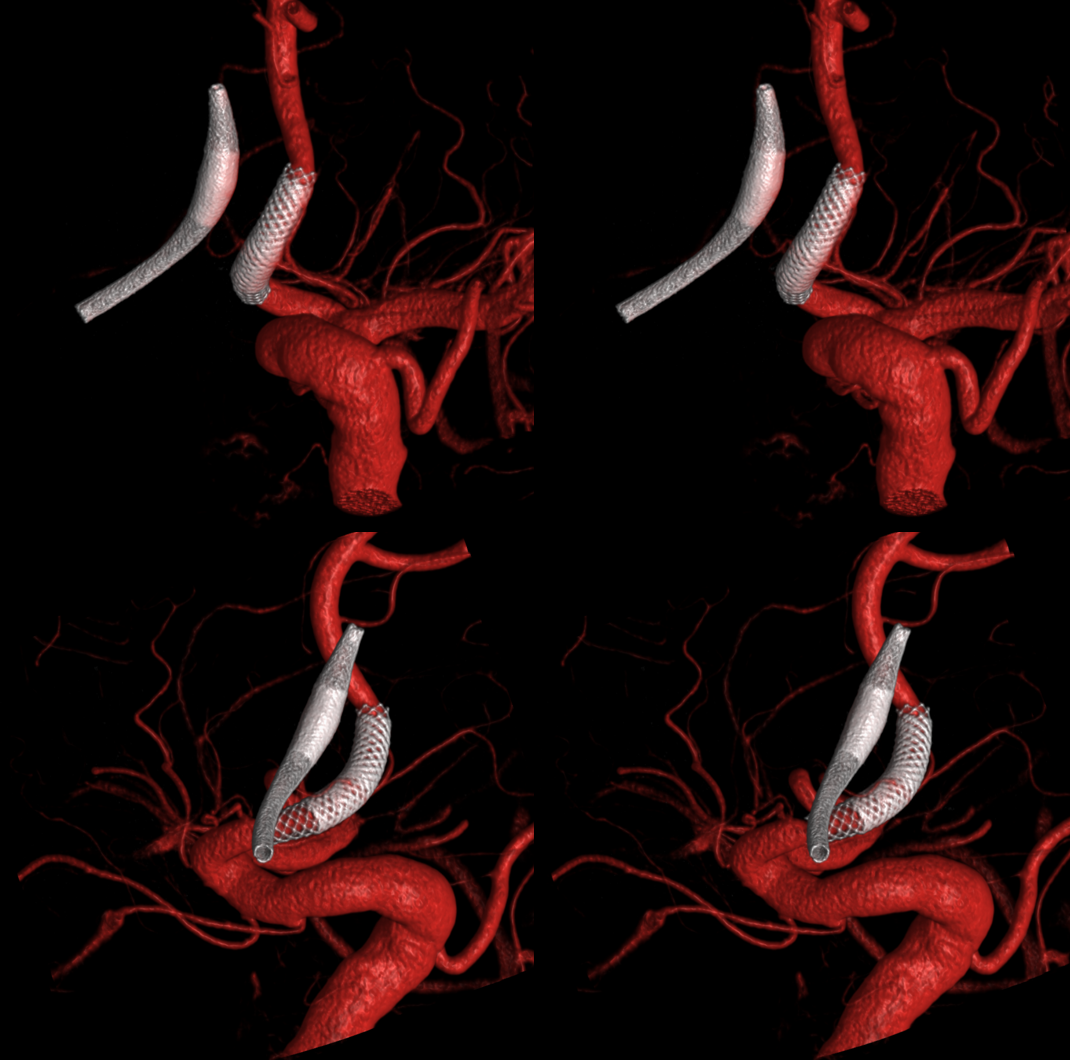
Stereo views of the two craniotomies, with translucent and sonolucent closure
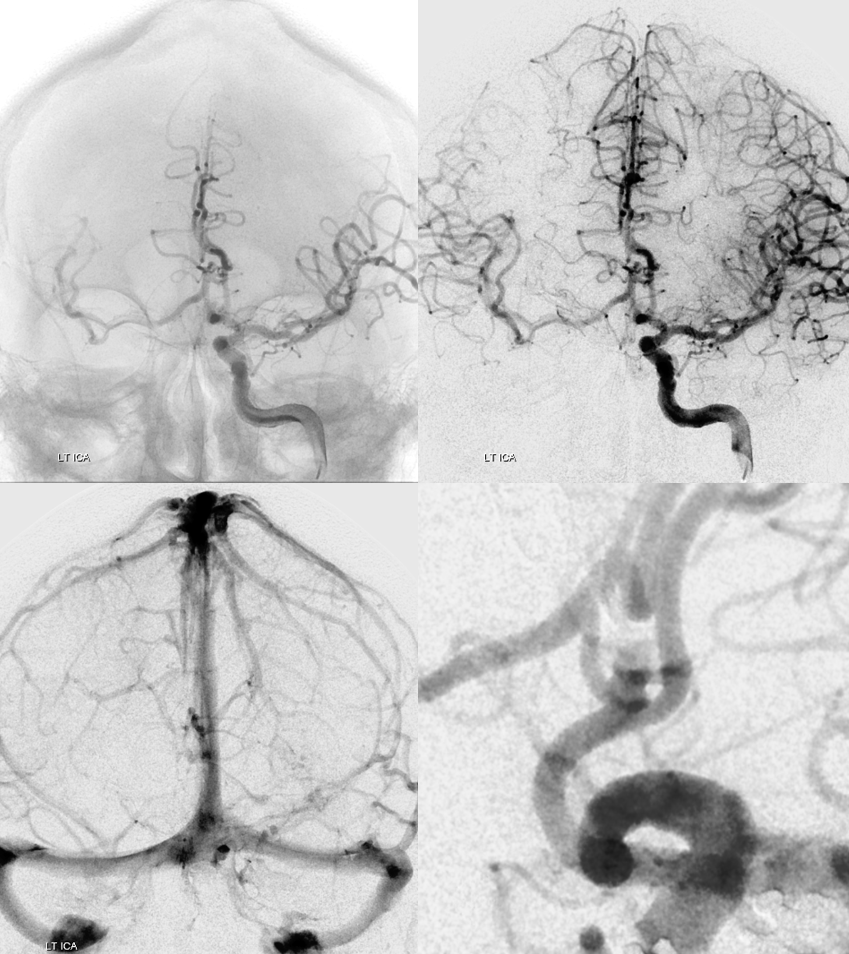
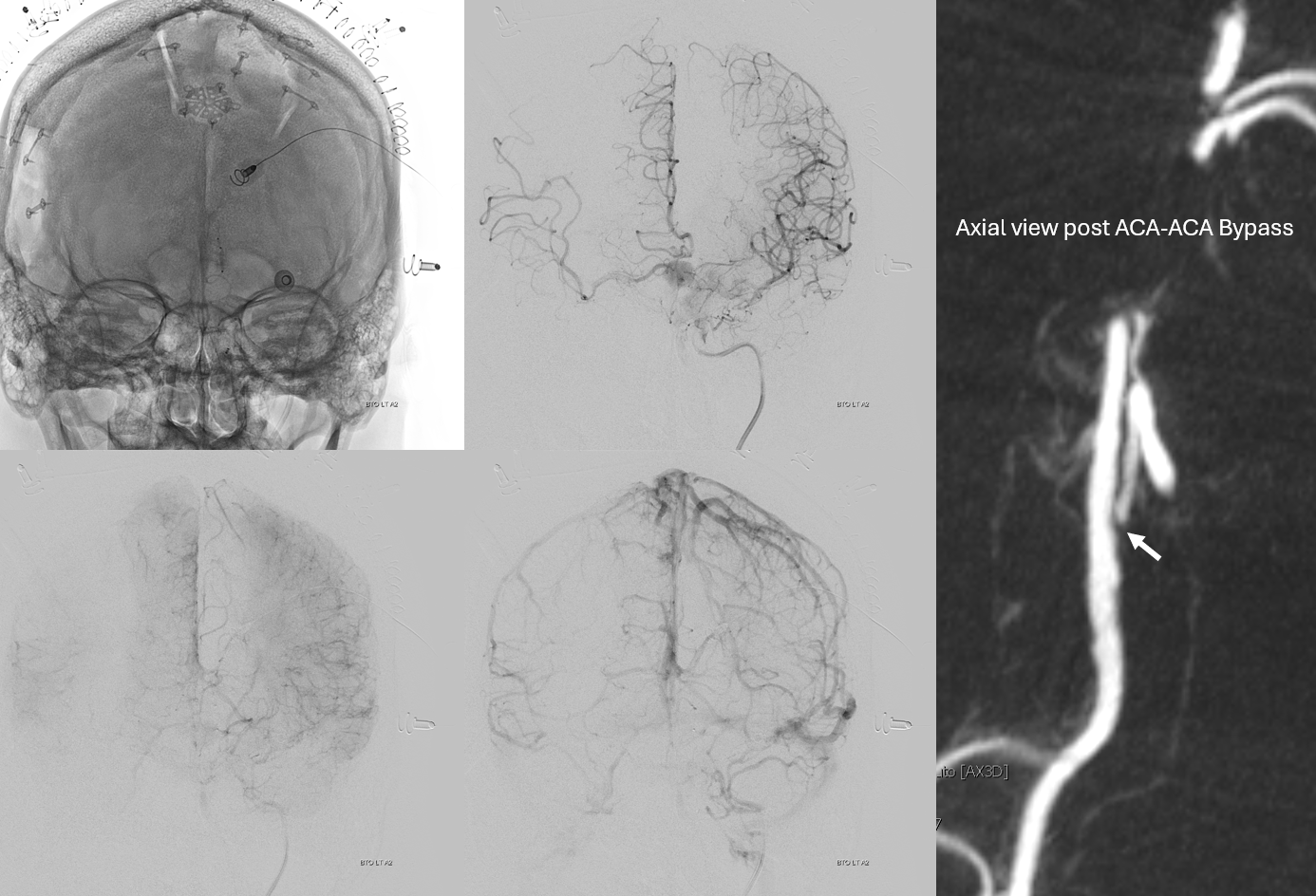
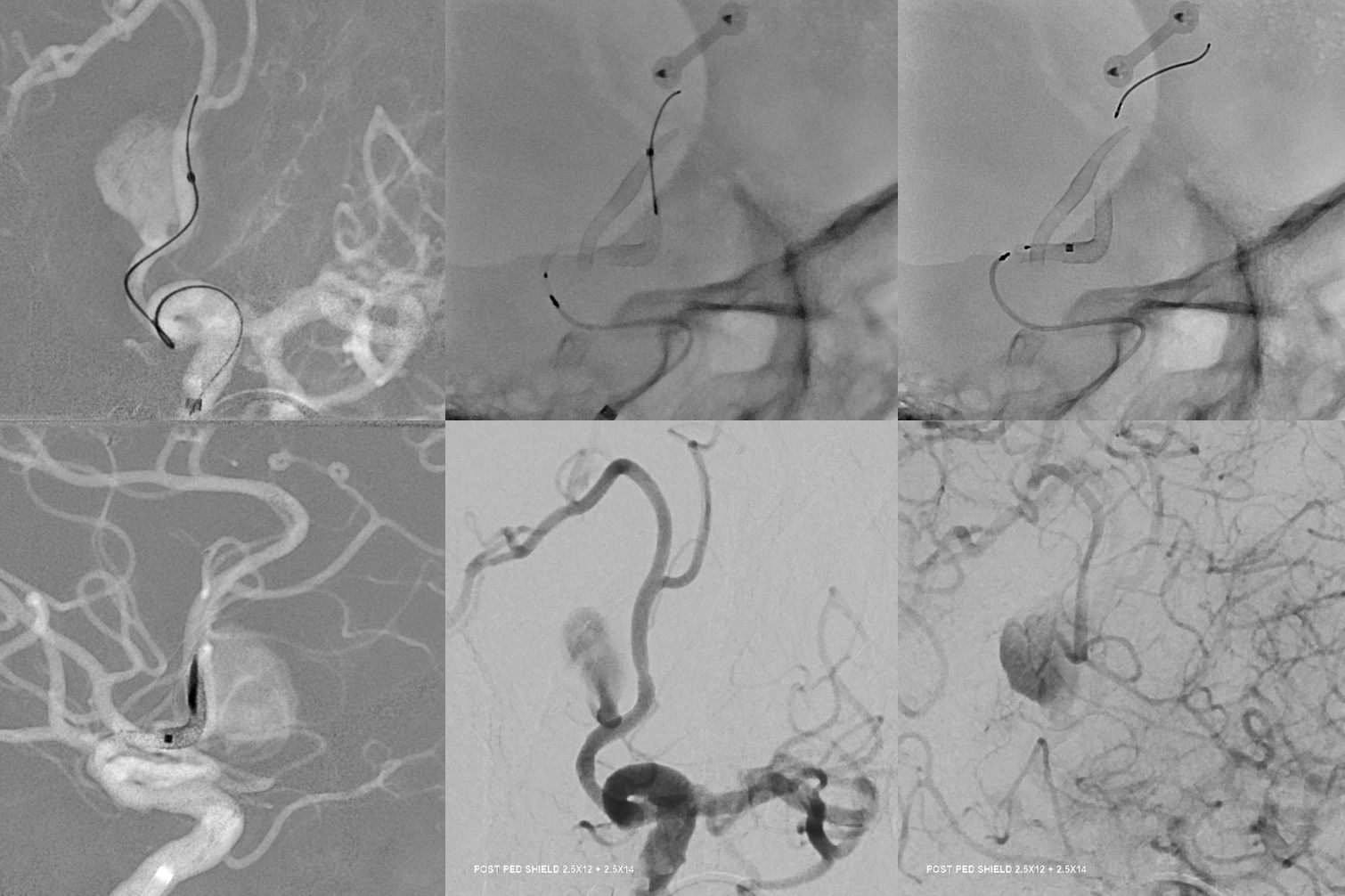
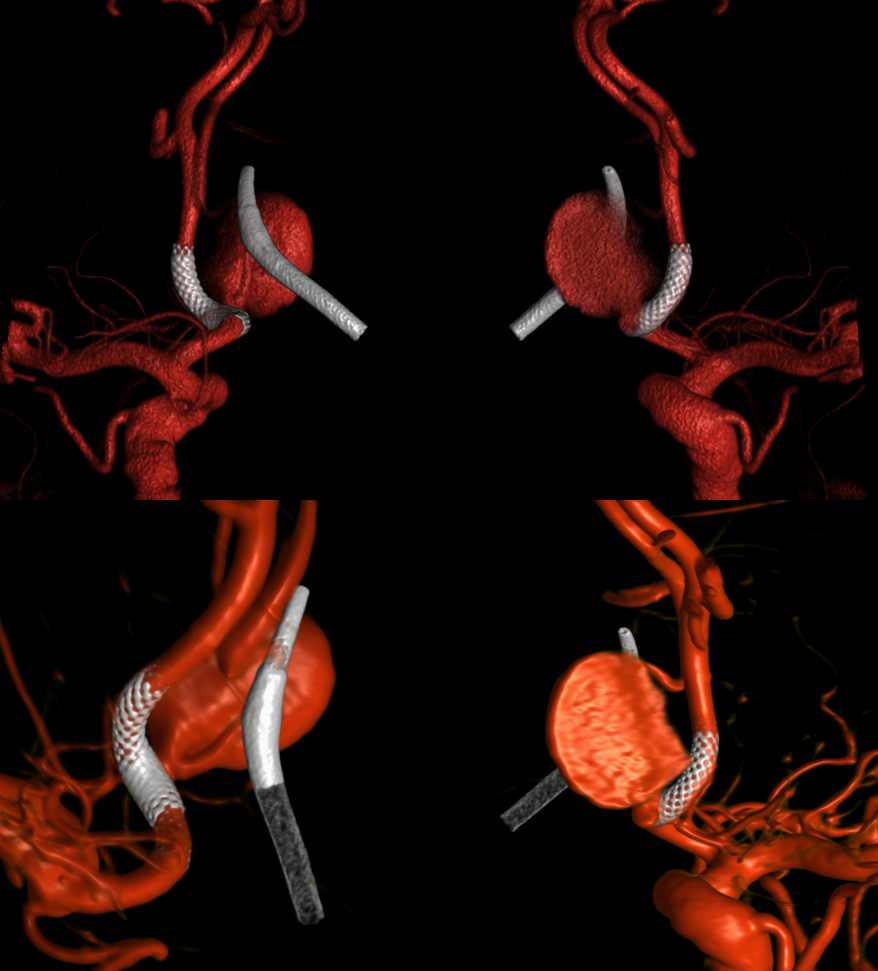
Can we sac the ACOM now? Coil aneurysm and the ACOM? Why not? Can argue for that. We choose H-Flow Diversion. A1-A2 bilaterally. On the right, we have to access the A1-A2 via the PCOM. This is not a job for 27 or 21 catheter. Plan for Silk Vista Baby on right and Pipeline Shield on left
Aristotle 14 soft and Scepter C 4×10
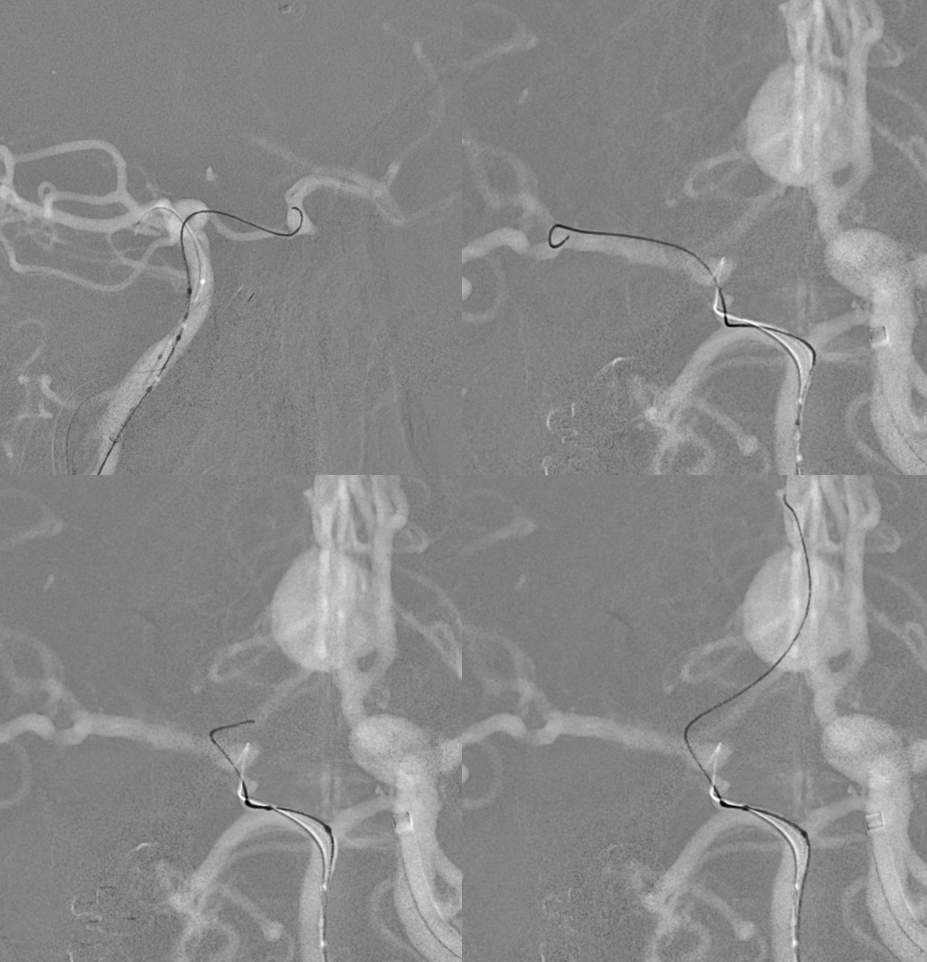
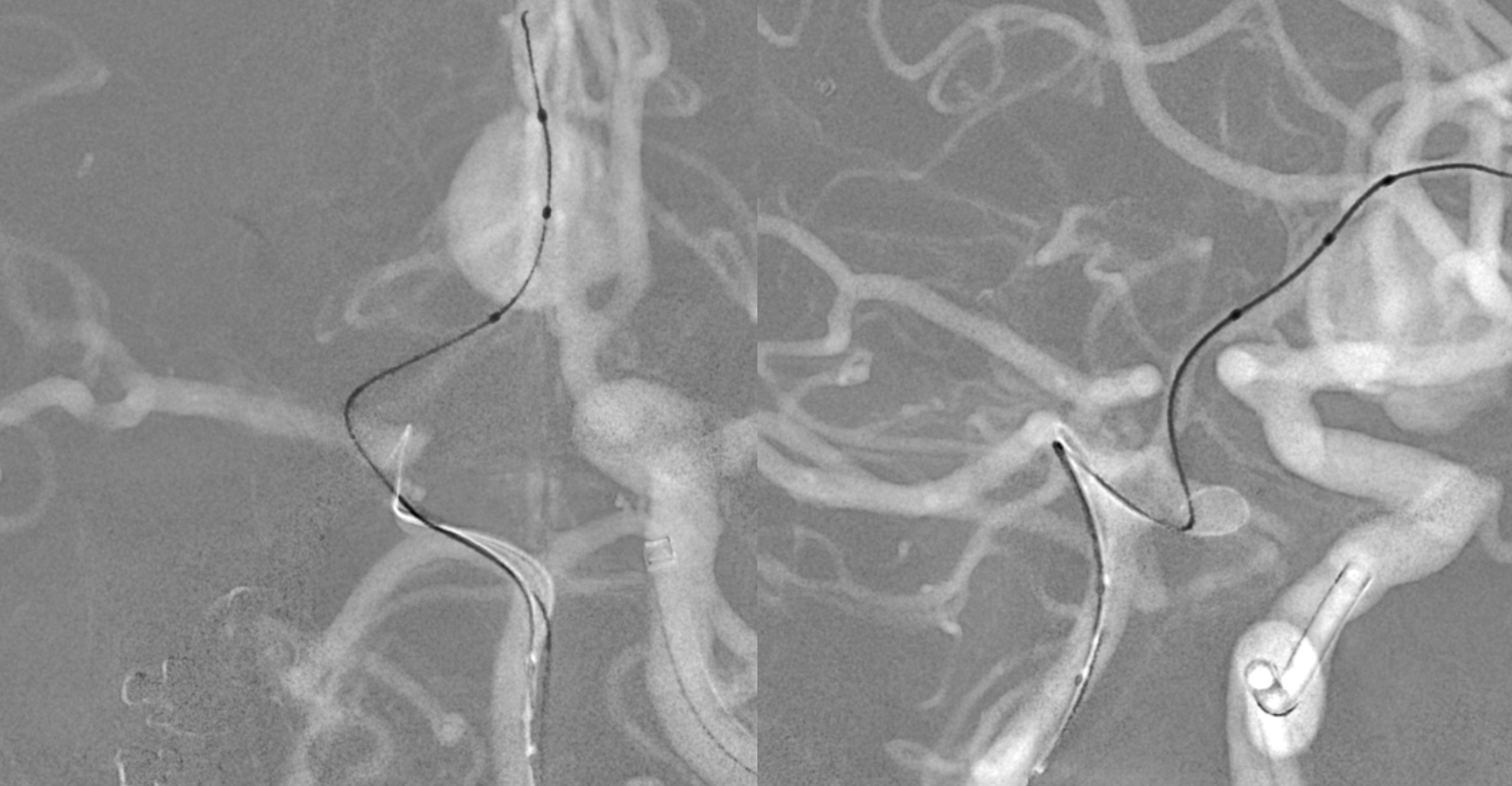
Now we do a BTO of the right A2. Its not a perfect occlusion there is a small endoleak. Still, the brisk filling of right A2 suggests what?
The first SVB is deployed. However, there is a concern. What is it? Look at the measurements of the SVB and the landing zones
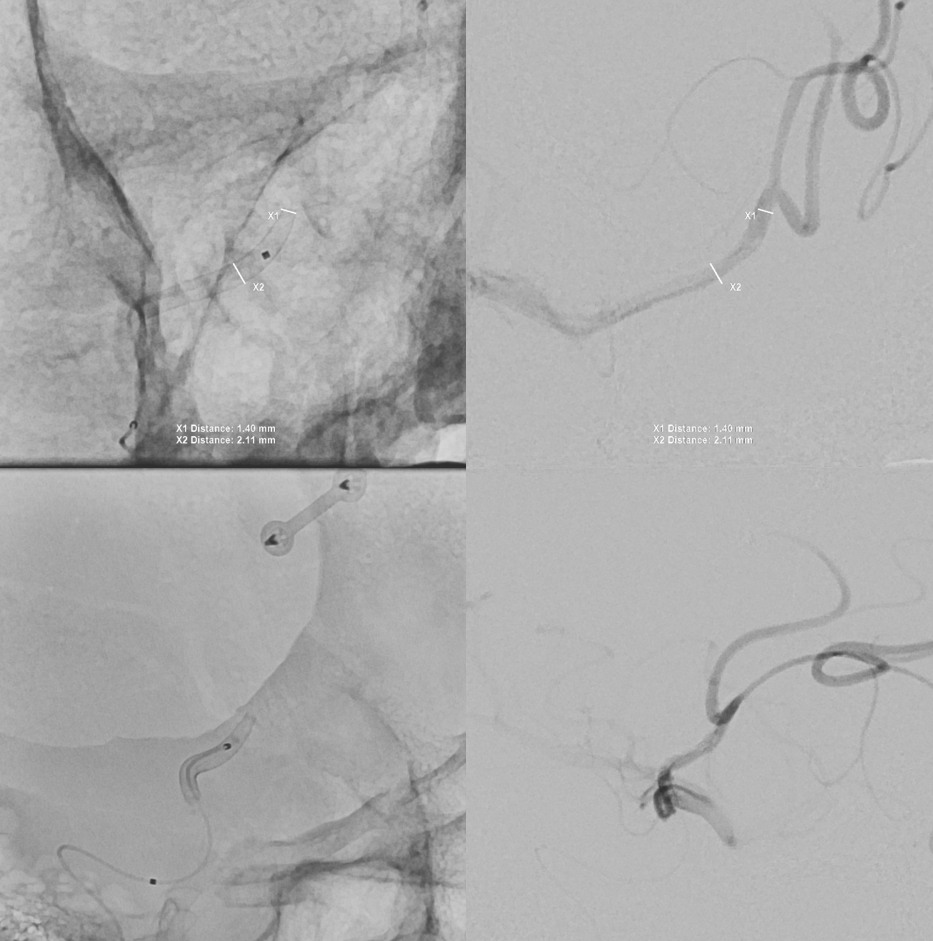
The answer is possible endoleak. The distal landing zone may be too short for a nitinol device. The diameter of the proximal SVB is smaller than the expected diameter of the A2 target. Its a critical point. If this is missed, the treatment may fail
The answer is to either balloon it or put in another device. We put in another SBV, now extending it into one of the A2 branches. Yes, one can argue that with working bypass you can just close the A1-A2 junction. Sure. But we did not know this before. And we can always do that later by coiling inside the SVB. Here, we keep options open.

Post SVB 2
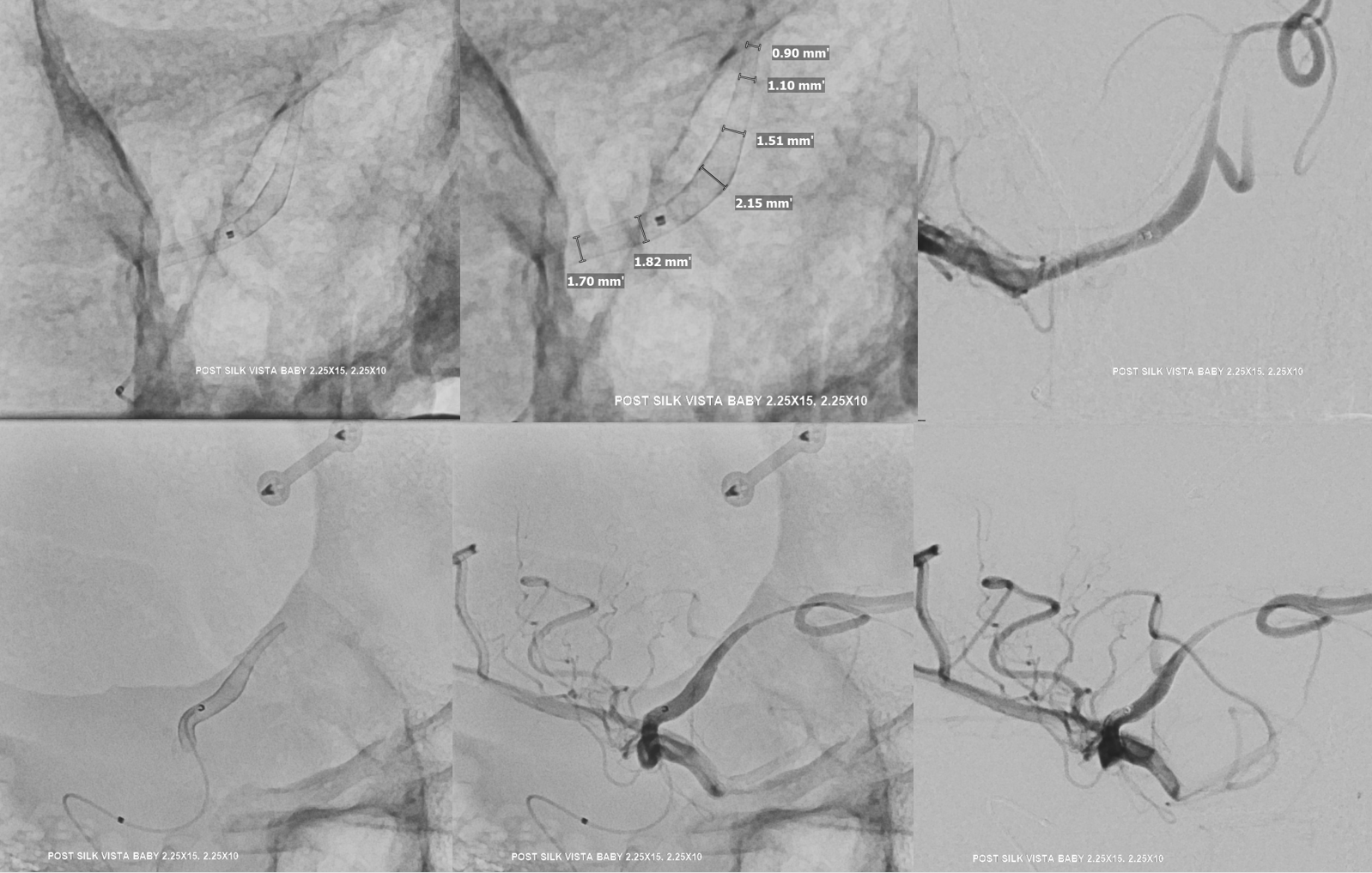
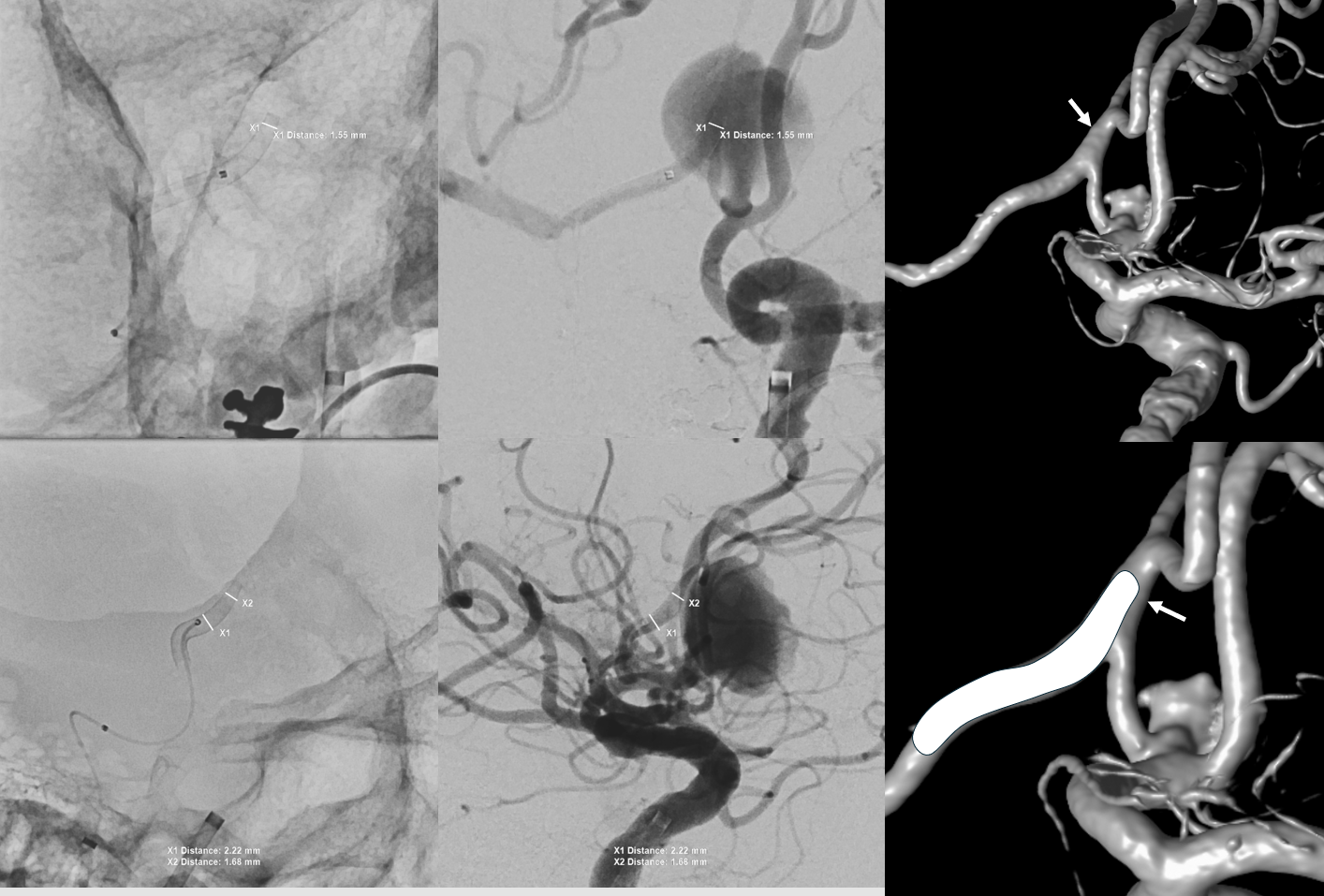
Look at the difference in measurements after SBV 2 (top row) and SBV 1 (bottom row). Arrows point to location of the SVB 1 distal landing zone

Now to the left side
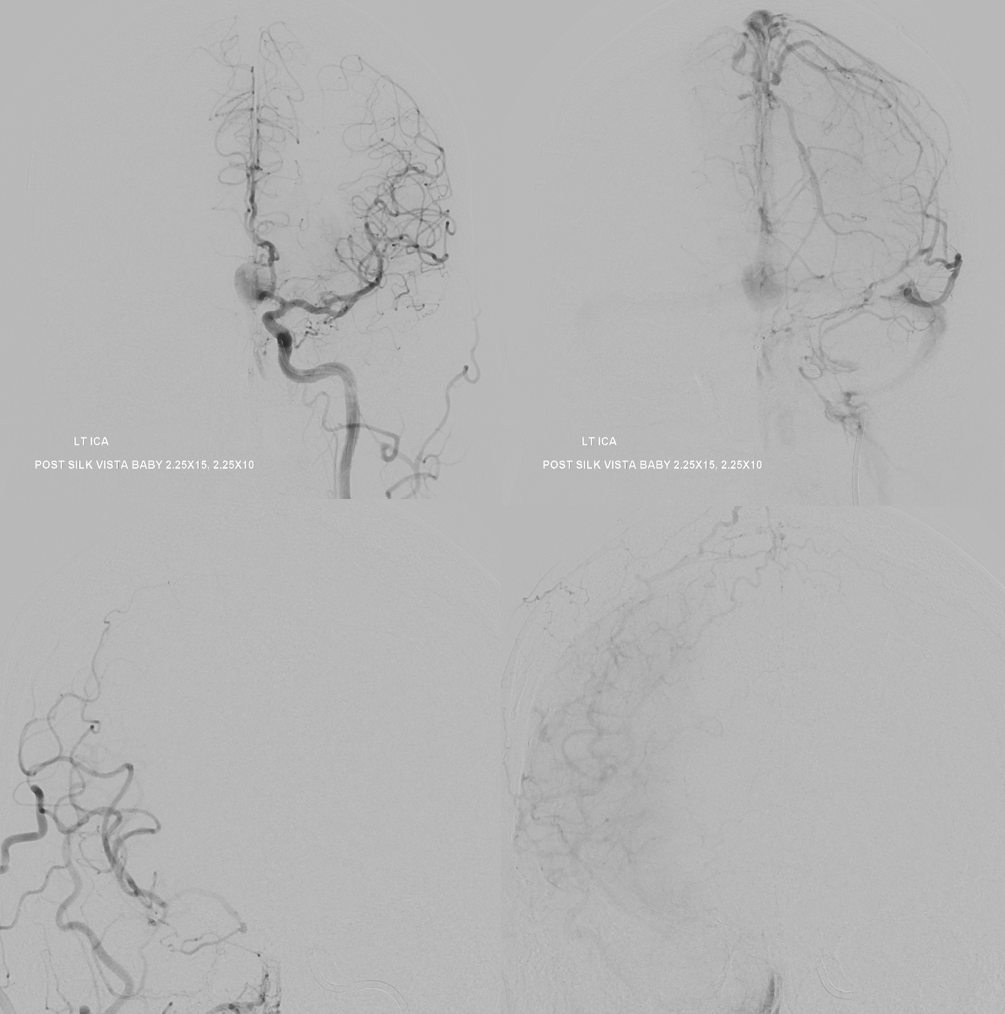
Two Pipe Shields are placed. This is how we work. This big one is not a job for one and done
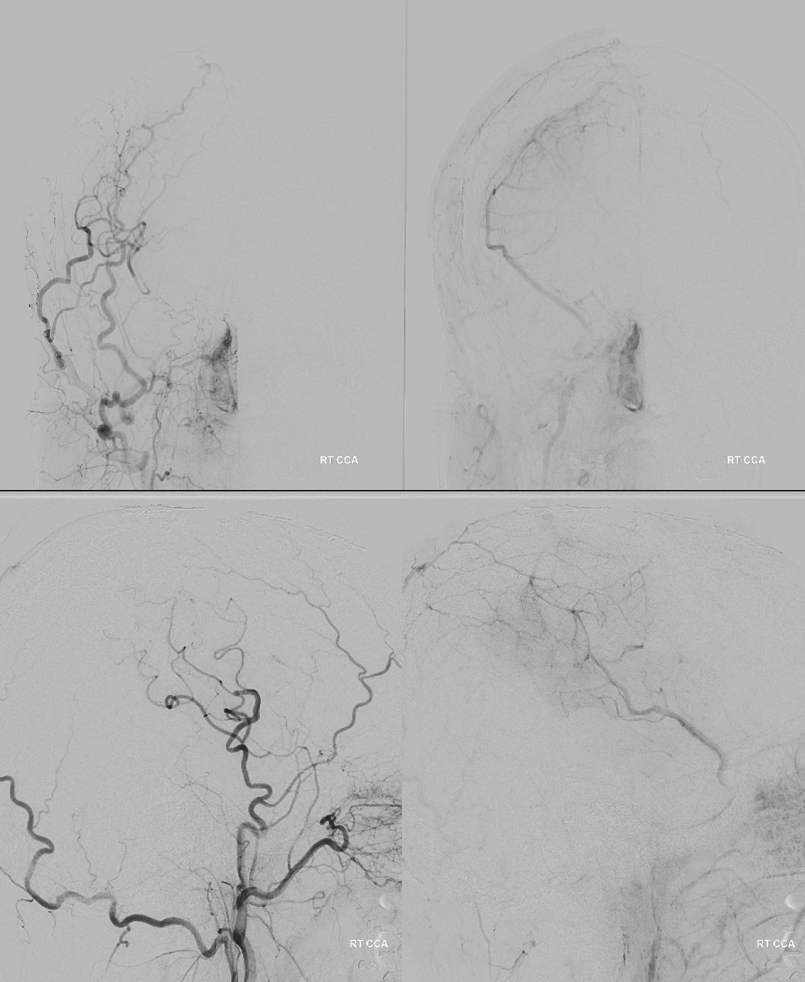
Post. Bilateral injections. The right ACA is supplied retrogradely via the ACA-ACA bypass. The MOST important finding here is that there is no longer flow across the ACOM. This is what flow modification is. Changing dynamics to impact aneurysm.
Movie
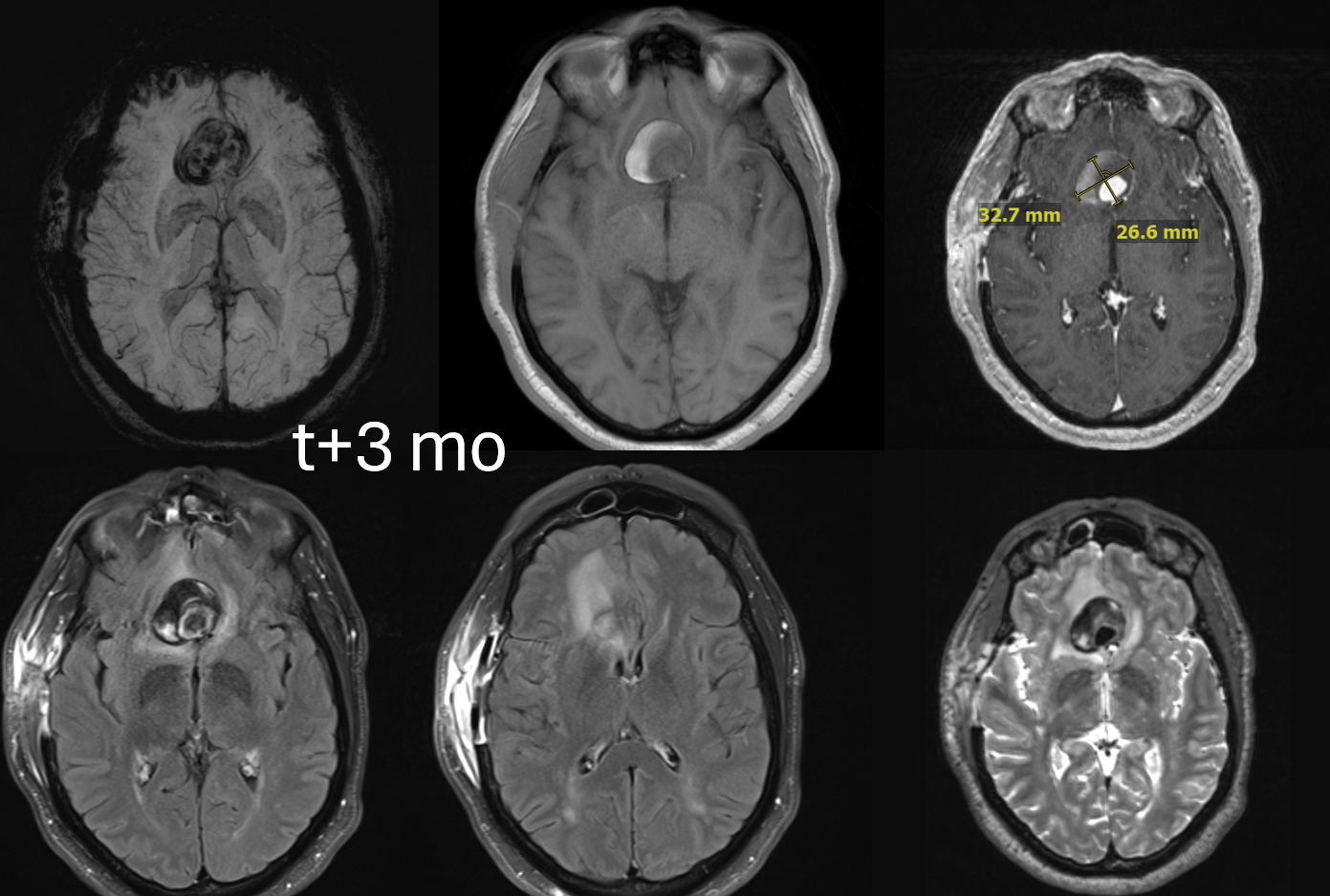
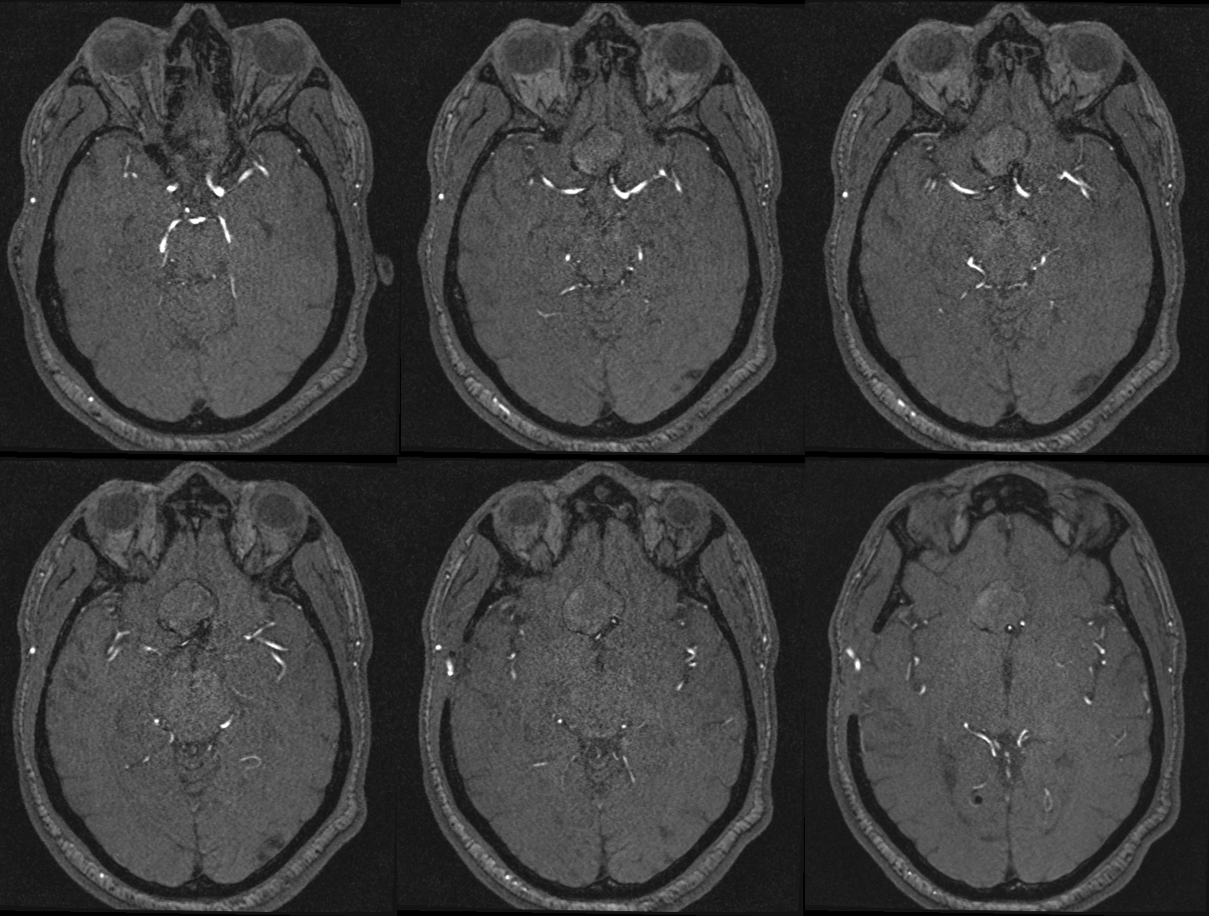
One month later — only 1 mo. Aneurysm thrombosed. Right A1-A2 patent — can tell on MRA even with two SVBs
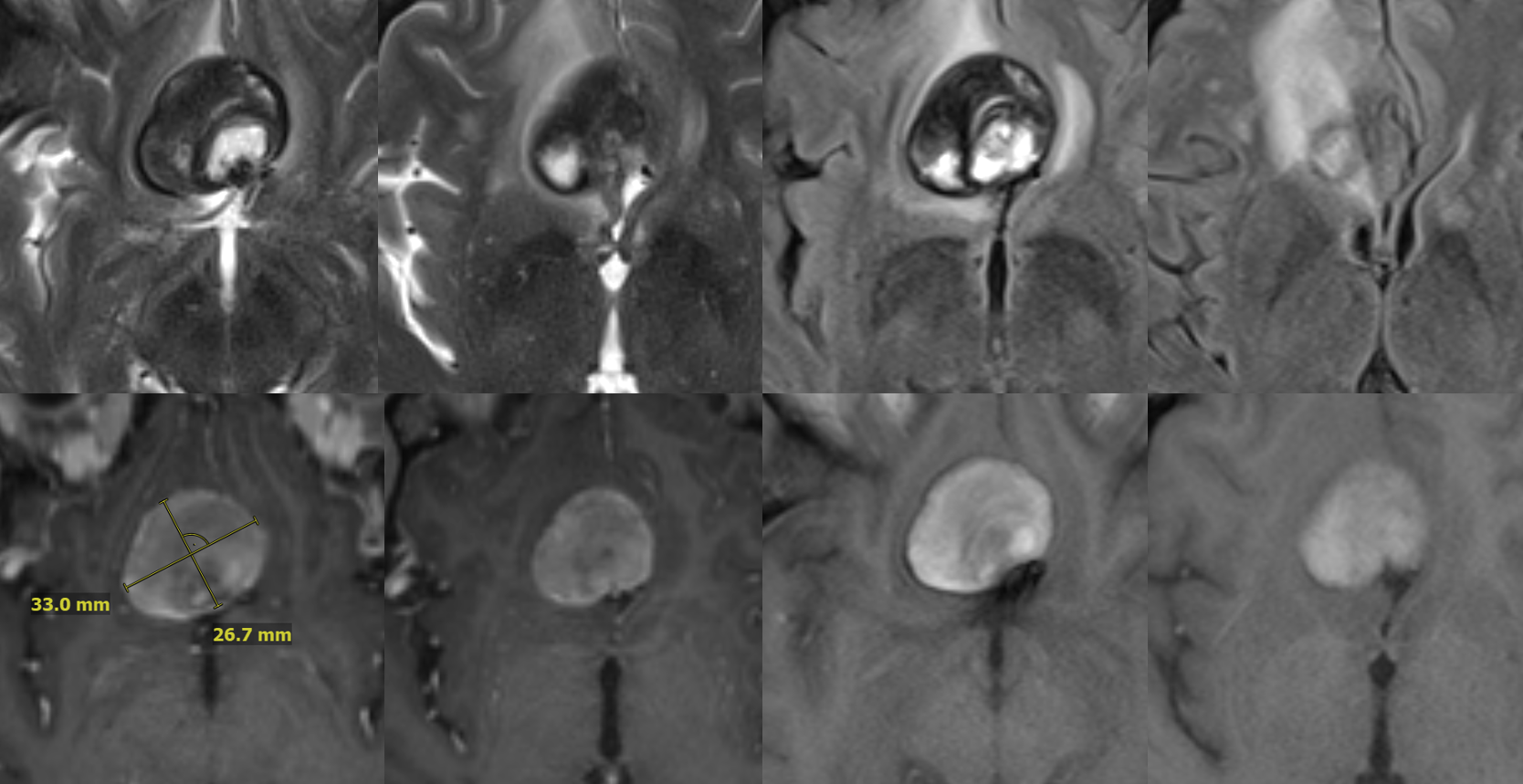
Several months later, MRI looks fantastic — no edema, smaller, etc. This MRI is actually enough to know the aneurysm is gone. Its more sure than angio.
MRA
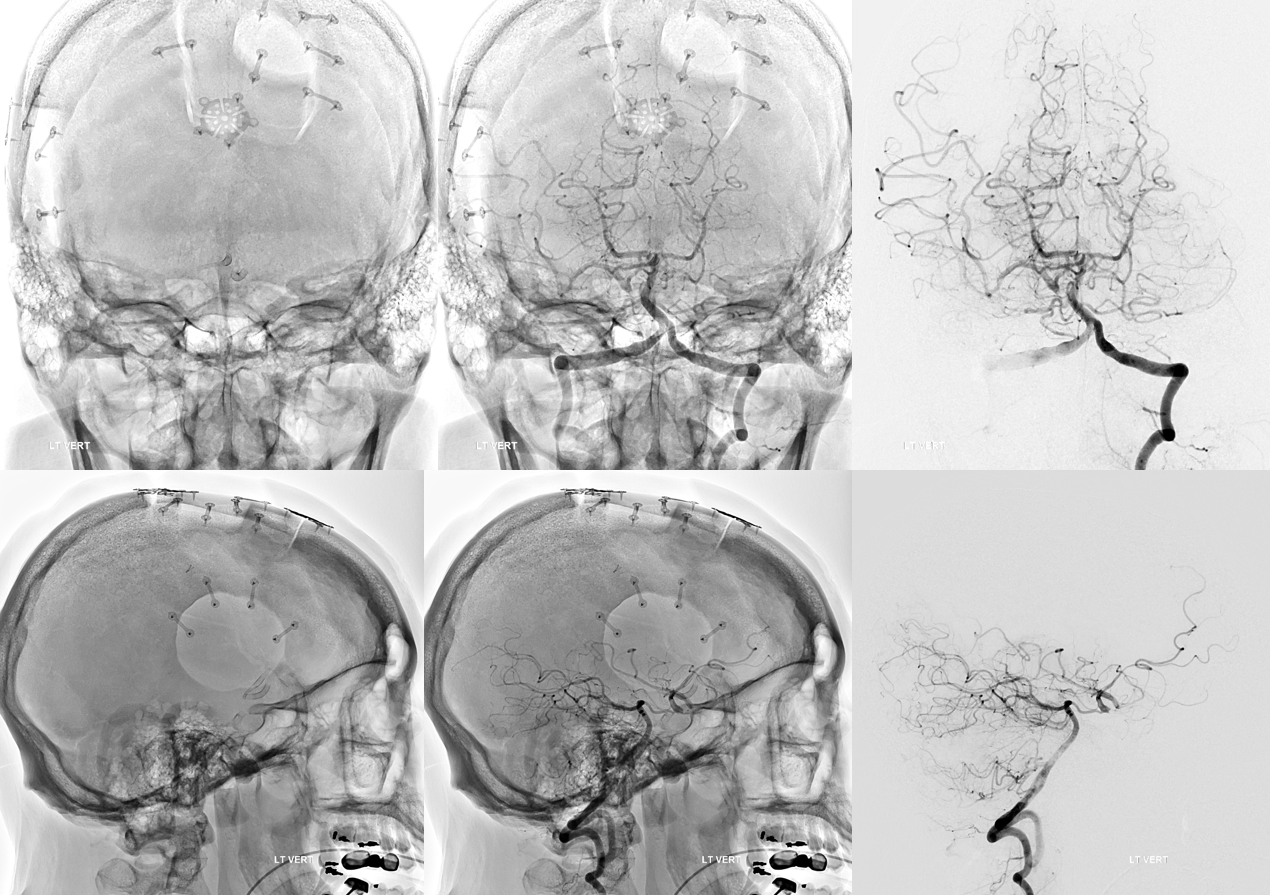
Robust bypass supports superior division and some more
No aneurysm, as suspected

Stereo pairs

Bypasses. Note A3-A3 patent bypass, as well as STA-MCA. Both seen thru radiolucent skull windows