This is a case of a patient with left-sided mastoiditis / abscess and secondary sigmoid/jugular thrombosis. Treated with antibiotics and anticoagulation. Three months later, he is admitted for another problem.
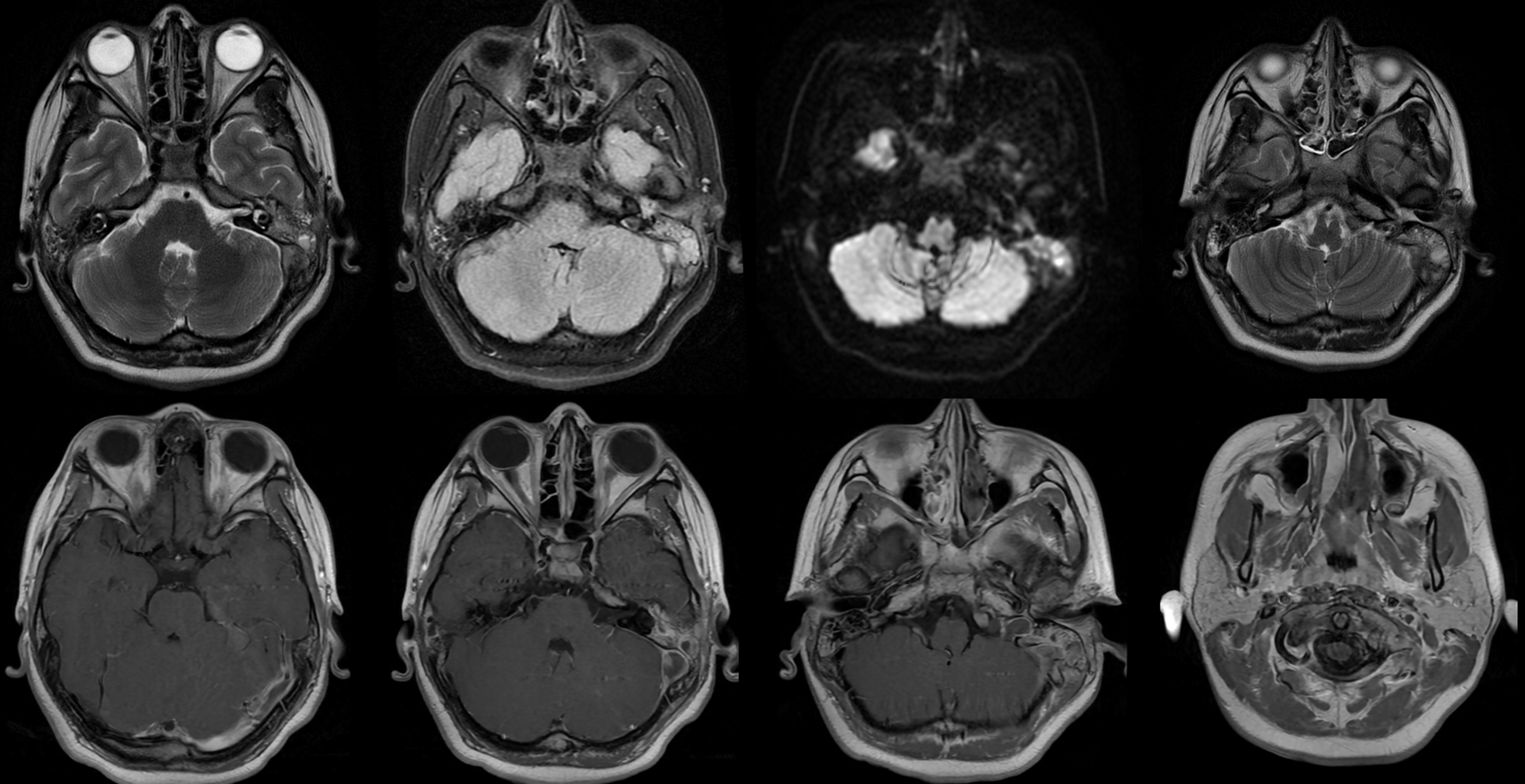
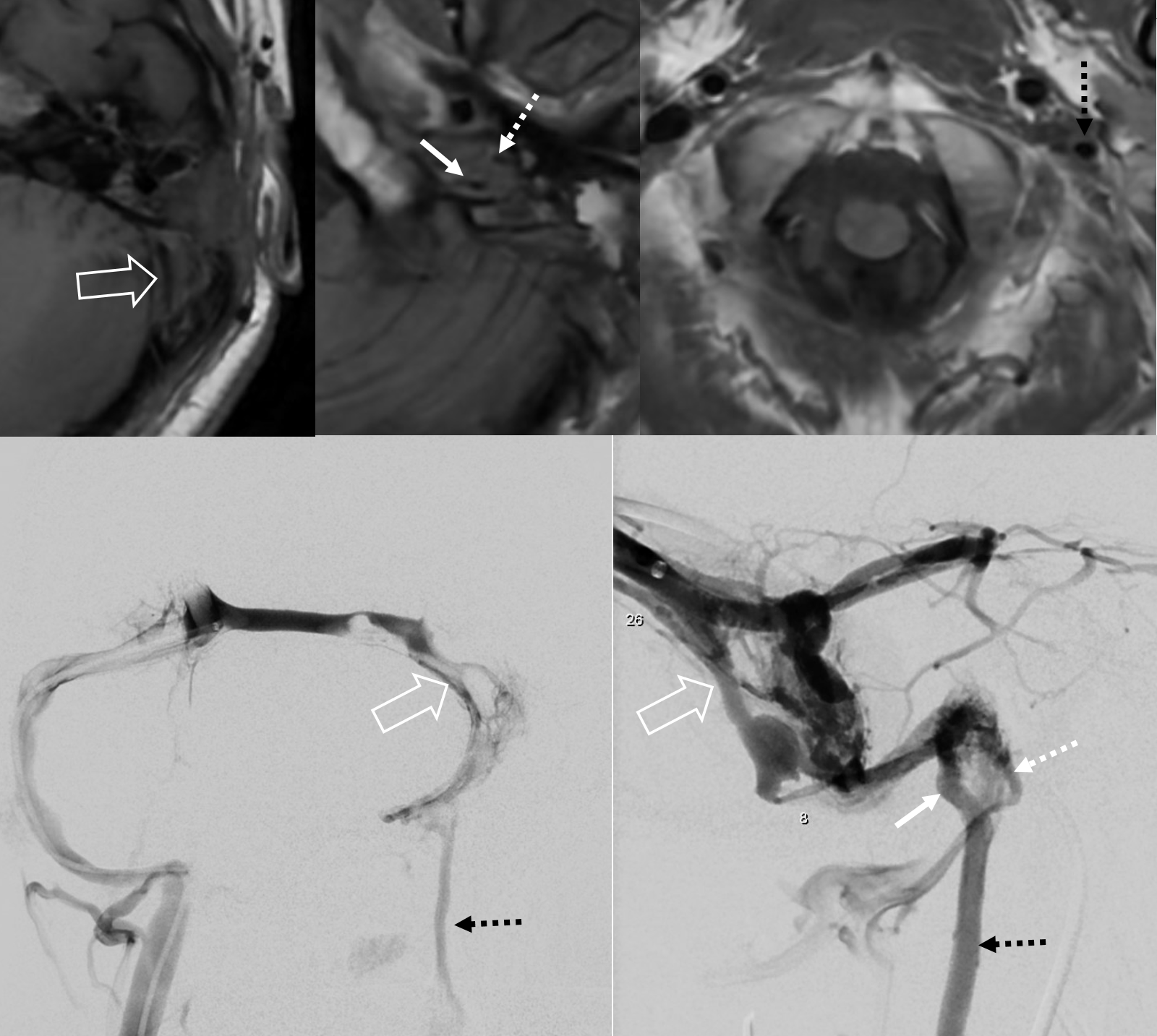
Initial scans:
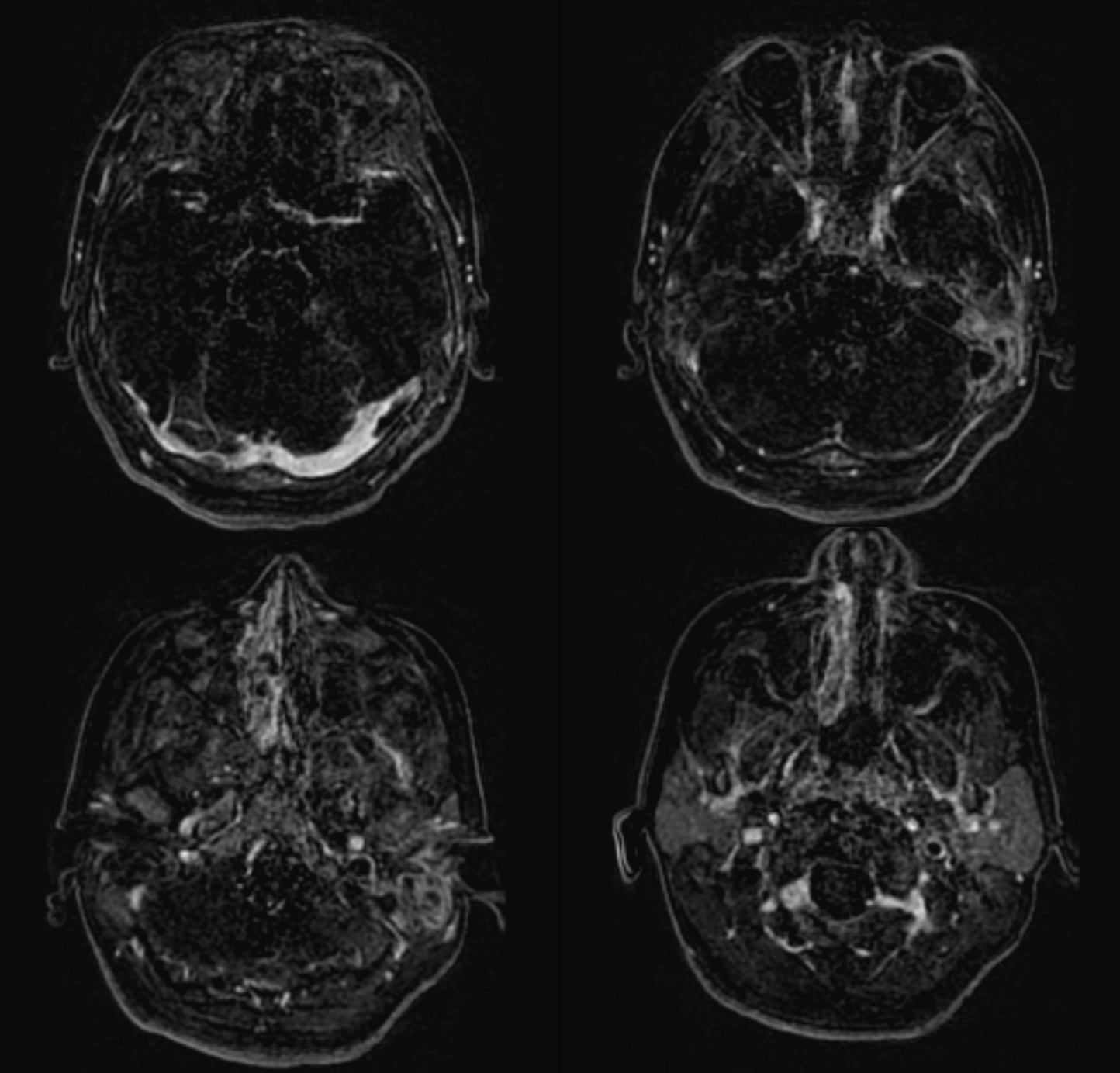
Three months later, infection is clinically cured. Sinus seems better. But there are problems…
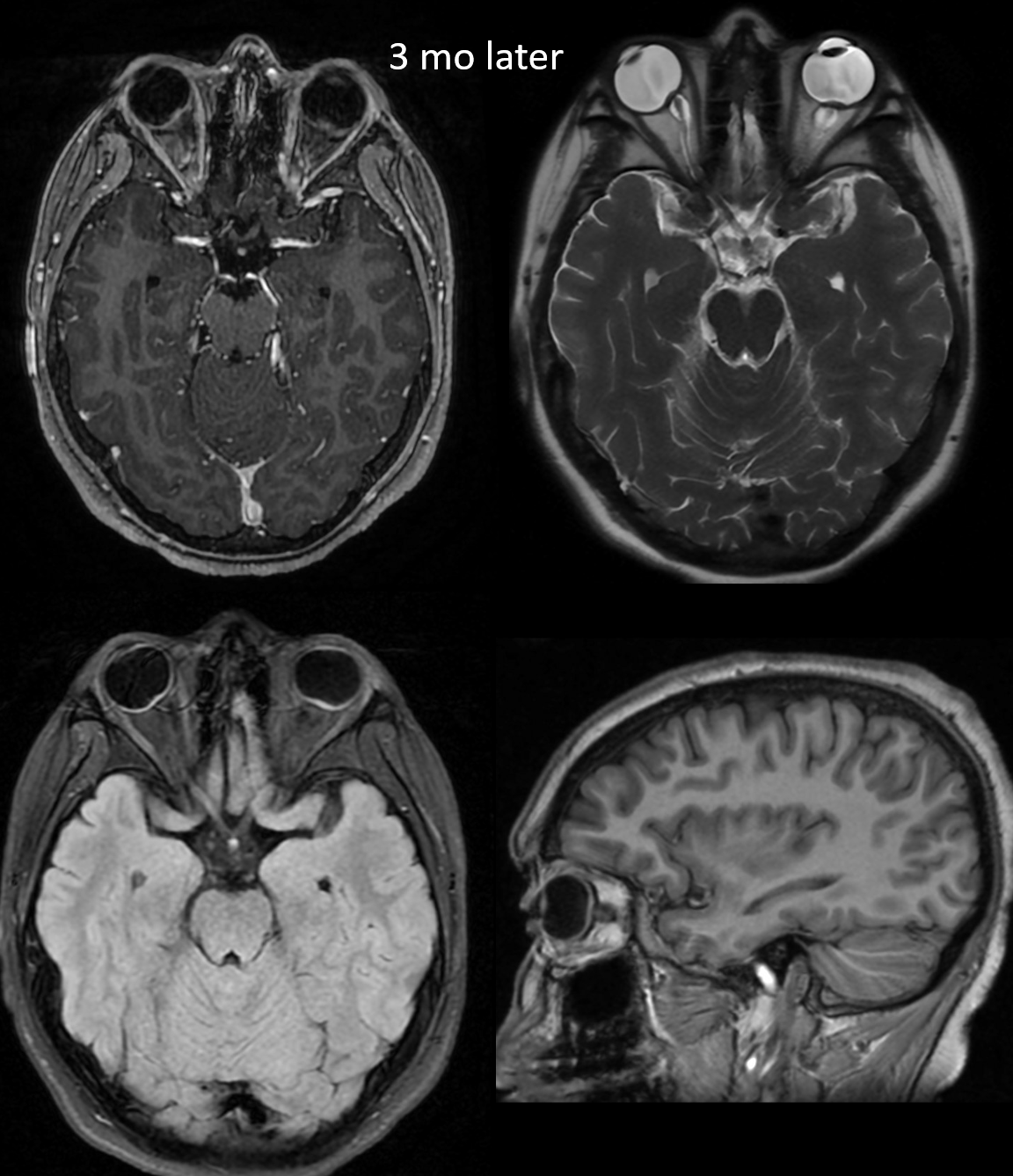
MRI below looks good right? What’s not to like?
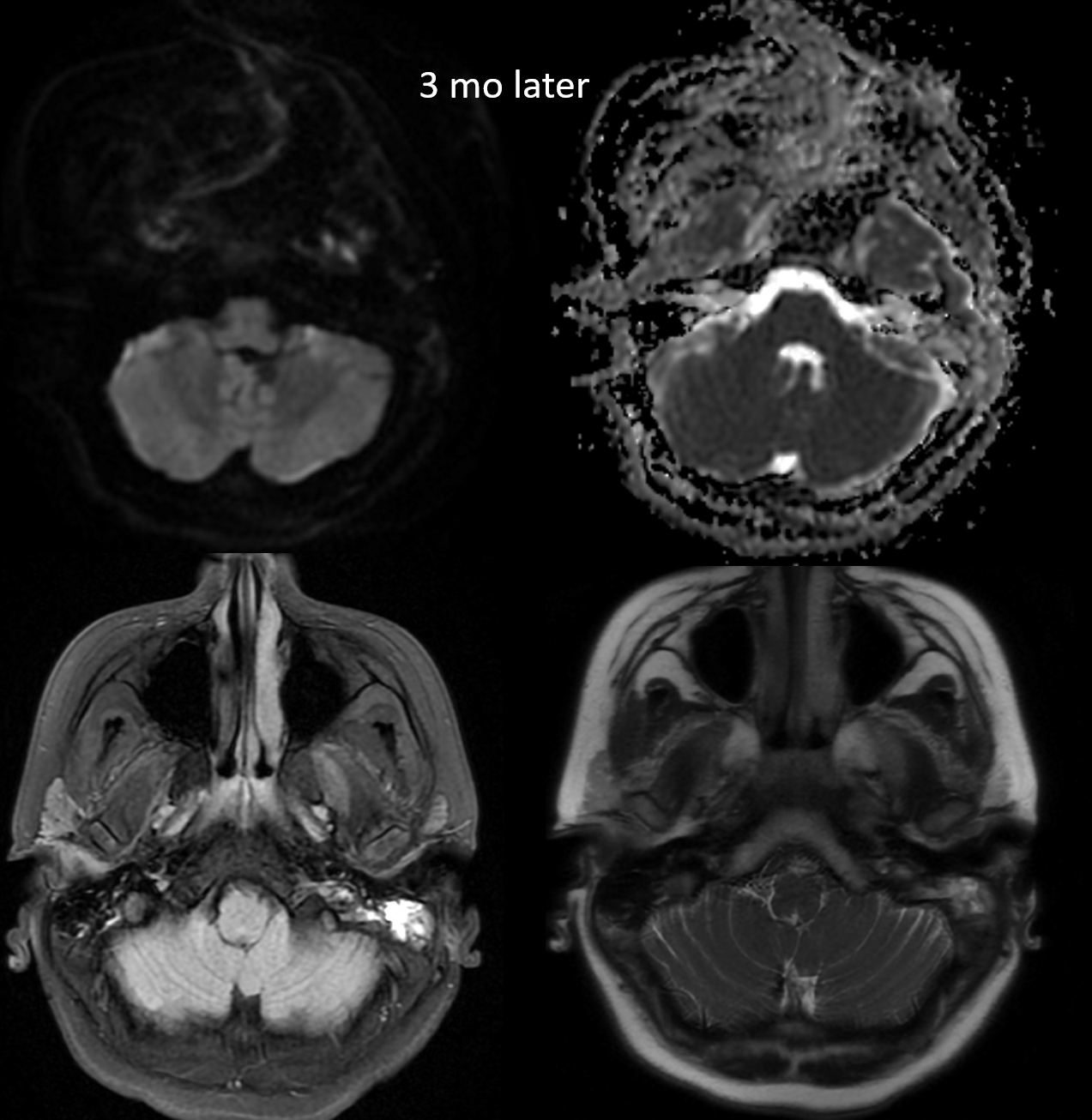
MRV — still some thrombus in the sigmoid sinus and jugular bulb, but much better
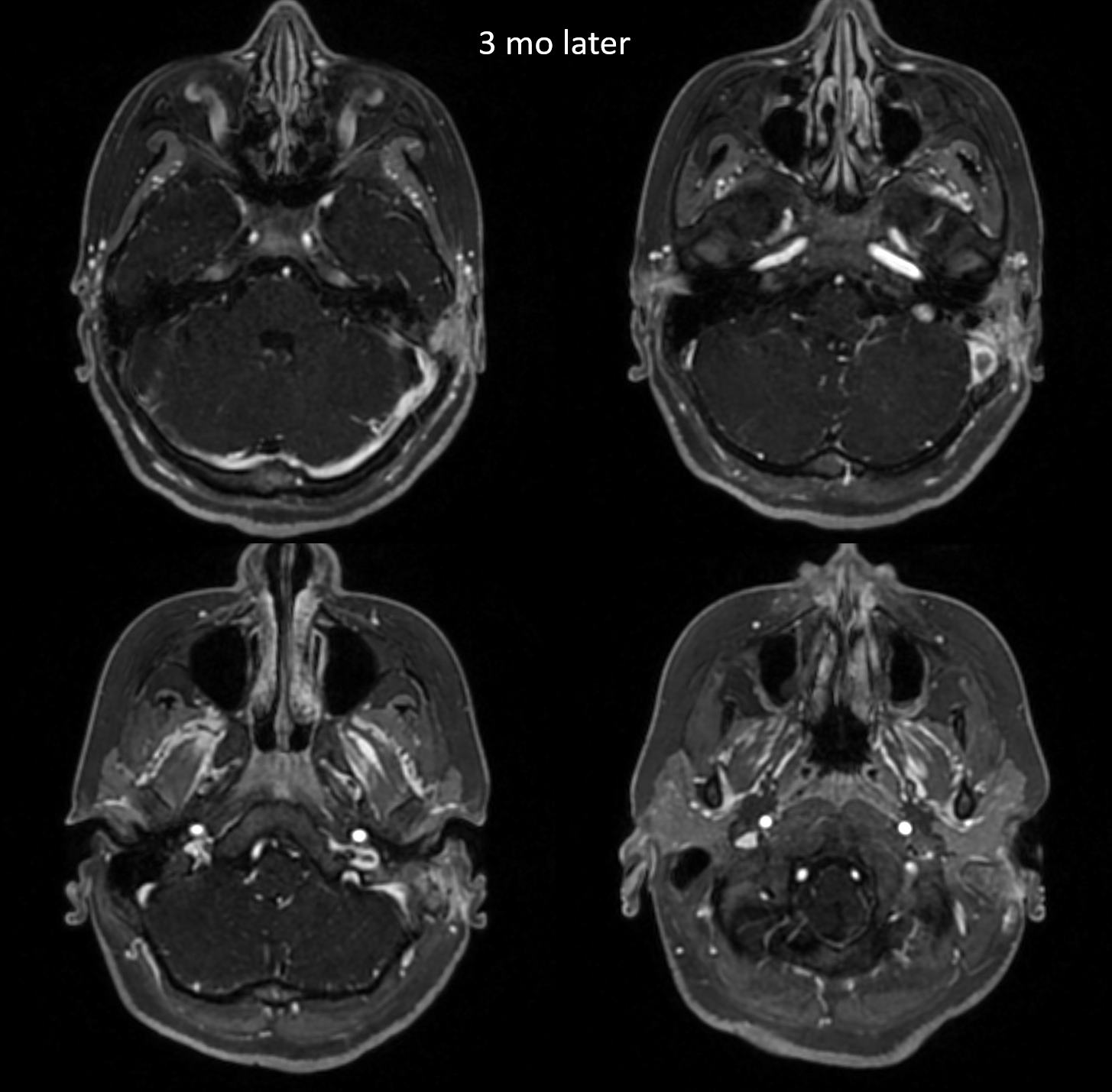
A short while later, another MRI looks even better. Unfortunately, the patient does not.
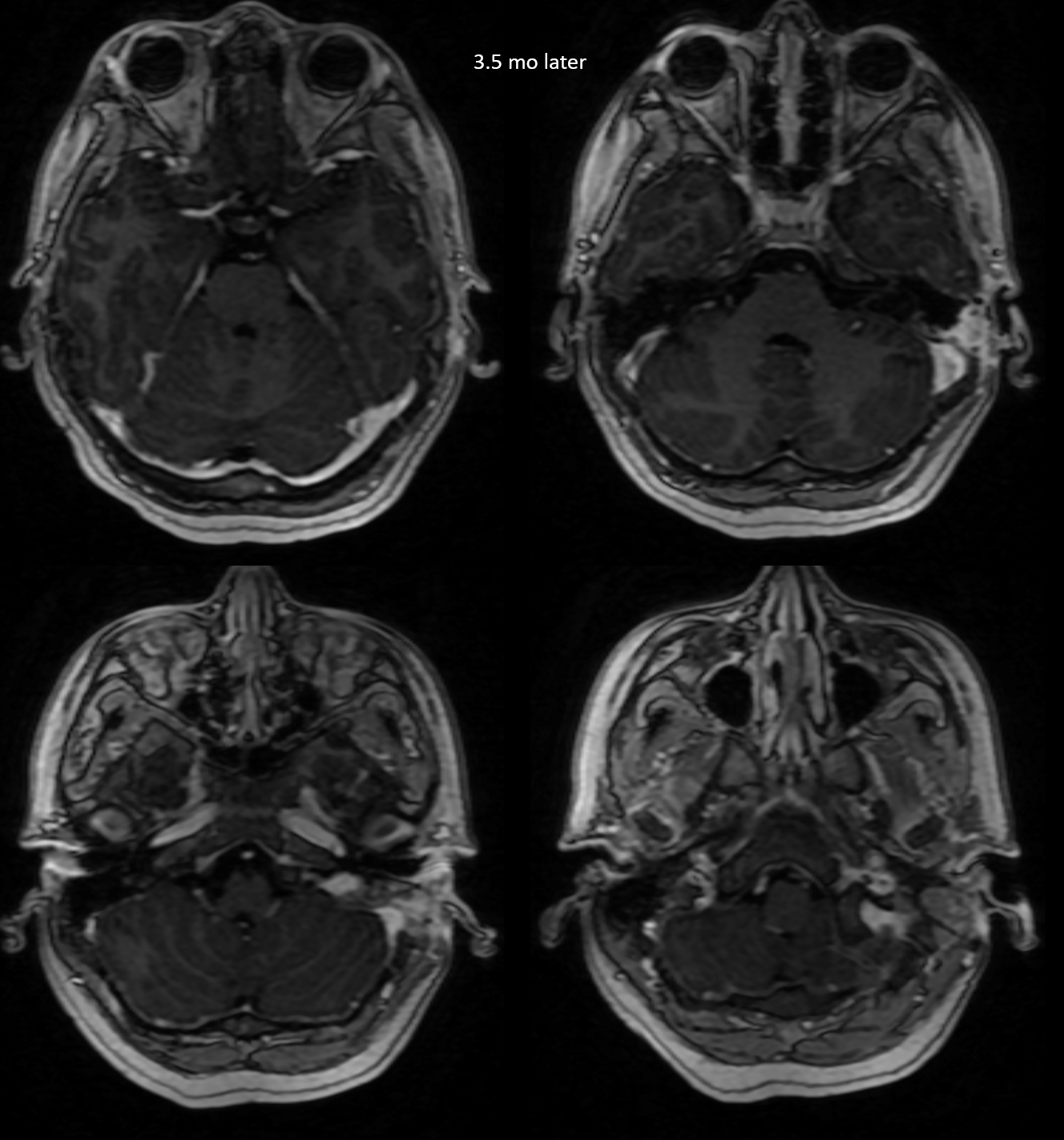
What is the problem?
We are called to see what can be done. By now, it is clinically very apparent that there is a venous drainage problem, despite improvements in MRI
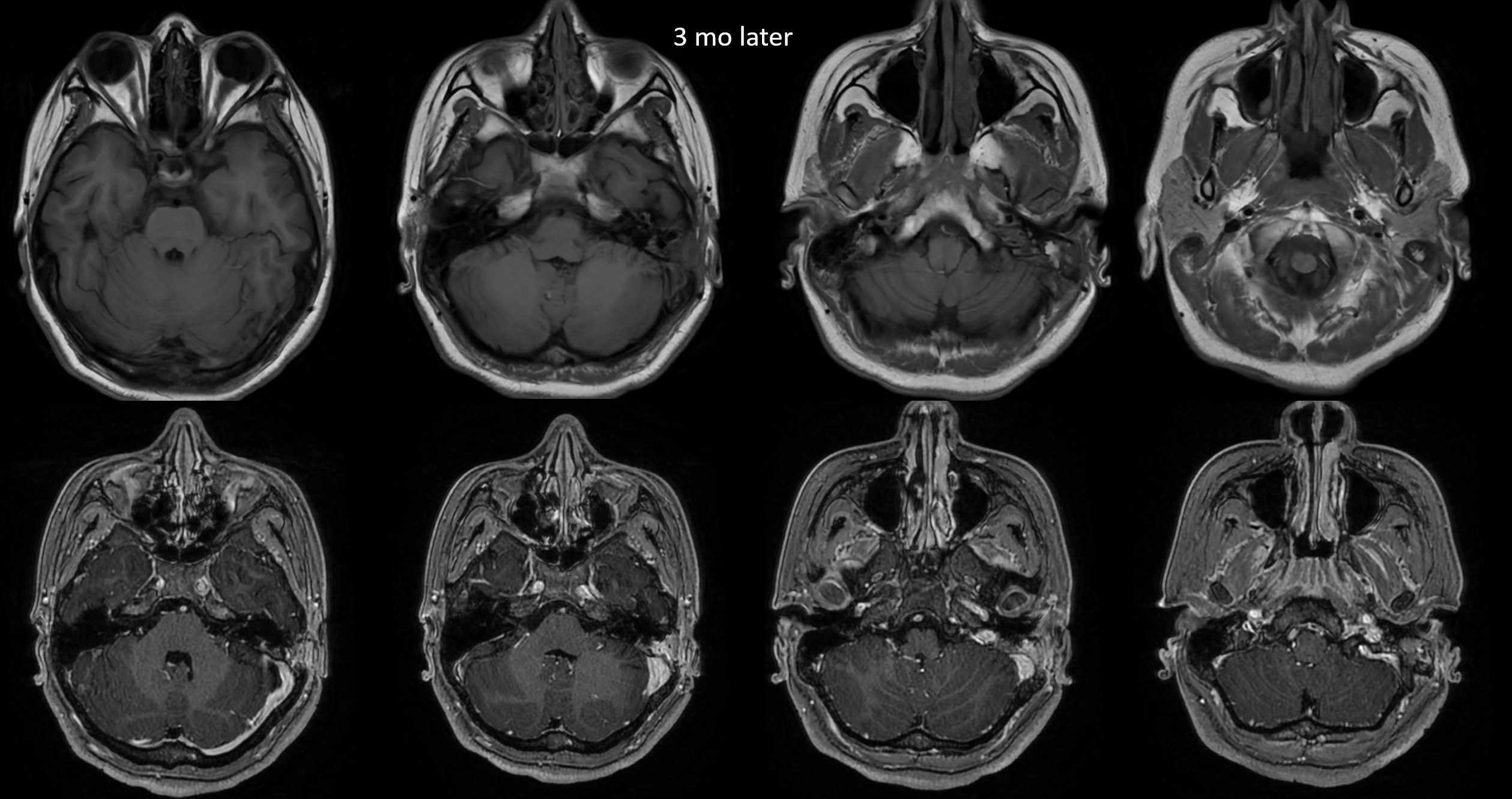
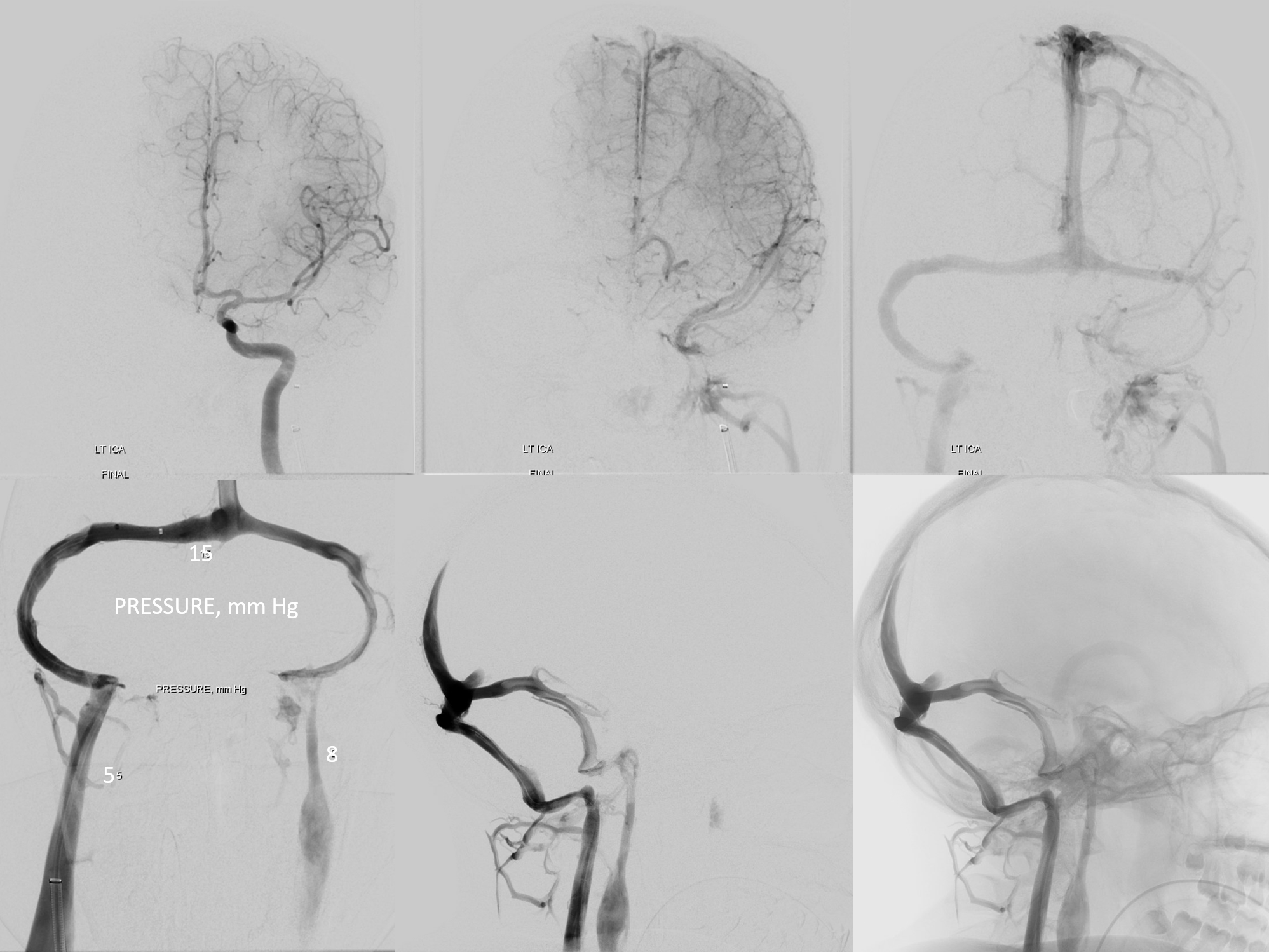
Angio venous phase images. See the problem?
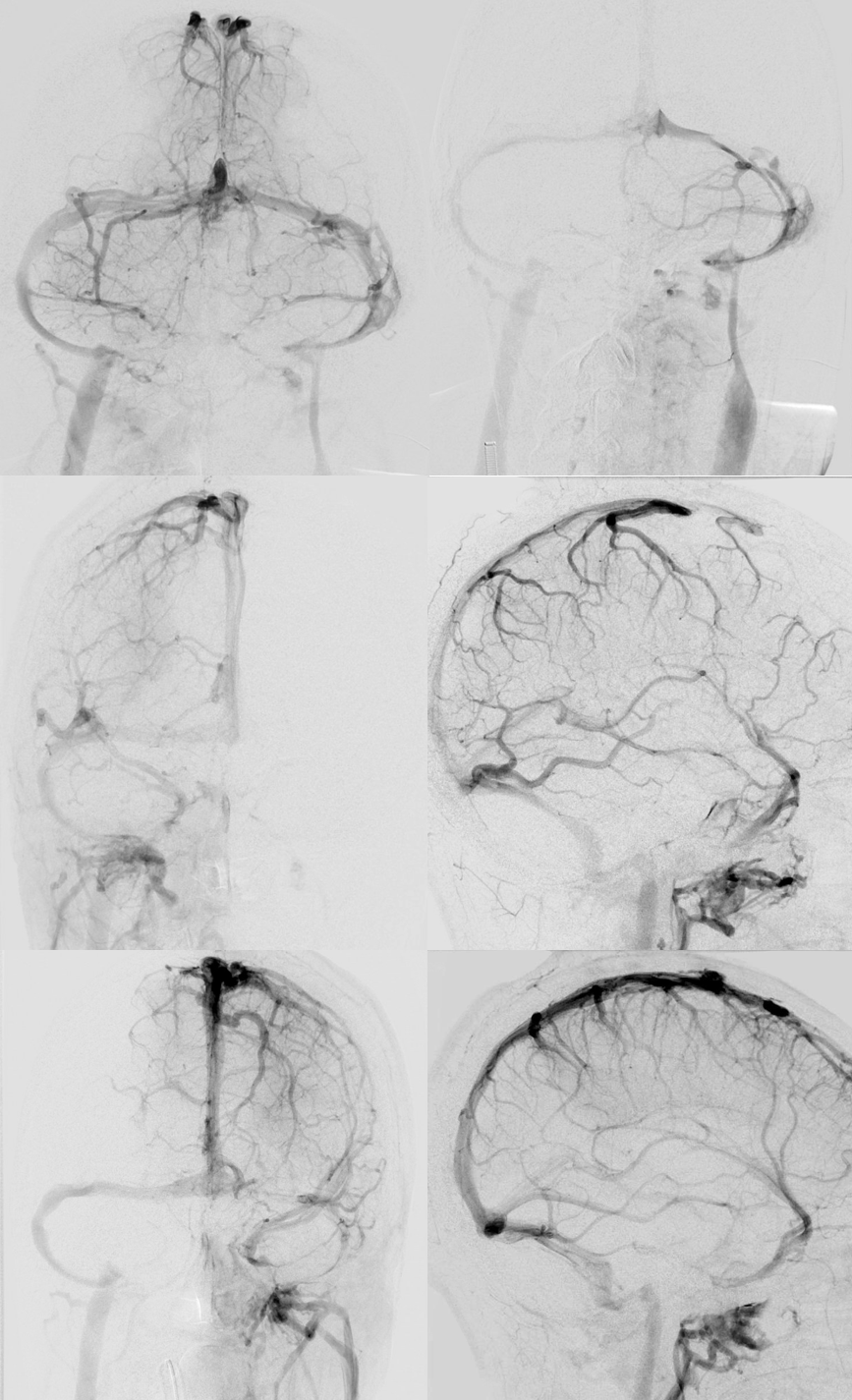
Note how much worse the sinus looks on angio than MR. Pressures are quite high. Also note lack of contralateral sinus stenosis (not thrombus, but the classic IIH narrowing). In other words, stenting the right side will not do anything.
The other important point is to note that, developmentally, the mastoid foramina are absent. So is a nameless but very common foramen at the torcular (lets call it peritorcular foramen) — see how important that can be in a case here. Unfortunately, there are none to be had.


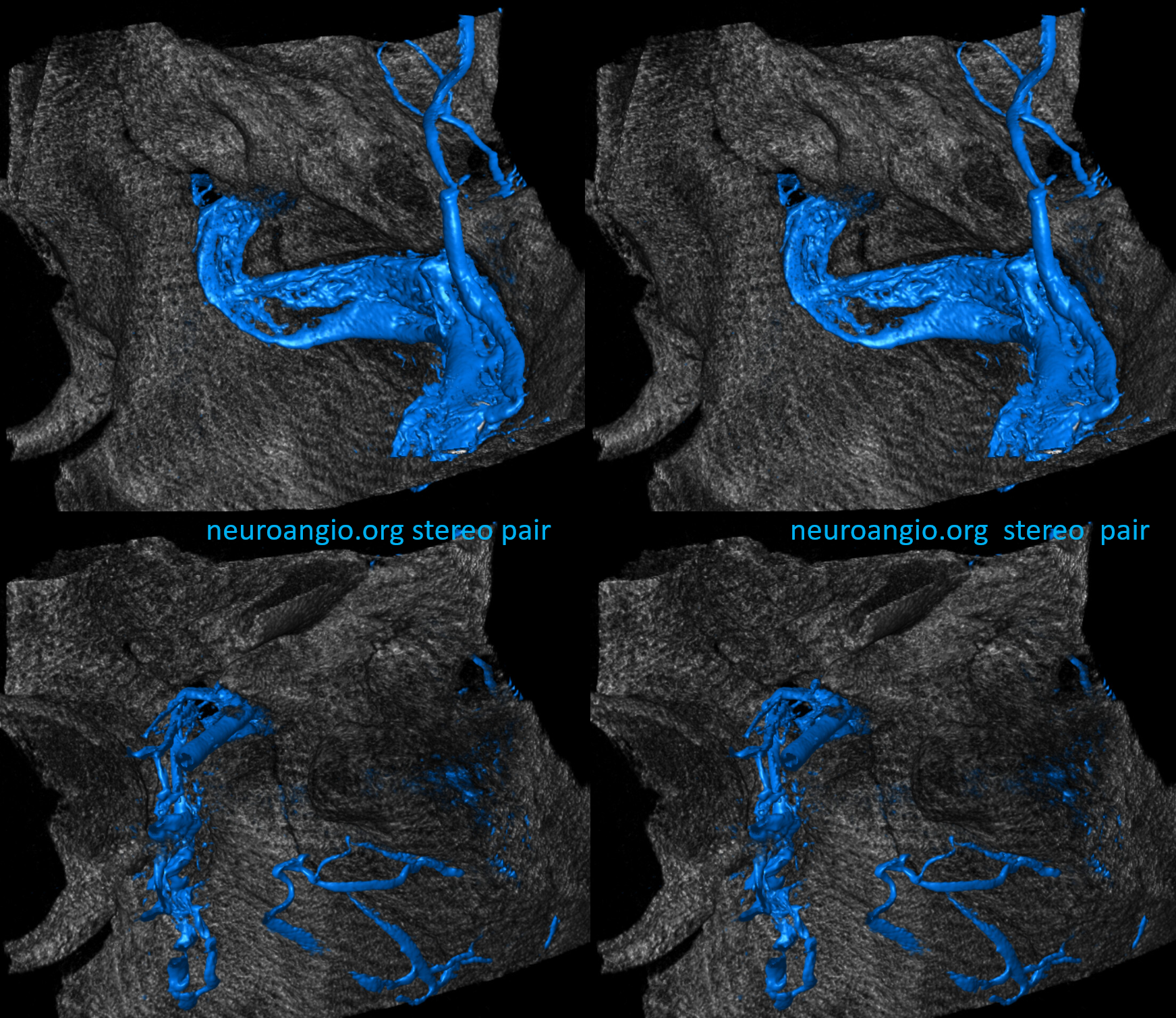
Stereo pairs VR DYNA Venous phase
One of the most important points about this case is how deceptively good contrast MRI/MRV look. This is actually quite common with subacute thrombus — it enhances. Therefore, everything in the sinus — flow and thrombus — looks white. It is important to know about this and not be fooled. The single best noninvasive study to look at venous sinuses is a CT Venogram. Not the usual choice, and usually not needed — but it is the best when there is uncertainty.
Here the best study is actually a pre-contrast T1. It shows the flow channels perfectly — even in the jugular bulb — see corresponding arrows below. Unfortunately it only works well on certain MRI machines — those where T1 is a true “black blood” sequence. For example, it does not work well on most Siemens units. GE machines do better with this.
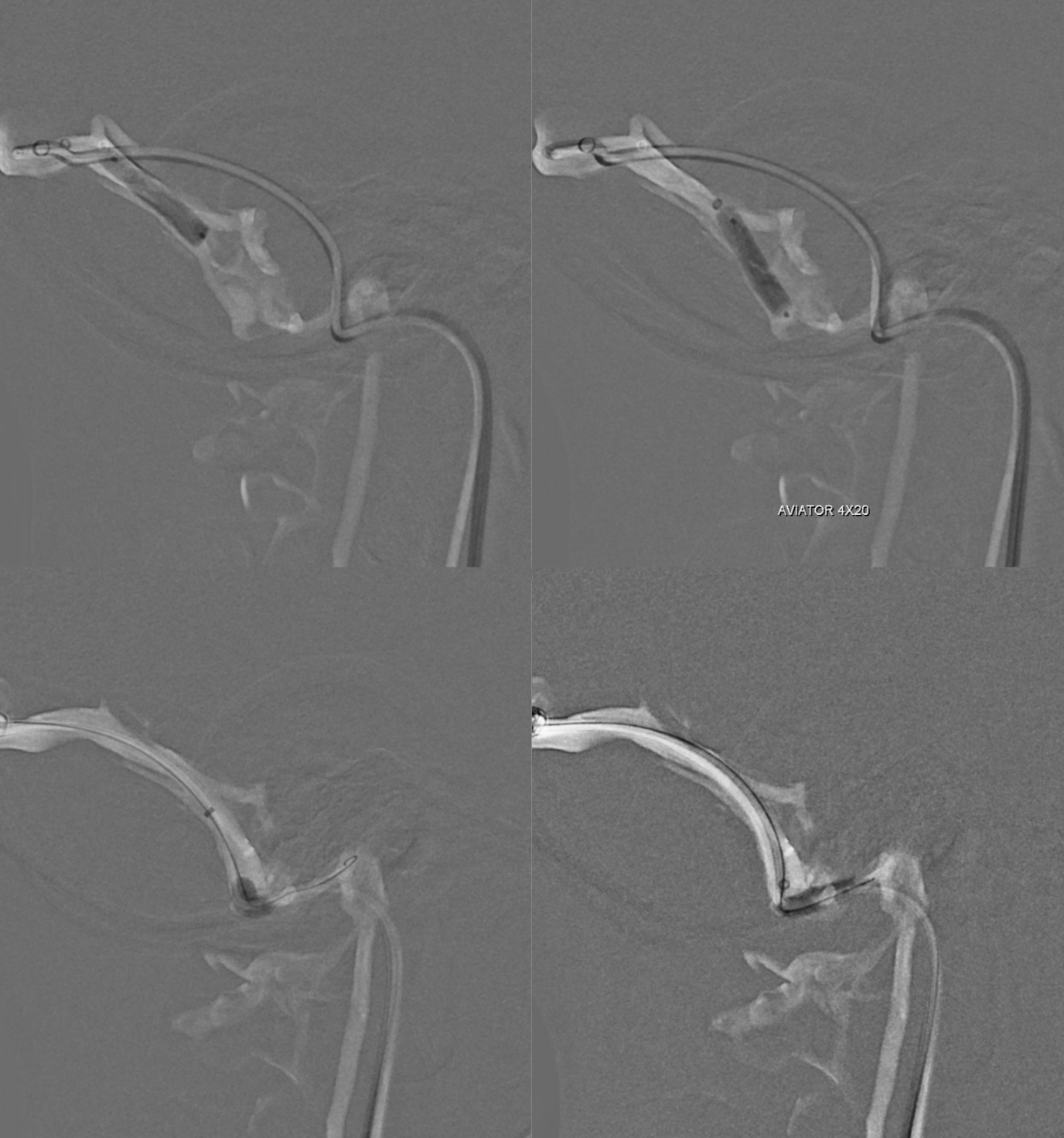
Getting through the recanalized sinus is easier said than done. Its a maze of cavernous channels inside organized thrombus/scar. Soft things do not work, and hard things must be used with care. None of it will come out with present-day aspiration or stent-trievers. Other thrombectomy tools may be explored.
We love the Offset for getting through things like chronic carotid occlusions. Here, used offset/Zoom 14 support wire, and 035 Terumo glide. These are long, painful cases to do.

Noncompliant balloon angioplasty

We were unable ot cross the bulb from above with either 14 or 35 wires or catheters. however the post venous images are improved — for example right siden now drains a bit to the left

Normally IJ angiopplasty is a not an undertaking we deem effective. However with thrombus it worked a little bit
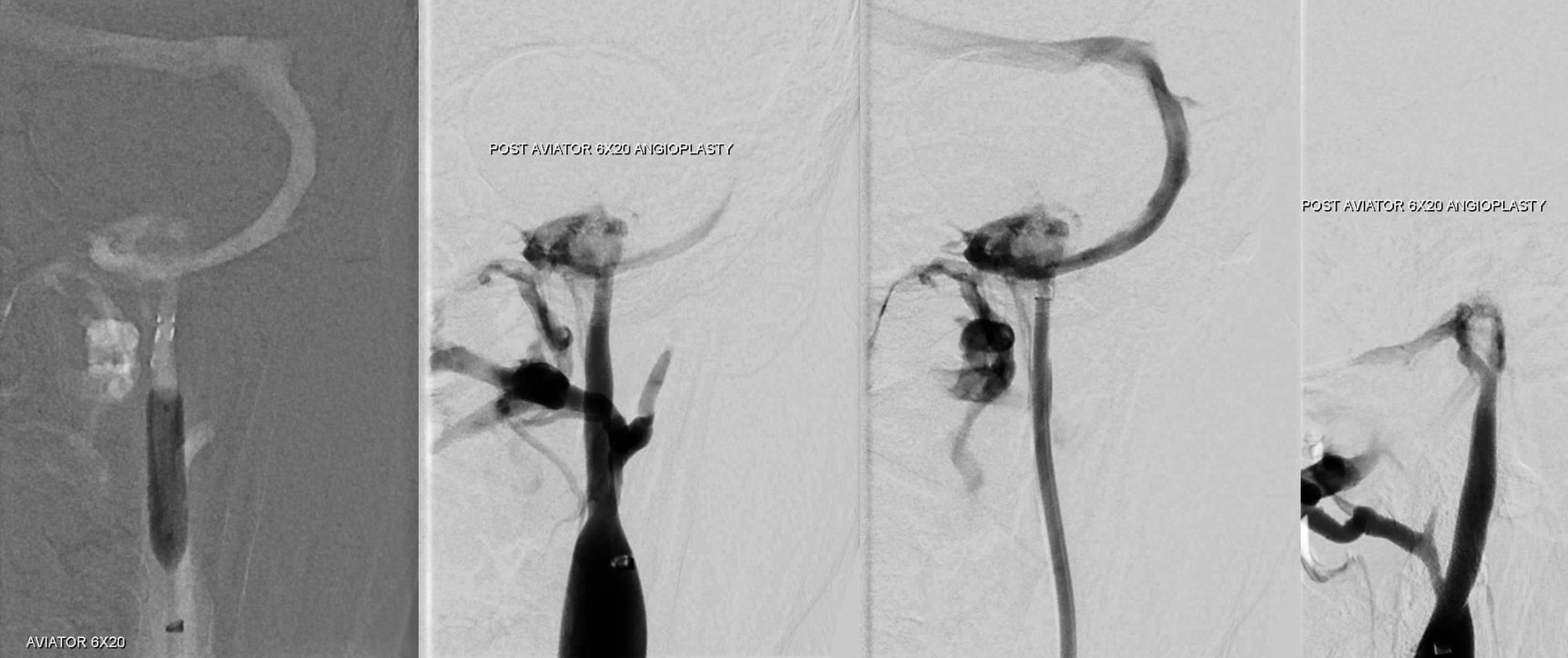
Images are better — but critically so are the venous pressures. 25 to 15 is very good. Hopefully this holds up
One of the morals of this story is that it is much easier to remove acute thrombus than deal with subacute/chronic scar. These are individual cases, and there is no standard of care either way. Acute thrombectomy is likely better. See related cases (no infection — 1 2)
