Not uncommonly, we perform thrombectomy of a more proximal occlusion to then discover that a more distal occlusion remains. Usually, this is correctly perceived to be the result of fragmentation (breakup) of the target embolus during its removal. However, that is not always the case. Tandem intracranial emboli are a real thing. HR-CBCT can show that.
This is correctly billed as a proximal right M2 occlusion. Dense MCA sign on right.
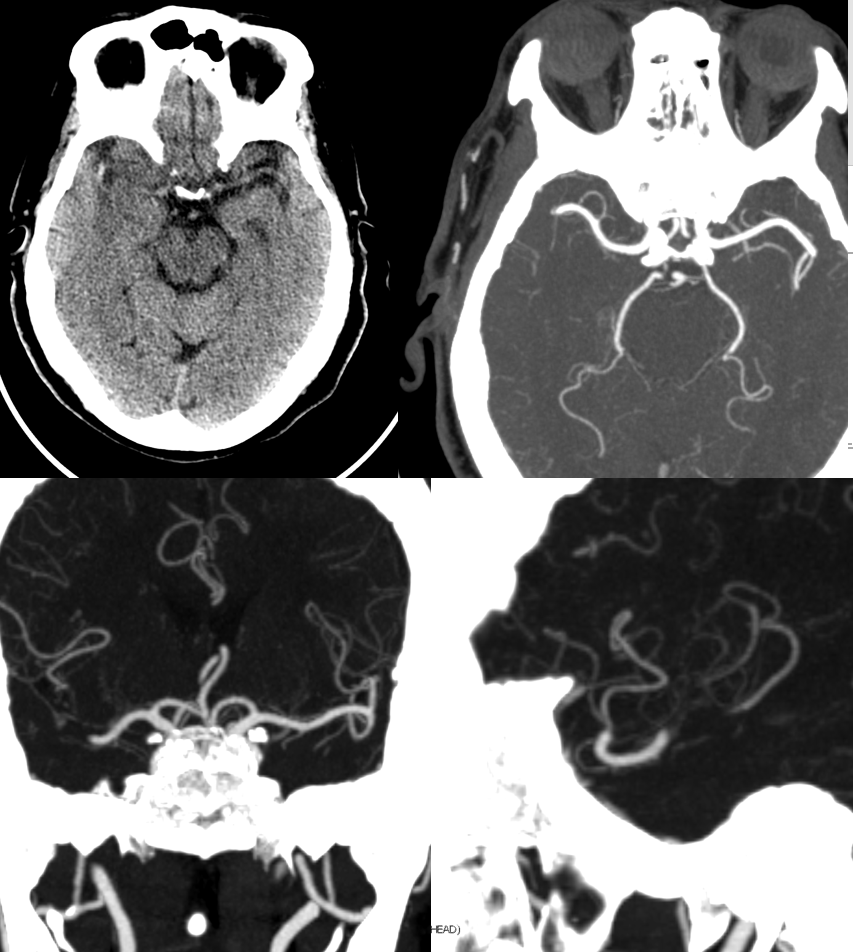
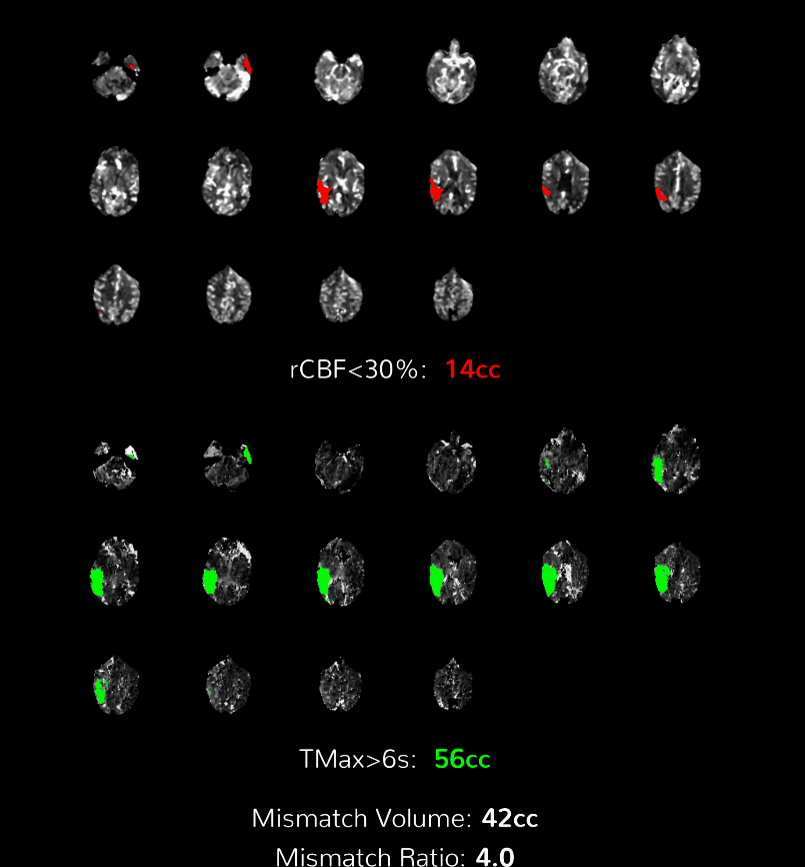
Perfusion
Angio
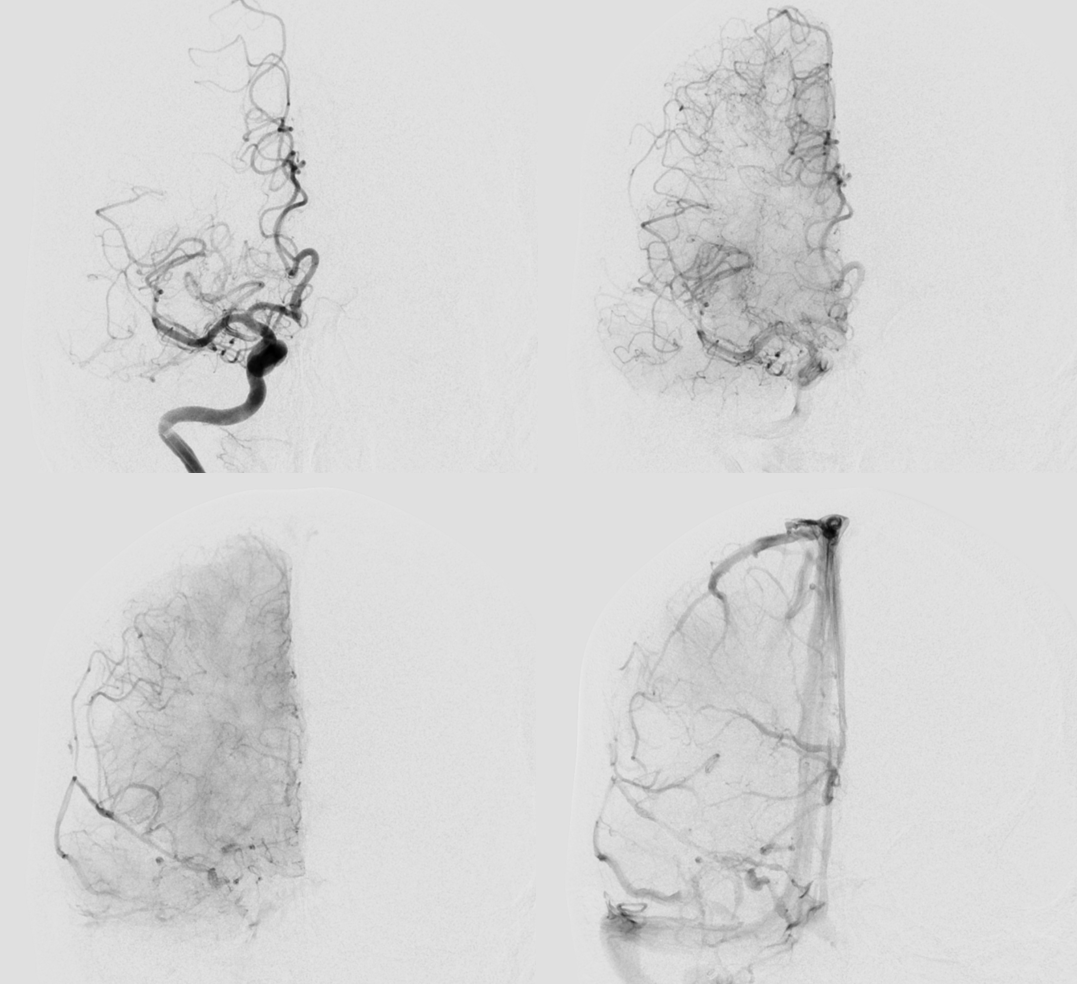
The proximal M2 occlusion is clearly visible
Lets do a dry DYNA. 20 sec 70 kEv spin, 35 cm FOV, noncontrast. Takes 3 minutes to do, including setup, acquisition, and analysis
Not much to see on source data
Reconstruction, original. See the two separate hyperdense areas?
This is definitely good enough. A secondary reconstruction in “normal” or “sharp” modes can make it a bit better, but not necessary
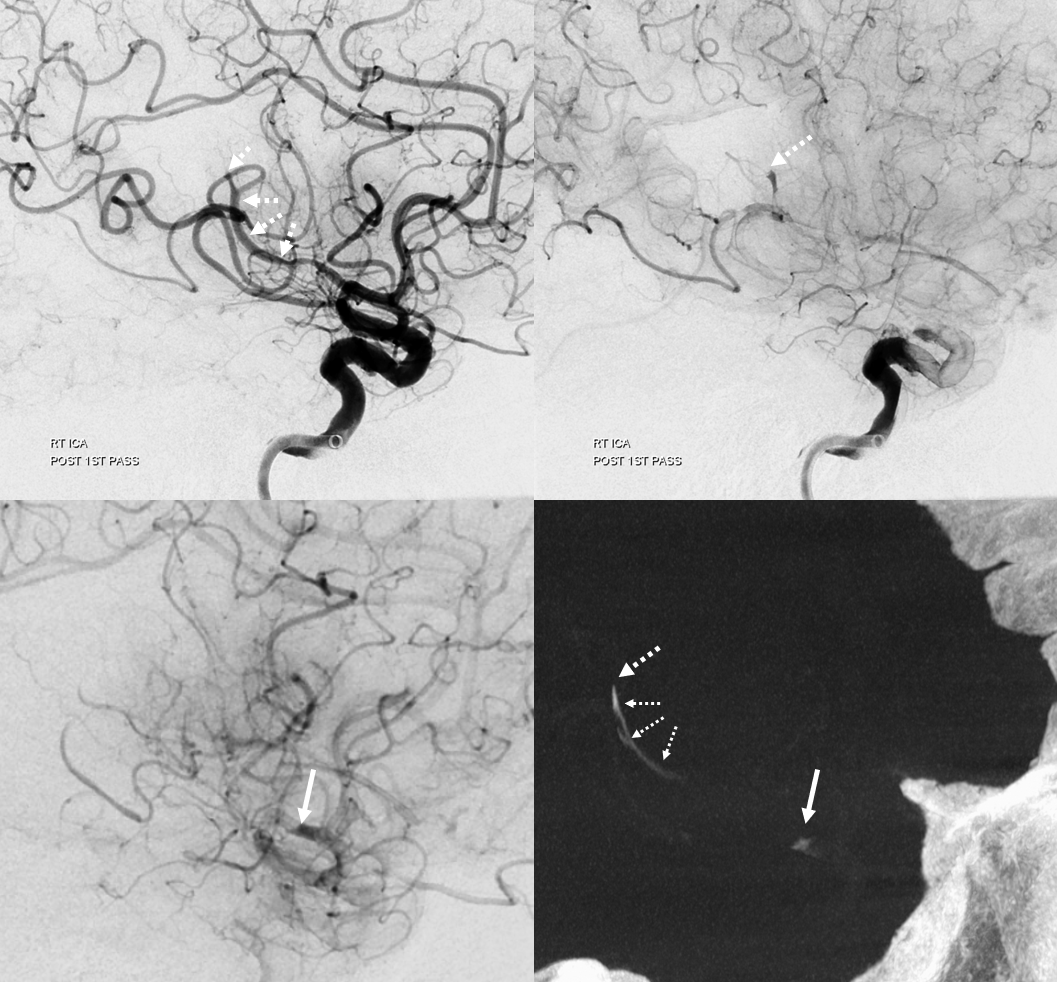
Now lets make a 3-5 mm thick MIP to see it better. We are looking at two occlusions. Each occlusion is at the distal end of the associated hyperdensity — where the contrast column stops (arrow – M2, dashed arrow — distal M2). Retrospectively one can see the distal occlusion on CTA, but not on catheter angio. Here we can definitively say that this is a tandem lesion, not a distal embolus after the upcoming proximal M2 aspiration.

Thrombectomy
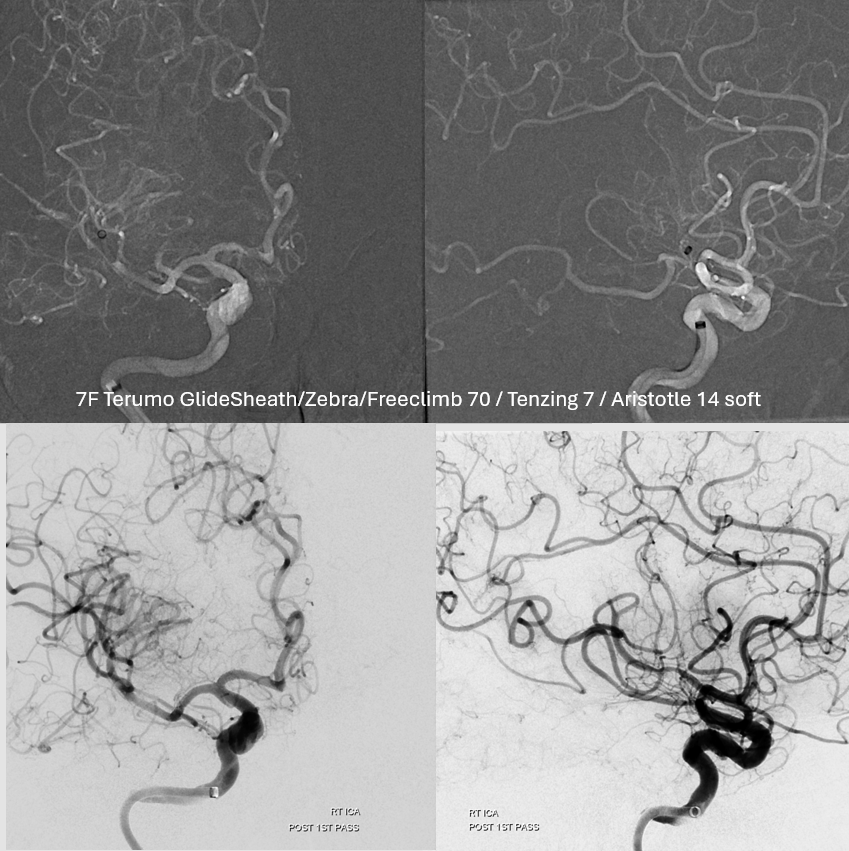
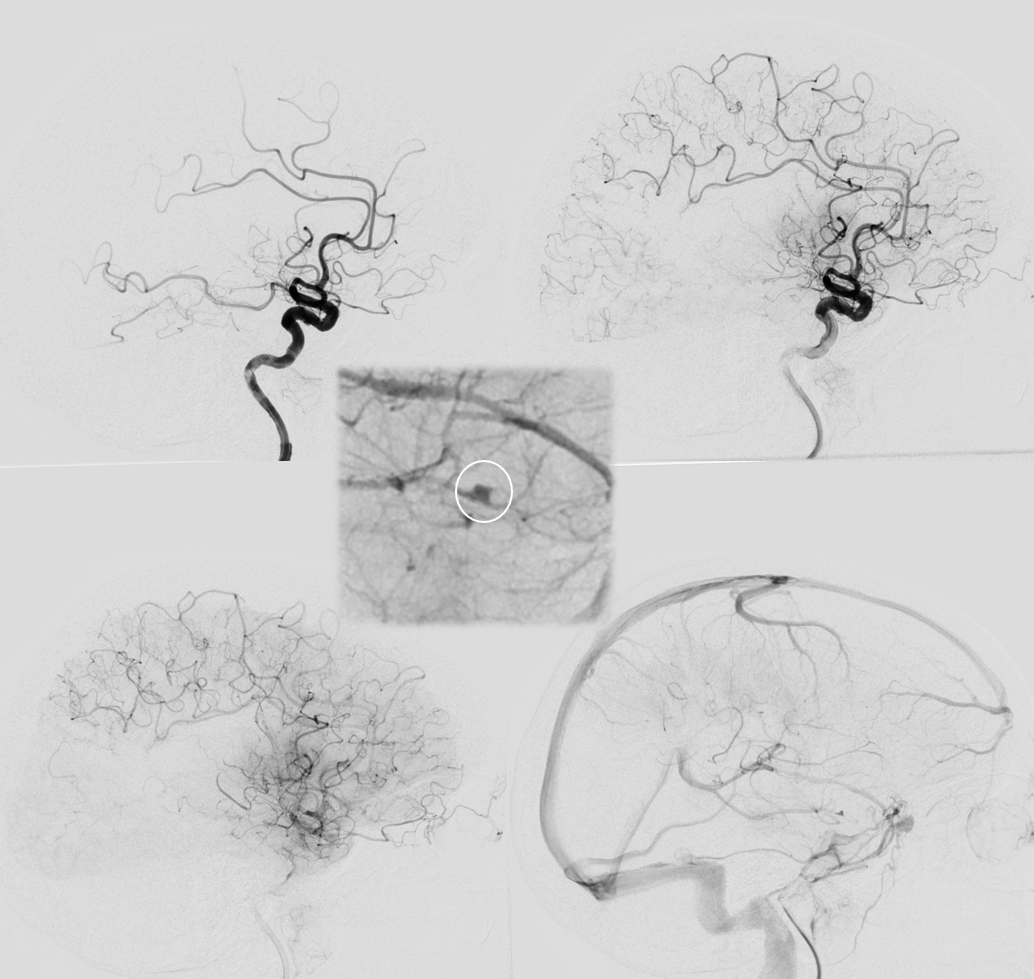
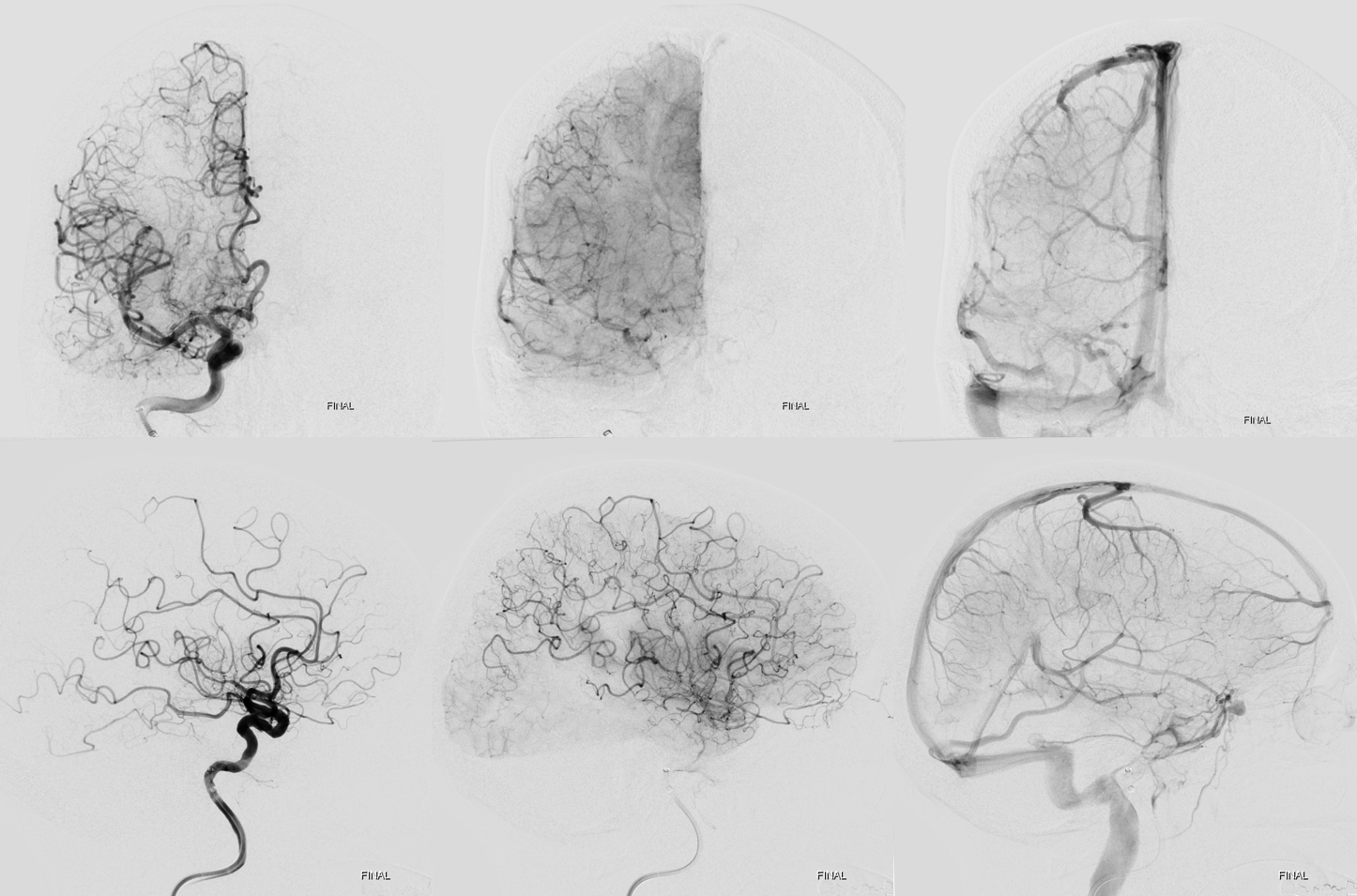
As predicted there is a second occlusion. See correlation between angios and DYNA
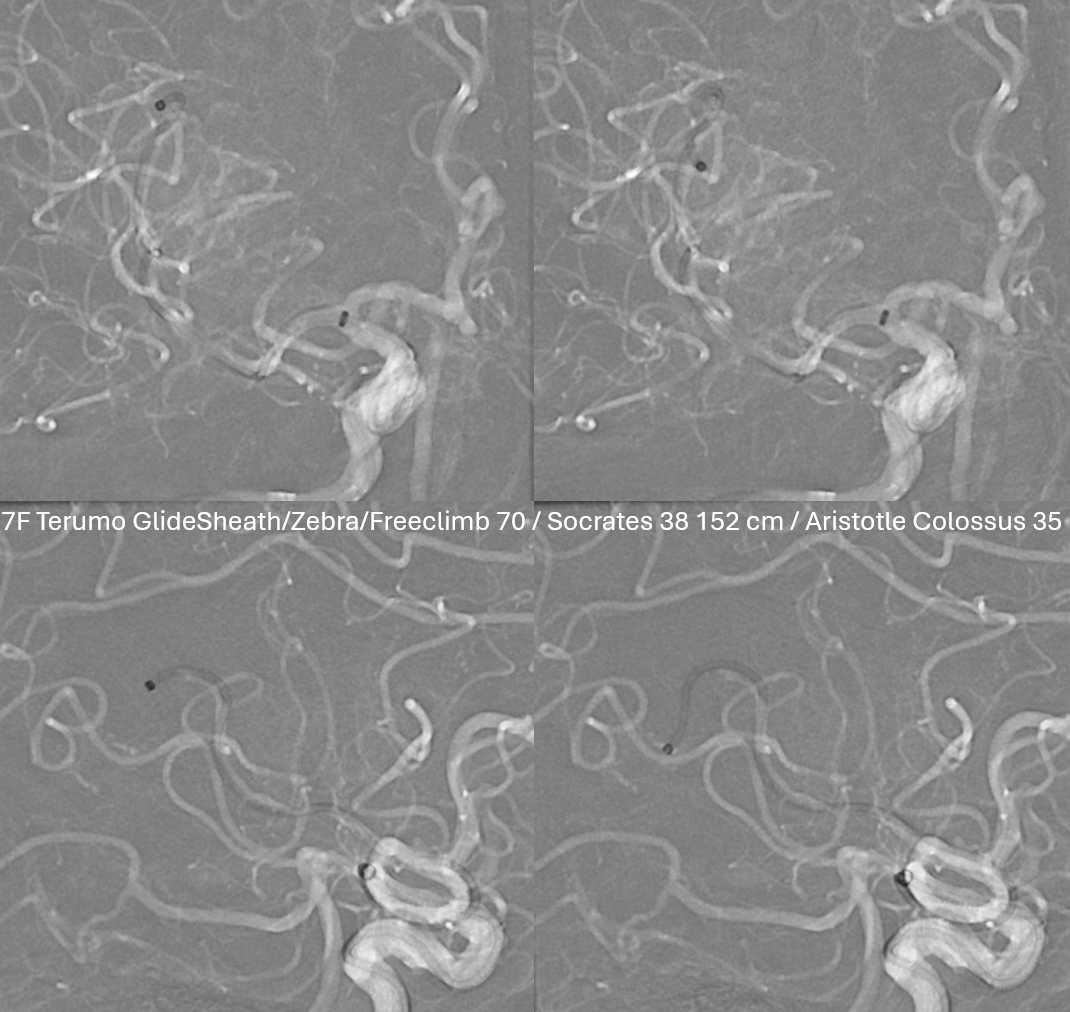
Distal (MEVO) thrombectomy
Post. There is still one branch from this area (dashed arrow) missing plus another one in the inferior division
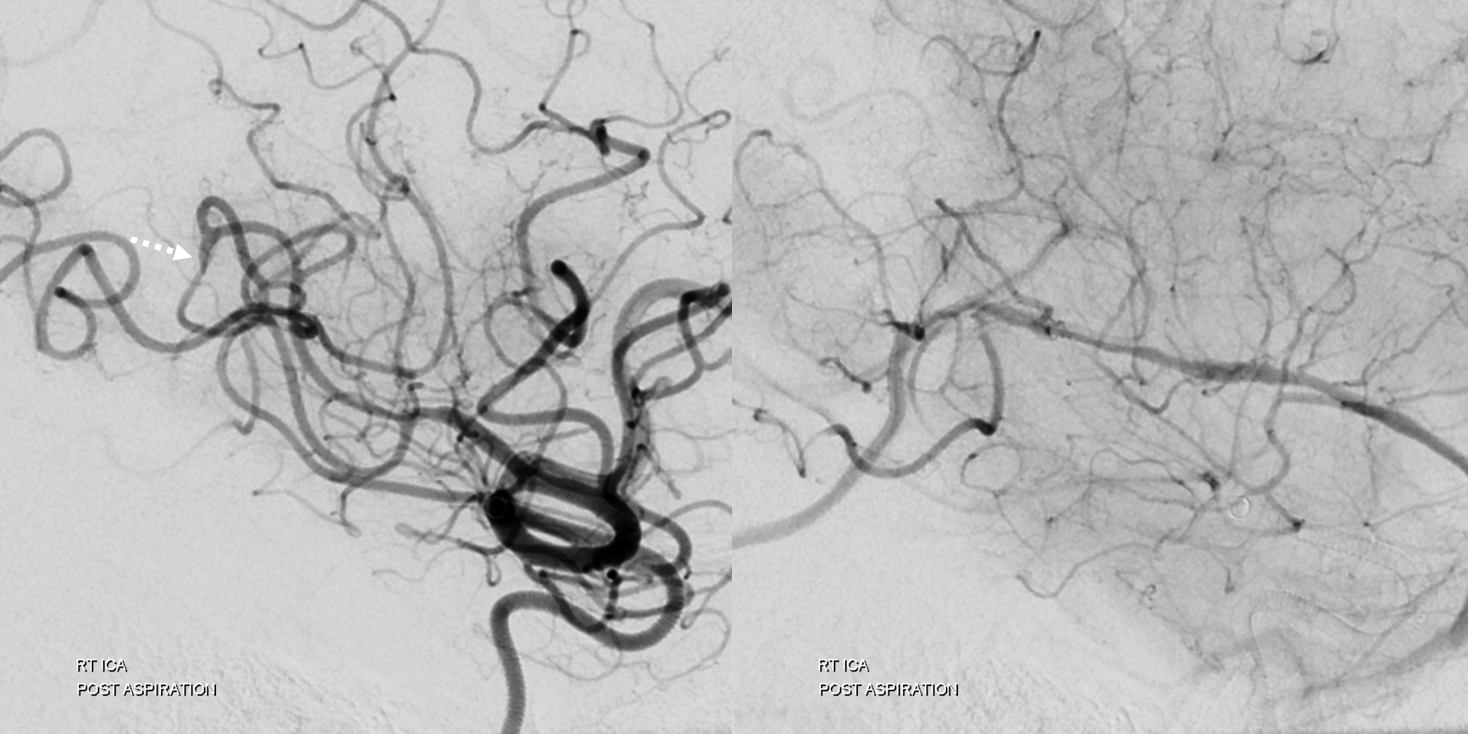
Post CT — some sylvian fissure contrast/blood. Clinically almost back to baseline.

